内科英文病历材料模板
- 格式:doc
- 大小:77.02 KB
- 文档页数:8
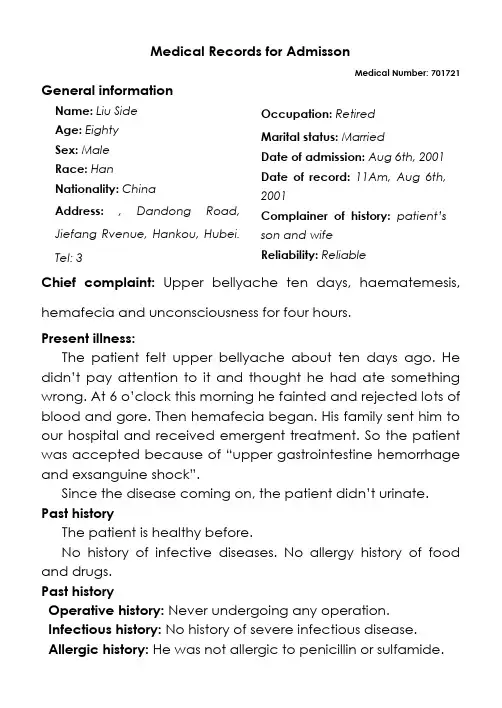
Medical Records for AdmissonMedical Number: 701721 General informationName:Liu SideAge: EightySex: MaleRace:HanNationality:ChinaAddress: , Dandong Road, Jiefang Rvenue, Hankou, Hubei. Tel: 3 Occupation: RetiredMarital status: MarriedDate of admission: Aug 6th, 2001 Date of record: 11Am, Aug 6th, 2001Complainer of history: patient’s son and wifeReliability: ReliableChief complaint: Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.Present illness:The patient felt upper bellyache about ten days ago. He didn’t pay attention to it and thought he had ate something wrong. At 6 o’clock this morning he fainted and rejected lo ts of blood and gore. Then hemafecia began. His family sent him to our hospital and received emergent treatment. So the patient was accepted because of “upper gastrointestine hemorrhage and exsanguine shock”.Since the disease coming on, the patient did n’t urinate. Past historyThe patient is healthy before.No history of infective diseases. No allergy history of food and drugs.Past historyOperative history: Never undergoing any operation. Infectious history: No history of severe infectious disease. Allergic history: He was not allergic to penicillin or sulfamide.Respiratory system: No history of respiratory disease. Circulatory system: No history of precordial pain.Alimentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease. Hematopoietic system:No history of anemia and mucocutaneous bleeding.Endocrine system: No acromegaly. No excessive sweats. Kinetic system: No history of confinement of limbs.Neural system: No history of headache or dizziness.Personal historyHe was born in Wuhan on Nov 19th, 1921 and almost always lived in Wuhan. His living conditions were good. No bad personal habits and customs.Menstrual history: He is a male patient.Obstetrical history: NoContraceptive history: Not clear.Family history: His parents have both deads.Physical examinationT 36.5℃, P 130/min, R 23/min, BP 100/60mmHg. He is well developed and moderately nourished. Active position. His consciousness was not clear. His face was cadaverous and the skin was not stained yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not found enlarged.HeadCranium:Hair was black and white, well distributed. No deformities. No scars. No masses. No tenderness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external auditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi.Septum nasi was in midline. No nares flaring. No tenderness in nasal sinuses.Eye:Bilateral eyelids were not swelling. No ptosis. No entropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or depressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect pupillary reactions to light were existent.Mouth: Oral mucous membrane was not smooth, and there were ulcer can be seen. Tongue was in midline. Pharynx was congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in midline.ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was neither narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities.Breast: Symmetric bilaterally.Lungs:Respiratory movement was bilaterally symmetric with the frequency of 23/min. thoracic expansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales.Heart:No bulge and no abnormal impulse or thrills in precordial area. The point of maximum impulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardial friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 150/min. Cardiac rhythm was not regular. No pathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominalwall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs.Extremities: No articular swelling. Free movements of all limbs. Neural system: Physiological reflexes were existent without any pathological ones.Genitourinary system: Not examed.Rectum: not exanedInvestigationBlood-Rt: Hb 69g/L RBC L WBC 1. 1G/L PLT 120G/LHistory summary1.P atient was male, 80 years old2.U pper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.3.N o special past history.4.P hysical examination: T 37.5℃, P 130/min, R 23/min, BP 100/60mmHg Superficial lymph nodes were not found enlarged. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs. No other positive signs.5.i nvestigation information:Blood-Rt: Hb 69g/L RBC L WBC 1.1G/L PLT 120G/LImpression: upper gastrointestine hemorrhageExsanguine shockSignature: He Lin (95-10033)。
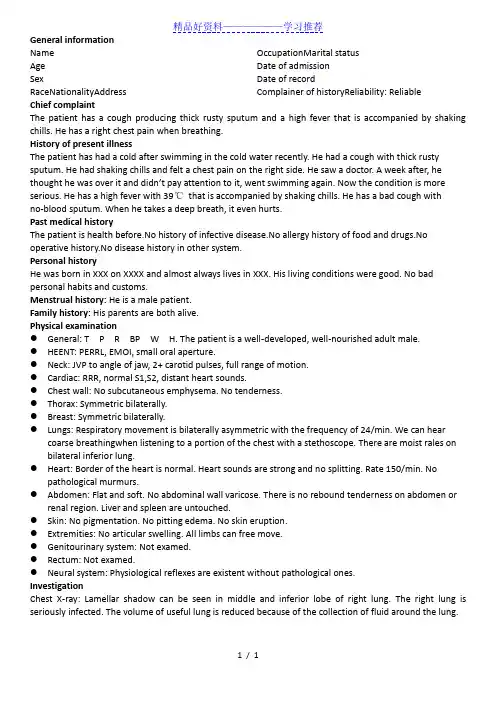
精品好资料——————学习推荐1 / 1 General informationName Age Sex RaceNationalityAddress OccupationMarital statusDate of admissionDate of recordComplainer of historyReliability: Reliable Chief complaintThe patient has a cough producing thick rusty sputum and a high fever that is accompanied by shaking chills. He has a right chest pain when breathing.History of present illnessThe patient has had a cold after swimming in the cold water recently. He had a cough with thick rusty sputum. He had shaking chills and felt a chest pain on the right side. He saw a doctor. A week after, he thought he was over it and didn’t pay attention to it, went swimming again. Now the condition is more serious. He has a high fever with 39℃ that is accompanied by shaking chills. He has a bad cough with no -blood sputum. When he takes a deep breath, it even hurts.Past medical historyThe patient is health before.No history of infective disease.No allergy history of food and drugs.No operative history.No disease history in other system.Personal historyHe was born in XXX on XXXX and almost always lives in XXX. His living conditions were good. No bad personal habits and customs.Menstrual history: He is a male patient.Family history: His parents are both alive.Physical examination● General: T P R BP W H. The patient is a well -developed, well -nourished adult male. ● HEENT: PERRL, EMOI, small oral aperture.● Neck: JVP to angle of jaw, 2+ carotid pulses, full range of motion.● Cardiac: RRR, normal S1,S2, distant heart sounds.● Chest wall: No subcutaneous emphysema. No tenderness.● Thorax: Symmetric bilaterally.● Breast: Symmetric bilaterally.● Lungs: Respiratory movement is bilaterally asymmetric with the frequency of 24/min. We can hearcoarse breathingwhen listening to a portion of the chest with a stethoscope. There are moist rales on bilateral inferior lung.● Heart: Border of the heart is normal. Heart sounds are strong and no splitting. Rate 150/min. Nopathological murmurs.● Abdomen: Flat and soft. No abdominal wall varicose. There is no rebound tenderness on abdomen orrenal region. Liver and spleen are untouched.● Skin: No pigmentation. No pitting edema. No skin eruption.● Extremities: No articular swelling. All limbs can free move.● Genitourinary system: Not examed.● Rectum: Not examed.● Neural system: Physiological reflexes are existent without pathological ones.InvestigationChest X -ray: Lamellar shadow can be seen in middle and inferior lobe of right lung. The right lung is seriously infected. The volume of useful lung is reduced because of the collection of fluid around the lung.。
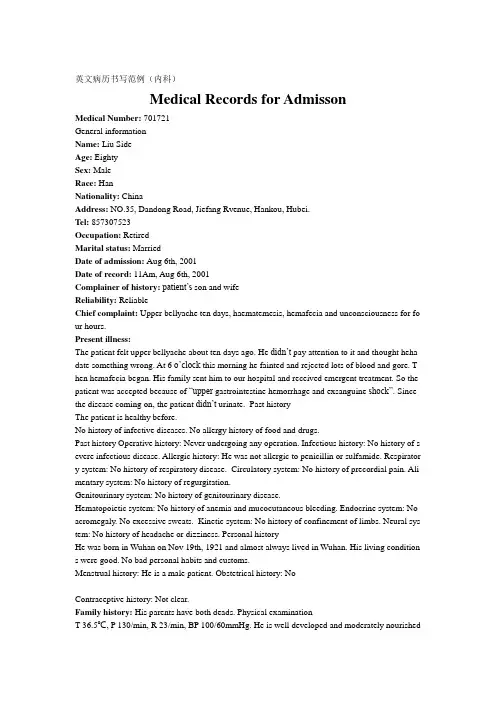
英文病历书写范例(内科)Medical Records for AdmissonMedical Number: 701721General informationName: Liu SideAge: EightySex: MaleRace: HanNationality: ChinaAddress: NO.35, Dandong Road, Jiefang Rvenue, Hankou, Hubei.Tel: 857307523Occupation: RetiredMarital status: MarriedDate of admission: Aug 6th, 2001Date of record: 11Am, Aug 6th, 2001Complainer of history:patient’s son and wifeReliability: ReliableChief complaint: Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for fo ur hours.Present illness:The patient felt upper bellyache about ten days ago. He didn’t pay attention to it and thought heha date something wrong. At 6 o’cloc k this morning he fainted and rejected lots of blood and gore. T hen hemafecia began. His family sent him to our hospital and received emergent treatment. So the patient was accepted because of “upper gastrointestine hemorrhage and exsanguine shock”. Since the disease coming on, the patient didn’t urinate. Past historyThe patient is healthy before.No history of infective diseases. No allergy history of food and drugs.Past history Operative history: Never undergoing any operation. Infectious history: No history of s evere infectious disease. Allergic history: He was not allergic to penicillin or sulfamide. Respirator y system: No history of respiratory disease. Circulatory system: No history of precordial pain. Ali mentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease.Hematopoietic system: No history of