脑死亡 米勒麻醉学第七版
- 格式:ppt
- 大小:2.13 MB
- 文档页数:32

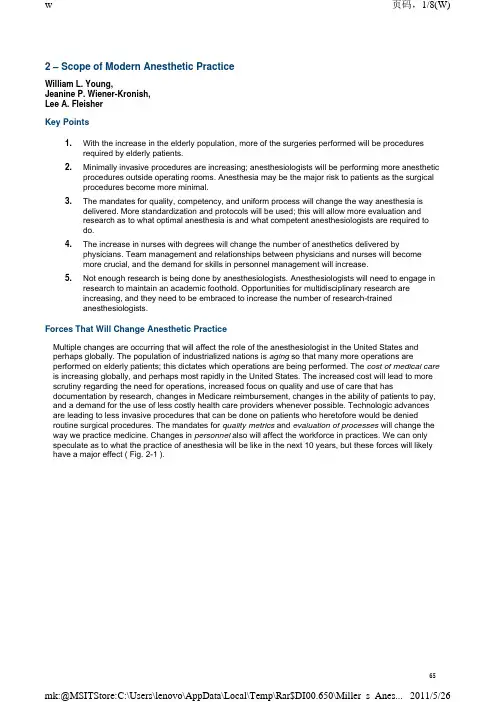
2 – Scope of Modern Anesthetic PracticeWilliam L. Young,Jeanine P. Wiener-Kronish,Lee A. FleisherKey Points1.With the increase in the elderly population, more of the surgeries performed will be proceduresrequired by elderly patients.2.Minimally invasive procedures are increasing; anesthesiologists will be performing more anestheticprocedures outside operating rooms. Anesthesia may be the major risk to patients as the surgicalprocedures become more minimal.3.The mandates for quality, competency, and uniform process will change the way anesthesia isdelivered. More standardization and protocols will be used; this will allow more evaluation andresearch as to what optimal anesthesia is and what competent anesthesiologists are required todo.4.The increase in nurses with degrees will change the number of anesthetics delivered byphysicians. Team management and relationships between physicians and nurses will becomemore crucial, and the demand for skills in personnel management will increase.5.Not enough research is being done by anesthesiologists. Anesthesiologists will need to engage inresearch to maintain an academic foothold. Opportunities for multidisciplinary research areincreasing, and they need to be embraced to increase the number of research-trainedanesthesiologists.Forces That Will Change Anesthetic PracticeMultiple changes are occurring that will affect the role of the anesthesiologist in the United States and perhaps globally. The population of industrialized nations is aging so that many more operations are performed on elderly patients; this dictates which operations are being performed. The cost of medical care is increasing globally, and perhaps most rapidly in the United States. The increased cost will lead to more scrutiny regarding the need for operations, increased focus on quality and use of care that has documentation by research, changes in Medicare reimbursement, changes in the ability of patients to pay, and a demand for the use of less costly health care providers whenever possible. Technologic advances are leading to less invasive procedures that can be done on patients who heretofore would be denied routine surgical procedures. The mandates for quality metrics and evaluation of processes will change the way we practice medicine. Changes in personnel also will affect the workforce in practices. We can only speculate as to what the practice of anesthesia will be like in the next 10 years, but these forces will likely have a major effect ( Fig. 2-1 ).Figure 2-1 Changing scope and settings of anesthesia and perioperative medicine. A,The Cure of Folly, by Hieronymus Bosch (c. 1450-1516), depicting the removal of stones in the head, thought to be a cure for madness. B, Friedrich Esmarch amputating with the use of anesthesia and with antisepsis. Woodcut from Esmarch's Handbuch der KriegschirurgischenTechnik (1877). C, Harvey Cushing performing an operation, with the Harvey Cushing Society observing, 1932. D and E, Placement of deep brain stimulator for the treatment of Parkinson's disease using a real-time magnetic resonance imaging technology (MR fluoroscopy). The procedure takes place in the MR suite of the radiology department. The patient isanesthetized (D) and moved into the bore of the magnet (E). F and G, A sterile field is created for intracranial instrumentation(F), and placement of electrodes is done using real-time guidance (G). (A, Courtesy of Museo del Prado, Madrid; B, courtesyof Jeremy Norman & Co, Inc; C, photograph by Richard Upjohn Light [Boston Medical Library]; D-G, courtesy of Paul Larson, MD, UCSF/SF Veterans Administration Medical Center.)Aging of SocietyWith the aging of the population and improvements in anesthetic and surgical