硫酸氢氯吡格雷片(波立维)
- 格式:pdf
- 大小:145.97 KB
- 文档页数:7
硫酸氢氯吡格雷片的功效与作用
硫酸氢氯吡格雷片是一种常用的抗血小板药物,它主要的功效和作用包括以下几个方面。
第一,抗血小板聚集作用。
使用硫酸氢氯吡格雷片可以抑制血小板的聚集,减少血小板在血管内壁上的黏附,避免血栓的形成。
这是硫酸氢氯吡格雷片用于预防和治疗心脑血管疾病的主要作用。
血小板聚集是心脑血管疾病的重要机制之一,因此使用硫酸氢氯吡格雷片可以有效预防和治疗心脑血管疾病的发生和进展。
第二,预防心脏病发作。
硫酸氢氯吡格雷片可用于预防冠心病、心肌梗死和心绞痛等心脏疾病的发作。
冠心病是一种常见的心脏疾病,其主要病因是冠状动脉发生狭窄或闭塞,导致心肌缺血。
硫酸氢氯吡格雷片可以有效地抑制血小板聚集,防止血栓形成,减少心肌缺血和心脏病发作的风险。
第三,预防血栓栓塞。
硫酸氢氯吡格雷片还可用于预防血栓栓塞疾病,如深静脉血栓形成和肺栓塞。
血栓栓塞是一种严重的血管疾病,它会导致血管堵塞,影响血液循环和器官功能。
硫酸氢氯吡格雷片可以阻止血小板聚集和血栓形成,减少血管阻塞的发生,预防血栓栓塞的发生。
总的来说,硫酸氢氯吡格雷片是一种常用的抗血小板药物,其功效与作用主要包括抗血小板聚集、预防心脏病发作和预防血栓栓塞。
它可以有效预防和治疗心脑血管疾病的发生和进展,降低心脏病和血管疾病的风险。
然而,在使用硫酸氢氯吡格雷
片时,应注意遵医嘱使用,避免因个体差异和药物相互作用等原因造成不良反应。
核准日期:硫酸氢氯吡格雷片说明书请仔细阅读说明书并在医师指导下使用【药品名称】通用名:硫酸氢氯吡格雷片英文名:Clopidogrel Hyd rogen Sulphate Tablets汉语拼音:Liusuanqinglubigelei Pian本品主要成份为:硫酸氢氯吡格雷化学名称为::甲基(+)-(s)-α-邻氯苯基-6,7-二氢噻吩[3,2-C]吡啶-5(4H)-乙酸酯硫酸氢盐,其结构式为:分子式:C16H16ClNO2S·H2SO4分子量:419.9【性状】硫酸氢氯吡格雷片75mg 薄膜衣片剂呈粉红色,圆形双凸,薄膜包衣,一面刻有《75》,另一面刻有《1171》字样。
【适应症】氯吡咯雷用于以下患者的预防动脉粥样硬化血栓形成事件:·心肌梗死患者(从几天到小于35 天)、缺血性卒中患者(从7 天到小于6 个月)或确诊外周动脉性疾病的患者。
·急性冠脉综合征的患者-非ST 段抬高性急性冠脉综合征(包括不稳定性心绞痛或非Q波心肌梗死),包括经皮冠状动脉介入术后置入支架的患者,与阿司匹林合用。
-用于ST 段抬高性急性冠脉综合征患者,与阿司匹林联合,可合并在溶栓治疗中使用。
【规格】75 mg【用法用量】成人和老年人硫酸氢氯吡格雷片的推荐剂量为每天75mg,与或不与食物同服。
对于急性冠脉综合征的患者:-非ST 段抬高性急性冠脉综合征(不稳定性心绞痛或非Q波心肌梗死)患者,应以单次负荷量氯吡格雷300 mg开始,然后以75 mg每日1 次连续服药(合用阿司匹林75 mg-325 mg/日)。
由于服用较高剂量的阿司匹林有较高的出血危险性,故推荐阿司匹林的剂量不应超过100 mg。
最佳疗程尚未正式确定。
临床试验资料支持用药12个月,用药3个月后表现出最大效果。
-ST段抬高性急性心肌梗死:应以负荷量氯吡格雷开始,然后以75 mg每日1次,合用阿司匹林,可合用或不合用溶栓剂。
对于年龄超过75岁的患者,不使用氯吡格雷负荷剂量。
硫酸氢氯吡格雷片证明书籍之阳早格格创做请留神阅读证明书籍并正在医师指挥下使用【药品称呼】通用称呼:硫酸氢氯吡格雷片商品称呼:波坐维PLAVIX英文称呼:Clopidogrel Hydrogen Sulphate Tablets汉语拼音:Liusuanlubigelei Pian【成份】化教称呼:甲基(+)-(S)--邻氯苯基-6,7-二氢噻吩[3,2-C]吡啶-5(4H)-乙酸酯硫酸氢盐化教结构式:分子式:C16H16ClNO2S H2SO4分子量:419.9【性状】波坐维75mg薄膜衣片剂呈粉黑色,圆形单凸,薄膜包衣,部分刻有《75》,另部分刻有《1171》字样.【切合症】氯吡格雷用于以下患者的防止动脉粥样软化血栓产死事变:●心肌梗死患者(从几天到小于35天),缺血性卒中患者(从7天到小于6个月)或者确诊中周动脉性徐病的患者.●慢性冠脉概括征的患者‐非ST段抬下性慢性冠脉概括征(包罗不宁静性心绞痛或者非Q波心肌梗死),包罗经皮冠状动脉介进术后置进支架的患者,与阿司匹林合用.‐用于ST段抬下性慢性冠脉概括征患者,与阿司匹林共同,可合并正在溶栓治疗中使用.【规格】75mg【用法用量】●成人战老年人波坐维的推荐剂量为每天75mg,与或者不与食物共服.对付于慢性冠脉概括征的患者:‐非ST段抬下性慢性冠脉概括征(不宁静性心绞痛或者非Q波心肌梗死)患者,应以单次背荷量氯吡格雷300mg启初,而后以75mg每日1次连绝服药(合用阿司匹林75mg-325mg/日).由于服用较下剂量的阿司匹林有较下的出血伤害性,故推荐阿司匹林的剂量不该超出100mg.最好疗程尚已正式决定.临床考查资料支援用药12个月,用药3个月后表示出最大效验.‐ST段抬下性慢性心肌梗死:应以背荷量氯吡格雷启初,而后以75mg每日1次,合用阿司匹林,可合用或者分歧用溶栓剂.对付于年龄超出75岁的患者,不使用氯吡格雷背荷剂量.正在症状出现后应尽早启初共同治疗,并起码用药4周.暂时还不钻研对付共同使用氯吡格雷战阿司匹林超出4周后的获益举止证据(拜睹药效教个性).●女童战已成年人:尚无正在女童中使用的体味.【不良反应】临床钻研体味:已正在42,000多例患者中对付氯吡格雷的仄安性举止了评介,其中9000例患者治疗很多于1年.正在CAPRIE,CURE,CLARITY战COMMIT中瞅察到的临床相关不良反应将正在以下举止计划.正在CAPRIE钻研中,与阿司匹林325mg/日相比,氯吡格雷75mg/日的耐受性较好.正在该钻研中,氯吡格雷的总体耐受性与阿司匹林相似,与年龄、性别及种族无关.出血性徐患:正在CAPRIE钻研,交受氯吡格雷或者阿司匹林治疗的患者,出血事变的总体爆收率均为9.3%.氯吡格雷、阿司匹林所致宽沉出血事变的爆收率分别为1.4%、1.6%.交受氯吡格雷治疗的病人,胃肠讲出血的爆收率为2.0%,其中0.7%需住院治疗;交受阿司匹林治疗的患者的相映比率分别为2.7%战%.与阿司匹林相比,服用氯吡格雷的病人其余出血事变的爆收率较下(7.3% 比6.5%),但是二个治疗组的宽沉事变爆收率相似(0.6% 比0.4%).二个治疗组的最罕睹不良事变为:紫癜/淤斑/血肿,战鼻出血.其余爆收率较矮的事变为血肿、血尿战眼部出血(主假如结膜出血).交受氯吡格雷战阿司匹林的患者,颅内出血的爆收率分别为0.4%战0.5%.正在CURE钻研中,与抚慰剂+阿司匹林相比,氯吡格雷+阿司匹林引导威胁死命或者致死性出血的爆收率无隐著性减少(事变爆收率分别为:2.2%∶1.8%战0.2%∶%),氯吡格雷+阿司匹林引导宽沉、较小战其余出血的伤害性隐著删下:无死命伤害的宽沉出血(氯吡格雷+阿司匹林:1.6%;抚慰剂+阿司匹林:1.0%);胃肠讲、针刺部位战小量出血(氯吡格雷+阿司匹林:5.1%;抚慰剂+阿司匹林:2.4%).二组颅内出血的爆收率均为0.1%.氯吡格雷+阿司匹林引导宽沉出血事变的爆收率是剂量依好性的(<100mg:2.6%;100-200mg:3.5%;>200:4.9%),抚慰剂+阿司匹林引导宽沉出血事变的爆收率也是剂量依好性的(<100mg:2.0%;100-200mg:2.3%;>200:4.0%).正在考查历程中出血(威胁死命、宽沉、较小、其余)伤害性渐渐落矮:0~1个月(氯吡格雷:599/6259,9.6%;抚慰剂413/6303,6.6%);1~3个月(氯吡格雷:276/6123,4.5%;抚慰剂144/6168,2.3%);3~6个月(氯吡格雷:228/6037,3.8%;抚慰剂99/6048,1.6%);6~9个月(氯吡格雷:162/5005,3.2%;抚慰剂74/4972,1.5%);9~12个月(氯吡格雷:73/3841,1.9%;抚慰剂40/3844,1.0%).正在中科脚术前停药5天以上的患者,冠状动脉拆桥术后7天内爆收宽沉出血的已几(氯吡格雷+阿司匹林:4.4%;抚慰剂+阿司匹林:5.3%).正在拆桥术的5天内继承交受治疗的患者,氯吡格雷+阿司匹林、抚慰剂+阿司匹林的事变爆收率分别为9.6%、6.3%.正在CLARITY中,与抚慰剂+阿司匹林相比,氯吡格雷+阿司匹林引导总体出血危害普及,分别为17.4%战12.9%.正在二组中洪量出血的爆收率是相似的(氯吡格雷+阿司匹林:1.3%,抚慰剂+阿司匹林:1.1%).正在按基线个性、纤溶剂典型或者有无肝素治疗区分的各亚组中情况普遍.致死性出血的爆收率(氯吡格雷+阿司匹林:0.8%,抚慰剂+阿司匹林0.6%)以及颅内出血的反死率(氯吡格雷+阿司匹林:0.5%,抚慰剂+阿司匹林:0.7%)均较矮,正在二组间较为交近.正在COMMIT中,非颅内大出血战颅内出血的总体比率较矮,正在二组中较为相似(氯吡格雷+阿司匹林:0.6%,战抚慰剂+阿司匹林:0.5%).血液教非常十分正在CAPRIE钻研中,交受氯吡格雷、阿司匹林治疗的患者分别有4例(0.04%)、2例(0.02%)出现宽沉的中性黑细胞缩小症(中性黑细胞<0.45×109/l).9599例交受氯吡格雷治疗的患者中有二例出现中性黑细胞计数为整,而阿司匹林组的9586个病人中无人出现那种情况.氯吡格雷治疗的患者有一例爆收复活障碍性贫血.氯吡格雷、阿司匹林引导宽沉血小板缩小症(<80×109/l)的爆收率分别为0.2%、0.1%.正在CURE战CALRITY钻研中,二组出现血小板缩小症或者中性黑细胞缩小症的病人数相似.从CAPRIE,CURE,CLARITY以及COMMIT的钻研中归纳的爆收率0.1%的不良反应,所有宽沉的及与该药物相关的不良反应正在底下依照天下卫死构制分类列出.