颈动脉支架手术步
- 格式:ppt
- 大小:5.52 MB
- 文档页数:22

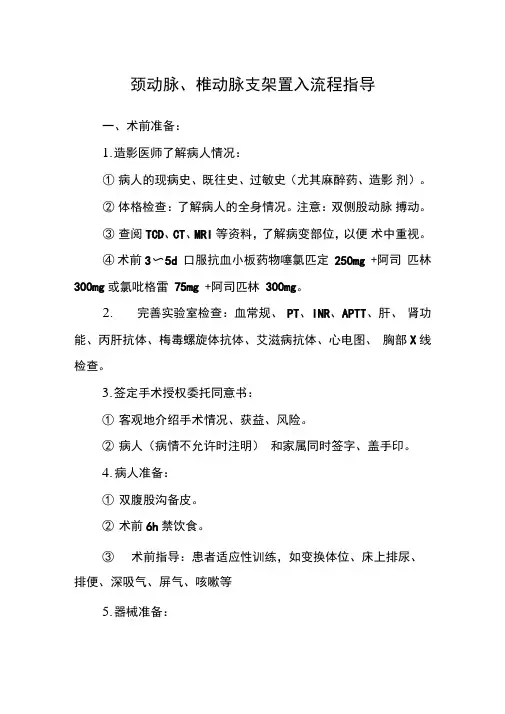
颈动脉、椎动脉支架置入流程指导一、术前准备:1.造影医师了解病人情况:①病人的现病史、既往史、过敏史(尤其麻醉药、造影剂)。
②体格检查:了解病人的全身情况。
注意:双侧股动脉搏动。
③查阅TCD、CT、MRI等资料,了解病变部位,以便术中重视。
④术前3〜5d 口服抗血小板药物噻氯匹定250mg +阿司匹林300mg或氯吡格雷75mg +阿司匹林300mg。
2.完善实验室检查:血常规、PT、INR、APTT、肝、肾功能、丙肝抗体、梅毒螺旋体抗体、艾滋病抗体、心电图、胸部X线检查。
3.签定手术授权委托同意书:①客观地介绍手术情况、获益、风险。
②病人(病情不允许时注明)和家属同时签字、盖手印。
4.病人准备:①双腹股沟备皮。
②术前6h禁饮食。
③术前指导:患者适应性训练,如变换体位、床上排尿、排便、深吸气、屏气、咳嗽等5.器械准备:6.药物准备:非离子型造影剂200ml、2%利多卡因10ml、软包0.9 %氯化钠1000ml X2、肝素钠4支、鱼精蛋白2支、0.9 %氯化钠500ml沦及常用抗过敏、降压药和抢救用药物。
7.术前用药:术前3h尼莫地平静脉微量泵3ml/h、术前30分钟鲁米那0.1肌注、碘过敏试验(术前造影剂1ml静脉注射,15min 后观察有无心慌、胸闷、皮疹等)。
静脉通道平衡盐液500ml。
二、操作程序:1.体位:病人仰卧,调整头位适宜,固定上肢,双腿稍分开并外展,接监护导联。
2.消毒:0.05%碘伏双侧腹股沟区消毒,上界平脐,下界大腿上1/3处,外界为腋中线,内界大腿内侧。
以穿刺点为中心向周围消毒两遍。
3.铺无菌单:由脐部至会阴铺第1块手术巾,第2块手术巾在穿刺点上方并与第1块垂直,第3、4块手术巾与第1、2块成45度角暴露右、左穿刺点。
4.无菌套覆盖影像增强器、操作面板和遮挡板。
5.穿手术衣,戴无菌手套,生理盐水冲洗手套,铺大手术单。
6、冲洗与抽吸:肝素盐水冲洗穿刺针、动脉鞘、泥鍬导丝、猪尾管,浸透J形导丝。
Chin J Stroke ·Volume 2.Number 5.2007【关键词】 颈动脉;支架;血管成形术颈动脉支架成形术的若干操作经验杜彬作者单位100050 北京市首都医科大学附属北京天坛医院急诊介入科通讯作者杜彬*****************颈动脉支架成形术(CAS)作为一种微创治疗方法,为某些特定颈动脉狭窄的群体提供了一种治疗方法。
CAS操作技能的高低直接影响到手术的成功率和围手术期并发症的发生率,乃至对CAS的可行性和有效性都会产生影响。
2006年意大利的一个颈动脉治疗跨学科专题小组提供了一份以循证医学为基础的专家共识[1]。
此共识建议对于具体的操作者来说,在获得了介入基本技术之后,还应具备以下条件:(1)2年内至少参与150例弓上血管手术操作(诊断或治疗),其中至少100例是作为主要术者;(2)2年内至少参与75例CAS,其中至少50例作为主要术者。
保持手术技能的最低要求,为每年作为主要术者至少需开展并记录50例颈动脉支架术。
由此可见,要想成为一名合格的手术操作者需要经过长期、系统的培训。
笔者认为CAS技能的高低与术者实践经验的丰富程度、经常使用的器材种类和对不同器材特性的了解程度等都有直接关系。
对于同一个病变,可能会有不同的处理方法,结果可能也都是好的,但最佳的处理方法一定是最简便、安全的方法,所需时间越短越好。
本文介绍CAS手术各步骤的操作过程,仅供参考。
1 术前准备加压袋包裹的软包装生理盐水(其内加入肝素500U)通过连接管与导引导管相连时,一定要注意排空连接管内和导引导管内的气泡。
加压袋的压力待气泡排空后再加到标准压力。
2 导引导管置入颈总动脉导引导管的置入是手术的第一步,也是决定手术成败的关键。
2.1 使用同轴技术放置导引导管 在导引导管(长度为90 cm)内插入导管(长度为125 cm),导管内再配以超滑导丝。
先将导丝选入颈外动脉分支远端,再在导管、导丝的协助下将导引导管送达靶病变的近心端,然后撤除导管和导丝。
颈动脉重度狭窄支架治疗适应证禁忌症一、颈动脉狭窄介入手术治疗适应症:1、症状性患者,曾在6个月内有过非致残性缺血性卒中或一过性脑缺血症状(TIA)的低中危外科手术风险患者,通过无创性成像或血管造影发现同侧颈内动脉直径狭窄超过50%,颈期围手术期卒中或死亡率小于6%;2、无症状患者,通过无创性成像或血管造影发现同侧颈内动脉直径狭窄超过70%,颈期围手术期卒中或死亡率小于3%;3、对于颈部解剖不利于CEA外科手术的患者应选择CAS,而不使用CEA。
4、对于TIA或轻卒中患者,如果没有早期血管重建术的禁忌证,可以在事件出现2周内进行干预。
对于大面积脑梗塞保留部分神经功能患者,应在梗塞至少2周后再进行CAS治疗。
5、CEA术后再狭窄,症状性或无症状性狭窄大于70%。
6、CEA高危患者:年龄大于80岁;心排血量低(EF<30%);未治疗或控制不良的心律失常;心功能不全;近期心梗病史;不稳定心绞痛;严重COPD;对侧颈动脉闭塞;串联病变;颈动脉夹层;假性动脉瘤等。
7、急诊患者,如假性动脉瘤;急性颈动脉夹层;外伤性颈动脉出血。
8、颈动脉血管重建术不推荐应用于已有严重残疾的脑梗死患者中。
二、颈动脉狭窄介入手术治疗禁忌症:绝对禁忌证:无症状颈动脉慢性完全性闭塞。
