食管癌淋巴结三野清扫
- 格式:ppt
- 大小:3.19 MB
- 文档页数:25
全腔镜与开放食管癌三野淋巴节清扫术的临床应用与分析吴君旭;张明军;石开虎;赵旭东;沙纪名;汪裕琪;徐彪【摘要】To compare perioperative complications and curative effect analysis of 3-field lymphadenectomy in tho-racic esophageal carcinomas and thoracoscopes esophageal carcinomas, retrospective analysis of 826 cases of esoph-ageal cancer patients. 52 cases were executed with thoracic surgery and 21 patients were executed with full thoras-copic surgery. The thoracic surgery group in the operation time, hospitalization time, postoperative drainage, post-operative analgesic drug application time, thoracic drainage gallery extraction time were significantly longer than the thoracoscopic sugery group. The number of resected lymph nodes in the thoracoscopic surgery group were signifi-cantly more than in the thoracic surgery group. Cardiovascular complications, pulmonary complications and anasto-motic fistula in the thoracoscopic surgery group were significantly more than in the thoracic surgery group. Thoras-copic esophagectomy with 3-field lymphadenectomy was just a change in the way and worth promoting.%回顾性分析食管癌患者826例,其中行颈、胸、腹三切口食管癌三野淋巴结清扫术52例(开放组),全腔镜下三野淋巴结清扫术21例(腔镜组),比较全腔镜与开放手术在食管癌三野淋巴结清扫术中围术期并发症发生情况与疗效分析。
二野清扫术和三野清扫术在胸中段食管癌淋巴结中的应用对比目的在胸中段食管癌淋巴结中分别应用二野清扫术和三野清扫术,比较分析应用效果。
方法选取2016年5月~2018年4月作为我院收治的胸中段食管癌患者100例,随机分成对照组与观察组各50例,将二野清扫术应用在对照组中,将三野清扫术应用到观察组中,比较两组患者的淋巴结清扫情况。
结果相较于观察组,对照组的淋巴结清扫数明显较低,差异有统计学意义(P<0.05);手术结束后,观察组患者的并发症发生率高于对照组,差异有统计学意义(P<0.05)。
结论在胸中段食管癌淋巴结中应用三野清扫术的效果较好,淋巴结清扫数目更多,且安全性也更高。
标签:二野清扫术;三野清扫术;胸中段食管癌;淋巴结目前,食道癌已经成为了一种最为高发的恶性肿瘤,且具有较高的死亡率。
而在对食道癌进行治疗时,多采用手术根治性切除,但治疗效果仍不理想,且具有较高的复发率,导致患者病情复发的原因主要为试管癌淋巴结复发。
为此,这也就使得胸中段食管癌患者淋巴結的清扫工作成为了一项至关重要的工作[1]。
在本文中就从我院选取100例胸中段食管癌患者,比较分析了二野清扫术与三野清扫术的清扫效果。
1 资料与方法1.1 一般资料选取2016年5月~2018年4月作为我院收治的胸中段食管癌患者100例,随机分成对照组与观察组各50例:对照组中有男性患者30例,女性患者20例,患者年龄介于42岁到71岁之间,平均年龄为(56.31±6.33)岁;观察组中有男性患者29例,女性患者21例,患儿年龄介于41岁到70岁之间,平均年龄为(55.29±6.31)岁。
比较两组患儿的基本情况(年龄、性别),差异不具有统计学意义(P>0.05),具有可比性。
1.2 方法将二野清扫术应用在对照组中,即右后外侧开胸联合上腹部正中切口;将三野清扫术应用到观察组中,即右后外侧开胸联合上腹部正中切口以及颈部U形切口[2]。
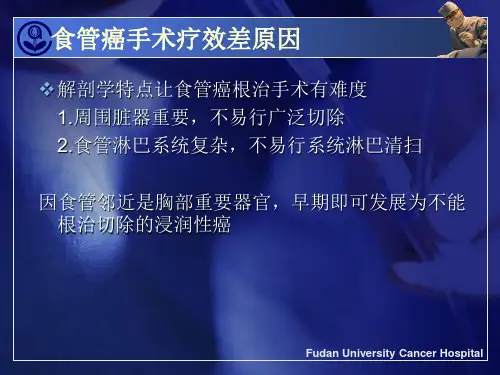
胸中上段食管癌三野淋巴结清扫及二野淋巴结清扫临床疗效比较佟倜;曹彬【摘要】目的:通过比较胸中上段食管癌三野淋巴结清扫及二野淋巴结清扫的结果,探讨胸中上段食管癌淋巴结清扫范围.方法:2008-2010年胸中上段食管癌手术治疗患者119例,接受三野淋巴结清扫术共46例(三野组),接受二野淋巴结清扫术共73例(二野组).结果:三野组患者淋巴结转移率(58.7%)明显高于二野组(39.7%)(P<0.05),主要差别在于三野组较高的颈部淋巴结转移率(21.7%)和较高的上纵隔淋巴结转移率,三野组与二野组患者上纵隔淋巴结转移率分别为28.2%和11.0%,组间比较差异有统计学意义(P<0.05).三野组及二野组患者术后并发症发生率分别为39.1%和16.4%,组间比较差异有统计学意义(P<0.01),2组差别主要体现为三野组患者较高的喉返神经损伤发生率.三野组及二野组患者术后1年生存率分别为95.6%和83.5%,三野组显著高于二野组(P<0.01).结论:与二野淋巴结清扫术比较,三野淋巴结清扫术能更彻底清扫颈部及上纵隔淋巴结,降低局部复发率,提高患者术后生存率,建议对排除远处转移的胸中上段食管癌患者行三野淋巴结清扫术.【期刊名称】《吉林大学学报(医学版)》【年(卷),期】2012(038)004【总页数】4页(P792-795)【关键词】食管鳞癌;三野淋巴结清扫术;二野淋巴结清扫术【作者】佟倜;曹彬【作者单位】吉林大学第二医院胸外科,吉林长春130041;吉林大学第二医院胸外科,吉林长春130041【正文语种】中文【中图分类】R735.1食管癌是我国常见的恶性肿瘤之一,外科手术切除仍是食管癌最主要的治疗方法。
经过70余年的发展,我国在食管癌的诊断和治疗方面取得了很大的进步,但是对于食管癌淋巴结清扫范围仍然存在较大争议[1]。
本文作者对2008—2010年在吉林大学第一医院和第二医院接受手术治疗的119例胸中上段食管癌患者进行回顾性分析,旨在探讨淋巴结清扫的合理范围。
全腔镜与开放食管癌三野淋巴结清扫术的临床应用摘要目的分析全腔镜下三野淋巴结清扫术应用于食管癌的疗效。
方法75例采用全腔镜下三野淋巴结清扫术治疗的食管癌患者作为观察组,71例采用颈、胸、腹三切口开放食管癌三野淋巴结清扫术治疗的食管癌患者作为对照组,对比两组患者的手术相关指标、并发症发生情况。
结果观察组手术时间(171.0±12.6)min、术中出血量(81.0±2.7)ml、住院时间(9.1±0.7)d、淋巴结清扫数(23.8±5.6)个、留置胸管时间(3.1±1.2)d、止痛药使用时间(2.6±0.2)d、并发症发生率5.33%均优于对照组的(263.0±35.7)min、(204.0±3.8)ml、(13.9±1.9)d、(17.3±3.4)个、(4.9±1.5)d、(5.7±0.8)d、21.13%,差异均具有统计学意义(P<0.05)。
