IDSA 隐球菌指南中文版 2010
- 格式:pdf
- 大小:1.83 MB
- 文档页数:34

IDSA MRSA指南解读仅限内部培训使用1前言•医学时讯中“备注”部分为医学顾问对指南内容的进一步解读•指南中包含斯沃产品说明书以外的信息。
切勿作为推广材料使用。
仅限内部培训使用2背景介绍•是IDSA制定的第一个关于MRSA感染治疗的指南•所有专家组成员参与了指南草案的准备和审核,并获得了外界同行的反馈意见。
•指南得到了儿童感染病学会、美国急救医师学会和美国儿科学会的审核和认可,并在公布前经IDSA SPGC和IDSA主任委员会审核和批准。
仅限内部培训使用3方法学•回顾和分析自1961年以来发表的数据。
利用计算机对PUBMED数据库中1961~2010年的英文文献进行检索•重点关注人类研究,但也包括动物模型实验研究和体外研究。
一些国际会议摘要也包括在内•由于随机临床试验极少,很多治疗推荐根据观察性研究或小规模病例分析结合专家组成员的意见而制定。
仅限内部培训使用4仅限内部培训使用5证据质量和推荐级别证据来自以临床经验、描述性研究或专家委员会报告为依据的权威专家观点III证据来自≥1项设计良好的非随机化临床试验;来自队列或病例对照分析研究(最好来自1个以上中心);来自多时间序列分析;或来自非对照性实验引人瞩目的结果II 证据来自≥1项设计适当的随机对照试验I证据质量推荐使用的证据不足C有中等证据支持推荐使用或反对使用的建议B有充足证据支持推荐使用或反对使用的建议A推荐级别定义类别/分级指南正文•药物评述•MRSA感染患者的治疗推荐I. 在CA-MRSA时代,SSTIs的治疗II. 复发性MRSA SSTIs的处理III. MRSA菌血症和感染性心内膜炎的治疗IV. MRSA肺炎的治疗V. MRSA引起的骨和关节感染的治疗VI. CNS MRSA感染的治疗VII. 辅助疗法在MRSA感染治疗中的地位VIII. 万古霉素剂量和监测的推荐IX. 万古霉素药敏结果如何来指导临床治疗X. 持续性MRSA菌血症及万古霉素治疗失败的处理XI. 新生儿MRSA感染的处理仅限内部培训使用6药物评述仅限内部培训使用7克林霉素经FDA批准用于金黄色葡萄球菌感染,但无明确的MRSA感染治疗的适应症在体外对CA-MRSA的敏感率高于HA-MRSA,各地区间有差异备注:在中国,根据CHINET监测网,MRSA对其敏感率<20%,一般情况下,治疗MRSA不建议选择此药物。
IDSA:新版曲霉菌病诊治指南欧阳学文原创 0706 步步非烟感染时间曲霉菌病是感染曲霉菌引起的一种真菌病,可累及皮肤、黏膜、眼、鼻、支气管、肺、胃肠道、神经系统、骨骼等多器官系统,严重者导致败血症,病例呈世界性分布。
病原体曲霉菌属丝状真菌,是一种常见的条件致病性真菌,广泛分布于自然界,其感染者并不少见。
时隔 8 年,美国感染病学会(IDSA)就曲霉菌病临床关注的热点问题,总结现有不同类型曲霉菌病相关证据,于近期发布了新版曲霉菌病诊治指南,替代旧版指南,旨在为临床医生诊治管理此病提供参考。
该新版指南于近期发表在 Clinical Infectious Diseases 杂志上。
现将主要内容简述如下。
流行病学与感染风险因素1. 易感者如何预防曲霉菌病?何为易感人群?(1)应将住院的异体造血干细胞移植(HSCT)接受者安置在受保护的环境中,以减少霉菌暴露机会(强烈推荐;证据级别低)。
(2)也应给予其他严重免疫功能低下的、易发生侵袭性曲霉菌病(IA)的高危患者相应防护措施,如急性白血病正在接受诱导/再诱导化疗方案治疗者(强烈推荐;证据级别低)。
(3)若住院无法提供防护病房的条件,推荐此类患者入住单独病房,且病房远离施工场地,也不允许将绿植或鲜花带入病房(强烈推荐;证据级别低)。
(4)建议对 IA 高危门诊患者采取合理防护措施,以减少霉菌暴露机会,包括避免园艺、施肥劳作或密切接触装修或施工场地(强烈推荐;证据级别低)。
(5)白血病诊疗中心与移植中心应当定期监测侵袭性霉菌感染。
若发现霉菌感染率超过基线水平,或者非高危人群发生侵袭性霉菌感染,应当立即对医源性感染情况进行评估(强烈推荐;证据级别低)。
曲霉菌病的诊治2. 如何确立侵袭性曲霉菌病的诊断?(6)在临床实验室推广使用分子生物学诊断技术以前,推荐采集足量组织和体液样本同时送检组织病理学/细胞学检查与真菌培养。
如果分离培养得到非典型菌株或考虑存在耐药,可采用分子生物学实验方法进行菌种鉴定(强烈推荐;证据级别低)。
美国传染病学会发热和中性粒细胞减少指南旨在为不断发展的流程提供合理的总结。
下面是2010年指南更新的推荐总结。
有关方法、背景和支持各个推荐的证据总结,详细描述见指南全文。
发热和中性粒细胞减少患者评估及治疗指南推荐Ⅰ.危险评估的作用及发热和中性粒细胞减少高危和低危患者的识别推荐1. 应对有发热表现者进行严重感染并发症的危险评估(A-Ⅱ)。
危险评估可确定经验性抗菌治疗类型(口服或静脉给药)、治疗场所(住院或门诊)和抗菌治疗疗程(A-Ⅱ)。
2. 大多数专家把有预期较长(时间>7天)及严重中性粒细胞减少(接受细胞毒性化疗后中性粒细胞绝对值[ANC]≤100细胞/mm3)和/或明显的内科合并病,包括低血压、肺炎、新发腹痛,或神经系统变化者认定为高危患者。
这类患者应首选入院接受经验性治疗(A-Ⅱ)。
3. 低危患者,包括预期较短(时间≤7天)的中性粒细胞减少,或无及少有合并病者,适合口服经验性治疗(A-Ⅱ)。
4. 正式的危险分类可使用多国癌症支持治疗学会(MASCC)评分系统(B-Ⅰ)。
ⅰ.高危患者MASCC评分<21(B-Ⅰ)。
所有按M ASCC评分或临床标准确定为高危的患者,如果还未住院,应首选入院接受经验性抗菌治疗(B-Ⅰ)。
ⅱ.低危患者MASCC评分≥21(B-Ⅰ)。
口服和/或门诊经验性抗菌治疗适用于仔细选择的低危患者(B -Ⅰ)。
Ⅱ. 初次评估期间应做的特殊检查和培养推荐5. 实验室检查应包括含有白细胞分类和血小板数量的完整血细胞(CBC)计数;血浆肌酐和尿素氮水平测定;电解质、肝脏转氨酶和总胆红素测定(A -Ⅲ)。
6. 推荐至少行两套血培养检查,如果存在中心静脉导管(CVC),一套采集自存在CVC的管腔,另一套同时采集自外周静脉区;如果无CVC,应送检不同静脉穿刺处的两套血培养检查(A-Ⅲ)。
对于体重<40kg的患者,血培养量应限制在<1%总血量(通常约为70mL/kg)(C-Ⅲ)。
7. 如有临床指征,应取得来自其他可疑感染部位的培养标本(A-Ⅲ)。
隐球菌病治疗实用指南为了帮助医师在治疗隐球菌病时正确选用抗真菌药,制定合理的给药方案。
美国国立变态反应和感染病研究院真菌病研究组(NIAID MSG)组织有关专家根据循证医学的原则制订了隐球菌病的处理指南。
该指南提出的建议适用于绝大多数隐球菌病患者。
虽然该指南系2000年制订,且所依据的临床证据均为国外资料,但由于该指南是在大量临床证据基础上制订对我们当前的临床实践仍具有重要的指导意义。
现将其主要内容编译供临床参考。
该指南的全文见Clinical InfectiousDisease 2000,30:710—718,并将于2008年更新。
本指南推荐强度和证据力度分级系统同其他美国感染病学会(IDSA)指南(附件)。
在过去的20余年,随着各类抗真菌药物的不断问世,新型隐球菌病的治疗发生了很大变化。
新型隐球菌病治疗方案的选择,主要取决于罹患部位和患者的免疫功能状况。
一、非HIV感染者隐球菌病的治疗指南(一)肺部及非中枢神经系统隐球菌病治疗目的为治愈感染并预防感染播散至中枢神经系统。
所有免疫缺陷者均应接受治疗,因易发生播散性感染。
有症状的患者均需治疗。
虽然所有培养阳性的无症状患者应接受治疗,但许多免疫功能正常的痰培养阳性患者即使不治疗亦预后良好。
肺外及中枢神经系统以外的感染(如骨骼或皮肤)需要特殊的抗真菌治疗。
持续性或难治性肺部或骨骼感染需要手术治疗。
所有患者需作腰穿以除外中枢神经系统感染。
肺部隐球菌病的治疗见表1。
早期适当治疗可降低病死率,防止中枢感染发生。
对于实体器官移植患者,可以防止感染导致的移植失败。
治疗主要的不良反应为药物相关的毒性反应,以及药物相互作用。
(二)中枢神经系统隐球菌病治疗目的为治愈感染并预防中枢神经系统后遗症,如脑神经瘫痪、听力丧失和失明。
中枢神经系统隐球菌病的治疗见表1。
治疗2周后需随访脑脊液(CSF)检查,如果培养阳性,需要延长诱导期疗程。
氟康唑联合氟胞嘧啶作为初始治疗疗效不佳,即使是低危患者。
Diagnosis and Management of ComplicatedIntra-abdominal Infection in Adults and Children: Guidelines by the Surgical Infection Societyand the Infectious Diseases Society of AmericaJoseph S.Solomkin,1John E.Mazuski,2John S.Bradley,3Keith A.Rodvold,7,8Ellie J.C.Goldstein,5Ellen J.Baron,6 Patrick J.O’Neill,9Anthony W.Chow,16E.Patchen Dellinger,10Soumitra R.Eachempati,11Sherwood Gorbach,12 Mary Hilfiker,4Addison K.May,13Avery B.Nathens,17Robert G.Sawyer,14and John G.Bartlett151Department of Surgery,the University of Cincinnati College of Medicine,Cincinnati,Ohio;2Department of Surgery,Washington University School of Medicine,Saint Louis,Missouri;Departments of3Pediatric Infectious Diseases and4Surgery,Rady Children’s Hospital of San Diego,San Diego,5R.M.Alden Research Laboratory,David Geffen School of Medicine at UCLA,Los Angeles,6Department of Pathology,Stanford University School of Medicine,Palo Alto,California;Departments of7Pharmacy Practice and8Medicine,University of Illinois at Chicago,Chicago;9Department of Surgery,The Trauma Center at Maricopa Medical Center,Phoenix,Arizona;10Department of Surgery,University of Washington, Seattle;11Department of Surgery,Cornell Medical Center,New York,New York;12Department of Medicine,Tufts University School of Medicine, Boston,Massachusetts;13Department of Surgery,Vanderbilt University Medical Center,Nashville,Tennessee;14Department of Surgery,University of