anemia and mucocutaneous bleeding. Endocrine system: No acromegaly. No excessive sweats. Kinetic system: No history of confinement of limbs. Neural sys tem: No history of headache or dizziness. Personal historyHe was born in Wuhan on Nov 19th, 1921 and almost always lived in Wuhan. His living condition s were good. No bad personal habits and customs.Menstrual history: He is a male patient. Obstetrical history: NoContraceptive history: Not clear.Family history: His parents have both deads. Physical examinationT 36.5℃, P 130/min, R 23/min, BP 100/60mmHg. He is well developed and moderately nourished.Active position. His consciousness was not clear. His face was cadaverous and the skin was not sta ined yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pi tting edema. Superficial lymph nodes were not found enlarged. HeadCranium: Hair was black and white, well distributed. No deformities. No scars. No masses. No ten derness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external au ditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nare s flaring. No tenderness in nasal sinuses. Eye: Bilateral eyelids were not swelling. No ptosis. No e ntropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or dep ressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect p upillary reactions to light were existent.Mouth: Oral mucous membrane was not smooth, and there were ulcer can be seen. Tongue was in midline. Pharynx was congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in mi dline. ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was nei ther narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities. Breast: Symmetric bilaterally.Lungs: Respiratory movement was bilaterally symmetric with the frequency of 23/min. thoracic e xpansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales. Heart: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum imp ulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardi al friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 150/min. Cardiac rhythm was not regular. No pathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal ty pe or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. T here was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular mur murs. Extremities: No articular swelling. Free movements of all limbs.Neural system: Physiological reflexes were existent without any pathological ones. Genitourinary system: Not examed. Rectum: not exanedInvestigationBlood-Rt: Hb 69g/L RBC 2.70T/L WBC 1. 1G/L PLT 120G/L History summary1. Patient was male, 80 years old2. Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.3. No special past history.4. Physical examination: T 37.5℃, P 130/min, R 23/min, BP 100/60mmHg Superficial lymph node s were not found enlarged. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill ne gative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs. No other positive signs. 5. investigation information:Blood-Rt: Hb 69g/L RBC 2.80T/L WBC 1.1G/L PLT 120G/LImpression: upper gastrointestine hemorrhage Exsanguine shock出院小结(DISCHARGE SUMMARY), ===============Department of GastroenterologyChanghai Hospital,No.174 Changhai Road Shanghai, China Phone: 86-21-25074725-803 DISCHARGE SUMMARYDA TE OF ADMISSION: October 7th, 2005 DA TE OF DISCHARGE: October 12th, 2005 ATTE NDING PHYSICIAN: Yu Bai, MD PA TIENT AGE: 18ADMITTING DIAGNOSIS:V omiting for unknown reason: acute gastroenteritis?BRIEF HISTORYA 18-year-old female with a complaint of nausea and vomiting for nearly one month who was see n at Department of Gastroenterology in Changhai Hospital, found to have acute gastroenteritis and non-atrophic gastritis. The patient was subsequently recovered and discharged soon after medicati on.REVIEW OF SYSTEMShe has had no headache, fever, chills, diarrhea, chest pain, palpitations, dyspnea, cough, hemopty sis, dysuria, hematuria or ankle edema.PAST MEDICAL HISTORYShe has had no previous surgery, accidents or childhood illness.SOCIAL HISTORY: She has no history of excessive alcohol or tobacco use.FAMIL Y HISTORYShe has no family history of cardiovascular, respiratary and gastrointestinal diseases. PHYSICAL EXAMINA TIONTemperature is 37, pulse 80, respirations 16, blood pressure 112/70. General: Plump girl in no app arent distress. HEENT: She has no scalp lesions. Her pupils are equally round and reactive to light and accommodation. Extraocular movements are intact. Sclerae are anicteric. Oropharynx is clear. There is no thyromegaly. There is no cervical or supraclvicular lymphadenopathy. Cardiovascular: Regular rate andrhythm, normal S1, S2. Chest: Clear to auscultation bilateral. Abdomen: Bowel sounds present, no hepatosplenomagaly. Extremities: There is no cyanosis, clubbing or edema. Neurologic: Cranial n erves II-XII are intact. Motor examination is 5/5 in the bilateral upper and lower extremities. Sens ory, cerebellar and gait are normal.LABORATORY DATAWhite blood cells count 5.9, hemoglobin 111g/L, hematocrit 35.4. Sodium 142, potassium 4.3, chl oride 106, CO2 25, BUN 2.6mmol/L, creatinine 57μmol/L, glucose 4.1mmol/L, Albumin 36g/L. Endoscopic ExamChronic non-atrophic gastritisHOSPITAL COURSEThe patient was admitted and placed on fluid rehydration and mineral supplement. The patient im proved, showing gradual resolution of nausea and vomiting. The patient was discharged in stable c ondition.DISCHARGE DIAGNOSIS Acute gastroenteritisChronic non-atrophic gastritisPROGNOSISGood. No medications needed after discharge. But if this patient can not get used to Chinese food, she had better return to UK as soon as possible to prevent the relapse of acute gastroenteritis. The patient is to follow up with Dr. Bai in one week. ___________________________ Yu Bai, MD D: 12/10/2005。

英文病历报告作文模板Patient Information- Name: [Patient's Full Name]- Gender: [Male/Female]- Age: [Patient's age]- Date of Admission: [MM/DD/YYYY]Chief ComplaintThe patient presented with [specific symptoms/complaints] which started [duration].History of Present IllnessThe patient reported [detailed description ofsymptoms/complaints]. The symptoms worsened over the past [duration]. The patient experienced [associated symptoms] and tried [any self-medication or home remedies] but noticed no improvement. There was no history of trauma or injury.Past Medical HistoryThe patient has a history of [chronic/acute medical conditions, if any] which includes [specific conditions]. The patient has taken[previous medications/treatments] for these conditions.Social HistoryThe patient has a [specific occupation] and lives in [specific area]. The patient does [specific habits] such as smoking or drinking alcohol [frequency]. There is no significant family medical history.Physical Examination- Vital Signs:- Blood Pressure: [value] mmHg- Heart Rate: [value] bpm- Respiratory Rate: [value] bpm- Temperature: [value]C- General Appearance:The patient appears [general appearance of the patient].- Systemic Examination:- Cardiovascular: [specific findings]- Respiratory: [specific findings]- Gastrointestinal: [specific findings]- Neurological: [specific findings]- Musculoskeletal: [specific findings]Laboratory and Imaging Findings- Blood Test Results:- Complete Blood Count: [values]- Biochemical Profile: [values]- Others: [specific findings]- Imaging:- [Specific imaging tests performed]- Results: [specific findings]DiagnosisAfter evaluating the patient's medical history, physical examination, and laboratory/imaging findings, the following diagnosis was made:[Primary Diagnosis]Treatment and ManagementThe patient was started on [specific treatment plan] which includes [medications, therapies, or procedures]. The patient wasadvised to [specific instructions] and scheduled for [follow-up tests/appointments, if any].Follow-upThe patient will be followed up in [specific time frame] to assess the response to treatment and manage any complications that may arise. The patient was given contact information for any urgent concerns or changes in symptoms.Discussion and ConclusionThis case report highlights the presentation, evaluation, and management of a patient with [specific condition]. The patient's symptoms were appropriately addressed through a systematic approach involving history taking, physical examination, and laboratory/imaging investigations. The provided treatment plan aims to address the underlying cause and improve the patient's overall well-being. Continuous monitoring and follow-up will guide further management decisions.Note: This medical case report is fictional and serves as a template for educational purposes. Any resemblance to actualpatients is purely coincidental.。
