病理学-炎症学习课件
- 格式:dps
- 大小:10.37 MB
- 文档页数:6

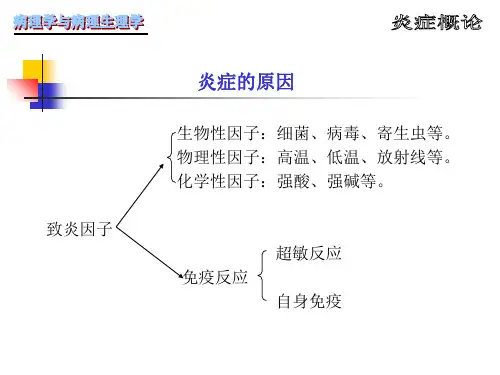

InflammationSkin blister result from burning Serous effusion accumulated within and underneath the epidermis of skinCarbuncle(痈) Furuncle(疖)Outlines of inflammation●General Considerations➢Definition; Inflammatory agents; Basic pathological changes ofinflammation; Local and systemic manifestations of Inflammation ●Acute inflammation➢The process of vascular and cellular events in inflammation,Inflammatory mediators➢The classification and outcomes of acute inflammation●Chronic inflammationPart 1 General ConsiderationsDefinitionInflammation is a protective response intended to eliminate the initial cause of cell injury as well as the necrotic cells and tissues resulting from the original insult.Components of acute and chronic inflammationInflammatory agents●Infections (bacterial, viral, parasitic) and microbialtoxins●Physical agents (e.g., irradiation, burns) and Trauma(blunt and penetrating)●Chemical agents (some environmental chemicals)●Ischemic and necrotic tissues●Foreign particle (dirt, sutures)●Allergic reactionsThe basic pathological changes●Alteration (degeneration, necrosis)●Exudation (hallmark, vascular change, leukocyte reaction, inflammatory mediators )●Proliferation (parenchymal and strmal cells)Exudation of plasma proteinsExudate and transudateCause inflammation non-inflammation Gross cloudy clearGravity >1.018 <1.018 Protein >30g/L < 30g/LCell no. >100/mm3<100/mm3 Coagulation + -Mucoprotein + -Local manifestations of Inflammation ●rubor (redness)●tumor (swelling)●calor (heat)●dolor (pain)Systemic manifestations of inflammation●Fever●Increased acute-phase proteins●Leukocytosis●Others: increased pulse and bloodpressure; decreased sweating; rigors;anorexiaPart 2 Acute inflammationThe process of acute inflammation ●Vascular events●Cellular events●Molecular eventsVascular Events●Changes in vascular caliber and flow➢Transient vasoconstriction of arterioles at the site of injury➢Vasodilation of precapillary arterioles then increases blood flow to the tissue●Increased vascular permeabilityThe major local manifestations of acute inflammation: (1)vascular dilation; (2) extravasation of plasma fluid and protein; (3) leukocyte emigration and accumulation in the site of injuryCellular Events1) Recruitment of leukocytes to sites of infection and injury2) Recognition of microbes and dead tissues3) Removal of the offending agents4) Release of leukocyte products and leukocyte-mediated tissue injury1) Recruitment of leukocytes to sites of infection and injury●Margination, rolling and adhesion toendothelium●Leukocyte migration throughendothelium●Chemotaxis and activationThe multiple process of leukocyte migration through blood vessels.Robbins and Cotran Pathologic Basis of Disease 7th editionChemotaxis●After extravasating from the blood, leukocytesmigrate toward sites of injury along a chemical gradient in a process called Chemotaxis.●Chemotactic Factors including bacterialproducts, chemokines, C5a, leukotriene B 42) Recognition of microbesLeukocyte receptors and responses3) Removal of the offending agents●Phagocytosis●Engulfment●Killing and degradationA. Phagocytosis:●Attachment●Engulfment●Fusion with lysosomesB. oxygen-dependentbactericidalmechanismRobbins Basic Pathology4) Release of leukocyte products and leukocyte-mediated tissue injury●Acute inflammation: e.g., acute respiratory distress syndrome; acute transplant rejection; reperfusion injury●Chronic inflammation: e.g., arthritis; asthma; chronic lung diseaseInflammatory Mediator●Function of chemical mediators: directing the vascular and cellular events in inflammation●Cell-derived or Plasma-derived mediators●Act as a complicated networkMediators Sources ActionsHistamine Mast cells, basophils,platelets Vasodilation, increased vascular permeability, endothelial activationSerotonin Platelets Vasodilation, increased vascular permeability Prostaglandins Mast cells,leukocytesVasodilation, pain, feverLeukotrienes Mast cells,leukocytes Increased vascular permeability, chemotaxis, leukocyte adhesion and activationPlatelet-activating factor Leukocytes, mastcellsVasodilation, increased vascular permeability,leukocyte adhesion, chemotaxis, degranulation,oxidative burstReactive oxygenspeciesLeukocytes