鼻咽癌精准放疗正常组织的勾画图谱王孝深
- 格式:pdf
- 大小:3.01 MB
- 文档页数:31
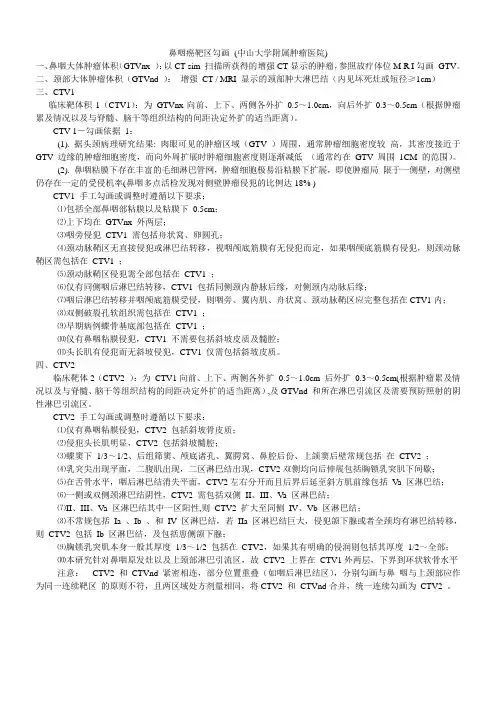
鼻咽癌靶区勾画(中山大学附属肿瘤医院)一、鼻咽大体肿瘤体积(GTVnx ):以CT sim 扫描所获得的增强CT显示的肿瘤,参照放疗体位M R I勾画GTV。
二、颈部大体肿瘤体积(GTVnd ):增强CT / MRI 显示的颈部肿大淋巴结(内见坏死灶或短径≥1cm)三、CTV1临床靶体积1(CTV1):为GTVnx向前、上下、两侧各外扩0.5~1.0cm,向后外扩0.3~0.5cm(根据肿瘤累及情况以及与脊髓、脑干等组织结构的间距决定外扩的适当距离)。
CTV 1-勾画依据1:(1). 据头颈病理研究结果: 肉眼可见的肿瘤区域(GTV )周围,通常肿瘤细胞密度较高,其密度接近于GTV 边缘的肿瘤细胞密度,而向外周扩展时肿瘤细胞密度则逐渐减低(通常约在GTV 周围1CM 的范围)。
(2). 鼻咽粘膜下存在丰富的毛细淋巴管网,肿瘤细胞极易沿粘膜下扩展,即使肿瘤局限于一侧壁,对侧壁仍存在一定的受侵机率(鼻咽多点活检发现对侧壁肿瘤侵犯的比例达18% )CTV1 手工勾画或调整时遵循以下要求:⑴包括全部鼻咽部粘膜以及粘膜下0.5cm;⑵上下均在GTVnx 外两层;⑶咽旁侵犯CTV1 需包括舟状窝、卵圆孔;⑷颈动脉鞘区无直接侵犯或淋巴结转移,视咽颅底筋膜有无侵犯而定,如果咽颅底筋膜有侵犯,则颈动脉鞘区需包括在CTV1 ;⑸颈动脉鞘区侵犯需全部包括在CTV1 ;⑹仅有同侧咽后淋巴结转移,CTV1 包括同侧颈内静脉后缘,对侧颈内动脉后缘;⑺咽后淋巴结转移并咽颅底筋膜受侵,则咽旁、翼内肌、舟状窝、颈动脉鞘区应完整包括在CTV1内;⑻双侧破裂孔软组织需包括在CTV1 ;⑼早期病例蝶骨基底部包括在CTV1 ;⑽仅有鼻咽粘膜侵犯,CTV1 不需要包括斜坡皮质及髓腔;⑾头长肌有侵犯而无斜坡侵犯,CTV1 仅需包括斜坡皮质。
四、CTV2临床靶体2(CTV2 ):为CTV1向前、上下、两侧各外扩0.5~1.0cm 后外扩0.3~0.5cm(根据肿瘤累及情况以及与脊髓、脑干等组织结构的间距决定外扩的适当距离),及GTVnd 和所在淋巴引流区及需要预防照射的阴性淋巴引流区。
鼻咽癌调强放射治疗靶区勾画-中国医学科学院肿瘤医院经验总结易俊林;曲媛;高黎;徐国镇;黄晓东;罗京伟;李素艳;肖建平;王凯;张世平【期刊名称】《肿瘤预防与治疗》【年(卷),期】2011(24)3【摘要】Objective : To summarize the experience and skill in contouring target volume of IMRT for nasopharyngeal carcimoma of our hospital. Methods: The intensity-modulated radiotherapy( IMRT ) technique has been applied since Novemher 2001 in our hospital. During the past 9 years, the methods and skill of contouring the target volume of nasopharyngeal carcinoma have been estahlished and improved. We intend to describe the detailed experience and tips in this field here. Results : we have established a complete protocol of contouring target volume of nasopharyngeal carcinoma and made it as a daily practice guideline, and we also accumulated abundant tips in dealing with some dilemma. All these were confirmed by the outcomes of 376 patients treated by IMRT in our department. Conclusion: The protocol of contouring target volume of nasopharyngeal carcinoma in IMRT is a fruit of whole wisdom of our department. We hope it may he useful in daily practice.%目的:总结我院鼻咽癌调强放射治疗靶区勾画及个体化处理经验.方法:自2001年11月到2010年7月我院已开展鼻咽癌调强放疗技术9年,通过不断摸索和完善,制定了鼻咽癌靶区勾画规范,本文描述在靶区勾画中的经验和技巧.结果:通过开展鼻咽癌调强放射治疗技术9年来的实践,我们制定了比较完善合理的鼻咽癌靶区勾画方法,并在一些细节和个体化处理上积累了丰富的经验,形成了日常临床实践的指南,通过治疗376例鼻咽癌,得到了良好的临床疗效.结论:我院鼻咽癌调强放射治疗靶区勾画经验与技巧取得了较好的临床疗效,可供其他单位鼻咽癌靶区勾画时参考.【总页数】8页(P157-163,172)【作者】易俊林;曲媛;高黎;徐国镇;黄晓东;罗京伟;李素艳;肖建平;王凯;张世平【作者单位】中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021;中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021;中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021;中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021;中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021;中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021;中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021;中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021;中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021;中国医学科学院中国协和医科大学肿瘤研究所肿瘤医院放射治疗科,北京,100021【正文语种】中文【中图分类】R739.63;R730.55【相关文献】1.图像引导鼻咽癌调强放射治疗靶区勾画研究进展 [J], 刘均;陈宏2.鼻咽癌旋转调强放射治疗与固定野动态调强放射治疗的剂量学比较 [J], 杨振;宾石珍;雷明军;刘归;张子健;吕知平3.建立鼻咽癌调强放射治疗靶区勾画指南的必要性 [J], 王孝深;胡超苏;应红梅;何霞云;朱国培;冯炎4.容积旋转调强放射治疗与9野静态调强放射治疗在侵犯颅内鼻咽癌患者中的剂量学特点 [J], 刘小慧5.《中国医刊》杂志、《中国临床医生》杂志与中国医学科学院肿瘤医院、秦皇岛市肿瘤医院共同举办“全国第二届肿瘤规范化、标准化诊治学术会” [J],因版权原因,仅展示原文概要,查看原文内容请购买。

鼻咽癌放射治疗危及器官自动勾画的几何和剂量学分析黄新;王新卓;薛涛;刘双童;刘斌;吴迪;张恒;王辉【期刊名称】《生物医学工程与临床》【年(卷),期】2024(28)1【摘要】目的探讨分析鼻咽癌容积旋转调强放射治疗(VMAT)中危及器官(OAR)自动勾画(AS)的几何和剂量学准确度,并检验OAR勾画的几何和剂量学之间的相关性,为放射治疗(简称放疗)患者OAR勾画提供参考依据。
方法回顾性选择120例鼻咽癌放疗患者,其中男性84例,女性36例;年龄11~82岁,中位年龄55岁;病灶位于颅底与软腭之间,垂直径和横径各3~4 cm,前后径2~3 cm。
其中随机数字法选择85例患者经AccuLearning深度学习训练平台训练形成AS模型,将AS模型导入AccuContour软件。
利用AS模型勾画未训练的35例鼻咽癌放疗患者的18个OAR。
比较AS与手动勾画(MS)OAR的几何度量有戴斯相似性系数(DSC)、杰卡德系数(JAC)、质心偏差(DC)、豪斯多夫距离(HD95)、对称位置平均表面距离(ASSD)、相对绝对体积差异(RAVD)。
在同一个VMAT计划下,通过剂量体积直方图(DVH),比较AS与MS勾画的OAR剂量学参数。
采用双尾Spearman来分析几何指标和剂量学绝对差异值之间的相关性。
结果AS勾画的OAR轮廓与MS勾画的OAR轮廓具有差异性。