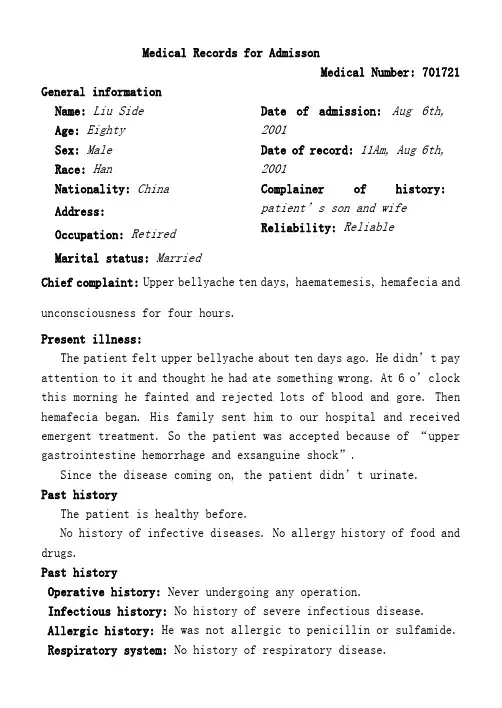
Medical Records for AdmissonMedical Number: 701721 General informationName:Liu SideAge: EightySex: MaleRace:HanNationality:China Address: Occupation: Retired Marital status: Married Date of admission:Aug 6th, 2001Date of record: 11Am, Aug 6th, 2001Complainer of history: patient’s son and wife Reliability: ReliableChief complaint: Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.Present illness:The patient felt upper bellyache about ten days ago. He didn’t pay attention to it and thought he had ate something wrong. At 6 o’clock this morning he fainted and rejected lots of blood and gore. Then hemafecia began. His family sent him to our hospital and received emergent treatment. So the patient was accepted because of “upper gastrointestine hemorrhage and exsanguine shock”.Since the disease coming on, the patient didn’t urinate.Past historyThe patient is healthy before.No history of infective diseases. No allergy history of food and drugs.Past historyOperative history: Never undergoing any operation.Infectious history: No history of severe infectious disease.Allergic history: He was not allergic to penicillin or sulfamide. Respiratory system: No history of respiratory disease.Circulatory system: No history of precordial pain.Alimentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease.Hematopoietic system:No history of anemia and mucocutaneous bleeding.Endocrine system: No acromegaly. No excessive sweats.Kinetic system: No history of confinement of limbs.Neural system: No history of headache or dizziness.Personal historyHe was born in Wuhan on Nov 19th, 1921 and almost always lived in Wuhan. His living conditions were good. No bad personal habits and customs. Menstrual history: He is a male patient.Obstetrical history: NoContraceptive history: Not clear.Family history: His parents have both deads.Physical examinationT 36.5℃, P 130/min, R 23/min, BP 100/60mmHg. He is well developed and moderately nourished. Active position. His consciousness was not clear. His face was cadaverous and the skin was not stained yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not found enlarged.HeadCranium:Hair was black and white, well distributed. No deformities. No scars. No masses. No tenderness.Ear:Bilateral auricles were symmetric and of no masses. No discharges were found in external auditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nares flaring. No tenderness in nasal sinuses. Eye:Bilateral eyelids were not swelling. No ptosis. No entropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs werenot projected or depressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect pupillary reactions to light were existent.Mouth: Oral mucous membrane was not smooth, and there were ulcer can be seen. Tongue was in midline. Pharynx was congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in midline.ChestChestwall:Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was neither narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities.Breast: Symmetric bilaterally.Lungs:Respiratory movement was bilaterally symmetric with the frequency of 23/min. thoracic expansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales.Heart:No bulge and no abnormal impulse or thrills in precordial area. The point of maximum impulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardial friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 150/min. Cardiac rhythm was not regular. No pathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs.Extremities: No articular swelling. Free movements of all limbs. Neural system:Physiological reflexes were existent without anypathological ones.Genitourinary system: Not examed.Rectum: not exanedInvestigationBlood-Rt: Hb 69g/L RBC 2.70T/L WBC 1. 1G/L PLT 120G/LHistory summary1.Patient was male, 80 years old2.Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.3.No special past history.4.Physical examination: T 37.5℃, P 130/min, R 23/min, BP 100/60mmHg Superficial lymph nodes were not found enlarged. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs. No other positive signs.5.investigation information:Blood-Rt: Hb 69g/L RBC 2.80T/L WBC 1.1G/L PLT 120G/L Impression: upper gastrointestinehemorrhageExsanguine shockSignature: He Lin (95-10033)。

英文病历标准模版Patient ProfileName: Si RuihuaDepartment: ___ Power ___Sex: FemalePresent Address: Electric Power Bureau Age: 80 yearsDate of n: May 17.2003nality: Chinese XinjiangDate of Record: May 17.2003Marital Status: MarriedReliability: Reliablen: Family ___History of Allergy: None reportedChief Complaints___。
breathlessness。
and precordial pain for the last hour。
There were no precipitating factors。
and the fort could not be relieved by rest。
As a result。
she came to the hospital for help。
She did not experience syncope。
cough。
headache。
diarrhea。
or vomiting during the course of the illness。
Her appetite。
sleep。
voiding。
and stool were normal.Medical History___.______。
___ distress。
She had a heart rate of 120 beats per minute and a blood pressure of 160/90 mmHg。
Her respiratory rate was 28 breaths per minute。
and her oxygen n was 90% on room air。
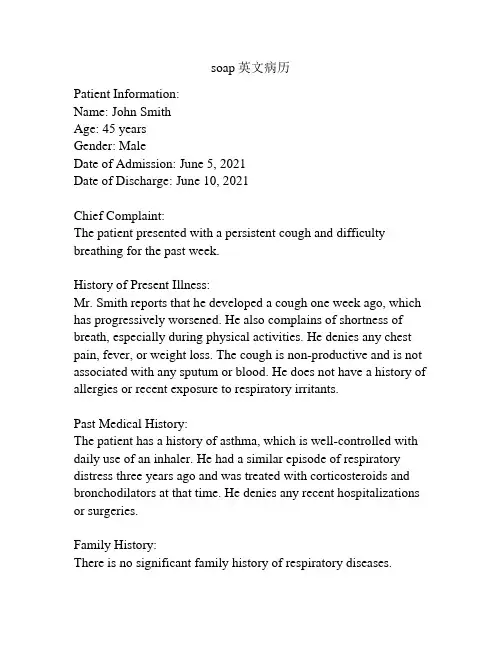
soap英文病历Patient Information:Name: John SmithAge: 45 yearsGender: MaleDate of Admission: June 5, 2021Date of Discharge: June 10, 2021Chief Complaint:The patient presented with a persistent cough and difficulty breathing for the past week.History of Present Illness:Mr. Smith reports that he developed a cough one week ago, which has progressively worsened. He also complains of shortness of breath, especially during physical activities. He denies any chest pain, fever, or weight loss. The cough is non-productive and is not associated with any sputum or blood. He does not have a history of allergies or recent exposure to respiratory irritants.Past Medical History:The patient has a history of asthma, which is well-controlled with daily use of an inhaler. He had a similar episode of respiratory distress three years ago and was treated with corticosteroids and bronchodilators at that time. He denies any recent hospitalizations or surgeries.Family History:There is no significant family history of respiratory diseases.Social History:Mr. Smith is a non-smoker and does not consume alcohol regularly. He works as an office manager and is not exposed to any occupational hazards. He lives with his wife and two teenage children. He denies any recent travel or contact with sick individuals.Physical Examination:Upon examination, the patient appears in no acute distress. Vital signs are stable with a temperature of 98.6°F (37°C), blood pressure of 120/80 mmHg, heart rate of 80 beats per minute, and respiratory rate of 16 breaths per minute. Auscultation of the lungs reveals bilateral wheezing and decreased breath sounds in the lower lung fields. There is no evidence of cyanosis or clubbing. The cardiovascular and abdominal examinations are within normal limits.Diagnostic Tests:A chest X-ray was ordered to evaluate the patient's respiratory symptoms. The X-ray showed bilateral diffuse patchy infiltrates, consistent with bronchial asthma. Pulmonary function tests were performed, revealing a decreased forced expiratory volume in one second (FEV1) and forced vital capacity (FVC), indicating obstructive lung disease.Assessment and Plan:The patient's symptoms, physical examination findings, and diagnostic test results are consistent with a diagnosis of exacerbation of bronchial asthma. The patient was started on a short course of oral corticosteroids, a short-acting bronchodilator,and an inhaled corticosteroid. He was also provided education regarding trigger avoidance and proper inhaler technique. Close follow-up was scheduled to monitor his response to treatment and adjust the management plan if necessary.Follow-Up:The patient will be seen for a follow-up visit in two weeks to evaluate his response to treatment and adjust his medication regimen if needed. He was instructed to monitor his lung function at home using a peak flow meter and seek medical attention if there is a significant decrease in his peak flow readings or if his symptoms worsen. The importance of regular follow-up visits and adherence to the prescribed medication regimen was emphasized. Summary:Mr. Smith, a 45-year-old male with a history of asthma, presented with a persistent cough and difficulty breathing. A diagnosis of exacerbation of bronchial asthma was made based on his symptoms, examination findings, and diagnostic tests. The patient was started on appropriate treatment and provided with education regarding trigger avoidance and inhaler technique. Close follow-up was arranged to monitor his response to treatment and ensure optimal management.。