相对禁忌证:(1)3个月内有颅内出血;(2)伴有颅内动脉瘤,并且不能提前或同时处理者;(3)2周内曾发生心肌梗死或较大范围脑梗死;(4)胃肠道疾病伴有活动性出血者;(5)难以控制的高血压;(6)对肝素、阿司匹林或其他抗血小板类药物有禁忌者;(7)对造影剂或所使用的材料或器材过敏者;(8)有严重心、肝、肾、肺疾病;(9)血管迂曲或变异,导管或支架等输送系统难以通过;(10)血管病变广泛或狭窄范围过大;(11)血管炎性狭窄,广泛的血管结构异常;三、颈动脉狭窄介入手术治疗可能的并发症或不良反应包括穿刺点的并发症,栓塞、血栓形成和高灌注脑出血造成的神经功能障碍,心动过缓、低血压、血管损伤和支架内血栓形成;病变处血管、操作路径血管及远端血管的损伤,心血管事件及死亡,支架内再狭窄等;导管、导丝断裂及所致并发症;造影剂过敏;穿刺点血肿、瘀斑、假性动脉瘤或夹层;下肢深静脉血栓形成。
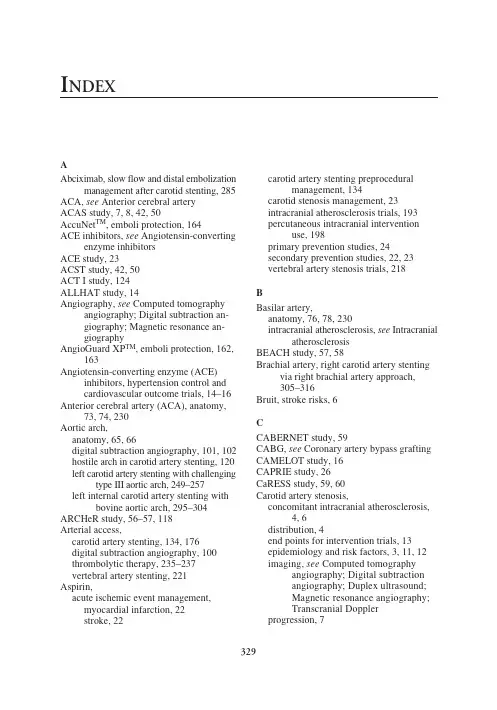
I NDEX329AAbciximab, slow flow and distal embolizationmanagement after carotid stenting, 285ACA,see Anterior cerebral artery ACAS study, 7, 8, 42, 50AccuNet TM , emboli protection, 164ACE inhibitors, see Angiotensin-convertingenzyme inhibitors ACE study, 23ACST study, 42, 50ACT I study, 124ALLHAT study, 14Angiography,see Computed tomographyangiography; Digital subtraction an-giography; Magnetic resonance an-giographyAngioGuard XP TM , emboli protection, 162,163Angiotensin-converting enzyme (ACE)inhibitors, hypertension control and cardiovascular outcome trials, 14–16Anterior cerebral artery (ACA), anatomy,73, 74, 230Aortic arch,anatomy, 65, 66digital subtraction angiography, 101, 102hostile arch in carotid artery stenting, 120left carotid artery stenting with challengingtype III aortic arch, 249–257left internal carotid artery stenting withbovine aortic arch, 295–304ARCHeR study, 56–57, 118Arterial access,carotid artery stenting, 134, 176digital subtraction angiography, 100thrombolytic therapy, 235–237vertebral artery stenting, 221Aspirin,acute ischemic event management,myocardial infarction, 22stroke, 22carotid artery stenting preproceduralmanagement, 134carotid stenosis management, 23intracranial atherosclerosis trials, 193percutaneous intracranial interventionuse, 198primary prevention studies, 24secondary prevention studies, 22, 23vertebral artery stenosis trials, 218BBasilar artery,anatomy, 76, 78, 230intracranial atherosclerosis, see IntracranialatherosclerosisBEACH study, 57, 58Brachial artery, right carotid artery stentingvia right brachial artery approach,305–316Bruit, stroke risks, 6CCABERNET study, 59CABG,see Coronary artery bypass grafting CAMELOT study, 16CAPRIE study, 26CaRESS study, 59, 60Carotid artery stenosis,concomitant intracranial atherosclerosis,4, 6distribution, 4end points for intervention trials, 13epidemiology and risk factors, 3, 11, 