英文病例表达模板
- 格式:pptx
- 大小:61.97 KB
- 文档页数:16
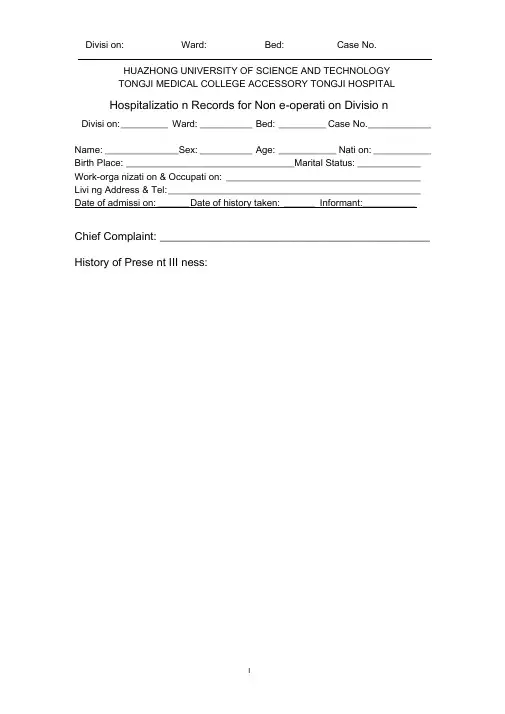
HUAZHONG UNIVERSITY OF SCIENCE AND TECHNOLOGYTONGJI MEDICAL COLLEGE ACCESSORY TONGJI HOSPITALHospitalizatio n Records for Non e-operati on Divisio nDivisi on: _________ Ward: __________ Bed: _________ Case No. ____________Name: ______________Sex: __________ Age: ___________ Nati on: ___________ Birth Place: ________________________________Marital Status: ____________ Work-orga nizati on & Occupati on: _____________________________________ Livi ng Address & Tel: ________________________________________________ Date of admissi on: ______ Date of history taken: ______ Informant:__________Chief Complaint: ____________________________________________History of Prese nt III ness:Past History:Gen eral Health Status: l.good 2.moderate 3.poorDisease history: (if any, please write dow n the date of on set, brief diag no sticand therapeutic course, and the results.)Respiratory system:1. None2.Repeated pharyngeal pain3.chronic cough4.expectoration:5. Hemoptysis6.asthma7.dyspnea8.chest painCirculatory system:1.No ne2.Palpitatio n3.exerti onal dysp nea4..cya no sis5.hemoptysis6.Edema of lower extremities7.chest pain8.s yn cope9.hypertensionDigestive system:1.None2.Anorexia3.dysphagia4.sour regurgitation5.eructation6.nausea7.Emesis8.melena9.abdominal pain 10.diarrhea11.hematemesis 12.Hematochezia 13.ja un diceUrinary system:1.N one2.Lumbar pain3.uri nary freque ncy4.uri nary urge ncy5.dysuria6.oliguria7.polyuria8.retention of urine9.ineontinence of urine10.hematuria ll.Pyuria 12.n octuria 13.puffy faceHematopoietic system:1.N one2.Fatigue3.dizz in ess4.gi ngival hemorrhage5.epistaxis6.subcuta neous hemorrhageMetabolic and en docri ne system:1.None2.Bulimia3.anorexia4.hot intoleranee5.cold intoleranee6.hyperhidrosis7.Polydipsia8.amenorrhea9.tremor of hands 10.character cha nge II.Marked obesity12.marked emaciati on 13.hirsutism 14.alopecia15.Hyperpigme ntatio n 16.sexual fun cti on cha ngeNeurological system:1.N one2.Dizz in ess3.headache4.paresthesia5.hypo mn esis6. Visual disturbanee7.lnsomnia8.somnolence9.s yn cope 10.c onv ulsi on II.Disturba nee of con scious ness12.paralysis 13. vertigoReproductive system:1.No ne2.othersMusculoskeletal system:1.None2.Migrating arthralgia3.arthralgia4.artrcocele5.arthremia6.Dysarthrosis7.myalgia8.muscular atrophyIn fectious Disease:1.N one2.Typhoid fever3.Dyse ntery4.Malaria 4.Schistosomiasis4. Leptospirosis 7.Tuberculosis 8.Epidemic hemorrhagic fever9.othersVacci ne ino culati on:1.No ne2.Yes3.Not clearVacci ne detail _________________________________________ Trauma an d/or operatio n history: Operati ons:1.No ne2.YesOperati on details: ______________________________________ Traumas:1.No ne2.YesTrauma details: _________________________________________ Blood tran sfusi on history:1.None2.Yes ( 1.Whole blood 2.Plasma3.Ingredient transfusion)Blood type: ___________ Tran sfusi on time: _________Tran sfusi on react ion1.None2.YesCli nic manifestation: ____________________________ Allergic history:1.No ne2.Yes3.Not clearallergen: _______________________________________________cli nical manifestation: ____________________________________Pers onal history:Custom livi ng address: ____________________________________________ Reside nt history in en demic disease area:Smoki ng: 1.No 2.YesAverage pieces per day; about yearsGivi ng-up 1.No 2.Yes (Time: )Drinking: 1.No 2.YesAverage grams per day; about yearsGivi ng-up 1.No 2.Yes(Time: ) Drug abuse: 1.No 2.YesDrug names: ______________________________________ Marital and obstetrical history:Married age: _________ years old Pregnancy ___________ t imesLabor ______________ times(1.Natural labor: ______ times 2.0perative labor: __________ times3. __________________ Natural abortion: _______________ times4.Artificial abortion: ____ times5. _______________________ Premature labor: _________ times6.stillbirth _________________ times)Health status of the Mate:1.Well2.Not fineDetails: _______________________________________________ Men strual history:Menarchal age: _______ Duration ________ d ay Interval ____ daysLast menstrual period: ____________ Menopausal age: ______ y ears oldAmount of flow: 1.small 2. moderate 3. largeDysme no rrheal: 1. prese nee 2.abse ncMe nstrual irregularity 1. No 2.Yes Family history: (especially pay atte ntio n to the in fectious and hereditary diseaserelated to the present illness)Father: l.healthy 2.ill: _________ 3.deceased cause: ____________________ Mother :1.healthy 2.ill: ________ 3.deceased cause: ____________________ Others: ________________________________________________________The an terior stateme nt was agreed by the in forma nt.Sig nature of in forma nt: Datetime:Physical Exam inationVital sig ns:Temperature: ______ C Blood pressure: ______ / ______ mmHg Pulse: ____ bpm (l.regular 2.irregular ) Respiration: __ bpm (l.regular 2.irregular )Gen eral con diti ons:Development: I.Normal 2.Hypoplasia 3.HyperplasiaNutrition : l.good 2.moderate 3.poor 4.cachexiaFacial expressi on: 1.no rmal 2.acute 3.chr onic other ___________________ Habitus: l.asthenic type 2.sthenic type 3.ortho-thenic typePositi on: l.active 2.positive pulsive 4.other _______________________ Consciousness: l.clear 2.somnolence 3.confusion 4.stupor 5.slight coma6. mediate coma7.deep coma8.deliriumCooperation: 1Yes 2.No Gait: 1.normal 2.abnormal _____Skin and mucosa:Color: 1.normal 2.pale 3.red ness 4.cya no sis 5.ja un dice 6.pigme ntatio nSk in erupti on: 1.No 2.Yes( type: _________ d istribution: _________________ )Subcuta neous bleed ing: 1.no 2.yes (type:______ distribution: ____________ ) Edema:1. no 2.yes ( locati on and degree ________________________________ ) Hair: 1.no rmal 2.abnormal(details ____________________________________ ) Temperature and moisture: normal cold warm dry moist dehydration Liver palmar :1.no2.yes Spider angioma (location: ________________________________ )Others: _________________________________________________________Lymph no des: enl argeme nt of superficial lymph no de:1. no2.yesDescripti on: ________________________________________________Head:Skull size:〔.normal 2.abnormal (description: __________________________ ) Skull shape: 1.no rmal 2.abnormal(description: _________________________ ) Hair distributio n :1. no rmal 2.abnormal(description: ____________________ ) Others: __________________________________________________________ Eye: exophthalmos: _________ eyelid: ___________ conjunctiva: _________ sclera: _______________ Cornea: _____________________Pupil: l.equally round and in size 2.un equal (R _____ mm L _______ m m)Pupil reflex:〔.normal 2.delayed (R __ s L _ s ) 3.abse nt (R _ L ___ )others: ______________________________________________________ Ear: Auricle〔.normal 2.desformation (description: ______________________ ) Discharge of exter nal auditory can al:1. no 2.yes (l.left 2.right quality: ___ )Mastoid tendern ess 1.no 2.yes (l.left 2.right quality: _________________ )Disturba nee of auditory acuity:1. no 2.yes(1」eft 2.right description: ___ ) Nose: Flaring of alae nasi :1.no 2.yes Stuffy discharge 1.no 2.yes(quality ____ ) Tendern ess over para nasal sinu ses:1. no 2.yes (location: ____________ ) Mouth: Lip ______________ Mucosa ____________ Tongue ________________ Teeth:1.normal 2.Agomphiasis 3. Eurodontia 4.others: _____________________Gum :1. normal 2.ab no rmal (Descripti on_________________________ )Tonsil: __________________________ P harynx: _____________________Sound: 1.no rmal 2.hoarse ness 3.others: ___________________________Neck:Neck rigidity 1. no 2.yes ( tra nsvers fin gers)Carotid artery: 1.normal pulsation 2.increased pulsation 3.marked distentionTrachea location: l.middle 2.deviation (〔.leftward ________ 2.rightward _____ ) Hepatojugular vein reflux: 1. n egative 2.positiveThyroid: 1.normal 2.enlarged ________ 3.bruit (1.no 2.yes ________________ ) Chest:Chest wall: 1.no rmal 2.barrel chest 3.pro minence or retractio n:(left _______ right ________ Precordial prominence _________ )Percussi on pai n over sternum 1.No 2.Yes Breast:〔.Normal 2.ab no rmal __ Lung: Inspection: respiratory movement〔.normal 2.abnormal ____________ Palpati on: vocal tactile fremitus:1. no rmal 2.ab no rmal ____________ pleural rubb ing sen sati on :1. no 2.yes __________________Subcuta neous crepitus sen sati on :1. no 2.yes ____________ Percussion:1. resonance 2. Hyperresonance &location _____________3 Flatness&location ________________________________4. dulln ess & location: _____________________________5. tympa ny &location: ______________________________lower border of lung: (detailed percussi on in respiratory disease) midclavicular line : R: ____ in tercostae L: ____ in tercostaemidaxillary line: R: ____ in tercostae L: ____ in tercostaescapular li ne: R: _______ in tercostae L: ____ in tercostaemoveme nt of lower borders:R: _____ cmL: _________ cm Auscultation: Breathing sound : 1.normal 2.abnormal _______________Rales:1. no 2.yes ________________________________ Heart: Inspection: Apical pulsation: 1.normal 2.unseen 3.increase 4.diffuseSubxiphoid pulsation: 1.no 2.yesLocati on of apex beat: 1. no rmal 2.shift ( ____ in tercosta,dista nee away from left MCL ____ cm) Palpati on:Apical pulsation:1. normal 2.lifting apex impulse 3.negative pulsationThrill:1. no 2.yes(location: __________ phase: ________________ )Percussi on: relative dull ness border: 1.no rmal 2.ab no rmal(Dista nee betwee n An terior Medli ne and left MCL _____ cm) Auscultation: Heart rate: __ bpm Rhythm:1.regular 2.irregular ______ Heart sound: 1.no rmal 2.abnormal ______________________Extra sound: 1.no 2.S3 3.9 4. opening snapP2 _____________ A _________ Pericardial frictio n soun d:1. no 2.yesMurmur: 1.no 2.yes (location __________ phase _____________quality _____ intensity ________ t ran smissio n _________effects of position ________________________________effects of respiration _____________________________ Peripheral vascular sig ns :1.N one2.paradoxical pulse3.pulsus alter nans4. Water hammer pulse5.capillary pulsati on6.pulse deficit7.Pistol shot sound8.Duroziezsig nAbdome n:Inspection: Shape: 1.normal 2.protuberanee 3.scaphoid 4.frog-belly Gastric patter n 1. no 2.yes In test inal pattern 1. no 2.yesAbdo minal vein varicosis 1.no 2.yes(direction: ______________ )Operatio n scarl. no 2.yes _______________________________ Palpation: l.soft 2. tensive (location: ______________________________ )Tendern ess: 1.no 2.yes(location: ______________________ )Rebo und tendern ess:1. no 2.yes(location: _____________ ) Fluctuatio n: l.prese nt 2.absce ntSuccussi on splash: 1.n egative 2.positiveLiver: ______________________________________________Percussion: Liver dullness border: 1.normal 2.decreased 3.absentUpper hepatic border:Right Midclavicular Line _______ In tercostaShift dullness:1.negative 2.positive Ascites: _____________ degreePai n on percussi on in costovertebral area: 1.n egative 2.positve __ Auscultation: Bowel sounds : 1.normal 2.hyperperistalsis 3.hypoperistalsis4.abse nee Gurgli ng soun d:1. no 2.yesVascular bruit 1.no 2.yes (location ____________________ ) Gen ital orga n: 1.un exam ined 2.no rmal 3.ab no rmalAnus and rectum: 1.un exam ined 2.no rmal 3.ab no rmalSpine and extremities:Spi ne: 1.no rmal 2.deformity (l.kyphosis 2.lo rdosis 3.scoliosis)3.Tenderness(location ____________________________ )Extremities: 1.no rmal 2.arthremia & arthrocele (location __________________ )3.A nkylosis (location _________ )4.Aropachy: 1.no 2.yes5.Muscular atrophy (location ______________________ )Neurological system: 1.no rmal 2.abnormal _____________________________ Importa nt exam in ati on results before hospitalizedSummary of the history: ______________________________________ Initial diagnosis: ____________________________________________Recorder:Corrector:。
病例报告英语作文模板高中Title: A Case Report: The Symptoms, Diagnosis, and Treatment of Influenza。
Introduction:Influenza, commonly known as the flu, is a contagious respiratory illness caused by influenza viruses. It can cause mild to severe illness and even lead to hospitalization or death, especially in high-risk groups. Here, we present a case report of a patient with influenza, detailing their symptoms, diagnosis, and treatment.Patient History:The patient, a 35-year-old male, presented to theclinic with complaints of fever, cough, sore throat, body aches, fatigue, and headache. The symptoms had started suddenly two days prior to the visit and had progressively worsened. The patient denied any recent travel history orcontact with sick individuals but reported exposure to crowded areas due to work.Clinical Examination:On examination, the patient appeared ill and fatigued. Vital signs revealed a temperature of 39.2°C (102.5°F), heart rate of 100 beats per minute, respiratory rate of 22 breaths per minute, and blood pressure within normal limits. Examination of the respiratory system revealed bilateral coarse crackles on auscultation.Diagnostic Evaluation:Given the patient's clinical presentation during the influenza season, a presumptive diagnosis of influenza was made. Nasopharyngeal swab specimens were collected for laboratory confirmation. Rapid influenza diagnostic tests (RIDTs) were performed, which yielded positive results for influenza A virus. Additionally, reverse transcription-polymerase chain reaction (RT-PCR) testing confirmed the presence of influenza A virus subtype H3N2.Treatment:Based on the diagnosis of influenza A, the patient was initiated on antiviral therapy with oseltamivir (Tamiflu). The treatment regimen included oral oseltamivir 75 mg twice daily for a duration of five days. In addition, supportive measures were implemented to alleviate symptoms and prevent complications. These measures included adequate hydration, rest, and over-the-counter analgesics for fever and body aches.Clinical Course:Following initiation of antiviral therapy and supportive measures, the patient's symptoms gradually improved over the course of the next week. Fever subsided within 48 hours of starting oseltamivir, and respiratory symptoms began to resolve. The patient was advised to complete the full course of antiviral therapy and to follow up if symptoms persisted or worsened.Discussion:Influenza is a common viral illness characterized by respiratory symptoms and systemic manifestations. It is typically diagnosed based on clinical presentation and confirmed by laboratory testing. Early initiation of antiviral therapy, such as oseltamivir, can reduce the severity and duration of symptoms, especially if started within 48 hours of symptom onset. Supportive measures play a crucial role in managing influenza, particularly in alleviating symptoms and preventing complications.Conclusion:This case report highlights the clinical presentation, diagnosis, and management of influenza in a young adult male. Prompt recognition of symptoms, timely diagnosis, and initiation of appropriate treatment are essential in managing influenza and preventing its spread in the community. Healthcare providers should remain vigilant during influenza season and advocate for vaccination as themost effective preventive measure against influenza infection.。

Divisi on: _________ Ward: __________ Bed: _________ Case No. ___________Name: _____________ Sex: __________ Age: ___________ Natio n: ___________ Birth Place: ________________________________ Marital Status: _____________ Work-orga nizatio n & Occupatio n: _____________________________________ Livi ng Address & Tel: _________________________________________________ Date of admissio n: ______ D ate of history taken: ______ Informant: __________Chief Complaint: ___________________________________________History of Present Illness:Past History:General Health Status: 1.good 2.moderate 3.poorDisease history:(if any, please write down the date of onset, brief diagnosticand therapeutic course, and the results.)Respiratory system:1. None2.Repeated pharyngeal pain3.chronic cough4.expectoration:5. Hemoptysis6.asthma7.dyspnea8.chest painCirculatory system:1.None2.Palpitation3.exertional dyspnea4..cyanosis5.hemoptysis6.Edema of lower extremities7.chest pain8.syncope9.hypertension Digestive system:1.None2.Anorexia3.dysphagia4.sour regurgitation5.eructation6.nausea7.Emesis8.melena9.abdominal pain 10.diarrhea11.hematemesis 12.Hematochezia 13.jaundiceUrinary system:1.None2.Lumbar pain3.urinary frequency4.urinary urgency5.dysuria6.oliguria7.polyuria 8.retention of urine 9.incontinence of urine 10.hematuria11.Pyuria 12.nocturia 13.puffy faceHematopoietic system:1.None2.Fatigue3.dizziness4.gingival hemorrhage5.epistaxis6.subcutaneous hemorrhageMetabolic and endocrine system:1.None2.Bulimia3.anorexia4.hot intolerance5.cold intolerance6.hyperhidrosis7.Polydipsia8.amenorrhea9.tremor of hands 10.character change 11.Marked obesity12.marked emaciation 13.hirsutism 14.alopecia15.Hyperpigmentation 16.sexual function changeNeurological system:1.None2.Dizziness3.headache4.paresthesia5.hypomnesis6. Visual disturbance7.Insomnia8.somnolence9.syncope 10.convulsion 11.Disturbance of consciousness12.paralysis 13. vertigoReproductive system:1.None2.othersMusculoskeletal system:1.None2.Migrating arthralgia3.arthralgia4.artrcocele5.arthremia6.Dysarthrosis7.myalgia8.muscular atrophyInfectious Disease:1.None2.Typhoid fever3.Dysentery4.Malaria 4.Schistosomiasis4. Leptospirosis 7.Tuberculosis 8.Epidemic hemorrhagic fever9.othersVaccine inoculation:1.None2.Yes3.Not clearVaccine detail _________________________________________ Trauma and/or operation history: Operations:1.None2.YesOperation details: _______________________________________ Traumas:1.None2.YesTrauma details: _________________________________________ Blood transfusion history:1.None2.Yes ( 1.Whole blood 2.Plasma3.Ingredient transfusion) Blood type:Transfusion time: ______Transfusion reaction1.None2.YesClinic manifestation: ____________________________ Allergic history:1.None2.Yes3.Not clear allergen: __________________________________clinical manifestation: _____________________________________Personal history:Custom living address_: __________________________________________Resident history in endemic disease are_a_: _________________________Smoking: 1.No 2.YesAverage ___pieces per day; about___yearsGiving-up 1.No 2.Yes (Time: _______________________ ) Drinking: 1.No 2.YesAverage ___grams per day; about ___yearsGiving-up 1.No 2.Yes(Time: _________________________ ) Drug abuse:1.No 2.YesDrug names: _______________________________________Marital and obstetrical history:Married age: _________ years old Pregnancy ______________ timesLabor _______________ times(〔.Natural labor: _____ times 2.0perative labor: __________ times3. __________________ Natural abortion: _______________ times4.Artificial abortion: ____ times5. _______________________ P remature labor: ________ times6.stillbirth________________________ t imes)Health status of the Mate:1.Well2.Not fineDetails: _______________________________________________Menstrual history:Menarchal age: ______ Duration ________ d ay Interval ________ daysLast menstrual period: ___________ Menopausal age: _____ years oldAmount of flow: 1.small 2. moderate 3. large Dysmenorrheal: 1. prese nee2.abse nc M enstrual irregularity 1. No 2.YesFamily history: (especially pay atte ntio n to the in fectious and hereditary diseaserelated to the present illness)Father: l.healthy 2.ill: ________ 3.deceased cause: ____________________ Mother:1.healthy 2.ill: ________ 3.deceased cause: ____________________ Others: ________________________________________________________The an terior stateme nt was agreed by the in forma nt.Sig nature of in forma nt: Datetime:Physical ExaminationVital signs:Temperature:0C Blood pressure: / mmHg Pulse: _________ bpm (l.regular 2.irregular ) Respirati on: _______ bpm (l.regular 2.irregular ) General conditions:Development:I.Normal 2.Hypoplasia 3.HyperplasiaNutrition: l.good 2.moderate 3.poor 4.cachexiaFacial expression 1. no rmal 2.acute 3.chro nic other __________________Habitus: l.asthenic type 2.sthenic type 3.ortho-thenic typePosition: l.active 2.positive pulsive 4.other ______________________ Consciousness l .clear 2.somnolence 3.confusion 4.stupor 5.slight coma6. mediate coma7.deep coma8.deliriumCooperation: 1Yes 2.No Gait: l.normal 2.abnormal ______Skin and mucosa:Color: 1.normal 2.pale 3.redness 4.cyanosis 5.jaundice 6.pigmentationSkin eruption:1.No 2.Yes( type: _________ distribution: __________________ ) Subcutaneous bleeding1: .no 2.yes (type: ____ distribution: ______________ )Edema:1. no 2.yes ( location and degree _______________________________ ) Hair: 1.normal 2.abnormal(details _____________________________________ ) Temperature and moisture:normal cold warm dry moist dehydration Liverpalmar : 1.no 2.yes Spider angioma(location: __________________________ ) Others: __________________________________________________________Lymph nodes: enlargement of superficial lymph node:1. no2.yesDescription: _______________________________________________Head:Skull size:1.normal 2.abnormal (description: ___________________________ ) Skull shape:1.normal 2.abnormal(description: __________________________ ) Hair distribution :1.normal 2.abnormal(description: ______________________ ) Others: ___________________________________________________________ Eye: exophthalmos: __________ e yelid: ___________ conjunctiva: _________ sclera: ________________ C ornea: ______________________Pupil: 1.equally round and in size 2.unequal (R _____ mm L _______ mm)Pupil reflex: 1.normal 2.delayed (R___s L___s ) 3.absent (R___L___) others:__________________________________________________________ Ear: Auricle 1.normal 2.desformation (description: _____________________ ) Discharge of external auditory canal:1.no 2.yes (1.left 2.right quality: ___ )Mastoid tenderness 1.no 2.yes (1.left 2.right quality: ________________ )Disturbance of auditory acuity:1.no 2.yes(1.left 2.right description: _____ ) Nose:Flaring of alae nasi :1.no 2.yes Stuffy discharge 1.no 2.yes(quality _____ ) Tenderness over paranasal sinuses:1.no 2.yes (location: ______________ ) Mouth: Lip _____________ Mucosa ____________ T ongue _______________ Teeth:1.normal 2.Agomphiasis 3. Eurodontia 4.others: _____________________Gum :1.normal 2.abnormal (Description __________________________ )Tonsil: __________________________ Pharynx: _____________________Sound: 1.normal 2.hoarseness 3.others: ____________________________ Neck:Neck rigidity 1.no 2.yes ( _____________ transvers fingers)Carotid artery: 1.normal pulsation 2.increased pulsation 3.marked distentionTrachea location:1.middle 2.deviation (1.leftward ________ 2.rightward ____ ) Hepatojugular vein reflux: 1. negative 2.positiveThyroid: 1.normal 2.enlarged ______ 3.bruit (1.no 2.yes _______________ )Chest:Chest wall: 1.normal 2.barrel chest 3.prominence or retraction: (left _______ right ___________ P recordial prominence _____________________ ) Percussion pain over sternum1.No 2.YesBreast: 1.Normal 2.ab no rmal _____________________________________Lung: Inspection: respiratory movement 1.normal 2.abnormal ___________ Palpation: vocal tactile fremitus:1. no rmal 2.ab no rmal ____________pleural rubb ing sen sati on :1. no 2.yes ___________________Subcuta neous crepitus sen sati on :1. no 2.yes _____________ Percussion:1resonance 2. Hyperresonance &location _____________3 Flatness&location ________________________________4. dulln ess & location: _____________________________5. tympa ny &location: _____________________________lower border of lung: (detailed percussi on in respiratory disease)midclavicular line : R: ____ i n tercostae L: ____ in tercostaemidaxillary line: R: _______ i n tercostae L: ____ in tercostaescapular li ne: R: ________ i n tercostae L: ____ in tercostaemoveme nt of lower borders:R: ______ cmL: _________ c m Auscultation: Breath ing sound : 1.no rmal 2.ab no rmal ___________Rales:1. no 2.yes _________________________________ Heart: lnspection:Apical pulsation: 1.normal 2.unseen 3.increase 4.diffuseSubxiphoid pulsation: 1.no 2.yesLocati on of apex beat: 1. no rmal 2.shift ( _____in tercosta,dista nee away from left MCL ____ cm) Palpation:Apical pulsation:1. normal 2.lifting apex impulse 3.negative pulsationThrill:1. no 2.yes(location: __________ phase: ________________ )Percussion relative dullness border: 1.normal 2.abnormal(Dista nee betwee n An terior Medli ne and left MCL ____ cm) Auscultation: Heart rate: __bpm Rhythm:1.regular 2.irregular ______Heart sound: 1.no rmal 2.abnormal ______________________Extra sound: 1.no 2.S3 3.® 4. opening snapP2 ____________ A _________ Pericardial frictio n soun d:1. no 2.yesMurmur: 1.no 2.yes (location ___________ phase ___________quality _____ i ntensity ________ tran smissio n _________effects of position ________________________________effects of respiration _____________________________Peripheral vascular signs1.None2.paradoxical pulse3.pulsus alternans4. Water hammer pulse5.capillary pulsation6.pulse deficit7.Pistol shot sound8.DuroziezsignAbdomen:Inspection:Shape: 1.normal 2.protuberance 3.scaphoid 4.frog-belly Gastricpattern 1.no 2.yes Intestinal pattern 1.no 2.yesAbdominal vein varicosis 1.no 2.yes(direction: _____________ )Operation scar1.no 2.yes _______________________________ Palpation: 1.soft 2. tensive (location:_____________________________ )Tenderness: 1.no 2.yes(location: _____________________ )Rebound tenderness:1.no 2.yes(location: _______________ )Fluctuation: 1.present 2.abscentSuccussion splash: 1.negative 2.positiveLiver: ______________________________________________Gallbladder:____________________ ______ M urphy sign: ___________Spleen:____________________Kidneys: _____________Abdominal mass: ______Others: _____________________________________________ Percussion:Liver dullness border: 1.normal 2.decreased 3.absentUpper hepatic border:Right Midclavicular Line _______ IntercostaShift dullness:1.negative 2.positive Ascites: _____________ degreePain on percussion in costovertebral area: 1.negative 2.positve ___ Auscultation: Bowel sounds : 1.normal 2.hyperperistalsis 3.hypoperistalsis4.absence Gurgling sound:1.no 2.yesVascular bruit 1.no 2.yes (location ___________________ ) Genital organ: 1.unexamined 2.normal 3.abnormalAnus and rectum: 1.unexamined 2.normal 3.abnormalSpine and extremities:Spine: 1.normal 2.deformity (1.kyphosis 2.lordosis 3.scoliosis)3.Tenderness(location _____________________________ )Extremities: 1.normal 2.arthremia & arthrocele (location _________________ )3.Ankylosis (location __________ )4.Aropachy: 1.no 2.yes5.Muscular atrophy (location ______________________ ) Neurological system1:.normal 2.abnormal ______________________________Important examination results before hospitalized Summary of the history: _____________________________________Initial diagnosis: ____________________________________________Recorder:Corrector:。
