爱必妥ERBITUX_西妥昔单抗cetuximab_使用说明书
- 格式:pdf
- 大小:638.14 KB
- 文档页数:16
西妥昔单抗注射液Cetuximab商品名:爱必妥英文名:Cetuximab Solution for Infusion汉语拼音:Xi Tuo Xi Dan Kang Zhu She Ye【警示语】警告:严重的输液反应。
在大约3%的患者中发生了严重的输液反应,其中一些为致命性的。
注意:因本品目前尚缺乏中国人应用的安全性、有效性数据,故必须在有相关产品应用经验的三级以上医院内(建议在国家临床肿瘤研究基地使用) ,与伊立替康联合用药试用于治疗表达表皮生长因子受体(EGFR) 、经含伊立替康细胞毒治疗失败后的转移性结直肠癌;本品必须在有经验医师的指导下使用。
【成份】本品每20ml溶液含:活性成分:西妥昔单抗100mg其他成分:氯化钠116.88mg,甘氨酸150.14mg,聚山梨酯80 2mg,一水合柠檬酸42.02mg,氢氧化钠(1M)调节pH值至5.5,注射用水加至20ml。
【性状】本品为注射用无色、澄清、透明溶液。
【适应症】西妥昔单抗用于治疗表达表皮生长因子受体(EGFR) 、RAS基因野生型的的转移性结直肠癌:与伊立替康联合用于经含伊立替康治疗失败后的患者。
西妥昔单抗联合FOLFOX(奥沙利铂+亚叶酸钙+5-氟尿嘧啶[5-FU])或FOLFIRI(伊立替康+亚叶酸钙+5-FU)一线治疗RAS野生型(wt)转移性结直肠癌(mCRC)患者、或联合伊立替康(irinotecan)用于对伊立替康化疗无效的患者。
与铂类和氟尿嘧啶化疗联合,用于一线治疗复发和/或转移性头颈部鳞癌。
【规格】100mg(20ml)/瓶【用法用量】西妥昔单抗必须在有使用抗癌药物经验的医师指导下使用。
在用药过程中及用药结束后1小时内,需密切监测患者的状况,并必须配备复苏设备。
在首次滴注本品之前至少1小时,患者必须接受抗组胺药物和皮质类固醇药物的预防用药。
建议在在后续治疗中,每次使用本品之前都对患者进行上述预防用药。
本品每周给药一次。

Phase I Study of Anti–Epidermal Growth Factor Receptor Antibody Cetuximab in Combination With Radiation Therapy in Patients With Advanced Head and Neck Cancer By Francisco Robert,Mark P.Ezekiel,Sharon A.Spencer,Ruby F.Meredith,James A.Bonner,M.B.Khazaeli, Mansoor N.Saleh,Delicia Carey,Albert F.LoBuglio,Richard H.Wheeler,Michael R.Cooper,and Harlan W.WaksalPurpose:To evaluate the safety,pharmacokinetics, and efficacy of a chimeric anti–epidermal growth factor receptor monoclonal antibody,cetuximab,in combina-tion with radiation therapy(RT)in patients with ad-vanced squamous cell carcinoma of the head and neck. Patients and Methods:We treated16patients infive successive treatment schedules.A standard dose esca-lation procedure was used;three patients entered onto the study at each dose level of cetuximab received conventional RT(70Gy,2Gy/d),and thefinal three patients received hyperfractionated RT(76.8Gy,1.2Gy bid).Cetuximab was delivered as a loading dose of100 to500mg/m2,followed by weekly infusions of100to 250mg/m2for7to8weeks.Circulating levels of cetuximab during therapy were determined using a biomolecular interaction analysis core instrument.Hu-man antichimeric antibody response was evaluated with a double-antigen radiometric assay.The recom-mended phase II/III dose was defined as the optimal cetuximab dose level based on the pharmacologic pa-rameters and adverse events.Results:The most commonly reported adverse events were fever,asthenia,transaminase elevation,nausea, and skin toxicities(grade1to2in most patients).Skin toxicity outside of the RTfield was not strictly dose-dependent;however,grade2or higher events were observed in patients treated with higher dose regimens. There was one grade4allergic reaction.Most acute adverse effects were associated with RT(xerostomia, mucositis,and local skin toxicity).No antibodies against cetuximab were detected.All patients achieved an objec-tive response(13complete and two partial remissions). Conclusion:Cetuximab can be safely administered with RT.The recommended dose for phase II/III studies is a loading dose of400to500mg/m2and a mainte-nance weekly dose of250mg/m2.J Clin Oncol19:3234-3243.©2001by American Society of Clinical Oncology.R ADIATION THERAPY(RT)is the mainstay of treat-ment for locally advanced,unresectable squamous cell carcinoma of the head and neck(SCCHN).However, with conventional fractionation of1.8to2.0Gy per fraction for a total dose of60to75Gy,the rate of relapse-free survival is approximately25%,and the majority of patients die from locoregional disease.1,2Tumor cell repopulation during treatment,tumor hypoxia,and intrinsic radioresis-tance represent biologic barriers implicated as causes of treatment failure after primary RT.3-5Numerous attempts to improve local control and long-term survival in advanced SCCHN have been undertaken,such as altered fractionated regimens,combined RT and chemotherapy,radiation sensitizers,and hyperbaric oxy-gen.6-11Although some of these therapeutic approaches have shown encouraging results,not all of them have shown an unequivocal survival benefit,and the treatments often are associated with significant toxicity.Thus,there is a need for newer therapies that produce long-term local control and less toxicity.One novel approach to treatment has been the develop-ment of new agents that target specific growth factors and growth factor receptors.One particular growth factor recep-tor and signal transduction system that has been shown to play an important role in the pathogenesis of SCCHN is the epidermal growth factor receptor(EGFR)and its li-gand.12-14The EGFR system represents a promising thera-peutic target because it is commonly overexpressed in these tumors.15-17Tumor levels of EGFR and its ligand,trans-forming growth factor alpha,have been shown to be significant predictors of tumor