标准肝体积公式评估-中国人正常肝脏体积预测公式的评估
- 格式:pdf
- 大小:539.25 KB
- 文档页数:5
标准肝体积计算公式肝体积计算是临床上常见的一项重要指标,它对于评估肝脏健康状况、诊断肝脏疾病、制定治疗方案等方面具有重要意义。
在临床实践中,我们需要准确地计算患者的肝体积,以便更好地进行诊断和治疗。
本文将介绍标准的肝体积计算公式,帮助大家更好地理解和应用这一重要的临床指标。
肝体积计算的标准公式如下:肝体积(ml)= 0.6 ×身高(cm)+ 0.5 ×体重(kg)2.4。
其中,肝体积以毫升(ml)为单位,身高以厘米(cm)为单位,体重以千克(kg)为单位。
这个公式是根据大量的临床数据和统计分析得出的,具有较高的准确性和可靠性。
下面我们将详细解释这个公式的计算原理和临床应用。
首先,我们来解释各个参数的含义。
身高是指患者的身体高度,通常以厘米为单位。
体重是指患者的体重,通常以千克为单位。
这两个参数是计算肝体积的基本数据,需要准确测量并记录。
在实际应用中,我们可以使用体重仪和身高尺等工具来进行测量,确保数据的准确性和可靠性。
接下来,我们来解释公式中的系数和常数。
0.6和0.5是两个系数,它们代表了身高和体重对肝体积的影响程度。
在这个公式中,身高的影响系数略大于体重,这是因为肝脏是一个相对较大的器官,身高对其体积的影响更为显著。
-2.4是一个常数,它代表了肝脏的基础体积,这是根据大量的临床数据和统计分析得出的结果。
在实际应用中,我们可以根据患者的身高和体重,利用这个公式来计算其肝体积。
例如,一个身高170厘米、体重70千克的患者,其肝体积计算结果为:肝体积(ml)= 0.6 × 170 + 0.5 × 70 2.4 = 102 + 35 2.4 = 134.6。
这个计算结果告诉我们,这个患者的肝体积约为134.6毫升。
通过这样的计算,我们可以快速、准确地得出患者的肝体积,为临床诊断和治疗提供重要参考。
需要注意的是,肝体积的计算结果可能会受到一些因素的影响,例如年龄、性别、肝脏疾病等。

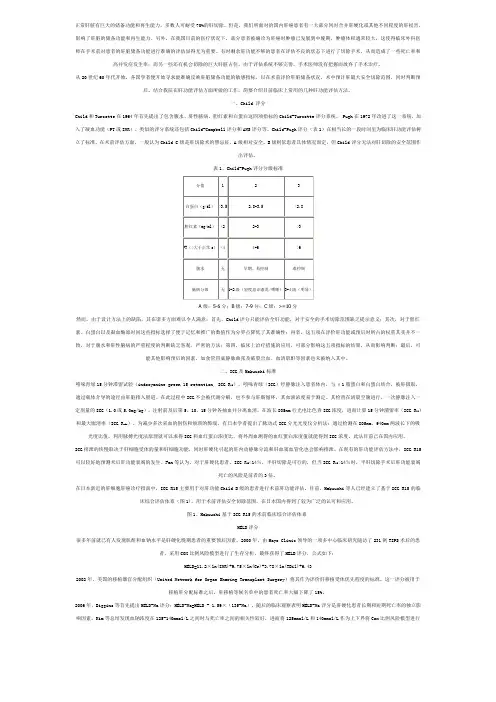
Zheng-Rong Shi, Lu-Nan Yan, Bo Li, Tian-Fu Wen, Liver Transplantation Division, Department of Surgery, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, ChinaAuthor contributions: Shi ZR, Yan LN participated in the research design and writing of the paper; all authors participated in the performance of the research; Shi ZR contributed analytic tools and data analysis.Correspondence to: Lu-Nan Yan, MD, PhD, Liver Trans-plantation Division, Department of Surgery, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China. yanlunan2009@ Telephone: +86-28-85422867 Fax: +86-28-85422867 Received: May 31, 2009Revised: July 16, 2009 Accepted: July 23, 2009Published online: August 28, 2009AbstractAIM: To evaluate different standard liver volume (SLV) formula and verify the applicability of the formulae for Chinese adults.METHODS:Data from 70 cases of living donor liver transplantation (LDLT) performed at our transplanta-tion centers between January 2008 and April 2009 were analyzed. SLV was estimated using our recently reported formula [the Chengdu formula: SLV (mL) = 11.5 × body weight (kg) + 334] and other reported formulae used for Chinese adults. Actual intraoperative liver volumes were obtained from a review of the patients’ medical records. RESULTS:The actual right liver volume was not signifi -cantly different from the estimated right liver volume de-termined by the Chengdu formula, but was signifi cantly smaller than estimates using the Heinemann, Urata, Vauthey, and Lee formulae (P < 0.01), and signifi cantly larger than estimates using the Fan formula (P < 0.05). CONCLUSION: The Chengdu formula was demon-strated to be reliable by its application in LDLT.© 2009 The WJG Press and Baishideng. All rights reserved.Key words: Standard liver volume; Living donor liver transplantation; Chinese adult; Liver volume formulaPeer reviewers: Silvio Nadalin, MD, PhD, Director of Transplant Program, Department of General, Visceral and Transplant Surgery, University Hospital Tübingen, Hoppe Seyler Strasse 3, 72076 Tübingen, Germany; Salvatore Gruttadauria, MD, Assistant Professor, Abdominal Transplant Surgery, ISMETT, Via E. Tricomi, 190127 Palermo, ItalyShi ZR, Yan LN, Li B, Wen TF. Evaluation of standard liver volume formulae for Chinese adults. World J Gastroenterol 2009; 15(32): 4062-4066 Available from: URL: http://www. /1007-9327/15/4062.asp DOI: http://dx.doi. org/10.3748/wjg.15.4062INTRODUCTIONLiving donor liver transplantation (LDLT) has been used to alleviate the shortage of available liver donors. Accurate estimation of the standard liver volume (SLV) of the living donor and recipient is crucial. Overestimation of the donor’s SLV may result in excessive hepatic resection leading to liver failure, while underestimation of the recipient’s SLV may result in small-for-size graft syndrome[1-5]. Since 2001, our transplant centers have carried out 212 LDLTs. We estimated the SLV using computed tomography (CT) or reported formulae. However, there was a difference between these estimates and the actual liver volumes (ALVs) for Chinese adults. Recently, we developed a new formula (named the Chengdu formula) to estimate SLV using data from 115 LDLTs[6]. The formula is: SLV (mL) = 11.5 × body weight (kg) + 334. Using this formula, the SLVs were evaluated in 76 cases of LDLT performed from January 2008 to April 2009. Its accuracy was compared to that of other internationally reported formulae[7-10] to assess which formula is the most accurate for Chinese adults. MATERIALS AND METHODSPatient selectionThe data from 76 living donors were analyzed. Inclusion criteria were: (1) a healthy adult donor, aged 19-59 years;(2) right liver graft without middle hepatic vein; (3) adult-to-adult LDLT; (4) single donor; (5) no history of long term drinking. Exclusion criteria: (1) donor age < 18 or > 60 years; (2) left hepatic graft or left lateral lobe graft;(3) double donor grafts; (4) adult-to-child transplant; (5) donors who were hepatitis B or C carriers[11-14].Clinical dataData of preoperative donors included age, sex, heightOnline Submissions: World J Gastroenterol 2009 August 28; 15(32): 4062-4066 wjg@ World Journal of Gastroenterology ISSN 1007-9327doi:10.3748/wjg.15.4062 © 2009 The WJG Press and Baishideng. All rights reserved.Evaluation of standard liver volume formulae for Chinese adultsZheng-Rong Shi, Lu-Nan Yan, Bo Li, Tian-Fu WenBRIEF ARTICLES(BH, measured to the nearest 1 cm), body weight (BW , measured to the nearest 0.5 kg), and body surface area (BSA) calculated using the DuBois formula: BSA (m 2) = BW (kg) 0.425 × BH (cm) 0.725 × 0.007184 or the Mosteller formula: BSA (m 2) = square root BH (cm) × BW (kg)/3600. From the diaphragm to the superior mesenteric artery plane, the entire liver image was scanned