国外GMP检查详细条款
- 格式:docx
- 大小:32.82 KB
- 文档页数:14

PscwgoGMP认证检查条款摘要PscwgoGMP认证是指医药产品的GMP认证,该认证的通过将证明医药产品符合相关的规范和标准,进而确保医药产品的质量和安全性。
本文档将介绍PscwgoGMP认证的检查条款,以帮助企业更好地了解认证的要求。
综述PscwgoGMP认证是全球GMP认证中的一种。
该认证为医药企业提供了在其工厂和办公室内创造高质量产品的标准指南。
通过PscwgoGMP认证,企业能够证明其生产过程和产品质量符合GMP的相关标准。
这些标准有助于确保产品的有效性、质量和安全性。
检查条款以下是PscwgoGMP认证的检查条款:1. 生产过程质量保证企业必须确保其产品的生产过程质量保证满足相关标准。
这包括确保生产场所的卫生条件和环境严格控制,保证原材料来源可靠,并且产品生产工艺符合产品要求。
2. 人员素质生产企业应确保员工的知识、技能和权限符合相关标准。
企业必须提供充分的培训,确保员工了解标准和制度,有能力履行其职责。
3. 生产记录生产企业必须记录其生产过程的每一个重要环节,并且记录必须包括企业的货源和生产记录。
生产记录应当满足定量和定性分析的要求。
4. 原材料控制企业必须保证其采用的原材料质量合格,并且来源可靠。
必须推行质量管理与质量控制,以确保原材料的质量和安全性。
5. 准确有效的分析方法生产企业应保证其使用的分析方法准确有效。
方法应基于严格详细的标准、公约和横向对照法(如正交试验等),并应得到认可和使用。
6. 检验证实生产企业必须保证其使用的检验方法符合标准,以证明生产过程和产品符合相关规范。
每一台检验设备应进行检验,以证明它的有效性和准确性。
7. 生产过程质量活动记录PscwgoGMP认证要求生产企业要记录其生产过程质量活动,并要妥善保管这些记录。
这些记录应包括所有重要的固定性过程、检验记录和处理计划,并且必须采取适当的措施记录操作。
8. 合格确认和批次记录生产企业应记录和审核产品相关批次信息,以限定和追踪有关不良事件及支援市场监测。
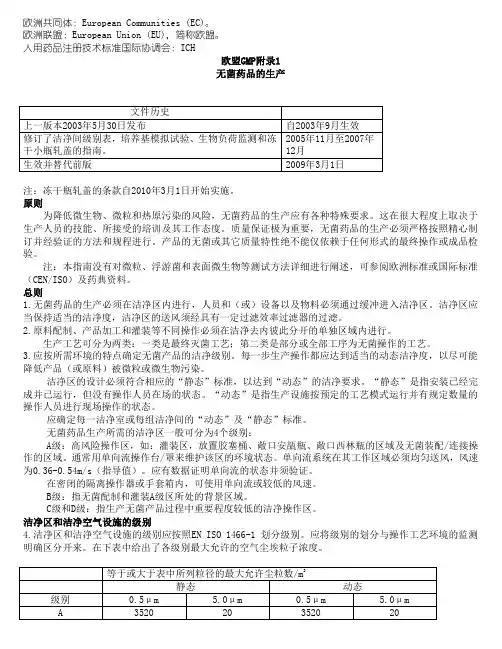
欧洲共同体:European Communities (EC)。
欧洲联盟:European Union (EU),简称欧盟。
人用药品注册技术标准国际协调会:ICH欧盟GMP附录1无菌药品的生产注:冻干瓶轧盖的条款自2010年3月1日开始实施。
原则为降低微生物、微粒和热原污染的风险,无菌药品的生产应有各种特殊要求。
这在很大程度上取决于生产人员的技能、所接受的培训及其工作态度。
质量保证极为重要,无菌药品的生产必须严格按照精心制订并经验证的方法和规程进行。
产品的无菌或其它质量特性绝不能仅依赖于任何形式的最终操作或成品检验。
注:本指南没有对微粒、浮游菌和表面微生物等测试方法详细进行阐述,可参阅欧洲标准或国际标准(CEN/ISO)及药典资料。
总则1.无菌药品的生产必须在洁净区内进行,人员和(或)设备以及物料必须通过缓冲进入洁净区。
洁净区应当保持适当的洁净度,洁净区的送风须经具有一定过滤效率过滤器的过滤。
2.原料配制、产品加工和灌装等不同操作必须在洁净去内彼此分开的单独区域内进行。
生产工艺可分为两类:一类是最终灭菌工艺;第二类是部分或全部工序为无菌操作的工艺。
3.应按所需环境的特点确定无菌产品的洁净级别。
每一步生产操作都应达到适当的动态洁净度,以尽可能降低产品(或原料)被微粒或微生物污染。
洁净区的设计必须符合相应的“静态”标准,以达到“动态”的洁净要求。
“静态”是指安装已经完成并已运行,但没有操作人员在场的状态。
“动态”是指生产设施按预定的工艺模式运行并有规定数量的操作人员进行现场操作的状态。
应确定每一洁净室或每组洁净间的“动态”及“静态”标准。
无菌药品生产所需的洁净区一般可分为4个级别:A级:高风险操作区,如:灌装区,放置胶塞桶、敞口安瓿瓶、敞口西林瓶的区域及无菌装配/连接操作的区域。
通常用单向流操作台/罩来维护该区的环境状态。
单向流系统在其工作区域必须均匀送风,风速为0.36-0.54m/s(指导值)。
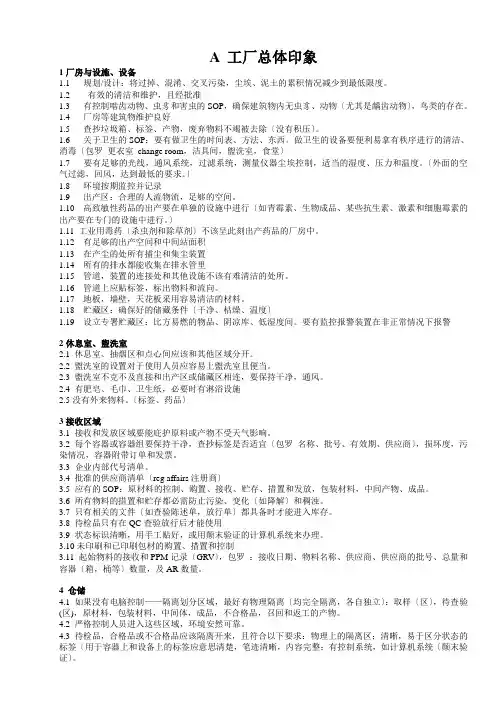
A 工厂总体印象1厂房与设施、设备1.1 规划/设计:将过掉、混淆、交叉污染,尘埃、泥土的累积情况减少到最低限度。
1.2 有效的清洁和维护,且经批准1.3 有控制啮齿动物、虫豸和害虫的SOP,确保建筑物内无虫豸、动物〔尤其是龋齿动物〕,鸟类的存在。
1.4 厂房等建筑物维护良好1.5 查抄垃圾箱、标签、产物,废弃物料不竭被去除〔没有积压〕。
1.6 关于卫生的SOP:要有做卫生的时间表、方法、东西。
做卫生的设备要便利易拿有秩序进行的清洁、消毒〔包罗更衣室change room,洁具间,盥洗室,食堂〕1.7 要有足够的光线,通风系统,过滤系统,测量仪器尘埃控制,适当的湿度、压力和温度。
〔外面的空气过滤,回风,达到最低的要求。
〕1.8 环境按期监控并记录1.9 出产区:合理的人流物流,足够的空间。
1.10 高致敏性药品的出产要在单独的设施中进行〔如青霉素、生物成品、某些抗生素、激素和细胞霉素的出产要在专门的设施中进行。
〕1.11 工业用毒药〔杀虫剂和除草剂〕不该呈此刻出产药品的厂房中。
1.12 有足够的出产空间和中间站面积1.13 在产尘的处所有捕尘和集尘装置1.14 所有的排水都能收集在排水管里1.15 管道,装置的连接处和其他设施不该有难清洁的处所。
1.16 管道上应贴标签,标出物料和流向。
1.17 地板,墙壁,天花板采用容易清洁的材料。
1.18 贮藏区:确保好的储藏条件〔干净、枯燥、温度〕1.19 设立专署贮藏区:比方易燃的物品、阴凉库、低湿度间。
要有监控报警装置在非正常情况下报警2休息室、盥洗室2.1 休息室、抽烟区和点心间应该和其他区域分开。
2.2 盥洗室的设置对于使用人员应容易上盥洗室且便当。
2.3 盥洗室不克不及直接和出产区或储藏区相连,要保持干净,通风。
2.4 有肥皂、毛巾、卫生纸,必要时有淋浴设施2.5没有外来物料。
〔标签、药品〕3接收区域3.1 接收和发放区域要能庇护原料或产物不受天气影响。
美国现行药品生产质量管理规范(cGMP)目录A-总则 (3)B-组织与人员 (3)C-厂房与设施 (4)D-设备 (7)E-成份、药品容器和密封件的控制 (8)F-生产和加工控制 (11)G-包装和标签控制 (13)H-贮存和销售 (16)I-实验室控制 (17)J-记录和报告 (20)K-退回的药品和回收处理 (25)A.总则211·1 范围(a) 本部分的条例包含人用或兽用药品制备的现行最低限度的药品生产质量管理规范(GMP)。
(b) 在本章里的这些针对药品的现行GMP条例和本章600至800的所有部分针对人用生物制品的现行GMP条例,除非明确另有说明者外,应认为是对本部分条例的补充,而不是代替。
本章其他部分或本章600至680各部分和本部分均可适用的条例,前部分的条例可代替本部分条例。
(c) 在考虑经提议的,发表在1978年9月29日联邦注册表(FR)上一项免除时,若产品及其所有成份是以人用物品形式作一般销售和消费,且这些产品根据其预期用途,亦可列入药品的范围内,则不应对这些非处方药(OTC)实施本部分条例,直至进一步的通知为止。
本章110部分和113至119部分的条例用于鉴别这些亦是食品的OTC药品是否按照GMP的要求生产、加工、包装和贮存。
211·3 定义本章210·3的定义适用于本部分。
B. 组织与人员211.22 质量控制部门的职责(a) 本部门有批准和拒收所有成份、药品包装容器、密封件、中间体、包装材料、标签及药品的职责与权力。
复查生产记录的权力,保证不产生差错,或若发生差错,保证他们充分调查这些差错。
本部门负责根据合同,批准或拒收由其它公司,生产、加工、包装或贮存的产品。
(b) 适当的实验室检验设备、批准(或拒收)的各种成份、药品容器、密封件、包装材料及药品,质量控制部门是可以获得的。
(c) 本部门有批准或驳回影响药品的均一性、效价或含量、质量及纯度的所有程序或规格标准的职责。
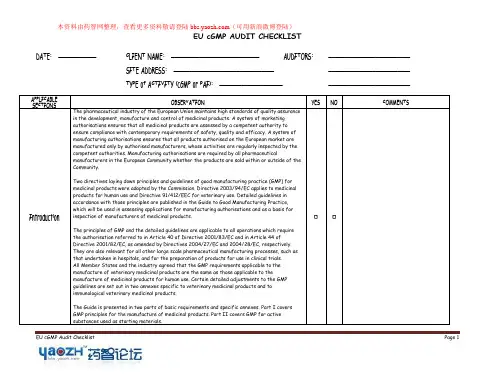
EU cGMP Audit Checklist Page 1EU cGMP AUDIT CHECKLISTDATE: ____________ CLIENT NAME: ____________________________ AUDITORS: __________________________ SITE ADDRESS: __________________________________________________________TYPE of ACTIVITY (cGMP or PAI): ______________________________________________APPLICABLE SECTIONSOBSERVATIONYESNOCOMMENTSIntroductionThe pharmaceutical industry of the European Union maintains high standards of quality assurance in the development, manufacture and control of medicinal products. A system of marketing authorisations ensures that all medicinal products are assessed by a competent authority to ensure compliance with contemporary requirements of safety, quality and efficacy. A system of manufacturing authorisations ensures that all products authorised on the European market are manufactured only by authorised manufacturers, whose activities are regularly inspected by the competent authorities. Manufacturing authorisations are required by all pharmaceuticalmanufacturers in the European Community whether the products are sold within or outside of the Community.Two directives laying down principles and guidelines of good manufacturing practice (GMP) for medicinal products were adopted by the Commission. Directive 2003/94/EC applies to medicinal products for human use and Directive 91/412/EEC for veterinary use. Detailed guidelines in accordance with those principles are published in the Guide to Good Manufacturing Practice, which will be used in assessing applications for manufacturing authorisations and as a basis for inspection of manufacturers of medicinal products.The principles of GMP and the detailed guidelines are applicable to all operations which require the authorisation referred to in Article 40 of Directive 2001/83/EC and in Article 44 ofDirective 2001/82/EC, as amended by Directives 2004/27/EC and 2004/28/EC, respectively. They are also relevant for all other large scale pharmaceutical manufacturing processes, such as that undertaken in hospitals, and for the preparation of products for use in clinical trials. All Member States and the industry agreed that the GMP requirements applicable to the manufacture of veterinary medicinal products are the same as those applicable to themanufacture of medicinal products for human use. Certain detailed adjustments to the GMP guidelines are set out in two annexes specific to veterinary medicinal products and to immunological veterinary medicinal products.The Guide is presented in two parts of basic requirements and specific annexes. Part I covers GMP principles for the manufacture of medicinal products. Part II covers GMP for active substances used as starting materials.EU cGMP Audit ChecklistPage 2Chapters of Part I on “basic requirements” are headed by principles as defined in Directives2003/94/EC and 91/412/EEC. Chapter 1 on Quality Management outlines the fundamental concept of quality assurance as applied to the manufacture of medicinal products. Thereafter, eachchapter has a principle outlining the quality assurance objectives of that chapter and a text which provides sufficient detail for manufacturers to be made aware of the essential matters to be considered when implementing the principle.Part II was newly established on the basis of a guideline developed on the level of ICH and publishe d as ICH Q7a on “active pharmaceutical ingredients”, which was implemented as GMP Annex 18 for voluntary application in 2001. According to the revised Article 47 and Article 51, respectively, of the Directive 2001/83/EC and Directive 2001/82/EC, as amended, detailed guidelines on the principles of GMP for active substances used as starting materials shall be adopted and published by the Commission. The former Annex 18 has been replaced by the new Part II of the GMP Guide, which has an extended application both for the human and the veterinary sector.In addition to the general matters of Good Manufacturing Practice outlined in Parts I and II, a series of annexes providing detail about specific areas of activity is included. For some manufacturing processes, different annexes will apply simultaneously (e.g. annex on sterile preparations and on radiopharmaceuticals and/or on biological medicinal products).A glossary of some terms used in the Guide has been incorporated after the annexes.The Guide is not intended to cover security aspects for the personnel engaged in manufacture. This may be particularly important in the manufacture of certain medicinal products such ashighly active, biological and radioactive medicinal products. However, those aspects are governed by other provisions of Community or national law.Throughout the Guide it is assumed that the requirements of the Marketing Authorisationrelating to the safety, quality and efficacy of the products are systematically incorporated into all the manufacturing, control and release for sale arrangements of the holder of the Manufacturing Authorisation.The manufacture of medicinal products has for many years taken place in accordance with guidelines for Good Manufacturing Practice and the manufacture of medicinal products is not governed by CEN/ISO standards. Harmonised standards as adopted by the European standardisation organisations CEN/ISO may be used at industry’s discretion as a tool forimplementing a quality system in the pharmaceutical sector. The CEN/ISO standards have been considered but the terminology of these standards has not been implemented in this third edition of the Guide.EU cGMP Audit Checklist Page 3It is recognised that there are acceptable methods, other than those described in the Guide, which are capable of achieving the principles of Quality Assurance. The Guide is not intended to place any restraint upon the development of any new concepts or new technologies which have been validated and which provide a level of Quality Assurance at least equivalent to those set out in this Guide. It will be regularly revised.EU cGMP Audit ChecklistPage 4APPLICABLESECTIONSOBSERVATION YES NO COMMENTS 1.0 QualityManagementPrinciples ∙Does the sponsor’s quality management appear to satisfy the criteria outlined in the principlesas detailed in the following statement?The holder of a Manufacturing Authorisation must manufacture medicinal products so as to ensure that theyare fit for their intended use, comply with the requirements of the Marketing Authorisation and do not placepatients at risk due to inadequate safety, quality or efficacy. The attainment of this quality objective is theresponsibility of senior management and requires the participation and commitment by staff in many differentdepartments and at all levels within th e company, by the company’s suppliers and by the distributors. To achievethe quality objective in a reliable manner there must be a comprehensively designed and correctly implementedsystem of Quality Assurance incorporating Good Manufacturing Practice and thus Quality Control. It should befully documented and its effectiveness monitored. All parts of the Quality Assurance system should beadequately resourced with competent personnel, and suitable and sufficient premises, equipment and facilities.There are additional legal responsibilities for the holder of the Manufacturing Authorisation and for theQualified Person(s).Quality Assurance ∙Is the QA group of the firm adhering to the major milestones outlined below?Quality Assurance is a wide ranging concept which covers all matters which individually or collectively influencethe quality of a product. It is the total sum of the organised arrangements made with the object of ensuringthat medicinal products are of the quality required for their intended use. Quality Assurance