Q4B 附件14 细菌内毒素测试
- 格式:pdf
- 大小:351.12 KB
- 文档页数:14
细菌内毒素检测方法细菌内毒素是一种细菌产生的有毒物质,它对人体和动物的健康造成了严重威胁。
因此,及时准确地检测细菌内毒素是非常重要的。
在本文中,我们将介绍几种常用的细菌内毒素检测方法,希望能够为相关领域的研究人员提供一些帮助。
首先,常用的细菌内毒素检测方法之一是生物学法。
这种方法利用动物(如小鼠、大鼠)或细胞培养物进行毒性试验,通过观察动物或细胞的生理、生化反应来判断细菌内毒素的毒性。
生物学法的优点是灵敏度高,能够检测到极微量的毒素,但缺点是操作复杂、耗时长、成本高,且容易受到其他因素的干扰。
其次,化学法也是一种常用的细菌内毒素检测方法。
这种方法利用化学试剂与细菌内毒素发生特异性反应,通过观察颜色、光度等变化来判断毒素的存在和含量。
化学法的优点是操作简便、结果可视化,但缺点是灵敏度相对较低,不能检测到极微量的毒素。
另外,免疫学法也是一种常用的细菌内毒素检测方法。
这种方法利用抗体与细菌内毒素发生特异性结合反应,通过免疫学方法(如免疫层析、免疫电泳)来检测毒素的存在和含量。
免疫学法的优点是灵敏度高、特异性强,但缺点是操作复杂、耗时长,且需要专门的实验设备和试剂。
最后,分子生物学法也是一种常用的细菌内毒素检测方法。
这种方法利用PCR、酶联免疫吸附试验(ELISA)等技术,通过检测细菌内毒素基因或蛋白来判断毒素的存在和含量。
分子生物学法的优点是灵敏度高、特异性强、操作简便,但缺点是需要专门的实验设备和试剂,且对操作人员的技术要求较高。
综上所述,针对细菌内毒素的检测,生物学法、化学法、免疫学法和分子生物学法都各有优缺点。
在实际应用中,可以根据实验的具体要求和条件选择合适的检测方法。
希望本文介绍的内容能够对相关领域的研究人员有所帮助,也希望在未来的研究中能够有更多更准确的细菌内毒素检测方法出现,为人类的健康保驾护航。
内毒素检测百科名片细菌内毒素是革兰氏阴性菌细胞壁上的一种脂多糖(LipopolySaccharide,LPS)和蛋白的复合物,当细菌死亡或自溶后便会释放出内毒素。
内毒素大量进入血液就会引起发热反应—“热原反应”。
内毒素与多种感染疾病密切相关,病情恶化往往伴随着内毒素含量的增加,病情缓解也常伴随着内毒素含量的减少。
因此,快速检测(1小时)血液、脏器内毒素含量可以为临床相关疾病的诊断预后提供参考。
厦门鲎试剂厂微板鲎试仪Elx808(配套IU)及配套软件(细菌内毒素分析仪)配合2005药典收录的光度法鲎试剂(动态浊度法鲎试剂、显色基质鲎试剂、动态显色法鲎试剂),可快速定量检测各种样品中的内毒素浓度,对于临床内毒素血症早期诊断、合理用药及药品检测具有重要价值。
内毒素测定方法有:凝胶法动态浊度法终点浊度法动态显色法终点显色法凝胶法系通过鲎试剂与内毒素产生凝集反应的原理来定性检测或半定量内毒素的方法。
凝胶法鲎试剂常见规格为0.1ml/支或0.5ml/支或者更大装量,使用时应加除热原水(细菌内毒素检查用水)复溶后使用。
凝胶法是通过观察有无凝胶形成作为反应的终点。
此法操作比较简单,经济,不需要专用测定设备,可以进行定性或半定量测定。
动态浊度法、终点浊度法、动态显色法、终点显色法,这四种方法都是定量检测内毒素的。
根据检测原理,终点浊度法和动态浊度法都属于浊度法。
浊度法系利用检测鲎试剂与内毒素反应过程中的浊度变化而测定内毒素含量的方法。
终点浊度法未见商品化产品。
动态浊度法(又称动态比浊法)是检测反应混合物的浊度上升某一预先设定的吸光度所需要的反应时间,或是检测浊度增加速度的方法。
终点显色法和动态显色法都是属于显色基质法。
显色基质法系利用鲎试剂与内毒素反应过程中产生的凝固酶使特定底物显色释放出的呈色团的多少而测定内毒素含量的方法,根据产物颜色判断内毒素浓度,又称为比色法。
厦门鲎试剂厂于2005年推出以鲎四肽为显色底物的鲎试剂盒,抗干扰能力强, 灵敏度高达0.005EU/ml, 质量达到国际领先水平。
细菌内毒素检测(凝胶法)标准操作目的:规范细菌内毒素的检测操作,保证细胞质量。
范围:适用于所有从治疗中心发放的细胞(包括CIK、DC、干细胞等)内毒素限量检测。
责任人:质量检测人员材料:一、电热干燥箱除外源性内毒素用,温度应能达到180℃。
二、恒温水浴箱或适宜的恒温器(37℃±1℃)。
三、水银温度计,精度在1℃以下,量程不小于50℃。
四、旋涡混合器。
五、可调式移液器六、0.25EU/ml鲎试剂。
七、细菌内毒素工作品。
八、凝胶法细菌内毒素检查用水。
九、实验用具无热原吸头(1000μl、200μl)、带铝盖的凝集管(10mm×75mm)、试管架、计时器、75%酒精棉球、封口膜、剪刀、镊子、砂轮。
所用玻璃器皿使用前须经250℃干烤至少1小时或180℃干烤至少4小时。
操作方法一、取样1、细胞发放前3天,取细胞培养液约2ml,分装于2个带铝盖的凝集管中各约1ml左右,如不立即试验4℃存放(可存放多长时间)。
2、细胞发放当天,取细胞生理盐水混悬液约2ml,分装于2个带铝盖的凝集管中各约1ml左右,如不立即试验4℃存放。
(可存放多长时间)。
3、取样应以无菌操作技术取样,所用器材在使用前应无热原或已去除热原。
二、鲎试剂灵敏度复核鲎试剂灵敏度复核的目的是考察鲎试剂的灵敏度是否正确、考察检验人员操作方法是否正确及实验条件是否符合规定。
在使用一批新的鲎试剂或试验条件发生了任何可能影响检验结果的改变时,应进行鲎试剂灵敏度复核实验。
(一)实验操作1、细菌内毒素工作品溶液的制备取细菌内毒素工作品一支,轻弹瓶壁,使粉末落入瓶底,然后用砂轮在瓶颈上部轻轻划痕,75%酒精棉球擦拭后启开,开启过程中应防止玻璃屑落入瓶内。
按照工作品说明书,加入规定量的细菌内毒素检查用水溶解其内容物,用封口膜将瓶口封严,置旋涡混合器上混合15分钟。
然后用倍倍稀释方式进行稀释,即0.5ml各浓度工作品溶液+0.5ml检查用水(以下稀释方式同此法),制备成4个浓度的细菌内毒素标准溶液,即2.0λ、0.5λ、0.25λ(λ为所复核的鲎试剂的标示灵敏度),每稀释一步均应在旋涡混合器上混合30秒钟。
细菌内毒素检测(凝胶法)标准操作目的:规范细菌内毒素的检测操作,保证细胞质量。
范围:适用于所有从治疗中心发放的细胞(包括CIK、DC、干细胞等)内毒素限量检测。
责任人:质量检测人员材料:一、电热干燥箱除外源性内毒素用,温度应能达到180℃。
二、恒温水浴箱或适宜的恒温器(37℃±1℃)。
三、水银温度计,精度在1℃以下,量程不小于50℃。
四、旋涡混合器。
五、可调式移液器六、0.25EU/ml鲎试剂。
七、细菌内毒素工作品。
八、凝胶法细菌内毒素检查用水。
九、实验用具无热原吸头(1000μl、200μl)、带铝盖的凝集管(10mm×75mm)、试管架、计时器、75%酒精棉球、封口膜、剪刀、镊子、砂轮。
所用玻璃器皿使用前须经250℃干烤至少1小时或180℃干烤至少4小时。
操作方法一、取样1、细胞发放前3天,取细胞培养液约2ml,分装于2个带铝盖的凝集管中各约1ml左右,如不立即试验4℃存放(可存放多长时间)。
2、细胞发放当天,取细胞生理盐水混悬液约2ml,分装于2个带铝盖的凝集管中各约1ml左右,如不立即试验4℃存放。
(可存放多长时间)。
3、取样应以无菌操作技术取样,所用器材在使用前应无热原或已去除热原。
二、鲎试剂灵敏度复核鲎试剂灵敏度复核的目的是考察鲎试剂的灵敏度是否正确、考察检验人员操作方法是否正确及实验条件是否符合规定。
在使用一批新的鲎试剂或试验条件发生了任何可能影响检验结果的改变时,应进行鲎试剂灵敏度复核实验。
(一)实验操作1、细菌内毒素工作品溶液的制备取细菌内毒素工作品一支,轻弹瓶壁,使粉末落入瓶底,然后用砂轮在瓶颈上部轻轻划痕,75%酒精棉球擦拭后启开,开启过程中应防止玻璃屑落入瓶内。
按照工作品说明书,加入规定量的细菌内毒素检查用水溶解其内容物,用封口膜将瓶口封严,置旋涡混合器上混合15分钟。
然后用倍倍稀释方式进行稀释,即0.5ml各浓度工作品溶液+0.5ml检查用水(以下稀释方式同此法),制备成4个浓度的细菌内毒素标准溶液,即2.0λ、0.5λ、0.25λ(λ为所复核的鲎试剂的标示灵敏度),每稀释一步均应在旋涡混合器上混合30秒钟。
细菌内毒素检测方法细菌内毒素是一种由细菌产生的毒素,它们可以对人体和动物造成严重的危害。
因此,检测细菌内毒素的方法显得尤为重要。
在本文中,我们将介绍几种常见的细菌内毒素检测方法,以帮助读者更好地了解和掌握这一领域的知识。
首先,常见的细菌内毒素检测方法之一是生物学检测法。
这种方法利用动物或细胞对内毒素的敏感性,通过观察它们的生理反应来判断样品中是否存在内毒素。
这种方法的优点是灵敏度高,能够检测到极小浓度的内毒素,但缺点是需要较长的检测时间,并且对实验动物的使用可能存在伦理和法律上的问题。
其次,化学检测法是另一种常用的细菌内毒素检测方法。
这种方法利用化学试剂与内毒素之间的特定反应来进行检测。
例如,内毒素在存在特定试剂时会发生颜色变化,通过观察颜色的变化来判断样品中是否存在内毒素。
化学检测法的优点是操作简单、快速,但缺点是对内毒素的种类和浓度有一定的限制。
另外,生物传感器技术也被广泛应用于细菌内毒素的检测。
生物传感器是一种能够将生物学识别元素与传感器技术相结合的新型检测技术,它能够实时、快速地检测样品中的内毒素,并且具有较高的灵敏度和特异性。
生物传感器技术的发展为细菌内毒素的检测提供了新的思路和方法。
此外,分子生物学方法也在细菌内毒素的检测中发挥着重要作用。
例如,聚合酶链式反应(PCR)技术可以通过扩增内毒素相关基因的方法来进行检测,而基因芯片技术则可以同时检测多种内毒素。
这些分子生物学方法具有高度的特异性和灵敏度,能够准确地检测样品中的内毒素,但需要较为复杂的实验操作和专业的设备。
综上所述,细菌内毒素的检测方法多种多样,每种方法都有其独特的优点和局限性。
在实际应用中,我们可以根据样品的特点和实验条件选择合适的检测方法,以确保检测结果的准确性和可靠性。
希望本文介绍的内容能够对读者有所帮助,使他们对细菌内毒素检测方法有更深入的了解。

细菌内毒素检测方法细菌内毒素是一种细菌产生的毒素,它们可以引起严重的疾病,甚至危及生命。
因此,及时准确地检测细菌内毒素对于预防和治疗疾病至关重要。
本文将介绍几种常见的细菌内毒素检测方法,希望能为相关领域的研究者和医护人员提供一些参考。
首先,常见的细菌内毒素检测方法之一是内毒素生物学检测法。
这种方法利用动物模型,将待检测的样品注射到动物体内,观察动物是否出现典型的内毒素中毒症状,如发热、休克等。
通过观察动物的生理指标和行为变化,可以初步判断样品中是否含有细菌内毒素。
这种方法的优点是直观、快速,但缺点是需要动物实验,不够环保,而且结果受动物个体差异影响较大。
其次,还有一种常用的细菌内毒素检测方法是内毒素化学检测法。
这种方法是利用化学试剂与细菌内毒素发生特定反应,产生可见的颜色变化或者荧光信号,从而检测样品中内毒素的含量。
