Rheumatol Int
DOI 10.1007/s00296-014-3137-5
Role of integrins and their ligands in osteoarthritic cartilage
Jian Tian · Fang?Jie Zhang · Guang?Hua Lei
Received: 25 May 2014 / Accepted: 17 September 2014 ? Springer-Verlag Berlin Heidelberg 2014
[1]. Radiographic evidence of OA occurs in the majority of people by 65 years of age, and among them about 80 % in people who aged over 75 years [2]. However, the pathogen-esis of this disease is not fully elucidated.
Cartilage damage is one of the major pathological changes in OA. Articular cartilage is an avascular, a neu-ral, alymphatic, and viscoelastic connective tissue that functions autonomously to bear loads and provide almost friction-free movement of diarthrodial joints [3]. Chondro-cytes, the only cell population of adult articular cartilage, are strongly involved in maintaining the dynamic equi-librium between synthesis and degradation of the extra-cellular matrix (ECM) [4]. Collagens represent the major structural components of the articular cartilage. Cartilage is made up of two main ECM macromolecules: type II collagen and aggrecan, a large aggregating proteoglycan [5, 6]. Cartilage destruction is thought to be mediated by two main enzyme families: the matrix metalloproteinases (MMPs) are responsible for the cartilage collagen break-down, whereas enzymes from disintegrin and metallopro-teinase domain with thrombospondin motifs (ADAMTS) family mediate cartilage aggrecan loss [7]. Activation of biochemical pathways involves the production of proin-flammatory cytokines, inflammation, degradation of the ECM by MMPs and ADAMTS, and cessation of ECM syn-thesis via dedifferentiation and apoptosis of chondrocytes [8, 9]. Therefore, the ECM is a vital cellular environment, and interactions between the cell and ECM are important in regulating many biological processes, which include cell growth, differentiation, and survival [10, 11].
Cell–matrix interactions control cell function and behav-ior by signal transduction through a variety of cell sur-face receptors. The integrins are the major family of ECM receptors, which can transmit information from the matrix to the cell. Integrin binding of ECM ligands results in the
Abstract Osteoarthritis (OA) is a degenerative disease, which is characterized by articular cartilage destruction, and mainly affects the older people. The extracellular matrix (ECM) provides a vital cellular environment, and interactions between the cell and ECM are important in reg-ulating many biological processes, including cell growth, differentiation, and survival. However, the pathogenesis of this disease is not fully elucidated, and it cannot be cured totally. Integrins are one of the major receptors in chondro-cytes. A number of studies confirmed that the chondrocytes express several integrins including α5β1, αV β3, αV β5, α6β1, α1β1, α2β1, α10β1, and α3β1, and some integrins ligands might act as the OA progression biomarkers. This review focuses on the functional role of integrins and their extracellular ligands in OA progression, especially OA car-tilage. Clear understanding of the role of integrins and their ligands in OA cartilage may have impact on future develop-ment of successful therapeutic approaches to OA.Keywords Chondrocyte · Integrin · Fibronectin · Tenascin C · Osteopontin · Osteoarthritis · Cartilage
Introduction
Osteoarthritis (OA) is a degenerative disease and is char-acterized by articular cartilage destruction along with changes occurring in other joint components including bone, menisci, synovium, ligaments, capsule, and muscles
Rheumatology
INTERNATIONAL
J. Tian · F.-J. Zhang · G.-H. Lei (*)
Department of Orthopaedics, Xiangya Hospital, Central South University, No. 87 Xiangya Road, Changsha 410008, Hunan, China
e-mail: gh.lei9640@https://www.doczj.com/doc/4111661342.html,; lgh9640@https://www.doczj.com/doc/4111661342.html,
Rheumatol Int
formation of signaling complexes, which play a key role in the regulation of cell survival, adhesion, proliferation, dif-ferentiation, and matrix remodeling [11, 12]. To develop new and successful approaches for the treatment for OA, it is essential to elucidate the role of integrins and their ligands in the pathogenesis of OA. In this study, we have reviewed the role of integrins and their ligands on the OA cartilage, consequently which contributes to OA progression. Integrins structure and function
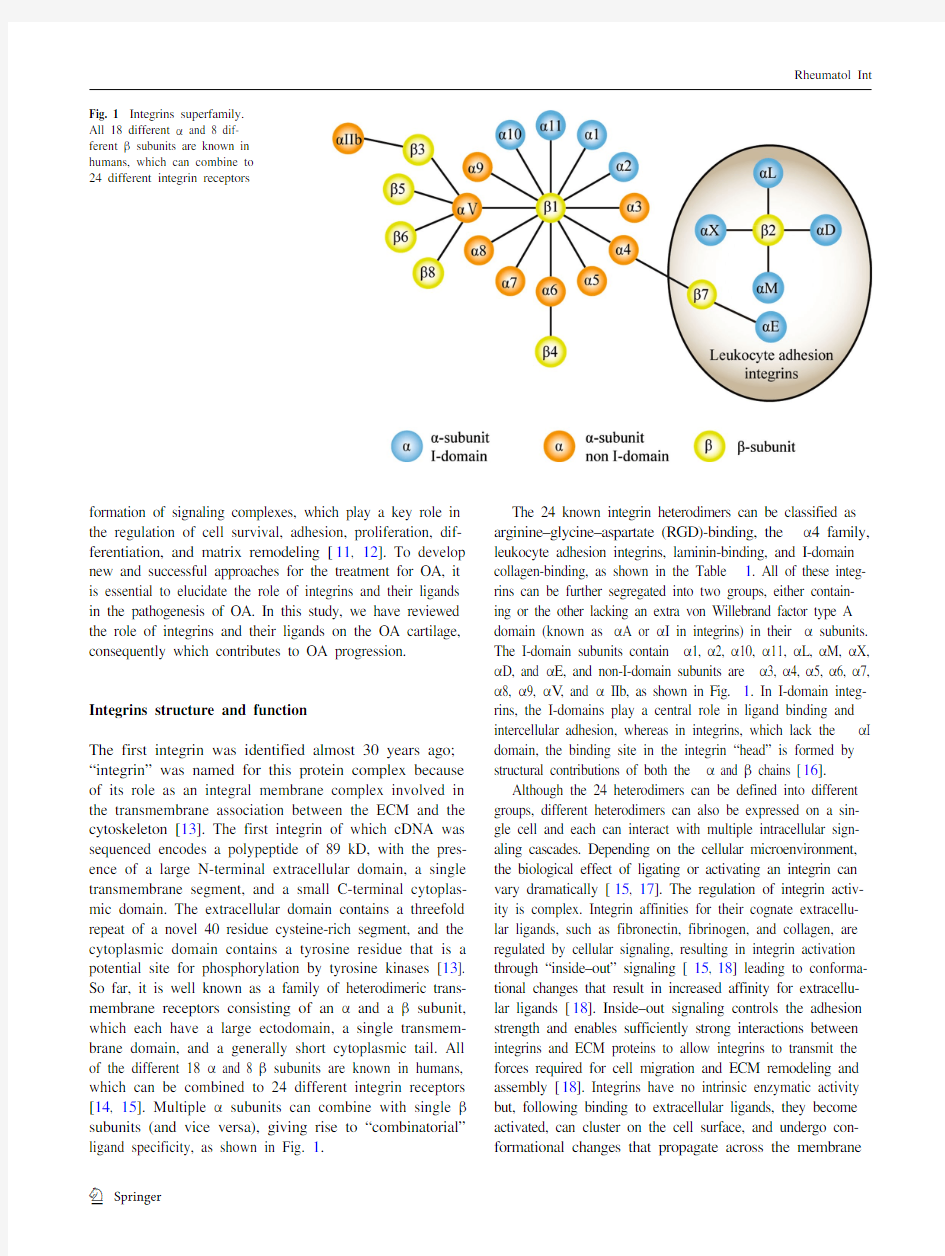
The first integrin was identified almost 30 years ago; “integrin” was named for this protein complex because of its role as an integral membrane complex involved in the transmembrane association between the ECM and the cytoskeleton [13]. The first integrin of which cDNA was sequenced encodes a polypeptide of 89 kD, with the pres-ence of a large N-terminal extracellular domain, a single transmembrane segment, and a small C-terminal cytoplas-mic domain. The extracellular domain contains a threefold repeat of a novel 40 residue cysteine-rich segment, and the cytoplasmic domain contains a tyrosine residue that is a potential site for phosphorylation by tyrosine kinases [13]. So far, it is well known as a family of heterodimeric trans-membrane receptors consisting of an α and a β subunit, which each have a large ectodomain, a single transmem-brane domain, and a generally short cytoplasmic tail. All of the different 18 α and 8 β subunits are known in humans, which can be combined to 24 different integrin receptors [14, 15]. Multiple α subunits can combine with single βsubunits (and vice versa), giving rise to “combinatorial” ligand specificity, as shown in Fig. 1.
The 24 known integrin heterodimers can be classified as arginine–glycine–aspartate (RGD)-binding, the α4 family, leukocyte adhesion integrins, laminin-binding, and I-domain collagen-binding, as shown in the Table 1. All of these integ-rins can be further segregated into two groups, either contain-ing or the other lacking an extra von Willebrand factor type A domain (known as αA or αI in integrins) in their α subunits. The I-domain subunits contain α1, α2, α10, α11, αL, αM, αX, αD, and αE, and non-I-domain subunits are α3, α4, α5, α6, α7, α8, α9, αV, and α IIb, as shown in Fig. 1. In I-domain integ-rins, the I-domains play a central role in ligand binding and intercellular adhesion, whereas in integrins, which lack the αI domain, the binding site in the integrin “head” is formed by structural contributions of both the α and β chains [16].
Although the 24 heterodimers can be defined into different groups, different heterodimers can also be expressed on a sin-gle cell and each can interact with multiple intracellular sign-aling cascades. Depending on the cellular microenvironment, the biological effect of ligating or activating an integrin can vary dramatically [15, 17]. The regulation of integrin activ-ity is complex. Integrin affinities for their cognate extracellu-lar ligands, such as fibronectin, fibrinogen, and collagen, are regulated by cellular signaling, resulting in integrin activation through “inside–out” signaling [15, 18] leading to conforma-tional changes that result in increased affinity for extracellu-lar ligands [18]. Inside–out signaling controls the adhesion strength and enables sufficiently strong interactions between integrins and ECM proteins to allow integrins to transmit the forces required for cell migration and ECM remodeling and assembly [18]. Integrins have no intrinsic enzymatic activity but, following binding to extracellular ligands, they become activated, can cluster on the cell surface, and undergo con-formational changes that propagate across the membrane
Fig. 1 Integrins superfamily. All 18 different α and 8 dif-ferent β subunits are known in humans, which can combine to
24 different integrin receptors
Rheumatol Int
(“outside–in”) to activate cytoplasmic kinase- and cytoskele-tal-signaling cascades. These in turn control cell attachment, movement, growth and differentiation, and survival [15, 17]. Therefore, integrin activation can increase ligand binding, resulting in outside–in signaling. Converse ligand binding can generate signals that cause inside–out signaling [18].