几何指标DSC、JAC、RAVD勾画质量表现最佳的是下颌骨,其均值±标准差分别为0.94±0.01、0.88±0.02、6.34±4.13。
左晶状体的HD95、ASSD结果最好,其均值±标准差分别为2.04±0.91、0.22±0.12。
DC均值±标准差最佳的是右眼球,为0.93±0.77。
DSC和JAC中勾画质量表现最差是视交叉,其均值±标准差分别为0.75±0.06、0.60±0.07。

Supplementary Table 1: Clinical characteristics of the 41 NPC patientsand 21 patients with NPC and unilateral TLNCharacteristic Value for the 41 NPC patients Value for the 21 NPC patients with unilateral Number 41 21GenderMale 31 16Female 10 5Age (years)≤ 40 13 8> 40 28 13T stage aT1 7 1T2 9 1T3 17 3T4 8 16N stage aN0 6 4N1 20 12N2 11 5N3 4 0Overall stage aI 2 1II 11 1III 16 3IV 12 16Radiation technique bVMAT 17 0Static IMRT 24 21ChemotherapyNo 6 3Yes 35 18Involved lateralityLeft side 13Right side 8Abbreviations: TLN, temporal lobe necrosis; IMRT, intensity modulated radiotherapy; VMAT, volumetric modulated arc therapya According to the 7th AJCC/UICC staging system.b All the patients were treated with IMRT including 17 with VMA T and 24 with static IMRT.Supplementary Table 2: Comparison of dosimetric parameters between temporal lobes with and without TLN using the two contouring methodsDosimetric parametersMethod 1a Method 2bt Mean difference P-value t Mean difference P-valueD0.1cc c 6.15 10.46 <0.001 6.09 10.40 <0.001 D0.5cc 5.08 8.03 <0.001 6.84 11.87 <0.001 D1cc 6.98 12.84 <0.001 7.01 12.86 <0.001 D5cc 7.12 14.28 <0.001 7.70 14.81 <0.001 D10cc 5.92 12.91 <0.001 6.55 13.45 <0.001 D15cc 4.70 10.09 <0.001 5.08 10.49 <0.001 D20cc 3.80 7.29 0.001 4.26 7.77 <0.001 D25cc 3.52 5.44 0.002 3.96 5.79 0.001 D30cc 3.44 3.45 0.004 4.18 4.24 0.001 D35cc 2.42 1.97 0.025 4.42 3.03 <0.001 D40cc 2.00 1.31 0.049 3.85 2.17 0.001 D1d7.06 12.54 <0.001 7.14 12.90 <0.001 D2 7.23 13.82 <0.001 7.25 14.12 <0.001 D5 7.84 14.89 <0.001 8.04 15.05 <0.001 D10 7.12 14.66 <0.001 7.01 14.16 <0.001 D15 6.17 13.02 <0.001 5.46 11.66 <0.001 D20 4.98 11.33 <0.001 4.58 9.12 <0.001 D25 4.61 8.91 <0.001 4.20 6.84 0.001 D30 4.21 7.05 0.001 4.23 4.96 <0.001 D35 4.62 5.75 <0.001 4.81 3.98 <0.001 D40 4.51 4.19 <0.001 4.39 3.00 <0.001 D45 4.03 3.14 0.001 3.98 2.27 0.001 D50 3.63 2.36 0.002 3.74 1.77 0.001 D55 3.61 1.76 0.002 3.67 1.51 0.002 D60 3.59 1.4 0.002 3.71 1.47 0.001 V10e 3.32 4.88 0.003 3.17 5.28 0.005 V20 5.13 5.86 <0.001 5.31 6.15 <0.001 V25 5.95 7.16 <0.001 6.16 6.79 <0.001 V30 6.97 8.72 <0.001 6.95 7.69 <0.001 V35 6.77 9.71 <0.001 6.86 8.18 <0.001 V40 6.18 10.01 <0.001 6.48 8.26 <0.001 V45 5.84 9.89 <0.001 6.10 8.03 <0.001 V50 2.72 3.37 0.013 5.81 7.78 <0.001 V55 5.19 8.61 <0.001 5.39 7.02 <0.001 V60 4.75 7.07 <0.001 4.78 5.75 <0.001 V65 3.88 4.93 0.001 3.88 4.01 0.001 V70 2.85 2.64 0.01 2.87 2.20 0.009 V75 2.06 0.83 0.042 2.19 0.72 0.041 Volume 2.92 3.62 0.009 2.26 3.10 0.035 Dmean 5.83 4.98 <0.001 5.83 4.36 <0.001 D1 of PRV f7.35 11.48 <0.001 7.50 11.80 <0.001 D5 of PRV 7.80 14.19 <0.001 8.20 14.73 <0.001 D10 of PRV 6.80 14.18 <0.001 7.27 14.73 <0.001 D15 of PRV 5.95 13.14 <0.001 5.72 12.45 <0.001D20 of PRV 4.93 11.02 <0.001 4.71 9.59 <0.001D25 of PRV 4.30 8.60 <0.001 4.29 7.15 <0.001D30 of PRV 4.01 6.77 0.001 4.20 5.25 <0.001D35 of PRV 3.94 5.07 0.001 4.26 3.92 <0.001D40 of PRV 4.16 3.88 <0.001 4.38 3.06 <0.001D45 of PRV 3.89 2.93 0.001 4.13 2.35 0.001D50 of PRV 3.70 2.23 0.001 3.91 1.88 0.001D55 of PRV 3.72 1.66 0.001 3.76 1.59 0.001D60 of PRV 3.44 1.25 0.003 3.57 1.40 0.002V20 of PRV 5.31 5.66 <0.001 5.21 5.72 <0.001V25 of PRV 5.73 6.88 <0.001 6.01 6.70 <0.001V30 of PRV 6.94 8.77 <0.001 6.70 7.73 <0.001V35 of PRV 6.59 9.40 <0.001 6.82 8.28 <0.001V40 of PRV 6.22 9.61 <0.001 6.52 8.31 <0.001V45 of PRV 5.96 9.92 <0.001 6.31 8.06 <0.001V50 of PRV 5.74 9.17 <0.001 6.04 7.78 <0.001V55 of PRV 5.53 8.47 <0.001 5.76 7.18 <0.001V60 of PRV 5.05 7.16 <0.001 5.17 6.08 <0.001V65 of PRV 4.33 5,.30 <0.001 4.38 4.51 <0.001V70 of PRV 3.18 2.99 0.005 3.42 2.66 0.003V75 of PRV 2.45 1.10 0.024 2.55 0.98 0.019 Abbreviations: PRV=planning organ at