12imaging,see Computed tomographyangiography; Digital subtraction angiography; Duplex ultrasound;Magnetic resonance angiography;Transcranial Doppler progression, 7330Carotid artery stenting (CAS),angiography, 124, 136, 143, 144anticoagulation, 134approaches,direct guide approach, 137guide approach, 136, 137selection of approach, 136sheath approach, 137arterial access, 134balloons,technique,postdilatation, 143predilatation, 140types, 152bilateral carotid stenosis patients, 145, 146 carotid endarterectomy comparative trials, CAVATAS study, 54overview, 53, 115–118SAPPHIRE study, 55, 118WallStent Trial, 53, 54case studies,carotid endarterectomy patch restenosisand aneurysm, 275–282internal carotid artery with string sign,265–273left carotid artery stenting withchallenging type III aortic arch,249–257left internal carotid artery stenting withbovine aortic arch, 295–304 right carotid artery stenting via rightbrachial artery approach, 305–316 slow flow and distal embolizationmanagement, 283–287tortuous left internal carotid arterystenting, 259–263catheters,diagnostic catheters, 149guide catheters, 149, 150complications,acute vessel closure, 181arterial access, 176catheterization, 177cerebral ischemia, 178, 179distal cerebral embolization, 179, 180emboli protection devices, 177, 178hyperperfusion syndrome, 182, 184late distal embolization, 184overview, 118, 175, 176reflex bradycardia and hypotension,181restenosis in stent, 185, 186retinal embolization, 180, 181stent deformation, 184stent thrombosis, 184emboli protection device,deployment, 138–140filter devices,AccuNet TM, 164AngioGuard XP TM, 162, 163design, 161, 162EmboShield TM, 164, 165FilterWire EZ TM, 166GuardWire TM for distal balloon occlusion protection, 169Interceptor® PLUS, 166, 168overview of types, 137, 138proximal balloon occlusion emboliprotection devices, 169–171 removal, 143Rubicon Embolic Filter, 168Spider TM, 166trials, 55, 56, 118, 159, 160meta-analysis of trials, 59, 60operator competency, 114, 115, 131–133 patient selection, 111–113, 118, 120–123, 131, 133peripheral guidewires,flexible guidewires, 148hydrophilic guidewires, 148, 149stiff guidewires, 149 postprocedural monitoring,duplex ultrasound, 145follow-up, 145hemodynamic monitoring, 144, 145medications, 145neurological assessment, 145 preprocedural