using a 7 mm thick layer. In the Leonardo workstation, the LV was measured by venous phase images [15,16]. All preoperative CT examinations of donors were performed by a single radiologist and all donor procedures were performed by the same surgical unit. The volume of the grafts was measured by a 3 L beaker using a drainage method intraoperatively and the error was less than 10 mL [17,18].Right liver graft without middle hepatic vein reconstruction from a living donor was performed as described, with temporary occlusion of the right portal vein (PV) and right hepatic artery and use of ultrasonography to guide parenchymal transection. The right hepatic duct, right hepatic artery, right portal vein branch, and right hepatic vein were transected approximately 2-3 mm from the con fl uence [19,20], leaving the donor’s main PV and confluence intact. The graft was flushed with University of Wisconsin solution through the PV and hepatic artery [21,22].The volume of 70 livers was calculated using the Chengdu standard LV formula [6] as described above. The estimated right LV (ERLV) was obtained by multiplying the SLV by the proportion of the LV contributed by the right lobe on CT. The actual right LV (ARLV) was obtained by intraoperative measurement. The differencebetween the ERLV and ARLV was statistically evaluated. The formulae of Heinemann et al [8], Urata et al [7], Vauthey et al [9], Lee et al [5], and Fan et al [4] in addition to our own formula [6] were used to determine the estimated SLV (ESLV) of our donor livers. The previously reported formulae are shown in Table 1. For each liver, we calculated the difference between the ALV and volume estimated by each formula (ELV).Statistical analysisAfter testing for normal distribution (kurtosis and skewness tests), descriptive statistics were calculated and data were expressed as means ± SD for age (year), BW (kg), BH (cm), body mass index (BMI), and BSA. The ERLV-ARLV and the ELV-ALV were compared by the 2-sided paired-samples t -test. P < 0.05 was considered statistically significant. All statistical analyses were performed using the SPSS (version 13.0) program.RESULTSSeventy donors (all Chinese; 53 men and 17 women; mean age, 32.21 ± 10.07; range, 19-57 years) met the selection criteria. All donors were related to the recipients.The characteristics of donors are shown in Table 2. All donors were considered healthy on the basis of BMI. All but one donor with a BMI of 17 kg/m 2 had a BMI of 18-28 kg/m 2. The mean volume of the right lobe on CT was 658.98 ± 81.14 mL and represented 55.4% ± 3.7% of the whole liver on CT.The mean ELV and mean ERLV using the Chengdu standard formula were 1058.70 ± 96.74 mL and 586.15 ± 67.17 mL, respectively. The mean ARLV was 578.58 ± 72.33 mL. Differences for individual donors between ERLV and ARLV were not signi fi cant (t = -1.882, P = 0.064). A plot of the relationship of ARLV to the ERLV calculated using the Chengdu formula is shown in Figure 1. The mean total LV determined preoperatively on CT was 1189.53 ± 114.75 mL. The mean RLV on CT without the middle hepatic vein was 658.98 ± 81.14 mL, and 55.4% ± 3.7% of the total LV . The ALV calculated from the volume of the graft and the ratio of the RLV to the total LV on CT (%) was 1050.10 ± 107.41 mL. The Heinemann, Urata, Vauthey, and Lee formulae signi fi cantly overestimated the LV (P < 0.01), while the Fan formula significantly underestimated the LV (P <Shi ZR et al . Liver volume formulae for Chinese adults 4063ESLV: Estimated standard liver volume; BSA: Body surface area; BW: Body weight; CT: Computed tomography; LDLT: Living donor liver transplantation.Table 2 Donor characteristicsMHV: Middle hepatic vein.0.05). There was no signi fi cant difference between ALV and ELV using the Chengdu formula (Figure 2).DISCUSSIONCT has become a standard method for assessing livergraft volume in living donors. Estimation of LV by CT (compared to actual volume) has a margin of error of 5%-25%[23,24]. In the present study, all donors had preoperative CT assessment of LV (mean total LV , 1189.53 ± 114.75 mL and mean volume of right lobe graft without middle hepatic vein, 658.98 ± 81.14 mL). The actual volume of the right liver was 578.58 ± 72.33 mL. In the present study, the LV on CT was 10%-20% higher than the ALV [25-27]. The reasons may be as follows: (1) Preoperative CT measurement is carried out under normal blood fl ow conditions. Perioperatively, liver resection interrupts the blood supply causing a loss of liquid volume, collapse of supporting structures, and thereby reduction in the volumeof the liver. (2) Sources of error (partial volume effect, inter-observer variation, and respiratory movements) may account for this difference [28].The difference between the ERLV (using our formula) and ARLV was compared to the difference between ERLV, calculated using the formulae of Heinemann, Urata, Vauthey, Lee, and Fan, and ARLV in our 70 donors. The Heinemann, Urata, Vauthey, and Lee formulae overestimated LV (P < 0.01)[29]. The reasons may include: ethnic differences (patients in Europe and the United States were Caucasian). All except the Sheung Tat Fan and Chengdu formulae were used to estimate LV from CT LV or autopsy LV. Estimates of LV by CT were 5%-25% higher than the ALV [30].Statistical analysis showed that the Fan formula tends to underestimate LV. The weight and height of the donors in our study were higher than of those in the Hong Kong group. This may be one of the reasons both results are very close (Table 3). Above all, we believe thatALV: Actual liver volume; ND: Not determined.Figure 1 Correlation between actual right liver volume (ARLV) and estimated right liver volume (ERLV) by the Chengdu formula. When both were the same, a dot would be on the linear line.500 600 700Graft ARLV700600500E R L VFigure 2 Correlation between actual liver volume (ALV) and estimated liver volume (ELV) by each formula. When both were the same, a dot would be on the linear line. Formulae of Urata, Heinemann, Vauthey, and Lee overestimated LV with respect to ALV. The Fan formula underestimated LV and the Chengdu formula gave a good estimate of ALV.4064 ISSN 1007-9327 CN 14-1219/R World J Gastroenterol August 28, 2009 Volume 15 Number 32700 900 1100 1300 1500ALV150013001100900700U r a t a700 1000 13001600ALV160013001000700H e i n e m a n n700 900 1100 1300 1500ALV150013001100900700L e e700 1000 1300 1600ALV160013001000700V a u t h e y700 900 1100 1300 1500ALV150013001100900700F a n700 800 900 1000 1100 1200 1300ALV14001300120011001000900800700C h e n g d uthe Chengdu formula was demonstrated to be reliable by its application in LDLT. We were limited to use of single center data in the present study, but we hope to improve the formula by using national multicenter data in the future[31].With development of living donor liver transplantation (LDLT), especially improvement of right graft adult-to-adult LDLT, the danger of donating has been paid more and more attention. The exact liver volume is not only relevant for the recipient, but also for the donor to avoid dangerous life-threatening residual liver volumes.Research frontiersScholars of different countries established several standard liver volume (SLV) formulae from clinical data. The authors estimated the SLV using computed tomography or reported formulae. However, there was a gap between these estimates and the actual liver volumes for Chinese adults. Recently, they developed a new formula (named the Chengdu formula) to estimate SLV using data from 115 LDLTs.Innovations and breakthroughsWith the Chengdu formula, the SLVs were evaluated in 76 cases of LDLT performed from January 2008 to April 2009. Its accuracy was compared to that of other internationally reported formulae to assess which formula is the most accurate for Chinese adults.ApplicationsWith national multicenter data in the future, the Chengdu formula for SLV can be improved. It may then be applied to the evaluation of donors for LDLT. TerminologyStandard liver volume: normal liver volume without disease affecting the volume of liver.Peer reviewVery interesting manuscript dealing with a very hot topic: determination of optimal size matching between graft and recipient in LDLT by means of race-adapted calculation of liver volumes. The recently published liver volume formula for Chinese people (Chengdu formula) has been demonstrated to be more reliable than others and therefore it should be adopted especially in this particular form of LT.REFERENCES1 Khalaf H, Shoukri M, Al-Kadhi Y, Neimatallah M, Al-Sebayel M. Accurate method for preoperative estimation of the right graft volume in adult-to-adult living donor liver transplantation. Transplant Proc 2007; 39: 1491-14952 Avolio AW, Siciliano M, Barbarino R, Nure E, AnnicchiaricoBE, Gasbarrini A, Agnes S, Castagneto M. Donor risk index and organ patient index as predictors of graft survival after liver transplantation. Transplant Proc 2008; 40: 1899-19023 Gruttadauria S, Marsh JW, Vizzini GB, di Francesco F,Luca A, Volpes R, Marcos A, Gridelli B. Analysis of surgical and perioperative complications in seventy-five right hepatectomies for living donor liver transplantation. World J Gastroenterol 2008; 14: 3159-31644 Fan ST, Lo CM, Liu CL, Yong BH, Chan JK, Ng IO. Safety ofdonors in live donor liver transplantation using right lobe grafts. Arch Surg 2000; 135: 336-3405 Lee SG, Park KM, Hwang S, Lee YJ, Kim KH, Ahn CS, ChoiDL, Joo SH, Jeon JY, Chu CW, Moon DB, Min PC, Koh KS, Han SH, Park SH, Choi GT, Hwang KS, Lee EJ, Chung YH, Lee YS, Lee HJ, Kim MH, Lee SK, Suh DJ, Kim JJ, Sung KB.Adult-to-adult living donor liver transplantation at the Asan Medical Center, Korea. Asian J Surg 2002; 25: 277-2846 Li FG, Yan LN, Li B, Zeng Y, Wen TF, Xu MQ, Wang W.Estimation formula of standard liver volume for Chinese adults. Sichuan Daxue Xuebao 2009; 40: 302-3067 Urata K, Kawasaki S, Matsunami H, Hashikura Y, IkegamiT, Ishizone S, Momose Y, Komiyama A, Makuuchi M.Calculation of child and adult standard liver volume for liver transplantation. Hepatology 1995; 21: 1317-13218 Heinemann A, Wischhusen F, Puschel K, Rogiers X.Standard liver volume in the Caucasian population. Liver Transpl Surg 1999; 5: 366-3689 Vauthey JN, Abdalla EK, Doherty DA, Gertsch P,Fenstermacher MJ, Loyer EM, Lerut J, Materne R, Wang X, Encarnacion A, Herron D, Mathey C, Ferrari G, Charnsangavej C, Do KA, Denys A. Body surface area and body weight predict total liver volume in Western adults.Liver Transpl 2002; 8: 233-24010 Chan SC, Liu CL, Lo CM, Lam BK, Lee EW, Wong Y, FanST. Estimating liver weight of adults by body weight and gender. World J Gastroenterol 2006; 12: 2217-222211 Trotter JF, Wisniewski KA, Terrault NA, Everhart JE,Kinkhabwala M, Weinrieb RM, Fair JH, Fisher RA, Koffron AJ, Saab S, Merion RM. Outcomes of donor evaluation in adult-to-adult living donor liver transplantation. Hepatology 2007; 46: 1476-148412 Duran C, Aydinli B, Tokat Y, Yuzer Y, Kantarci M, AkgunM, Polat KY, Unal B, Killi R, Atamanalp SS. Stereological evaluation of liver volume in living donor liver trans-plantation using MDCT via the Cavalieri method. Liver Transpl 2007; 13: 693-69813 Morimoto T, Ichimiya M, Tanaka A, Ikai I, Yamamoto Y,Nakamura Y, Takada Y, Inomata Y, Honda K, Inamoto T, Tanaka K, Yamaoka Y. Guidelines for donor selection and an overview of the donor operation in living