2010冠状动脉CTA专家共识
- 格式:pdf
- 大小:394.06 KB
- 文档页数:40

2010年冠状动脉CT血管造影专家共识解读刘斌;赵世华【期刊名称】《心血管病学进展》【年(卷),期】2011(32)1【摘要】专家共识旨在陈述冠状动脉CT血管造影(coronary computed tomographic angiography,CCTA)对于疑似或确诊冠状动脉疾病的临床应用现状.鉴于目前还没有足够的循证医学证据确立CCTA的临床实践指南,故该共识未提供CCTA应用的明确推荐意见.共识的内容旨在根据业已出版的同行评议文献并经专家委员会讨论,总结出CCTA目前在临床应用中的长处和短处.因此既不是一个全面的综述,也不是对CCTA技术进行指导,并且也没有专门陈述CCTA检查的适应证.因为有关心脏CT和磁共振成像的适应证标准以及冠状动脉钙化CT检测的临床意义此前业已发表.%Thia document presents an expert consensus overview of the current and emerging clinical uses of coronary CTA in patients with suspected or known coronary anery disease ( CAD ) . The intention of this document is to summarize the strengths and weaknesses of current clinical uses of coronary CTA as reflected in the published peer-reviewed literature and as interpreted by the writing committee. The document is not intended primarily as either a comprehensive literature review or as an instruction guide for those interested in performing or interpreting coronary computed tomoWaphy ( CT) angiograms. The document also does not offer specific staLements ratjng the appropriateness of various potential clinical uses of coronary CTA , as this has been dealt with in theACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 Appropnateness Critena for Cardiac Computed Tomography and Cardiac Magnetic Resonance Imaging. Finally, this document does not address the evaluation of coronary calcium using CT, except as it pertains to CTA studies in patients with suspected or known CAD, since this topic has also been covered in the ACCF/AHA 2007 Clinical Expert Consensus Document on Coronary Artery Calcium Scoring by Computed Tomography in Global Cardiovascular Risk Assessment and in Evaluation of Patients With Chest Pain.【总页数】4页(P39-42)【作者】刘斌;赵世华【作者单位】安徽医科大学附属第一医院放射科,安徽,合肥,230022;中国医学科学院,阜外心血管病医院放射科,北京,100037【正文语种】中文【中图分类】R816.2【相关文献】1.ACCF/SCAI/SVMB/SIR/ASIIN 2007年颈动脉支架置入术临床专家共识文件美国心脏病学会基金会特别工作组关于临床专家共识文件的报告(ACCF/SCAI/SVMB/SIR/ASIIN颈动脉支架置人术临床专家共识文件委员会)与美国介入与治疗神经放射学学会、心血管造影和介入治疗学会、血管医学和生物学学会、介入放射学学会联合发布 [J], Bates ER(著);Babb JD(著);Casey DE Jr(著);Cates CU(著);Duckwiler GR(著);Feldman TE(著);Gray WA (著);Ouriel K(著);Peterson ED(著);Rosenfield K(著);Rundback JH(著);Safian RD(著);Sloan MA(著);White CJ(著);刘慧慧(译);吴延华(译);靳勇(译);曹勇军(译);刘春风(译)2.改善认知,践行共识《成人2型糖尿病胰岛素临床应用中国专家共识》解读 [J], 母义明3.遵循专家共识规范β受体阻滞剂临床应用《β受体阻滞剂在心血管疾病中临床应用的专家共识》解读 [J], 黄峻4.立足现状,聚焦共识《中国2型糖尿病合并肥胖管理专家共识》解读 [J],5.专家共识——心血管疾病合并糖尿病口服降糖药物应用专家共识解读 [J],因版权原因,仅展示原文概要,查看原文内容请购买。
冠状动脉钙化病变诊治中国专家共识(全文)随着经皮冠状动脉介入治疗(PCI)的不断发展,介入治疗更多涉及到更为复杂的病变,而冠状动脉钙化病变经常贯穿于各种复杂病变,增加了冠状动脉介入治疗的难度,是心血管介入医师所面临的主要挑战之一,尤其是严重钙化病变,或伴有扭曲、成角、弥漫的严重钙化病变,手术即刻的并发症以及早期和晚期主要不良心血管事件的发生率明显升高。
正确地识别、评估钙化病变,选择恰当的介入治疗技术,对于提高手术成功率、减少手术相关并发症、改善患者近、远期预后都非常重要。
其中,冠状动脉斑块旋磨术是处理冠状动脉严重钙化病变的重要手段,正确使用可有效地消蚀冠状动脉钙化病变,为最终置入冠状动脉支架创造良好的手术条件。
在复习该领域相关资料和研究进展的前提下,来自国内的介入心脏病学专家共同起草了《冠状动脉钙化病变诊治中国专家共识》,以期对钙化病变的介入治疗提供指导。
一、冠状动脉钙化病变的流行病学及对冠状动脉介入治疗的影响流行病学资料显示,冠状动脉钙化随年龄增加而增加,在40~49岁人群中的发生率为50%,60~69岁人群中的发生率为80%。
冠状动脉狭窄程度越高,通常伴有钙化的概率也越大。
高龄、脂质代谢异常、糖尿病、甲状旁腺功能亢进、慢性肾病、肾透析及高钙血症的患者是冠状动脉钙化病变的高发人群,而且其病变的钙化程度较严重。
与钙化程度低的患者相比,钙化程度高的患者其所有的冠心病事件、非致死性心肌梗死及冠心病猝死事件的相对危险度更高。
冠状动脉钙化病变的存在,尤其是严重内膜钙化病变,明显增加了PCI 的难度和风险,其难度在于如下几点。
(1)钙化病变往往伴随血管成角、扭曲病变,以及对血管扩张的反应较差,所以增加了介入相关器械通过的难度,增加了PCI相关并发症,如介入器械不能到位、支架脱落、导丝断裂、支架纵向压缩等风险的发生。
(2)钙化病变属于高阻力病变,球囊扩张时难以充分扩张,甚至会发生球囊破裂等情况;通常需要较高的压力扩张钙化病变,发生血管夹层、穿孔、破裂、无复流等概率明显增加。

Writing Committee Members Daniel B.Mark,MD,MPH,FACC,FAHA,Chair*Daniel S.Berman,MD,FACC†‡Matthew J.Budoff,MD,FACC,FAHA§J.Jeffrey Carr,MD,FACC,FAHAʈThomas C.Gerber,MD,FACC,FAHA¶#Harvey S.Hecht,MD,FACC§Mark A.Hlatky,MD,FACC,FAHAJohn McB.Hodgson,MD,FSCAI,FACC**Michael uer,MD,FACC,FAHA*Julie ler,MD,FACC*Richard L.Morin,P H DʈDebabrata Mukherjee,MD,FACCMichael Poon,MD,FACC‡Geoffrey D.Rubin,MD,FAHA¶#Robert S.Schwartz,MD,FACC***American College of Cardiology Foundation Representative;†Amer-ican Society of Nuclear Cardiology Representative;‡Society of Cardio-vascular Computed Tomography Representative;§Society of Athero-sclerosis Imaging and Prevention Representative;ʈAmerican College ofRadiology Representative;¶American Heart Association Representa-tive;#North American Society for Cardiovascular Imaging Represen-tative;**Society for Cardiovascular Angiography and InterventionsRepresentativeACCFTask Force Members Robert A.Harrington,MD,FACC,FAHA,ChairEric R.Bates,MD,FACCCharles R.Bridges,MD,MPH,FACC,FAHAMark J.Eisenberg,MD,MPH,FACC,FAHAVictor A.Ferrari,MD,FACC,FAHAMark A.Hlatky,MD,FACC,FAHAAlice K.Jacobs,MD,FACC,FAHASanjay Kaul,MD,MBBS,FACCDavid J.Moliterno,MD,FACCDebabrata Mukherjee,MD,FACCRobert S.Rosenson,MD,FACC,FAHAJames H.Stein,MD,FACC,FAHA††Howard H.Weitz,MD,FACCDeborah J.Wesley,RN,BSN,CCA††Former Task Force member during this writing effortThis document was approved by the American College of Cardiology Foundation Board of Trustees in November2009,the American College of Radiology in January 2010,the American Heart Association Science Advisory and Coordinating Commit-tee in January2010,the North American Society for Cardiovascular Imaging in January2010,the Society of Atherosclerosis Imaging and Prevention in January2010, the Society for Cardiovascular Angiography and Interventions in January2010,and the Society of Cardiovascular Computed Tomography in January2010.The American College of Cardiology Foundation requests that this document be cited as follows:Mark DB,Berman DS,Budoff MJ,Carr JJ,Gerber TC,Hecht HS, Hlatky MA,Hodgson JM,Lauer MS,Miller JM,Morin RL,Mukherjee D,Poon M, Rubin GD,Schwartz RS.ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT2010 expert consensus document on coronary computed tomographic angiography:a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents.J Am Coll Cardiol2010;55:2663–99.This article has been copublished in the June8,2010,issue of Circulation and e-published in Catheterization and Cardiovascular Interventions.Copies:This document is available on the World Wide Web sites of the American College of Cardiology()and the American Heart Association(my. ).For copies of this document,please contact Elsevier Inc.Reprint Department,fax(212)633-3820.e-mail reprints@.Permissions:Modification,alteration,enhancement,and/or distribution of this document are not permitted without the express permission of the American College of Cardiology Foundation.Please contact Elsevier’s permission department at healthpermissions@.Preamble (2664)1.Introduction (2665)1.1.Writing Committee Organization (2665)1.2.Document Development Process (2665)1.2.1.Relationships With Industry and Other Entities (2665)1.2.2.Consensus Development (2665)1.2.3.External Peer Review (2665)1.2.4.Final Writing Committee and Task ForceSign-Off on the Document (2665)1.2.5.Document Approval (2666)1.3.Purpose of This Expert Consensus Document (2666)2.Executive Summary (2666)3.Perspective and Scope of This Document (2668)4.Coronary CT Angiography:Brief Overview ofthe Technology (2668)4.1.Patient Selection and Preparation (2668)4.2.Coronary CT Image Acquisition (2669)4.2.1.Temporal Resolution of a CT Scan (2669)4.2.2.Spatial Resolution of a CT Scan (2669)4.3.Image Reconstruction and Interpretation (2670)5.Diagnostic Imaging of Coronary Arteries:Important Concepts (2671)6.Assessment of Left Ventricular Function:Important Concepts (2672)7.General Issues in Clinical Test Evaluation (2673)7.1.Key Clinical Questions (2673)7.1.1.Assessing Diagnostic Accuracy (2673)7.1.2.Likelihood Ratios and Receiver-OperatorCharacteristic Curves (2673)7.1.3.Assessing Prognostic Value (2674)7.1.4.Assessing Therapeutic Value (2674)8.Current Coronary CT Angiography Applications..26748.1.Diagnostic Accuracy of Coronary CT Angiographyin Stable Patients With Suspected CAD (2674)8.1.1.Coronary Anatomic Subgroup Data (2676)parison of Coronary CT Angiography WithStress Perfusion Imaging (2677)parison of Coronary CT Angiography WithFractional Flow Reserve (2678)8.2.Prognostic Evaluation of CoronaryCT Angiography in Stable Patients WithSuspected Coronary Disease (2678)e of Coronary CT Angiography in theAssessment of Patients With AcuteChest Pain (2679)e of Coronary CT Angiography in PreoperativeEvaluation of Patients Before NoncoronaryCardiac Surgery (2680)e of Coronary CT Angiography in theFollow-Up of Cardiac Transplant Patients (2680)e of Coronary CT Angiography in PatientsWith Prior Coronary Bypass Surgery (2680)e of Coronary CT Angiography in PatientsWith Prior Coronary Stenting (2681)8.8.Other Patient Subgroup Data (2682)8.9.Assessment of Global and Regional LeftVentricular Function (2682)9.Emerging Applications (2683)9.1.Noncalcified Coronary Plaque Imaging andIts Potential Clinical Uses (2683)9.2.Assessing Atherosclerotic Burden (2683)9.3.Identification of Vulnerable Plaques (2684)9.4.Left Ventricular Enhancement Patterns (2684)10.Areas Without Consensus (2684)10.1.Incidental Extracardiac Findings (2684)e of Coronary CT Angiography inAsymptomatic High-Risk Individuals (2686)10.3.The“Triple Rule-Out”in the EmergencyDepartment (2686)11.Safety Considerations (2687)11.1.Patient Radiation Dose (2687)11.2.Intravenous Contrast (2689)12.Cost-Effectiveness Considerations (2690)13.Quality Considerations (2691)References (2692)Appendix1.Author Relationships With Industryand Other Entities (2697)Appendix2.Peer Reviewer Relationships WithIndustry and Other Entities (2698)PreambleThis document was developed by the American College of Cardiology Foundation(ACCF)Task Force on Clinical Expert Consensus Documents(ECDs)and cosponsored by the American College of Radiology(ACR),American Heart Association(AHA),American Society of Nuclear Cardiology(ASNC),North American Society for Cardio-vascular Imaging(NASCI),Society of Atherosclerosis Im-aging and Prevention(SAIP),Society for Cardiovascular Angiography and Interventions(SCAI),and Society of Cardiovascular Computed Tomography(SCCT)to provide2664Mark et al.JACC Vol.55,No.23,2010 Expert Consensus on CT Angiography June8,2010:2663–99a perspective on the current state of computed tomographic angiography(CTA).ECDs are intended to inform practi-tioners and other interested parties of the opinion of the ACCF and document cosponsors concerning evolving areas of clinical practice and/or technologies that are widely available or new to the practice community.Topics are chosen for coverage because the evidence base,the experi-ence with technology,and/or the clinical practice are not considered sufficiently