Virginia,Charlottesville;15Department of Medicine,Johns Hopkins University School of Medicine,Baltimore,Maryland;and16Department of Medicine,University of British Columbia,Vancouver,British Columbia,and17St Michael’s Hospital,Toronto,Ontario,CanadaEvidence-based guidelines for managing patients with intra-abdominal infection were prepared by an Expert Panel of the Surgical Infection Society and the Infectious Diseases Society of America.These updated guidelines replace those previously published in2002and2003.The guidelines are intended for treating patients who either have these infections or may be at risk for them.New information,based on publications from the period2003–2008,is incorporated into this guideline document.The panel has also added recommendations for managing intra-abdominal infection in children,particularly where such management differs from that of adults;for appendicitis in patients of all ages;and for necrotizing enterocolitis in neonates.EXECUTIVE SUMMARYThe2009update of the guidelines contains evidence-based recommendations for the initial diagnosis and sub-sequent management of adult and pediatric patients with complicated and uncomplicated intra-abdominal infec-tion.The multifaceted nature of these infections has led to collaboration and endorsement of these recommen-dations by the following organizations:American Society for Microbiology,American Society of Health-SystemReceived7October2009;accepted9October2009;electronically published 23December2009.Reprints or correspondence:Dr Joseph S.Solomkin,Dept of Surgery,University of Cincinnati College of Medicine,231Albert B.Sabin Way,Cincinnati OH45267-0558(joseph.solomkin@).Clinical Infectious Diseases2010;50:133–64ᮊ2009by the Infectious Diseases Society of America.All rights reserved. 1058-4838/2010/5002-0001$15.00DOI:10.1086/649554Pharmacists,Pediatric Infectious Diseases Society,andSociety of Infectious Diseases Pharmacists.These guidelines make therapeutic recommendationson the basis of the severity of infection,which is definedfor these guidelines as a composite of patient age,phys-iologic derangements,and background medical con-ditions.These values are captured by severity scoringsystems,but for the individual patient,clinical judg-ment is at least as accurate as a numerical score[1–4].“High risk”is intended to describe patients with a rangeThis guideline might be updated periodically.To be sure you have the mostrecent version,check the Web site of the journal(http://www.journals.uchicago.edu/page/cid/IDSAguidelines.html).It is important to realize that guidelines cannot always account for individualvariation among patients.They are not intended to supplant physician judgmentwith respect to particular patients or special clinical situations.The InfectiousDiseases Society of America considers adherence to these guidelines to bevoluntary,with the ultimate determination regarding their application to be madeby the physician in the light of each patient’s individual circumstances.by guest on August 31, 2011Downloaded fromTable 1.Clinical Factors Predicting Failure of Source Control for Intra-abdominal InfectionDelay in the initial intervention (124h)High severity of illness (APACHE II score у15)Advanced ageComorbidity and degree of organ dysfunctionLow albumin levelPoor nutritional statusDegree of peritoneal involvement or diffuse peritonitis Inability to achieve adequate debridement or control of drainagePresence of malignancyNOTE.APACHE,Acute Physiology and Chronic Health Evaluation.of reasons for increased rates of treatment failure in addition to a higher severity of infection,particularly patients with an anatomically unfavorable infection or a health care–associatedinfection [5](Table 1).Initial Diagnostic Evaluation 1.Routine history,physical examination,and laboratory studies will identify most patients with suspected intra-abdom-inal infection for whom further evaluation and management is warranted (A-II).2.For selected patients with unreliable physical examination findings,such as those with an obtunded mental status or spinal cord injury or those immunosuppressed by disease or therapy,intra-abdominal infection should be considered if the patient presents with evidence of infection from an undetermined source (B-III).3.Further diagnostic imaging is unnecessary in patients with obvious signs of diffuse peritonitis and in whom immediate surgical intervention is to be performed (B-III).4.In adult patients not undergoing immediate laparotomy,computed tomography (CT)scan is the imaging modality of choice to determine the presence of an intra-abdominal infec-tion and its source (A-II).Fluid Resuscitation 5.Patients should undergo rapid restoration of intravascular volume and additional measures as needed to promote phys-iological stability (A-II).6.For patients with septic shock,such resuscitation should begin immediately when hypotension is identified (A-II).7.For patients without evidence of volume depletion,in-travenous fluid therapy should begin when the diagnosis of intra-abdominal