英文大病例写作示例
- 格式:doc
- 大小:63.50 KB
- 文档页数:5
医学病例报告英语作文Title: Medical Case Report: Management of Chronic Hypertension in a Middle-aged Female Patient。
Abstract:This case report discusses the presentation, diagnosis, and management of chronic hypertension in a middle-aged female patient. The patient, Mrs. X, presented with a history of hypertension and was experiencing persistent elevated blood pressure despite lifestyle modifications and medication adherence. Through a comprehensive assessment, including medical history, physical examination, and diagnostic tests, the patient was diagnosed with chronic hypertension. The management approach involved pharmacological intervention, lifestyle modifications, and regular monitoring. This case highlights the importance of tailored treatment strategies and multidisciplinary care in managing chronic hypertension effectively.Introduction:Chronic hypertension, characterized by persistently elevated blood pressure levels, is a significant public health concern globally. It predisposes individuals to various cardiovascular complications, including stroke, heart failure, and renal dysfunction. This case report focuses on the management of chronic hypertension in a middle-aged female patient, emphasizing the importance of individualized treatment plans to achieve optimal blood pressure control and reduce the risk of associated complications.Case Presentation:Mrs. X, a 55-year-old female, presented to the clinic with a chief complaint of persistently elevated blood pressure readings despite adherence to antihypertensive medication. She reported a history of hypertension for the past ten years and a family history of cardiovascular diseases. On physical examination, her blood pressure was consistently elevated, averaging around 160/100 mmHgdespite being on a combination therapy of angiotensin-converting enzyme (ACE) inhibitor and diuretic.Diagnostic Assessment:Given the patient's history and physical examination findings, further diagnostic workup was pursued to assess the extent of target organ damage and potential secondary causes of hypertension. Laboratory investigations,including renal function tests, lipid profile, and electrolyte levels, were within normal limits. An electrocardiogram (ECG) revealed left ventricular hypertrophy, indicative of long-standing hypertension. Additionally, a renal ultrasound ruled out renal artery stenosis as a secondary cause of hypertension.Diagnosis:Based on the clinical presentation, diagnostic findings, and exclusion of secondary causes, Mrs. X was diagnosedwith chronic primary hypertension. The diagnosis was supported by her longstanding history of hypertension,family history of cardiovascular diseases, and evidence of target organ damage on ECG.Management:The management approach for Mrs. X's chronic hypertension involved a combination of pharmacological therapy and lifestyle modifications. Considering her persistent elevation in blood pressure despite the current medication regimen, the treatment plan was adjusted. A calcium channel blocker (amlodipine) was added to her existing therapy to achieve better blood pressure control. Furthermore, Mrs. X was counseled on dietary modifications, including a low-sodium diet and increased consumption of fruits and vegetables. She was also encouraged to engage in regular physical activity and weight management.Follow-up and Monitoring:Mrs. X was scheduled for regular follow-up visits to monitor her blood pressure response to the adjusted treatment regimen and assess for any adverse effects ofmedication. Additionally, she was advised to monitor her blood pressure at home using a digital blood pressure monitor and maintain a record for review during follow-up visits. Laboratory investigations, including renal function tests and electrolyte levels, were scheduled periodically to monitor for potential medication-related complications.Outcome:With the adjusted treatment regimen and adherence to lifestyle modifications, Mrs. X demonstrated significant improvement in blood pressure control. Subsequent follow-up visits showed a gradual reduction in her blood pressure readings, with values consistently below 140/90 mmHg. Repeat ECG performed six months later showed regression of left ventricular hypertrophy, indicating improvement in cardiac function. Mrs. X reported improved quality of life and compliance with the treatment