well developed to be evaluated by the formal ACCF/AHA practice guidelines process.Often the topic is the subject of ongoing investigation.Thus,the reader should view the ECD as the best attempt of the ACCF and document cosponsors to inform and guide clinical practice in areas where rigorous evidence may not be available or the evidence to date is not widely accepted. When feasible,ECDs include indications or contraindica-tions.Some topics covered by ECDs will be addressed subsequently by the ACCF/AHA Practice Guidelines Committee.The task force makes every effort to avoid any actual or potential conflicts of interest that might arise as a result of an outside relationship or personal interest of a member of the writing panel.Specifically,all members of the writing panel are asked to provide disclosure statements of all such relationships that might be perceived as real or potential conflicts of interest to inform the writing effort.These statements are reviewed by the parent task force,reported orally to all members of the writing panel at thefirst meeting,and updated as changes occur.The relationships and industry information for writing committee members and peer reviewers are published in Appendix1and Ap-pendix2of the document,respectively.Robert A.Harrington,MD,FACC,FAHAChair,ACCF Task Force onClinical Expert Consensus Documents 1.Introduction1.1.Writing Committee OrganizationThe writing committee consisted of acknowledged experts in thefield of CTA,as well as a liaison from the ACCF Task Force on Clinical ECDs,the oversight group for this document.In addition to2ACCF members,the writing committee included2representatives from the ACR and AHA and1representative from ASNC,NASCI,SAIP, SCAI,and SCCT.Representation by an outside organiza-tion does not necessarily imply endorsement.1.2.Document Development Process1.2.1.Relationships With Industry and Other Entities At itsfirst meeting,each member of the writing committee reported all relationships with industry and other entities relevant to this document topic.This information was updated,if applicable,at the beginning of all subsequent meetings and full committee conference calls.As noted in the Preamble,relevant relationships with industry and other entities of writing committee members are published in Appendix1.1.2.2.Consensus DevelopmentDuring thefirst meeting,the writing committee discussed the topics to be covered in the document and assigned lead authors for each section.Authors conducted literature searches and drafted their sections of the document outline. Over a series of meetings and conference calls,the writing committee reviewed each section,discussed document con-tent,and ultimately arrived at consensus on a document that was sent for external peer review.Following peer review,the writing committee chair engaged authors to address re-viewer comments andfinalize the document for document approval by participating organizations.Of note,telecon-ferences were scheduled between the writing committee chair and members who were not present at the meetings to ensure consensus on the document.1.2.3.External Peer ReviewThis document was reviewed by15official representatives from the ACCF(2representatives),ACR(2representa-tives),AHA(2representatives),ASNC(1representative), NASCI(2representatives),SAIP(2representatives),SCAI (2representatives),and SCCT(2representatives),as well as 10content reviewers,resulting in518peer review com-ments.See list of peer reviewers,affiliations for the review process,and corresponding relationships with industry and other entities in Appendix2.Peer review comments were entered into a table and reviewed in detail by the writing committee chair.The chair engaged writing committee members to respond to the comments,and the document was revised to incorporate reviewer comments where deemed appropriate by the writing committee.In addition,a member of the ACCF Task Force on Clinical ECDs served as lead reviewer for this document. This person conducted an independent review of the doc-ument at the time of peer review.Once the writing committee documented its response to reviewer comments and updated the manuscript,the lead reviewer assessed whether all peer review issues were handled adequately or whether there were gaps that required additional review. The lead reviewer reported to the task force chair that all comments were handled appropriately and recommended that the document go forward to the task force forfinal review and sign-off.1.2.4.Final Writing Committee and Task ForceSign-Off on the DocumentThe writing committee formally signed off on thefinal document,as well as the relationships with industry that would be published with the document.The ACCF Task Force on Clinical ECDs also reviewed and formally ap-proved the document to be sent for organizational approval.2665JACC Vol.55,No.23,2010Mark et al. June8,2010:2663–99Expert Consensus on CT Angiography1.2.5.Document ApprovalThefinal version of the document,along with the peer review comments and responses to comments were circu-lated to the ACCF Board of Trustees for review and approval.The document was approved in