staging and clinical out-come.17,18In addition,several studies have reported that repopulation of epithelial tumor cells after exposure to radiation is related to the activation and expression of EGFR.19,20Thesefindings suggest that EGFR blockade may be important in reducing tumor cell repopulation by modulation of cellular proliferation and enhancement of tumor radioresponse.From the Division of Hematology/Oncology,Department of Radia-tion Oncology,Comprehensive Cancer Center,University of Alabamaat Birmingham,and Birmingham Veterans Administration,Birming-ham,AL;University of Utah Medical Center,Salt Lake City,UT;andImClone Systems,Inc,Somerville,NJ.Submitted December12,2000;accepted March29,2001.Supported by grant no.5U01CA743392from the National Institutesof Health,Bethesda,MD.Address reprint requests to Francisco Robert,MD,University ofAlabama at Birmingham,Comprehensive Cancer Center,WallaceTumor Institute,Rm230,1824Sixth Ave South,Birmingham,AL35294-3300;email:pacorobertuab@.©2001by American Society of Clinical Oncology.0732-183X/01/1913-32343234Journal of Clinical Oncology,Vol19,No13(July1),2001:pp3234-3243Inhibition of the EGFR-induced signal transduction path-ways,either by higher than physiologic concentrations of epidermal growth factor or by monoclonal antibodies (mAbs)directed at the EGFR,has been shown to inhibit the growth of EGFR-expressing human cancer cells.21-23One such antibody is cetuximab (C225;ImClone Systems,Inc,Somerville,NJ),a mouse-human chimeric anti-EGFR mAb that binds with high affinity to the receptor,blocks ligand-induced activation of receptor tyrosine kinase,and induces dimerization and downregulation of the EGFR,which prevents further receptor binding and activation by the ligands.24-28In addition,cetuximab has been shown to inhibit the proliferation of a variety of cultured human tumor cell lines that overexpress EGFR and to enhance the antitumor activity of several chemotherapeutic agents in xenograft models.27,28-30Furthermore,we and others have shown that cetuximab enhanced the radioresponse of EGFR-expressing A431tumor cells in vitro and in tumor xenografts.31,32Given the correlation of EGFR expression with poor prognosis and the fact that preclinical studies identified cetuximab as a radiosensitizer,a phase I study was under-taken to assess the interaction of cetuximab and RT in patients with locally advanced,unresectable SCCHN.The purposes of this study were to establish a safety profile of cetuximab administered over a range of dose levels during RT and to determine the dose-dependent pharmacokinetics and human immune response to the antibody.PATIENTS AND METHODSThis single-center,phase I,open-label study evaluated different dose levels of cetuximab with concomitant RT in patients with locally advanced SCCHN.Five treatment groups (Table 1)with at least three assessable patients were considered for this study to determine the recommended phase II/III dose.Patients received eight to nine weekly infusions of cetuximab.The initial infusion was a loading dose of either 100,200,400,or 500mg/m 2administered over 60to 120minutes.Subsequent infusions of cetuximab consisted of 100-,200-,or 250-mg/m 2maintenance doses administered over 60minutes.Single daily fractions or twice-daily hyperfractionated RT was started on day 8(week 2)of the treatment course and continued for approximately 7weeks.The protocol was approved by the institutional review board,and all patients gave written informed consent before they were entered onto the study.Patient EligibilityPatients enrolled onto this study were at least 18years old and had a histologically confirmed diagnosis of SCCHN.The inclusion criteria were as follows:all sites of the head and neck except the nasopharynx,stage III or IV 33disease or recurrent disease that was not resectable for curative intent,no evidence of metastatic disease,and no history of prior RT or chemotherapy.In addition,patients had a Karnofsky performance status of at least 60%and preserved hematologic param-eters (absolute neutrophil count Ն1,500/L,platelet count Ն100,000/L,and hemoglobin level Ն9gm/dL),liver function (alkaline phosphatase Ͻ2.6times the normal limit,AST level Ͻ2.6times the normal limit,and total bilirubin Ͻ1.5times the normal limit),and normal renal function (creatinine Ͻ 1.5times the normal limit).Exclusion criteria were pregnancy or lactation,prior murine mAb or cetuximab therapy,significant comorbid conditions,or investigational therapy for diseases within 1month of study entry.Representative tumor tissue (paraffin tumor blocks)for EGFR assessment was obtained before the start of the study,but a positive result was not required as a prestudy parameter because of the high reported expression