infection is first suspected (B-III).Timing of Initiation of Antimicrobial Therapy 8.Antimicrobial therapy should be initiated once a patient receives a diagnosis of an intra-abdominal infection or once such an infection is considered likely.For patients with septic shock,antibiotics should be administered as soon as possible(A-III).9.For patients without septic shock,antimicrobial therapy should be started in the emergency department (B-III).10.Satisfactory antimicrobial drug levels should be main-tained during a source control intervention,which may ne-cessitate additional administration of antimicrobials just before initiation of the procedure (A-I).Elements of Appropriate Intervention 11.An appropriate source control procedure to drain in-fected foci,control ongoing peritoneal contamination by di-version or resection,and restore anatomic and physiological function to the extent feasible is recommended for nearly all patients with intra-abdominal infection (B-II).12.Patients with diffuse peritonitis should undergo an emer-gency surgical procedure as soon as is possible,even if ongoing measures to restore physiologic stability need to be continuedduring the procedure (B-II).13.Where feasible,percutaneous drainage of abscesses and other well-localized fluid collections is preferable to surgical drainage (B-II).14.For hemodynamically stable patients without evidenceof acute organ failure,an urgent approach should be taken.Intervention may be delayed for as long as 24h if appropriate antimicrobial therapy is given and careful clinical monitoring is provided (B-II).15.In patients with severe peritonitis,mandatory or sched-uled relaparotomy is not recommended in the absence of in-testinal discontinuity,abdominal fascial loss that prevents ab-dominal wall closure,or intra-abdominal hypertension (A-II).16.Highly selected patients with minimal physiological de-rangement and a well-circumscribed focus of infection,suchas a periappendiceal or pericolonic phlegmon,may be treatedwith antimicrobial therapy alone without a source control pro-cedure,provided that very close clinical follow-up is possible (B-II).Microbiologic Evaluation17.Blood cultures do not provide additional clinically rel-evant information for patients with community-acquired intra-abdominal infection and are therefore not routinely recom-mended for such patients (B-III).18.If a patient appears clinically toxic or is immunocom-promised,knowledge of bacteremia may be helpful in deter-mining duration of antimicrobial therapy (B-III).19.For community-acquired infections,there is no provenvalue in obtaining a routine Gram stain of the infected material (C-III).by guest on August 31, 2011 Downloaded fromTable2.Agents and Regimens that May Be Used for the Initial Empiric Treatment of Extra-biliary Complicated Intra-abdominal InfectionRegimen Community-acquired infectionin pediatric patientsCommunity-acquired infection in adultsMild-to-moderate severity:perforated or abscessed appendicitisand other infections ofmild-to-moderate severityHigh risk or severity:severe physiologic disturbance,advanced age,or immunocompromised stateSingle agent Ertapenem,meropenem,imipenem-cilastatin,ticarcillin-clavulanate,andpiperacillin-tazobactam Cefoxitin,ertapenem,moxifloxacin,tigecycline,and ticarcillin-clavulanicacidImipenem-cilastatin,meropenem,dori-penem,and piperacillin-tazobactamCombination Ceftriaxone,cefotaxime,cefepime,orceftazidime,each in combination withmetronidazole;gentamicin or tobra-mycin,each in combination with met-ronidazole or clindamycin,and with orwithout ampicillin Cefazolin,cefuroxime,ceftriaxone,cefotaxime,ciprofloxacin,or levoflox-acin,each in combination withmetronidazole aCefepime,ceftazidime,ciprofloxacin,orlevofloxacin,each in combinationwith metronidazole aa Because of increasing resistance of Escherichia coli tofluoroquinolones,local population susceptibility profiles and,if available,isolate susceptibility should be reviewed.20.For health care–associated infections,Gram stains may help define the presence of yeast(C-III).21.Routine aerobic and anaerobic cultures from lower-risk patients with community-acquired infection are considered op-tional in the individual patient but may be of value in detecting epidemiological changes in the resistance patterns of pathogens associated with community-acquired intra-abdominal infection and in guiding follow-up oral therapy(B-II).22.If there is significant resistance(ie,resistance in10%–20%of isolates)of a common community isolate(eg,Esche-richia coli)to an antimicrobial regimen in widespread local use, routine culture and susceptibility studies should be obtained for perforated appendicitis and other community-acquired in-tra-abdominal infections(B-III).23.Anaerobic cultures are not necessary for patients with community-acquired intra-abdominal infection if empiric an-timicrobial therapy active against common anaerobic pathogens is provided(B-III).24.For higher-risk patients,cultures from the site of infec-tion should be routinely