中枢神经系统可塑性机制的探讨
- 格式:pdf
- 大小:258.08 KB
- 文档页数:37
脑神经系统的可塑性及相关疾病的研究随着科学技术的不断进步和基础研究的深入探索,人们对于脑神经系统的可塑性及相关疾病的研究也越来越深入和全面。
脑神经系统是人类生命活动的中枢,掌控着我们的思维、情感、记忆等重要功能,因此,相关的疾病的研究也显得极为重要。
脑神经系统的可塑性是指大脑不断变化和适应不同环境的能力。
脑神经系统不像许多器官一样是静态的,它会不断适应不同的刺激和需求而改变自己的结构和功能。
这种可塑性包括神经元的形态、突触连接的数量和强度、神经元之间的信号传递等方面。
脑神经系统的可塑性是人类大脑能够适应不同环境和不断学习、思考等高级功能的基础。
例如,当我们学习新的语言、习惯体育运动、阅读等新事件时,大脑就会不断适应,并进行结构和功能上的调整。
这种适应性是我们日常生活中的应有之义。
然而,脑神经系统的可塑性也可能导致一系列的疾病。
例如脑卒中、阿尔茨海默病、帕金森病等,这些疾病会导致神经元的损伤和死亡,从而减少神经元之间的突触联系以及信号传递,进而进一步破坏大脑的结构和功能。
这些疾病都有某种程度的可预防性和可控性,因此相关研究显得极为重要。
阿尔茨海默病是一种脑部退化性疾病,它是老年人群体发病率最高的一种疾病。
目前学界普遍认为,阿尔茨海默病的发生和神经环路的缺陷有关。
神经环路是指神经元之间相互连接形成的网络,这个网络的结构和纤维的连通性对于大脑的正常功能至关重要。
研究表明,关于大脑神经环路的结构和功能的信息对于阿尔茨海默病的早期检测和治疗至关重要。
帕金森病也是一种常见的神经退行性疾病,它影响了人类许多基本的运动功能。
帕金森病与神经元化学物质的不平衡有关。
这种神经元化学物质的不平衡导致了神经元之间的联系破坏和信号传递受阻。
随着相关研究的深入,我们可以通过控制这种化学物质的不平衡,从而更好地治疗和预防帕金森病。
可以看出,脑神经系统的可塑性对于我们的生命活动有着非常重要的作用,同时也是神经退行性疾病进行深入研究的基础。
神经元的突触可塑性及其与认知功能的关系神经元是人体神经系统中起着非常重要作用的细胞,神经元的突触可塑性对于神经系统的正常功能起着至关重要的作用。
本文将围绕神经元的突触可塑性及其与认知功能的关系展开阐述。
一、神经元的突触可塑性突触可塑性是指神经元之间互相传递信号的连接点——突触的强度和效能会在不同的情况下发生变化,这种变化可以持续数秒钟到数小时,被称为突触可塑性。
突触可塑性广泛存在于中枢神经系统中,根据学习和记忆发生的时序和空间范围不同,突触可塑性可以分为同步和异步两种。
同步突触可塑性是指在时间上相邻的事件引起突触的可塑性转变,例如前一刺激后的刺激引起的突触可塑性改变,这种突触可塑性主要起到信息传递方面的作用,可以加强信号传递强度,提高信息的稳定性和可靠性。
而异步突触可塑性指的是在相隔一定时间内的事件引起的突触可塑性的转变,例如标记的神经活动和刺激密度相关的突触可塑性变化,这种变化主要起到空间方面的作用,可以使神经元的接收场进一步扩大,提高识别范围和灵敏度。
二、神经元的突触可塑性对认知功能的影响神经元的突触可塑性是认知功能实现的重要基础,神经元的突触可塑性可能影响大脑中不同认知过程:言语加工、空间认知、学习和记忆等。
语言是人类的一项最重要的认知功能,这也是人类大脑中功能体系中最为复杂的之一。
语言加工的过程涉及颞叶和额叶等多个脑区进行更高级别的意义处理和语法处理,而有机体的生命体验必然涉及到相邻的神经元之间的相互作用。
实验证实神经元的突触可塑性可以影响人类的语言处理。
在一个瞬间,大脑的成千上万神经元被活动,不同神经元之间的新的互连关系被建立,有机体的生命体验也就涉及到相邻神经元或特定突触之间的相互作用。
空间定向是认知过程中的另一个核心功能,主要涉及大脑中众多不同系统之间的相互作用。
研究显示突触可塑性可以影响空间定向的实现过程。
例如,负责空间定向的海马体可以发生同步或异步突触可塑性变化。
学习和记忆是人类大脑中最为复杂、最重要的认知功能之一。
兴奋剂对神经系统的影响与神经可塑性研究近年来,随着体育竞技水平的提高和竞争的加剧,使用兴奋剂成为一些运动员追求胜利的手段。
然而,兴奋剂的使用不仅仅对体能和肌肉产生影响,还会对神经系统产生一系列的影响。
本文将探讨兴奋剂对神经系统的影响以及神经可塑性研究的相关进展。
兴奋剂,也称为禁药,主要包括激素类药物、中枢神经刺激剂和血液增氧剂等。
这些药物在体内发挥着促进肌肉力量和增加耐力的作用,从而提高运动表现。
然而,兴奋剂的使用也存在一系列的负面影响,尤其是对神经系统的影响。
首先,兴奋剂的使用可能会对运动员的神经稳定性产生影响。
神经稳定性是指神经系统保持稳定的能力,长期使用兴奋剂可能导致神经系统的过度兴奋,进而影响神经的传导速度和稳定性。
一些研究表明,兴奋剂的滥用可能导致神经信号传导的不稳定,从而影响运动员的反应速度和协调性。
其次,兴奋剂还可能对神经递质的合成和释放产生影响。
神经递质是神经细胞间传递信号的化学物质,对于神经系统的正常功能至关重要。
一些研究发现,兴奋剂的使用可能导致神经递质的不平衡,进而影响神经信号的传递。
这可能导致运动员在进行高强度运动时出现无法控制的肌肉抽搐或者运动协调不良的情况。
此外,兴奋剂还可能对神经可塑性产生影响。
神经可塑性是神经系统适应环境变化和学习记忆的能力。
一些研究表明,兴奋剂的使用可能抑制神经可塑性的发展,从而影响运动员的学习和技能训练。
这种影响可能导致运动员无法充分利用训练所带来的效益,从而无法达到最佳竞技水平。
为了更好地理解兴奋剂对神经系统的影响,许多研究致力于神经可塑性的研究。
神经可塑性研究主要关注神经元之间的连接和突触可塑性,以及神经元的功能和结构的改变。
一些实验研究表明,使用兴奋剂可能导致神经突触的异常发展和突触可塑性的改变。
这种改变可能导致神经元之间的连接变得不稳定,进而影响神经信号的传递和信息处理。
总之,兴奋剂的使用对神经系统产生了一系列的影响。
兴奋剂可能影响神经的稳定性、神经递质的合成和释放,以及神经可塑性的发展。
中枢神经系统重塑过程分子机制解析中枢神经系统重塑是指在损伤或创伤后,神经系统通过一系列的分子机制来修复和重建受损部分的过程。
这一过程在人类和其他动物中都存在,并且对于恢复神经功能至关重要。
本文将深入分析中枢神经系统重塑的分子机制,并探讨其在神经科学研究和临床应用中的潜力。
首先,中枢神经系统重塑的过程需要借助于神经元的塑性。
神经元是神经系统的基本结构单位,其具有高度可塑性,能够在发育过程或受伤后重新连接和形成新的突触连接。
神经元的重塑过程主要包括突触增强和突触生成两个方面。
突触增强是指原有突触连接的加强和增多,促进了信息传递和学习记忆的形成。
这一过程主要通过调节突触前后神经元的活动来实现。
例如,当某个神经元受到损伤时,周围神经元会释放神经递质以促进其再生和修复。
此外,突触增强还可以通过神经递质的释放增加或改变突触后神经元的反应性,从而增加突触传递的效率。
突触生成是指在损伤或创伤后新形成的突触连接。
这一过程主要依赖于神经元的发育和再生机制。
在损伤较轻或创伤后,神经元能够通过轴突再生和突触重组来恢复突触连接。
此外,神经元还能够通过轴突的延长和突触的生长来建立新的连接,使受损的神经网络恢复功能。
中枢神经系统重塑的分子机制主要包括神经生长因子的调节、基因表达的变化和炎症反应的调控。
神经生长因子是一类可以促进神经元发育和再生的蛋白质,如神经营养因子(neurotrophins)和神经生长因子(growth factors)。
这些因子通过结合到神经元表面的受体,并激活下游信号传导途径,促进神经元的突触增强和突触生成。
基因表达的变化在中枢神经系统重塑过程中起着重要作用。
损伤或创伤后,许多基因的表达模式会发生变化,从而导致神经元的发育和再生。
一些基因可以调控神经元的轴突生长和突触形成,如轴突導向因子(axonal guidance factors)和突触凝聚因子(synapse consolidation factors)。
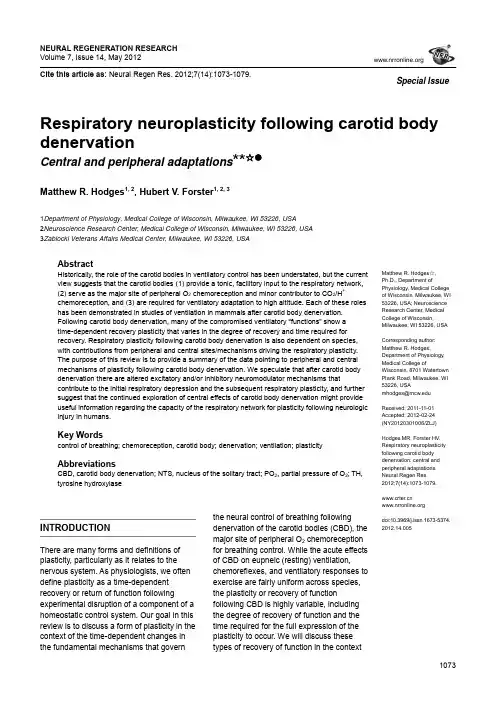
NEURAL REGENERATION RESEARCH Volume 7, Issue 14, May 2012Cite this article as: Neural Regen Res. 2012;7(14):1073-1079.1073Matthew R. Hodges ☆, Ph.D., Department ofPhysiology, Medical College of Wisconsin, Milwaukee, WI 53226, USA; Neuroscience Research Center, Medical College of Wisconsin,Milwaukee, WI 53226, USACorresponding author: Matthew R. Hodges,Department of Physiology, Medical College ofWisconsin, 8701 Watertown Plank Road, Milwaukee, WI 53226, USAmhodges@Received: 2011-11-01 Accepted: 2012-02-24 (NY20120301006/ZLJ)Hodges MR, Forster HV. Respiratory neuroplasticity following carotid body denervation: central and peripheral adaptations. Neural Regen Res. 2012;7(14):1073-1079.doi:10.3969/j.issn.1673-5374.2012.14.005Respiratory neuroplasticity following carotid body denervationCentral and