Expression of integrins in chondrocytes
Previous studies confirmed that the chondrocytes express several integrins including α5β1, αV β3, αV β5, α6β1, α1β1,
α2β1, and α10β1 [18–23], while α3β1 was expressed by occasional cells only [24]. The expression level of above-mentioned integrins was in different percentages and in dif-ferent zones. Fetal chondrocytes strongly expressed β1 and β5 chains [24, 25]. Chondrocytes from osteoarthritic car-tilage expressed high levels of β1 integrin and all of the α chains. The α1 was the most frequently expressed α chain, followed by α3, α5, α2, αv. Integrin expression decreased from the least to the most damaged zone of articular car-tilage, and cell cycle analysis showed that proliferating chondrocytes (S phase) were prevalent in the latter zone. The expression of β2, β3, β2, and β5 is usually very low
Table 1 24 human integrin heterodimers and their ligands ADAMs a disintegrin and metalloproteinases, ICAM intercellular adhesion molecules, VCAM vascular adhesion molecules, TGF β LAP trans-forming growth factor β latency-associated peptide, MadCaM mucosal address in cell adhesion molecule, VEGF vascular endothelial growth factor
Human integrins Ligands Cellular and tissue distribution
RGD -binding α5β1Fibronectin
Chondrocytes , endothelial cells
α8β1Fibronectin, vitronectin, tenascin C, osteopontin, nefronectin Smooth muscle cells αV β1Fibronectin, vitronectin Smooth muscle cells, fibroblasts, osteoclasts, tumor cells αV β3
Fibrinogen, fibronectin, vitronectin, tenascin C, osteopontin, bone sialoprotein, MMP-2Smooth muscle cells, fibroblasts, osteoclasts, tumor cells, Chondrocytes, endothelial cells, platelets, epithelial cells,
leukocytes
αV β5Vitronectin Smooth muscle cells, fibroblasts, osteoclasts, Chondrocytes,
platelets, leukocytes, epithelial cells
αV β6Fibronectin, TGF-β LAP Epithelial cells, carcinoma cells αV β8Vitronectin Melanoma, kidney, brian, ovary, uterus, placenta αIIb β3Fibrinogen Fibronectin, vitronectin
Platelets The α4 family α4β1Fibronectin, VCAM
Leukocytes, endothelial cells,α4β7Fibronectin, VCAM, MadCaM
Leukocytes,
α9β1
Tenascin C, osteopontin, ADAMs, factor XIII, VCAM, VEGF-C, VEGF-D
Endothelial cells, keratinocytes
Leukocyte adhesion integrins αD β2ICAM, VCAM Leukocytes αM β2ICAM, VCAM, iC3b, factor X, fibrinogen Leukocytes αL β2ICAM Leukocytes αX β2Fibrinogen, plasminogen, heparin, iC3b Leukocytes αE β7E-cadherin Leukocytes,Laminin -binding α3β1Laminins (collagens)Keratinocytes
α6β1Laminins, ADAMs Endothelial cells, Chondrocytes α6β4Laminins Endothelial cells
α7β1
Laminins
Differentiated muscle cells I -domain collagen -binding α1β1Collagens, semaphorin7A, (laminins)Endothelial cells, Chondrocytes
α2β1Collagens, tenascin C, (laminins)Keratinocytes, endothelial cells, Chondrocytes, platelets α10β1Collagens Chondrocytes
α11β1
Collagens
Mesenchymal non-muscle cells
Rheumatol Int
[25]. With immunohistochemical methods using monoclo-nal and polyclonal antibodies, the integrin pattern in joint cartilage from rats corresponded largely to integrin expres-sion described for human cartilage tissue: β1, α1, α3, and αv subunits and the α5β1 and αvβ3 heterodimers were con-sistently expressed [26]. Moreover, an inverse correlation was demonstrated between the severity of the anatomical changes found in the zones and the phenotypic/metabolic changes in the cells. These results, together with the well-known inside–out signaling function of the adhesion mol-ecules, highlight the key role of matrix interactions in the pathogenesis of the anatomic changes in OA cartilages [22, 27]. Expression of integrins on chondrocytes is correlated with the degree of cartilage damage in human OA [22].
All of the α5β1, αVβ3, and αVβ5 contain the RGD-binding domain; α6β1 and α3β1 contain the laminin-binding domain, while α1β1, α2β1, and α10β1 contain the I-domain collagen-binding motif. The α5β1 integrin serves as the primary chondrocyte fibronectin (FN) receptor [28], while αV-containing integrins bind to vitronectin [29] and osteopontin (OPN) [30], and may serve as alternative FN receptors. αVβ3 integrin binds to tenascin C [31]. All of the α1β1, α2β1, and α10β1 integrins can serve as receptors for collagens [32–34], and α6β1 and α3β1 integrins could bind to certain cartilage extracellular matrix proteins such as laminin [35–37]. The aforementioned integrins and their corresponding ligands all played the important roles in OA pathologic changes.
Important roles of integrins in OA cartilage
Integrins mediate cells adhesion
The cartilage surface defect is a common change in OA. The initial adhesion of transplanted chondrocytes to sur-rounding host cartilage may be important in the repair of articular defects [38]. Adhesion may set position for cells to secrete molecules that fill the defect and integrate repair tissue with host tissue, while chondrocytes are known to become increasingly adherent to cartilage with time. It is well known that Annexins (mainly A5), CD44, and integ-rins are the important molecules involved in chondrocyte adhesion with ECM.
In vitro experiments, under the conditions in which chondrocytes were cultured in high-density monolayer, released with trypsin, and allowed to recover in suspen-sion for 2 h at 37 °C, β1-integrins appear to mediate chon-drocyte adhesion to a cut cartilage surface. Delineation of the mechanisms of adhesion may have clinical impli-cations by allowing cell manipulations or matrix treat-ments to enhance chondrocyte adhesion and retention at a defect site [39]. Under the culture and seeding conditions in high-density or low-density monolayer, β1, α5β1, and αVβ5 integrins mediate human chondrocyte adhesion to cartilage [19]. These chondrocyte integrins have a potential role in the initial adhesion and retention of chondrocytes at a cartilage defect site following clinical procedures of chondrocyte transplantation [19]. In an experiment about the chondrocytes attached to hyaline or calcified carti-lage and bone, freshly isolated (primary) or passaged (P1) chondrocytes were seeded on the top of bone plugs having either a surface composed of mid-deep zone hyaline carti-lage or calcified cartilage or bone only. Both primary and passaged chondrocytes attached efficiently to all of the three surfaces (over 88 % of seeded cells). The chondro-cytes showed a punctate distribution of β1-integrin and vin-culin, which are colocalized with actin, suggesting that the cells formed focal adhesions. Blocking either β1-integrin or αVβ5 integrin partially inhibited (between 27–48 and 26–37 %, respectively) attachment of both primary and pas-saged chondrocytes to all surfaces. Blocking αVβ3 had no effect on adhesion [38].
Besides cell adhesion, integrins also mediate chondro-cytes adhesion to their extracellular ligands. Cell adhesion assays revealed that both α1β1 and α2β1 can serve as chon-drocyte adhesion receptors for types II and VI collagen. In cell lines expressing both integrins, α1β1 was the preferen-tial receptor for type VI collagen, while α2β1 was the pref-erential receptor for type II collagen [23]. Thus, α1β1 and α2β1 integrins play the roles to mediate chondrocyte adhe-sion to types II and VI collagen, respectively [23]. α1β1 also mediates chondrocyte adhesion to type VI collagen [40]. Integrins also mediate attachment of chondrocytes to fibronectin and matrix Gla protein (MGP) [41].
Integrins in chondrocytes mechanotransduction
In OA, mechanical forces play an important role in tissue homeostasis and remodeling [42]. Chondrocytes are poten-tially exposed to a variety of different mechanical forces including stretch, shear, or compressive forces in vivo [42]. Matrix synthesis and chondrocyte proliferation are up-regulated by the physiological levels of mechanical forces [43]. It is well know that integrins as mechanoreceptors regulate the cellular response to both changes in the ECM and mechanical stresses that chondrocytes are subjected to [44–46]. Integrin activity is important in the early cel-lular responses to mechanical stimulation, regulating the activation of a number of intracellular cascades that induce changes in gene expression and tissue remodeling. In nor-mal human articular chondrocytes, integrin activation, con-sequent to mechanical stimulation in vitro, results in tyros-ine phosphorylation of regulatory proteins and subsequent secretion of autocrine and paracrine acting soluble media-tors including substance P and interleukin 4 [47]. Normal
Rheumatol Int
chondrocytes in monolayer exposed to 0.33-Hz mechanical stimulation for 20 min resulted in increased GAG synthesis that was blocked by the presence of antibodies to α5 and αVβ5 integrins and CD47. These studies suggested that αVβ5 integrin plays a role in the regulation of chondrocyte responses to biomechanical stimulation [48]. In vitro stud-ies showed that the primary monolayer cultures of human chondrocytes have an electrophysiological response after intermittent pressure-induced strain characterized by a membrane hyperpolarization of approximately 40 %. The cultured chondrocyte’s hyperpolarization was found to be inhibited by RGD peptides and antibodies to the α5 and β1 integrin subunits [49], and the hyperpolarization response was associated with opening of small conductance (SK) calcium-dependent K+ channels via α5β1 integrin stretch activated ion channels and a number of integrin-associated signaling molecules including the involvement of the actin cytoskeleton and tyrosine phosphorylation [50]. Thus, α5β1 is an important chondrocyte mechanoreceptor and a potential regulator of chondrocyte function [49]. Integrin α1β1 is a key participant in chondrocyte transduction of a hypo-osmotic stress. Furthermore, integrin α1β1 influences osmotransduction is independent of matrix binding, but likely dependent on the chondrocyte osmosensor transient receptor potential vanilloid-4 [51].
Treatment of chondrocytes with interleukin-1 (IL-1) resulted in diminished synthesis and enhanced catabolism of matrix proteoglycans [52]. Within chondrocytes, expo-sure of interleukin-1β (IL-1β) induces the release of nitric oxide (NO) and prostaglandin E2 (PGE2) via activation of inducible nitric oxide synthase (iNOS) and cyclooxygenase (COX-2) enzymes, independently of integrins [53, 54]. This effect can be reversed by integrin with the applica-tion of dynamic compression three-dimension agarose con-structs. Mechanical loading and IL-1β influence the release of NO and PGE2 from articular chondrocytes. The integ-rin-binding peptide, GRGDSP, abolishes or reverses the compression-induced alterations in the presence or absence of IL-1β. Thus, integrins act abrogating the NO and PGE2 release by directly influencing the expression levels of iNOS and COX-2 in the presence and absence of IL-1β in three-dimension agarose constructs [55, 56].
In the mechanical stress stimuli situation, integrins regu-late responses of human articular chondrocytes to mechani-cal stimulation via several pathway or downstream com-ponents. For example, mechanical signals control SOX-9, VEGF, and c-Myc expression and cell proliferation dur-ing inflammation via integrin-linked kinase, B-Raf, and ERK1/2-dependent signaling in articular chondrocytes [43]. Integrin-associated protein (CD47/IAP) is necessary for chondrocyte mechanotransduction. Through interac-tions with α5β1 integrin and thrombospondin, CD47/IAP may modulate chondrocyte responses to mechanical signals [57]. Furthermore, ankle joint chondrocytes appeared to show significant differences in levels of the integrin-asso-ciated proteins CD98, CD147, and galectin 3, PKC gamma, and differences in responses to glutamate were seen. This might be related to modified integrin-dependent mecha-notransduction as a result of changes in the expression of integrin regulatory molecules such as CD98 or differen-tial expression and function of downstream components of the mechanotransduction pathway such as PKC or NMDA receptors [58]. RACK1-mediated translocation of activated PKCα to the cell membrane and modulation of integrin-associated signaling are likely to be important in regula-tion of downstream signaling cascades controlling chon-drocyte responses to mechanical stimuli [59]. Recently, Whitney et al. [60] found that ultrasound (US) has emerged as a technique to deliver mechanical stress, and their find-ings suggested US signals through integrin receptors to the MAPK/Erk pathway via a mechanotransduction pathway involving FAK, Src, p130Cas, and CrkII.
Integrins regulate cells proliferation and differentiation
Cell–cell interactions play an important role in the develop-ment of cartilage. Heterologous and homologous cell–cell interactions are critical for chondrogenic differentiation during development. Chondrocyte survival and in situ dif-ferentiation are integrin-mediated [61]. Integrin β1, β5, and α5 might be involved in signal transmission for the chon-drocyte survival and dedifferentiation [62, 63]. The lack of β1 integrins on chondrocytes leads to severe chondrodys-plasia associated with high mortality rate around birth [64]. Deletion of β1 integrins in the limb bud results in multi-ple abnormalities of the knee joints; however, it neither accelerate articular cartilage destruction, perturb cartilage metabolism, nor influence intracellular mitogen-activated proteins kinase (MAPK) signaling pathways [64]. When β1 integrin gene is inactivated in the mutant mice chondro-cytes, chondrodysplasia of various severity is developed in mice. β1-deficient chondrocytes have an abnormal shape, and they are failed to arrange into columns in the growth plate [65]. This is caused by the lack of motility, which is in turn caused by a loss of adhesion to collagen type II, reduced binding to and impaired spreading on fibronectin, and an abnormal F-actin organization. In addition, mutant chondrocytes show decreased proliferation caused by a defect in G1/S transition and cytokinesis. Altogether, these findings establish that β1-integrin-dependent motility and proliferation of chondrocytes are mandatory events for endochondral bone formation to occur [65].
Cell–cell interactions between articular chondrocytes and synovial fibroblasts have enhanced binding between these two cell types compared to background binding of the labeled cells to the tissue culture plastic surface and
Rheumatol Int
chondrocytes, specifically bound to synovial fibroblasts through RGD-dependent receptors. Therefore, β1 integrins are involved in this adhesion process, and these heterolo-gous cell interactions appear to have a negative influence on chondrogenic differentiation [66]. Articular chondrocytes undergo an obvious phenotypic change when cultured in monolayers. During this change, or dedifferentiation, α5β1 integrin was found to be involved in the induction of type I and type III pro-collagen expression. Elated RAS viral (r-ras) oncogene homolog (RRAS) was considered to regu-late the progression of dedifferentiation by modulating the affinity and avidity of α5β1 integrin to ligands. Echistatin (a potent disintegrin) inhibits dedifferentiation of monolayer-cultured chondrocytes [67]. In chondrocytes, during expan-sion for tissue engineering, a candidate for signal transmis-sion during dedifferentiation is integrin α5β1 in conjunction with its ligand fibronectin [68]. Other receptors, like vitron-ectin and OPN (αVβ3) or laminin (α6β1) or their ligands, do not seem to be involved in signal transmission for dedi-fferentiation. In addition, the GPIIb/IIIa receptor seems to assist the process of dedifferentiation. Intracellularly, ILK, ICAP1, and CD47 might assist the transduction of the inte-grin-dependent signals [68]. In tissue engineering research, it was confirmed that the mesenchymal stem cells (MSCs) with high chondrogenic differentiation potential are highly α10 positive and propose α10 as a potential marker to pre-dict the differentiation state of MSCs [69].