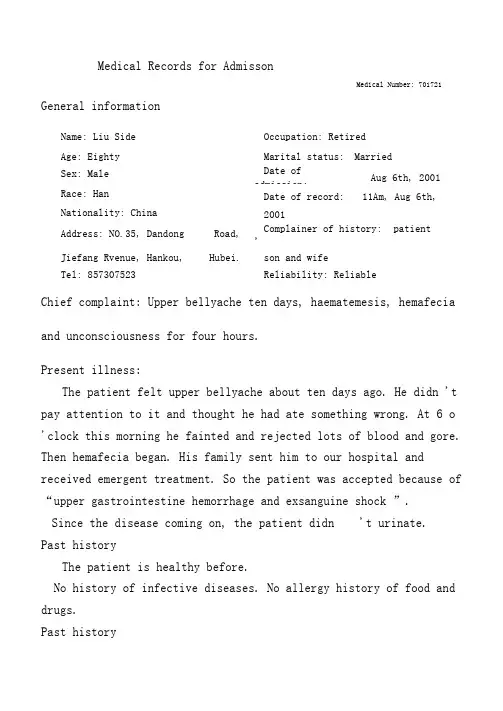
Medical Records for AdmissonMedical Number: 701721 General informationName: Liu Side Occupation: RetiredAge: Eighty Marital status: MarriedSex: Male Date ofadmission: Aug 6th, 2001Race: Han Date of record: 11Am, Aug 6th, Nationality: China 2001Address: NO.35, Dandong Road,Complainer of history: patient 'Jiefang Rvenue, Hankou, Hubei. son and wifeTel: 857307523 Reliability: ReliableChief complaint: Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.Present illness:The patient felt upper bellyache about ten days ago. He didn 't pay attention to it and thought he had ate something wrong. At 6 o 'clock this morning he fainted and rejected lots of blood and gore. Then hemafecia began. His family sent him to our hospital and received emergent treatment. So the patient was accepted because of “upper gastrointestine hemorrhage and exsanguine shock ”.Since the disease coming on, the patient didn 't urinate.Past historyThe patient is healthy before.No history of infective diseases. No allergy history of food and drugs.Past historyOperative history: Never undergoing any operation.Infectious history: No history of severe infectious disease. Allergic history: Hewas not allergic to penicillin or sulfamide. Respiratory system: No history of respiratory disease.Circulatory system: No history of precordial pain. Alimentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease. Hematopoietic system: No history of anemia and mucocutaneous bleeding.Endocrine system: No acromegaly. No excessive sweats.Kinetic system: No history of confinement of limbs.Neural system: No history of headache or dizziness. PersonalhistoryHe was born in Wuhan on Nov 19th, 1921 and almost always lived in Wuhan. His living conditions were good. No bad personal habits and customs.Menstrual history: He is a male patient.Obstetrical history: No Contraceptive history: Not clear.Family history: His parents have both deads.Physical examinationT 36.5 °C , P 130/min, R 23/min, BP100/60mmHg.He is well developed and moderately nourished. Active position. His consciousness was not clear. His face was cadaverous and the skin was not stained yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not found enlarged.HeadCranium: Hair was black and white, well distributed. No deformities. No scars. No masses. No tenderness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external auditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nares flaring. No tenderness in nasal sinuses.Eye: Bilateral eyelids were not swelling. No ptosis. No entropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or depressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect pupillary reactions to light were existent.Mouth: Oral mucous membrane was not smooth, and there wereulcer can be seen. Tongue was in midline. Pharynx was congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in midline.ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was neither narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities.Breast: Symmetric bilaterally.Lungs: Respiratory movementwas bilaterally symmetric with the frequency of 23/min. thoracic expansion and tactile fremitus weresymmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales.Heart: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum impulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardial friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 150/min. Cardiac rhythm was not regular. No pathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomenor renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs. Extremities: No articular swelling. Free movementsof all limbs. Neural system: Physiological reflexes were existent without any pathological ones.Genitourinary system: Not examed. Rectum: not exanedInvestigationBlood-Rt: Hb 69g/L RBC 2.70T/L WBC 1. 1G/L PLT 120G/LHistory summary1. Patient was male, 80 years old2. Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.3. No special past history.4. Physical examination: T 37.5 °C, P 130/min, R 23/min, BP100/60mmHgSuperficial lymph nodes were not found enlarged. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs. No other positive signs.5. investigation information:Blood-Rt: Hb 69g/L RBC 2.80T/L WBC 1.1G/L PLT 120G/LImpression: uppergastrointestinehemorrhageExsanguine shockSignature: He Lin (95-10033)。
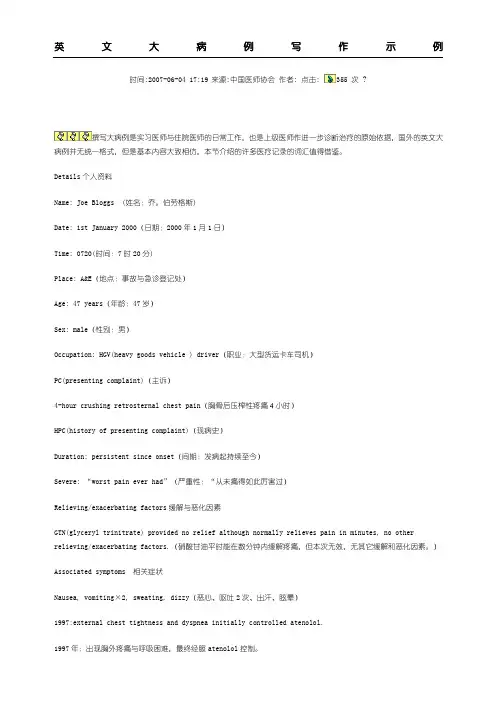
英文大病例写作示例时间:2007-06-04 17:19来源:中国医师协会作者: 点击: 355 次 ?撰写大病例是实习医师与住院医师的日常工作,也是上级医师作进一步诊断治疗的原始依据,国外的英文大病例并无统一格式,但是基本内容大致相仿,本节介绍的许多医疗记录的词汇值得借鉴。
Details个人资料Name: Joe Bloggs(姓名:乔。
伯劳格斯)Date: 1st January 2000(日期:2000年1月1日)Time: 0720(时间:7时20分)Place: A&E(地点:事故与急诊登记处)Age: 47 years(年龄:47岁)Sex: male(性别:男)Occupation: HGV(heavy goods vehicle ) driver(职业:大型货运卡车司机)PC(presenting complaint)(主诉)4-hour crushing retrosternal chest pain(胸骨后压榨性疼痛4小时)HPC(history of presenting complaint)(现病史)Duration: persistent since onset(间期:发病起持续至今)Severe: “worst pain ever had”(严重性:“从未痛得如此厉害过)Relieving/exacerbating factors缓解与恶化因素GTN(glyceryl trinitrate) provided no relief although normally relieves pain in minutes, no other relieving/exacerbating factors.(硝酸甘油平时能在数分钟内缓解疼痛,但本次无效,无其它缓解和恶化因素。
)Associated symptoms相关症状Nausea, vomiting×2, sweating, dizzy(恶心、呕吐2次、出汗、眩晕)1997:external chest tightness and dyspnea initially controlled atenolol.1997年:出现胸外疼痛与呼吸困难,最终经服atenolol控制。
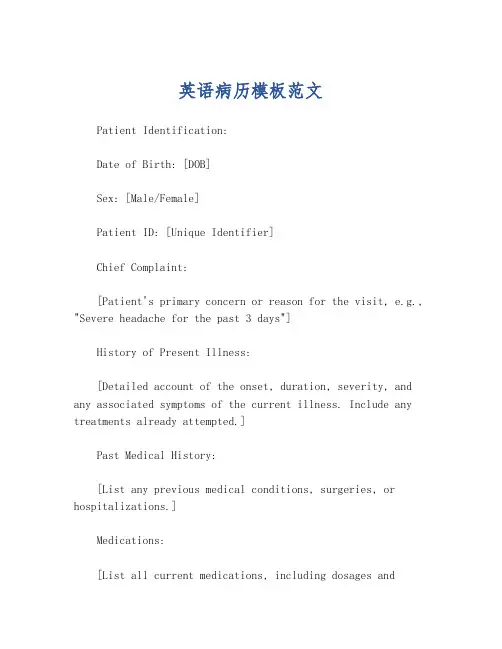
英语病历模板范文Patient Identification:Date of Birth: [DOB]Sex: [Male/Female]Patient ID: [Unique Identifier]Chief Complaint:[Patient's primary concern or reason for the visit, e.g., "Severe headache for the past 3 days"]History of Present Illness:[Detailed account of the onset, duration, severity, and any associated symptoms of the current illness. Include any treatments already attempted.]Past Medical History:[List any previous medical conditions, surgeries, or hospitalizations.]Medications:[List all current medications, including dosages andfrequency.]Allergies:[Note any known allergies to medications, foods, or environmental factors.]Family Medical History:[Provide information on any significant medicalconditions in the patient's family.]Social History:[Include relevant lifestyle factors such as smoking status, alcohol consumption, exercise habits, and occupation.]Review of Systems:[Briefly summarize the patient's current state inrelation to various body systems, e.g., "No chest pain, no shortness of breath."]Physical Examination:[Record findings from the physical examination, including vital signs, general appearance, and specific observations related to the chief complaint.]Assessment:[Summarize the likely diagnosis or condition based on the information gathered.]Plan:[Outline the proposed treatment plan, including medications, referrals, follow-up appointments, and any necessary tests or procedures.]。
医学英语病历写作范文Chief Complaint: Left leg pain with recent fall.History of Present Illness: The patient is a 65-year-old male who presents to the emergency department with a chief complaint of left leg pain. He states that he fell down a flight of stairs approximately 3 hours prior to presentation. He reports that he is in moderate to severe pain, which is localized to his left lower extremity. He denies any associated numbness or tingling. He has no prior history of leg pain or injury.Past Medical History: The patient has a history of hypertension, which is well-controlled with medication. He has no other significant medical history.Social History: The patient is married and has two children. He is a retired construction worker. He smokes one pack of cigarettes per day and drinks alcohol socially.Family History: The patient's father has a history of coronary artery disease. His mother has a history of Alzheimer's disease.Physical Examination:Vital signs: Blood pressure 140/80 mmHg, heart rate 80 bpm, respiratory rate 18 breaths per minute, temperature 98.6°F (37°C).General: The patient is in moderate distress due to pain. He is alert and oriented to person, place, and time.HEENT: Normocephalic and atraumatic. Pupils are equal and reactive to light. Extraocular movements are intact. No conjunctival injection or discharge. Tympanic membranes are intact and mobile.Neck: Supple