thereforeincorporates Good Manufacturing Practice plus other factors outside the scope of this Guide. The system ofQuality Assurance appropriate for the manufacture of medicinal products should ensure that:i.medicinal products are designed and developed in a way that takes account of the requirements of GoodManufacturing Practice and Good Laboratory Practice;ii.production and control operations are clearly specified and Good Manufacturing Practice adopted;iii.managerial responsibilities are clearly specified;iv.arrangements are made for the manufacture, supply and use of the correct starting and packaging materials;v.all necessary controls on intermediate products, and any other in-process controls and validations are carried out;vi.the finished product is correctly processed and checked, according to the defined procedures;vii.medicinal products are not sold or supplied before a Qualified Person has certified that each production batch has been produced and controlled in accordance with the requirements of the Marketing Authorisation and any otherregulations relevant to the production, control and release of medicinal products;viii.satisfactory arrangements exist to ensure, as far as possible, that the medicinal products are stored, distributed and subsequently handled so that quality is maintained throughout their shelf life;ix.there is a procedure for Self-Inspection and/or quality audit which regularly appraises the effectiveness andapplicability of the Quality Assurance system.cGMP ∙Does the QA group adhere to cGMP concepts as outlined below?Good Manufacturing Practice is that part of Quality Assurance which ensures that products are consistentlyproduced and controlled to the quality standards appropriate to their intended use and as required by theMarketing Authorisation or product specification. Good Manufacturing Practice is concerned with bothproduction and quality control. The basic requirements of GMP are that:EU cGMP Audit Checklist Page 51.0 Quality Managementi.all manufacturing processes are clearly defined, systematically reviewed in the light of experience and shown to be capable of consistently manufacturing medicinal products of the required quality and complying with their specifications;ii. critical steps of manufacturing processes and significant changes to the process are validated; iii. all necessary facilities for GMP are provided including: iv. appropriately qualified and trained personnel; v. adequate premises and space; vi. suitable equipment and services;vii. correct materials, containers and labels; viii. approved procedures and instructions; ix. suitable storage and transport;x. instructions and procedures are written in an instructional form in clear and unambiguous language, specifically applicable to the facilities provided;xi. operators are trained to carry out procedures correctly;xii.records are made, manually and/or by recording instruments, during manufacture which demonstrate that all thesteps required by the defined procedures and instructions were in fact taken and that the quantity and quality of the product was as expected. Any significant deviations are fully recorded and investigated;xiii. records of manufacture including distribution which enable the complete history of a batch to be traced, are retained in a comprehensible and accessible form;xiv. the distribution (wholesaling) of the products minimises any risk to their quality; xv. a system is available to recall any batch of product, from sale or supply;xvi.complaints about marketed products are examined, the causes of quality defects investigated and appropriate measures taken in respect of the defective products and to prevent reoccurrence.Quality Control∙ Does the QA group adhere to the QC principles outlined below?Quality Control is that part of Good Manufacturing Practice which is concerned with sampling, specifications and testing, and with the organisation, documentation and release procedures which ensure that the necessary and relevant tests are actually carried out and that materials are not released for use, nor products released for sale or supply, until their quality has been judged to be satisfactory. The basic requirements of Quality Control are that:i.adequate facilities, trained personnel and approved procedures are available for sampling, inspecting and testing starting materials, packaging materials, intermediate, bulk, and finished products, and where appropriate for monitoring environmental conditions for GMP purposes;ii. samples of starting materials, packaging materials, intermediate products, bulk products and finished products are taken by personnel and by methods approved by Quality Control; iii. test methods are validated;iv. records are made, manually and/or by recording instruments, which demonstrate that all the required sampling, inspecting and testing procedures were actually carried out. Any deviations are fully recorded and investigated; v.the finished products contain active ingredients complying with the qualitative and quantitative composition of the Marketing Authorisation, are of the purity required, and are enclosed within their proper containers and correctly labelled;vi.records are made of the results of inspection and that testing of materials, intermediate, bulk, and finished products is formally assessed against specification. Product assessment includes a review and evaluation of relevant production documentation and an assessment of deviations from specified procedures;vii. no batch of product is released for sale or supply prior to certification by a Qualified Person that it is in accordance with the requirements of the Marketing Authorisation;viii.sufficient reference samples of starting materials and products are retained to permit future examination of theEU cGMP Audit Checklist Page 61.0 Quality Managementproduct if necessary and that the product is retained in its final pack unless exceptionally large packs are produced.Product QualityReviewDoes the QA group adhere to the following principles regarding product quality review?Regular periodic or rolling quality reviews of all licensed medicinal products, including export only products, should be conducted with the objective of verifying the consistency of the existing process, theappropriateness of current specifications for both starting materials and finished product to highlight any trends and to identify product and process improvements. Such reviews should normally be conducted and documented annually, taking into account previous reviews, and should include at least:i. A review of starting materials and packaging materials used for the product, especially those from new sources; ii. A review of critical in-process controls and finished product results;iii. A review of all batches that failed to meet established specification(s) and their investigation;iv. A review of all significant deviations or non-conformances, their related investigations, and the effectiveness of resultant corrective and preventative actions taken;v. A review of all changes carried out to the processes or analytical methods;vi. A review of Marketing Authorisation variations submitted/granted/refused, including those for third country (export only) dossiers;vii. A review of the results of the stability monitoring programme and any adverse trends;viii. A review of all quality-related returns, complaints and recalls and the investigations performed at the time; ix. A review of adequacy of any other previous product process or equipment corrective actions;x. For new marketing authorisations and variations to marketing authorisations, a review of post-marketing commitments;xi. The qualification status of relevant equipment and utilities, e.g. HVAC, water, compressed gases, etc; xii.A review of Technical Agreements to ensure that they are up to date.The manufacturer and marketing authorisation holder, where different, should evaluate the results of thisreview and an assessment should be made whether corrective and preventative action or any revalidation should be undertaken. Reasons for such corrective actions should be documented. Agreed corrective and preventative actions should be completed in a timely and effective manner. There should be management procedures for the ongoing management and review of these actions and the effectiveness of these procedures verified during self inspection. Quality reviews may be grouped by product type, e.g. solid dosage forms, liquid dosage forms, sterile products, etc. where scientifically justified.Where the marketing authorisation holder is not the manufacturer, there should be a technical agreement in place between the various parties that defines their respective responsibilities in producing the quality review. The Qualified Person responsible for final batch certification together with the marketing authorisation holder should ensure that the quality review is performed in a timely manner and is accurate.EU cGMP Audit Checklist Page 7APPLICABLE SECTIONS OBSERVATIONYESNOCOMMENTS2.0 PersonnelPrinciple∙ Does the sponsor have adequate personnel systems in place to meet the criteria outlined in the following statement?The establishment and maintenance of a satisfactory system of quality assurance and the correct manufacture of medicinal products relies upon people. For this reason there must be sufficient qualified personnel to carry out all the tasks which are the responsibility of the manufacturer. Individual responsibilities should be clearly understood by the individuals and recorded. All personnel should be aware of the principles of Good Manufacturing Practice that affect them and receive initial and continuing training, including hygiene instructions, relevant to their needs.General∙ Is the sponsor in compliance with the following statements?2.1 The manufacturer should have an adequate number of personnel with the necessary qualifications and practical experience. The responsibilities placed on any one individual should not be so extensive as to present any risk to quality.2.2 The manufacturer must have an organisation chart. People in responsible positions should have specific duties recorded in written job descriptions and adequate authority to carry out their responsibilities. Their duties may be delegated to designated deputies of a satisfactory qualification level. There should be no gaps or unexplained overlaps in the responsibilities of those personnel concerned with the application of Good Manufacturing Practice.Key Personnel∙ Is the sponsor in compliance with the following areas?2.3 Key Personnel include the head of Production, the head of Quality Control, and if at least one of these persons is not responsible for the duties described in Article 51 of Directive 2001/83/EC,1 the QualifiedPerson(s) designated for the purpose. Normally key posts should be occupied by full-time personnel. The heads of Production and Quality Control must be independent from each other. In large organisations, it may be necessary to delegate some of the functions listed in 2.5, 2.6 and 2.7.2.4 The duties of the Qualified Person(s) are fully described in Article 51 of Directive 2001/83/EC, and can be summarised as follows:a. for