obtained,particularly in patients with prior antibiotic exposure,who are more likely than other pa-tients to harbor resistant pathogens(A-II).25.The specimen collected from the intra-abdominal focus of infection should be representative of the material associated with the clinical infection(B-III).26.Cultures should be performed from1specimen,pro-vided it is of sufficient volume(at least1mL offluid or tissue, preferably more)and is transported to the laboratory in an appropriate transport system.For optimal recovery of aerobic bacteria,1–10mL offluid should be inoculated directly into an aerobic blood culture bottle.In addition,0.5mL offluid should be sent to the laboratory for Gram stain and,if indi-cated,fungal cultures.If anaerobic cultures are requested,at least0.5mL offluid or0.5g of tissue should be transportedin an anaerobic transport tube.Alternately,for recovery of anaerobic bacteria,1–10mL offluid can be inoculated directlyinto an anaerobic blood culture bottle(A-I).27.Susceptibility testing for Pseudomonas,Proteus,Acine-tobacter,Staphylococcus aureus,and predominant Enterobac-teriaceae,as determined by moderate-to-heavy growth,shouldbe performed,because these species are more likely than othersto yield resistant organisms(A-III).RECOMMENDED ANTIMICROBIAL REGIMENSThe antimicrobials and combinations of antimicrobials de-tailed in Tables2–4are considered adequate for empiric treat-ment of community-and health care–associated intra-abdom-inal infection as indicated.Community-Acquired Infection of Mild-to-Moderate Sever-ity in Adults28.Antibiotics used for empiric treatment of community-acquired intra-abdominal infection should be active againstenteric gram-negative aerobic and facultative bacilli and entericgram-positive streptococci(A-I).29.Coverage for obligate anaerobic bacilli should be pro-vided for distal small bowel,appendiceal,and colon-derivedinfection and for more proximal gastrointestinal perforationsin the presence of obstruction or paralytic ileus(A-I).30.For adult patients with mild-to-moderate community-acquired infection,the use of ticarcillin-clavulanate,cefoxitin, ertapenem,moxifloxacin,or tigecycline as single-agent therapyor combinations of metronidazole with cefazolin,cefuroxime, ceftriaxone,cefotaxime,levofloxacin,or ciprofloxacin are pref-erable to regimens with substantial anti-Pseudomonal activity(Table2)(A-I).by guest on August 31, 2011Downloaded fromTable3.Recommendations for Empiric Antimicrobial Therapy for Health Care–Associated Complicated Intra-abdominal InfectionOrganisms seen in health care–associated infection at the local institutionRegimenCarbapenem a Piperacillin-tazobactamCeftazidime or cefepime,each with metronidazole Aminoglycoside Vancomycin!20%Resistant Pseudomonas aeruginosa,ESBL-producing Enterobacteriaceae,Acinetobacter,or other MDR GNBRecommended Recommended Recommended Not recommended Not recommendedESBL-producing Enterobacteriaceae Recommended Recommended Not recommended Recommended Not recommended P.aeruginosa120%resistant toceftazidimeRecommended Recommended Not recommended Recommended Not recommendedMRSA Not recommended Not recommended Not recommended Not recommended Recommended NOTE.ESBL,extended-spectrum b-lactamase;GNB,gram-negative bacilli;MDR,multidrug resistant;MRSA,methicillin-resistant Staphylococcus aureus.“Recommended”indicates that the listed agent or class is recommended for empiric use,before culture and susceptibility data are available,at institutions that encounter these isolates from other health care–associated infections.These may be unit-or hospital-specific.a Imipenem-cilastatin,meropenem,or doripenem31.Ampicillin-sulbactam is not recommended for use be-cause of high rates of resistance to this agent among com-munity-acquired E.coli(B-II).32.Cefotetan and clindamycin are not recommended for use because of increasing prevalence of resistance to these agents among the Bacteroides fragilis group(B-II).33.Because of the availability of less toxic agents demon-strated to be at least equally effective,aminoglycosides are not recommended for routine use in adults with community-acquired intra-abdominal infection(B-II).34.Empiric coverage of Enterococcus is not necessary in pa-tients with community-acquired intra-abdominal infection (A-I).35.Empiric antifungal therapy for Candida is not recom-mended for adult and pediatric patients with community-acquired intra-abdominal infection(B-II).36.The use of agents listed as appropriate for higher-severity community-acquired infection and health care–associated in-fection is not recommended for patients with mild-to-moderate community-acquired infection,because such regimens may carry a greater risk of toxicity and facilitate acquisition of more-resistant organisms(B-II).37.For those patients with intra-abdominal infection of mild-to-moderate severity,including acute diverticulitis and various forms of appendicitis,who will not undergo a source control procedure,regimens listed for treatment of mild-to-moderate–severity infection