peripheral adaptations **☆●Matthew R. Hodges 1, 2, Hubert V. Forster 1, 2, 31Department of Physiology, Medical College of Wisconsin, Milwaukee, WI 53226, USA2Neuroscience Research Center, Medical College of Wisconsin, Milwaukee, WI 53226, USA 3Zablocki Veterans Affairs Medical Center, Milwaukee, WI 53226, USAAbstractHistorically, the role of the carotid bodies in ventilatory control has been understated, but the current view suggests that the carotid bodies (1) provide a tonic, facilitory input to the respiratory network, (2) serve as the major site of peripheral O 2 chemoreception and minor contributor to CO 2/H +chemoreception, and (3) are required for ventilatory adaptation to high altitude. Each of these roles has been demonstrated in studies of ventilation in mammals after carotid body denervation. Following carotid body denervation , many of the compromised ventilatory “functions” show a time-dependent recovery plasticity that varies in the degree of recovery and time required for recovery. Respiratory plasticity following carotid body denervation is also dependent on species, with contributions from peripheral and central sites/mechanisms driving the respiratory plasticity. The purpose of this review is to provide a summary of the data pointing to peripheral and central mechanisms of plasticity following carotid body denervation. We speculate that after carotid body denervation there are altered excitatory and/or inhibitory neuromodulator mechanisms thatcontribute to the initial respiratory depression and the subsequent respiratory plasticity, and further suggest that the continued exploration of central effects of carotid body denervation might provide useful information regarding the capacity of the respiratory network for plasticity following neurologic injury in humans.Key Wordscontrol of breathing; chemoreception, carotid body; denervation; ventilation; plasticityAbbreviationsCBD, carotid body denervation; NTS, nucleus of the solitary tract; PO 2, partial pressure of O 2; TH, tyrosine hydroxylaseINTRODUCTIONThere are many forms and definitions of plasticity, particularly as it relates to the nervous system. As physiologists, we often define plasticity as a time-dependent recovery or return of function followingexperimental disruption of a component of a homeostatic control system. Our goal in this review is to discuss a form of plasticity in the context of the time-dependent changes in the fundamental mechanisms that governthe neural control of breathing followingdenervation of the carotid bodies (CBD), the major site of peripheral O 2 chemoreception for breathing control. While the acute effects of CBD on eupneic (resting) ventilation,chemoreflexes, and ventilatory responses to exercise are fairly uniform across species, the plasticity or recovery of functionfollowing CBD is highly variable, including the degree of recovery of function and the time required for the full expression of the plasticity to occur. We will discuss these types of recovery of function in the contextSpecial Issueof potential sites of respiratory plasticity following CBD, including upregulation of other peripheral sites of chemosensitivity and the potential for altered central mechanisms that govern blood gas homeostasis and chemoreflexes.THE NEURAL CONTROL OF BREATHING AND THE VARIOUS “DRIVES” TO BREATHERespiratory rhythm and pattern-generating neurons in the brainstem comprise a flexible oscillatory neural network that establishes the frequency of breathing and shapes coordinated activity of the respiratory pump and airway muscles. The output of this network is highly dependent upon tonic, excitatory “drives” that determine network excitability and ventilatory output. Based on the tight homeostatic control of resting arterial CO2 (eupneic P a CO2) and the effect of hypercapnia on ventilation, it was concluded by Haldane and Priestly that “CO2 is the factor that drives breathing”[1]. This suggested little or no role for the carotid bodies as a potential eupneic drive to breathe. As stated by Comroe and Schmidt in 1938, the “carotid body reflexes constitute an accessory mechanism, brought into action by emergencies such as foreign chemicals, anoxemia, and unusually large increases in CO2 te nsion in the blood”[2]. The