plan.Discussion:This case illustrates the challenges encountered inmanaging chronic hypertension, particularly in patientswith resistant hypertension despite medication adherence.It underscores the importance of a comprehensive diagnostic approach to identify underlying causes and assess target organ damage. Individualized treatment strategies,including pharmacological therapy tailored to the patient's needs and preferences, are essential in achieving optimal blood pressure control. Furthermore, lifestylemodifications play a crucial role in hypertension management and should be integrated into the treatment plan. Multidisciplinary collaboration involving physicians, nurses, pharmacists, and allied healthcare professionals is vital in providing holistic care to patients with chronic hypertension.Conclusion:Effective management of chronic hypertension requires a multidimensional approach involving pharmacological therapy, lifestyle modifications, and regular monitoring. This case report highlights the successful management of chronic hypertension in a middle-aged female patient throughtailored treatment strategies and collaborative care. By addressing individual patient needs and optimizing blood pressure control, healthcare providers can mitigate the risk of cardiovascular complications and improve patient outcomes in individuals with chronic hypertension.。
Good morning. Today, I am honored to present a case report on a patient who recently visited our medical facility. This case highlights a complex medical condition that required a multidisciplinary approach for diagnosis and treatment. I will discuss the patient's history, physical examination findings, laboratory and imaging results, and the subsequent management plan.Patient Information:- Name: John Smith- Age: 45 years- Gender: Male- Date of admission: March 15, 2023- Date of discharge: March 30, 2023Medical History:John Smith presented to our emergency department with a chief complaint of progressive shortness of breath and fatigue over the past two weeks. He reported a history of hypertension and type 2 diabetes mellitus,which were well-controlled on medication. He denied any recent illnesses, fever, cough, or weight loss.Physical Examination:On admission, Mr. Smith was found to have a blood pressure of 160/95 mmHg, heart rate of 110 bpm, respiratory rate of 22 breaths per minute, and tempera ture of 37.2°C. His general appearance was anxious, and he had significant edema in both lower extremities. Cardiovascular examination revealed a grade II/VI systolic ejection murmur at the left sternal border, and pulmonary examination was notable for bilateral wheezing and rales.Laboratory and Imaging Results:- Complete blood count (CBC): Mild anemia with hemoglobin of 10.2 g/dL, white blood cell count of 12,000/µL, and platelet count of 150,000/µL.- Electrolytes, renal function tests, and liver function tests were within normal limits.- Serologic tests for HIV, hepatitis B, and hepatitis C were negative.- Chest X-ray: Bilateral pulmonary edema and cardiomegaly.- Echocardiogram: Severe left ventricular dysfunction with an ejection fraction of 25%.- CT scan of the chest: Pulmonary embolism involving the left main pulmonary artery.Diagnosis:Based on the clinical presentation, laboratory findings, and imaging results, the patient was diagnosed with acute pulmonary embolism (PE) with secondary pulmonary hypertension and left ventricular dysfunction.Management Plan:- Anticoagulation therapy with heparin and apixaban was initiated to prevent further thromboembolic events.- Mechanical ventilation was required due to severe respiratory distress.- Inotropic support was provided to manage hypotension and improve cardiac output.- Treatment for secondary pulmonary hypertension included diuretics, nitrates, and inhaled bronchodilators.- Antibiotics were prescribed for a suspected lower respiratory tract infection.- The patient was also started on a low-sodium diet and received education on fluid management.Outcome:After a week of intensive care, Mr. Smith's clinical status improved significantly. His respiratory distress resolved, and he was able to beweaned off mechanical ventilation. His blood pressure stabilized, and the inotropic support was discontinued. By the time of discharge, his ejection fraction had improved to 30%, and he was discharged on apixaban and hydrochlorothiazide to manage his hypertension and diabetes.Conclusion:This case report illustrates the importance of early diagnosis and treatment of pulmonary embolism, which can be a life-threatening condition. The multidisciplinary approach, including emergency medicine, cardiology, pulmonology, and critical care, was crucial in managing this complex case. Mr. Smith's recovery demonstrates the potential for successful outcomes with appropriate medical intervention.Thank you for your attention, and I would be happy to answer any questions you may have.。