levels in SCCHN.17,18The presence of the EGFR was determined in a two-step immunostaining process,which involved,first,the binding of a murine anti-EGFR antibody (M225)to the receptor and,second,the detection and visualization of bound antibody by application of an enzyme chromogenic reagent.Tumors were considered to overexpress EGFR if positive cytoplasmic rimming was observed in 10%or more of the cells.All patients were evaluated initially by a multidisciplinary team that consisted of radiation oncologists,otolaryngologists,and medical oncologists.The stage of the tumor was determined on the basis of a physical examination,chest x-ray,and computed tomography or magnetic resonance imaging of the head and neck.A routine blood chemical analysis,complete blood count,and urinalysis were per-formed within 2weeks before enrollment.Dental evaluation was performed in each patient,and at least 10days were allowed for healing gingivae after extraction.DefinitionsDose-limiting toxicity (DLT)was defined as grade 3or higher toxicity as determined by the Cancer and Leukemia Group B expanded common toxicity criteria and the Radiation Therapy Oncology GroupTable 1.Study DesignTreatment Group No.of PatientsRTCetuximab Loading Dose (mg/m 2)Cetuximab Loading Infusion Time (min)Cetuximab Maintenance Dose(mg/m 2)Cetuximab Maintenance Infusion Time (min)13qd 10060100q 1wk ϫ76024*qd 20060200q 1wk ϫ76033qd 400120200q 1wk ϫ76043qd 500120250q 1wk ϫ76053bid 400120250q 1wk ϫ760Abbreviations:qd,single daily fraction,bid,twice-daily fractions;q 1wk,once a week.*One patient was replaced because of a grade 4allergic reaction during the initial infusion of cetuximab.3235CETUXIMAB PLUS RT IN HEAD-NECK CANCER(RTOG)acute radiation morbidity scoring criteria.Excluded from thedefinition of DLT were allergic reactions,asthenia,grade3mucositis, and grade3skin toxicity(within and outside of the RTfields).The definition of grade3skin toxicity outside of the RTfield was expanded to include confluence,pain,and erosion of the skin.Grade4skin toxicity was defined as exfoliative or ulcerating generalized dermatitis. Any patients who experienced a grade4allergic reaction were removed from the study and replaced in the same treatment group.The maximum-tolerated dose was defined as the highest dose level at which zero of three or one offive patients experienced a DLT.The recommended phase II/III dose was defined as the optimal cetuximab dose level based on pharmacologic parameters and adverse events. Investigational AgentCetuximab(C225)was provided by ImClone Systems as an inject-able solution in either10-mL or50-mL vials that contained2mg/mL of the antibody.Before infusion,cetuximab wasfiltered with a 0.22-m protein-sparingfilter.Treatment PlanPatients were enrolled sequentially ontofive treatment groups that comprised at least three assessable patients in each group,with all patients at the preceding dose level having received at least two doses of cetuximab(Table1).Dose escalation proceeded in the absence of a study drug–related DLT.If,at any dose level,one of the three patients experienced a DLT,two additional patients were to be enrolled at that dose level.Patients received eight to nine weekly cetuximab infusions with an initial loading dose on day1that ranged from100to500mg/m2 administered intravenously over60or120minutes(Table1).Subse-quent infusions of cetuximab consisted of100-,200-,and250-mg/m2 maintenance doses administered over60minutes.Patients received a test dose of cetuximab(20mg)over10minutes before the initial loading dose.They received the remainder of their infusion after completion of the observation period(30minutes).Patients were premedicated with diphenhydramine(50mg intravenously)and an H2 blocker before the test dose.All treatments were given in the outpatient setting.Vital-sign measurements were obtained before administration of cetuximab,midway through the infusion,and every15minutes during the1-hour observation period after administration of the antibody therapy.The weekly doses of cetuximab were scheduled for Mondays and were administered before RT.An additional weekly infusion of cetuximab(ninth dose)was given to patients who required RT breaks.If a patient experienced a grade1or2allergic reaction,premedita-tion with50mg of diphenhydramine and an H2receptor antagonist was administered before each treatment with cetuximab.The duration of the remaining and subsequent infusions was increased,but it did not exceed4hours.Concurrent treatment with oral diphenhydramine and a topical antibiotic was considered for skin toxicity grades1through3. In addition,cetuximab dose reduction and/or dose delays were required for grade3skin toxicity.In the event of a grade4skin toxicity or grade 