中山大学教授颜光美M1“灭癌”病毒 有望进行临床试验
- 格式:docx
- 大小:149.29 KB
- 文档页数:12
新型天然溶瘤病毒M1可精确杀灭癌细胞引自“医学论坛网”【期刊名称】《中国肿瘤临床》【年(卷),期】2014(000)020【摘要】“在杀死癌细胞的同时,也杀死了正常细胞。
”这个困惑了全世界医生和癌症病人的怪圈,终于有望打破。
《美国科学院院报》最近发表了一篇重点论文指出,中国科学家发现,一种叫做M1的天然病毒能特异性杀死癌细胞而不伤害正常细胞。
这种新型溶瘤病毒有望成为下一代抗癌利器。
这项研究成果是由中国中山大学中山医学院颜光美团队独立完成并具完全的自主知识产权。
全球癌症发病率呈现快速增长态势,现有的治疗手段远远未能满足临床需求。
该团队历经多年潜心研究,终于从中国海南岛分离得到一种M1的天然病毒。
颜光美团队使用细胞培养方法发现,M1病毒能选择性地感染并杀死包括肝癌、结直肠癌、膀胱癌、黑色素瘤在内的多种癌细胞,而对正常细胞无毒副作用。
整体动物模型证明,M1病毒“像长了眼睛一样准确找到肿瘤组织并将其杀灭”,正常器官则不受影响。
除细胞水平及动物实验之外,课题组还使用大量临床标本进一步证实了上述新型溶瘤病毒的有效性和特异性。
更为重要的是,研究工作还证明了M1病毒作用的分子遗传学机理,找到了特异的负性生物标志物。
一种特别的基因与疗效有关。
这个发现为精准的临床用药和实施个体化疗法提供了可靠的科学依据,也会极大地增加未来临床试验取得成功的机会。
这些结果表明,如同“精确制导”一般的新型天然溶瘤病毒M1,将会安全而有效地治疗癌症,有望成为攻克人类癌症的新一代利器。
【总页数】1页(P1317-1317)【作者】引自“医学论坛网”【作者单位】引自“医学论坛网”【正文语种】中文【相关文献】1.食品天然防腐剂可杀灭癌细胞 [J],2.溶瘤病毒M1诱导宫颈癌细胞C-33A凋亡的作用及机制 [J], 肖晓;周雅思;彭楚茵;邓金清;王来友;朱文博3.携带TRAIL基因的新型溶瘤病毒体外诱导肝癌细胞凋亡 [J], 刘永靖;陈飞虎;苏长青;王星华;钱炎珍;钱其军4.天然病毒M1可杀伤肝癌等癌细胞 [J],5.中山大学分离出一种能杀灭癌细胞的天然病毒 [J],因版权原因,仅展示原文概要,查看原文内容请购买。
“杀灭最后一个癌细胞”只是幻想山东华圣中医肿瘤研究所所长济南华圣医院院长王现军经过长期科学知识的普及和抗癌理念的宣传,许多癌症患者以及他们的亲友,早已走出了“癌症是不治之症”、“癌症等于死亡”的认识误区。
他们认识到,癌症是可防可治的一类疾病,特别是早期发现并早期治疗,会取得非常理想的治疗效果;即使是明确诊断的时候病情已经到了中晚期,只要坚持积极正确的治疗方法,也不是没有临床治愈的可能。
于是,便满怀希望地进行手术,按部就班地接受一次次的放疗和化疗。
随着治疗过程的进展,患者的医学影像检查和生化检验报告不断更新,这些报告显示:患者的瘤体在不断缩小,肿瘤组织在变性、坏死,患者体内的癌细胞在逐步地减少。
在这种情形之下,不少人都会产生一种天真而美好的想法:我们只要坚持不懈地治疗下去,总有一天,会把体内的最后一个癌细胞给杀死,那时候,不就把癌症彻底治愈了吗?而现实却并不这么简单。
癌症是一种全身性的疾病,病灶本身只是局部的集中体现。
手术可以一次性地拿掉大部分的癌细胞,但是无法全部清除。
即使是所谓的“根治术”、“大范围清扫”也只是相对而言,手术范围越大,对人体造成的功能残损就约严重。
放射线和化学药品可以有效地杀灭癌细胞。
但是放射线治疗只能针对病灶局部实施,而且有终生最大剂量的限制,不可以无休止地照射下去;化疗药物可以作用于全身,但是它只是成比例地杀灭癌细胞,同时也对人体正常的组织和器官带来巨大伤害。
化疗药物带来的骨髓抑制、消化道反应、免疫抑制、心肺肝肾损伤、神经系统反应等毒副作用,也使患者无法接受持续的治疗。
由此看来,“杀灭最后一个癌细胞”的想法是难以实现的,坚持这样做的结果,必然是加重痛苦,加速死亡,生命和肿瘤同归于尽。
正确的做法是:对于大部分癌症患者特别是中晚期的患者,在经过治疗取得临床上缓解以后,把治疗的重点转移到调整机体平衡、保护和强化免疫系统功能方面来,扶正祛邪,抑制体内残存癌细胞的分裂增殖,使患者获得更高的生活质量和更长的生存时间。
新型“可复制型活药”溶瘤病毒M1的药动学研究
作者:
来源:《科学中国人》2024年第06期
中山大学中山医学院颜光美/林园团队解释了溶瘤病毒M1作为一种新型“可复制型活药”的药代动力学特征,并基于它的关键调控机制建立了特异性增效策略。
相关成果发表于《药学学报》英文刊(Acta Pharmaceutica Sinica B)。
溶瘤病毒是一类新兴的抗癌“活药”,可选择性感染并杀伤肿瘤细胞,同时不损伤正常组织。
研究人员系统解析了溶瘤病毒M1在免疫健全小鼠体内的药动学特征,并鉴定了对溶瘤病毒M1分布和代谢起关键调控作用的通路。
在此基础上,研究人员通过使用临床药物鲁索替尼成功改善了溶瘤病毒M1的药动学特性,并进一步提升了它的抗腫瘤疗效和机体免疫激活水平。
![M1病毒变异体及其应用[发明专利]](https://uimg.taocdn.com/1141620f9b89680202d825c5.webp)
专利名称:M1病毒变异体及其应用
专利类型:发明专利
发明人:颜光美,林园,郭莉,林子青,吴广恩申请号:CN202010486178.7
申请日:20200601
公开号:CN112011519A
公开日:
20201201
专利内容由知识产权出版社提供
摘要:本发明提供一种M1病毒。
本发明进一步提供所述病毒的一系列应用,所述应用包括但不限于:病毒载体、抗肿瘤剂、药物组合物。
本发明的病毒能够有效抑制多种肿瘤细胞的生长,同时具有肿瘤靶向性,对正常的细胞无毒性;可以经静脉注射的方式给药,具有操作上的便捷性。
申请人:广州威溶特医药科技有限公司
地址:510663 广东省广州市高新技术产业开发区科学城揽月路3号广州国际企业孵化器G区416-428房间
国籍:CN
代理机构:北京市万慧达律师事务所
代理人:谢敏楠
更多信息请下载全文后查看。
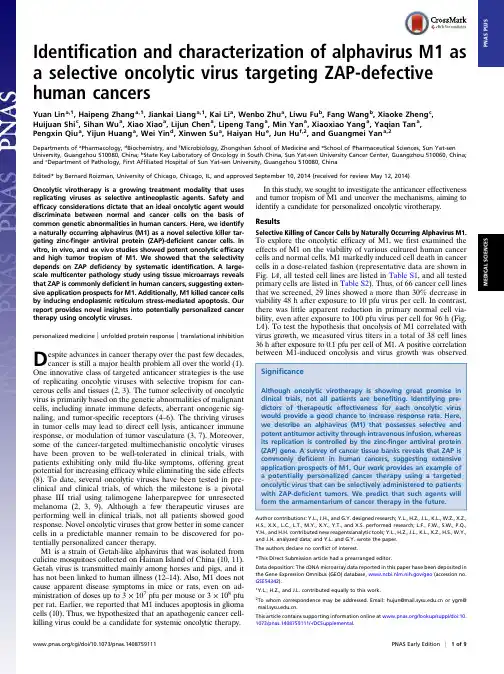
Identification and characterization of alphavirus M1as a selective oncolytic virus targeting ZAP-defective human cancersYuan Lin a,1,Haipeng Zhang a,1,Jiankai Liang a,1,Kai Li a,Wenbo Zhu a,Liwu Fu b,Fang Wang b,Xiaoke Zheng c,Huijuan Shi c,Sihan Wu a,Xiao Xiao a,Lijun Chen a,Lipeng Tang a,Min Yan a,Xiaoxiao Yang a,Yaqian Tan a,Pengxin Qiu a,Yijun Huang a,Wei Yin d,Xinwen Su a,Haiyan Hu e,Jun Hu f,2,and Guangmei Yan a,2Departments of a Pharmacology,d Biochemistry,and f Microbiology,Zhongshan School of Medicine and e School of Pharmaceutical Sciences,Sun Yat-sen University,Guangzhou510080,China;b State Key Laboratory of Oncology in South China,Sun Yat-sen University Cancer Center,Guangzhou510060,China; and c Department of Pathology,First Affiliated Hospital of Sun Yat-sen University,Guangzhou510080,ChinaEdited*by Bernard Roizman,University of Chicago,Chicago,IL,and approved September10,2014(received for review May12,2014)Oncolytic virotherapy is a growing treatment modality that uses replicating viruses as selective antineoplastic agents.Safety and efficacy considerations dictate that an ideal oncolytic agent would discriminate between normal and cancer cells on the basis of common genetic abnormalities in human cancers.Here,we identify a naturally occurring alphavirus(M1)as a novel selective killer tar-geting zinc-finger antiviral protein(ZAP)-deficient cancer cells.In vitro,in vivo,and ex vivo studies showed potent oncolytic efficacy and high tumor tropism of M1.We showed that the selectivity depends on ZAP deficiency by systematic identification.A large-scale multicenter pathology study using tissue microarrays reveals that ZAP is commonly deficient in human cancers,suggesting exten-sive application prospects for M1.Additionally,M1killed cancer cells by inducing endoplasmic reticulum stress-mediated apoptosis.Our report provides novel insights into potentially personalized cancer therapy using oncolytic viruses.personalized medicine|unfolded protein response|translational inhibition D espite advances in cancer therapy over the past few decades,cancer is still a major health problem all over the world(1). One innovative class of targeted anticancer strategies is the use of replicating oncolytic viruses with selective tropism for can-cerous cells and tissues(2,3).The tumor selectivity of oncolytic virus is primarily based on the genetic abnormalities of malignant cells,including innate immune defects,aberrant oncogenic sig-naling,and tumor-specific receptors(4–6).The thriving viruses in tumor cells may lead to direct cell lysis,anticancer immune response,or modulation of tumor vasculature(3,7).Moreover, some of the cancer-targeted multimechanistic oncolytic viruses have been proven to be well-tolerated in clinical trials,with patients exhibiting only mild flu-like symptoms,offering great potential for increasing efficacy while eliminating the side effects (8).To date,several oncolytic viruses have been tested in pre-clinical and clinical trials,of which the milestone is a pivotal phase III trial using talimogene laherparepvec for unresected melanoma(2,3,9).Although a few therapeutic viruses are performing well in clinical trials,not all patients showed good response.Novel oncolytic viruses that grow better in some cancer cells in a predictable manner remain to be discovered for po-tentially personalized cancer therapy.M1is a strain of Getah-like alphavirus that was isolated from culicine mosquitoes collected on Hainan Island of China(10,11). Getah virus is transmitted mainly among horses and pigs,and it has not been linked to human illness(12–14).Also,M1does not cause apparent disease symptoms in mice or rats,even on ad-ministration of doses up to3×107pfu per mouse or3×108pfu per rat.Earlier,we reported that M1induces apoptosis in glioma cells(10).Thus,we hypothesized that an apathogenic cancer cell-killing virus could be a candidate for systemic oncolytic therapy.In this study,we sought to investigate the anticancer effectiveness and tumor tropism of M1and uncover the mechanisms,aiming to identify a candidate for personalized oncolytic virotherapy. ResultsSelective Killing of Cancer Cells by Naturally Occurring Alphavirus M1. To explore the oncolytic efficacy of M1,we first examined the effects of M1on the viability of various cultured human cancer cells and normal cells.M1markedly induced cell death in cancer cells in a dose-related fashion(representative data are shown in Fig.1A,all tested cell lines are listed in Table S1,and all tested primary cells are listed in Table S2).Thus,of66cancer cell lines that we screened,29lines showed a more than30%decrease in viability48h after exposure to10pfu virus per cell.In contrast, there was little apparent reduction in primary normal cell via-bility,even after exposure to100pfu virus per cell for96h(Fig. 1A).To test the hypothesis that oncolysis of M1correlated with virus growth,we measured virus titers in a total of38cell lines 36h after exposure to0.1pfu per cell of M1.A positive correlation between M1-induced oncolysis and virus growth wasobserved Author contributions:Y.L.,J.H.,and G.Y.designed research;Y.L.,H.Z.,J.L.,K.L.,W.Z.,X.Z.,H.S.,X.X.,L.C.,L.T.,M.Y.,X.Y.,Y.T.,and X.S.performed research;L.F.,F.W.,S.W.,P.Q., Y.H.,and H.H.contributed new reagents/analytic tools;Y.L.,H.Z.,J.L.,K.L.,X.Z.,H.S.,W.Y.,and J.H.analyzed data;and Y.L.and G.Y.wrote the paper.The authors declare no conflict of interest.