management,antiplatelet therapy, 134neurological assessment, 133noninvasive imaging, 133 prognostic factors, 118, 120–123 prospects, 123, 124registries,ARCHeR, 56–57, 118BEACH, 57, 58CABERNET, 59global carotid artery stent registry, 60MAVeRIC, 59SECURITY, 58, 118sheaths, 151stents,placement, 140, 143RX AccuLink TM, 156331self-expanding stents, 152, 153, 156, 157Xact®, 157trends in United States, 60, 61Carotid endarterectomy (CEA),anesthesia, 34, 38carotid artery stenting comparison trials, see Carotid artery stentingclamping and shunting, 35, 38, 39clinical trials,asymptomatic carotid stenosis, 41, 42,48, 50symptomatic carotid stenosis, 40, 41, 50 closure, 36, 38complications, 39, 53, 118contraindications, 44, 51, 52endarterectomy, 36historical perspective, 33, 34, 48, 113incision and dissection, 34, 35indications, 44, 50, 51, 113, 114outcome factors, 38, 39stenting in patch restenosis and aneurysm, 275–282CAS,see Carotid artery stenting CASANOVA study, 41CAST study, 22CATS study, 25CAVATAS study, 54CCA,see Common carotid arteryCEA,see Carotid endarterectomy Cilostazol, intracranial atherosclerosis trials, 193Circle of Willis, anatomy, 81, 230 Clopidogrel,carotid artery stenting preproceduralmanagement, 134percutaneous intracranial intervention use, 198secondary prevention studies, 26, 27 Common carotid artery (CCA),anatomy, 69carotid artery stenting considerations, 120 origins, 65, 69Computed tomography angiography (CTA), carotid artery stenting follow-up, 90image processing, 88, 89limitations, 90resolution, 88vertebral artery stenosis, 215Coronary artery bypass grafting (CABG), stroke risks with carotid artery stenosis, 9 Coronary artery disease, carotid artery stenosis association, 6, 7, 9, 118CREST study, 124CTA,see Computed tomography angiography CURE study, 26DDCCT study, 20Diabetes,carotid artery stenosis risks, 20, 21management, 21Digital subtraction angiography (DSA), aortic arch angiogram, 101, 102arterial access, 100complications, 108, 109contrast agent, 100duplex ultrasound comparison studies, 87, 88 heparin anticoagulation, 100indications, 99, 100nonselective vertebral artery angiography, 104–106reverse-curved catheters, 106, 108selective carotid angiography, 102–104vertebral artery stenosis, 217, 218views, 101Dipyridamole, secondary prevention studies, 24, 25DSA,see