注意缺陷-多动障碍(ADHD)评估表教学内容
- 格式:doc
- 大小:117.50 KB
- 文档页数:7
注意缺陷多动障碍(ADHD)早期识别与精心护理流程1.儿童注意缺陷多动障碍的健康教育2.孩子有多动症表现,你却还不知道?3.注意缺陷与多动障碍简介4.儿童多动症的介绍5.儿童多动症6.什么是多动症儿童注意缺陷多动障碍的健康教育儿童注意缺陷多动障碍(ADHD)又称小儿多动症,是儿童期最为常见的精神卫生问题,其突出表现为注意力缺陷,以多动为主的行为障碍及冲动性。
文献报道在小学生中患病率为5%~10%.这类患儿如处理不当,常会影响其学习及性格的发展。
有跟踪研究发现25%~50%患儿在成人期有人格障碍,易冲动及有反社会行为,在学习和事业上的成就明显低于同龄人。
可见,对ADHD患儿的治疗和健康教育十分重要。
1.病因和主要表现关于ADHD的致病因素,国内外许多专家进行研究探讨,普遍认为可能与下列因素有关:(1)因感染、中毒或外伤等导致轻微脑损伤;(2)遗传因素;(3)大脑某些生理功能缺陷;(4)家庭环境及教育方式不良等因素。
总之,本病是多种病因所致的一组综合征,或者是在某些先天遗传素质不良,某种神经递质缺陷的基础上,加上后天某些因素造成的脑损伤或精神创伤,促使了症状的出现或发展。
主要症状表现为注意力不集中,不持久,容易分散;活动过多,不能静坐片刻,不遵守纪律,行为障碍,性情急躁,任性冲动,有攻击性行为,自控能力差,学习困难,上课不专心,缺乏必要的注意力,缺乏坚持性,致使其学习成绩落后。
2.治疗方法对于学龄前儿童,主要是实施教育及行为治疗,很少需要药物治疗。
因为在较小的儿童药物治疗副作用较明显,还可能出现分离性焦虑,依附行为,烦躁不安等不良反应,造成管理上更加困难。
对个别极严重对家庭造成严重的干扰时,才考虑在医生严密观察下小剂量用药。
而学龄儿童,由于需要尽快地帮助他们在课堂上集中注意力,因此,除教育外,常需配合药物治疗。
常用的药物有精神兴奋剂,抗抑郁剂等。
3.健康教育的内容与方法ADHD是一种复杂的、可引起多种问题的精神障碍。

(内容设置和项目说明可以参考--)对注意缺陷多动障碍儿童(ADHD)的感觉统合训练/一,注意缺损多动障碍的界定注意缺损多动障碍是一组以注意力缺损,多动,冲动,唤醒不足,角色管理失控行为为主要表现特征的行为情绪的综合症候群,是儿童期常见的心理障碍之一.主要的行为表现有以下五方面:1.注意力缺损 ADHD儿童的注意障碍一方面表现为主动注意功能极差,难以根据一定的任务和要求自觉地把注意力集中在某项活动或任务上.另一方面又表现出被动注意功能相对亢进,非常易于被外界任何小变化所吸引,将注意力转向无关事物.2.多动注意缺损多动儿童不分场合,特别好动.3.冲动此障碍儿童往往行动之前缺乏思考,难以在做出某一行动前思考其行为的后果.4.唤醒不足 ADHD儿童对那些要求长时间坚持注意的活动表现出倦怠,懒散,不能做到有始有终,常常半途而废,虎头蛇尾,思想开小差,易分心,不能一心一意,全神贯注地做一件事.5.角色管理失控行为注意缺损多动儿童,由于情绪不稳定,缺乏克制力,往往表现得较幼稚,任性,他们要什么立刻就得满足,一不顺心就发脾气,摔东西.二,感觉统合的意义,作用美国加利福尼亚大学的a.j.ayres,根据神经生理学的理论,最初提出了感觉统合这一理论和方法.她认为,作为人类行为,动作发育的基本感觉系统,如触觉系,前庭感觉系,本体感觉系,这些系统对于人类的认知发展起着重要作用.国内资料报道:存在感觉统合失调的儿童中,各种运动协调失衡的约占28%,学习困难的约占31%,注意缺陷多动障碍的约占41%,可见感觉统合失调与多动症,学习困难有密切的关系.学习能力一般指获得知识与保持知识的能力,与听,说,读,写等一般学校技能关系密切,如感觉统合失调,前庭系统不健全,肌张力不足,平衡觉差,大小肌群协调能力不足,以致于视觉,听觉,手眼口协调配合运动差;患儿坐在椅子上,很难维持举头姿势,常下巴垫在手背趴在桌子上,或动来动去就是控制不住自己的体位.由于知觉发育不足,听的识别力和专注力差,以致于注意力涣散;视知觉发育不足,视空间距离感差,影响阅读能力的发展,看书时感到吃力,阅读常窜行,漏行,掉字而不喜欢看书.视知觉的不成熟而影啊手,眼运动的协调.针对多动症患儿的感觉统合失调,前庭功能不全,触觉不当,本体感不足,以致整个身体协调不良等进行感觉运动强化训练,对于矫正由于运动感觉不足或运动感觉扭曲等错误对感觉住处而产生的身体协调不良,身体形象不明等具有较好的作用,加强正确的运动感觉刺激为建立,恢复其健康和正常的运动模式是感觉统合训练的目的所在.人类对于一些简单的动作和行为往往是无意识进行的,但要完成一些复杂的,高难度的动作和行为时,需要有意识地调节和控制,也就是说,对来自外界环境以及自身内部的各种各样的感觉刺激和信息,进行选择,整理,有序的工作,是通过大脑神经系统来完成的.一旦感觉统合发生问题,就会出现种种障碍,如动作不协调,不能完成复杂的动作和行为,不能正常地进行日常的生活,学习和游戏,因此,矫治ADHD儿的感觉统合障碍是极为重要的.三,ADHD儿童感觉统合治疗原则在设计运动感觉的活动时,应注意以下几个原则:(1)运动不只是平面性的,而且要有立体性的;(2)不但要注意"动",而且要注意"静";(3)要注意"动","静"运动配合时对身体的协调作用.在训练初期,运动发展的强化主要在高速活动时的平衡能力,促进身体和地心引力上的正确协调,能持久保持安定姿势的能力等方面.动态训练应包括回转,上下,左右的摇晃,有助于前庭系统的发展,对安定姿势和制平衡的能力,有功效的训练项目可安排大笼球,摇木马,旋转盘,平衡台,跳床,滑板,吊竖筒等.静态训练主要是加强对自己身体各部分位置的认知,在"动","静'协调运动时,掌握站,坐,卧位的正常姿势的保持.在触觉学习训练中,以改善触觉防御过度,改善人际关系为主要目的,训练项目可安排有各种不同触觉的刺激:温,冷,湿,压等固有感觉,用不同的教具如沙土,粘土,棕刷,毛巾,地毯,木块,铁块等做游戏.洗澡时磨擦身体肌肤,抓痒,口腔周围的面肌触摸,舌头的运动等都有助于触觉健全和敏感抑制.空间知觉一强化训练:眼球运动改善,视知觉的学习训练,提高空间认知,距离判断能力,使视一动协调更顺畅,眼一手配合更精确."静"态训练的游戏可做拼图接龙,连点线成图,平衡台接投球,趴地推球,立定投篮等项目."动"态训练的游戏可做跳床,跳床上边跳边接投球,滑板,推击障碍物,有助于空间距离觉及判断力的发展. 四,ADHD儿童的感觉统合治疗:对具有感觉统合障碍的ADHD儿,治疗的最终目的是改善ADHD儿大脑神经系统的统合功能,根据每一个ADHD 儿所存在的问题,进行有目的,有计划的感觉统合训练,这对提高ADHD儿的语言,认知,思考等学习能力,是一种行之有效的方法.感觉统合训练方法如下:1.触觉刺激的训练触觉在人类感觉系统机能中占有很重要的位置.胎儿在胎内的感觉体验,出生时通过产道的感觉体验,出生后与外界的温度,事物,以及和他人皮肤接触的感觉体验等,这对提高胎儿和新生儿神经系统的机能起着重要的作用.触觉刺激对于ADHD儿神经系统整体感觉的统合以及感觉认知,感觉运动起作用.如用软毛刷,干毛巾或丝稠等柔软的布类,轻擦孩子的背部,腹部,腕部,颜面部,手,脚等部位的皮肤.手背及前腕部是触觉防卫最小的部位,由于这些部位是和正常的环境相互作用接触最多的部位,而身体的腹侧部,颜,足部位对刺激敏感,触觉防卫大,往往是难以接受的部位。

adhd课程设计一、课程目标知识目标:1. 学生能够理解ADHD(注意力缺陷多动障碍)的定义、症状及影响。
2. 学生能够掌握识别和区分ADHD与一般儿童行为的技巧。
3. 学生能够了解ADHD的成因、治疗方法及教育干预策略。
技能目标:1. 学生能够运用所学知识分析并评估同伴的行为,判断是否可能存在ADHD 症状。
2. 学生能够设计并实施适合ADHD患者的学习活动和心理支持方案。
3. 学生能够运用沟通技巧,与ADHD患者建立良好的人际关系,提供适当帮助。
情感态度价值观目标:1. 培养学生对ADHD患者的同理心,消除歧视和误解,形成关爱和支持的态度。
2. 培养学生关注特殊教育群体,提高社会责任感和关爱他人的意识。
3. 培养学生认识到每个人的独特性,尊重差异,学会包容和接纳。
课程性质:本课程以科普教育为主,结合心理学、教育学等多学科知识,旨在提高学生对ADHD的认识和理解。
学生特点:考虑到学生所在年级的特点,课程内容以生动、形象的方式呈现,结合实际案例,提高学生的学习兴趣和参与度。