The signaling cascades involved in these processes of integrin regulating cells proliferation and differentiation mainly were MAPK, and GTPases as Ras and Raf, and subsequent apoptosis in human articular chondrocytes. Ras activation stimulates the extracellular signal-regulated kinase (ERK) MAPK cascade [70]. Loss of chondrogenic potential is accompanied by reduced expression in key signaling proteins of the MAPK pathway and apoptosis [71]. Activation of the chondrogenic transcription factor Sox-9 seems to be mediated by the MAPK pathway [72]. Ras-activated Raf–MEK–ERK signaling pathway can specifically control the expression of individual integrin subunits in a variety of human and mouse cell lines [73]. In articular chondrocytes, the affinity of αVβ5 integrin for ligands was regulated by the small GTPase R-Ras. R-Ras was gradually activated in monolayer-cultured chondro-cytes after plating, which caused a gradual decline in the cartilage matrix gene expression through enhanced Vβ5 integrin activation and the subsequent increase in ERK signaling [74].
Integrins in cartilage homeostasis
Osteoarthritis-affected cartilage exhibits enhanced expres-sion of FN and OPN mRNA. Ligation of α5β1 using acti-vating mAb JBS5 (which acts as agonist similar to FN N-terminal fragment) up-regulates the inflammatory medi-ators such as NO and PGE2, as well as the cytokines, IL-6, and IL-8. In contrast, αVβ3 complex-specific function-blocking mAb (LM609), which acts as an agonist similar to OPN, attenuates the production of IL-1β, NO, and PGE2 in a dominant negative fashion by osteoarthritis-affected carti-lage and activated bovine chondrocytes. These demonstrate a cross talk in signaling mechanisms among integrins and show that integrin-mediated “outside–in” and “inside–out” signaling very likely influences cartilage homeostasis, and its deregulation may play a role in the pathogenesis of oste-oarthritis [75]. In the α1-KO mice, more severe cartilage degradation, glycosaminoglycan depletion, and synovial hyperplasia were found as compared with the wild-type (WT) mice [76]. MMP-2 and MMP-3 expressions were increased in the OA-affected areas. In cartilage from α1-KO mice, the cellularity was reduced and the frequency of apoptotic cells was increased. Therefore, deficiency in the α1 integrin subunit is associated with an earlier deregula-tion of cartilage homeostasis and an accelerated, aging-dependent development of OA [76].
Integrin α1β1 plays a vital role in mediating chondrocyte responses to two contrasting factors that are critical play-ers in the onset and progression of OA—inflammatory IL-1 and anabolic TGF-β [77]. In a rat OA experimental model, an increased expression of α5 and α2 integrins was found at OA late stages, which was correlated with the changes in the ECM content, as a consequence of the increased MMPs activity. In addition, in the rat OA experimental model, the presence of α4 integrin since OA early stages was corre-lated with the loss of proteoglycans and clusters formation [78]. However, at late OA stages, the increased expression of α4 integrin in the middle and deep zones of the cartilage was also correlated with the abnormal endochondral ossi-fication of the cartilage through its interaction with OPN. Finally, these findings concluded that ECM–chondrocytes interaction through specific cell receptors is essential to maintain the cartilage homeostasis. However, as the integ-rins cell signaling is ligand-dependent, changes in the ECM contents may induce the activation of either anabolic or catabolic processes, which limits the reparative capacity of chondrocytes, favoring OA severity [78].
Fibroblast growth factor (FGF) and insulin-like growth factor (IGF) have been implicated as contributing factors in cartilage homeostasis [79, 80]. FGF-18 most likely exerts anabolic effects in human articular chondrocytes by induc-ing ECM formation, chondrogenic cell differentiation, and inhibiting cell proliferation [79, 81]. The role of FGF-8 has been identified as a catabolic mediator in rat and rab-bit articular cartilage [82]. IGF-1 is a major growth factor involved in cartilage matrix synthesis and repair. IGF-1 promotes synthesis of collagen type II, proteoglycans, and other matrix components [83]. Chondrocytes from
Rheumatol Int
osteoarthritic cartilage respond poorly to IGF-1 stimulation [84]. Integrin signaling works in concert with FGF and IGF via MAPK [85]. The proliferative response of rabbit sternal chondrocytes to FGF required FN binding to the α5β1 inte-grin [86]. In addition, FGF and IGF-1 induce proteoglycan synthesis in chondrocytes adherent to FN but not albumin, suggesting stimulatory signal transduced by α5β1 [63, 87]. Ligands for integrins in OA cartilage
Extracellular ligands–intracellular receptors interactions control cell attachment, movement, growth and differentia-tion, and survival. Several surface protein ligands can bind to integrins, and the ligands might be of vital importance in OA. These ligands, collagen type II deposition, seem to be increased in the deeper cartilage zones during the oste-oarthritic process, as a sign of tissue repair response [88, 89]. Collagen type I, fibronectin, tenascin, and osteopontin show enhanced deposition in the upper, fibrillated osteoar-thritic cartilage, suggesting a common mediator controlled pathway [88, 89].
Fibronectin and fibronectin fragments
Fibronectin is an adhesive multifunctional glycoprotein of 450 kD found in the ECM of many tissues, including artic-ular cartilage [90]. Cartilage fibronectin is a normal com-ponent of human cartilage and a normal product of mature chondrocytes [91, 92], as well as synovial membrane, and the type B synoviocyte is responsible for FN production [93]. FN is tenfold increased in OA cartilage [91] and two-fold in OA synovial fluid [94]; thus, FN is a marker for OA [94]. However, native FN has no catabolic effect on carti-lage [95]. FN is readily degraded into fragments (FN-fs) by proteinases, and activation of extracellular proteolysis in OA may lead to the fragmentation of FN. Fn-fs may also be generated within cartilage and amplify cartilage damage [96] Indeed, the increased levels of FN-fs of 30–200 kD are found in cartilage and synovial fluid from patients with OA [96]. FN-fs can cause cartilage to release MMPs, resulting in severe proteoglycan depletion, and others have shown that fragments also enhance MMPs expression in synovial fibroblasts [97]. FN-fs mediate MMPs up-regulation and cartilage damage through proline-rich tyrosine kinase 2, c-src, NF-κB, and protein kinase C delta [98]. The presence of these fragments suggests the pathologic consequences in arthritis [97].
Integrins can regulate FN-fs action. MMP production by the central cell-binding FN-fs is probably mediated by α5β1 integrin, because anti-α5β1 integrin antibody and RGD-containing peptide induce MMP-1 and gelatinase in rabbit synovial fibroblasts [99]. MMP-13 production by human chondrocytes could also stimulated by FN-fs and the adhesion-blocking antibody to the α5β1 integrin [100]. When using antisense oligonucleotides to α5, integrin sub-units have also shown the involvement of α5 integrin in car-tilage proteoglycan degradation induced by NH2-terminal heparin-binding and NH2-terminal gelatin-binding FN-fs without cell-binding RGD sequence in addition to the cen-tral cell-binding FN-f [101]. FN-fs active in chondrocytic chondrolysis can be chemically cross-linked to the α5 inte-grin receptor subunit [102].
FN-f’s another receptor, Toll-like receptors (TLRs), also plays important roles in human chondrocytes and osteo-arthritic cartilage [103, 104]. TLRs are usually increased in OA cartilage lesions [105]. TLR-2 and TLR-4 ligands strongly induce the catabolic responses in chondrocytes and treatment with TLR ligands led to the phosphorylation of all 3 MAPKs and activation of NF-κB [105]. The FN-fs mediate its proinflammatory effects via TLR by the extra type III domain A splice variant of FN [106]. In murine studies, the FN-fs (FN III 13–14 in the C-terminal heparin-binding region)-induced aggrecanase activity was found inhibited in TLR4 knockout mice but not in wild-type mice, suggesting that FN-fs induce joint damage via TLR4 4 activation [107].
Tenascin C
Tenascin C (TN-C) is a modular, multifunctional ECM glycoprotein. Tenascin is intimately associated with the development of articular cartilage and other permanent cartilages, whereas the absence or reduced amounts of this matrix protein characterize transient cartilages, which undergo maturation and are replaced by bone [108]. In human articular cartilage, TN-C expression decreases dur-ing the maturation of chondrocytes, and almost disappears in adults; however, in OA patients, TN-C expression in the knee cartilage and TN-C levels in the synovial fluid are sig-nificantly enhanced [109]. TN-C, including the large-var-iant subunits, is a useful biochemical marker for OA pro-gression in the later stages of disease [110]. The elevated levels of TN-C can induce inflammatory mediators and promote matrix degradation in OA [109], and TN-C in syn-ovial fluid may serve dual roles as a marker of joint damage and a stimulant of further joint degradation [111].
In OA cartilage, TN-C staining is shown in the cartilage surface overlying CS-positive areas [112]. The distribu-tion of TN-C is related to CS production and chondrocyte proliferation in OA cartilage, and that TN-C has effects on DNA synthesis, proteoglycan content, and aggrecan mRNA expression in vitro. TN-C may also be responsible for the repair in human OA cartilage [112]. In addition, recombi-nant TN-C fragments containing the same regions as those identified from OA cartilage mediate cartilage degradation
Rheumatol Int
by the induction of aggrecanase activity. TN-C fragments mapping to the EGF-L and FN type III domains 3–8 of TN-C had the highest levels of aggrecan-degrading ability that was not observed either with full-length TN-C or with other domains of TN-C. TN-C fragments represent a novel mechanism for cartilage degradation in arthritis and may present new therapeutic targets for the inhibition of carti-lage degradation [113]. In TN-C knockout mice, the carti-lage repair was found significantly slower than that in WT mice, and that the deficiency of TN-C progressed during cartilage degeneration [114]. Although TN-C interaction with α9β1 integrin as the anautocrine and paracrine man-ners in the joint tissue microenvironment contributes to the pathogenesis of RA [115], the exact mechanism of TN-C in OA cartilage degradation is unclear. Whether TN-C plays its important role in OA pathogenesis via integrin were not determined, and need further research.
Osteopontin
Osteopontin is a 44- to 75-kD multifunctional phospho-protein secreted by many cell types including chondro-cytes and fibroblast-like synoviocytes [89, 116]. Expres-sion of OPN mRNA isolated from human OA cartilage was enhanced as compared with normal cartilage [89]. In patients with knee OA, the elevated OPN in plasma, syno-vial fluid, and articular cartilage is associated with progres-sive joint damage. OPN may serve as a biochemical marker for determining disease severity and could be predictive of prognosis with respect to the progression of knee OA [117, 118]. In cartilage of OA patients, Xu et al. [119] analyzed the phosphorylation level of OPN in OA cartilage and nor-mal cartilage by immunoprecipitation, and found a higher phosphorylation level of OPN in OA cartilage than in nor-mal cartilage, suggesting that OPN phosphorylation might be related to the cartilage degeneration.
Attur et al. [120] found that the addition of recombinant OPN to human OA-affected cartilage under ex vivo con-ditions suppressed spontaneous production of nitric oxide and prostaglandin E2. These findings suggest that OPN is overexpressed in OA cartilage and functions as an endog-enous inhibitor of production of inflammatory mediators in cartilage. OPN deficiency exacerbated both aging-asso-ciated and instability-induced OA. Both structural changes and an increased loss of proteoglycan from cartilage tissue were augmented in the absence of OPN. OPN deficiency also led to the induction of MMP-13 [121]. Usually, in OA progression, OPN plays important role as an intrinsic regu-lator [122]. In addition, OPN may mediate bone resorption by osteoclasts in arthritis through ligation with its receptor, αVβ3 integrin. OPN is regarded as a potential therapeutic target molecule in the prevention of bone destruction in arthritis [123].Conclusions
The hallmark pathological change in OA is cartilage dam-age. Several integrins have been found they expressed in chondrocyte cartilage and can also bind to some extracellu-lar ligands proteins such as fibronectin, collagens, tenascin C, and osteopontin. Some ligands may act as the OA pro-gression biomarkers. Furthermore, not only the integrins or just the ligand play roles alone in OA, but also the inter-actions of ligand–receptor between integrins and the ECM proteins are of great concern in mediating cells or matrix adhesion, in chondrocytes mechanotransduction, in regu-lating cells proliferation and differentiation and in keeping cartilage homeostasis. However, the roles of some integrin ligands such as laminin, tenascin C, and osteopontin are not elucidated completely and thus need further investiga-tion. Clear understanding of the role of integrins and their ligands in OA cartilage may have impact on future develop-ment of successful therapeutic approaches to OA. Acknowledgments This work was supported by the Grants from the National Natural Science Foundation of China (No. 81272034, 81201420, 81472130), the Hunan Provincial Innovation Foundation for Postgraduate (CX2012B086), and the Fundamental Research Funds for the Central Universities of Central South University (2013 zzts081). Conflict of interest The authors declare that they have no conflict of interest.