risk volume; D mean= mean dose; TLN=temporal lobe necrosis;a Temporal lobe including the basal ganglia and insula, excluding parahippocampal gyrus and hippocampusb Temporal lobe including parahippocampal gyrus and hippocampus, excluding basal ganglia and insula.c D0.1cc is the minimum dose received by the ‘‘hottest’’ 0.1ml of the organ, the other D with suffixes expresses the same meaning, but the suffix numbers represent the absolute volume.d D1 is the minimum dose received by the ‘‘hottest’’ 1% of the organ, the other D with suffixes express the same meaning, but the suffix nu mbers represent the percentage of volume.e V10 is the percentage of volume of temporal lobe that receives more than 10 Gy, the other V with suffixes express the same meaning, but the suffix numbers represent the doses received.f D1of PRV is the minimum dose received by the ‘‘hottest’’ 1% of the planning organ at risk volume of temporal lobe volume, the other Dx of PRV, Vx of PRV express the same meaning, but the prefix parameter represent the percentage of volume or the dose received.Supplementary Table 3: Anatomic boundaries of the organs at risk in NPC.Organ StandardTPS name [20]Cranial Caudal Anterior Posterior Lateral MedialTMJ TMjoint a Disappearance ofarticular cavity Appearance of thehead of mandible orone slice superior tothe sigmoid notch ofthe neck of mandibleArticular condyle of thetemporal bone, ant.edge of mandibularcondyleSurface of fossaglenoidLat. edge ofmandibular condyle orsurface of fossaglenoidBrainstem BrainStem Optic tract or thedisappearance ofposterior cerebralartery Foramen magnum Post. edge of prepon-tine cistern or basilararteryAnt. edge of forthventricle ormesencephalicaqueductPosterior cerebralartery, anteriorinferior cerebellarartery, cerebellarpeduncleOptic chiasm Chiasm One or two slicessuperiorly Pituitary orsuprasellar cisternOptic canal Infundibulum Internal carotidarteries, middlecerebral arteriesTongue(oral cavity)b Tongue Post. edge of thehard palate or softpalateDisappearance ofanterior belly ofdigastric musclePost. edge of mandibleor is freePalate, oropharynx,the palatine tonsil,hyoid boneMed. edge of themandible or inferioralveoli socketLarynx(larynx and laryngopharynx) Larynx Cranial edge ofepiglottisCaudal edge of cricoidcartilageAnt. edge of thyroidcartilage or cricoidcartilageIncluding arytenoidcartilage, the superiorand inferior horns ofthyroid cartilage andpost. edge ofpharyngeal constrictorMed. edge of hyoidbone, lat. edge ofthyroid cartilage andcricoid cartilage,cervical vessels,nerves, and lateralthyroidUpper Pharyngeal- Caudal edge of Cranial edge of hyoid Nasopharynx, Longus capitis m., Carotid sheathpharyngeal constrictor [22] Const_Upper pterygoid plates bone oropharynx,laryngopharynx, base oftonguelongus colli m., bodyof cervical vertebraMiddle pharyngeal constrictor [22] Pharyngeal-Const_MiddleCranial edge ofhyoid boneCaudal edge of hyoidboneLaryngopharynx Longus capitis m.,longus colli m., bodyof cervical vertebraHyoid boneInferior pharyngeal constrictor [22] Pharyngeal-Const_LowerCaudal edge ofhyoid boneCaudal edge of cricoidcartilageLaryngopharynx orcricoids cartilageLongus capitis m.,longus colli m., bodyof cervical vertebraThyroid cartilage orthyroid glandTrachea Trachea Caudal edge ofcricoid cartilage Two centimetersbelow the caudal edgeof the clavicularheadPost. edge of isthmus ofthyroid glandAnt. edge ofesophagusLateral thyroid gland One-twomillimetersexpanded from thelumen of tracheaSubman- dibular gland Submandibular a Inferior edge ofmedial pterygoid orthe level of C3Appearance of fatspace ofsubmandibulartriangleLat. surface ofmylohyoid m. orhyoglossus m.Parapharyngeal space,cervical vessels andpost. belly of digastricm.,sternocleidomastoidm.Ramus of themandible,subcutaneous fat orplatysmaCervical vessels,superior and middlepharyngealconstrictor