教学要求:教师应注重启发式教学,引导学生主动思考、提问,注重培养学生的实践操作能力和团队合作精神。
同时,关注学生的情感态度变化,适时进行调整和引导,确保课程目标的实现。
通过对课程目标的分解,为教学设计和评估提供明确的方向。
二、教学内容1. ADHD基础知识:- ADHD的定义、症状及分类- ADHD的成因及影响因素- ADHD的发病率及性别、年龄差异2. ADHD的识别与评估:- 行为观察与记录- 评估工具的使用(如:儿童行为评定量表)- ADHD与一般儿童行为的区别3. ADHD的治疗与教育干预:- 药物治疗与非药物治疗- 教育干预策略(如:行为疗法、学习辅导)- 家庭、学校及社会支持体系的作用4. 个性化教育方案设计:- 针对ADHD学生的教学策略- 学习环境与课堂管理的调整- 与ADHD学生有效沟通的技巧5. 案例分析与实操演练:- 分析真实案例,了解ADHD学生的需求- 设计实际操作活动,提升学生解决问题的能力- 团队合作,开展模拟教学活动教学内容依据课程目标,结合教材相关章节,进行科学、系统地组织。
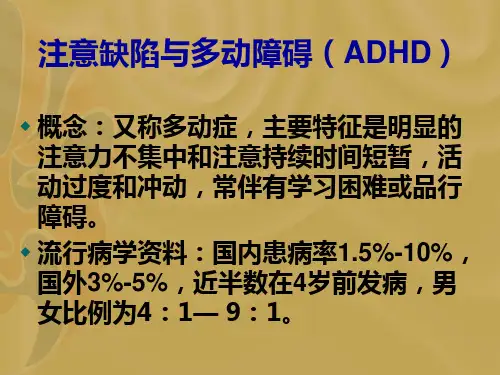
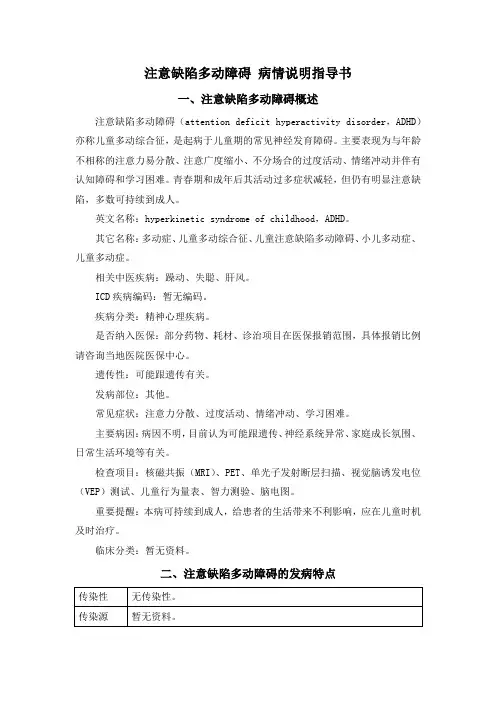
注意缺陷多动障碍病情说明指导书一、注意缺陷多动障碍概述注意缺陷多动障碍(attention deficit hyperactivity disorder,ADHD)亦称儿童多动综合征,是起病于儿童期的常见神经发育障碍。
主要表现为与年龄不相称的注意力易分散、注意广度缩小、不分场合的过度活动、情绪冲动并伴有认知障碍和学习困难。
青春期和成年后其活动过多症状减轻,但仍有明显注意缺陷,多数可持续到成人。
英文名称:hyperkinetic syndrome of childhood,ADHD。
其它名称:多动症、儿童多动综合征、儿童注意缺陷多动障碍、小儿多动症、儿童多动症。
相关中医疾病:躁动、失聪、肝风。
ICD疾病编码:暂无编码。
疾病分类:精神心理疾病。
是否纳入医保:部分药物、耗材、诊治项目在医保报销范围,具体报销比例请咨询当地医院医保中心。
遗传性:可能跟遗传有关。
发病部位:其他。
常见症状:注意力分散、过度活动、情绪冲动、学习困难。
主要病因:病因不明,目前认为可能跟遗传、神经系统异常、家庭成长氛围、日常生活环境等有关。
检查项目:核磁共振(MRI)、PET、单光子发射断层扫描、视觉脑诱发电位(VEP)测试、儿童行为量表、智力测验、脑电图。
重要提醒:本病可持续到成人,给患者的生活带来不利影响,应在儿童时机及时治疗。
临床分类:暂无资料。
二、注意缺陷多动障碍的发病特点三、注意缺陷多动障碍的病因病因总述:本病病因和发病机制尚不清楚,目前认为可能跟遗传、神经系统异常、家庭成长氛围、日常生活环境等有关。
这些因素可单独存在,也可综合致病。
基本病因:1、遗传ADHD具有家族聚集现象,患者双亲患病率20%,一级亲属患病率10.9%,二级亲属患病率4.5%。
同卵双生子同病率51%~64%,异卵双生子同病率33%。
2、神经系统相关影响因素(1)神经发育异常:磁共振成像发现患者额叶发育异常,胼胝体和尾状核体积减小。
功能磁共振研究报道本病患儿尾状核、额区、前扣带回代谢减少。
ATTENTION DEFICIT HYPERACTIVITY DISORDERKEY FACTS■Attention deficit hyperactivity disor-der (ADHD) is one of the most com-monly diagnosed mental disordersin U.S. children and adolescents,affecting up to 3 to 5 percent ofschool-age children (Cantwell,1996; Wolraich et al., 1996).■There is no single diagnostic tool forADHD. To diagnose the disorder, ahealth professional considers achild’s or adolescent’s history andsymptoms and rules out otherpotential causes of inattention,hyperactivity, and impulsivity.■The exact cause of ADHD is notknown. Children and adolescentswith ADHD may have low levels ofcertain neurotransmitters in brainregions controlling attention andimpulsivity.■Many children and adolescents withADHD improve as they grow up.One-third have no symptoms bythe time they reach adulthood(Cantwell, 1996; Dulcan, 1997).■Children and adolescents withADHD are at risk for school under-performance, social isolation, andlow self-esteem.DESCRIPTION OF SYMPTOMSInattention, hyperactivity, and impulsivity problems fall along a continuum. For some children and ado-lescents such symptoms do not impair functioning enough to warrant a diagnosis of ADHD, but the symp-toms nevertheless cause frustration in the child or adolescent or those near her, or impede her learning to some degree. DSM-PC describes these inattention and hyperactivity/impulsivity problems as follows.When a child’s or adolescent’s inattention and/or hyperactivity and impulsivity occur in many different settings over a long period and impair his functioning, this indicates that he may have a disorder rather than a problem. In order to meet the criteria for ADHD, these symptoms need to have been present before age 7.Further information on the diagnosis of ADHD is available in the American Academy of Pediatrics’ clinical practice guide-lines, “Diagnosis and Evaluation of the Child with Attention-Deficit/Hyperactivity Disorder” (American Academy of Pediatrics, 2000); Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment(Barkley, 1998); Diagnosis and Treatment of Attention Deficit Hyperactivity Disorder (ADHD): NIH Consensus Statement(1998); and “Practice Parameters for the Assessment and Treatment of Children, Adolescents, and