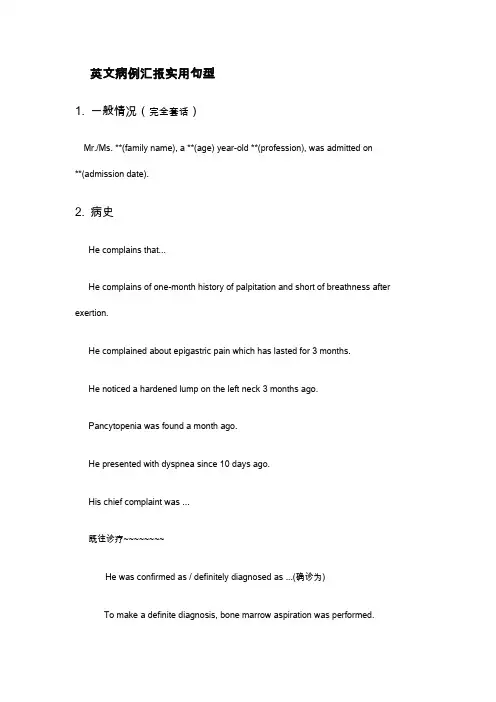
英文病例汇报实用句型1. 一般情况(完全套话)Mr./Ms. **(family name), a **(age) year-old **(profession), was admitted on**(admission date).2. 病史He complains that...He complains of one-month history of palpitation and short of breathness after exertion.He complained about epigastric pain which has lasted for 3 months.He noticed a hardened lump on the left neck 3 months ago.Pancytopenia was found a month ago.He presented with dyspnea since 10 days ago.His chief complaint was ...既往诊疗~~~~~~~~He was confirmed as / definitely diagnosed as ...(确诊为)To make a definite diagnosis, bone marrow aspiration was performed.He was suspected as...(疑似)The discomfort tended to worsening, which urged him to seek for medical care.He has been given 3 cycles of DA regimen for chemotherapy and complete remission was achieved only after the first cycle.He was given the thyroidectomy of the left lobe in local hospital.He was treated with antibiotics (details unknown), which didn't take effect as expected.The general condition is good at present.He was pain free now and hemodynamically stable.3. 查体Nothing noteworthy was found in the physical examination.There was nothing remarkable in the physical examination except for…The physical examination was otherwise normal except that…(上点小菜~~~血液科常见体征)皮肤粘膜generalized pallor,scattered petechiae,oral mucosal hematoma淋巴结enlarged lymph nodes头部yellow eyes (yellow-stained sclera)胸部tenderness in sternum,coarse breath sound, cardiac murmur, arrhythmia腹部enlargement of liver,splenomegaly4.辅助检查The laboratory findings suggested/indicated/demonstrated/showed that…Bone marrow film was performed, which confirmed the diagnosis of ALL.The results of blood routine showed that WBC count was 4,000 /cm3, while NEU count 2,500/cm3, hemoglobin 100 g/L, PLT count 100,000 /cm3.(/cm3 is pronounced as per cubic millimeter)Chest CT scan supported the diagnosis of NHL.Welcome To Download !!!欢迎您的下载,资料仅供参考!。
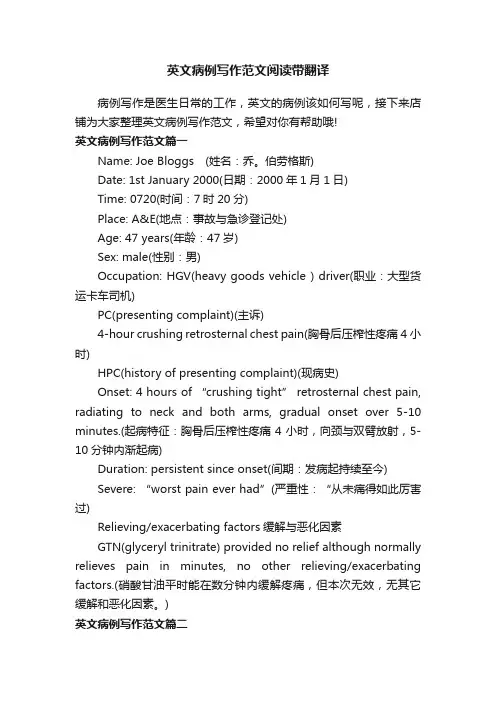
英文病例写作范文阅读带翻译病例写作是医生日常的工作,英文的病例该如何写呢,接下来店铺为大家整理英文病例写作范文,希望对你有帮助哦!英文病例写作范文篇一Name: Joe Bloggs (姓名:乔。
伯劳格斯)Date: 1st January 2000(日期:2000年1月1日)Time: 0720(时间:7时20分)Place: A&E(地点:事故与急诊登记处)Age: 47 years(年龄:47岁)Sex: male(性别:男)Occupation: HGV(heavy goods vehicle ) driver(职业:大型货运卡车司机)PC(presenting complaint)(主诉)4-hour crushing retrosternal chest pain(胸骨后压榨性疼痛4小时)HPC(history of presenting complaint)(现病史)Onset: 4 hours of “crushing tight” retrosternal chest pain, radiating to neck and both arms, gradual onset over 5-10 minutes.(起病特征:胸骨后压榨性疼痛4小时,向颈与双臂放射,5-10分钟内渐起病)Duration: persistent since onset(间期:发病起持续至今)Severe: “worst pain ever had”(严重性:“从未痛得如此厉害过)Relieving/exacerbating factors缓解与恶化因素GTN(glyceryl trinitrate) provided no relief although normally relieves pain in minutes, no other relieving/exacerbating factors.(硝酸甘油平时能在数分钟内缓解疼痛,但本次无效,无其它缓解和恶化因素。

英文病历报告作文模板Patient Information- Name: [Patient's Full Name]- Gender: [Male/Female]- Age: [Patient's age]- Date of Admission: [MM/DD/YYYY]Chief ComplaintThe patient presented with [specific symptoms/complaints] which started [duration].History of Present IllnessThe patient reported [detailed description ofsymptoms/complaints]. The symptoms worsened over the past [duration]. The patient experienced [associated symptoms] and tried [any self-medication or home remedies] but noticed no improvement. There was no history of trauma or injury.Past Medical HistoryThe patient has a history of [chronic/acute medical conditions, if any] which includes [specific conditions]. The patient has taken[previous medications/treatments] for these conditions.Social HistoryThe patient has a [specific occupation] and lives in [specific area]. The patient does [specific habits] such as smoking or drinking alcohol [frequency]. There is no significant family medical history.Physical Examination- Vital Signs:- Blood Pressure: [value] mmHg- Heart Rate: [value] bpm- Respiratory Rate: [value] bpm- Temperature: [value]C- General Appearance:The patient appears [general appearance of the patient].- Systemic Examination:- Cardiovascular: [specific findings]- Respiratory: [specific findings]- Gastrointestinal: [specific findings]- Neurological: [specific findings]- Musculoskeletal: [specific findings]Laboratory and Imaging Findings- Blood Test Results:- Complete Blood Count: [values]- Biochemical Profile: [values]- Others: [specific findings]- Imaging:- [Specific imaging tests performed]- Results: [specific findings]DiagnosisAfter evaluating the patient's medical history, physical examination, and laboratory/imaging findings, the following diagnosis was made:[Primary Diagnosis]Treatment and ManagementThe patient was started on [specific treatment plan] which includes [medications, therapies, or procedures]. The patient wasadvised to [specific instructions] and scheduled for [follow-up tests/appointments, if any].Follow-upThe patient will be followed up in [specific time frame] to assess the response to treatment and manage any complications that may arise. The patient was given contact information for any urgent concerns or changes in symptoms.Discussion and ConclusionThis case report highlights the presentation, evaluation, and management of a patient with [specific condition]. The patient's symptoms were appropriately addressed through a systematic approach involving history taking, physical examination, and laboratory/imaging investigations. The provided treatment plan aims to address the underlying cause and improve the patient's overall well-being. Continuous monitoring and follow-up will guide further management decisions.Note: This medical case report is fictional and serves as a template for educational purposes. Any resemblance to actualpatients is purely coincidental.。

Admission RecordName:* Nativity: * district, * citySex:male Race: HanAge:55 Date of admission:2020-09-07 14:30 Marital status: be married Date of record:2020-09-07 15:23 Occupation:teacher Complainer:patient himself Medical record Number: * Reliability: reliablePresent address: NO*, building*, * village,* district, *city, *provinceChief complaint: cough and sputum for more than 6 years, worsening for 2 weeksHistory of present illness: The patient complained of having paroxysmal cough and sputum 6 years ago. At that time, he was diagnosed as “COPD” in another hospital and no regular treatment was applied. Cough and sputum worsened and were accompanied by tachypnea 2 weeks ago with no inducing factors. Small amounts of white and mucous sputum were hard to cough up. Compared to daytime, tachypnea worsened in the night or when sputum can’t be cough up. The patient can’t lie flat at the night because of prominent tachypnea and prefer a high pillow. He had no fever, no chest pain, no dizziness, no diarrhea, no abdominal pain, no obvious decrease of activity tolerance. On 20*-0*-*, the patient went to *Hospital for medical consultation. CT lung imaging indicated: lesion accompanied by calcification in the superior segment, the inferior lobe of the right lung, the possibility of obsolete tuberculosis; emphysema, bullae formation and sporadic inflammation of bilateral lung; calcified lesion in the inferior lobe of the left lung; arteriosclerosis of coronary artery.Pulmonary function tests indicated:d obstructive ventilation dysfunction; bronchial dilation test was negative2.moderate decrease of diffusion function, lung volume, residual volume and the ratio of lungvolume; residual volume were normalThe patient was diagnosed as “AECOPD” and prescribed cefoxitin to anti-infection for a week, Budesonide and Formoterol to relieve bronchial muscular spasm and asthma,amb roxol to dilute sputum, and traditional Chinese medicine (specific doses were unknown).The patient was discharged from the hospital after symptoms of cough and sputum slightly relieved with a prescription of using Moxifloxacin outside the hospital for 1 week. Cough and sputum were still existing, thus the patient came to our hospital for further treatment and the outpatient department admitted him in the hospital with “COPD”. His mental status, appetite, sleep, voiding, and stool were normal. No obvious decrease or increase of weight.Past history: The patient was diagnosed as type 2 diabetes 1 years ago and take Saxagliptin (5mg po qd) without regularly monitoring the levels of blood sugar. The patient denies hepatitis, tuberculosis, malaria, hypertension, mental illness, and cardiovascular diseases. Denies surgical procedures, trauma, transfusion, food allergy and drug allergy. The history of preventive inoculation is not quite clear.Personal history: The patient was born in *district, * city and have lived in * since birth. He denies water contact in the schistosome epidemic area. Smoking 10 cigarettes a day for 20 years and have stopped for half a month. Denies excessive drinking and contact with toxics.Marital history: Married at age