医学英语阅读:英文病历
- 格式:docx
- 大小:37.71 KB
- 文档页数:3

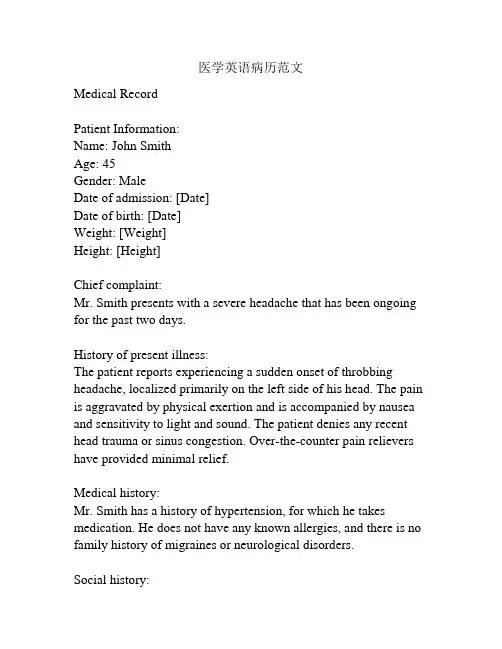
医学英语病历范文Medical RecordPatient Information:Name: John SmithAge: 45Gender: MaleDate of admission: [Date]Date of birth: [Date]Weight: [Weight]Height: [Height]Chief complaint:Mr. Smith presents with a severe headache that has been ongoing for the past two days.History of present illness:The patient reports experiencing a sudden onset of throbbing headache, localized primarily on the left side of his head. The pain is aggravated by physical exertion and is accompanied by nausea and sensitivity to light and sound. The patient denies any recent head trauma or sinus congestion. Over-the-counter pain relievers have provided minimal relief.Medical history:Mr. Smith has a history of hypertension, for which he takes medication. He does not have any known allergies, and there is no family history of migraines or neurological disorders.Social history:The patient is a smoker, consuming approximately 10 cigarettes per day. He drinks alcohol in moderation, primarily on social occasions. He denies any illicit drug use. His occupation involves long hours of computer work.Physical examination:On examination, the patient appears to be in mild distress due to the headache. His vital signs are within normal limits. Neurological examination reveals no focal deficits, and his cranial nerves appear to be intact. There is no evidence of meningeal irritation. His neck is supple, and there is no nuchal rigidity. The remainder of the physical examination is unremarkable. Laboratory tests:Blood tests, including a complete blood count and comprehensive metabolic panel, were performed. All results were within normal limits.Imaging studies:A brain MRI was ordered to rule out any structural abnormalities. The scan revealed no evidence of intracranial hemorrhage, mass, or other abnormalities.Assessment and plan:Mr. Smith is presenting with a severe headache consistent with a migraine without aura. He will be prescribed a triptan medication for acute management of his headache. He will also be counseled on lifestyle modifications, including smoking cessation and stress reduction techniques. A follow-up appointment will be scheduled in two weeks to evaluate the effectiveness of the treatment plan.Additionally, the patient is advised to seek immediate medical attention if his symptoms worsen or if he develops any new neurological symptoms.Signature: [Physician's Name]Date: [Date]。
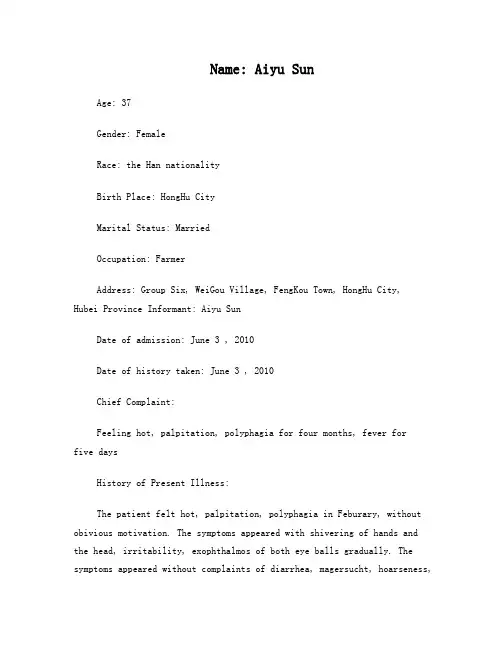
Name: Aiyu SunAge: 37Gender: FemaleRace: the Han nationalityBirth Place: HongHu CityMarital Status: MarriedOccupation: FarmerAddress: Group Six, WeiGou Village, FengKou Town, HongHu City,Hubei Province Informant: Aiyu SunDate of admission: June 3 , 2010Date of history taken: June 3 , 2010Chief Complaint:Feeling hot, palpitation, polyphagia for four months, fever forfive daysHistory of Present Illness:The patient felt hot, palpitation, polyphagia in Feburary, without obivious motivation. The symptoms appeared with shivering of hands and the head, irritability, exophthalmos of both eye balls gradually. The symptoms appeared without complaints of diarrhea, magersucht, hoarseness,blurred vision and so on. The patient did not go to receive any medical treatment. From April, the symptoms above became more severe, with powerless of limbs. The patient went to local hospital on 27th, April. Examination result: FT3>25pg/ml↑,FT4>8npg/dl↑,TSH<0.01uIU/ml↓;WBC6.11*109/L, N7.01*109/L; ALT 52u/L↑, AST 41u/L. The patient was diagnosed as “hyperthyroidism, cacergasia of liver”. The patient took Tapazole 5mg tid , propanolol, inosine, drugs for liver protection and WBC raising from then on. The symptoms described above was relievedafter taking these medicines. On 12nd, May, the bood routine was still normal: WBC 5.8*109/L, N 3.1*109/L. But five days ago, without obivious motivation, the patient had a pharynx ache, fever, which was highest at 38.7°C,with headache and catarrhus. The pati ent was diagnosed as “upper respiratory infection, hyperthyroidism, agranulemia” and gave antiinfection therapy. But the fever continued, the therapy effect was not well. The patient comes to our hospital today. The blood routine today is WBC 0.15*109/L↓, N0*109/L↓↓↓, and the outpatient department receives the patient to our ward as“hyperthyroidism, agranulemia”.During the course of disease, sleep and psyche were acceptable. Polyphagia lasted. Stool and urine were as usual. Physical strength descended. Weight was stable.Past History:General Health Status: good √moderate poorInfectious Disease: √no yes(if any, please write down date of onset, brief diagnostic and therapeutic, course )Typhoid fever Dysentery Malaria Schistosomiasis Leptospirosis Tuberculosis Epidemic hemorrhagic fever othersAllergic history: √no yes (clinical manifestation: allergen: ) Trauma and/or operation history: √no yes- 1 -Review of Symptoms:Respiratory system: √no yesRepeated pharyngeal pain:chronic cough: expectoration: Hemoptysis: asthma: dyspnea: chest pain:Circulatory system:√no yesPalpitation: exertional dyspnea: cyanosis: hemoptysis: Edema of lower extremities: chest pain: syncope: hypertension:Digestive system:√no yesAnorexia: dysphagia: sour regurgitation: eructation: nausea: Emesis: melena: abdominal pain: diarrhea: hematemesis: Hematochezia: jaundice:Urinary system:√no yesLumbar pain: urinary frequency: urinary urgency: dysuria: oliguria: Polyuria: retention of urine: incontinence of urine: hematuria: Pyuria: nocturia: puffy face:Hematopoietic system:√no yesFatigue: dizziness: gingival hemorrhage: epistaxis: subcutaneous hemorrhage:Metabolic and endocrine system:√no yesBulimia: anorexia: hot intolerance: hyperhidrosis: cold intolerance: Polydipsia: amenorrhea: tremor of hands: character change: Marked obesity: marked emaciation: hirsutism: alopecia: Hyperpigmentation: sexual function change: impotence: amenorrhea:Musculoskeletal system:√no yesMigrating arthralgia: arthralgia: artrcocele: arthremia: Dysarthrosis: myalgia: muscular atrophy:Neurological system:√no yesDizziness: headache: paresthesia: hypomnesis: Visual disturbance: Insomnia: somnolence: syncope: convulsion:Disturbance of consciousness: paralysis: vertigo:Personal history:Resident history in endemic disease area:√no yesSmoking: √no