脑出血大病历
- 格式:doc
- 大小:27.00 KB
- 文档页数:3
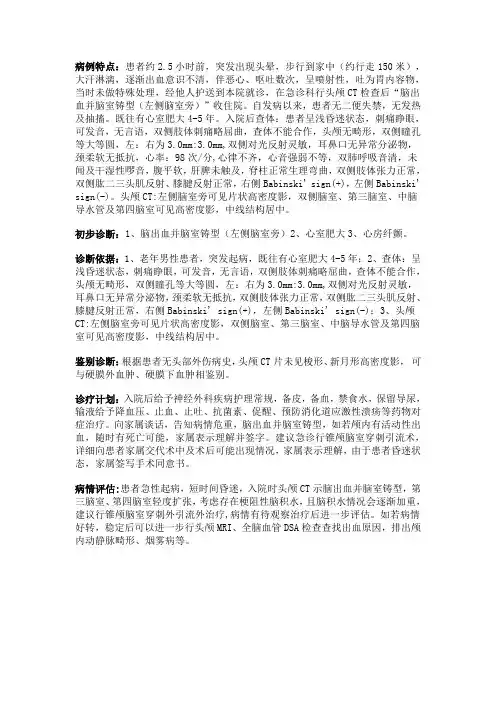
病例特点:患者约2.5小时前,突发出现头晕,步行到家中(约行走150米),大汗淋漓,逐渐出血意识不清,伴恶心、呕吐数次,呈喷射性,吐为胃内容物,当时未做特殊处理,经他人护送到本院就诊,在急诊科行头颅CT检查后“脑出血并脑室铸型(左侧脑室旁)”收住院。
自发病以来,患者无二便失禁,无发热及抽搐。
既往有心室肥大4-5年。
入院后查体:患者呈浅昏迷状态,刺痛睁眼,可发音,无言语,双侧肢体刺痛略屈曲,查体不能合作,头颅无畸形,双侧瞳孔等大等圆,左:右为3.0mm:3.0mm,双侧对光反射灵敏,耳鼻口无异常分泌物,颈柔软无抵抗,心率:98次/分,心律不齐,心音强弱不等,双肺呼吸音清,未闻及干湿性啰音,腹平软,肝脾未触及,脊柱正常生理弯曲,双侧肢体张力正常,双侧肱二三头肌反射、膝腱反射正常,右侧Babinski' sign(+),左侧Babinski' sign(-)。
头颅CT:左侧脑室旁可见片状高密度影,双侧脑室、第三脑室、中脑导水管及第四脑室可见高密度影,中线结构居中。
初步诊断:1、脑出血并脑室铸型(左侧脑室旁)2、心室肥大3、心房纤颤。
诊断依据:1、老年男性患者,突发起病,既往有心室肥大4-5年;2、查体:呈浅昏迷状态,刺痛睁眼,可发音,无言语,双侧肢体刺痛略屈曲,查体不能合作,头颅无畸形,双侧瞳孔等大等圆,左:右为3.0mm:3.0mm,双侧对光反射灵敏,耳鼻口无异常分泌物,颈柔软无抵抗,双侧肢体张力正常,双侧肱二三头肌反射、膝腱反射正常,右侧Babinski' sign(+),左侧Babinski' sign(-);3、头颅CT:左侧脑室旁可见片状高密度影,双侧脑室、第三脑室、中脑导水管及第四脑室可见高密度影,中线结构居中。
鉴别诊断:根据患者无头部外伤病史,头颅CT片未见梭形、新月形高密度影,可与硬膜外血肿、硬膜下血肿相鉴别。
诊疗计划:入院后给予神经外科疾病护理常规,备皮,备血,禁食水,保留导尿,输液给予降血压、止血、止吐、抗菌素、促醒、预防消化道应激性溃疡等药物对症治疗。
脑出血后遗症病历模板范文英文回答:After suffering from a cerebral hemorrhage, I experienced various sequelae that have significantly impacted my daily life. One of the most noticeable effects is the weakness and lack of coordination in my right side. This condition, known as hemiparesis, makes it difficultfor me to perform simple tasks such as brushing my teeth or tying my shoelaces. I often struggle to maintain balance and stability while walking, and I require the assistance of a cane or walker for support.Another common aftereffect of the cerebral hemorrhage is aphasia, which affects my ability to communicate effectively. I often struggle to find the right words or form coherent sentences. This can be frustrating and sometimes leads to misunderstandings or misinterpretations. For example, I may intend to say "I need to go to the store," but end up saying something completely unrelatedlike "I like the color blue." This language impairment has made it challenging for me to express myself and engage in conversations with others.Additionally, I have experienced cognitive difficulties, such as memory loss and difficulty concentrating. I often forget appointments, names, and important details. This can be quite embarrassing and has caused me to rely heavily on reminders and notes to help me stay organized. I also findit challenging to focus on tasks for an extended period of time, as my mind tends to wander.Furthermore, I have noticed changes in my emotionalstate since the cerebral hemorrhage. I often feel more irritable and easily frustrated, which can lead tooutbursts of anger or sadness. These mood swings have strained my relationships with family and friends, as they may not understand the underlying reasons for my emotional reactions.中文回答:在脑出血之后,我经历了各种后遗症,对我的日常生活产生了显著影响。