methods, the fraction of the elderly population undergoing surgical procedures is increasing in the United States (see Chapter 71 ). Use of surgical services in older patients is not unexpectedly higher than in younger patients. In the Centers for Disease Control and Prevention report of inpatient hospitalizations for 2005, there were 45 million procedures performed on inpatients with a similar number of outpatient procedures. From 1995 through 2004, the rate of hip replacements for patients 65 years old and older increased 38%, and the rate of knee replacements increased 70%. There seems to be a direct correlation between age and use of surgical services.[1]Changes in Location of Care DeliveryBecause of the high costs to the insurance industry, the pressure to move less invasive surgical procedures to locations remote from the hospital setting will continue, frequently motivated by changes in reimbursement.[2] Providing anesthesia in ambulatory surgical settings and offices has increased dramatically over the last several decades (see Chapter 78 ). As procedures become less invasive than those currently performed in the operating room, they will be performed in procedure units. It will be important to determine the need for anesthesiologists to provide traditional anesthesia and moderate to deep levels of conscious sedation in these settings. Postoperative care has been shifted from the medical setting to the families, which may present difficulties in elderly patients. Anesthesiologists must be involved in determining which patients are appropriate candidates to have different procedures in these different locations of care, and the level of monitoring needed to perform these procedures safely.[3]Cost of Medical CareAs the cost of health care in the United States approaches 15% of the gross national product, there hasbeen increased interest in determining the factors that are increasing the costs, attempting to find methods to decrease the cost, and obtaining more valuable health care for the money spent. The primary driver of cost in the United States apparently is technical progress, as health care costs are increasing throughout the world, regardless of the insurance system. [4] [5] [6] The increase in elderly patients and patients with chronic disease in the population also is increasing health care costs.[7]The increase in cost has led to a movement to get more value for the money spent. Pay-for-performance programs have been created (i.e., rewarding medical care that is consistent with published evidence and not paying for care that is inconsistent with evidence). [8] [9] [10] The concept and reality of pay-for-performance programs has now moved to other countries, including the United Kingdom.[11]In the nonsurgical arena, the concept of pay-for-performance has been studied for several years. [12] [13] In addition to paying for performance, in the United States, there is increasing emphasis on not paying for “never” events, such as decubitus ulcers or urinary tract infections, unless they are present on admission to the hospital. Because of the role of anesthesiologists in the entire continuum of perioperative care, including postoperative intensive care and pain management, we have an opportunity to influence many of the practices that can be associated with poor outcomes and increased cost, but that traditionally have not been considered under our domain of care.Appropriate and timely administration of antibiotics has a significant impact on surgical site infection, but before the initiation of the Surgical Care Improvement Project, many anesthesiologists were arguing that control of antibiotics was not within their domain (see Chapter 5 ).