yes: about___yearsDrinking:√no occasional frequent: about____years average____ml/day Others:In April 2009, the patient was diagnosed as “polyp of vocal cord” in our hospital and got medicine thrapy.Menstrual history:Menarchal age: 21 years old duration__5__days/ interval_30_daysLast menstrual period: 2010.5.1 menopausal age: _13_years oldAmount of flow: small √moderate largedysmenorrheal: p resence √absenceMarital and obstetrical history:Married age: 21 years old pregnancy_4__times natural labour: 3 timesAbortion: 2 times premature labour: 0 times still birth: 0 timesDystocia and its course:0Family history:(pay attention to the infectious and hereditary disease related to the present illness)Father: √healthy ill: deceased cause:Mother: √healthy ill: deceased cause:Others: noPhysical ExaminationGeneral conditions:Temperature: 37.3°C pulse:88 times per minute (√regular irregular)Blood pressure:139/84mmHg respiration: 20 times per minute(√regular irregular) Development: √normal HypoplasiaNutrition: good √moderate poor cachexiaFacial expression: √normal acute chronic other( )Posture: √active semi-reclining position other ( )Mental status:√clear confusion somnolence delirium comaGait: √normal abnormal cooperation: √yes noSkin and mucosa:Color:√normal pale cyanosis stained yellow pigmentationrash:√no yes: (type: distribution: )subcutan eous hemorrhage: √no yes (type: distribution: )Hair distribution: √normal hypertrichosis oligotrichosisalopecial(location: ) Temperature and moisture: √normal cold warm dry moist dehydrationEdema: √no yes ( location and degree )Liver palmar : √no yes spider angioma:√no yes (location: )Others: noLymph nodes:enlargement of superfacial lymph node: √no yes (location and description: ) Head: without abnormityCranium: without abnormityEye: exophthalmos: exophthalmos of both eye ballseyelid: without descensusconjunctiva: without edemasclera: without stained yellowCornea: √normal abnormal ( od os )Pupil:√equally round and equal in size: unequal (od os )Pupil reflex: √normal delayed (od os ) absent (od os ) others:Ear: di scharge of external auditory canal:√normal (left right quality: ) Mastoid tenderness : no (left right )disturbance of rough hearing test: yes √noNose: flaring of alae nasi:√no yesstuffy discharge:√no yestenderness over paranasal sinuses: √no ye s(location: )Mouth: lip: redMucosa: without ulcerationTongue: stretched tongue is in the middleGum: nomalTonsil: Ⅰ°enlargement of both sidesPharynx: congestionsound: √normal hoarseness teeth: √normal absent carieNeck:neck rigidit y √no yes (distance between sternum and mandible:______transvers fingers) Carotid artery: √normal pulsation increased pulsation marked distention Trachea:√middle deviation (leftward rightward )Hepatojugular vein reflux: negativeThyroid: normal √enla rged bruitChest:Chest wall: √normal barrel chest prominence or retraction: (left right ) Precordial prominence: √no yespercussion pain over sternum:√no yesBreast: normalLung:Inspection: normal respiratory movementPalpation:vocal tactile fremitus: normalpleural rubbing sensation: √no yesSubcutaneous crepitus sensation:√no yesPercussion: √resonanc dullness Flatness Hyperresonance tympany lower border of lung: (detailed percussion in respiratory disease) midclavicular line : right:_6__cm left:_6__cmmidaxillary line: right:_8__cm left:_8__cmscapular line: right:_10__cm left:_10__cmAuscultation: breathing sound :√normal abnormalRales: √no yes (moist dry ) location:Heart:Inspection:apical pulsation:√normal unseen increase diffuse sSubxiphoid pulsation: √no yesLocation of apex beat:√normal shift (distance away from leftMCL___cm) Palpation:apical pulsation: √normal lifting apex impulse negative pulsationThrill:√no yes (location: ) phase:Percussion:relative dullness border:√Normal decreased absent increaseR(cm) line L(cm)2 Ⅱ 22 Ⅲ 43 Ⅳ 6Ⅴ8Distance between anterior median line and MCL 8.5cm Auscultation: heart rate: 88bpm rhythm: regularheart sound:√normal abnormalextra s ound:√no S3 gallop S4 opening snap:murmur: √no yes:location timing quality intensity transmission:effects of position:effects of respiration:P2 = A2 pericardial friction sound:√no yesPeripheral vascular sign: √no yes: paradoxical pulse pu lsus alternansWater hammer pulse capillary pulsationpulse deficit Pistol shot sound Duroziez sign Abdomen:Inspection: shape: √normal distention scaphoid frog-bellygastric pattern:√no yes visible intestinal peristalsis:√no yesabdominal vein v aricose: √no yes (direction: )operation scar:√no yesPalpation: √soft guarding (location: )Tenderness: √no yes (location: )rebound tenderness:√no yes (location: )fluctuation succussion splash:√no yesliver: can’t be touch ed under the ribsgallbladder: can’t be touched under the ribsMurphy sign: negativespleen: can’t be touched under the ribskidneys: kidney zones without Percussion painabdominal mass :can’t be touchedPercussion: liver dullness border: √normal decreased absen tUpper hepatic border locates at right midclavicularline5_intercostal spaceShift dullness: negativePain on percussion in costovertebral area:√no yes R L Auscultation: bowel sounds : √normal hyperperistalsis hypoperistalsis absenceVascular bruit :√no yes (location )Genital organ: √unexamined normal abnormalAnus and rectum:√unexamined normal abnormalSpine and extremities:Spine: √normal deformity (kyphosis lordosis scoliosis )Tenderness (location )Extremities: √normal arthremia(loc ation ) arthrocele (location ) Ankylosis (location ) aropachy Muscular tenderness(location ) muscular atrophy (location )Neurological system:Abdominal reflex++ cremasteric reflex- knee reflex++Kernig`s sign(R- L- ) Brudzinski`s sign:(R- L- ) Babinski sign (R- L- )Opphenheim sign(R- L- )Gordon sign (R- L- ) Lasegue sign (R- L- ) Others: noImportant exam results from out-patient service: X-ray number:no27th, April, local hospital: FT3>25pg/ml↑,FT4>8npg/dl↑,TSH<0.01uIU/ml↓;WBC 6.11*109/L, N 7.01*109/L;ALT 52u/L↑, AST 41u/L.12nd, May, local hospital: Blood-rt: WBC 5.8*109/L, N 3.1*109/L3rd, June, our hospital: Blood-rt: WBC 0.15*109/L↓, N0*109/L↓↓↓Summary of case history:1 Patient Aiyu Sun, female, 37 years old.2 Chief Complaint: Feeling hot, palpitation, polyphagia for four months, fever for five days3 Past History: General health status was moderate. In April 2009, the patient was diagnosed as “polyp of vocal cord” in our hospital and got medicine thrapy. The patient deny history of TB, HBV, schistosome infection, DM, HBP, heart diseases and other special diseases. The patient deny history of allergy, trama, surgery operation and blood transfusion.4 Physical Examination: T37.3°C P88 times per minute BP:139/84mmHg R: 20 times per minute. Normal development, moderate nutrition, active posture, clear mental status, cooperated examination. There is no yellow stained in the skin and mucosa. There is no enlargement of superfacial lymph nodes. Head shape and cranium are normal. There is exophthalmos of both eye balls. Both tonsils are Ⅰ°enlarged. Pharynx is congestion. No neck rigidity. Trachea is in the middle. Thyroid of both sides isⅡ°enlarged, without vascular bruit. Breathing sound of the lung is normal. And there is no rale. Heart rhythm is regular, without any obvious murmur at each valve zone. Abdomen shape is normal. Abdomen is soft, without tenderness or rebound tenderness. Liver and spleen can’t be touched under the ribs. Kidney zones are without percussion pain. Both hands are shivering. There is no edema of both lower limbs.5 exam results:27th, April, local hospital: FT3>25pg/ml↑,FT4>8npg/dl↑,TSH<0.01uIU/ml↓;WBC 6.11*109/L,N 7.01*109/L; ALT 52u/L↑, AST 41u/L.12nd, May, local hospital: Blood-rt: WBC 5.8*109/L, N 3.1*109/L;3rd, June, our hospital: Blood-rt: WBC 0.15*109/L↓, N0*109/L↓↓↓Primary diagnosis:1 Hyperthyroidism2 Agranulemia:(1)Induced by drugs;(2)Hematopoietic system diseases?(such as aplastic anemia,MDS,leukemia etc.)3 Acute upper respiratory infection4 Other diseases which cause fever: such as other infections, connective tissue diseases etc.Corrected diagnosis (date 2010.6.4)1 Hyperthyroidism2 Agranulemia: Induced by drugs3 Acute upper respiratory infectionsignature:writer: Yanling LiangRevisor:。
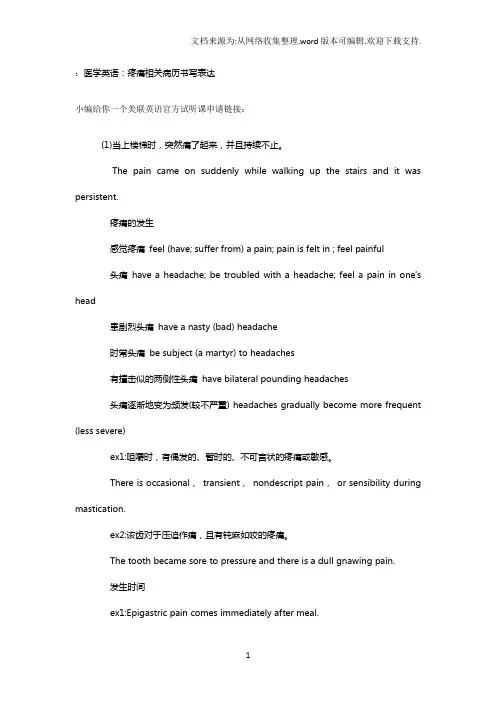
:医学英语:疼痛相关病历书写表达小编给你一个美联英语官方试听课申请链接:(1)当上楼梯时,突然痛了起来,并且持续不止。
The pain came on suddenly while walking up the stairs and it was persistent.疼痛的发生感觉疼痛feel (have; suffer from) a pain; pain is felt in ; feel painful头痛have a headache; be troubled with a headache; feel a pain in one's head患剧烈头痛have a nasty (bad) headache时常头痛be subject (a martyr) to headaches有撞击似的两侧性头痛have bilateral pounding headaches头痛逐渐地变为频发(较不严重) headaches gradually become more frequent (less severe)ex1:咀嚼时,有偶发的、暂时的、不可言状的疼痛或敏感。
There is occasional,transient,nondescript pain,or sensibility during mastication.ex2:该齿对于压迫作痛,且有钝麻如咬的疼痛。
The tooth became sore to pressure and there is a dull gnawing pain.发生时间ex1:Epigastric pain comes immediately after meal.ex2:Colic pain came on and off since yesterday.ex3:This pain has been relentlessly postprandial,regardless of the character of her meals.ex4:The joint pains were present mainly at night,with relief during the day.ex5:The mild frontal headaches were usually present upon awakening,but not severe enough to require analgesics.ex6:The pain usually commenced within 30 minutes after meals and lasted 1 to 3 hours.发生原因ex1:He described the pain as dull and aching,occurring approximately once a week,unrelated to food intake,and radiating to his back.(2)起初疼痛无变化,但数小时时变成发作性的痛。
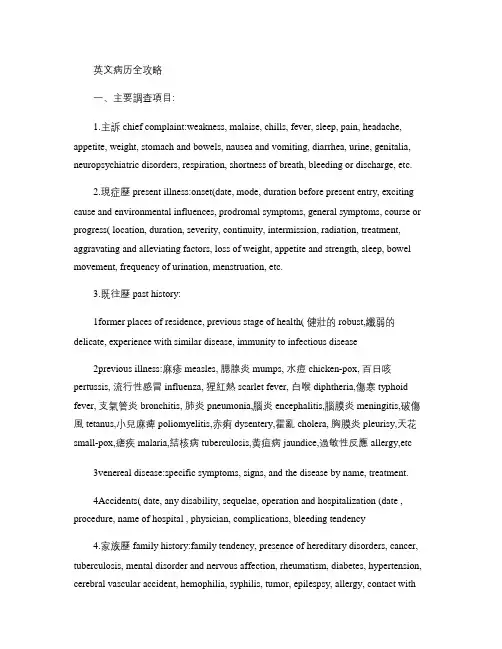
英文病历全攻略一、主要調查項目:1.主訴chief complaint:weakness, malaise, chills, fever, sleep, pain, headache, appetite, weight, stomach and bowels, nausea and vomiting, diarrhea, urine, genitalia, neuropsychiatric disorders, respiration, shortness of breath, bleeding or discharge, etc.2.現症歷present illness:onset(date, mode, duration before present entry, exciting cause and environmental influences, prodromal symptoms, general symptoms, course or progress( location, duration, severity, continuity, intermission, radiation, treatment, aggravating and alleviating factors, loss of weight, appetite and strength, sleep, bowel movement, frequency of urination, menstruation, etc.3.既往歷past history:1former places of residence, previous stage of health( 健壯的robust,纖弱的delicate, experience with similar disease, immunity to infectious disease2previous illness:麻疹measles, 腮腺炎mumps, 水痘chicken-pox, 百日咳pertussis, 流行性感冒influenza, 猩紅熱scarlet fever, 白喉diphtheria,傷寒typhoid fever, 支氣管炎bronchitis, 肺炎pneumonia,腦炎encephalitis,腦膜炎meningitis,破傷風tetanus,小兒麻痺poliomyelitis,赤痢dysentery,霍亂cholera, 胸膜炎pleurisy,天花small-pox,瘧疾malaria,結核病tuberculosis,黃疸病jaundice,過敏性反應allergy,etc3venereal disease:specific symptoms, signs, and the disease by name, treatment.4Accidents( date, any disability, sequelae, operation and hospitalization (date , procedure, name of hospital , physician, complications, bleeding tendency4.家族歷family history:family tendency, presence of hereditary disorders, cancer, tuberculosis, mental disorder and nervous affection, rheumatism, diabetes, hypertension, cerebral vascular accident, hemophilia, syphilis, tumor, epilespsy, allergy, contact withdiseased individuals, relationship of patient’s childhood and adult life, age, health condition, and cause of death of parents, grandparents, self , spouse, siblings , or relatives.5.個人歷personal history:1Social history:fears, metal status, education, financial condition, number of dependents, family harmony or fractious , hygienic condition at home2Marital history:duration of marriage, 1st or 2nd marriage, age and death of spouse and children , cause and age at time of death, number of children , pregnancies, 流產次數miscarriages, 死產數stillbirths3occupational history:duration of employment, past work, exact nature of work, exposure to occupational hazards, whether work is satisfactory or not.4Habits:alcohol, tobacco, narcotic, coffee, tea, appetite, food habits, regularity of meals, rapidity of eating , bowel movements, sleep, exercise, interests, etc.6.系統檢查system review:1General:nutrition, fever, night sweats, tremor, weight gain or loss, weakness, allergy.2Skin:蕁蔴疹hives, rash, eczema3Head:trauma, headache, loss of hair4Eyes:vision, pain glasses diplopia.5Ears:pain, discharge, deafness, tinnitus.6Nose:obstruction, discharge, epistaxis, rhinitis.7Mouth:teeth, lips, gums, tongue, disturbance in taste.8Throat.:sore throat, tonsillitis, 膿性扁桃腺炎quinsy, dysphagia9Neck:adenitis, goiter , rigidity10Cardiorespiratory:palpitation, tachycardia, blood pressure, chest pain, dyspnea, cough , hemoptysis , seasonal cold, expectoration.11Gastrointestinal:appetite, nausea, vomiting, distress(before or after meals, melena, colic, jaundice, fullness, hernia, hemorrhoid, constipation, diarrhea, frequency of bowel movement , heartburn, idiosyncrasies, relation of symptoms to eating, type and quantity of food12Genito-urinary:dysuria, urinary frequency, dribbling , hematuria, pyuria, nocturia and volume, enuresis, incontinence, sores about external genitalia, symptoms suggestive of syphilis(mucous patches, falling hair, urethral discharge, exposure to venereal infection, obstetric history, catamenia(age of onset, date of last period, cycle and amount, periodicity , dysmenorrheal, menopause leucorrhea, associated headache13Neuromuscular:神經過敏nervousness, emotional stress, weakness, muscle or joint pains, convulsion, numbness, neuralgia, anesthesia, muscular atrophies or dysatrophies, deformities.二、病歷與時態1.現症歷(present illness:1A.現在式:表示一般的真理、職業、人格、習慣和現在的事實、動作或狀態。