medicinal products manufactured within the European Community, a Qualified Person must ensurethat each batch has been produced and tested/checked in accordance with the directives and the marketing authorisation;2 b. for medicinal products manufactured outside the European Community, a Qualified Person mustensure that each imported batch has undergone, in the importing country, the testing specified in paragraph 1 (b) of Article 51; c. a Qualified Person must certify in a register or equivalent document, as operations are carried outand before any release, that each production batch satisfies the provisions of Article 51.The persons responsible for these duties must meet the qualification requirements laid down in Article 493 of2.0 Personnelthe same Directive, they shall be permanently and continuously at the disposal of the holder of theManufacturing Authorisation to carry out their responsibilities. Their responsibilities may be delegated, butonly to other Qualified Person(s).2.5 The head of the Production Department generally has the following responsibilities:i.to ensure that products are produced and stored according to the appropriate documentation inorder to obtain the required quality;ii.to approve the instructions relating to production operations and to ensure their strictimplementation;iii.to ensure that the production records are evaluated and signed by an authorised person before theyare sent to the Quality Control Department;iv.to check the maintenance of his department, premises and equipment;v.to ensure that the appropriate validations are done;vi.to ensure that the required initial and continuing training of his department personnel is carried outand adapted according to need.2.6 The head of the Quality Control Department generally has the following responsibilities:i.to approve or reject, as he sees fit, starting materials, packaging materials, and intermediate, bulkand finished products;ii.to evaluate batch records;iii.to ensure that all necessary testing is carried out;iv.to approve specifications, sampling instructions, test methods and other Quality Control procedures;v.to approve and monitor any contract analysts;vi.to check the maintenance of his department, premises and equipment;vii.to ensure that the appropriate validations are done;viii.to ensure that the required initial and continuing training of his department personnel is carried outand adapted according to need.Other duties of the Quality Control Department are summarised in Chapter 6.2.7 The heads of Production and Quality Control generally have some shared, or jointly exercised,responsibilities relating to quality. These may include, subject to any national regulations:∙the authorisation of written procedures and other documents, including amendments;∙the monitoring and control of the manufacturing environment;∙plant hygiene;∙process validation;∙training;∙the approval and monitoring of suppliers of materials;∙the approval and monitoring of contract manufacturers;∙the designation and monitoring of storage conditions for materials and products;EU cGMP Audit Checklist Page 8EU cGMP Audit Checklist Page 92.0 Personnel∙ the retention of records;∙ the monitoring of compliance with the requirements of Good Manufacturing Practice;∙the inspection, investigation, and taking of samples, in order to monitor factors which may affect product quality.Training∙ Is the sponsor in compliance with the following areas?2.8 The manufacturer should provide training for all the personnel whose duties take them into production areas or into control laboratories (including the technical, maintenance and cleaning personnel), and for other personnel whose activities could affect the quality of the product.2.9 Besides the basic training on the theory and practice of Good Manufacturing Practice, newly recruited personnel should receive training appropriate to the duties assigned to them. Continuing training should also be given, and its practical effectiveness should be periodically assessed. Training programmes should be available, approved by either the head of Production or the head of Quality Control, as appropriate. Training records should be kept.2.10 Personnel working in areas where contamination is a hazard, e.g. clean areas or areas where highly active, toxic, infectious or sensitising materials are handled, should be given specific training.2.11 Visitors or untrained personnel should, preferably, not be taken into the Production and Quality Control areas. If this is unavoidable, they should be given information in advance, particularly about personal hygiene and the prescribed protective clothing. They should be closely supervised.2.12 The concept of Quality Assurance and all the measures capable of improving its understanding and implementation should be fully discussed during the training sessions.Personnel Hygiene∙ Is the sponsor in compliance with the following areas?2.13 Detailed hygiene programmes should be established and adapted to the different needs within the factory. They should include procedures relating to the health, hygiene practices and clothing of personnel.These procedures should be understood and followed in a very strict way by every person whose duties take him into the production and control areas. Hygiene programmes should be promoted by management and widely discussed during training sessions.2.14 All personnel should receive medical examination upon recruitment. It must be the manufacturer’sresponsibility that there are instructions ensuring that health conditions that can be of relevance to the quality of products c ome to the manufacturer’s knowledge. After the first medical examination, examinations should be carried out when necessary for the work and personal health.2.15 Steps should be taken to ensure as far as is practicable that no person affected by an infectious disease or having open lesions on the exposed surface of the body is engaged in the manufacture of medicinal products.2.16 Every person entering the manufacturing areas should wear protective garments appropriate to the operations to be carried out.2.0 Personnel2.17 Eating, drinking, chewing or smoking, or the storage of food, drink, smoking materials or personalmedication in the production and storage areas should be prohibited. In general, any unhygienic practice withinthe manufacturing areas or in any other area where the product might be adversely affected, should beforbidden.2.18 Direct contact should be avoided between the operator’s hands and the exposed product as well as withany part of the equipment that comes into contact with the products.2.19 Personnel should be instructed to use the hand-washing facilities.2.20 Any specific requirements for the manufacture of special groups of products, for example sterilepreparations, are covered in the annexes.EU cGMP Audit Checklist Page 10EU cGMP Audit Checklist Page 11APPLICABLE SECTIONS OBSERVATIONYESNOCOMMENTS3.0 Premises & EquipmentPrinciple∙ Is the sponsor in compliance with the following areas?Premises and equipment must be located, designed, constructed, adapted and maintained to suit the operations to be carried out. Their layout and design must aim to minimise the risk of errors and permit effective cleaning and maintenance in order to avoid cross-contamination, build up of dust or dirt and, in general, any adverse effect on the quality of products.Premises∙ Is the sponsor in compliance with the following areas?General3.1 Premises should be situated in an environment which, when considered together with measures to protect the manufacture, presents minimal risk of causing contamination of materials or products.3.2 Premises should be carefully maintained, ensuring that repair and maintenance operations do not present any hazard to the quality of products. They should be cleaned and, where applicable, disinfected according to detailed written procedures.3.3 Lighting, temperature, humidity and ventilation should be appropriate and such that they do not adversely affect, directly or indirectly, either the medicinal products during their manufacture and storage, or the accurate functioning of equipment.3.4 Premises should be designed and equipped so as to afford maximum protection against the entry of insects or other animals.3.5 Steps should be taken in order to prevent the entry of unauthorised people. Production, storage and quality control areas should not be used as a right of way by personnel who do not work in them.Production Area3.6 In order to minimise the risk of a serious medical hazard due to cross-contamination, dedicated and self contained facilities must be available for the production of particular medicinal products, such as highlysensitising materials (e.g. penicillins) or biological preparations (e.g. from live micro-organisms). The production of certain additional products, such as certain antibiotics, certain hormones, certain cytotoxics, certain highly active drugs and non-medicinal products should not be conducted in the same facilities. For those products, in exceptional cases, the principle of campaign working in the same facilities can be accepted provided thatspecific precautions are taken and the necessary validations are made. The manufacture of technical poisons, such as pesticides and herbicides, should not be allowed in premises used for the manufacture of medicinal products.3.7 Premises should preferably be laid out in such a way as to allow the production to take place in areas connected in a logical order corresponding to the sequence of the operations and to the requisite cleanliness levels.。
生物成品GMP查抄指南GMP INSPECTION GUIDELINE FOR BIO-PRODUCT由国家食品药品监督办理局颁布ISSUED BY SFDA OF CHINA1. 机构与人员COMPANY ORGANIZATION AND PERSONNEL→0402:生物成品出产企业出产和质量办理负责人是否具有相应的专业常识〔细菌学、病毒学、生物学、分子生物学、生物化学、免疫学、医学、药学等〕,并具有丰富的实践经验以确保在其出产、质量办理中履行其职责。
Whether the personnel who are in charge of the bio-products production and quality management that have the corresponding knowledge background on Bacteriology, Virology, Biology, Molecular Biology, Biochemistry, Immunology, Medicine,Pharmaceutics etc. and to possess abundant experience to insure fulfilling theresponsibilities in the production and quality management.→0702:从事生物成品制造的全体人员〔包罗清洁人员、维修人员〕是否按照其出产的成品和所从事的出产操作进行专业〔卫生学、微生物学等〕和平安防护培训。
Whether all the personnel (including the cleaning stuff and maintenance stuff) that related with the bio-products production who have received the professional training on production and corresponding knowledge (Hygiene, Microbiology etc.) and security training.2. 厂房与设施PREMISE AND FACILITY→*2201:出产用菌毒种与非出产用菌毒种、出产用细胞与非出产用细胞、强毒与弱毒、死毒与活毒、脱毒前与脱毒后的成品和活疫苗与灭活疫苗、人血液成品、预防成品等加工或灌装是否同时在同一出产厂房内进行。