Digital subtraction angiography Duplex ultrasound (DUS),bilateral carotid stenosis, 85–87carotid artery stenting follow-up, 87digital subtraction angiography compari-son studies, 87, 88intimal–medial thickness measurement,87limitations, 84, 85modes, 84recommendations, 85Duplex ultrasound, vertebral artery stenosis, 213, 214DUS,see Duplex ultrasoundEECA,see External carotid arteryECST study, 17, 41Emboli protection device (EPD),clinical trials, 55, 56, 118, 159, 160complications, 177, 178deployment, 138–140filter devices,AccuNet TM, 164AngioGuard XP TM, 162, 163design, 161, 162EmboShield TM, 164, 165332FilterWire EZ TM, 166Interceptor® PLUS, 166, 168Rubicon Embolic Filter, 168Spider TM, 166GuardWire TM for distal balloon occlusion protection, 169overview of types, 137, 138proximal balloon occlusion emboliprotection devices, 169–171 removal, 143Emboli protection device, vertebral artery stenting, 223EmboShield TM, emboli protection, 164, 165 EPD, see Emboli protection deviceESPS-2 study, 24, 25EUROPA study, 15EVA-3S study, 55External carotid artery (ECA), anatomy,70, 71FFilterWire EX TM, left carotid artery stenting with challenging type III aortic arch,251FilterWire EZ TM,emboli protection, 166innominate artery interventions, 323right carotid artery stenting via rightbrachial artery approach, 310GGemfibrozil, hyperlipidemia control, 20 Gooseneck, mechanical embolectomy, 241, 242, 294GuardWire TM, emboli protection, 169HHOPE study, 14, 15HPS trial, 19Hyperlipidemia,carotid artery stenosis risks, 11, 12, 17control,gemfibrozil, 20statins, 18–20stroke risks, 17, 18Hyperperfusion syndrome,carotid artery stenting complication,182, 184carotid endarterectomy association,121, 122vertebral artery stenting, 225 Hypertension,carotid artery stenosis risks, 11, 12control,angiotensin-converting enzymeinhibitors, 14–16carotid stenosis patient trials, 17comparative trials, 14goals, 16, 17stroke risks, 13, 14IICA,see Internal carotid arteryIMT,see Intimal–medial thickness Innominate artery, ostial stenosis andpercutaneous intervention case study, diagnosis and angiographic findings, 318, 321difficulty, 321, 322history, 317, 318postintervention course, 323technique, 323Interceptor® PLUS, emboli protection, 166, 168Internal carotid artery (ICA),anatomy, 71–73, 230intracranial atherosclerosis, see