[14] Anesthesiologists tend to focus on intraoperative cardiac arrests and other short-term outcomes, such as postoperative nausea and vomiting (see Chapters 33 and 86 [Chapter 33] [Chapter 86] ). Anesthesiologists will need to rethink this approach for other “never” conditions, such as urinary tract infections because they help determine the need for Foley catheters. Anesthesiologists and intensivists also can have a significant impact on the rate of ventilator-associated pneumonia. Some of these proposed measures, particularly the use of ventilator-associated pneumonia as a quality measure, have become quite controversial, however.[15] Pain is considered the fifth vital sign, and the management of postoperative pain is another area in which anesthesiologists can have a significant impact with respect to cost and potential interaction with other members of the hospital team. Process Assessment and Quality MetricsAnesthesiology was among the first professions to focus on reducing the risk of complications, and anesthesiologists were among the first groups to develop evidence-based guidelines and standards, as shown by the American Society of Anesthesiologists standards and practice parameters (see Chapter 5 ).[16] It will be important to continue to be involved in multidisciplinary approaches to surgical care. Examples where anesthesiologists were initially less involved include the Society of Thoracic Surgeons database and the National Surgical Quality Improvement Project. [17] [18] More recently, anesthesiologists have become involved in both groups, and the Society of Cardiovascular Anesthesiologists have begun discussions with the Society of Thoracic Surgeons. Anesthesiologists have been involved from an early stage in quality initiatives with the Institute of Healthcare Improvement and the Surgical Care Improvement Project.[19] Other quality measures that will have an impact on anesthesiologists include the new demand for metrics of competency, to be measured on a focused and an ongoing basis. Defining competency will demand that anesthesiologists adhere to more protocols, and that the concept of safe anesthesia be standardized. Rather than stifling medical innovation, standardization should be viewed as a mechanism for evaluating process and outcomes because comparisons cannot be made without standardization. Anesthesiologists will need to engage in creating quality and competency metrics, or these instruments will be created by others. This is an opportunity to formulate meaningful metrics that can be used in training physicians. Metrics also will be sought for nurse anesthetists and other health care professionals.Changing processes has become a cottage industry in medical care, with courses being offered on how to change behaviors and processes in medical care. These mandates offer the opportunity for more research as to whether changing processes leads to improved patient outcomes. These mandates also allow anesthesiologists to assume a leadership role in team management. For anesthesiologists to accomplish this role, new skills need to be taught, including leadership training, improved communication skills, and improved relationship training.One advantage that anesthesiologists have is a long tradition and training in system approaches to care. These date back to the original checklists for the anesthesia machine. It is crucial that this skill set be disseminated beyond the intraoperative setting. Many ambulatory surgery centers are directed by anesthesiologists.Changes in PersonnelThere are approximately 250,000 active physicians, one third of whom are older than 55 years old and likely to retire by 2020.