欧盟托管法案(EU)20171569临床试验药GMP原则和指南COMMISSION DELEGATED REGULATION (EU) 2017/1569 of 23 May 2017supplementing Regulation (EU) No 536/2014 of the EuropeanParliament and of the Council by specifying principles of and guidelines forgood manufacturing practice for investigational medicinal products for humanuse and arrangements for inspections(Text with EEA relevance)欧盟托管法案(EU)2017/1569 2017年5月23日补充欧洲议会和欧盟委员会法规(EU)No.536/2014说明人用临床试验用药GMP原则和指南以及检查安排THEEUROPEAN COMMISSION,欧盟委员会Havingregard to the Treaty on the Functioning of the European Union,关于欧盟职能条约Havingregard to Regulation (EU) No 536/2014 of the European Parliament and of theCouncil of 16 April 2014 on clinical trials on medicinal products for humanuse, and repealing Directive 2001/20/EC[1],and in particular Article 63(1) thereof, 关于欧盟议会和委员会2014年4月16日关于人用临床试验用药的法规(EU)536/2014,以及即将废止的指令2001/20/EC,尤其是其中第63(1)条Whereas: 鉴于(1) The good manufacturing practice forinvestigational medicinal products for human use ensures that there isconsistency between batches of the same investigational medicinal product usedin the same or different clinical trials, andthat changes during thedevelopment of an investigational medicinal product are adequately documentedand justified. The manufacturing of investigational medicinal products presentsadditional challenges comparing to the manufacturing of authorised medicinal productsbecause there are no fixed routines, there is a variety of clinical trialdesigns and consequently packaging designs. Those challenges are due to theneed, often, of randomisation and to disguise the identity of theinvestigational medicinal products for the purpose of clinical trial(blinding). The toxicity, potency and sensitising potential of investigationalmedicinal products for human use may not be fully understood at the time of thetrial, and the need to minimise all risks of cross-contamination is thereforeof even greater importance than for authorised medicinal products. Because ofthis complexity, the manufacturing operations should be subject to a highlyeffective pharmaceutical quality system.人用临床试验用药GMP确保了用于相同或不同临床试验中的同种临床试验用药批次间的一致性,确保在临床试验用药研发期间的变更具有充分的记录和论证。

GUIDE TO GOOD MANUFACTURINGPRACTICE FOR MEDICINAL PRODUCTS药品GMP检查指南.PIC/S July 2004Reproduction prohibited for commercial purposes.Reproduction for internal use is authorised,provided that the source is acknowledged.Editor: PIC/S SecretariatP.O. Box 5695CH-1211 Geneva 11e-mail: daniel.brunner@web site: :// 1 July 2004 PE 009-2TABLE OF CONTENT目录INTRODUCTION介绍 (1)CHAPTER 1 QUALITY MANAGEMENT 质量管理 (4)PRINCIPLE 原则 (4)QUALITY ASSURANCE 质量保证 (4)GOOD MANUFACTURING PRACTICE FOR MEDICINAL PRODUCTS (GMP) 药品GMP (6)QUALITY CONTROL 质量控制 (7)CHAPTER 2 PERSONNEL 人员 (10)PRINCIPLE 原则 (10)GENERAL 通则 (10)KEY PERSONNEL 关键人员 (10)TRAINING 培训 (13)PERSONAL HYGIENE 个人卫生 (14)CHAPTER 3 PREMISES AND EQUIPMENT 厂房和设备 (16)PRINCIPLE 原则 (16)PREMISES General总则 (16)Production Area 生产区域 (17)Storage Areas 储存区域 (19)Quality Control Areas 质量控制区域 (20)Ancillary Areas 辅助区域 (20)EQUIPMENT 设备 (21)CHAPTER 4 DOCUMENTATION 文件 (23)PRINCIPLE 原则 (23)GENERAL 总则 (23)DOCUMENTS REQUIRED 必需的文件 (25)MANUFACTURING FORMULA AND PROCESSING INSTRUCTIONS 生产方法和加工指示 (27)PACKAGING INSTRUCTIONS 包装指示 (28)BA TCH PROCESSING RECORDS 批加工记录 (29)BA TCH PACKAGING RECORDS 批包装记录 (30)PROCEDURES AND RECORDS 程序和记录 (32)CHAPTER 5 PRODUCTION 生产 (36)PRINCIPLE 原则 (36)GENERAL 通则 (36)PREVENTION OF CROSS-CONTAMINATION IN PRODUCTION 生产过程中防止交叉污染 (38)V ALIDATION 验证 (39)STARTING MA TERIALS 起始物料 (40)PROCESSING OPERA TIONS - INTERMEDIATE AND BULK PRODUCTS 加工操作:中间体和散装产品 (42)PACKAGING MATERIALS 包装材料 (42)PACKAGING OPERATIONS 包装操作 (43)FINISHED PRODUCTS 最终成品 (45)REJECTED, RECOVERED AND RETURNED MATERIALS 拒绝的,回收的和退回的物料46CHAPTER 6 QUALITY CONTROL 质量控制 (48)PRINCIPLE 原则 (48)GENERAL 通则 (48)GOOD QUALITY CONTROL LABORATORY PRACTICE 优良质量控制实验室实践 (49)DOCUMENTATION 文件 (49)SAMPLING 取样 (50)TESTING 检测 (52)CHAPTER 7 CONTRACT MANUFACTURE AND ANAL YSIS 合同加工和分析 (55)PRINCIPLE 原则 (55)GENERAL 通则 (55)THE CONTRACT GIVER 合同提供人 (55)THE CONTRACT ACCEPTOR 合同接受人 (56)THE CONTRACT 合同 (57)CHAPTER 8 COMPLAINTS AND PRODUCT RECALL 抱怨和产品召回 (59)PRINCIPLE 原则 (59)COMPLAINTS 抱怨 (59)RECALLS 召回 (60)CHAPTER 9 SELF INSPECTION 自检 (61)PRINCIPLE 原则 (61)ANNEX 1 MANUFACTURE OF STERILE MEDICINAL PRODUCTS无菌药品的生产 (63)PRINCIPLE (63)GENERAL (63)BLOW/FILL/SEAL TECHNOLOGY (67)TERMINALL Y STERILISED PRODUCTS (67)ASEPTIC PREPARA TION (68)PERSONNEL (68)PREMISES (70)EQUIPMENT (71)SANITATION (71)PROCESSING (71)STERILISATION (73)STERILISATION BY HEA T (74)MOIST HEAT (75)DRY HEAT (75)STERILISATION BY RADIATION (75)STERILISATION WITH ETHYLENE OXIDE (76)FILTRATION OF MEDICINAL PRODUCTS WHICH CANNOT BE STERILISED IN THEIR FINAL CONTAINER (77)FINISHING OF STERILE PRODUCTS (77)QUALITY CONTROL (78)ANNEX 2 MANUFACTURE OF BIOLOGICAL MEDICINAL PRODUCTS FOR HUMAN USE人用生物药品的生产 (79)SCOPE (79)PRINCIPLE (79)PERSONNEL (80)PREMISES AND EQUIPMENT (81)ANIMAL QUARTERS AND CARE (82)DOCUMENTATION (82)PRODUCTION (83)QUALITY CONTROL (84)ANNEX 3 MANUFACTURE OF RADIOPHARMACEUTICALS 放射性药品的生产 (85)PRINCIPLE (85)PERSONNEL (85)PREMISES AND EQUIPMENT (85)PRODUCTION (86)QUALITY CONTROL (86)DISTRIBUTION AND RECALLS (86)ANNEX 4 MANUFACTURE OF VETERINARY MEDICINAL PRODUCTS OTHER THAN IMMUNOLOGICALS MANUFACTURE OF PREMIXES FOR MEDICATED FEEDING STUFFS 除为预混合加药饲料原料生产的免疫产品以外的,兽药产品的生产 (87)THE MANUFACTURE OF ECTOPARASITICIDES (88)THE MANUFACTURE OF VETERINARY MEDICINAL PRODUCTS CONTAINING PENICILLINS (88)RETENTION OF SAMPLES (point 1.4. viii and point 6.14.) (88)STERILE VETERINARY MEDICINAL PRODUCTS (88)ANNEX 5 MANUFACTURE OF IMMUNOLOGICAL VETERINARY MEDICAL PRODUCTS免疫兽药产品的生产 (89)PRINCIPLE (89)PERSONNEL (89)PREMISES (90)EQUIPMENT (93)ANIMALS AND ANIMAL HOUSES (94)DISINFECTION - WASTE DISPOSAL (94)PRODUCTION (95)STARTING MA TERIALS (95)QUALITY CONTROL (98)ANNEX 6 MANUFACTURE OF MEDICINAL GASES药用气体的生产 (99)1. PRINCIPLE (99)2. PERSONNEL (99)3. PREMISES AND EQUIPMENT (99)4. DOCUMENTA TION (100)5. PRODUCTION (101)6. QUALITY CONTROL (104)7. STORAGE AND RELEASE (105)ANNEX 7 MANUFACTURE OF HERBAL MEDICINAL PRODUCTS草药产品的生产 (108)PRINCIPLE (108)PREMISES (108)DOCUMENTATION (108)SAMPLING (109)QUALITY CONTROL (110)ANNEX 8 SAMPLING OF STARTING AND PACKAGING MA TERIALS起始物料和包装材料的取样 (111)PRINCIPLE (111)PERSONNEL (111)STARTING MA TERIALS (111)PACKAGING MATERIAL (112)ANNEX 9 MANUFACTURE OF LIQUIDS, CREAMS AND OINTMENTS流体,霜体和膏体药品的生产 (113)PRINCIPLE (113)PRODUCTION (113)ANNEX 10 MANUFACTURE OF PRESSURISED METERED DOSE AEROSOL PREPARATIONS FOR INHALATION吸入式剂量仪的气雾剂的生产 (115)PRINCIPLE (115)GENERAL (115)PREMISES AND EQUIPMENT (115)PRODUCTION AND QUALITY CONTROL (116)ANNEX 11 COMPUTERISED SYSTEMS 计算机化系统 (117)PRINCIPLE (117)PERSONNEL (117)V ALIDATION (117)ANNEX 12 USE OF IONISING RADIATION IN THE MANUFACTURE OF MEDICINAL PRODUCTS使用离子放射生产药品 (120)INTRODUCTION (120)RESPONSIBILITIES (120)DOSIMETRY (121)V ALIDATION OF THE PROCESS (121)COMMISSIONING OF THE PLANT (122)PREMISES (124)PROCESSING (124)DOCUMENTATION (126)MICROBIOLOGICAL MONITORING (126)ANNEX 13 MANUFACTURE OF INVESTIGA TIONAL MEDICINAL PRODUCTS观察期药品的生产 (127)PRINCIPLE (127)GLOSSARY (128)QUALITY MANAGEMENT (130)PERSONNEL (130)PREMISES AND EQUIPMENT (130)DOCUMENT A TION (131)PRODUCTION (132)QUALITY CONTROL (136)RELEASE OF BATCHES (137)SHIPPING (139)COMPLAINTS (139)RECALLS AND RETURNS (139)DESTRUCTION (140)ANNEX 14 MANUFACTURE OF PRODUCTS DERIVED FROM HUMAN BLOOD OR HUMAN PLASMA生产自人类血液或人体组织分离的产品 (143)PRINCIPLE (143)GLOSSARY (144)QUALITY MANAGEMENT (144)PREMISES AND EQUIPMENT (145)BLOOD AND PLASMA COLLECTION (145)TRACEABILITY AND POST COLLECTION MEASURES (146)PRODUCTION AND QUALITY CONTROL (147)RETENTION OF SAMPLES (148)DISPOSAL OF REJECTED BLOOD, PLASMA OR INTERMEDIATES (148)ANNEX 15 QUALIFICATION AND V ALIDATION 确认和验证 (149)PRINCIPLE (149)PLANNING FOR V ALIDATION (149)DOCUMENTATION (150)QUALIFICATION (150)PROCESS V ALIDATION (151)CLEANING VALIDATION (153)CHANGE CONTROL (154)REV ALIDATION (154)GLOSSARY (154)[ANNEX 16] [QUALIFIED PERSON AND BA TCH RELEASE]*经授权的人员和批放行 (157)ANNEX 17 PARAMETRIC RELEASE参数放行 (158)1. PRINCIPLE (158)2. PARAMETRIC RELEASE (158)3. PARAMETRIC RELEASE FOR STERILE PRODUCTS (158)4. GLOSSARY (160)[ANNEX 18] [GMP GUIDE FOR ACTIVE PHARMACEUTICAL INGREDIENTS] 17原料药GMP 指南 (161)GLOSSARY术语表 (162)GUIDE TO GOOD MANUFACTURING PRACTICE FOR MEDICINAL PRODUCTS药品GMP指南INTRODUCTION介绍为进一步消除药品贸易壁垒,促进许可证的一致性,以及确保整个欧洲在研发,生产和控制药品中保持高标准的质量保证,根据药品检查协会(PIC)同意,药品检查使用一致的GMP原则,和药品检查合作计划表中的欧洲药品GMP及其附录。
国外GMP检查详细条款1. 引言国外GMP(Good Manufacturing Practice)是一种旨在确保制药企业生产的药品符合质量标准和安全性要求的制度。
在国际贸易中,许多国家和地区都要求进口的药品符合其GMP要求。
因此,制药企业为了顺利出口产品,必须进行严格的GMP检查。
本文将详细介绍国外GMP检查的主要条款和要求,并提供一些实用的建议,以帮助企业提升其GMP水平,达到国际标准。
2. GMP检查的目的与范围国外GMP检查的目的是确保制药企业符合以下要求:•药品的质量、安全性和有效性已得到充分保证;•制药过程已被正确记录和验证;•生产环境卫生标准得到维护和控制;•物料和成品的储存和配送符合相关标准;•物料和成品的质量控制得到有效实施。
GMP检查范围包括制造过程、设备设施、人员培训、记录管理、环境卫生、质量控制和文件审核等方面。
3. GMP检查的主要条款和要求3.1 制造过程•制造过程的每个步骤都必须被准确、完整地记录下来;•所有原材料和中间产品必须经过有效的标识和追溯;•所有生产车间必须设立适当的控制措施,确保生产过程的稳定性和一致性;•根据标准操作程序(SOP),对制造过程进行管理和监控;•对制造过程中出现的问题和偏差必须进行记录、调查和纠正。
3.2 设备设施•生产设备必须经过校准、验证和维护;•设备的保养记录必须完备;•设备的应急修理计划必须制定和执行;•设备有必要的清洁和灭菌程序。
3.3 人员培训•所有从事制药工作的人员必须接受适当的培训;•培训内容必须包括GMP要求、卫生要求、操作规程以及紧急情况处理等;•培训记录必须保存并随时提供给检查机构。
3.4 记录管理•所有GMP相关的记录必须保存并随时提供给检查机构;•记录必须真实、准确且易于读取,任何修改必须有明确的记录和理由;•所有记录必须及时归档并防止损坏或丢失。
3.5 环境卫生•生产车间必须处于良好的卫生状态;•有必要的清洁程序和控制措施;•控制空气、水、压力和温度等环境参数。
美国GMP中⽂稿(CGMP)GOOD MANUFACTURE PRACTICE 美国药品⽣产质量管理规范CGMP⼆三年⼗⼆⽉⽬录210.1 cGMP法规的地位 2 210.2 cGMP法规的适⽤性 2 210.3 定义 2 211-A- 总则 4 211-B- 组织与⼈员 4 211-C- ⼚房和设施 5 211-D- 设备7 211-E- 成份药品容器和密封件的控制8 211-F- ⽣产和加⼯控制10 211-G- 包装和标签控制11 211-H- 贮存和销售13 211-I- 实验室控制14 211-J- 记录和报告16 211-K- 退回的药品和回收处理20210部分⼈⽤及兽⽤药品的⽣产加⼯包装或贮存的CGMP210.1 cGMP法规的地位(a) 在本部分及21CFR 211226部分中陈述的法规是在药品⽣产加⼯包装或贮存中使⽤的现⾏⽣产质量管理规范及使⽤的设施或控制的最低标准以保证该药品符合联邦⾷品药品及化妆品法对安全性的要求具有均⼀性和效价(或含量)并符合或代表其⽣产过程的质量及纯度等特征(b) 凡是在药品⽣产加⼯包装或贮存过程中存在任何不符合本部分及21CFR 211226部分中陈述的法规的药品依据联邦⾷品药品及化妆品法501 (a)(2)-(B)该药应被视为劣药同时导致该事故发⽣的负责⼈应受相应的法规的制裁210.2 cGMP法规的适⽤性(a) 本部分及21CFR 211226适⽤于普通药品21CFR 600680适⽤于⼈⽤⽣物制品除⾮另有明确规定否则上述两者之间应该是相互补充⽽不是相互取代如有上述两部分的法规不适⽤的药品则可⽤特定的具体法规来替代210.3 定义(a) 在联邦⾷品药品及化妆品法201部分中包含的定义和解释说明适⽤于21CFR 211 226部分中的术语(b) 下⾯定义的术语适⽤于本部分及21CFR 211226(1) 法(Act)指联邦⾷品药品及化妆品法修订版(21 U.S.C 301 et seq.)(2) 批(Batch)指在规定限度内按照某⼀⽣产指令在同⼀⽣产周期内⽣产出来的具有同⼀性质和质量的⼀定数量的药品或其它物料(3) 组分(Component)指⽤于药品⽣产的所有成份包括那些未在药品中出现的成份(4) 药品(Drug Product)指成品制剂(如⽚剂胶囊剂⼝服液等)通常含有⼀种活性成份并伴有⾮活性成份(但不是必需的)本术语也包括不含有活性成份但作为安慰剂使⽤的成品制剂(5) 纤维(Fiber)指长度⼤于其宽度的3倍的任何微粒状污染物(6) ⽆纤维脱落的过滤器(Non-fiber-releasing filter)指任何经过适当的预处理(如清洗或冲洗)后不会将纤维脱落到已过滤的组分或药品中的所有过滤器所有含⽯棉过滤器均被认为是有纤维脱落的过滤器(7) 活性成份(Active Ingredient)是指所有⽤于保证药物活性或其他在疾病的诊断治愈缓解治疗或预防中起直接作⽤或影响⼈或其他动物⾝体结构或功能的组分本术语包括那些能承受药品⽣产中的化学变化和为了保证其指定的活性或作⽤以⼀种经调整的形式存在于药品中的组分(8) ⾮活性成份(Inactive ingredient)指不同于活性成份的其他组分(9) 中间产品(In-process material)是指所有经制备复合混合或由化学反应得到的⽤于药品⽣产或制备的物料(10)批lot指⼀批或是⼀批中特定的均⼀部分在指定的范围内具有相同的性质和质量或者若为由连续的⽣产过程制造出的药品批指在单位时间或单位数量⽣产出的特定的均⼀的部分并且确保该部分在指定的范围内具有均⼀性质与质量(11) 批号(Lot number, control number batch number)指由字母数字符号或他们的组合组成由此可确定某批药品或物料的⽣产加⼯包装贮存或销售的情况(12) 药品的⽣产加⼯包装或贮存(Manufacture, processing, packing, or holding of adrug product)包括药品的包装和标签操作检验质量控制(13) 药⽤物料(medicated feed)指在21CFR 558.3中定义的B型和C型药⽤物料该物料含有联邦⾷品药品及化妆品法201(g)部分中定义的⼀种或⼀种以上的药物药⽤物料的⽣产应符合21CFR 226部分中的要求(14) 药⽤预混合料(medicated premix)指21CFR 558.3中定义的A型药⽤物质该预混合料含有联邦⾷品药品及化妆品法201(g)部分中定义的⼀种或⼀种以上的药物药⽤预混合料⽣产应符合21CFR 226部分中的要求(15) 质量控制部门(Quality control unit)指由企业任命负责质量控制相关责任的任何⼈员或组织机构(16) 含量或效价Strength指() 原料药的浓度(如以重量/重量重量/体积单位剂量/体积为基础)和/(或) () 活性(效价)也即由适当的实验室检测或由⾜够的临床数据得出的指定的药品治疗活性(如可表达为对照于某标准的单位的术语)(17) 理论产量(Theoretical yield)指在⽣产加⼯或包装某种药品的任⼀适当阶段中并且基于所使⽤的组分的数量在实际⽣产中⽆任何损失或错误的情况下应能⽣产的数量(18) 实际产量(Actual yield)指某种药品在⽣产加⼯包装的任⼀适当的阶段实际⽣产出的数量(19) ⽐率(Percentage of theoretical yield)实际产量(⽣产加⼯或包装某种药品的适当阶段)与理论产量(在相同阶段)的⽐率以百分数表⽰(20)验收标准(Acceptance criteria)建⽴在相应的取样⽅法基础上的药品的质量检验标准和合格不合格标准(如合格质量⽔平和不合格的质量⽔平)是决定批准或拒收⼀批(或其他⽣产单元的⼩组)药品的必需因素(21) 代表性样品(Representative sample)指⼀个样品按合理的标准抽取如随机取样法并包含若⼲单位元以能保证样品准确描绘被取样品的物料A总则211·1范围a 本部分的条例包含⼈⽤或兽⽤药品制备的现⾏最低限度的药品⽣产质量管理规范GMPb 