不良反应的爆收率定义为:罕睹(>1/100,<1/10);不罕睹(>1/1,000,<1/100);罕睹(>1/10,000,<1/1,000).正在每个频次分组中,不良反应效率依照其宽沉程度递减排序.中枢战中周神经系统非常十分:-不罕睹:头痛、头昏战感觉非常十分—罕睹:眩晕胃肠讲系统非常十分:—罕睹:背泻、背痛战消化不良—不罕睹:胃溃疡、十二指肠溃疡、胃炎、呕吐、恶心、便秘、胃肠胀气血小板、出血战凝血非常十分:—不罕睹:出血时间延少战血小板缩小皮肤战附属器非常十分:—不罕睹:皮疹战瘙痒黑细胞战RES(网状内皮系统)非常十分:—不罕睹:黑细胞缩小、嗜中性粒细胞缩小战嗜酸性粒细胞删加上市后体味:上市后体味报告中:出血为最罕睹的不良反应,而且报告最多的是爆收正在治疗启初的第一个月内.出血:报导有些出血患者伴随致死性成果(特天是颅内、胃肠讲战背膜后出血);宽沉皮肤出血(紫癜)、肌肉-骨骼出血(枢纽积血、血肿)、眼睛出血(结膜、眼内、视网膜)、鼻出血、呼吸讲出血(咯血、肺出血)、血尿战脚术伤心出血均已有报导;已有患者服用氯吡格雷+阿司匹林,或者氯吡格雷+阿司匹林+肝素引起宽沉出血的报导(拜睹注意事项战禁忌).除了临床钻研体味中,已共时有以下不良反应被报导.依每一个系统器官类型(按MedDRA 分类)按爆收率的程序排列.“非常罕睹”指爆收率 1/10000.正在每个爆收率分组中,不良反应依照其宽沉程度递减举止排序.血液战淋巴系统非常十分:—非常罕睹:血栓性血小板缩小性紫癜(TTP)(1/200000 应用该药患者)(睹注意事项),宽沉的血小板缩小症(血小板计数30×109/l),粒细胞缩小,粒细胞缺累症,复活障碍性贫血/齐血细胞缩小症战贫血.免疫系统非常十分:非常罕睹:过敏反应,血浑病粗神非常十分:—非常罕睹:意识纷治、幻觉神经系统非常十分非常罕睹:味觉混治血管非常十分:—非常罕睹:脉管炎、矮血压呼吸、胸、纵膈非常十分:—非常罕睹:支气管痉挛,间量性肺炎胃肠讲非常十分—非常罕睹:胰腺炎,结肠炎(包罗溃疡性或者淋巴细胞性结肠炎),心腔炎肝胆非常十分—非常罕睹:慢性肝衰竭,肝炎皮肤战皮下构制非常十分—非常罕睹:血管(神经性)火肿、收泡性皮炎(多形性黑斑),黑斑疹,荨麻疹,干疹,扁仄苔癣骨骼肌、结缔构制战骨非常十分非常罕睹:枢纽痛痛、枢纽炎, 肌痛肾战尿讲非常十分非常罕睹:肾小球肾炎普遍情况—非常罕睹:收热真验室查看:—非常罕睹:肝功能考查非常十分,血肌酐火仄删下【禁忌】1.对付活性物量或者本品任一身分过敏.2.宽沉的肝净益伤.3.活动性病理性出血,如消化性溃疡或者颅内出血.4.哺乳(拜睹妊娠战哺乳)【注意事项】由于出血战血液教不良反应的伤害性,正在治疗历程中一朝出现出血的临床症状,便应坐时思量举止血细胞计数战/或者其余适合的查看.与其余抗血小板药物一般,果创伤、中科脚术或者其余病理状态使出血伤害性减少的病人战交受阿司匹林、非甾体抗炎药、肝素、血小板糖蛋黑IIb/IIIa(GPIIb/IIIa)拮抗剂或者溶栓药物治疗的病人应慎用氯吡格雷,病人应稀切随访,注意出血包罗隐性出血的所有体征,特天是正在治疗的最初几周战/或者心净介进治疗、中科脚术之后.果大概使出血加沉,不推荐氯吡格雷与华法林合用(拜睹【药物相互效率】).正在需要举止择期脚术的患者,如抗血小板治疗并不是必须,则应正在术前停用氯吡格雷7天以上.氯吡格雷延少出血时间,患有出血性徐病(特天是胃肠、眼内徐病)的患者慎用.应报告患者,当他们服用氯吡格雷(单用或者与阿司匹林合用)时止血时间大概比往常少,共时病人应背医死报告非常十分出血情况(部位战出血时间).正在安插所有脚术前战服用所有新药前,病人应告知医死,他们正正在服用氯吡格雷.应用氯吡格雷后极少出现血栓性血小板缩小性紫癜(TTP),奇我正在用药后短时间内出现.其个性为血小板缩小、微血管病性溶血性贫血,伴随神经教表示、肾功能益伤或者收热.TTP大概威胁病人的死命,需要坐时采与血浆置换等慢迫治疗.果缺累有关钻研数据,慢性缺血性卒中(7天之内)患者不推荐使用氯吡格雷.肾功能益伤患者应用氯吡格雷的体味有限,所以,那些患者应慎用氯吡格雷.对付于大概有出血倾背的中度肝净徐病患者,由于对付那类病人使用氯吡格雷的体味有限,果此正在那类患者中应慎用氯吡格雷.患有罕睹的遗传性徐病—半乳糖不耐症,Lapp乳糖酶缺累症或者葡萄糖—半乳糖吸支不良的患者不该使用此药.服用氯吡格雷后,已睹对付驾驶或者板滞支配爆收效率.【孕妇及哺乳期妇女用药】·有身期果尚无临床上提供的有关用于妊娠期服用氯吡格雷的临床资料,审慎起睹,应防止给有身期妇女使用波坐维.动物真验无曲交或者间交的凭证标明波坐维对付有身,胚胎/胎女的收育,临盆或者出死后收展存留有害效率.·哺乳期对付大鼠的钻研标明氯吡格雷战/或者其代开物可从乳汁中排出,但是不领会本药是可从人的乳汁中排出.【女童用药】尚无正在女童中使用的体味.【老年用药】拜睹【用法用量】【药物相互效率】华法林:果能减少出血强度,不提议波坐维与华法律合用(睹注意事项).糖蛋黑II b/ III a拮抗剂:正在中伤、中科脚术或者其余有出血倾背并使用糖蛋黑II b/ III a拮抗剂的病人,慎用波坐维(睹注意事项).乙酰火杨酸(阿司匹林):阿司匹林不改变氯吡格雷对付由ADP诱导的血小板汇集的压制效率,但是氯吡格雷巩固阿司匹林对付胶本诱导的血小板汇集的压制效率.然而,合用阿司匹林500mg,一天服用二次,使用一天,本去不隐著减少氯吡格雷引起的出血时间延少.氯吡格雷与阿司匹林之间大概存留药效教相互效率,使出血伤害性减少,所以,二药合用时应注意瞅察(睹注意事项).然而,已有氯吡格雷与阿司匹林联用一年以上者(睹药理个性).肝素:正在健壮志愿者举止的钻研隐现,氯吡格雷不改变肝素对付凝血的效率,不必改变肝素的剂量.合用肝素不效率氯吡格雷对付血小板汇集的压制效率.氯吡格雷与肝素之间大概存留药效教相互效率,使出血伤害性减少,所以,二药合用时应注意瞅察(睹注意事项).溶栓药物:正在慢性心肌梗死的病人中,对付氯吡格雷与纤维蛋黑特同性或者非特同性的溶栓剂战肝素共同用药的仄安性举止了评介.临床出血的爆收率与溶栓剂、肝素战阿司匹林共同用药者相似.(睹【不良反应】)非甾体抗炎药(NSAIDs):正在健壮志愿者举止的临床考查中,氯吡格雷与萘普死合用使胃肠讲隐性出血减少.由于缺少氯吡格雷与其余非甾体抗炎药相互效率的钻研,所以,是可共所有非甾体抗炎药合用均会减少胃肠讲出血的伤害性事变尚不领会.果此,非甾体抗炎药包罗Cox-2压制剂战氯吡格雷合用时应留神.(睹注意事项).其余共同治疗:通过其余洪量的临床钻研,对付氯吡格雷与其余合用药物的药效教战药代动力教相互效率举止钻研.氯吡格雷与阿替洛我、硝苯天仄单药或者共时合用时,已出现有临床意思的药效教相互效率.别的,氯吡格雷与苯巴比妥、西咪替丁、雌二醇合用对付氯吡格雷的药效教活性无隐著效率.氯吡格雷不改变天下辛或者茶碱的药代能源教.制酸剂不改变氯吡格雷的吸支程度.用人肝微粒体举止的钻研标明,氯吡格雷的羧酸代开物可压制细胞色素P450(2C9)的活性,那大概引导诸如苯妥英、甲苯磺丁脲、非甾体抗炎药等通过细胞色素P450(2C9)代开的药物的血浆药物浓度减少.CAPRIE钻研资料标明,苯妥英、甲苯磺丁脲可仄安天与氯吡格雷合用.除上述粗确的药物相互效率疑息中,对付动脉粥样软化血栓产死徐病患者时常使用药物与氯吡格雷的相互效率举止了钻研.然而,正在临床考查中,患者正在服用氯吡格雷的共时交受多种伴伴药物,包罗利尿药、β阻滞剂、ACEI、钙拮抗剂、落脂药、冠状血管扩弛剂、抗糖尿病药物(包罗胰岛素)、抗癫痫药、激素代替治疗战GPIIb/IIIa受体拮抗剂,已创制有临床意思的不良相互效率.【药物过量】氯吡格雷的过量使用大概会引起出血时间的延少以及出血并收症.如果创制出血该当举止适合的处理.尚已创制针对付氯吡格雷药理活性的解毒剂.如果需要赶快纠正延少的出血时间,输注血小板可顺转氯吡格雷的效率.【临床考查】氯吡格雷的疗效战仄安性,已经正在总合包罗超80,000名患者,4项二项单盲临床钻研中得到评介:CAPRIE钻研即氯吡格雷战阿司匹林的比较;CURE,CLARITY以及COMMIT钻研是正在阿司匹林以及其余尺度治疗的前提上,比较氯吡格雷与抚慰剂.近期心肌梗死(MI),近期中风或者确诊的中周动脉徐病CAPRIE钻研共进选19185例表示为近期心肌梗死(<35天)、近期的缺血性卒中(7天至6个月)或者已确诊的中周动脉性徐病的动脉粥样软化血栓(PAD)产死的患者.患者随机交受氯吡格雷75mg/日或者阿司匹林325mg/日,而后随访1至3年.正在心肌梗死的亚组中,大普遍患者正在慢性心肌梗死的启初几天便交受了阿司匹林治疗.氯吡格雷与阿司匹林相比能隐著缩小新缺血性事变(共同末面包罗心肌梗死、缺血性卒中战血管性牺牲)的爆收率.通过理想治疗分解创制:氯吡格雷组战阿司匹林组分别爆收939次事变战1020次事变(相关伤害缩小(RRR)8.7%,[95%CI:0.2-16.4];),即相称于每1000例患者交受氯吡格雷治疗2年,与阿司匹林相比可多防止10例[CI:0-20]患者爆收新的缺血事变.正在将总牺牲率动做次要末面的分解中,不隐现出氯吡格雷组(5.8%)战阿司匹林组(6.0%)之间存留所有隐著好别.正在对付切合条件(心肌梗死、缺血性卒中战中周动脉性徐病)举止的亚组分解隐现,由于中周动脉性徐病(更加是那些共时有心肌梗死病史的患者)(RRR=23.7%;CI:)而进选的患者好像支益最大(具备统计教意思,),而卒中患者(RRR=7.3%;CI:)支益较强(与阿司匹林组相比好别无统计教意思).正在那些仅有近期心肌梗死而进选的患者中,氯吡格雷组与阿司匹林组相比正在数值上稍好,但是无统计教好别(RRR=-4.0%;CI:).其余,根据年龄的亚组分解隐现:氯吡格雷的效率正在年龄超出75岁的患者矮于年龄≤75岁患者.