related liver transplantation. Transpl Int 1996; 9: 208-21314 Yamashiki N, Sugawara Y, Tamura S, Kaneko J, NojiriK, Omata M, Makuuchi M. Selection of liver-transplant candidates for adult-to-adult living donor liver transplantation as the only surgical option for end-stage liver disease. Liver Transpl 2006; 12: 1077-108315 Frericks BB, Kirchhoff TD, Shin HO, Stamm G, MerkesdalS, Abe T, Schenk A, Peitgen HO, Klempnauer J, Galanski M, Nashan B. Preoperative volume calculation of the hepatic venous draining areas with multi-detector row CT in adult living donor liver transplantation: Impact on surgical procedure. Eur Radiol 2006; 16: 2803-281016 Iida T, Yagi S, Taniguchi K, Hori T, Uemoto S, YamakadoK, Shiraishi T. Signifi cance of CT attenuation value in liver grafts following right lobe living-donor liver transplantation.Am J Transplant 2005; 5: 1076-108417 Kim BS, Kim TK, Kim JS, Lee MG, Kim JH, Kim KW, SungKB, Kim PN, Ha HK, Lee SG, Kang W. Hepatic venous congestion after living donor liver transplantation with right lobe graft: two-phase CT fi ndings. Radiology 2004; 232: 173-18018 Cho JY, Suh KS, Lee HW, Cho EH, Yang SH, Cho YB, Yi NJ,Kim MA, Jang JJ, Lee KU. Hypoattenuation in unenhanced CT reflects histological graft dysfunction and predicts 1-year mortality after living donor liver transplantation.Liver Transpl 2006; 12: 1403-141119 Choi JY, Lee JY, Lee JM, Kim SH, Lee MW, Han JK, ChoiBI. Routine intraoperative Doppler sonography in the evaluation of complications after living-related donor liver transplantation. J Clin Ultrasound 2007; 35: 483-49020 Kato H, Usui M, Azumi Y, Ohsawa I, Kishiwada M, SakuraiH, Tabata M, Isaji S. Successful laparoscopic splenectomy after living-donor liver transplantation for thrombocytopenia caused by antiviral therapy. World J Gastroenterol 2008; 14: 4245-424821 Ohdan H, Tashiro H, Ishiyama K, Ide K, Shishida M, IreiT, Ohira M, Tahara H, Itamoto T, Asahara T. Microsurgical hepatic artery reconstruction during living-donor liver transplantation by using head-mounted surgical binocular system. Transpl Int 2007; 20: 970-97322 Oya H, Sato Y, Yamamoto S, Takeishi T, Nakatsuka H,Kobayashi T, Hara Y, Hatakeyama K. Surgical proceduresShi ZR et al. Liver volume formulae for Chinese adults 4065for decompression of excessive shear stress in small-for-size living donor liver transplantation--new hepatic vein reconstruction. Transplant Proc 2005; 37: 1108-111123 Lee SS, Kim KW, Park SH, Shin YM, Kim PN, Lee SG, LeeMG. Value of CT and Doppler sonography in the evaluation of hepatic vein stenosis after dual-graft living donor liver transplantation. AJR Am J Roentgenol 2007; 189: 101-10824 Asakuma M, Fujimoto Y, Bourquain H, Uryuhara K, HayashiM, Tanigawa N, Peitgen HO, Tanaka K. Graft selection algorithm based on congestion volume for adult living donor liver transplantation. Am J Transplant 2007; 7: 1788-179625 del Pozo JL. Update and actual trends on bacterial infectionsfollowing liver transplantation. World J Gastroenterol 2008;14: 4977-498326 Miraglia R, Maruzzelli L, Caruso S, Milazzo M, Marrone G,Mamone G, Carollo V, Gruttadauria S, Luca A, Gridelli B.Interventional radiology procedures in adult patients who underwent liver transplantation. World J Gastroenterol 2009;15: 684-69327 Shoji M, Ohkohchi N, Fujimori K, Koyamada N, SekiguchiS, Kawagishi N, Tsukamoto S, Shirahata Y, Sato K, SatomiS. The safety of the donor operation in living-donor liver transplantation: an analysis of 45 donors. Transpl Int 2003;16: 461-46428 Kawagishi N, Ohkohchi N, Fujimori K, Doi H, SakuradaM, Kikuchi H, Oikawa K, Takayama J, Satomi S. Safety of the donor operation in living-related liver transplantation: analysis of 22 donors. Transplant Proc 1998; 30: 3279-328029 Yoshizumi T, Taketomi A, Kayashima H, Yonemura Y,Harada N, Ijichi H, Soejima Y, Nishizaki T, Maehara Y.Estimation of standard liver volume for Japanese adults.Transplant Proc 2008; 40: 1456-146030 Hirata M, Harihara Y, Kitamura T, Hisatomi S, KatoM, Dowaki S, Mizuta K, Sugawara Y, Kita Y, Kubota K, Takayama T, Kawarasaki H, Hashizume K, Makuuchi M.The infl uence of donor age to graft volume increase rate in living donor liver transplantation. Transplant Proc 2001; 33: 1416-141731 Schiano TD, Bodian C, Schwartz ME, Glajchen N, Min AD.Accuracy and signifi cance of computed tomographic scan assessment of hepatic volume in patients undergoing liver transplantation. Transplantation 2000; 69: 545-550S- Editor Tian L L- Editor Cant MR E- Editor Ma WH4066 ISSN 1007-9327 CN 14-1219/R World J Gastroenterol August 28, 2009 Volume 15 Number 32。
了修正,得出了新的MELDNa评分:MELD-Na=MELD - Na-0.025MELD(140-Na)+140。
新的MELD-Na评分可以更好地预测自登记后90天内的死亡率,当血钠在1 25mmol/L~140mmol/L这一区间时,血钠每降低1mmol/L,死亡的风险就会升高5%。
三、CT体积计算基于肝脏移植的需要,Urata等在1995年总结了96例日本患者的数据,得到了标准肝脏体积的计算公式,成人单位体重的肝脏体积为20.5±1.9ml/kg,单位体表面积的肝脏体积为712.0±51.2ml/m2,同时肝脏重量和体积之间存在1.19ml/g的转换系数。
欧美各国学者也已总结出了不同种族人群的肝脏体积(或重量)与体重(或体表面积)之间的计算公式,但各种族人群的公式不一定通用。
活体肝移植的经验告诉我们,全肝30%~35%的剩余体积对供体是较为安全的。
一般意义上认为40%的估计标准肝体积或移植物受体重量比为0.8%的供肝对受体是必需的,小于这一低限则容易发生小肝综合征,但目前已有报道的肝移植术后存活的体积极限为受体体重的0.59%。
随着计算机技术的发展,CT体积计算可以较准确地计算出解剖性肝切除后的剩余肝体积。
但肝脏实质病变对肝功能的影响却无法从CT作出准确的判断,CT所能显示的仅仅是肝脏的形态和体积。
因而,在活体肝移植供体的术前评估中,肝脏穿刺组织学检查依然是常规术前项目,在合并肝脏实质病变的肝脏肿瘤安全切除范围的评估中仍需要更多地依赖临床医师的个人经验。
四、去唾液酸糖蛋白受体功能显像技术从前面介绍的几种肝功能评估方法可以看出,除了CT三维成像技术能计算出剩余肝的体积,其余评估均无法预测术后剩余肝脏的功能。
另外,在肝脏病变情况下体积并不能代表功能,故目前尚缺乏一种三维的肝脏功能评估系统,应用该系统,可模拟手术切除,并能反映出剩余肝脏的功能,最后用以推算出手术风险供临床医师。
标准肝体积计算公式
肝脏体积是评估肝功能和疾病诊断中的重要指标之一。
下面我将介绍一种常用
的计算肝脏体积的标准公式。
在临床上,常用的计算肝脏体积的公式是根据肝脏的长轴、短轴和横断面面积
来计算的。
这个公式被称为康奈尔公式,公式如下:
肝脏体积(cm³)= 0.52 ×长轴(cm)×短轴(cm)×横断面面积(cm²)
根据这个公式,我们可以通过测量肝脏的长轴和短轴,以及计算肝脏横断面的
面积,来估算肝脏的体积。
这种方法相对简便,并被广泛应用于临床实践中。
为了测量肝脏的长轴和短轴,常常使用超声或影像学技术,如计算机断层扫描(CT)或磁共振成像(MRI)。
通过这些技术,医生可以获取肝脏的长轴和短轴