Adults with Attention-Deficit/Hyperactivity Disorder” (Dulcan, 1997).Description of Symptoms (continued)INTERVENTIONSThese general interventions may help primary care health professionals to identify children and adolescents with ADHD and related problems and to manage their symptoms. (See Bright Futures Case Studies for Primary Care Clinicians:Attention-Deficit/Hyperactivity Disorder: The Restless Pupil [Frazer and Knight, 2001] at http://www.pedicases. org.)Child or Adolescent1.If the school or family expresses concern about achild’s or adolescent’s disruptive behavior orinattention, or if screening questions reveal con-cerns in these areas, further information should be gathered. Scales for assessing ADHD includethe Vanderbilt ADHD Diagnostic Teacher Rating Scale (Wolraich, 1998), SNAP-IV (Swanson,1991), ADHD Rating Scale-IV (DuPaul, 1998), and Conners’ Rating Scales (Conners, 1997). For achild or adolescent to meet the criteria forADHD, his symptoms need to be present in sever-al different settings, including home and school.Therefore, obtaining information from theschool as well as the child or adolescent and fam-ily is critical. Rating scales, report cards, and writ-ten and/or verbal comments from schoolpersonnel about a child’s or adolescent’s presen-tation and performance provide a fuller picture of his academic and behavioral functioning. Psy-choeducational testing should also be considered to identify any learning disabilities that may be affecting academic performance. Obtain a careful social history from the family to identify anyongoing or recent stressors that may also beaffecting the child’s or adolescent’s functioning(American Academy of Pediatrics, 2000). (SeeTool for Health Professionals: Vanderbilt ADHD Diagnostic Teacher Rating Scale, Mental HealthTook Kit, p. 54.)2.Assess for the following other possible underlyingor associated medical or psychosocial concerns:•Low birthweight•Mental retardation•Drug or alcohol exposure in utero•Neurotoxin exposure (e.g., lead poisoning)•Central nervous system infections•Head injury•Thyroid dysfunction•Child abuse and neglect•Foster home placements3.Assess for mood problems and disorders by ask-ing the child or adolescent about his mood, abili-ty to have fun, and sleep. Assess for anxietyproblems and disorders by asking about worries, separation problems, and somatic complaints.Children and adolescents with symptoms ofADHD and depression or anxiety present particu-lar diagnostic and treatment challenges. A mental health professional such as a child psychiatrist,child psychologist, or clinical social worker who engages with a child or adolescent in individual consultation and therapy may be able to helpclarify diagnoses, develop a treatment plan, and stabilize symptoms. Medication interventions fora child or adolescent with ADHD and anxiety ormood symptoms can be complicated. Referral to or consultation with a child psychiatrist or devel-opmental-behavioral pediatrician is recommend-ed. (See Pharmacological Interventions, p. 210.)ADHD4.Children and adolescents with ADHD may also benefit from individual or group therapy that focuses on •Learning impulse control •Building self-esteem •Acquiring coping skills •Building social skills5.Children with ADHD may feel that they are “bad”because of their social and academic difficulties.Adolescents may experience feelings of failure and low self-esteem. Talk with the child or adolescent in developmentally appropriate language about ADHD and its treatment, explaining that you know he does not mean to cause problems but needs help to control his behavior and