结论全腔镜下三野淋巴结清扫术用于食管癌的治疗中安全、有效,值得临床治疗推广使用。
关键词全腔镜;三野淋巴结清扫术;食管癌食管癌是发生于食管上的一种恶性肿瘤,治疗方式有很多,如手术治疗、放疗、中药治疗、综合治疗等[1],但公认效果较好的是手术治疗。
20世纪末我国开始采用颈、胸、腹三切口开放食管癌三野淋巴结清扫术对食管癌进行治疗,近年来全腔镜下三野淋巴结清扫术开始应用于食管癌治疗中。
本研究通过对本院食管癌患者治疗方式的对比研究,探究全腔镜下三野淋巴结清扫术的应用效果,现报告如下。
1 资料与方法1. 1 一般资料选取2014年4月~2016年4月本院收治的146例行三野淋巴结清扫术患者,75例采用全腔镜下三野淋巴结清扫术治疗的食管癌患者作为观察组,71例采用颈、胸、腹三切口开放食管癌三野淋巴结清扫术治疗的食管癌患者作为对照组。
观察组中男39例,女36例;平均年龄(58.6±3.7)岁;其中Ⅰ期16例,Ⅱ期37例,Ⅲ期22例。

胸腔镜下食管癌三野清扫术的临床护理摘要:目的探讨在胸腔镜下行食管癌三野清扫术治疗的具体护理措施。
方法将我院2012.1-2015.1收治的68例食管癌患者作为本次研究观察对象,按住院床位单双号分为A、B两组,分别给予开胸手术及常规护理与胸腔镜下食管癌三野清扫术与围术期系统化护理,分析两组患者术后恢复情况,以评估两种治疗护理方法的应用效果。
结果 A组患者在术后胸导管拔除时间、术后疼痛程度以及住院恢复时间上均落后于B组,差异显著(P<0.05)。
结论行胸腔镜下食管癌三野清扫术配合围术期系统化护理,可有效降低术后疼痛与其他并发症出现,缩短住院时间,促进患者病情恢复,建议推广。
关键词:胸腔镜;食管癌三野清扫术;护理食管癌是临床消化内科常见的恶性肿瘤之一,患者早期症状无特异性,一旦出现吞咽困难预示病情已进入中晚期,因此针对该病需早诊断、早治疗[1]。
目前治疗食管癌的原则还是以手术切除为主,但随着人们生活水平的日益提升,人们的观念已逐渐从疾病生存期转移至预后生活质量上。
传统开胸手术对患者创伤较大,术后并发症多,不利于术后康复,而随着腔镜技术的不断成熟,通过胸腔镜进行食管癌三野清扫术,可彻底清除病灶,并进行相对系统化的淋巴结清扫,且已被大量实验证明为可提高食管癌远期疗效的可靠手术[2]。
但手术仍然存在一定的风险与并发症情况,护理工作也因此发挥其重要作用,现就胸腔镜下行食管癌三野清扫术采取相应的护理措施进行讨论,总结如下。
1 资料与方法1.1 一般资料将2012.1-2015.1我院收治并经相关检查确诊为食管癌的68例患者,所选患者均为自愿参与,并与家属共同签署知情同意书。
将其护理方式的不同分为A、B两组各34例,A组患者中男性25例,女性9例,年龄42~75岁,中位年龄53.5岁,B组患者中男性23例,女性11例,年龄44~76岁,中位年龄54.5岁,收集两组患者的一般资料不具备显著性差异(P>0.05),存在可比性。
食管癌三野淋巴结清扫的临床探讨【摘要】目的探讨食管癌三野淋巴结清扫的临床应用。
方法颈部B 超检查,发现淋巴结长径≥1 cm,短径长径>0.5 的患者行三野淋巴结清扫,为三野淋巴结清扫组79例,余行二野淋巴结清扫,为二野淋巴结清扫组89例。
结果二野淋巴结清扫组喉返神经损伤发生率10.11%,三野淋巴结清扫组喉返神经损伤发生率22.78%,两组比较差异有统计学意义(P<0.05)。
两组颈部淋巴结复发比较差异有统计学意义(P<0.05)。
结论食管癌三野淋巴结清扫能够显著的降低颈部淋巴结复发,减少术后的复发可以延长患者生命,改善患者生活质量,术中应解剖知识全面、严格操作技巧减少并发症发生。
【关键词】食管癌;三野淋巴结清扫;临床探讨中国是世界上食管癌高发地区之一,全世界每年死于食管癌约30 万人,食管癌死亡占全国恶性肿瘤死亡率的21.8%,仅次于胃癌,居第二位[1]。
食管癌目前最有效的治疗手段仍为手术根治性切除,然而远期效果并不理想。
淋巴道转移是食管癌常见的转移方式。
淋巴结状态是影响患者术后的生存情况的最重要预后因素,淋巴结切除的范围对手术食管癌存在着争议,三野清扫可提高食管癌分期的准确性、局部控制率及患者长期生存率哺,但该术式有较高的并发症发生率和病死率。
为了探讨食管癌三野淋巴结清扫的临床应用,我们对此进行了研究,现汇报如下。
1 资料与方法1.1 一般资料本组病例来自2004年1月至2010年1月收治的食管癌168例。
其中男108例,女60例。
胸上段38例,胸中段64例,胸下段66例;肿瘤长度3~11 cm,平均5.8 cm。
组织分化程度:高分化35例,中分化83例,低分化50例。
肿瘤浸润深度T1期18例,T2期50例,T3期74例,T4期26例。
1.2 方法1.2.1 分组所有病例进行颈部B 超检查,发现淋巴结长径≥1 cm,短径长径>0.5 的患者行三野淋巴结清扫,为三野淋巴结清扫组79例,余行二野淋巴结清扫,为二野淋巴结清扫组89例。
胸腔镜下胸段食管鳞癌2.5野淋巴结清扫术与3野淋巴结清扫术对比摘要:目的:比较胸腔镜下胸段食管鳞癌2.5野淋巴结清扫术和3野淋巴结清扫术的治疗效果和并发症发生率。
方法:选取2015年6月至2020年6月在我院行胸腔镜下胸段食管鳞癌围手术期淋巴结清扫术的患者,分为2.5野组和3野组,分别采用对照研究的方法进行分析,对两组患者的术前、术中和术后情况进行对比分析。
结果:2.5野组患者手术时间短、术中出血量少、术后疼痛评分低、胸腔引流管拔除时间早、住院时间短,但术后淋巴结转移和远处转移率高于3野组。
两组患者在术后并发症的发生率、恢复时间和生存率方面无显著差异。
结论:3野淋巴结清扫术对胸段食管鳞癌患者的淋巴结转移和远处转移率明显降低,但手术时间长、出血量多、疼痛评分高、床位占用时间长。
2.5野淋巴结清扫术可减轻患者手术创伤、加速术后康复,但需要更多的术后随访和治疗监测,尤其是对于高淋巴结转移患者。
关键词:胸腔镜,胸段食管鳞癌,淋巴结清扫,并发症,生存率Abstract:Objective: To compare the treatment effect and incidence of complications between video-assisted thoracoscopic surgery (VATS) for squamous cell carcinoma (SCC) of the thoracic esophagus with 2.5-station lymph node clearance and 3-station lymph node clearance.Methods: Patients who underwent VATS with lymph node clearance during surgery for SCC of the thoracic esophagus at our hospital from June 2015 to June 2020 were selected and divided into the 2.5-station group and the 3-station group. A comparative analysis was conducted