[20] Although in the 1960s enrollment in U.S. medical schools doubled, during the years 1980 through 2005, the enrollment has been flat. There has been zero growth in U.S. medical school graduates. In this same interval, the U.S. population grew by more than 70 million, creating a discrepancy between the supply of medical school graduates and the demand for physician-associated care.There also has been a significant increase in the number of women in medical schools, so that about 50% of medical students are now women.[21] Women tend not to work as many hours as their male counterparts, even when part-time status is taken into consideration.[22] Also, today's younger physicians choose to work fewer hours than their older counterparts, regardless of gender. [20] [23]There has been a steady use of international medical graduates; 60,000 international medical graduates are used as residents and constitute 25% of all residents in training.[24] There also has been an increase in the number of osteopath schools and schools offering advanced degrees in nursing, including training of nurses to become nurse anesthetists.[20] Given the increase in demand for medical care resulting from the increase in the geriatric population, this need will most likely be met by a combination of physicians and nonphysician personnel.ResearchIn terms of creative new investigations, most benchmarks suggest that the specialty of anesthesiology fares poorly compared with other disciplines, especially clinical disciplines. Using data gleaned from publicly available National Institutes of Health (NIH) sources, Reves[25] produced a troubling figure showing that anesthesiology ranked second to the last for many medical disciplines. The exact position on any such figure would undoubtedly change from year to year. The fact that U.S. anesthesiology inhabits the lowest quartile is of concern, however, because the external forces on the practice components are generally applicable to all specialties.NIH is not the only source of funding that may influence the specialty of anesthesiology; it is not even the largest portion of total research funding in the United States ( Fig. 2-2 ).[26] For all sources, there has been a doubling over the last decade in research expenditures for health and biomedical science research, although compared with biologically based disciplines, health services research is considerably less well funded. In anesthesiology journals, the fraction of non-U.S., original peer-reviewed articles has increased dramatically. This increase does not seem to be attributable directly to research support. Adjusted per capita, research support in Europe is only 10% of that in the United States, even though the proportion of scientists in the population is similar.[27]Figure 2-2 Research expenditures in the United States, 1994 to 2003, by funding source (see text).There is no a priori reason why anesthesiology should differ from any other medical specialty in terms of research output. In our opinion, it should excel. One might argue that practitioners at academic institutions might be better compared in terms of surgical versus medical specialties, but even in that comparison we fare poorly. One line of remedy is to develop clinician-scientist training programs further, such as the NIH T-32 model. This approach is limited, however, by the fact that selection of individuals entering the specialty has already occurred.One of the most exciting and promising developments in this regard has been the initiative by several programs in the United States to construct a special residency track that allows training for scientific independence to occur roughly in parallel with clinical residency training over the course of a 4-year track after internship. Such an approach recognizes that, to change the culture of the specialty, we must build from the ground up. Not all physicians who enter anesthesiology training go on to participate in the research/academic sector. Similar to other highly visible specialties, however, a sufficiently large cadre will be