References
1. Hunter DJ, Felson DT (2006) Osteoarthritis. BMJ 332:639–642
2. Arden N, Nevitt MC (2006) Osteoarthritis: epidemiology. Best
Pract Res Clin Rheumatol 20:3–25
3. Kuettner KE, Aydelotte MB, Thonar EJ (1991) Articular carti-
lage matrix and structure: a mini review. J Rheumatol Suppl 27: 46–48
4. Loeser RF (2009) Aging and osteoarthritis: the role of chon-
drocyte senescence and aging changes in the cartilage matrix.
Osteoarthritis Cartilage 17:971–979
5. Roughley PJ (2001) Articular cartilage and changes in arthritis:
noncollagenous proteins and proteoglycans in the extracellular matrix of cartilage. Arthritis Res 3:342–347
6. Eyre D (2002) Collagen of articular cartilage. Arthritis Res
4:30–35
7. Davidson RK, Waters JG, Kevorkian L, Darrah C, Cooper A,
Donell ST, Clark IM (2006) Expression profiling of metallopro-
teinases and their inhibitors in synovium and cartilage. Arthritis Res Ther 8:R124
8. Goldring MB, Goldring SR (2007) Osteoarthritis. J Cell Physiol
213:626–634
9. Hashimoto M, Nakasa T, Hikata T, Asahara H (2008) Molecular
network of cartilage homeostasis and osteoarthritis. Med Res Rev 28:464–481
10. Lin CQ, Bissell MJ (1993) Multi-faceted regulation of cell dif-
ferentiation by extracellular matrix. FASEB J 7:737–743
11. Adams JC, Watt FM (1993) Regulation of development and
differentiation by the extracellular matrix. Development 117: 1183–1198
Rheumatol Int
12. Reid DL, Aydelotte MB, Mollenhauer J (2000) Cell attachment,
collagen binding, and receptor analysis on bovine articular chondrocytes. J Orthop Res 18:364–373
13. Tamkun JW, DeSimone DW, Fonda D, Patel RS, Buck C, Hor-
witz AF, Hynes RO (1986) Structure of integrin, a glycoprotein involved in the transmembrane linkage between fibronectin and actin. Cell 46:271–282
14. Brakebusch C, Bouvard D, Stanchi F, Sakai T, Fassler R (2002)
Integrins in invasive growth. J Clin Invest 109:999–1006
15. Hynes RO (2002) Integrins: bidirectional, allosteric signaling
machines. Cell 110:673–687
16. Gahmberg CG, Fagerholm SC, Nurmi SM, Chavakis T, Mar-
chesan S, Gronholm M (2009) Regulation of integrin activity and signalling. Biochim Biophys Acta 1790:431–444
17. Schwartz MA, Ginsberg MH (2002) Networks and crosstalk:
integrin signalling spreads. Nat Cell Biol 4:E65–E68
18. Shattil SJ, Kim C, Ginsberg MH (2010) The final steps of integ-
rin activation: the end game. Nat Rev Mol Cell Biol 11:288–300 19. Kurtis MS, Schmidt TA, Bugbee WD, Loeser RF, Sah RL
(2003) Integrin-mediated adhesion of human articular chondro-
cytes to cartilage. Arthritis Rheum 48:110–118
20. Kim SJ, Kim EJ, Kim YH, Hahn SB, Lee JW (2003) The modu-
lation of integrin expression by the extracellular matrix in artic-
ular chondrocytes. Yonsei Med J 44:493–501
21. Lahiji K, Polotsky A, Hungerford DS, Frondoza CG (2004)
Cyclic strain stimulates proliferative capacity, alpha2 and alpha5 integrin, gene marker expression by human articular chondrocytes propagated on flexible silicone membranes. In Vitro Cell Dev Biol Anim 40:138–142
22. Lapadula G, Iannone F, Zuccaro C, Grattagliano V, Covelli M,
Patella V, Lo BG, Pipitone V (1997) Integrin expression on chondrocytes: correlations with the degree of cartilage damage in human osteoarthritis. Clin Exp Rheumatol 15:247–254
23. Loeser RF, Sadiev S, Tan L, Goldring MB (2000) Integrin
expression by primary and immortalized human chondrocytes: evidence of a differential role for alpha1beta1 and alpha2beta1 integrins in mediating chondrocyte adhesion to types II and VI collagen. Osteoarthritis Cartilage 8:96–105
24. Salter DM, Hughes DE, Simpson R, Gardner DL (1992) Integ-
rin expression by human articular chondrocytes. Br J Rheuma-
tol 31:231–234
25. Iannone F, Corrado A, Grattagliano V, Cantatore FP, Patella
V, Lapadula G (2001) Phenotyping of chondrocytes from human osteoarthritic cartilage: chondrocyte expression of beta integrins and correlation with anatomic injury. Reumatismo 53:122–130
26. Forster C, Kociok K, Shakibaei M, Merker HJ, V ormann J,
Gunther T, Stahlmann R (1996) Integrins on joint cartilage chondrocytes and alterations by ofloxacin or magnesium defi-
ciency in immature rats. Arch Toxicol 70:261–270
27. Salter DM, Godolphin JL, Gourlay MS (1995) Chondrocyte
heterogeneity: immunohistologically defined variation of inte-
grin expression at different sites in human fetal knees. J Histo-
chem Cytochem 43:447–457
28. Gong J, Ko TC, Brattain MG (1998) Disruption of fibronectin
binding to the alpha 5 beta 1 integrin stimulates the expres-
sion of cyclin-dependent kinases and DNA synthesis through activation of extracellular signal-regulated kinase. J Biol Chem 273:1662–1669
29. Ruoslahti E, Pierschbacher MD (1987) New perspectives in cell
adhesion: RGD and integrins. Science 238:491–497
30. Miyauchi A, Alvarez J, Greenfield EM, Teti A, Grano M,
Colucci S, Zambonin-Zallone A, Ross FP, Teitelbaum SL, Cheresh D, Et A (1991) Recognition of osteopontin and related peptides by an alpha v beta 3 integrin stimulates immediate cell signals in osteoclasts. J Biol Chem 266:20369–20374
31. Nikkari L, Haapasalmi K, Aho H, Torvinen A, Sheppard D, Lar-
java H, Heino J (1995) Localization of the alpha v subfamily of integrins and their putative ligands in synovial lining cell layer.
J Rheumatol 22:16–23
32. Camper L, Hellman U, Lundgren-Akerlund E (1998) Isolation,
cloning, and sequence analysis of the integrin subunit alpha10,
a beta1-associated collagen binding integrin expressed on chon-
drocytes. J Biol Chem 273:20383–20389
33. Enomoto M, Leboy PS, Menko AS, Boettiger D (1993) Beta 1
integrins mediate chondrocyte interaction with type I collagen, type II collagen, and fibronectin. Exp Cell Res 205:276–285
34. Pfaff M, Gohring W, Brown JC, Timpl R (1994) Binding of
purified collagen receptors (alpha 1 beta 1, alpha 2 beta 1) and RGD-dependent integrins to laminins and laminin fragments.
Eur J Biochem 225:975–984
35. Durr J, Lammi P, Goodman SL, Aigner T, von der Mark K
(1996) Identification and immunolocalization of laminin in car-
tilage. Exp Cell Res 222:225–233
36. Delwel GO, de Melker AA, Hogervorst F, Jaspars LH, Fles DL,
Kuikman I, Lindblom A, Paulsson M, Timpl R, Sonnenberg A (1994) Distinct and overlapping ligand specificities of the alpha 3A beta 1 and alpha 6A beta 1 integrins: recognition of laminin isoforms. Mol Biol Cell 5:203–215
37. Belkin AM, Stepp MA (2000) Integrins as receptors for
laminins. Microsc Res Tech 51:280–301
38. Wang H, Kandel RA (2004) Chondrocytes attach to hyaline or
calcified cartilage and bone. Osteoarthritis Cartilage 12:56–64
39. Kurtis MS, Tu BP, Gaya OA, Mollenhauer J, Knudson W,
Loeser RF, Knudson CB, Sah RL (2001) Mechanisms of chon-
drocyte adhesion to cartilage: role of beta1-integrins, CD44, and annexin V. J Orthop Res 19:1122–1130
40. Loeser RF (1997) Growth factor regulation of chondrocyte
integrins. Differential effects of insulin-like growth factor 1 and transforming growth factor beta on alpha 1 beta 1 integ-
rin expression and chondrocyte adhesion to type VI collagen.
Arthritis Rheum 40:270–276
41. Loeser RF (1994) Modulation of integrin-mediated attachment
of chondrocytes to extracellular matrix proteins by cations, reti-
noic acid, and transforming growth factor beta. Exp Cell Res 211:17–23
42. Adams MA (2006) The mechanical environment of chondro-
cytes in articular cartilage. Biorheology 43:537–545
43. Perera PM, Wypasek E, Madhavan S, Rath-Deschner B, Liu J,
Nam J, Rath B, Huang Y, Deschner J, Piesco N, Wu C, Agarwal S (2010) Mechanical signals control SOX-9, VEGF, and c-Myc expression and cell proliferation during inflammation via inte-
grin-linked kinase, B-Raf, and ERK1/2-dependent signaling in articular chondrocytes. Arthritis Res Ther 12:R106
44. Xu GK, Yang C, Du J, Feng XQ (2014) Integrin activation and
internalization mediated by extracellular matrix elasticity: a biomechanical model. J Biomech 47:1479–1484
45. Baker EL, Zaman MH (2010) The biomechanical integrin. J
Biomech 43:38–44
46. Kock LM, Schulz RM, van Donkelaar CC, Thummler CB,
Bader A, Ito K (2009) RGD-dependent integrins are mecha-
notransducers in dynamically compressed tissue-engineered cartilage constructs. J Biomech 42:2177–2182
47. Millward-Sadler SJ, Salter DM (2004) Integrin-dependent sig-
nal cascades in chondrocyte mechanotransduction. Ann Biomed Eng 32:435–446
48. Holledge MM, Millward-Sadler SJ, Nuki G, Salter DM (2008)
Mechanical regulation of proteoglycan synthesis in normal and osteoarthritic human articular chondrocytes—roles for alpha5 and alphaVbeta5 integrins. Biorheology 45:275–288
49. Wright MO, Nishida K, Bavington C, Godolphin JL, Dunne
E, Walmsley S, Jobanputra P, Nuki G, Salter DM (1997)
Rheumatol Int
Hyperpolarisation of cultured human chondrocytes following cyclical pressure-induced strain: evidence of a role for alpha 5 beta 1 integrin as a chondrocyte mechanoreceptor. J Orthop Res 15:742–747
50. Wright M, Jobanputra P, Bavington C, Salter DM, Nuki G
(1996) Effects of intermittent pressure-induced strain on the electrophysiology of cultured human chondrocytes: evidence for the presence of stretch-activated membrane ion channels.
Clin Sci (Lond) 90:61–71
51. Jablonski CL, Ferguson S, Pozzi A, Clark AL (2014) Integrin
alpha1beta1 participates in chondrocyte transduction of osmotic stress. Biochem Biophys Res Commun 445:184–190
52. Aydelotte MB, Raiss RX, Caterson B, Kuettner KE (1992)
Influence of interleukin-1 on the morphology and proteoglycan metabolism of cultured bovine articular chondrocytes. Connect Tissue Res 28:143–159
53. Amin AR, Attur M, Abramson SB (1999) Nitric oxide synthase
and cyclooxygenases: distribution, regulation, and intervention in arthritis. Curr Opin Rheumatol 11:202–209
54. Chowdhury TT, Bader DL, Lee DA (2006) Dynamic compres-
sion counteracts IL-1beta induced iNOS and COX-2 activity by human chondrocytes cultured in agarose constructs. Biorheol-
ogy 43:413–429
55. Chowdhury TT, Appleby RN, Salter DM, Bader DA, Lee DA
(2006) Integrin-mediated mechanotransduction in IL-1beta stim-
ulated chondrocytes. Biomech Model Mechanobiol 5:192–201
56. Chowdhury TT, Akanji OO, Salter DM, Bader DL, Lee DA
(2008) Dynamic compression influences interleukin-1beta-
induced nitric oxide and prostaglandin E2 release by articular chondrocytes via alterations in iNOS and COX-2 expression.