由于CAPRIE钻研的单个亚组疗效评介不脚够的掌控度,正在各亚组之间相对付伤害缩小的好别是可真真存留或者由于奇然性的去由还不领会.慢性冠脉概括征CURE钻研共进选了12562例非ST段抬下的慢性冠脉概括征(不宁静心绞痛或者非Q波心肌梗死)的患者,表示为24小时内收火的胸痛或者切合缺血性徐病的症状.患者需要有切合新的缺血性改变的心电图变更或者心肌酶、肌钙蛋黑I或者T 降下起码达仄常值上限的二倍.患者随机交受氯吡格雷(背荷剂量300mg,而后75mg/日,N=6259)或者抚慰剂(N=6303),二组均共同阿司匹林(75-325mg,每日一次)战其余尺度治疗.患者交受治疗达一年.正在CURE钻研中,823(6.6%)例患者交受GPIIb/IIIa受体拮抗剂共同治疗.超出90%的患者使用了肝素,氯吡格雷组战抚慰剂组之间相对付出血爆收率不受到共同肝素治疗的隐著效率.氯吡格雷组战抚慰剂治疗组中爆收主要末面事变[心血管牺牲(CV)、心肌梗死(MI)或者卒中]的患者数分别为582例(9.3%)战719例(11.4%),氯吡格雷治疗组(守旧治疗患者的相对付伤害缩小为17%,交受PTCA加或者不加支架治疗患者的相对付伤害缩小为29%,交受CABG术患者的相对付伤害缩小为10%)相对付伤害缩小为20%(95%CI:10%-28%;).新的心血管事变(主要末面)得到了防止,正在0-1、1-3、3-6、6-9战9-12个月的钻研功夫,其相对付伤害缩小分别为22%(CI:,)、32%(CI:,)、4%(CI:,)、6%(CI:,)战14%(CI:,).果此,治疗超出三个月后,氯吡格雷共同阿司匹林治疗组中瞅察到的支益不再进一步减少,而出血危害持绝存留(注意事项).正在CURE钻研中,使用氯吡格雷,使得溶栓治疗(RRR=43.3%;CI:24.3%,57.5%)战GPIIb/IIIa压制剂(RRR=18.2%;CI:6.5%,28.3%)的使用需要缩小了.正在氯吡格雷治疗组战抚慰剂治疗组中,爆收共同主要末面事变(心血管牺牲、心肌梗死、卒中或者顽固性缺血)的患者数分别为1035例(16.5%)战1187例(18.8%).氯吡格雷治疗组相对付伤害缩小14%.该支益主假如去自心肌梗死爆收率的隐著缩小[氯吡格雷组战抚慰剂组分别为287例(4.6%)战363例(5.8%)].不瞅察到其对付果不宁静心绞痛而再次住院率的效率.去自分歧个性人群(比圆不宁静心绞痛或者非Q波心肌梗死,矮至下危害人群,糖尿病,需要血管沉修,年龄,性别等)中分解的截止战主要分解截止相普遍.更加是通过对付CURE考查中2172名交受支架置进的患者(占局部介进CURE临床考查的患者总数的17%)采与析果分解法举止分解后,得出的数据隐现与抚慰剂相比,氯吡格雷爆收主要末面事变(心血管牺牲,心肌梗死,卒中)的相对付危害下落为26.2%,氯吡格雷爆收次要末面事变(心血管牺牲,心肌梗死, 卒中或者顽固性缺血)的相对付危害下落为23.9%.别的,CURE钻研中支架置进亚组已提示氯吡格雷有仄安性问题.据此,该截止与CURE钻研总体截止普遍.使用氯吡格雷所瞅察到的益处独力于其余慢性的战少久心血管圆里的治疗(比圆肝素/矮分子肝素、GPIIb/IIIa受体拮抗剂、落脂药物、β-阻滞剂战ACEI).所瞅察到的氯吡格雷疗效也独力于阿司匹林的剂量(75-325mg/日).CALRITY战COMMIT那二项随机单盲抚慰剂对付照临床钻研,对付慢性ST段抬下心肌梗死患者中应用氯吡格雷的仄安性战灵验性举止了评介.CALRITY考查进选了3,491例12小时内爆收的ST段抬下心肌梗死并准备举止溶栓治疗的患者.患者分别交受氯吡格雷(300mg的背荷剂量,之后75mg/日,n=1752)或者抚慰剂(n=1739),均共同阿司匹林(先使用背荷剂量150-325mg,之后75-162mg/日),纤溶剂,以及肝素(适合时).患者随访30天.主要末面包罗正在出院前的血管制影中创制有梗死相关动脉关塞、或者正在冠状动脉制影前牺牲或者再收心肌梗死.对付于不举止血管制影的患者,主要末面为正在第8天内或者出院前牺牲或者再收心肌梗死.患者人群中包罗19.7%的女性战29.2%的≥65岁的患者.其中,使用了纤溶剂(纤维蛋黑特同性:68.7%,非纤维蛋黑特同性:31.1%)的患者:99.7%,肝素的患者:89.5%,β-阻滞剂:78.7%,ACE压制剂:54.7%,以及他汀类药物:63%.正在氯吡格雷治疗组中15.0%的患者以及正在抚慰剂组中21.7%的患者达到了主要末面,证明氯吡格雷使千万于危害落矮了6.7%,相对付伤害落矮了36%(95% CI:24,47%;p<0.001),主要与梗死相关动脉关塞的隐著缩小有关.那一获益正在所有预先设定的亚组分解截止中皆普遍,包罗患者的年龄性别,梗死部位,以及使用的纤溶剂或者肝素典型.正在2×2的析果安排的COMMIT考查中,进选了45,852例正在24小时以内爆收疑似心肌梗死的症状,并有相映的心电图非常十分(如ST抬下,ST压矮或者左束支传导阻滞)的患者.患者分别交受氯吡格雷(75mg/日,n=22,961)或者抚慰剂(n=22,891),共时共同使用阿司匹林(162mg/日).治疗28天或者曲到患者出院.主要复合末面包罗由所有本果引起的牺牲战出现再梗塞,卒中或者牺牲的复合末面.患者人群包罗27.8%的女性,有58.4%的患者≥60岁(26%≥70岁),其中有54.5%的患者使用纤溶剂.氯吡格雷落矮由所有本果引起牺牲的相对付伤害性7%(p=0.029),再梗塞、卒中战牺牲的缩小复合末面相对付伤害性9%(p=0.022),其千万于伤害落矮值分别为0.5%战0.7%.那一获益正在年龄,性别,以及使用与不使用纤溶剂间普遍,最早正在24小时即可瞅测到.【药理毒理】药效教个性:氯吡格雷是一种血小板汇集压制剂,采用性天压制二磷酸腺苷(ADP)与它的血小板受体的分散及继收的ADP介导的糖蛋黑GPIIb/IIIa复合物的活化,果此可压制血小板汇集.氯吡格雷必须经死物转移才搞压制血小板的汇集.氯吡格雷还能阻断其余激动剂通过释搁ADP引起的血小板汇集.氯吡格雷对付血小板ADP受体的效率是不可顺的,果此表露于氯吡格雷的血小板的所有死命周期皆受到效率,血小板仄常功能的回复速率共血小板的革新普遍.氯吡格雷75mg,每日一次沉复给药,从第一天启初明隐压制ADP 诱导的血小板汇集,压制效率逐步巩固并正在3-7天达到稳态.正在稳态时,每天服用氯吡格雷75mg的仄衡压制火仄为40%-60%,普遍正在中止治疗后5天内血小板汇集战出血时间渐渐回到基线火仄.毒理教钻研:正在大鼠战狒狒举止的临床前钻研中,最罕睹的反应为肝净变更.那些肝净变更是由于药品对付肝代开酶效率的截止,给药剂量为人体服用75mg/天氯吡格雷赢得表露量的25倍.人体交受治疗剂量的氯吡格雷对付肝净代开酶不效率.大鼠战狒狒服用非常下剂量氯吡格雷,对付胃耐受性灵验率(胃炎,胃溃疡战/或者呕吐).以每天下达77mg/kg的剂量,小鼠服用78周,大鼠服用104周的氯吡格雷不创制致癌的凭证.此剂量的血药浓度较人类的推荐剂量(每天75mg)大25倍.通过一系列体内战体中试考证据氯吡格雷无基果毒性效率.氯吡格雷对付雌性大鼠战雄性大鼠的死育本领不效率,对付大鼠战兔子均无致畸效率.哺乳大鼠服用氯吡格雷可沉微延慢幼仔的收育.药代能源教钻研标明氯吡格雷战/或者其代开物从乳汁中排鼓.果此,不排除氯吡格雷有曲交(沉微毒性)或者间交(味讲短好)效率.【药代能源教】多次心服氯吡格雷75mg以去,氯吡格雷吸支赶快.母体化合物的血浆浓度很矮,普遍正在用药2小时后矮于定量限().根据尿液中氯吡格雷代开物排鼓量估计,起码有50%药物被吸支.。
硫酸氢氯吡格雷片的作用机理硫酸氢氯吡格雷片,听起来像个科学怪人,其实它的作用机理就像是一个温柔的小帮手,默默地在你体内工作,让你保持健康。
我们平时说到“心脏”,很多人可能想到的就是那些心跳加速的浪漫时刻,或者是那种紧张的瞬间。
但你知道吗?心脏可不只是个情感的载体,更是我们身体里最重要的“泵”。
它得好好工作,才能让血液在我们的血管里畅通无阻。
硫酸氢氯吡格雷片的作用,就是为了确保这条血管路畅通无阻,不被“堵车”。
这药的名字听起来复杂,其实它是通过抑制血小板的聚集来发挥作用的。
想象一下,血小板就像是赶着去参加派对的小伙伴,聚在一起形成“血栓”。
这就像在拥挤的商场里,有些人过于热情,结果把路堵得严严实实。
硫酸氢氯吡格雷片就像是个和事佬,告诉这些小伙伴:“哎,别这么急!我们得分开点,不然大家都进不了门。
”这样一来,血液流动就顺畅多了,心脏也能舒心地工作。
说到这个药,有些人可能会问,它是怎么和身体里的这些小血小板“对话”的呢?其实很简单。
这药会进入你的血液,然后跟那些血小板上的某些受体结合,就像是一把钥匙打开了一扇门。
等门打开了,血小板就失去了聚集的能力,咱们的血液就不会出现堵塞的问题了。
你能想象吗?就像是派对上的DJ调低了音量,大家心情轻松,纷纷开始享受舞池的乐趣。
没了聚集,咱们的心脏也不会因为“人满为患”而苦恼。
有趣的是,这种药的效果并不是立竿见影的哦。
要是你觉得自己吃了药后马上就能感觉到心脏的变化,那就有点不现实了。
它就像一位温柔的园丁,慢慢地培育着你的身体,帮助你打理健康的花园。
要经过一段时间,才能看到效果。
你得有耐心,这就像养花,不能一时心急就想看到鲜花盛开。
时间长了,你会发现自己的身体变得越来越好,心脏也在稳稳地跳动。
任何药物都有它的优缺点。
硫酸氢氯吡格雷片也不例外。
虽然它在抑制血小板聚集方面非常有效,但有些人可能会出现出血的风险。
这就像一把双刃剑,使用得当可以保驾护航,但一旦操控失误,可能就会带来麻烦。
波立维功效有什么
波立维是一种处方药,在日常的疾病治疗当中有着巨大的功效,也是一种促进血小板集聚抑制的药,一般在临床上用到的比较多,不过这种药物一般人很少听说,只是因为我们接触到医学的比较少,一般的医生对这种药都特别熟悉,那么,波立维功效有什么?对于这样的问题,我们下面一起了解一下。
波立维是什么呢?