英语简要病历报告作文Title: Patient Medical Report: A Case of Respiratory Infection。
Date: April 16, 2024。
Patient Information:Name: [Patient Name]Age: [Age]Gender: [Gender]Date of Admission: [Date]Admitting Physician: Dr. [Physician Name]Chief Complaint:The patient presents with symptoms of cough, fever, shortness of breath, and fatigue.History of Present Illness:The patient, [Patient Name], a [Age]-year-old [Gender], presented to the emergency department with complaints of cough, fever, shortness of breath, and fatigue for the past five days. The cough was productive, with yellowish-green sputum. The fever was intermittent and associated with chills. The patient also reported experiencing mild chest pain exacerbated by coughing.Past Medical History:The patient has a past medical history significant for asthma, for which they use an inhaler as needed. There are no known allergies to medications.Medications:The patient takes [Medication Name] for asthma asneeded.Social History:The patient is a non-smoker and denies any history of alcohol or illicit drug use. They work as a [Occupation] and have no recent travel history.Family History:There is no significant family history of respiratory illnesses.Physical Examination:On physical examination, the patient was febrile with a temperature of [Temperature], tachycardic with a heart rate of [Heart Rate], and tachypneic with a respiratory rate of [Respiratory Rate]. Oxygen saturation was [Oxygen Saturation]% on room air. Lung auscultation revealed coarse crackles in the lower lung fields bilaterally. There was no evidence of cyanosis, clubbing, or peripheral edema. 。
病例英文作文模版英文:As a medical professional, I have encountered numerous interesting and challenging cases throughout my career. One particular case that stands out in my memory is the story of a young woman who came to our clinic complaining of severe abdominal pain. She was in her early twenties and had been experiencing this pain for several months, but had been too afraid to seek medical help until now.Upon further examination and some diagnostic tests, we discovered that she had a large ovarian cyst that needed to be surgically removed. The surgery was successful, and the young woman made a full recovery. However, what struck me the most about this case was not the medical aspect, but the emotional journey that the patient went through.She was initially very hesitant to undergo surgery, as she was afraid of the potential risks and complications. Ittook a lot of patience and reassurance from our medicalteam to help her overcome her fears and make the decisionto go through with the procedure. This experience taught me the importance of not only treating the physical symptomsof a patient, but also addressing their emotional and psychological needs.中文:作为一名医务人员,我在我的职业生涯中遇到了许多有趣和具有挑战性的病例。

英文病历标准模版Patient ProfileName: Si RuihuaDepartment: ___ Power ___Sex: FemalePresent Address: Electric Power Bureau Age: 80 yearsDate of n: May 17.2003nality: Chinese XinjiangDate of Record: May 17.2003Marital Status: MarriedReliability: Reliablen: Family ___History of Allergy: None reportedChief Complaints___。
breathlessness。
and precordial pain for the last hour。
There were no precipitating factors。
and the fort could not be relieved by rest。
As a result。
she came to the hospital for help。
She did not experience syncope。
cough。
headache。
diarrhea。
or vomiting during the course of the illness。
Her appetite。
sleep。
voiding。
and stool were normal.Medical History___.______。
___ distress。
She had a heart rate of 120 beats per minute and a blood pressure of 160/90 mmHg。
Her respiratory rate was 28 breaths per minute。
and her oxygen n was 90% on room air。
医学英语阅读:英文病历导读:本文医学英语阅读:英文病历,仅供参考,如果觉得很不错,欢迎点评和分享。
a sample of complete historypatient's name: mary swanchart number: 660518date of birth:10-5-1993sex: femaledate of admission: 10-12-2000date of discharge: 10-15-2000final discharge summarychief complaint:coughing, wheezing with difficult respirations.present illness:this is the first john hopkins hospital admission for this seven-year-old female with a history of asthma since the age of 3 who had never been hospitalized for asthma before and had been perfectly well until three days prior to admission when the patient development shortness of breath and was unresponsive to tedral or cough medicine.the wheezing progressed and the child was taken to john hopkins hospital emergency room where the child was given epinephrine and oxygen. she was sent home. the patient was brought back to the er three hours later was admitted.pasthistory:the child was a product of an 8.5-month gestation. the mother had toxemia of pregnancy. immunizations: all. feeding: good. allergies: chocolate, dog hair, tomatoes.family history:the mother is 37, alive and well. the father is 45, alive and well. two sibs, one brother and one sister, alive and well. the family was not positive for asthma, diabetes, etc.review of systems:negative except for occasional conjunctivitis and asthma.physical examination on admission:the physical examination revealed a well-developed and well-nourished female, age 7, with a pulse of 96, respiratory rate of 42 and temperature of 101.0℉. she was in a mist tent at the time of examination.funduscopic examination revealed normal fundi with flat discs. nose and throat were somewhat injected, particularly the posterior pharynx. the carotids were palpable and equal. ears were clear. thyroid not palpable. the examination of the chest revealed bilateral inspiratory and expiratory wheezes. breath sounds were decreased in the left anterior lung field. the heart was normal. abdomen was soft and symmetrical, no palpable liver, kidney, or spleen. the bowel sounds were normal. pelvic: normal female child. rectal deferred. extremities negative.impression:bronchial asthma, and pharyngitis.laboratory data:the white count on admission was 13,600 with hgb of 13.0. differential revealed 64 segs and 35 lymphs with 3 eos. adequate platelets. sputum culture and sensitivity revealed alpha hemolytic streptococcus sensitive to penicillin. chest x-ray on admission showed hyperaeration and prominent bronchovascular markings. the child was started on procaine penicillin 600,000 unites im q.d in accordance with the culture and sensitivity of the sputum.hospital course:。