脑出血病历书写范文英文回答:I remember the day vividly. It was a sunny afternoon when I suddenly felt a sharp pain in my head. It felt like someone was hitting me with a hammer. I tried to ignore it at first, thinking it would go away on its own. But as the pain intensified, I knew something was seriously wrong.I stumbled to the nearest hospital, clutching my headin agony. The doctors rushed me into the emergency room and performed a series of tests. It was then that they discovered I had suffered a cerebral hemorrhage, also known as a brain bleed.The doctor explained that a cerebral hemorrhage occurs when a blood vessel in the brain ruptures and bleeds into the surrounding tissue. This can be caused by various factors such as high blood pressure, trauma, or a weak blood vessel. In my case, it was due to untreatedhypertension.The doctor informed me that immediate treatment was crucial to prevent further damage to my brain. They performed a craniotomy to remove the blood clot and relieve the pressure on my brain. I was then placed in theintensive care unit for close monitoring.During my recovery, I experienced a range of symptoms.I had difficulty speaking and understanding others, a condition known as aphasia. It was frustrating not being able to communicate effectively. Physical therapy helped me regain strength and coordination, but it was a long and arduous process.The support of my family and friends was invaluable during this time. They encouraged me to keep pushing forward and never give up. It was their love and encouragement that kept me going, even on the darkest days.Now, several months later, I am proud to say that I have made significant progress in my recovery. While Istill have some lingering effects, such as occasional headaches and fatigue, I am grateful to be alive and ableto enjoy life once again.中文回答:我清楚地记得那天的情景。
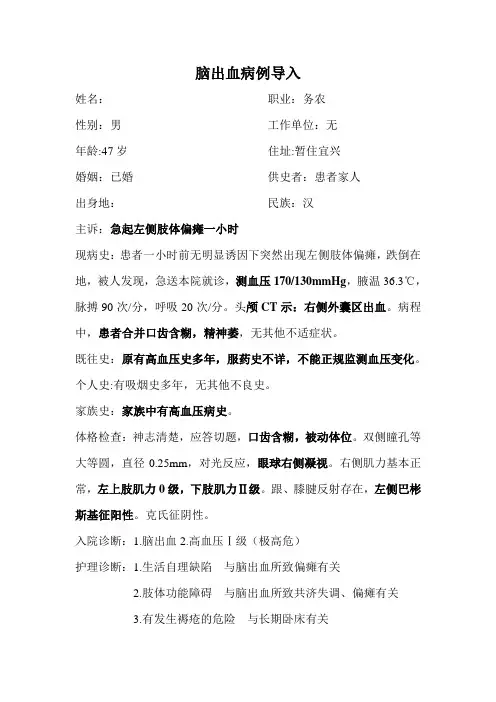
脑出血病例导入姓名:职业:务农性别:男工作单位:无年龄:47岁住址:暂住宜兴婚姻:已婚供史者:患者家人出身地:民族:汉主诉:急起左侧肢体偏瘫一小时现病史:患者一小时前无明显诱因下突然出现左侧肢体偏瘫,跌倒在地,被人发现,急送本院就诊,测血压170/130mmHg,腋温36.3℃,脉搏90次/分,呼吸20次/分。
头颅CT示:右侧外囊区出血。
病程中,患者合并口齿含糊,精神萎,无其他不适症状。
既往史:原有高血压史多年,服药史不详,不能正规监测血压变化。
个人史:有吸烟史多年,无其他不良史。
家族史:家族中有高血压病史。
体格检查:神志清楚,应答切题,口齿含糊,被动体位。
双侧瞳孔等大等圆,直径0.25mm,对光反应,眼球右侧凝视。
右侧肌力基本正常,左上肢肌力0级,下肢肌力Ⅱ级。
跟、膝腱反射存在,左侧巴彬斯基征阳性。
克氏征阴性。
入院诊断:1.脑出血2.高血压Ⅰ级(极高危)护理诊断:1.生活自理缺陷与脑出血所致偏瘫有关2.肢体功能障碍与脑出血所致共济失调、偏瘫有关3.有发生褥疮的危险与长期卧床有关4.潜在并发症:脑疝与脑水肿有关5.恐惧与担心疾病预后有关护理措施1.一般护理:要绝对卧床休息,24~48h尽量避免搬动,头部抬高30°,防止再度出血。
保持静脉补液通畅,遵医嘱给予快速脱水剂。
做好基础护理,保持床褥清洁干燥,定时翻身拍背,防止褥疮。
2.严密观察:严密观察生命体征变化,神志瞳孔变化,发现异常及时汇报医生处理。
3.保持肢体功能:用软枕垫起双下肢,保持功能位,防止足下垂;每日做关节运动和肌肉按摩,防止肌肉萎缩和畸形。
4.心理护理:耐心解释病情病因,治疗措施,预后情况,鼓励病人及家属参与康复锻炼;讲解疾病相关知识,增强病人信心。
【下载本文档,可以自由复制内容或自由编辑修改内容,更多精彩文章,期待你的好评和关注,我将一如既往为您服务】。
脑出血病历好地符合您的需求】病例:脑出血导致左侧肢体偏瘫该患者为47岁的男性,职业为农民,无工作单位,目前暂住宜兴。
患者已婚,由其家人提供病史。
他的主诉是急起左侧肢体偏瘫,已持续一小时。