with full range of motion. No masses or tenderness.Chest: Auscultation reveals clear breath soundsbilaterally. No wheezes, rales, or rhonchi.Cardiovascular: Regular rate and rhythm. No murmurs, rubs, or gallops.Abdomen: Soft and non-tender. No masses or organomegaly.Extremities: Left lower extremity: Examination reveals swelling and tenderness of the left knee. There is a palpable step-off deformity of the lateral aspect of theleft knee. Active and passive range of motion is limiteddue to pain. Distal pulses are palpable and capillaryrefill is brisk. Sensation is intact. Right lower extremity: Examination reveals no abnormalities.Neurological Examination:Mental status: Alert and oriented to person, place,and time. No deficits in attention, memory, or language.Cranial nerves: No deficits.Motor: Strength is 5/5 in both upper and lower extremities. No atrophy or fasciculations.Sensory: Sensation is intact to light touch, pinprick, and temperature in all four extremities.Diagnostic Studies:X-ray of the left knee: The X-ray shows a displaced lateral tibial plateau fracture.Assessment:Left knee pain.Displaced lateral tibial plateau fracture.Plan:The patient will be admitted to the hospital for further evaluation and treatment.He will be placed in a knee immobilizer and will be started on pain medication.Orthopedic surgery will be consulted for further management.。
Admission Notes (2)A 60-year-old married male was admitted on March 10,2010, with a two-month palpitation and a thoracalgia.Since this March, the patient has frequently felt palpitations a chest pain upon physical exertion, the latter radiating into the left shoulder and arm. One attack lasts about five minutes. He has a feeling of suffocation. It seems as if something heavy were pressing hard on his chest. He has a slight cough and expectorates a little mucous sputum during the attack.. Because he has not had any treatment before, the symptoms mentioned above have also deteriorated this week and his legs have been swollen as well, he came to the hospital for medical treatment.During his illness, he has been feeling weak but he has had a goodappetite, and his bowel motions and micturition have remained normal.He said that he had been perfectly healthy and had never had rheumatic fever or heart trouble previously.There is nothing particular in his family medical history.PE T: 36.7”C; P:100/min. R:20/min.;BP:140/80mmHg(19—11kPa).Well developed and nourished. In his right mind and in voluntary position. No dyspnea or cyanosis detected. No eruption or purpura over skin. Superficial lymph nodes impalpable. Skull and head organs not abnormal. Neck soft and supple and free of venous engorgement. Trachea in midline. Thyroid not enlarged. Chest symmetrical. Lungs clear. Heart enlarged and leftward without irregular beats. Heart rate 100/min. A grade—IIIharsh blowing systolic murmur heard at the apical area with no thrill felt or diastolic murmur heard. Abdomen flat with no tenderness. Liver felt 2 fb below costal margin. Hepatojugular reflux negative. Spleen not palpable. No shifting dullness over abdomen heard. Slight edema in both ankles present. Bilateral knee jerk reflexes active. No pathological neural reflex found.Chest fluoroscopy reveals general cardiac enlargement.ECG shows:1.sinus rhythm2.left ventricular hypertrophy3.chronic coronary insufficiency Diagnosis: Coronary Heart Disease Left V entricular HypertrophyAngina Pectoris Signature: Date:。
英语作文病历模板英文回答:Medical History Template。
Patient Information。
Name:Date of Birth:Gender:Address:Phone Number:Email Address:Reason for Visit。
What brings you to the clinic today?Medical History。
Past Medical History。
Do you have any past medical conditions?Have you ever been hospitalized or had surgery?Do you currently take any medications?Do you have any allergies?Family Medical History。
Do any of your close family members have any medical conditions?Have any of your close family members passed away at a young age due to illness?Social History。
What is your occupation?Are you currently married or in a relationship? Do you have any children?Do you smoke, drink alcohol, or use drugs?Physical Examination。
General Appearance:Height:Weight:BMI:Vital Signs:Blood pressure: Pulse:Respiratory rate: Temperature:Cardiovascular:Heart rate:Heart sounds:Blood pressure: Respiratory:Respiratory rate: Lung sounds:Abdomen:Girth:Soft and non-tender: Liver span:Musculoskeletal:Range of motion:Strength:Reflexes:Skin:Color:Texture:Turgor:Assessment。
英语写病历作文模板 Patient History Template。
英文回答:General Information。
Name:Age:Gender:Occupation:Address:Phone number:Emergency contact:Medical History。
Past medical history: List any previous illnesses, surgeries, hospitalizations, or accidents.Family medical history: Note any history of chronic diseases, such as heart disease, cancer, or diabetes, in the patient's family.Allergies: List any known allergies to medications, foods, or other substances.Medications: List all current medications, including prescription drugs, over-the-counter medications, and herbal supplements.Social history: Discuss the patient's lifestyle, including diet, exercise, smoking, alcohol use, and drug use.Present Illness。
Chief complaint: State the patient's primary reasonfor seeking medical attention.History of present illness: Describe the onset, duration, severity, and progression of the patient's symptoms.Physical Examination。
HUAZHONG UNIVERSITY OF SCIENCE AND TECHNOLOGY TONGJI MEDICAL COLLEGE ACCESSORY TONGJI HOSPITALHospitalization Records for None-operation Division Division: __________ Ward: __________ Bed: _________ Case No. ___________Name: ______________ Sex: __________ Age: ___________ Nation: ___________ Birth Place: ________________________________ Marital Status:____________ Work-organization & Occupation: _______________________________________ Living Address & Tel: _________________________________________________ Date of admission: _______Date of history taken:_______ Informant:__________ Chief Complaint: ___________________________________________________History of Present Illness:___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________Past History:General Health Status: 1.good 2.moderate 3.poorDisease history: (if any, please write down the date of onset, brief diagnosticand therapeutic course, and the results.)Respiratory system:1. None2.Repeated pharyngeal pain3.chronic cough4.expectoration:5. Hemoptysis6.asthma7.dyspnea8.chest pain_______________________________________________________________ Circulatory system:1.None2.Palpitation3.exertional dyspnea4..cyanosis5.hemoptysis6.Edema of lower extremities7.chest pain8.syncope9.hypertension_______________________________________________________________ Digestive system:1.None2.Anorexia3.dysphagia4.sour regurgitation5.eructation6.nausea7.Emesis8.melena9.abdominal pain 10.diarrhea11.hematemesis 12.Hematochezia 13.jaundice_______________________________________________________________ Urinary system:1.None2.Lumbar pain3.urinary frequency4.urinary urgency5.dysuria6.oliguria7.polyuria8.retention of urine9.incontinence of urine10.hematuria 11.Pyuria 12.nocturia 13.puffy face_______________________________________________________________ Hematopoietic system:1.None2.Fatigue3.dizziness4.gingival hemorrhage5.epistaxis6.subcutaneous hemorrhage_______________________________________________________________ Metabolic and endocrine system:1.None2.Bulimia3.anorexia4.hot intolerance5.cold intolerance6.hyperhidrosis7.Polydipsia8.amenorrhea9.tremor of hands 10.character change 11.Marked obesity12.marked emaciation 13.hirsutism 14.alopecia15.Hyperpigmentation 16.sexual function change_______________________________________________________________ Neurological system:1.None2.Dizziness3.headache4.paresthesia5.hypomnesis6. Visual disturbance7.Insomnia8.somnolence9.syncope 10.convulsion 11.Disturbance of consciousness12.paralysis 13. vertigo_______________________________________________________________ Reproductive system:1.None2.others_______________________________________________________________Musculoskeletal system:1.None2.Migrating arthralgia3.arthralgia4.artrcocele5.arthremia6.Dysarthrosis7.myalgia8.muscular atrophy_______________________________________________________________ Infectious Disease:1.None2.Typhoid fever3.Dysentery4.Malaria 4.Schistosomiasis4.Leptospirosis 7.Tuberculosis 8.Epidemic hemorrhagic fever9.others_______________________________________________________________ Vaccine inoculation:1.None2.Yes3.Not clearVaccine