are recommended,with a possi-bility of early oral therapy(B-III).High-Risk Community-Acquired Infection in Adults38.The empiric use of antimicrobial regimens with broad-spectrum activity against gram-negative organisms,including meropenem,imipenem-cilastatin,doripenem,piperacillin-tazobactam,ciprofloxacin or levofloxacin in combination with metronidazole,or ceftazidime or cefepime in combination with metronidazole,is recommended for patients with high-severity community-acquired intra-abdominal infection,as defined by APACHE II scores115or other variables listed in Table1(Table2)(A-I).39.Quinolone-resistant E.coli have become common insome communities,and quinolones should not be used unlesshospital surveys indicate190%susceptibility of E.coli to quin-olones(A-II).40.Aztreonam plus metronidazole is an alternative,but ad-dition of an agent effective against gram-positive cocci is rec-ommended(B-III).41.In adults,routine use of an aminoglycoside or anothersecond agent effective against gram-negative facultative andaerobic bacilli is not recommended in the absence of evidencethat the patient is likely to harbor resistant organisms thatrequire such therapy(A-I).42.Empiric use of agents effective against enterococci is rec-ommended(B-II).e of agents effective against methicillin-resistant S.au-reus(MRSA)or yeast is not recommended in the absence of evidence of infection due to such organisms(B-III).44.In these high-risk patients,antimicrobial regimensshould be adjusted according to culture and susceptibility re-ports to ensure activity against the predominant pathogens iso-lated in culture(A-III).Health Care–Associated Infection in Adults45.Empiric antibiotic therapy for health care–associated in-tra-abdominal infection should be driven by local microbio-logic results(A-II).46.To achieve empiric coverage of likely pathogens,mul-tidrug regimens that include agents with expanded spectra ofactivity against gram-negative aerobic and facultative bacillimay be needed.These agents include meropenem,imipenem-cilastatin,doripenem,piperacillin-tazobactam,or ceftazidimeby guest on August 31, 2011Downloaded fromTable4.Agents and Regimens that May Be Used for the Initial Empiric Treatment of Biliary Infection in AdultsInfection RegimenCommunity-acquired acute cholecystitis of mild-to-moderate severity Cefazolin,cefuroxime,or ceftriaxoneCommunity-acquired acute cholecystitis of severe physiologic disturbance, advanced age,or immunocompromised state Imipenem-cilastatin,meropenem,doripenem,piperacillin-tazobactam, ciprofloxacin,levofloxacin,or cefepime,each in combination with metronidazole aAcute cholangitis following bilio-enteric anastamosis of any severity Imipenem-cilastatin,meropenem,doripenem,piperacillin-tazobactam,ciprofloxacin,levofloxacin,or cefepime,each in combination withmetronidazole aHealth care–associated biliary infection of any severity Imipenem-cilastatin,meropenem,doripenem,piperacillin-tazobactam,ciprofloxacin,levofloxacin,or cefepime,each in combination with metroni-dazole,vancomycin added to each regimen aa Because of increasing resistance of Escherichia coli tofluoroquinolones,local population susceptibility profiles and,if available,isolate susceptibility should be reviewed.or cefepime in combination with metronidazole.Aminogly-cosides or colistin may be required(Table3)(B-III).47.Broad-spectrum antimicrobial therapy should be tai-lored when culture and susceptibility reports become available, to reduce the number and spectra of administered agents(B-III).Antifungal Therapy48.Antifungal therapy for patients with severe community-acquired or health care–associated infection is recommended if Candida is grown from intra-abdominal cultures(B-II). 49.Fluconazole is an appropriate choice for treatment if Candida albicans is isolated(B-II).50.Forfluconazole-resistant Candida species,therapy with an echinocandin(caspofungin,micafungin,or anidulafungin) is appropriate(B-III).51.For the critically ill patient,initial therapy with an echi-nocandin instead of a triazole is recommended(B-III).52.Because of toxicity,amphotericin B is not recommended as initial therapy(B-II).53.In neonates,empiric antifungal therapy should be started if Candida is suspected.If C.albicans is isolated,fluconazole is an appropriate choice(B-II).Anti-enterococcal Therapy54.Antimicrobial therapy for enterococci should be given when enterococci are recovered from patients with health care–associated infection(B-III).55.Empiric anti-enterococcal therapy is recommended for patients with health care–associated intra-abdominal infection, particularly those with postoperative infection,those who have previously received cephalosporins or other antimicrobial agents selecting for Enterococcus species,immunocompromised patients,and those with valvular heart disease or prosthetic intravascular materials(B-II).56.Initial empiric anti-enterococcal therapy should be di-rected against Enterococcus faecalis.Antibiotics that can poten-tially be used against this organism,on the basis of