*This Direct Submission article had a prearranged editor.Data deposition:The cDNA microarray data reported in this paper have been deposited in the Gene Expression Omnibus(GEO)database,/geo(accession no. GSE54342).1Y.L.,H.Z.,and J.L.contributed equally to this work.2To whom correspondence may be addressed.Email:hujun@ or ygm@ .This article contains supporting information online at /lookup/suppl/doi:10. 1073/pnas.1408759111/-/DCSupplemental./cgi/doi/10.1073/pnas.1408759111PNAS Early Edition|1of9M E D I C A L S C I E N C E S P N A S P L U S(Fig.1B ),indicating that cancer-selective replication leads to the cancer-targeting property of M1.To further evaluate the in vivo antitumor potential of M1,we established three preclinical tumor models,including the Hep3B human hepatocellular carcinoma (HCC)s.c.xenograft model in BALB/c-nu/nu mice (Fig.1C and D ),the 4T1mouse breast cancer orthotopic model in immunocompetent BALB/c mice (Fig.1E ),and the B16mouse skin melanoma s.c.model in C57BL/6mice (Fig.1F ).After palpable tumors formed,mice in each model were randomized to receive either six doses of intratumoral injection (2×106pfu per dose)or two doses of i.v.infusion of M1(3×107pfu per dose).In parallel,mice were treated with vehicle as nega-tive controls.Consistent with the in vitro experiments,evident antitumor effects were observed in M1-treated animals.It is noteworthy that M1-treated mice remained asymptomatic throughout the treatment,and no obvious difference in body weight between control and M1-treated groups was detected (Fig.1C –F ).Moreover,to evaluate the safety and potential toxicity of M1,we i.v.injected two doses of M1(3×107pfu per dose)into immunocompetent BALB/c mice.All eight of the M1-injected mice survived until 27d postinjection,when they were killed.Body weight was measured every 3d.There was no significantdifference in body weight between control and M1-injected groups during the course of the study (Fig.S1A ).After autopsy,histological analyses of vital tissues,including brain,heart,kidney,liver,lung,skeletal muscle,and spleen,were performed by H&E staining.None of the M1-or mock-injected BALB/c mice showed any abnormal pathology (Fig.S1B ).Complete blood count (CBC)analysis showed decreased WBCs after M1injection,whereas other parameters of CBC analysis,including percentage of neu-trophil granulocytes,percentage of lymphocytes,RBC count,and platelet count,remained unchanged (Fig.S1C ).The observations of mortality,body weight,histopathology,and CBC analysis support the conclusion that M1is safe to animals.We proposed that the antitumor activity and safety of M1are based on high tumor tropism.To further assess the in vivo se-lectivity of M1,we established tumor xenografts with two HCC cell lines:Hep3B cells (sensitive to M1)on the left hind flank of nude mice and cell line PLC cells (resistant to M1)on the right hind flank of nude mice.When palpable tumors developed,mice were treated with one dose of i.v.-delivered M1(3×107pfu),and biodistribution of viral RNA genome was quantified within 96h postinfection by quantitative RT-PCR (qRT-PCR).As we expected,M1was more than 1,000times enriched inHep3BFig.1.Selective oncolytic efficacy of M1in vitro and in vivo.(A )Cell viability assays were performed on a panel of cancer cell lines and primary normal cells 48and 96h after exposure to M1,respectively.N,primary normal cell;T,tumor cell.(B )Viral titers (MOI =0.1pfu per cell;36h)and cell viability (MOI =10pfu per cell;48h)in various infected cell lines.Virus was collected from both supernatant and cell lysate;r is the Pearson correlation coefficient.(A and B )Values are means of three independent experiments.(C –F )Tumor growth (solid symbols)and body weight (open symbols)of tumor-bearing mice.(C and D )Nude,(E )BALB/c,and (F )C57BL/6mice were treated with either vehicle or M1intratumorally (i.t.)or i.v.(n =9per group).Data are shown in means ±SDs.(G and H )Biodistribution of systemically delivered M1.Viral RNA was quantified by qRT-PCR and normalized to the expression of β-actin.Means ±SDs are shown (n =6per group).ns,not significant;Tumor_R,PLC;Tumor_S,Hep3B.*represents not detectable results.2of 9|/cgi/doi/10.1073/pnas.1408759111Lin et al.Fig.2.M1triggers prolonged and severe ER stress-mediated apoptosis in susceptible cancer cells.(A)Observation of ER distension in Hep3B cells infected with M1by transmission EM.Middle shows higher magnification from the box in Top.(Scale bars:500nm.)Quantification of ER distension is also presented.(B)Observation of chromatin condensation in infected Hep3B cells by transmission EM.Red arrows,condensed chromatin;white arrows,nuclear envelope. (Scale bars:1μm.)Quantification of condensed nuclei is also presented.(A and B)Means±SDs from three independent experiments are shown.(C–F)The effect of M1on ER stress signal pathways.Western blot analyses of(C)BiP,(D)phosphorylated eIF-2α(S51),(E)phosphorylated JNK(Y183/Y185),and(F) cleaved casepase-12(Clv-casp-12)are shown.GAPDH andα-tubulin served as loading controls.The ratio between phosphorylated eIF-2αandα-tubulin was calculated.Pro-casp-12,pro-caspase-12.(D)Detection of protein synthesis after M1infection(MOI=10,12h)by L-AHA-biotin labeling and Western blot.(G and H)Caspase activity in Hep3B and LoVo cells treated with M1(MOI=1pfu per cell).CTL,control;hpi,hours postinfection.**P<0.05.Lin et al.PNAS Early Edition|3of9M E D I C A L S C I E N C E S P N A S P L U Stumor tissue than any other tissues tested(Fig.1G).Similar results can be observed in immunocompetent C57BL/6mice bearing B16melanoma(Fig.1H).The finding that the high level of viral RNA in sensitive tumor tissue remained stable for at least4d supports the conclusion that M1efficiently targets and selectively replicates in cancer cells.Tumor-Selective Replication of M1Induces Endoplasmic Reticulum Stress-Mediated Apoptosis in Cancer Cells.We next explored the mechanism whereby M1killed cancer cells.Transmission EM showed a progressive distension of endoplasmic reticulum(ER) lumen as early as6h post-M1infection in Hep3B cells(Fig.2A). At24h after M1treatment,catastrophic destruction of ER and condensation of chromatin were observed(Fig.2A and B),in-dicating that M1induced a prolonged and severe ER stress that mediated apoptosis(15).One consequence of ER stress is the synthesis of chaperones that help proteins to fold properly(16, 17).Western blot analyses showed that one of these chaperones, BiP(an HSP70molecular chaperone,the induction of which is commonly used as a marker of ER stress),was strongly increased after M1infection(Fig.2C).Another symbolic event of ER stress is the phosphorylation of eIF-2α(eukaryotic translation initiation factor2,subunit alpha)and subsequent translational inhibition,helping to alleviate the load of unfolded proteins(17). To test the effect of M1on host translational machinery,newly synthesized proteins were labeled with L-azidohomoalaine-biotin (L-AHA,which is an analog of methionine)and detected by Western blot using HRP-conjugated antibiotin antibody.We observed significant phosphorylation of eIF-2αand the corre-sponding inhibition of host protein synthesis by M1treatment(Fig. 2D).We also examined the induction kinetics of PERK(protein kinase R-like ER kinase)and PKR(protein kinase R)after M1 infection and observed that PERK expression was significantly induced by M1infection in a time-dependent manner,whereas the induction of PKR expression was not remarkable(Fig.S2),sug-gesting that eIF-2αphosphorylation was mainly stimulated by ER stress-activated PERK.In contrast to the results obtained in sen-sitive cancer cells,M1did not cause increase in BiP,phosphory-lation of eIF-2α,or translation inhibition in L-02normal liver cells (Fig.2C and D).Similarly,pronounced phosphorylation of eIF-2αwas not observed in M1-infected primary normal hepatocytes(Fig. S3).Translation