类风湿关节炎诊断及治疗指南(2010年)。
- 格式:ppt
- 大小:424.00 KB
- 文档页数:36

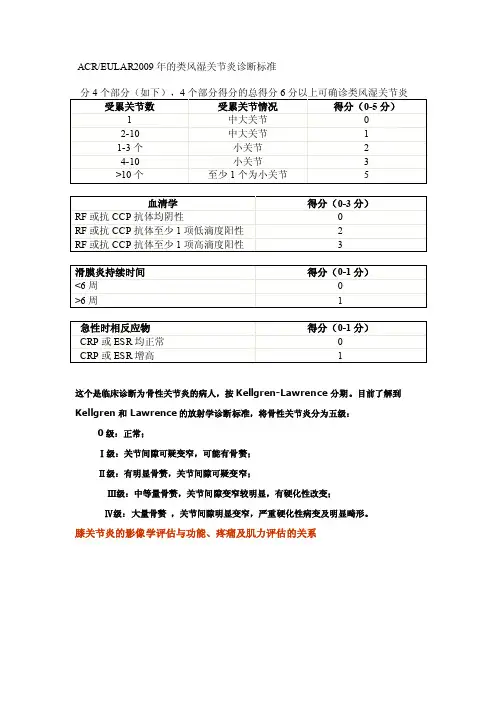
ACR/EULAR2009年的类风湿关节炎诊断标准这个是临床诊断为骨性关节炎的病人,按Kellgren-Lawrence分期。
目前了解到Kellgren和Lawrence的放射学诊断标准,将骨性关节炎分为五级:0级:正常;Ⅰ级:关节间隙可疑变窄,可能有骨赘;Ⅱ级:有明显骨赘,关节间隙可疑变窄;Ⅲ级:中等量骨赘,关节间隙变窄较明显,有硬化性改变;Ⅳ级:大量骨赘,关节间隙明显变窄,严重硬化性病变及明显畸形。
膝关节炎的影像学评估与功能、疼痛及肌力评估的关系Para Español haga clic aquí.FAST FACTS∙OA is the most common form of joint disease in humans and is a leading cause of disability among the elderly.∙It typically occurs in the hand joints, spine, hips and knees.∙It is caused by cartilage breakdown and subsequent bony changes of the joints.∙Although the joint changes are irreversible, only a small number of patients will progress to the point that requires joint replacement surgery.∙OA symptoms can vary greatly among patients. Y our rheumatologist can make the diagnosis and prescribe appropriate treatment recommendations for you.In osteoarthritis, the cartilage between the bones in the joint breaks down, and bony enlargement occurs.WHA T IS OSTEOARTHRITIS?Osteoarthritis (OA) is a slowly progressive joint disease typically seen in middle-age to elderly people. It occurs when the joint cartilage breaks down, causing the underlying bone to fail. OA symptoms include joint pain, stiffness, knobby swelling, cracking noises with joint movements and decreased function. It typically affects the joints of the hands and spine and weight-bearing joints such as the hips and knees.WHO GETS OSTEOARTHRITIS?OA typically occurs in patients age 40 and above. However, some risk factors might cause it to occur sooner (see below). It affects people of all races and gender.WHA T ARE THE RISK FACTORS FOR OSTEOARTHRITIS?∙Older age∙Family members with OA∙Obesity∙Joint trauma or repetitive use of jointsHOW IS OSTEOARTHRITIS DIAGNOSED?OA usually is diagnosed by having typical symptoms and physical examination as described above. In some cases, imaging studies may be useful to tell the extent of disease or to help rule out other joint problems.The circles on this figure indicate joints that are commonly affected by osteoarthritis.HOW IS OSTEOARTHRITIS TREATED?The goal of treatment is to reduce pain and improve function of the affected joints. This can be achieved with a combination of physical measures, drug therapy and, sometimes, surgery.Physical measures– Exercise, support devices and thermal therapy are useful in OA. Some forms of unproven alternative treatment such as spa, massage, acupuncture and chiropractic manipulation can help relieve pain for a short duration, but usually are costly and require repeated treatments.Drug Therapy– Available forms of drug therapy include topical and oral agents. Topical drugs, which include capsaicin cream, lidocaine, and diclofenac gel, can be applied directly on the skin overlying the affected joints. Oral pain relievers such as acetaminophen, and nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used as first-line treatment. For more serious pain, stronger medications, such as narcotics, may be required. Joint injections with corticosteroids or a form of lubricant called hyaluronic acid (HA) derivatives have proven effective for some patients.Surgery– Arthroscopy and/or joint replacement is considered when the joint is seriously damaged, or the patient is in intractable pain and experiencing significant loss of function.Supplements– Many over-the-counter nutritional supplements have been used for treatment of OA, but most lack good research data to support their effectiveness and safety. Among the most widely used areglucosamine/chondroitin sulfate, calcium and vitamin D, and omega-3 fatty acids. To ensure safety and avoid drug interaction, consult your doctor or pharmacist before using any of these agents, especially in combination with prescribed drugs.LIVING WITH OSTEOARTHRITISThere is no cure for OA, but you can manage how it impacts your lifestyle. For instance, giving proper positioning and support to the neck and back during sitting or sleeping; adjusting furniture, such as raising a chair or toilet seat; and avoiding trauma and repetitive motions of the joint, especially frequent bending, are great starts.Adding regular exercise to your daily activities will improve muscle strength. Exercises that increase strength of the quadriceps muscles (the front thigh muscles) also can help decrease knee pain and reduce subsequent disability associated with osteoarthritis. Working with a physical or occupational therapist can help you learn the best exercises and choose appropriate assistive devices for your joints.Weight loss in obese people can reduce pain and progression of OA. Achieving and keeping an ideal weight will make a difference in your overall comfort levels.POINTS TO REMEMBER∙OA is the most common form of arthritis and can occur together with other types of arthritis.∙Evaluation by your doctor will help confirm the diagnosis and develop an appropriate treatment plan for your condition.∙The goal of treatment in OA is to reduce pain and improve function.