November2009. The document was then sent to the governing boards of the ACR,AHA,ASNC,NASCI,SAIP,SCAI,and SCCT for endorsement consideration,along with the peer review comments/responses for their respective official peer review-ers.ACCF,ACR,AHA,NASCI,SAIP,SCAI,and SCCT formally endorsed this document.This document will be considered current until the ACCF Task Force on Clinical ECDs revises or withdraws it from publication.1.3.Purpose of This Expert Consensus Document This document presents an expert consensus overview of the current and emerging clinical uses of coronary CTA in patients with suspected or known coronary artery disease (CAD).Since the evidence base for this technology is not felt to be sufficiently mature to support a clinical practice guideline at present,this ECD offers an alternative vehicle in which the state of the art of coronary CTA can be described without the requirement to provide explicit rec-ommendations accompanied by formal ratings of the quality of available evidence.The intention of this document is to summarize the strengths and weaknesses of current clinical uses of coronary CTA as reflected in the published peer-reviewed literature and as interpreted by the writing committee.The document is not intended primarily as either a comprehensive litera-ture review or as an instruction guide for those interested in performing or interpreting coronary computed tomography (CT)angiograms.The document also does not offer specific statements rating the appropriateness of various potential clinical uses of coronary CTA,as this has been dealt with in the ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/ SIR2006Appropriateness Criteria for Cardiac Computed Tomography and Cardiac Magnetic Resonance Imaging (1).Finally,this document does not address the evaluation of coronary calcium using CT,except as it pertains to CTA studies in patients with suspected or known CAD,since this topic has also been covered in the ACCF/AHA2007 Clinical Expert Consensus Document on Coronary Artery Calcium Scoring by Computed Tomography in Global Cardiovascular Risk Assessment and in Evaluation of Pa-tients With Chest Pain(1a).2.Executive SummaryAdvances in CT imaging technology,including the intro-duction of multidetector row systems with electrocardio-graphic gating,have made imaging of the heart and the coronary arteries feasible.The potential to obtain informa-tion noninvasively comparable to that provided by invasive coronary angiography has been the major driving force behind the rapid growth and dissemination of cardiac CT imaging.In the future,the ability of CTA to provide information not currently available from invasive angiogra-phy may provide the basis for a major shift in how patients with atherosclerotic cardiovascular disease are classified and managed.Currently,cardiac CTA can provide information about coronary anatomy and left ventricular(LV)function that can be used in the evaluation of patients with suspected or known CAD.The technology for performing coronary CT angiograms is evolving at a rate that often outpaces research evaluating its incremental benefits.Multidetector CT technology prior to64-channel or“slice”systems should now be considered inadequate for cardiac imaging(except for studies limited to assessing coronary calcium).The incremental value of re-cently introduced CT hardware with128-,256-,and 320-channel systems over64-channel systems has not yet been determined.As with any diagnostic technology,cor-onary CTA has technical limitations with which users should be familiar,and proper patient selection and prepa-ration are important to maximize the diagnostic accuracy of the test.Most cardiac CTA examinations result in a large 4-dimensional(4D)dataset of the heart obtained over the entire cardiac cycle.Physicians who interpret these exami-nations must be able to analyze the image data interactively on a dedicated workstation and combine knowledge of the patient with expertise in coronary anatomy,coronary patho-physiology,and CT image analysis techniques and limita-tions.In addition,integration of coronary CTA data into clinical practice requires that the results be evaluated in terms of what was known diagnostically and prognostically before the test was performed and,thus,what incremental information the test provides.The ability of a test such as coronary CTA to provide incremental diagnostic informa-tion that alters management(as contrasted with increasing diagnostic certainty alone)is heavily dependent both on the pretest probability and on the alternative diagnostic strate-gies considered.The published literature on the diagnostic accuracy of 64-channel coronary CTA compared with invasive coronary angiography as of June2009consists of3multicenter cohort studies along with over45single-center studies,many of the latter involving fewer than100patients.This literature reflects careful selection of study subjects and test interpre-tation by expert readers,typically with exclusion of patients who would be expected to have lower quality studies,such as those with irregular heart rates(e.g.,atrialfibrillation), obesity,or inability to comply