to focus.6.Encourage the child or adolescent to break diffi-cult tasks up into manageable parts, take short breaks, and write homework assignments in a special notebook.7.Encourage the child or adolescent to pursue his talents and interests (e.g., drawing, learning to play the drums, taking karate classes). Successeswill boost his self-esteem and promote positive interactions with adults and peers.Family1.Parents may feel they are to blame for theirchild’s or adolescent’s behavior problems. High-light the child’s strengths and specific needs, and point out the parents’ skills in supervising and caring for the child or adolescent, even during challenging periods.2.Discuss with parents any concerns they have about ADHD and about handling their child’s or adolescent’s behavior. Help parents give their child or adolescent positive feedback, communi-cate realistic and clear expectations, and set con-sistent and appropriate limits. For children and adolescents with significant behavior problems,consider referring parents to a developmental-behavioral pediatrician or a mental health profes-sional (e.g., child psychiatrist, child psychologist,clinical social worker), who can assist the family in developing a behavior plan for their child or adolescent.3.Encourage parents to establish routines for their child or adolescent to help her learn organiza-tional skills. It may be useful for parents to draw or write the routine and display it at home (e.g.,for a younger child, create a chart that shows brushing teeth, washing face, getting pajamas;for an older child or adolescent, create a chart illustrating the child’s or adolescent’s and fami-ly’s daily and weekly schedule).4.Ask about a family history of ADHD, learning dis-orders, depression, and anxiety. Explain that the family needs to help the child or adolescent com-pensate for ADHD (e.g., by finding activities thatbuild on her interests and strengths) and thatADHD can improve over time.5.Talk with parents about the role of medication intreating ADHD. Explain that it is often helpfulbut is not a cure. Children and adolescents with ADHD benefit most from a combination ofefforts by their family, their school, and healthprofessionals.6.Help family members identify the child’s or ado-lescent’s talents, stressing the importance ofbuilding self-esteem. Physical activities (e.g.,organized sports, biking, dancing, in-line skating, jumping rope, bowling) can help channel highenergy levels in children and adolescents withhyperactivity or impulsivity, and structuredgroup activities can promote social skills. Remind families that safety gear is especially importantfor children and adolescents with ADHD.7.Assess the quality of the relationship betweeneach parent and the child or adolescent, andencourage parents to spend regular time withtheir child or adolescent. For many male children and adolescents with ADHD, time spent playing or engaging in other activities with their father or another positive male role model is especiallyimportant.cate family members about ADHD, and con-nect them with supportive resources, such asChildren and Adults with Attention Deficit/Hyperactivity Disorder (CHADD). Informationabout CHADD can be found on the organiza-tion’s Web site at .9.Refer parents or siblings experiencing high levelsof stress, difficulty coping, or psychiatric symp-toms to a mental health professional such as aclinical social worker, psychologist, or munity and School1.After obtaining appropriate permission, involveteachers, guidance counselors, and school-based health and mental health professionals in assess-ing the