∙At present, there is no available therapy that can reverse the damage of OA in the joint, but many studies are underway.TO FIND A RHEUMA TOLOGISTFor more information about rheumatologists, click here.Learn more about rheumatologists and rheumatology health professionals.FOR MORE INFORMATIONThe American College of Rheumatology has compiled this list to give you a starting point for your own additional research. The ACR does not endorse or maintain these Web sites, and is not responsible for any information or claims provided on them. It is always best to talk with your rheumatologist for more information and before making any decisions about your care.Arthritis FoundationUpdated August 2009Written by Thitinan Srikulmontree, MD, and reviewed by the American College of Rheumatology Patient Education Task Force.This patient fact sheet is provided for general education only. Individuals should consult a qualified health care provider for professional medical advice, diagnoses and treatment of a medical or health condition.© 2010 American College of Rheumatology5次坐-立试验在膝骨关节炎患者功能评估中的价值。
类风湿性关节炎的诊断标准风湿性关节炎(Rheumatoid Arthritis,RA)是一种慢性炎性关节病,全身性诊断标准(2010年版)可用于诊断RA。
诊断标准包括:1. 精确定义的弥漫性关节炎活动(至少4周)- 对应弥漫性关节炎列表(synovial joint lists)4项或更多关节的活动性的发炎。
2. 同一时间至少有1个细胞培养定量检测(Radiographic Quantitative Assay,RQA)阳性反应- 血清共行联合抗体(CommonAssociated Immunoglobulin,CAI-IgG或IgA)蛋白水平较正常检测值增高,或,用现代囊膜色素(Modern Mucopigment)测试显示抗体滴度大于常值。
3. 同时有至少2处活动性骨质结核损伤- 可用X光检查、磁共振成像(MRI)或其他影像学检查,根据发病规律判断多处骨质结核损伤。
4. 其他相关的免疫性和血清学检查的阳性反应- 这些检查包括:血清C-反应蛋白(CRP)水平高于正常范围;粪便抗IgA抗体检测(Fecal Antibody Test for IgA)阳性;180度双侧抗体评估测定(Double Blind Assessment,DBA)阳性;RQA测定的抗体IgG水平高于常规检查值;血清促炎因子(Serum Inflammatory Factors,SIF)测定高于正常范围;RA抗原(Rheumatoid Antigen)水平增高;抗核抗体(Anti-nuclear Antibody, ANA)阳性;抗类风湿抗体(Anti-Rheumatic Antibody,ARA)阳性。
以上8个检查项目,至少满足4条标准,同时兼具以上4个特征可以诊断RA。
另外,还需要更详细的检查,如血常规检查,白细胞介素-6(Interleukin—6,IL—6),粪便抗体测定,以及对病因的进一步研究,如肿瘤基因突变检查等。
骨关节炎诊断及治疗指南中华医学会风湿病学分会1概述骨关节炎(Osteoarthritis,OA)是一种最常见的关节疾病。
是以关节软骨的变性、破坏及骨质增生为特征的慢性关节病。
本病的发生与衰老、肥胖、炎症、创伤、关节过度使用、代谢障碍及遗传等因素有关。
骨关节炎在中年以后多发,女性多于男性。
本病在40岁人群的患病率为10%-17%,60岁以上为50%,而在75岁以上人群则高达80%。
该病有一定的致残率。
本病按病因分为原发性骨关节炎和继发性骨关节炎。
前者是指原因不明的骨关节炎,与遗传和体质因素有一定关系,多见于中老年人;后者是指继发于关节外伤、先天性或遗传性疾病、内分泌及代谢病、炎性关节病、地方性关节病、其他骨关节病等。
有时很难鉴别原发性骨关节炎和继发性骨关节炎。
问诊和体格检查可以帮助判断病因。
影像学检查有助于继发性骨关节炎的诊断。
本病按是否伴有临床症状分为症状性骨关节炎和放射学骨关节炎。
前者伴有明显的骨关节炎临床症状,而后者无临床症状只有X线骨关节炎表现。
2临床表现2.1常见症状和体征本病好发于膝、髋、手(远端指间关节、第一腕掌关节)、足(第一跖趾关节、足跟)、脊柱(颈椎及腰椎)等负重或活动较多的关节。
2.1.1关节疼痛及压痛:本病最常见的表现是关节局部的疼痛和压痛。
负重关节及双手最易受累。
一般早期为轻度或中度间断性隐痛,休息时好转,活动后加重,随病情进展可出现持续性疼痛,或导致活动受限。
关节局部可有压痛,在伴有关节肿胀时尤为明显。
疼痛在阴冷、潮湿和雨天会加重。
2.1.2关节肿大:早期为关节周围的局限性肿胀,随病情进展可有关节弥漫性肿胀、滑囊增厚或伴关节积液。
后期可在关节部位触及骨赘。
2.1.3晨僵:患者可出现晨起或关节静止一段时间后僵硬感,称为晨僵,活动后可缓解。
本病的晨僵时间一般数分钟至十几分钟,很少超过半小时。
2.1.4关节摩擦音(感):多见于膝关节。
由于软骨破坏、关节表面粗糙,出现关节活动时骨摩擦音(感)。

2010类风湿性关节炎诊断标准一、诊断标准概述类风湿性关节炎(RA)是一种慢性自身免疫性疾病,其主要特点是炎症性多系统损害,导致关节疼痛、肿胀和僵硬,并最终导致关节畸形。
RA的诊断通常基于临床、实验室和影像学检查的综合结果。
以下是2010年ACR/EULAR提出的类风湿性关节炎诊断标准。
二、疾病历史和家族史1. 至少一个关节肿胀或疼痛,持续至少6周;2. 至少一个关节活动受限或畸形;3. 炎症性滑膜炎的典型症状(如关节晨僵,活动后缓解,以及皮肤下的类风湿结节);4. 类风湿因子(RF)阳性;5. 有RA的家族史。
注:满足以上至少四项可诊断为RA。
三、临床表现1. 关节表现:RA常影响多个关节,尤其是手足小关节,表现为肿胀、疼痛和僵硬。
随着病情发展,可出现关节活动受限、畸形和功能受损。
2. 系统表现:RA可累及身体其他器官和系统,如皮肤、眼睛、肺、心脏、血管等。
常见症状包括疲劳、体重减轻、发热、盗汗、贫血等。
四、实验室检查1. 类风湿因子(RF):RF是一种自身抗体,在约70%的RA患者中可检测到。
但RF阳性并不一定意味着RA的诊断,因为其在其他自身免疫性疾病和感染性疾病中也可能出现。
2. 抗瓜氨酸抗体(ACAs):包括抗CCP抗体和抗AKA抗体。
这些抗体在RA患者中具有较高的特异性,有助于早期诊断。
3. 其他实验室指标:包括血沉(ESR)、C反应蛋白(CRP)、白细胞计数等,这些指标可反映疾病活动度。
五、影像学检查1. X线检查:X线平片可显示关节炎症、增生和畸形等病变。
2. 超声检查:关节超声可用于评估滑膜炎的严重程度和治疗效果,且具有无创、便捷的优势。
3. MRI检查:MRI对软组织的显示能力优于X线和超声,可更早地发现关节病变。
六、病理学检查1. 滑膜活检:通过关节镜或切开手术获取滑膜组织样本进行病理检查,可观察到RA特征性的滑膜病理改变。
2. 皮下结节活检:类风湿结节是RA的典型表现,对其活检可显示类风湿性肉芽肿。
类风湿关节炎病证结合诊疗指南1范围本《指南》规定了类风湿关节炎的流行病学、诊断要点、辨证论治、中成药选择、外治疗法、预防调摄、治疗推荐等。
本《指南》适用于类风湿关节炎病证结合诊断和治疗。
2规范性引用文件下列文件对于本规范的应用是必不可少的。
凡是注明日期的引用文件,仅所注明日期的版本适用于本规范。
凡是不注明日期的引用文件,其最新版本(包括所有的修改版本)适用于本文件。
证据推荐级别及证据水平,参照[1]2001年牛津证据分级与推荐意见强度。
GB/T1.1-2009《标准化工作导则第1部分:标准的结构和编写》《中医药标准制定管理办法(试行)》GB/T16751.1-1997《中医临床诊疗术语-疾病部分》GB/T16751.2-1997《中医临床诊疗术语-证候部分》2015American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis3术语及定义下列术语和定义适用于本规范。
3.1病证结合Combination of Diseaseand Syndrome辨病与辨证相结合的研究模式,主要是指现代医学诊断疾病结合辨证论治模式。
3.2药品不良反应adverse drug reaction,ADR合格药品在正常用法用量下出现的与用药目的无关的有害反应。
4流行病学类风湿关节炎(Rheumatoid arthritis,RA)是一种以对称性多关节炎为主要临床表现的自身免疫性疾病,以关节滑膜慢性炎症、关节的进行性破坏为特征。
目前发病原因不明,可能与遗传、免疫、感染、环境等因素有关,该病属于中医风湿病(痹证、痹病)范畴,中医诊断为“尪痹”[2]。
RA几乎见于世界所有的地区和各种族;目前患病人数约占世界总人口的1.0%,中国的发病率大约为0.28-0.4%[3]。
RA可以发生于任何年龄,女性高发年龄为45~54岁,男性随年龄增加而发病率上升,男女罹患本病的比例约为1:3[4]。

ARTHRITIS&RHEUMATISMVol.62,No.9,September2010,pp2569–2581DOI10.1002/art.27584©2010,American College of Rheumatology2010Rheumatoid Arthritis Classification CriteriaAn American College of Rheumatology/European League Against RheumatismCollaborative InitiativeDaniel Aletaha,1Tuhina Neogi,2Alan J.Silman,3Julia Funovits,1David T.Felson,2Clifton O.Bingham,III,4Neal S.Birnbaum,5Gerd R.Burmester,6Vivian P.Bykerk,7Marc D.Cohen,8Bernard Combe,9Karen H.Costenbader,10Maxime Dougados,11Paul Emery,12Gianfranco Ferraccioli,13Johanna M.W.Hazes,14Kathryn Hobbs,15Tom W.J.Huizinga,16Arthur Kavanaugh,17Jonathan Kay,18Tore K.Kvien,19Timothy Laing,20 Philip Mease,21Henri A.Ménard,22Larry W.Moreland,23Raymond L.Naden,24 Theodore Pincus,25Josef S.Smolen,1Ewa Stanislawska-Biernat,26Deborah Symmons,27 Paul P.Tak,28Katherine S.Upchurch,18JirˇíVencovsky´,29Frederick