m.,hyoid bone, post.belly of thedigastric m.,mylohyoid m. orhyoglossus m.Esophagus [22] Esophagus Caudal edge ofcricoid cartilage Two centimetersbelow the caudal edgeof the clavicular headTrachea Vertebral body orlongus colli m.Fat space or thyroidglandOptic nerve [23] OpticNerve a Below the superiorrectus Superior the inferiorrectusPosterior edge of thecenter of globeOptic canalTemporal lobe TemporalLobe a Cranial edge of the Base of middle cranial Temporal bone and Petrous part of Temporal bone Cavernous sinus,sylvian fissure fossa sylvian fissure,greaterwing of sphenoid temporal lobe,tentorium ofcerebellum, incisurapreoccipitalissphenoid sinus,sella turcica, andsylvian fissure(includingparahippocampalgyrus andhippocampusParotid gland [21] Parotid a External auditorycanal, mastoidprocessAppearance post. partsubmandibular spaceMasseter m. post.border mandibularbone, medial pterygoidm.Ant. bellysternocleidomastoidm., lat. side post. bellyof the digastric m.(posterior medial),mastoid processSubmandibular fat,platysmaPost. belly of thedigastric m., styloidprocess,parapharyngealspace,sternocleidomastoidSpinal cord SpinalCord Disappearance ofcerebellum Two centimetersbelow the inferioredge of the clavicularheadExclude the subarachnoid spaceBrachial plexus [24] BrachialPlexus a Caudal edge of C4 Caudal edge of T1 atneural foramina andone to two CT slicesbelow the clavicularhead as the posterioraspect of theneurovascularbundleAnterior scalene muscle Middle scalenemuscleFat space Spinal cordThyroid gland Thyroid Caudal edge ofpyriform sinus ormidpoint of thyroidcartilage Body of fifth toseventh cervicalvertebraSternohyoid orsternocleidomastoidCervical vessels orlongus colli m.Cervical vessels orsternocleidomastoidThyroid cartilage orcricoids cartilage oresophagus orpharyngealconstrictorMandible Mandible The mandible be contoured as whole organ but not be divided into the left and the right. Contouring of the mandible should include alveolar bone and exclude the teeth.Inner ear Ear_Inner a Cochlea and IAC should be individually delineated and named.Middle ear Ear_Middle a Tympanic cavity, bony part of ET should be individually delineated and named.Eyes Eyes a Ensure the retina to be contoured completely.Lens Lens a The boundary between the lens and the vitreum is obviousPituitary Pituitary The pituitary is located in the hypophysial fossa. Insure the organ be contoured completely but not beyond the surrounding bone. The pituitary is ovoid and can be visualized on 1-2 slices on CT scans of 3 mm thicknessAbbreviations: TMJ, temporomandibular joint; ET, Eustachian tube; IAC, internal auditory canal; m., muscle.a The organs should be divided into left and right, and the standard TPS name of laterality is indicated by appending an underscore character ( _ ), followed by L or R,respectively. For example, the left parotid is named Parotid_L; the right parotid is named Parotid_R.b include the base of the tongue, body of tongue and mouth floor.Supplementary table 4: Abbreviations mentioned in the manuscript. Abbreviations Full nameOAR organ at riskTMJ temporomandibular jointNPC nasopharyngeal carcinomaPC pharyngeal constrictorET Eustachian tubeROC receiver operating characteristicTLN temporal lobe necrosisIAC internal auditory canalRT radiotherapyGTV gross target volumeCTV clinical target volumePTV planning target volumePRV planning organ at risk volumeDmean mean doseDmax maximum doseS.E. standard errorSNHL sensorineural hearing lossOME otitis media with effusionIMRT intensity modulated radiotherapyVMAT volumetric modulated arc therapyAUC Area under the curveDx(xcc) minimum dose received by the ‘‘hottest’’ x% (or x ml) of the organ Vx volume percentage of the organ receiving ≥ X GySupplementary Figure 1. Receiver operating characteristic (ROC) curve analysis for the D1 of the PRV using two different