child’s or adolescent’s functioning and in implementing a treatment plan.2.Assess for any possible learning disabilities or spe-cial education needs (DuPaul and Stoner, 1994).Public schools are obligated to assess childrenwhose school performance may be impaired by ADHD or a learning disability. For example, achild or adolescent suspected of having ADHDshould receive a functional behavioral assess-ment conducted by a qualified school profession-al (e.g., school psychologist) to help design abehavior modification program for the class-room. Be aware that children and adolescentswith ADHD may be eligible for special education services under the “other health impaired” dis-ability category. These services include the devel-opment of an Individualized Education Program (IEP). (See Tool for Families: Individualized Edu-cation Program [IEP] Meeting Checklist, Mental Health Tool Kit, p. 120.) Some parents may appre-ciate assistance from the primary care health pro-fessional in contacting the school. Considerparticipating in school conferences or IEP plan-ning meetings for the child or adolescent. Ensure that parents know that their child or adolescent may also qualify for services under Section 504 of the Rehabilitation Act. For further informationabout eligibility and services, families can consult the school’s special education coordinator, thelocal school district, the state department of edu-cation’s special education division, the U.S.Department of Education’s Office of Special Edu-cation Programs (/offices/OSERS/OSEP), the Individuals with DisabilitiesEducation Act (IDEA) ’97 Web site (http://www./offices/OSERS/IDEA), or the U.S. JusticeDepartment’s Civil Rights Division (http://www./crt/edo).3.Work with the school to develop a plan to reducedistracting stimuli for the child or adolescent as much as possible and to ensure that expectations are reinforced clearly and consistently. Suggestthat classroom seating be arranged to address the child’s or adolescent’s needs. Talk with theschool about providing children or adolescents with ADHD with extra support at transitiontimes during the school day.4.Encourage teacher-parent communication, andsuggest that the child or adolescent work onimproving organizational skills by keeping a“homework notebook” in which she recordsassignments and in which parents and teachers record ideas, observations, and praise pertaining to her successes. Suggest that homework time be broken up into 10- to 30-minute chunks withshort breaks in between for play or rest.5.For a child or adolescent who is taking medica-tion for ADHD symptoms, contact should bemaintained with teachers and/or other schoolpersonnel (e.g., the school nurse), to obtaininformation about possible changes in the child’s or adolescent’s classroom behavior and academic performance. Because the time course of somestimulant medications (e.g., methylphenidate) is relatively brief, teachers’ input about the medica-tion’s effectiveness is important. Behavior rating scales like the Conners’ Rating Scales (Conners, 1997) can assist teachers in providing informa-tion about behavior change. In addition, possible changes in the child’s or adolescent’s academic performance (e.g., the amount of work complet-ed correctly) should be assessed, as academic per-formance could be improved or deleteriouslyaffected by stimulant medication.6.For children under age 5, intervention servicesmay be available through IDEA. The local school district or the state department of education can provide specific information about availableresources. (See #2, above.)7.ADHD self-help groups such as CHADD can pro-vide information, referrals, and support services.PHARMACOLOGICAL INTERVENTIONSChildren and adolescents with ADHD usually require multiple interventions to address their diffi-culties. It has been shown that pharmacological interventions can be effective in improving func-tioning in children and adolescents with ADHD. Guidelines for considering a medication trial are offered below.