Wolfe,30and Gillian Hawker31This criteria set has been approved by the American College of Rheumatology(ACR)Board of Directors and the Euro-pean League Against Rheumatism(EULAR)Executive Committee.This signifies that the criteria set has been quantita-tively validated using patient data,and it has undergone validation based on an external data set.All ACR/EULAR-approved criteria sets are expected to undergo intermittent updates.The American College of Rheumatology is an independent,professional,medical and scientific society which does not guarantee,warrant,or endorse any commercial product or service.Objective.The1987American College of Rheuma-tology(ACR;formerly,the American Rheumatism As-sociation)classification criteria for rheumatoid arthri-tis(RA)have been criticized for their lack of sensitivity in early disease.This work was undertaken to develop new classification criteria for RA.Methods.A joint working group from the ACR and the European League Against Rheumatism devel-This article is published simultaneously in the September 2010issue of Annals of the Rheumatic Diseases.Supported by the American College of Rheumatology and the European League Against Rheumatism.1Daniel Aletaha,MD,MSc,Julia Funovits,Dipl.Ing,Josef S. Smolen,MD:Medical University of Vienna,Vienna,Austria;2Tuhina Neogi,MD,PhD,FRCPC,David T.Felson,MD,MPH:Boston University School of Medicine,Boston,Massachusetts;3Alan J.Sil-man,FRCP,FmedSci,DSc(Hons):Arthritis Research UK,Chester-field,UK;4Clifton O.Bingham,III,MD:Johns Hopkins University,Baltimore,Maryland;5Neal S.Birnbaum,MD:California PacificMedical Center and University of California,San Francisco;6Gerd R.Burmester,MD:Charite´Hospital–University Medicine Berlin,FreeUniversity and Humboldt University Berlin,Berlin,Germany;7VivianP.Bykerk,MD,FRCPC:Mount Sinai Hospital and University ofToronto,Toronto,Ontario,Canada;8Marc D.Cohen,MD:NationalJewish Medical and Research Center,Denver,Colorado;9BernardCombe,MD,PhD:Lapeyronie Hospital and Montpellier I University,Montpellier,France;10Karen H.Costenbader,MD,MPH:Brighamand Women’s Hospital and Harvard University,Boston,Massachu-setts;11Maxime Dougados,MD:Cochin Hospital,Assistance PubliqueHoˆpitaux de Paris,and Paris-Descartes University,Paris,France; 12Paul Emery,MD,MA,FRCP:University of Leeds and NIHR Leeds Musculoskeletal Biomedical Research Unit,Leeds,UK;13GianfrancoFerraccioli,MD:School of Medicine,Catholic University of theSacred Heart,Rome,Italy;14Johanna M.W.Hazes,MD,PhD:Erasmus Medical Center,University Medical Center Rotterdam,andUniversity of Rotterdam,Rotterdam,The Netherlands;15KathrynHobbs,MD:University of Colorado School of Medicine,Denver;Arthritis&Rheumatism An Official Journal of the American College of Rheumatology and 2569oped,in3phases,a new approach to classifying RA.The work focused on identifying,among patients newly presenting with undifferentiated inflammatory synovi-tis,factors that best discriminated between those who were and those who were not at high risk for persistent and/or erosive disease—this being the appropriate cur-rent paradigm underlying the disease construct“rheu-matoid arthritis.”Results.In the new criteria set,classification as “definite RA”is based on the confirmed presence of synovitis in at least1joint,absence of an alternative diagnosis that better explains the synovitis,and achieve-ment of a total score of6or greater(of a possible10) from the individual scores in4domains:number and site of involved joints(score range0–5),serologic abnormality(score range0–3),elevated acute-phase response(score range0–1),and symptom duration(2 levels;range0–1).Conclusion.This new classification system rede-fines the current paradigm of RA by focusing on fea-tures at earlier stages of disease that are associated with persistent and/or erosive disease,rather than defining the disease by its late-stage features.This will refocus attention on the important need for earlier diagnosis and institution of effective disease-suppressing therapy to prevent or minimize the occurrence of the undesir-able sequelae that currently comprise the paradigm underlying the disease construct“rheumatoid arthri-tis.”IntroductionRheumatoid arthritis(RA)is a chronic inflam-matory disease characterized by joint swelling,joint tenderness,and destruction of synovial joints,leading to severe disability and premature mortality(1–5).Given16Tom W.J.Huizinga,MD,PhD:Leiden University Medical Centre, Leiden,The Netherlands;17Arthur Kavanaugh,MD:University of California,San Diego;18Jonathan Kay,MD,Katherine S.Upchurch, MD:UMassMemorial Medical Center and University of Massachu-setts Medical School,Worcester;19Tore K.Kvien,MD,PhD:Diakon-hjemmet Hospital,Oslo,Norway;20Timothy Laing,MD:University of Michigan,Ann Arbor;21Philip Mease,MD:Swedish Medical Center and University of Washington,Seattle;22Henri A.Me´nard,MD: McGill University Health Centre and McGill University,Montreal, Quebec,Canada;23Larry W.Moreland,MD:University of Pittsburgh, Pittsburgh,Pennsylvania;24Raymond L.Naden,MB ChB,FRACP: Ministry of Health,Auckland,New Zealand;25Theodore Pincus,MD: New York University Hospital for Joint Diseases,New