of 27 and have two daughters. Both the mate and daughters are healthy.Family history: Denies familial hereditary diseases.Physical ExaminationT: 36.5℃ P:77bpm R: 21 breaths/min BP:148/85mmHgGeneral condition:normally developed, well-nourished, normal facies, alert, active position, cooperation is goodSkin and mucosa: no jaundiceSuperficial lymph nodes: no enlargementHead organs: normal shape of headEyes:no edema of eyelids; no exophthalmos; eyeballs move freely; no bleeding spots of conjunctiva; no sclera jaundice; cornea clear; pupils round, symmetrical in size and acutely reactive to light.Ears: no deformity of auricle; no purulent secretion of the external canals; no tenderness over mastoidsNose: normal shape; good ventilation;no nasal ale flap; no tenderness over nasal sinus; Mouth: no cyanosis of lips; no bleeding spots of mouth mucosa; no tremor of tongue; glossy tongue in midline; no pharynx hyperemia; no enlarged tonsils seen and no suppurative excretions; Neck: supple without rigidity, symmetrical; no cervical venous distension; Hepatojugular reflux is negative; no vascular murmur; trachea in midline; no enlargement of thyroid glandChest: symmetrical; no deformity of thoraxLung:Inspection:equal breathing movement on two sidesPalpation: no difference of vocal fremitus over two sides;Percussion: resonance over both lungs;Auscultation: decreased breath sounds over both lungs; no dry or moist rales audible; no pleural friction rubsHeart:Inspection: no pericardial protuberance; Apex beat seen 0.5cm within left mid-clavicular at fifth intercostal space;Palpation: no thrill felt;Percussion: normal dullness of heart bordersAuscultation: heart rate 78bpm; rhythm regular; normal intensity of heart sounds; no murmurs or pericardial friction sound audiblePeripheral vascular sign: no water-hammer pulse; no pistol shot sound; no Duroziez’s murmur; no capillary pulsation sign; no visible pulsation of carotid arteryAbdomen:Inspection: no dilated veins; no abnormal intestinal and peristaltic waves seenPalpation: no tenderness or rebounding tenderness; abdominal wall flat and soft; liver and spleen not palpable; Murphy's sign is negativePercussion: no shifting dullness; no percussion tenderness over the liver and kidney regionAuscultation: normal bowel sounds.External genitalia: uncheckedSpine: normal spinal curvature without deformities; normal movementsExtremities: no clubbed fingers(toes); no redness and swelling of joints; no edema over both legs; no pigmentation of skins of legsNeurological system: normal muscle tone and myodynamia; normal abdominal and bicipital muscular reflex; normal patellar and heel-tap reflex; Babinski sign(-);Kerning sign(-) ; Brudzinski sign(-)Laboratory DataKey Laboratory results including CT imaging and pulmonary function test have been detailed in the part of history of present illness.Abstract*, male, 55 years old. Admitted to our hospital with the chief complaint of cough and sputum for more than 6 years, worsening for 2 weeks. Cough and sputum worsened and were accompanied by tachypnea 2 weeks ago. The patient can’t lie flat in the night because of prominent tachypnea and prefer a high pillow.Physical Examination: T: 36.5℃,P: 77bpm, R: 21 breaths per minute, BP:148/85mmHg. Decreased breath sounds over both lungs; no dry or moist rales audible.Laboratory data: CT lung imaging indicates: lesion accompanied by calcification in superior segment, inferior lobe of right lung, possibility of obsolete tuberculosis; emphysema, bullae formation and sporadic inflammation of bilateral lung; calcified lesion in inferior lobe of left lung. Pulmonary function tests indicate: mild obstructive ventilation dysfunction, bronchial dilation test was negative moderate decrease of diffusion function.Primary Diagnosis:1.AECOPD2.Type 2 Diabetes3.Primary Hypertension Doctor’s Signature:。

英文病历标准模版Patient ProfileName: Si RuihuaDepartment: ___ Power ___Sex: FemalePresent Address: Electric Power Bureau Age: 80 yearsDate of n: May 17.2003nality: Chinese XinjiangDate of Record: May 17.2003Marital Status: MarriedReliability: Reliablen: Family ___History of Allergy: None reportedChief Complaints___。
breathlessness。
and precordial pain for the last hour。
There were no precipitating factors。
and the fort could not be relieved by rest。
As a result。
she came to the hospital for help。
She did not experience syncope。
cough。
headache。
diarrhea。
or vomiting during the course of the illness。
Her appetite。
sleep。
voiding。
and stool were normal.Medical History___.______。
___ distress。
She had a heart rate of 120 beats per minute and a blood pressure of 160/90 mmHg。
Her respiratory rate was 28 breaths per minute。
and her oxygen n was 90% on room air。
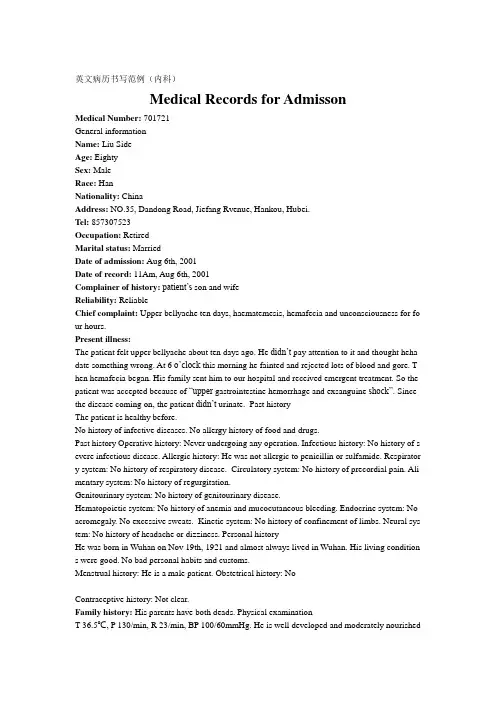
英文病历书写范例(内科)Medical Records for AdmissonMedical Number: 701721General informationName: Liu SideAge: EightySex: MaleRace: HanNationality: ChinaAddress: NO.35, Dandong Road, Jiefang Rvenue, Hankou, Hubei.Tel: 857307523Occupation: RetiredMarital status: MarriedDate of admission: Aug 6th, 2001Date of record: 11Am, Aug 6th, 2001Complainer of history:patient’s son and wifeReliability: ReliableChief complaint: Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for fo ur hours.Present illness:The patient felt upper bellyache about ten days ago. He didn’t pay attention to it and thought heha date something wrong. At 6 o’cloc k this morning he fainted and rejected lots of blood and gore. T hen hemafecia began. His family sent him to our hospital and received emergent treatment. So the patient was accepted because of “upper gastrointestine hemorrhage and exsanguine shock”. Since the disease coming on, the patient didn’t urinate. Past historyThe patient is healthy before.No history of infective diseases. No allergy history of food and drugs.Past history Operative history: Never undergoing any operation. Infectious history: No history of s evere infectious disease. Allergic history: He was not allergic to penicillin or sulfamide. Respirator y system: No history of respiratory disease. Circulatory system: No history of precordial pain. Ali mentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease.Hematopoietic system: No history of anemia and mucocutaneous bleeding. Endocrine system: No acromegaly. No excessive sweats. Kinetic system: No history of confinement of limbs. Neural sys tem: No history of headache or dizziness. Personal historyHe was born in Wuhan on Nov 19th, 1921 and almost always lived in Wuhan. His living condition s were good. No bad personal habits and customs.Menstrual history: He is a male patient. Obstetrical history: NoContraceptive history: Not clear.Family history: His parents have both deads. Physical examinationT 36.5℃, P 130/min, R 23/min, BP 100/60mmHg. He is well developed and moderately nourished.Active position. His consciousness was not clear. His face was cadaverous and the skin was not sta ined yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pi tting edema. Superficial lymph nodes were not found enlarged. HeadCranium: Hair was black and white, well distributed. No deformities. No scars. No masses. No ten derness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external au ditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nare s flaring. No tenderness in nasal sinuses. Eye: Bilateral eyelids were not swelling. No ptosis. No e ntropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or dep ressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect p upillary reactions to light were existent.Mouth: Oral mucous membrane was not smooth, and there were ulcer can be seen. Tongue was in midline. Pharynx was congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in mi dline. ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was nei ther narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities. Breast: Symmetric bilaterally.Lungs: Respiratory movement was bilaterally symmetric with the frequency of 23/min. thoracic e xpansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales. Heart: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum imp ulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardi al friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 150/min. Cardiac rhythm was not regular. No pathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal ty pe or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. T here was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular mur murs. Extremities: No articular swelling. Free movements of all limbs.Neural system: Physiological reflexes were existent without any pathological ones. Genitourinary system: Not examed. Rectum: not exanedInvestigationBlood-Rt: Hb 69g/L RBC 2.70T/L WBC 1. 1G/L PLT 120G/L History summary1. Patient was male, 80 years old2. Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.3. No special past history.4. Physical examination: T 37.5℃, P 130/min, R 23/min, BP 100/60mmHg Superficial lymph node s were not found enlarged. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill ne gative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs. No other positive signs. 5. investigation information:Blood-Rt: Hb 69g/L RBC 2.80T/L WBC 1.1G/L PLT 120G/LImpression: upper gastrointestine hemorrhage Exsanguine shock出院小结(DISCHARGE SUMMARY), ===============Department of GastroenterologyChanghai Hospital,No.174 Changhai Road Shanghai, China Phone: 86-21-25074725-803 DISCHARGE SUMMARYDA TE OF ADMISSION: October 7th, 2005 DA TE OF DISCHARGE: October 12th, 2005 ATTE NDING PHYSICIAN: Yu Bai, MD PA TIENT AGE: 18ADMITTING DIAGNOSIS:V omiting for unknown reason: acute gastroenteritis?BRIEF HISTORYA 18-year-old female with a complaint of nausea and vomiting for nearly one month who was see n at Department of Gastroenterology in Changhai Hospital, found to have acute gastroenteritis and non-atrophic gastritis. The patient was subsequently recovered and discharged soon after medicati on.REVIEW OF SYSTEMShe has had no headache, fever, chills, diarrhea, chest pain, palpitations, dyspnea, cough, hemopty sis, dysuria, hematuria or ankle edema.PAST MEDICAL HISTORYShe has had no previous surgery, accidents or childhood illness.SOCIAL HISTORY: She has no history of excessive alcohol or tobacco use.FAMIL Y HISTORYShe has no family history of cardiovascular, respiratary and gastrointestinal diseases. PHYSICAL EXAMINA TIONTemperature is 37, pulse 80, respirations 16, blood pressure 112/70. General: Plump girl in no app arent distress. HEENT: She has no scalp lesions. Her pupils are equally round and reactive to light and accommodation. Extraocular movements are intact. Sclerae are anicteric. Oropharynx is clear. There is no thyromegaly. There is no cervical or supraclvicular lymphadenopathy. Cardiovascular: Regular rate andrhythm, normal S1, S2. Chest: Clear to auscultation bilateral. Abdomen: Bowel sounds present, no hepatosplenomagaly. Extremities: There is no cyanosis, clubbing or edema. Neurologic: Cranial n erves II-XII are intact. Motor examination is 5/5 in the bilateral upper and lower extremities. Sens ory, cerebellar and gait are normal.LABORATORY DATAWhite blood cells count 5.9, hemoglobin 111g/L, hematocrit 35.4. Sodium 142, potassium 4.3, chl oride 106, CO2 25, BUN 2.6mmol/L, creatinine 57μmol/L, glucose 4.1mmol/L, Albumin 36g/L. Endoscopic ExamChronic non-atrophic gastritisHOSPITAL COURSEThe patient was admitted and placed on fluid rehydration and mineral supplement. The patient im proved, showing gradual resolution of nausea and vomiting. The patient was discharged in stable c ondition.DISCHARGE DIAGNOSIS Acute gastroenteritisChronic non-atrophic gastritisPROGNOSISGood. No medications needed after discharge. But if this patient can not get used to Chinese food, she had better return to UK as soon as possible to prevent the relapse of acute gastroenteritis. The patient is to follow up with Dr. Bai in one week. ___________________________ Yu Bai, MD D: 12/10/2005。
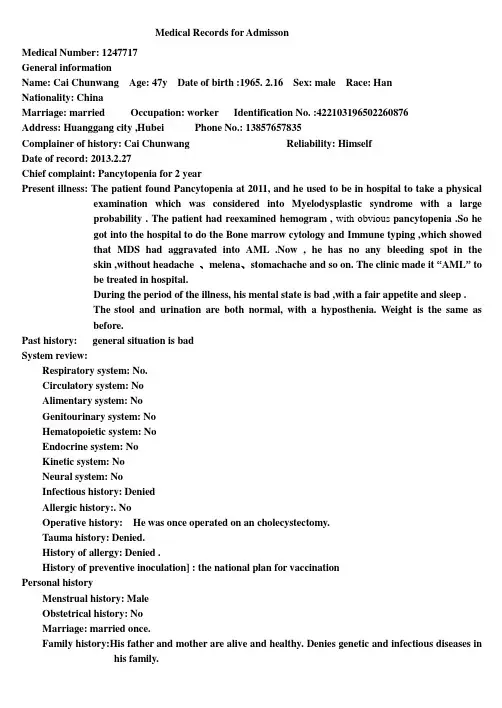
Medical Records for AdmissonMedical Number: 1247717General informationName: Cai Chunwang Age: 47y Date of birth :1965. 2.16 Sex: male Race: HanNationality: ChinaMarriage: married Occupation: worker Identification No. :422103************Address: Huanggang city ,Hubei Phone No.: 138********Complainer of history:Cai Chunwang Reliability: HimselfDate of record: 2013.2.27Chief complaint: Pancytopenia for 2 yearPresent illness: The patient found Pancytopenia at 2011, and he used to be in hospital to take a physical examination which was considered into Myelodysplastic syndrome with a largeprobability . The patient had reexamined hemogram , with obvious pancytopenia .So hegot into the hospital to do the Bone marrow cytology and Immune typing ,which showedthat MDS had aggravated into AML .Now , he has no any bleeding spot in theskin ,without headache 、melena、stomachache and so on. The clinic made it “AML” tobe treated in hospital.During the period of the illness, his mental state is bad ,with a fair appetite and sleep .The stool and urination are both normal, with a hyposthenia. Weight is the same asbefore.Past history: general situation is badSystem review:Respiratory system: No.Circulatory system: NoAlimentary system: NoGenitourinary system: NoHematopoietic system:NoEndocrine system:NoKinetic system:NoNeural system:NoInfectious history: DeniedAllergic history:. NoOperative history: He was once operated on an cholecystectomy.Tauma history: Denied.History of allergy: Denied .History of preventive inoculation] : the national plan for vaccinationPersonal historyMenstrual history:MaleObstetrical history:NoMarriage: married once.Family history:His father and mother are alive and healthy. Denies genetic and infectious diseases in his family.Physical examinationT 37℃, P95 /min, R 20 /min, BP 124/78 mmHg. He is well developed and moderately nourished. Active position. The skin was not stained yellow. Cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not found enlarged in his neck.HeadCranium: size : normal large small deformity. No coxycephaly squared skull deforming skull. No tenderness mass sunk .Ear: Auricle is normal .No excretions of external auditory canal. No Tenderness of mastoid.Nose: Shape is normal .No nosalala flap obsruction excretions nasal sinus tenderness .Eye: Eyes eyelid、eye ball、Sclera、Pupils and reaction to light are normal.Mouth: Mouth lips is normal .Opening of parotid gland duct: normal .Tongue : normal.Gums: normal .lead line tooth:regular.Tonsils: pharynx: voice: normal.Neck: No resistence.Hepatojugular reflux:(-).thyroid: normal.ChestChest wall: normalThorax : normal.Breast:normal symmetricalLungs : Inspection : movement of respiration : normal .Intercostal space :normal .Palpation : vocal fremitus : normal .pluernal friction rubs: No.Subcutaneous crepitus: No.percussion:resonance.Dusculation: breath regular.Breath sound: normal.Rale: No.Vocal conduction:norma .Plueral friction rubs: No.Heart:Inspection:bulging in precordial region : No.apex impulse:normal. position: normal .Palpation: apex impulse : normal .Thrills :No.Percardial friction rub s:NO.Percussion:relative cardiac outline: normal.Ausculation: heart rate 95bpm/min ,rhythm:regular.Heart sound:S1 normal.S2 normal.S3 No. S4 no. Extra heartsound No. Opening snap others murmurs: N.Pericardial friction rubs no. Peripheral vessals:normal.Abdomen:Inspection: shape normal .Abdominal respiration: existence .Umbilicus: normal protruding excretions others: NO.Palpation: soft.Tenderness: NO.Mass NO.li ver:can’t be touched.gallbladder: can’t be touched.tenderness No.spleen: can’t be touched.Kideny:can’t betouched.tenderness mobility tenderness of ureters: No.Percussion: borders of liver dull:existence .pper borders of liver on right midclavicular line intercostal space shifting dullnessNo. tenderness in renal region No.Ausculation : borhorygmus normal .Gurgling No.vessalbruits No.Extremities: Spine : normal.Spinous process :no.Mobility : normal. Extremeties: normal.Neural system:not found any abnormality.Genitourinary system: not examined.Rectum:not examinedHistory summary1.General information: Cai Chunwang ,male ,47y.2.Chief complaint: Pancytopenia for 2 year.3. past history: general situation is bad, Infectious history: Denied. Allergic history:. No.Operative history:He was once operated on an cholecystectomy. Tauma history: Denied. History of allergy:Denied . Historyof preventive inoculation] : the national plan for vaccination4. Physical examination: T 37℃, P95 /min, R 20 /min, BP 124/78 mmHg. his mental state is bad.Superficial lymph nodes were not found enlarged in his neck. heart rate 95 bpm/min ,rhythm:regular.Heart sound:S1 normal. S2 normal. S3 No. S4 no. shape normal . Abdominal respiration: existence .Umbilicus: normal protruding excretions others: NO. Palpation: soft. Tenderness: NO. Mass NO.liver:can’t be touched. gallbladder: can’t be touched. tenderness No. spleen: can’t be touched.Kideny:can’t be touched. tenderness mobility tenderness of ureters: No. Percussion: borders of liver dull: existence . pper borders of liver on right midclavicular line intercostal space shifting dullness No.tenderness in renal region No. Ausculation : borhorygmus normal . Gurgling No. vessal bruits No.movement of respiration : normal . Intercostal space :normal . Palpation : vocal fremitus : normal .pluernal friction rubs: No. Subcutaneous crepitus: No. percussion: resonance. Dusculation: breath regular. Breath sound: normal. Rale: No. Vocal conduction: norma .5.Specialist case:serious anemia. The skin was not stained yellow. Cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not found enlarged in his neck.No tenderness of sternum. Ausculation of the heart and lung has not obvious abnormality. Abdomen is soft . Tenderness: NO. Mass NO. liver:can’t be touched. gallbladder: can’t be touched. tenderness No. spleen: can’t be touched. Extremeties are normal .6 . investigation information: one medical record of 2013 year.Impression: AMLSignature: Huang QiulanDate: 2013.2.27。
