一例感染性心内膜炎患者的病例分析.pdf
- 格式:pdf
- 大小:3.49 MB
- 文档页数:23
结核性脑膜炎、浸润性肺结核-病例分析病史摘要:患者,女,36岁。
因头痛、呕吐、发热急诊入院。
患者于20多天前因受冷感冒头疼,伴有寒战、高热(体温不详),以后头痛加重,呈刺跳痛,尤其前额部明显。
10天前开始出现喷射性呕吐,呕吐物为食物残渣,无血。
当地医院诊断为“流感”,予以相应治疗(具体用药不详),症状未见明显改善。
2天前自觉双下肢麻木,乏力,急诊入安。
既往无特殊病史。
查体:体温40℃,脉率110/min。
慢性病容,消瘦,嗜睡,神志恍惚,合作欠佳,双眼无水肿,瞳孔等大对称,对光反射存在。
心肺检查无明显异常,腹部稍凹陷,全腹有压痛。
浅反射及腹壁反射减弱,浅感觉存在,膝反射及跟腱反射未引出,颈强直。
克氏征、布氏征阳性。
化验检查:WBC 9.2X109/L,N:0.5,L:0.14。
脑脊液压力高,细胞数高,查见抗酸杆菌。
X线检查:双肺上部各有一结节状阴影,边缘见模糊的云雾状阴影。
分析题:1、根据所学知识做出诊断并说明诊断依据。
2、根据病理学知识解释相应症状、体征、化验结果。
参考答案:1、结核性脑膜炎、浸润性肺结核。
依据:头痛、呕吐、发热;颈强直、克氏征、布氏征阳性;脑脊液压力高、查见抗酸杆菌;X线所见。
2、脑脊液循环障碍→颅内压升→头痛、呕吐;结核累及脑膜→脑膜刺激征(颈强直、克氏征、布氏征阳性);浸润性肺结核→X线所见;感染、脑脊液中抗酸杆菌及中枢神经受损→发热。
小叶性肺炎--病例分析患儿,男,3岁。
因咳嗽、咳痰、气喘9天、加重3天入院。
体格检查:体温39℃,脉搏165次/min,呼吸30次/min。
患者呼吸急促、面色苍白,口周围青紫,神萎,鼻翼扇动。
两肺背侧下部可闻及湿性啰音。
心率165次/min,心音钝,心律齐。
实验室检查:血常规:白细胞24×109/L,分类:嗜中性粒细胞0.83,淋巴细胞0.17。
X线胸片:左右肺下叶可见灶状阴影。
临床诊断:小叶性肺炎、心力衰竭。
入院后曾用抗生素及对症治疗,但病情逐渐加重,治疗无效死亡。
SLE并心脏病变114例分析庄宇;谭志明【摘要】目的探讨系统性红斑狼疮(SLE)患者心脏受累病变类型、发生概率及积极治疗干预的变化.方法回顾性分析笔者所在医院114例SLE住院患者,分析心电图、心肌酶及心脏彩超结果及治疗随访结果对照.结果 SLE心脏病变包括心率失常、心力衰竭、心源性休克、心脏瓣膜病变、心包积液、心包炎及急性心肌梗塞.结论系统性红斑狼疮患者心脏受累发生率高,尤其对心率失常及心包积液、心力衰竭需早期明确诊断及积极干预治疗.积极治疗干预与其存活率密切相关.【期刊名称】《中外医学研究》【年(卷),期】2011(009)025【总页数】2页(P12-13)【关键词】系统性红斑狼疮;心脏瓣膜疾病;心肌病;心力衰竭;心包积液;超声心动描记术【作者】庄宇;谭志明【作者单位】惠州市中心人民医院,广东,惠州516001;惠州市中心人民医院,广东,惠州516001【正文语种】中文系统性红斑狼疮(SLE)是一种自身免疫性疾病,心血管受累是SLE患者第三大死亡原因[1]。
众所周知SLE患者动脉粥样硬化的发生概率极高。
心脏也作为重要的狼疮受累靶器官,其受累影响程度及对狼疮生存期及预后的重要性随着相关研究的深入其认识得到更多的关注。
有报道约10%~50%患者出现心脏病变,可由于疾病本身,也可能由于长期服用糖皮质激素治疗引起。
心脏病变包括心包炎、心肌炎、心内膜及瓣膜病变等,依个体病变不同,表现有胸闷、胸痛、心悸、心脏扩大、充血性心力衰竭、心律失常、心脏杂音等,少数患者发生冠状动脉梗塞死亡[2]。
为此,笔者回顾性分析本院2007~2010年114例SLE住院患者的资料。
研究SLE活动程度和心脏病变之间的关系,探讨系统性红斑狼疮(SLE)患者心脏受累病变类型、发生概率及积极治疗干预的变化。
1 资料与方法1.1 一般资料为114例笔者所在医院2007~2010年SLE小于65岁确诊为SLE的住院患者。
女101例,男13例,平均年龄(35±8)岁。
感染性心内膜炎临床路径(2017年版)一、感染性心内膜炎临床路径标准住院流程(一)适用对象。
第一诊断感染性心内膜炎(ICD-10:I33.004)。
(二)诊断依据。
改良DUCK标准:感染性心内膜炎的主要标准:1.病原学诊断标准:1)2次血培养分离到典型的感染性心内膜炎典型微生物:(1)草绿色链球菌、牛链球菌、HACKE组、金黄属葡萄球菌;(2)社区获得性肠球菌,且无原发病灶。
2)符合感染性心内膜炎的持续菌血症定义如下:(1)至少两次间隔12小时以上的血标本培养阳性;(2)3次血培养均阳性,或≥4次血培养时大多数阳性(第一次和最后一次标本采取时间至少间隔1小时);3)贝纳特氏立克次体(Q热)血培养阳性或I相 IgG 抗体滴度>1:800。
2.心内膜受累证据:1)超声心动图表现如下:(1)摆动的心内团块,位于反流血流喷射路径上的瓣膜或支撑结构上,或位于植入材料上,且没有其他解剖结构可以解释;(2)脓肿;(3)人工瓣膜新发生的部分裂开。
2)新发瓣膜反流(原“杂音的加重或改变”不是充分标准)。
3.次要诊断标准:1)易患感染性心内膜炎的心脏病或静脉吸毒;2)体温>38℃;3)血管现象,大动脉栓塞,化脓性肺栓塞,真菌性动脉瘤,颅内出血,结膜出血,和Janeway损害;4)免疫现象:肾小球肾炎,Osler’s结,Roth’s斑,和类风湿因子阳性;5)微生物学证据:血培养阳性,但不符合上述主要标准或活动性感染病原体血清学证据。