findings of Fencl and others in awake goats that alveolar ventilation was linearly related to cerebrospinal fluid pH across several chronic acid base conditions certainly reinforced a minimal role for the carotid bodies[3].This view has changed substantially, as it has now become apparent that the carotid chemoreceptors provide an important tonic excitatory “drive” to breathe[4-5], a contribution perhaps best shown by studies of CBD[6-7]. We also now appreciate the contributions of multiple neuromodulatory inputs into the respiratory network as additional sources of tonic, excitatory inputs to breathe, including serotonin (5-HT), norepinephrine, substance P, acetylcholine and others (Figure 1), which may be altered with changes in the awake or sleep state. Moreover, many of these neuromodulators of breathing might also provide substrates for recovery of function following CBD, as seen in other forms of respiratory plasticity such as long term facilitation following intermittent hypoxia[9-10]. Overall, there are several important contributory “drives” to breathe, including peripheral and central chemoreceptor inputs and neuromodulators.PERIPHERAL CHEMORECEPTION: THE CAROTID BODIESThe goal of the respiratory control system is to provide the appropriate neuromuscular output for adequate alveolar gas exchange and maintenance of arterial blood gases. To achieve this objective, a network of brainstem nuclei generates respiratory rhythm and coordinated respiratory muscle activity patterns, with major chemical feedback from the peripheral O2 (carotid bodies) and central CO2/H+ chemoreceptors.The carotid body chemoreceptors are located bilaterally at the bifurcation of the common carotid arteries. Afferent innervation of the carotid bodies is supplied via the carotid sinus nerve (a branch of the cranial nerve IX), which project to the nucleus of the solitary tract (NTS) via the petrosal ganglia. The carotid bodies are thought as the major (if not sole) site for respiratory O2 chemoreception, due to the presence of clusters of neuron-like type I cells termed glomus cells, which are thought to serve as the primary “sensors”. Indeed, it was shown by Lahiri and Delaney that the carotid bodies can directly “sense” O2, and to a lesser extent CO2[11]. Recording single nerve fibers from the carotid sinus, they were able to demonstrate that the discharge rate of the carotid bodies varied significantly by alterations in the partial pressure of O2 (PO2) at a constant PCO2, and to a lesser extent by alterations in PCO2 at constant levels of PO2[11]. It has been shown that the glomus cells also contain several neurotransmitters and receptors[12], transducing sensory information via calcium-dependent neurotransmission[13]. The carotid body glomus cells also express a complement of membrane channels particularly suited for their role as chemoreceptors. Taken together, the hypothesis remains that the carotid bodies contribute greatly to O2 chemoreception and to a lesser extent to CO2 chemoreception in part or totally through its intrinsic chemosensitivity.In spite of their low intrinsic sensitivity to PaCO2, the carotid chemoreceptors are a major determinant of the hypercapnic ventilatory response through a positive interaction with central CO2/H+ chemoreceptors. This interaction was elegantly demonstrated in the studies of Figure 1 Multiple excitatory and inhibitory neuromodulators provide an additional respiratory “drive” through multiple g protein-coupled receptors. Adaptedfrom[8].1074Blain and colleagues in an awake dog preparation with isolated carotid body perfusion. In these studies, when the carotid body activity was increased by perfusion with hypoxic blood central CO2 sensitivity was increased, while attenuating carotid body activity with hyperoxic and hypocapnic blood depressed central CO2 sensitivity[14]. These and other experiments have led to the novel concept of peripheral and central chemoreceptors interdependence[4], the nature of which remains to be determined.In addition to their role as the acute “sensors” of hypoxia, the carotid chemoreceptors mediate anotherhypoxia-dependent physiologic phenomenon called high altitude ventilatory acclimatization. Eupneic ventilatory adaptation is multi-phasic