detail __________________________________________ Trauma and/or operation history:Operations:1.None2.YesOperation details:_______________________________________ Traumas:1.None2.YesTrauma details:_________________________________________ Blood transfusion history:1.None2.Yes ( 1.Whole blood 2.Plasma3.Ingredient transfusion)Blood type:____________ Transfusion time:___________Transfusion reaction1.None2.YesClinic manifestation:_____________________________ Allergic history:1.None2.Yes3.Not clearallergen:________________________________________________clinical manifestation:_____________________________________Personal history:Custom living address:____________________________________________ Resident history in endemic disease area:_____________________________ Smoking: 1.No 2.YesAverage ___pieces per day; about___yearsGiving-up 1.No 2.Yes (Time:_______________________) Drinking: 1.No 2.YesAverage ___grams per day; about ___yearsGiving-up 1.No 2.Yes(Time:________________________) Drug abuse:1.No 2.YesDrug names:_______________________________________ _______________________________________________________________Marital and obstetrical history:Married age: __________years old Pregnancy ___________timesLabor _______________times(1.Natural labor: _______times 2.Operative labor: ________times3.Natural abortion: ______times4.Artificial abortion: _______times5.Premature labor:__________times6.stillbirth__________times)Health status of the Mate:1.Well2.Not fineDetails: _______________________________________________ Menstrual history:Menarchal age: _______ Duration ______day Interval ____daysLast menstrual period: ____________ Menopausal age: ____years oldAmount of flow: 1.small 2. moderate 3. largeDysmenorrheal: 1. presence 2.absence Menstrual irregularity 1. No 2.Yes Family history: (especially pay attention to the infectious and hereditary diseaserelated to the present illness)Father: 1.healthy 2.ill:________ 3.deceased cause: ___________________ Mother:1.healthy 2.ill:________ 3.deceased cause: ___________________ Others: ________________________________________________________ The anterior statement was agreed by the informant.Signature of informant: Datetime:Physical ExaminationVital signs:Temperature:______0C Blood pressure:_______/_______mmHg Pulse: _____ bpm (1.regular 2.irregular_____________________________) Respiration: ___bpm (1.regular 2.irregular____________________________) General conditions:Development: 1.Normal 2.Hypoplasia 3.HyperplasiaNutrition: 1.good 2.moderate 3.poor 4.cachexiaFacial expression: 1.normal 2.acute 3.chronic other_____________________ Habitus: 1.asthenic type 2.sthenic type 3.ortho-thenic typePosition: 1.active 2.positive pulsive 4.other_______________________ Consciousness: 1.clear 2.somnolence 3.confusion 4.stupor 5.slight coma6.mediate coma7.deep coma8.deliriumCooperation: 1Yes 2.No Gait: 1.normal 2.abnormal______Skin and mucosa:Color: 1.normal 2.pale 3.redness 4.cyanosis 5.jaundice 6.pigmentationSkin eruption:1.No 2.Yes( type: __________distribution:__________________) Subcutaneous bleeding: 1.no 2.yes (type:_______distribution:______________) Edema:1. no 2.yes ( location and degree________________________________) Hair: 1.normal 2.abnormal(details_____________________________________) Temperature and moisture: normal cold warm dry moist dehydration Liver palmar : 1.no 2.yes Spider angioma (location:________________) Others: __________________________________________________________ Lymph nodes: enlargement of superficial lymph node:1.no2.yesDescription: ________________________________________________ Head:Skull size:1.normal 2.abnormal (description:____________________________) Skull shape:1.normal 2.abnormal(description:___________________________) Hair distribution :1.normal 2.abnormal(description:______________________) Others:___________________________________________________________ Eye: exophthalmos:___________eyelid:____________conjunctiva:__________ sclera:________________Cornea:_______________________Pupil: 1.equally round and in size 2.unequal (R______mm L_______mm)Pupil reflex: 1.normal 2.delayed (R___s L___s ) 3.absent (R___L___)others:______________________________________________________ Ear: Auricle 1.normal 2.desformation (description:_______________________) Discharge of external auditory canal:1.no 2.yes (1.left 2.right quality:_____)Mastoid tenderness 1.no 2.yes (1.left 2.right quality:__________________)Disturbance of auditory acuity:1.no 2.yes(1.left 2.right description:_______) Nose: Flaring of alae nasi :1.no 2.yes Stuffy discharge 1.no 2.yes(quality______) Tenderness over paranasal sinuses:1.no 2.yes (location:_______________) Mouth: Lip______________Mucosa_____________Tongue________________ Teeth:1.normal 2. Agomphiasis 3. Eurodontia 4.others:____________________Gum :1.normal 2.abnormal (Description____________________________)Tonsil:___________________________Pharynx:_____________________Sound: 1.normal 2.hoarseness 3.others:_____________________________ Neck:Neck rigidity 1.no 2.yes (______________transvers fingers)Carotid artery: 1.normal pulsation 2.increased pulsation 3.marked distention Trachea location: 1.middle 2.deviation (1.leftward_______2.rightward______) Hepatojugular vein reflux: 1. negative 2.positiveThyroid: 1.normal 2.enlarged _______ 3.bruit (1.no 2.yes ________________)Chest:Chest wall: 1.normal 2.barrel chest 3.prominence or retraction:( left________right_________Precordial prominence__________) Percussion pain over sternum 1.No 2.YesBreast: 1.Normal 2.abnormal _______________________________________ Lung:Inspection: respiratory movement 1.normal 2.abnormal_____________ Palpation: vocal tactile fremitus:1.normal 2.abnormal _______________pleural rubbing sensation:1.no 2.yes______________________Subcutaneous crepitus sensation:1.no 2.yes________________ Percussion:1. resonance 2. Hyperresonance &location_____________3 Flatness&location_________________________________4. dullness & location:_______________________________5.tympany &location:_______________________________lower border of lung: (detailed percussion in respiratory disease)midclavicular line : R:_____intercostae L:_____intercostaemidaxillary line: R:______intercostae L:_____intercostaescapular line: R:______intercostae L:_____intercostaemovement of lower borders:R:_______cmL:__________cm Auscultation: Breathing sound : 1.normal 2.abnormal _______________Rales:1.no 2.yes__________________________________ Heart: Inspection:Apical pulsation: 1.normal 2.unseen 3.increase 4.diffuseSubxiphoid pulsation: 1.no 2.yesLocation of apex beat: 1.normal 2.shift (______ intercosta,distance away from left MCL______cm) Palpation:Apical pulsation:1. normal 2.lifting apex impulse 3.negative pulsationThrill:1.no 2.yes(location:___________ phase:_________________)Percussion: relative dullness border: 1.normal 2.abnormalAuscultation: Heart rate:___bpm Rhythm:1.regular 2.irregular_______Heart sound: 1.normal 2.abnormal________________________Extra sound: 1.no 2.S3 3.S4 4. opening snapP2_________ A2_________Pericardial friction sound:1.no 2.yesMurmur: 1.no 2.yes (location____________phase_____________quality______intensity________ transmission___________effects of position_________________________________effects of respiration______________________________Peripheral vascular signs:1.None2.paradoxical pulse3.pulsus alternans4. Water hammer pulse5.capillary pulsation6.pulse deficit7.Pistol shot sound8.Duroziez signAbdomen:Inspection: Shape: 1.normal 2.protuberance 3.scaphoid 4.frog-bellyGastric pattern 1.no 2.yes Intestinal pattern 1.no 2.yesAbdominal vein varicosis 1.no 2.yes(direction:______________ )Operation scar1.no 2.yes ________________________________ Palpation: 1.soft 2. tensive (location:____________________________)Tenderness: 1.no 2.yes(location:_______________________)Rebound tenderness:1.no 2.yes(location:________________)Fluctuation: 1.present 2.abscentSuccussion splash: 1.negative 2.positiveLiver:_______________________________________________Gallbladder: __________________Murphy sign:____________Spleen:______________________________________________Kidneys:____________________________________________Abdominal mass:______________________________________Others:______________________________________________ Percussion: Liver dullness border: 1.normal 2.decreased 3.absentUpper hepatic border:Right Midclavicular Line ________IntercostaShift dullness:1.negative 2.positive Ascites:_____________degreePain on percussion in costovertebral area: 1.negative 2.positve ____ Auscultation: Bowel sounds : 1.normal 2.hyperperistalsis 3.hypoperistalsis4.absence Gurgling sound:1.no 2.yesVascular bruit 1.no 2.yes (location_____________________) Genital organ: 1.unexamined 2.normal 3.abnormalAnus and rectum: 1.unexamined 2.normal 3.abnormalSpine and extremities:Spine: 1.normal 2.deformity (1.kyphosis 2.lordosis 3.scoliosis)3.Tenderness(location______________________________)Extremities:1.normal 2.arthremia & arthrocele (location_________________)3.Ankylosis (location__________)4.Aropachy: 1.no 2.yes5.Muscular atrophy (location_______________________) Neurological system:1.normal 2.abnormal_______________________________ _____________________________________________________________________Important examination results before hospitalized___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ Summary of the history:______________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ Initial diagnosis:_____________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________Recorder:Corrector:。