4allergic reaction,the patient was removed from the study.RT began on day8(week2).Patients in four initial treatment groups received once-daily RT that consisted of2.0Gy per fraction,five fractions per week,for a total dose of70Gy in7weeks.After administration of50Gy,boostfields to the primary tumor and gross nodal disease with margin were given with photons or electrons in the 4-to20-MeV range.The entire neck and supraclavicular regions were irradiated to a dose of at least44Gy.Patients in the last treatment group received RT bid that consisted of1.2Gy per fraction,10fractions per week,for a total of76.8Gy in7weeks.After administration of45.6 Gy,boostfields to the primary tumor and gross nodal disease with margin were given with photons or electrons in the4-to20-MeV range. The entire neck and supraclavicular regions were irradiated to a dose of at least45.6Gy.Treatment breaks because of confluent mucositis (gradeՆ3)were allowed,but they were restricted to5days. Surgical treatment was used only after the completion of therapy. Neck dissection was permitted for any patient with residual cervical adenopathy or as a planned treatment for any nodal disease with an initial diameter of3cm or more.Pharmacokinetics and Whole-Body Retention DataSerum samples for analysis of circulating cetuximab were obtained during each treatment at the following time intervals:before the infusion of cetuximab and at1,24,48,72,and96hours after infusion with doses1,4,and8.Samples were collected before infusion and1 hour after infusion with doses2,3,5,6,and7.Serum concentrations of cetuximab were determined using a Bio-sensor(Pharmacia,Uppsala,Sweden)biomolecular interaction analysis core instrument,which measures changes in surface plasmon reso-nance.In this method,a serum sample that contains the antibody is flowed over a dextran-coated foldfilm to which EGFR has been conjugated.The binding of cetuximab to the immobilized EGFR produces a change in the angle of light reflected from the goldfilm,and from this relationship,a standard curve can be created to express the concentration of cetuximab in the serum sample.In addition,whole-body probe counts were performed after radiola-beled antibody infusion in patients in treatment groups1through4 only.For each dose,approximately1mg of cetuximab was radiola-beled with10mCi of iodine-131(131I)and was administered intrave-nously over2to3minutes after the infusion of thefirst(loading dose) and last maintenance dose of unlabeled cetuximab.Radiolabeling was performed under aseptic conditions using standard iodogen methodol-ogy.Quality control of the radiolabeled product was monitored by immunoreactivity,high-performance liquid chromatography analy-sis,limulus amebocyte lysate assay,and sterility testing.To block uptake of131I by the thyroid,patients received a saturated solution of potassium iodide,beginning48hours before the administration of 131I-cetuximab and continuing for14days.Serial total-body sodium iodide probe counts were measured to determine whole-body retention data from each patient during thefirst andfinal131I-cetuximab infusions.The residence time(area under the curve of a percentage of the injected dose)was calculated using a trapezoidal integration method.The biologic half-life(T1/2)for131I-cetuximab also was derived from a monoexponential regressionfit of whole-body count data.Human Antichimeric Antibody ResponsePatients were monitored to determine whether the administration of cetuximab resulted in the production of human antichimeric antibodies (HACAs).Sera obtained before thefirst infusion and throughout the subsequent treatment period were analyzed with a double-antigen radiometric assay specific for cetuximab.34,35The results are expressed as nanograms per milliliter of bound antibody.A positive response is greater than10ng/mL antibody bound and greater than two times the preinfusion levels.3236ROBERT ET ALCriteria for Toxicity and ResponseSystemic and local adverse events were graded in accordance with the Cancer and Leukemia Group B expanded common toxicity criteria and the RTOG morbidity scoring criteria.Safety was assessed by physical examination and laboratory evaluations(complete blood count,chemical profile,and urinalysis)for the duration of the treatment and follow-up.The initial tumor response assessment was performed4to6weeks after treatment was completed.Tumor response was determined by physical examination and imaging studies(computed tomography or magnetic resonance imaging).Extended follow-up was performed at approximately3-month intervals.A complete response was defined as resolution of all evidence of measurable and assessable disease.A partial response was defined as a50%or greater reduction in the sum of the