在本章⾥的这些针对药品的现⾏GMP条例和本章600⾄800的所有部分针对⼈⽤⽣物制品的现⾏GMP条例除⾮明确另有说明者外应认为是对本部分条例的补充⽽是不代替本章其他部分或本章600⾄680各部分和本部分均可适⽤的条例前部分的条例可代替本部分条例c 在考虑经提议的发表在1978年9⽉29⽇联邦注册表FR上⼀项免除时若产品及其所有成份是以⼈⽤物品形式作⼀般销售和消费且这些产品根据其预期⽤途亦可列⼊药品的范围内则不应对这些⾮处⽅药OTC实施本部分条例直⾄进⼀步的通知为⽌本章110部分和113⾄119部分的条例⽤于鉴别这些变是⾷品的OTC药品是否按照GMP的要求⽣产加⼯包装和贮存211·3定义本章210·3中的定义适⽤于本部分B组织与⼈员211·22质量控制部门的职责a 本部门有批准和拒收所有成份药品包装容器密封件中间体包装材料标签及药品的职责与权⼒复查⽣产记录和权⼒保证不产⽣差错或若发⽣差错保证他们充分调查这差错本部门负责根据合同批准或拒收由其它公司⽣产加⼯包装或贮存的药品b 适当的实验室检验设备批准或拒收各种成份药品容器密封件包装材料及药品质量控制部门是可以获得的c 本部门有批准或驳回影响药品的均⼀性效价或含量质量及纯度的所有程序或规格标准的职责d 适⽤于本部门的职责与程序应成⽂字材料并应遵循211·25⼈员资格a 每位从事药品⽣产加⼯包装或仓贮⼯作⼈员应接受培训教育及有实践经验完成委派的各项职务培训是按照现⾏GMP包括本章中的现⾏GMP条例和这些条例要求的成⽂程序中涉及雇员的内容邀请合格⼈员指导并连续多次培训保证雇员熟悉现⾏GMP对他们的要求b 负责监督药品的⽣产加⼯包装或仓贮⼯作的每⼀个⼯作⼈员应受教育培训及有经验完成委派的各项职务以此作为提供药品具有安全性均⼀性效价或含量质量及纯度的保证c 有⾜够量招待和监督每种药品的⽣产加⼯包装或仓贮的合格⼈员211·28⼈员职责a 从事药品⽣产加⼯包装或仓贮的⼈员应穿着适合于其履⾏职责的清洁⾐服按需要头部脸部⼿部臂部另外罩防⽌药物受污染b ⼈员保持良好的个⼈卫⽣和健康c 未经监督⼈员允许其他⼈员不能进⼊限制进⼊的建筑物和设施d 任何⼈在任何时间明显地表现出现有影响药品安全性和质量的疾病或开放性`损伤应避免接触各种成份药品容器包装设备密封件中间体直⾄监督⼈员结对药品有不利影响的健康情况211·34顾问为了对问题提出意见聘请顾问顾问应对药品⽣产加⼯包装或仓贮提出建议他们受过⾜够的教育培训且有丰富的实践经验保留他们的姓名地址任何的顾问资格及服务形式等履历资料C⼚房和设施211·42设计与建造特征a 任何⽤于某类药品⽣产加⼯包装或贮存的⼚房或建筑群⼤⼩适宜结构与位置使其易于清洁保养适合操作b 建筑物有⾜够空间来有条理地安装设备和放置材料避免不同类的成份药品容器密封件标签中间体或药品等相互混放防⽌污染通过⼚房的上述物料其流向在设计时要防⽌污染c 操作应在明确规定的⼤⼩适中的地区内进⾏这些地区内进⾏这些地区按规定各⾃分隔开以防⽌污染下列操作须在单独的地区内进⾏1 发放给⽣产或包装前质量控制部门取样期间成份药品容器密封件及标签的签收鉴别贮存及拒收2 在处理前拒收的成份药品容器密封件及标签的贮存3 已发放的成份药品容器密封件及标签的贮存4 中间体的贮存5 ⽣产与加⼯操作6 包装和贴标签操作7 药品发放前的隔离贮存8 发放后药品的贮存9 控制室与实验室操作10⽆菌操作及有关操作地板墙壁和天花板平滑坚硬表⾯易清洁温度与湿度控制空⽓经⾼效过滤器在正压下过滤层流或⾮层流均可环境监测系统创造⽆菌环境房间和设备清洁消毒系统控制⽆菌环境的设备维修系统d青霉素⽣产加⼯及包装设备与⽣产其他⼈⽤药品的设备分开211·44照明所有地区均须提供充⾜的照明211·46通风空⽓过滤空⽓加热与冷却a 提供⾜够的通风b 提供⾜够能控制空⽓正压微⽣物尘⼟温度和湿度的设备适应药品⽣产加⼯和贮存需要c 空⽓过滤系统包括预过滤器和微粒物质空⽓过滤器空⽓经过滤才送⾄⽣产区如果空⽓是再循环到⽣产区应测量尘埃含量控制从⽣产区带来的尘埃在⽣产区⽣产中发⽣空⽓污染应以排⽓系统或其他系统充分抽出空⽓控制污染d 青霉素⽣产加⼯和包装的空⽓输送系统应与其他⼈⽤药品的空⽓输送系统完全分开211·48管件a 在持续正压下应对药品⽆污染的管道系统内供应饮⽤⽔饮⽤⽔应符合环境保护机构制订的基本饮⽤⽔条例标准40CFR141部分不符合该标准的⽔不许进⼊⽔系统b 排⽔设备应有⾜够的⼤⼩可直接连接排⽔管及安装防⽌虹吸倒流的空⽓破坏设备或其他机械设备43FR450771978年9⽉29⽇修正于48FR114261983年3⽉18⽇211·50污⽔和废料来⾃⽔⼚和附近建筑物的污⽔垃圾及其他废料⽤安全卫⽣的⽅法处理211·52洗涤和盥洗设备提供洗涤和盥洗设备包括热冷⽔肥皂清洁剂空⽓⼲燥器或专⽤⽑⼱及进⼊厕所的清洁设备211·56a 所有⽤作药品⽣产加⼯包装及贮存的三房应保持清洁卫⽣的环境且不受啮齿动物鸟类及其他害⾍侵害扰实验动物除外垃圾和有机废料定时以卫⽣的⽅法控制处理b 填写分配卫⽣清洁任务的详细的清洁项⽬⽅法设备⽤于清洁⼚房和设施的材料的⼀览表c 填写适⽤的杀⿏剂杀昆⾍剂杀真菌剂熏蒸剂去垢剂和消毒剂⼀览表防⽌这些物品对设备成份药品容器密封件包装材料标签或药品污染除依据联邦杀⾍剂杀真菌剂及杀⿏剂法规7U.S.C135已登记和使⽤的品种外其他的不⽤211·58保养任何⽤于药品⽣产加⼯包装或贮存的⼚保持良好状态D设备211·63设备的设计尺⼨及位置药品⽣产加⼯包装或贮存设备设计合理⼤⼩适当布置合理便于操作清洁和保养211·65设备制造a 设备表⾯与各种成⼈中间体或药品接触不产⽣化学反应和作⽤保证药品的安全性均⼀性效价或含量质量或纯度改变b 操作所需之物质如滂沱剂冷却剂等不能进⼊设备⾥与成⼈药品容器封⼝物品中间体或药品接触保证药品的安全性均⼀性效价或含量质量或纯度不变211·67设备清洁与保养a 相隔⼀定时间对设备与⼯具进⾏清洁保养和消毒防⽌出故障与污染影响药品的安全性均⼀性效价或含量质量或纯度b 制订药品⽣产加⼯包装或贮存设备包括⽤具的清洁和保养⽂字程序并执⾏这些程序包括但不⼀定限于以下内容1 分配清洁保养任务2 保养和清洁细⽬⼀览表3 详细说明⽤于清洁和保养的设备物品和⽅法拆卸和装配设备的⽅法必须保证适合清洁和保养的要求4 除去或擦去前批遗留物的鉴定5 已清除了污染的清洁设备的保护6 使⽤前检查清洁的设备7 保留保养清洁消毒的记录按211·180及211·182的说明检查211·68⾃动化设备机械化设备和电⼦设备a ⽤于药品⽣产加⼯包装和贮存的⾃动化机械化或电⼦包括计算机或其它类型的设备按惯例对其设计之成⽂条款作标定检查或核对保证其⼯作性能良好保留检查标定核对等⽂字记录b 对保障重要⽣产变化的计算机或有关系统进⾏操作培训操作记录或其他记录只能由被认可的⼈员制订向计算机或有关系统输⼊或从中输出的各种⽅案其他记录或资料应核查其准确性输⼊计算机或关系统内的档案资料除与实验室共同分析计算的结果可消除外其他的应保留⽂字记录与相应的证明资料⼀起保存事先设计好的硬件复制品或多各选择系统台复印件磁带或微型胶卷等保证其⽀持资料正确可靠及完整出现资料改动⾮⼈为消除或遗失时应维修211·72过滤器⽤于⽣产加⼯的液体过滤器或⼈⽤注射药品的包装材料不许释放出纤维的进⼊产品除⾮不得以不在⽣产加⼯中使⽤释放纤维的过滤器或注射药品的包装材料若必须使⽤⼀种能释放纤维素的过滤器最后应使⽤⼀⾮释放纷纷物平均最⼤孔径为0.22µm(如实际⽣产条件限制可⽤0.45µm)的附加过滤器过滤降低注射剂内微粒量使⽤含⽯板的过滤器最后⽤或不⽤特殊⾮释放纤维过滤器均可以但要根据FDA有关部门提供的该⾮释放纤维过滤器会或可能损害注射剂的安全性和有效性的证据⽽定E成分药品容器和密封件控制211·80总要求a 有⽂字详细说明成份药品容器密封件的签收鉴定贮存装运取样检验和批准或拒收程序并遵循b 成份药品容器和密封件应专⼈管理和在防⽌污染的环境下贮存c 药品容器的包装袋或包装箱或密封件应离地⾯放置保持适当间隔全球清洁和检查d ⽤明显的已接收的每装货量中的批号代码对成分药品容器或密封件加以鉴别此代码⽤于记录每批货的放置地⽅对每批货的情况如隔离批准或拒收等作检查211·82未检验的成份药品容器和密封件的接收与贮存a 接收时和验收前对每个或编组的成份容器药品容器和密封件进⾏⽬检给内容物容器损坏或拆封和污染等情况作适当的标志b 成份药品容器各密封件应隔离贮存直⾄经检验为⽌合格可发放在符合211·80要求的地区中贮存211·84成份药品容器和封⼝物品的试验批准或拒收a 每批成份药品容器和封⼝物品在未经质量部门取样检查合格前不准使⽤检验合格后发放使⽤b 收集每批的每⼀装货量的代表性样品供检验⽤容数⽬和每⼀容器⾥物质的取样量是有适当的标准的例如成份的变异性统计学标准可信限要求的精密度供应商过去的质量历史21·170要求分析和留样所需的数量等c 收集样品程序1 ⽤适当的⽅法清洁选出成份容器2 打开容器取样重新封⼝防⽌其内容物受污染和其他成分药品容器或密封件的污染3 必要时使⽤灭菌设备和⽆菌取样技术4 如果需要从容器顶部中部和底部的成分中取样样品须混合5 鉴定样品容器⽬的是确定如下资料被取样的材料名称批号被取样的容器取样⽇期及样品收集⼈的名字等6 已取样的容器应作标志表⽰样品已取出d 样品检验程序1 ⼀个药品的每个成分最少做⼀个特性试验如有专⼀特性实验就应采⽤2 依照所有成⽂的规格标准检验每个成份的纯度含量和质量⽣产⼚家代替上述试验规定⽣产⼚家最少要做个成份特别试验可承认这些成分的供应者扫提供的分析报告规定隔⼀定时间⽣产⼚家定期验证供应午的试验结果证明供应者的分析结果是正确的3 依照成⽂规程检验容器和密封件⽣产⼚家代替上友谊赛试验规定⽣产⼚家对这些容器或封⼝物品最少做⼀次⽬检可承认供应者的检验证书规定⽣产⼚家定期验证供应者的试验结果证明其试验结果是正确的4 必要时⽤显微镜检测成分5 每批易受污物昆⾍或其他外来杂物污染的某⼀成份药品容器或密封件鉴于其预期⽤途在使⽤前应做微⽣物试验e任何批号的成份药品容器或密封件若符合已成⽂的均⼀性效价或含量质量纯度等的规格标准和本部分d的有关试验可批准使⽤任何批号的上述材料不符合这些规格应拒收211·86获准作⽤的成份药品容器和密封件先⼊库者先⽤若产⽣的偏差是暂时的和适当这种偏差是容许的211·87获准的成份药品容器和密封件的复检经质量控制部门批准或拒收的成份药品容器密封件若长期贮存或曝露在空⽓热或其他可能对其产⽣不良影响的环境后应依照211·84对均⼀性效价或含量质量纯度等复检211·89拒收的成份药品容器和封⼝物品拒收的成份药品容器和封⼝物品应经鉴定和在隔离系统下加以控制防⽌在⽣产和加⼯使⽤211·94药品密封容器和密封件a 药品包装容器和密封件应不起反应不吸着不吸附不致改变药品的安全性均⼀性含量或效价质量和纯度⽽超出制定的或其它颁布的规定要求b 容器封⼝系统应对贮藏和使⽤过程中可预见的能引起药品变质或污染的外部因素提供⾜够的防护c 药品容器和密封件应清洁灭菌和除热原保证其适⽤于预期⽬的d 药品容器和密封件的标准或规格检验⽅法指清洁和消毒⽅法除热原过程应成⽂并遵循F .⽣产和加⼯控制211·100成⽂的规程偏差a 编写为保证药品的均⼀性含量或效价质量及纯度⽽设计的⽣产和加⼯控制程序这些程序包括本部内全部要求这些成⽂程序包括变化须经有关部门起草复查和批准然后再经质量控制部门复查与批准b 在实施各种⽣产和加⼯控制功能中遵循已制定的⽣产和加⼯控制程序并在招待时以⽂件加以证明程序中出现的任何偏差应作记录并提出证据211·101成分的进料成⽂的⽣产和控制程序包括下⾯的内容其设计应保证所⽣产的药品具有核武器原有的均⼀性含量和效价质量和纯度a 按处⽅配制的药品保证其活性成份含量不低于100%标⽰量或规定量b ⽣产药品⽤的成份应称量测量或适当粉碎若⼀种成份从原来容器转移到另⼀容器内⽤下列资料以鉴别(1) 成份名称或项⽬代码(2) 接收或控制号(3) 在新容器中的重量或份量(4) 使⽤此成分2配制的⼀批药品包含其产品名称含量和批号c成份的称重测量或粉碎操作应受到严密的监督所盛成份已⽤于⽣产的每⼀容器须经第⼆⼈检查保证1 此成份是由质量控制⼈员发放的2 重量或份量正确批⽣产记录⼀致3 容器经严格鉴别d每⼀成份投料时⼀⼈操作另⼀⼈核对211·103 产量计算在药品⽣产加⼯或贮存的每⼀适当阶段结束时测算实际产量与理论产量的百分⽐211·105设备鉴别a 在整个⽣产周期内同批药品⽣产使⽤的全部混合和贮存容器⽣产线和主要设备应严格识别标⽰出药品的成份需要时不须标出所处的加⼯阶段b ⼀种药品每批⽣产使⽤的主要设备以⼀鉴别性识别号或代号加以识别此鉴别号或代号记录在该批号产品的记录本若⽣产中只使⽤⼀种特殊型号的设备可⽤该设备名字代替鉴别性识别或代号211·110中间体和药品的取样与检验a 制订和遵循说明每批的加⼯过程控制及对加⼯过程中材料的适当样品实⾏检验或检查的成⽂程序保证药品的⼀致性和完整性上述控制程序包括但不限于如下内容1 ⽚剂或胶囊的重量变化2 崩解时间3 充分混和保证均匀4 溶解时间和溶解速率5 溶液的澄明度溶解完全性及PH值b 考虑上述特性⽽制定的有效中间加⼯规格与药品最终规格⼀致此中间加⼯规格应在以前可靠的加⼯⽅法稳定性评估和经应⽤统计学程序断定认为合适的基础上制定的样品测试保证药品和中间体符合规格标准c 在⽣产加⼯期间如在重要阶段的开始由质量控制部门审定决定联取舍d 不合格的中间体在隔离系统下鉴别及控制防⽌其在征税或加⼯操作中使⽤211·111⽣产时间限制在适当时候制定完成每⼀⽣产阶段的时间限制保证药品质量制定的时间限制产⽣偏差如这些偏差不损害药品质量是可以接受的这些偏差应有⽂字⽂件证明是正当的211·113微⽣物污染的控制a 制订和遵循预防不需消毒药品有害微⽣物的适当程序b 制订和遵循预防已消毒药品微⽣物污染的适当程序这些程序包括所有消毒过程的验证211·115返⼯a 制订和遵循指导⼈合格批号返⼯及保证返⼯批号达标的程序b 没有质量控制部门复检与批准不许进⾏返⼯G.包装和标签控制211·122材料的检查和使⽤标准a 制订详细标签和包装材料的接收鉴别贮存半年取样检验的程序并遵循这些成⽂程序在接收⽤于药品包装和贴标签前有代表性地对其取样与检验b 符合成⽂规格标准的标签和包装材料可批准发放使⽤不符合规格者不得⽤于⽣产c 接收每批不同标签和包装材料⽆须签收测试⽆论是接收或拒收须保留其记录d ⽤于不同药品含量剂型及成份数量的标签和标⽰材料分别贮存并持上适当牌证只限经核准⼈员接近贮存地区e 作废和陈旧的标签标⽰材料及其他包装材料应销毁f 排字印刷在不同药品或同⼀药品不同规格的品种上`使⽤排字印刷考虑在印刷期间和印刷后印刷品的设置切裁和管理等应制订包装和标签⼯作专门控制程序g 在药品印标签的⽣产线其上的或与其有关的印刷设备应受到临近保证所有印痕与本批产品记录中说明的印痕⼀致211·125标签的发放a 严格控制已发放的⽤于药品的标签b 已发放的⼀批标签材料须认真检查其⽆⼀性应与⼀批或单批⽣产记录中说明的标签⼀致c 核对发放的已使⽤的及回收的标签若发现成品数量与发出的标签数量不符差额超出根据历史⽔平先前定下的数量范围则需对这些偏差作出评估按照211·192要求调查原因d 超出有关批号或控制号标签全部应销毁e 回收的标签如保留应加上证明标志贮存防⽌混淆f 制订发放标签的详细控制程序并遵循211·130包装和标签操作设计保证标签标⽰及包装材料正确⽤于药品的程序并遵循这些程序结合下列a 预防混合和由物理的或其他操作空间物质引起的交叉b 带批号或控制呈药品的鉴别检查该药品的制造和控制历史c 包装⼯作开展前检查包装和标签材料的适⽤性和正确性且这些检验所提供的证明⽂件应符合批⽣产记录d 使⽤前⽴即检查包装和贴标签设备保证所有药品离开先前的操作同时移开不适⽤于随后操作的包装材料检查结果以批⽣产记录形式提供证明⽂件211·132⼈⽤百处⽅药OTC保险包装的要求a ⼀般来说在联邦⾷品药物和化妆品法规下FDA有权制定⾮处⽅药保险包装的统⼀国家要求提⾼⾮处⽅药包装的可靠性和有助保证⾮⾃主药的安全与效果⼀种零售OTC药品⽪肤科药⽛粉胰岛素喉⽚除外没有包装在保险包装内或或没有适当的标签根据联邦法规501部分属掺假药根据502部分或两者飞⾏属错贴标签b 保险包装每个⽣产者和包装者应将零售OTC药品装⼊保险包装内若此药易受公众影响该药应在内保持⾄售出。
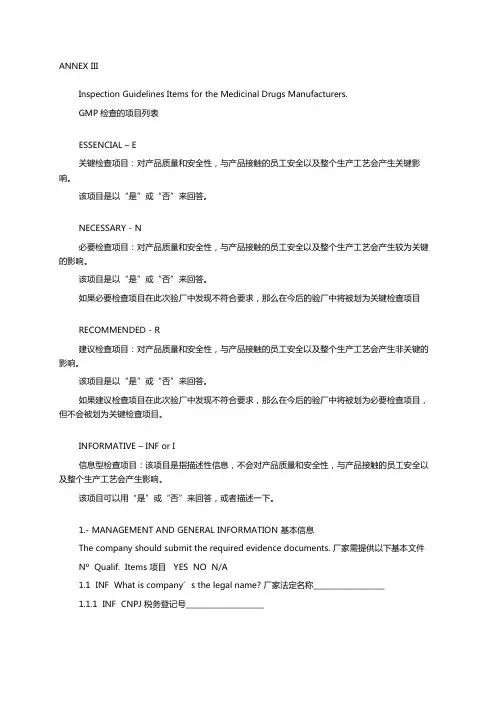
ANNEX IIIInspection Guidelines Items for the Medicinal Drugs Manufacturers.GMP检查的项目列表ESSENCIAL – E关键检查项目:对产品质量和安全性,与产品接触的员工安全以及整个生产工艺会产生关键影响。
该项目是以“是”或“否”来回答。
NECESSARY - N必要检查项目:对产品质量和安全性,与产品接触的员工安全以及整个生产工艺会产生较为关键的影响。
该项目是以“是”或“否”来回答。
如果必要检查项目在此次验厂中发现不符合要求,那么在今后的验厂中将被划为关键检查项目RECOMMENDED - R建议检查项目:对产品质量和安全性,与产品接触的员工安全以及整个生产工艺会产生非关键的影响。
该项目是以“是”或“否”来回答。
如果建议检查项目在此次验厂中发现不符合要求,那么在今后的验厂中将被划为必要检查项目,但不会被划为关键检查项目。
INFORMATIVE – INF or I信息型检查项目:该项目是指描述性信息,不会对产品质量和安全性,与产品接触的员工安全以及整个生产工艺会产生影响。
该项目可以用“是”或“否”来回答,或者描述一下。
1.- MANAGEMENT AND GENERAL INFORMATION 基本信息The company should submit the required evidence documents. 厂家需提供以下基本文件Nº Qualif. Items 项目 YES NO N/A1.1 INF What is company’s the legal name? 厂家法定名称___________________1.1.1 INF CNPJ 税务登记号_____________________1.1.2 INF Adress 地址: Street / Avenue: ____________________________________N0 _____________, Complement:__________________________Neighborhood:_____________________City:_____________________State:_________________ZIP Code:________________Telephone: ______________________Fax:_________________________________Email: _____________________________1.2 INF Inspection Period:验厂日期 ____/____/____ to ______/_____/_____1.2.1 INF Reason for inspection:验厂原因 ______________________________________1.3 INF Date of last inspection:上次验厂日期 ____/____/____1.3.1 INF Reason for last inspection: 上次验厂原因_______________________1.4 INF Does the company have a Good Manufacturing Practices (GMP) Certification? 公司有GMP证书吗1.4.1 INF Date of Certificate Issue 有的话,证书颁发日期____/___/___1.5 INF Name of the Responsible Technician: 技术负责人姓名____________1.6 E Is the responsible pharmacist presents?负责的药剂师在场吗1.7 E Is there an evidence of his/her certification by the proper agency?有没有相关部门发给过他相关证件?1.8 N Has the company presented an Organizational Chart?公司有没有出示组织机构图?1.9 I Does the company have an Operating Certificate granted by the proper Agency of the National Sanitary Surveillance Agency?公司有没有国家卫生监督局所颁发的运营证书?1.9.1 INF Number 证书号_______________________________________________1.9.2 INF Authorized Activities: 各工叙0 Storing 存储 0 Packaging包装 0 Distribution 销售 0 Exporting 出口0 Importing 进口0 Manufacture 加工 0 Production 生产 0 Transport 运输 0 Re-packaging 再包装0 Extraction 抽提0 Expedition发货 0 Fractioning 分馏 0 Synthesizing 合成 0 Transforming 转化 0 Purifying 纯化1.10 I Does the company have a Special Operating Certificate, granted by the proper Agency of the National Sanitary Surveillance Agency?公司有没有国家卫生监督局所颁发的特别的运营证书?1.10.1 INF Number: 有的话,编号_____________________1.10.2 INF Authorized Activities: 各工叙0 Storing 存储 0 Packaging包装 0 Distribution 销售 0 Exporting 出口0 Importing 进口0 Manufacture 加工 0 Production 生产 0 Transport 运输 0 Re-packaging 再包装0 Extraction 抽提0 Expedition发货 0 Fractioning 分馏 0 Synthesizing 合成 0 Transforming 转化 0 Purifying 纯化 0 Manipulating 操作1.11 I Are the records and inventories of substances subject to a special control conducted according to the Sanitary Laws in place? 根据卫生部的要求,物料的记录和存货清单是否有进行特定的管理?1.12 I Are the losses arising from the manufacture processes of products subject to special controls and properly recorded?产品生产过程中物料的损失是否经过特别控制,并被记录?1.13 I Does the company have an Operating License / Sanitary Authorization from the local Agency?公司有没有当地卫生部授权的生产执照1.13.1 INF Number:执照号 _______________________1.14 Does the company have an authorization from the proper Agencies related to:公司是否有相关部门颁发的下列相关授权/批准:1.14.1 N Environment Protection?环境保护?1.14.2 N Facilities safety (Fireman)? 设施安全(消防员)1.14.3 N Does the company responsible for transportation of raw materials and/or finished products have an operating authorization for such activities, from the proper Sanitary Agency?公司对原粉和/或制剂的运输是否有卫生部门授权/批准?1.15 N Was the building architectural plan presented?厂房建筑方案是否有出示?1.15.1 INF What is the total site area? 总面积 _______________ m21.15.2 INF What is the built area? 建筑面积_____________________m21.15.3 INF How many buildings are there in the plant? 厂里有几栋楼______________1.16 INF Is there a restaurant / cafeteria in the plant?厂里有食堂/自助餐厅吗1.17 N Is there an updated Occupational Health Plan properly signed by the responsible physician? 有没有更新的由负责医生所签字的职业健康计划1.18 N Was a list of proprietary products presented, for those products that are in the market and for the ones that are not?是否有一张已上市的和未上市的专利产品列列表1.18.1 E Are all such products properly registered at the proper National Sanitary Agency?