susceptibilitytesting of the individual isolate,include ampicillin,piperacillin-tazobactam,and vancomycin(B-III).57.Empiric therapy directed against vancomycin-resistant Enterococcus faecium is not recommended unless the patient isat very high risk for an infection due to this organism,suchas a liver transplant recipient with an intra-abdominal infection originating in the hepatobiliary tree or a patient known to be colonized with vancomycin-resistant E.faecium(B-III).Anti-MRSA Therapy58.Empiric antimicrobial coverage directed against MRSAshould be provided to patients with health care–associated in-tra-abdominal infection who are known to be colonized withthe organism or who are at risk of having an infection due tothis organism because of prior treatment failure and significant antibiotic exposure(B-II).59.Vancomycin is recommended for treatment of suspectedor proven intra-abdominal infection due to MRSA(A-III). Cholecystitis and Cholangitis in Adults60.Ultrasonography is thefirst imaging technique used for suspected acute cholecystitis or cholangitis(A-I).61.Patients with suspected infection and either acute cho-lecystitis or cholangitis should receive antimicrobial therapy,as recommended in Table4,although anaerobic therapy is not indicated unless a biliary-enteric anastamosis is present(B-II).62.Patients undergoing cholecystectomy for acute chole-cystitis should have antimicrobial therapy discontinued within24h unless there is evidence of infection outside the wall ofthe gallbladder(B-II).63.For community-acquired biliary infection,antimicrobialactivity against enterococci is not required,because the path-ogenicity of enterococci has not been demonstrated.For se-lected immunosuppressed patients,particularly those with he-by guest on August 31, 2011Downloaded fromTable5.Initial Intravenous Pediatric Dosages of Antibiotics for Treatment of Com-plicated Intra-abdominal InfectionAntibiotic,age range Dosage a Frequency of dosing Amikacin b15–22.5mg/kg/day Every8–24h Ampicillin sodium c200mg/kg/day Every6h Ampicillin-sulbactam c200mg/kg/day of ampicillin component Every6h Aztreonam c90–120mg/kg/day Every6–8h Cefepime c100mg/kg/day Every12h Cefotaxime c150–200mg/kg/day Every6–8h Cefotetan c40–80mg/kg/day Every12h Cefoxitin c160mg/kg/day Every4–6h Ceftazidime c150mg/kg/day Every8h Ceftriaxone c50–75mg/kg/day Every12–24h Cefuroxime c150mg/kg/day Every6–8hCiprofloxacin20-30mg/kg/day Every12h Clindamycin20–40mg/kg/day Every6–8h Ertapenem3months to12years15mg/kg twice daily(not to exceed1g/day)Every12hу13years1g/day Every24h Gentamicin b3–7.5mg/kg/day Every2–4h Imipenem-cilastatin c60–100mg/kg/day Every6h Meropenem c60mg/kg/day Every8h Metronidazole30–40mg/kg/day Every8h Piperacillin-tazobactam c200–300mg/kg/day of piperacillin component Every6–8h Ticarcillin-clavulanate c200–300mg/kg/day of ticarcillin component Every4–6h Tobramycin b 3.0–7.5mg/kg/day Every8–24h Vancomycin b40mg/kg/day as1h infusion Every6–8ha Dosages are based on normal renal and hepatic function.Dose in mg/kg should be based on total body weight.Further information on pediatric dosing can be obtained elsewhere[186–188].b Antibiotic serum concentrations and renal function should be monitored.c b-Lactam antibiotic dosages should be maximized if undrained intra-abdominal abscesses may be present.patic transplantation,enterococcal infection may be significant and require treatment(B-III).Pediatric Infection64.Routine use of broad-spectrum agents is not indicated for all children with fever and abdominal pain for whom there is a low suspicion of complicated appendicitis or other acute intra-abdominal infection(B-III).65.Selection of specific antimicrobial therapy for pediatric patients with complicated intra-abdominal infection should be based on considerations of the origin of infection(community vs health care),severity of illness,and safety of the antimicrobial agents in specific pediatric age groups(A-II).66.Acceptable broad-spectrum antimicrobial regimens for pediatric patients with complicated intra-abdominal infection include an aminoglycoside-based regimen,a carbapenem(im-ipenem,meropenem,or ertapenem),a b-lactam/b-lactamase–inhibitor combination(piperacillin-tazobactam or ticarcillin-clavulanate),or an advanced-generation cephalosporin(cefo-taxime,ceftriaxone,ceftazidime,or cefepime)with metroni-dazole(Tables2and5)(B-II).67.For children with severe reactions to b-lactam antibi-otics,ciprofloxacin plus metronidazole or an aminoglycoside-based regimen are recommended(B-III).68.Necrotizing enterocolitis in neonates is managed withfluid resuscitation,intravenous broad-spectrum antibiotics (potentially including antifungal agents),and bowel decom-pression.Urgent or emergent operative intervention,consistingof either laparotomy or percutaneous drainage,should be per-formed when there is evidence of bowel perforation.Intra-operative Gram stains and cultures should be obtained(B-III).69.Broad-spectrum antibiotics that may be useful in neo-nates with this condition include ampicillin,gentamicin,and metronidazole;ampicillin,cefotaxime,and metronidazole;or meropenem.Vancomycin may be used instead of ampicillinfor suspected MRSA or ampicillin-resistant enterococcal infec-tion.Fluconazole or amphotericin B should be used if the Gramstain or cultures of specimens obtained at operation are con-sistent with a fungal infection(B-II).Pharmacokinetic Considerations70.Empiric therapy of patients with complicated intra-abdominal infection requires the use of antibiotics at optimalby guest on August 31, 2011Downloaded from。