医学英语病历写作范文Chief Complaint: Left leg pain with recent fall.History of Present Illness: The patient is a 65-year-old male who presents to the emergency department with a chief complaint of left leg pain. He states that he fell down a flight of stairs approximately 3 hours prior to presentation. He reports that he is in moderate to severe pain, which is localized to his left lower extremity. He denies any associated numbness or tingling. He has no prior history of leg pain or injury.Past Medical History: The patient has a history of hypertension, which is well-controlled with medication. He has no other significant medical history.Social History: The patient is married and has two children. He is a retired construction worker. He smokes one pack of cigarettes per day and drinks alcohol socially.Family History: The patient's father has a history of coronary artery disease. His mother has a history of Alzheimer's disease.Physical Examination:Vital signs: Blood pressure 140/80 mmHg, heart rate 80 bpm, respiratory rate 18 breaths per minute, temperature 98.6°F (37°C).General: The patient is in moderate distress due to pain. He is alert and oriented to person, place, and time.HEENT: Normocephalic and atraumatic. Pupils are equal and reactive to light. Extraocular movements are intact. No conjunctival injection or discharge. Tympanic membranes are intact and mobile.Neck: Supple with full range of motion. No masses or tenderness.Chest: Auscultation reveals clear breath soundsbilaterally. No wheezes, rales, or rhonchi.Cardiovascular: Regular rate and rhythm. No murmurs, rubs, or gallops.Abdomen: Soft and non-tender. No masses or organomegaly.Extremities: Left lower extremity: Examination reveals swelling and tenderness of the left knee. There is a palpable step-off deformity of the lateral aspect of theleft knee. Active and passive range of motion is limiteddue to pain. Distal pulses are palpable and capillaryrefill is brisk. Sensation is intact. Right lower extremity: Examination reveals no abnormalities.Neurological Examination:Mental status: Alert and oriented to person, place,and time. No deficits in attention, memory, or language.Cranial nerves: No deficits.Motor: Strength is 5/5 in both upper and lower extremities. No atrophy or fasciculations.Sensory: Sensation is intact to light touch, pinprick, and temperature in all four extremities.Diagnostic Studies:X-ray of the left knee: The X-ray shows a displaced lateral tibial plateau fracture.Assessment:Left knee pain.Displaced lateral tibial plateau fracture.Plan:The patient will be admitted to the hospital for further evaluation and treatment.He will be placed in a knee immobilizer and will be started on pain medication.Orthopedic surgery will be consulted for further management.。
Union Hospital affiliated to Huazhong University of Science and TechnologyAdmission Record 0000337023Department: Respiratory Medicine Area: J17 Respiratory Medicine Bed No. 109031 Case No. 1565825Name: Hou Deguang Gender: Male Date of Birth:15/9/ 1936 Age:78 Nationality: ChinaID No. 42021 Ethnicity: Han Occupation: other Marital status: MarriedAddress: Nanchong,Sichuan Tel No.Source of History: Patient herself Reliability: ReliableAdmission Date & Time: 4/11/2021 14:36Chief Complaint: Found pleural effusion for about 2 months.Present Illness: The patient received the chest CT scan in the Wuhan Traditional Medicine Hospital two months ago and found right-side pleural effusion, right-sidepulmonary atelectasis. After that, he was hospitalized in the EndocrinologyDept of our hospital for poor management of blood glucose level. On thisadmission, He received the thoracocentesis, and the laboratory examinationresults indicated the large possibility of tuberculous pleural effusion. Nospecial treatment was given at that time. The patient was aware of a sense ofpolypnea after long walk, without cough, expectoration, night sweats, chestdistress, thoracalgia, wheeze, dyspnea and can lie down to sleep at night. Thereturn-visit in the clinic at October 13th showed that there were a few pleuraleffusion on the right side and is hard to be localized. Now the patient came toour hospital for further treatment and was admitted as “Pleural effusionorigin unknown〞.Since the onset of the disease, the patient’s sp irit, appetite and sleep arenormal. Nocturia for 1 time per night. Stool are as usual. No obvious weightand physical strength change.Past History: General Health Status: Relatively bad; Respiratory Syste m: Chronic bronchitis for about 10 years; Circulatory System: Hypertension for about 20years, highest reached 180/95mmHg, took Amlodipine orally 5mg qd, BP managementis good. Diagnosed of coronary heart disease in 2007, underwentintracoronary stent implantation in 2021, 3 stents were implanted; DigestiveSystems: None; Urinary System: Benign prostatic hyperplasia for about 5 years,Diabetic nephropathy for 3 years; Hematologic System: Thrombocytopenia for 2years; Endocrine System: None. Nervous System: Lacunar infarction in 2021;Motor System: None; Infection History: No infection of hepatitis and TB. Others:None special; Preventive Inoculation: In accordance with the stateplan;Operation History:underwent intracoronary stent implantation in 2021, 3stents was implantated; Blood Transfusion History:None; Traumatic History:None; Allergic History: None;Personal History: Habitual Residence: Hubei; Residential Environment: No exposure history to toxic substances and infected water; Travelling History: None; Smoking History:Smoking for about 40 years, 3 cigarettes per day. Quit smoking in 2021;Drinking History: Drinking for 40 years, 150g-350g per day, Quit drinking in2021;Marital History: Married,Menstrual History: MaleFamily History:Father is deceased, mother is deceased. No other infective and hereditary diseases.Physical ExaminationVital Signs: T:℃. P:86 bpm, regular. R: 20min, regular. BP: 132/74 mmHg. Height: 164cm.Weight: 64kg. Expression: Normal. Development: Well. Nutritional status: Fairly.Consciousness: Conscious. Spirit: Well. Gait: Normal. Position: Active.Coordination with Examination: Cooperative.Skin and Lymph Nodes:No jaundice. Some scattered scratch in hands and abdomen, No subcutaneous bleeding, edema, nodules or unusual pigmentation. Liverpalm(-). Spider angioma(-). No swelling of general superficial lymphnodes.HEENT(Head, Eye, Ear, Nose, Throat): Normal skull. No baldness, no scars. Eyes: No ptosis.Conjuctiva normal. The pupils are round, symmetric and responsive to lightand accommodation is normal. Ears: Externally normal. Canals clear. Drumsnormal. Noses: No abnormalities noted. Month and Throat: lips red, tongue red,no swelling of tonsils.Neck: Motion free. Thyroid is not enlarged. No abnormal pulsations. Trachea in middle. Carotid: Pulse is normal. Hepatojugular reflux sign(-). Vascular bruit: None.Chest and Lung:Normal contour. Breast normal. Inspection: respiratory movement symmetric and regular. Palpation: Normal and symmetric. No pleural friction fremitus. Percussion: both sides resonance. Auscultation: right-side breath sounds weaken, left-side is normal. No moist or dry rales. No pleural friction rubs.Heart:No protrusion of precordium. Normal apical impulse. No thrill. No enlarged cardiac dullness border. Heart rate: 88bpm, rhythm normal. No abnormal and extra cardiac sounds or cardiac murmurs. No peripheral vascular signs.Abdomen:Flat abdomen. No gastric or intestinal pattern. No visible peristalsis. Normal bowel sound. No rigidity. No mass palpable. No tenderness and rebound tenderness. Liver and spleen are not palpable. Kidneys are not palpable. No percussion tenderness over kidney regions. No shifting dullness.Rectum: Normal anus and perineum.Genitourinary System: Normal.Neural System: Normal.Extremities: No joint disease. Muscle strength normal. Pathological reflex (-).Specialty Examination: Right-side breath sounds weaken, left side normal. No moist or dry rales, No swelling of general superficial lymph nodes. No edema inneither lower extremities.Accessory Examination:Discharge record of Endocrinology Dept. of our hospital at September 2021; Clinic examination at October 13th: a few pleural effusion on theright side and is hard to be localized.History summary: 1. Hou Deguang, male, 78 yr.2. Admitted for 〞Found plaural effusion for about 2 months〞.3. T:℃. P:86 bpm, regular. R: 20min, regular. BP: 132/74 mmHg.Expression: Normal. Spirit clear. Cardiac sounds normal, HR: 72 bpm, rhythmnormal, No abnormal and extra cardiac sounds or cardiac murmurs. Right-side breathsounds weaken, left side normal. No moist or dry rales, no pleural friction rubs.Flat abdomen. No rigidity.4. Special examination:Trachea in middle. Contour symmetric.Respiratory movement regular. Right-side breath sounds weaken, left side normal. Nomoist