•Given the prevalence of ADHD and its respon-siveness to stimulant medication, primary carehealth professionals may consider a medication trial. For further information on the use of med-ications and the treatment of ADHD, see Ameri-can Academy of Pediatrics (2001), Dulcan (1997), Morgan (1999), Spencer et al. (2000), and Wilens (1999). Ongoing communication with the child’s or adolescent’s family and school (followingguidelines for confidentiality) via mechanismssuch as rating scales is essential in monitoring a child’s or adolescent’s response to medications.•Children and adolescents who do not respond toa stimulant trial, who experience adverse effects,or who show evidence of mood or anxiety symp-toms, substance abuse, developmental delays, tic disorders, or significant family stress may becomplicated to treat. Some primary care health professionals feel comfortable treating children and adolescents with ADHD complicated byother associated problems. For those who do not, referral to a developmental-behavioral pediatri-cian, child neurologist, or child psychiatrist isrecommended.Resources for FamiliesChildren and Adults with Attention Deficit/ Hyperactivity Disorder (CHADD)8181 Professional Place, Suite 201Landover, MD 20785Phone: (800) 233-4050, (301) 306-7070Web site: LD OnLineWeb site: (LD OnLine is a service of the Learning Project at WETA, Washington, DC, in association with the Coordinated Campaign for Learning Disabilities.)National Attention Deficit Disorder Association (NADDA)1788 Second Street, Suite 200Highland Park, IL 60035Phone: (847) 432-ADDA (2332)Web site: Selected BibliographyAmerican Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Attention-Deficit/Hyperactivity Disorder. 2000. Clinical practice guide-line: Diagnosis and evaluation of the child withattention-deficit/hyperactivity disorder. Pediatrics105(5):1158–1170. Web site: http://www.aap.org/policy/ac0002.html.American Academy of Pediatrics, Committee on Quality Improvement, Subcommittee on Attention-Deficit/Hyperactivity Disorder. 2001. Clinical practice guide-line: Treatment of the school-aged child with atten-tion-deficit/hyperactivity disorder. Pediatrics108(4):1033-1044. Web site: /policy/s0120.html.American Psychiatric Association. 1994. Diagnostic and Sta-tistical Manual of Mental Disorders(4th ed.) (DSM-IV).Washington, DC: American Psychiatric Association.American Psychiatric Association. 2000. Diagnostic and Statistical Manual of Mental Disorders(4th ed., textrevision) (DSM-IV-TR). Washington, DC: AmericanPsychiatric Association.Barkley RA. 1998. Attention Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment(2nd ed.). NewYork, NY: Guilford Press.Barkley RA. 2000. T aking Charge of ADHD: The Complete, Authoritative Guide for Parents(rev. ed.). New York,NY: Guilford Press.Biederman J. 1998. Attention-deficit/hyperactivity disor-der: A life-span perspective. Journal of Clinical Psychiatry 59(7Suppl.):4S–16S.Biederman J, Faraone SV, Mick E, et al. 1999. Clinical cor-relates of ADHD in females: Findings from a largegroup of girls ascertained from pediatric and psychi-atric referral sources. Journal of the American Academy of Child and Adolescent Psychiatry38(8):966–975. Cantwell