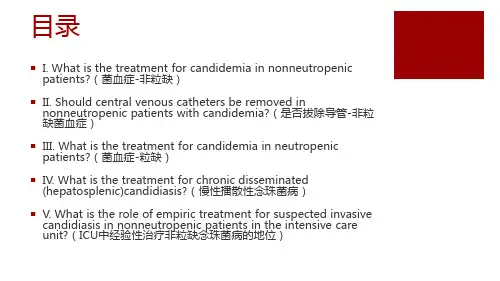
2016年由美国感染病学会更新的念珠菌病管理临床实践指南之杨若古兰创作布景念珠菌属形成的侵袭性感染很大程度上与医疗进展相干,并被广泛认为是形成院内感染发病及死亡的次要缘由.至多有15种分歧的念珠菌属惹起人类疾病,但超出90%的侵入性感染是由5种罕见的病原形成,它们是白色念珠菌、光滑念珠菌、热带念珠菌、近平滑念珠菌和克柔念珠菌.这些生物有统一的的潜在毒性、抗真菌药物敏感性和流行病学,但综合来说,由这些无机体形成的成心义的感染统称为侵袭性念珠菌病.不属于典型的侵袭性疾病的粘膜念珠菌感染,特别是那些涉及口咽、食道和阴道的感染,这项指南也将他们涵盖在内.自比来2009年对指南的修订至今,根据对于确诊或疑似侵袭性念珠菌病的诊断、预防和医治等方面的新数据,我们对医治建议进行了次要点窜.以下是2016年对念珠菌病管理的修订建议.因为与儿科的关联,指南得到了美国儿科学会和儿科感染疾病协会的审阅和认可.指南同样得到了真菌病研讨组的撑持.研讨组在拟定指南的过程中不断遵守IDSA采取的指南拟定流程,包含证据的质量分级(非常低,低,中,高)和推荐强度(弱或强)的零碎方法.指南其实不是打算替代个别病人管理的临床判断.对方法,布景和证据总结的具体描述均能在指南中找到全文.I.非中性粒细胞减少患者念珠菌血症的医治建议1.棘白菌素类药物被推荐作为初始医治(卡泊芬净:负荷剂量70 mg,然后每天50毫克;米卡芬净:每日100毫克;阿尼芬净:负荷剂量200毫克,然后100毫克每天)(强烈推荐;高级别证据).2.静脉打针或口服氟康唑,800毫克(12毫克/公斤)负荷剂量,然后400毫克(6毫克/公斤)每天,是可以接受的、棘白菌素作为初始医治的替代方案,限于那些病情不严重和那些被认为不成能有氟康唑耐药的念珠菌属感染的患者(强烈推荐;高级别证据).3.推荐对所有血源性和其他临床相干的念珠菌分离菌株进行唑类敏感性检测.对于前期使用一种棘白霉素类药物医治的患者、感染光滑念珠菌或近平滑念珠菌的患者,应当进行棘白菌素类药敏检测(强推荐;低级别证据).4.对于临床症状波动,分离出对氟康唑敏感的念珠菌(如白色念珠菌)感染,初始抗真菌医治后反复血培养结果阴性的患者,推荐将棘白霉素类更换为氟康唑(通常在5-7天5. 光滑念珠菌感染的患者,只要当分离株对于氟康唑或伏立康唑敏感时,应考虑将药物更换为更高剂量的氟康唑800mg/d(12mg/kg)或伏立康唑200-300mg(3-4mg/kg) 每日两次(强推荐;低级别证据).6. 如果不克不及耐受、没法获得其他抗真菌药物或耐药,两性霉素B脂质体(AmB)(3-5mg/kg/d)是一个合理的选择(强推荐;高级别证据).7.使用两性霉素B脂质体医治5-7天后,对氟康唑敏感的念珠菌感染患者,临床症状波动,且在抗真菌医治后反复血培养均为阴性时,推荐更换为氟康唑继续医治(强推荐;高级别证据).8. 对于可疑唑类和棘白霉素类药物耐药的念珠菌感染患者,推荐使用两性霉素B脂质体(3-5mg/kg/d)(强推荐;低级别证据).9. 给予伏立康唑400mg(6mg/kg)q12h两次,然后200mg(3mg/kg)q12h保持可无效医治念珠菌血症,但作为初始医治较氟康唑没有明显上风(强推荐;中级别证据).伏立康唑口服制剂被推荐为因为克柔念珠菌感染的菌血症降阶梯医治方案(强推荐;低级别证据).10.所有非中性粒细胞减少的念珠菌血症患者在诊断后的一周内都应当进行具体的眼科检查,最好由一位眼科医师来履行(强推荐;低级别证据).11. 血培养应当每天进行或隔日进行,以确定念珠菌血症被终止的时间点(强推荐;低级别证据).12. 推荐无明显的转移性并发症念珠菌血症医治时间为2周,应从记录念珠菌从血液中被清除和因为念珠菌所致症状经医治缓解后开始计算(强推荐;中级别证据).II.非中性粒细胞减少念珠菌血症患者是否该革除中间静脉导管?13. 念珠菌菌血症患者考虑感染为中间静脉导管来源及导管可以被平安革除时,中间静脉导管应当尽早革除;但这一做法需根据患者个体差别而定(强推荐;中级别证据).III.中性粒细胞减少念珠菌血症患者的医治建议14.任意一种棘白菌素类药物被推荐用于初始医治(卡泊芬净:首剂70mg,保持剂量50mg/d;米卡芬净:100mg/d;阿尼芬净:首剂负荷200mg,保持量100mg /d)(强推荐;中级别证据).15. 两性霉素B脂质体(3-5mg/kg/d)是一个无效的方案,但因为其潜在毒性其实不被青睐(强推荐;中级别证据).16. 氟康唑,负荷剂量800mg(12mg/kg),保持剂量400mg/d(6mg/kg),可用作非危重症患者和未使用唑类药物医治患者的替代医治方案(弱推荐;低级别证据).17. 氟康唑400mg/d(6mg/kg),能够作为持续中性粒细胞减少且病情波动患者降阶梯医治的选择,这些患者均为敏感菌株感染且血流的病原菌已被清除(弱推荐;低级别证据).18. 伏立康唑第一个24h给予400mg(6mg/kg)两次,然后200mg(3mg/kg)q12h保持可用于须要覆盖曲霉的情况(弱推荐;低级别证据).中性粒细胞减少的念珠菌血症患者,病情波动、念珠菌曾经在血液中被清除,而且分离的念珠菌对伏立康唑敏感,伏立康唑被推荐作为降阶梯医治方案(弱推荐;低级别证据).19. 对于克柔念珠菌感染的念珠菌血症患者,棘白霉素类药物,两性霉素B脂质体,或伏立康唑均被推荐(强推荐;低级别证据).20. 推荐无明显的转移性并发症的念珠菌血症医治最短时间为2周,应从记录念珠菌从血液中被清除、念珠菌所致中性粒细胞减少的症状经医治缓解后开始计算(强推荐;低级别证据).21. 当中性粒细胞减少恢复,眼科检查能发现的脉络膜和玻璃体感染是巨大的;是以,在中性粒细胞减少恢复当前的一周内应散瞳行眼底镜检查(强推荐;低级别证据).22. 中性粒细胞减少患者,念珠菌血症患者的感染源并不是次要来自中间静脉导管(如:胃肠道来源).中间静脉导管是否革除需根据患者个体差别而定(强推荐;低级别证据).23. 对于持续性念珠菌血症患者,当估计会发生持久中性粒细胞减少可考虑输注粒细胞集落刺激因子(G-CSF)(弱推荐;低级别证据).IV.慢性播散性(肝脾)念珠菌病的医治建议24.两性霉素B初始医治,3-5mg/Kg每天或棘白菌素类药物(米卡芬净:每日100毫克;卡泊芬净:70 mg负荷剂量,然后每天50毫克;阿尼芬净:200 mg负荷剂量,然后每天100毫克),推荐使用几个礼拜,然后序贯口服氟康唑,400毫克(6毫克/公斤)每天,次要用于那些不成能有氟康唑耐药的念珠菌病感染患者(强烈推荐;低级别证据).25.医治应持续到影象学病变接收,这通常须要几个月.抗真菌医治过早间断可导致复发(强烈推荐;低级别证据).26.如果患者须要接受化疗或造血干细胞移植,慢性播散性念珠菌病该当及时医治,抗真菌医治应当在高风险期持续利用以预防复发(强烈推荐;低级别证据).27.那些衰弱的持续发烧患者,可考虑短期(1-2周)使用非甾体类抗炎药或糖皮质激素医治(弱推荐;低级别证据).V.经验性医治在ICU非中性粒细胞减少患者疑似侵袭性念珠菌病中饰演的角色?28.对于有侵袭性念珠菌病高危身分和不明缘由发热的危重患者,该当根据临床风险身分和侵袭性念珠菌感染的标记物和/或无菌部位的培养结果等进行评估,及时给予经验性医治(强烈推荐;中等级别证据).对于有上述风险身分和有感染性休克的临床症状患者应尽可能早的开始经验性抗真菌医治(强烈推荐;中等级别证据).29.在ICU非中性粒细胞减少患者疑似念珠菌病的首选经验性医治是棘白菌素类药物(卡泊芬净:负荷剂量70 mg,然后每天50毫克;米卡芬净:每日100毫克;阿尼芬净:负荷剂量200毫克,100毫克每天)(强烈推荐;中等级别证据).30.氟康唑800毫克(12毫克/公斤)的负荷剂量,然后400毫克(6毫克/公斤)每天,对那些比来没有三唑类药物流露史和那些没有氟康唑耐药的念珠菌菌株定植的患者是可以接受的替代方案(强烈推荐;中等级别证据).31.两性霉素B脂质制剂,每日3-5mg/Kg,是不克不及耐受其他抗真菌药物患者的一种选择(强烈推荐;低级别证据).32.对疑似侵袭性念珠菌病经验性医治有改善的患者推荐医治时间为2周,与念珠菌血症的医治不异(弱推荐;低级别证据).33.对那些经验性抗真菌医治4-5天无临床应对的患者,和那些开始抗真菌医治后始终没有侵袭性念珠菌感染的证据,或者有非依附培养的高度阴性猜测价值的诊断检测阴性,应考虑停止抗真菌医治(强烈推荐;低级别证据).VI.在ICU预防侵袭性念珠菌感染的措施34.氟康唑800毫克(12毫克/公斤)的负荷剂量,然后400毫克(6毫克/公斤)每日,可用于具有侵袭性念珠菌病高发生率的成人ICU中具有高危身分的患者(弱推荐;中等级别证据).35.棘白菌素类药物可作为替代医治方案(卡泊芬净:70 mg负荷剂量,然后每天50毫克;净:200 mg负荷剂量,然后每天100毫克;或米卡芬净:每日100毫克)(弱推荐;低级别证据).36.推荐ICU患者用洗必泰每日洗澡,这已被证实是可以减少包含念珠菌血症的血流感染发生率(弱推荐;中等级别证据).VII.重生儿念珠菌病包含中枢神经零碎感染如何医治?侵袭性念珠菌病、念珠菌血症的医治方法是什么?37.两性霉素B脱氧胆酸,1mg/Kg每天,建议用于重生儿播散性念珠菌病(强烈推荐;中等级别证据).38.静脉打针或口服氟康唑,12mg/Kg每天,对没有接受过氟康唑预防的患者是一个合理的替代医治方案(强烈推荐;中等级别证据).39.两性霉素B脂质制剂,每日5mg/Kg,是一种替代方案,但应谨慎使用,特别是在泌尿零碎受累患者(弱推荐;低级别证据).40.棘白菌素应谨慎使用,普通仅限于抢救医治或因为耐药或者毒性没法使用两性霉素B脱氧胆酸或氟康唑的情况(弱推荐;低级别证据).41.对于血或尿液念珠菌培养阳性的患者,推荐腰椎穿刺和视网膜检查(强烈推荐;低级别证据).42.对于持续血培养念珠菌阳性的患者推荐CT或超声检查泌尿生殖道、肝脏和脾脏(强烈推荐;低级别证据).43.强烈推荐去除深静脉置管(强烈推荐;中等级别证据).44.对于没有明显转移病灶的念珠菌血症患者推荐医治时间为念珠菌从血流中清除而且清除了形成念珠菌血症的病灶后2周(强烈推荐;低级别证据).重生儿中枢神经零碎念珠菌感染的医治方法45.初始医治,推荐两性霉素B脱氧胆酸钠静脉点滴,1mg/Kg每日(强烈推荐;低级别证据).46.另一种替代方案是两性霉素B脂质体,5mg/Kg每天(强烈推荐;低级别证据).47.此外,氟胞嘧啶,25mg/Kg,每日4次,可作为抢救医治用于对初始AMB医治无临床反应的患者,但副感化发生很频繁(弱推荐;低级别证据).48.