病例报告英文范文医护英语English:The patient, a 45-year-old male, presented to the emergency department complaining of severe chest pain radiating to his left arm and shortness of breath. On examination, his blood pressure was 180/110 mmHg, heart rate 110 bpm, and oxygen saturation 92% on room air. ECG revealed ST-segment elevation in leads II, III, and aVF, consistent with an inferior myocardial infarction. He was promptly started on aspirin, clopidogrel, and sublingual nitroglycerin. Intravenous morphine was administered for pain relief. He was transferred to the coronary care unit for further management, where he underwent emergent coronary angiography showing complete occlusion of the right coronary artery. Percutaneous coronary intervention (PCI) was performed, resulting in successful revascularization. The patient's symptoms improved, and he was discharged home with instructions for cardiac rehabilitation and secondary prevention measures, including dual antiplatelet therapy, statin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy.Translated content:患者为45岁男性,就诊于急诊科,主诉严重胸痛放射至左臂,呼吸急促。
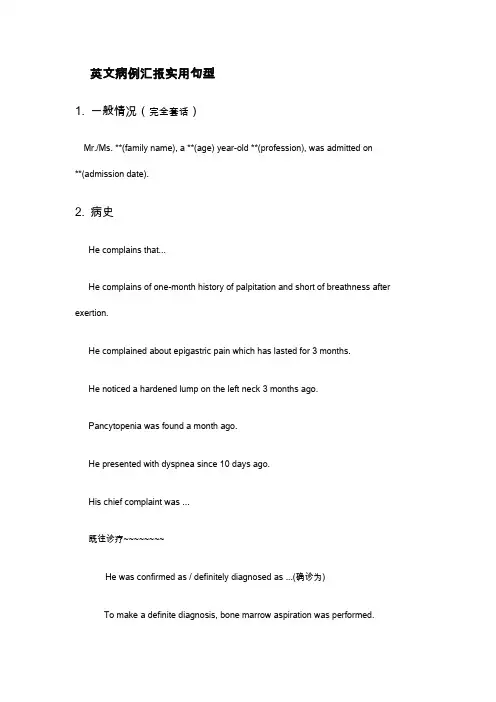
英文病例汇报实用句型1. 一般情况(完全套话)Mr./Ms. **(family name), a **(age) year-old **(profession), was admitted on**(admission date).2. 病史He complains that...He complains of one-month history of palpitation and short of breathness after exertion.He complained about epigastric pain which has lasted for 3 months.He noticed a hardened lump on the left neck 3 months ago.Pancytopenia was found a month ago.He presented with dyspnea since 10 days ago.His chief complaint was ...既往诊疗~~~~~~~~He was confirmed as / definitely diagnosed as ...(确诊为)To make a definite diagnosis, bone marrow aspiration was performed.He was suspected as...(疑似)The discomfort tended to worsening, which urged him to seek for medical care.He has been given 3 cycles of DA regimen for chemotherapy and complete remission was achieved only after the first cycle.He was given the thyroidectomy of the left lobe in local hospital.He was treated with antibiotics (details unknown), which didn't take effect as expected.The general condition is good at present.He was pain free now and hemodynamically stable.3. 查体Nothing noteworthy was found in the physical examination.There was nothing remarkable in the physical examination except for…The physical examination was otherwise normal except that…(上点小菜~~~血液科常见体征)皮肤粘膜generalized pallor,scattered petechiae,oral mucosal hematoma淋巴结enlarged lymph nodes头部yellow eyes (yellow-stained sclera)胸部tenderness in sternum,coarse breath sound, cardiac murmur, arrhythmia腹部enlargement of liver,splenomegaly4.辅助检查The laboratory findings suggested/indicated/demonstrated/showed that…Bone marrow film was performed, which confirmed the diagnosis of ALL.The results of blood routine showed that WBC count was 4,000 /cm3, while NEU count 2,500/cm3, hemoglobin 100 g/L, PLT count 100,000 /cm3.(/cm3 is pronounced as per cubic millimeter)Chest CT scan supported the diagnosis of NHL.Welcome To Download !!!欢迎您的下载,资料仅供参考!。
英文病例写作范文阅读带翻译病例写作是医生日常的工作,英文的病例该如何写呢,接下来店铺为大家整理英文病例写作范文,希望对你有帮助哦!英文病例写作范文篇一Name: Joe Bloggs (姓名:乔。
伯劳格斯)Date: 1st January 2000(日期:2000年1月1日)Time: 0720(时间:7时20分)Place: A&E(地点:事故与急诊登记处)Age: 47 years(年龄:47岁)Sex: male(性别:男)Occupation: HGV(heavy goods vehicle ) driver(职业:大型货运卡车司机)PC(presenting complaint)(主诉)4-hour crushing retrosternal chest pain(胸骨后压榨性疼痛4小时)HPC(history of presenting complaint)(现病史)Onset: 4 hours of “crushing tight” retrosternal chest pain, radiating to neck and both arms, gradual onset over 5-10 minutes.(起病特征:胸骨后压榨性疼痛4小时,向颈与双臂放射,5-10分钟内渐起病)Duration: persistent since onset(间期:发病起持续至今)Severe: “worst pain ever had”(严重性:“从未痛得如此厉害过)Relieving/exacerbating factors缓解与恶化因素GTN(glyceryl trinitrate) provided no relief although normally relieves pain in minutes, no other relieving/exacerbating factors.(硝酸甘油平时能在数分钟内缓解疼痛,但本次无效,无其它缓解和恶化因素。