英文病历范文Title: English Medical Record Sample (Creating and Expanding on a Matching Content)Medical RecordNa John SmithDate of Birth: February 15, 1985Gender: MaleNationality: AmericanOccupation: AccountantChief Complaint:The patient presented with a complaint of persistent cough, shortness of breath, and chest pain for the past week.History of Present Illness:The symptoms initially started as a mild cough, which gradually worsened over the week. The patient also experienced shortness of breath, especially during physical activities. He reported occasional chest pain, which was sharp in nature and intensified during deep breaths. The patient denied any fever, night sweats, or weight loss.Past Medical History:The patient has a history of asthma since childhood and has been using an inhaler as needed. He had a similar episode ofpersistent cough and shortness of breath six months ago, which resolved with a course of oral steroids. No other significant medical history was reported.Social History:The patient is a non-smoker and denies any alcohol or illicit drug use. He lives with his wife and two children in a smoke-free environment. The patient works as an accountant and does not have any known occupational exposures.Family History:There is no significant family history of respiratory diseases or any chronic illnesses.Review of Systems:The review of systems was unremarkable except for the respiratory symptoms mentioned above.Physical Examination:On examination, the patient appeared to be in no acute distress. Vital signs were within normal limits. Auscultation of the lungs revealed mild wheezing bilaterally. Heart sounds were normal, and there were no signs of peripheral edema or cyanosis. Other systemic examinations were within normal limits.Investigations:Laboratory investigations, including complete blood count, liver and kidney function tests, and electrolyte levels, were all within normal range. Chest X-ray showed hyperinflation of lungs and no evidence of infiltrates or consolidation.Assessment and Plan:Based on the history, clinical findings, and investigations, the patient's symptoms and past medical history suggest asthma exacerbation. Initial management includes a trial of short-acting bronchodilators, oral corticosteroids, and close monitoring of symptoms. The patient was educated about proper inhaler technique and advised to follow up in one week for reassessment.Education and Counseling:The patient was counseled on the importance of adherence to the prescribed medication and the need to avoid triggers for asthma exacerbation, such as allergens and respiratory infections. He was also provided with a written asthma action plan for self-management and advised to seek medical attention if symptoms worsen or do not improve within a week.Follow-up:The patient will be scheduled for a follow-up visit in one week to reassess symptoms, evaluate response to treatment, andadjust the management plan accordingly.This medical record documents the patient's chief complaint, history of present illness, past medical history, social and family history, physical examination findings, investigations, diagnosis, and treatment plan. It serves as a comprehensive guide for healthcare professionals involved in the patient's care.。
HUAZHONG UNIVERSITY OF SCIENCE AND TECHNOLOGY TONGJI MEDICAL COLLEGE ACCESSORY TONGJI HOSPITALHospitalization Records for None-operation Division Division: __________ Ward: __________ Bed: _________ Case No. ___________Name: ______________ Sex: __________ Age: ___________ Nation: ___________ Birth Place: ________________________________ Marital Status:____________ Work-organization & Occupation: _______________________________________ Living Address & Tel: _________________________________________________ Date of admission: _______Date of history taken:_______ Informant:__________ Chief Complaint: ___________________________________________________History of Present Illness:___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________Past History:General Health Status: 1.good 2.moderate 3.poorDisease history: (if any, please write down the date of onset, brief diagnosticand therapeutic course, and the results.)Respiratory system:1. None2.Repeated pharyngeal pain3.chronic cough4.expectoration:5. Hemoptysis6.asthma7.dyspnea8.chest pain_______________________________________________________________ Circulatory system:1.None2.Palpitation3.exertional dyspnea4..cyanosis5.hemoptysis6.Edema of lower extremities7.chest pain8.syncope9.hypertension_______________________________________________________________ Digestive system:1.None2.Anorexia3.dysphagia4.sour regurgitation5.eructation6.nausea7.Emesis8.melena9.abdominal pain 10.diarrhea11.hematemesis 12.Hematochezia 13.jaundice_______________________________________________________________ Urinary system:1.None2.Lumbar pain3.urinary frequency4.urinary urgency5.dysuria6.oliguria7.polyuria8.retention of urine9.incontinence of urine10.hematuria 11.Pyuria 12.nocturia 13.puffy face_______________________________________________________________ Hematopoietic system:1.None2.Fatigue3.dizziness4.gingival hemorrhage5.epistaxis6.subcutaneous hemorrhage_______________________________________________________________ Metabolic and endocrine system:1.None2.Bulimia3.anorexia4.hot intolerance5.cold intolerance6.hyperhidrosis7.Polydipsia8.amenorrhea9.tremor of hands 10.character change 11.Marked obesity12.marked emaciation 13.hirsutism 14.alopecia15.Hyperpigmentation 16.sexual function change_______________________________________________________________ Neurological system:1.None2.Dizziness3.headache4.paresthesia5.hypomnesis6. Visual disturbance7.Insomnia8.somnolence9.syncope 10.convulsion 11.Disturbance of consciousness12.paralysis 13. vertigo_______________________________________________________________ Reproductive system:1.None2.others_______________________________________________________________Musculoskeletal system:1.None2.Migrating arthralgia3.arthralgia4.artrcocele5.arthremia6.Dysarthrosis7.myalgia8.muscular atrophy_______________________________________________________________ Infectious Disease:1.None2.Typhoid fever3.Dysentery4.Malaria 4.Schistosomiasis4.Leptospirosis 7.Tuberculosis 8.Epidemic hemorrhagic fever9.others_______________________________________________________________ Vaccine inoculation:1.None2.Yes3.Not clearVaccine detail __________________________________________ Trauma and/or operation history:Operations:1.None2.YesOperation details:_______________________________________ Traumas:1.None2.YesTrauma details:_________________________________________ Blood transfusion history:1.None2.Yes ( 1.Whole blood 2.Plasma3.Ingredient transfusion)Blood type:____________ Transfusion time:___________Transfusion reaction1.None2.YesClinic manifestation:_____________________________ Allergic history:1.None2.Yes3.Not clearallergen:________________________________________________clinical manifestation:_____________________________________Personal history:Custom living address:____________________________________________ Resident history in endemic disease area:_____________________________ Smoking: 1.No 2.YesAverage ___pieces per day; about___yearsGiving-up 1.No 2.Yes (Time:_______________________) Drinking: 1.No 2.YesAverage ___grams per day; about ___yearsGiving-up 1.No 2.Yes(Time:________________________) Drug abuse:1.No 2.YesDrug names:_______________________________________ _______________________________________________________________Marital