for a native lowlander upon sojourn to high altitude, characterized by an initial stimulation of ventilation due to the hypoxemia, a ventilatory roll-off or depression due to a relative hyperventilation, and then an increase to an intermediate level of ventilation. It is the final phase of acclimatization that fails to occur in animals following CBD, implicating a key role for the carotid bodies in mediating the physiologic ventilatory adaptation to high altitude[15-16]. Finally, another important contribution of the carotid bodies is the breath to breath, or minute-to-minute stabilization of breathing. This is achieved by providing the ventilatory “error signal”, presumably through rapid transduction of chemoreceptor inputs through afferents. This mechanism is also thought to prevent deviations between the levels of ventilation and that required by metabolic rate[17].CAROTID BODY DENERVATION (CBD): ACUTE EFFECTSDenervation of the carotid bodies in most cases has dramatic effects on respiratory control. There are two distinct phases during which these physiologic disturbances occur: (1) an acute phase (days to weeks), and (2) a recovery phase (weeks to years). During the acute phase, CBD causes most adult mammals to hypoventilate (ventilation reduced relative to metabolic rate). Remarkably, the degree of hypoventilation (increased PaCO2) documented in the period immediately after CBD is fairly consistent across mammalian species, including ponies (12-15 mm Hg), goats (11 mm Hg), humans (~9 mm Hg) rats (8-9 mm Hg), and piglets (8-9 mm Hg)[6-7, 18-20]. In addition, the hypoxic ventilatory response is severely attenuated, as indicated by the attenuated ventilatory responses to venous infusions of NaCN, which mimics hypoxia at sites of O2 chemoreception[6, 19-20]. In addition, mammals do not acclimatize to high altitude following CBD. The hypercapnic ventilatory response, or CO2 sensitivity is also reduced following CBD[6-7, 17], which is a striking effect in light of the supposedly minor role for the carotid bodies in the hypercapnic ventilatory response as suggested by several studies[21-24]. The denervation- induced hypoventilation has been also shown to persist during moderate exercise challenges. In summary, several mammalian species hypoventilate at rest and during moderate exercise, display reduced ventilatory responses to hypoxia and hypercapnia, and fail to acclimatize to high altitude sojourn after CBD[25].IS THERE RESPIRATORY PLASTICITY FOLLOWING CBD?In most species studied to date, the acute attenuation of ventilation and chemosensitivity after CBD diminish over time. However, degree of plasticity or recovery of function and the time required for this plasticity are highly variable (reviewed in[25]). For example, adult cats[26] and goats[6] have been shown to exhibit substantial recovery from CBD within 2-3 weeks, while other species like dogs[23], ponies[7, 27], and humans[18] require months to years to demonstrate significant recovery in resting PaCO2. Moreover, there is variation in the degree of recovery observed in chemoreflexes and/or the ventilatory response to exercise. Some affected ventilatory control mechanisms recover more fully than others, perhaps suggesting more than onesite/mechanism of plasticity following CBD.Where does this form of respiratory plasticity originate, and by what mechanism(s)? The peripheral chemoreflex (as indicated by the ventilatory response to NaCN) and eupneic PaCO2 both recover to some degree in the months and years following CBD in ponies[25] (Figure 2).Figure 2 The relationship between ventilation (V I (L/min)) and PaCO2 (Torr) in an adult goat before carotid body denervation (pre-CBD) and on multiple days after CBD.Note the hypoventilation (rightward shift in PaCO2, and the reduction in ventilation for a given level of PaCO2 following CBD. Note also the recovery of CO2 sensitivity by day 15 post-CBD. Adapted from[6].PaCO2 (Torr)39 41 43 45 47 49 51 53 55 57 59Pre-CBDDay 1Day 2Day 4Day 7Day 151075However, there is far greater recovery toward pre-CBD levels in eupneic PaCO2, where the peripheral chemoreflex shows a significant, but minimal recovery. In these same ponies, further denervation of the aortic arch after this CBD-dependent plasticity has