products of the longest perpendicular diameters of measurable lesions,with no new lesion development.Progressive disease was defined as a greater than25%increase of the sum of the products of the maximum diameters of the measurable lesions or the appearance of a new lesion.In addition to analyzing tumor response,we analyzed several clinical events,including the time to progression,actuarial locoregional progression-free survival,and overall survival.These data were analyzed using the Kaplan-Meier method.36The Student’s t test was used for the comparison of the resident time and biologic T1/2 between thefirst and last radiolabeled antibody infusions.RESULTSPatient CharacteristicsA total of16patients were enrolled onto this study between April1997and August1998.Table2outlines thecharacteristics of the patients.The median age was55years (range,34to72years).Fifteen patients were treatment-naı¨ve,and one patient with recurrent disease had been treated previously with surgery.The majority of patients (81%)had stage IV disease.Nodal metastases were present in81%of the patients,and six patients had N2disease.Of a total of15patients tested for tumor EGFR expression, only two were negative.Of the16patients,15received the planned cetuximab infusions and RT,with minimal interruption or delay. One patient in the second treatment group developed a reversible grade4anaphylactic reaction approximately5 minutes into thefirst infusion,which required his re-moval from the study.ToxicityA total of125cetuximab infusions were administered, with a mean of eight infusions per patient.Treatment with cetuximab and RT was well tolerated.The adverse events encountered in the present study for all patients and by treatment group are listed in Tables3and4,respectively. The most common adverse experiences thought to be related to the antibody therapy were asthenia,fever,nausea, and skin toxicities.Skin toxicities included acneiform-follicular rashes(mainly on the scalp,face,and truck)and maculopapular eruptions.The onset of these cutaneous manifestations usually occurred during thefirst3weeks of therapy,with complete resolution or stabilization with continued therapy.Only one patient(treatment group4) developed grade3skin toxicity related to cetuximab(out of the RTfield),which was characterized by symptomatic (pruritic)generalized maculopapular eruption after thefirst antibody infusion.The incidence of skin toxicity outside of the RTfields was not strictly dose-dependent;however, grade2and higher skin eruptions were observed only in patients treated with higher-dose regimens(treatment groups4and5).Four patients experienced allergic reactions during the first infusion(Table3).Two of these patients had a grade3 or higher reaction;one patient with reversible anaphylactic reaction(grade4)was removed from the study.Patients with allergic reactions lower than grade4received subse-quent infusions with premedication(diphenhydramine and H2-receptor antagonists),and the time of infusions was increased.No further allergic manifestations were observed in these patients after these treatment alterations.Most of the acute grade2and higher adverse events observed during treatment were associated with standardTable2.Patient CharacteristicsCharacteristicNo.of Patients(Nϭ16) Age,yearsMedian55 Range34-72 SexMale12 Female4 Performance status90%3 80%7 70%6 Primary siteOral cavity3 Oropharynx9 Larynx2 Hypopharynx2 AJCC stageIII3IV13 Tumor stageT23T36T47 Nodal stageN04N16N26 Abbreviation:AJCC,American Joint Committee on Cancer.3237CETUXIMAB PLUS RT IN HEAD-NECK CANCERaggressive irradiation,ie,xerostomia,mucositis,odynopha-gia,and local skin toxicity in the radiotherapyfields(Table 4).The incidence of confluent mucositis and local skin toxicity was virtually the same in all of the treatment groups.Long-term effects of treatment included mild to moderate xerostomia in the great majority of the patients and one case of soft tissue necrosis with exposure of bone. Pharmacokinetics and Whole-Body Retention DataThe cetuximab concentration-versus-time data during treatment for thefive treatment groups are shown in Fig1. Visual inspection of the individual concentration versus time curves indicates that circulating cetuximab peak and trough levels increased progressively in patients treated with loading doses of100to500mg/m2and maintenance weekly doses of100to250mg/m2.The mean serum peak levels in thefirst four treatment groups were358,656, 1,291,and1,478nmol/L.Mean serum trough levels in the same treatment groups were39,202,504,and772nmol/L.It is obvious that the interpatient variability with thesefixed regimens is high,especially at higher doses of cetuximab. The mean Km(the concentration of the antibody at which its