Intracranial atherosclerosisstenting,considerations, 120, 121left internal carotid artery stenting withbovine aortic arch, 295–304 string sign case study, 265–273tortuous left internal carotid artery,259–263Intimal–medial thickness (IMT),duplex ultrasound, 87prognostic value of carotid evaluation, 6 Intraarterial thrombolysis, see Thrombolytic therapyIntracranial atherosclerosis,antithrombotic therapy, 193bypass surgery, 193cilostazol trials, 193distribution, 190, 192epidemiology, 190natural history, 192percutaneous intervention,angioplasty, 205antithrombotic therapy, 198, 199arch aortography, 199guide/sheath delivery, 199, 201historical perspective, 193, 194lesion wiring, 201, 203, 204outcomes, 194–196, 198333postprocedural care, 207sedation, 198stenting technique, 205–207vertebral artery stenting, 222, 223 stroke risks, 189MMagnetic resonance angiography (MRA), limitations, 91techniques, 90, 91vertebral artery stenosis, 215MATCH study, 26, 27MAVeRIC study, 59MCA,see Middle cerebral artery Mechanical embolectomy,devices, 241, 242limitations, 242thrombolysis adjunct, 294Mechanical Embolus Removal in Cerebral Ischemia (MERCI), mechanicalembolectomy, 241MERCI,see Mechanical Embolus Removal in Cerebral IschemiaMiddle cerebral artery (MCA),anatomy, 73, 230intracranial atherosclerosis, see Intracranial atherosclerosisMO.MA system, emboli protection device, 170, 171MRA,see Magnetic resonance angiography Myocardial infarction, aspirin management, 22NNASCET study, 17, 39, 41, 42, 48, 50, 53, 118PPCA,see Posterior cerebral arteryPEACE study, 15, 16Peripheral arterial disease, carotid artery stenosis association, 6, 7Posterior cerebral artery (PCA), anatomy, 80, 81, 230Posterior circulation, embolism and syndromes, 211, 212PROACT II study, 232RReflex bradycardia, carotid artery stenting complication, 181Retinal embolization, carotid artery stenting complication, 180, 181Rubicon Embolic Filter, emboli protection, 168RX AccuLink TM, carotid artery stenting, 156 SSALT study, 22SAPPHIRE study, 55, 118SECURITY study, 58, 118Smoking,carotid artery stenosis risks, 12, 21cessation, 21Spider TM, emboli protection, 166 SSYLVIA study, 219Statins,hyperlipidemia control, 18–20neuroprotective effects after acute stroke, 20Stenting,see Carotid artery stenting; Intracranial atherosclerosis; Vertebral