York,New York;26Ewa Stanislawska-Biernat,MD,PhD:Institute of Rheumatol-ogy,Warsaw,Poland;27Deborah Symmons,MD,FFPH,FRCP: University of Manchester,Manchester,UK;28Paul P.Tak,MD,PhD: Academic Medical Center,University of Amsterdam,Amsterdam, The Netherlands;29Jirˇı´Vencovsky´,MD,DSc:Institute of Rheumatol-ogy,Prague,Czech Republic;30Frederick Wolfe,MD:National Data Bank for Rheumatic Diseases and University of Kansas,Wichita; 31Gillian Hawker,MD,MSc,FRCPC:Women’s College Hospital and University of Toronto,Toronto,Ontario,Canada.Dr.Aletaha has received consulting fees,speaking fees, and/or honoraria from Abbott,Bristol-Myers Squibb,UCB,Schering-Plough,Wyeth,and Roche(less than$10,000each).Dr.Bingham has received consulting fees,speaking fees,and/or honoraria from UCB, Roche,Genentech,Celgene,and Merck Serono(less than$10,000 each);he has received research and/or educational grant support from Bristol-Myers Squibb,Genentech,UCB,Centocor,Abbott,and Am-gen.Dr.Birnbaum has received consulting fees,speaking fees,and/or honoraria from Amgen,Pfizer,Centocor,Abbott,and UCB(less than $10,000each).Dr.Burmester has received consulting fees,speaking fees,and/or honoraria from Abbott,Bristol-Myers Squibb,Pfizer, UCB,and Roche(less than$10,000each).Dr.Bykerk has received consulting fees,speaking fees,and/or honoraria from Amgen,Wyeth, Abbott,Schering-Plough,Roche,Bristol-Myers Squibb,and UCB(less than$10,000each);her spouse is employed by Genzyme and owns stock in the company.Dr.Cohen has received consulting fees, speaking fees,and/or honoraria from UCB,Genentech,Bristol-Myers Squibb,and Human Genome Sciences(less than$10,000each).Dr. Combe has received consulting fees,speaking fees,and/or honoraria from Abbott,Bristol-Myers Squibb,Pfizer,Roche,Schering-Plough, and Merck,Sharpe,and Dohme(less than$10,000each).Dr.Emeryhas received consulting fees,speaking fees,and/or honoraria from Pfizer,Abbott,Centocor,UCB,Roche,Bristol-Myers Squibb,and Merck,Sharpe,and Dohme(less than$10,000each).Dr.Ferraccioli holds a patent for T cell receptor clonotype analysis(PCT/IB2008/ 053152NP).Dr.Huizinga has received consulting fees,speaking fees, and/or honoraria from Schering-Plough,Bristol-Myers Squibb,UCB, Biotest AG,Wyeth/Pfizer,Novartis,Roche,Sanofi-Aventis,Abbott, and Axis-Shield(less than$10,000each).Dr.Kavanaugh has con-ducted clinical research for Amgen,Abbott,Bristol-Myers Squibb, UCB,Roche,Centocor,Genentech,and Sanofi-Aventis.Dr.Kay has received consulting fees from Array BioPharma,Bristol-Myers Squibb, Celgene,Centocor,Genentech,Roche,UCB,and Sanofi-Aventis(less than$10,000each).Dr.Mease has received consulting fees,speaking fees,and/or honoraria from Abbott,Amgen,Biogen Idec,Bristol-Myers Squibb,Centocor,Roche,Genentech,UCB,Pfizer,Novartis, and Eli Lilly(less than$10,000each).Dr.Me´nard has received un-restricted educational and research grants as well as consulting and speaking fees from Abbott,Amgen,Inova,Merck,Pfizer,Roche, Schering-Plough,UCB,and Wyeth(less than$10,000each)and investigator-initiated research grants from Bristol-Myers Squibb,Euro-Immun AG,and Roche(more than$10,000each);he owns stock or stock options in Merck;and he has a license agreement with Euro-Immun AG for an anti-Sa enzyme-linked immunosorbent assay.Dr. Moreland has received consulting fees,speaking fees,and/or honoraria from Biogen Idec,Centocor,Pfizer,Takeda,KaloBios,ChemoCen-tryx,UCB,Genentech,Incyte,and Eli Lilly(less than$10,000each). Dr.Naden has received consulting fees from the American College of Rheumatology in regard to the methodology of developing weighted scoring systems(more than$10,000).Dr.Pincus has received consult-ing fees,speaking fees,and/or honoraria from Amgen,Abbott,Bristol-Myers Squibb,Centocor,UCB,Wyeth,and Genentech(less than $10,000each)and investigator-initiated research grants from Amgen, Bristol-Myers Squibb,UCB,and Centocor.Dr.Stanislawska-Biernat has received speaking fees from Abbott and Pfizer(less than$10,000 each).Dr.Vencovsky´has received speaking fees from Pfizer,UCB, Abbott,Roche,and Merck,Sharpe,and Dohme(less than$10,000 each).Address correspondence and reprint requests to Alan J. Silman,MD,FRCP,Arthritis Research UK,Copeman House,Ches-terfield S417TD,UK.E-mail:a.silman@.Submitted for publication January22,2010;accepted in revised form May20,2010.2570ALETAHA ET ALthe presence of autoantibodies,such as rheumatoid factor(RF)and anti–citrullinated protein antibody (ACPA)(tested as anti–cyclic citrullinated peptide[anti-CCP]),which can precede the clinical manifestation of RA by many years(6–9),RA is considered an auto-immune disease(10,11).Autoimmunity and the overall systemic and articular inflammatory load drive the de-structive progression of the disease.However,although structural changes,which can be visualized by conven-tional radiography or other imaging techniques,best distinguish RA from other arthritic disorders(12),joint damage is rarely apparent in the very early stages of disease,but rather accumulates consistently over time (13–16).Over the last decade,the optimal use of disease-modifying antirheumatic drugs(DMARDs),in particu-lar the anchor DMARD methotrexate(MTX)(17–19), and