elimination is half of its maximum)for this group of patients was482nmol/L.The inadequacy of thefirst two dosing regimens is readily apparent.The concentrations of cetuximab generated with these two dosing regimens per-sistently fell below the population Km,which indicates that within this dose range,saturation of drug clearance was not achieved.A complete analysis of the pharmacokinetic data will be presented in a separate report.The sodium iodide probe count data from thefirst and last infusion of cetuximab for thefirst four treatments groups is shown in Fig2.The mean value for the residence time in the first infusion was85.3hours,as compared with83.7hours for the last infusion(Pϭ.69;t test).The mean biologic T1/2 was94.5hours with thefirst infusion and89.6hours with the last infusion.Individual patient data indicate a trend in the residence time and biologic T1/2with increased doses of cetuximab.HACA ResponseThe sera of14patients who completed therapy were analyzed for the presence of HACAs.None of these patients developed an immune response to cetuximab.Clinical ResponsesFifteen patients were assessable for response and locore-gional control.Thirteen patients achieved a complete re-Table3.Adverse Events During Therapy*EventGradeTotal No. 1234Allergic reaction†11114 Asthenia703010 Chills10001 Fever380011 Injection site reaction20002 Anorexia12003 Diarrhea21003 Xerostomia†2130015 Odynophagia†0411015 Nausea1440018 Vomiting41005 Mucositis†0411015 Skin toxicity outside RTfields‡1031014 Skin toxicity within RTfields§195015 Arthralgia13004 Myalgia21003 Paresthesia10001 Alopecia10001 Conjunctivitis10001 Anemia1200012 Leukopenia90009 Thrombocytopenia40004 Creatinine elevation10001 Alkaline phosphataseelevation60006 AST elevation80008*Number of adverse events during the administration of125cetuximab infusions plus RT.†Worst toxicity during therapy.‡Worst cetuximab-related skin toxicity during therapy.§Worst RT-induced skin toxicity.Table4.Adverse Events by Treatment GroupToxicity GradeNo.of Patients by Treatment Group12345 Mucositis100000211011322322400000 Odynophagia100000211110322223400000 Xerostomia100011233322300000400000 Skin,infield100001232121301211400000 Skin,outside of the RTfield1233112000123000104000003238ROBERT ET ALsponse,and two patients achieved a partial response (Table 5).One of the partial responders,a patient with a T3N2cMo tumor,underwent bilateral neck dissection after completion of RT for persistent disease and has remained free of disease for more than 22months.The median duration of response for all patients was 28months.The median follow-up of surviving patients was 36months (range,23to 42months).Six patients had relapsed,with a median time to progression of 8months (range,4.5to 31months).All recurrences were at the locoregionalsites.Five of these patients died from progressive disease,and the cause of death of one patient is unknown.The actuarial 1-and 2-year disease-free survival rates were 73%and 65%,respectively.The median survival of these pa-tients has not been reached.DISCUSSIONThe combination of cetuximab and RT was well tolerated in this group of patients with advanced SCCHN.The most common reported cetuximab-related adverse eventswereFig 1.Serum levels of cetux-imab during therapy shown on a semilogarithmic plot scale at dose levels of (A)100/100mg/m 2,(B)200/200mg/m 2,(C)400/200mg/m 2,(D)500/250mg/m 2,and (E)400/250mg/m 2loading and maintenance regimens.3239CETUXIMAB PLUS RT IN HEAD-NECK CANCERfever,asthenia,transaminase elevation,nausea,and skin toxicities.These adverse events were grades 1and 2in the majority of the patients and were not related to the dose level of the antibody therapy.Only one patient experienced grade 3skin toxicity (a follicular/maculopapular rash)outside of the RT fields.Otherwise,the majority of the grade 2and 3skin toxicities were within the RT fields and not necessarily related to cetuximab therapy.In addition to the skin toxicity,one patient experienced a grade 4anaphy-lactic reaction shortly after the initiation of the first cetux-imab infusion,which was completely reversible.The re-mainder of the grade 2and 3antibody-related local/systemic toxicities were of little consequence and required no cetuximab dose modification or RT delays.In recent studies of hyperfractionated RT alone or com-bined RT and chemotherapy,the most common grade 3adverse event was acute mucositis in 67%to 77%of patients.11,37,38In the first report of RTOG 9003,the incidence of grade 3or worse acute mucositis was 25%for standard fractionation and 43%for altered fractionation RT.9In that study,the incidence of grade 3or higher skin toxicity was 7%for standard fractionation and 9%for altered fractionation RT.In our study,the incidence