医学英语病历写作范文Chief Complaint: Left leg pain with recent fall.History of Present Illness: The patient is a 65-year-old male who presents to the emergency department with a chief complaint of left leg pain. He states that he fell down a flight of stairs approximately 3 hours prior to presentation. He reports that he is in moderate to severe pain, which is localized to his left lower extremity. He denies any associated numbness or tingling. He has no prior history of leg pain or injury.Past Medical History: The patient has a history of hypertension, which is well-controlled with medication. He has no other significant medical history.Social History: The patient is married and has two children. He is a retired construction worker. He smokes one pack of cigarettes per day and drinks alcohol socially.Family History: The patient's father has a history of coronary artery disease. His mother has a history of Alzheimer's disease.Physical Examination:Vital signs: Blood pressure 140/80 mmHg, heart rate 80 bpm, respiratory rate 18 breaths per minute, temperature 98.6°F (37°C).General: The patient is in moderate distress due to pain. He is alert and oriented to person, place, and time.HEENT: Normocephalic and atraumatic. Pupils are equal and reactive to light. Extraocular movements are intact. No conjunctival injection or discharge. Tympanic membranes are intact and mobile.Neck: Supple with full range of motion. No masses or tenderness.Chest: Auscultation reveals clear breath soundsbilaterally. No wheezes, rales, or rhonchi.Cardiovascular: Regular rate and rhythm. No murmurs, rubs, or gallops.Abdomen: Soft and non-tender. No masses or organomegaly.Extremities: Left lower extremity: Examination reveals swelling and tenderness of the left knee. There is a palpable step-off deformity of the lateral aspect of theleft knee. Active and passive range of motion is limiteddue to pain. Distal pulses are palpable and capillaryrefill is brisk. Sensation is intact. Right lower extremity: Examination reveals no abnormalities.Neurological Examination:Mental status: Alert and oriented to person, place,and time. No deficits in attention, memory, or language.Cranial nerves: No deficits.Motor: Strength is 5/5 in both upper and lower extremities. No atrophy or fasciculations.Sensory: Sensation is intact to light touch, pinprick, and temperature in all four extremities.Diagnostic Studies:X-ray of the left knee: The X-ray shows a displaced lateral tibial plateau fracture.Assessment:Left knee pain.Displaced lateral tibial plateau fracture.Plan:The patient will be admitted to the hospital for further evaluation and treatment.He will be placed in a knee immobilizer and will be started on pain medication.Orthopedic surgery will be consulted for further management.。
英文病历示例患者,李华,男,69岁,退休教师,因心悸一年,加重5个月于1989年6月6日入院。
一年前患者健康。
1988年5月感到轻微心悸,在工作劳累,快走及上楼时感气短,傍晚下肢浮肿,休息后则减轻。
近5个月来,心悸气短明显加重。
以致不能行走,亦不能平卧,不得不坐着度过整夜,有时咳嗽,咳少量白色粘液,无血。
患者无寒战、发热、胸痛或关节疼痛,排尿正常。
系统复习无特殊,1949年曾患“大叶肺炎”,无药物过敏史。
个人史:生在西安,曾去过中国南方,但无疫水接触史,抽烟一天10支,1945年结婚,其妻健康,有一女孩亦健康,其父死于胃癌,其母健在。
查体:体温36.8℃,脉搏90次/分,呼吸28次/分,BP23.5/13.3kPa,发育良好,营养中等,体胖、半卧位,颜面苍白,全身浮肿,神智清楚,查体合作。
皮肤无红斑、黄疸、紫瘢。
淋巴结未触及。
头部、眼、鼻、耳、口正常,但口唇紫绀。
颈软,颈静脉无充盈,甲状腺未触及,无细震颤或搏动,气管正中。
胸廓两侧对称,呼吸动度对称,无异常浊音区,但在两肺底部可闻一些湿罗音。
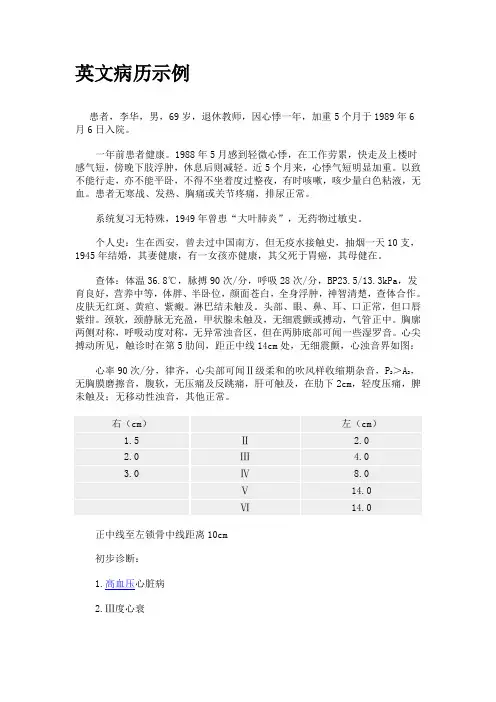
心尖搏动所见,触诊时在第5肋间,距正中线14cm处,无细震颤,心浊音界如图:心率90次/分,律齐,心尖部可闻Ⅱ级柔和的吹风样收缩期杂音,P2>A2,无胸膜磨擦音,腹软,无压痛及反跳痛,肝可触及,在肋下2cm,轻度压痛,脾未触及;无移动性浊音,其他正常。
正中线至左锁骨中线距离10cm初步诊断:1.高血压心脏病2.Ⅲ度心衰AN EXAMPLE OF IN-PATIENT′S MEDICAL CASE HISTORY IN ENGLISHPatient Li Hua, mate,69 years old, a retired teacher, was admitted on June 6,1989,because of palpitation for one year and becoming worse in recent 5 months.The patient was quite well until one year before May,1988, He felt slight palpitation and dyspnia during hard work, fast walk , or climbing stairs, There was swelling of legs in the evening but he felt better after having a rest. In recent 5months, palpitation and dyspnia became so serious that he could neither walk nor lie down.He had to sit up during the whole night, Sometimes he coughed with small amounts of sputum, but without blood. He had no chill, fever, chest pain or sore joints. The urinating was normal.There was nothing else abnormal in the case history review except a cured lobor pneumonia in 1949. He had no history of drug allergy.Personal history:The patient was born in Xi’an in 1923. He had been to the south of China but did not contact contaminated water. He smoked about 10 cigarettes daily. He got married in 1945. His wife was healthy .They had a daughter who was also healthy. His father died of stomach cancer.His mather was well.Physical Examination:T.36.8C, P. 96/min, R. 28/min, BP.23.5/13.3kPa. The patient, an old fatty man who developed well and moderately nourished, was lying in bed with a semifallous position. He looked pale and suffered from general edima. He was mentally normal and cooperative in the examination.There was no eruption, no jaundice, no purpura on the skin, and the lymphnodes were not palpable. The head, eyes, nose, ears, mouth were normal while the lips were cyanotic. The neck was soft, there was no venous engorgement. Thyroid glands were not palpable, there were no thrill or brunt. The trachea was in midline. The chest and respiratory movements were symmetrical. There was no abnormal dullness but some moist rales were heard in the base areas of the both lungs. The points of maximal impulse (PMI) were not visible but palpable in the 6thcostal interspace, 14cm form the middle line, there was no thrill. The cardiac dullness, 14cm from the middle line, there was no thrill. The cardiac dullness were as follows;The distance from midsternal line to midclavicular line was 10cm. The heart rate was 96/min, regular. There was a grade Ⅱsoft blowinglikesystolic murmurat the apex,P2>A2, but no pericardium friction sound washeard. Abdominal wall was soft without tenderness. The liver was palpable 2cm below the costal margin with slight tenderness. The spleen was not palpable and there was no shifting dull ness. The rest was normal.Impression:disease withdegreeⅢ heart failureSignature ×××。
医学英语病历写作范文Chief Complaint: Patient presents with chest pain and shortness of breath for 3 days.History of Present Illness: The patient, a 55-year-old male, reports experiencing sudden onset of chest pain 3 days ago. The pain is described as sharp and crushing, radiating to the left arm. He also reports associated shortness of breath and diaphoresis. The symptoms are aggravated with physical activity and alleviated with rest. There is no history of similar episodes in the past.Past Medical History: The patient has a history of hypertension and hyperlipidemia. He is on regular medications including amlodipine and atorvastatin.Family History: The patient's father had a history of myocardial infarction at the age of 60. His mother has hypertension and diabetes.Social History: The patient is a non-smoker and denies alcohol or recreational drug use. He is currently employed as a manager and reports moderate stress at work.Review of Systems: The patient denies any recent weight changes, fever, or chills. There is no history of cough, sputum production, or hemoptysis. He denies any gastrointestinal symptoms such as nausea, vomiting, or abdominal pain.Physical Examination:- Vital signs: Blood pressure 140/90 mmHg, heart rate 90 bpm, respiratory rate 20 breaths per minute, oxygen saturation 96% on room air.- General: The patient appears uncomfortable and diaphoretic.- Cardiovascular: Regular rhythm, no murmurs, rubs, or gallops. Capillary refill time is less than 2 seconds.- Respiratory: Clear breath sounds bilaterally, no wheezing or crackles.Assessment and Plan:1. Rule out acute coronary syndrome: The patient's presentation is concerning for acute coronary syndrome given the symptoms of chest pain, shortness of breath, anddiaphoresis. ECG and cardiac enzymes will be obtained to evaluate for myocardial ischemia.2. Blood pressure management: The patient's blood pressure is elevated, and optimization of antihypertensive medications will be addressed.3. Lipid management: Given the patient's history of hyperlipidemia, lipid panel will be obtained to assess for dyslipidemia and adjust medications as needed.4. Stress management: The patient's moderate stress at work will be addressed through counseling and potential referral to a stress management program.中文病历:主诉:患者因胸痛和呼吸急促已3天。
CASEMedical Number: 682786 General informationName:Wang RunzhenAge: Forty threeSex: FemaleRace:HanOccupation: Teacher Nationality:ChinaMarital status: Married Address: NO.38, Hangkong Road, Jiefang Rvenue, Hankou, Hubei. Tel: 82422500Date of admission: Jan 11st, 2001 Date of record: 11Am, Jan 11st, 2001Complainer of history: the patient herselfReliability: ReliableChief complaint: Right breast mass found for more than half a month.Present illness: Half a month ago, the patient suddenly felt pain in her right chest when she put up her hand. After touching it, she found a mass in her right breast, but no tendness, and the patient didn’t pay attention it. Then the pain became more and more serious, so the patient went to tumour hospital and received a pathology centesis. Her diagnosis was breast cancer. Then she came to our hospital and asked for an operation.Since onset, her appetite was good, and both her spiritedness and physical energy are normal. Defecation and urination are normal, too.Past historyOperative history: Never undergoing any operation. Infectious history: No history of severe infectious disease. Allergic history: She was not allergic to penicillin or sulfamide. Respiratory system: No history of respiratory disease.Circulatory system: No history of precordial pain.Alimentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease. Hematopoietic system:No history of anemia and mucocutaneous bleeding.Endocrine system: No acromegaly. No excessive sweats. Kinetic system: No history of confinement of limbs.Neural system: No history of headache or dizziness.Personal historyShe was born in Wuhan on Nov 19th, 1957 and almost always lived in Wuhan. She graduated from senior high school. Her living conditions were good. No bad personal habits and customs.Menstrual history: The first time when she was 14. Lasting 3 to 4 days every times and its cycle is about 30 days.Obstetrical history: Pregnacy 3 times, once nature production, abortion twice.Contraceptive history: Not clear.Family history: His parents have both died.Physical examinationT 36.4℃, P 80/min, R 20/min, BP 90/60mmHg. She is well developed and moderately nourished. Active position. The skin was not stained yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not enlarged.HeadCranium: Hair was black and well distributed. No deformities. No scars. No masses. No tenderness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external auditory canals. Notenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nares flaring. No tenderness in nasal sinuses.Eye:Bilateral eyelids were not swelling. No ptosis. No entropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or depressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect pupillary reactions to light were existent.Mouth: Oral mucous membrane was smooth, and of no ulcer or erosion. Tongue was in midline. Pharynx was not congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in midline.ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was neither narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities.Breast:Symmetric bilaterally. Neither nipples nor skin were retracted. Elasticity was fine.Lungs:Respiratory movement was bilaterally symmetric with the frequency of 20/min. Thoracic expansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales.Heart:No bulge and no abnormal impulse or thrills in precordial area. The point of maximum impulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardial friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 80/min.Cardiac rhythm was regular. No pathological murmurs. Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. There was not tenderness and rebound tenderness on abdomen or renal region. Liver was not reached. Spleen was not enlarged. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus 5/min. No vascular murmurs. Extremities: No articular swelling. Free movements of all limbs. Neural system: Physiological reflexes were existent without any pathological ones.Genitourinary system: Not examed.Rectum: not exanedInvestigationNo.Professional ExaminationThere are a about 3*3*2 cm mass in outer-up field of her right breast. It is hard but no tendness. It can be moved and its surface is smooth. The skin of her breast is normal. Corresponding superficial lymph nodes don’t enlarge.History summary1.P atient was a teacher, female, 43 years old.2.R ight breast mass found for more than half a month.3.N o special past history.4.P hysical examination showed no abnormity in lung, heart and abdoman. Information about her breast can be seen above.5. Shorting of investigation information.Impression: Breast cancer (right)Signature: He Lin (95-10033)。
英文病历范文Title: English Medical Record Sample (Creating and Expanding on a Matching Content)Medical RecordNa John SmithDate of Birth: February 15, 1985Gender: MaleNationality: AmericanOccupation: AccountantChief Complaint:The patient presented with a complaint of persistent cough, shortness of breath, and chest pain for the past week.History of Present Illness:The symptoms initially started as a mild cough, which gradually worsened over the week. The patient also experienced shortness of breath, especially during physical activities. He reported occasional chest pain, which was sharp in nature and intensified during deep breaths. The patient denied any fever, night sweats, or weight loss.Past Medical History:The patient has a history of asthma since childhood and has been using an inhaler as needed. He had a similar episode ofpersistent cough and shortness of breath six months ago, which resolved with a course of oral steroids. No other significant medical history was reported.Social History:The patient is a non-smoker and denies any alcohol or illicit drug use. He lives with his wife and two children in a smoke-free environment. The patient works as an accountant and does not have any known occupational exposures.Family History:There is no significant family history of respiratory diseases or any chronic illnesses.Review of Systems:The review of systems was unremarkable except for the respiratory symptoms mentioned above.Physical Examination:On examination, the patient appeared to be in no acute distress. Vital signs were within normal limits. Auscultation of the lungs revealed mild wheezing bilaterally. Heart sounds were normal, and there were no signs of peripheral edema or cyanosis. Other systemic examinations were within normal limits.Investigations:Laboratory investigations, including complete blood count, liver and kidney function tests, and electrolyte levels, were all within normal range. Chest X-ray showed hyperinflation of lungs and no evidence of infiltrates or consolidation.Assessment and Plan:Based on the history, clinical findings, and investigations, the patient's symptoms and past medical history suggest asthma exacerbation. Initial management includes a trial of short-acting bronchodilators, oral corticosteroids, and close monitoring of symptoms. The patient was educated about proper inhaler technique and advised to follow up in one week for reassessment.Education and Counseling:The patient was counseled on the importance of adherence to the prescribed medication and the need to avoid triggers for asthma exacerbation, such as allergens and respiratory infections. He was also provided with a written asthma action plan for self-management and advised to seek medical attention if symptoms worsen or do not improve within a week.Follow-up:The patient will be scheduled for a follow-up visit in one week to reassess symptoms, evaluate response to treatment, andadjust the management plan accordingly.This medical record documents the patient's chief complaint, history of present illness, past medical history, social and family history, physical examination findings, investigations, diagnosis, and treatment plan. It serves as a comprehensive guide for healthcare professionals involved in the patient's care.。
病历写作的作文医学英语Title: Writing Medical Records: A Guide to Effective Communication in Medical English。
Introduction。
Writing medical records is a critical aspect of healthcare practice, facilitating communication among healthcare providers and documenting patient care.Effective medical record writing requires proficiency in medical English to ensure clarity, accuracy, and compliance with professional standards. This guide aims to provide insights into writing medical records in English, covering key components and language considerations.1. Understanding the Purpose of Medical Records。
Medical records serve multiple purposes, including:Documenting patient health history, assessments, andtreatment plans.Facilitating communication among healthcare providers.Ensuring continuity of care.Supporting billing and insurance claims.Serving as legal documents in medical litigation.2. Components of Medical Records。
1 病历case histroy一般事项date of admission /marital status /present address /correspondence / occupatio n主诉chief complaints现病史present illness / history of present illness既往史past medical history家族史family history个人病史personal history / social history曾用药物medications过敏史allergies系统回顾system review / review of system体检physical examination一般资料physical data 生理指标physical signs一般状况或全身状况general appearance头眼与耳鼻喉head ,eyes,ear,nose,throat ,略作heent.胸部与心肺CHEST,heart,and lungs腹部abodoms四肢extremities神经系统nervous system,Neurological,略作CNC或Neuro,骨骼肌系统Musculoskeletal泌尿生殖系统Genitourinary化验室资料laboratory data/ studies /diagnosis血液检查blood test化学7项指标chem.-7心脑电图electrocardiogram / electroencephalogram , 略作EKG/EEGX线检查与x光片X-ray examination, x-ray slides,计算机X线断层扫描与核磁共振扫描资料computerized x-ray tomography and nuclear mag netic resonance spectroscopy dta. CT AND NMR其他检查资料other lab data印象与诊断impression and diagnosis住院治疗情况hospital course出院医嘱discharge instructions / recommendations出院后用药discharge medications2 看病时用英文1) 一般病情:He feels headache, nausea and vomiting. (他覺得頭痛、噁心和想吐。