occurred eliminated the partially restored hypoxic ventilatory response, but had no effect on eupneic breathing[26]. This suggests that the recovery of the hypoxic ventilatory response following CBD depends upon aortic innervation, while the plasticity driving blood gases back toward “normal” may depend on a separate, potentially central mechanism. Similarly, CBD in neonatal piglets caused acute hypoventilation and attenuation of the hypoxic and NaCN responses, which showed varying degrees of recovery several days later[28]. Upon recovery, NaCN injections in the ascending aortic arch of CBD piglets elicited a hyperpnea, but the same injections in sham denervated piglets failed to increase ventilation, further suggesting that the aortic chemoreceptors become functional after CBD and may contribute to the recovery of ventilatory sensitivity to hypoxia. The area of the aorta with increased chemosensitivity was further shown to contain greater 5-HT content in CBD piglets compared to sham CBD piglets, and the aortic NaCN-dependent hyperpnea following CBD was shown to be attenuated by 5-HT receptor antagonists[29]. The sum of the data suggests that the plasticity following CBD may depend on: (1) multiple mechanisms at multiple sites, where the site of plasticity driving the normalization of eupneic ventilation may include the brainstem respiratory network, and (2) neuromodulators and their receptors, such as 5-HT.CENTRAL EFFECTS OF PERIPHERAL CHEMORECEPTOR DENERVATIONClearly, CBD acutely causes hypoventilation at rest (PaCO2 + 8-15 mm Hg), and blood and brain acidosis, and decreases CO2 sensitivity[6-7]. This period of significant hypoventilation, increased PaCO2, and decreased CSF pH should provide an increased stimulus to central CO2/pH chemoreceptors. Specifically, increasing PaCO2 by 8 mm Hg (by increasing inspired CO2) increases ventilation from 5 to 20 L/min in goats prior to CBD[6] (Figure 3). However, PaCO2 increases10 mmHg at rest due to decreased ventilation by day 4 after CBD, and further increases in PaCO2 by increasing inspired CO2 have far less of a stimulatory effect on ventilation. Why is breathing not stimulated under these conditions? One possibility is that the sensitivity of central chemoreceptors is reduced following CBD, as shown by a reduced ventilatory response to focal acidification of the medullary raphé nuclei in goats after bilateral CBD[30] (Figure 4). Based on the hypothesis that the carotid bodies tonically “drive” the respiratory network, one might hypothesize generalized decreases in neuronal excitability or activity.Figure 3 Chronic effects of carotid body denervation (CBD) on eupneic PaCO2 (Torr) and the NaCN response ratio (index of peripheral chemosensitivity to hypoxia) in ponies before and up to 52 months after CBD.Note the recovery in resting PaCO2 is greater that the minimal, but significant recovery peripheral chemoreflex. Adapted from[25].Figure 4 Ventilation, tidal volume (V T), breathing frequency (f) and O2 consumption (VO2), expressed as a percentage of control, before, during and after focal acidification in the medullary raphé in awake goats before and after bilateral carotid body denervation (CBD). “a”denotes significantly different from CBD ( P < 0.05)Note that the ventilatory response to raphé acidification is reduced following CBD. Adapted from[30].605550454035PaCO2(Torr)987654321NaCNresponseratio0 1 3 12 10 17 22 34 48 52Week MonthTime0 10 20 30 40 50 60Time (minute)a aaa a10761077Indeed, cytochrome oxidase, which is a general marker of neuronal activity, has been shown to be decreased at a key site in the respiratory network, the pre-Bötzinger complex, following CBD in neonatal rats [31]. This reduced neuronal activity could result from a reduction inexcitatory glutamatergic inputs, a concept consistent with the observations of Hoop et al [32]. who showed that the radiotracer CSF transfer rate of [13N] glutamine (a marker of glutamate bioavailability) was markedly reduced following CBD, but not during chronic hypoxia. Ifneuronal activity, and glutamatergic “drive” are reduced following CBD, a compensatory upregulation ofexcitatory receptors might occur. This may indeed be the case, as the ventilatory responses to raphé injections of the glutamate