through the method of controlled study to compare the preoperative, intraoperative, and postoperative situations of patients in the two groups.Results: Patients in the 2.5-station group had shorter operation time, less intraoperative bleeding, lower postoperative pain scores, earlier removal of chest drainage tube, shorter hospital stay, but higher rates of postoperative lymph node and distant metastasis compared with the 3-station group. There was no significant difference in the incidence of postoperative complications, recovery time, andsurvival rate between the two groups.Conclusion: The 3-station lymph node clearance can significantly reduce the lymph node and distant metastasis rates of SCC patients with thoracic esophagus, but it requires longer operation time, more intraoperative bleeding, higher pain scores, and longer bed occupancy time. The 2.5-station lymph node clearance can reduce surgical trauma and accelerate postoperative recovery but requires more postoperative follow-up and treatment monitoring, especially for patients with high lymph node metastasis.Keywords: Video-assisted thoracoscopic surgery, squamous cell carcinoma of thoracic esophagus, lymph node clearance, complications, survival ratVideo-assisted thoracoscopic surgery (VATS) has become increasingly popular for the treatment of squamouscell carcinoma of the thoracic esophagus due to its minimally invasive nature. However, the optimal extent of lymph node clearance during VATS remains controversial.Previous studies have shown that more extensive lymph node clearance can lead to improved survival rates in patients with esophageal cancer, but also result inlonger operation time, more intraoperative bleeding, higher pain scores, and longer bed occupancy time. These complications can negatively impact postoperative recovery and increase healthcare costs.On the other hand, the 2.5-station lymph node clearance, which involves removal of lymph nodes in the area surrounding the tumor and the stations immediately adjacent to it, has been found to reduce surgical trauma and accelerate postoperative recovery. However, this approach may require more postoperative follow-up and treatment monitoring, especially for patients with high lymph node metastasis.Therefore, the choice of lymph node clearance extent should be determined based on individual patient factors, such as tumor stage, lymph node involvement, and overall health status, as well as the surgeon's expertise and experience. Proper preoperative evaluation and postoperative care can also help minimize complications and improve prognosisAnother important factor that should be taken into consideration when performing lymph node clearance is the patient's age. Older patients may have poorer overall health and a higher risk of complications, such as wound infections, delayed wound healing, andcardiovascular events. Therefore, extensive lymph node dissection may not be appropriate for elderly or frail patients with limited life expectancy or significant comorbidities.Additionally, lymph node clearance may have some negative effects on the patient's quality of life. It can cause nerve damage, lymphedema, and