of alphavirus mRNA has been shown to be re-sistant to eIF-2αphosphorylation because of the highly stable RNA hairpin loop located downstream of the AUG initiator co-don(18).Thus,the high production of M1viral protein triggers prolonged and severe ER stress in sensitive cancer cells.We next examined the ER stress-induced apoptotic pathways (19–21).Western blot analyses revealed that the JNK pathway and caspase-12cascades were activated by M1infection(Fig.2E and F)in susceptible cancer cells,whereas C/EBP(CCAAT-enhancer–binding protein)homologous protein was not induced(Fig.S4). Conversely,both JNK signal and caspase-12activity remained unchanged in L-02cells after M1infection,which would be expected by the absence of M1-induced ER stress(Fig.2E and F). We next tested the downstream caspase cascades in M1-suscep-tible cancer cells by detecting the activity of caspase-9and apo-ptotic executioner caspase-3.Both caspases were activated after M1infection(Fig.2G and H),indicating that the M1-induced ER stress leads to apoptotic cell death.Systematic Identification of Host Factors That Contribute to Tumor Tropism of M1.The finding that M1preferentially replicated in and killed cancer cells urged us to probe the molecular mecha-nism of M1selectivity.Given that type I IFNs are well-known factors triggering antiviral effect against a broad range of viruses (22),we investigated whether IFN signal is involved in M1se-lectivity.Indeed,pretreatment with type I IFNs conferred re-sistance to M1in sensitive cancer cells(Fig.S5A).However,type I IFNs were not induced after M1infection in resistant cells(Fig. S5B),because it was reported that type I IFNs were not induced by alphavirus(at least at early time points)(23).Consistently, inhibition of type I IFNs signaling using IFN-αand IFN-βneu-tralizing antibodies or siRNA targeting IFN-αreceptor subunit IFNAR1did not affect the resistance to M1(Fig.S5C and D). These observations suggest that resistant cells do not exploit type I IFNs to establish the antiviral state against M1.We also found that M1viral RNA and protein levels increased dramatically as early as4h after infection in Hep3B cells but not L-02cells(Fig.3A and B),indicating that constitutively expressed intracellular antiviral factors are responsible for the resistanceof Fig.3.Expression profile and RNAi screening identify zinc-finger antiviral protein(ZAP)as a host factor that contributes to tumor tropism of M1.(A)L-02and Hep3B cells were treated with M1(MOI=10pfu per cell)for1–4h.The levels of viral genomic RNA and endogenous controlβ-actin were analyzed by qRT-PCR.The graph shows the means±SDs of the relative level of expression(normalized to endogenous controls)obtained in three independent experiments.(B)Western blot analysis of parallel samples from A.The protein levels of viral structural protein E1and nonstructural protein NS3were determined,and β-actin served as a loading control.(C)Schematic representation of systematic identification of host factors that regulate M1replication.(D)The results of the screen are shown with the siGENOME siRNA pools ranked in order of z score from lowest(decreased cell count)to highest(increased cell count).The position of ZAP is indicated.(E)Phase–contrast images of L-02cells treated first with siRNA(48h)followed by M1infection(MOI=30pfu per cell;48h)and crystal violet(0.1%)staining.CTL,control;DB,database;hpi,hours postinfection;siNC,negative control siRNA.(Scale bars:100μm.)4of9|/cgi/doi/10.1073/pnas.1408759111Lin et al.L-02cells.Therefore,we compared the transcriptional profiles of these two cell lines to identify candidate cell-encoded suppressors of M1replication.Considering that gene products in the IFN pathway are frequently defective in cancer (5,24,25)and IFN-stimulated genes (ISGs)are crucial antiviral effectors against alphavirus (26),we compiled a list of 317IFN-related genes (IRGs)from published data (the inclusion criteria are stated in Fig.3C and Table S3,and the expressions of IRGs are listed in Table S4).The IRGs with twofold-higher basal expression in L-02cells compared with Hep3B cells were submitted to the DAVID bioinformatics online tool (/)(27)for functional anal-ysis;53candidate genes were identified because of their previously reported antiviral effects.To test the antivirus effects against M1,we used an arrayed library of siRNA pools to target 53candidate genes in L-02cells (Fig.3C ).siRNA-transfected cells were either mock-infected or infected with M1(30pfu virus per cell)for 48h.Morphological changes were observed,and cell numbers were counted after crystal violet staining.We analyzed data from three independent screenings.Subtracting those genes with siRNA alone that was cytotoxic,we identified ZAP as a host factor against M1(Fig.3D and E and Table S5).ZAP Deficiency Is Necessary for the High Tumor Specificity of M1.ZAP is an ISG that inhibits the replication of certain viruses by inducing viral RNA degradation and translational inhibition (28–30).To investigate the role of ZAP,we examined the expression of ZAP in eight cell lines,including four M1-resistant cell lines and four M1-sensitive ones.We observed significantly reduced amounts of ZAP mRNA and protein levels in all four susceptible cells (Fig.4A and B ).In light of the evidence that ZAP is defective in M1-susceptible cells,we used gene silencing to address the contribution of ZAP to the antiviral state of resistant cell lines.Specifically,L-02,PLC,or cell line HCT 116cells were transfected with either a ZAP-specific siRNA or a nontargeting siRNA control.After 48h,the cultures were exposed to M1,and virus replication and cell viability were measured 48h after infection.The results showed that de-pletion of ZAP overcomes the resistance to M1in that it leads to increased viral replication,viral RNA,viral protein expression,and M1-induced cell death (Fig.4C –F ).The silencing efficiency was >80%according to Western blot analyses (Fig.4F ).The next question that we posed is whether ectopic expression of ZAP is able to confer resistance to M1.Consistently,susceptible cells transfected with vectors expressing ZAP showed decreased viral yield,decreased viral RNA and protein expressions,and fi-nally,suppressed viral oncolysis compared with negativecontrolFig.4.The sensitivity of cancer cells to M1requires ZAP deficiency.(A )mRNA levels of ZAP in different cell lines normalized to the expressions of β-actin and TBP.Means ±SDs of three independent experiments are shown.(B )Protein levels of ZAP in different cells.β-actin was used as a loading control.(C –F )Resistant cells transfected with siNC or siZAP were infected with M1for 48h.(C )Cell viability evaluated by MTT assay,(D )viral yield determined by TCID 50assay,(E )viral RNA quantified by qRT-PCR,and (F )viral protein analyzed by Western blot are shown.(G –J )Sensitive cells were transfected with plasmids expressing GFP (negative control)or ZAP for 48h and infected with M1for 48h.(G )Cell viability,(H )viral yield,(I )viral RNA,and (J )viral protein were measured by respective methods.Data are means ±SDs from three independent experiments.(C –E and G –I )All are compared with respective control groups.(C and G )Each color represents one cell line.ND,not detectable;ns,not significant;siNC,negative control siRNA;TBP,TATA box binding protein;TCID 50,median tissue culture infective dose.