4.感染性心内膜炎的诊断标准:1)病理学诊断标准(1)赘生物、栓塞的赘生物或心内脓肿标本培养或组织学检查确认微生物;(2)组织学检查确定的赘生物或心内脓肿,表明活动性心内膜炎。
2)临床诊断标准(1)2条主要标准;(2)1条主要标准+3条次要标准;(3)5条次要标准。
3)疑似感染性心内膜炎临床诊断标准(1)1条主要标准+1条次要标准;(2)3条次要标准。
4)除外感染性心内膜炎的标准(1)确诊其他疾病;(2)临床症状在抗生素治疗后4天内缓解;(3)在抗生素治疗4天内,手术或尸检没有发现感染性心内膜炎的病理学证据;(4)没有达到疑似感染性心内膜炎的标准。
中文題目:罕見Klebsiella Oxytoca 感染性感染性心內膜炎心內膜炎: 病例報告英文題目: A rare infective endocarditis caused by Klebsiella Oxytoca : A Case Report 作者: 陳柏升 陳儒逸 陳雅萍 李威霆* 林立人服務單位: 國立成功大學醫學院附設醫院 內科部 小兒科部*摘要一位71歲女性歲女性患者患者患者因持續性的高燒及全身無力約因持續性的高燒及全身無力約10天的時間至本院求診。
根據根據連續四連續四套結果為陽性之血液培養套結果為陽性之血液培養及透過胸前及經食道超音波證實位於僧帽瓣前葉之贅生物及透過胸前及經食道超音波證實位於僧帽瓣前葉之贅生物(大小約為0.6 X 1.3 公分),我們將其診斷為Klebsiella oxytoca 心內心內膜炎膜炎。
以靜脈注射第一代抗生素cefazolin 治療治療四週的時間四週的時間,患者患者完全康復出院完全康復出院。
A rare infective endocarditis caused by Klebsiella Oxytoca: A Case ReportPo-Sheng Chen, Ju-Yi Chen, Ya-Ping Chen, Wei-Ting Lee, Li-Jen LinDivision of Cardiology, Department of Medicine, National Cheng Kung University Medical Center, Tainan, Taiwan.Conflicts of interest: noneRunning title: Community-acquired Klebsiella oxytoca endocarditisKey words: Infective endocarditis; Klebsiella oxytocaReprint requests and correspondence to:Li-Jen Lin, MDDivision of Cardiology, Department of MedicineNational Cheng Kung University Medical Center138 Sheng-Li Road, Tainan 70428, TaiwanE-mail: linl@.tw; Tel: 886-6-235-3535 ext, 2382; Fax: 886-6-275-3834AbstractWe report the case of a 71-year-old woman who presented with persistent high fever and progressive weakness for 10 days. Klebsiella oxytoca infective endocarditis was diagnosed based on four sets of positive blood culture of Klebsiella oxytoca together with fluttering vegetation (0.6 cm in diameter × 1.3 cm long) on the base of the anterior mitral leaflet. The diagnosis was documented using transthoracic and transesophageal echocardiograms. After 4 weeks of intravenous cefazolin therapy, the patient completely recovered.INTRODUCTIONKlebsiella species are rare causal microorganisms that may account for 1.2% of native valve endocarditis,[1-7] among which, Klebsiella oxytoca endocarditis is extremely rare. There has been only one such case reported: in 1985, Klebsiella oxytoca endocarditis occurred after transurethral resection of a patient’s prostate gland.