是否所有产品都在当地卫生部有注册1.19 INF What is the company’s production installed capacity, per line / pharmaceutical form?(Attach documentation)公司每条生产线的设计产能(附上文件)1.20 R Was the updated floor plan, approved by the proper Sanitary Agency, presented?有没有卫生部门批准的更新的平面图?1.21 R Are the people and materials flows indicated in the floor plan, updated and approved by the proper Sanitary Agency?人流和物流是否标注在平面图中,并经相关卫生部门批准?1.22 INF Does the company contract third parties’ services fo r the production of their products?产品的生产是否有委托第三方?1.22.1 INF Which are the outsourced products and stages? 委托第三方生产的产品有哪些?进程如何?_____________________________________________________________________________________________________ __________________1.22.2 INF Which are the contracted companies? 委托那些第三方公司______________1.22.3 N Were the Outsourcing Agreements submitted to the evaluation by the proper Sanitary Agency?与委托公司(第三方)协议是否递交给卫生部进行评估?1.22.4 INF Does the company contract third partie s’ services for the production of products subject to special control?委托第三方进行的生产是否经过特殊控制?1.22.4.1 INF Which are the contracted companies? 与哪些公司订约________________1.23 INF Does the company contract third parties’ services for the analysis of raw materials and/or products?原粉及制剂的分析是否有委托第三方?1.23.1 INF Which are the contracted companies? _委托哪家公司?_______________1.23.2 N Which are the conducted assays?做的哪些分析__________________1.23.3 N Were the Outsourcing Agreements for analysis of raw material and/or products submitted to the evaluation by the proper Sanitary Agency?把原粉和制剂的分析委托给第三方的协议是否有递交给相关卫生部门,并由卫生部来评估?1.24 INF Does the company import any raw materials?公司有进口原材料吗?1.25 INF Does the company import any intermediate product?公司有进口中间产品吗?1.26 INF Does the company import any bulk product?公司有进口原液(原粉)吗?1.27 INF Does the company import any finished product?公司有进口制剂吗?1.28 R Has the company submitted the list of imported products (intermediate, bulk, finished products)? 公司有递交进口产品清单吗(包括中间产品,原液(原粉),制剂)1.29 INF Have the lines where imported products are manufactured already been granted a Certificate from the proper Sanitary Agency in Brazil? 进口产品的生产线是否得到巴西卫生部门的许可证1.29.1 N If the answer is NO, has the company already asked for the inspection by the proper Sanitary Agency in Brazil?如果没有,公司是否要求巴西卫生部门来检查?1.30 INF Does the company export finished products?公司出口成品制剂吗1.30.1 R Has the company submitted the list of exported finished products?公司有递交出口的制剂列表吗1.31 INF Is the company active in business related to industrialization of products having a different nature or purpose, subject to an Authorization from the proper Sanitary Agency? 公司从事特殊性质/目的的产品工业化,是否得到相关卫生部门许可/授权?1.31.1 INF Specify All Products. 列出这些所有产品_________________________1.32 N Has the company produced 03 (three) recorded pilot product batches, according to the applicable law? 根据相关法律规定,公司是否有3个批次试生产?1.32.1 INF Where are these batches?这些批号产品在哪里1.32.2 N Are there records?有记录吗2.- PREMISES 厂房设施2.1- Generalities 概述Nº Qualif. Items YES NO N/A2.1.1 INF Are there pollution or contamination sources near the company? 工厂附近有污染源吗2.1. 2 R Are the access ways paved?路有铺好吗2.1.3 N Are the areas surrounding the buildings clean?工厂大楼附近的区域洁净吗2.1.4 R As to the external appearance, do(es) the building present a good conservation state (absence of cracks, leaking, etc.)根据外观来看,工厂大楼是否完好无损(没有破裂,渗漏等等)2.1.5 N Are the effluents treated?废水有处理吗2.1.5.1 INF Which are the treatments? 怎么处理____________________________________________________2.1.5.2 N Are there records? 有处理的记录吗2.1.6 N Are the facilities built in a way to protect against entry of insects and other animals?工厂的建造能否防止昆虫以及别的动物的进入2.1.6.1 N Is there a program in place for prevention and control of insects and other animals?有防止和控制昆虫以及别的动物进入的措施吗?2.2. Ancillary Facilities 辅助设施Nº Qualif. Items YES NO N/A2.2.1 Dressing-Rooms and Bathrooms更衣室和浴室2.2.1.1 R Are there enough changing rooms?有足够多的更衣室吗2.2.1.1.1 N Are the hygiene conditions appropriate?更衣室有良好的卫生条件吗2.2.1.2 R Are there enough bathrooms?有足够多的浴室吗2.2.1.2.1 N Are the hygiene conditions appropriate and is there cold and/or hot water, soap and disposable towels or driers?浴室有良好的卫生条件吗,有冷水/热水,肥皂和一次性毛巾和烘干机吗2.2.1.2.2 N Is the access to the bathrooms independent from the production and storage areas?浴室通道是否与生产及仓储区分离开来?2.2.2 Maintenance / Facilities 维护/设施2.2.2.1 INF Are the maintenance areas physically separated from the production areas?维护区域有跟生产区域分开吗2.2.2.2 INF Is there a specific area for the steam generator equipment?蒸汽发生器有在特定区域呢?2.2.2.2.1 INF Is industrial steam produced? 有生产工业用的蒸汽吗2.2.2.2.2 INF Is pure steam produced?有生产纯蒸汽吗2.2.2.3 INF Is there a specific area for the air compressor? 空气压缩机有在特定区域吗2.2.2.4 INF Is there a specific area for the purified water producing equipment? 纯化水生产的设备是在特定区域吗2.2.2.5 INF Is there a specific area for injection water production equipment? 注射用水生产的设备是在特定区域吗2.2.2.6 INF Is there a specific area for air conditioning equipment? 空调系统的设备有没有在特定区域2.2.2.7 INF Is there a central container for the dust coming from the air exhausting system? 是否有集中收集来自排风系统灰尘的容器?2.2.2.8 N Is there a power generator, if required in an emergency?在紧急状况下,是否有电力发电机2.2.2.9 N Are the water, steam, gas, compressed air and electricity ducts properly labeled?水,蒸汽,气体,压缩空气以及electricity ducts是否有合适区分?2.2.3 Bioterium2.2.3.1 N Are the bioterium facilities independent from the other facilities? 细菌微生物设施与其他设施隔离开来吗2.2.3.2 N Are all the activities carried out in this area compliant with the previously defined Standard Operating Procedures (SOP)?在这里所进行的操作是否遵循SOP2.2.3.2.1 N Are there records for the critical operations defined in the relevant Standard Operating Procedures (SOP)? 是否记录SOP中规定的关键操作?2.2.3.3 N Are the hygienic conditions adequate?那里有合适的卫生条件吗2.2.3.4 N Are there exclusive bathrooms and changing rooms for the staff working with animals? 进行动物实验的员工是否有专门的浴室和更衣室2.2.3.4.1 N Are the hygienic conditions adequate?那里有合适的卫生条件吗2.2.3.5 INF What are the species of the animals? 哪些动物_____________________________________________________2.2.3.6 INF Is the animals’ origin known? 动物的来源知道吗2.2.3.7 INF Is the available area large enough to accommodate the various species utilized?动物实验室是否足够大可以住各种需要用的动物2.2.3.8 N Is the bioterium’s ventilation and/or air conditioning system independent from the other company’s facilities? 细菌微生物房的通风系统/空调系统与工厂其他设施隔开吗2.2.3.9 N Is the light sufficient? 光充足吗2.2.3.10 N Is there a quarantine area for animals? 动物有检疫区域吗2.2.3.11 N Is there a room for inoculated animals? 有动物接种室吗2.2.3.12 N Is there a room for disinfection and drying of boxes, cages, feeders and other required materials ?有对盒子,笼子,进食器和其他需要的材料进行来消毒干燥的房间吗2.2.3.13 N Is there an adequate place for material, food and beds storage for the animals?有没有一个合适的地方来对于动物所需的材料,食品和床进行存储2.2.3.14 N Does the Standard Operating Procedures (SOP) define the treatment to be given to animals dejects and corpses? SOP里有没有规定如何处理动物的废弃物尸体2.2.3.14.1 N Is there an adequate place to store animals dejects and corpses? 有没有足够的地方储存动物尸体?2.2.3.15 N Is there a capacitated professional, responsible for the bioterium? 是否有负责细菌微生物的专业人员?3.- STORAGE ROOM / MATERIALS AND PRODUCTS 仓储区/物料和成品3.1.- GeneralitiesNº Qualif. Items YES NO N/A3.1.1 N Are floors, walls and ceilings appropriate for the activities conducted in the area? 地面, 墙和天花板是否适合于对这块区域的操作3.1.1.1 N Are such items in good conservation state?以上这些地方都保持完好吗3.1.1.2 N Are they easy to clean? 容易清洁吗3.1.1.3 N Are they clean? 干净吗3.1.2 N Is there any protection against entry of rodents, insects, birds and other animals?这些地方有没有防止啮齿动物, 昆虫, 鸟和其他动物进入的措施呢3.1.2.1 N Is there a preventive system in place, related to such? 对以上动物有防护系统吗3.1.2.2 INF Who is the person responsible for carrying out such system?执行这一系统的负责人_______________________________3.1.2.3 INF Were there indications of the presence of rodents, insects, birds or other animals? 当啮齿动物, 昆虫, 鸟和其他动物出现时有指示吗3.1.4 R Is the light adequate? 光照充足吗3.1.5 INF Is it necessary to have humidity and temperature control in the store rooms? 在仓储区有必要对湿度和温度进行控制吗3.1.5.1 N In case it is necessary, are there humidity and temperature controlling devices? 如果有必要, 有湿度和温度控制仪吗3.1.5.2 N Are there records? 有温度和湿度记录吗3.1.6 N Are the temperature and humidity in accordance with the required parameters established for the stored materials and products?温度和湿度是否符合仓储区物料和产品的要求的参数3.1.6.1 N Should there be deviations related to the established parameters, was the cause investigated? 测量值与规定的参数会有偏差吗?起因调查了吗?3.1.6.2 N Are preventive and/or corrective actions taken in relation to the identified causes?有没有对已知的起因实施预防和整改3.1.6.3 N Are there records? 有相关记录吗3.1.7 INF Is a cold chamber necessary? 需要冷库吗3.1.7.1 I Is there a cold chamber? 有冷库吗3.1.7.1.1 N Is the temperature controlled? 冷库温度有控制吗3.1.7.1.2 N Are there temperature records? 有温度记录吗3.1.7.1.3 R Is there an alarm system in the cold chamber, to alert when a temperature deviation occurs? 当温度偏差发生时,冷库里有警报装置吗,3.1.7.1.4 INF What was the reading of the temperature at the time of inspection?验厂时冷库里温度读数多少 ___________ 0C3.2.- Specific ConditionsNº Qualif. Items YES NO N/A3.2.1 N Are all the activities conducted in this area compliant with the previously defined Standard Operating Procedures (SOP)? 在这个区域中所有操作都遵循之前定义的SOP吗3.2.1.1 N Are there records of critical operations defined in the relevant Standard Operating Procedures (SOP)?SOP中规定的关键操作有记录吗?3.2.2.1 N Are the protective suits clean and in good conditions? 防护服干净,完好吗3.2.3 N Are the scales/balances regularly inspected and calibrated? 天平或称有定期检查和校准吗3.2.3.1 INF How often are the scales/balances inspected? 天平或称多久查一次_____3.2.3.1.1 N Are there records? 有记录吗3.2.3.1.2 N Is the inspection conducted by means of standard weights, properly calibrated? 是根据标准砝码来校准的吗3.2.3.2 INF How often are the scales/balances calibrated? 天平或称多久校准一次_____3.2.4 N Is the storage organization rational and correct, aiming at preserving the integrity and identification of materials and products? 仓储结构是否合理,能够识别/区分存放的物料和产品?3.2.5 Is there an area / system limiting or restricting the use of materials/products, respecting the previously defined status for: 在以下定义的情况下, 有没有一个区域/系统来限制物料/产品的使用,3.2.5.1 N Quarantined? 检疫3.2.5.2 N Approved? 批准3.2.5.3 N Returned? 退回3.2.6 Are there areas / systems for keeping: 这些区域/系统用来放3.2.6.1 N Raw materials? 原材料3.2.6.2 N Packaging materials? 包材3.2.6.3 N Intermediate products? 中间产品3.2.6.4 N Bulk products? 原液(原粉)3.2.6.5 N Finished products? 制剂3.2.7 Is there a specific place, supplied with a safety device for keeping substances and products subject to special control, for: 有没有特定区域, 可以提供安全装置来存放需要特殊控制的物料/产品3.2.7.1 E Raw materials? 原材料3.2.7.2 E Intermediate products? 中间产品3.2.7.3 E Finished products? 制剂3.2.8 N Do the control and recording system for storage of intermediate products and bulk products include the maximum permitted storage period of time, before packing?在包装之前,对中间产品和原液(原粉)的控制和记录系统中是否有允许的最长储存期3.2.9 N Do the control and recording system for shipping observe the correspondent sequence relation for batches and expiry dates? 发货的管理以及记录系统是否按照相关批次及过期日期的顺序来进行的?3.2.10 N Are all stored materials and products within the validity term? 所有储存的物料和产品都有效期内吗3.2.11 N Is there a separate, safe and identified area for storage of expired products and/or material, while awaiting their final destination? 有没有一个单独的,安全的,识别的区域来存放过期产品和/或过期物料,在等待它们最终的结果时3.2.11.1 N Will such products and/or materials be destroyed later? 