*P <0.05;**P <0.01;#P <0.05;##P <0.01;&P <0.05;&&P <0.01.Lin et al.PNAS Early Edition |5of 9M E D I C A L S C I E N C E SP N A S P L U S(GFP)(Fig.4G–J).Thus,we showed that ZAP is a host inhibitor that restrains M1replication and that M1specifically targets cancer cells carrying ZAP deficiency.Selective Oncolysis of M1Against Human ex Vivo Cancer Tissues Is ZAP Deficiency-Dependent.To validate the ZAP deficiency-dependent antitumor efficacy of M1,we carried out ex vivo experiments on primary human liver and colon tumor surgical samples by tumor histoculture end-point staining computer image analysis(TECIA) (31,32).Consistent with the in vitro and in vivo oncolytic effects, in23of35(66%)liver cancer samples and9of12(75%)colon cancer samples,exposure to M1triggered a decrease in the via-bility of cultured tumor tissue(percentage of inhibition>10%) (Fig.5A and B),supporting the therapeutic potential of M1against human cancers.Additionally,low mRNA levels of ZAP in tumor tissues cor-related to high ex vivo oncolytic efficacy of M1(Fig.5C).This correlation provided additional support to the hypothesis that the selective antineoplastic effect of M1virus is dependent on ZAP deficiency and indicated that ZAP deficiency may serve as a biomarker for response to M1oncolytic virotherapy.ZAP Deficiency Is Common in Human Cancers.To elucidate the po-tential for personalized therapy of M1for human cancers,we conducted a large-scale multicenter molecular pathology study of ZAP expression in various cohorts of human cancer specimens. ZAP immunohistochemistry(IHC)was performed on eight tissue microarrays(TMAs)containing paired tumor and adjacent non-neoplastic clinical specimens from506patients.ZAP expression was represented by mean staining intensity that was calculated using Imagescope software(Aperio).Overall,69%of liver cancer, 52%of colon cancer,and61%of bladder cancer TMAs showed low levels of ZAP in tumor tissue compared with respective noncancer tissue(Fig.6),implying that ZAP may be a biomarker for liver,colon,and bladder cancer and that M1may serve as a potential oncolytic agent for personalized cancer therapy. DiscussionOver the last several decades,increased understanding of mo-lecular virology and oncology has made it possible for us to select and/or tailor novel viruses for anticancer virotherapy(4).Here, we identify a naturally occurring alphavirus M1as a selective oncolytic agent targeting ZAP-deficient cancer cells.The onco-lytic effect of M1is potent and selective in that it kills a diverse range of cancer cell lines without inducing toxicity in primary normal cells.In addition,M1is efficacious in three aggressive, chemotherapy-refractory,preclinical tumor models on systemic infusion or intratumoral injection.To reveal M1as a clinically relevant therapeutic agent,we show that M1inhibits viability of primary human hepatic and colorectal tumor explants.Two factors are critical for oncolytic virotherapy,including effective delivery to tumor tissues and rapid virus growth within tumor sites(33).We have found that i.v.administration of M1is an effective means of delivering virus to tumor,and because of its high tumor tropism,M1thrives only within the tumor tissue. As a consequence,M1is exceptionally safe to the treated animals (M1does not cause mortality in immune-competent mice or rats, and all examined animals remained asymptomatic throughout the treatment)and may target metastatic tumors.It is of great use in the clinic to elucidate the molecular mech-anism of tumor tropism and identify biomarkers that predict an-titumor efficacies for each oncolytic virus(8).However,although plenty of natural and genetically engineered viral oncolytic agents have been developed,only few reports specified the mechanism of selectivity,including that reovirus requires an activated oncogenic Ras signaling(34)and that vesicular stomatitis virus(VSV)re-quires defects in IFN pathway(35).We hereby show that the resis-tance to M1in L-02and HCT116cells is type I IFN-independent (Fig.S5).Instead,we provide conclusive evidence that ZAP de-ficiency,which is common in human cancers,is essential for M1-selective replication and oncolysis in cancer cells,suggesting a great potential for personalized cancer therapy.One of the advantages of M1for human cancer treatment is that tumor biopsies can be prescreened for expression of ZAP,thus decreasing costs and ex-pediting the treatment of cancer patients.Our study also estab-lishes a successful model for identification of predictors of response to oncolytic virus using comparative expression profiling,functional screening,and TMA.We postulate that this model could add the breadth of opportunities for discovering novel markers that predict effectiveness to oncolytic virotherapy.It has been well-studied that ZAP is a host ISG that inhibits the replication of alphaviruses(28),filoviruses(36),and retro-viruses(37)but does not affect growth of other viruses,including VSV,poliovirus,yellow fever virus,and HSV-1(28).ZAP binds to viral RNA and recruits mRNA degradation machinery,lead-ing to decreased levels of viral RNA(38).ZAP also blocks translation of Sindbis viral RNA(28).We have found that both M1viral RNA and protein levels are dampened after ectopic expression of ZAP in susceptible cancer cell lines and vice versa, indicating that the production of M1is caused by the lack of ZAP-mediated antiviral activity(most likely viral RNA degra-dation but not excluding translational inhibition). Nevertheless,antitumor activity of a certain oncolytic virus differs among cancer cell lines(39).Our data also confirm that some cancer cells show poor response to M1(Table S1).Clearly, there are great opportunities to potentiate oncolytic efficiency by practical tactics,including use of chemical molecules tosensitize Fig.5.The ex vivo antineoplastic effect of M1depends on ZAP deficiency.(A and B)Ex vivo antitumor effect of M1on clinical tumor explants.Surgical(A) liver and(B)colon cancer specimens were divided into∼1-mm3particles and treated with M1(2×107pfu),vehicle,or HgCl2.Tissue viability was assessed by TECIA after MTT staining.(C)ZAP mRNA expression(normalized to the expression ofβ-actin)in parallel samples from A and B.Box-and-whisker plots showing median(horizontal line),interquartile range(box),and maximum/minimum range(whiskers)of the data.Resistant,M1-induced inhibition≤10%(n=12); Sensitive,M1-induced inhibition>10%(n=17).6of9|/cgi/doi/10.1073/pnas.1408759111Lin et al.cancer cells to oncolytic virus and exploitation of gene-armed therapeutic viruses.Some studies reported the enhanced oncolytic efficacy through rational design of combinational therapies (40).The use of com-bination therapeutic strategy would largely decrease the dosage of oncolytic virus and chemical drug,thus reducing the side effects and costs.Elucidation of molecular details of oncolytic agents could provide a breakthrough in the development of therapeutic strategies combining oncolytic viruses with small molecules.Some chemovirus combination therapies have been reported,including that histone deacetylase (HDAC)inhibitors enhance oncolysis of HSV or VSV by suppressing innate immunity (40),inositol-requiring enzyme 1(IRE1-α)inhibitors boost oncolytic efficacy of Maraba virus by inhibiting the ER stress response (41),and Smac mimetic compounds promote antitumor efficacy of VSV by exploiting the virus-stimulating cytokine storm (42).Understanding the molecular biology of M1-induced ER stress and subsequent cell death will help us to discover synergic compounds for combination therapy,such as IRE1-αinhibitors inducing ER stress (41).We are currently exploring the use of multiple ER stress inducers,some of which are in clinical trials,to facilitate the effectiveness of M1.Arming oncolytic viruses with therapeutic genes has been proven to be a successful strategy to increase the potency of these viruses (43).Additionally,previous work indicated that expression vectors based on alphaviruses (such as Sindbis virus and Semliki Forest virus)have been used extensively (44),and novel replication-competent vectors are being investigated for potential therapeutic applications (45,46).Thus,M1can be further armed with several complementary therapeutic proteins (e.g.,GM-CSF or IL-12)or noncoding RNAs to enhance the oncolytic efficacy mostly but not exclusively by unleashing anticancer immune response (7,8).Overall,our findings highlight an example of a potentially personalized cancer therapy using a targeted oncolytic virus that can be selectively administered to patients