temporal lobe contouring methods in 21 NPC patients with unilateral TLN.Supplementary Figure 2. Recommended atlas of the tympanic cavity, Eustachian tube (ET), cochlea, IAC, TMJ, temporal lobe, brainstem, parotid gland,spinal cord, optic nerve, chiasm, submandibular gland, pituitary, mandible, eyes, lens, brachial plexus, tongue(oral cavity), larynx, pharyngeal constrictors and trachea as OARs based on CT-MRI fusion in NPC patients.Supplementary References 1: The list of literatures relative to OARs contouring1.Baxi S, Park E, Chong V, Chung HT. Temporal changes in IMRT contouring of organs atrisk for nasopharyngeal carcinoma - the learning curve blues and a tool that could help.Technol Cancer Res Treat 2009; 8:131-140.2.Gondi V, Tome WA, Rowley HA, Mehta MP. Hippocampal Contouring: A ContouringAtlas for RTOG 0933. 2011.3.Penumetcha N, Kabadi S, Jedynak B, et al. Feasibility of geometric-intensity-basedsemi-automated delineation of the tentorium cerebelli from MRI scans. J Neuroimaging 2011; 21:e148-55.4.Chau RM, Leung SF, Kam MK, et al. A split-organ delineation approach for doseoptimisation for intensity-modulated radiotherapy for advanced T-stage nasopharyngeal carcinoma. Clin Oncol (R Coll Radiol) 2008; 20:134-41.5.Bonilha L, Kobayashi E, Cendes F, Li LM. The importance of accurate anatomicassessment for the volumetric analysis of the amygdala. Braz J Med Biol Res 2005;38:409-18.6.Wang SZ, Yan XJ, Guo M, et al. Clinical analysis of otitis media with effuse after 3Dplanning system based radiotherapy of nasopharyngeal carcinoma. China Oncol 2006;16:503–7.7.Walker GV, Ahmed S, Allen P, et al. Radiation-induced middle ear and mastoidopacification in skull base tumors treated with radiotherapy. Int J Radiat Oncol Biol Phys 2011; 81:e819-e823.8.Wang SZ, Wang WF, Guo M, et al. Analysis of anatomic factors controlling the morbidityof radiation-induced otitis media with effusion. Radiotherapy and Oncology 2007; 85: 463–468.9.Wang SZ, Li J, Miyamoto CT, et al. A study of middle ear function in the treatment ofnasopharyngeal carcinoma with IMRT technique. Radiotherapy and Oncology 2009;93:530-3.10.Hsin CH, Chen TH, Young YH, Liu WS. Comparison of otologic complications betweenintensity-modulated and two-dimensional radiotherapies in nasopharyngeal carcinoma patients. Otolaryngology-Head and Neck Surgery 2010; 143: 662-8.11.Bhandare N, Antonelli PJ, Morris CG, Malayapa RS, Mendenhall WM.Ototoxicity after radiotherapy for head and neck tumors. Int J Radiat Oncol Biol Phys 2007;67:469-79.12.Petsuksiri J, Sermsree A, Thephamongkhol K, et al. Sensorineural hearing loss afterconcurrent chemoradiotherapy in nasopharyngeal cancer patients. Radiat Oncol 2011; 6:19.13.Pacholke HD, Amdur RJ, Schmalfuss IM, Louis D, Mendenhall WM. Contouring themiddle and inner ear on radiotherapy planning scans. Am J Clin Oncol 2005; 28:143-147. 14.Pan CC, Eisbruch A, Lee JS, Snorrason RM, Ten Haken RK, Kileny PR. Prospective studyof inner ear radiation dose and hearing loss in head-and-neck cancer patients. Int J Radiat Oncol Biol Phys 2005; 61:1393-1402.15.Low WK, Burgess R, Fong KW, Wang DY. Effect of radiotherapy on retro-cochlearauditory pathways. Laryngoscope 2005; 115:1823-1826.16.Chen WC, Jackson A, Budnick AS, et al. Sensorineural hearing loss in combined modalitytreatment of nasopharyngeal carcinoma. Cancer 2006; 106 (Suppl. 