History taking of coughPatient Name: Mrs. PennyAge: 35History conducted by: Doctor ZhangHistory conducted on: 31/08/2014 4:00pm.Source: The patient gives her own history and appears to be a reliable sourceChief complaint: Productive coughHistory of present illnessMrs. Penny is a 40-year-old yellow Chinese female who works in No.1 middle school as a teacher. She has been noticing worsening cough for 1 week, which is from dry to be with white sputum, and the volume of sputum is about 1 tea spoon per time. There is no accompanying chest pain or any other symptoms. The cough is relatively constant throughout the day and night but does vary in severity and it is severest right after waking up in the morning. Changing body positions, especially standing up, worsens the cough. Mrs. Penny finds no ways to relief it. She had a cold and a 39°C fever one week ago, and then started to cough as a result. She has been taken several days off due to the cough and sought for another doctor’s help in a community hospital 3 days ago, but those prescribed penicillin and antitussive did n’t work.Past medical history1.Mrs. Penny once had tonsillitis at 6 years old, accepting penicillinwith dose unknown.2.At 35 years old, she received appendectomy after appendicitis withoutblood transfusion.3.She has been experienced chronic cough for 5 years, which is associatedwith cold whether especially winter days. And the cough will last for3 months each year. She didn’t look for any treatments or drugs.MedicationsShe took penicillin 3 days ago. No known drugs allergies.Family historyMrs. Penny’s son is 12 years old and he is healthy.Social HistoryMrs. Penny is a Chinese teacher in No.1 middle school. She is married and has a 12-year-old son. She denies past or present tobacco and alcohol use.Review of systemsGeneral-as is indicated in the history of present illness, no fevers or chills; appetite not assessed; denies fatigue, malaise, weight loss Skin – denies rashes and skin lesions anywhere on her body. HEENT:∙Head – Denies headache; denies dizziness or syncope∙Ears –denies difficulty or changes in her hearing, denies tinnitus ∙Eyes – denies problems or changes in her vision; denies blurred vision; denies seeing spots∙Nose – Denies congestion or rhinorrhea∙Throat – denies dysphagia or sore throatCardiovascular – denies chest pain; denies palpitationPulmonary –denies shortness of breath, endorses cough with white sputum Gastrointestinal – denies abdominal pain; denies diarrhea or constipation; denies bloody bowel movementGenitourinary – denies dysuria; denies increased frequency or urgency of urinationNeurologic – denies numbness and tingling; denies paresthesias Musculoskeletal – denies any muscle or joint painHematopoietic – denies easy bruisingPsychiatric – denies depression, anxiety, mental disturbance, difficulty sleeping, suicidal ideation, hallucinations, paranoia Endocrine –denies polyuria, polydipsia, polyphagia, weight change, heat or cold intoleranceHeme/Lymphatic: denies easy or excessive bruising, history of blood transfusions, anemia, bleeding disorder, adenopathy, chills, sweats Allergic/Immunologic: denies urticarial, hay fever, frequent urinary tract infections; denies HIV high risk behaviorsReferences:1.https:///medselect/resources/sample-notes/sample-write-up-12./portfolio/patient-care/write-ups/sample-write-up/3.https:///wiki/Review_of_systems4.https:///medselect/resources/sample-notes。
医学英语阅读:英文病历
a sample of complete history
patient's name: mary swan
chart number: 660518
date of birth:10-5-1993
sex: female
date of admission: 10-12-2000
date of discharge: 10-15-2000
final discharge summary
chief complaint:
coughing, wheezing with difficult respirations.
present illness:
this is the first john hopkins hospital admission for this seven-year-old female with a history of asthma since the age of 3 who had never been hospitalized for asthma before and had been perfectly well until three days prior to admission when the patient development shortness of breath and was unresponsive to tedral or cough medicine.
the wheezing progressed and the child was taken to john hopkins hospital emergency room where the child was given epinephrine and oxygen. she was sent home. the patient was brought back to the er three hours later was admitted.past history:
the child was a product of an 8.5-month gestation. the mother had toxemia of pregnancy. immunizations: all. feeding:good. allergies: chocolate, dog hair, tomatoes.
family history:
the mother is 37, alive and well. the father is 45,
alive and well. two sibs, one brother and one sister, alive and well. the family was not positive for asthma, diabetes, etc.
review of systems:
negative except for occasional conjunctivitis and asthma.
physical examination on admission:
the physical examination revealed a well-developed and well-nourished female, age 7, with a pulse of 96, respiratory rate of 42 and t emperature of 101.0℉. she was in a mist tent at the time of examination.
funduscopic examination revealed normal fundi with flat discs. nose and throat were somewhat injected, particularly
the posterior pharynx. the carotids were palpable and equal. ears were clear. thyroid not palpable. the examination of the chest revealed bilateral inspiratory and expiratory wheezes. breath sounds were decreased in the left anterior lung field. the heart was normal. abdomen was soft and symmetrical, no palpable liver, kidney, or spleen. the bowel sounds were normal. pelvic: normal female child. rectal deferred. extremities negative.
impression:
bronchial asthma, and pharyngitis.
laboratory data:
the white count on admission was 13,600 with hgb of 13.0. differential revealed 64 segs and 35 lymphs with 3 eos. adequate platelets. sputum culture and sensitivity revealed alpha hemolytic streptococcus sensitive to penicillin. chest
x-ray on admission showed hyperaeration and prominent bronchovascular markings. the child was started on procaine penicillin 600,000 unites im q.d in accordance with the
culture and sensitivity of the sputum.
hospital course:。