arteries Stroke,aspirin management, 22carotid bruit association, 6economic burden, 4embolism origins, 211etiology, 4, 231intracranial atherosclerosis risks, 189prevalence, 4, 229risk factors,carotid artery stenosis, 7–9hyperlipidemia, 17, 18hypertension, 13, 14secondary prevention studies,clopidogrel, 26, 27dipyridamole, 24, 25ticlopidine, 25warfarin, 27statin neuroprotective effects, 20treatment,see Mechanical embolectomy;Thrombolytic therapy Subclavian artery, anatomy, 68, 69TTCD,see Transcranial Doppler Thrombolytic therapy,indications and contraindications, 233,234intracranial hemorrhage, 244patient selection, 232, 233percutaneous intervention,adjunctive pharmacotherapy, 239angiography, 234, 235arterial access, 235–237334case study, 289–294clot disruption, 239–241periprocedural medical management,243, 244recanalization technique, 237, 238 PROACT protocol, 232Ticlopidine, secondary prevention studies, 25 TNT study, 19Transcranial Doppler (TCD),limitations, 94microembolic signals, 93, 94principles, 91–93sensitivity and specificity by artery, 93transcranial color-coded duplexsonography, 94, 95UUKPDS trial, 21Ultrasonography,see Duplex ultrasound;Transcranial DopplerVVALUE study, 16Vertebral arteries,anatomy, 76, 212, 213, 230digital subtraction angiography, 104–106 intracranial atherosclerosis, see Intracranial atherosclerosisposterior circulation symptoms, 212stenosis,diagnosis,computed tomography angiography,215digital subtraction angiography,217, 218duplex ultrasound, 213, 214magnetic resonance angiography,215medical treatment, 218surgical management, 218, 219 stenting,arterial access, 221complications,distal embolization, 224, 225hyperperfusion syndrome, 225restenosis in stent, 225spasm, 223, 224stroke, 225emboli protection devices, 223extracranial stenting technique, 221,222indications, 219, 220intracranial stenting technique, 222,223outcomes, 219postprocedural care, 225preoperative preparation, 220prospects, 225, 226WWallStent Trial, 53, 54Warfarin,intracranial atherosclerosis trials, 193secondary prevention studies, 27vertebral artery stenosis trials, 218 WARSS trial, 27WASID study, 193, 218XXact®, carotid artery stenting, 157。
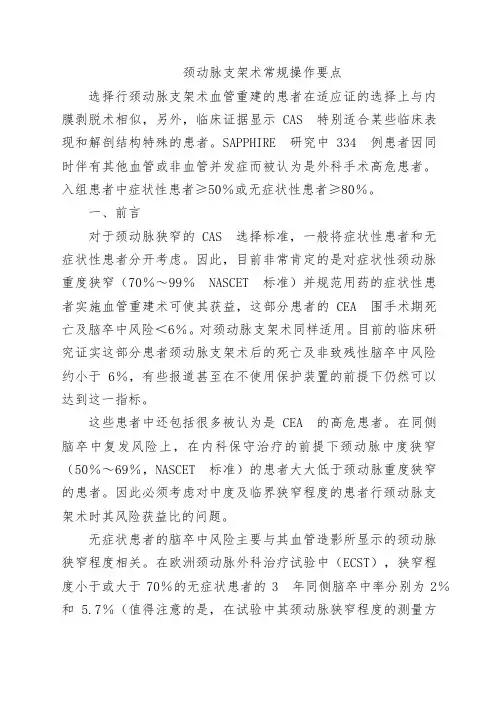
颈动脉支架术常规操作要点选择行颈动脉支架术血管重建的患者在适应证的选择上与内膜剥脱术相似,另外,临床证据显示CAS 特别适合某些临床表现和解剖结构特殊的患者。