receptor-specific excitatory neurotoxin ibotenic acid was greatly enhanced following CBD (Figure 5;[30]).Alternatively, the reduction in respiratory network excitability may result from alterations in excitatory neuromodulatory inputs. Roux et al. determined that tyrosine hydroxylase (TH) staining in the A1(ventrolateral NTS) noradrenergic cell group wasreduced (about 35%) 15 days after CBD, and increased in the A2 (129%) and A1 (ventrolateral medulla: 51%) 90 days post-CBD [33]. This reduction in TH could translate to a decrease in excitatory neuromodulatory input to the respiratory network. However, in a follow-up study, these investigators showed that chronic hypoxia alone was sufficient to enhance TH expression in noradrenergic cell groups independent of CBD, suggesting that the recovery from CBD may not be related to altered THexpression [34].CBD eliminates excitatory afferent inputs from the carotid bodies to the NTS, which has numerous target nuclei, including the ventral respiratory group,retrotrapezoid nucleus [35-36] (RTN), and medullary raphé nuclei [37-39]. Thus, reduced NTS activity could result in reduced neuronal activity/excitability of RTN and/or 5-HT raphé neurons. Consistent with this hypothesis are the data demonstrating that generation of neuronal dysfunction of the ventrolateral medullary surface in an area that includes both serotonergic and glutamatergic RTN neurons by thermode cooling slows ventilation at rest during wakefulness in intact animals, but leads to sustained apnea after CBD [40]. Finally, as discussed previously focal acidification of the medullary raphé increases ventilation 30% in adult awake goats before CBD, but this response was significantly reduced after CBD (Figure 4). The sum of these data point to direct and indirect pathways by which peripheralchemoreceptors may modulate central neurons thought to serve as CO 2/H + chemoreceptor neurons.SUMMARY AND CONCLUSIONSThe concepts that the input from the carotid bodies: (1) constitute a major excitatory drive to breathe, (2) serve as the major source of peripheral O 2chemoreception, and (3) significantly contribute to CO 2/H + chemoreception is exemplified by the major effects of CBD in multiple mammalian species. Therespiratory plasticity, or restoration of function that occurs following CBD likely includes an upregulation of additional, normally quiescent sites of peripheralchemoreception potentially involving 5-HT. However, the data indicate that these conditional, peripheral sitescannot account for all of the plasticity in the mechanisms that govern eupneic breathing. Thus, we conclude that within the respiratory network there is an additional site/mechanism (s) of plasticity. Future work aiming to elucidate brainstem mechanisms of plasticity following peripheral lesions may prove useful harnessing and maximizing the capacity for the restoration of function in human disease and/or trauma.Author contributions: Mathew R. Hodges and Hubert V. Forster contributed to the writing and editing of the manuscript, and Mathew R. Hodges prepared the figures. Conflicts of interest: None declaredFunding: NIH NHLBI HL097033 (MRH) and VA Merit Review 2885-02P (HVF)Figure 5 Ventilation (expressed as a percentage ofcontrol) for up to 5 hours after 10 µL injections of ibotenic acid into the caudal or rostral raphé in carotid body intact or carotid body denervation (CBD) goats.Note the enhanced stimulatory effect of ibotenic acid in the rostral medullary raphé in goats that had prior CBD, suggesting altered raphé glutamate receptor activity. Adapted from [30]. 050 100 150 200 250300Time (minute) 350300 250 200 150100 V 1 (% o f c o n t r o l )REFERENCES[1] Haldane JS, Priestley JG. The regulation of thelung-ventilation. J Physiol. 1905;32:225-266.[2] Comroe JH, Schmidt CM. The part played by reflexesfrom the carotid in the chemical regulation of therespiration in the dog. Am J Physiol. 1938;121:75-97. [3] Fencl V, Miller TB, Pappenheimer JR. Studies on therespiratory response to disturbances of acid-base balance, with deductions concerning the ionic composition ofcerebral interstitial fluid. Am J Physiol. 1966;210:459-472.[4] Smith CA, Forster HV, Blain GM, et al. An interdependentmodel of central/peripheral chemoreception: evidence and implications for ventilatory control. Respir PhysiolNeurobiol. 