available to replenish those who leave active practice and further build up intellectual capital for future generations.One of the challenges in training is the inherent and increasingly diverse nature of the disciplines involved in any one-subject area. The term “interdisciplinary research” has become a tautology. Practically all new frontiers lie at the boundaries of established departmental or specialty divisions, which are largely a historical relic of 19th century or early 20th century conceptualizations. A look at any large institution's roster of academic divisions yields a growing number of “centers,” “programs,” and “institutes,” reflecting the ever-increasing interdependency of branches in biomedical knowledge. [28] [29] In basic science departments, with conjugate names such as “Physiology and Cellular Biophysics,” “Anatomy and Cell Biology,” “Biochemistry and Biophysics,” and “Cellular and Molecular Pharmacology,” it is becoming increasingly difficult to differentiate one faculty research program from another, solely on the basis of thetopics and methods of study. Although this differentiation is clearly less complicated for domains that do not involve patient care, the trend is evident. One might cite the example of endovascular surgery as anexample in the collision of science, technology, and historical boundaries of medical specialties.[30]Medical research is at one level original creative work that involves systemic investigation of medical phenomena with the direct or indirect consequence of improving health care. Activity that might be subsumed under “medical research” is scholarly synthesis of available data to generate new insights into phenomena. Scholarship that involves this synthesis is perhaps underappreciated and underemphasized. The most common type of publication in this category is the review article. Although often review articlesare written by the individuals performing the original research, this is neither a necessary nor a sufficient precondition for a meaningful review. Especially for clinically oriented reviews, a broad perspective on a particular clinical practice may not only be sufficient, but also desirable.Ramachandran[31] quotes Medwar: “An imaginative conception of what might be true is the starting point of all great discoveries in science.” Ramachandran says that if he would show the reader a talking pig, it is unlikely that he or she would respond: “Ah, but that's just one pig. Show me a few more, and then I might believe you!” In this regard, an unintended consequence of moving toward quantitative indices for impact of biomedical journals has led to the demise of the case report. The case report is just such a Medwarian “imaginative conception of what might be true.” It is also an ideal setting in which to perform a synthesis of available knowledge on a particular topic. Well-written and timely case reports can add significantly to the medical literature and provide an “early warning” function before laborious efforts are undertaken to conduct larger scale efforts to characterize a particular complication or phenomenon. Finally, case reports are“entry-level” scholarly activities that students, residents, and junior faculty can use as a stairstep to more complex modes of writing.An area of potentially increasing contribution of anesthesia and perioperative care is in the realization of clinical trials for efficacy of surgical therapy. It is not unreasonable to assume that reimbursement fordelivery of clinical care in the future may be increasingly tied to participation in some form of organized assessment of efficacy, such as a randomized controlled trial (e.g., the case of lung reduction surgery).