DP. 1996. Attention deficit disorder: A review of the past 10 years. Journal of the American Academy ofChild and Adolescent Psychiatry35(8):978–987. Conners CK. 1997. Conners’ Rating Scales (revised CRS-R, long version). North Tonawanda, NY: Multi-HealthSystems. Phone: (800) 456-3003; Web site: http://www.mhs.co.Diagnosis and treatment of attention deficit hyperactivity disorder (ADHD): NIH consensus statement.1998.16(2):1–37. Web site: /consensus/cons/110/110_intro.htm.Dulcan M. 1997. Practice parameters for the assessment and treatment of children, adolescents, and adultswith attention-deficit/hyperactivity disorder. Journalof the American Academy of Child and Adolescent Psychi-atry36(10Suppl.):85S–121S.DuPaul GJ. 1998. A DHD Rating Scale-IV: Checklists, Norms and Clinical Interpretation.New York, NY: GuilfordPress.DuPaul GJ, Stoner GD. 1994. ADHD in the Schools: Assess-ment and Intervention Strategies.New York, NY: Guil-ford Press.Frazer C, Knight JR. 2001. Attention-deficit/hyperactivity disorder: The restless pupil. In Knight JR, Frazer C,Emans SJ, eds., Bright Futures Case Studies for PrimaryCare Clinicians: Child Development and Behavior.Boston, MA: Bright Futures Center for Education inChild Growth and Development, Behavior, and Ado-lescent Health. Web site: .Jensen PS, Martin D, Cantwell DP. 1997. Comorbidity in ADHD: Implications for research, practice, and DSM-V. Journal of the American Academy of Child and Adoles-cent Psychiatry36(8):1065–1079.Kaplan HI, Sadock BJ. 1995. Comprehensive Textbook of Psychiatry(6th ed.). Baltimore, MD: Williams &Wilkins.Morgan AM, ed. 1999. Attention-deficit/hyperactivity dis-order. Pediatric Clinics of North America46(5).Philadelphia, PA: W. B. Saunders.Spencer T, Biederman J, Wilens T. 2000. Pharmacothera-py of attention-deficit/hyperactivity disorder. Childand Adolescent Psychiatry Clinics of North America9(1):77–97.Swanson JM. 1991. The SNAP-IV Teacher and Parent Rat-ing Scale. Irvine, CA: University of California. Website: .Wilens TE. 1999. Straight Talk About Psychiatric Medica-tions for Kids.New York, NY: Guilford Press. Wolraich ML. 1998. Vanderbilt Teacher Behavior Evalua-tion Scale (VTBES).Nashville, TN: Vanderbilt ChildDevelopment Center. Web site: http://peds.mc./VCHWEB_1/rating~1.html.Wolraich ML, Felice ME, Drotar D, eds. 1996. The Classifi-cation of Child and Adolescent Mental Diagnoses in Pri-mary Care: Diagnostic and Statistical Manual for Primary Care (DSM-PC) Child and Adolescent Version.Elk Grove Village, IL: American Academy of Pediatrics.。
拓德注意缺陷多动障碍评定量表《深入理解拓德注意缺陷多动障碍评定量表》一、引言拓德注意缺陷多动障碍(ADHD)是一种常见的儿童和青少年心理障碍,其特征包括注意力不集中、多动和冲动行为。
在临床实践中,对ADHD进行评估是至关重要的,而拓德注意缺陷多动障碍评定量表(ADHD Rating Scale-IV)是一种常用的评定工具。
本文将深入探讨ADHD评定量表的使用和意义,帮助读者更全面地理解ADHD的评定和诊断。
二、ADHD评定量表的基本信息1. ADGD评定量表的概述- ADHD评定量表是一种由专业人士用于评估儿童和青少年ADHD症状的标准化工具,它包括对于症状的观察和家长或老师的问卷调查。
2. 评定量表的历史与发展- ADHD评定量表最早由心理学家约瑟夫·B·科尔施(Joseph B. Coresh)和其他专家于1981年首次提出。
3. 评定量表的结构和特点- ADHD评定量表主要包括对于ADHD核心症状的评估,如注意力不集中、多动和冲动行为的观察和描述。
评定者需要根据儿童或青少年的行为表现进行评分,以判断其是否存在ADHD症状。
三、ADHD评定量表的使用方法和注意事项1. 评定流程- 对于儿童和青少年进行ADHD评定时,评定者需要深入了解被评定者的行为表现,并结合家长和老师的反馈进行分析和判断。
2. 评分标准- ADHD评定量表包含一系列针对症状的具体问题,评定者需要根据被评定者的具体表现进行评分,并根据评分标准进行判断。
3. 注意事项- 在使用ADHD评定量表时,评定者需要注意评定者的芳龄、性别、文化背景等因素,以避免评定偏差。
四、ADHD评定量表的意义和作用1. 评定的临床意义- ADHD评定量表是临床评定ADHD的重要工具,它能够帮助评定者全面地了解被评定者的ADHD症状表现,为后续的诊断和治疗提供重要参考。
2. 评定结果的应用- 评定结果可以为医生和专业人士提供诊断和干预方案的重要依据,帮助被评定者及其家人更好地理解和应对ADHD问题。
注意缺陷-多动障碍(A D H D)评估表编号:注意缺陷-多动障碍(ADHD)评估表—父母问卷(共2页)姓名_________ 性别____ 年龄____ 年级______ 出生日期________ 填表日期________提示:在填写此表格时,请根据你的孩子过去6个月的行为举止来认真填写此表格。