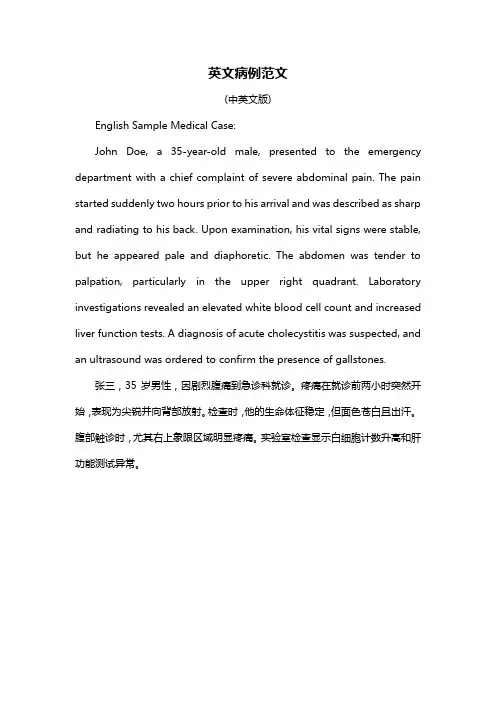
英文病例范文(中英文版)English Sample Medical Case:John Doe, a 35-year-old male, presented to the emergency department with a chief complaint of severe abdominal pain. The pain started suddenly two hours prior to his arrival and was described as sharp and radiating to his back. Upon examination, his vital signs were stable, but he appeared pale and diaphoretic. The abdomen was tender to palpation, particularly in the upper right quadrant. Laboratory investigations revealed an elevated white blood cell count and increased liver function tests. A diagnosis of acute cholecystitis was suspected, and an ultrasound was ordered to confirm the presence of gallstones.张三,35岁男性,因剧烈腹痛到急诊科就诊。
疼痛在就诊前两小时突然开始,表现为尖锐并向背部放射。
检查时,他的生命体征稳定,但面色苍白且出汗。
腹部触诊时,尤其右上象限区域明显疼痛。
实验室检查显示白细胞计数升高和肝功能测试异常。
As an English teacher,I would like to provide you with a detailed example of a patient report written in English.Here is a sample paragraph that you can use as a reference:Upon my visit to the clinic today,I was greeted by the receptionist who promptly attended to my registration.After a brief wait,I was called into the consultation room where I met with Dr.Smith.I began by explaining my symptoms,which included a persistent cough,mild fever,and general fatigue over the past week.Dr.Smith attentively listened to my description and proceeded to conduct a thorough physical examination.He used a stethoscope to listen to my chest and checked my blood pressure,which was slightly elevated at140/90mmHg.Following the examination,Dr.Smith suggested that I undergo a chest Xray and a complete blood count CBC to rule out any potential respiratory infections or other underlying conditions.He also recommended a course of antibiotics and advised me to stay hydrated and get plenty of rest.I was provided with a prescription for the medication and was scheduled for a followup appointment in a weeks time to monitor my progress and discuss the results of the tests.Throughout the consultation,Dr.Smith was professional,empathetic,and informative, ensuring that I understood the possible causes of my symptoms and the importance of adhering to the prescribed treatment plan.I left the clinic feeling reassured and confident in the care I received.This paragraph provides a comprehensive account of a patients visit to a clinic,including the symptoms experienced,the examination process,the tests recommended,and the treatment plan provided by the doctor.It also highlights the patients feelings and the doctors approach to the consultation.。
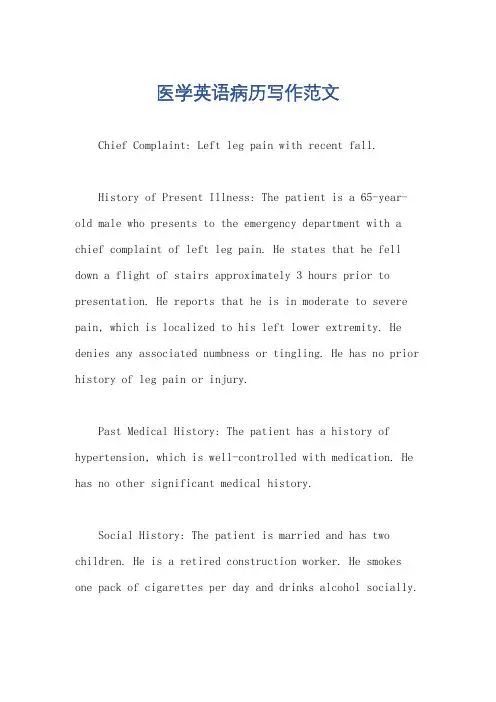
医学英语病历写作范文Chief Complaint: Left leg pain with recent fall.History of Present Illness: The patient is a 65-year-old male who presents to the emergency department with a chief complaint of left leg pain. He states that he fell down a flight of stairs approximately 3 hours prior to presentation. He reports that he is in moderate to severe pain, which is localized to his left lower extremity. He denies any associated numbness or tingling. He has no prior history of leg pain or injury.Past Medical History: The patient has a history of hypertension, which is well-controlled with medication. He has no other significant medical history.Social History: The patient is married and has two children. He is a retired construction worker. He smokes one pack of cigarettes per day and drinks alcohol socially.Family History: The patient's father has a history of coronary artery disease. His mother has a history of Alzheimer's disease.Physical Examination:Vital signs: Blood pressure 140/80 mmHg, heart rate 80 bpm, respiratory rate 18 breaths per minute, temperature 98.6°F (37°C).General: The patient is in moderate distress due to pain. He is alert and oriented to person, place, and time.HEENT: Normocephalic and atraumatic. Pupils are equal and reactive to light. Extraocular movements are intact. No conjunctival injection or discharge. Tympanic membranes are intact and mobile.Neck: Supple with full range of motion. No masses or tenderness.Chest: Auscultation reveals clear breath soundsbilaterally. No wheezes, rales, or rhonchi.Cardiovascular: Regular rate and rhythm. No murmurs, rubs, or gallops.Abdomen: Soft and non-tender. No masses or organomegaly.Extremities: Left lower extremity: Examination reveals swelling and tenderness of the left knee. There is a palpable step-off deformity of the