[32] Such considerations are especially pertinent for procedures that are highly reimbursed, but controversial in terms of efficacy, as in the case of minimally symptomatic cerebrovascular diseases. [30] [33] Perverse incentives can drive clinical practice and influence expert opinion. In addition to insights into the delivery of perioperative medical care, anesthesiologists can help provide an “honest broker” function in such settings.In the clinical and policy research domain, anesthesiologists have an opportunity to study all aspects of surgical care. By joining or leading multidisciplinary teams, they can ask questions relevant to the patient undergoing surgery and not just undergoing anesthesia. Anesthesiologists must take leading roles inhelping to define best surgical practice.Why is it important that anesthesiology maintain the strongest possible profile in research and scholarly contributions to medical knowledge? Besides the intuitive sense that medical specialties must strive for advancing their domains, there is a strategic necessity of significant proactive involvement in scholarly and investigative pursuits. In the modern medical marketplace, physicians are not the only stakeholders in the delivery of health care. Physicians, particularly those in professorial tracks, traditionally conduct the bulk of investigative research, however. The advent of higher-level, doctoral degrees in nursing could significantly change this dynamic. The public that we serve, and the various governmental and institutional bodies that regulate health care delivery, should have a clear vision of our mission and approach.References1.. National Center for Health Statistics: Health, United States, 2007, with Chartbook on Trends in the Health of Americans. Available at /books/bv.fcgi?indexed=google&rid=healthus07.chapter.trend-tables20072.. Ruther MM, Black C: Medicare use and cost of short-stay hospital services by enrollees with cataract, 1984. Health Care Financ Rev 1987; 9:91-99.3.. Fleisher LA, Pasternak LR, Herbert R, et al: Inpatient hospital admission and death after outpatient surgery in elderly patients: Importance of patient and system characteristics and location of care. ArchSurg 2004; 139:67-72.4.. Cutler DM: Your Money or Your Life: Strong Medicine for America's Health Care System. New York, Oxford University Press, 2004.5.. Bodenheimer T: High and rising health care costs, part 2: Technologic innovation. Ann InternMed 2005; 142:932-937.6.. Mongan JJ, Ferris TG, Lee TH: Options for slowing the growth of health care costs. N Engl JMed 2008; 358:1509-1514.7.. Thorpe KE: The rise in health care spending and what to do about it. Health Aff (Millwood) 2005; 24:1436-1445.8.. Rosenthal MB: Nonpayment for performance? Medicare's new reimbursement rule. N Engl JMed 2007; 357:1573-1575.9.. Shortell SM, Rundall TG, Hsu J: Improving patient care by linking evidence-based medicine and evidence-based management. JAMA 2007; 298:673-676.10.. Lee TH: Pay for performance, version 2.0?. N Engl J Med 2007; 357:531-533.11.. Campbell S, Reeves D, Kontopantelis E, et al: Quality of primary care in England with the introduction of pay for performance. N Engl J Med 2007; 357:181-190.12.. Lindenauer PK, Remus D, Roman S, et al: Public reporting and pay for performance in hospital quality improvement. N Engl J Med 2007; 356:486-496.13.. Centers for Medicare and Medicaid Services: Medicare Program; Hospital Outpatient Prospective Payment System and CY 2007 Payment Rates; CY 2007 Update to the Ambulatory Surgical Center Covered Procedures List; Medicare Administrative Contractors; and Reporting Hospital Quality Data for FY 2008 Inpatient Prospective Payment System Annual Payment Update Program—HCAHPS Survey, SCIP, and Mortality, Vol 71. Dept of Health and Human Services. Federal Register, 2006.14.. Griffin FA: Reducing surgical complications. Jt Comm J Qual Patient Saf 2007; 33:660-665.15.. Klompas