2010;173:288-297.[5] Forster HV, Smith CA. Contributions of central andperipheral chemoreceptors to the ventilatory response toCO2/H+. J Appl Physiol. 2010;108:989-994.[6] Pan LG, Forster HV, Martino P, et al. Important role ofcarotid afferents in control of breathing. J Appl Physiol.1998;85:1299-1306.[7] Bisgard GE, Forster HV, Orr JA, et al. Hypoventilation inponies after carotid body denervation. J Appl Physiol.1976;40:184-190.[8] Doi A, Ramirez JM. Neuromodulation and theorchestration of the respiratory rhythm. Respir PhysiolNeurobiol. 2008;164:96-104.[9] Baker-Herman TL, Mitchell GS. Phrenic long-termfacilitation requires spinal serotonin receptor activationand protein synthesis. J Neurosci. 2002;22:6239-6246. [10] Fuller DD, Zabka AG, Baker TL, et al. Phrenic long-termfacilitation requires 5-HT receptor activation during but not following episodic hypoxia. J Appl Physiol.2001;90:2001-2006; discussion 2000.[11] Lahiri S, DeLaney RG. Stimulus interaction in theresponses of carotid body chemoreceptor single afferentfibers. Respir Physiol. 1975;24:249-266.[12] Ichikawa H. Innervation of the carotid body:Immunohistochemical, denervation, and retrogradetracing studies. Microsc Res Tech. 2002;59:188-195. [13] Kumar P. Sensing hypoxia in the carotid body: fromstimulus to response. Essays Biochem. 2007;43:43-60. [14] Blain GM, Smith CA, Henderson KS, et al. Peripheralchemoreceptors determine the respiratory sensitivity ofcentral chemoreceptors to CO(2). J Physiol. 2010;588:2455-2471.[15] Forster HV, Bisgard GE, Klein JP. Effect of peripheralchemoreceptor denervation on acclimatization of goatsduring hypoxia. J Appl Physiol. 1981;50:392-398.[16] Forster HV, Bisgard GE, Rasmussen B, et al. Ventilatorycontrol in peripheral chemoreceptor-denervated poniesduring chronic hypoxemia. J Appl Physiol. 1976;41:878-885. [17] Forster HV, Pan LG, Lowry TF, et al. Important role ofcarotid chemoreceptor afferents in control of breathing ofadult and neonatal mammals. Respir Physiol. 2000;119:199-208.[18] Dahan A, Nieuwenhuijs D, Teppema L. Plasticity of centralchemoreceptors: effect of bilateral carotid body resectionon central CO2 sensitivity. PLoS medicine. 2007;4:e239.[19] Olson EB, Vidruk EH, Dempsey JA. Carotid body excisionsignificantly changes ventilatory control in awake rats. JAppl Physiol. 1988;64:666-671.[20] Lowry TF, Forster HV, Pan LG, et al. Effects on breathingof carotid body denervation in neonatal piglets. J ApplPhysiol. 1999;87:2128-2135.[21] Edelman NH, Epstein PE, Lahiri S, et al. Ventilatoryresponses to transient hypoxia and hypercapnia in man.Respir Physiol. 1973;17:302-314.[22] Bellville JW, Whipp BJ, Kaufman RD, et al. Central andperipheral chemoreflex loop gain in normal and carotidbody-resected subjects. J.Appl.Physiol.1979;46:843-853.[23] Rodman JR, Curran AK, Henderson KS, et al. Carotidbody denervation in dogs: eupnea and the ventilatoryresponse to hyperoxic hypercapnia. J Appl Physiol.2001;91:328-335.[24] Smith CA, Rodman JR, Chenuel BJ, et al. Response timeand sensitivity of the ventilatory response to CO2 inunanesthetized intact dogs: central vs. peripheralchemoreceptors. J Appl Physiol. 2006;100:13-19.[25] Forster HV. Plasticity in the control of breathing followingsensory denervation. J Appl Physiol. 2003;94:784-794. [26] Smith PG, Mills E. Restoration of reflex ventilatoryresponse to hypoxia after removal of carotid bodies in the cat. Neuroscience.1980;5:573-580.[27] Bisgard GE, Forster HV, Klein JP. Recovery of peripheralchemoreceptor function after denervation in ponies. J Appl Physiol.1980;49:964-970.[28] Serra A, Brozoski D, Hodges M, et al. Effects of carotidand aortic chemoreceptor denervation in newborn piglets.J Appl Physiol. 2002;92:893-900.[29] Serra A, Brozoski D, Simeon T, et al. Serotonin andserotonin receptor expression in the aorta of carotid intact and denervated newborns. Respir Physiol Neurobiol.2002;132:253-264.[30] Hodges MR, Opansky C, Qian B, et al. Carotid bodydenervation alters ventilatory responses to ibotenic acidinjections or focal acidosis in the medullary raphe. J ApplPhysiol. 2005;98:1234-1242.[31] Liu Q, Wong-Riley MT. Postnatal changes in cytochromeoxidase expressions in brain stem nuclei of rats:implications for sensitive periods. J Appl Physiol. 