lateral aspect of theleft knee. Active and passive range of motion is limiteddue to pain. Distal pulses are palpable and capillaryrefill is brisk. Sensation is intact. Right lower extremity: Examination reveals no abnormalities.Neurological Examination:Mental status: Alert and oriented to person, place,and time. No deficits in attention, memory, or language.Cranial nerves: No deficits.Motor: Strength is 5/5 in both upper and lower extremities. No atrophy or fasciculations.Sensory: Sensation is intact to light touch, pinprick, and temperature in all four extremities.Diagnostic Studies:X-ray of the left knee: The X-ray shows a displaced lateral tibial plateau fracture.Assessment:Left knee pain.Displaced lateral tibial plateau fracture.Plan:The patient will be admitted to the hospital for further evaluation and treatment.He will be placed in a knee immobilizer and will be started on pain medication.Orthopedic surgery will be consulted for further management.。
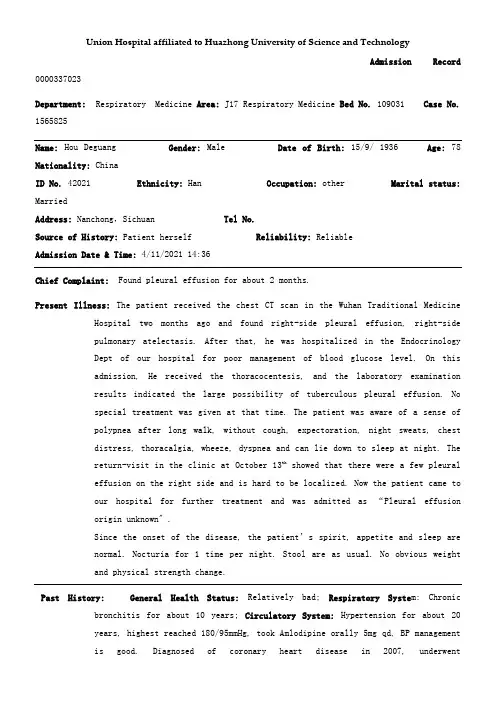
Union Hospital affiliated to Huazhong University of Science and TechnologyAdmission Record 0000337023Department: Respiratory Medicine Area: J17 Respiratory Medicine Bed No. 109031 Case No. 1565825Name: Hou Deguang Gender: Male Date of Birth:15/9/ 1936 Age:78 Nationality: ChinaID No. 42021 Ethnicity: Han Occupation: other Marital status: MarriedAddress: Nanchong,Sichuan Tel No.Source of History: Patient herself Reliability: ReliableAdmission Date & Time: 4/11/2021 14:36Chief Complaint: Found pleural effusion for about 2 months.Present Illness: The patient received the chest CT scan in the Wuhan Traditional Medicine Hospital two months ago and found right-side pleural effusion, right-sidepulmonary atelectasis. After that, he was hospitalized in the EndocrinologyDept of our hospital for poor management of blood glucose level. On thisadmission, He received the thoracocentesis, and the laboratory examinationresults indicated the large possibility of tuberculous pleural effusion. Nospecial treatment was given at that time. The patient was aware of a sense ofpolypnea after long walk, without cough, expectoration, night sweats, chestdistress, thoracalgia, wheeze, dyspnea and can lie down to sleep at night. Thereturn-visit in the clinic at October 13th showed that there were a few pleuraleffusion on the right side and is hard to be localized. Now the patient came toour hospital for further treatment and was admitted as “Pleural effusionorigin unknown〞.Since the onset of the disease, the patient’s sp irit, appetite and sleep arenormal. Nocturia for 1 time per night. Stool are as usual. No obvious weightand physical strength change.Past History: General Health Status: Relatively bad; Respiratory Syste m: Chronic bronchitis for about 10 years; Circulatory System: Hypertension for about 20years, highest reached 180/95mmHg, took Amlodipine orally 5mg qd, BP managementis good. Diagnosed of coronary heart disease in 2007, underwentintracoronary stent implantation in 2021, 3 stents were implanted; DigestiveSystems: None; Urinary System: Benign prostatic hyperplasia for about 5 years,Diabetic nephropathy for 3 years; Hematologic System: Thrombocytopenia for 2years; Endocrine System: None. Nervous System: Lacunar infarction in 2021;Motor System: None; Infection History: No infection of hepatitis and TB. Others:None special; Preventive Inoculation: In accordance with the stateplan;Operation History:underwent intracoronary stent implantation in 2021, 3stents was implantated; Blood Transfusion History:None; Traumatic History:None; Allergic History: None;Personal History: Habitual Residence: Hubei; Residential Environment: No exposure history to toxic substances and infected water; Travelling History: None; Smoking History:Smoking for about 40 years, 3 cigarettes per day. Quit smoking in 2021;Drinking History: Drinking for 40 years, 150g-350g per day, Quit drinking in2021;Marital History: Married,Menstrual History: MaleFamily History:Father is deceased, mother is deceased. No other infective and hereditary diseases.Physical ExaminationVital Signs: T:℃. P:86 bpm, regular. R: 20min, regular. BP: 132/74 mmHg. Height: 164cm.Weight: 64kg. Expression: Normal. Development: Well. Nutritional status: Fairly.Consciousness: Conscious. Spirit: Well. Gait: Normal. Position: Active.Coordination with Examination: Cooperative.Skin and Lymph Nodes:No jaundice. Some scattered