or dry rales, no pleural friction rubs.5. Accessory Examination: Discharge record of Endocrinology Dept of ourhospital at September 2021; Clinic examination at October 13th: a few pleuraleffusion on the right side and is hard to be localized.6. Past history: Respiratory Syste m: Chronic bronchitis for about 10years; Circulatory System: Hypertension for about 20 years, highest reached180/95mmHg, took Amlodipine orally 5mg qd, BP management is good. Diagnosed ofcoronary heart disease in 2007, underwent intracoronary stent implantation in2021, 3 stents was implantated; Digestive Systems: None; Urinary System: Benignprostatic hyperplasia for about 5 years, Diabetic nephropathy for 3 years;Hematologic System: Thrombocytopenia for 2 years; Endocrine System: None.Nervous System: Lacunar infarction in 2021; Motor System: None;InfectionHistory: No infection of hepatitis and TB. Others: None special; PreventiveInoculation: In accordance with the stateplan; Operation History:underwentintracoronary stent implantation in 2021, 3 stents was implantated; BloodTransfusion History: None; Traumatic History: None; Allergic History: None; Impression: 1. Right-side pleural effusion origin unknown: TB? Tumor?2. II diabetes mellitus, Diabetic nephropathy3. Hypertension III, high risk4. Coronary heart disease, post-intracoronary stent implantation5. Lacunar infarction6. Thrombocytopenia7. Benign prostatic hyperplasiaRecorder: Cheng LongDate & Time: 4/11/2021 16:14Checker: Xu JuanjuanDate & Time: 5/11/2021 10:22。
英语病例报告范文I am writing to provide a case report of a patient who presented with symptoms of chest pain and shortness of breath. The patient, a 55-year-old man, arrived at the emergency department complaining of sudden onset chest pain that radiated to his left arm. 本文将介绍一位55岁男性患者的病例报告,该患者出现胸痛和呼吸困难症状。
这位患者突然出现胸痛,疼痛向左臂放射。
Upon arrival, the patient was noted to be diaphoretic and tachypneic, with a blood pressure of 150/90 mmHg and a heart rate of 110 beats per minute. Further assessment revealed he had a history of hypertension and smoking. High-sensitivity troponin levels were elevated, indicating a possible myocardial infarction. 到达医院后,患者被发现出现出汗和呼吸急促的症状,血压为150/90mmHg,心率为每分钟110次。
进一步评估显示他有高血压和吸烟史。
高敏肌钙蛋白水平升高,提示可能发生心肌梗死。
The patient was immediately started on oxygen therapy and given aspirin and nitroglycerin for symptom relief. An ECG showed ST-segment elevations in leads II, III, and aVF, suggestive of an inferiormyocardial infarction. He was promptly taken to the catheterization lab for emergent angiography. 患者立即开始吸氧疗法,并服用阿司匹林和硝化甘油缓解症状。
CASEMedical Number: 682786General informationName: Wang RunzhenAge: Forty threeSex: FemaleRace: HanOccupation: TeacherNationality: ChinaMarital status: MarriedAddress: NO.38, Hangkong Road, Jiefang Rvenue, Hankou, Hubei. Tel: 82422500Date of admission: Jan 11st, 2001Date of record: 11Am, Jan 11st, 2001Complainer of history: the patient herselfReliability: ReliableChief complaint: Right breast mass found for more than half a month.Present illness: Half a month ago, the patient suddenly felt pain in her right chest when she put up her hand. After touching it, she found a mass in her right breast, but no tendness, and the patient didn’t pay attention it. Then the pain became more and more serious, so the patient went to tumour hospital and received a pathology centesis. Her diagnosis was breast cancer. Then she came to our hospital and asked for an operation.Since onset, her appetite was good, and both her spiritedness and physical energy are normal. Defecation and urination are normal, too.Past historyOperative history: Never undergoing any operation.Infectious history: No history of severe infectious disease.Allergic history: She was not allergic to penicillin or sulfamide.Respiratory system: No history of respiratory disease.Circulatory system: No history of precordial pain.Alimentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease.Hematopoietic system: No history of anemia and mucocutaneous bleeding.Endocrine system: No acromegaly. No excessive sweats.Kinetic system: No history of confinement of limbs.Neural system: No history of headache or dizziness.Personal historyShe was born in Wuhan on Nov 19th, 1957 and almost always lived in Wuhan. She graduated from senior high school. Her living conditions were good. No bad personal habits and customs.Menstrual history: The first time when she was 14. Lasting 3 to 4 days every times and its cycle is about 30 days.Obstetrical history: Pregnacy 3 times, once nature production, abortion twice.Contraceptive history: Not clear.Family history: His parents have both died.Physical examinationT 36.4℃, P 80/min, R 20/min, BP 90/60mmHg. She is well developed and moderately nourished. Active position. The skin was not stained yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not enlarged.HeadCranium: Hair was black and well distributed. No deformities. No scars. No masses. No tenderness. Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external auditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nares flaring. No tenderness in nasal sinuses.Eye: Bilateral eyelids were not swelling. No ptosis. No entropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or depressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect pupillary reactions to light were existent.Mouth: Oral mucous membrane was smooth, and of no ulcer or erosion. Tongue was in midline. Pharynx was not congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in midline. ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was neither narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities.Breast: Symmetric bilaterally. Neither nipples nor skin were retracted. Elasticity was fine.Lungs: Respiratory movement was bilaterally symmetric with the frequency of 20/min. Thoracic expansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales.Heart: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum impulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardial friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 80/min. Cardiac rhythm was regular. No pathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. There was not tenderness and rebound tenderness on abdomen or renal region. Liver was not reached. Spleen was not enlarged. No masses. Fluidthrill negative. Shifting dullnessnegative. Borhorygmus 5/min. No vascular murmurs.Extremities: No articular swelling. Free movements of all limbs.Neural system: Physiological reflexes were existent without any pathological ones.Genitourinary system: Not examed.Rectum: not exanedInvestigationNo.Professional ExaminationThere are a about 3*3*2 cm mass in outer-up field of her right breast. It is hard but no tendness. It can be moved and its surface is smooth. The skin of her breast is normal. Corresponding superficial lymph nodes don’t enlarge.History summary1. Patient was a teacher, female, 43 years old.2. Right breast mass found for more than half a month.3. No special past history.4. Physical examination showed no abnormity in lung, heart and abdoman. Information about her breast can be seen above.5. Shorting of investigation information.Impression: Breast cancer (right)Signature: xxx。
英语写病历作文模板 Patient History Template。
英文回答:General Information。
Name:Age:Gender:Occupation:Address:Phone number:Emergency contact:Medical History。
Past medical history: List any previous illnesses, surgeries, hospitalizations, or accidents.Family medical history: Note any history of chronic diseases, such as heart disease, cancer, or diabetes, in the patient's family.Allergies: List any known allergies to medications, foods, or other substances.Medications: List all current medications, including prescription drugs, over-the-counter medications, and herbal supplements.Social history: Discuss the patient's lifestyle, including diet, exercise, smoking, alcohol use, and drug use.Present Illness。
Chief complaint: State the patient's primary reasonfor seeking medical attention.History of present illness: Describe the onset, duration, severity, and progression of the patient's symptoms.Physical Examination。
临床案例模板英语作文英文回答:Clinical Case Template。
Demographic Information:Name: John Doe。
Age: 55。
Gender: Male。
Occupation: Software Engineer。
Chief Complaint:Intermittent chest pain for the past 2 weeks。
History of Present Illness:The patient is a 55-year-old male who presents with a 2-week history of intermittent chest pain. The pain is described as a squeezing sensation that radiates to theleft arm. It occurs with exertion and is relieved by rest. The patient also reports shortness of breath and fatigue.The patient has no history of coronary artery disease, but he does have a history of hypertension and hyperlipidemia. He is a current smoker and drinks alcohol socially.Past Medical History:Hypertension。
Hyperlipidemia。
Social History:Current smoker。
Drinks alcohol socially。
Family History:Father died of myocardial infarction at age 60。