Biorheology 45:257–274
57. Orazizadeh M, Lee HS, Groenendijk B, Sadler SJ, Wright MO,
Lindberg FP, Salter DM (2008) CD47 associates with alpha 5 integrin and regulates responses of human articular chondro-
cytes to mechanical stimulation in an in vitro model. Arthritis Res Ther 10:R4
58. Orazizadeh M, Cartlidge C, Wright MO, Millward-Sadler SJ,
Nieman J, Halliday BP, Lee HS, Salter DM (2006) Mechanical responses and integrin associated protein expression by human ankle chondrocytes. Biorheology 43:249–258
59. Lee HS, Millward-Sadler SJ, Wright MO, Nuki G, Al-Jamal R,
Salter DM (2002) Activation of Integrin-RACK1/PKCalpha sig-
nalling in human articular chondrocyte mechanotransduction.
Osteoarthritis Cartilage 10:890–897
60. Whitney NP, Lamb AC, Louw TM, Subramanian A (2012) Inte-
grin-mediated mechanotransduction pathway of low-intensity continuous ultrasound in human chondrocytes. Ultrasound Med Biol 38:1734–1743
61. Hirsch MS, Lunsford LE, Trinkaus-Randall V, Svoboda KK
(1997) Chondrocyte survival and differentiation in situ are inte-
grin mediated. Dev Dyn 210:249–263
62. Goessler UR, Bugert P, Bieback K, Sadick H, Baisch A,
Hormann K, Riedel F (2006) In vitro analysis of differen-
tial expression of collagens, integrins, and growth factors in cultured human chondrocytes. Otolaryngol Head Neck Surg 134:510–515
63. Pulai JI, Del CMJ, Loeser RF (2002) The alpha5beta1 integ-
rin provides matrix survival signals for normal and osteoar-
thritic human articular chondrocytes in vitro. Arthritis Rheum 46:1528–1535
64. Raducanu A, Hunziker EB, Drosse I, Aszodi A (2009) Beta1
integrin deficiency results in multiple abnormalities of the knee joint. J Biol Chem 284:23780–23792
65. Aszodi A, Hunziker EB, Brakebusch C, Fassler R (2003) Beta1
integrins regulate chondrocyte rotation, G1 progression, and cytokinesis. Genes Dev 17:2465–2479
66. Ramachandrula A, Tiku K, Tiku ML (1992) Tripeptide RGD-
dependent adhesion of articular chondrocytes to synovial fibro-
blasts. J Cell Sci 101(Pt 4):859–871
67. Tanaka N, Ikeda Y, Yamaguchi T, Furukawa H, Mitomi H,
Nakagawa T, Tohma S, Fukui N (2013) alpha5beta1 integrin induces the expression of noncartilaginous procollagen gene expression in articular chondrocytes cultured in monolayers.
Arthritis Res Ther 15:R127
68. Goessler UR, Bugert P, Bieback K, Huber K, Fleischer LI, Hor-
mann K, Riedel F (2005) Differential modulation of integrin expression in chondrocytes during expansion for tissue engi-
neering. In Vivo 19:501–507
69. Varas L, Ohlsson LB, Honeth G, Olsson A, Bengtsson T, Wiberg
C, Bockermann R, Jarnum S, Richter J, Pennington D, John-
stone B, Lundgren-Akerlund E, Kjellman C (2007) Alpha10 integrin expression is up-regulated on fibroblast growth factor-
2-treated mesenchymal stem cells with improved chondrogenic differentiation potential. Stem Cells Dev 16:965–978
70. Marshall CJ (1994) MAP kinase kinase kinase, MAP kinase
kinase and MAP kinase. Curr Opin Genet Dev 4:82–89
71. Schulze-Tanzil G, Mobasheri A, de Souza P, John T, Shakibaei
M (2004) Loss of chondrogenic potential in dedifferentiated chondrocytes correlates with deficient Shc-Erk interaction and apoptosis. Osteoarthritis Cartilage 12:448–458
72. de Crombrugghe B, Lefebvre V, Behringer RR, Bi W, Murakami
S, Huang W (2000) Transcriptional mechanisms of chondrocyte differentiation. Matrix Biol 19:389–394
73. Woods D, Cherwinski H, Venetsanakos E, Bhat A, Gysin S,
Humbert M, Bray PF, Saylor VL, McMahon M (2001) Induc-
tion of beta3-integrin gene expression by sustained activation of the Ras-regulated Raf-MEK-extracellular signal-regulated kinase signaling pathway. Mol Cell Biol 21:3192–3205
74. Fukui N, Ikeda Y, Tanaka N, Wake M, Yamaguchi T, Mitomi
H, Ishida S, Furukawa H, Hamada Y, Miyamoto Y, Sawabe M, Tashiro T, Katsuragawa Y, Tohma S (2011) Alphavbeta5 integ-
rin promotes dedifferentiation of monolayer-cultured articular chondrocytes. Arthritis Rheum 63:1938–1949
75. Attur MG, Dave MN, Clancy RM, Patel IR, Abramson SB,
Amin AR (2000) Functional genomic analysis in arthritis-
affected cartilage: yin-yang regulation of inflammatory media-
tors by alpha 5 beta 1 and alpha V beta 3 integrins. J Immunol 164:2684–2691
76. Zemmyo M, Meharra EJ, Kuhn K, Creighton-Achermann L,
Lotz M (2003) Accelerated, aging-dependent development of osteoarthritis in alpha1 integrin-deficient mice. Arthritis Rheum 48:2873–2880
77. Parekh R, Lorenzo MK, Shin SY, Pozzi A, Clark AL (2014)
Integrin alpha1beta1 differentially regulates cytokine-mediated responses in chondrocytes. Osteoarthritis Cartilage 22:499–508 78. Almonte-Becerril M, Costell M, Kouri JB (2014) Changes
in the integrins expression are related with the osteoarthritis severity in an experimental animal model in rats. J Orthop Res 9:1161–1166
79. Ellman MB, Yan D, Ahmadinia K, Chen D, An HS, Im HJ
(2013) Fibroblast growth factor control of cartilage homeosta-
sis. J Cell Biochem 114:735–742
80. Schmidt MB, Chen EH, Lynch SE (2006) A review of the
effects of insulin-like growth factor and platelet derived growth factor on in vivo cartilage healing and repair. Osteoarthritis Car-
tilage 14:403–412
81. Ellsworth JL, Berry J, Bukowski T, Claus J, Feldhaus A, Hol-
derman S, Holdren MS, Lum KD, Moore EE, Raymond F, Ren H, Shea P, Sprecher C, Storey H, Thompson DL, Waggie K, Yao L, Fernandes RJ, Eyre DR, Hughes SD (2002) Fibroblast growth factor-18 is a trophic factor for mature chondrocytes and their progenitors. Osteoarthritis Cartilage 10:308–320
Rheumatol Int
82. Uchii M, Tamura T, Suda T, Kakuni M, Tanaka A, Miki I (2008)
Role of fibroblast growth factor 8 (FGF8) in animal models of osteoarthritis. Arthritis Res Ther 10:R90
83. Loeser RF (1997) Growth factor regulation of chondrocyte
integrins. Differential effects of insulin-like growth factor 1 and transforming growth factor beta on alpha 1 beta 1 integ-
rin expression and chondrocyte adhesion to type VI collagen.
Arthritis Rheum 40:270–276
84. Loeser RF, Shanker G, Carlson CS, Gardin JF, Shelton BJ,
Sonntag WE (2000) Reduction in the chondrocyte response to insulin-like growth factor 1 in aging and osteoarthritis: studies in a non-human primate model of naturally occurring disease.
Arthritis Rheum 43:2110–2120
85. Loeser RF (2002) Integrins and cell signaling in chondrocytes.
Biorheology 39:119–124
86. Enomoto-Iwamoto M, Iwamoto M, Nakashima K, Mukudai Y,
Boettiger D, Pacifici M, Kurisu K, Suzuki F (1997) Involve-
ment of alpha5beta1 integrin in matrix interactions and prolif-
eration of chondrocytes. J Bone Miner Res 12:1124–1132
87. Clancy RM, Rediske J, Tang X, Nijher N, Frenkel S, Philips M,
Abramson SB (1997) Outside-in signaling in the chondrocyte.
Nitric oxide disrupts fibronectin-induced assembly of a subplas-
malemmal actin/rho A/focal adhesion kinase signaling com-
plex. J Clin Invest 100:1789–1796
88. Pfander D, Rahmanzadeh R, Scheller EE (1999) Presence and
distribution of collagen II, collagen I, fibronectin, and tenas-
cin in rabbit normal and osteoarthritic cartilage. J Rheumatol 26:386–394
89. Pullig O, Weseloh G, Gauer S, Swoboda B (2000) Osteopontin
is expressed by adult human osteoarthritic chondrocytes: pro-
tein and mRNA analysis of normal and osteoarthritic cartilage.
Matrix Biol 19:245–255
90. Wurster NB, Lust G (1984) Synthesis of fibronectin in normal
and osteoarthritic articular cartilage. Biochim Biophys Acta 800:52–58
91. Brown RA, Jones KL (1990) The synthesis and accumulation of
fibronectin by human articular cartilage. J Rheumatol 17:65–72 92. Rees JA, Ali SY, Brown RA (1987) Ultrastructural localisation
of fibronectin in human osteoarthritic articular cartilage. Ann Rheum Dis 46:816–822
93. Mapp PI, Revell PA (1985) Fibronectin production by synovial
intimal cells. Rheumatol Int 5:229–237
94. Lust G, Burton-Wurster N, Leipold H (1987) Fibronectin as a
marker for osteoarthritis. J Rheumatol 14:28–29
95. Yasuda T, Poole AR (2002) A fibronectin fragment induces type
II collagen degradation by collagenase through an interleukin-
1-mediated pathway. Arthritis Rheum 46:138–148
96. Homandberg GA, Wen C, Hui F (1998) Cartilage damaging
activities of fibronectin fragments derived from cartilage and synovial fluid. Osteoarthritis Cartilage 6:231–244
97. Xie DL, Meyers R, Homandberg GA (1992) Fibronec-
tin fragments in osteoarthritic synovial fluid. J Rheumatol 19:1448–1452
98. Ding L, Guo D, Homandberg GA (2009) Fibronectin frag-
ments mediate matrix metalloproteinase upregulation and car-
tilage damage through proline rich tyrosine kinase 2, c-src, NF-kappaB and protein kinase Cdelta. Osteoarthritis Cartilage 17:1385–1392
99. Werb Z, Tremble PM, Behrendtsen O, Crowley E, Damsky
CH (1989) Signal transduction through the fibronectin recep-
tor induces collagenase and stromelysin gene expression. J Cell
Biol 109:877–889
100. Forsyth CB, Pulai J, Loeser RF (2002) Fibronectin fragments and blocking antibodies to alpha2beta1 and alpha5beta1 integrins stimulate mitogen-activated protein kinase signal-
ing and increase collagenase 3 (matrix metalloproteinase 13)
production by human articular chondrocytes. Arthritis Rheum
46:2368–2376
101. Homandberg GA, Costa V, Ummadi V, Pichika R (2002) Anti-sense oligonucleotides to the integrin receptor subunit alpha(5)
decrease fibronectin fragment mediated cartilage chondrolysis.