with ZAP-defective tumors.We predict that such agents will form the arsenal for the war on cancer in the future.Materials and MethodsCell Culture.Cell lines were purchased from American Type Culture Collection,Shanghai Institute of Cell Biology,and Guangzhou Institute of Biomedicine and Health.Cells were cultured in DMEM,RPMI-1640,or F-12supplemented with 10%(vol/vol)FBS and 1%penicillin/streptomycin (Life Technologies).Primary normal cells were purchased from ScienCell Research Laboratories and cultured according to instructions.Primary cancer cells were isolated from surgical tumor tissues using 0.1%trypsin.Specimens were obtained from consenting patients who underwent tumor resection.The institutional review board of Sun Yat-sen University Cancer Center has approved all human studies.Virus.M1was grown in Vero cells.Virus titer was determined by TCID 50assay using BHK-21cells and converted to pfu.The variant of M1in this study was described previously (10).Cell Viability Assay.Cells were seeded in 96-well plates at 4,000cells per well in 0.1mL media.After treatment,3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)was added to cells (1mg/mL final con-centration),and cells were allowed to grow at 37°C for another 3h.MTT-containing media were removed,and MTT precipitate was dissolved in 100μL DMSO.The optical absorbance was determined at 570nm using a microplate reader (iMark;Bio-Rad).Animal Models.This study was approved by the Animal Ethical and Welfare Committee of Sun Yat-sen University.For the intratumoral injection model,5×106Hep3B cells were inoculated s.c.into the hind flank of 4-wk-old female BALB/c-nu/nu mice.After 4d,palpable tumors developed (50mm 3),and mice were randomized to receive six doses of either M1(2×106pfu per dose)or vehicle intratumorally within 10d.Tumor length and width were measured every other day,and the volume was calculated according to the formula (length ×width 2)/2.Mice were weighed every other day.The observers were blinded to the group allocation.For evaluation of systemic antitumor effect,Hep3B s.c.xenografts were developed as described above,2×1064T1mammary carcinoma cells were injected orthotopically into the inguinal mammary fat pads of 6-wk-old fe-male BALB/c mice,and 2×106B16melanoma cells were inoculated s.c.into the hind flank of 6-wk-old female C57BL/6mice.After 3–5d,each animal was injected i.v.two times 3d apart with either M1(3×107pfu per dose)or vehicle.Tumor volume was calculated,and body weight was measured every 3d.The study was randomized and single blind.For the M1biodistribution study,5×106Hep3B and PLC HCC cells were injected s.c.into the left and right hind flanks,respectively,of 4-wk-old female BALB/c-nu/nu mice.After 4d,each animal received i.v.delivery of 3×107pfu M1.Mice were killed 1–4d after M1injection,and presence of virus was quantified by qRT-PCR from tissue samples,including tumors,brain,heart,kidney,liver,lung,muscle,and spleen.Similar experiments were performed with B16melanoma cells in 6-wk-old female C57BL/6mice.For the safety evaluation study,6-wk-old female BALB/c mice were i.v.-injected with two doses of either M1(3×107pfu per dose)or vehicle.Mice were weighed every 3d.After euthanasia,blood samples were submitted to the clinical laboratory of the First Affiliated Hospital of Sun Yat-sen University for CBC analysis,and vital tissues (including brain,heart,kidney,liver,lung,skeletal muscle,and spleen)were histologically analyzed after H&Estaining.Fig.6.Distribution of ZAP deficiency in clinical cancer specimens.(A )Representative cores of ZAP immunostaining in TMA.Higher magnification shown in the box.(Scale bars:50μm.)(B )Statistical analysis of IHC staining intensity.Box-and-whisker plots showing median (horizontal line),interquartile range (box),and 5th –95th percentiles (whiskers)of the data.Dots indicate outliers.***P <0.001.(C )Distribution of ZAP deficiency in cancers.N,nonneoplastic;T,tumor.Lin et al.PNAS Early Edition |7of 9M E D I C A L S C I E N C E SP N A S P L U S。
mAbs:自身免疫性疾病的潜在治疗抗体2014年10月28日讯/生物谷BIOON/ --通过天然免疫选择和靶向蛋白技术的组合,A * STAR研究者已经制造出一种抗体,能够在人类细胞和小鼠实验模型中有效地阻断与疾病相关的炎症通路。
感染或受伤事件发生后,信号蛋白白细胞介素1β(IL-1β)帮助免疫系统进行快速免疫反击。
然而,过量的IL-1β活性可导致有害的炎症,促进疾病状态如各种自身免疫性疾病。
IL-1β抑制剂是药物研发的活跃区域,Cheng-I Wang和同事最近生成IL-1β特异性抗体,这可能是解决炎症性疾病的关键。
哺乳动物免疫系统已经进化能产生抗体,能结合外来分子,并且具有显著的亲和性和特异性。
Wang和同事们利用蛋白质工程,获得一个有前途的抗体,被证明能够结合并抑制人类和小鼠的IL-1β。
研究人员集中在抗体的一小部分氨基酸,即可能有助于抗体结合IL-1β的氨基酸,随机置换这些氨基酸位点并产生抗体变体的一个库。
通过筛选该抗体变体库,Wang和同事获得性能显着提高的抗体,得到了20〜50倍更好亲和力的抗体变体。
这些抗体的最好变体是P2D7,其在抑制IL-1β上比康纳单抗(市售消炎药)更有效。
康纳单抗和P2D7绑定相同的蛋白质,但识别相同分子上不同位点。
此外,P2D7结合至小鼠和猴子版本的IL-1β蛋白,并具有高亲和力的,而康纳单抗却没有此功效。
研究人员利用小鼠模型显示,P2D7能对抗关节炎和腹膜炎症状,甚至延长了已经注射了人骨髓瘤细胞动物的存活。
(生物谷)本文系生物谷原创编译整理,欢迎转载!转载请注明来源并附原文链接。
谢谢!doi:10.4161/mabs.28614PMC:PMID:A novel human anti-interleukin-1βneutralizing monoclonal antibody showing in vivo efficacyGoh, A. X. H., Bertin-Maghit, S., Yeo, S. P., Ho, A., Derks, H. et al.The pro-inflammatory cytokine interleukin (IL)-1βis a clinical target in many conditions involving dysregulation of the immune system; therapeutics that block IL-1βhave been approved to treat diseases suchas rheumatoid arthritis (RA), neonatal onset multisystem inflammatory diseases, cryopyrin-associated periodic syndromes, active systemic juvenile idiopathic arthritis. Here, we report the generation and engineering of a new fully human antibody that binds tightly to IL-1βwith a neutralization potency more than 10 times higher than that of the marketed antibody canakinumab. After affinity maturation, the derived antibody shows a >30-fold increased affinity to human IL-1βcompared with its parent antibody. This anti-human IL-1βIgG also cross-reacts with mouse and monkey IL-1β, hence facilitating preclinical development. In a number of mouse models, this antibody efficiently reduced or abolished signs of disease associated with IL-1βpathology. Due to its high affinity for the cytokine and its potency both in vitro and in vivo, we propose that this novel fully human anti-IL-1βmonoclonal antibody is a promising therapeutic candidate and a potential alternative to the current therapeutic arsenal.Cancer Cell:癌症外染色体微小分子新功能来源:生物谷2014-10-28 18:092014年10月28日讯/生物谷BIOON/ --近日研究发现,通过癌细胞释放的外染色体、微小的病毒型颗粒可以表达导致肿瘤生长的微RNA分子。
第 43 卷第 1 期2024年 1 月Vol.43 No.1Jan.2024中南民族大学学报(自然科学版)Journal of South-Central Minzu University(Natural Science Edition)近红外光协同免疫疗法增强抗肿瘤效果研究进展祝红达,杨朝波,刘阅,张子林,马凯,关业能(湖北工业大学a. 生物工程与食品学院;b. 发酵工程教育部重点实验室;c. 工业微生物湖北省重点实验室,武汉430068)摘要肿瘤免疫疗法虽然在一定程度上克服了传统疗法存在的复发可能性大的问题,但也存在应答率低、部分患者不良反应大的局限性. 近红外光可以直接或间接激活免疫系统,且可实时成像进而监测治疗效果及评估在治疗过程中产生的不良反应,因此近红外光协同下的免疫疗法可增强抗肿瘤效果、降低各自单独使用时所引起的不良反应,是一种非常有前景的治疗方法. 故对近年来近红外光协同的免疫激活治疗肿瘤的设计策略、应用、问题及对策方面进行了综述.关键词近红外光;免疫疗法;协同效应;肿瘤治疗中图分类号R73-36 文献标志码 A 文章编号1672-4321(2024)01-0037-08doi:10.20056/ki.ZNMDZK.20240106Research progress of near-infrared light synergistic immunotherapy forenhancing anti-cancer effectZHU Hongda,YANG Chaobo,LIU Yue,ZHANG Zilin,MA Kai,GUAN Yeneng(Hubei University of Technology a. College of Bioengineering and Food; b. Key Laboratory of Fermentation Engineering,Ministry of Education; c. Hubei Key Laboratory of Industrial Microbiology, Wuhan 430068, China)Abstract Although tumor immunotherapy can reduce the possibility of recurrence of cancer of traditional chemotherapy,it has a low response rate for some poorly immunogenic tumors. Near infrared light can directly or indirectly activate the immune system, monitor the treatment effect and evaluate the adverse reactions through real-time imaging in the treatment process. Therefore,near infrared light combined with immunotherapy not only enhances the anticancer effect,but also reduces the adverse reactions, which has potential clinical application value. This review summaried the design strategy,application, problems and countermeasures of near-infrared light synergistic immune activation in the treatment of tumors. Keywords near-infrared light; immunotherapy; synergistic effect; cancer therapy传统的肿瘤治疗方法(手术、化疗和放疗)在本质上都是局部直接根除肿瘤细胞和组织,虽有一定的疗效但通常难以治愈,特别是化疗由于靶向性差造成的副作用严重,还会导致免疫系统功能的降低. 