Killing of microbes, tissue damageNitric oxide Endothelium,macrophagesVascular smooth muscle relaxation, killing of microbesCytokines (TNF, IL-1)Macrophages,endothelial cells,mast cells Local endothelial activation (expression of adhesion molecules), fever/pain/anorexia/hypotension, decreased vascular resistance (shock)Chemokines Leukocytes,activatedmacrophages Chemotaxis, leukocyte activationCell-derived mediatorsGeneration of arachidonic acid metabolites and their roles in inflammationMajor effects of IL-1 and TNFMediators Sources ActionsComplement products (C5a, C3a, C4a)Plasma(produced in liver)Leukocyte chemotaxis and activation,vasodilation (mast cell stimulation)Kinins Plasma(produced in liver)Increased vascular permeability, smooth muscle contraction, vasodilation, painProteases activated during coagulation Plasma(produced in liver)Endothelial activation, leukocyte recruitmentplasma protein-derived mediatorsInterrelationships between the four plasma mediatorsRole in InflammationMediators Vasodilation Prostaglandins, Nitric oxide, Histamine Increased vascular permeability Histamine and serotonin, C3a and C5a,BradykininLeukotrienes C 4, D 4, E 4, PAF, Substance PChemotaxis, leukocyte recruitment and activationTNF, IL-1, Chemokines, C3a, C5a, Leukotriene B 4Fever IL-1, TNF, ProstaglandinsPainProstaglandins, Bradykinin Tissue damage Lysosomal enzymes of leukocytes, Reactive oxygen speciesNitric oxideRole of Mediators in InflammationInflammatoryMediator VasodilatationVascular permeabilityEDEMA VESOACTIVE MEDIATORS •Histamine •Bradykinin •C3a C5a •LT PG •PAF •NO TISUE INJURY•Trauma •Ischemia •Neoplasm •Infectious agents •Foreign particlePRODUCTION OF INFLAMMATORY MEDIATORSCHEMOTACTIC FACTORS•C 5a•LTB4•IL-8, TNF inflammatory cellsACUTEINFLAMMATION Neutrophils,Platelets,Mast cellCHRONIC INFLAMMATIONMacrophages,Lymphocytes, PlateletsClassification of inflammation ●Clinical classification●Pathological classificationClinical Classification ●Acute inflammation●Chronic inflammationCharacteristics of Acute Inflammation●Short duration: days to months●Acute injuries induced by inflammatory agents●Exudation: fluid, plasma proteins, neutrophils●Abscess formation●Complete resolution can be reached if the injury is limited or short-lived●Severe injury healing by scar formation●Spreading : septicemia, pyemia,( metastatic abscess)●Progression to chronic inflammationCharacteristics of Chronic Inflammation●Long duration: months to years●Persistent infection, prolonged exposure to harmful agents ●Prolonged tissue destruction, loss of normal structure and function●chronic inflammatory cell Infiltration: Macrophages, Lymphocytes, Plasma cells●persistent new vessel regeneration and fibroblast proliferation: Resulting in fibrosisPathological Classification●Alteration Inflammation (acute)●Exudation Inflammation (acute)●Proliferation Inflammation (chronic)Alteration Inflammation Viral hepatitis (hepatocyte necrosis) Epidemic Type B Encephalitis (neuronal necrosis)Poliomyelitis (neuronal necrosis)Alteration inflammation----Viral hepatitisExudation Inflammation ●Serous Inflammation●Fibrinous Inflammaion●Suppurative Inflammation➢Phlegnomous Inflammation➢Superficial Suppuration➢Abscess●Hemorrhagic InflammationSerous I nflammation●Features:Outpouring of a watery, relatively protein-poor fluid (effusion, with 3%-5% plasma proteins, Albumin)●Location:Mucosa, body cavities (peritoneal, pleural & pericardial cavities) , Loose connective tissues●Pathologic changes:Inflammatory edema, blister, hydrops, Catarrh●Outcome:complete resolutionSerous InflammationFibrinous Inflammation●Causes: M ore severe injuries can result in greater vascular permeability. L arger molecules(esp. fibrinogen)come out through the endothelial cells.●Pathologic changes: E osinophilic meshwork of threads or sometimes as an amorphous coagulum.●Location:Mucosa, pericardium , peritonium, body cavities, LungFibrinous Inflammation●Pathologic changes:➢Mucosa: Pseudomembraneous➢Pericardium: Shaggy heart➢Lung: lobar pneumonia●Outcome:➢Resolution:Restore normal tissue structure ➢Organization: scar formationFibrinous Inflammation of Larynx & Trachea due todiphtheriaFibrinous Inflammation of Intestine Pseudomembrane (Bacillary Dysentery)Fibrinous Inflammation of Pericardial Cavity。