and obstetrical history:Married age: __________years old Pregnancy ___________timesLabor _______________times(1.Natural labor: _______times 2.Operative labor: ________times3.Natural abortion: ______times4.Artificial abortion: _______times5.Premature labor:__________times6.stillbirth__________times)Health status of the Mate:1.Well2.Not fineDetails: _______________________________________________ Menstrual history:Menarchal age: _______ Duration ______day Interval ____daysLast menstrual period: ____________ Menopausal age: ____years oldAmount of flow: 1.small 2. moderate 3. largeDysmenorrheal: 1. presence 2.absence Menstrual irregularity 1. No 2.Yes Family history: (especially pay attention to the infectious and hereditary diseaserelated to the present illness)Father: 1.healthy 2.ill:________ 3.deceased cause: ___________________ Mother:1.healthy 2.ill:________ 3.deceased cause: ___________________ Others: ________________________________________________________ The anterior statement was agreed by the informant.Signature of informant: Datetime:Physical ExaminationVital signs:Temperature:______0C Blood pressure:_______/_______mmHg Pulse: _____ bpm (1.regular 2.irregular_____________________________) Respiration: ___bpm (1.regular 2.irregular____________________________) General conditions:Development: 1.Normal 2.Hypoplasia 3.HyperplasiaNutrition: 1.good 2.moderate 3.poor 4.cachexiaFacial expression: 1.normal 2.acute 3.chronic other_____________________ Habitus: 1.asthenic type 2.sthenic type 3.ortho-thenic typePosition: 1.active 2.positive pulsive 4.other_______________________ Consciousness: 1.clear 2.somnolence 3.confusion 4.stupor 5.slight coma6.mediate coma7.deep coma8.deliriumCooperation: 1Yes 2.No Gait: 1.normal 2.abnormal______Skin and mucosa:Color: 1.normal 2.pale 3.redness 4.cyanosis 5.jaundice 6.pigmentationSkin eruption:1.No 2.Yes( type: __________distribution:__________________) Subcutaneous bleeding: 1.no 2.yes (type:_______distribution:______________) Edema:1. no 2.yes ( location and degree________________________________) Hair: 1.normal 2.abnormal(details_____________________________________) Temperature and moisture: normal cold warm dry moist dehydration Liver palmar : 1.no 2.yes Spider angioma (location:________________) Others: __________________________________________________________ Lymph nodes: enlargement of superficial lymph node:1.no2.yesDescription: ________________________________________________ Head:Skull size:1.normal 2.abnormal (description:____________________________) Skull shape:1.normal 2.abnormal(description:___________________________) Hair distribution :1.normal 2.abnormal(description:______________________) Others:___________________________________________________________ Eye: exophthalmos:___________eyelid:____________conjunctiva:__________ sclera:________________Cornea:_______________________Pupil: 1.equally round and in size 2.unequal (R______mm L_______mm)Pupil reflex: 1.normal 2.delayed (R___s L___s ) 3.absent (R___L___)others:______________________________________________________ Ear: Auricle 1.normal 2.desformation (description:_______________________) Discharge of external auditory canal:1.no 2.yes (1.left 2.right quality:_____)Mastoid tenderness 1.no 2.yes (1.left 2.right quality:__________________)Disturbance of auditory acuity:1.no 2.yes(1.left 2.right description:_______) Nose: Flaring of alae nasi :1.no 2.yes Stuffy discharge 1.no 2.yes(quality______) Tenderness over paranasal sinuses:1.no 2.yes (location:_______________) Mouth: Lip______________Mucosa_____________Tongue________________ Teeth:1.normal 2. Agomphiasis 3. Eurodontia 4.others:____________________Gum :1.normal 2.abnormal (Description____________________________)Tonsil:___________________________Pharynx:_____________________Sound: 1.normal 2.hoarseness 3.others:_____________________________ Neck:Neck rigidity 1.no 2.yes (______________transvers fingers)Carotid artery: 1.normal pulsation 2.increased pulsation 3.marked distention Trachea location: 1.middle 2.deviation (1.leftward_______2.rightward______) Hepatojugular vein reflux: 1. negative 2.positiveThyroid: 1.normal 2.enlarged _______ 3.bruit (1.no 2.yes ________________)Chest:Chest wall: 1.normal 2.barrel chest 3.prominence or retraction:( left________right_________Precordial prominence__________) Percussion pain over sternum 1.No 2.YesBreast: 1.Normal 2.abnormal _______________________________________ Lung:Inspection: respiratory movement 1.normal 2.abnormal_____________ Palpation: vocal tactile fremitus:1.normal 2.abnormal _______________pleural rubbing sensation:1.no 2.yes______________________Subcutaneous crepitus sensation:1.no 2.yes________________ Percussion:1. resonance 2. Hyperresonance &location_____________3 Flatness&location_________________________________4. dullness & location:_______________________________5.tympany &location:_______________________________lower border of lung: (detailed percussion in respiratory disease)midclavicular line : R:_____intercostae L:_____intercostaemidaxillary line: R:______intercostae L:_____intercostaescapular line: R:______intercostae L:_____intercostaemovement of lower borders:R:_______cmL:__________cm Auscultation: Breathing sound : 1.normal 2.abnormal _______________Rales:1.no 2.yes__________________________________ Heart: Inspection:Apical pulsation: 1.normal 2.unseen 3.increase 4.diffuseSubxiphoid pulsation: 1.no 2.yesLocation of apex beat: 1.normal 2.shift (______ intercosta,distance away from left MCL______cm) Palpation:Apical pulsation:1. normal 2.lifting apex impulse 3.negative pulsationThrill:1.no 2.yes(location:___________ phase:_________________)Percussion: relative dullness border: 1.normal 2.abnormalAuscultation: Heart rate:___bpm Rhythm:1.regular 2.irregular_______Heart sound: 1.normal 2.abnormal________________________Extra sound: 1.no 2.S3 3.S4 4. opening snapP2_________ A2_________Pericardial friction sound:1.no 2.yesMurmur: 1.no 2.yes (location____________phase_____________quality______intensity________ transmission___________effects of position_________________________________effects of respiration______________________________Peripheral vascular signs:1.None2.paradoxical pulse3.pulsus alternans4. Water hammer pulse5.capillary pulsation6.pulse deficit7.Pistol shot sound8.Duroziez signAbdomen:Inspection: Shape: 1.normal 2.protuberance 3.scaphoid 4.frog-bellyGastric pattern 1.no 2.yes Intestinal pattern 1.no 2.yesAbdominal vein varicosis 1.no 2.yes(direction:______________ )Operation scar1.no 2.yes ________________________________ Palpation: 1.soft 2. tensive (location:____________________________)Tenderness: 1.no 2.yes(location:_______________________)Rebound tenderness:1.no 2.yes(location:________________)Fluctuation: 1.present 2.abscentSuccussion splash: 1.negative 2.positiveLiver:_______________________________________________Gallbladder: __________________Murphy sign:____________Spleen:______________________________________________Kidneys:____________________________________________Abdominal mass:______________________________________Others:______________________________________________ Percussion: Liver dullness border: 1.normal 2.decreased 3.absentUpper hepatic border:Right Midclavicular Line ________IntercostaShift dullness:1.negative 2.positive Ascites:_____________degreePain on percussion in costovertebral area: 1.negative 2.positve ____ Auscultation: Bowel sounds : 1.normal 2.hyperperistalsis 3.hypoperistalsis4.absence Gurgling sound:1.no 2.yesVascular bruit 1.no 2.yes (location_____________________) Genital organ: 1.unexamined 2.normal 3.abnormalAnus and rectum: 1.unexamined 2.normal 3.abnormalSpine and extremities:Spine: 1.normal 2.deformity (1.kyphosis 2.lordosis 3.scoliosis)3.Tenderness(location______________________________)Extremities:1.normal 2.arthremia & arthrocele (location_________________)3.Ankylosis (location__________)4.Aropachy: 1.no 2.yes5.Muscular atrophy (location_______________________) Neurological system:1.normal 2.abnormal_______________________________ _____________________________________________________________________Important examination results before hospitalized___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ Summary of the history:______________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ Initial diagnosis:_____________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________ ___________________________________________________________Recorder:Corrector:。