2003;95: 2285-2291.[32] Hoop B, Masjedi MR, Shih VE, et al. Brain glutamatemetabolism during hypoxia and peripheralchemodenervation. J Appl Physiol. 1990;69:147-154.1078[33] Roux JC, Peyronnet J, Pascual O, et al. Ventilatory andcentral neurochemical reorganisation of O2 chemoreflexafter carotid sinus nerve transection in rat. J Physiol.2000;522(Pt 3):493-501.[34] Roux JC, Pequignot JM, Dumas S, et al. O2-sensing aftercarotid chemodenervation: hypoxic ventilatoryresponsiveness and upregulation of tyrosine hydroxylasemRNA in brainstem catecholaminergic cells. Eur JNeurosci. 2000;12:3181-3190.[35] Mulkey DK, Stornetta RL, Weston MC, et al. Respiratorycontrol by ventral surface chemoreceptor neurons in rats.Nat Neurosci. 2004;7:1360-1369.[36] Takakura AC, Moreira TS, Colombari E, et al. Peripheralchemoreceptor inputs to retrotrapezoid nucleus (RTN)CO2-sensitive neurons in rats. J Physiol. 2006;572:503-523.[37] Thor KB, Helke CJ. Serotonin and substance Pcolocalization in medullary projections to the nucleustractus solitarius: dual-colour immunohistochemistrycombined with retrograde tracing. J Chem Neuroanat.1989;2:139-148. [38] Jean A. The nucleus tractus solitarius: neuroanatomic,neurochemical and functional aspects. Arch Int PhysiolBiochim Biophys. 1991;99:A3-52.[39] Nuding SC, Segers LS, Shannon R, et al. Central andperipheral chemoreceptors evoke distinct responses insimultaneously recorded neurons of the raphe-pontomedullary respiratory network. Philos Trans R SocLond B Biol Sci. 2009;364:2501-2516.[40] Pan LG, Forster HV, Ohtake PJ, et al. Effect of carotidchemoreceptor denervation on breathing duringventrolateral medullary cooling in goats. J Appl Physiol.1995;79:1120-1128.(Edited by Sheikh PB/Zhao LJ/Song LP)1079。
慢性疼痛对中枢神经系统的影响及调控机制慢性疼痛是一种令人痛苦且困扰人的疾病,长期的疼痛刺激不仅影响身体健康,也会对中枢神经系统产生重要的影响,进而对其他生理功能产生负面影响。
本文将探讨慢性疼痛对中枢神经系统的影响,并介绍其中的调控机制。
一、慢性疼痛对中枢神经系统的影响1. 神经可塑性的改变慢性疼痛刺激可以导致中枢神经系统中的突触可塑性产生变化。
研究表明,慢性疼痛可以引起突触传递的异常增强,使原本无痛刺激也能引起剧痛反应。
这种可塑性的改变可能与疼痛信号在中枢神经系统中的加强和扩散有关,进一步加剧了疼痛感受。
2. 神经炎症反应的激活慢性疼痛会引发中枢神经系统中的炎症反应,导致神经胶质细胞活化和炎症因子的释放。
这些炎症因子包括肿瘤坏死因子-α(TNF-α)、白介素-1β(IL-1β)等,它们会进一步介导神经炎症反应,并通过激活炎症信号通路增强疼痛感受。
3. 大脑结构的改变慢性疼痛还可以导致中枢神经系统中的大脑结构发生改变。
研究发现,长期的疼痛刺激会使大脑皮层区域发生萎缩,神经元密度降低。
这些结构改变可能与慢性疼痛患者的记忆、情绪和认知功能障碍有关。
二、慢性疼痛对中枢神经系统的调控机制1. 疼痛信号传导的调控中枢神经系统对疼痛信号的传导起着重要的调控作用。
研究发现,内源性痛阈调控系统通过产生与疼痛信号相互作用的内啡肽等物质来减轻疼痛感受。
此外,脑干的痛阈调控系统以及大脑皮层区域也能通过神经调节和认知过程来调节疼痛感受。
2. 炎症反应的调控中枢神经系统对神经炎症反应有着复杂的调控机制。
一方面,神经胶质细胞在神经炎症过程中发挥着重要作用,它们能够分泌炎症因子并调节炎症反应。
另一方面,大脑区域如下丘脑和杏仁核等则通过神经调节途径调控炎症反应的强度和持续时间。
3. 神经可塑性的调控神经可塑性的改变可以通过多种机制来调控。
神经递质的释放和突触传递的调节、神经营养因子的改变以及突触后钙离子浓度的调节等都可以影响神经可塑性。
NMDA受体介导突触可塑性相关离子通道机制介绍NMDA受体是神经元中最重要的离子通道之一,它在神经元之间的连接和信息传递中发挥关键作用。
NMDA受体介导的突触可塑性,也被称为长时程突触可塑性,是神经系统中学习和记忆形成的基础。
本文将详细探讨NMDA受体介导的突触可塑性相关的离子通道机制。
NMDA受体的结构和功能NMDA受体是一种离子通道蛋白质,主要存在于中枢神经系统的突触间隙中。
它是由多个亚单位组成的复合体,包括GluN1、GluN2和GluN3亚单位。
其中,GluN1亚单位是必需的,而GluN2和GluN3亚单位则对受体的功能具有调节作用。
NMDA受体的活化需要同时满足两个条件:首先,细胞内需要存在足够的兴奋性氨基酸(如谷氨酸)作为共激动剂,其次,细胞内要充足地形成正常动作电位。
这是因为NMDA受体的结构上包含一个钙离子通道和一个镁离子通道,而这两个通道只有在细胞内发生去除性镁离子阻滞时才能打开。
当NMDA受体活化时,离子通道打开,钙离子进入细胞内,从而引起突触可塑性的发生。
突触可塑性与离子通道的调节突触可塑性是指突触连接强度会随时间的变化而变化的能力。
NMDA受体介导的长时程突触可塑性有两种类型:长时程增强(LTP)和长时程抑制(LTD)。
LTP指的是突触传递强度的增强,而LTD则指的是突触传递强度的减弱。
NMDA受体介导的突触可塑性与多种离子通道有关。
首先,NMDA受体活化所需的电位变化可以由细胞内过量的钠离子和钙离子通道的开放产生。
这些离子通过膜电位的改变使得NMDA受体去除性镁离子阻滞,从而引起NMDA受体的活化,进而触发突触可塑性过程。
其次,NMDA受体的活化还依赖于钾离子通道的调节。
神经元兴奋时,细胞内钾离子浓度会逐渐减少,导致钾离子通道关闭。
这种钾离子通道的调节作用有助于维持细胞内的兴奋性水平,从而使得NMDA受体的活化更容易发生。
此外,NMDA受体的活化还与钙离子通道有关。
当NMDA受体活化后,钙离子通道会打开,使大量钙离子进入细胞内。
生理学中的神经可塑性机制神经可塑性机制是指神经系统能够在外界刺激下发生一系列的改变和迁移的过程。
这种机制在人类的生存和适应外界环境的过程中扮演着非常重要的角色。
神经可塑性机制主要分为两种类型,一种是短期可塑性,另一种是长期可塑性。
短期可塑性通常是短暂的,很快就会消失,主要是由于神经元内部的电活动发生的改变所导致的。
而长期可塑性则是相对持久的,能够在数小时、数天或更长时间内持续下去。
长期可塑性的形成主要依赖于基因、营养、应激等因素。
神经可塑性机制在人类学习、记忆等方面也起着重要的作用。
例如,在人类的语言习得过程中,神经可塑性机制的作用就非常显著。
人类的语言能力主要是依赖于大脑的语言中枢区域。
研究发现,当人类进行语言学习时,这些语言区域的连接会发生调整,这种调整能够增强区域之间的联系,从而提高语言学习和记忆的效率。
在神经可塑性机制的过程中,神经元之间的突触扮演着非常重要的角色。
突触是神经元之间传递信息必不可少的结构。
而突触可以通过多种方式进行调整,包括调整突触前、突触后的细胞膜通道等。
这些调整能够影响到神经元之间的信号传递,从而影响到神经元的功能和行为。
神经可塑性机制的形成还与神经递质的变化密切相关。
神经递质是神经元之间传递信息的化学物质,它能够在神经元之间进行信息传递。
而当神经元受到外界刺激时,它会分泌出一些神经递质,在神经元之间进行传递。
这些神经递质的分泌和突触连接的调整,能够共同影响到神经元之间的信号传递,从而影响到神经元的行为和功能。
总之,神经可塑性机制在人类生理学中扮演着非常重要的角色。
这种机制能够帮助人类适应外界环境,并且在语言习得、学习和记忆等方面发挥着非常重要的作用。
未来的研究需要进一步探讨神经可塑性机制的本质以及其在疾病预防和治疗方面的应用。