scratch in hands and abdomen, No subcutaneous bleeding, edema, nodules or unusual pigmentation. Liverpalm(-). Spider angioma(-). No swelling of general superficial lymphnodes.HEENT(Head, Eye, Ear, Nose, Throat): Normal skull. No baldness, no scars. Eyes: No ptosis.Conjuctiva normal. The pupils are round, symmetric and responsive to lightand accommodation is normal. Ears: Externally normal. Canals clear. Drumsnormal. Noses: No abnormalities noted. Month and Throat: lips red, tongue red,no swelling of tonsils.Neck: Motion free. Thyroid is not enlarged. No abnormal pulsations. Trachea in middle. Carotid: Pulse is normal. Hepatojugular reflux sign(-). Vascular bruit: None.Chest and Lung:Normal contour. Breast normal. Inspection: respiratory movement symmetric and regular. Palpation: Normal and symmetric. No pleural friction fremitus. Percussion: both sides resonance. Auscultation: right-side breath sounds weaken, left-side is normal. No moist or dry rales. No pleural friction rubs.Heart:No protrusion of precordium. Normal apical impulse. No thrill. No enlarged cardiac dullness border. Heart rate: 88bpm, rhythm normal. No abnormal and extra cardiac sounds or cardiac murmurs. No peripheral vascular signs.Abdomen:Flat abdomen. No gastric or intestinal pattern. No visible peristalsis. Normal bowel sound. No rigidity. No mass palpable. No tenderness and rebound tenderness. Liver and spleen are not palpable. Kidneys are not palpable. No percussion tenderness over kidney regions. No shifting dullness.Rectum: Normal anus and perineum.Genitourinary System: Normal.Neural System: Normal.Extremities: No joint disease. Muscle strength normal. Pathological reflex (-).Specialty Examination: Right-side breath sounds weaken, left side normal. No moist or dry rales, No swelling of general superficial lymph nodes. No edema inneither lower extremities.Accessory Examination:Discharge record of Endocrinology Dept. of our hospital at September 2021; Clinic examination at October 13th: a few pleural effusion on theright side and is hard to be localized.History summary: 1. Hou Deguang, male, 78 yr.2. Admitted for 〞Found plaural effusion for about 2 months〞.3. T:℃. P:86 bpm, regular. R: 20min, regular. BP: 132/74 mmHg.Expression: Normal. Spirit clear. Cardiac sounds normal, HR: 72 bpm, rhythmnormal, No abnormal and extra cardiac sounds or cardiac murmurs. Right-side breathsounds weaken, left side normal. No moist or dry rales, no pleural friction rubs.Flat abdomen. No rigidity.4. Special examination:Trachea in middle. Contour symmetric.Respiratory movement regular. Right-side breath sounds weaken, left side normal. Nomoist or dry rales, no pleural friction rubs.5. Accessory Examination: Discharge record of Endocrinology Dept of ourhospital at September 2021; Clinic examination at October 13th: a few pleuraleffusion on the right side and is hard to be localized.6. Past history: Respiratory Syste m: Chronic bronchitis for about 10years; Circulatory System: Hypertension for about 20 years, highest reached180/95mmHg, took Amlodipine orally 5mg qd, BP management is good. Diagnosed ofcoronary heart disease in 2007, underwent intracoronary stent implantation in2021, 3 stents was implantated; Digestive Systems: None; Urinary System: Benignprostatic hyperplasia for about 5 years, Diabetic nephropathy for 3 years;Hematologic System: Thrombocytopenia for 2 years; Endocrine System: None.Nervous System: Lacunar infarction in 2021; Motor System: None;InfectionHistory: No infection of hepatitis and TB. Others: None special; PreventiveInoculation: In accordance with the stateplan; Operation History:underwentintracoronary stent implantation in 2021, 3 stents was implantated; BloodTransfusion History: None; Traumatic History: None; Allergic History: None; Impression: 1. Right-side pleural effusion origin unknown: TB? Tumor?2. II diabetes mellitus, Diabetic nephropathy3. Hypertension III, high risk4. Coronary heart disease, post-intracoronary stent implantation5. Lacunar infarction6. Thrombocytopenia7. Benign prostatic hyperplasiaRecorder: Cheng LongDate & Time: 4/11/2021 16:14Checker: Xu JuanjuanDate & Time: 5/11/2021 10:22。