the availability of new biologic agents(11,20),have dramatically enhanced the success of RA management. Moreover,it has been recognized that early therapeutic intervention improves clinical outcomes and reduces the accrual of joint damage and disability(21–23).Undoubt-edly,treating patients at a stage at which evolution of joint destruction can still be prevented would be ideal. However,at present,clinical trials of RA treatments are hampered by lack of criteria allowing for study enroll-ment of patients at early stages of disease.Thus,to date it has not been possible to effectively investigate the efficacy of early interventions in terms of their ability to prevent later-stage RA,since there are no validated or accepted uniform criteria to classify such individuals with early disease.The standard and accepted means of defining RA is by use of classification criteria.Classification criteria enable the stratification of groups of individuals into those with and those without RA in order to standardize recruitment into clinical trials and related studies,and provide the basis for a common approach to disease definition that can be used to compare across studies and centers.The classification criteria set that is in widespread international use to define RA is the1987 American College of Rheumatology(ACR;formerly the American Rheumatism Association)criteria(24).These criteria are well accepted as providing the benchmark for disease definition,but have a significant limitation in that they were derived by trying to discriminate patients with established RA from those with a combination of other definite rheumatologic diagnoses.They are there-fore not helpful in achieving the goal of identifying patients who would benefit from early effective interven-tion,as discussed above.Indeed,with modern therapies,the goal is to prevent individuals from reaching the chronic,erosive disease state that is exemplified in the 1987criteria for RA.A joint working group of the ACR and the European League Against Rheumatism(EULAR)was therefore formed to develop a new approach for classi-fication of RA.While classification criteria are poten-tially adopted for use as aids for diagnosis,the focus of this endeavor was not on developing diagnostic criteria or providing a referral tool for primary care physicians. Indeed,a separate body of work is needed to develop such tools,which may be informed by classification criteria.Thus,the specific charge was to develop new classification criteria for RA to facilitate the study of persons at earlier stages of the disease.It was with this framework in mind that the working group developed the2010ACR/EULAR classification criteria for RA. Overview on hypothesis and methods of Phases1and2A priori,the working group focused on develop-ing an approach that would be appropriate for newly presenting patients with undifferentiated inflammatory synovitis,in order to identify that subset of patients who are at sufficiently high risk of persistent and/or erosive disease—this being the appropriate current paradigm underlying the disease construct“rheumatoid arthritis”—to be classified as having RA.It was recog-nized that such a scheme should not be developed using existing criteria sets as the“gold standard,”because of the inherent circularity.The goal set forth was to develop a set of rules to be applied to newly presenting patients with undifferentiated synovitis that would1) identify the subset at high risk of chronicity and erosive damage;2)be used as a basis for initiating disease-modifying therapy;and3)not exclude the capture of patients later in the disease course.To achieve these goals,the working group de-vised a3-phase program.Phase1was a data-driven approach based on cohorts of real-world patients with early arthritis,to identify factors,and their relative weights,that were associated with the subsequent deci-sion by a physician to start MTX treatment.Phase2was a consensus-driven,decision science–based approach, informed by the data from Phase1,to refine these factors and their weights using a series of“paper pa-tients,”as well as to identify any other factors that may be of relevance based on current clinical thinking.Phase 3,which is the focus of this report,describes the derivation,from the previous2phases,of the finalACR/EULAR CLASSIFICATION CRITERIA FOR RA2571classification criteria set.The details of the methods and results from Phases1and2are provided elsewhere (25,26),and are briefly summarized below.Phase1.The aim of Phase1was to identify the contributions of clinical and laboratory variables that in practice were the most predictive of the decision to initiate DMARD therapy in a population of patients with early undifferentiated synovitis.Initiation of DMARD therapy was used as an indicator of the physician’s opinion that the patient was at risk of developing persistent and/or erosive arthritis that we would currently consider to be RA.Data on3,115 patients from9early arthritis cohorts who were consid-ered not to have evidence of another possible diagnosis explaining their presentation were obtained.Between July2007and November2008an