的尺寸,然后用这些尺寸计算出肝脏的体积。
需要注意的是,在计算肝脏体积时,使用的单位必须一致。
一般情况下,公式
中的尺寸都以厘米(cm)为单位,面积以平方厘米(cm²)为单位。
保持单位的一
致性非常重要,以确保计算结果的准确性。
总结起来,标准肝脏体积计算公式是康奈尔公式,通过测量肝脏的长轴和短轴,并计算出肝脏的横断面面积,可以估算肝脏的体积。
这个公式在临床实践中是一种常用且可靠的计算方法,帮助医生评估肝功能和进行疾病诊断。

标准肝体积计算公式肝脏是人体内重要的器官之一,它不仅具有排毒、合成蛋白质和胆汁等重要功能,还承担着调节血糖和脂肪代谢的重要作用。
因此,了解肝脏的生理特性和计算肝体积的标准公式对于临床诊断和治疗具有重要意义。
本文将介绍肝体积的计算方法以及其在临床上的应用。
肝体积的计算是通过影像学检查得出的,常用的方法有CT扫描、MRI和B超等。
在进行肝体积计算时,需要准确测量肝脏的长度、宽度和厚度,并根据这些数据应用相应的计算公式得出肝体积。
下面将介绍标准的肝体积计算公式:肝体积(ml)=0.55×长轴(cm)×短轴(cm)×厚度(cm)。
在这个公式中,长轴、短轴和厚度分别代表肝脏在影像上的三个方向的尺寸。
通过测量这些尺寸并代入公式,便可以得出肝体积的近似数值。
需要注意的是,这个计算公式是基于椭球体积的计算方法,因此在实际应用中可能存在一定的误差,但一般来说误差范围在可接受范围内。
肝体积的计算对于临床诊断和治疗具有重要的指导意义。
首先,肝体积的变化可以反映肝脏的生理状态,如肝硬化、脂肪肝等疾病会导致肝体积的改变,因此通过肝体积的计算可以对这些疾病进行诊断和监测。
其次,在肝移植手术中,肝体积的计算可以帮助医生评估移植肝的大小和适配性,从而提高手术的成功率。
此外,肝体积的计算还可以指导肝肿瘤的治疗,如手术切除、放疗和化疗等。
总之,肝体积的计算公式是临床医学中的重要工具,它可以帮助医生了解肝脏的生理状态,指导临床诊断和治疗。
通过准确测量肝脏的尺寸并应用标准的计算公式,可以得出肝体积的近似数值,为临床工作提供重要参考。
希望本文的介绍能够帮助大家更好地理解肝体积的计算方法及其在临床上的应用,为医学工作者和患者提供参考和帮助。
肝癌转化治疗策略要点(完整版)摘要以外科为主导的综合治疗是肝癌诊疗的重要共识。
肝切除术、肝移植术是肝癌患者获得长期生存的重要手段。
随着肝脏外科技术的发展,肝脏手术已无禁区。
转化治疗为初始不可切除肝癌患者带来了手术根治的希望。
本文对剩余肝体积不足肝癌的转化治疗、肿瘤学不可切除中晚期肝癌的降期转化治疗、转化后手术时机选择等问题进行探讨,并就形成肝癌转化治疗的规范进行展望。
肝癌转化治疗是将不可切除肝癌转为可切除肝癌。
肝癌不可切除的原因主要包括两方面:一是患者全身情况不能承受手术创伤、肝功能不能耐受、剩余肝体积(future liver remnant,FLR)不足等外科学不可切除情况;二是技术可切除,但切除以后不能获得比非手术治疗更好的疗效,称为肿瘤学不可切除。
笔者认为肝癌转化治疗就是运用积极的治疗方法,消除肝癌不可切除因素,将不可切除的手术转化为可根治性切除的手术,在围手术期安全的前提下达到手术安全性和彻底性。
本文对FLR不足和肿瘤学不可切除肝癌的转化治疗方法和应对策略作一探讨。
一、FLR不足肝癌的转化治疗FLR是否足够是影响术后肝功能衰竭和围手术期死亡的决定性因素。
目前临床上评估肝脏储备功能主要通过吲哚氰绿滞留试验定量肝脏储备功能。
吲哚氰绿15 min滞留率(indocyanine green retention rate at 15 minute,ICG R15)<10%的患者可耐受大范围的肝切除,同时必须保留足够的FLR才可以降低肝切除术后肝功能衰竭的发生率:对于正常肝脏,FLR/标准肝体积(standard liver volume,SLV)需大于30%;对于慢性肝病患者,FLR/SLV需大于40%;对于肝硬化患者,FLR/SLV则要超过50%。
对于前期评估FLR不足的患者,或邻近肝内重要管道的肝脏肿瘤,若要达到切缘>1 cm的目标,需实施计划性肝切除。
目前,对于有计划使FLR再生、肥大的过程还没有共识的专业名词,较常用的名词包括"养肝技术""增肝技术""预留肝脏容积扩增技术(future liver remnant augumentation technique,FLRAT)"等,笔者认为"FLRAT"更为贴切。
肝脏体积(liver volume,LV)测量不仅可以定量评价肝脏大小,还能间接反映肝功能情况,具有广泛而重要的临床应用价值,在评估肝硬化肝功能储备、肝脏肿瘤手术方式选择和预后评价、肝移植中都有重要意义。
1 肝脏体积测量方法常用的肝脏体积测量方法包括水测法、B超、SPECT、CT和MRI。
水测法被认为能够测量肝脏的实际体积,B超、SPECT、CT、MRI测量肝脏体积原理基本相同,又各有其优缺点,以下分别做简单介绍。
1.1 水测法将离体肝脏室温下放入盛满水的容器,放入标本后使容器内水外溢,收集全部溢出的水并测量其体积,即为待测肝脏体积。
该方法只能用于离体肝脏测量,不能用于术前活体肝体积评估。
Heinemann等[1]观察到在死亡当时至死后检查这段时间中LV无明显变化,但由于死亡原因不同,如循环血容量减少或心源性休克,及其他情况导致肝淤血,死后LV可能会比真实情况减少或增多[2]。
又由于肝脏的比重近似于水的比重[3,4],有学者在原位肝移植后,取下的肝脏在去除附着的韧带、胆囊、门静脉结构和其他组织,但不去除移出肝中的血液(因为活体肝含有大量血液)后立即称取肝脏重量,以此作为肝脏的实测体积,认为这种方法避免了经过福尔马林固定后因组织萎缩造成的人为误差[5]。
1.2 B超测量肝脏体积利用超声探头平行或垂直于人体纵轴得到肝脏纵切面或横截面,由计算机分别测出这些平行切面的面积,将所测面积与平行面积体间的距离进行积分,即可得到肝脏体积值。
V an Thiel等[3]发现超声测量肝脏体积值接近水测法体积值,而且比CT更准确。
Hatsuno等[6]比较超声和CT测量左外叶体积,发现没有明显差异,但超声测量值略低于CT测量值。
超声测量肝脏体积优势在于安全、无射线辐射或无需使用造影剂、可重复、价格较低,但超声检查易受操作者经验及腹腔内肠道气体、钙化等因素干扰,这些直接影响到断层的截取、肝脏边界的确定,使最后得出的结果存在误差。

肝功能的评估发表时间:2009-03-23 发表者:赵中辛 (访问人次:861)对肝硬化患者肝功能的储备及预后评估是临床医师高度关注的课题。
由于肝功能是多方面的, 影响肝硬化患者预后的因素比较复杂, 各种单项指标在判断肝硬化患者预后方面均有一定的临床价值, 同时又存在一定的局限性。
因此, 长期以来人们注重利用多项指标进行综合判别, 即把能体现肝功能损害程度的一些主要指标分成不同等级, 以判断肝硬化患者的预后。
一个好的模型标准应该是指标较少、容易获得, 且客观、易于推广。
在循证医学方法的指导下, 人们通过经验总结、回顾性研究或前瞻性研究对肝脏功能作出了分级、评分或将肝功能量化。
以下将就世界上使用最为广泛的两种肝脏功能评估方法进行介绍。
1 (Child-Turcotte-Pugh)CTP分级1.1 CTP分级的演变1961年Child和他的同事总结了131名肝硬化门静脉高压患者或其他门静脉高压患者门腔静脉吻合术后的病死率,将肝硬化患者根据病情的严重程度分为轻、中、重组。
1964年Ch ild和Turcotte将Child-Turcotte分级作为专著“Surgery and Portal Hypertension”中的一章而发表,当时采用了到目前仍常用的五项指标(白蛋白、腹水、肝性脑病、胆红素、营养状况),将肝硬化患者分为A、B、C组。
A组患者没有黄疸、腹水与肝性脑病,白蛋白水平正常,营养状况较好,可以正常工作;C组患者为晚期肝病患者:有黄疸、腹水、肝性脑病,甚至昏迷,营养状况较差,白蛋白水平较低;B组介于A组与C组之间。
他们还对1 28名进行了选择性门腔静脉分流术后的患者的病死率进行了回顾性研究,其中A、B、C组的病死率分别为0%、9%、53%,即证实了此分级可较好的评价肝功能的储备。
虽然上述的指标的选择与分级没有经过实验证明、统计学证实,但经过40余年的临床实践,Child-Turcotte分级仍得到广泛的应用。
肝切除术患者肝储备功能的评估肝切除术后一个严重的并发症是肝功能衰竭(简称肝衰)。
它一旦发生往往导致病人死亡,是肝切除手术死亡的主要原因之一。
肝衰的发生常常是由于对不能耐受肝切除的肝脏施行了肝切除或由于切肝量过大、超过了肝脏的代偿能力所致。
正常肝脏具有强大的储备功能,可以耐受75%的切肝量。
但在我国乃至亚洲,肝切除的主要适应证是肝细胞性肝癌(简称肝癌),而80%左右的肝癌伴有不同程度的肝硬化。
发生硬化的肝脏还有多少储备功能、还能耐受多大范围的肝切除?这是在施行每例肝癌肝切除术前所要回答的问题。
事实上,人们一直在研究精确的肝储备功能检测方法,希望籍此在术前能够确定安全的切肝量。
目前临床上,在肝切除前除了作常规的肝功能试验外,越来越多采用新的更加敏感的肝功能指标来评估肝储备功能,以指导肝切除手术适应证和切肝量的掌握。
(一)常规肝功能检查常规肝功能检查项目包括胆红素、白蛋白、球蛋白、白/球蛋白比、丙氨酸转氨酶(ALT)和门冬氨酸转氨酶(AST)、蛋白电泳、凝血酶原时间等。
1.胆红素:肝脏处理胆红素的储备能力较大,因此,一旦血清胆红素水平明显升高,则表明肝功能受损较重。
一般认为胆红素>50μmol /L,不宜行任何类型肝切除;胆红素40~50μmol/L,经保肝治疗后降至30μmol/L以下,而其他肝功能指标基本正常,可行肝楔形切除、单肝段切除;胆红素20~30μmol/L,可行双肝段切除。
需要指出的是,不可将肝癌伴有黄疽均判为肝功能失代偿而放弃手术治疗,部分病例是由于肿瘤压迫、胆管癌栓等阻塞胆管而引起的黄疽,临床上须注意鉴别,此时胆红素升高以结合型为主,多伴有肝内胆管扩张、碱性磷酸酶(ALP)升高,这类病人需要手术治疗,也往往能耐受手术。
2.白蛋白和球蛋白:血清白蛋白>40g/L常表明肝储备功能良好,肝切除不受限制;白蛋白在正常值的低限(35g/L),则表示肝储备功能有限,肝切除范围应限制在2个肝段以内;白蛋白在31~34g/L之间,经保肝、补充白蛋白治疗后能上升至35g/L以上,可行单肝段或肝楔形切除;白蛋白≤30g/L,则表明肝功能已失代偿,不宜作任何类型肝切除。
标准肝脏体积计算公式咱们先来聊聊啥是标准肝脏体积计算公式。
这玩意儿可重要啦,在医学里头那是相当关键的一个东西。
就说我之前遇到过这么一档子事儿。
有个朋友的亲戚,因为身体不舒服去医院检查,医生提到了肝脏体积的问题。
这可把他们一家人给弄懵了,啥是肝脏体积?咋算?标准肝脏体积计算公式,其实就是通过一系列的测量和计算方法,来得出一个相对准确的肝脏体积数值。
这对于判断肝脏的健康状况、疾病诊断以及手术规划都特别有用。
一般来说,常用的计算方法会考虑到人的身高、体重、体表面积这些因素。
比如说,有一种计算公式是这样的:肝脏体积(ml)= 706.2×体表面积(m²)+ 2.4。
这里的体表面积呢,又有专门的计算方式。
咱们再深入一点,为啥要算这个肝脏体积呢?想象一下,肝脏就像一个工厂,要是这个工厂的大小出了问题,那它干活儿的效率能正常吗?比如说,肝脏要是萎缩变小了,可能就没办法正常处理身体里的各种物质,毒素排不出去,营养合成也受影响。
还有啊,医生在准备给病人做肝脏相关的手术时,也得先搞清楚肝脏的体积。
不然一刀下去,切多了切少了都不行。
切多了,肝脏功能不够用;切少了,病又治不好。
另外,不同年龄段、不同性别的人,肝脏体积也会有所不同。
小孩子在成长过程中,肝脏也跟着长大;而成年人的肝脏体积相对稳定,但随着年龄增长或者某些疾病的影响,也可能会发生变化。
再回到我朋友亲戚那个事儿,后来经过医生详细的解释和计算,搞清楚了肝脏体积的情况,也制定了合适的治疗方案。
总之,标准肝脏体积计算公式虽然听起来有点复杂,但它真的是医学诊断和治疗中的一个重要工具,能帮助医生更好地了解咱们身体里这个重要的“化工厂”的状况,从而给出更准确有效的治疗方案。
希望大家都能重视自己的健康,让身体里的每个“零件”都正常运转!。
国人正常肝脏体积计算公式的研究及意义
肝脏是人体中最大的脏器之一,其大小和体积与人的年龄、性别、身高、体重、肥胖程度、肝病状态等有关。
因此,了解人体中肝脏的
正常大小和体积的计算公式对于医疗诊断和治疗非常重要。
目前常用的计算肝脏体积的公式有两种:线性方法和体积法。
线
性方法是根据肝脏的长、宽、高来计算其体积,常用公式为:肝脏体
积(ml)=0.681×长(cm)×宽(cm)×高(cm)+8.785。
而体积法
是利用影像学技术(如CT、MRI等)测量肝脏的体积,并根据体积公
式计算。
体积法因其精度高,应用范围广而在临床上更为常用。
了解人体中肝脏的正常体积可以帮助医生判断肝脏是否偏大或偏小,对于肝脏疾病的诊断和治疗也有很大的帮助。
例如,对于肝硬化、肝癌等疾病,肝脏的大小与体积的变化可以作为诊断标准之一,也可
以通过检测肝脏体积的变化来判断治疗的有效性。
总之,计算人体中肝脏的正常大小和体积,对于肝脏疾病的诊断
和治疗具有重要的意义。
肝体积
正常成年人肝脏的平均积为1250.2±141.0 cm3,其与体表面积、身高、体重呈正相关,相关系数分别为0.96、0.90、 0.79.