这样的产品和/或物料今后会被销毁吗3.2.12 N Is there a system for inventory control? 有物料管理系统吗3.2.12.1 INF Which system?_ 有哪些系统___________________________________3.2.12.2 N If there are computer systems for materials and products management, does the company assure the system’s safety? 如果有经计算机系统来对物料和产品管理,那么公司能不能保证系统的安全3.2.13 INF Are regular inventories conducted? 定期清点存货吗?3.2.13.1 N Are there records? 有具体记录吗3.2.14 R R Are stored materials and products away from the floor and walls, in order to facilitate cleaning and conservation? 为了保证洁净,所储存的物料和产品是否不接触地板和墙面呢3.3.- Raw materials receipt and storage 原料接收与储存Nº Qualif. Items YES NO N/A3.3.1 N Is the available area consistent with the volume of operations? 是否有足够区域来完成相应操作3.3.2 N Are all the activities carried out in this area compliant with the previously defined Standard Operating Procedures (SOP)? 所有在这区域进行的操作是否符合先前定义的SOP3.3.2.1 N Are there records for the critical operations described in the relevant Standard Operating Procedures (SOP)? 是否记录SOP中的关键操作?3.3.3 N Are raw materials correctly labeled by the supplier/manufacturer? 供应商/生产商有没有对原材料正确地贴标3.3.3.1 N Is the label properly adhered to the container’s body? 标签有没有正确地贴在容器上3.3.4 N Does every raw material batch receive a registration number on receipt? 每一批原料在接收时都有登记号吗?3.3.4.1 N Is the registration number used to identify the raw material up to its final utilization? 登记号是用来识别原料,直到其最后使用之前3.3.5 N Does the label from the company permit the correct identification, visualization or electronic control of the raw material status?标签能否对原料的状态做出正确的识别,可视化或电子控制3.3.5.1 N Is it properly adhered to the container’s body? 标签是正确地贴在容器上吗?3.3.6 N Does the raw material stay quarantined and properly identified as such, before being released by Quality Control? 在QC放行之前,原料是否同样有被检疫和标识?3.3.6.1 N In case of computer controlled inventories, is the use of a quarantined raw material blocked until its release by an authorized person?在电脑控制存货记录的情况下,待检疫的原材料是否是在授权人放行之后才能使用3.3.7 N Is a raw material already approved and identified as such, transferred to the correspondent area/system? 原料是否经批准和识别,然后转入相应区域3.3.8 I Are raw materials used only after release by Quality Control? 原料是否只是在被QC 放行后才使用3.3.9 N Is the expiry date indicated in the label? 过期日期是否有在标签中显示3.3.10 N Is there a reanalysis program for stored raw materials, respecting the validity term established by the manufacturer thereof? 是否对原辅料厂家制定的有效期进行重新分析的程序3.3.10.1 N Is the reanalysis date indicated in the label/system, where applicable? 如果进行重新分析的话,标签/系统中是否有重新分析的日期3.3.11 N Is there a program for Suppliers’ Qualification? 有关于了解供应商资质的程序吗3.3.11.1 N Are the suppliers of active substances qualified? 活性物质供应商合格吗?3.3.11.2 N Are there defined criteria for monitoring the program? 有没有设定的标准来监测控这些程序3.3.12 Does program include: 项目是否包括:3.3.12.1 INF Evaluation of the supplying history? 供应历史的评价3.3.12.2 INF Preliminary evaluation through a questionnaire? 通过调查问卷做初步估计3.3.12.3 INF Quality audits? 质量审核3.3.13 N Are the rejected raw materials properly identified and segregated? 不合格的原料是否适当地鉴别与隔离?3.4.- Packaging materials receipt and storage 包材接收与储存Nº Qualif. Items YES NO N/A3.4.1 N Is the available area consistent with the volume of operations? 是否有足够区域来完成相应操作3.4.2 N Are all the activities carried out in this area compliant with the previously defined Standard Operating Procedures (SOP)? 所有在这区域进行的操作是否符合先前定义的SOP3.4.2.1 N Are there records for the critical operations described in the relevant Standard Operating Procedures (SOP)? 是否记录SOP中的关键操作3.4.3 N Are packaging materials correctly labeled by the supplier/manufacturer? 供应商/生产商对包材是否都有正确的标签3.4.4 N Do packaging materials receive a registration number on receipt? 包材在接收时是否都有一个登记号码?3.4.4.1 N Is the registration number used to identify the packaging material up to its final utilization? 原材料在最后使用之前,其登记号一直用来识别/标识吗3.4.5 N Does the label from the company permit the correct identification, and visualization of the packaging material status? (rejected, quarantined and approved )?标签能否对包材的状态做出正确的识别,可视化或电子控制(退回,检疫还是批准)3.4.6 N Are all the material batches sampled by Quality Control, according to proper and reliable statistical systems? 根据统计系统,是否所有批的原材料QC都要进行取样?3.4.7 N Is the quantity of sampled material according to the established sampling procedure? 材料取样的量是否根据建立的取样程序?3.4.8 N Does the packaging material stay quarantined and properly identified as such, before being released by Quality Control?在QC放行之前,包材是否有被检疫和识别3.4.9 N Is a packaging material already approved and identified as such, transferred to the correspondent area/system? 包材是否在被批准和鉴别后,转入相应区域3.4.10 N Are the rejected materials properly identified and segregated?不合格包材是否有恰当地标识和隔离?3.4.11 R Are the materials deemed old or obsolete destroyed? 旧的原材料是否会被销毁3.4.11.1 N Are there records? 有相关记录吗3.4.12 N Is there a locked sector in the store room, with restricted access, for the printed material? 仓库是否有个锁定的区域,并有限制人员进入,来放已印好的包材3.4.12.1 N Is the access to the restricted area permitted only to authorized personnel? 只有指定人员才能进入这个限定区域吗?3.5.- Intermediate and bulk products receipt and storage 中间产品和原液(原粉)的接收和储存Nº Qualif. Items YES NO N/A3.5.1 Is there an area for storage of products? 有区域来存放以下产品吗3.5.1.1 I Intermediate products? 中间产品3.5.1.2 N Bulk products? 原液(原粉)3.5.2 N Are all the activities carried out in this area compliant with the previously defined Standard Operating Procedures (SOP)? 所有在这区域进行的操作是否符合先前定义的SOP3.5.2.1 N Are there records for the critical operations described in the relevant Standard Operating Procedures (SOP)? 是否记录SOP中规定的关键操作?3.5.3 Are defined procedures for receipt and storage of intermediate and bulk products: 中间产品和原液(原粉)的储存和接受是否所设定的程序3.5.3.1 N Locally produced? 当地生产的3.5.3.2 I Imported? 进口的3.5.4 I Are there locked storerooms or facilities, with restricted access, for intermediate and bulk products subject to special control? 在储藏室中是否有个锁定的区域或设施,并有限制人员进入,用于存放需要特殊控制的中间产品和原液(原粉)3.5.5 N Do the control and recording system for shipping intermediate and bulk products observe the correspondent sequence relation for batches and maximum storage term established for each product? 对中间产品和原液(原粉)的控制和记录系统是否遵循每个产品的批次及最大储存期限的顺序?3.5.6 N Is the storage of intermediate and bulk products conducted with the proper care and safety, in order to prevent potential mixing during control process and shipping errors, as well as accidents when being handled? 为了防止控制过程中可能的混淆,运输错误以及操作中的事故,中间产品和原液(原粉)是否适当安全的储存?3.5.7 N Do the intermediate and bulk products stay quarantined and properly identified as such, before being released by Quality Control? 在QC放行之前,中间产品和原液(原粉)是否有被检疫和识别3.6.- Finished Products receipt and storage 制剂接收和仓储Nº Qualif. Items YES NO N/A3.6.1 N Is there an area for storage of finished products? 有存放制剂的区域吗3.6.2 N Are all the activities carried out in this area compliant with the previously defined Standard Operating Procedures (SOP)? 所有在这区域进行的操作是否跟先前定义的SOP一致3.6.2.1 N Are there records for the critical operations described in the relevant Standard Operating Procedures (SOP)? 是否记录SOP中规定的关键操作?3.6.3 N Do the registration and control system for shipping of finished products observe the correspondent sequence relation for batches and validity term? 制剂运输的记录和控制系统是否遵守批记次和有效期的顺序3.6.4 N Is the storage conducted with the proper care and safety, in order to prevent potential mixing during control and shipping errors, as well as accidents when being handled? 为了防止控制过程中可能的混淆,运输错误以及操作中的事故,制剂是否适当安全的储存?3.6.5 N Do the finished products stay quarantined and properly identified as such, before being released by Quality Control? 在QC放行之前,制剂是否有被检疫和识别3.6.5.1 N If there are computer systems for materials and products management, does the company assu re the system’s safety? 如果有计算机系统来管理物料和产品,那能保证系统的安全吗3.6.6 N Are the products safely stacked? 产品保存安全吗3.6.7 I Are there locked storerooms or facilities, with restricted access, for products subject to special control? 是否有个锁定的区域或设施来存放需要特殊控制的产品,并有限制人员进入3.6.8 N Does the company have established procedures concerning products whose expiry dates are near to their due date?公司有没有建立一套关于即将到效期产品的规程3.6.8.1 N Are such procedures complied with? 这些程序符合相关规定吗3.6.8.2 N Are there records? 有相关规定吗3.6.9 N Does the company have distribution records for products, allowing for tracking of primary distribution client? 公司有没有产品的销售记录,允许跟踪一级分销商3.6.9.1 N Are all primary distribution clients properly authorized by the appropriate Sanitary Agency? 所有一级分销商是否有相关卫生部授权3.7. Raw Materials Sampling Area 原材料取样区Nº Qualif. Items YES NO N/A3.7.1 N Is there a specific room for raw materials sampling? 有没有专门的原材料取样区?3.7.2 N Are all the activities carried out in this area compliant with the previously defined Standard Operating Procedures (SOP)?所有在这区域进行的操作是否跟先前定义的SOP一致3.7.2.1 N Are there records for the critical operations described in the relevant Standard Operating Procedures (SOP)? 是否记录SOP中规定的关键操作?3.7.3 N Are the employees properly dressed (uniformed)? 员工有没有合理着装(制服)3.7.3.1 N Are the uniforms clean? 制服干净吗3.7.4 N Do they wear personal protection equipment, where necessary? 如果需要,他们有戴防护设备吗3.7.5 N Do the facilities present proper hygiene conditions? 设施有良好的卫生条件吗3.7.6 R Does the area have temperature and relative humidity control, where necessary?如果需要,那里有温度和相对湿度的控制吗3.7.6.1 N Are there records? 有相关记录吗3.7.7 N Should there be deviations related to the established parameters, is the cause investigated? 温湿度测试值和设定值之间有没有偏差,如果有,有调查过什么原因吗3.7.7.1 N Are there preventive and/or corrective actions related to the identified causes? 对于这些被识别的原因,有防护或整改的措施吗3.7.7.2 N Are there records? 有相关记录吗3.7.8 INF Are equipment for measurement of pressure differentials required? 需不需要测量压差的设备3.7.8.1 N If yes, are such equipments available?如果需要,是否有这样的设备?3.7.8.2 N Are there records? 有相关记录吗3.7.9 INF Are sterile raw materials sampled? 无菌的原料取样吗3.7.9.1 N Is sampling carried out under Laminar Flow, installed in a classified area? 取样在百级层流下(洁净级为背景)进行吗3.7.9.2 N Are the Laminar Flow and the Area qualified? 百级层流区域条件合格吗3.7.9.3 N Are there records? 有相关记录吗3.7.10 N Are the instruments and appliances used for sampling appropriate? 有没有适当的取样设备与仪器吗3.7.10.1 N Are the instruments and containers that have contact with the raw material cleansed or sterilized, before and after use? 跟原料直接接触的仪器和容器在使用前后有没有进行清洗和灭菌3.7.10.2 N Are such materials identified concerning their cleansing status? 上述仪器或容器是否有洁净状态的标识3.7.11 N Are the sampled containers labeled?取样容器有没有贴标签3.7.12 Content identification testing for containers of the active substances is performed: 装活性物质的容器是否做鉴别测试3.7.12.1 N For all containers? 所有容器吗3.7.12.2 N In a statistical sampling, in the case of Large-Volume Parentereal(注射)Solutions (LVPS) manufacturers, provided that the supplier is qualified: 按统计学取样,对于大容量注射器而言,如果供应商合格,那是否做容器的鉴别测试3.7.13 N Is identification testing for content of an statistical sampling of excipients performed? 辅料容器是否进行鉴别测试3.7.14 N Are the sampling containers labeled and closed after sampling? 做完采样后,取样容器贴上标签并密封吗4.- COMPLAINTS 投诉Nº Qualif. Items YES NO N/A4.1 NN Is there a person appointed for receiving complaints? 是否有专人负责接收投诉4.2 NN Are there Standard Operating Procedures (SOP) for evaluation and actions to be taken concerning the complaints? 是否有SOP来规定如何处理投诉4.3 N Is there a person in charge of decisions and actions to be taken?是否有人负责对投诉做决定和采取措施。
|
||生活|
一个人总要走陌生的路,看陌生的风景,听陌生的歌,然后在某个不经意的瞬间,你会发现,原本费尽心机想要忘记的事情真的就这么忘记了..