此评估建立于当你的孩子――用药期间――非用药期间――不肯定症状从不偶尔经常频繁1.不能仔细注意细节或常发生粗心大意所致的错误0 1 2 3 2在学习工作或活动时,注意力难以持久0 1 2 33.与之对话时,心不在焉,似听非听0 1 2 34.不听从指令而难以完成各项工作和任务(并非因为不理解教导所致)0 1 2 35.难以完成或组织各项工作和活动0 1 2 36.逃避、不喜欢或不愿参加那些需要精力持久的工作或活动0 1 2 37.遗失作业或活动所需要的东西,如玩具,作业本,铅笔或课本0 1 2 38.易因声音或其它外界刺激而分心0 1 2 39.遗忘日常活动0 1 2 310.手或足有很多小动作,或在座位扭动0 1 2 3 11在要求安坐的场合擅自离开座位0 1 2 312.在要求坐好的场合奔来奔去或爬上爬下0 1 2 313.不能安静地参加游戏或活动0 1 2 314.似被发动机驱动地一刻不停地活动0 1 2 315.讲话过多0 1 2 316.在他人问题还没问完时就急于回答0 1 2 317.难以静侯轮换0 1 2 318.在他人交谈时插嘴或打断他人的活动0 1 2 319.与成人争论0 1 2 320.发脾气0 1 2 321.经常拒绝大人的要求或不听规劝0 1 2 3 22故意激怒他人0 1 2 323.把自己的过错或无礼归咎于他人0 1 2 324.易被他人激怒或烦扰0 1 2 325.生气或愤恨0 1 2 326.不屑一顾或冷漠0 1 2 327.恃强凌辱弱,威胁或恐吓他人(如:坑别人)0 1 2 328.攻击行为0 1 2 329.为脱离烦恼或逃避责任而说谎0 1 2 330.未经批准逃学0 1 2 331.对人残忍0 1 2 332.偷窃有价值的东西0 1 2 333.故意损毁公物或他人的财产012334.使用可致严重伤害的武器如棒,刀,砖,枪等0 1 2 335.残忍对待动物0 1 2 336.纵火以至造成损害0 1 2 337.擅自闯入他人的房屋,商铺,汽车0 1 2 338.未经允许而夜归0 1 2 339.半夜离家出走0 1 2 340.强迫他人进行性活动0 1 2 341.恐慌,焦虑,或担心0 1 2 342.因害怕犯错而不敢尝试新事物0 1 2 343.自觉无用或自卑0 1 2 344.自责,内疚0 1 2 345感到孤独\不受欢迎\或不被别人喜欢:抱怨“没人喜欢我”0 1 2 346.伤心,难过,抑郁0 1 2 347.多愁善感0 1 2 3学习成绩与社会职能分数优秀优良一般差很差48.总体成绩(如:总评) 1 2 3 4 549.语文 1 2 3 4 550.英语 1 2 3 4 551.数学 1 2 3 4 552.与父母关系 1 2 3 4 553.与兄弟姐妹关系 1 2 3 4 554.与同学关系 1 2 3 4 555.参加集体活动(如:团队精神) 1 2 3 4 5父母评语:以下为工作人员所填问题1-9中得分为2或3共几项:----------------------------------------------------------------- 问题10-18中得分为2或3共几项:-------------------------------------------------------------- 问题1-18中共有几项阳性症状------------------------------------------------------------------- 问题19-26中得分为2或3共几项:-------------------------------------------------------------- 问题27-40中得分为2或3共几项:-------------------------------------------------------------- 问题41-47中得分为2或3共几项:-------------------------------------------------------------- 问题48-55中得分为4或5共几项:-------------------------------------------------------------- 学习成绩平均得分-------------------------------------------------------------------------------------编号:注意缺陷-多动障碍(ADHD)评估表—教师问卷(共2页)学生姓名_____________ 性别______ 年级________ 老师姓名__________ 科目__________提示:请根据孩子入学以来或者最近6个月的举止行为来认真填写此表格。
此评估建立于当你的孩子――用药期间――非用药期间――不肯定症状从不偶尔经常频繁1.不能仔细注意细节或常发生粗心大意所致的错误0 1 2 32.在学习工作或活动时,注意力难以持久0 1 2 33.与之对话时,心不在焉,似听非听0 1 2 34.不听从指令而难以完成各项工作和任务(并非因为不理解指令)0 1 2 35.难以完成或组织各项工作和活动0 1 2 36.逃避,不喜欢或不愿参加那些需要精力持久的工作或活动0 1 2 37.遗失作业或活动所需要的东西,如玩具,作业本,铅笔或课本0 1 2 38.易因声音或其它外界刺激而分心0 1 2 39.遗忘日常活动0 1 2 310.手或足有很多小动作或在座位扭动0 1 2 311.在要求安坐的场合擅自离开座位0 1 2 312.在要求坐好的场合奔来奔去或爬上爬下0 1 2 313.不能安静地参加游戏或活动0 1 2 314.似被发动机驱动地一刻不停地活动0 1 2 315.讲话过多0 1 2 316.在他人问题还没问完时就急于回答0 1 2 317.难以静侯轮换0 1 2 318.在他人交谈时插嘴或打断他人的活动0 1 2 319.发脾气0 1 2 320.经常拒绝大人的要求或不听规劝0 1 2 321.生气或愤恨0 1 2 322.不屑一顾或冷漠0 1 2 323.恃强凌辱弱,威胁或恐吓他人0 1 2 324.对他人躯体攻击0 1 2 325.为获得利益或逃避责任而说谎(如:“坑”别人)0 1 2 326.对人残忍0 1 2 327.偷窃有价值的东西0 1 2 328.故意损毁公物或他人的财产012329.恐慌,焦虑,或担心0 1 2 3 30多愁善感0 1 2 3 31因怕犯错而不敢尝试新事物0 1 2 332.自觉无用或自卑0 1 2 333.自责,内疚0 1 2 334.感到孤独\不受欢迎\或不被别人喜欢:抱怨“没人喜欢我”0 1 2 335.伤心,难过,抑郁0 1 2 3 学习成绩优秀优良一般差很差36.阅读 1 2 3 4 537.数学 1 2 3 4 538.写作 1 2 3 4 5课堂行为及纪律平分优秀优良一般差很差39.与同学关系 1 2 3 4 540.听从指令 1 2 3 4 541.遵守课堂秩序 1 2 3 4 542.按时完成作业 1 2 3 4 543.组织技巧 1 2 3 4 5老师评语:以下为工作人员所填问题1-9中得分为2或3共几项:--------------------------------------------------------------------------问题10-18中得分为2或3共几项:-----------------------------------------------------------------------问题1-18中共有几项阳性症状----------------------------------------------------------------------------问题19-28中得分为2或3共几项:-----------------------------------------------------------------------问题29-35中得分为2或3共几项:-----------------------------------------------------------------------问题36-43中得分为4或5共几项:-----------------------------------------------------------------------学习成绩平均得分----------------------------------------------------------------------------------------------。