近年来肿瘤免疫疗法得到极大的发展,如免疫检查点抑制剂、细胞因子、癌症疫苗等,其通过活化免疫细胞激活免疫系统达到杀死肿瘤细胞的目的[1]. 2015年美国食品药品监督管理局(FDA)批准将免疫检查点抑制剂用于非小细胞肺癌的治疗,使其成为最耀眼的抗癌明星[2],但患者的实际响应率偏低,部分患者出现较严重的免疫相关不良事件(irAEs)[3]. 为了降低免疫疗法的副作用,许多研究试图用多种方法联合免疫疗法用于肿瘤的治疗,其中光疗特别是近红外光(650~1700 nm)由于其优异的光物理学参数在医学领域的诊断与治疗方面被广泛关注. 首先,近红外光以非电离方式进行辐收稿日期2021-08-12作者简介祝红达(1974-),女,副教授,博士,研究方向:药物及活性成分的递送系统,E-mail:*********************基金项目中国临床肿瘤学会江苏恒瑞肿瘤研究基金资助项目(Y-H2019-0325);湖北工业大学绿色工业科技引领计划自主探索项目(202015)第 43 卷中南民族大学学报(自然科学版)射,不会对组织造成明显的伤害及遗传毒性[4];其次,用于近红外的设备与辐射设备相比要便宜得多[5];最后,近红外激光在医学领域已有数十年的发展,其安全性和方法理论有一定的保障[6],这些优势给予近红外光以巨大的临床应用潜能. 近红外光联合免疫疗法策略不仅增强了原发肿瘤细胞的凋亡,远端肿瘤和肿瘤转移也被明显抑制[7]. 本文对近年来近红外光协同免疫疗法增强抗肿瘤的设计策略、应用、现存问题及未来展望进行综述.1 近红外光协同免疫疗法的设计策略1.1 光热疗法协同免疫治疗光热治疗(PTT)是基于能够将光能转换为热能的光热转化剂的一种治疗方法,其靶向肿瘤细胞后,在近红外光的照射下光热转化剂吸收光子能量使其从基态单重态转化为激发单重态,激发的光热试剂通过与周围分子之间的碰撞返回基态,动能的增加会导致肿瘤部位周围微环境温度升高而消融肿瘤细胞[8],造成肿瘤细胞的DNA及蛋白质等的不可逆损坏而抑制肿瘤细胞的生长[9];同时肿瘤细胞凋亡产生免疫原性细胞死亡(ICD),释放损伤相关的分子模式(DAMPs)[10],刺激树突状细胞(DC)的成熟并激活杀伤性的免疫细胞、提高相关细胞因子表达水平[11](图1). 目前研究较多的光热转化剂有CuS[12]、金纳米粒子[13]、有机聚合物[14]及小分子染料[15]等.佐剂的加入可以改善免疫细胞的功能[16],因此PTT与免疫佐剂的联合使用成了近年来治疗远端肿瘤的研究热点. Guo 等[11]设计了基于壳聚糖包裹的可生物降解中空CuS纳米颗粒包载免疫佐剂寡聚脱氧核苷酸(CpG),该纳米粒子治疗平台结合了PTT 和免疫治疗,光热消融诱导的肿瘤细胞死亡抑制肿瘤的生长,而免疫佐剂则增强宿主的抗肿瘤免疫. 结果表明联合光热免疫治疗比免疫治疗或单独光热治疗对初次治疗和远端未治疗的肿瘤更有效.PAN等[17]选用抗原卵清蛋白(OVA)包裹小分子染料吲哚菁绿(ICG)构建OVA-ICG纳米疫苗并评价在动物实验中肿瘤光热免疫治疗效果[18]. 结果显示该纳米疫苗具有抗原载药率高(80.8%)、产率高(>90%)、近红外吸收和荧光强、重复性好、稳定性好、生物相容性好等优点;在标记/跟踪DC方面较灵敏,能够协同光热免疫治疗肿瘤并有效地预防肿瘤. 该策略为大规模、重复制备高抗原负载率的多功能纳米疫苗用于肿瘤治疗提供了一种较为简便可靠的方法.除免疫佐剂外,针对免疫检查点抑制剂如PD-L1和抗CTLA4抗体也可以极大地增强PTT介导免疫反应[19-20]. 原位自体癌症疫苗(inCVAX)[21]由于抗原来自癌细胞本身,丧失了增值活性,保留了免疫原性,这使得其在联合PTT时对不同的癌症均有疗效[22]. 将免疫佐剂和免疫检查点抑制剂合用于PTT 治疗可综合各自的优势而产生协同作用[18].1.2 光动力疗法协同免疫治疗光动力治疗(PDT)被认为是癌症的一种替代疗法. 光敏剂在光照条件下吸收光子变为激发电子态,能量发射为荧光、热和/或其他形式的光物理能量,如产生自由基及其离子并将能量传递给肿瘤细胞部位的氧气而产生具有细胞毒性的活性氧(ROS),特别是高活性的单线态氧(1O2)达到抗肿瘤目的[8],这样的特征使得其在癌症的治疗中发挥着重要的作用. 在肿瘤部位PDT介导肿瘤细胞对免疫的响应如图2所示[23]:首先在近红外光的照射下产生大量的ROS导致细胞凋亡,而凋亡的肿瘤细胞会募集单核细胞等具有清除功能的细胞同时诱导部分细胞因子的释放,将单核细胞转化为肿瘤相关巨噬细胞(TAM),而TAM对小分子药物、尺寸较大的颗粒等有一定的吞噬作用,这使得光敏剂在TAM中富集成为可能[24],在PDT作用下,光敏剂将肿瘤部位的氧气转化为可以杀灭癌细胞的单线态氧(1O2),死亡的癌细胞作为抗原刺激免疫细胞的活化激活免疫反应.将疫苗[25]、免疫检查点抑制剂[26]、IDO酶抑制剂[27]、酸性神经酰胺酶抑制剂[28]等用于抗肿瘤研究时发现,在PDT作用下可以明显激活免疫系统增强抗肿瘤活性. XU等[29]设计一种基于上转换纳米颗粒(UCNPs)的多功能纳米粒子UCNP-Ce6-R837,不仅可以用于近红外诱导的PDT直接杀伤肿瘤细胞,还可以通过触发树突状细胞的成熟和细胞因子的分泌刺激免疫应答. 这种基于UCNP-Ce6-R837的PDT结合临床批准的CTLA4免疫检查点阻断疗法抑制调节性T细胞(Treg)的活性,能够有效地消除原发肿瘤,在免疫反应的作用下有效抑制远端肿瘤;此外该光动纳米粒子能诱导记忆T细胞的成熟产生长期免疫记忆效应进而有效防止肿瘤的复发. 该研究证明了以UCNP为基础的PDT与肿瘤免疫治38第 1 期祝红达,等:近红外光协同免疫疗法增强抗肿瘤效果研究进展疗相结合在消除原发肿瘤、抑制远处肿瘤、防止肿瘤复发方面具有显著的协同治疗效果.在临床应用方面,PDT 从1970年开始用于临床治疗,因其良好的重现性、选择性、低毒性以及微创等特点而被FDA 批准用于晚期的癌症患者[30],推荐用于不能手术的癌症患者[31].1.3 光化学疗法协同免疫治疗在低能量的近红外光作用下硅酞菁衍生物IRDye700DX (IR700)发生光致反应,能引起细胞膜的应激反应,使跨膜靶蛋白损伤而降低细胞膜的完整性导致细胞死亡[32]. NAGAYA 等[33]构建基于近红外光免疫治疗(NIR -PIT )的复合体(APC )IR700,其在690 nm 近红外光的激活下可增强抗肿瘤的治疗. 采用近红外光直接照射肿瘤细胞使其膨胀致细胞膜破裂,触发ICD 进而激活热休克蛋白70和90(HSP70/90)等应激物及死亡信号钙网蛋白(CRT )、 腺嘌呤核苷三磷酸(ATP )和高迁移率族蛋白B1(HMGB1)[34],这些物质协同促进DC 的成熟,随后在DC 的提呈作用下激发免疫反应[35],诱导CD8+T 细胞的增值杀死肿瘤细胞(图3). 复合体中光活性的染料IR700可与多种抗体结合,其本身无毒性且易通过尿液排出体外[34]. 复合物中抗体的靶向性使得NIR -PIT 具有很强的选择性,这也是该方法与传统肿瘤治疗方法的最大不同点,不会对正常的非靶向细胞造成明显的副作用[36].近红外光免疫治疗已经在靶向于EGFR 、HER2、GPC3等肿瘤治疗方面成功应用[33]. NAGAY 等[37]描述了NIR -PIT 的有效性,将靶向表达间皮素的A431/图1 光热治疗协同免疫治疗的原则概述[11]Fig.1 Overview of the principles of photothermal therapy combined with immunotherapy [11]39第 43 卷中南民族大学学报(自然科学版)图3 NIR -PIT 诱导的免疫原性细胞死亡激活免疫反应[35]Fig.3 NIR -PIT induced immunogenic cell death activates the immune response [35]图2 光动力疗法介导的免疫反应[23]Fig.2 photodynamic therapy mediated immune response [23]40第 1 期祝红达,等:近红外光协同免疫疗法增强抗肿瘤效果研究进展H9细胞的人源化抗体(hYP218)偶联到光吸收剂IR700上并与细胞共同孵育. 体外实验表明hYP218-IR700有细胞特异性杀伤作用. 荷瘤小鼠动物实验结果表明hYP218-IR700具有较高的肿瘤聚集率和较高的肿瘤背景比(TBR),近红外光照射组的肿瘤生长受到明显的抑制.1.4 近红外荧光成像协同免疫治疗如1.2所述,光敏物质在近红外光照条件下吸收光子变为激发电子态后能够将能量发射为荧光或磷光,这使得近红外成像可以和多种光谱、多种治疗方法联合使用对复杂的免疫系统成像[38]. 与可见光相比,近红外光特别是第二近红外(NIR-II)具有更高的信号背景比(SBR)、更高的灵敏度以及成像的高分辨率等[39],这些特性赋予近红外光以优异的成像能力. 因此采用合适的荧光团标记抗体[40],疫苗[41],免疫细胞(T细胞[42],B细胞[43],巨噬细胞[38],DC细胞[44],NK细胞[45])制备成探针,再利用近红外荧光成像可以实现免疫相关生物分子的实时监控[46],可以确定它们的生物分布及表达水平从而评估治疗效果,为治疗过程的安全性提供保障.WAN等[47]将荧光团(IR-BGP6)通过共价结合的方式结合到程序性细胞死亡配体-1单克隆抗体(PD-L1 mAb)上制备成探针(anti-PD-L1-BGP6),分析了不同细胞系内PD-L1的表达水平,实现了非侵入性的体内分子成像. 肿瘤与正常组织信号背景比高达≈9.5,与在组织内非特异性蓄积的NIR-II荧光团相比,IR-BGP6标记的PD-L1显著提高分子成像性能,并且该荧光团能够在肾脏快速排泄(在注射后10 h内一般91%通过尿排出)不会引起蓄积毒性.1.5 多种光疗协同免疫的复合疗法多种光疗协同免疫的复合疗法是当前研究的热点,一方面是复合疗法在发挥疗效的同时也能大大降低对正常组织的伤害,另一方面得益于纳米技术和材料科学的飞速发展,基于纳米材料的光疗可能达到最佳的治疗效果. 单一的光照治疗方式可能无法完全杀死肿瘤细胞而导致肿瘤细胞转移,多种光疗协同作用下可以产生足够的抗原物质[48],再辅以免疫治疗可以进一步增强抗肿瘤活性同时防止复发. 多种光疗协同治疗可以在完全消融癌细胞的前提下使PTT更温和地升温而避免对正常组织的损伤,降低PDT光敏剂可能带来的毒副作用,可视化治疗过程控制治疗效果及避免对正常细胞的损害. HAN等[49]开发了一种超低强度近红外光同步激活的协同Chemo/PTT/PDT纳米平台,该纳米平台由高发射上转换(UC)核、二氢卟吩e6(Ce6)光敏剂和抗癌药物盐酸阿霉素(DOX)共负载于介孔二氧化硅(MS)壳中组成,聚乙二醇修饰的石墨烯(PGO)作为光热试剂和智能开关促进药物的释放. 低于皮肤最大允许照射功率(0.33 W/cm2)的808 nm超低强度近红外光照射(0.25 W/cm2)下的轻度高热可诱导肿瘤细胞不可逆性死亡,并最大量地促进化疗药物的释放;来自UC的660 nm光激活Ce6产生PDT的活性氧,540 nm光可以用于可视化处理过程;动物体内外抗肿瘤实验表明,超低强度近红外光同步激活的Chemo/PTT/PDT纳米平台具有显著的疗效,并且光损伤最小.2 近红外光协同免疫疗法在不同肿瘤中的应用研究近红外光协同免疫疗法是非常有前景的治疗方法,近红外光可以直接及间接激活免疫系统,可同时进行成像监测治疗效果、评估在治疗过程中产生的不良反应,因此在肿瘤治疗方面具有很大的临床应用潜力. 近红外光协同免疫治疗的研究中几乎都涉及纳米材料,这些纳米材料虽然表现出强大的功能和有效性,但其长期毒性及体内蓄积目前仍然不是很明确,因此在临床转化方面还有大量的工作需要做,值得鼓励的是目前已有获批临床研究的项目.采用FDA批准的Erbitux®(Cetuximab)抗体与光吸收剂IR700的结合物(RM1929/ ASP1929)构建NIR-PIT治疗平台用于复发性头颈癌患者的治疗,目前已成功地通过了Ⅰ/Ⅱ期临床试验,为了克服近红外光在组织中有限穿透深度,在肿瘤组织内插入了圆柱形扩散光纤,增强光线在整个肿瘤中的传递. 选用RM1929最大可行剂量640 mg/m2,注射给药24 h后用使用690 nm近红外光50 J/cm2照射表面病变或100 J/cm2照射间位病变. 结果显示:治疗有较好的肿瘤抑制效果,尽管在治疗部位周围观察到出血和疼痛,但未观察到剂量限制性毒性或光敏性,是一种安全的治疗方法(NCT02422979).在肝癌、肺癌、乳腺癌等的临床前研究中,光热或光动联合免疫治疗都表现出令人满意的抗肿瘤效果. HANAOKA等[50]用光敏剂IR700偶联抗GPC3人源性重链抗体(HN3)分别在体外和体内对荷瘤41第 43 卷中南民族大学学报(自然科学版)小鼠进行光免疫治疗(PIT),结果表明IR700-HN3和IR700-YP7(免疫球蛋白)介导下的NIR-PIT在体外和体内均可导致肿瘤细胞死亡,而IR700-HN3表现更强抗肿瘤效果. LI等[51]构建具有荧光成像能力的近红外/pH双响应纳米复合物CE7Q/CQ/SV(由两种铯基纳米材料CE7Q和CQ混合后负载SV),将分子靶向药物厄洛替尼(Er)、生存素 shRNA表达质粒(SV)和光热剂七甲基菁染料(Cy7)整合在一个平台上,用于近红外(NIR)荧光成像和对携带表皮生长因子受体(EGFR)突变的非小细胞肺癌(NSCLC)的三联治疗. 所得CE7Q/CQ/S具有良好的光热效应、良好的DNA结合能力和pH/NIR双响应释放行为,体内外实验结果表明,生存素基因表达下调和光热效应可与Er协同作用,在Er敏感或Er耐药的EGFR 突变的非小细胞肺癌(NSCLC)细胞中均有满意的抗肿瘤效果,该复合治疗纳米平台有望成为治疗非小细胞肺癌的候选药物.肺转移在肿瘤细胞的生长过程中是较为常见的现象,单一光疗很难达到完全抑制的效果. LI 等[52]构建了一种由半导体聚合物纳米颗粒(SPN)核心和由单线态氧(1O2)可切割连接物连接的免疫检查点抑制剂(NLG919)组成的纳米平台(OSPs)用于乳腺癌的治疗. OSPs在近红外激光照射下能够同时产生热量和氧气进行联合光疗,在消融肿瘤的同时产生肿瘤相关抗原;近红外照射可触发1O2-可裂解接头的裂解,触发免疫刺激剂从OSPs远程释放调节免疫抑制的肿瘤微环境,最终导致了小鼠异种移植瘤模型中原发/远处肿瘤的生长和肺转移的抑制. 3 总结与展望近红外光协同免疫疗法可增强抗肿瘤效果、降低各自单独使用时所引起的不良反应,具有很大的临床应用潜能,但发展过程中还有一些瓶颈问题需要解决. 首先,在利用近红外光协同免疫治疗的过程中会构建或使用一些具有高光活性、靶向性、可生物降解等优势的纳米载体,虽被证实有效但多限于体外实验或动物实验数据,况且由于个体差异及体内复杂多变的生物环境使得纳米材料在人体内的作用难以预测,临床转化方面还有大量的工作要做;其次,对于在使用PTT治疗肿瘤时所产生的温度以多少较为合适目前尚没有明确的定论,过低可能无法有效消融肿瘤细胞,过高又可能对正常组织造成伤害,还需要大量的研究去探索适宜的温度范围;再者,与可见光相比近红外光尤其是NIR-II在组织穿透方面有了极大的提高,在浅表层的肿瘤细胞杀伤方面有一定的疗效,但是在深层肿瘤细胞的损害方面依然达不到理想结果,因此近红外光的作用下协同免疫疗法用于临床仍然有很长的路要走. 若能将一些先进的技术如抗干扰能力强传输路径远的光纤技术用于增强近红外光的穿透深度,将可能对深层肿瘤达到治愈的效果.参考文献[1]SHEKARIAN T,VALSESIA-WITTMANN S,CAUX C,et al. Paradigm shift in oncology:Targeting the immunesystem rather than cancer cells [J]. Mutagenesis, 2015, 30(2): 205-211.[2]WEBSTER R M. The immune checkpoint inhibitors: Where are we now [J]. Nat Rev Drug Discov,2014,13(12):883-884.[3]MARTIN J D, CABRAL H, STYLIANOPOULOS T, et al.Improving cancer immunotherapy using nanomedicines:Progress,opportunities and challenges [J]. Nat Rev ClinOncol, 2020, 17(4): 251-266.[4]HUSSAIN T, NGUYEN Q T. Molecular imaging for cancer diagnosis and surgery [J]. Adv Drug Deliv Rev, 2014, 66:90-100.[5]HE X,GAO J,GAMBHIR S S,et al. Near-infrared fluorescent nanoprobes for cancer molecular imaging: Statusand challenges [J]. Trends Mol Med,2010,16(12):574-583.[6]KASHIWAGI S,BRAUNS T,GELFAND J,et al. Laser vaccine adjuvants. History,progress,and potential [J].Hum Vaccin Immunother, 2014, 10(7): 1892-1907.[7]LI J,YU X,JIANG Y,et al. Second near-infrared photothermal semiconducting polymer nanoadjuvant forenhanced cancer immunotherapy [J]. Adv Mater,2020:e2003458.[8]LI X, LOVELL J F, YOON J, et al. Clinical development and potential of photothermal and photodynamic therapiesfor cancer [J]. Nat Rev Clin Oncol,2020,17(11):657-674.[9]HILDEBRANDT B,WUST P,AHLERS O,et al. The cellular and molecular basis of hyperthermia [J]. Crit RevOncol Hematol, 2002, 43(1): 33-56.