关于三个病人病历的报告英语作文英文回答:Case 1:A 65-year-old male with a history of hypertension and hyperlipidemia presents with a chief complaint of progressive shortness of breath and fatigue. He has been experiencing exertional dyspnea for the past 6 months, which has gradually worsened over the past few weeks. He now has difficulty walking up a flight of stairs without stopping to rest. He also complains of fatigue and decreased exercise tolerance.Physical examination reveals an obese male with a blood pressure of 150/90 mmHg, a heart rate of 90 bpm, and a respiratory rate of 20 breaths per minute. Auscultation of the chest reveals bibasilar crackles.Chest X-ray shows cardiomegaly and interstitial edema.Echocardiogram demonstrates a left ventricular ejection fraction of 40% and mild mitral regurgitation.Diagnosis:Heart failure with preserved ejection fraction (HFpEF)。
英语病例报告范文I am writing to provide a case report of a patient who presented with symptoms of chest pain and shortness of breath. The patient, a 55-year-old man, arrived at the emergency department complaining of sudden onset chest pain that radiated to his left arm. 本文将介绍一位55岁男性患者的病例报告,该患者出现胸痛和呼吸困难症状。
这位患者突然出现胸痛,疼痛向左臂放射。
Upon arrival, the patient was noted to be diaphoretic and tachypneic, with a blood pressure of 150/90 mmHg and a heart rate of 110 beats per minute. Further assessment revealed he had a history of hypertension and smoking. High-sensitivity troponin levels were elevated, indicating a possible myocardial infarction. 到达医院后,患者被发现出现出汗和呼吸急促的症状,血压为150/90mmHg,心率为每分钟110次。
进一步评估显示他有高血压和吸烟史。
高敏肌钙蛋白水平升高,提示可能发生心肌梗死。
The patient was immediately started on oxygen therapy and given aspirin and nitroglycerin for symptom relief. An ECG showed ST-segment elevations in leads II, III, and aVF, suggestive of an inferiormyocardial infarction. He was promptly taken to the catheterization lab for emergent angiography. 患者立即开始吸氧疗法,并服用阿司匹林和硝化甘油缓解症状。
CASEMedical Number: 794615 General informationName: Liu **Age: Sixty-fiveSex: MaleRace:HanNationality:ChinaMarital status: MarriedNative place:TianjinAddress: Hedong District, Tianjin, Hebei , Admiralty Street Ying Fuk Lane 33-207Occupation: RetirementDate of admission:August 14th 2014 Date of record: August 14th, 2014 Complainer of history: the patient herselfReliability: ReliableTel:136……Chief complaint: Intermittent chest tightness , Pharyngeal tighteness more than a month , become serious for 8 daysPresent illness:more than a month before admission ,the Patient felt intermittent chest tightness and pharyngeal tightness with back discomfort after exertion , which continued 15 minutes and relieved itself ,and he did not receive treatment . At the same time , he had no sweat , no dizziness , no headache, no amaurosis ,no syncope, no chest pain , no cough , no sputum or hemoptysis, no dyspnea, no abdominal pain , no nausea, no vomiting or fever . In eight days before admission , the Patient felt chest tightness and pharyngeal tightness with back discomfort without obvious incentive for 10 minutes.He felt more serious than before. So he came to our hospital , his Cardiac enzymes were normal and diagnosised with " the unstable angina " , then he received anticoagulant , expanding crown , lipid-lowering therapy. He was checked by coronary angiography on August 13, 2014 ,and it showed: multivessel coronary artery lesions. He came to the Cardiovascular Surgery for the sake of surgical revascularization .Since onset, his appetite is good, both his spiritedness and sleep are normal. His defecation and urination are normal, too.His weight is notsignificantly changePast historyHe has history of hypertension for 10 years, the highest 180 / 110mmHg, taking the compound antihypertensive tablets and nifedipine, the blood pressure control at 130 / 80mmHg .He denays history of operation and severe infectious disease . He is allergic to sulfamide.Review of systems:Respiratory system: no history of Sore throat, chronic cough, sputum, hemoptysis , wheezing , dyspnea , chest painCirculatory system: no history of Palpitation, hemoptysis , syncope, edema of lower limbs, precordial painAlimentary system:no history of anorexia , sour regurgitation , belching ,nausea, vomittingGenitourinary system:No history of lumbago, frequent micturition, urgent micturition, urodynia , dysuria, hematuria, nocturia, polyuria, oliguria, facial edemaHematopoietic system:No history of fatigue, dizziness, blurred vision, gingival bleeding, subcutaneous hemorrhage ,ostealgia ,epistaxis Metabolic and endocrine system:No history of excessive appetite, anorexia, sweats, cold intolerance, polydipsia, tremor hands, change of character, obvious