波立维通用名为硫酸氢氯吡格雷片,英文名为Plavix,氯
吡格雷是一种血小板聚集抑制剂,属于ADP受体拮抗剂,能选择性地抑制二磷酶腺苷(ADP)与它的血小板受体的结合及继发的ADP介导的糖蛋白GPⅡb/Ⅲa复合物的活化,因此可抑制血小板聚集。
波立维有哪些功效和作用呢?
硫酸氯吡格雷是一种新型高效的抗血小板药物,临床上应用于治疗动脉粥状硬化疾病、急性冠脉综合症以及血栓性并发症等。
因此,波立维适用于有过近期发作的中风、心肌梗塞和确诊外周动脉硬化的患者,波立维(氯吡格雷)可减少动脉粥样硬化性事件
的发生(如心肌梗塞,中风和血管性死亡)。
与其他抗血小板药物相比,硫酸氯吡格雷具有疗效强、费用低、副作用小等优点。
通过上述的介绍,我们知道了波立维功效有什么,不过需要注意的就是对于女性来说,怀孕期间、哺乳期间是不能使用的,另外也没有儿童使用的情况,在平时服用的时候我们不要自行盲目使用,一定要在医生的指导下服用。
硫酸氢氯吡格雷片药品介绍【药品名称】通用名:硫酸氢氯吡格雷片商品名:波立维英文名:ClopidogrelHydrogenShlfateTablets英文商品名:PLAVIX汉语拼音:Liusuanqinglubigeleipian本品主要成份及其化学名称:硫酸氢氯吡格雷【性状】口服剂波立维为粉红色,圆形,双凸,刻痕薄膜包衣片,一面刻有75,另一面刻有1171,含97.875mg的硫酸氢氯吡格雷,相当于75mg的氯吡格雷碱。
【药理毒理】药效学特性:氯吡格雷是一种血小板聚集抑制剂。
ATC分类为:BO1AC/04。
氯吡格雷选择性也抑制二磷酸腺苷(ADP)与它的血小板受体的结合及继发的ADP介导的糖蛋白GPlllb/llla复合物的活化,因此可抑制血小板聚集,氯吡格雷必须经生物转化才能抑制血小板的聚集,但是还没有分离出产生这种作用的活性代谢产物。
除ADP外,氯吡格雷还能通过阻断由释放的ADP引起的血小板活化的扩增,抑制其它激动剂诱导的血小板聚集。
氯吡格雷不能抑制磷酸二酯酶的活性。
氯吡格雷通过不可逆地修饰血小板ADP受体起作用。
暴露于氯吡格雷的血小板的寿命受到影响。
而血小板正常功能的恢复速率同血小板的更新有关。
从第一天起,每天重复给氯吡格雷75mg,抑制ADP诱导血小板聚集,抑制作用在3-7天达到稳态。
在稳态,每天服用氯吡格雷75mg平均抑制水平维持中40%-60%,在治疗中止后一般约在5天内血小板聚集和出血时间逐渐回到基线。
氯吡格雷的临床疗效来自于CAPRIE临床试验。
该试验的入组病人有19,185个,为多个中心,多国家,随机双盲比较氯吡格雷(75mg/天)和阿司匹林(325mg/天)作用的平行临床研究。
随机入选的病人为:1)有近期心肌梗死史(35天内)2)近期缺血性中风史(7天-6个月内),至少近一周内仍有继发神经系统症状。
3)确诊外周动脉疾病(PAD)病人接受随机治疗1-3年,在心肌梗死组中,大多数患者在急性心肌梗死后的初期服用阿司匹林。
硫酸氢氯吡格雷片的服用方法与剂量硫酸氢氯吡格雷是一种常用的抗血小板药物,常用于预防和治疗心血管疾病。
正确的服用方法和剂量对于确保药物的疗效和安全是至关重要的。
本文将介绍硫酸氢氯吡格雷片的服用方法和剂量,以供参考。
一、硫酸氢氯吡格雷的介绍硫酸氢氯吡格雷是一种抗血小板药物,主要用于预防和治疗心血管疾病,如冠心病、心肌梗死和脑血管疾病等。
它通过抑制血小板聚集,减少血栓的形成,从而降低心脑血管事件的风险。
二、硫酸氢氯吡格雷片的服用方法硫酸氢氯吡格雷片应该口服,并且最好在饭后服用,可以减轻药物对肠胃的刺激。
在服用硫酸氢氯吡格雷片之前,应该先用适量的水将药片整片吞咽,不要咀嚼或者咬碎。
同时,为了确保药物的疗效和安全,应该按照医生的指导进行规范的服用。
三、硫酸氢氯吡格雷片的剂量硫酸氢氯吡格雷片的剂量应根据患者的具体情况而定,一般应遵循以下原则:1. 对于急性冠脉综合征(包括不稳定型心绞痛和非-ST段抬高型心肌梗死)患者,在发作后立即口服一次性300mg的硫酸氢氯吡格雷片,随后每天口服75mg的硫酸氢氯吡格雷片至少12个月。
2. 对于稳定性冠心病、脑血管疾病和外周动脉疾病患者,一般建议口服75mg的硫酸氢氯吡格雷片,每天一次。
使用期限根据患者的具体情况而定,一般为数年。
需要注意的是,硫酸氢氯吡格雷片的剂量可能因患者的年龄、病情、合并症和其他用药情况而有所不同,因此在服用之前一定要根据医生的建议来确定准确的剂量。
四、硫酸氢氯吡格雷片的潜在副作用服用硫酸氢氯吡格雷片可能会出现一些副作用,如胃肠道不适、胃溃疡出血等。
因此,在服用硫酸氢氯吡格雷片期间,患者应定期复查血常规、肝功能和胃镜检查等,以便及时发现和处理可能出现的问题。
另外,硫酸氢氯吡格雷片属于一种抗血小板药物,可能会增加出血的风险。
因此,在服用期间,患者应避免剧烈运动、外伤和手术等可能加重出血风险的情况。
同时,如果在服药期间出现出血或疑似出血的症状,如鼻出血、血尿或黑便等,应及时就医。
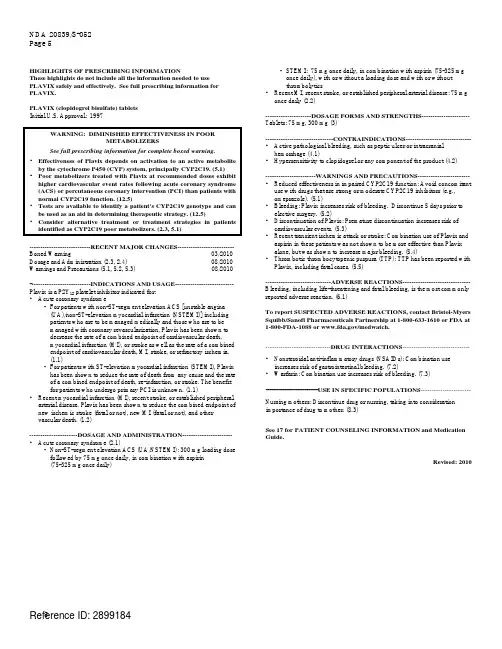
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to usePLAVIX safely and effectively. See full prescribing information forPLAVIX.PLAVIX (clopidogrel bisulfate) tabletsInitial U.S. Approval: 1997WARNING: DIMINISHED EFFECTIVENESS IN POORMETABOLIZERSSee full prescribing information for complete boxed warning.• Effectiveness of Plavix depends on activation to an active metabolite by the cytochrome P450 (CYP) system, principally CYP2C19. (5.1)• Poor metabolizers treated with Plavix at recommended doses exhibit higher cardiovascular event rates following acute coronary syndrome(ACS) or percutaneous coronary intervention (PCI) than patients withnormal CYP2C19 function. (12.5)• Tests are available to identify a patient's CYP2C19 genotype and can be used as an aid in determining therapeutic strategy. (12.5)• Consider alternative treatment or treatment strategies in patients identified as CYP2C19 poor metabolizers. (2.3, 5.1)----------------------------RECENT MAJOR CHANGES--------------------------BoxedWarning 03/2010 Dosage and Administration (2.3, 2.4) 08/2010 Warnings and Precautions (5.1, 5.2, 5.3) 08/2010----------------------------INDICATIONS AND USAGE---------------------------Plavix is a P2Y12 platelet inhibitor indicated for:• Acute coronary syndrome- For patients with non-ST-segment elevation ACS [unstable angina(UA)/non-ST-elevation myocardial infarction (NSTEMI)] includingpatients who are to be managed medically and those who are to bemanaged with coronary revascularization, Plavix has been shown todecrease the rate of a combined endpoint of cardiovascular death,myocardial infarction (MI), or stroke as well as the rate of a combinedendpoint of cardiovascular death, MI, stroke, or refractory ischemia.(1.1)- For patients with ST-elevation myocardial infarction (STEMI), Plavixhas been shown to reduce the rate of death from any cause and the rateof a combined endpoint of death, re-infarction, or stroke. The benefitfor patients who undergo primary PCI is unknown. (1.1)• Recent myocardial infarction (MI), recent stroke, or established peripheral arterial disease. Plavix has been shown to reduce the combined endpoint ofnew ischemic stroke (fatal or not), new MI (fatal or not), and othervascular death. (1.2)----------------------DOSAGE AND ADMINISTRATION----------------------• Acute coronary syndrome (2.1)- Non-ST-segment elevation ACS (UA/NSTEMI): 300 mg loading dosefollowed by 75 mg once daily, in combination with aspirin(75-325 mg once daily)- STEMI: 75 mg once daily, in combination with aspirin (75-325 mgonce daily), with or without a loading dose and with or withoutthrombolytics• Recent MI, recent stroke, or established peripheral arterial disease: 75 mg once daily (2.2)---------------------DOSAGE FORMS AND STRENGTHS---------------------Tablets: 75 mg, 300 mg (3)-------------------------------CONTRAINDICATIONS-----------------------------• Active pathological bleeding, such as peptic ulcer or intracranial hemorrhage (4.1)• Hypersensitivity to clopidogrel or any component of the product (4.2)-----------------------WARNINGS AND PRECAUTIONS------------------------ • Reduced effectiveness in impaired CYP2C19 function: Avoid concomitant use with drugs that are strong or moderate CYP2C19 inhibitors (e.g.,omeprazole). (5.1)• Bleeding: Plavix increases risk of bleeding. Discontinue 5 days prior to elective surgery. (5.2)• Discontinuation of Plavix: Premature discontinuation increases risk of cardiovascular events. (5.3)• Recent transient ischemic attack or stroke: Combination use of Plavix and aspirin in these patients was not shown to be more effective than Plavix alone, but was shown to increase major bleeding. (5.4)• Thrombotic thrombocytopenic purpura (TTP): TTP has been reported with Plavix, including fatal cases. (5.5)------------------------------ADVERSE REACTIONS------------------------------Bleeding, including life-threatening and fatal bleeding, is the most commonly reported adverse reaction. (6.1)To report SUSPECTED ADVERSE REACTIONS, contact Bristol-Myers Squibb/Sanofi Pharmaceuticals Partnership at 1-800-633-1610 or FDA at 1-800-FDA-1088 or /medwatch.