[1] Here we report the first case of community-acquired Klebsiella oxytoca endocarditis.CASE REPORTA 71-year-old woman presented with persistent fever and generalized weakness for 10 days. She also had deteriorating shortness of breath. She had not traveled abroad. Her past medical history included diabetes mellitus, hypertension, and mild chronic renal insufficiency, all which had been regularly treated. When the patient arrived at the emergency room, her body temperature was 39.4°C and blood pressure was 178/78 mmHg. Her respiratory rate was 18 per minute, her conjunctiva appeared slightly pale, and her jugular veins were not engorged. She had a grade 2/6 diastolic murmur at the left upper sternal border and a grade2/6 pansystolic murmur at the apex. Chest auscultation showed some crackles in both lower lung fields. Her liver and spleen were not palpable. She had no conjunctival hemorrhage, Janeway’s lesion, Osler node, or splinter hemorrhage. Her eye-ground checkup showed no Roth’s spots.Hemograms showed hemoglobin at 9.42 gm/dl, white blood cells at 14,000/cmm with 95% segmented forms, monocytes at 3%, and lymphocytes at 2%; platelets at 309,000/cmm.A blood biochemistry showed serum creatinine at 2.7 mg/dl, blood urine nitrogen at 41 mg/dl, serum sodium concentration at 147 mmol/l, serum potassium level at 3.5 mmol/l, serumC-reactive protein at 64 mg/l, AST at 25 mg/dl, and ALT at 26 mg/dl. Her urinalysis was normal. A chest X-ray showed mild pulmonary congestion and cardiomegaly. Twelve-lead electrocardiograms revealed a normal sinus rhythm and left ventricular hypertrophy with secondary ST-T changes. Arterial blood gas showed a pH of 7.395, paO2 at 95 mm Hg, paCO2 at 36 mm Hg, and HCO3− at 22 mEq/l. The patient also had mild mitral regurgitation, aortic regurgitation, and concentric left ventricular hypertrophy. The cardiac chambers were not dilated, and the left ventricular systolic function was normal. Transesophageal echocardiograms clearly revealed fluttering vegetation (0.6 cm in diameter × 1.3 cm long) with a fine connection to the mitral valve on the ventricular side of the anterior mitral leaflet base (Fig. 1). Ultrasonograms of the liver and kidneys were unrevealing. Four sets of blood cultures showed Klebsiella oxytoca, which is susceptible to