患者一小时前突然出现左侧肢体偏瘫,跌倒在地。
他被送往医院就诊,检查结果显示他的血压为170/130mmHg,腋温为36.3℃,脉搏90次/分,呼吸20次/分。
头颅CT检查显示右侧外囊区出血。
在病程中,患者还出现口齿含糊、精神萎靡等症状。
患者有多年的高血压史,但服药史不详,也没有进行正规的血压监测。
他有吸烟史,但没有其他不良史。
患者的家族中有高血压病史。
在体格检查中,患者神志清楚,应答切题,但口齿含糊,需要被动体位。
双侧瞳孔等大等圆,直径0.25mm,对光反应,眼球右侧凝视。
右侧肌力基本正常,左上肢肌力级,下肢肌力Ⅱ级。
跟、膝腱反射存在,左侧巴彬斯基征阳性。
克氏征阴性。
患者的入院诊断为脑出血和高血压Ⅰ级(极高危)。
护理诊断包括生活自理缺陷与脑出血所致偏瘫有关、肢体功能障碍与脑出血所致共济失调、偏瘫有关、有发生褥疮的危险与长期卧床有关、潜在并发症:脑疝与脑水肿有关、恐惧与担心疾病预后有关。
为了治疗患者,我们采取了一系列护理措施。
这些措施包括一般护理,如绝对卧床休息、避免搬动、头部抬高30°、保持静脉补液通畅等;严密观察,如严密观察生命体征变化、神志瞳孔变化等;保持肢体功能,如用软枕垫起双下肢、每日做关节运动和肌肉按摩等;以及心理护理,如耐心解释病情病因、治疗措施、预后情况、鼓励病人及家属参与康复锻炼等。
以上是我们对该患者的护理措施,希望能够帮助他尽快康复。

急性脑出血病历模板范文英文回答:Acute cerebral hemorrhage, also known as acute stroke, is a medical condition characterized by bleeding in the brain. It is a serious and life-threatening condition that requires immediate medical attention.In my case, I experienced sudden and severe headache, along with weakness and numbness on one side of my body. I also had difficulty speaking and understanding others. These symptoms are common in acute cerebral hemorrhage and are caused by the bleeding in the brain, which puts pressure on the surrounding tissues and disrupts their normal function.Upon arrival at the hospital, the medical team performed a series of tests to confirm the diagnosis. They conducted a physical examination, including checking my blood pressure and neurological assessment. They alsoordered a CT scan to visualize the bleeding in the brainand determine its location and extent.Once the diagnosis was confirmed, the medical team immediately started the treatment. They administered medication to control my blood pressure and prevent further bleeding. They also monitored my vital signs closely and provided supportive care to ensure my comfort and stability.During my hospital stay, I received physical therapyand speech therapy to regain my strength and improve my communication skills. The medical team also provided education and support to me and my family, explaining the importance of lifestyle modifications and medication adherence to prevent future episodes.Overall, the treatment and care I received were excellent. The medical team was knowledgeable and compassionate, and they took the time to listen to my concerns and answer my questions. They made me feel comfortable and reassured throughout my recovery process.中文回答:急性脑出血,也被称为急性中风,是一种在脑部出血的医疗情况。
甲脑出血病历临床005班朱川病史简述:男性患者,45岁,于13日上午9时许在工地干活时,突发左侧肢体无力,不能站立,左手不能持物,伴有头痛、恶心,但未吐出。
急来我院急诊,行头颅CT检查,示右侧基底节区出血(急性期)。
予甘露醇、脑复康、雷尼替丁等药物治疗,并收入院。
有低热,饮食差,睡眠欠佳等表现,否认有意识障碍及抽搐。
患者既往体健,否认有高血压、糖尿病史,否认外伤手术史。
体温36.6 C,心率72次/分,呼吸20次/分,血压185/105mmHg o 嗜睡,时有烦躁,查体欠合作,答话尚切题,全身皮肤黏膜未见明显黄染,全身浅表淋巴结未及肿大,口唇未见明显紫纟甘,双肺呼吸音粗,未闻及明显干湿罗音,心率72次/ 分,律齐,心前区瓣膜未闻及明显病理杂音,腹平软,肝脾无肿大,双下肢未见水肿。
神经系统查体:神昏,嗜睡,语言欠利。