年龄、性别对成人肝脏体积大小的影响无显著性.
由体表面积推导正常人群标准肝脏体积公式为:LV(cm3)=613×BSA(m2)+162.8.
体表面积(m2)=0.0061×身高(cm)+0.0128×体重(kg)-0.1529
中国人适用的通式为体表面积S=0.0061×身高+0.0124×体重-0.0099.
如:身高170厘米,体重70公斤,他的体表面积=0.0061*170+0.124*70=1.905平方米给你一个简单好记好算的.
(身高+体重)/100 - 0.6 身高单位是“厘米”,体重单位是“公斤”.
体表面积,身材大小不同,人体的基础代谢总量也显然不同,基础代谢与人体的体表面积呈比例关系。
基础代谢率如果以单位体表面积表示,则比较恒定。
因此基础代谢率以KJ·体表面积(m2)-1·h-1”表示。
人体的体表面积与体重及身高显著相关。
我国成年人的体表面积可以按下式计算: A:体表面积(m2) H:身高(cm) W:体重(kg) A=0.00659H+0.0126W-0.1603
人体体表面积计算法计算我国人的体表面积,一般认为许文生氏公式尚较适用,即:
体表面积(m2)=0.0061×身高(cm)+0.0128×体重(kg)-0.1529。
Zheng-Rong Shi, Lu-Nan Yan, Bo Li, Tian-Fu Wen, Liver Transplantation Division, Department of Surgery, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, ChinaAuthor contributions: Shi ZR, Yan LN participated in the research design and writing of the paper; all authors participated in the performance of the research; Shi ZR contributed analytic tools and data analysis.Correspondence to: Lu-Nan Yan, MD, PhD, Liver Trans-plantation Division, Department of Surgery, West China Hospital, Sichuan University, Chengdu 610041, Sichuan Province, China. yanlunan2009@ Telephone: +86-28-85422867 Fax: +86-28-85422867 Received: May 31, 2009Revised: July 16, 2009 Accepted: July 23, 2009Published online: August 28, 2009AbstractAIM: To evaluate different standard liver volume (SLV) formula and verify the applicability of the formulae for Chinese adults.METHODS:Data from 70 cases of living donor liver transplantation (LDLT) performed at our transplanta-tion centers between January 2008 and April 2009 were analyzed. SLV was estimated using our recently reported formula [the Chengdu formula: SLV (mL) = 11.5 × body weight (kg) + 334] and other reported formulae used for Chinese adults. Actual intraoperative liver volumes were obtained from a review of the patients’ medical records. RESULTS:The actual right liver volume was not signifi -cantly different from the estimated right liver volume de-termined by the Chengdu formula, but was signifi cantly smaller than estimates using the Heinemann, Urata, Vauthey, and Lee formulae (P < 0.01), and signifi cantly larger than estimates using the Fan formula (P < 0.05). CONCLUSION: The Chengdu formula was demon-strated to be reliable by its application in LDLT.© 2009 The WJG Press and Baishideng. All rights reserved.Key words: Standard liver volume; Living donor liver transplantation; Chinese adult; Liver volume formulaPeer reviewers: Silvio Nadalin, MD, PhD, Director of Transplant Program, Department of General, Visceral and Transplant Surgery, University Hospital Tübingen, Hoppe Seyler Strasse 3, 72076 Tübingen, Germany; Salvatore Gruttadauria, MD, Assistant Professor, Abdominal Transplant Surgery, ISMETT, Via E. Tricomi, 190127 Palermo, ItalyShi ZR, Yan LN, Li B, Wen TF. Evaluation of standard liver volume formulae for Chinese adults. World J Gastroenterol 2009; 15(32): 4062-4066 Available from: URL: http://www. /1007-9327/15/4062.asp DOI: http://dx.doi. org/10.3748/wjg.15.4062INTRODUCTIONLiving donor liver transplantation (LDLT) has been used to alleviate the shortage of available liver donors. Accurate estimation of the standard liver volume (SLV) of the living donor and recipient is crucial. Overestimation of the donor’s SLV may result in excessive hepatic resection leading to liver failure, while underestimation of the recipient’s SLV may result in small-for-size graft syndrome[1-5]. Since 2001, our transplant centers have carried out 212 LDLTs. We estimated the SLV using computed tomography (CT) or reported formulae. However, there was a difference between these estimates and the actual liver volumes (ALVs) for Chinese adults. Recently, we developed a new formula (named the Chengdu formula) to estimate SLV using data from 115 LDLTs[6]. The formula is: SLV (mL) = 11.5 × body weight (kg) + 334. Using this formula, the SLVs were evaluated in 76 cases of LDLT performed from January 2008 to April 2009. Its accuracy was compared to that of other internationally reported formulae[7-10] to assess which formula is the most accurate for Chinese adults. MATERIALS AND METHODSPatient selectionThe data from 76 living donors were analyzed. Inclusion criteria were: (1) a healthy adult donor, aged 19-59 years;(2) right liver graft without middle hepatic vein; (3) adult-to-adult LDLT; (4) single donor; (5) no history of long term drinking. Exclusion criteria: (1) donor age < 18 or > 60 years; (2) left hepatic graft or left lateral lobe graft;(3) double donor grafts; (4) adult-to-child transplant; (5) donors who were hepatitis B or C carriers[11-14].Clinical dataData of preoperative donors included age, sex, heightOnline Submissions: World J Gastroenterol 2009 August 28; 15(32): 4062-4066 wjg@ World Journal of Gastroenterology ISSN 1007-9327doi:10.3748/wjg.15.4062 © 2009 The WJG Press and Baishideng. All rights reserved.Evaluation of standard liver volume formulae for Chinese adultsZheng-Rong Shi, Lu-Nan Yan, Bo Li, Tian-Fu WenBRIEF ARTICLES(BH, measured to the nearest 1 cm), body weight (BW , measured to the nearest 0.5 kg), and body surface area (BSA) calculated using the DuBois formula: BSA (m 2) = BW (kg) 0.425 × BH (cm) 0.725 × 0.007184 or the Mosteller formula: BSA (m 2) = square root BH (cm) × BW (kg)/3600. From the diaphragm to the superior mesenteric artery plane, the entire liver image was scanned using a 7 mm thick layer. In the Leonardo workstation, the LV was measured by venous phase images [15,16]. All preoperative CT examinations of donors were performed by a single radiologist and all donor procedures were performed by the same surgical unit. The volume of the grafts was measured by a 3 L beaker using a drainage method intraoperatively and the error was less than 10 mL [17,18].Right liver graft without middle hepatic vein reconstruction from a living donor was performed as described, with temporary occlusion of the right portal vein (PV) and right hepatic artery and use of ultrasonography to guide parenchymal transection. The right hepatic duct, right hepatic artery, right portal vein branch, and right hepatic vein were transected approximately 2-3 mm from the con fl uence [19,20], leaving the donor’s main PV and confluence intact. The graft was flushed with University of Wisconsin solution through the PV and hepatic artery [21,22].The volume of 70 livers was calculated using the Chengdu standard LV formula [6] as described above. The estimated right LV (ERLV) was obtained by multiplying the SLV by the proportion of the LV contributed by the right lobe on CT. The actual right LV (ARLV) was obtained by intraoperative measurement. The differencebetween the ERLV and ARLV was statistically evaluated. The formulae of Heinemann et al [8], Urata et al [7], Vauthey et al [9], Lee et al [5], and Fan et al [4] in addition to our own formula [6] were used to determine the estimated SLV (ESLV) of our donor livers. The previously reported formulae are shown in Table 1. For each liver, we calculated the difference between the ALV and volume estimated by each formula (ELV).Statistical analysisAfter testing for normal distribution (kurtosis