expert working group developed an analysis strategy that related an agreed-upon list of standardized clinical and laboratory vari-ables collected at baseline to the initiation of DMARD treatment within the next12months.MTX initiation was used as the gold standard for this purpose.The analytical process aimed to identify the independent contribution of each variable on this list and included univariate regression modeling,a subsequent principal components analysis,and a multivariate regression model that included all identified components(25).The resulting list of informative variables identified during that process and the weights based on the odds ratios are shown in Table1.Phase2.Phase2consisted of a consensus-based, decision science–informed approach,which took place between November2008and June2009.The purpose of this phase was to derive a clinician-based judgment on the relative contribution of clinical and laboratory fac-tors deemed to be important in influencing the proba-bility of developing“persistent inflammatory and/or erosive arthritis that is currently considered to be RA”(hereinafter referred to as“developing RA”).An expert panel was assembled,comprising12 rheumatologists from Europe and12from North Amer-ica with extensive experience in the diagnosis and man-agement of RA.They provided real-life case scenarios of patients with early undifferentiated inflammatory arthri-tis representing low to high probability of developing RA.A2-day workshop was held in May2009in which domains(factors)and categories within those domains that were important in determining the probability of developing RA were identified.When appropriate, these judgments were informed by the results of Phase1 and other available literature.The relative importance or weights of these domains and their categories were determined by means of decision science theory and conjoint adaptive technology,using the computerized 1000Minds program()in an inter-active and iterative process(26).This analysis permitted the calculation of an individual’s score of the likelihood of developing RA from0to100,where a higher score indicated greater likelihood of RA development.The domains,categories,and weights derived during that initial process are shown in Table2.Objectives,methods,and results of Phase3Objectives of Phase3.In Phase3the working group integrated the findings of the first2phases, refined the scoring system,and determined the optimal cut point to define“definite RA.”The goal of this final phase was to utilize the results of Phases1and2to develop a scoring system that would be applicable to newly presenting patients with undifferentiated inflam-matory arthritis to permit identification of those with a high probability of developing persistent and/or erosive RA.Being intended for use with newly presenting patients,the scoring system should be robust enough that it could be applied repeatedly during the early course of disease,such that a patient identified as not classifiable as having definite RA at initial presentation might be classified as having definite RA at a subsequent time point.The work was not aimed at classifying subjects with established disease,either active or inac-tive.However,the working group recognized that pa-tients may present for the first time with disease that is at a later stage and being treated.Thus,although it was not the explicit charge of the working group to provideTable1.Summary of Phase1results*Variable Comparison Relative weight†Swollen MCP joint Present vs.absent 1.5Swollen PIP joint Present vs.absent 1.5Swollen wrist Present vs.absent 1.6Hand tenderness Present vs.absent 1.8Acute-phase response Low-level abnormal vs.normal 1.2Highly abnormal vs.normal 1.7Serology Low-positive vs.negative 2.2(RF or ACPA)High-positive vs.negative 3.9*MCPϭmetacarpophalangeal;RFϭrheumatoid factor;ACPAϭantiϪcitrullinated protein antibody.†Derived from odds ratios from the multivariate regression model,and interpreted as the increase in the odds of having rheumatoidarthritis(RA)with as opposed to without the respective feature(e.g.,weight of1.5for swelling of proximal interphalangeal[PIP]jointsmeans that the odds of having RA is1.5-fold in patients with asopposed to patients without swelling of a PIP joint).2572ALETAHA ET ALrules for the classification of such patients,it is appro-priate to have a single criteria system that could be applied to all patients;these issues were addressed by the expert panel during Phase3.Determination of the optimal cut point for defi-nite rheumatoid arthritis.Determination of the optimal cut point to classify an individual as having definite RA was achieved using2complementary approaches,mir-roring the approaches used in the first2phases:data-informed and consensus-based.From the consensus-based approach,the expert panel was asked to examine the rankings of case scenarios based on the new scoring system and to indicate,in their opinion,the point at which the cases changed from“probable”to“definite”RA.Four cases were excluded due to missing domain information(nϭ2)or ineligibility(2cases were more likely another diagnosis).For the remaining50cases,the mean