双侧瞳孔等大等圆,直径3.5mm,光反应灵敏,眼球各向活动灵活充分,未引出明显复视及眼震, 左侧鼻唇沟稍浅,伸舌左偏,颈部抵抗,克氏征阳性,布氏征阳性,左侧肢体肌张力减低,左上肢肌力0级,左下肢肌力1级,双侧病理征阴性,左侧深浅感觉较右侧减退。
定位诊断:定性诊断:患者年龄超过40岁,自活动中起病,病程较急,短时间内达到高峰,故定性为脑出血。
辅助检查:头颅CT(04.10.09)示右侧基底节区出血(急性期)鉴别诊断:1、脑梗死:多在睡眠时发病,不伴颅内高压,病情发展缓慢,有时需数天症状达到高峰,头颅CT示病灶部有低密度灶。
且头颅CT为区别脑梗死和脑岀血的最可靠方法,故据此排除本病。
2、颅内占位性病变:颅内肿瘤、硬膜下血肿、脑脓肿均可呈卒中样发作,岀现偏瘫及局灶症状。
硬膜下血肿有外伤史,本病可排除,脑脓肿、颅内肿瘤病情相对缓慢,行头颅CT检查可以鉴别。
急性期治疗:保持安静,调整血压,防止继续出血,控制脑水肿,降低颅压,加强护理,防治并发症。
恢复期治疗:病情平稳,血肿大部分消失后,可考虑康复治疗。
脑出血病历分析【脑出血病历分析】1. 引言脑出血是一种严重危及生命的疾病,其突发性和高死亡率备受关注。
通过对某病例的脑出血病历进行分析,我们可以更好地理解这一疾病的发病机制、临床表现、诊断和治疗方法等诸多方面。
2. 病人信息及入院情况本次分析的病人是一位56岁的男性,他突然出现严重头痛、乏力和言语不清等症状,并在这些症状发作后不久被紧急送往医院。
病人无明显的既往病史,但有家族中的高血压病史。
3. 体征和初步检查结果病人入院时,出现明显的昏迷状态,血压升高,心跳加快,体温略高。
神经系统检查发现病人意识丧失,双眼视力减退,颅内压增高。
头颅CT检查显示了脑出血的高密度影像。
4. 诊断和进一步检查根据症状和初步检查结果,医生初步诊断为脑出血。
为了确定出血的原因以及出血范围的大小,进一步进行了脑磁共振成像(MRI)、脑血管造影和血液检查等检查。
MRI显示出血位于左侧大脑半球的深部,脑血管造影发现左侧中动脉瘤。
血液检查结果显示血小板减少,凝血功能异常。
5. 治疗和恢复过程在确诊为脑出血后,病人被转入神经外科重症监护室,进行紧急手术治疗。
手术采用了介入手术的方法,成功地修补了破裂的中动脉瘤,并停止了出血。
术后病人接受了积极的抗休克、脱水和减压治疗,并通过药物控制血压和凝血功能来降低再出血和并发症的风险。
经过数周的治疗和康复训练,病人逐渐苏醒,恢复了一定的生活自理能力。
6. 讨论与总结本病历的分析显示了脑出血的临床特点和处理方法。
脑出血常常突发且危急,诊断和治疗的迅速性至关重要。
脑出血的起因往往与高血压以及血管畸形等有关。
虽然手术治疗是控制出血的最有效方法,但后续的康复治疗同样重要。
对于脑出血患者,康复训练可以改善他们的神经功能和生活质量。
7. 对脑出血的理解和观点脑出血是一种严重的脑血管疾病,患者的生命常常受到严重威胁。
预防和控制高血压以及定期进行身体检查是预防脑出血的重要措施。
在遭受脑出血的病人康复过程中,家人的支持和患者的积极治疗配合都非常重要。
脑出血死亡病历讨论记录范文英文版Discussion Record of a Cerebral Hemorrhage Death CaseBackground:On [Insert Date], a 58-year-old male patient with a history of hypertension presented to the emergency department with sudden onset of severe headache, vomiting, and loss of consciousness. Upon arrival, the patient was found to be in a coma with a Glasgow Coma Scale (GCS) score of 8. Initial computed tomography (CT) scan of the brain revealed a large intracerebral hemorrhage in the left parietal region.Treatment:The patient was immediately admitted to the intensive care unit (ICU) for management. Intravenous (IV) mannitol was given to reduce intracranial pressure, and the patient was started on a ventilator to assist with breathing. Conservative managementwas planned with close monitoring of the patient's neurological status and serial CT scans to assess the hematoma's progression.Course of Disease:Over the next 24 hours, the patient's condition worsened. He developed bilateral pupillary dilation and decerebrate posturing. Repeated CT scans showed no significant change in the size of the hematoma. Despite aggressive management, the patient did not respond to treatment.Cause of Death:On the second day of admission, the patient succumbed to the hemorrhage due to severe brain damage. The cause of death was attributed to the massive intracerebral hemorrhage.Discussion:The case was discussed among the medical team to identify potential areas of improvement in patient