内毒素化学检测法具有灵敏度高、操作简便的特点,可以快速、准确地检测出内毒素的存在,是目前常用的内毒素检测方法之一。
此外,分子生物学检测方法也被广泛应用于细菌内毒素的检测。
这种方法利用PCR、酶联免疫吸附测定法(ELISA)等技术,通过检测细菌内毒素的基因或蛋白质水平来确定样品中内毒素的含量。
分子生物学检测方法具有高度的特异性和准确性,可以对样品进行快速、精准的检测,是目前内毒素检测的主流方法之一。
综上所述,针对细菌内毒素的检测,我们可以选择合适的方法进行检测。
内毒素生物学检测法直观快速,但需要动物实验;内毒素化学检测法操作简便,准确性高;分子生物学检测方法具有高度的特异性和准确性。
在实际应用中,我们可以根据具体的需求和条件选择合适的检测方法,以确保检测结果的准确性和可靠性。
希望本文介绍的方法能够为相关领域的研究和临床工作提供一些帮助,促进细菌内毒素检测技术的进步和应用。
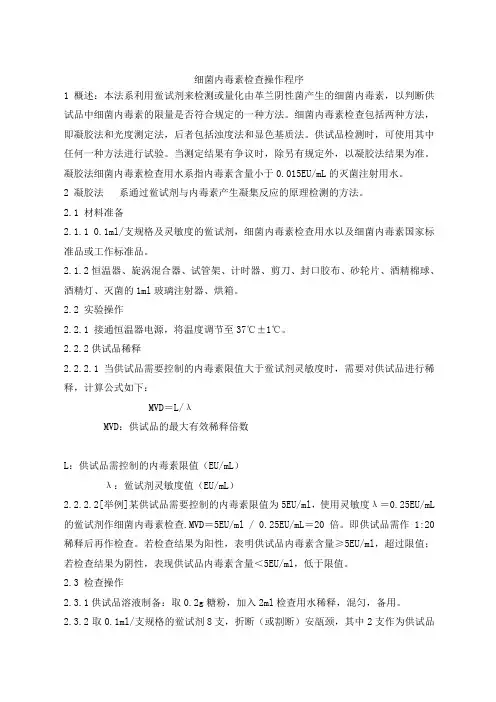
细菌内毒素检查操作程序1 概述:本法系利用鲎试剂来检测或量化由革兰阴性菌产生的细菌内毒素,以判断供试品中细菌内毒素的限量是否符合规定的一种方法。
细菌内毒素检查包括两种方法,即凝胶法和光度测定法,后者包括浊度法和显色基质法。
供试品检测时,可使用其中任何一种方法进行试验。
当测定结果有争议时,除另有规定外,以凝胶法结果为准。
凝胶法细菌内毒素检查用水系指内毒素含量小于0.015EU/mL的灭菌注射用水。
2 凝胶法系通过鲎试剂与内毒素产生凝集反应的原理检测的方法。
2.1 材料准备2.1.1 0.1ml/支规格及灵敏度的鲎试剂,细菌内毒素检查用水以及细菌内毒素国家标准品或工作标准品。
2.1.2 恒温器、旋涡混合器、试管架、计时器、剪刀、封口胶布、砂轮片、酒精棉球、酒精灯、灭菌的1ml玻璃注射器、烘箱。
2.2 实验操作2.2.1 接通恒温器电源,将温度调节至37℃±1℃。
2.2.2供试品稀释2.2.2.1 当供试品需要控制的内毒素限值大于鲎试剂灵敏度时,需要对供试品进行稀释,计算公式如下:MVD=L/λMVD:供试品的最大有效稀释倍数L:供试品需控制的内毒素限值(EU/mL)λ:鲎试剂灵敏度值(EU/mL)2.2.2.2[举例]某供试品需要控制的内毒素限值为5EU/ml,使用灵敏度λ=0.25EU/mL 的鲎试剂作细菌内毒素检查.MVD=5EU/ml / 0.25EU/mL=20倍。
即供试品需作1:20稀释后再作检查。
若检查结果为阳性,表明供试品内毒素含量≥5EU/ml,超过限值;若检查结果为阴性,表现供试品内毒素含量<5EU/ml,低于限值。
2.3 检查操作2.3.1供试品溶液制备:取0.2g糖粉,加入2ml检查用水稀释,混匀,备用。
2.3.2 取0.1ml/支规格的鲎试剂8支,折断(或割断)安瓿颈,其中2支作为供试品管,2支作为阴性对照管,2支作为阳性对照管。
2支供试品阳性管。
2.3.3 阴性对照管加入0.2ml水,其余各管加入0.1ml水复溶;供试品管各加入0.1ml 供试品溶液,阳性对照管加入0.1ml2.0λ浓度的内毒素溶液,供试品阳性对照管加入0.1ml供试品阳性对照溶液[用被测供试品溶液将同一支细菌内毒素工作标准品制成2.0λ浓度的同毒素溶液。

细菌内毒素检测标准细菌内毒素是一种由细菌产生的有毒物质,它可以对人体和动物的健康造成严重危害。
因此,对细菌内毒素的检测是非常重要的。
目前,国际上已经建立了一系列的细菌内毒素检测标准,以确保检测结果的准确性和可靠性。
首先,细菌内毒素检测标准包括了样品的采集和处理方法。
在采集样品时,需要注意避免污染和样品损坏,同时还要确保样品的代表性。
对于不同类型的样品,比如食品、药品、环境样品等,都有相应的采集和处理方法,以保证检测结果的准确性。
其次,细菌内毒素检测标准还包括了检测方法和技术的要求。
目前常用的检测方法包括生物学检测方法、化学检测方法和免疫学检测方法等。
这些方法各有优缺点,可以根据实际情况选择合适的方法进行检测。
同时,检测设备和仪器的精密度和准确性也是检测标准中非常重要的一部分。
另外,细菌内毒素检测标准还规定了检测结果的解读和评定标准。
对于检测结果的阳性和阴性判定,以及毒素含量的测定,都有相应的标准和规定。
这些标准旨在保证检测结果的准确性和可比性,从而为食品安全、医药卫生等领域提供可靠的数据支持。
最后,细菌内毒素检测标准还包括了实验室质量控制和质量保证体系的要求。
实验室需要建立完善的质量管理体系,包括设备校准、人员培训、实验操作规范等,以确保检测结果的准确性和可靠性。
总的来说,细菌内毒素检测标准是一套系统完整的标准体系,它涵盖了样品采集、检测方法、结果解读和质量保证等方方面面。
这些标准的建立和执行,对于保障食品安全、医药卫生等领域的公共健康具有重要意义。
希望各相关单位和人员能够严格执行这些标准,确保细菌内毒素检测工作的准确性和可靠性。
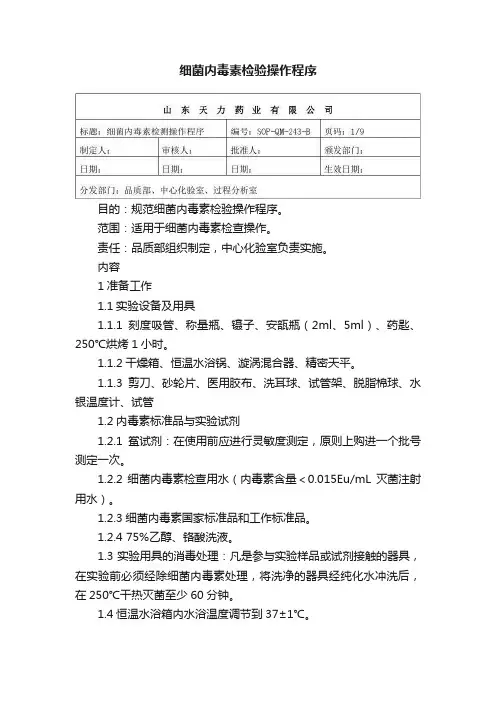
细菌内毒素检验操作程序目的:规范细菌内毒素检验操作程序。
范围:适用于细菌内毒素检查操作。
责任:品质部组织制定,中心化验室负责实施。
内容1准备工作1.1实验设备及用具1.1.1刻度吸管、称量瓶、镊子、安瓿瓶(2ml、5ml)、药匙、250℃烘烤1小时。
1.1.2干燥箱、恒温水浴锅、漩涡混合器、精密天平。
1.1.3剪刀、砂轮片、医用胶布、洗耳球、试管架、脱脂棉球、水银温度计、试管1.2内毒素标准品与实验试剂1.2.1鲎试剂:在使用前应进行灵敏度测定,原则上购进一个批号测定一次。
1.2.2细菌内毒素检查用水(内毒素含量<0.015Eu/mL灭菌注射用水)。
1.2.3细菌内毒素国家标准品和工作标准品。
1.2.4 75%乙醇、铬酸洗液。
1.3实验用具的消毒处理:凡是参与实验样品或试剂接触的器具,在实验前必须经除细菌内毒素处理,将洗净的器具经纯化水冲洗后,在250℃干热灭菌至少60分钟。
1.4恒温水浴箱内水浴温度调节到37±1℃。
2鲎试剂灵敏度复核2.1根据鲎试剂灵敏度的标示值(如:λ=0.25 EU/ml),细菌内毒素工作标准品加入1ml 细菌内毒素检查用水溶解,在漩涡混合器上混匀15分钟。
2.2将工作标准品制备成2λ、λ、0.5λ、0.25λ四个浓度(0.5 EU/ml、0.25 EU/ml、0.125 EU/ml、0.06 EU/ml)的内毒素标准溶液,备用。
例:工作标准品为160 EU/ml 时30秒。
2.3取18支0.25 EU/ml 鲎试剂,每支中加入0.1mlBET 水,然后分别加入0.1ml2.2中制备好的4个浓度的标准液,按浓度从高到低依次加入,每个浓度加4支,;最后2支加入0.1mlBET 水作阴性对照。
2.4将上述试管用医用胶布封口,垂直放入37℃±1℃水浴锅中,保温60±2分钟。
放入水浴前把水搅动几下,以使水温均匀。
再次检查温度是否在所要求的范围,注意保温和取放过程应避免受到振动造成的假阴性结果。
细菌内毒素检查细菌内毒素检查1、实验原理2、实验试剂3、试验器具4、检查⽅法概述5、供试品溶液的制备6、内毒素限值的确定7、最⼤有效稀释倍数(MVD)的确定8、鲎试剂灵敏度复核9、⼲扰试验10、供试品的细菌内毒素检查1、实验原理:利⽤鲎试剂与微量内毒素产⽣凝聚反应的现象,以判断供试品中细菌内毒素的限量是否符合规定的⼀种⽅法。
细菌内毒素的量⽤内毒素单位(EU)表⽰。
2、实验试剂:①鲎试剂:从海洋⽆脊椎动物“鲎”的蓝⾊⾎液中提取的变形细胞溶解物,经低温冷冻⼲燥精制的⽣物制剂。
鲎试剂的⽣物活性以其能检出细菌内毒素的最低有效浓度表⽰,即鲎试剂的灵敏度,单位为EU/ml。
当使⽤新批号的鲎试剂或试验条件发⽣可能影响检验结果的改变时,应进⾏鲎试剂灵敏度复核试验。
②细菌内毒素国家标准品:系⾃⼤肠埃希菌提取精制得到的内毒素,⽤于标定细菌内毒素⼯作标准品和标定,仲裁鲎试剂灵敏度。
③细菌内毒素⼯作标准品:系以细菌内毒素国家标准品为基准标定其效价,⽤于试验中鲎试剂灵敏度复核、⼲扰试验及各种阳性对照。
④细菌内毒素检查⽤⽔:指内毒素含量少于0.015EU/ml(⽤于凝胶法)或0.005 EU/ml (⽤于光度测定法),且对内毒素试验⽆⼲扰作⽤的灭菌注射⽤⽔。
3、实验器具:刻度吸管、凝聚管(10×75mm)、三⾓瓶、⼩试管(10×100mm)、试管架、洗⽿球、封⼝膜或⾦属试管帽、时钟、脱脂棉、吸⽔纸、剪⼑砂轮。
耐热器⽫常⽤⼲热灭菌法(250℃,30分钟以上)去除,塑料⽤具应选⽤⽆内毒素并且对试验⽆⼲扰的器械(⽬前多为⽆热源的⼀次性⽤品)。
4、检验⽅法概述①凝胶法:限量法、半限量法②光度测定法:浊度法(终点浊度法和动态浊度法)、显⾊基质法(终点浊度法和动态浊度法)凝胶法:最简单、经济、应⽤⼴泛、中国药典的“仲裁”⽅法,对⼲扰相对不敏感,较光度测定法不灵敏。
5、供试品溶液的制备某些供试品需进⾏复溶、稀释或在⽔性溶液中浸取制成供试品溶液。
细菌内毒素检测方法(译自英国药典版,等同欧洲药典版。
见原文之附录BP2004EP5XIV A方法)2.6.14.本文所描述的五种方法用于检测产品中是否存在细菌内毒素,而这些方法适用于药典中的细菌内毒素的检查法限度试验方法的制定者希望弄清楚,如在--.生产中能否降低其产品中的内毒素的含量,本篇幅中有关使用这些测试的相关方法将在补充的附录被提供。
细菌内毒素的检测原理是利用鲎变形细胞的溶解物来进行的(,,,试验)。
将含内毒素的溶液加入鲎变形细胞的溶解物可产生浑浊、沉淀或混合物的凝胶化反应。
反应速度依赖于溶液中的内毒素的浓度、和温度;反应要求有一定量pH 的二价阳离子、一个原凝酶系和可溶性蛋白的创造,而这些都哪由鲎变形细胞的溶解物提供。
采用从染色基因肽中释放的染料浓度来进行测定样品的内毒素浓度。
下面五种方法将在后面文章中介绍;方法:凝胶法;限度试验A方法:半定量凝胶法B方法:动力学浑浊法C方法:动力学发色肽方法D方法:发色肽终点法E当一篇专门文献中介绍内毒素的测定而没有指明某一种方法时,那么测试的方法就是按照方法。
次种方法已经得到证实,否则,产品的有效检测将会在A 专门文献中特别提到。
很多专著以“细菌内毒素限定浓度”的概念给出了细菌内毒素指标,也即某种产品所含细菌内毒素浓度不能超过限定浓度,要想证明产品符合要求,就必须表明产品所含内毒素的含量是少于内毒素限定浓度的。
试验是利用一种能避免微生物污染的方式进行的。
检测前的准备工作中,必须证实如下内容:1——所以的设备器皿不吸附内毒素。
——溶解物的灵敏度λ,λ是被定义为标记的溶解物敏感度或者最低内毒素浓度被用于制作标准曲线的(定量法)。
——干扰素的排除;如有必要时,需对设备和器具进行处理,以减少其本身所带内毒素。
除非特别指明外,否则在文献中从方法A到E中均采用相同标准。
在本篇附录中,术语说明中包括任何其他的容器,诸如一个微滴定率的极板等。