SAPPHIRE 研究中334 例患者因同时伴有其他血管或非血管并发症而被认为是外科手术高危患者。
入组患者中症状性患者≥50%或无症状性患者≥80%。
一、前言对于颈动脉狭窄的CAS 选择标准,一般将症状性患者和无症状性患者分开考虑。
因此,目前非常肯定的是对症状性颈动脉重度狭窄(70%~99%NASCET 标准)并规范用药的症状性患者实施血管重建术可使其获益,这部分患者的CEA 围手术期死亡及脑卒中风险<6%。
对颈动脉支架术同样适用。
目前的临床研究证实这部分患者颈动脉支架术后的死亡及非致残性脑卒中风险约小于6%,有些报道甚至在不使用保护装置的前提下仍然可以达到这一指标。
这些患者中还包括很多被认为是CEA 的高危患者。
在同侧脑卒中复发风险上,在内科保守治疗的前提下颈动脉中度狭窄(50%~69%,NASCET 标准)的患者大大低于颈动脉重度狭窄的患者。
因此必须考虑对中度及临界狭窄程度的患者行颈动脉支架术时其风险获益比的问题。
无症状患者的脑卒中风险主要与其血管造影所显示的颈动脉狭窄程度相关。
在欧洲颈动脉外科治疗试验中(ECST),狭窄程度小于或大于70%的无症状患者的3 年同侧脑卒中率分别为2%和 5.7%(值得注意的是,在试验中其颈动脉狭窄程度的测量方法是不同的,导致了同样的病变用ECST 测量的狭窄程度大于用NASCET 方法测量出的狭窄程度)。
在ACAS 试验及ACST 试验中药物治疗的患者,其5 年死亡及同侧脑卒中风险为12%。
因此,为使无症状颈动脉重度狭窄的人获益,其围手术期病死率及术后脑卒中风险不能超过3%,在扩展对于无症状颈动脉重度狭窄患者行支架术的适应证前,也应该达到这一目标。
由于颈动脉中度狭窄(<60%)的无症状患者其脑血管事件发生率很低,还没有数据表明血管成形术可改善其长期的预后,而规范内科治疗可做到。
颈动脉支架置入术常规操作流程颈动脉支架置入术常规操作流程步骤一、选择入路:常规选择股动脉入路,股动脉穿刺置8F动脉鞘。
步骤二、导引导管到位:1.选择导管、导丝:根据主动脉弓的分型、颈总动脉迂曲程度和颈总动脉血管壁的斑块情况选择导引导管。
2.准备:冲洗,8F导引导管尾端连接Y阀+三通+加压滴注,泥鳅导丝经Y阀尾端插入导引导管,泥鳅导丝不出头,打开滴注持续冲洗。
3.置入:导引导管进入动脉鞘后进造影导丝20cm左右,透视下将导引导管头端送至升主动脉远端。
导丝回撤到导管内,翻转导管头回撤,弹入无名动脉(或左颈内动脉)。
固定导管,出导丝,泥鳅导丝在动脉腔内摆动前行,头端置于颈外动脉主干。
固定泥鳅导丝,沿导丝送导引导管头端至颈总动脉距离病变近侧约2cm处。
导引导管头端轴线要与颈总动脉的走行轴线平行,避免直接抵住血管壁,避开颈总动脉的动脉粥样硬化斑块。
步骤三、造影:1.导引导管到位后撤出泥鳅导丝,常规造影,选择最佳工作角度,再次分析评估病变(测量狭窄的病变的长度及血管的直径,计算狭窄率,分析成角、钙化、溃疡斑块等可能影响手术的因素),最后确认手术方案。
2.同时进行颅内段造影,以便术后对比。
步骤四、保护装置:1.选择:根据病变结构特点选择合适的保护装置。
如选择远端保护装置,保护伞的直径与狭窄远端颈内动脉直径一致或稍大一点。
2.准备:肝素盐水冲洗,排气泡,保护伞收至输送导管内,根据病变形态将保护伞导丝头端塑形,将扭控子安装至保护伞导丝的尾端,准备好备用。
3.到位:打开Y阀,沿保护伞导入鞘,将保护伞置入8F导引导管。
在路图指引下,旋转扭控子将保护伞小心通过颈内动脉C1段狭窄处,至颈内动脉C1段远端较为平直的区域作为保护伞的目标“着陆区”。
(保护伞目标着陆区域:颈内动脉C1段远端,距离病变约4cm,避免过高——会诱发痉挛,避免过低——会影响支架置入操作。
)4.释放:左手拇指及食指在Y阀处固定保护伞导丝,右手撤下保护伞输送导管,保护伞顺利打开。
颈动脉椎动脉支架流程颈动脉和椎动脉支架术是一种介入治疗方法,用于治疗颈动脉狭窄或阻塞的情况。
下面是实施颈动脉和椎动脉支架治疗的详细流程:1.术前准备:在实施手术之前,医生会进行详细的病史询问和身体检查。
此外,还会对患者做一些检查,如彩超、CT血管造影等,以确定颈动脉或椎动脉是否需要支架治疗。
2.麻醉:在手术开始前,会对患者进行全身麻醉或局部麻醉。
3.穿刺:医生会选择适当的穿刺部位,通常是在大腿或手腕上,这取决于患者的具体情况。
然后,医生会在穿刺部位进行消毒,使用无菌操作将导管插入动脉。
4.引导导丝:在穿刺部位插入导管后,医生会将一根细导丝通过导管引入动脉系统中,并通过X光或血管造影仪的引导下推进到颈动脉或椎动脉的狭窄或阻塞部位。
5.扩张血管:一旦导丝到达狭窄或阻塞的血管段,医生会通过导丝引导下的球囊导管将血管扩张。
球囊导管充气时会膨胀,从而扩大血管的通道,并改善血液流量。
6.支架放置:在扩张血管后,需要将支架放入血管内。
支架是作为血管的支撑物,能够保持血管的张力和通道的畅通。
医生会将折叠的支架通过导管引导下送入血管,然后将其释放并展开,以覆盖狭窄或阻塞的血管段。
7.球囊扩张(可选步骤):在放置支架后,医生可能会使用球囊导管再次扩张血管以确保支架的定位和张力。
8.检查和完善:支架放置后,医生会进行血管造影或其他相关检查,以确保治疗的成功。
如果需要,医生还会进行其他操作,如清除血栓、栓塞物或其他危险物质。
9.结束手术:手术结束后,导管会被拔出,导航的穿刺部位会进行压迫止血,然后覆盖伤口进行消毒和敷料包扎。
10.术后观察:患者在术后会留院观察一段时间,以确保手术后的康复状况良好。