management. It was noted that early surgical intervention might have been beneficial in this case, considering the large size of the hematoma and the patient's deteriorating condition. There wasalso a consensus among the team to improve patient education on the importance of regular follow-up and strict control of hypertension to prevent such complications.Conclusion:This case highlights the importance of prompt diagnosis and aggressive management of intracerebral hemorrhage. Future cases should be evaluated for surgical intervention early to prevent further brain damage and improve outcomes.中文版脑出血死亡病历讨论记录范文背景:[插入日期],一名有高血压病史的58岁男性患者突然出现严重头痛、呕吐和意识丧失,被送至急诊科。
急性脑出血病历范文英文回答:Patient Name: [姓名]Gender: [性别]Age: [年龄]Date of Admission: [入院日期]Presenting Complaint:The patient was admitted to the hospital with a sudden onset of severe headache, dizziness, and loss of consciousness. The family members reported that the patient had difficulty speaking and weakness on the right side of the body.Medical History:The patient has a history of hypertension and has been on antihypertensive medication for the past five years. There is no known history of diabetes, heart disease, or previous stroke.Physical Examination Findings:Upon admission, the patient was unconscious with a Glasgow Coma Scale (GCS) score of 7. The blood pressure was elevated at 180/100 mmHg. Neurological examination revealed right-sided hemiparesis and decreased muscle tone. The patient's pupils were equal and reactive to light.Diagnostic Tests:1. Computed Tomography (CT) scan: The CT scan showed a hyperdense lesion in the left basal ganglia region, consistent with acute intracerebral hemorrhage.2. Complete Blood Count (CBC): The CBC showed a normal white blood cell count and hemoglobin level.3. Coagulation profile: The coagulation profile was within normal limits, ruling out any coagulation disorders.Diagnosis:Based on the clinical presentation and imaging findings, the patient was diagnosed with acute intracerebral hemorrhage.Treatment:The patient was immediately transferred to theintensive care unit (ICU) for close monitoring and management. The treatment included:1. Blood pressure control: Intravenous antihypertensive medications were administered to maintain the bloodpressure below 140/90 mmHg.2. Neurological support: The patient was intubated and mechanically ventilated to ensure adequate oxygenation.Intracranial pressure monitoring was initiated to detect any signs of increased intracranial pressure.3. Symptomatic management: Analgesics were given to alleviate the patient's headache and pain.Outcome:The patient's condition gradually improved over the course of hospitalization. Repeat CT scans showed a reduction in the size of the hemorrhage. The patient regained consciousness and started showing signs of improvement in motor function.中文回答:患者姓名,[姓名]性别,[性别]年龄,[年龄]入院日期,[入院日期]主诉:患者因突发剧烈头痛、头晕和意识丧失而入院。