4):820-829.17.Bhandare N, Jackson A, Eisbruch A, Radiation therapy and hearing loss. Int J Radia OncolBiol Phy 2010; 76:S50-7.18.Zuur CL, Simis YJ, Lamers EA, et al. Risk factors for hearing loss in patients treated withintensity-modulated radiotherapy for head-and-neck tumors. Int J Radiat Oncol Biol Phys 2009; 74:490-6.19.Parashar B, Kuo C, Kutler D, et al. Importance of contouring the cervical spine levels ininitial intensity-modulated radiation therapy radiation for head and neck cancers: implications for re-irradiation. J Cancer Res Ther 2009; 5:36-40.20.Kong FM, Ritter T, Quint DJ, et al. Consideration of dose limits for organs at risk ofthoracic radiotherapy: atlas for lung, proximal bronchial tree, esophagus, spinal cord, ribs, and brachial plexus. Int J Radiat Oncol Biol Phys 2011; 81:1442-1457.21.Leung WM, Tsang NM, Chang FT, Lo CJ. Lhermitte's sign among nasopharyngeal cancerpatients after radiotherapy. Head Neck 2005; 27:187-194.22.Harari PM, Song S, Tome WA. Emphasizing Conformal Avoidance vs. Target Definitionfor IMRT Treatment Planning in Head and Neck Cancer. Int J Radiat Oncol Biol Phys 2010; 77: 950–958.23.Ezhi M, Starkschall G, Mohan R, Cox J, Komski R. Validation of a model-basedsegmentation approach to propagating normal anatomic regions of interest through the 10 phases of respiration. Int J Radiat Oncol Biol Phys 2008; 71: 900-6.24.Weiss W, Wijesooriya K, Ramakrishnan V, Keall P. Comparison of intensity-modulatedradiotherapy planning based on manual and automatically generated contours using deformable image registration in four-dimensional computed tomography of lung cancerpatients. Int J Radiat Oncol Biol Phys 2008; 70: 572–581.25.Qatarneh SM, Noz ME, Hyodymaa S, Maguire GQ, Kramer EL, Crafoord J. Evaluation ofa segmentation procedure to delineate organs for use in construction of a radiation therapyplanning atlas. Int J Med Inform 2003; 69: 39-55.26.Pak D, Vineberg K, Feng F, Ten Haken RK, Eisbruch A. Lhermitte sign after chemo-IMRTof head-and-neck cancer: incidence, doses, and potential mechanisms. Int J Radiat Oncol Biol Phys 2012; 83(5):1528-33.27.Uhl M, Sterzing F, Habl G, et al. CT-myelography for high-dose irradiation of spinal cordand paraspinal tumors with helical tomotherapy: revival of an old tool. Strahlenther Onkol 2011; 187:416-20.28.Brouwer CL, Steenbakkers RJ, Van den Heuvel E, et al. 3D Variation in delineation ofhead and neck organs at risk. Radiat Oncol 2012; 7:32.29.Schreibmann E, Fox T. Towards automated planning for unsealed source therapy. J ApplClin Med Phys 2012; 13:3789.30.Urbano TG, Clark CH, Hansen VN, et al. Intensity Modulated Radiotherapy (IMRT) inlocally advanced thyroid cancer: Acute toxicity results of a phase I study. Radiother Oncol 2007; 85:58-63.31.Zwicker F, Roeder F, Hauswald H, et al. Reirradiation with intensity-modulatedradiotherapy in recurrent head and neck cancer.Head Neck 2011; 33:1695-702.32.Park SH, Park HC, Park SW, et al. Multi-institutional Comparison of Intensity ModulatedRadiation Therapy (IMRT) Planning Strategies and Planning Results for Nasopharyngeal Cancer. J Korean Med Sci 2009; 24:248-55.33.Eisbruch A, Marsh LH, Dawson LA, et al. Recurrences near base of skull after IMRT forhead-and-neck cancer: implications for target delineation in high neck and for parotid gland sparing. Int J Radiat Oncol Biol Phys 2004; 59:28-42.34.Claus F, Duthoy W, Boterberg T, et al. Intensity modulated radiation therapy fororopharyngeal and oral cavity tumors: clinical use and experience. Oral Oncol 2002;38:597-604.35.Chen AM, Li BQ, Farwell DG, Marsano J, Vijayakumar S, Purdy JA. Improved dosimetricand clinical outcomes with intensity-modulated radiotherapy for head-and-neck cancer of unknown primary origin. Int J Radiat Oncol Biol Phys 2011; 79:756-62.36.Dirix P, Nuyts S. Evidence-based organ-sparing radiotherapy in head and neck cancer.Lancet Oncol 2010; 11:85-91.37.Strigari L, Benassi M, Arcangeli G, Bruzzaniti V, Giovinazzo G, Marucci L. A novel doseconstraint to reduce xerostomia in head-and-neck cancer patients treated with intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 2010; 77:269-76. 