M, Kulldorff M, Platt R: Risk of misleading ventilator-associated pneumonia rates with use of standard clinical and microbiological criteria. Clin Infect Dis 2008; 46:1443-1446.16.. Arens JF: A practice parameters overview. Anesthesiology 1993; 78:229-230.17.. Khuri SF: The NSQIP: A new frontier in surgery. Surgery 2005; 138:837-843.18.. Tong BC, Harpole Jr DH: Audit, quality control, and performance in thoracic surgery: A North American perspective. Thorac Surg Clin 2007; 17:379-386.19.. QualityNet: Available at /dcs/ContentServer?pagename=QnetPublic/Page/QnetHomepage20.. Salsberg E, Grover A: Physician workforce shortages: Implications and issues for academic health centers and policymakers. Acad Med 2006; 81:782-787.21.. AAMC Data Book: U.S. Medical School Women Applicants, Accepted Applicants, and Matriculants.Washington, DC, Association of American Medical Colleges, 2005.22.. Heiligers PJ, Hingstman L: Career preferences and the work-family balance in medicine: Gender differences among medical specialists. Soc Sci Med 2000; 50:1235-1246.23.. Jovic E, Wallace JE, Lemaire J: The generation and gender shifts in medicine: An exploratory survey of internal medicine physicians. BMC Health Serv Res 2006; 6:55.24.. Graduate medical education. JAMA 2005; 294:1129-1143.25.. Reves JG: We are what we make: Transforming research in anesthesiology.Anesthesiology 2007; 106:826-835.26.. Moses 3rd H, Dorsey ER, Matheson DH, et al: Financial anatomy of biomedical research.JAMA 2005; 294:1333-1342.27.. Philipson L: Medical research activities, funding, and creativity in Europe: Comparison with research in the United States. JAMA 2005; 294:1394-1398.28.. Columbia University Medical Center. Academic and Clinical Departments, Centers andInstitutions: Available at /depts/200829.. University of California San Francisco. Department Chairs, ORU Directors, and Assistants: Available at /listbuilder/chairs_dirs_assts.htm 200830.. Fiehler J, Stapf C: ARUBA—beating natural history in unruptured brain AVMs by intervention.Neuroradiology 2008; 50:465-467.31.. Ramachandran VS, Blakeslee S: Phantoms in the Brain: Probing the Mysteries of the Human Mind . New York, William Morrow, 1998.32.. Centers for Medicare and Medicaid Services: Lung Volume Reduction Surgery (LVRS). Available at /MedicareApprovedFacilitie/LVRS/List.asp 200833.. Mathiesen T: Arguments against the proposed randomised trial (ARUBA). Neuroradiology 2008; 50:469-471.。
人体死亡的判定关系到人的生死,而“人命至重,贵于千金”。
随着社会的发展和医学的进步,人体死亡的判定标准也在演变,这种演变既是一个科学技术问题,又蕴含着伦理问题。
脑死亡标准的提出和实施是一个科学技术问题,而应不应该实施和如何实施就是一个伦理问题(实质伦理和程序伦理),后者即实施脑死亡的伦理价值和应遵循的伦理原则。
一、死亡标准的演变死亡标准,亦即人们用以衡量与判断死亡的标准或尺度,它随着社会的发展和医学科学的进步在不断地演变。
人类社会的早期以呼吸停止作为判断死亡的标准,后来演变为以心肺功能停止(即心跳、呼吸停止)为死亡的标志,后者已沿袭了数千年之久。
但是,现代大量的临床实践证明,死亡不是生命的骤然停止,而是一个连续发展的过程。
在许多情况下,心搏骤停之时,脑、肝、肾等器官组织并未死。
当代人工维持心肺功能的技术和药物的应用,心跳、呼吸停止的病人经抢救也可以复苏,甚至治愈出院,这说明心肺功能停止不一定意味着死亡。
相反,某些实际上已丧失脑功能的病人,也能在生命维持装置的监护下,使心跳、呼吸持续很长时间,但作为人的自我意识或意识经验能力已经丧失。
因此,医学高技术的发展向传统的心肺功能停止的死亡标准提出了挑战,加之器官移植的迅速发展需要新鲜器官,于是促使国外的医学家纷纷探索新的死亡标准。
1968年召开的世界第22届医学大会上,美国哈佛大学医学院特设委员会提出了把“脑功能不可逆丧失”作为新的死亡标准,即将脑死亡确定为人的死亡标准,并提出判断的四条标准:①出现不可逆转的昏迷,即对外部的刺激和内部需要没有接受性和反应性;②自主的肌肉运动和自主呼吸消失;③诱导反射缺失;④脑电波平直。
以上四条标准还要求持续24小时观察及反复测试结果无变化,而且要排除低体温(<32.2℃)或刚服用过巴比妥类药物等中枢神经抑制剂的病例,即可宣布死亡。
[1]这个标准提出以后,开始也有争论:一是对脑电波平直24小时后能否可复的问题。
后来,美国做了大量的脑死亡病例统计表明,除少数服用过安定药物的病例外,脑死亡病人的脑电波在24小时后是不可复的,这就支持了脑死亡的哈佛标准。
麻醉科不可错过的8大经典书目什么?麻醉科医生也要看书?麻醉科医生看什么书?清晰记得研究生复试的时候,一个康复医学科的哥们问:“兄弟,你报考的是什么科?”我很得意的回答他:“麻醉科!”“什么?麻醉科也有研究生?!”我差点没接住他的下巴,但他肯定被我的白眼秒杀了。
多年后仍有不少人关心我说:“麻醉科医生还看什么书啊,不就打一针完事了么?”老少童鞋们,我现在严肃告诉你们,麻醉科医生不仅要看外科书,还要看内科书,以及其他麻醉学相关的书籍。
下面让我们来818 工作在神秘手术室不见天日的蒙面医生们需要看的麻醉书籍吧。
1 《麻醉》没错,我很正经推荐的第一本书是小说。
一针下去,一个家庭从此支离破碎,这样的事,可能发生在世界上每个地方,也可能发生在你我每个人身上,不要等到一切都无可挽回时,一个人痛苦流泪……本人亲身经历过两次全身麻醉,很庆幸,两次都没有发生麻醉事故,所以现在能够愉快的给大家推荐这本书籍。
麻醉并不是打一针那么简单,“只有小手术,没有小麻醉。
”这部最刻骨铭心的医情小说将深刻地告诉你麻醉的重要性及危险性。