脑出血恢复期病历书写范文英文回答:Patient Name: [Patient's Name]Date of Admission: [Date of Admission]Date of Discharge: [Date of Discharge]Chief Complaint:The patient was admitted to the hospital with a chief complaint of sudden onset severe headache, dizziness, and loss of consciousness.History of Present Illness:The patient had no significant past medical history. However, the patient experienced a sudden episode of severe headache, followed by dizziness and loss of consciousness.The family members immediately called emergency services, and the patient was rushed to the hospital.Physical Examination:Upon arrival, the patient was unconscious with a Glasgow Coma Scale (GCS) score of 6. The vital signs were unstable, with a blood pressure of 180/100 mmHg, heart rate of 110 beats per minute, and respiratory rate of 20 breaths per minute. The neurological examination revealed right-sided weakness and decreased sensation.Diagnostic Workup:A computed tomography (CT) scan of the brain was performed, which revealed a left-sided intracerebral hemorrhage. The patient also underwent a magnetic resonance imaging (MRI) scan to assess the extent of the hemorrhage and any associated complications.Treatment:The patient was immediately admitted to the intensive care unit (ICU) and closely monitored. The blood pressure was carefully managed to maintain a systolic blood pressure below 140 mmHg. The patient received medications to reduce intracranial pressure and prevent further bleeding. Physical therapy and occupational therapy were initiated to improve motor function and daily activities.Progress and Prognosis:During the hospital stay, the patient gradually regained consciousness and showed improvement in neurological deficits. The right-sided weakness and decreased sensation improved significantly. The patient was able to perform activities of daily living independently. The blood pressure was well controlled, and there were no signs of recurrent bleeding.Discharge Plan:The patient was discharged with a prescription for antihypertensive medication to maintain blood pressurewithin the normal range. Follow-up appointments were scheduled with the neurologist and rehabilitation team for further evaluation and therapy.中文回答:患者姓名,[患者姓名]入院日期,[入院日期]出院日期,[出院日期]主诉:患者因突发剧烈头痛、头晕和意识丧失而被送入医院。
脑干出血病历模板范文# 脑干出血病历一、基本信息姓名:[患者姓名]性别:[男/女]年龄:[X]岁职业:[例如工人、教师等]入院日期:[具体日期]记录日期:[具体日期]二、主诉这患者啊,就突然说脑袋疼得像要炸开了似的,然后就开始晕乎乎的,站都站不稳,还吐了好几次呢,就赶紧送咱们这儿来了。
三、现病史患者之前身体还算可以,没什么大毛病。
就今天上午啊,正干着活(或者正做着啥事儿呢),突然就感觉脑袋“嗡”的一下,那疼痛就像有人在脑袋里敲鼓一样,而且是越敲越猛。
紧接着啊,就觉得天旋地转的,周围的东西都在转圈圈。
腿也发软,差点就直接瘫倒在地上了。
这还不算完,胃里也开始翻江倒海的,吐了好几回,吐出来的都是些吃进去的东西。