decreased mobility and range of motion, especially in the upper extremities. Therefore, minimally invasive procedures, such as sentinel lymph node biopsy, should be used when appropriate to reduce the impact on the patient's daily activities and overall function.In conclusion, lymph node clearance is an important part of the surgical management of cancer, but its extent should be based on the patient's individual factors, tumor stage, and overall health status. Surgeons should use their expertise and experience to make the best decision for each patient, while also considering the potential negative effects on quality of life. Proper preoperative evaluation and postoperative follow-up can help minimize complications and improve care outcomesFurthermore, patients undergoing lymph node dissection should be provided with appropriate education onpotential complications and postoperative care. This may include instructions on wound care, monitoring for signs of infection or lymphedema, and steps to reduce the risk of developing complications such as deep vein thrombosis or pulmonary embolism. Patients should also be counseled on the potential impact of lymph node dissection on their quality of life, such as the risk of developing lymphedema and how to manage this condition.There is ongoing research aimed at improving the surgical management of cancer and reducing the morbidity associated with lymph node dissection. For example, sentinel lymph node biopsy is a relatively new technique that allows surgeons to identify thefirst lymph node(s) that are likely to contain cancer cells, allowing for more selective removal of lymph nodes, and reducing the risk of complications. Additionally, advances in imaging, such as the use of intraoperative near-infrared fluorescence imaging, are allowing surgeons to more accurately identify and remove cancerous tissue, while also minimizing the amount of surrounding healthy tissue that is removed.In summary, lymph node clearance is an important component of the surgical management of cancer, and should be tailored to the individual patient's needsand tumor characteristics. Surgeons should weigh the potential benefits and risks of lymph node dissection, and strive to reduce the morbidity associated withthis procedure. Patients should be educated on the potential complications associated with lymph node dissection and provided with appropriate postoperative care instruction. Advances in surgical techniques and imaging technologies are improving the accuracy and safety of lymph node dissection, and ongoing research in this area will continue to advance treatment options for patients with cancerIn conclusion, lymph node dissection remains an important diagnostic and staging tool for various types of cancer. While it is associated with potential benefits in terms of disease control and survival, it also carries risks and potential complications. Advances in surgical techniques and imaging technologies are helping to improve the accuracy and safety of this procedure, and ongoing research is needed to further optimize patient outcomes. Patients must also be aware of the potential complications and receive appropriate postoperative care to minimize the risks associated with this procedure。