with instructions for breath holding.In addition,because the cohorts for these studies were assembled from patients referred for invasive coronary angiography,they do not necessarily reflect,in terms of obstructive CAD prevalence or clinical presentation,the population to which coronary CTA is most likely to be applied in clinical practice.Accepting these caveats,some consistent conclusions emerge from this literature that may be useful in clinical decision making.In these studies,2666Mark et al.JACC Vol.55,No.23,2010 Expert Consensus on CT Angiography June8,2010:2663–99overall sensitivity and specificity on a per-patient basis are both high,and the number of indeterminate studies due to inability to image important coronary segments in the select cohorts represented is less than5%.In most circumstances, a negative coronary CT angiogram rules out significant obstructive coronary disease with a very high degree of confidence,based on the post-test probabilities obtained in cohorts with a wide range of pretest probabilities.However, post-test probabilities following a positive coronary CT angiogram are more variable,due in part to the tendency to overestimate disease severity,particularly in smaller and more distal coronary segments or in segments with artifacts caused by calcification in the arterial walls.At present,data on the prognostic value of coronary CTA using64-channel or greater systems remain quite limited.Furthermore,no large-scale studies have yet made a direct comparison of long-term outcomes following conventional diagnostic im-aging strategies versus strategies involving coronary CTA. As with invasive coronary angiography,the results of coronary CTA are often not concordant with stress single-photon emission computed tomography(SPECT)myocar-dial perfusion imaging(MPI).The differences in the pa-rameters measured by MPI(“function”or“physiology”)and CTA(“anatomy”)must be considered when making patient management decisions with these studies.Of note,a normal MPI does not exclude the presence of coronary atheroscle-rosis although it does signify a very low risk of future major adverse events over the short to intermediate term.Con-versely,coronary CTA allows detection of some coronary atherosclerotic plaques that are not hemodynamically sig-nificant.The optimal management of such disease has not been established.Neither test can presently identify with any reasonable clinical probability nonobstructive coronary plaques that might rupture in the future and cause acute myocardial infarction(MI).Invasive coronary angiography has a similar limitation.Studies comparing coronary CTA with fractionalflow reserve(FFR)measured as part of invasive coronary angio-graphic studies complement the MPI comparisons de-scribed in the preceding text by showing that coronary CTA anatomic data do not provide very accurate insights into the probability that specific lesions will produce clinically sig-nificant ischemia.Similar observations have been made about the relationship of FFR data and the anatomic information provided by invasive coronary angiography.In the context of the emergency department evaluation of patients with acute chest discomfort,currently available data suggest that coronary CTA may be useful in the evaluation of patients presenting with an acute coronary syndrome (ACS)who do not have either acute electrocardiogram (ECG)changes or positive cardiac markers.However, existing data are limited,and large multicenter trials com-paring CTA with conventional evaluation strategies are needed to help define the role of this technology in this category of patients.Coronary CTA imaging of patients with prior coronary bypass surgery yields very accurate information about the state of the bypass grafts but less accurate information about the native arteries distal to the bypasses and the ungrafted arteries.Because chest pain after bypass surgery might be associated with disease progression in either a graft or a native coronary artery,the difficulty of accurately assessing the native vessels is an important limitation for the clinical use of coronary CTA in the post-bypass patient. Coronary stents pose some significant technical chal-lenges for coronary CTA,since the metal in the stents may create several types of artifacts in the images.Special algorithms are now routinely used that may reduce some of these artifacts during image reconstruction.The literature suggests that in patients who have large diameter stents, good image quality,and whose clinical presentation suggests low-to-intermediate probability for restenosis,64-channel coronary CTA can be used to rule out severe in-stent restenosis.There are no studies that directly compare a coronary CTA strategy with an invasive coronary angiog-raphy strategy in patients with coronary stents,and such data will be required to understand the efficiencies and tradeoffs of these2strategies in this population.The literature on the assessment of LV function using cardiac CTA in patients with suspected or known CAD is much smaller than that for diagnostic coronary imaging. One likely reason is that echocardiography already