家里人一看这情况可吓坏了,赶紧打了120就送到咱们医院来了。
在来医院的路上,患者意识就有点迷糊了,答非所问的。
四、既往史患者以前呢,有点高血压,就像一颗隐藏的小炸弹一样,一直在身体里。
但是他自己也没太当回事儿,有时候想起来就吃点降压药,想不起来就算了。
也没有什么糖尿病啊,心脏病之类的其他大病。
不过呢,患者平时抽烟比较厉害,一天得抽个[X]根烟,就像个小烟囱似的。
喝酒也不少,隔三岔五就得喝上几杯,白酒啤酒都来者不拒。
五、个人史患者出生在[出生地],在那儿长大的。
工作环境嘛,[描述工作环境,例如有点嘈杂,有灰尘之类的]。
平时饮食也不太规律,早餐经常不吃,中午就随便对付一口,晚上有时候又吃得特别多。
作息时间也不太好,经常熬夜,不是看电视就是玩手机,不到半夜不睡觉。
六、家族史家里人呢,他老爸有高血压,看来这高血压还有点家族遗传的意思。
其他的像什么癌症啊,遗传病之类的,家里人倒没发现有。
七、体格检查1. 生命体征体温:[X]℃,就像小火炉似的,有点低热,可能是身体里的炎症在作怪呢。
脉搏:[X]次/分,跳得有点快,就像着急赶路的小马蹄一样。
呼吸:[X]次/分,呼吸也有点急促,感觉像刚跑完步似的。
血压:[X]mmHg,这个血压啊,比平时高不少呢,高血压这个小恶魔又开始兴风作浪了。
脑出血后遗症病历模板范文# 脑出血后遗症病历。
一、基本信息。
姓名:[患者姓名]性别:[男/女]年龄:[X]岁。
职业:[具体职业]住址:[详细住址]二、主诉。
“大夫啊,我之前脑出血了,现在这左边身子就不太听使唤,走路歪歪斜斜的,手也没什么劲儿,还麻得很呢。
”三、现病史。
患者于[发病日期]无明显诱因突发头痛,那疼得啊,就像脑袋要炸开似的,接着就开始恶心、呕吐。
家人一看这情况可吓坏了,赶紧送到咱们医院。
当时做了CT检查,发现是脑出血,出血量大概有[X]毫升呢。
然后就住院进行了紧急治疗,具体就是保守治疗,在医院里躺了好一阵子。
经过治疗后,命算是保住了,可这身体啊,就落下了毛病。
现在呢,患者左边肢体活动不利索。
走路的时候,就像个刚学步的小娃娃,摇摇晃晃的,得有人在旁边扶着点,不然保不准就摔倒了。
这左手啊,拿个轻东西都费劲,想攥紧拳头都不容易,而且老是感觉麻酥酥的,就像有好多小蚂蚁在手上爬来爬去似的。
说话也不利索,有时候想表达个事儿,得费好大劲儿才能说清楚,急得患者直冒汗。
记忆力也大不如前了,刚说过的事儿,转头就忘,患者自己都觉得这脑子像是被浆糊给糊住了。
四、既往史。
患者以前身体还算可以,没什么大病。
就是血压有点高,平时也不太当回事儿,药也是想起来就吃,想不起来就不吃的。
也没有糖尿病、心脏病这些乱七八糟的病。
年轻的时候抽过烟,不过后来戒了,偶尔会喝点小酒。
五、个人史。
患者出生并成长在本地,没去过什么特别的地方。
饮食上啊,比较喜欢吃咸的和油腻的东西,像什么红烧肉啊,咸鱼啊,那都是患者的最爱。
平时运动也不多,没事就喜欢在家里看看电视、打个盹儿。
六、家族史。
家里人身体都还不错,没听说有什么遗传病。
父母都是正常去世的,也不是因为什么大病。
七、体格检查。
1. 生命体征。
体温:[具体体温]℃,正常得很。
脉搏:[X]次/分,也比较平稳。
呼吸:[X]次/分,呼吸还挺顺畅的。
血压:[X]mmHg,还是有点高呢,这可得注意了。
脑出血大病历-回复脑出血大病历是一份医学文件,用于记录患者患上脑出血的详细病情和医学处理过程。
它是医生们诊断和治疗该病时的重要工具,并为其他医护人员提供患者的健康状况。
在本文中,我们将详细讨论脑出血大病历的主要内容和步骤,以增加对该疾病的认识。
脑出血大病历通常开始于第一页的患者信息部分。
这部分包括患者的个人信息,如姓名、年龄、性别和住址。
此外,医生还会记录患者的就诊日期、主诉和症状描述。
在病程记录部分,医生会详细描述患者的病程,即疾病的发展过程。
医生会记录患者何时出现症状以及症状的严重程度。
例如,医生可能会询问患者何时出现头痛、呕吐、意识改变或神经系统问题等症状,以便做出准确的诊断。
接下来,医生会做一份详细的体格检查记录。
这包括测量患者的体温、脉搏、呼吸和血压等基本生命体征。
此外,医生还会检查患者的神经系统功能,以了解脑出血对神经系统的影响。
脑出血大病历的下一部分是实验室检查结果。
医生通常会要求患者进行一系列实验室检查,以帮助诊断和确定疾病的严重程度。
这些检查可能包括血液和尿液检查、凝血功能检查、电解质水平检测以及其他必要的检查。
医生会在病历中记录这些检查的结果,并与正常参考值进行比较,以确定任何异常。
此外,在脑出血大病历中,医生还会记录任何特殊的影像学检查结果,以帮助评估脑出血的程度和定位。
这些影像学检查通常包括头部CT (computed tomography)扫描、MRI(magnetic resonance imaging)和脑血管造影等。
这些检查结果可以帮助医生确定是否需要进行手术或其他治疗。
接下来,医生会记录对患者进行的治疗措施。
这包括药物治疗、手术治疗或其他治疗方法。
医生会详细说明每种治疗措施的目的、剂量和频次,并记录患者的疗效。
例如,医生可能会在病历中写下患者接受了一种特定的抗凝药物,并测量血压以监控治疗效果。
在病历中的最后部分通常是医生的评估和建议。
医生会总结患者的病情、治疗过程和预后,并提供针对患者的建议。
首次病程录患者:***,*性,**岁,宿迁市宿城区龙河镇******人,因“左侧肢体活动受限一月”入院,患者一月前无明显诱因突然出现左侧肢体活动受限,言语不清,于市人民医院查头颅CT示:右侧基底节区脑出血,诊断‘脑出血,高血压病3级极高危,2型糖尿病’住院于手术治疗,好转出院,今到我院就诊,查随机血糖示:18.3mmol/L,为进一步诊治,门诊拟以:“脑出血,高血压病3级极高危,2型糖尿病”收住院,病程中患者无畏寒、发热,无咯血胸痛,无心悸、呼吸困难,无晕厥抽搐,无腹痛腹泻,无恶心、呕吐等不适,饮食睡眠尚可,二便正常。
既往有‘高血压病’病史十年余,血压最高达170/100mmHg,平素为正规口服降压药,血压控制欠佳。
入院查体:T:36.5℃P:87次/分R:20次/分BP:160/100mmHg,发育正常,营养中等,神志清楚,精神差,轮椅推入病房,对答切题。
查体合作,全身皮肤粘膜及巩膜无黄染,未见有蜘蛛痣及肝掌.全身浅表淋巴结未扪及肿大。
头颅正常,五官端正,双眼睑无水肿、充血、下垂,双侧瞳孔等圆等大,对光反射灵敏,鼻通气良好,无脓性分泌物。
口唇无紫绀,舌伸自然,咽红,扁桃体无肿大。