微创三野淋巴结清扫治疗胸段食管癌的疗效任自学;张荣新;张安庆;张干;周经月;解明华;王圣应【摘要】Objective To explore the safety, effectiveness and economy of combined thoracoscopic and laparoscopic selective three-field lymphadenectomy with radical resection of esophageal carcinoma in the treatment of thoracic esophageal carcinoma. Methods The clinical data of 103 esophagectomy patients ever treated in our hospital from Jul 2012 to Feb 2016, with selective three-field lymphadenectomy by combined thoracoscopic and laparoscopic minimally invasive operation or open operation were retrospectively analyzed. The mortality rate, in-cidence of anastomotic leak, incidence of pulmonary infection, incidence of recurrent laryngeal nerve injury, number of harvested lymph nodes, and hospitalization costs between the patients with minimally invasive operation ( minimal invasion group, 48 cases) and the patients with open operation ( open operation group, 55 cases) were compared. Results There were statistically significant differences between the two groups in the incidence of arrhythmia, incidence of pulmonary infection, blood loss and operation time, incidence of hoarseness, while in the incidence of intraoperative death, chylothorax, dehiscence of abdominal incision, postoperative hemorrhoea and anastomotic leak, no signifi-cant difference was found. The minimal invasion group had a greater number of harvested lymph nodes with significant difference, and pa-tients in the group cost more in the hospitalization expense. Conclusion It is safe to applycombined thoracoscopic and laparoscopic minimally invasive three-field lymphadenectomy with radical resection of esophageal carcinoma in the treatment of thoracic esophageal carcinoma, but the hospitalization expense would be higher.%目的:探讨胸腹腔镜联合进行选择性三野淋巴结的食管癌根治术治疗胸段食管癌的安全性、有效性及经济性。
胸中上段食管癌三野淋巴结清扫及二野淋巴结清扫预后比较分析郭伟鹏【摘要】Objective To explore and analyze the prognosis of three-field lymph node dissection and two-field lymph node dissection for upper thoracic esophageal carcinoma. Methods 120 patients with esophageal carcinoma who were accepted by our hospital from October 2010 to October 2011 were selected as the research subject. They were randomly and equally divided into the three-field lymph node dissec-tion group and the two-field lymph node dissection group. Contrast the rate of lymph nodes metastasis, rate of surgical survival and complica-tions of two groups after treatment. Results After the operation treatment, cervical lymph node and mediastinal lymph node metastasis rates in were 18. 33% and 20. 00% respectively, and the total incidence of complications is 30. 00%. They were all lower than two-field lymph node dissection group. Meanwhile, the survival rate of three-field lymph node dissection group was 83. 33% which was obviously higher than 58. 33% in the two-field lymph node dissection group with a statistical significance (P<0. 05). Conclusion Three-field lymph node dis-section can effectively improve the prognosis and clinical curative effect in treatment of upper thoracic esophageal carcinoma.%目的:探讨并分析胸中上段食管癌三野淋巴结清扫及二野淋巴结清扫对患者的不同预后情况。