[10]CHEN Q,WEN J,LI H,et al. Recent advances in different modal imaging-guided photothermal therapy [J].Biomaterials, 2016, 106: 144-166.[11]NG C W,LI J C,PU K Y. Recent Progresses in42第 1 期祝红达,等:近红外光协同免疫疗法增强抗肿瘤效果研究进展phototherapy-synergized cancer immunotherapy [J].Advanced Functional Materials, 2018, 28(46):1804688.[12]GUO L R, YAN D D, YANG D F, et al. Combinatorial photothermal and immuno cancer therapy using chitosan-coated hollow copper sulfide nanoparticles [J]. AcsNano, 2014, 8(6): 5670-5681.[13]ALMEIDA J P, FIGUEROA E R, DREZEK R A. Gold nanoparticle mediated cancer immunotherapy [J].Nanomedicine, 2014, 10(3): 503-514.[14]ZHEN X,XIE C,JIANG Y,et al. Semiconducting photothermal nanoagonist for remote-controlled specificcancer therapy [J]. Nano Lett, 2018, 18(2): 1498-1505.[15]LI X, NAYLOR M F, LE H, et al. Clinical effects of in situ photoimmunotherapy on late-stage melanoma patients:A preliminary study [J]. Cancer Biol Ther,2010,10(11): 1081-1087.[16]SETH A,HEO M B,SUNG M H,et al. Infection-mimicking poly(gamma-glutamic acid)as adjuvantmaterial for effective anti-tumor immune response [J].Int J Biol Macromol, 2015, 75: 495-504.[17]PAN J,WANG Y,ZHANG C,et al. Antigen-directed fabrication of a multifunctional nanovaccine withultrahigh antigen loading efficiency for tumorphotothermal-immunotherapy [J]. Adv Mater, 2018, 30(8): 1704408.[18]CHEN Q, XU L, LIANG C, et al. Photothermal therapy with immune-adjuvant nanoparticles together withcheckpoint blockade for effective cancer immunotherapy[J]. Nat Commun, 2016, 7: 13193.[19]WANG C,XU L,LIANG C,et al. Immunological responses triggered by photothermal therapy with carbonnanotubes in combination with anti-CTLA-4 therapy toinhibit cancer metastasis [J]. Adv Mater,2014,26(48): 8154-8162.[20]CANO-MEJIA J, BURGA R A, SWEENEY E E, et al.Prussian blue nanoparticle-based photothermal therapycombined with checkpoint inhibition for photothermalimmunotherapy of neuroblastoma [J]. Nanomedicine,2017, 13(2): 771-781.[21]ZHOU F, LI X, NAYLOR M F, et al. InCVAX--a novel strategy for treatment of late-stage,metastatic cancersthrough photoimmunotherapy induced tumor-specificimmunity [J]. Cancer Lett, 2015, 359(2): 169-177.[22]CHIANG C L, COUKOS G, KANDALAFT L E. Whole tumor antigen vaccines:Where are we[J]. Vaccines(Basel), 2015, 3(2): 344-372.[23]RAJENDRAKUMAR S K, UTHAMAN S, CHO C S, et al.Nanoparticle-based phototriggered cancer immunotherapyand its domino effect in the tumor microenvironment[J]. Biomacromolecules, 2018, 19(6): 1869-1887.[24]KORBELIK M, HAMBLIN M R. The impact of macrophage-cancer cell interaction on the efficacy of photodynamictherapy [J]. Photochem Photobiol Sci, 2015, 14(8): 1403-1409.[25]KLEINOVINK J W, DRIEL P BVAN, SNOEKS T J, et al.Combination of photodynamic therapy and specificimmunotherapy efficiently eradicates established tumors [J].Clin Cancer Res, 2016, 22(6): 1459-1468.[26]WANG D,WANG T,LIU J,et al. Acid-activatable versatile micelleplexes for PD-L1 blockade-enhancedcancer photodynamic immunotherapy [J]. Nano Lett,2016, 16(9): 5503-5513.[27]MUNN D H,SHAFIZADEH E,ATTWOOD J T,et al.Inhibition of T cell proliferation by macrophage tryptophancatabolism [J]. J Exp Med, 1999, 189(9): 1363-1372.[28]KORBELIK M,BANATH J,ZHANG W,et al.Interaction of acid ceramidase inhibitor LCL521 with tumorresponse to photodynamic therapy and photodynamictherapy-generated vaccine [J]. Int J Cancer,2016,139(6): 1372-1378.[29]XU J,XU L,WANG C,et al. Near-infrared-triggered photodynamic therapy with multitasking upconversionnanoparticles in combination with checkpoint blockadefor immunotherapy of colorectal cancer [J]. ACS Nano,2017, 11(5): 4463-4474.[30]PARK W,CHO S,HAN J,et al. Advanced smart-photosensitizers for more effective cancer treatment [J].Biomater Sci, 2017, 6(1): 79-90.[31]YANO T,HATOGAI K,MORIMOTO H,et al.Photodynamic therapy for esophageal cancer [J]. AnnTransl Med, 2014, 2(3): 29.[32]SATO K, ANDO K, OKUYAMA S, et al. Photoinduced ligand release from a silicon phthalocyanine dyeconjugated with monoclonal antibodies: A mechanism ofcancer cell cytotoxicity after near-infraredphotoimmunotherapy [J]. ACS Cent Sci, 2018, 4(11):1559-1569.[33]NAGAYA T,CHOYKE P L,KOBAYASHI H. Near-infrared photoimmunotherapy for cancers of thegastrointestinal tract [J]. Digestion, 2020: 1-8.[34]MITSUNAGA M,OGAWA M,KOSAKA N,et al. Cancer cell-selective in vivo near infrared photoimmunotherapytargeting specific membrane molecules [J]. Nat Med,2011,17(12): 1685-1691.[35]KOBAYASHI H,CHOYKE P L. Near-infrared photoimmunotherapy of cancer [J]. Acc Chem Res,43第 43 卷中南民族大学学报(自然科学版)2019, 52(8): 2332-2339.[36]KOBAYASHI H,GRIFFITHS G L,CHOYKE P L.Near-infrared photoimmunotherapy:Photoactivatableantibody-drug conjugates (ADCs)[J]. BioconjugChem, 2020, 31(1): 28-36.[37]NAGAYA T,NAKAMURA Y,SATO K,et al. Near infrared photoimmunotherapy with an anti-mesothelinantibody [J]. Oncotarget, 2016, 7(17): 23361-23369.[38]JI Y,WANG Z,BAO K,et al. Targeted molecular imaging of TLR4 in hepatocellular carcinoma usingzwitterionic near-infrared fluorophores [J]. QuantImaging Med Surg, 2019, 9(9): 1548-1555.[39]DING B,XIAO Y,ZHOU H,et al. Polymethine thiopyrylium fluorophores with absorption beyond 1000nm for biological imaging in the second near-infraredsubwindow [J]. J Med Chem,2019,62(4):2049-2059.[40]MARUOKA Y,NAGAYA T,NAKAMURA Y,et al.Evaluation of early therapeutic effects after near-infraredphotoimmunotherapy (NIR-PIT)using luciferase-luciferinphoton-Counting and fluorescence imaging [J]. MolPharm, 2017, 14(12): 4628-4635.[41]LINDSAY K E,BHOSLE S M,ZURLA C,et al.Visualization of early events in mRNA vaccine deliveryin non-human primates via PET-CT and near-infraredimaging [J]. Nat Biomed Eng, 2019, 3(5): 371-380.[42]YOUNISS F M, SUNDARESAN G, GRAHAM L J, et al.Near-infrared imaging of adoptive immune cell therapyin breast cancer model using cell membrane labeling[J]. PLoS One, 2014, 9(10): e109162.[43]THOREK D L, TSAO P Y, ARORA V, et al. In vivo,multimodal imaging of B cell distribution and responseto antibody immunotherapy in mice [J]. PLoS One,2010, 5(5): e10655.[44]KIM E J, BHUNIYA S, LEE H, et al. In vivo trackingof phagocytic immune cells using a dual imaging probewith gadolinium-enhanced MRI and near-infraredfluorescence [J]. ACS Appl Mater Interfaces,2016,8(16): 10266-10273.[45]UONG T N T,LEE K H,AHN S J,et al. Real-time tracking of ex vivo-expanded natural killer cells towardhuman triple-negative breast cancers [J]. FrontImmunol, 2018, 9: 825.[46]JI Y,JONES C,BAEK Y,et al. Near-infrared fluorescence imaging in immunotherapy [J]. Adv DrugDeliv Rev, 2020, 167: 121-134.[47]WAN H, MA H, ZHU S, et al. Developing a bright NIR-II fluorophore with fast renal excretion and its applicationin molecular imaging of immune checkpoint PD-L1 [J].Adv Funct Mater, 2018, 28(50): 1804956.[48]CANTU T,WALSH K,PATTANI V P,et al. Conductive polymer-based nanoparticles for laser-mediated photothermalablation of cancer:Synthesis,characterization,and in vitroevaluation [J]. Int J Nanomedicine, 2017, 12: 615-632.[49]HAN R,TANG K,HOU Y,et al. Ultralow-intensity near infrared light synchronously activated collaborative chemo/photothermal/photodynamic therapy [J]. Biomater Sci, 2020,8(2): 607-618.[50]HANAOKA H, NAGAYA T, SATO K, et al. Glypican-3 targeted human heavy chain antibody as a drug carrierfor hepatocellular carcinoma therapy [J]. MolecularPharmaceutics, 2015, 12(6): 2151-2157.[51]LI Z,ZHU L,LIU W,et al. Near-infrared/pH dual-responsive nanocomplexes for targeted imaging andchemo/gene/photothermal tri-therapies of non-small celllung cancer [J]. Acta Biomater, 2020, 107: 242-259.[52]LI J, CUI D, HUANG J, et al. Organic semiconducting pro-nanostimulants for near-infrared photoactivatablecancer immunotherapy [J]. Angew Chem Int Ed Engl,2019, 58(36): 12680-12687.(责编&校对姚春娜)44。
空气负离子自然疗法是如何治疗癌症的尽管癌症可防可治的观念已有一定普及,但不少人仍然“谈癌色变”。
近日,中山大学医学院颜光美课题组发现灭癌病毒M1的消息在国内引起了轰动,癌症患者们一边欣喜于看到了攻克癌症的曙光,一边却担心癌症攻克之路的漫长。
其实除了传统的癌症治疗方法,一些自然疗法对癌症治疗也有很好的辅助作用,癌症患者要重视。