provides a readily available,noninvasive means of assessing ventric-ular function and wall motion and does so without exposing patients to ionizing radiation or iodinated contrast agents. Available comparisons with cardiovascular magnetic res-onance(CMR)suggest that CTA estimation of LV ejection fraction is accurate over a wide range of values.Accuracy may,however,be reduced at higher heart rates due to difficulties in capturing end-systolic and end-diastolic phases e of some newer strategies to reduce the radiation dose of coronary CTA studies,such as sequential scanning,will eliminate the ability to assess LV function with the same study.The writing committee considered several emerging ap-plications where empirical data were deemed insufficient to support development of a consensus.Imaging of noncalci-fied coronary plaques may in the future become a useful application for coronary CTA,but it has no role in current practice since there are insufficient data to assess its clinical utility.CTA assessment of total atherosclerotic burden and potential plaque vulnerability similarly will require substan-tial additional technical development and clinical investiga-tion to define their potential value in patient management. The writing committee identified3areas without con-sensus:the interpretation of incidental noncardiacfindings on the CT examination,the use of coronary CTA in asymptomatic subjects,and the“triple rule-out”examina-tion of patients with acute chest pain in the emergency department.2667JACC Vol.55,No.23,2010Mark et al. June8,2010:2663–99Expert Consensus on CT AngiographyUse of coronary CTA raises2important safety issues:1) the amount of radiation absorbed by the body tissues;and2) the exposure to iodinated contrast agents that have the potential to produce allergic reactions and acute renal injury. Median effective radiation dose(which is a calculated rather than empirically measured quantity)for coronary CTA with current technology was12mSv in a cross-sectional inter-national study of50sites(both academic and community) assessed in2007.Individual sites in this study varied from a median of5to30mSv.In a15-hospital imaging registry in Michigan in2007,prospective use of a set of best practice radiation dose reduction recommendations resulted in a reduction in the average scan effective radiation dose from 21mSv to10mSv with no reduction in image quality. Several preliminary economic studies using claims data and/or modeling have examined the use of coronary CTA in the diagnostic evaluation of suspected coronary disease and in the evaluation of acute chest pain in the emergency department.Within the limits imposed by the data avail-able,these studies suggest that a diagnostic strategy using coronary CTA may potentially reduce both the time spent in the diagnostic process and the overall costs of clinical evaluation in selected populations,particularly in lower-risk subjects who otherwise would have been subjected to more expensive and possibly less accurate testing strategies.How-ever,longer-term empirical studies will be required to establish the full economic impact of this technology in contemporary practice.3.Perspective and Scope of This Document This document focuses on the perspective of clinicians caring for patients with suspected or known CAD in evaluating the potential current uses for cardiac CTA. Therefore,the use of cardiac CTA for other primary clinical questions,such as the diagnosis of pulmonary embolism, pulmonary parenchymal disease,pericardial disease,cardiac masses,arrhythmogenic right ventricular dysplasia,thoracic aortic disease,and congenital heart disease will not be directly addressed.Such disorders,of course,are relevant to the subject matter of this report when they are identified by the cardiac CT angiogram as a possible cause of the patient’s symptoms.This report does consider cardiac CT angio-graphic estimation of LV ejection fraction and evaluation of regional wall-motion abnormalities because thesefindings may help refine the assessment of the severity and clinical relevance of CAD.Detection of coronary calcium by CT has been addressed in the ACCF/AHA2007Clinical Expert Consensus Document on Coronary Artery Calcium Scoring by CT in Global Cardiovascular Risk Assessment and in Evaluation of Patients With Chest Pain(1a),and therefore will not be considered here except where assess-ment of coronary calcification is relevant to the performance and interpretation of coronary rmation provided by coronary CTA that is relevant to the patient with suspected or known CAD is considered to the extent made possible by the available published evidence.The writing committee felt that abstracts and oral presentations were not sufficiently reliable sources to be used in the construction of this document.4.Coronary CT Angiography:Brief Overview of the Technology Noninvasive coronary imaging requires a system capable of acquiring motion-free,high spatial resolution images within less than20seconds,while patients are holding their breath. Current generation64-channel multidetector row com-puted tomography(MDCT)fulfills these requirements