and skewness tests), descriptive statistics were calculated and data were expressed as means ± SD for age (year), BW (kg), BH (cm), body mass index (BMI), and BSA. The ERLV-ARLV and the ELV-ALV were compared by the 2-sided paired-samples t -test. P < 0.05 was considered statistically significant. All statistical analyses were performed using the SPSS (version 13.0) program.RESULTSSeventy donors (all Chinese; 53 men and 17 women; mean age, 32.21 ± 10.07; range, 19-57 years) met the selection criteria. All donors were related to the recipients.The characteristics of donors are shown in Table 2. All donors were considered healthy on the basis of BMI. All but one donor with a BMI of 17 kg/m 2 had a BMI of 18-28 kg/m 2. The mean volume of the right lobe on CT was 658.98 ± 81.14 mL and represented 55.4% ± 3.7% of the whole liver on CT.The mean ELV and mean ERLV using the Chengdu standard formula were 1058.70 ± 96.74 mL and 586.15 ± 67.17 mL, respectively. The mean ARLV was 578.58 ± 72.33 mL. Differences for individual donors between ERLV and ARLV were not signi fi cant (t = -1.882, P = 0.064). A plot of the relationship of ARLV to the ERLV calculated using the Chengdu formula is shown in Figure 1. The mean total LV determined preoperatively on CT was 1189.53 ± 114.75 mL. The mean RLV on CT without the middle hepatic vein was 658.98 ± 81.14 mL, and 55.4% ± 3.7% of the total LV . The ALV calculated from the volume of the graft and the ratio of the RLV to the total LV on CT (%) was 1050.10 ± 107.41 mL. The Heinemann, Urata, Vauthey, and Lee formulae signi fi cantly overestimated the LV (P < 0.01), while the Fan formula significantly underestimated the LV (P <Shi ZR et al . Liver volume formulae for Chinese adults 4063ESLV: Estimated standard liver volume; BSA: Body surface area; BW: Body weight; CT: Computed tomography; LDLT: Living donor liver transplantation.Table 2 Donor characteristicsMHV: Middle hepatic vein.0.05). There was no signi fi cant difference between ALV and ELV using the Chengdu formula (Figure 2).DISCUSSIONCT has become a standard method for assessing livergraft volume in living donors. Estimation of LV by CT (compared to actual volume) has a margin of error of 5%-25%[23,24]. In the present study, all donors had preoperative CT assessment of LV (mean total LV , 1189.53 ± 114.75 mL and mean volume of right lobe graft without middle hepatic vein, 658.98 ± 81.14 mL). The actual volume of the right liver was 578.58 ± 72.33 mL. In the present study, the LV on CT was 10%-20% higher than the ALV [25-27]. The reasons may be as follows: (1) Preoperative CT measurement is carried out under normal blood fl ow conditions. Perioperatively, liver resection interrupts the blood supply causing a loss of liquid volume, collapse of supporting structures, and thereby reduction in the volumeof the liver. (2) Sources of error (partial volume effect, inter-observer variation, and respiratory movements) may account for this difference [28].The difference between the ERLV (using our formula) and ARLV was compared to the difference between ERLV, calculated using the formulae of Heinemann, Urata, Vauthey, Lee, and Fan, and ARLV in our 70 donors. The Heinemann, Urata, Vauthey, and Lee formulae overestimated LV (P < 0.01)[29]. The reasons may include: ethnic differences (patients in Europe and the United States were Caucasian). All except the Sheung Tat Fan and Chengdu formulae were used to estimate LV from CT LV or autopsy LV. Estimates of LV by CT were 5%-25% higher than the ALV [30].Statistical analysis showed that the Fan formula tends to underestimate LV. The weight and height of the donors in our study were higher than of those in the Hong Kong group. This may be one of the reasons both results are very close (Table 3). Above all, we believe thatALV: Actual liver volume; ND: Not determined.Figure 1 Correlation between actual right liver volume (ARLV) and estimated right liver volume (ERLV) by the Chengdu formula. When both were the same, a dot would be on the linear line.500 600 700Graft ARLV700600500E R L VFigure 2 Correlation between actual liver volume (ALV) and estimated liver volume (ELV) by each formula. When both were the same, a dot would be on the linear line. Formulae of Urata, Heinemann, Vauthey, and Lee overestimated LV with respect to ALV. The Fan formula underestimated LV and the Chengdu formula gave a good estimate of ALV.4064 ISSN 1007-9327 CN 14-1219/R World J Gastroenterol August 28, 2009 Volume 15 Number 32700 900 1100 1300 1500ALV150013001100900700U r a t a700 1000 13001600ALV160013001000700H e i n e m a n n700 900 1100 1300 1500ALV150013001100900700L e e700 1000 1300 1600ALV160013001000700V a u t h e y700 900 1100 1300 1500ALV150013001100900700F a n700 800 900 1000 1100 1200 1300ALV14001300120011001000900800700C h e n g d uthe Chengdu formula was demonstrated to be reliable by its application in LDLT. We were limited to use of single center data in the present study, but we hope to improve the formula by using national multicenter data in the future[31].With development of living donor liver transplantation (LDLT), especially improvement of right graft adult-to-adult LDLT, the danger of donating has been paid more and more attention. The exact liver volume is not only relevant for the recipient, but also for the donor to avoid dangerous life-threatening residual liver volumes.Research frontiersScholars of different countries established several standard liver volume (SLV) formulae from clinical data. The authors estimated the SLV using computed tomography or reported formulae. However, there was a gap between these estimates and the actual liver volumes for Chinese adults. Recently, they developed a new formula (named the Chengdu formula) to estimate SLV using data from 115 LDLTs.Innovations and breakthroughsWith the Chengdu formula, the SLVs were evaluated in 76 cases of LDLT performed from January 2008 to April 2009. Its accuracy was compared to that of other internationally reported formulae to assess which formula is the most accurate for Chinese adults.ApplicationsWith national multicenter data in the future, the Chengdu formula for SLV can be improved. It may then be applied to the evaluation of donors for LDLT. TerminologyStandard liver volume: normal liver volume without disease affecting the volume of liver.Peer reviewVery interesting manuscript dealing with a very hot topic: determination of optimal size matching between graft and recipient in LDLT by means of race-adapted calculation of liver volumes. The recently published liver volume formula for Chinese people (Chengdu formula) has been demonstrated to be more reliable than others and therefore it should be adopted especially in this particular form of LT.REFERENCES1 Khalaf H, Shoukri M, Al-Kadhi Y, Neimatallah M, Al-Sebayel M. Accurate method for preoperative estimation of the right graft volume in adult-to-adult living donor liver transplantation. Transplant Proc 2007; 39: 1491-14952 Avolio AW, Siciliano M, Barbarino R, Nure E, AnnicchiaricoBE, Gasbarrini A, Agnes S, Castagneto M. Donor risk index and organ patient index as predictors of graft survival after liver transplantation. Transplant Proc 2008; 40: 1899-19023 Gruttadauria S, Marsh JW, Vizzini GB, di Francesco F,Luca A, Volpes R, Marcos A, Gridelli B. Analysis of surgical and perioperative complications in seventy-five right hepatectomies for living donor liver transplantation. World J Gastroenterol 2008; 14: 3159-31644 Fan ST, Lo CM, Liu CL, Yong BH, Chan JK, Ng IO. Safety ofdonors in live donor liver transplantation using right lobe grafts. Arch Surg 2000; 135: 336-3405 Lee SG, Park KM, Hwang S, Lee YJ, Kim KH, Ahn CS, ChoiDL, Joo SH, Jeon JY, Chu CW, Moon DB, Min PC, Koh KS, Han SH, Park SH, Choi GT, Hwang KS, Lee EJ, Chung YH, Lee YS, Lee HJ, Kim MH, Lee SK, Suh DJ, Kim JJ, Sung KB.Adult-to-adult living donor liver transplantation at the Asan Medical Center, Korea. Asian J Surg 2002; 25: 277-2846 Li FG, Yan LN, Li B, Zeng Y, Wen TF, Xu MQ, Wang W.Estimation formula of standard liver volume for Chinese adults. Sichuan Daxue Xuebao 2009; 40: 302-3067 Urata K, Kawasaki S, Matsunami H, Hashikura Y, IkegamiT, Ishizone S, Momose Y, Komiyama A, Makuuchi M.Calculation of child and adult standard liver volume for liver transplantation. Hepatology 1995; 21: 1317-13218 Heinemann A, Wischhusen F, Puschel K, Rogiers X.Standard liver volume in the Caucasian population. Liver Transpl Surg 1999; 5: 366-3689 Vauthey JN, Abdalla EK, Doherty DA, Gertsch P,Fenstermacher MJ, Loyer EM, Lerut J, Materne R, Wang X, Encarnacion A, Herron D, Mathey C, Ferrari G, Charnsangavej C, Do KA, Denys A. Body surface area and body weight predict total liver volume in Western adults.Liver Transpl 2002; 8: 233-24010 Chan SC, Liu CL, Lo CM, Lam BK, Lee EW, Wong Y, FanST. Estimating liver weight of adults by body weight and gender. World J Gastroenterol 2006; 12: 2217-222211 Trotter JF, Wisniewski KA, Terrault NA, Everhart JE,Kinkhabwala M, Weinrieb RM, Fair JH, Fisher RA, Koffron AJ, Saab S, Merion RM. Outcomes of donor evaluation in adult-to-adult living donor liver transplantation. Hepatology 2007; 46: 1476-148412 Duran C, Aydinli B, Tokat Y, Yuzer Y, Kantarci M, AkgunM, Polat KY, Unal B, Killi R, Atamanalp SS. Stereological evaluation of liver volume in living donor liver trans-plantation using MDCT via the Cavalieri method. Liver Transpl 2007; 13: 693-69813 Morimoto T, Ichimiya M, Tanaka A, Ikai I, Yamamoto Y,Nakamura Y, Takada Y, Inomata Y, Honda K, Inamoto T, Tanaka K, Yamaoka Y. Guidelines for donor selection and an overview of the donor operation in living related liver transplantation. Transpl Int 1996; 9: 208-21314 Yamashiki N, Sugawara Y, Tamura S, Kaneko J, NojiriK, Omata M, Makuuchi M. Selection of liver-transplant candidates for adult-to-adult living donor liver transplantation as the only surgical option for end-stage liver disease. Liver Transpl 2006; 12: 1077-108315 Frericks BB, Kirchhoff TD, Shin HO, Stamm G, MerkesdalS, Abe T, Schenk A, Peitgen HO, Klempnauer J, Galanski M, Nashan B. Preoperative volume calculation of the hepatic venous draining areas with multi-detector row CT in adult living donor liver transplantation: Impact on surgical procedure. Eur Radiol 2006; 16: 2803-281016 Iida T, Yagi S, Taniguchi K, Hori T, Uemoto S, YamakadoK, Shiraishi T. Signifi cance of CT attenuation value in liver grafts following right lobe living-donor liver transplantation.Am J Transplant 2005; 5: 1076-108417 Kim BS, Kim TK, Kim JS, Lee MG, Kim JH, Kim KW, SungKB, Kim PN, Ha HK, Lee SG, Kang W. Hepatic venous congestion after living donor liver transplantation with right lobe graft: two-phase CT fi ndings. Radiology 2004; 232: 173-18018 Cho JY, Suh KS, Lee HW, Cho EH, Yang SH, Cho YB, Yi NJ,Kim MA, Jang JJ, Lee KU. Hypoattenuation in unenhanced CT reflects histological graft dysfunction and predicts 1-year mortality after living donor liver transplantation.Liver Transpl 2006; 12: 1403-141119 Choi JY, Lee JY, Lee JM, Kim SH, Lee MW, Han JK, ChoiBI. Routine intraoperative Doppler sonography in the evaluation of complications after living-related donor liver transplantation. J Clin Ultrasound 2007; 35: 483-49020 Kato H, Usui M, Azumi Y, Ohsawa I, Kishiwada M, SakuraiH, Tabata M, Isaji S. Successful laparoscopic splenectomy after living-donor liver transplantation for thrombocytopenia caused by antiviral therapy. World J Gastroenterol 2008; 14: 4245-424821 Ohdan H, Tashiro H, Ishiyama K, Ide K, Shishida M, IreiT, Ohira M, Tahara H, Itamoto T, Asahara T. Microsurgical hepatic artery reconstruction during living-donor liver transplantation by using head-mounted surgical binocular system. Transpl Int 2007; 20: 970-97322 Oya H, Sato Y, Yamamoto S, Takeishi T, Nakatsuka H,Kobayashi T, Hara Y, Hatakeyama K. Surgical proceduresShi ZR et al. Liver volume formulae for Chinese adults 4065for decompression of excessive shear stress in small-for-size living donor liver transplantation--new hepatic vein reconstruction. Transplant Proc 2005; 37: 1108-111123 Lee SS, Kim KW, Park SH, Shin YM, Kim PN, Lee SG, LeeMG. Value of CT and Doppler sonography in the evaluation of hepatic vein stenosis after dual-graft living donor liver transplantation. AJR Am J Roentgenol 2007; 189: 101-10824 Asakuma M, Fujimoto Y, Bourquain H, Uryuhara K, HayashiM, Tanigawa N, Peitgen HO, Tanaka K. Graft selection algorithm based on congestion volume for adult living donor liver transplantation. Am J Transplant 2007; 7: 1788-179625 del Pozo JL. Update and actual trends on bacterial infectionsfollowing liver transplantation. World J Gastroenterol 2008;14: 4977-498326 Miraglia R, Maruzzelli L, Caruso S, Milazzo M, Marrone G,Mamone G, Carollo V, Gruttadauria S, Luca A, Gridelli B.Interventional radiology procedures in adult patients who underwent liver transplantation. World J Gastroenterol 2009;15: 684-69327 Shoji M, Ohkohchi N, Fujimori K, Koyamada N, SekiguchiS, Kawagishi N, Tsukamoto S, Shirahata Y, Sato K, SatomiS. The safety of the donor operation in living-donor liver transplantation: an analysis of 45 donors. Transpl Int 2003;16: 461-46428 Kawagishi N, Ohkohchi N, Fujimori K, Doi H, SakuradaM, Kikuchi H, Oikawa K, Takayama J, Satomi S. Safety of the donor operation in living-related liver transplantation: analysis of 22 donors. Transplant Proc 1998; 30: 3279-328029 Yoshizumi T, Taketomi A, Kayashima H, Yonemura Y,Harada N, Ijichi H, Soejima Y, Nishizaki T, Maehara Y.Estimation of standard liver volume for Japanese adults.Transplant Proc 2008; 40: 1456-146030 Hirata M, Harihara Y, Kitamura T, Hisatomi S, KatoM, Dowaki S, Mizuta K, Sugawara Y, Kita Y, Kubota K, Takayama T, Kawarasaki H, Hashizume K, Makuuchi M.The infl uence of donor age to graft volume increase rate in living donor liver transplantation. Transplant Proc 2001; 33: 1416-141731 Schiano TD, Bodian C, Schwartz ME, Glajchen N, Min AD.Accuracy and signifi cance of computed tomographic scan assessment of hepatic volume in patients undergoing liver transplantation. Transplantation 2000; 69: 545-550S- Editor Tian L L- Editor Cant MR E- Editor Ma WH4066 ISSN 1007-9327 CN 14-1219/R World J Gastroenterol August 28, 2009 Volume 15 Number 32。