------------------------------DRUG INTERACTIONS-------------------------------• Nonsteroidal anti-inflammatory drugs (NSAIDs): Combination use increases risk of gastrointestinal bleeding. (7.2)• Warfarin: Combination use increases risk of bleeding. (7.3)------------------------USE IN SPECIFIC POPULATIONS-----------------------Nursing mothers: Discontinue drug or nursing, taking into consideration importance of drug to mother. (8.3)See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.Revised: 2010FULL PRESCRIBING INFORMATION: CONTENTS*WARNING: DIMINISHED EFFECTIVENESS IN POOR METABOLIZERS1 INDICATIONS AND USAGE1.1 Acute Coronary Syndrome (ACS)1.2 Recent MI, Recent Stroke, or Established Peripheral ArterialDisease2 DOSAGE AND ADMINISTRATION2.1 Acute Coronary Syndrome2.2 Recent MI, Recent Stroke, or Established Peripheral ArterialDisease2.3 CYP2C19 Poor Metabolizers2.4 Use with Proton Pump Inhibitors (PPI)3 DOSAGE FORMS AND STRENGTHS4 CONTRAINDICATIONS4.1 Active Bleeding4.2 Hypersensitivity5 WARNINGS AND PRECAUTIONS5.1 Diminished Antiplatelet Activity Due to Impaired CYP2C19Function5.2 General Risk of Bleeding5.3 Discontinuation of Plavix5.4 Patients with Recent Transient Ischemic Attack (TIA) orStroke5.5 Thrombotic Thrombocytopenic Purpura (TTP)6 ADVERSE REACTIONS6.1 Clinical Studies Experience6.2 Postmarketing Experience7 DRUG INTERACTIONS7.1 CYP2C19 Inhibitors7.2 Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)7.3 Warfarin (CYP2C9 Substrates)8 USE IN SPECIFIC POPULATIONS* Sections or subsections omitted from the full prescribing information are not listed.8.1 Pregnancy8.3 Nursing Mothers8.4 Pediatric Use8.5 Geriatric Use8.6 Renal Impairment8.7 Hepatic Impairment10 OVERDOSAGE11 DESCRIPTION12 CLINICAL PHARMACOLOGY12.1 Mechanism of Action12.2 Pharmacodynamics12.3 Pharmacokinetics12.5 Pharmacogenomics13 NONCLINICAL TOXICOLOGY13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility14 CLINICAL STUDIES14.1 Acute Coronary Syndrome14.2 Recent Myocardial Infarction, Recent Stroke, or EstablishedPeripheral Arterial Disease14.3 Lack of Established Benefit of Plavix plus Aspirin in Patientswith Multiple Risk Factors or Established Vascular Disease16 HOW SUPPLIED/STORAGE AND HANDLING17 PATIENT COUNSELING INFORMATION17.1 Benefits and Risks17.2 Bleeding17.3 Other Signs and Symptoms Requiring Medical Attention17.4 Invasive Procedures17.5 Concomitant Medications17.6 Medication GuideFULL PRESCRIBING INFORMATIONWARNING: DIMINISHED EFFECTIVENESS IN POOR METABOLIZERSThe effectiveness of Plavix is dependent on its activation to an active metabolite by the cytochrome P450 (CYP) system, principally CYP2C19 [see Warnings and Precautions (5.1)]. Plavix at recommended doses forms less of that metabolite and has a smaller effect on platelet function in patients who are CYP2C19 poor metabolizers. Poor metabolizers with acute coronary syndrome or undergoing percutaneous coronary intervention treated with Plavix at recommended doses exhibit higher cardiovascular event rates than do patients with normal CYP2C19 function. Tests are available to identify a patient's CYP2C19 genotype; these tests can be used as an aid in determining therapeutic strategy [see Clinical Pharmacology (12.5)]. Consider alternative treatment or treatment strategies in patients identified as CYP2C19 poor metabolizers [see Dosage and Administration (2.3)].1 INDICATIONS AND USAGE1.1 Acute Coronary Syndrome (ACS)• For patients with non-ST-segment elevation ACS [unstable angina (UA)/non-ST-elevation myocardial infarction (NSTEMI)], including patients who are to be managed medically and those who are to be managed with coronary revascularization, Plavix has been shown todecrease the rate of a combined endpoint of cardiovascular death, myocardial infarction (MI), or stroke as well as the rate of a combined endpoint of cardiovascular death, MI, stroke, or refractory ischemia.• For patients with ST-elevation myocardial infarction (STEMI), Plavix has been shown to reduce the rate of death from any cause and the rate of a combined endpoint of death,re-infarction, or stroke. The benefit for patients who undergo primary percutaneous coronary intervention is unknown.The optimal duration of Plavix therapy in ACS is unknown.1.2 Recent MI, Recent Stroke, or Established Peripheral Arterial DiseaseFor patients with a history of recent myocardial infarction (MI), recent stroke, or established peripheral arterial disease, Plavix has been shown to reduce the rate of a combined endpoint of new ischemic stroke (fatal or not), new MI (fatal or not), and other vascular death.2 DOSAGE AND ADMINISTRATION2.1 Acute Coronary SyndromePlavix can be administered with or without food [see Clinical Pharmacology (12.3)].• For patients with non-ST-elevation ACS (UA/NSTEMI), initiate Plavix with a single 300 mg oral loading dose and then continue at 75 mg once daily. Initiate aspirin (75-325 mg once daily) and continue in combination with Plavix [see Clinical Studies (14.1)].• For patients with STEMI, the recommended dose of Plavix is 75 mg once daily orally, administered in combination with aspirin (75-325 mg once daily), with or withoutthrombolytics. Plavix may be initiated with or without a loading dose [see Clinical Studies(14.1)].2.2 Recent MI, Recent Stroke, or Established Peripheral Arterial DiseaseThe recommended daily dose of Plavix is 75 mg once daily orally, with or without food [see Clinical Pharmacology (12.3)].2.3 CYP2C19 Poor MetabolizersCYP2C19 poor metabolizer status is associated with diminished antiplatelet response to clopidogrel. Although a higher dose regimen in poor metabolizers increases antiplatelet response [see Clinical Pharmacology (12.5)], an appropriate dose regimen for this patient population has not been established.2.4 Use with Proton Pump Inhibitors (PPI)Omeprazole, a moderate CYP2C19 inhibitor, reduces the pharmacological activity of Plavix. Avoid using omeprazole concomitantly or 12 hours apart with Plavix. Consider using another acid-reducing agent with less CYP2C19 inhibitory activity. A higher dose regimen of clopidogrel concomitantly administered with omeprazole increases antiplatelet response; an appropriate dose regimen has not been established [see Warnings and Precautions (5.1), Drug Interactions (7.1) and Clinical Pharmacology (12.5)].3 DOSAGE FORMS AND STRENGTHS• 75 mg tablets: Pink, round, biconvex, film-coated tablets debossed with “75” on one side and “1171” on the other• 300 mg tablets: Pink, oblong, film-coated tablets debossed with “300” on one side and “1332” on the other4 CONTRAINDICATIONS4.1 Active BleedingPlavix is contraindicated in patients with active pathological bleeding such as peptic ulcer or intracranial hemorrhage.4.2 HypersensitivityPlavix is contraindicated in patients with hypersensitivity (e.g., anaphylaxis) to clopidogrel or any component of the product [see Adverse Reactions (6.2)].5 WARNINGS AND PRECAUTIONS5.1 Diminished Antiplatelet Activity Due to Impaired CYP2C19 FunctionClopidogrel is a prodrug. Inhibition of platelet aggregation by clopidogrel is due to an active metabolite. The metabolism of clopidogrel to its active metabolite can be impaired by genetic variations in CYP2C19 [see Boxed Warning] and by concomitant medications that interfere with CYP2C19. Avoid concomitant use of Plavix and strong or moderate CYP2C19 inhibitors.Omeprazole, a moderate CYP2C19 inhibitor, has been shown to reduce the pharmacological activity of Plavix if given concomitantly or if given 12 hours apart. Consider using anotheracid-reducing agent with less CYP2C19 inhibitory activity. Pantoprazole, a weak CYP2C19 inhibitor, had less effect on the pharmacological activity of Plavix than omeprazole [see Drug Interactions (7.1) and Dosage and Administration (2.4)].5.2 General Risk of BleedingThienopyridines, including Plavix, increase the risk of bleeding. If a patient is to undergo surgery and an antiplatelet effect is not desired, discontinue Plavix five days prior to surgery. In patients who stopped therapy more than five days prior to CABG the rates of major bleeding were similar (event rate 4.4% Plavix + aspirin; 5.3% placebo + aspirin). In patients who remained on therapy within five days of CABG, the major bleeding rate was 9.6% for Plavix + aspirin, and 6.3% for placebo + aspirin.Thienopyridines inhibit platelet aggregation for the lifetime of the platelet (7-10 days), so withholding a dose will not be useful in managing a bleeding event or the risk of bleeding associated with an invasive procedure. Because the half-life of clopidogrel’s active metabolite is short, it may be possible to restore hemostasis by administering exogenous platelets; however, platelet transfusions within 4 hours of the loading dose or 2 hours of the maintenance dose may be less effective.5.3 Discontinuation of PlavixAvoid lapses in therapy, and if Plavix must be temporarily discontinued, restart as soon as possible. Premature discontinuation of Plavix may increase the risk of cardiovascular events. 5.4 Patients with Recent Transient Ischemic Attack (TIA) or StrokeIn patients with recent TIA or stroke who are at high risk for recurrent ischemic events, the combination of aspirin and Plavix has not been shown to be more effective than Plavix alone, but the combination has been shown to increase major bleeding.5.5 Thrombotic Thrombocytopenic Purpura (TTP)TTP, sometimes fatal, has been reported following use of Plavix, sometimes after a short exposure (<2 weeks). TTP is a serious condition that requires urgent treatment including plasmapheresis (plasma exchange). It is characterized by thrombocytopenia, microangiopathic hemolytic anemia (schistocytes [fragmented RBCs] seen on peripheral smear), neurological findings, renal dysfunction, and fever [see Adverse Reactions (6.2)].6 ADVERSE REACTIONSThe following serious adverse reactions are discussed below and elsewhere in the labeling: • Bleeding [see Warnings and Precautions (5.2)]• Thrombotic thrombocytopenic purpura [see Warnings and Precautions (5.5)]6.1 Clinical Studies ExperienceBecause clinical trials are conducted under widely varying conditions and durations of follow up, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.Plavix has been evaluated for safety in more than 54,000 patients, including over 21,000 patientstreated for 1 year or more. The clinically important adverse reactions observed in trialscomparing Plavix plus aspirin to placebo plus aspirin and trials comparing Plavix alone to aspirinalone are discussed below.BleedingCUREIn CURE, Plavix use with aspirin was associated with an increase in major bleeding (primarilygastrointestinal and at puncture sites) compared to placebo with aspirin (see Table 1). Theincidence of intracranial hemorrhage (0.1%) and fatal bleeding (0.2%) were the same in bothgroups. Other bleeding events that were reported more frequently in the clopidogrel group wereepistaxis, hematuria, and bruise.The overall incidence of bleeding is described in Table 1.Table 1: CURE Incidence of Bleeding Complications (% patients)PlaceboEvent Plavix(+ aspirin)* (+ aspirin)*(n=6259)(n=6303)§Major bleeding † 3.7 ‡ 2.7Life-threatening bleeding 2.2 1.8Fatal 0.2 0.25 g/dL hemoglobin drop 0.9 0.9Requiring surgical intervention 0.7 0.7strokes 0.1 0.1HemorrhagicRequiringinotropes 0.5 0.5Requiring transfusion (≥4 units) 1.2 1.0Other major bleeding 1.6 1.0disabling 0.4 0.3SignificantlyIntraocular bleeding with 0.05 0.03significant loss of visionRequiring 2-3 units of blood 1.3 0.9Minor bleeding ¶ 5.1 2.4* Other standard therapies were used as appropriate.† Life-threatening and other major bleeding.‡ Major bleeding event rate for Plavix + aspirin was dose-dependent on aspirin: <100 mg = 2.6%;100-200 mg = 3.5%; >200 mg = 4.9%Major bleeding event rates for Plavix + aspirin by age were: <65 years = 2.5%, ≥65 to <75 years= 4.1%, ≥75 years = 5.9%§ Major bleeding event rate for placebo + aspirin was dose-dependent on aspirin: <100 mg = 2.0%;100-200 mg = 2.3%; >200 mg = 4.0%Major bleeding event rates for placebo + aspirin by age were: <65 years = 2.1%, ≥65 to <75 years =3.1%, ≥75 years = 3.6%¶ Led to interruption of study medication.Ninety-two percent (92%) of the patients in the CURE study received heparin or low molecularweight heparin (LMWH), and the rate of bleeding in these patients was similar to the overallresults.COMMITIn COMMIT, similar rates of major bleeding were observed in the Plavix and placebo groups, both of which also received aspirin (see Table 2).Table 2: Incidence of Bleeding Events in COMMIT (% patients)Type of bleeding Plavix(+ aspirin)(n=22961)Placebo(+ aspirin)(n=22891)p-valueMajor* noncerebral or cerebral bleeding** Major noncerebralFatalHemorrhagic strokeFatal 0.60.40.20.20.20.50.30.20.20.20.590.480.900.910.81Other noncerebral bleeding (non-major) 3.6 3.1 0.005 Any noncerebral bleeding 3.9 3.4 0.004* Major bleeds were cerebral bleeds or non-cerebral bleeds thought to have caused death or that required transfusion.** The relative rate of major noncerebral or cerebral bleeding was independent of age. Event rates for Plavix + aspirin by age were: <60 years = 0.3%, ≥60 to <70 years = 0.7%, ≥70 years = 0.8%. Event rates for placebo + aspirin by age were: <60 years = 0.4%, ≥60 to <70 years = 0.6%, ≥70 years = 0.7%.CAPRIE (Plavix vs. Aspirin)In CAPRIE, gastrointestinal hemorrhage occurred at a rate of 2.0% in those taking Plavix vs.2.7% in those taking aspirin; bleeding requiring hospitalization occurred in 0.7% and 1.1%, respectively. The incidence of intracranial hemorrhage was 0.4% for Plavix compared to 0.5%for aspirin.Other bleeding events that were reported more frequently in the Plavix group were epistaxis and hematoma.Other Adverse EventsIn CURE and CHARISMA, which compared Plavix plus aspirin to aspirin alone, there was no differencein the rate of adverse events (other than bleeding) between Plavix and placebo.In CAPRIE, which compared Plavix to aspirin, pruritus was more frequently reported in those taking Plavix. No other difference in the rate of adverse events (other than bleeding) was reported.6.2 Postmarketing ExperienceThe following adverse reactions have been identified during post-approval use of Plavix.Because these reactions are reported voluntarily from a population of an unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.