38.Zhang Y, Lin J, Zhou W, Tang J, Liao Y. Dosimetric verification and clinical efficacyof intensity modulated radiotherapy in nasopharyngeal carcinoma. Zhong Nan Da Xue Xue Bao Yi Xue Ban 2009;34: 879-8539.van Rij CM, Oughlane-Heemsbergen WD, Ackerstaff AH, Lamers EA, Balm AJ, RaschCR. Parotid gland sparing IMRT for head and neck cancer improves xerostomia related quality of life. Radiat Oncol 2008; 3:41.40.Huang K, Xia P, Chuang C, Weinberg V, et al. Intensity-modulated chemoradiation fortreatment of stage III and IV oropharyngeal carcinoma: the University of California-SanFrancisco experience. Cancer 2008; 113:497-507.41.Seung S, Bae J, Solhjem M, et al. Intensity-modulated radiotherapy for head-and-neckcancer in the community setting. Int J Radiat Oncol Biol Phys 2008; 72:1075-81.42.Bhide S, Clark C, Harrington K, Nutting CM. Intensity Modulated Radiotherapy ImprovesTarget Coverage and Parotid Gland Sparing When Delivering Total Mucosal Irradiation in Patients With Squamous Cell Carcinoma of Head and Neck of Unknown Primary Site Med Dosim 2007; 32:188-95.43.Guerrero Urbano MT, Clark CH, et al. Target volume definition for head and neck intensitymodulated radiotherapy: pre-clinical evaluation of PARSPORT trial guidelines. Clin Oncol (R Coll Radiol) 2007; 19:604-13.44.Lee NY, de Arruda FF, Puri DR, et al. A comparison of intensity-modulated radiationtherapy and concomitant boost radiotherapy in the setting of concurrent chemotherapy for locally advanced oropharyngeal carcinoma. Int J Radiat Oncol Biol Phys 2006; 66:966-74.45.Braam PM, Terhaard CH, Roesink JM, Raaijmakers CP. Intensity-modulatedradiotherapy significantly reduces xerostomia compared with conventional radiotherapy.Int J Radiat Oncol Biol Phys 2006; 66:975-80.46.de Arruda FF, Puri DR, Zhung J, et al. Intensity-modulated radiation therapy for thetreatment of oropharyngeal carcinoma: the Memorial Sloan-Kettering Cancer Center experience. Int J Radiat Oncol Biol Phys 2006; 64:363-73.47.Kwong DL, Pow EH, Sham JS, et al. Intensity-modulated radiotherapy for early-stagenasopharyngeal carcinoma: a prospective study on disease control and preservation of salivary function. Cancer 2004; 101:1584-93.48.Chao KS, Ozyigit G, Blanco AI, et al. Intensity-modulated radiation therapy fororopharyngeal carcinoma: impact of tumor volume. Int J Radiat Oncol Biol Phys 2004;59:43-50.49.Parliament MB, Scrimger RA, Anderson SG, et al. Preservation of oral health-relatedquality of life and salivary flow rates after inverse-planned intensity- modulated radiotherapy (IMRT) for head-and-neck cancer. Int J Radiat Oncol Biol Phys 2004;58:663-73.50.van Asselen B, Dehnad H, Raaijmakers CP, Roesink JM, Lagendijk JJ, Terhaard CH. Thedose to the parotid glands with IMRT for oropharyngeal tumors: the effect of reduction of positioning margins. Radiother Oncol 2002; 64:197-204.51.Lee N, Xia P, Quivey JM, et al. Intensity-modulated radiotherapy in the treatment ofnasopharyngeal carcinoma: an update of the UCSF experience. Int J Radiat Oncol Biol Phys 2002; 53:12-22.52.Sultanem K, Shu HK, Xia P, et al. Three-dimensional intensity-modulated radiotherapy inthe treatment of nasopharyngeal carcinoma: the University of California-San Francisco experience. Int J Radiat Oncol Biol Phys 2000; 48:711-22.53.Wu Q, Manning M, Schmidt-Ullrich R, Mohan R. The potential for sparing of parotids andescalation of biologically effective dose with intensity-modulated radiation treatments of head and neck cancers: a treatment design study. Int J Radiat Oncol Biol Phys 2000;46:195-205.54.Butler EB, Teh BS, Grant WH 3rd, et al. Smart (simultaneous modulated acceleratedradiation therapy) boost: a new accelerated fractionation schedule for the treatment of headand neck cancer with intensity modulated radiotherapy. Int J Radiat Oncol Biol Phys 1999;45:21-32.55.Grégoire V, Jeraj R, Lee JA, O'Sullivan B. Radiotherapy for head and neck tumours in2012 and beyond: conformal, tailored, and adaptive? Lancet Oncol 2012; 13:e292-300. 