cut point defining definite RA was65.7(median66.1;range60.0–70.3)of a total possible score of100.A data-driven verification of that cut point was then attempted,in which the new scoring system was applied to3of the existing cohorts used for Phase1(the Etude et Suivi des Polyarthrites Indifferenciees Re-centes data set from France,the Norwegian data set,and the Rotterdam Early Arthritis Cohort data set from Rotterdam)(25).These cohorts were chosen based on the completeness of data and the collected variables, enabling calculation of the patients’probability scores at baseline.The disease characteristics of these cohorts were not substantively different from those of the re-maining cohorts(data not shown).The area under the curve(AUC)for the3 receiver operating characteristic(ROC)curves(which plot sensitivity against1Ϫspecificity for the range of scores)indicated good discrimination of those who did versus those who did not receive MTX(or another DMARD/biologic agent)within a year(AUC0.82for Norway,0.66for France,and AUC0.69for Rotterdam; PϽ0.0001for all).The probability scores similarly discriminated between those who fulfilled the1987ACR criteria at12months and those who did not(AUC for the ROC curves0.88[Norway],0.67[France],and0.72 [Rotterdam]).Visual inspection of the diagnostic test parameters associated with curves that used MTX initi-ation as the outcome showed a maximum slope for both the positive and negative likelihood ratios between a score of60/100and70/100,with flattening thereafter(67 in the Norway cohort,66in the French cohort,and66in the Rotterdam cohort).The cut point of60–70that was derived from expert consensus was therefore supported by these data.Given the consistency with the consensus-based approach,and to maximize sensitivity of the criteria,a cut point of60was deemed to be most appropriate.Rationale for the composition and weight of the final criteria.For development of the final criteria set, the results and weights from the comprehensive Phase2 process(26)were used as a starting point.Based onTable2.Summary of Phase2results and subsequent modificationsExact (0Ϫ100)Rescaled(0Ϫ10)Rounded to0.5(0Ϫ10)Joint involvement*1large000Ͼ1Ϫ10large,asymmetric10.2 1.021Ͼ1Ϫ10large,symmetric16.1 1.61 1.51Ϫ3small21.2 2.1224Ϫ10small28.8 2.883Ͼ10,including at least1small joint50.8 5.085Serology†Negative RF andnegative ACPA000Low-positive RF orlow-positive ACPA22.0 2.202High-positive RF orhigh-positive ACPA33.9 3.39 3.5Acute-phase reactants‡Normal CRP andnormal ESR000Abnormal CRP orabnormal ESR5.90.590.5Duration of symptoms§Ͻ6weeks000Ն6weeks9.30.931*Joint involvement refers to any swollen or tender joint on examina-tion.Distal interphalangeal joints,first carpometacarpal joints,andfirst metatarsophalangeal joints are excluded from assessment.Catego-ries of joint distribution are classified according to the location andnumber of the involved joints,with placement into the highest categorypossible based on the pattern of joint involvement.“Large joints”refers to shoulders,elbows,hips,knees,and ankles.“Small joints”refers to the metacarpophalangeal joints,proximal interphalangealjoints,second through fifth metatarsophalangeal joints,thumb inter-phalangeal joints,and wrists.“Symmetric”is defined as bilateralinvolvement of at least1region.In the category“Ͼ10joints,”at least1of the involved joints must be a small joint;the other joints caninclude any combination of large and additional small joints,as well asother joints not specifically listed elsewhere(e.g.,temporomandibular,acromioclavicular,sternoclavicular,etc.).†Negative refers to IU values that are less than or equal to the upperlimit of normal(ULN)for the laboratory and assay;low-positive refersto IU values that are higher than the ULN butՅ3times the ULN forthe laboratory and assay;high-positive refers to IU values that areϾ3times the ULN for the laboratory and assay.Where rheumatoid factor(RF)information is only available as positive or negative,a positiveresult should be scored as low-positive for RF.ACPAϭantiϪcitrullinated protein antibody.‡Normal/abnormal is determined by local laboratory standards.CRPϭC-reactive protein;ESRϭerythrocyte sedimentation rate.§Duration of symptoms refers to patient self-report of the duration ofsigns or symptoms of synovitis(e.g.,pain,swelling,tenderness)ofjoints that are clinically involved at the time of assessment,regardlessof treatment status.ACR/EULAR CLASSIFICATION CRITERIA FOR RA2573these categories and weights,we aimed in the final steps of the project to simplify the criteria in order to ensure that they were user friendly.We used the results of the data-driven Phase1as a guide for these adaptations,and verified at each step that the main properties of the criteria were not altered and that classification of pa-tients remained unchanged.The general steps toward simplification are shownTable3.The2010American College of Rheumatology/European League Against Rheumatism classi-fication criteria for rheumatoid arthritisScoreTarget population(Who should be tested?):Patients who1)have at least1joint with definite clinical synovitis(swelling)*2)with the synovitis not better