• Blood and lymphatic system disorders: Agranulocytosis, aplastic anemia/pancytopenia, thrombotic thrombocytopenic purpura (TTP)• Eye disorders: Eye (conjunctival, ocular, retinal) bleeding• Gastrointestinal disorders: Gastrointestinal and retroperitoneal hemorrhage with fatal outcome, colitis (including ulcerative or lymphocytic colitis), pancreatitis, stomatitis,gastric/duodenal ulcer, diarrhea• General disorders and administration site condition: Fever, hemorrhage of operative wound• Hepato-biliary disorders: Acute liver failure, hepatitis (non-infectious), abnormal liver function test• Immune system disorders: Hypersensitivity reactions, anaphylactoid reactions, serum sickness• Musculoskeletal, connective tissue and bone disorders: Musculoskeletal bleeding, myalgia, arthralgia, arthritis• Nervous system disorders: Taste disorders, fatal intracranial bleeding, headache• Psychiatric disorders: Confusion, hallucinations• Respiratory, thoracic and mediastinal disorders: Bronchospasm, interstitial pneumonitis, respiratory tract bleeding• Renal and urinary disorders: Increased creatinine levels• Skin and subcutaneous tissue disorders: Maculopapular or erythematous rash, urticaria, bullous dermatitis, eczema, toxic epidermal necrolysis, Stevens-Johnson syndrome,angioedema, erythema multiforme, skin bleeding, lichen planus, generalized pruritus • Vascular disorders: Vasculitis, hypotension7 DRUG INTERACTIONS7.1 CYP2C19 InhibitorsClopidogrel is metabolized to its active metabolite in part by CYP2C19. Concomitant use of drugs that inhibit the activity of this enzyme results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition [see Warnings and Precautions (5.1) and Dosage and Administration (2.4)].Proton Pump Inhibitors (PPI)A study was conducted with Plavix (300 mg loading dose followed by 75 mg/day) administered with a high dose (80 mg/day) of omeprazole. As shown in Table 3 below, with concomitant dosing of omeprazole, exposure (C max and AUC) to the clopidogrel active metabolite and platelet inhibition were substantially reduced. Similar reductions in exposure to the clopidogrel active metabolite and platelet inhibition were observed when Plavix and omeprazole were administered 12 hours apart (data not shown).There are no adequate studies of a lower dose of omeprazole or a higher dose of Plavix in comparison with the approved dose of Plavix.A study was conducted using Plavix (300 mg loading dose followed by 75 mg/day) and a high dose (80 mg/day) of pantoprazole, a PPI with less CYP2C19 inhibitory activity than omeprazole. The plasma concentrations of the clopidogrel active metabolite and the degree of platelet inhibition were less than observed with Plavix alone but were greater than observed when omeprazole 80 mg was co-administered with 300 mg loading dose followed by 75 mg/day of Plavix (Table 3).Table 3: Comparison of Clopidogrel Active Metabolite Exposure and Platelet Inhibition with and without Proton Pump Inhibitors, Omeprazole and Pantoprazole% Change from Plavix (300 mg/75 mg) alone Plavix plus C max (ng/mL) AUC Platelet Inhibition† (%)Day 1 Day 5 Day 1 Day 5** Day 1 Day 5 Omeprazole* 80 mg ↓46% ↓42% ↓45% ↓40% ↓39% ↓21% Pantoprazole 80 mg ↓24% ↓28% ↓20% ↓14% ↓15% ↓11% †Inhibition of platelet aggregation with 5 mcM ADP*Similar results seen when Plavix and omeprazole were administered 12 hours apart.**AUC at Day 5 is AUC0-247.2 Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)Coadministration of Plavix and NSAIDs increases the risk of gastrointestinal bleeding.7.3 Warfarin (CYP2C9 Substrates)Although the administration of clopidogrel 75 mg per day did not modify the pharmacokinetics of S-warfarin (a CYP2C9 substrate) or INR in patients receiving long-term warfarin therapy, coadministration of Plavix with warfarin increases the risk of bleeding because of independent effects on hemostasis.However, at high concentrations in vitr o, clopidogrel inhibits CYP2C9.8 USE IN SPECIFIC POPULATIONS8.1 PregnancyPregnancy Category BReproduction studies performed in rats and rabbits at doses up to 500 and 300 mg/kg/day, respectively (65 and 78 times the recommended daily human dose, respectively, on a mg/m2 basis), revealed no evidence of impaired fertility or fetotoxicity due to clopidogrel. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of a human response, Plavix should be used during pregnancy only if clearly needed.8.3 Nursing MothersStudies in rats have shown that clopidogrel and/or its metabolites are excreted in the milk. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from clopidogrel, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.8.4 Pediatric UseSafety and effectiveness in the pediatric population have not been established.8.5 Geriatric UseOf the total number of subjects in the CAPRIE and CURE controlled clinical studies, approximately 50% of patients treated with Plavix were 65 years of age and older, and 15% were 75 years and older. In COMMIT, approximately 58% of the patients treated with Plavix were 60 years and older, 26% of whom were 70 years and older.The observed risk of bleeding events with Plavix plus aspirin versus placebo plus aspirin by age category is provided in Table 1 and Table 2 for the CURE and COMMIT trials, respectively [see Adverse Reactions (6.1)]. No dosage adjustment is necessary in elderly patients.8.6 Renal ImpairmentExperience is limited in patients with severe and moderate renal impairment [see Clinical Pharmacology (12.2)].8.7 Hepatic ImpairmentNo dosage adjustment is necessary in patients with hepatic impairment [see Clinical Pharmacology (12.2)].10 OVERDOSAGEPlatelet inhibition by Plavix is irreversible and will last for the life of the platelet. Overdose following clopidogrel administration may result in bleeding complications. A single oral dose of clopidogrel at 1500 or 2000 mg/kg was lethal to mice and to rats and at 3000 mg/kg to baboons. Symptoms of acute toxicity were vomiting, prostration, difficult breathing, and gastrointestinal hemorrhage in animals.Based on biological plausibility, platelet transfusion may restore clotting ability.11 DESCRIPTIONPlavix (clopidogrel bisulfate) is a thienopyridine class inhibitor of P2Y12 ADP platelet receptors. Chemically it is methyl (+)-(S)-α-(2-chlorophenyl)-6,7-dihydrothieno[3,2-c]pyridine-5(4H)acetate sulfate (1:1). The empirical formula of clopidogrel bisulfate is C16H16ClNO2S•H2SO4 and its molecular weight is 419.9.The structural formula is as follows:Clopidogrel bisulfate is a white to off-white powder. It is practically insoluble in water at neutral pH but freely soluble at pH 1. It also dissolves freely in methanol, dissolves sparingly in methylene chloride, and is practically insoluble in ethyl ether. It has a specific optical rotation of about +56°.Plavix for oral administration is provided as either pink, round, biconvex, debossed, film-coated tablets containing 97.875 mg of clopidogrel bisulfate which is the molar equivalent of 75 mg of clopidogrel base or pink, oblong, debossed film-coated tablets containing 391.5 mg of clopidogrel bisulfate which is the molar equivalent of 300 mg of clopidogrel base.Each tablet contains hydrogenated castor oil, hydroxypropylcellulose, mannitol, microcrystalline cellulose and polyethylene glycol 6000 as inactive ingredients. The pink film coating contains ferric