56.Scrimger R. Salivary gland sparing in the treatment of head and neck cancer. Expert RevAnticancer Ther 2011; 11:1437-48.57.Anand AK, Jain J, Negi PS, et al. Can dose reduction to one parotid gland preventxerostomia?--A feasibility study for locally advanced head and neck cancer patients treated with intensity-modulated radiotherapy. Clin Oncol (R Coll Radiol) 2006; 18:497-504. 58.Faggiano E, Fiorino C, Scalco E, et al. An automatic contour propagation method to followparotid gland deformation during head-and-neck cancer tomotherapy. Phys Med Biol 2011;56:775-91.59.Feng M, Demiroz C, Karen A, et al. Normal Tissue Anatomy for Oropharyngeal Cancer:Contouring Variability and Its Impact on Optimization. Int J Radiat Oncol Biol Phys, 2012;84:e245-9.60.Mukesh M, Benson R, Jena R, et al. Interobserver variation in clinical target volume andorgans at risk segmentation in post-parotidectomy radiotherapy: can segmentation protocols help? The British Journal of Radiology 2012; 85: e530–e536.61.Loo SW, Martin WM, Smith P, Cherian S, Roques TW. Interobserver variation in parotidgland delineation: a study of its impact on intensity-modulated radiotherapy solutions witha systematic review of the literature. Br J Radiol 2012; 85:1070-7.。
常见肿瘤放疗靶区勾画(2)——⿐咽癌(1)导读进⼊21世纪以来,调强放射治疗(intensity modulated radiation therapy, IMRT)成为治疗⿐咽癌的主流放疗技术。
IMRT成功治疗⿐咽癌的三个主要环节是:靶区的准确勾画,精确的计划设计,精确照射。
其中靶区的准确勾画是前提条件,⼀旦靶区勾画出了问题,后⾯的两个环节都会相应出问题,⿐咽癌的局部控制率就会随之下降。
局部失败后导致继发的远处转移率增加,总⽣存率下降;局部失败后的挽救治疗效果差,后遗症发⽣率⾼,严重影响患者的⽣活质量。
因此,有必要系统掌握靶区勾画的相关知识。
1⿐咽癌靶区勾画的影像学要求1强调治疗前要有完整的影像学检查资料,MRI是⿐咽癌靶区勾画⾸选的影像学⼯具,多序列、多相位扫描,平扫+增强都要做。
靶区勾画者要有扎实的影像解剖知识和读⽚技能。
2⿐咽原发肿瘤GTV勾画细节2建议采⽤CT/MRI融合技术勾画GTV,强调不能⽚⾯依赖MRI,要衡量融合误差,综合CT和MRI的所有信息,对于显⽰肿瘤侵犯引起的成⾻性改变,CT优于MRI。
3⿐咽原发肿瘤CTV勾画原则与细节3强调建⽴统⼀的CTV勾画指南的必要性,介绍CTV勾画指南的数据来源,以实际的T2 和T4期⿐咽癌病例显⽰CTV的勾画范围。
2颈部淋巴结CTV勾画原则与细节4列举了⼏个代表性的淋巴结影像学分区和复旦⼤学附属肿瘤医院⼀系列针对⿐咽癌淋巴结转移分布规律的研究,总结了淋巴结分布规律,规定了根据淋巴结分期⽽个体化设定CTV的总体原则,特别指出了II区淋巴结上界、茎突后间隙(VIIb)、咽后淋巴结、IIa淋巴结外侧界、V区淋巴结后界、腮腺淋巴结(VIII区)、IVb区淋巴结的勾画细节以及勾画依据。
(王孝深欧丹)动动⼿指,关注放疗青咖汇(责任编辑:包永兴)。
鼻咽癌总结之二:靶区勾画篇(2)1.1 CTV定义1.11 国内北派、南派少部分:无CTV1、CTV2,只有一个CTV,其范围相当于CTV2范围,剂量为60Gy。
1.12 中肿极大部分:区分肿瘤侵犯高危区域和低危区域分为CTV1(60Gy)、CTV2(54Gy)。
1.2 CTV 的勾画1.21 北美、国内北派、中肿少部分:无论GTV大小、侵犯范围情况,根据鼻咽癌侵犯危及解剖概率,包全所有危及解剖,特别是颅底诸孔、翼腭窝。
1.22 中肿大部分:以GTV为基准,根据肿瘤对数与距离呈反比的观点,界定距离肿瘤1.6-2.0cm区域为危及区域即CTV。
2. CTV1、CTV2界定事项:2.1 CTV1为GTV上下外扩6mm,两侧外扩6-10mm,前缘扩7-10mm,后缘扩3-5mm。
CTV2的扩法与CTV1类似,但可略小。
CTV1与GTV需间隔一定距离,而CTV2与CTV1可以紧贴,特别是极贴近脑干这样的一级危及器官。
如果斜坡骨质无受侵,CTV1紧贴皮质,CTV2包一半髓质,如斜坡皮质受侵,CTV1包一半髓质CTV2包皮质后缘。
CTV1和CTV2前界在鼻腔、鼻中隔处不按GTV轮廊内凹而应向鼻腔方向外凸;到鼻底处近口咽部,即硬腭下缘处应适当往GTV方向回缩,减少口腔粘膜反应。
如果两侧无侵犯翼内肌、翼外肌,CTV2两侧缘至卵圆孔外缘。
CTV1和CTV2到蝶窦部位应整体向前方移,即减少后缘增加前缘,从矢状位看呈倾斜向前势。
2.2 从乳突尖出现平面,二腹肌出现,即Ⅱ区淋巴结出现开始勾画颈部淋巴引流区。
CTV2双侧均向后伸展包括胸锁乳突肌下间隙;2.3 双侧腮腺深叶应包在CTV2内,而口咽前间隙无需包括在内。
2.4 CTV2不常规包括Ⅰ区,根据2010年ⅠB区预防照射共识,其适应症:Ⅱa区淋巴结融合或者≥3cm,ⅠB区淋巴结阳性,同侧颈部≥3个区域阳性,超过鼻腔后1/3侵犯,侵犯口腔或软腭或腮腺或颌下腺。
2.5 在舌骨水平,咽后淋巴结消失平面,CTV2左右分开而且后界向后延至斜方肌前缘包括Ⅴa区淋巴结(新观点:GTV(包括咽后阳性淋巴结)向下2cm,即7个CT层面后左右分开CTV2,但CTV2需包全咽后外侧间隙);2.6 一侧或双侧颈淋巴结阴性,CTV2可以只需包括一侧或双侧Ⅱ、Ⅲ、Ⅴa区淋巴结,若有阳性淋巴结需扩大至同侧Ⅳ、Ⅴb区淋巴结(胸锁关节上2cm);2.7 胸锁乳突肌本身一般其厚度1/3~1/2包括在CTV2,如果其有明确的侵润则包括其厚度1/2~全部。
鼻咽癌知识要点局部侵犯:前:鼻腔、翼腭窝、上颌窦,并可进一步侵犯眼眶;后:颈椎体、椎管;上:颅底结构,如筛窦、蝶窦、海绵窦、枕骨体、硬脑膜、颞叶下:口咽各壁;外:咽旁间隙、颞下窝,并可通过咽鼓管侵犯内耳、中耳、外耳;淋巴引流:最常见转移至咽后、颈深、颈后淋巴结,基本遵循II区III区 IV区 Va区 Vb区(跳跃性转移少见);刻下淋巴结转移几乎为0,颌下淋巴结转移<4%。
咽后淋巴结转移时,同侧II、III区淋巴结转移风险明显增加。
MRI淋巴结转移标准:1、短径≥10mm(咽后淋巴结≥5mm或任何可见咽后淋巴结内侧组);2、中央坏死、环状强化;3、淋巴结包膜受侵(特征包括:淋巴结边缘不规则强化、周边脂肪间隙消失、淋巴结相互融合);4、同一高危区域≥3个淋巴结,其中1个短径≥8mm(高危区定义:N0者,II 区;N+者,N+区下一区)。
靶区勾画:距离+结构≥109个肿瘤细胞,直径≥1cm,肉眼可见,为肿瘤密集区,GTV 66-70Gy;106个肿瘤细胞,显微镜可见,为高危区,CTV60-66Gy;150-54Gy。
<106个肿瘤细胞,难发现,为低危区,CTV2CTV1由GTV向前、上、下、双侧方向各外扩0.5-1cm(上下在GTV外两层; 周围有重要器官可外扩0.2-0.3cm),向后外扩0.2-0.3cm。
包括鼻咽部全部粘膜层及下方0.5cm;同侧口咽。
CTV2向前、上、下、双侧方向各外扩0.5-1cm,向后外扩0.2-0.3cm 鼻咽部:由CTV1(周围有重要器官可外扩0.2-0.3cm)。
包括鼻咽部全部粘膜层及下方0.5cm;对侧口咽;双侧卵圆孔。
颈部:N+所在区域及其向下1-2个颈区。
Ib区预防照射指征:1、Ib区N+;2、IIa区N+≥3cm 或侵及下颌下腺;3、肿瘤侵犯鼻腔、口咽、软腭等部位。
斜坡:明显侵犯时,CTV1包括全髓质, CTV2包括全斜坡未侵犯时, CTV1包括椎前肌,CTV2包括髓质前广泛颅底受侵:CTV1包括整个颅底。