Osteoarthritis Cartilage 10:381–393
102. Homandberg GA, Costa V, Wen C (2002) Fibronectin fragments active in chondrocytic chondrolysis can be chemically cross-
linked to the alpha5 integrin receptor subunit. Osteoarthritis Cartilage 10:938–949
103. Chang ZL (2010) Important aspects of Toll-like receptors, ligands and their signaling pathways. Inflamm Res 59:791–808 104. Sillat T, Barreto G, Clarijs P, Soininen A, Ainola M, Pajarinen J, Korhonen M, Konttinen YT, Sakalyte R, Hukkanen M, Ylinen
P, Nordstrom DC (2013) Toll-like receptors in human chondro-
cytes and osteoarthritic cartilage. Acta Orthop 84:585–592 105. Kim HA, Cho ML, Choi HY, Yoon CS, Jhun JY, Oh HJ, Kim HY (2006) The catabolic pathway mediated by Toll-like recep-
tors in human osteoarthritic chondrocytes. Arthritis Rheum 54:2152–2163
106. Gondokaryono SP, Ushio H, Niyonsaba F, Hara M, Takenaka H, Jayawardana ST, Ikeda S, Okumura K, Ogawa H (2007) The
extra domain A of fibronectin stimulates murine mast cells via
toll-like receptor 4. J Leukoc Biol 82:657–665
107. Sofat N, Robertson SD, Wait R (2012) Fibronectin III 13-14 domains induce joint damage via toll-like receptor 4 activation
and synergize with interleukin-1 and tumour necrosis factor. J
Innate Immun 4:69–79
108. Pacifici M, Iwamoto M, Golden EB, Leatherman JL, Lee YS, Chuong CM (1993) Tenascin is associated with articular carti-
lage development. Dev Dyn 198:123–134
109. Patel L, Sun W, Glasson SS, Morris EA, Flannery CR, Chocka-lingam PS (2011) Tenascin-C induces inflammatory mediators
and matrix degradation in osteoarthritic cartilage. BMC Muscu-
loskelet Disord 12:164
110. Hasegawa M, Hirata H, Sudo A, Kato K, Kawase D, Kinoshita N, Yoshida T, Uchida A (2004) Tenascin-C concentration in synovial fluid correlates with radiographic progression of knee
osteoarthritis. J Rheumatol 31:2021–2026
111. Chockalingam PS, Glasson SS, Lohmander LS (2013) Tenas-cin-C levels in synovial fluid are elevated after injury to the
human and canine joint and correlate with markers of inflam-
mation and matrix degradation. Osteoarthritis Cartilage 21:339–345
112. Nakoshi Y, Hasegawa M, Akeda K, Iino T, Sudo A, Yoshida T, Uchida A (2010) Distribution and role of tenascin-C in human
osteoarthritic cartilage. J Orthop Sci 15:666–673
113. Sofat N, Robertson SD, Hermansson M, Jones J, Mitchell P, Wait R (2012) Tenascin-C fragments are endogenous inducers
of cartilage matrix degradation. Rheumatol Int 32:2809–2817 114. Okamura N, Hasegawa M, Nakoshi Y, Iino T, Sudo A, Imanaka-Yoshida K, Yoshida T, Uchida A (2010) Deficiency of tenascin-
C delays articular cartilage repair in mice. Osteoarthritis Carti-
lage 18:839–848
115. Asano T, Iwasaki N, Kon S, Kanayama M, Morimoto J, Minami A, Uede T (2014) Alpha9beta1 integrin acts as a critical intrin-
sic regulator of human rheumatoid arthritis. Rheumatology (Oxford) 53:415–424
116. Zhang FJ, Gao SG, Cheng L, Tian J, Xu WS, Luo W, Song Y, Yang Y, Lei GH (2013) The effect of hyaluronic acid on oste-
opontin and CD44 mRNA of fibroblast-like synoviocytes in patients with osteoarthritis of the knee. Rheumatol Int 33:79–83 117. Honsawek S, Tanavalee A, Sakdinakiattikoon M, Chayanupat-kul M, Yuktanandana P (2009) Correlation of plasma and syno-
vial fluid osteopontin with disease severity in knee osteoarthri-
tis. Clin Biochem 42:808–812
Rheumatol Int
118. Gao SG, Li KH, Zeng KB, Tu M, Xu M, Lei GH (2010) Ele-vated osteopontin level of synovial fluid and articular carti-
lage is associated with disease severity in knee osteoarthritis patients. Osteoarthritis Cartilage 18:82–87
119. Xu M, Zhang L, Zhao L, Gao S, Han R, Su D, Lei G (2013) Phosphorylation of osteopontin in osteoarthritis degenerative cartilage and its effect on matrix metalloprotease 13. Rheumatol Int 33:1313–1319
120. Attur MG, Dave MN, Stuchin S, Kowalski AJ, Steiner G, Abramson SB, Denhardt DT, Amin AR (2001) Osteopontin: an intrinsic inhibitor of inflammation in cartilage. Arthritis Rheum 44:578–584
121. Matsui Y, Iwasaki N, Kon S, Takahashi D, Morimoto J, Mat-sui Y, Denhardt DT, Rittling S, Minami A, Uede T (2009)
Accelerated development of aging-associated and instability-
induced osteoarthritis in osteopontin-deficient mice. Arthritis Rheum 60:2362–2371
122. Cheng C, Gao S, Lei G (2014) Association of osteopontin with osteoarthritis. Rheumatol Int. doi:10.1007/s00296-014-3036-9
[Epub ahead of print]
123. Ohshima S, Kobayashi H, Yamaguchi N, Nishioka K, Umeshita-Sasai M, Mima T, Nomura S, Kon S, Inobe M, Uede T, Saeki Y (2002) Expression of osteopontin at sites of bone erosion in a murine experimental arthritis model of collagen-induced arthri-
tis: possible involvement of osteopontin in bone destruction in arthritis. Arthritis Rheum 46:1094–1101
1 JAK-STAT 信号通路 1) JAK 与STAT 蛋白 JAK-STAT 信号通路是近年来发现的一条由细胞因子刺激的信号转导通路,参与细胞的增殖、分化、凋亡以及免疫调节等许多重要的生物学过程。与其它信号通路相比,这条信号通路的传递过程相对简单,它主要由三个成分组成,即酪氨酸激酶相关受体、酪氨酸激酶JAK和转录因子STAT。 (1) 酪氨酸激酶相关受体( tyrosine kinase associated receptor ) 许多细胞因子和生长因子通过JAK-STAT 信号通路来传导信号,这包括白介素2?7 (IL-2?7 )、GM-CSF (粒细胞/巨噬细胞集落刺激因子)、GH (生长激素)、EGF (表皮生长因子)、PDGF (血小板衍生因子)以及IFN (干扰素)等等。这些细胞 因子和生长因子在细胞膜上有相应的受体。这些受体的共同特点是受体本身不具有激酶活性,但胞内段具有酪氨酸激酶JAK 的结合位点。受体与配体结合后,通过与之相结合的JAK 的活化,来磷酸化各种靶蛋白的酪氨酸残基以实现信号从胞外到胞内的转递。 (2) 酪氨酸激酶JAK ( Janus kinase ) 很多酪氨酸激酶都是细胞膜受体,它们统称为酪氨酸激酶受体( receptor tyrosine kinase, RTK ),而JAK 却是一类非跨膜型的酪氨酸激酶。JAK 是英文Janus kinase 的缩写,Janus 在罗马神话中是掌管开始和终结的两面神。之所以称为两面神激酶,是因为JAK既能磷酸化与其相结合的细胞因子受体,又能磷酸化多个含特定 SH2结构域的信号分子。JAK蛋白家族共包括4个成员:JAK1、JAK2、JAK3以及Tyk2,它们在结构上有7个JAK同源结构域(JAK homology domain, JH ),其中JH1结构域为激酶区、JH2结构域是“假”激酶区、JH6和JH7是受体结合区域。 (3) 转录因子STAT ( signal transducer and activator of transcription ) STAT 被称为“信号转导子和转录激活子”。顾名思义,STAT在信号转导和转录激活上发挥了关键性 的作用。目前已发现STAT家族的六个成员,即STAT1-STAT6。STAT蛋白在结构上可分为以下几个功能区段:N-端保守序列、DNA结合区、SH3结构域、SH2结构域及C-端的转录激活区。其中,序列上最保守和功能上最重要的区段是SH2结构域,它具 有与酪氨酸激酶Src的SH2结构域完全相同的核心序列“ GTFLLRFSS ”。 2) JAK-STAT 信号通路 与其它信号通路相比,JAK-STAT 信号通路的传递过程相对简单。信号传递过程如下:细胞因子与相应的受体结合后引起受体分子的二聚化,这使得与受体偶联的JAK激酶相互接近并通过交互的酪氨酸磷酸化作用而活化。JAK激活后催化受体上的酪氨酸残 基发生磷酸化修饰,继而这些磷酸化的酪氨酸位点与周围的氨基酸序列形成“停泊位
Toll样受体信号通路的研究进展 摘要Toll样受体(Toll-like receptor,TLR)是近年来发现的一类模式识别受体,通过识别病原相关分子模式(pathogen-associated molecular pattern,PAMP)激活天然免疫。而髓样分化因子(myeloid differentiation factor 88,MyD88)是TLR信号通路中的一个关键接头分子,在传递上游信息和疾病发生发展中具有重要的作用。本文对Toll样受体、髓样分化因子88的分子结构和基本功能,及Toll样受体的信号传导通路进行了综述。 关键词Toll样受体;髓样分化因子88;信号通路;负调控机制 免疫系统识别“非我”和“自我”的过程是依赖于不同的受体来完成的,作为先天性免疫系统的重要组成部分及连接获得性免疫与先天性免疫的“桥梁”, TLRs 是生物的一种模式识别受体(pattern recognition receptor, PRR),它主要通过识别病原相关分子模式PAMPs来启动免疫反应。而MyD88是Toll受体信号通路中的一个关键接头分子,是第一个被鉴定的含TIR结构域的接头蛋白分子,在传递上游信息和疾病发生发展中具有重要的作用。 1TLR的结构与基本功能 Toll样受体一词来自对果蝇的研究,是决定果蝇背腹分化的基因所编码的一种跨膜受体蛋白,同时还参与果蝇的免疫反应,具有介导抗真菌感染信号转导的功能[1]。后来在哺乳动物也发现有与Toll受体同源的受体分子,统称为称为Toll 样受体TLRs。 TLRs是广泛分布在免疫细胞尤其非特异免疫细胞以及某些体细胞表面的一类模式识别受体,它们可以直接识别结合某些病原体或其产物所共有的高度保守的特定分子结构,即病原相关分子模式。迄今为止,已经发现哺乳动物至少有13种toll样受体,其中人的toll样受体鉴定出11种(TLR1-TLR11) [2]。TLRs识别的配基各不相同,其中TLR1-TLR5的结构已被确定,但只有TLR2与TLR4的功能被部分揭示。TLR4主要介导G-菌感染后LPS的信号转导,而TLR2主要介导G+感染后脂蛋白、脂多肽等的信号转导。它们都最终导致该转录因子的转位与相应免疫基因的活化而转录,释放前炎症因子及辅助刺激分子起到调节炎症反应的作用,从而提示TLRs可能在先天性免疫系统中起重要作用[3-4]。 TLRs家族成员具有相似的结构特征。它们均为Ⅰ型跨膜受体,由胞外区、跨膜区和胞内区3个功能区组成。胞外区序列差异大,是与配体结合的特异部位,主要包括十几至二十几个串联的富亮氨酸重复基序(leucine-rich repeats, LRRs),LRR