正如作者渡边淳一所期望:这部小说,如果能够促成人们对医疗过失的反省,并为杜绝此类事故而敲响警钟的话,那无疑将是一大幸事。
麻醉小伙伴们,赶紧去阅读吧。
2 《米勒麻醉学》第 7 版《米勒麻醉学》是麻醉学领域公认的最经典、最权威的巨著,她从基本原理到高级亚专业常规,内容涵盖当代麻醉实践的所有范畴。
它会引导你解决学习和工作中面临的技术上、科学上以及临床上的问题。
毕业时导师给我的寄语:“要成为优秀的麻醉医师,你要多读《米勒麻醉学》。
”遗憾的是导师并没有送一套“葵花宝典”给我,因为他知道我早就有了,而且是6 册包装的。
(请不要问我为什么是6 册,你懂的。
)本人也有幸参加第8 版某章节某部分内容的翻译工作,据可靠消息称,汉化版《米勒麻醉学》第8 版将在近期横空出世,敬请期待哦。
未来的麻醉届大牛小牛们,《米勒麻醉学》你必须拥有。
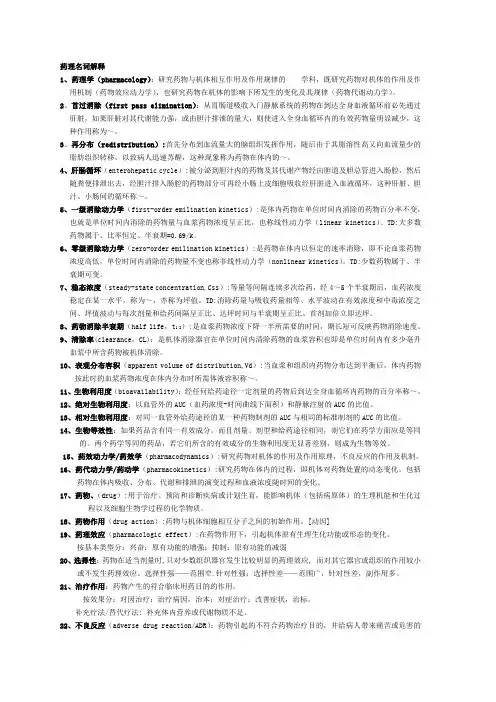
药理名词解释1、药理学(pharmacology):研究药物与机体相互作用及作用规律的学科,既研究药物对机体的作用及作用机制(药物效应动力学),也研究药物在机体的影响下所发生的变化及其规律(药物代谢动力学)。
2、首过消除(first pass elimination):从胃肠道吸收入门静脉系统的药物在到达全身血液循环前必先通过肝脏,如果肝脏对其代谢能力强,或由胆汁排泄的量大,则使进入全身血循环内的有效药物量明显减少,这种作用称为~。
3、再分布(redistribution):首先分布到血流量大的脑组织发挥作用,随后由于其脂溶性高又向血流量少的脂肪组织转移,以致病人迅速苏醒,这种现象称为药物在体内的~。
4、肝肠循环(enterohepatic cycle):被分泌到胆汁内的药物及其代谢产物经由胆道及胆总管进入肠腔,然后随粪便排泄出去,经胆汁排入肠腔的药物部分可再经小肠上皮细胞吸收经肝脏进入血液循环,这种肝脏、胆汁、小肠间的循环称~。
5、一级消除动力学(first-order emilination kinetics):是体内药物在单位时间内消除的药物百分率不变,也就是单位时间内消除的药物量与血浆药物浓度呈正比,也称线性动力学(linear kinetics)。
TD:大多数药物属于、比率恒定、半衰期=0.69/k。
6、零级消除动力学(zero-order emilination kinetics):是药物在体内以恒定的速率消除,即不论血浆药物浓度高低,单位时间内消除的药物量不变也称非线性动力学(nonlinear kinetics)。
TD:少数药物属于、半衰期可变。
7、稳态浓度(steady-state concentration,Css):等量等间隔连续多次给药,经4~5个半衰期后,血药浓度稳定在某一水平,称为~,亦称为坪值。
TD:消除药量与吸收药量相等、水平波动在有效浓度和中毒浓度之间、坪值波动与每次剂量和给药间隔呈正比、达坪时间与半衰期呈正比、首剂加倍立即达坪。
米勒麻醉学简要内容一、米勒麻醉学是什么嘿,小伙伴们,今天咱们来聊聊米勒麻醉学。
这米勒麻醉学啊,那可是麻醉学领域里相当厉害的一本书呢。
它就像是一个装满了麻醉知识的大宝库,里面啥都有。
从麻醉的基本概念到各种复杂的麻醉技术,从麻醉药物的特性到不同病人状况下的麻醉应对方法。
比如说啊,它会告诉你给一个老年人做麻醉和给一个年轻人做麻醉那可大不一样呢。
老年人身体机能下降,对麻醉药物的耐受程度可能就没年轻人那么好,在麻醉的剂量、种类选择上都得特别小心。
二、书中的重要概念1. 麻醉深度这可是个很关键的概念哦。
就像是你在控制一艘船的航行深度一样,麻醉深度也得刚刚好。
太浅了呢,病人在手术中会感觉到疼痛,那可就糟糕了;太深了呢,又可能会引发各种并发症。
它是通过观察病人的一些生理指标来判断的,像心率、血压、呼吸频率啥的。
2. 麻醉诱导这就像是麻醉的开场白。
是把病人从清醒状态带入麻醉状态的过程。
这个过程得做得稳稳当当的,就像飞机起飞一样,不能出岔子。
在这个阶段,麻醉医生要根据病人的体重、身体状况等因素准确地给予麻醉药物。
三、麻醉药物在米勒麻醉学中的体现1. 局部麻醉药局部麻醉药就像是一个个小小的麻醉士兵,它们只在身体的某个局部区域发挥作用。
比如说你牙疼去看牙医,牙医可能就会给你用局部麻醉药,让你的牙齿周围麻木起来,这样拔牙或者补牙的时候你就不会觉得疼啦。
在米勒麻醉学里,它会详细介绍不同局部麻醉药的作用机制、药效持续时间、适用范围等。
2. 全身麻醉药全身麻醉药可就更厉害了,它们能让整个身体都进入麻醉状态。
就像给全身的神经系统放个假一样。
但是呢,全身麻醉药也有很多种类,每种的特点都不一样。
有些麻醉药起效快,但是苏醒时间也长;有些则相反。
四、不同手术类型中的麻醉应用1. 外科手术麻醉外科手术各种各样,从小小的割阑尾手术到大型的心脏手术。
对于割阑尾这种相对简单的手术,麻醉的重点可能是保证病人在手术过程中没有疼痛,同时又能快速苏醒。
脑死亡标准相关内容与法条脑死亡是现代医学领域的一个重要概念,用于确定一个人是否已经完全失去了脑功能,不再具备自主呼吸和意识。
脑死亡被视为判断人的死亡的一个重要标准,对于器官移植、医疗护理和生命伦理学等方面都有重要的指导作用。
下面将详细介绍脑死亡标准的相关内容和法条。
1. 脑死亡标准的定义脑死亡是指脑干完全停止功能,包括对外界刺激的反应和对内环境的调节能力等。
这意味着大脑、脑干、小脑等重要脑部结构已经无法正常工作。
脑死亡被认为是多临床领域的确定死亡的一个标准。
2. 脑死亡的诊断标准根据世界卫生组织的建议,脑死亡的诊断需要满足以下条件:- 患者的原因明确且无法逆转,如颅脑损伤、脑出血等;- 患者完全昏迷且无自主呼吸;- 患者无脑干反射,包括眼球运动、瞳孔反射等;- 检测两次间隔一定时间的脑电图显示无电活动。
3. 脑死亡的法律地位脑死亡在许多国家都被法律所承认,且通常被视为确认人死亡的最可靠标准之一。
这一观点得到了许多跨国和国际组织的支持,如世界卫生组织、国际伦理学委员会等。
脑死亡判定的法律依据包括但不限于以下几个方面:3.1 法律文件和法规许多国家和地区制定了相关的法律文件和法规来规范脑死亡的判定和使用,以确保准确和可靠的判定过程。
这些法律文件通常对脑死亡的定义、诊断标准、脑死亡声明和器官移植等问题进行了明确规定。
3.2 法庭判例一些法庭在处理与脑死亡相关的案件时,明确了脑死亡作为确认人死亡的合法依据。
这些判例为脑死亡的法律地位提供了进一步的法律依据。
3.3 生命伦理学指南许多国际和国家级的伦理学组织都发布了关于脑死亡的指南,这些指南对脑死亡的定义、诊断标准和法律地位等进行了详细论述。
这些指南通常得到了更广泛的社会认可并反映在相关的法律制度中。
总结起来,脑死亡标准是现代医学界、法律界以及生命伦理学领域的一个重要概念。
它既有明确定义和诊断标准,也在许多国家和地区获得了明确的法律地位。
这为我们正确理解和应用脑死亡标准提供了重要的法律依据,并确保了合理和可靠的判定过程。
脑死亡的名词解释护理学导论脑死亡的名词解释及护理学导论悲痛的家属聚集在医院的病房前,望着躺在床上的亲人。
面色苍白,没有一丝生命的征兆。
医生走来,带着沉重的表情,告诉他们这个可怕的事实:亲人已经脑死亡。
脑死亡是一个充满争议和困惑的概念。
它指的是脑部完全且不可逆转的功能停止。
也就是说,大脑不再发挥作用,无法控制身体的生理功能,包括呼吸、血液循环和消化系统。
在医学领域,脑死亡被认为是死亡的一个标志。
然而,要理解脑死亡的概念和处理方法,并不是一件容易的事情。
要明白脑死亡的概念,首先需要理解大脑的功能。
大脑是人体掌控生理和认知功能的主要部位。
它负责意识、感知、记忆和思维等活动。
当大脑受到重大损伤或缺血时,会导致神经元无法正常工作,继而引发脑死亡。
诊断脑死亡的标准通常会根据不同地区和医疗机构的规定而有所不同。
但一般来说,医生会进行一系列测试来确认患者是否存在脑死亡。
这些测试包括神经系统检查、脑电图和血液流量测量等。
根据国际标准,至少要进行两次测试,间隔时间通常为6小时。
一旦确认了脑死亡,医生和医护人员将转向护理患者和支持家属的工作。
对于这些医护人员来说,护理脑死亡患者是一项重要且复杂的任务。
他们需要提供细致、周到的临终关怀,同时兼顾遵守法律和伦理的要求。
在护理脑死亡患者方面,有几个关键点需要注意。
首先是维持生命支持措施。
脑死亡患者的身体无法自主维持生理功能,需要依靠机械设备来保持呼吸和心跳。
医护人员负责监测和调整这些设备,确保患者的身体得到必要的支持。
其次是临终关怀。
尽管患者的大脑已经停止工作,但身体的其他器官仍然可以继续运作。
医护人员需要提供情感支持和疼痛缓解,以确保患者在最后时刻能够得到尊严和宽慰。
同时,他们也需要与患者的亲属沟通,帮助他们理解和接受这个过程。
对于医护人员来说,还有一个重要的职责是脑死亡器官移植的协调工作。
在某些情况下,脑死亡患者的身体器官可以用于供体器官移植,挽救其他患者的生命。
医护人员需要与器官捐献团队合作,确保移植程序的顺利进行,同时也需要与家属进行沟通和协商,以便得到他们的同意和支持。