本试验包括如下试剂和标准溶液制备:标准细菌内毒素BRP;与国际标准相比较,对标准内毒素BRP进行效准,并以国际标准单位来表示。
Q4B Evaluation and Recommendation of Pharmacopoeial Texts for Use in the ICH Regions Annex 14: Bacterial Endotoxins TestGeneral ChapterThis draft guidance, when finalized, will represent the Food and Drug Administration's (FDA's) current thinking on this topic. It does not create or confer any rights for or on any person and does not operate to bind FDA or the public. You can use an alternative approach if the approach satisfies the requirements of the applicable statutes and regulations. If you want to discuss an alternative approach, contact the FDA staff responsible for implementing this guidance. If you cannot identify the appropriate FDA staff, call the appropriate number listed on the title page of this guidance.For questions regarding this draft document contact (CDER) Robert King 301-796-1242, or (CBER) Christopher Joneckis 301-827-0373.5 10 15 20 25 30 Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 201023 INTERNATIONAL CONFERENCE ON HARMONISATION OF TECHNICAL4 REQUIREMENTS FOR REGISTRATION OF PHARMACEUTICALS FOR HUMAN USE6789 E VALUATION AND R ECOMMENDATION OFP HARMACOPOEIAL T EXTS FOR U SE IN THE ICH R EGIONS11 ON12 B ACTERIAL E NDOTOXINS T EST G ENERAL C HAPTER13 Q4B A NNEX 1414161718 Current Step 2 Version 119 dated 10 June 20102122232426272829 At Step 2 of the ICH Process, a consensus draft text or guideline, agreed by the appropriate ICHExpert Working Group, is transmitted by the ICH Steering Committee to the regulatory31 authorities of the three ICH regions (the European Union, Japan and the USA) for internal and32 external consultation, according to national or regional procedures.Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 2010333435363738394041424344 Q4B Annex 1445 Document History4647 Current Step 2 version48Code History Date Q4B Annex 14 Approval by the Steering Committee under Step 2 and release10 June 2010for public consultation.495051Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 20105253 E VALUATION AND R ECOMMENDATION OF54 P HARMACOPOEIAL T EXTS FOR U SE IN THE ICH R EGIONS55 ON56 B ACTERIAL E NDOTOXINS T EST G ENERAL C HAPTER57 Q4B Annex 145859 Draft ICH Consensus Guideline60 Released for Consultation on 10 June 2010, at Step 2 of the ICH Process616263 TABLE OF CONTENTS646566 1. INTRODUCTION (1)6768 2. Q4B OUTCOME (1)6970 3. TIMING OF ANNEX IMPLEMENTATION (1)7172 4. CONSIDERATIONS FOR IMPLEMENTATION (1)7374 4.1 General Consideration (1)7576 4.2 FDA Consideration (2)7778 4.3 EU Consideration (2)7980 4.4 MHLW Consideration (2)8182 4.5 Health Canada Consideration (2)8384 5. REFERENCES USED FOR THE Q4B EVALUATION (2)85Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 20108687 E VALUATION AND R ECOMMENDATION OF88 P HARMACOPOEIAL T EXTS FOR U SE IN THE ICH R EGIONS89 ON90 B ACTERIAL ENDOTOXINS T EST G ENERAL C HAPTER9192 Q4B Annex 14939495 1. INTRODUCTION9697 This annex is the result of the Q4B process for the Bacterial Endotoxins Test General Chapter.9899 The proposed texts were submitted by the Pharmacopoeial Discussion Group (PDG).100101 2. Q4B OUTCOME102103104 2.1. Analytical Procedures105106 The ICH Steering Committee, based on the evaluation by the Q4B Expert Working 107 Group (EWG), recommends that the analytical procedures described in the official108 pharmacopoeial texts, Ph.Eur. 2.6.14. Bacterial Endotoxins, JP 4.01 Bacterial109 Endotoxins Test, and USP General Chapter <85> Bacterial Endotoxins Test, can be 110 used as interchangeable in the ICH regions subject to the following conditions:111112 2.1.1 Any of the three techniques can be used for the test. In the event of doubt or113 dispute, the gel-clot limit test should be used to make the final decision on114 compliance for the product being tested.115116 2.1.2 The Endotoxin Reference Standard should be calibrated to the current WHO117 (World Health Organization) International Standard for Endotoxin.118119 2.2 Acceptance Criteria120 The evaluated texts did not contain acceptance criteria. Endotoxin limits should be121 specified in the application dossier unless otherwise specified in an individual monograph. 