颈软,气管居中,双侧甲状腺无肿大。
颈静脉无怒张,胸廓无畸形,呼吸动度一致,双肺叩诊清音,呼吸音清,未闻及干湿性啰音。
心前区无隆起,无抬举样搏动,心尖搏动位于左锁骨中线第五肋间区,心率87次/分,律齐,各瓣膜听诊区未闻及病理性杂音。
腹部平软,全腹无压痛,无反跳痛及肌紧张。
肝区无叩击痛,肝脾肋下未触及,无移动性浊音,肠鸣音4次/分。
双肾区无叩击痛,四肢及脊柱无畸形,左侧肢体肌力1级,肌张力减低,活动受限,右侧肢体肌力肌张力均正常,双下肢无水肿,生理反射存在,左侧巴氏征阳性,右侧病理放射未引出。
肛门及外生殖器未查。
辅助检查:查头颅CT示:右侧基底节区脑出血,随机血糖示:18.3mmol/L。
初步诊断:1、脑出血,2、高血压病3级极高危,3、2型糖尿病,诊断依据:1、患者为老年男性,56岁,因“左侧肢体活动受限一月”入院;2、病史:既往有‘高血压病’病史十年余,血压最高达170/100mmHg,平素为正规口服降压药,血压控制欠佳,3、临床表现:左侧肢体活动受限,言语不清,4 查体:BP:160/100mmHg,神志清楚,精神差,左侧肢体肌力1级,肌张力减低,活动受限,左侧巴氏征阳性,左侧病理放射未引出。
脑出血大病历
1 / 3
姓名:xxxx 病史陈述者:患者女儿
性别:女 通讯处:xxxxxxxxxxx
年龄:61岁 家庭通讯地址:xxxxxxxx
籍贯:河北省蠡县 亲属姓名:xxxx
民族:汉族 通讯处:xxxxxxxxxx
职业:农民 入院日期:2013 年 3月 11 日 12时 00 分
婚姻状况:已婚
病史采集:2013 年 3 月 11 日 12 时10 分
主诉:头晕伴恶心呕吐3天
现病史:患者缘于3天前骑车时突然出现头晕,摔倒在地,出现意识不清,为一过性,几分钟
后被家人叫醒,可回忆当时情况,患者头晕持续不能缓解,伴有视物旋转,不敢睁眼,自觉
天旋地转,伴有呕吐,呈非喷射性,呕吐物为胃内容物,不伴有头痛,无耳鸣,耳聋,无吞
咽困难、饮水呛咳,无肢体活动及感觉障碍,无肢体抽搐,急就诊于当地医院,查头CT(2013-3-8
河北省蠡县医院)示:右小脑出血,第四脑室受压。 给予输液治疗(具体不详),患者未再
出现呕吐,头晕症状未见明显改善,为求进一步诊治遂来我院。
自发病以来,精神欠佳,饮食量少,睡眠尚充足,保留导尿,未见大便,体重无明显变
化。
既往否认高血压、糖尿病、心脏病病史。
既往史:既往否认高血压、糖尿病、心脏病病史。否认肝炎、结核病史及密切接触史。否认
手术、外伤及输血史,否认食物及药物过敏史,预防接种史不详。
个人史:生于原籍,久居本地,未到过牧区及疫区,居住条件一般,否认粉尘及毒物接触史,
否认性病及冶游史,24岁结婚,育有1女2子,配偶及子女体健。
月经史: 18 3-5/30 46,无痛经史。
家族史:否认家族中其它类似病史,否认传染病史及遗传病史。
体格检查
T36.3℃ P60次/分 R19次/分 Bp183 /108mmHg
发育正常,营养中等,平卧位,病容无特殊,体检合作。全身皮肤无黄染、紫癜、皮疹
及浮肿。表浅淋巴结未触及。头颅无畸形,眼睑无水肿,结膜无充血,巩膜无黄染,外耳道
无分泌物,乳突无压痛。鼻腔通畅,鼻窦无压痛。牙无龋病及缺损,牙龈无出血,扁桃体不
大,咽部无充血。颈软,无颈静脉怒张,未闻血管杂音,气管居中,甲状腺不大。胸部无畸
形,呼吸运动对称,呼吸音清晰,未闻及干湿罗音。心界不大,心率60次/分,律齐,各瓣
膜听诊区未闻及杂音。腹平软,无压痛及反跳痛,无包块,肝、脾未触及,肝上界右锁骨中
线第五肋间,肝、脾区无叩击痛,腹部无移动性浊音,肠鸣音正常存在。脊柱无畸形,无压
痛、叩击痛。肋脊角无叩击痛。四肢无畸形,关节无红肿及运动障碍。外生殖器发育正常,
肛门无外痔、肛裂。
神经系统检查
脑出血大病历
2 / 3
1.一般情况 意识清晰,情感正常,定向力、记忆力、计算力好,理解判断好,自知力存在。
无幻觉、妄想。
言语:正常,无失语及构音不良。
姿势及步态:正常。
2.头颅 头颅大小正常,形状正常,双侧对称,头皮无压痛,无叩击痛,未闻及血管杂音,
头皮无异常。
脑膜神经根症状:颈抵抗约四横指,Kernig(-),Brudzinski(-),LaSegue征(-)。
3.颅神经
1) 嗅神经 嗅觉正常。
2) 视神经 视力 粗测正常。
视野 双侧无缺损。
眼底 未窥入。
瞬目反射 存在。
3) 动眼神经、滑车神经、展神经 睑裂对称,无上睑下垂,眼球各方向运动正常,无复视及
眼球震颤,瞳孔等大,直径2.5mm,等圆,直接、间接光反应均灵敏,调节反射好。
4) 三叉神经 双侧面部痛觉、触觉双侧对称,正常;张口下颌无偏斜,无咀嚼肌萎缩及无力,
双侧角膜反射存在。
5) 面神经 额纹两侧对称,皱额有力;两侧面部对称,无面肌痉挛;呲牙时双侧鼻唇沟对称,
无变浅;鼓腮时无漏气;口角无下垂;双侧闭目有力,舌前2/3味觉正常。
6) 听神经 双侧Rinne试验均气导>骨导,Weber试验居中,Schwabach试验正常。无眩晕
及眼球震颤。
7) 舌咽神经、迷走神经 发音正常,声音无嘶哑,饮水无呛咳,发“阿”音时双侧软腭上提正
常,悬雍垂居中,咽反射正常,咽下运动正常,舌后1/3味觉存在。
8) 副神经 转头及耸肩运动欠合作,胸锁乳突肌上部无萎缩。
9) 舌下神经 张口时舌在口腔正中,伸舌居中,舌肌无萎缩及纤颤。
4.运动系统 右利手
1) 肌容:躯干及四肢肌肉正常,无萎缩及肥大。
2) 不自主运动:无。
3) 肌张力:四肢肌张力正常。
4) 肌力:四肢肌力V级。
5) 共济运动:指鼻试验稳准,跟膝胫试验稳准,轮替试验协调。
6) 步态:卧位。
7) Romberg氏征:欠合作。
5.感觉系统
1) 浅感觉:未见异常。
2) 深感觉:未见异常。
3) 复合感觉:未见异常。
脑出血大病历
3 / 3
6.反射
1) 深反射:肱二头肌肌腱、肱三头肌肌腱、桡骨膜反射、膝腱、踝腱反射(++),无髌阵挛、
踝阵挛。
2) 浅反射:腹壁反射、跖反射正常存在;肛门反射存在。
3) 病理反射:双侧Babinski(+),双划征(+),双侧Hoffmann,Gordon, Chaddock, ,
Oppenhiem,Rossolemo,均未引出。掌颌反射、下颌反射阴性。
7.植物神经系统: 正力型,性征正常,器官发育正常,无汗液分泌障碍,眼心反射正常,
皮肤划纹征正常。
辅助检查
头CT(2013-3-8 xxxxx医院)示:右小脑出血,第四脑室受压 。
初步诊断:
脑出血
医师:xxx