reasonably well(2).This section will briefly review selected technical and interpretive issues specifically relevant to the performance of MDCT coronary imaging.Readers of the literature should not be confused by the fact that several equivalent terms are used to refer to this technology, including multidetector CT,multidetector row CT,multi-slice CT,and multichannel CT.Appropriate patient selection and preparation are ma-jor preimaging determinants of image quality.Key as-pects of the imaging process include heart rate and rhythm control,the proper timing of the scan relative to the introduction of the intravenous contrast bolus into the circulation,and minimization of patient motion. Interactive image reconstruction techniques are critical to proper diagnostic interpretation but cannot remedy defi-ciencies in collection of raw radiographic data.The determinants of patient radiation dose and the trade-offs between radiation dose and image quality are discussed in Section11,Safety Considerations.4.1.Patient Selection and PreparationImage quality of coronary CTA is improved by achieving a slow,regular heart rate,excluding very obese patients, selecting patients able to cooperate with instructions to be motionless and to hold their breath during imaging,and by assessing the presence and distribution of coronary calcifi-cation.All of these are evident from an initial patient evaluation except coronary calcification,which is typically assessed during the precontrast scans taken at the start of imaging.At present,there is nofirm consensus on the extent of coronary calcification that precludes a technically adequate coronary CT angiogram.Innovations in the scan-ning process currently under investigation may reduce the importance of this issue in the future.Patient preparation steps include achieving intravenous access,typically in an antecubital vein suitable for contrast administration at aflow rate of4to6mL/s,and adminis-tering preprocedure beta blockade when needed to achieve the desired heart rate and rhythm.Administration of sublingual nitroglycerin can be used to enhance coronary vasodilatation at the time of imaging.Rehearsal of the2668Mark et al.JACC Vol.55,No.23,2010 Expert Consensus on CT Angiography June8,2010:2663–99。

欧洲分叉俱乐部第一个10年冠脉分叉病变介入治疗专家共识解读医心评论来源:《医心评论》杂志2019年第1期作者:哈尔滨医科大学附属第二医院候静波据统计资料显示,冠状动脉分叉病变约占整个PCI事件的15%~20%,在手术即刻成功率及远期心脏事件方面,仍然是最具挑战性的冠脉病变之一,主要关注问题之一是治疗复杂性相关的晚期支架血栓形成。
欧洲分叉病变俱乐部(EBC)成立于2004年,旨在促进业界学术交流。
针对分叉病变管理的思考,EBC每年召开一次小型会议,由医生、工程师、生物学家、物理学家、流行病学家和统计学家专门对分叉病变进行详细讨论。
每次会议最终达成一个共识,反映了除介入心脏病专家意见外的很多其他科学家对分叉病变的综合看法。
今年是EBC成立10周年,为此,专家组成员将其近十年期间的年度会议精华内容进行了总结制定成共识。
一、分叉病变的分类分叉病变的简单描述、狭窄量化和PCI技术选择并不简单,因此在最初的两次年度会议中,EBC大多致力于冠状动脉分叉病变分类讨论及治疗,最后共识提出了分叉病变的简化和通用的Medina分类标准(图1)。
EBC还提出对每个在分叉支架置入术中应用的各种技术具有精确的分类系统,便于描述的MADS分类(图2)。
Medina分类可能需要一些描述的改进,但由此增加的复杂性恐怕妨碍全球采用该系统,因此被省略。
更精确的病变描述可以综合考虑到两个分支之间的角度,侧支(SB)病变长度,观察/预期直径,以及TIMI血流,钙化情况,斑块分布,以及是否伴有溃疡。
此外,目前越来越能获得分叉病变的客观评价,如功能性评估、定量分析和腔内影像可能有助于进一步描述。
二、分叉病变治疗策略分叉处理技术应考虑分支的通畅性,这可能影响预后,或者侧支狭窄可能导致症状。
因此,EBC共识指出,侧支(SB)直径和长度都可作为评估缺血心肌范围的替代物;如果术者认为分支很重要,在主支置入支架前首先在分支置入导丝。
1. 单支架还是双支架策略?基于大量随机研究和注册研究比较单支架策略和双支架策略的证据,以及KISSS原则(保持简单、快速和安全),EBC推荐在大多数分叉病变中应用必要时分支支架技术(Provitional),即是首先主支支架,分支仅在严重再狭窄或血流受限时必要支架。
冠状动脉微血管疾病诊断和治疗中国专家共识(2023版)自从1967年Likoff等首先报道了一组冠状动脉造影正常的冠心病患者的临床表现以来,冠状动脉微血管疾病)的基础和临床研究已历经半个世纪。
2013年,欧洲心脏病学会稳定性冠状动脉疾病治疗指南首次将此病列入冠心病的临床类型,并提出了初步的诊断和治疗建议。
2017年,中华医学会心血管病学分会基础研究学组、介入心脏病学组、女性心脏健康学组以及动脉粥样硬化和冠心病学组编写了《冠状动脉微血管疾病诊断和治疗的中国专家共识》,这是国际上第一部关于CMVD的专家共识。
此后,有关CMVD的国际共识性文件迅速增多。
2018年,国际冠状动脉舒缩障碍研究组提出了1型冠状动脉微血管功能异常即原发性CMVD的国际诊断标准。
2019年,ESC发布了慢性冠脉综合征的诊断和治疗指南,将微血管性心绞痛归纳为慢性冠脉综合征的一个重要类型,并提出了相应的诊断和治疗策略。
2019年,美国心脏协会发布了冠状动脉非阻塞性心肌梗死诊断和治疗的科学声明,指出微血管性心绞痛、微血管痉挛和冠状动脉慢血流现象可能是MINOCA的重要病因。
2020年,欧洲经皮心血管介入协会和ESC联合发布了冠状动脉非阻塞性心肌缺血的共识性文件,提出CMVD和(或)心外膜下冠状动脉痉挛是INOCA 的主要病因。
CMVD的定义、临床分型和流行病学一、定义CMVD是指在动脉粥样硬化性和非动脉粥样硬化性致病因素的作用下,冠状前小动脉、小动脉和毛细血管的结构和功能异常所导致的急性和慢性心肌缺血的临床综合征。
二、临床分型CMVD的流行病学数据多来源于欧美国家人群,部分研究纳入了亚洲人群,目前未见CMVD发病率种族差异的报道。
CMVD发病率在不同的临床类型中差异较大,由于疾病定义和诊断标准的差异,不同研究中发病率从最低的10%至最高的80%不等。
由于随访终点和时程的差异,不同研究中CMVD患者的死亡率和心血管不良事件的发生率亦有较大差别。
ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 冠状动脉CT血管造影专家共识解读作者:吕滨中国医学科学院阜外心血管病医院最近,美国心脏病学院基金会(ACCF)、美国放射学院(ACR)、美国心脏协会(AHA)、北美心血管影像协会(NASCI)、动脉粥样硬化影像与预防协会(SAIP)、血管造影和介入学会(SCAI)和心血管CT协会(SCCT)联合公布了心脏冠状动脉CT 血管造影(CTA)专家共识。
公布该“共识”的目的是,当前冠状动脉CTA对筛查冠心病和已知冠心病患者的评估均得到广泛应用,但是尚没有足够的循证医学证据公布指南(Guideline)。
因此,“共识”可以被理解为是“指南”公布前的替代文件。
该“共识”在前言中指出,目前冠状动脉CTA虽然在排除冠心病(存在≥50%的管腔狭窄)方面具有很高的价值(阴性预测值>95%),但是在狭窄率的精确诊断上有一定限度(假阳性或高估病变的比率较大),特别是对于钙化病变。
CT提供的信息与传统经导管造影一样在判断斑块危险性和何时破裂时受限。
有部分研究结果显示CTA在急诊室的应用价值:对于不典型胸痛、心电图和心肌酶学检查指标不确定的患者有排查的价值。
对于诊断急性冠脉综合征(AcuteCoronary Syndrome,ACS)并确定肇事血管和肇事病灶有一定价值,甚至能够进行危险分层和指导治疗方案的制定。
但是,这样的研究过少,多中心、大规模的循证医学证据尚显不足。
对于冠状动脉支架术后患者的复查,CTA对于较粗大的支架能够评估一定程度的再狭窄,但是大部分金属支架内的再狭窄在CT上评估受限。
基于CTA支架随访结果建立起的指导治疗的策略,是否与基于冠状动脉造影结果的治疗策略相一致,目前尚缺乏这样的大规模的临床研究结果。
冠状动脉旁路移植术(Coronary Artery Bypass Grafting,CABG)后的随访,CTA能够显示搭桥血管的通畅情况及其狭窄,但是对于固有冠状动脉的狭窄和病变进展,以及经桥血管的逆行灌注(Run-off)评估受限。
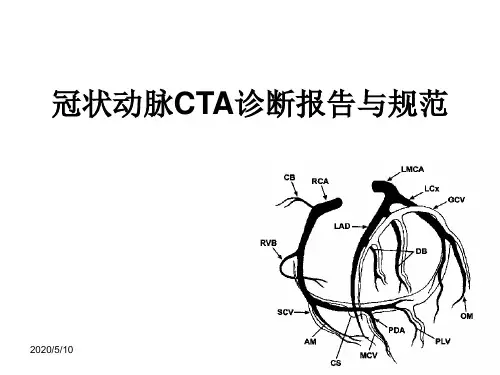
冠状动脉CT血管成像的适用标准及诊断报告书写规范摘要本文系统阐述了冠状动脉CT血管成像(CCTA )的临床适用标准,包括主要的检查适应证,以及相对禁忌证和限度,对主要适应证的推荐级别作了较为详尽的规定。
本文重点阐述了CCTA图像判读规程和诊断报告书写规范,依据扫描模式和程序,逐一阐明了CCTA读片的规程,以及诊断报告书写过程中应该加以描述的内容,对重点应该描述和诊断的核心内容进行了推荐,并给予了推荐等级,以示其重要性。