explained by another disease†Classification criteria for RA(score-based algorithm:add score of categories A–D;a score ofՆ6/10is needed for classification of a patient as having definite RA)‡A.Joint involvement§1large joint¶02Ϫ10large joints11Ϫ3small joints(with or without involvement of large joints)#24Ϫ10small joints(with or without involvement of large joints)3Ͼ10joints(at least1small joint)**5B.Serology(at least1test result is needed for classification)††Negative RF and negative ACPA0Low-positive RF or low-positive ACPA2High-positive RF or high-positive ACPA3C.Acute-phase reactants(at least1test result is needed for classification)‡‡Normal CRP and normal ESR0Abnormal CRP or abnormal ESR1D.Duration of symptoms§§Ͻ6weeks0Ն6weeks1*The criteria are aimed at classification of newly presenting patients.In addition,patients with erosivedisease typical of rheumatoid arthritis(RA)with a history compatible with prior fulfillment of the2010criteria should be classified as having RA.Patients with longstanding disease,including those whosedisease is inactive(with or without treatment)who,based on retrospectively available data,havepreviously fulfilled the2010criteria should be classified as having RA.†Differential diagnoses vary among patients with different presentations,but may include conditions suchas systemic lupus erythematosus,psoriatic arthritis,and gout.If it is unclear about the relevant differentialdiagnoses to consider,an expert rheumatologist should be consulted.‡Although patients with a score ofϽ6/10are not classifiable as having RA,their status can be reassessedand the criteria might be fulfilled cumulatively over time.§Joint involvement refers to any swollen or tender joint on examination,which may be confirmed byimaging evidence of synovitis.Distal interphalangeal joints,first carpometacarpal joints,and firstmetatarsophalangeal joints are excluded from assessment.Categories of joint distribution are classifiedaccording to the location and number of involved joints,with placement into the highest category possiblebased on the pattern of joint involvement.¶“Large joints”refers to shoulders,elbows,hips,knees,and ankles.#“Small joints”refers to the metacarpophalangeal joints,proximal interphalangeal joints,second throughfifth metatarsophalangeal joints,thumb interphalangeal joints,and wrists.**In this category,at least1of the involved joints must be a small joint;the other joints can include anycombination of large and additional small joints,as well as other joints not specifically listed elsewhere(e.g.,temporomandibular,acromioclavicular,sternoclavicular,etc.).††Negative refers to IU values that are less than or equal to the upper limit of normal(ULN)for thelaboratory and assay;low-positive refers to IU values that are higher than the ULN butՅ3times the ULNfor the laboratory and assay;high-positive refers to IU values that areϾ3times the ULN for thelaboratory and assay.Where rheumatoid factor(RF)information is only available as positive or negative,a positive result should be scored as low-positive for RF.ACPAϭantiϪcitrullinated protein antibody.‡‡Normal/abnormal is determined by local laboratory standards.CRPϭC-reactive protein;ESRϭerythrocyte sedimentation rate.§§Duration of symptoms refers to patient self-report of the duration of signs or symptoms of synovitis(e.g.,pain,swelling,tenderness)of joints that are clinically involved at the time of assessment,regardlessof treatment status.2574ALETAHA ET AL。
类风湿性关节炎诊疗指南一、疾病概述类风湿性关节炎通常会侵犯双侧对称性的多个关节,尤其是手、足小关节。
其病因尚不明确,但可能与遗传、环境、感染、内分泌等多种因素有关。
在病理上,主要表现为滑膜炎症、增生,形成血管翳,侵犯关节软骨、骨和肌腱等组织,导致关节破坏和畸形。
二、临床表现1、关节症状疼痛:常为对称性、持续性疼痛,关节活动时疼痛加剧。
肿胀:关节周围软组织肿胀,可伴有关节积液。
晨僵:晨起时关节僵硬,活动后逐渐减轻,持续时间常超过 1 小时。
畸形:晚期可出现关节畸形,如掌指关节半脱位、手指向尺侧偏斜等。
2、关节外表现类风湿结节:常见于关节伸侧、受压部位或经常摩擦处。
肺部病变:如间质性肺炎、胸膜炎等。
心脏病变:心包炎较为常见。
眼部病变:巩膜炎、角膜炎等。
神经系统病变:周围神经受压引起的感觉和运动障碍。
三、诊断标准目前常用的诊断标准包括:1、关节晨僵至少 1 小时,持续 6 周以上。
2、有 3 个或 3 个以上关节肿胀,持续 6 周以上。
3、掌指关节、近端指间关节或腕关节肿胀,持续 6 周以上。
4、对称性关节肿胀,持续 6 周以上。
5、皮下类风湿结节。
6、手和腕关节的 X 线片显示有骨侵蚀或骨质疏松。
7、血清类风湿因子阳性(滴度>1:32)。
符合以上 7 项中的 4 项即可诊断为类风湿性关节炎,但应注意排除其他疾病。
四、检查方法1、实验室检查类风湿因子(RF):约 70% 80%的患者 RF 阳性,但 RF 阳性不一定都是类风湿性关节炎,其他疾病如干燥综合征、系统性红斑狼疮等也可阳性。
抗环瓜氨酸肽抗体(抗 CCP 抗体):对类风湿性关节炎的诊断具有较高的特异性。
红细胞沉降率(ESR)和 C 反应蛋白(CRP):可反映疾病的活动程度。
血常规:可出现贫血、血小板增多等。
2、影像学检查X 线:早期可见关节周围软组织肿胀,骨质疏松;晚期可见关节间隙狭窄、关节面破坏、关节畸形等。
磁共振成像(MRI):能更早期发现滑膜炎症、骨髓水肿等病变。
2010 ACR/EULAR 类风湿关节炎分类标准发表时间:2010-09-18 发表者:张昌丽 (访问人次:310)目标人群:有下列表现的患者:1、有至少一个关节具有明确的临床滑膜炎(肿胀)【新标准目的在于给新症患者分类。
另外,具有侵蚀性疾病如类风湿关节炎典型表现,其病史符合2010标准的,应该分类为类风湿关节炎。
患者有长期疾病,包括那些疾病处于非活动期(经过治疗或未经治疗),基于回顾性的可以获得的资料,先前符合2010年标准的,也应分类为类风湿关节炎。
】2、具有滑膜炎,用其他疾病不能得到更好解释的【不同表现的患者鉴别诊断也不同,但是系统性红斑狼疮,银屑病关节炎和痛风应该可以包括在内。
如果不清楚应该考虑哪些相关的鉴别诊断,应该咨询风湿病学专家】RA分类标准(评分算法:A-D的项目评分相加;患者如果按下列标准评分≥6/10,明确诊断为类风湿性关节炎)【虽然患者评分不足6分的不能分类为类风湿关节炎,但是他们的状态可以再次评价,随着时间推移,可能会符合标准。
】A:受累关节【指的是查体时发现的任何肿胀或触痛的关节,可通过滑膜炎的影像学证据证实。
在评估中,远端指间关节,第一腕掌和第一跖趾关节除外。
关节分布的分类根据受累关节的位置和数量,划入最可能受累关节类目。
】- 1个大关节(0分)【大关节指的是肩关节,肘关节,髋关节,膝关节和踝关节】- 2-10大关节(1分)- 1-3小关节(有或没有大关节)(2分)【小关节指的是掌指关节,近端指间关节,2-5跖趾关节,拇指指间关节和腕关节】- 4-10小关节(有或没有大关节)(3分)-超过10个小关节(至少一个小关节)(5分)【在这一条中,至少一个受累关节必须是小关节;其他关节可以包括任何大的或额外的小关节的组合,如其他别处未特别列出的关节(颞颌关节,肩峰锁骨关节,胸锁关节)】B:血清学(至少需要1项结果)【阴性指的是低于或等于当地实验室正常值的上限。
低滴度阳性指的是国际单位值高于正常值上限,但是低于正常值上限3倍。