cefazolin, amikacin, ceftriaxone, cefuroxime, levofloxacin, and imipenem, but resistant to gentamicin, sulfamethoxazole, and trimethoprim according to a standard disk susceptibility test. The patient’s urine culture was negative.The patient was given 1 gram of intravenous cefazolin every 8 hours for 4 weeks. Herfever subsided 4 days after antibiotic treatment began. Blood cultures repeated after 4 weeks of antibiotic treatment were negative. The patient was in good condition at her 4-month follow-up visit, when echocardiograms showed negligible residual vegetation.DISCUSSIONThis is the first case report of community-acquired Klebsiella oxytoca endocarditis. The diagnosis was based on one major (oscillating intracardiac mass on the mitral valve) and three minor (predisposing cardiac mitral and aortic valvular regurgitation, fever ≥ 38°C, and positive blood cultures) modified Duke criteria for infective endocarditis.[8] This is also the first reported case of Klebsiella oxytoca endocarditis that completely meets the modified Duke criteria.Klebsiella species, the same as other Gram-negative bacteria, are an uncommon but ominous cause of bacterial endocarditis.[9] Klebsiella endocarditis accounts for 1.2% of native valve endocarditis and 4.1% of prosthetic valve endocarditis.[9] Klebsiella oxytoca endocarditis, however, is less often encountered. The mortality of Klebsiella endocarditis is higher than for other Gram-negative endocarditis.[9,10,11] Similar to other Gram-negative bacterial endocarditis, aggressive antibiotic therapy is necessary to treat Klebsiella endocarditis.Third-generation cephalosporin and aminoglycosides are often used in combination,[9]and a 6-week treatment course seems prudent for Klebsiella endocarditis. Inthe present case of Klebsiella oxytoca endocarditis, however, 4 weeks of cefazolin treatment eliminated the pathogen. This is quite different from reported experience with other types of Klebsiella endocarditis.The portals of entry for Klebsiella oxytoca bacteremia include, in decreasing order of frequency, the hepatobiliary tract (58-65%), an intravascular or urinary catheter (7-12%), the urinary tract (5%), the skin and soft tissues (5%), and the peritoneal cavity (2%).