122123 3. TIMING OF ANNEX IMPLEMENTATION124125 When this annex is implemented (incorporated into the regulatory process at ICH Step 5) in a 126 region, it can be used in that region. Timing might differ for each region.127128 4. CONSIDERATIONS FOR IMPLEMENTATION129130 4.1 General Consideration131132 When sponsors or manufacturers change their existing methods to the implemented133 Q4B-evaluated pharmacopoeial texts that are referenced in Section 2.1 of this annex, 134 any change notification, variation, and/or prior approval procedures should be handled 135 in accordance with established regional regulatory mechanisms pertaining to compendial 136 changes.137Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 2010138139 Bacterial Endotoxins Test General Chapter140141142 4.2 FDA Consideration143144 Based on the recommendation above, and with reference to the conditions set forth in 145 this annex, the pharmacopoeial texts referenced in Section 2.1 of this annex can be 146 considered interchangeable. However, FDA might request that a company147 demonstrate that the chosen method is acceptable and suitable for a specific material 148 or product, irrespective of the origin of the method.149150 4.3 European Union Consideration151152 For the European Union, regulatory authorities can accept the reference in a marketing 153 authorisation application, renewal or variation application citing the use of the154 corresponding text from another pharmacopoeia as referenced in Section 2.1, in155 accordance with the conditions set out in this annex, as fulfilling the requirements for 156 compliance with the Ph. Eur. Chapter 2.6.14. on the basis of the declaration of157 interchangeability made above.158159 4.4 MHLW Consideration160161 The pharmacopoeial texts referenced in Section 2.1 of this annex can be used as162 interchangeable in accordance with the conditions set out in this annex. Details of 163 implementation requirements will be provided in the notification by MHLW when this 164 annex is implemented.165166 4.5 Health Canada Consideration167168 In Canada any of the pharmacopoeial texts cited in Section 2.1 of this annex and used 169 in accordance with the conditions set out in this annex can be considered170 interchangeable.171172173 5. REFERENCES USED FOR THE Q4B EVALUATION174175 5.1 The PDG Stage 5B sign-off document (Rev. 1 – Correction 1): Japanese176 Pharmacopoeial Forum, Volume 18, number 4 (December 2009).177178 5.2 The pharmacopoeial references for the Bacterial Endotoxins Test General Chapter for 179 this annex are:180181 5.2.1 European Pharmacopoeia (Ph. Eur.):182 Supplement 6.6 (official January 1, 2010), Bacterial Endotoxins (reference183 01/2010:20614).184185 5.2.2 Japanese Pharmacopoeia (JP):186 General Test 4.01 Bacterial Endotoxins Test as it will appear in the JP Sixteenth 187 Edition (March 31, 2011). The draft English version of the JP text provided by 188 MHLW is appended (see Appendix A).189190 5.2.3 United States Pharmacopeia (USP):191 Text for <85> Bacterial Endotoxins Test, USP 33 Reissue (published April 2010 192 and official October 1, 2010).193Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 2010194195196 APPENDIX A197198 Draft JP XVI English Text Provided by MHLW199200 4. Biological Tests/Biochemical Tests/Microbial Tests201 4.01 Bacterial Endotoxins Test202203 This test is harmonized with the European Pharmacopoeia and the U. S. Pharmacopeia. 204205 Bacterial Endotoxins Test is a test to detect or quantify bacterial endotoxins of gram206 negative bacterial origin using an amoebocyte lysate prepared from blood corpuscle207 extracts of horseshoe crab (Limulus polyphemus or Tachypleus tridentatus). There are 208 two types of techniques for this test: the gel-clot techniques, which are based on gel209 formation by the reaction of the lysate TS with endotoxins, and the photometric210 techniques, which are based on endotoxin-induced optical changes of the lysate TS. The 211 latter include turbidimetric techniques, which are based on the change in lysate TS212 turbidity during gel formation, and chromogenic techniques, which are based on the213 development of color after cleavage of a synthetic peptide-chromogen complex.214 Proceed by any one of these techniques for the test. In the event of doubt or dispute, 215 the final decision is made based on the gel-clot techniques, unless otherwise indicated. 216 The test is carried out in a manner that avoids endotoxin contamination.217218 1. Apparatus219 Depyrogenate all glassware and other heat-stable materials in a hot-air oven using a 220 validated process. Commonly used minimum time and temperature settings are 30221 minutes at 250°C. If employing plastic apparatus, such as multi-well plates and tips for 222 micropipettes, use only that which has been shown to be free of detectable endotoxin and 223 which does not interfere with the test.224225 2. Preparation of Solutions226227 2.1 Standard Endotoxin Stock Solution228 Prepare Standard Endotoxin Stock Solution by dissolving Japanese Pharmacopoeia 229 Reference Standard Endotoxin in water for bacterial endotoxins test (BET). Endotoxin is 230 expressed in Endotoxin Units (EU). One EU is equal to one International Unit (IU) of 231 endotoxin.232233 2.2 Standard Endotoxin Solution234 After mixing Standard Endotoxin Stock Solution thoroughly, prepare appropriate serial 235 dilutions of Standard Endotoxin Solution, using water for BET. Use dilutions as soon as 236 possible to avoid loss of activity by adsorption.237238 2.3 Sample Solutions239 Unless otherwise specified, prepare sample solutions by dissolving or diluting drugs, 240 using water for BET. If necessary, adjust the pH of the solution to be examined so that 241 the pH of the mixture of the lysate TS and sample solution falls within the specified pH 242 range for the lysate to be used. This usually applies to a sample solution with a pH in theFinal STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 2010243 range of 6.0 to 8.0. TSs or solutions used for adjustment of pH may be prepared using 244 water for BET, and then stored in containers free of detectable endotoxin. The TSs or 245 solutions must be validated to be free of detectable endotoxin and interfering factors. 246247 3. Determination of Maximum Valid Dilution248 The Maximum Valid Dilution (MVD) is the maximum allowable dilution of a sample 249 solution at which the endotoxin limit can be determined.250 Determine the MVD from the following equation:251252 Endotoxin limit × Concentration of sample solution253 MVD = ―――――――――――――――――――――――254 λ255256 Endotoxin limit:257 The endotoxin limit for injections, defined on the basis of dose, equals K/M, where 258 K is a minimum pyrogenic dose of endotoxin per kg body mass (EU/kg), and M is 259 equal to the maximum bolus dose of product per kg body mass. When the product is 260 to be injected at frequent intervals or infused continuously, M is the maximum total 261 dose administered in a single hour period.262 Concentration of sample solution:263 mg/mL in the case of endotoxin limit specified by mass (EU/mg)264 mEq/mL in the case of endotoxin limit specified by equivalent (EU/mEq)265 Units/mL in the case of endotoxin limit specified by biological unit (EU/Unit)266 mL/mL in the case of endotoxin limit specified by volume (EU/mL)267 λ: the labeled lysate sensitivity in the gel-clot techniques (EU/mL) or the lowest point 268 used (EU/mL) in the standard regression curve of the turbidimetric or chromogenic 269 techniques270271 4. Gel-clot techniques272 The gel-clot techniques detect or quantify endotoxins based on clotting of the lysate TS 273 in the presence of endotoxin. To ensure both the precision and validity of the test,274 perform the tests for confirming the labeled lysate sensitivity (4.1.1) and for interfering 275 factors (4.1.2) as described under Preparatory testing (4.1).276 4.1 Preparatory testing277 4.1.1 Test for confirmation of labeled lysate sensitivity278 The labeled sensitivity of lysate is defined as the lowest concentration of endotoxin 279 that is needed to cause the lysate TS to clot under the conditions specified for the lysate 280 to be used.281 The test for confirmation of the labeled lysate sensitivity is to be carried out when each 282 new lot of lysate is used or when there is any change in the experimental conditions283 which may affect the outcome of the test.284 Prepare standard solutions having four concentrations equivalent to 2 λ, λ, 0.5 λ and 285 0.25 λ by diluting the Standard Endotoxin Stock Solution with water for BET. Mix a 286 volume of the lysate TS with an equal volume of one of the standard solutions (usually, 287 0.1 mL aliquots) in each test tube. When single test vials or ampoules containing288 lyophilized lysate are used, add solutions directly to the vial or ampoule.289 Keep the tubes (or containers such as vials or ampoules) containing the reaction290 mixture usually at 37 ± 1°C for 60 ± 2 minutes, avoiding vibration. To test the integrity 291 of the gel after incubation, invert each tube or container through approximately 180° inFinal STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 2010292 one smooth motion. If a firm gel has formed that remains in place upon inversion, record 293 the result as positive. A result is negative if either a firm gel is not formed, or if a fragile 294 gel has formed but flows out upon inversion.295 Making the standard solutions of four concentrations one set, test four replicates of the 296 set.297 The test is valid when 0.25 λ of the standard solution shows a negative result in each 298 set of tests. If the test is not valid, repeat the test after verifying the test conditions.299 The endpoint is the last positive test in the series of decreasing concentrations of300 endotoxin. Calculate the geometric mean endpoint concentration of the four replicate 301 series using the following formula:302303 Geometric Mean Endpoint Concentration = antilog (∑e/f )304 ∑e = the sum of the log endpoint concentrations of the dilution series used305 f= the number of replicates306 If the geometric mean endpoint concentration is not less than 0.5 λ and not more than 2 307 λ, the labeled sensitivity is confirmed, and is used in tests performed with this lysate. 