ATM Ataxia telangiectasia mutated (ATM) is a serine/threonine protein kinase that is recruited and activated by DNA double-strand breaks. It phosphorylates several key proteins that initiate activation of the DNA damage checkpoint, leading to cell cycle arrest, DNA repair or apoptosis. Several of these targets, including p53, CHK2 and H2AX are tumor suppressors. The protein is named for the disorder Ataxia telangiectasia caused by mutations of ATM.[1] Contents 1 Introduction 2 Structure 3 Function 4 Regulation 5 Role in cancer 6 Interactions 7 See also 8 References 9 Further reading 10 External links Introduction[edit] Throughout the cell cycle the DNA is monitored for damage. Damages result from errors during replication, by-products of metabolism, general toxic drugs or ionizing radiation. The cell cycle has different DNA damage checkpoints, which inhibit the next or maintain the current cell cycle step. There are two main checkpoints, the G1/S and the G2/M, during the cell cycle, which preserve correct progression. ATM plays a role in cell cycle delay after DNA damage, especially after double-strand breaks (DSBs).[2] ATM together with NBS1 act as primary DSB sensor proteins. Different mediators, such as Mre11 and MDC1, acquire post-translational modifications which are generated by the sensor proteins. These modified mediator proteins then amplify the DNA damage signal, and transduce the signals to downstream effectors such as CHK2 and p53. Structure[edit] The ATM gene codes for a 350 kDa protein consisting of 3056 amino acids.[3] ATM belongs to the superfamily of Phosphatidylinositol 3-kinase-related kinases (PIKKs). The PIKK superfamily comprises six Ser/Thr-protein kinases that show a sequence similarity to phosphatidylinositol 3-kinases (PI3Ks). This protein kinase family includes amongst others ATR (ATM- and RAD3-related), DNA-PKcs (DNA-dependent protein kinase catalytic subunit) and mTOR (mammalian target of rapamycin). Characteristic for ATM are five domains. These are from N-Terminus to C-Terminus the HEAT repeat domain, the FRAP-ATM-TRRAP (FAT) domain, the kinase domain (KD), the PIKK-regulatory domain (PRD) and the FAT-C-terminal (FATC) domain. The
1 JAK-STAT信号通路 1) JAK与STAT蛋白 JAK-STAT信号通路是近年来发现的一条由细胞因子刺激的信号转导通路,参与细胞的增殖、分化、凋亡以及免疫调节等许多重要的生物学过程。与其它信号通路相比,这条信号通路的传递过程相对简单,它主要由三个成分组成,即酪氨酸激酶相关受体、酪氨酸激酶JAK和转录因子STAT。 (1) 酪氨酸激酶相关受体(tyrosine kinase associated receptor) 许多细胞因子和生长因子通过JAK-STAT信号通路来传导信号,这包括白介素2?7(IL-2?7)、GM-CSF(粒细胞/巨噬细胞集落刺激因子)、GH(生长激素)、EGF(表皮生长因子)、PDGF (血小板衍生因子)以及IFN(干扰素)等等。这些细胞因子和生长因子在细胞膜上有相应的受体。这些受体的共同特点是受体本身不具有激酶活性,但胞内段具有酪氨酸激酶JAK的结合位点。受体与配体结合后,通过与之相结合的JAK的活化,来磷酸化各种靶蛋白的酪氨酸残基以实现信号从胞外到胞内的转递。 (2) 酪氨酸激酶JAK(Janus kinase) 很多酪氨酸激酶都是细胞膜受体,它们统称为酪氨酸激酶受体(receptor tyrosine kinase, RTK),而JAK却是一类非跨膜型的酪氨酸激酶。JAK是英文Janus kinase的缩写,Janus在罗马神话中是掌管开始和终结的两面神。之所以称为两面神激酶,是因为JAK既能磷酸化与其相结合的细胞因子受体,又能磷酸化多个含特定SH2结构域的信号分子。JAK蛋白家族共包括4个成员:JAK1、JAK2、JAK3以及Tyk2,它们在结构上有7个JAK同源结构域(JAK homology domain, JH),其中JH1结构域为激酶区、JH2结构域是“假”激酶区、JH6和JH7是受体结合区域。 (3) 转录因子STAT(signal transducer and activator of transcription)STAT被称为“信号转导子和转录激活子”。顾名思义,STAT在信号转导和转录激活上发挥了关键性的作用。目前已发现STAT家族的六个成员,即STAT1-STAT6。STAT蛋白在结构上可分为以下几个功能区段:N-端保守序列、DNA结合区、SH3
cAMP信号通路 信号分子:1.激素 2.局部介质3.神经递质 受体:G蛋白偶联受体 胞内应答过程:激素→G蛋白耦联受体→G蛋白→腺苷酸环化酶→cAMP→依赖cAMP的蛋白激酶A→基因调控蛋白→基因转录 举例:1.多发性骨髓瘤:通过调变细胞内环腺苷酸浓度可以诱导多种肿瘤细胞增殖阻滞和凋亡,成为肿瘤治疗新途径。 2.肝损伤:对乙酰氨基酚致药物性肝脏损伤可能与cAMP-PKA 信号通路有关。 3.研究人员已经确定了这其中的机制,现在,一种能抑制Epac的新的候选药物——称为ESI Epac特异性抑制剂,也已经被证明能够保护正常小鼠免受致命性立克次氏体感染。目前,研究人员正在设计第二代ESI——更有效,即使在最高剂量也无毒。也有来自预备试验的迹象表明,ESI能够保护动物抗击一些致命的病毒感染。 磷脂酰肌醇信号通路 信号分子:1.激素 2.局部介质3.神经递质 受体:酶耦联型受体 胞内应答过程:Ca2+活化各种Ca2+结合蛋白引起细胞反应,钙调素(calmodulin,CaM)由单一肽链构成,具有四个钙离子结合部位。结合钙离子发生构象改变,可激活钙调素依赖性激酶(CaM-Kinase)。细胞对Ca2+的反应取决于细胞内钙结合蛋白和钙调素依赖性激酶的种类。 IP3信号的终止是通过去磷酸化形成IP2,或被磷酸化形成IP4。Ca2+由质膜上的Ca2+泵和Na+-Ca2+交换器将抽出细胞,或由内质网膜上的钙泵抽进内质网 DG通过两种途径终止其信使作用:一是被DG-激酶磷酸化成为磷脂酸,进入磷脂酰肌醇循环;二是被DG酯酶水解成单酯酰甘油。由于DG代谢周期很短,不可能长期维持PKC活性,而细胞增殖或分化行为的变化又要求PKC长期活性所产生的效应。现发现另一种DG生成途径,即由磷脂酶催化质膜上的磷脂酰胆碱断裂产生的DG,用来维持PKC的长期效应。 举例:1.肿瘤治疗:该通路调节肿瘤细胞的增殖和存活,其活性异常不仅能导致细胞恶性转化,而且与肿瘤细胞的迁移、黏附、肿瘤血管生成以及细胞外基质的降解等相关。 2.肝癌:PIK3R1在肝癌组织中表达上调,PIK3R1可能通过激活PI3K/AKT信号通路促进HepG2细胞的增殖. 生物技术15-1 曹文祥
Rheumatol Int DOI 10.1007/s00296-014-3137-5 Role of integrins and their ligands in osteoarthritic cartilage Jian Tian · Fang?Jie Zhang · Guang?Hua Lei Received: 25 May 2014 / Accepted: 17 September 2014 ? Springer-Verlag Berlin Heidelberg 2014 [1]. Radiographic evidence of OA occurs in the majority of people by 65 years of age, and among them about 80 % in people who aged over 75 years [2]. However, the pathogen-esis of this disease is not fully elucidated. Cartilage damage is one of the major pathological changes in OA. Articular cartilage is an avascular, a neu-ral, alymphatic, and viscoelastic connective tissue that functions autonomously to bear loads and provide almost friction-free movement of diarthrodial joints [3]. Chondro-cytes, the only cell population of adult articular cartilage, are strongly involved in maintaining the dynamic equi-librium between synthesis and degradation of the extra-cellular matrix (ECM) [4]. Collagens represent the major structural components of the articular cartilage. Cartilage is made up of two main ECM macromolecules: type II collagen and aggrecan, a large aggregating proteoglycan [5, 6]. Cartilage destruction is thought to be mediated by two main enzyme families: the matrix metalloproteinases (MMPs) are responsible for the cartilage collagen break-down, whereas enzymes from disintegrin and metallopro-teinase domain with thrombospondin motifs (ADAMTS) family mediate cartilage aggrecan loss [7]. Activation of biochemical pathways involves the production of proin-flammatory cytokines, inflammation, degradation of the ECM by MMPs and ADAMTS, and cessation of ECM syn-thesis via dedifferentiation and apoptosis of chondrocytes [8, 9]. Therefore, the ECM is a vital cellular environment, and interactions between the cell and ECM are important in regulating many biological processes, which include cell growth, differentiation, and survival [10, 11]. Cell–matrix interactions control cell function and behav-ior by signal transduction through a variety of cell sur-face receptors. The integrins are the major family of ECM receptors, which can transmit information from the matrix to the cell. Integrin binding of ECM ligands results in the Abstract Osteoarthritis (OA) is a degenerative disease, which is characterized by articular cartilage destruction, and mainly affects the older people. The extracellular matrix (ECM) provides a vital cellular environment, and interactions between the cell and ECM are important in reg-ulating many biological processes, including cell growth, differentiation, and survival. However, the pathogenesis of this disease is not fully elucidated, and it cannot be cured totally. Integrins are one of the major receptors in chondro-cytes. A number of studies confirmed that the chondrocytes express several integrins including α5β1, αV β3, αV β5, α6β1, α1β1, α2β1, α10β1, and α3β1, and some integrins ligands might act as the OA progression biomarkers. This review focuses on the functional role of integrins and their extracellular ligands in OA progression, especially OA car-tilage. Clear understanding of the role of integrins and their ligands in OA cartilage may have impact on future develop-ment of successful therapeutic approaches to OA.Keywords Chondrocyte · Integrin · Fibronectin · Tenascin C · Osteopontin · Osteoarthritis · Cartilage Introduction Osteoarthritis (OA) is a degenerative disease and is char-acterized by articular cartilage destruction along with changes occurring in other joint components including bone, menisci, synovium, ligaments, capsule, and muscles Rheumatology INTERNATIONAL J. Tian · F.-J. Zhang · G.-H. Lei (*) Department of Orthopaedics, Xiangya Hospital, Central South University, No. 87 Xiangya Road, Changsha 410008, Hunan, China e-mail: gh.lei9640@https://www.doczj.com/doc/4111661342.html,; lgh9640@https://www.doczj.com/doc/4111661342.html,