|-----郭敬明
药品GMP认证检查评定标准
一、药品GMP认证检查项目共259项,其中关键项目(条款号前加“*”)92项,一般项目167项。
二、药品GMP认证检查时,应根据申请认证的范围确定相应的检查项目,并进行全面检查和评定。
三、检查中发现不符合要求的项目统称为“缺陷项目”。
其中,关键项目不符合要求者称为“严重缺陷”,一般项目不符合要求者称为“一般缺陷”。
四、缺陷项目如果在申请认证的各剂型或产品中均存在,应按剂型或产品分别计算。
五、在检查过程中,企业隐瞒有关情况或提供虚假材料的,按严重缺陷处理。
检查组应调查取证并详细记录。
六、结果评定
(一)未发现严重缺陷,且一般缺陷≤20%,能够立即改正的,企业必须立即改正;不能立即改正的,企业必须提供缺陷整改报告及整改计划,方可通过药品GMP认证。
(二)严重缺陷或一般缺陷>20%的,不予通过药品GMP认证。
药品GMP认证检查项目。
GMP条款及12个附录(每个章节均有国家局问答)
GMP条款及12个附录
第一章总则
第二章质量管理
第三章机构与人员
第四章厂房与设施
第五章设备
第六章物料与产品
第七章确认与验证
第八章文件管理
第九章《生产管理》
第十章《质量控制与质量保证》
第十章《质量控制与质量保证》
第十一章《委托生产与委托检验》
第十二章《产品发运与召回》
第十三章《自检》
第十四章《附则》
附录1《无菌药品》
附录1《无菌药品》问答
附录2《原料药》
附录3《生物制品》附录4《血液制品》
附录5《中药制剂》
附录6 放射性药品附录7 中药饮片附录8 医用氧
附录9《取样》
附录10《计算机化系统》附录11《确认与验证》附录12 生化药品。
gmp条款230条GMP(Good Manufacturing Practice)是一种药品生产和质量管理的国际标准,旨在确保药品的安全性、质量和有效性。
本文将详细解读GMP条款230条,涉及到的内容包括:一、设备验证和维护在药品生产过程中,设备的验证和维护是非常重要的环节。
根据GMP条款230条的规定,企业应当对所有与药品生产有关的设备进行验证,并确保其符合相关标准和要求。
验证工作应当包括设备安装、操作和清洁等方面的检查和测试。
同时,企业还应当建立设备维护计划,并定期检查和维护设备的正常运行。
二、设备清洗设备的清洗是保证药品质量和安全的重要步骤。
根据GMP条款230条的规定,企业应当建立设备清洗的操作规程,并确保其得到严格执行。
清洗工作应当包括清洗剂的选择、清洗程序的制定和执行、清洗后的检查和验证等方面。
此外,企业还应当建立清洗记录,以备日后审查。
三、设备维护设备的维护是保障药品生产连续性和质量稳定性的关键环节。
根据GMP条款230条的规定,企业应当建立设备维护计划,并记录设备维护的内容和结果。
维护工作包括定期检查设备的运行状况、更换易损件、进行预防性维护等。
企业还应当建立设备维护记录,以备日后追溯和审查。
四、设备更换和淘汰设备的更换和淘汰是确保药品生产设备处于良好状态的重要措施。
根据GMP条款230条的规定,企业应当建立设备更换和淘汰的程序和计划,并定期进行检查和评估。
当设备出现重大缺陷、无法修复或达到使用寿命时,应当及时更换或淘汰,并记录相关信息。
五、设备使用人员培训设备使用人员的培训是保障药品生产质量和安全的重要环节。
根据GMP条款230条的规定,企业应当对设备使用人员进行培训,并确保其熟悉设备的操作、维护和清洗等要求。
培训应当包括理论知识和实际操作,并建立培训记录。
六、设备故障和事故处理设备故障和事故的处理是保障药品生产连续性和紧急情况应对能力的重要环节。
根据GMP条款230条的规定,企业应当建立设备故障和事故处理的程序,并进行定期的演练和培训。
Audit Checklist for Drug IndustryDisclaimerThe following checklist is intended to aid in the systematic GMP audit of a facility that manufactures drug components or finished products.The adequacy of any procedures is subject to the interpretation of the auditor. Therefore, the author accepts no liability for any subsequent regulatory observations or actions stemming from the use of this audit checklist.Instructions for Using this Audit Checklist:Before starting an on-site audit, plan the audit. Review past audits, note indications of possible problem areas and items, if any, that were identified for corrective action in a previous audit. If you are not already familiar with this facility, learn the type of product produced here and how it is organized by personnel and function. What does your "customer", ., your superior or senior facility management, expect to learn from this audit?The checklist is to be used with a notebook into which detailed entries can be made during the audit.While the checklist is to guide the auditor, is not intended to be a substitute for knowledge of the GMP regulations.Although a single question may be included about any requirement, the answer will usually be a multi-part one since the auditor should determine the audit trail for several products that may use many different components. Enter details in your notebook and cross reference your comments with the questions.At least three production batches should be selected for thorough analysis to include: (a) traceability of all components or materials used in the subject batches,(b) documentation of raw material or component, in-process, and finished goodstesting for the subject product batches, (c) warehousing and distribution records as they would relate to a possible recall.Responses entered on the checklist should be consistent. "X" is recommended for "NO"; a checkmark for "YES"; "n/a" for not applicable to questions that do not apply. An asterisk and notebook page number should be entered on the checklist to identify where relevant comments or questions are recorded in your notebook.The notebook used should be a laboratory-type notebook with bound pages. the notebook should be clearly labeled as to the audit type, date, and auditor(s). Many auditors prefer to use a notebook for a single audit so it may be filed with the checklist and the final report.The references to sections in the GMP regulation are for your convenience shoulda question arise. In some instances, two or more sections within the GMPregulation may have bearing on a specific subject. The headings in the GMP regulation will usually offer some guidance on the areas covered in each section.A general suggestion for a successful audit is to spend most of your time on major issues and a smaller portion of your time on small issues. there may be observations that you may wish to point out to supervisory personnel that deserve attention, but do not belong in an audit report because they are relatively insignificant. By the same token, too many small items suggests a trend of non-compliance and deserve attention as such. When citing these, be specific.Question Instructions/questions (note any exceptions and comments in notebook).Yes, No, or NA Document N°; archiving areaGeneral Controls。
欧洲药品生产质量管理规范2008版目录目录第一章质量管理.................................................................. 错误!未定义书签。
原则…………… ................................................................ 错误!未定义书签。
质量保证........................................................................... 错误!未定义书签。
药品生产质量管理规范(GMP)............................................. 错误!未定义书签。
质量控制(QC).................................................................... 错误!未定义书签。
产品质量回顾.................................................................... 错误!未定义书签。
第二章人员 ....................................................................... 错误!未定义书签。
原则… .............................................................................. 错误!未定义书签。
通则… .............................................................................. 错误!未定义书签。
关键人员........................................................................... 错误!未定义书签。
A 工厂总体印象1厂房与设施、设备1.1 规划/设计:将差错、混淆、交叉污染,灰尘、泥土的累积情况减少到最低限度。
1.2 有效的清洁和维护,且经批准1.3 有控制啮齿动物、昆虫和害虫的SOP,确保建筑物内无昆虫、动物(尤其是龋齿动物),鸟类的存在。
1.4 厂房等建筑物维护良好1.5 检查垃圾箱、标签、产品,废弃物料不断被清除(没有积压)。
1.6 关于卫生的SOP:要有做卫生的时间表、方法、工具。
做卫生的设备要方便易拿有秩序进行的清洁、消毒(包括更衣室?change room,洁具间,盥洗室,食堂)1.7 要有足够的光线,通风系统,过滤系统,测量仪器灰尘控制,适当的湿度、压力和温度。
(外面的空气过滤,回风,达到最低的要求。
)1.8 环境定期监控并记录1.9 生产区:合理的人流物流,足够的空间。
1.10 高致敏性药品的生产要在单独的设施中进行(如青霉素、生物制品、某些抗生素、激素和细胞霉素的生产要在专门的设施中进行。
)1.11 工业用毒药(杀虫剂和除草剂)不应出现在生产药品的厂房中。
1.12 有足够的生产空间和中间站面积1.13 在产尘的地方有捕尘和集尘装置1.14 所有的排水都能收集在排水管里1.15 管道,装置的连接处和其他设施不应有难清洁的地方。
1.16 管道上应贴标签,标出物料和流向。
1.17 地板,墙壁,天花板采用容易清洁的材料。
1.18 贮藏区:确保好的储藏条件(干净、干燥、温度)1.19 设立专署贮藏区:比如易燃的物品、阴凉库、低湿度间。
要有监控报警装置在非正常情况下报警2休息室、盥洗室2.1 休息室、吸烟区和点心间应该和其他区域分开。
2.2 盥洗室的设置对于使用人员应容易上盥洗室且便利。
2.3 盥洗室不能直接和生产区或储藏区相连,要保持干净,通风。
2.4 有肥皂、毛巾、卫生纸,必要时有淋浴设施2.5没有外来物料。
(标签、药品)3接收区域3.1 接收和发放区域要能保护原料或产品不受天气影响。
3.2 每个容器或容器组要保持干净,检查标签是否合适(包括名称、批号、有效期、供应商),损坏度,污染情况,容器附带订单和发票。
3.3 企业内部代号清单。
3.4 批准的供应商清单(reg affairs注册商)3.5 应有的SOP:原材料的控制、购买、接收、贮存、处理和发放,包装材料,中间产品、成品。
3.6 所有物料的处理和贮存都必须防止污染、变化(如降解)和混杂。
3.7 只有相关的文件(如检验报告单,放行单)都具备时才能进入库存。
3.8 待检品只有在QC检验放行后才能使用3.9 状态标识清晰,用手工贴好,或用经过验证的计算机系统来管理。
3.10未印刷和已印刷包材的购买、处理和控制3.11 起始物料的接收和PPM记录(GRV),包括:接收日期、物料名称、供应商、供应商的批号、总量和容器(箱,桶等)数量,及AR数量。
4 仓储4.1 如果没有电脑控制——隔离划分区域,最好有物理隔离(均完全隔离,各自独立):取样(区),待检验(区),原材料,包装材料,中间体,成品,不合格品,召回和返工的产品。
4.2 严格控制人员进入这些区域,环境安全可靠。
4.3 待检品,合格品或不合格品应该隔离开来,且符合以下要求:物理上的隔离区;清晰,易于区分状态的标签(用于容器上和设备上的标签应意思清楚,字迹清晰,内容完整;有控制系统,如计算机系统(经过验证)。
4.4 用于控制和监控环境的SOP:贮存温度,湿度,无直接光照,没有暴露在空气中。
4.5 要离开地板(比如用一个托盘,不直接接触地面),与其它物料和墙壁也要保持合理的距离。
4.6 每一批整体维护4.7 取过样的容器应能背识别4.8 执行先进先出4.9 复检日期,合适的系统监控贮存期。
5取样区5.1 独立的区域,光照,通风,集尘器。
5.2 仪器设备的SOP。
5.3 清洁的SOP和记录。
5.4 防止交叉污染。
5.5 取的样品能够代表整批5.6 SOP包括:方法,所用的仪器,取样量,任何需要再次分装的操作指导、取样容器的类型和状态,应观察的一些特殊的预防措施(无菌或有害的物料),取样工具的清洗和储藏5.7 取样标签包括:样品名(所含物质名称),批号,取样日期,取样者,样品来源(来自哪一个容器)。
5.8 注意:避免取样过程中和取样后发生污染和变质。
取样后容器的重新密封。
6 已放行物料区6.1只有QC放行的物料6.2 状态标志清晰。
6.3 由具有责任心的,经过适当培训的人员发放,。
6.4 接收数量、流转、返回数量的记录。
6.5 差异调查。
6.6 适当的标签(状态清晰,不太多标签):品名、相关的内容代码、接收时的批号、状态、失效期或复检期。
6.7先进先出6.8 没有过期的材料。
7 不合格品区7.1 制定区域,进入受控制。
7.2 SOP:标签,责任划分。
7.3 不合格原因有文件证明8 退货品区8.1 专用的区域,进入受控8.2 从市场退回的产品除非能证明质量是令人满意的,否则要销毁。
8.3 SOP9 已印刷的包装材料区域9.1 人员进入受控制9.2 每个物品分开存放,易于识别,整个区域独立且上锁。
9.3由有责任心并经过适当培训的人员负责管理。
9.4 发放:严格、有序、细致的控制。
9.5 避免混杂:在密闭容器内运输。
多余的物品如果会导致混杂,则必须销毁返回的物料。
整批完整的保存。
9.6 箔:温度和湿度的控制。
10 成品库10.1 由质量控制部门(QC)放行物料,在有效期内。
10.2 由指定的人员发放。
10.3 正确的物料被准确的称量到干净的,正确贴标的容器。
10.4在现场没有其他外来物料。
10.5 每个被发放物料的名称、数量、体积要由药师或其他合法授权人员独立地检查并签字。
10.6 分发的物料,每一批要放在一起并且有明显的标签。
10.7 清洁SOP和记录。
10.8 天平的校准与维护的SOP和记录。
10.9 光线充足、通风和集尘器。
11 生产区11.1 人流、物流、墙壁、地板、温度、交叉污染。
11.2混合要由药师审核,签字。
11.3 每个区域,每次只能生产一个产品,或者必须没有混淆、交叉污染的危险。
11.4 同一批物料放在一起。
11.5 在开始生产之前,对厂区和设备的卫生进行检查。
11.6产品和物料要有防止微生物和其它污染源污染的措施。
11.7 原材料、散装物料的集装箱(bulk containers),主要设备一览表,用标签标志清楚(区分开),在生产阶段标明处理的物料的批号和流向。
11.8 管道连接正确11.9 进入受控制11.10 偏差受控制11.11 计算产量和收率,不一致的地方则要调查并解释。
11.12 签字确认关键步骤11.13 有中测站做过程控制实验11.14 包装物或设备进入生产区之前,清除其上不适当的标签。
11.15 已经做了环境检测。
11.16 避免交叉污染,定期有效的检查,有SOP11.17 避免灰尘产生和传播11.18 生产前要经过批准,(有生产指令)11.19 中间产品和待包装品:储存条件,控制周期和标签。
11.20 重加工的SOP11.21 口服固体制剂的标准的特殊要求?11.22 无菌制剂(产品)的标准?11.23 special for LCO,气雾剂。
11.24 管道标志:清楚地显示内容物名称和流向。
11.25 在生产区域内没有:吃东西、喝水(酒)、吃零食、抽烟,或存有食物、饮料,私人药品等私人物品。
11.26 操作者不得裸手直接接触原料、中间产品和成品。
11.27 洁净服提供给进入生产区的人(包括参观人员、生产人员、高级管理者和检查者),工作服定期、经常清洗,不得穿出规定区域外。
11.28 有故障的设备应移走或至少标识清楚,标明有故障。
11.29 清洁SOP11.30 设备在清洁、干燥的环境中储藏。
11.31 完整的清洁记录,显示上一批产品11.32 记录填写清晰符合规范,复核人签字没有涂改的,用墨水或其它不能擦掉的笔填写。
11.33 记录及时,和操作同步。
11.34 记录错误更正:原来的字迹留存,修改者签名和修改日期,加上修改的原因。
没有涂改。
12 包装12.1 区域适当(空间足够,照明充足,空气流通)12.2 SOP12.3 包装文件、规范的要求,标签和贴签。
12.4 作废的印刷包材的销毁,而且有记录。
12.5 包装线很好地分开,或用物理栅栏隔离,防止混淆。
12.6 包装线清场/启用:检查清单,由药师签字。
12.7 在包装场所或包装线上挂上包装的品名和批号。
12.8 对进入包装部门的物料要核对,品名,与包装指令一致。
12.9 贴签后要尽快包装密封12.10 打印(如批号和有效期)操作要复核并记录。
12.11 手工包装要加强警惕,防止不经意的混淆。
12.13 过程控制:以下应以列表的形式定期检查并签名:包装后的外观包装的数量/体积或者数量一致包材是否齐全产品与在用的包装材料是否正确检查任一印刷完了的,印刷是正确的,?密封完整。
监视器的功能是正确的。
12.14 生产时定期检查自动控制设备和监测器。
经常确认它们是好的12.15 从包装线上取走的样品不能返回。
12.16 每次包装工序完成要计算收率12.17 特别注意控制未用完的包材。
12.18 包装结束:清洁,清除包材、标签、未使用的而已打印代号的包装材料已被销毁并有记录。
13 成品放行13.1 成品在放行前应隔离13.2 文件一致,完整。
由QA审核整套文件。
(SOP)13.3 由药师放行14 QC实验室14.1 建筑:与生产区分开,是独立的14.2 清洁情况:地板、墙、天花板,集尘/通风,光照,管道,线路,记录/记录本14.3 附有对生物制品/放射性样品/青霉素的特殊要求14.4 人员受到良好的培训和管理,工作主动。
14.5 有足够的空间避免混淆和交叉污染。
有足够的,合适的地方储存样品和记录。
14.7 仪器设备:位置、状态,有记录本。
每个设备都有SOP(操作、清洁、校准/复查),维护记录。
14.8 文件:取样SOP,样品和记录的保存,稳定性试验,与质量有关的投诉的调查,所有物料和产品的检验,检验的管理,标签的控制(SOP),维护记录,质量标准,主文件,记录本,检验结果,检验报告单,标签,趋势分析,自检,批准,归档情况课本(参考书,药典)重新检测的SOP:在检测不符时,在重新取样时,结果没有平均时。
主要的文件要随时可得。
它们包括:质量标准、取样规程、检验规程和记录(包括分析记录表/实验室记录本)、分析报告,或是证书,环境监控的数据、分析方法的验证记录、校准和维护的SOP及记录。
检验记录:名称、产品数量、相关代号、接收日期、取样和测试的日期,生产人员或是提供产品的人,提供者的批号。
检验的执行,14.9 提供分析室的试验记录:数据来源(如:重量、读数、记录表等),结果和计算过程被记录并被重点检查和复核14.10 检验(起始物料)被记录,(主要内容)包括:取样日期、检验日期、物料名称和数量、批的编号,检测结果、分析者,COA的参照,分析者签名、状态结论。