308 4.1.2 Test for interfering factors309 This test is performed to check for the presence of enhancing or inhibiting factors for 310 the reaction in sample solutions.311 Prepare the solutions A, B, C and D according to Table 4.01-1, and test solutions A 312 and B and solutions C and D in quadruplicate and in duplicate, respectively. Concerning 313 the incubation temperature, incubation time, and procedure for the confirmation of gel 314 formation, follow the procedure described in 4.1.1.315 The geometric mean endpoint concentrations of B and C solutions are determined by 316 using the formula described in 4.1.1.317 This test must be repeated when there is any change in the experimental conditions which 318 may affect the outcome of the test.319320 Table 4.01-1Solution Endotoxin concentration/Solution to whichendotoxin is addedDiluentDilutionfactorEndotoxinconcentrationNumber ofreplicatesA*1 0/Sample solution — — — 4B*2 2λ/Sample solution Samplesolution12482λ1λ0.5λ0.25λ4C*3 2λ/Water for BET WaterforBET12482λ1λ0.5λ0.25λ2D*4 0/Water for BET — — — 2 321 *1 Negative control. Sample solution only.322 *2 Sample solutions added with standard endotoxin (for testing interfering factors). 323 *3 Standard endotoxin solutions for confirmation of the labeled lysate sensitivity. 324 *4 Negative control. Water for BET only.Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 2010325 The test is valid if solutions A and D show no reaction and the result for solution C 326 confirms the labeled lysate sensitivity.327 If the geometric mean endpoint concentration of solution B is not less than 0.5 λ and 328 not greater than 2 λ, the sample solution being examined does not contain interfering 329 factors and complies with the test for interfering factors. Otherwise the sample solution 330 interferes with the test.331 If the sample under test does not comply with the test at a dilution less than the MVD, 332 repeat the test using a greater dilution, not exceeding the MVD. The use of a more333 sensitive lysate permits a greater dilution of the sample to be examined. Furthermore, 334 interference of the sample solution or diluted sample solution may be eliminated by335 suitable treatment, such as filtration, neutralization, dialysis or heat treatment. To336 establish that the treatment chosen effectively eliminates interference without loss of 337 endotoxins, perform the assay described above using the preparation to be examined to 338 which Standard Endotoxin has been added and which has then been submitted to the 339 chosen treatment.340 4.2 Limit test341 This method tests whether or not a sample contains endotoxins greater than the342 endotoxin limit specified in the individual monograph based on the gel formation in the 343 presence of endotoxins at a concentration of more than the labeled lysate sensitivity. 344 4.2.1 Procedure345 Prepare solutions A, B, C and D according to Table 4.01-2. Making these four346 solutions one set, test two replicates of the set.347 In preparing solutions A and B, use the sample solutions complying with 4.1.2.348 Concerning the test conditions including the incubation temperature, incubation time, and 349 procedure for the confirmation of gel formation, follow the procedure described in 4.1.1. 350351 Table 4.01-2SolutionEndotoxin concentration/Solution to which endotoxin is addedNumber ofreplicatesA*1 0/Sample solution 2B*2 2λ/Sample solution 2C*3 2λ/Water for BET 2D*4 0/Water for BET 2 352 *1 Sample solution for the limit test. The solution may be diluted not to exceed the MVD. 353 *2 Positive control. Sample solution at the same dilution as solution A, containing354 standard endotoxin at a concentration of 2λ.355 *3 Positive control. Standard endotoxin solution containing standard endotoxin at a356 concentration of 2λ.357 *4 Negative control. Water for BET only.358 4.2.2 Interpretation359 The test is valid when both replicates of solutions B and C are positive and those of 360 solution D are negative.361 When a negative result is found for both replicates of solution A, the sample complies 362 with the Bacterial Endotoxins Test.363 When a positive result is found for both replicates of solution A, the sample does not 364 comply with the test.Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 2010365 When a positive result is found for one replicate of solution A and a negative result is 366 found for the other, repeat the test. In the repeat test, the sample complies with the test if 367 a negative result is found for both replicates of solution A. The sample does not comply 368 with the test if a positive result is found for one or both replicates of solution A.369 However, if the sample does not comply with the test at a dilution less than the MVD, 370 the test may be repeated using a greater dilution, not exceeding the MVD.371 4.3 Quantitative Test372 This method measures endotoxin concentrations of samples by determining an373 endpoint of gel formation.374 4.3.1 Procedure375 Prepare solutions A, B, C and D according to Table 4.01-3. Making these four376 solutions one set, test two replicates of the set. When preparing solutions A and B, use 377 sample solutions complying with 4.1.2. Concerning the test conditions, follow the378 procedure described in 4.1.1.379380 Table 4.01-3Solution Endotoxin concentration/Solution to whichendotoxin is addedDiluentDilutionFactorEndotoxinconcentrationNumber ofreplicatesA*1 0/Sample solution WaterforBET1248————2B*2 2λ/Sample solution — 1 2λ 2C*3 2λ/Water for BET WaterforBET12482λ1λ0.5λ0.25λ2D*4 0/Water for BET — — — 2 381 *1 Sample solutions for the Quantitative test. The dilution range of the dilution series may 382 be changed as appropriate, but not exceeding the MVD.383 *2 Positive control. Sample solution at the same dilution as the solution A diluted at the 384 lowest dilution factor, containing standard endotoxin at a concentration of 2λ.385 *3 Standard endotoxin solutions for confirmation of the labeled lysate sensitivity.386 *4 Negative control. Water for BET only.387388 4.3.2 Calculation and interpretation389 The test is valid when the following three conditions are met: (a) both replicates of the 390 negative control solution D are negative, (b) both replicates of the positive product391 control solution B are positive and (c) the geometric mean endpoint concentration of 392 solution C is in the range of 0.5 λ to 2 λ.393 The endpoint is defined as the maximum dilution showing the last positive test in the 394 dilution series of solution A, and the endotoxin concentration of the sample solution is 395 calculated by multiplying the endpoint dilution factor by λ.396 If none of the dilutions of solution A is positive, report the endotoxin concentration of 397 the sample solution as less than λ × the lowest dilution factor of the sample solution.Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 2010398 If all dilutions are positive, the endotoxin concentration of the sample solution is399 reported as equal to or greater than the greatest dilution factor of solution A multiplied by 400 λ.401 Calculate the endotoxin concentration (in EU per mL, in EU per mg or mEq or in EU 402 per Unit) of the sample, based on the endotoxin concentration of the sample solution. The 403 sample complies with the Bacterial Endotoxins Test if the endotoxin concentration of the 404 sample in both replicates meets the requirement for the endotoxin limit (in EU per mL, in 405 EU per mg or mEq or in EU per Unit) specified in the individual monograph.406407 5. Photometric quantitative techniques408 5.1 Turbidimetric technique409 This technique measures the endotoxin concentrations of samples based on the410 measurement of turbidity change accompanying gel formation of the lysate TS. This411 technique is classified as either endpoint-turbidimetric or kinetic-turbidimetric.412 The endpoint-turbidimetric technique is based on the quantitative relationship between 413 the concentration of endotoxins and the turbidity of the reaction mixture at a specified 414 reaction time.415 The kinetic-turbidimetric technique is based on the quantitative relationship between 416 the concentration of endotoxins and either the time needed to reach a predetermined417 turbidity of the reaction mixture or the rate of turbidity development.418 The test is usually carried out at 37 ± 1°C, and turbidity is expressed in terms of either 419 absorbance or transmission.420 5.2 Chromogenic technique421 This technique measures the endotoxin concentrations of sample solutions based on the 422 measurement of chromophore released from a synthetic chromogenic substrate by the 423 reaction of endotoxins with the lysate TS. This technique is classified as either endpoint424 chromogenic or kinetic-chromogenic.425 The endpoint-chromogenic technique is based on the quantitative relationship between 426 the concentration of endotoxins and the release of chromophore at the end of an427 incubation period.428 The kinetic-chromogenic technique is based on the quantitative relationship between 429 the concentration of endotoxins and either the time needed to reach a predetermined430 absorbance (or transmittance) of the reaction mixture or the rate of color development. 