of grade 3mucositis was 73%,and the incidence of grade 3in-field skin toxicity was 33%.An important relevant issue is whether cetuximab increases the local toxicity of RT.Our data suggest some enhanced toxicity,which implies a biologic interaction between the antibody and RT.How-ever,a definite conclusion cannot be reached at this time because of the small number of patients in this study.A critical issue in clinical studies with an anti-EGFR mAb is definition of the optimal biologic dose and schedule.The hypothesis that has driven the clinical development of cetuximab is that complete saturation of EGFR binding might require saturation of the mechanism(s)responsible for the antibody’s elimination from the body.Indeed,it is likely that a major route for cetuximab clearance involves the binding of the antibody to EGFR on hepatocytes,with subsequent internalization of the cetuximab-EGFR com-plex.On the basis of this hypothesis,the optimal biologic dose is the lowest dose of cetuximab required to continu-ously maintain zero-order antibody elimination.Analysis of the pharmacokinetic data of previous phase I studies has shown that cetuximab displayed nonlinear phar-macokinetics,with antibody doses in the range of 200to 400mg/m 2associated with complete saturation of systemic clearance.39On the basis of these findings,therecom-Fig 2.Whole-body retention data after 131I-cetuximab admin-istration during the first and last infusions at different dose levels (100/100mg/m 2,patient nos.1to 3;200/200mg/m 2,patient nos.4,6,and 7;400/200mg/m 2,patient nos.8to 10;and 500/250mg/m 2,patient nos.11to 13).(A)Residence time;(B)biologic T 1/2.Table 5.Clinical Response and DurationPatient No.Treatment GroupPrimary Site TNM/StageClinical ResponseDuration of Response (months)11Base of tongue T3N1M0/III CR 621Tonsil T3N0M0/III CR 39ϩ31TonsilT2N2BM0/IV CR 37ϩ42Base of tongue T3N2BM0/IV CR 33ϩ52Tonsil T3N0M0/III CR 2862LarynxT4N1M0/IV CR 373Retromolar trigone T4N2BM0/IV CR 28ϩ83Oral tongue T4N1M0/IV CR 393Hypopharynx T4N0M0/IV CR 5ϩ104TonsilT2N2BM0/IV CR 30ϩ114Floor of mouth T4N0M0/IV PR 3124TonsilT4N1M0/IV CR 25ϩ135Soft palate T2N2CM0/IV CR 11145Tonsil T3N1M0/IV CR 24ϩ155Larynx T3N2CM0/IV PR 21ϩAbbreviations:TNM,AJCC primary tumor,nodal status,and distant metastases staging system;CR,complete response;PR,partial response.3240ROBERT ET AL。
美国食物和药物治理局(FDA)已批准cetuximab作为医治晚期结肠癌的药物上市。
Cetuximab 是迄今第一个取得批准医治结肠癌的单克隆抗体药物。
瑞士已批准了MerckKgaA公司的抗癌药物Erbitux(cetuximab,西妥昔单抗)(也称C-225),用于对irinotecan (伊立替康)标准疗法不再响应的结肠癌患者。
这是Erbitux在全球的首次获批。
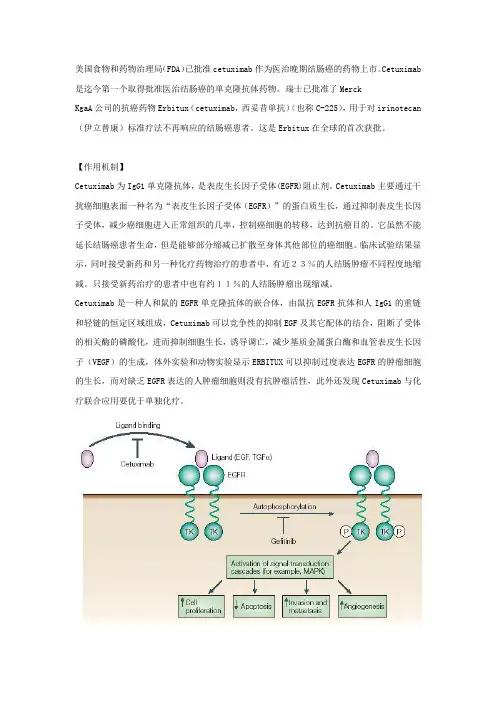
【作用机制】Cetuximab为IgG1单克隆抗体,是表皮生长因子受体(EGFR)阻止剂。
Cetuximab主要通过干扰癌细胞表面一种名为“表皮生长因子受体(EGFR)”的蛋白质生长,通过抑制表皮生长因子受体,减少癌细胞进入正常组织的几率,控制癌细胞的转移,达到抗癌目的。
它虽然不能延长结肠癌患者生命,但是能够部分缩减已扩散至身体其他部位的癌细胞。
临床试验结果显示,同时接受新药和另一种化疗药物治疗的患者中,有近23%的人结肠肿瘤不同程度地缩减。
只接受新药治疗的患者中也有约11%的人结肠肿瘤出现缩减。
Cetuximab是一种人和鼠的EGFR单克隆抗体的嵌合体,由鼠抗EGFR抗体和人IgG1的重链和轻链的恒定区域组成,Cetuximab可以竞争性的抑制EGF及其它配体的结合,阻断了受体的相关酶的磷酸化,进而抑制细胞生长,诱导调亡,减少基质金属蛋白酶和血管表皮生长因子(VEGF)的生成,体外实验和动物实验显示ERBITUX可以抑制过度表达EGFR的肿瘤细胞的生长,而对缺乏EGFR表达的人肿瘤细胞则没有抗肿瘤活性,此外还发现Cetuximab与化疗联合应用要优于单独化疗。
>【药代动力学】【适应症】晚期结肠癌肺癌【禁忌症】【用法与用量】intravenous use only联合OXALIPLATIN的方案:Cetuximab 400 mg/m2 loading one dose week #1 of cycle #1250 mg/m2 weekly starting on week #2andoxaliplatin 85 mg/m2 dl,LV 200 mg/m2, d1 & d2,5-FU 400 mg/m2 bolusthen 600 mg/m2 CI (22 hours)d1 & d2 (FOLFOX4)every 2 weeks【不良反应】最常见的非血液毒性包括痤疮状皮疹,感染及疲劳。
爱必妥(西妥昔单抗)——爱必妥2006-07-03 11:19:53 作者:来源:中国新药网浏览次数:2512 文字大小:【大】【中】【小】简介:爱必妥™(西妥昔单抗)是一种IgG1单克隆抗体,能与表皮生长因子受体(EGFR)特异性结合,阻断内源性配体介导的EGFR信号传导通路,从而抑制肿瘤的生长。
目前大量临床研究显示,爱必妥™用于转移性结直 ...关键字:爱必妥西妥昔单抗Erbitux cetuximab直肠癌爱必妥™(西妥昔单抗)是一种IgG1单克隆抗体,能与表皮生长因子受体(EGFR)特异性结合,阻断内源性配体介导的EGFR信号传导通路,从而抑制肿瘤的生长。
目前大量临床研究显示,爱必妥™用于转移性结直肠癌以及头颈部鳞状细胞癌等多种实体肿瘤的治疗取得了良好的疗效。
自2003年12月在瑞士上市以来,爱必妥™已在全球50余个国家注册并上市。
2005年12月,中国SFDA批准爱必妥™联合伊立替康用于治疗经含伊立替康方案化疗失败且表达表皮生长因子受体的转移性结直肠癌。
2006年7月,爱必妥™在中国成功上市。
爱必妥™以带橡皮塞和铝封的无色玻璃瓶包装,每瓶含有50ml注射液,每毫升注射液含2mg西妥昔单抗有效成分。
本品为静脉输注使用。
爱必妥™为处方药,须在专业医师的指导下使用。
爱必妥(西妥昔单抗)——大肠癌生物靶向治疗新药★第一个获准上市的靶向单克隆抗体,治疗转移性结直肠癌。
★靶向的生物导弹,精确打击肿瘤细胞而很少伤及正常细胞。
★阻断肿瘤细胞信号传导,抑制癌细胞增殖,透导肿瘤细胞凋亡。
★爱必妥与FOLFOX-4联合应用达到最高缓解率(81%)。
”★耐受性好,不良反应轻。
药品名称:爱必妥注射 (Erbitux)通用名:西妥昔单抗英文名: cetuximab制造商: 德国默克勃林格殷格翰性状本品除活性成分外,还含有以下成分:磷酸二氢钠20 mg、磷酸氢二钠66 mg、氯化钠424 mg、注射用水加至50 mL。
利妥昔单抗注射液Rituximab【成份】本品主要活性成分为利妥昔单抗辅料:枸橼酸钠、聚山梨酯80、氯化钠、盐酸(37%)和注射用水【性状】无色或淡黄色澄明液体【适应症】复发或耐药的滤泡性中央型淋巴瘤(国际工作分类B、C和D亚型的B细胞非霍奇金淋巴瘤)的治疗。
先前未经治疗的CD20阳性III-IV期滤泡性非霍奇金淋巴瘤,患者应与化疗联合使用。
CD20阳性弥漫大B细胞性非霍奇金淋巴瘤(DLBCL)应与标准CHOP化疗(环磷酰胺、阿霉素、长春新碱、强的松)8个周期联合治疗。
【规格】100mg/10ml/瓶【用法用量】用法和使用说明:在无菌条件下抽取所需剂量的利妥昔单抗,置于无菌无致热原的含0.9%生理盐水或5%葡萄糖溶液的输液袋中,稀释到利妥昔单抗的浓度为1mg/ml。
轻柔的颠倒注射袋使溶液混合并避免产生泡沫。
由于本品不含抗微生物的防腐剂或抑菌制剂,必须检查无菌技术。
静脉使用前应观察注射液有无微粒或变色。
利妥昔单抗稀释后通过独立的不与其他药物混用的输液管静脉滴注,适用于不卧床患者的治疗。
利妥昔单抗的治疗应在具有完备复苏设备的病区内进行,并在有经验的肿瘤医师或血液科医师的直接监督下进行。
对出现呼吸系统症状或低血压的患者至少监护24小时。