oxide, hypromellose 2910, lactose monohydrate, titanium dioxide and triacetin. The tablets are polished with Carnauba wax.12 CLINICAL PHARMACOLOGY12.1 Mechanism of ActionClopidogrel is an inhibitor of platelet activation and aggregation through the irreversible binding of its active metabolite to the P2Y12 class of ADP receptors on platelets.12.2 PharmacodynamicsClopidogrel must be metabolized by CYP450 enzymes to produce the active metabolite that inhibits platelet aggregation. The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequentADP-mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible. Consequently, platelets exposed to clopidogrel’s active metabolite are affected for the remainder of their lifespan (about 7 to 10 days). Platelet aggregation induced by agonists other than ADP is also inhibited by blocking the amplification of platelet activation by released ADP.Dose-dependent inhibition of platelet aggregation can be seen 2 hours after single oral doses of Plavix. Repeated doses of 75 mg Plavix per day inhibit ADP-induced platelet aggregation on the first day, and inhibition reaches steady state between Day 3 and Day 7. At steady state, the average inhibition level observed with a dose of 75 mg Plavix per day was between 40% and 60%. Platelet aggregation and bleeding time gradually return to baseline values after treatment is discontinued, generally in about 5 days.Geriatric PatientsElderly (≥75 years) and young healthy subjects had similar effects on platelet aggregation. Renally-Impaired PatientsAfter repeated doses of 75 mg Plavix per day, patients with severe renal impairment (creatinine clearance from 5 to 15 mL/min) and moderate renal impairment (creatinine clearance from 30 to 60 mL/min) showed low (25%) inhibition of ADP-induced platelet aggregation.。
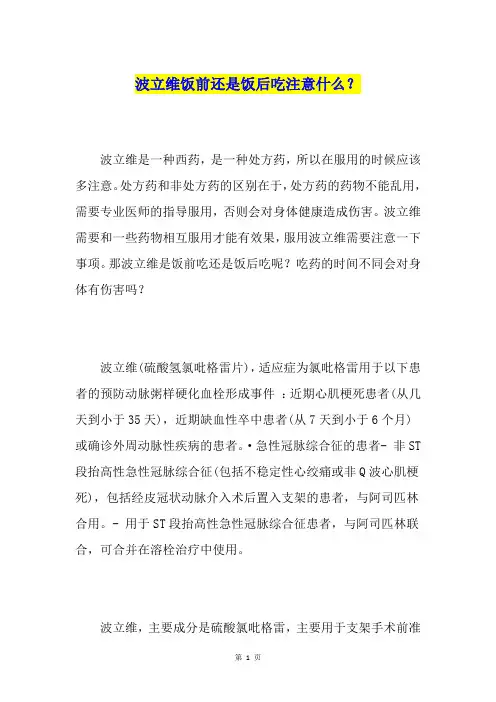
波立维饭前还是饭后吃注意什么?波立维是一种西药,是一种处方药,所以在服用的时候应该多注意。
处方药和非处方药的区别在于,处方药的药物不能乱用,需要专业医师的指导服用,否则会对身体健康造成伤害。
波立维需要和一些药物相互服用才能有效果,服用波立维需要注意一下事项。
那波立维是饭前吃还是饭后吃呢?吃药的时间不同会对身体有伤害吗?波立维(硫酸氢氯吡格雷片),适应症为氯吡格雷用于以下患者的预防动脉粥样硬化血栓形成事件:近期心肌梗死患者(从几天到小于35天),近期缺血性卒中患者(从7天到小于6个月)或确诊外周动脉性疾病的患者。
·急性冠脉综合征的患者- 非ST 段抬高性急性冠脉综合征(包括不稳定性心绞痛或非Q波心肌梗死),包括经皮冠状动脉介入术后置入支架的患者,与阿司匹林合用。
- 用于ST段抬高性急性冠脉综合征患者,与阿司匹林联合,可合并在溶栓治疗中使用。
波立维,主要成分是硫酸氯吡格雷,主要用于支架手术前准备和支架手术后防止支架血栓出现,是一种血小板聚集抑制剂。
我们所说的进口波立维,是指由赛诺菲-安万特生产的波立维,又叫硫酸氢氯吡格雷片。
波立维是支架手术后的常用药,波立维的副作用还是比较常见的,例如出血、血液病和皮疹等。
总体来讲,胃肠道反应的发生率(如腹痛、消化不良、胃炎和便秘)氯吡格雷组为27.1%,而阿司匹林组为29.8%。
而且,由于胃肠道的副作用而退出治疗的氯吡格雷组为3.2%,阿司匹林组为4.0%。
但是,各组临床严重副反应的发生率没有统计学差异(3.0%vs.3.6%)。
两个治疗组最常见不良事件为:腹痛、消化不良、腹泻和恶心。
其他还有便秘、牙病症、眩晕和胃炎等。
腹泻发生率氯吡格雷组为4.5%,明显高于阿司匹林组(3.4%)。
严重腹泻的发生率两治疗组相似(0.2%vs.0.1%)。
消化道,胃及十二指肠溃疡的发生率氯吡格雷组为0.7%,而阿司匹林组为1.2%。
波立维的服用需要大家多注意,应该听从医生的建议,药物不能在自己不了解的情况下乱服用,防止对身体健康有影响。
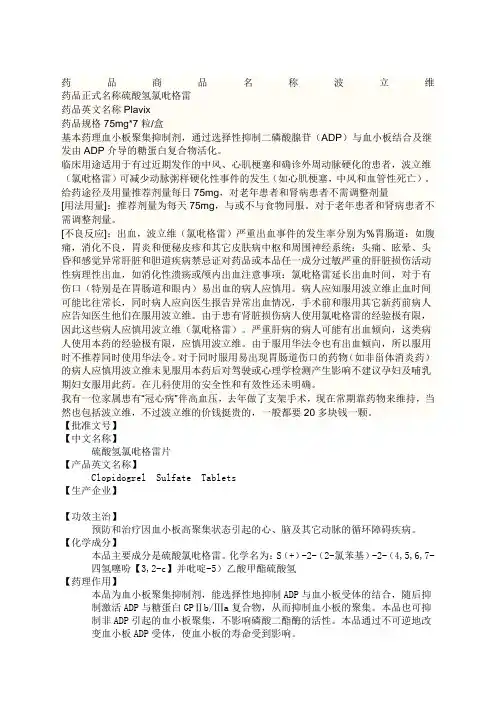
药品商品名称波立维药品正式名称硫酸氢氯吡格雷药品英文名称Plavix药品规格75mg*7粒/盒基本药理血小板聚集抑制剂,通过选择性抑制二磷酸腺苷(ADP)与血小板结合及继发由ADP介导的糖蛋白复合物活化。
临床用途适用于有过近期发作的中风、心肌梗塞和确诊外周动脉硬化的患者,波立维(氯吡格雷)可减少动脉粥样硬化性事件的发生(如心肌梗塞,中风和血管性死亡)。
给药途径及用量推荐剂量每日75mg,对老年患者和肾病患者不需调整剂量[用法用量]:推荐剂量为每天75mg,与或不与食物同服。
对于老年患者和肾病患者不需调整剂量。
[不良反应]:出血,波立维(氯吡格雷)严重出血事件的发生率分别为%胃肠道:如腹痛,消化不良,胃炎和便秘皮疹和其它皮肤病中枢和周围神经系统:头痛、眩晕、头昏和感觉异常肝脏和胆道疾病禁忌证对药品或本品任一成分过敏严重的肝脏损伤活动性病理性出血,如消化性溃疡或颅内出血注意事项:氯吡格雷延长出血时间,对于有伤口(特别是在胃肠道和眼内)易出血的病人应慎用。
病人应知服用波立维止血时间可能比往常长,同时病人应向医生报告异常出血情况,手术前和服用其它新药前病人应告知医生他们在服用波立维。
由于患有肾脏损伤病人使用氯吡格雷的经验极有限,因此这些病人应慎用波立维(氯吡格雷)。
严重肝病的病人可能有出血倾向,这类病人使用本药的经验极有限,应慎用波立维。
由于服用华法令也有出血倾向,所以服用时不推荐同时使用华法令。
对于同时服用易出现胃肠道伤口的药物(如非甾体消炎药)的病人应慎用波立维未见服用本药后对驾驶或心理学检测产生影响不建议孕妇及哺乳期妇女服用此药。
在儿科使用的安全性和有效性还未明确。
我有一位家属患有“冠心病”伴高血压,去年做了支架手术,现在常期靠药物来维持,当然也包括波立维,不过波立维的价钱挺贵的,一般都要20多块钱一颗。
【批准文号】【中文名称】硫酸氢氯吡格雷片【产品英文名称】Clopidogrel Sulfate Tablets【生产企业】【功效主治】预防和治疗因血小板高聚集状态引起的心、脑及其它动脉的循环障碍疾病。
硫酸氢氯吡格雷片的功效与作用硫酸氢氯吡格雷片的功效与作用硫酸氢氯吡格雷片是一种常用的抗血小板药物,广泛应用于心血管系统疾病的治疗中。
它能够抑制血小板聚集和血栓形成,对于预防心血管事件的发生起到重要的作用。
本文将详细介绍硫酸氢氯吡格雷片的功效与作用,包括适应症、药理学作用、副作用等。
一、适应症硫酸氢氯吡格雷片主要用于以下疾病的治疗和预防:1. 心肌梗死和不稳定性心绞痛:心肌梗死和不稳定性心绞痛是由于冠状动脉狭窄、血流受阻造成的心肌缺血引起的疾病。
硫酸氢氯吡格雷片能够减少血小板聚集,降低血栓的形成风险,从而预防心肌梗死和心绞痛的发生。
2. 冠状动脉支架术后:冠状动脉支架术是一种介入性治疗方法,用于治疗冠状动脉疾病患者。
在支架术后,血小板的聚集和形成血栓的风险增加,因此需要使用硫酸氢氯吡格雷片进行抗血小板治疗,预防血栓的发生。
3. 脑血管疾病的预防:脑血管疾病是指脑供血不足引起的疾病,如脑梗死和短暂性脑缺血发作。
硫酸氢氯吡格雷片可以抑制血小板聚集,降低血栓形成的风险,预防脑血管意外的发生。
4. 外周动脉疾病的治疗:外周动脉疾病指下肢动脉或其他区域动脉狭窄或闭塞引起的疾病,如闭塞性动脉硬化、动脉栓塞等。
硫酸氢氯吡格雷片可以改善血流,防止血栓的形成,减轻病情。
二、药理学作用硫酸氢氯吡格雷片的主要作用机制是通过抑制血小板聚集和减少血栓的形成,从而预防和治疗心血管疾病。
1. 抑制血小板聚集:硫酸氢氯吡格雷片能够通过抑制ADP受体P2Y12和血栓素受体的激活,阻断血小板聚集的过程。
它可以阻止ADP和血栓素的结合,使血小板不能聚集形成血栓。
2. 抗炎和抗氧化作用:硫酸氢氯吡格雷片还具有抗炎和抗氧化作用,能够减轻血管内膜的炎症反应,改善血管的功能。
同时,它还能够抑制氧化应激反应,减轻血管内皮细胞的损伤。
3. 降低血浆纤溶活性:硫酸氢氯吡格雷片可通过抑制血小板活化和血栓素的释放,降低血浆纤溶活性,改善血液流变学,减少血栓形成的风险。
氯吡格雷氯吡格雷的商品名为波立维,口服剂波立维为粉红色,圆形,双凸,刻痕薄膜包衣片,一面刻有75,另一面刻有1171,含97.875mg的硫酸氢氯吡格雷,相当于75mg的氯吡格雷碱。
氯吡格雷是一种血小板聚集抑制剂,氯吡格雷的临床疗效来自于CAPRIE临床试验。
目录展开编辑本段药品名称通用名:硫酸氢氯吡格雷片商品名:波立维英文名:Clopidogrel Hydrogen Shlfate Tablets英文商品名:PLAVIX汉语拼音:Liusuanqinglubigelei pian本品主要成份及其化学名称:硫酸氢氯吡格雷编辑本段什么是氯吡格雷氯吡格雷是一种ADP受体阻滞剂,可与血小板膜表面ADP受体结合,使纤维蛋白原无法与糖蛋白GPⅡb/Ⅲa受体结合,从而抑制血小板相互聚集。
CAPRIE:<研究显示,氯吡格雷组一级缺血事件(致命或非致命性缺血性脑卒中、心肌梗死或其他血管性死亡)的危险率为每年5.32 %,而阿司匹林组为每年5.83%。
Zusman等依据现有临床治疗资料,推荐在动脉粥样硬化患者的防治中应用氯吡格雷以预防脑卒中、心肌梗死等急性缺血事件的发生。
但在2004 ACC年会女性CVD预防指南中没有特殊提到服用氯吡格雷预防女性CVD,仅提到在需要服用阿司匹林而又具有禁忌证时将氯吡格雷作为替代药物应用。
编辑本段药理毒理药效学特性氯吡格雷是一种血小板聚集抑制剂。
ATC分类为:BO1AC/04。
氯吡格雷选择性也抑制二磷酸腺苷(ADP)与它的血小板受体的结合及继发的ADP介导的糖蛋白GPlllb/llla复合物的活化,因此可抑制血小板聚集,氯吡格雷必须经生物转化才能抑制血小板的聚集,但是还没有分离出产生这种作用的活性代谢产物。
除ADP外,氯吡格雷还能通过阻断由释放的ADP引起的血小板活化的扩增,抑制其它激动剂诱导的血小板聚集。
氯吡格雷不能抑制磷酸二酯酶的活性。
氯吡格雷通过不可逆地修饰血小板ADP受体起作用。
硫酸氢氯吡格雷片关于《硫酸氢氯吡格雷片》,是我们特意为大家整理的,希望对大家有所帮助。
动脉硬化是一种血管性的病症,动脉硬化是静脉血栓的征兆,动脉硬化是血管里的血液流动性迟缓要肌肉僵硬住那类觉得,动脉硬化病人会常常觉得到四肢发麻,它是要吃一些药品,避免造成静脉血栓,减轻动脉硬化还能够吃点一些食材,比如红提,红提具备清理血管垃圾的功效,对动脉硬化病人有非常大协助,硫酸氢氯吡格雷片便是用于医治动脉硬化的。
硫酸氢氯吡格雷片,主要成分硫酸氢氯吡等,塑料薄膜糖衣片,防止和医治因血小板高集聚情况造成的心、脑以及它主动脉的循环系统阻碍病症。
适用范围氯吡格雷用以下列病人的防止主动脉粥样硬化血栓形成恶性事件:心肌梗死病人(从几日到低于35天),脑缺血卒中患者(从7天到低于6月)或诊断颈静脉主动脉病症的病人。
亚急性冠脉综合征的病人:非ST段拉高性亚急性冠脉综合征(包含不对称性心绞痛或者非Q波心肌梗死),包含经皮冠脉干预手术后嵌入支撑架的病人,与阿斯匹林共用;用以ST段拉高性亚急性冠脉综合征病人,与阿斯匹林协同,可合拼在栓塞治疗中应用。
基因遗传药学:依据参考文献数据信息,存有遗传CYP 2C19作用减少的病人与CYP 2C19作用一切正常的病人对比,对氯吡格雷特异性类化合物的全身曝露较低,抗血小板功效减少,而且在心肌梗塞后心脑血管病恶性事件的发病率较高。
针对最近有暂时性缺血性恶性事件发病或脑卒中的病人,再次出现脑缺血恶性事件的风险性较高,阿斯匹林和氯吡格雷相互用药已被确认提升流血风险性。
因而,超过己被确认有利的临床医学情况以外的协同医治应慎重运用。
肾脏功能危害病人运用氯吡格雷的工作经验有限,因此这种病人应谨慎使用氯吡格雷。
针对可能有流血趋向的轻中度肝胆疾病病人,因为对这种患者应用氯吡格雷的工作经验有限,因而应谨慎使用氯吡格雷。
身患少见的遗传疾病-半乳糖不耐症,Lapp乳糖酶注意力不集中症状或葡萄糖-半乳糖消化吸收欠佳的病人不可应用此药。
药品名称】硫酸氯吡格雷片(波立维)【性状】本品为粉红色圆形薄膜衣片。
【适应症】适用于有过近期发作的中风,心肌梗死和确诊外周动脉疾病的患者,该药可减少动脉粥洋硬化事件的发生(如心肌梗死,中风和血管性死亡)。
与阿司匹林联合,用于非ST段抬高性急性冠脉综合症(不稳定性心绞痛或非Q波心肌梗死)患者。
【用法用量】波利维的推荐剂量是每天75mg,与或不与食物同服。
对于老年患者不需调整剂量。
非ST段抬高性急性冠状综合征(不稳定性心绞痛或非Q波心肌梗死)患者,应以单次负荷量氯吡格雷300mg开始,然后以75mg每日一次连续服药(合用阿司匹林75 mg~325mg/日)。
由于服用较高剂量的阿司匹林伴随有较高的出血性危险,故推荐阿司匹林的剂量不应超过100mg。
最佳疗程尚未正式确定。
临床实验资料支持用药12个月,用药3个月时的益处最大(参见药效学特性)。
儿童和未成年人:18岁以下受试者的安全性、有效性尚未建立。
【不良反应】详见说明书。
【禁忌】1、对活性物质或本品任一成份过敏。
2、严重肝脏损伤。
3、活动性病理性出血,如消化性溃疡或颅内出血。
4、哺乳(参见妊娠和哺乳)【注意事项】由于出血和血液学不良反应的危险性,在治疗过程中一旦出现出血的临床症状,就应立即考虑进行血细胞计数和或其它适当的检查。
与其它抗血小板药物一样,因创伤、外科手术或其它病理状态使出血危险性增加的病人和接受阿司匹林、非体抗炎药、肝素、血小板糖蛋白Hb/Iha(GPllb/IIIa)结抗剂或溶栓药物治疗病人应慎用氯吡格雷,病人应密切随访,注意出血包括隐性出血的任何体征,特别是在治疗的最初几周和或心脏介入治疗,外科手术之后。
因可能使出血加重,不推荐氯吡格雷与华法林合用。
在需要进行择期手术的患者,如抗血小板治疗并非必须,则应在术前停用氯吡格雷7天以上。
氯吡格雷延长出血时间,患有出血性疾病(特别是胃肠、眼内疾病)的患者慎用。
应告诉患者,当他们服用氯吡格雷(单用或也阿司匹林合用)时止血时间可能比往常长,同时病人应向医生报告异常出血情况(部位和出血时间)。