对初始医治有应对的患者的降阶梯医治,推荐氟康唑,每日12mg/Kg,推荐用于对氟康唑敏感菌株的医治(强烈推荐;低级别证据).49.医治应持续到所有的症状、体征、脑脊液和影象学异常均得到好转(强烈推荐;低级别证据).50.感染中枢神经零碎(CNS)的设备,包含脑室切开引流和分流安装,应当尽可能的移除(强烈推荐;低级别证据).重生儿ICU的预防措施有哪些建议?51.在侵袭性真菌病发生率高(> 10%)的护理机构,对于体重低于1公斤的重生儿,推荐静脉打针或口服氟康唑预防,3–6mg/kg,1周2次,持续 6周(强烈推荐,高级别证据).52.口服制霉菌素,10万单位,每日3次,持续6周,对出生体重小于1500克的重生儿,如果可以使用制霉素或因为耐药而没法使用氟康唑,可作为替代医治方案,(弱推荐;中等级别证据).53.口服乳铁蛋白(100mg/d)可能是对体重<1500 g的重生儿无效,但在美国的病院目前不成用(弱推荐;中等级别证据).VIII.对于腹腔内念珠菌感染的医治建议54.对有腹腔内感染临床证据和有念珠菌感染高危身分的患者,包含比来的腹部手术,吻合口漏或坏死性胰腺炎的患者,应考虑经验性抗真菌医治(强烈推荐;中等级别证据).55.腹腔内念珠菌感染的医治应包含泉源控制、适当的引流和/或清创(强烈推荐;中等级别证据).56.抗真菌医治的选择同于念珠菌血症或ICU非中性粒细胞减少患者的经验性医治(见第I和V节)(强烈推荐;中等级别证据).57.医治时间应以泉源控制的充分性和临床医治应对情况来决定(强烈建议;低级别证据).IX.从呼吸道分离的念珠菌须要医治吗?58.分离于呼吸道分泌物的念珠菌通常为定植菌,很少须要抗真菌医治(强烈推荐;中等级别证据).如何医治念珠菌心内膜炎?59.对于自体瓣膜心内膜炎,初始医治推荐两性霉素B脂质体 3-5mg/kg 每日1次,可加用氟胞嘧啶 25mg/kg 每日4次,或者大剂量的棘白菌素类药物(卡泊芬净 150mg 每日1次,米卡芬净150mg 每日1次,或者阿尼芬净 200mg 每日1次)(强烈推荐;低级别证据).60.对于氟康唑敏感的念珠菌感染的病人,若已临床波动,且已清除血流中的念珠菌,推荐使用氟康唑 400-800mg (6-12mg/kg)每日1次,作为降阶梯医治方案(强烈推荐;低级别证据).61. 对于分离出伏立康唑和泊沙康唑敏感而对于氟康唑不敏感的念珠菌,也可口服伏立康唑200-300mg(3-4mg/kg)每日2次,或者泊沙康唑片 300mg 每日1次,作为降阶梯医治(弱推荐,非常低级别证据).62. 推荐行瓣膜置换术;术后抗真菌医治至多持续6周以上,对于有瓣周脓肿或者其它并发症的病人抗真菌医治时间应当更长(强烈推荐;低级别证据).63. 对于不克不及行瓣膜置换术的患者,若菌群对氟康唑敏感,推荐持久使用氟康唑 400-800mg(6-12mg/kg)每日1次,以按捺感染(强烈推荐;低级别证据).64. 对于人工瓣膜心内膜炎,推荐按照自体瓣膜心内膜炎的抗真菌方案进行医治(强烈推荐;低级别证据).为预防感染复发,推荐使用氟康唑(400-800mg/kg 每日1次)持久抗真菌医治(强烈推荐;低级别证据).如何医治心内植入物相干的感染?65. 对于起搏器和植入式心脏除颤器相干感染,应移除植入安装(强烈推荐;中级别证据).66. 抗真菌医治方案和自体瓣膜心内膜炎的抗真菌医治方案不异(强烈推荐;低级别证据).67. 对于局限于发生器囊袋的感染,建议移除植入安装后继续给予4周的抗真菌医治(强烈推荐;低级别证据).68. 对于侵及导线的感染,建议移除导线后至多继续抗真菌医治6周以上(强烈推荐;低级别证据).69. 若心室辅助安装不克不及被移除,推荐按照自体瓣膜心内膜炎的抗真菌方案进行医治(强烈推荐;低级别证据).如果菌群对于氟康唑敏感,只需植入安装未被移除,建议使用氟康唑持久抗真菌医治(强烈推荐;低级别证据).如何医治念珠菌化脓性血栓性静脉炎?70. 如果可以的话,建议革除导管,切开引流,或者行静脉切除术(强烈推荐;低级别证据).71. 如果有念珠菌血症,血流中念珠菌清除后,继续给予两性霉素B脂质体(3-5mg/kg 每日1次),或者氟康唑[400-800mg(6-12mg/kg)每日1次],或者棘白菌素类(卡泊芬净 150mg 每日1次;米卡芬净 150mg 每日1次;或者阿尼芬净 200mg 每日1次)至多医治2周以上(强烈推荐;低级别证据).72. 对于初始医治使用两性霉素B或者棘白菌素类药物的病人,待临床情况波动以后,若念珠菌对于氟康唑敏感,应考虑降阶梯医治,改用氟康唑 400-800mg(6-12mg/kg)每日1次(强烈推荐;低级别证据).73. 如果临床症状和培养结果皆转为阴性,血栓的完整治愈可以作为停用抗真菌医治的根据(强烈推荐;低级别证据).念珠菌骨髓炎的医治建议74.氟康唑400毫克(6毫克/公斤)每天持续6-12个月,或棘白菌素类药物(卡泊芬净50-70mg每天持续12个月或米卡芬净每日100毫克,或阿尼芬净每日100毫克)利用至多2周,序贯氟康唑400毫克(6mg/Kg)每天,持续6-12个月(强烈推荐;低级别证据).75.两性霉素B脂质制剂,每日3-5mg/Kg,利用至多2周,序贯氟康唑,400mg(6mg/Kg),持续6-12个月是一个较有吸引力的替代方案(弱建议;低级别证据).76.在部分病例推荐进行手术清创术(强推荐,低级别证据)脓毒性关节炎的医治建议77.氟康唑400mg(6mg/Kg)每天,持续6周或棘白菌素类药物(卡泊芬净50-70mg每天,米卡芬净100mg每天,或阿尼芬净100mg每天)利用2周,后序贯氟康唑,400mg (6mg/Kg)每天,至多利用4周(强烈推荐;低级别证据).78.两性霉素B脂质制剂,5mg/Kg每天,持续2周,序贯氟康唑,400mg(6mg/kg)每天,至多4周是较有吸引力的替代方案(弱推荐;低级别证据).79.所有化脓性关节炎病例推荐内科引流(强推荐、中等级别证据).80.对假肢安装相干的化脓性关节炎,推荐移除安装(强烈推荐;中级证据).81.如果假体安装没法移除,分离菌是敏感的,推荐氟康唑,400mg(6mg/Kg)每天(强烈推荐;低级证据).XII.念珠菌眼内炎的医治建议念珠菌眼内炎的通常处理建议82.所有念珠菌血症患者应当做视网膜检查,最好由眼科大夫进行,对于非中性粒细胞减少患者须要在医治的第一周内是否存在眼内炎(强烈建议;低级别证据);对于中性粒细胞减少的患者,建议推迟到中性粒细胞恢复后在进行眼底检查(强烈推荐;低级别证据).83.眼部感染程度(脉络膜视网膜炎,伴或不伴黄斑受累,伴或不伴玻璃体炎)应当由眼科大夫来判定(强烈推荐;低级别证据).84.抗真菌医治和内科干预的决定应当由眼科大夫和传染病医师共同拟定(强烈推荐;低级别证据).不伴玻璃体炎的念珠菌脉络膜视网膜炎的医治建议85.氟康唑/伏立康唑敏感株,氟康唑,负荷剂量800毫克(12mg/Kg),然后400–800mg(6–12mg/Kg)每天或伏立康唑,负荷剂量第一天400mg(6 mg/kg)静脉利用2次,然后300mg(4mg/Kg)静脉或口服,每日2次(强烈推荐;低级别证据).86.氟康唑/伏立康唑耐药株,两性霉素B脂质体,3-5mg/kg每天静脉利用,联合或不联合氟胞嘧啶,25mg/Kg,每日4次(强烈推荐;低级别证据).87.有黄斑受累的,抗真菌药物如上所述,同时须要进行玻璃体腔打针两性霉素B脱氧胆酸盐,5-10µg/ 0.1ml无菌打针用水,或伏立康唑,100µg/ 0.1ml无菌水或生理盐水,以确保及时高水平的抗真菌活性(强烈推荐;低级别证据).88.医治时间至多应为4-6周时间,终极须要通过反复的眼科检查确定损伤得到治愈(强烈推荐;低级别证据).伴玻璃体炎的念珠菌脉络膜视网膜炎的医治建议89.伴随玻璃体炎的脉络膜视网膜炎抗真菌医治如上所述方案加上玻璃体腔打针两性霉素B脱氧胆酸盐,5-10µg/ 0.1ml无菌打针用水或伏立康唑,100µg/ 0.1毫升无菌水或生理盐水(强烈推荐;低级别证据).90.应考虑行玻璃体切除术以减少病原体负载,不适合零碎抗真菌制剂医治的真菌性脓肿应及时移除(强烈推荐;低级别证据).91.医治时间至多应为4-6周时间,终极疗程取决于反复的眼科检查确定损伤得到治愈(强烈推荐;低级别证据).XIII.中枢神经零碎念珠菌感染的医治建议5mg/kg 每日1次,可加用氟胞嘧啶 25mg/kg 每日4次(强烈推荐;低级别证据).400-800mg(6-12mg/kg)每日1次,作为降阶梯医治(强烈推荐;低级别证据).94.医治应持续到症状、体征、脑脊液和影象学检查皆恢复正常为止(强烈推荐;低级别证据).95.如果可能,建议移除被感染了的中枢神经零碎内置入物,包含脑室引流管、分流管、脑深部电刺激器、神经假体重建安装和释放化疗药物的高分子聚合晶片(强烈推荐;低级别证据).96.若脑室内置入物不克不及被移除,可将0.01mg-0.5mg 脱氧胆酸两性霉素B溶解在2mL的5%葡萄糖溶液中,通过脑室置入物通路直接脑室内给药(弱推荐;低级别证据).XIV.念珠菌导致的尿路感染医治建议无症状的念珠菌尿医治建议97. 只需条件答应,建议去除诱因,如革除膀胱留置导尿管(强烈推荐;低级别证据).98. 不推荐抗真菌医治,除非病人合并有以下导致感染播散的高危身分,如粒细胞减少,极低体重重生儿(小于1500g)或需行泌尿系手术(强烈推荐;低级别证据).99. 粒细胞减少病人和极低体重重生儿的医治可参照念珠菌血症的医治(见III和VII节)(强烈推荐;低级别证据).100. 需行泌尿系手术的病人建议手术前后数天给予口服氟康唑 400mg(6mg/kg)每日1次,或者两性霉素B脱氧胆酸盐每日1次(强烈推荐;低级别证据).有症状的念珠菌膀胱炎医治建议101. 对于氟康唑敏感的菌群,建议口服氟康唑 200mg (3mg/kg)每日1次疗程2周(强烈推荐;中级别证据).102. 针对氟康唑耐药的光滑念珠菌,建议脱氧胆酸两性霉素B 每日1次疗程1-7天,或者口服氟胞嘧啶 25mg/kg 每日4次疗程7-10天(强烈推荐;低级别证据).103. 针对克柔念珠菌,建议脱氧胆酸两性霉素B 每日1次疗程1-7天(强烈推荐;低级别证据).104. 如果可能,强烈建议革除膀胱留置导尿管(强烈推荐;低级别证据).105. 针对氟康唑耐药菌属导致的膀胱炎,如光滑念珠菌和克柔念珠菌,每日给予50mg脱氧胆酸两性霉素B用灭菌打针用水配成1L,连续膀胱冲洗5天可能无效(弱推荐;低级别证据).有症状的上行感染念珠菌肾盂肾炎医治建议106.对于氟康唑敏感的菌群,推荐口服氟康唑 200-400mg (3-6mg/kg)每日1次疗程2周(强烈推荐;低级别证据).107. 针对氟康唑耐药的光滑念珠菌,推荐脱氧胆酸两性霉素B 每日1次疗程1-7天,可加用氟胞嘧啶 25mg/kg 每日4次(强烈推荐;低级别证据).108. 针对氟康唑耐药的光滑念珠菌,可以考虑单用氟胞嘧啶口服25mg/kg 每日4次疗程2周(弱推荐;低级别证据).109. 针对克柔念珠菌,推荐脱氧胆酸两性霉素B 每日1次疗程1-7天(强烈推荐;低级别证据).110. 强烈建议解除尿路梗阻(强烈推荐;低级别证据).111.对于留置肾盂造瘘管或输尿管支架的病人,如果可行,应考虑移除或者更换(弱推荐;低级别证据).伴真菌球构成的念珠菌尿路感染医治建议112.对于成人患者,强烈建议手术医治(强烈推荐;低级别证据)113. 抗真菌医治建议按照上文提到的膀胱炎或者肾盂肾炎的医治方案(强烈推荐;低级别证据).114. 如果有肾盂造瘘管,建议25-50mg两性霉素B脱氧胆酸盐加入200-500mL灭菌打针用水中进行冲洗(强烈推荐,低级别证据).XV.念珠菌外阴阴道炎的医治建议115.对于无并发症的念珠菌外阴阴道炎医治,外用抗真菌药物,没有一剂优于另一个的建议(强烈推荐,高级别证。