每名患者均应被严密监护,监测是否发生细胞因子释放综合征(见【注意事项】)。
对出现严重反应的患者,特别是有严重呼吸困难,支气管痉挛和低氧血症的患者应立即停止滴注。
还应该评估患者是否出现肿瘤溶解综合征,例如可以进行适当的实验室检查。
预先存在肺功能不全或肿瘤肺浸润的患者必须进行胸部X线检查。
所有的症状消失和实验室检查恢复正常后才能继续滴注,此时滴注速度不能超过原滴注速度的一半。
如再次发生相同的严重不良反应,应考虑停药。
利妥昔单抗绝不能未稀释就静脉滴注,制备好的注射液也不能用于静脉推注。
滤泡性非霍奇金淋巴瘤:每次滴注利妥昔单抗前应预先使用解热镇痛药(例如扑热息痛)和抗组胺药(例如苯海拉明)。
爱必妥(西妥昔单抗注射液)说明书【爱必妥药品名称】商品名称:爱必妥通用名称:西妥昔单抗注射液英文名称:CetuximabSolutionforInfusion【爱必妥成份】爱必妥主要成份为西妥昔单抗。
【爱必妥性状】爱必妥为注射用溶液,无色,可能含有与产品相关的白色可见的无定形颗粒。
【爱必妥药理作用】爱必妥可与表达于正常细胞和多种癌细胞表面的EGF受体特异性结合,并竞争性阻断EGF 和其他配体,如α转化生长因子(TGF-α)的结合。
爱必妥是针对EGF受体的IgG1单克隆抗体,两者特异性结合后,通过对与EGF受体结合的酪氨酸激酶(TK)的抑制作用,阻断细胞内信号转导途径,从而抑制癌细胞的增殖,诱导癌细胞的凋亡,减少基质金属蛋白酶和血管内皮生长因子的产生。
爱必妥单剂治疗或与化疗、放疗联合治疗时的药动学呈非线性特征。
当剂量从20mg/m2增加到400mg/m2时,药时曲线下面积(AUC)的增加程度超过剂量的增长倍数。
当剂量从20mg/m2增加到200mg/m2时,清除率(Cl)从0.08L/(m2.h)下降至0.02L/(m2.h),当剂量>200mg/m2时,Cl不变。
表观分布容积(Vd)与剂量无关,接近2~3L/m2。
爱必妥400mg/m2滴注2小时后,平均血药浓度(Cmax)为184μg/ml(92~327μg/ml),平均消除半衰期(t1/2)为97小时(41~213小时)。
按250mg/m2滴注1小时后,平均Cmax 为140μg/ml(120~170μg/ml)。
在推荐剂量下(初始400mg/m2,以后一周250mg/m2)到第3周时,爱必妥达到稳态血药浓度,峰值、谷值波动范围分别为168~235和41~85μg/ml。
平均t1/2为114小时(75~188小时)。
【爱必妥临床评价】一项多中心随机Ⅱ期临床对照研究评价了爱必妥治疗转移性结直肠癌的疗效。
329例EGF受体过度表达的受试者中,206例为男性,平均59岁(26~84岁),58为结肠癌患者,40为直肠癌患者,其中63%的患者用奥沙利铂(oxaliplatin)治疗无效。

英文商品名:ERBITUX原产地英文药品名:Cetuximab份子结构名:西妥昔单抗包装规格及销售价:100毫克/50毫升/瓶( 附加过滤器)中文剂型:注射剂100毫克/20毫升/瓶( 免过滤器)计价单位:瓶生产厂家:德国默克里昂制药公司适应症:结肠直肠癌扩大适应症:鼻咽癌, 肺癌西妥昔单抗本品单剂治疗或与化疗、放疗联合治疗时的药动学呈非线性特的增加程度超过剂量的增长倍数。
当剂量从20mg/m2增加到200mg/m2时,清除率(Cl)从0.08L/(m2.h)下降至0.02L/(m2.h),接近2~3L/m2。
本品400mg/m2滴注2小时后,平均最大血药浓度(Cmax)为184μg/ml(92~327μg/ml),平均消除半衰期(t1/2)为97小时(41~213小时)。
按250mg/m2滴注1小时后,平均Cmax为140μg/ml (120~170μg/ml)。
在推荐剂量下(初始400mg/m2,以后一周范围分别为168~235和41~85μg/ml。
平均t1/2为114小时(75~188小时)。
一项多中心随机Ⅱ期临床对照研究评价了本品治疗转移性结直肠癌的疗效,329例EGF受体过度表达的受试者中,206例为男性,平均59岁(26~84岁),58%为结肠癌患者,40%为直肠癌患者,其中63%的患者用奥沙利铂(oxaliplatin)治疗无效。
研究中患者随机分成2组,本品和伊立替康联用组218例,本品单用组111例。
本品的初始剂量为一周400mg,随后一周250mg,治疗终点为疾病进展或出现不能耐受的不良反应。
伊立替康的使用剂量为每3周350mg/m2,每2周180mg/m2,或第6周4次125mg/m2。
结果显示,联合治疗组和本品单用组有效率分别为22.9%和10.8%。
疗效平均持续时间,联合治疗组和本品单用组分别为5.7和4.2个月;与本品单用组相比,联合治疗组患者明显延缓了疾病的进展。
另一项多中心单组开放性临床研究,评价了138例EGF受体过度表达的转移性结直肠癌患者接受本品与伊立替康联用的疗效。
RItuximab 说明书• 1 适应证和用途1.1 非霍奇金淋巴瘤(NHL)Rituxan?(利妥昔单抗rituximab)适用于治疗患者有:1)复发或难治,低度或滤泡性,CD20-阳性,B-细胞NHL用作单药。
2)既往未治疗过滤泡性,CD20-阳性,B-细胞NHL与CVP(环磷酰胺、长春新碱、强的松)化疗联用。
3)非进展(包括稳定疾病),低度,CD20-阳性,B-细胞NHL,作为单药,一线CVP 化疗后。
4)既往未治疗过弥漫性大B-细胞, CD20-阳性NHL与CHOP或其它基于蒽环类化疗方案联用1.2 慢性淋巴细胞白血病(CLL)Rituxan?(利妥昔单抗)适用于与氟达拉滨和环磷酰胺(FC)联用,为既往未治疗过和既往治疗过CD20-阳性CLL患者的治疗(01/2010修订)。
1.3 类风湿样关节炎(RA)Rituxan?(利妥昔单抗)与甲氨蝶呤联用适用于治疗成年中度-至严重活动性类风湿样关节炎对一种或更多TNF拮抗剂治疗反应有不充分的患者(09/2009修订)。
1.4 使用的限制有严重,活动性感染患者建议不要使用Rituxan(01/2010修订)。
2 剂量和给药方法2.1 给药不要给予静脉推注或大丸注射。
每次输注前预先给药[见剂量和给药方法(2.6)]。
只给予静脉(IV)输注[见剂量和给药方法(2.6)]。
1)首次输注:开始输注速率50 mg/hr。
缺乏输注毒性,增加输注速率每30分钟增量50 mg/hr至最大400 mg/hr。
2)随后输注:开始输注速率100 mg/hr。
缺乏输注毒性,增加速率30分钟间隔增量100 mg/hr至最大400 mg/hr。
3)对输注反应中断输注或减慢输注率[见黑框警告,警告和注意事项(5.1)]。
在以前速率一半继续输注at one-half改善症状。
2.2 对非霍奇金淋巴瘤(NHL)的推荐剂量推荐剂量是375 mg/m2作为IV输注按下列日程:1)复发或难治,低度或滤泡性,CD20-阳性,B-细胞NHL给予每周1次共4或8剂。
西妥昔单抗说明书【药品名称】通用名称:西妥昔单抗商品名称:_____【成份】本品主要成份为西妥昔单抗。
【性状】本品为无色或淡黄色澄明液体。
【适应症】本品用于治疗转移性结直肠癌,以及头颈部鳞状细胞癌。
【规格】_____【用法用量】1、转移性结直肠癌在开始治疗前,应进行 KRAS 基因状态检测。
KRAS 野生型的患者适用西妥昔单抗治疗。
推荐初始剂量为 400mg/m²,静脉输注,输注时间约120 分钟。
此后每周250mg/m²,静脉输注,输注时间约60 分钟。
2、头颈部鳞状细胞癌初始剂量为 400mg/m²,静脉输注,输注时间约 120 分钟。
此后每周 250mg/m²,静脉输注,输注时间约 60 分钟。
【不良反应】使用西妥昔单抗可能会出现一系列不良反应。
常见的不良反应包括皮肤反应,如痤疮样皮疹、皮肤干燥、瘙痒、甲沟炎等;还可能出现输液反应,如发热、寒战、呼吸困难等。
此外,可能会有胃肠道反应,如恶心、呕吐、腹泻等;以及血液学毒性,如白细胞减少、贫血等。
皮肤反应通常在治疗开始后的第 1-2 周出现,多数为轻至中度。
对于皮肤反应,应注意保持皮肤清洁,避免阳光直射,并根据症状的严重程度使用相应的药物治疗。
输液反应可能在首次输注时发生,也可能在后续输注时出现。
在输注过程中应密切监测患者的生命体征,一旦出现输液反应,应立即停止输注,并给予相应的治疗。
如果出现严重的不良反应,如严重的输液反应、呼吸困难、心脏功能异常等,应立即停止使用西妥昔单抗,并进行积极的治疗。
【禁忌】对本品活性成份或其它任何成份过敏者禁用。
【注意事项】1、在使用西妥昔单抗之前,应告知医生患者的过敏史、疾病史和正在使用的其他药物。
2、治疗期间应定期进行血液学检查,包括血常规、肝肾功能等,以监测药物的不良反应。
3、患者在接受西妥昔单抗治疗期间应避免接种活疫苗。
4、对于有眼部疾病史的患者,应密切监测眼部症状。
抗 Cetuximab【适应证】与伊立替康联用治疗表达EGFR、经伊立替康治疗失败的转移性结直肠癌。
【注意事项】(1)如出现轻中度超敏反应,应减慢本品的滴注速率,一旦发生严重超敏反应,应立即并永久停用,并进行紧急处理。
(2)给药时发生呼吸困难可能与本品相关,老年患者、体能状况低下或伴有肺部疾病的患者可能存在更高的与呼吸困难相关的风险。
(3)发生严重(3级)皮肤反应,须中断治疗。
(4)体能状况低下或伴有心肺疾病的患者慎用。
(5)注意监测血清中镁的水平,需要时应补充镁。
(6)用药过程中及用药结束后1小时内,需密切监测患者的状况,并须配备复苏设备。
(7)首次滴注本品之前,患者须接受抗组胺药物治疗,建议在一次使用本品前都进行这种治疗。
(8)伊立替康须在本品滴注结束1小时后开始使用。
(9)本品须在有经验的医师指导下使用。
建议检测EGFR。
【禁忌证】已知对本品有严重超敏反应(3级或4级)者,妊娠及哺乳期妇女。
【不良反应】急性气道阻塞,支气管痉挛,喘鸣,嘶哑,说话困难,风疹,低血压,发热,寒战,恶心,皮疹,结膜炎,呼吸困难,粉刺样皮疹,指甲病,甲床炎,低血镁症。
【用法和用量】静脉滴注:初始剂量一次400mg/m2,滴注120分钟,之后一周给药1次250 mg/m2,滴注60分钟,最大滴注速率不得超过5ml/min。
治疗持续至病情进类化疗+5-氟尿嘧啶(CT)方案获准用作头颈部复发性局部区域性或转移性鳞状细胞癌的一线治疗。
此前,爱必妥已获准联合放疗(一线治疗)或作为单药治疗(行标准治疗后)用于某些类型的结肠癌及头颈部非转移性癌症的治疗。
“西妥昔单抗联合顺铂或卡铂及5-氟尿嘧啶用作头颈部复发性和(或)转移性鳞状细胞癌的一线治疗”(EXTREME)试验的结果支持批准爱必妥的这项新适应症。
EXTREME试验显示,西妥昔单抗+CT联合治疗的疗效优于单用CT。
爱必妥获准用于治疗头颈部局部区域性或转移性鳞状细胞癌11月7日,美国FDA和百时美施贵宝(联合礼来)宣布,爱必妥(Erbitux,西妥昔单抗)联合铂2011年11月7日,美国食品药品管理局(FDA)和百时美施贵宝(联合礼来)宣布爱必妥(Erbitux®,西妥昔单抗)联合铂类化疗+5-氟尿嘧啶(CT)方案获准用作头颈部复发性局部区域性或转移性鳞状细胞癌的一线治疗方案。