[5,7] We were not able to specify the portal of entry in the present case.SUMMARYThis was a rare case of Klebsiella oxytoca endocarditis diagnosed using modified Duke criteria. The patient was given 4 weeks of cefazolin treatment and recovered completely.References1.Watanakunakorn C. 1985. Klebsiella oxytoca endocarditis after transurethral resection ofthe prostate gland. Southern Medical Journal.78:356-7.2.Dhawan VK. 2002. Infective endocarditis in elderly patients. Clinical Infectious Diseases.34:806-12.3.Werner GS, Schulz R, Fuchs JB, et al. 1996. Infective endocarditis in the elderly in theera of transesophageal echocardiography: clinical features and prognosis compared with younger patients. Am J Med.100:90-7.4.Leport C, Bure A, Leport J, Vilde JL. 1987. Incidence of colonic lesions in Streptococcusbovis and enterococcal endocarditis. Lancet.1(8535):748.5.Kim BN, Kim JR, Woo JH. 2002. Retrospective analysis of clinical and microbiologicalaspects of Klebsiella oxytoca bacteremia over a 10-year period. Eur J Clin Microbiol Infect Dis.21:419-26.6.Podschun R, Ullmann U. 1998. Klebsiella spp. as nosocomial pathogens: epidemiology,taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Review. 11:589-603.7.Lin RD, Hsueh PR, Chang SC, Chen YC, Hsieh WC, Luh KT. 1997. Bacteremia due toKlebsiella oxytoca: clinical features of patients and antimicrobial susceptibilities of the isolates. Clin Infect Dis.24:1217-22.8.Li JS, Sexton DJ, Mick N, et al. 2000. Proposed modifications to the Duke criteria for thediagnosis of infective endocarditis. Clin Infect Dis. 30:633-8.9.Michael J. Anderson, Edward N. Janoff. 1998. Klebsiella endocarditis: report of twocases and reviews. Clin Infect Dis. 26: 468-74.10.Geraci JE, Wilson WR. 1982. Endocarditis due to gram-negative bacteria. Mayo ClinProc. 57: 145-8.11.Polk RE. 1997. Infectious endocarditis. In: Pharmacotherapy: a pathophysiologicapproach. 3rd ed. Stamford, Connecticut: Appleton & Lange.Figure LegendFig. 1. Transesophageal echocardiography revealed fluttering vegetation originating from the base of the anterior mitral leaflet (white arrow).。

感染性心内膜炎病历摘要男,68岁,间断发热伴体重下降、腹胀、双下肢水肿3月。
患者3个月前行多颗牙齿根管治疗后约一周开始出现发热,体温约波动在37.5~38.℃之间,自觉症状尚可,日常生活和工作不受影响,在住宅楼附近的社区诊所就诊,静滴抗生素(类型不详)后,体温降至正常,但间隔2-5天后,患者又出现发热,再次使用抗生素后体温又可以降至正常,但停药后间隔几日又重新出现发热,仍为中低度热型,自测体温未超过39℃,患者未引起明显重视,一直间断在社区诊所使用抗生素,三周前感到体力明显下降,上三层楼感觉费力,食欲下降,腹胀,体重明显减轻,有时候出现双下肢轻度水肿,到附近医院消化内科就诊,行肝胆B超、胃镜、结肠镜和腹部CT检査,未发现异常,患者要求做心脏B超,心脏B超提示二尖瓣极重度关闭不全,左心扩大,EF38%,遂入住心内科,结合患者既往有心脏瓣膜病史和此次发热前有牙科根管治疗的情况,该院心内科考虑感染性心内膜炎可能,于是停抗生素做血培养,多次血培养结果提示牛型链球菌,患者要求出院,转入我院继续治疗。