431 The test is usually carried out at 37 ± 1°C.432 5.3 Preparatory testing433 To assure the precision and validity of the turbidimetric or chromogenic techniques, 434 perform both Test for assurance of criteria for the standard curve (5.3.1) and Test for 435 interfering factors (5.3.2), as indicated below.436 5.3.1 Test for assurance of criteria for the standard curve437 The test is to be carried out when each new lot of lysate is used or when there is any 438 change in the experimental conditions which may affect the outcome of the test.439 Using the Standard Endotoxin Solution, prepare at least three endotoxin concentrations 440 to generate the standard curve within the range of endotoxin concentrations indicated by 441 the instructions for the lysate used. Perform the test using at least three replicates of each 442 standard endotoxin concentration according to the optimal conditions for the lysate used 443 (with regard to volume ratios, incubation time, temperature, pH, etc.). If the desired range 444 is greater than two logs, additional standards should be included to bracket each log445 increase in the range of the standard curve.Final STEP 2 - Annex 14 Bacterial Endotoxins Test for Tallinn June 9, 2010446 If the absolute value of the correlation coefficient, | r |, is greater than or equal to 0.980 447 for the range of endotoxin concentrations set up, the criteria for the standard curve are 448 valid and the curve complies with the test.449 If the standard curve does not comply with the test, repeat the test after verifying the 450 test conditions.451 5.3.2 Test for interfering factors452 Prepare solutions A, B, C and D according to Table 4.01-4. Perform the test on these 453 solutions following the optimal conditions for the lysate used (with regard to volume of 454 sample solution and lysate TS, volume ratio of sample solution to lysate TS, incubation 455 time, etc.).456 The test for interfering factors must be repeated when any condition changes, which is 457 likely to influence the result of the test.458459460 Table 4.01-4SolutionEndotoxin concentration Solution to whichendotoxin is addedNumber of testtubes or wellsA*1 0 Sample solution Not less than 2B*2 Middle concentration of thestandard curveSample solution Not less than 2 C*3 At least 3 concentrations Water for BET Each not less than 2D*4 0 Water for BET Not less than 2 461 *1 Sample solution only (for assaying endotoxin concentration in the sample solution). 462 The sample solution may be diluted not to exceed the MVD.463 *2 Sample solution at the same dilution as solution A, containing added standard464 endotoxin at a concentration equal to or near the middle of the standard curve.465 *3 Standard endotoxin solutions at the concentrations used in 5.3.1 (for the standard466 curve).467 *4 Negative control. Water for BET only.468 The test is valid when the following conditions are met.469 1: The absolute value of the correlation coefficient of the standard curve generated 470 using solution C is greater than or equal to 0.980.471 2: The result with solution D does not exceed the limit of the blank value required in 472 the description of the lysate employed, or it is less than the endotoxin detection limit 473 of the lysate employed.474 Calculate the recovery of the endotoxin added to solution B from the concentration 475 found in solution B after subtracting the endotoxin concentration found in solution A. 476 When the recovery of the endotoxin added to solution B is within 50% to 200%, the 477 sample solution under test is considered to be free of interfering factors and the solution 478 complies with the test.479 When the endotoxin recovery is out of the specified range, the sample solution under 480 test is considered to contain interfering factors. If the sample under test does not comply 481 with the test, repeat the test using a greater dilution, not exceeding the MVD.482 Furthermore, interference of the sample solution or diluted sample solution not to exceed 483 the MVD may be eliminated by suitable treatment, such as filtration, neutralization,484 dialysis or heat treatment. To establish that the treatment chosen effectively eliminates 485 interference without loss of endotoxins, perform the assay described above using the。