本部专家共识联合了数十位专家共同修订完成,并特意邀请了部分心血管内科和外科专家加入,以保证本共识能够更加切合临床实际工作情况,并更加适用于临床工作。
2004年64排CT问世以来,冠状动脉CT血管成像(coronary CT angiography , CCTA )获得快速临床应用与发展,不仅表现在成像能力的不断提高和新技术的不断涌现,更表现在CCTA临床应用的循证医学证据更加充足,临床认可度和昔及率更咼。
CCTA临床应用的第1个十年,是技术规范化推广与冠心病"解剖学”诊断的时代,临床需要CCTA这一无创技术的落地应用。
国际上连续发表专家共识或指南,国内专家也发表了心脏冠状动脉多排CT临床应用专家共识和心脏冠状动脉CT血管成像技术规范化应用中国指南,致力于该技术的普及与规范化应用。
冠心病"解剖学"诊断的范畴,包括CCTA能够快速进行冠心病的诊断与排查,识别冠状动脉斑块类型,显示严重钙化病变和慢性完全闭塞(chronic total occlusion , CTO ),指导经皮冠状动脉介入(percutaneous coronary intervention , PCI)治疗f并进行患者风险分层和预测心血管事件等。
CCTA进入第2个十年后,标志着以心肌CT 灌注(CT perfusion f CTP )和CT 血流储备分数(CT derived fractional flow reserve , CT-FFR )为代表的冠心病"功能学"诊断时代的到来。
2010冠状动脉CTA专家共识导言这份共识文件由美国心脏病学基金会(ACCF)临床专家共识文件(ECDs)专责小组联合美国放射学会(ACR)、美国心脏病协会(AHA)、美国核心脏病学会(ASNC)、北美心血管影像学会(NASCI)、动脉硬化影像及预防学会(SAIP)、心血管造影及介入治疗学会(SCAI)、心血管计算机断层学会(SCCT)共同编写,对计算机断层血管造影(CTA)的现状提出一些观点和看法。
专家共识旨在为从业者及相关人员提供ACCF及其共同编写者对于已经广泛应用或新出现的临床实践和(或)技术手段的开展领域的观点。
一些主题没有出现在共识中是由于相关循证学证据、技术经验、和(或)临床实践尚未考虑成熟,有待ACCF/AHA实践指南进行评估。
本文内容经常是正处于调查研究中的项目,所以读者应该把这份专家共识视为ACCF及其共同编写者在尚无严格循证证据或循证证据尚未被广泛接受的领域提供信息及指导临床实践的最大尝试。
ECDs会适当的包含适应征和禁忌征。
一些ECDs中未发布的内容将会由ACCF/AHA临床实践委员会随后颁布。
专家小组尽一切努力防止透露编写成员的外在联系或个人兴趣引起的实际存在或潜在的利益冲突。
特别指出,所有编写成员都被要求做出声明,保证表述出他们所能感知的实际或潜在的能够影响编写努力的利益冲突。
这些声明将由监审负责组在第一次会议时口头通知所有编写成员,并在修改时更新。
编写委员会及审稿人的关系和行业信息在附表1和附表2中分别显示。
Robert A. Harrington, MD, FACC, FAHA 主席,美国心脏病学基金会(ACCF)临床专家共识文件(ECDs)专责小组J Am Coll Cardiol. 2010;55(23):2663-2699.1.绪论1.1编写委员会组织编写委员会包括CTA领域的知名专家, ACCF临床专家共识文件(ECDs)专责小组中的联络成员,以及文件监督组。
除两名ACCF成员外,编写委员会包括2名ACR和AHA的代表,ASNC, NASCI, SAIP, SCAI, SCCT的代表各1名。
外部组织的陈述并不一定必须表示赞同。
1.2文件发展过程1.2.1与行业及其他实体的关系在第一次会议上,每一名编写委员会的成员都报告了所有与文件主题相关的行业及其他实体的关系。
如果可行的话,这份报告将在以后每次会议及委员会全体电话会议的开始都被更新。
如导言中所示,行业及其他实体的相关联系在附表1中可见。
1.2.2共识的发展过程第一次会议中,编写委员会讨论了共识文件所涵盖的主题并指定了每一章节的主编人选,编者指导文献检索并起草所在章节的轮廓。
经过一系列的会议及电话会议,编写委员会检查每一个章节,讨论文件内容,并最终达成可供外界同行评审的共识文件。
经过评审,编写委员会主席要求编者们为评论加注并完成最终能交予参与组织进行批准的文件。
值得注意的是,电话会议的召开是为了保证文件中的共识能在编写委员会主席与成员缺席的状况下达成。
1.2.3外界评审这份文件由来自ACCF (2名代表), ACR (2名代表), AHA (2名代表), ASNC (1名代表), NASCI (2名代表), SAIP (2名代表), SCAI (2名代表), 和SCCT (2名代表), 以及 10名内容审阅人共同评审, 使其包含了 518 个同行评审注释。
附表2中可见同行评审人员的名单,评审过程的从属关系,以及行业及其他实体的相应联系。
同行评审注释被录入一张表格并由编写委员会主席详细审阅。
主席要求编写委员会成员对注释做出回应,修订文件并在编写委员会认为合适的地方加入评审注释。
另外,一位来自ACCF临床专家共识文件(ECDs)专责小组的成员担任这份文件的主评审,此人在同行评审的同时指导对这份文件的一个独立评审,当编写委员会对评论注释做出回应并修改原稿时,这位主审人评估同行评审的观点是否把握十足或着存在需要附加评审的缺陷。
主审人向专责小组主席报告所有注释均有据可依并建议将文件交由专责小组进行最终评审及签收。
1.2.4最终编写委员会及专责小组在文件上签字收稿编写委员会正式签收文件以及将随同文件一起发表的行业关系,ACCF临床专家共识文件(ECDs)专责小组同时正式审阅并核准这份即将送交组织批准的文件。
1.2.5文件的正式批准文件的最终版本和同行注释以及对注释的回应将送交ACCF董事会进行审阅并正式批准。
文件于2009年11月被正式批准,随后文件连同对各自官方同行评审人的评审注释/回应一同被送交ACR, AHA, ASNC, NASCI, SAIP, SCAI, SCCT董事会进行签注,这份文件将会高度流通直到ACCF临床专家共识文件(ECDs)专责小组将其修订或从出版物上收回。
1.3 这份专家共识文件的目的这份文件提出了专家共识对于当代及新兴临床中对怀疑或已知冠心病患者应用CTA的总体看法,当前,这项技术的循证学证据尚未充分成熟到可以给出一份临床实践指南,专家共识文件(ECDs)提供了一种可供选择的手段,使我们在描述CTA的技术发展水平时无需要求提供由现有证据质量等级下正式明确的建议。
这份共识旨在通过同行已经发表的文献以及写作委员会的解释说明来总结当代医学中运用CTA的优势与弱点,而非广泛的回顾文献或为对CTA感兴趣的人提供用法说明指导。
文件亦不提供评价CTA各种潜在临床应用的特别说明,因为其在ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006心脏CT和心脏MRI应用标准[1]中已被达成。
最后,在文件中除了在怀疑或已知冠心病患者中做研究以外,未提及应用CT评估冠脉钙化,因为此主题已被涵盖在ACCF/AHA 2007全球心血管危险评估及胸痛病人评价中应用CT进行冠脉钙化评分文件中(1a)。
2.执行摘要CT影像技术的进步,包括心电图门控多排系统的引进,已经使心脏及冠脉成像成为可能。
与有创性的血管造影相比,通过无创的手段获取信息是推动心脏CT影像技术迅猛成长及分化的动力。
在未来,无需有创的血管造影,CTA可能为冠心病患者的分级和治疗提供依据。
现今,CTA所提供的冠脉解剖及左室功能情况可以用来评价怀疑或已确诊的冠心病患者。
冠脉CTA技术的进步往往快过对其优劣进行评价的速度。
在心脏成像中,多排CT应当被认为并不优于64排或“薄扫”系统(除了评价心脏钙化)。
近期引进128,256,320排系统CT与64排相比,其优势价值未被肯定。
如所有诊断技术一样,CTA的技术局限包括操作者的熟练程度,病人的选择以及检查前的准备,这些对于检查结果的精确性都很重要。
绝大多数心脏CTA都会产生一个跨越整个心动周期的心脏四维数据集。
检查报告医师必须能够在专属工作站上交互式分析影像数据并具备对病人冠脉解剖、冠脉病生理学、CT影像分析技术及专业知识。
另外,将CTA数据整合进临床实践还需要根据病人的诊断和预后,以及检查的附加信息来评价检查结果。
冠脉CTA能够提供改变治疗方案有效信息的能力有赖于预试的概率以及可替代诊断策略的考虑。
截止到2009年6月,已发表的比较64排CTA与有创冠脉造影的文献包括3个多中心队列研究以及超过45个单中心队列研究,而后者中很多研究的样本都少于100名病人。
文献反映了研究组别的精细选择以及专家读者的详细解释,特别要排除一些研究质量低的患者,如心律失常(房颤)、肥胖、或不能遵嘱屏气的患者。
另外,因为队列是由转入有创冠脉造影的病人集合而成,所以他们并不一定必须根据冠心病的发病率及临床表现代表最适合行CTA的人群。
接受了这些告诫,一些出自这篇文献的一致性结论可能会对临床决策有所帮助。
在这些研究中,每一名患者的灵敏度及特异度都很高,在选择队列中无法获得重要冠脉节段图像而导致的模糊研究数目低于5%。
基于在队列中获得的检查后概率及大范围检查前概率,大多数情况下,阴性冠脉CTA结果在排除明显冠脉闭塞性疾病方面有很高的信度。
然而,阳性CTA结果的检查后概率更具可变性,这一部分是因为对疾病严重程度的过度估计,特别是在较小的或较远的冠脉节段或由于动脉钙化引起的陈旧病变。
当前,研究应用64排或更高级系统进行冠脉CTA对于评估预后价值的数据仍就有限。
另外,没有大规模的研究来比较常规影像检查策略与冠脉CTA的远期效果。
正如有创的冠脉血管造影一样,冠脉CTA的结果经常与单光子发射式计算机断层(SPECT)、心肌灌注显像(MPI)不吻合。
在决定病人治疗方案时,由MPI(“功能”或“生理”)和CTA(“解剖”)评判产生参数的不同必须被考虑在内。
众所周知,即便冠脉硬化的表现仅预示在短期或中期存在很低的风险,一个常规MPI也不能将其排除。
相反,冠脉CTA能够发现一些不会显著影响血流动力学的冠脉硬化斑块。
治疗这些疾病的最佳方案并未建立。
现在这两种检查手段都不能指出未闭塞的冠脉斑块在未来脱落(破裂)并引起急性心梗的合理临床概率。
有创冠脉血管造影存在同样的局限性。
通过展示出冠脉CTA的解剖数据不能精确洞察到能够引起显著临床缺血的细节病变概率,研究将对比冠脉CTA与血流储备分数(FFR)评价作为有创冠脉造影研究的一部分,用来补充上文中的MPI对照组。
对于FFR数据与有创冠脉血管造影解剖数据关系的相似观察已经展开。
在急诊科评价胸部不适的病人时,现有资料显示冠脉CTA可能有利于评价无急性ECG改变或无心脏标志物阳性的急性冠脉综合征(ACS)患者。
但是现有数据是有限的,冠脉CTA在处理此类病人时所扮演的角色仍需对比冠脉CTA与常规手段的多中心试验来定义。
对于既往CABG的病人,冠脉CTA能够显示移植血管的精细图像,而对距离移植物较远的原位血管和未移植血管的精细显像稍差。
因为旁路移植术后病人的胸痛往往与移植血管和原位冠脉的病变进展相关,所以评估原位血管困难是冠脉CTA应用于既往旁路手术病人的主要局限。
由于支架中的金属物质能在图像中形成多种伪影,冠脉支架对冠脉CTA提出了一些重大的技术挑战。
现在,在图像再现时一些特殊运算法则被常规应用来减少伪影。
文献显示在植入大直径支架的病人(高质量图像),以及临床症状提示支架内再狭窄概率低或中等的病人中间,可以应用64排冠脉CT来排除严重的支架内再狭窄。
现在还没有研究直接对比冠脉CTA与有创血管造影在已植入支架病人中的应用,我们需要这些数据来了解这两种手段在此类人群中的功效和权衡。
应用心脏CTA评价怀疑或已知冠心病患者左室功能的文献远少于将其应用于冠脉成像的文献。
这可能是由于超声心动已经提供了一种无创且易接受的评估心室功能及室壁运动的手段,而且无需病人接触放射线或碘造影剂。
已有与心脏磁共振(CMR)的对照显示,CTA在评价左室射血分数上有很大优势。