Toll样受体信号通路图 TLR家族成员(TLR3除外)诱导的炎症反应都经过一条经典的信号通路(图1),该通路起始于TLRs的一段胞内保守序列—Toll/IL-1受体同源区(Toll/IL-1receptorhomologousregion,TIR).TIR可激活胞内的信号介质—白介素1受体相关蛋白激酶(IL-1Rassociatedkinase,IRAK)IRAK-1和IRAK-4、肿瘤坏死因子受体相关因子6(TNFR-associatedfactor6,TRAF-6)、促分裂原活化蛋白激酶(mitogenactivatedproteinkinase,MAPK)和IκB激酶(IκBkinase,IκK),进而激活核因子κB(nuclearfactorκB,NF-κB),诱导炎症因子的表达。 Toll-liker Receptor Signaling 本信号转导涉及的信号分子主要包括: CD14,MD-2,TRAM,TRIF,TIRAP,MyD88,TLR1,TLR2,TLR3,TLR4,TLR5,TLR6,TLR7,TLR8,TLR9,IRAK-1,IRAK-2,IRAK-4,IRAK-M,TRAF6,TRIAD3A,ST2L,SOCS1,RIG-I,FADD,TOLLIP,RIP1,A20,UEV1A,Ubc13,ECSIT,MEKK-1,TAK1,
TBK1,MKK3/6,p38,TAB1/2,MKK4/7,JNK,IKKα,IKKβ,IKKγ,IKKε,NEMO,IκBα,NF-κB,p65/RelA,Casp-8,IRF-3,IRF-7,MA VS等
TOLL样受体7(TLR7)增殖分化信号通路论文 【提示】本文仅提供摘要、关键词、篇名、目录等题录内容。为中国学术资源库知识代理,不涉版权。作者如有疑义,请联系版权单位或学校。 【摘要】目的探讨TLR7的激活对HaCaT细胞增殖与分化的影响及其可能的机制。方法培养HaCaT细胞,以不同剂量的TLR7配体Gardiquimod经不同的时间体外刺激HaCaT细胞,MTT及流式细胞术分析TLR7的激活对HaCaT细胞增殖的影响。以不同剂量的TLR7配体Gardiquimod经不同的时间体外刺激HaCaT细胞,加入氯化钙诱导HaCaT细胞分化,Western-Blot分析HaCaT细胞的分化Markers(颗粒层:Keratin1,基底层:Keratin5和棘层:Involucrin)并以此分析TLR7的激活对氯化钙诱导HaCaT细胞分化的影响。 Western-blotting分析TLR7在HaCaT细胞中激活的信号通路 PI3K-AKT和RAS-MAPK等。在TLR7配体Gardiquimod处理HaCaT细胞前1h,分别加入特异性阻断剂(PD98059及LY2940002)阻断TLR7配体Gardiquimod激活的相关信号通路,然后分析阻断剂对TLR7配体Gardiquimod调控HaCaT细胞增殖及分化影响,从而探讨PI3K-AKT 和RAS-MAPK信号通路在TLR7配体Gardiquimod对HaCaT细胞增殖及分化调控中的作用。结果MTT及流式细胞分析结果显示:TLR7配体Gardiquimod促进HaCaT细胞增殖,且具有时间及剂量依赖性;TLR7配体Gardiquimod能够抑制氯化钙诱导的HaCaT细胞分化markers (Keratin1及Involucrin)的表达,存在时间效应及剂量效应;信号通路分析揭示TLR7配体Gardiquimod能够增加ERK1/2和MAPK的水平;阻断剂的研究发现TLR7配体Gardiquimod部分依赖PI3K-AKT
Toll 样受体(TLRs)是一个模式识别受体家族,它们在进化上高度保守,从线虫到哺乳 动物都存在TLRs,目前在哺乳动物中已发现 12 个成员[1].TLRs 主要表达于抗原递 呈细胞及一些上皮细胞,为玉型跨膜蛋白,胞外区具有富含亮氨酸的重复序列,能够 特异识别病原微生物进化中保守的抗原分子———病原相关分子模式 (pathogen-associatedmolecular patterns, PAMPs)[2].为了有效地抵抗入侵的病原体,机体需要对多种 PAMPs 产生适当的免疫应答,TLRs 可以通过识别 PAMPs 诱发抵抗病原体的免疫反应.而且 TLRs 也参与识别有害的内源性物质.TLRs 的激活可诱导很强的免疫反应,有利于机体抵抗病原体感染或组织损伤,但是过度的免疫反应也会带来不利影响,如产生内毒素休克、自身免疫性疾病等.为了保证 TLRs 介导正确的免疫应答,机体 存在精密的负调控机制,及时抑制 TLRs 信号,维持机体的免疫平衡[3]TLR 家族成员(TLR3 除外)诱导的炎症反应都经过一条经典的信号通路(图 1),该通路起始于TLRs 的一段胞内保守序列———Toll/IL-1 受体同源区(Toll/IL-1 receptor homologous region,TIR).TIR可激活胞内的信号介质———白介素 1 受体相关蛋白激酶 (IL-1R associated kinase, IRAK) IRAK-1 和IRAK-4、肿瘤坏死因子受体相关因子 6(TNFR-associated factor 6, TRAF-6)、促分裂原活化蛋白激酶(mitogen activated protein kinase,MAPK)和 I资B激酶 (I资B kinase, I资K ),进而激活核因子资 B(nuclear factor 资B,NF-资B),诱导炎症因子的表达.TLRs 信号通路上的许多接头蛋白都具有 TIR结构域:髓系分化因子 88(myeloid differentiationfactor 88, MyD88)、MyD88- 接头蛋白相似物(MyD88-adaptor like,Mal)、含有 TIR 结构能诱导干扰 素茁的接头分子 (TIR domain-containingadaptor inducing interferon 茁,TRIF)、TRIF 相关接头分子(TRIF-related adaptor molecule,TRAM)和SARM (sterile 琢 and armadillo motif-containingprotein)[4].它们参与 TLRs 所介导的信号转导,其中 MyD88 最重要,参与了除 TLR3 外所有 TLRs介导的信号转导.MyD88 首先通过 TIR 与 TLRs 相结合,接着募集下游信号分子 IRAK-4,IRAK-4 磷酸化激活IRAK-1,随后 活化 TRAF6.活化的 TRAF6 具有泛素连接酶(E3)的活性,能够结合泛素结合酶(E2),进而泛素化降解 IKK-酌.这种泛素化降解可以活化TGF-茁激酶(TGF-茁 activated kinase 1, TAK1) 和TAK1 结合蛋白 (TAK1 binding protein, TAB1、TAB2、 TAB3).活化的 TAK1 会催化 IKK-茁磷酸化,最终激活 NF-资B,促使炎症因子的表达.除了共同的 NF-资B 激活通路,不同的 TLRs 还存在着其特有的信号通路,一些TLRs 具有募集 Mal、TRAM 和 TRIF 的作用.不同的接头分子在信号传导中发挥的作 用不同[5],TRIF 在脂多糖(LPS)激活的 TLR4 途径和 Poly(I∶C)激活的 TLR3 途径中都起到了重要的作用,而 TRAM 仅在 TLR4 的途径中发挥作用.TLRs 的激活是一把双刃剑,它可以通过刺激先天性免疫应答和提高获得性免疫反应来保护机体,但是它所引 起的持续性炎症反应也会对机体产生损伤,自身免疫、慢性炎症和感染性疾病都与它 有一定关系.例如LPS 持续刺激TLR4 就可以引起严重的败血病和感染性休克,此外,类风湿性关节炎、慢性阻塞性肺心病、结肠炎、哮喘、心肌病、狼疮和动脉粥样硬化
彭英才教授,博士生导师,河北大学电子信息工程学院,保定071002 赵新为副教授,日本东京理科大学理学部,河北大学客座教授 刘明研究员,中国科学院微电子研究中心,北京100029 1福间雅夫.应用物理(日文,2002;71:964 2Ono Y.,et al.IEEE Trans.Electron Devices,2000;47:147 3W ang T.H.,et al.Appl.Phys.Lett.,2001;78:2160 4Dutta A.,et al.Jpn.J.Appl.Phys.,2000;39:4647 5李国华.物理,2001;30:436 6裕之.电子通信学会志(日文,1997;80:717 7Peng Y.C.,et al.Semiconductor Photonics and Technology,2000;6:129 8W ang Z.G.,et al.Science in China,2000;43:861 9Hu ffaker P.L.,et al.Appl.Phys.Lett.,1997;70:1781 10王占国.世界科技研究与发展,2000;22:111徐少辉等.物理,2002;31:558 12K ane B.E.Nature,1998;393:133 13Smet J.H.,et al.Nature,2002;415:281 Several Active Fields in the N anometer Q uantum De2 vices Peng Y ing2cai①,Zhao X in2wei②,Liu Ming③ ①Pro fessor,Supervisor o f Ph.D.Candidates,College o f Electronic and In2 formational Engineering,H ebei Univer sity,Baoding071002
细胞受体类型、特点 及重要的细胞信号转导途径 学院:动物科学技术学院 专业:动物遗传育种与繁殖 姓名:李波 学号:2015050509
目录 1、细胞受体类型及特点 (3) 1.1离子通道型受体 (3) 1.2 G蛋白耦联型受体 (3) 1.3 酶耦联型受体 (3) 2、重要的细胞信号转导途径 (4) 2.1细胞内受体介导的信号传递 (4) 2.2 G蛋白偶联受体介导的信号转导 (5) 2.2.1激活离子通道的G蛋白偶联受体所介导的信号通路 (5) 2.2.2激活或抑制腺苷酸环化酶的G蛋白偶联受体 (5) 2.2.3 激活磷脂酶C、以lP3和DAG作为双信使 G蛋白偶联受体介导的信号通路 (6) 2.2 酶联受体介导的信号转导 (7) 2.2.1 受体酪氨酸激酶及RTK-Ras蛋白信号通路 (7) 2.2.2 P13K-PKB(Akt)信号通路 (8) 2.2.3 TGF-p—Smad信号通 (8) 2.2.4 JAK—STAT信号通路 (9)
1、细胞受体类型及特点 受体(receptor)是一种能够识别和选择性结合某种配体(信号分子)的大分子物质,多为 糖蛋白,一般至少包括两个功能区域,与配体结合的区域和产生效应的区域,当受体与配 体结合后,构象改变而产生活性,启动一系列过程,最终表现为生物学效应。受体与配体 问的作用具有3个主要特征:①特异性;②饱和性;③高度的亲和力。 根据靶细胞上受体存在的部位,可将受体分为细胞内受体(intracellular receptor)和细 胞表面受体(cell surface receptor)。细胞内受体介导亲脂性信号分子的信息传递,如胞内 的甾体类激素受体。细胞表面受体介导亲水性信号分子的信息传递,膜表面受体主要有三类:①离子通道型受体(ion—channel—linked receptor);②G蛋白耦联型受体(G—protein —linked receptor);③酶耦联的受体(enzyme—linked recep—tor)。第一类存在于可兴奋 细胞。后两类存在于大多数细胞,在信号转导的早期表现为激酶级联事件,即为一系列蛋 白质的逐级磷酸化,借此使信号逐级传送和放大。 1.1离子通道型受体 离子通道型受体是一类自身为离子通道的受体,即配体门通道(1igand—gated channel),主要存在于神经、肌肉等可兴奋细胞,其信号分子为神经递质。神经递质通过 与受体的结合而改变通道蛋白的构象,导致离子通道的开启或关闭,改变质膜的离子通透性,在瞬间将胞外化学信号转换为电信号,继而改变突触后细胞的兴奋性。如:乙酰胆碱 受体以三种构象存在,两分子乙酰胆碱的结合可以使之处于通道开放构象,但该受体处于 通道开放构象状态的时限仍十分短暂,在几十毫微秒内又回到关闭状态。然后乙酰胆碱与 之解离,受体则恢复到初始状态,做好重新接受配体的准备。离子通道型受体分为阳离子 通道,如乙酰胆碱、谷氨酸和五羟色胺的受体,和阴离子通道。 1.2 G蛋白耦联型受体 三聚体GTP结合调节蛋白(trimeric GTP—binding regulatory protein)简称G蛋白, 位于质膜胞质侧,由a、p、-/三个亚基组成,a和7亚基通过共价结合的脂肪酸链尾结合在膜上,G蛋白在信号转导过程中起着分子开关的作用,当a亚基与GDP结合时处于关闭 状态,与GTP结合时处于开启状态,“亚基具有GTP酶活性,能催化所结合的ATP水解,恢复无活性的三聚体状态,其GTP酶的活性能被RGS(regulator of G protein signaling)增强。RGS也属于GAP(GTPase activating protein)。 G蛋白耦联型受体为7次跨膜蛋白(图10—6),受体胞外结构域识别胞外信号分子并 与之结合,胞内结构域与G蛋白耦联。通过与G蛋白耦联,调节相关酶活性,在细胞内产 生第二信使,从而将胞外信号跨膜传递到胞内。G蛋白耦联型受体包括多种神经递质、肽 类激素和趋化因子的受体,在味觉、视觉和嗅觉中接受外源理化因素的受体亦属G蛋白耦 联型受体。 1.3 酶耦联型受体 酶耦联型受体(enzyme linked receptor)分为两类,其一是本身具有激酶活性,如肽类 生长因-子(EGF,PDGF,CSF等)受体;其二是本身没有酶活性,但可以连接非受体酪氨酸 激酶,如细胞因子受体超家族。这类受体的共同点是:①通常为单次跨膜蛋白;②接受配 体后发生二聚化而激活,起动其下游信号转导。
Toll样受体、信号通路及其免疫的研究 Toll样受体最早是在研究果蝇胚胎发育过程中发现的,它不仅是果蝇胚胎发育过程中的必需蛋白,而且在免疫应答过程中具有重要作用[1]。Toll 样受体(TLRs)是一个模式识别受体家族,它们在进化上高度保守,从线虫到哺乳动物都存在TLRs,它能识别病原微生物进化中保守分子,如脂多糖(LPs)、肽聚糖、酵母多糖以及病原微生物的核酸等等.脂多糖受体TLR4是发现的第一个TLRs,至今在动物中已经发现15种TLRs(在人体已经发现11个成员,即TLRl~TLRl0和TLRl4,小鼠不表达TLR10,但发现了TLR11—13[2],在鸡中发现了TLR15[3]。哺乳动物的TLRs同果蝇的TLRs一样,同属于I型跨膜蛋白,主要由3个功能区构成:胞外区、跨膜区和胞内区。胞外区具有富含亮氨酸的重复序列,能够特异识别病原微生物进化中保守的抗原分子——病原相关分子模式(pathogen-associated molecular patterns, PAMPs)[4]。为了有效地抵抗入侵的病原体,机体需要对多种PAMPs产生适当的免疫应答,TLRs可以通过识别PAMPs诱发抵抗病原体的免疫反应。而且TLRs也参与识别有害的内源性物质. 1. Toll样受体 1.1 Toll样受体的发现Toll是在昆虫中发现的一个受体蛋白,参与昆虫胚胎发育时背腹肌极性的建立。进一步研究发现,Toll胞内区与哺乳动物中自介素-1受体(IL-1R)的胞内区具有很高的同源性,下游的信号转导通路通过NF—kB样因子发挥作用。IL-1R是免疫相关分子,而且昆虫中抗微生物的多肽基因上游大多有NF—kB样因子结合位点,是否Toll蛋白也参与昆虫的天然免疫反应调控?研究证实Toll参与昆虫的抗真菌免疫.真菌感染时果蝇Toll 通路被激活,诱导大量的抗真菌肽Drosomycin,Toll的突变导致果蝇极易受到真菌的感染[1]。.哺乳动物存在Toll的同源分子,即TLRs。TLRs是一个受体家族。 1.2 TLRs分子特征TLRs为一类Ⅰ型跨膜蛋白,其细胞外区域存在由18~31个氨基酸组成的富含亮氨酸的重复单位(LRR motif)XLXXLXLXXL(X代表任何氨基酸,L为亮氨酸)每个LRR由24~29个氨基酸组成,为8折叠一环一a螺旋的结构。整个LRR结构域形成一个马蹄型的结构,参与识别各种病原体。它们的细胞外区域较长,在550~980氨基酸之间,而且同源性较差,如TLR2与TLR4细胞外区域的同源性只有24%。提示TLRs各个分子之间所结合的配体具有不同的结构、性质;但各个分子种属间的差异较小,如人和小鼠的TLR4胞外区有53%相同,而胞质区则高达83%,提示着它们是一组非常保守的分子,执行着相似的功能。TLRs的胞内区含有Toll/IL-1受体同源(Toll/IL-1 receptor homologous region, TIR), 其中包括3个保守盒(conserved boxes),参与信号转导。TIR是一个保守结构,其中的23个氨基酸的位置是固定的,所形成的三个结构域分别为这些分子的标志区域和信号介导区域。具有TIR结构域[5]分子现在发现的共有31种,如MyD88、IL-1相关蛋白激酶(IRAK)、肿瘤坏死因子受体相关因子6(TRAF6)等。 1.3 TLRs的配体(PAMP)及其特异性TLRs配体按来源可分为外源性和内源性配体。外源性配体主要来自病原微生物,是微生物进化过程中的保守成分,如细菌的脂多糖、胞壁酸、肽聚糖以及细菌和病毒的核酸等。内源性配体来自宿主细胞,如热休克蛋白、细胞外基质降解成分等等,内源性配体在机体应激或是组织损伤时释放[6,7]。TLR4识别G-菌的LPS;TLR2可识别G+菌、分枝杆菌及真菌的PAMP。TLR9识别细菌特殊序列胞嘧啶磷酸鸟(CpG-DNA);TLR5 识别细菌鞭毛蛋白。 目前对TLR生物学作用研究的焦点集中在介导对LPS的反应,而LPS的生物活性成分是脂质A。3种天然对大剂量LPS耐受的小鼠C3H/HeJ、C57BL/10ScCr、C57BL/10ScN,