食疗:谷肉果菜,食养尽之早在2000年前,《黄帝内经》就有一句名言;“谷肉果菜,食养尽之。
”这是说,治疗病症不仅要靠药物,还要配合饮食调养。
癌症是一种慢性的消耗性疾病,会耗掉人体的营养,时间一长,病人就会营养不良,晚期的癌症病人更为突出,越来越消瘦,中医称为“失荣”,西医称为“恶病质”。
所以,无论早期或者晚期的癌症病人,都要想办法得到全面的营养供给。
对癌症病人来说,最重要的是谷肉果菜巧安排,把握“四个要”:要合理搭配;要少量多餐;要容易消化;要变换花样。
其次要适当吃一些有一定抗癌作用的食物,比如苡仁、红薯、莴笋、竹笋、平菇、猴头菇。
抗癌:要使用空气负离子疗法空气负离子疗法即通过自然因子——负氧离子进行治疗保健,是一种注重于人类自愈能力的自然疗法,对于癌症患者而言,使用负离子疗法能够有效改善癌症患者的生存质量,延长癌症患者的寿命。
癌症患者可以在室内放一台空气负离子健康机,空气负离子健康机利用负离子转换器与纳子富勒烯负离子释放器是释放出的等同于大自然的生态级负离子会通过呼吸进入人体引起一系列列的化学物理生物反应,全面调节患者体质。
医学研究表明:对人体有医疗保健作用的是小粒径空气负离子。
因为只有小粒径的空气负离子才易于透过人体的血脑屏障,发挥其生物效应。
临床研究证实,人体得到带负电可提供大量电子的负离子,能够阻止可能致癌的恶性循环,癌细胞就会被防止或者抑制,另外,空气负离子健康机释放的生态级空气负离子透过人体血脑屏障,可以调节因恶性肿瘤引起的体内酸碱失衡和氧化还原状况失衡,维持体内环境的稳定性,促进正常的新陈代谢,减轻消除放化疗的不良反应,对患者的治疗非常有益。
抑制癌细胞需要大补吗?*导读:长沙彭先生问:我的一位朋友得了胃癌,我给他买了很多补品,可是我的另外一位朋友说在补身体的同时也补了癌细胞,会起反作用的,请问癌症病人需要大补吗?首先要提醒患者分清补养药和治疗药的区别。
何种肿瘤用何药,何时以补为主、何时以攻为主,何时宜攻补兼施,要针对病情体质等用药。
一般来说,保健品的有效含量较低,只起辅助作用,10元钱的保健品只相当于1元钱的治疗药,不能用补养药代替治疗药,以免贻误治疗,而且补养药也不是每种体质、不同癌症时期的人都能随便吃,最好在中医医生的指导下服用。
原则上,患癌症的病人应增加营养,保持体重,尤其是晚期癌症病人。
现在还没有证据证明营养物会只补癌细胞而不使身体受益。
河北副主任医师刘志华癌症患者呼吸也有讲究?不错,郑州市第三人民医院肿瘤二病区主任朱眉提醒说,对于癌症病人来说,要学会呼吸。
朱眉主任解释说,癌症病人在康复期需要更多的氧气。
但是,癌细胞的生物学特点是无氧代谢,癌细胞内的葡萄糖在无氧条件下可产生乳酸,对癌症病人很不利。
如果癌症病人掌握正确的呼吸方式,可以获得更多的氧气,使癌细胞代谢率降低,让它长得慢一些或起到抑制作用。
在医学上,呼吸分为胸式呼吸和腹式呼吸。
胸式深呼吸,能使肺上部的肺泡开放,腹式深呼吸,除了肺上部的肺泡开放,肺下部的肺泡也能打开。
癌症病人如果仅用胸式呼吸,这种呼吸每次换气量很小,正常呼吸频率下通气不足,会使体内二氧化碳累积,导致脑部缺氧,出现头晕、乏力。
因此,癌症病人要学会用腹式呼吸。
此外,全身呼吸法也是一种很科学的呼吸方法。
方法是:先慢慢由鼻孔吸气,吸气过程中,胸廓上提,腹部慢慢鼓起,再继续吸气,使整个肺充满空气。
这个过程需5-10秒,然后屏气5-10秒,呼出肺里的空气,停顿2-3秒钟后,开始新一次的呼吸。
癌症患者呼吸也有讲究?不错,郑州市第三人民医院肿瘤二病区主任朱眉提醒说,对于癌症病人来说,要学会呼吸。
朱眉主任解释说,癌症病人在康复期需要更多的氧气。
漳州二中2016—2017学年度高三上学期期初摸底考生物试卷考试时间:90分钟;命题人:刘炜红姓名:___________班级:___________学号:___________第I卷(选择题)一、单选题(本题共30道小题,每小题2分,共60分)1。
下图中,W、X、Y、Z四点中光照强度不能限制光合作用强度的是()A.W、X B.X、Y C.Y、Z D.Z、W2。
磷酸化是指在某些物质分子上加入一个磷酸基团,如三磷酸腺苷(ATP)就是由二磷酸腺苷(ADP)磷酸化而来.下列结构中不能发生ADP磷酸化的是( )A.细胞质基质 B.叶绿体基质C.叶绿体类囊体薄膜D.线粒体内膜3。
于人体细胞分化、衰老、凋亡和癌变的叙述,正确的是() A.细胞分化导致基因选择性表达,细胞种类增多B.细胞衰老表现为酶活性降低,细胞核体积减小C.细胞凋亡受基因控制,不利于个体生长发育D.石棉和黄曲霉毒素是相同类型的致癌因子4.在细胞有丝分裂的分裂期开始时,如果它的染色体数为N,DNA 含量为Q,则该细胞分裂后每个子细胞中的染色体数和DNA含量分别是( )A.N和Q B.N/2和Q/2 C.N和Q/2 D.N/2和Q5。
下列关于癌细胞的叙述,错误的是( )A.癌细胞具有无限增殖的能力B.细胞癌变可以由病毒感染引发C.原癌基因只存在于癌细胞中D.癌细胞的转移与细胞间黏着性下降有关6.下列关于细胞生命历程的说法正确的是()A.细胞凋亡发生在胚胎发育过程中,细胞分化发生在整个生命过程中B.多细胞生物个体衰老过程中,既有细胞的衰老死亡,也有大量新细胞经分裂产生并发生细胞分化,所以个体衰老和细胞衰老无直接关系C.细胞分化是永久性的变化,一般不可逆转D.放疗、化疗方法通过抑制癌细胞DNA复制和诱导癌细胞突变成正常细胞,达到治疗的目的7.下列关于植物光合作用和细胞呼吸的叙述,正确的是() A.无氧和零下低温环境有利于水果的保鲜B.CO2的固定过程发生在叶绿体中,C6H12O6分解成CO2的过程发生在线粒体中C.光合作用过程中光能转变为化学能,细胞呼吸过程中化学能转变为热能和ATPD.夏季连续阴天,大棚中白天适当增加光照,夜晚适当降低温度,可提高作物产量8.利用小球藻培养液进行光合作用实验时,在其中加入抑制暗反应的药物后,发现在同样的光照条件下释放氧气的速率下降.主要原因是( )A.叶绿素吸收光能的效率下降B.NADPH等的积累,光反应速率减慢C.合成ATP所需酶的活性受到抑制D.暗反应中生成水减少,使光反应的原料不足9。
基因—病毒策略:癌症治疗新希望作者:杨昆来源:《祝您健康》 2015年第1期杨昆上海市科普作家协会医药卫生专业委员会长期以来,人类对付癌症的手段大体上有手术、化疗和放疗三种。
对于早期癌症,手术可以将其一网打尽,而目前确诊的癌症约2/3 已属晚期,此时手术,漏网的癌细胞会很快“东山再起”。
另一方面,由于癌细胞是自身细胞演变而来,其生物代谢和分裂繁殖与正常细胞无本质区别,化疗和放疗常常是六亲不认,敌我不分,在杀灭癌细胞的同时,也会伤害人体正常组织细胞。
今天,当传统的治疗方法对很多中晚期肿瘤患者束手无策时,生物治疗就成为战胜癌症的一种有力武器。
中国科学院院士刘新垣运用超级干扰素以及癌症的“靶向基因- 病毒治疗”策略,有望达到战胜癌症的目的。
上述治疗方法已经在动物试验以及一些临床试验中获得成功。
一位四川农村的黄大娘,患非小细胞肺癌,行走都很困难,经用超级干扰素数月治疗后,恢复良好,生活已能自理,还能干些轻松的农活。
易女士2004 年患胃癌,经超级干扰素治疗,已痊愈出院,并恢复了工作。
李先生是一位公司董事,患了肾癌,经超级干扰素治疗,已痊愈7 ~ 8 年了,他现在是拥有亿元资产的公司老板。
一个人被一种病毒感染之后,就产生一种物质可以干扰防止另一种病毒的再感染,这种物质就叫干扰素。
刘新垣院士于20 世纪末与魏光文等学者共同发现了超级干扰素。
这种超级干扰素是将干扰素-a-co 的基因进行60 多处改造而得到。
它不仅有很好的抗病毒作用,经初步临床试验表明,还有很好的抗癌作用。
目前的研究表明,超级干扰素能够升高癌组织中一种被称之为“Caspase3”的活性(一种起凋亡杀伤作用的关键分子),而保护癌细胞不凋亡的分子“Bcl-2”的活性则下降。
杀伤癌细胞分子的活性升高,而保护癌细胞分子的活性下降,这就大大提高了超级干扰素对癌细胞的直接杀伤作用。
过去干扰素是癌症治疗的辅助药物(即二线药物),是通过提高机体的免疫功能间接起到抗癌作用,极少用于直接(即一线药物)治疗癌症。
中山大学教授颜光美:M1“灭癌”病毒有望明年进行临床试验2017-08-24 12:09:00来源: 南方都市报(深圳)举报分享到:∙易信∙微信∙QQ空间∙微博ooo(原标题:中山大学教授颜光美:M1“灭癌”病毒有望明年进行临床试验)时隔三年,中山大学药理学教授颜光美的团队又带来了好消息,他们向外界公布了“溶瘤病毒M1”的最新进展。
此次,该抗癌新药的研究更进一步:不仅在猴子这一非人灵长类动物身上证实了M1病毒的安全性,还发现和其他药物联用让M1增效的机制,甚至揭秘了M1病毒可以引起肿瘤“内斗”的灭癌原理。
团队部分成员合影,右二是颜光美教授。
如果把研发抗癌新药的过程比作10公里长跑,2014年,颜光美接受南方记者采访时认为,团队顺利跑完了第一公里,而现在他说,路程已走了一半。
这几年,仍有大量癌症患者向他发来邮件,希望使用病毒进行治疗,颜光美都拒绝了,此次,他也带来了临床试验的最新消息,“预计2018年可以进行M1病毒的临床试验。
”药物或可享受绿色通道更快进入临床试验2014年,颜光美的实验团队在全球内首次发现,在自然界存在的病毒M1具有选择性杀伤多种肿瘤细胞的特性。
这种在海南蚊虫上发现的病毒,只在马和猪之间传播,但被团队证实,可以钻入癌细胞体内,通过扩增裂解方式杀伤肿瘤细胞,“以毒攻毒”。
颜光美团队在小鼠和人体肿瘤组织上进行的实验显示,M1对肝癌、结直肠癌、膀胱癌细胞的杀伤作用最明显,对黑色素瘤、脑癌和前列腺癌等癌细胞也起作用。
实验发现,M1病毒对体外培养的部分人类癌症细胞,抑制率高达90%;对肿瘤模型小鼠体内的癌细胞,抑制率达50%—60%。
他们还对临床病例中切除下来的肿瘤组织进行实验发现,对敏感病例的癌组织的抑制率达60%—70%。
所谓抑制率,指的是M1病毒杀死肿瘤或抑制肿瘤增殖的比率。
论文发表在2014年10月2日的《美国国家科学院院刊》上,经国内媒体报道后,引起轰动。
胡骏博士和邱鹏新研究员给食蟹猴进行CT检查。
又是三年,颜光美说,自2014年研究被报道伊始,每个星期,都有患者发来邮件,希望使用病毒制剂,或是询问研究进度,来自齐齐哈尔的一家四口人,甚至直接登门拜访。
颜光美尽量一一回复,“我很理解,亲人得了癌症,是什么样的心情。
人的精神向往会产生很大的作用,有了期待,也许病人就能等到那一天。
”除了患者,这项研究也得到了省领导的关注。
溶瘤病毒M1的临床转化研究还获得国家“十三五”重大新药创制科技重大专项资金的支持。
在这些支持下,溶瘤病毒M1将可能享受绿色通道以更快的速度进入临床试验。
现阶段,颜光美教授课题组正在紧锣密鼓的进行新药申报前的临床前研究,他说,有望2018年申请临床试验批件,正式进入临床试验阶段,届时,部分受试患者就能最先注射到这一药物。
抗癌新药研发已走了一半疗效要用临床说话“整个研究还算顺利,除了睡着的几个小时没考虑(这项研究),其他时间都在考虑。
”今年颜光美已有60岁,因为年龄原因,他退出了中山大学副校长这一领导岗位,有媒体希望专访他,被拒绝了。
“我说自己主要的兴趣在研究上,如果有了科研进展,我会跟大家沟通。
”获得了众多关注的目光,让颜光美更加珍惜时间,退下来后,颜光美一天都没休息过。
团队的成员凌晨一两点,可能也会接到他的微信。
但颜光美很欣喜,因为现在精力很集中,“100%花在研究工作上,这两三月研究的进展特别快,这是我特别觉得高兴的事情。
如果有机会做成新药,那是非常幸运的。
”颜光美教授团队的主要研究成员。
自然界存在的病毒中,只有一小部分会对人体致病。
团队通过体外细胞系和小动物模型上证实,M1病毒虽然可以攻破肿瘤的防线,但对正常细胞并没有损伤作用。
但人体毕竟不是动物,病毒是否会对人体有毒副作用?在2014年成果公布后,团队紧锣密鼓,挑选了“最接近人类”的非人灵长类动物食蟹猴进行验证。
团队成员、中山大学副教授胡骏在肇庆找到了合适的实验猴厂,这里既能给猴子做B超,还能做CT、核磁共振(MRI), “广州医院也有核磁共振,但猴子去做肯定不方便。
”接下来的两年里,胡骏有一半时间就住在山上的猴厂,不定期地给食蟹猴静脉注射了18次溶瘤病毒M1,密切记录食蟹猴的日常行为表现、生化指标和重要器官的影像结果。
“在这个过程中,每天也提心吊胆,每次检查结果出来就赶紧去看。
”胡骏说。
研究人员正在显微镜下观察M1对肿瘤细胞的杀伤作用。
数据结果让人欣喜:在观察的半年时间内,食蟹猴都没有出现任何不良临床反应,核磁共振检查也未发现任何器官出现损害。
为什么是18次?颜光美说,因为怕反复注射引起人体过敏反应等副作用,因此在食蟹猴身上注射了多次,“如果一个疗程使用6次,那我们打18次,看会不会有影响。
”“在猴子身上是安全的,在人身上有很大的机会也是安全的。
这个结果强烈提示,M1病毒具有良好的安全性,为将来M1病毒在临床的应用提供了保障。
”颜光美说。
这一成果也在2016年6月22日发表在基因治疗领域的权威期刊《人类基因治疗》。
强强联手 M1病毒增效3600倍除了验证M1病毒的安全性,颜光美也在考虑另一个问题:抗癌药物研发已有200年历史,针对各种癌症的药物达数百种之多,知识有一个继承关系,M1病毒和现有的抗癌药物有无协同作用?为此,团队的博士张海鹏带领另外三位博士,挑选了350种有代表性的小分子靶向药物,筛选了8个月。
在对比后,张海鹏等人逐渐缩小范围,并定格到一类靶向内质网相关降解通路(ERAD)的抗癌药物,它适用于多发性骨髓瘤和多种晚期实体瘤。
课题组在小鼠的肝脏上注射人肝癌细胞,建立了原位肝癌模型,并对小鼠注射低剂量的溶瘤病毒和ERAD抑制剂,结果显示,小鼠的生存期延长了一倍以上。
单独使用低剂量M1病毒攻击,肿瘤模型小鼠体内的癌细胞,抑制率为23.6%。
而在用了增效剂后,抑制率提高至72.3%。
临床肿瘤手术标本的离体培养组织上,这一联合应用的效果也得到验证。
此联合疗法在食蟹猴模型上没有引起不良反应。
不止如此。
这一抗癌药物能显著增强M1病毒的抗肿瘤活性,增幅高达3600倍。
“比如,以前用1个病毒可以杀伤1个肿瘤细胞,现在能杀伤3600个。
”“溶瘤病毒M1是自动锁定肿瘤细胞的制导导弹,而ERAD抑制剂的加入,如同在导弹上绑定了自带筛选功能的烈性炸药包,强强联手,效果不言自明。
”颜光美说,这也给研究带来了新思路,病毒M1除了“单打独斗”外,也可以和别的药物联用提高疗效。
有意思的是,两种药物是否应该搭配应用于病人,“有据可循”。
“通过检测ERAD通路中一个叫做VCP的蛋白质来预测。
”张海鹏解释,具体来说,如果肿瘤组织上的VCP蛋白高表达,提示病人适合溶瘤病毒M1和ERAD抑制剂联合方案,如若低表达,则代表不适合。
让人兴奋的是,在肝癌病人中,肿瘤组织高表达VCP是很常见的。
该治疗方案将给难治的肝癌带来新希望。
但张海鹏说,不只是肝癌,该方案对膀胱癌、结直肠癌也有显著的增效作用,“不同的肿瘤或许可以筛选出不同的增效剂。
”这一研究成果也在2017年8月24日凌晨发表在国际上转化医学领域的权威期刊《科学·转化医学》。
溶瘤病毒M1引发肿瘤细胞“内斗”在研究过程中,团队博士生蔡静偶然的新发现,破解了另一谜题。
在一次做实验时,蔡静用标记上红色荧光的M1病毒感染肿瘤细胞,感染后,如果细胞带有红色标记,说明感染上了病毒。
随后,她对肿瘤细胞进行“凋亡染色”,发现一个有意思的现象:被感染的肿瘤细胞周围,有很多旁边的肿瘤细胞没有红色标记,即没有感染M1病毒,但也发生了死亡。
是谁杀死了这些旁边的肿瘤细胞?随后的两年多时间里,蔡静专注破解这一难题。
最终她发现,M1病毒居然可以诱导肿瘤细胞,释放具有细胞毒性的因子,进而杀伤这些细胞周围尚未感染M1的肿瘤细胞。
这是一种非常有趣的现象,学术界称之为“旁观者效应”,意为处于感染细胞周围的旁观细胞遭受杀灭。
而且,实验发现,30%癌细胞是被M1病毒杀死的,而剩下的70%,均是被癌细胞放出的因子杀死的。
颜光美如是解析这一现象:病毒要在活细胞里生存,如果试着从肿瘤细胞的角度来理解这种行为,可以发现,肿瘤细胞在受到溶瘤病毒胁迫时,似乎抱着一种“断臂求生”的心态释放信号,杀灭周围的细胞,让病毒无法靠近,以保全远端的肿瘤细胞。
这一创新性的成果,与2017年6月27日发表在国际上具有很高影响力的权威期刊《美国国家科学院院刊》。
解析:新药离上市还有多久?已制备注射制剂上市时间尚无法预估按照法律规定,新药研发需通过科学研究、临床前、用于人体的一、二、三期临床试验等阶段,才可以上市销售,用于临床治疗患者。
一期临床试验考查药物的安全性,二期考查药物的有效性,三期试验用数量更多的实验样本进一步研究,上市后还要在临床中进行大规模的研究,验证药效。
颜光美说,目前,团队研发药物的工艺技术难题已经解决,M1病毒经过发酵、纯化的步骤后,最后将制成冻干粉,成为静脉注射的制剂。
国际上现行使用的溶瘤病毒注射液,需要将溶液冷冻到负80 ,运输受到限制。
而制成冻干粉,可以放置在2 -8 当中,普通冰箱即可保存,使用很方便。
颜光美说,药物纯化是极为艰难的步骤,不少研发药物走到这一步后,止步不前。
“打通了这个技术关节,我扎扎实实高兴了好几天。
”目前,团队正在进行新药申报前的临床前研究,预计2018年可以进行M1病毒的临床实验,届时,药物将可在病人身上进行首试。
“做完一期试验,最快需要一年时间。
”颜光美说,新药审批需要多长时间,“这不是我能决定的,时间还没办法预估。
”病毒是否对所有肿瘤有效果?11种癌症均有不同抑制效果颜光美说,今年3月,美国FDA批了一类抗癌生物标志物,如果多种癌症都具有这个生物标志物的话,则可被批准治疗。
“这是未来抗癌药物发展的新方向,这就是我们计划做的。
”目前研究显示,溶瘤病毒M1对10种高发癌症(肺癌,肝癌,结直肠癌,乳腺癌,胰腺癌,前列腺癌,宫颈癌,胶质瘤,鼻咽癌,胃癌),以及广东高发的鼻咽癌都有不同程度的抑制作用。
此前,该团队已找到M1病毒靶向杀伤癌细胞的特征物--锌指抗病毒蛋白(ZAP)。
目前,针对ZAP的诊断试剂盒已在报批,VCP的诊断试剂盒已准备委托公司研发。
如若新药成功研发,这11种肿瘤病人可以先通过检测,确定体内癌细胞缺乏ZAP,便可以进行溶瘤病毒M1治疗。
如果VCP蛋白高表达,病人则适合溶瘤病毒M1和ERAD抑制剂联合方案。
背景:M1病毒曾被封存40年M1病毒的发现可以追溯至上世纪60年代。
1964年,一群科学家在海南岛“抓获”了50只蚊子,从这些蚊子体内,他们分离出了这种病毒。
他们发现,M1除了在马和猪身上会引起非常轻微的类似感冒的症状,对人和绝大多数动物都几乎没有致病性。
于是,这群科学家对M1丧失了兴趣,病毒被封存。
2004年,当时正在做博士论文的胡骏在一次实验中偶然发现,M1病毒可以将大鼠来源的胶质瘤细胞溶解掉。