家族史:无特殊既往史:因为患者既往有10年二尖瓣脱垂病史,但未行治疗,无其他慢性病病史。
查体:患者轻度贫血貌,精神差,无力体型,T37.2℃,R22次/分,P96次/分,BP100/80mmHg。
神志清楚,呼吸平稳,自动体位。
口唇无发绀,气管居中,无三凹征。
胸廓对称,双侧呼吸运动一致,双肺叩诊呈清音,双肺听诊可闻及少许湿性啰音。
心界向左下扩大,二尖听诊区可闻及明显收缩期杂音约Ⅲ级,性质柔和,向腋下传导,未闻及弃马律,颈静脉充盈,肝颈征阳性,肝肋下1指,双下肢轻度凹陷性水肿。
神经等系统检查未见异常。
相关检查:1.血常规WBC11.3G/L:RBC:4.22×1012/L;HGB 90g/L,PLT 332x109/L。
2.ESR28mm/h。
3.动脉血气分析(未吸氧)未见异常。
4.心脏超声:二尖瓣重度关闭不全,二尖瓣多发赞生物形成,左心扩大,左室6.8cm EF38%。
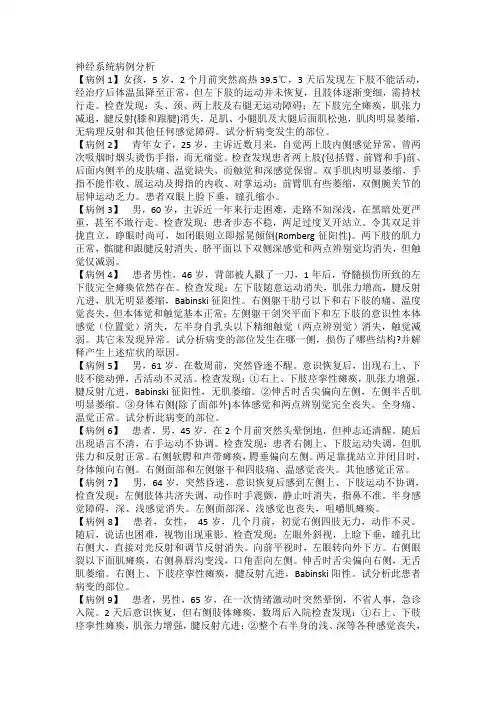
神经系统病例分析【病例1】女孩,5岁,2个月前突然高热39.5℃,3天后发现左下肢不能活动,经治疗后体温虽降至正常,但左下肢的运动并未恢复,且肢体逐渐变细,需持杖行走。
检查发现:头、颈、两上肢及右腿无运动障碍;左下肢完全瘫痪,肌张力减退,腱反射(膝和跟腱)消失,足肌、小腿肌及大腿后面肌松弛,肌肉明显萎缩,无病理反射和其他任何感觉障碍。
试分析病变发生的部位。
【病例2】青年女子,25岁,主诉近数月来,自觉两上肢内侧感觉异常,曾两次吸烟时烟头烫伤手指,而无痛觉。
检查发现患者两上肢(包括臂、前臂和手)前、后面内侧半的皮肤痛、温觉缺失,而触觉和深感觉保留。
双手肌肉明显萎缩,手指不能作收、展运动及拇指的内收、对掌运动;前臂肌有些萎缩,双侧腕关节的屈伸运动乏力。
患者双眼上脸下垂,瞳孔缩小。
【病例3】男,60岁,主诉近一年来行走困难,走路不知深浅,在黑暗处更严重,甚至不敢行走。
检查发现:患者步态不稳,两足过度叉开站立。
令其双足并拢直立,睁眼时尚可,如闭眼则立即摇晃倾倒(Romberg征阳性)。
两下肢的肌力正常,髌腱和跟腱反射消失。
脐平面以下双侧深感觉和两点辨别觉均消失,但触觉仅减弱。
【病例4】患者男性,46岁,背部被人戳了一刀,1年后,脊髓损伤所致的左下肢完全瘫痪依然存在。
检查发现:左下肢随意运动消失,肌张力增高,腱反射亢进,肌无明显萎缩,Babinski征阳性。
右侧躯干肋弓以下和右下肢的痛、温度觉丧失,但本体觉和触觉基本正常;左侧躯干剑突平面下和左下肢的意识性本体感觉(位置觉)消失,左半身自乳头以下精细触觉(两点辨别觉)消失,触觉减弱。
其它未发现异常。
试分析病变的部位发生在哪一侧,损伤了哪些结构?并解释产生上述症状的原因。
【病例5】男,61岁,在数周前,突然昏迷不醒。
意识恢复后,出现右上、下肢不能动弹,舌活动不灵活。
检查发现:①右上、下肢痉挛性瘫痪,肌张力增强,腱反射亢进,Babinski征阳性,无肌萎缩。
②伸舌时舌尖偏向左侧,左侧半舌肌明显萎缩。
《内科学》病例分析(注:此病理分析大多不完整,只有诊断名称,请大家翻阅相关内容。
感谢提供资料以及参与总结的人员!)08级影像预防上消化道出血肝炎啊神马的1、诊断及鉴别诊断2、诊断依据3、进一步检查4、治疗原则2008级临床临床、法医、妇幼统一考试两个呼吸系统的(囊状支气管扩张)和消化系统的(急性胰腺炎)09级专升本(本大题共2小题, 共20分)1、(病例摘要):患者,男,36岁,司机。
反复发作上腹疼痛三年,黑便一天入院。
患者3年前起每于秋冬季节反复发作上腹隐痛不适,多于餐后2~3h或后半夜发生,进食后有所减轻,时有反酸、嗳气。
一天前又发剑突下腹痛,随后解稀糊状柏油样黑便。
1天来共排柏油样黑便4次,共约1000ml,便后感头昏,心悸。
查体:血压80/50 mmHg,HR120次/分,面色苍白,四肢厥冷,脉搏细数,神志恍惚。
无肝掌、蜘蛛痣。
腹平软, 剑突下有深压痛,无反跳痛。
肝、脾肋下未触及。
肠鸣音8次/分钟。
化验粪隐血(++++) 1)请你提出对该病人目前病情的初步诊断?根据病情提出主要诊断?(5分)2)如何观察判断病人出血停止或继续?(5分)2、一老年患者,大量输液过程中突然出现严重气急,极度烦躁不安,大汗淋漓,面色青灰,皮肤湿冷,伴咳嗽,咳出大量粉红色泡沫样痰液,查体:心率126次/分,律齐,呼吸28次/分,两肺满布湿罗音及哮鸣音。
问题:请你对该患者目前病情变化做出初步诊断并提出紧急处理要点?(10分)四、病例分析(2*10') 2007级临床、法医、妇幼(一系、二系联考)1.支气管哮喘急性发作;气胸题目在那书上的254页,答案在586页,第7题(1)最可能的诊断是?(2)进一步检查?(3)治疗?2.酒精性脂肪肝题目在那书上的388页,答案在636页,第13题(1)诊断和鉴别诊断是?(2)进一步检查?(3)治疗?题目基本上来源于人民卫生出版社的那本辅导书。
06级的题目都是从华科那本辅导书上来的。