obesity, emaciation, hirsutism hair, losing pigmentation, chang of sexual functionMusculoskeletal system: No floating arthralgia,no arthraliga ,no swelling of joints, no deformiteies of jionts ,no myalgia ,no atrophy of muscle. Neural system:No history of headache ,dizziness, vertigo, syncope, degeneration of memory, visual disturbance, insomnia, disturbance of consciousness, tremor, spasm, paralysis, paresthesiaPersonal historyHe was born in Tianjin, and almost always lived inTianjin. He has history of smoking for 40 years , average40 pieces per day .And no history of drinkingObstetrical history:get married at 24 years old,have a daughter ,she is healthyFamily history: Deny family genetic historyPhysical examinationVital signs:T 36.9℃, P 68/min, R 18/min, BP 164/84mmHg.General condition:He is well developed and moderately nourished. Passive position. The skin was not stained yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Lymphnodes: Superficial lymph nodes were not enlarged or pressing pain. HeadCranium: Hair was black and well distributed. No deformities. No scars. No masses. No tenderness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external auditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose:No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nares flaring. No tenderness in nasal sinuses.Eye:Bilateral eyelids were not swelling. No ptosis. No entropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or depressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect pupillary reactions to light were existent.Mouth: Oral mucous membrane was smooth, and of no ulcer or erosion. Tongue was in midline. Pharynx was not congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was notenlarged. Trachea was in midline.ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was neither narrowed nor widened. No tenderness. Thorax: Symmetric bilaterally. No deformities.Breast:Symmetric bilaterally. Neither nipples nor skin were retracted. Elasticity was fine.Lungs:Inspection: Respiratory movement was bilaterally symmetric with the frequency of 18/min. Intercostal space was not wide or narrow Palpation: Thoracic expansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus.percussion: Resonance was heard. No abnormal breath sound was heard. Lower borders was in the sixth intercostal space on Collarbone midline, the eighth intercostal space on midaxillary line ,the tenth intercostal space on scapular line.Space range of mobility:right 7.9cm,left 7.8cm Ausculation: breath regular, No wheezes. No rales.Heart:Inspection: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum impulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse.Palpation : apex impulse was normal .no thrill, no percardial friction rubs Percussion: relative cardiac outline was not enlargeRight(cm) intercostal space left(cm)2.0 二 2.03.0 三4.03.6 四 5.6五8.2The distance between clavicle middle line and the midline was 9.0cm Ausculation: No pericardial friction sound. Heart sounds were strong and no splitting. Rate 68/min. Cardiac rhythm was regular. No pathological murmurs.No Pericardial friction rubsPeripheral vessals: normal pistal shot of big arteries,no Duroziez’s sign ,no water hammer pulse, no capillary pulsation, no paradoxical pulse, no pulsus alternansAbdomen:Inspection: Flat and symmetry. No bulge or depression .No gastral pattern and intestinal pattern. No venous distention of abdomen . No purple striae . No surgical scars or herniaPalpation: soft. There was not tenderness and rebound tenderness on abdomen or renal region. Liver was not reached. Spleen was not enlarged. No masses. Gallbladder can’t be touched,Murphy was negative. percussion: borders of liver dull was existence.Upper borders of liver on right midclavicular line the fifth intercostal space,which was 9.8cm far from the down edge of the liver. Shifting dullness negative. ausculation : Borhorygmus 5/min, which was not increased or decreased. No vascular murmurs.No gurgling or peritoneal fricativesGenitalia ,rectum and Anus: normalLaboratory findingscoronary angiography showed: multivessel coronary artery lesions (2014-8-13)Abstract1.Patient was a retirement worker ,male, 65 years old.2.Intermittent chest tightness , Pharyngeal tighteness more than a month , become serious for 8 days3.He has history of hypertension for 10 years, the highest 180 / 110mmHg, taking the compound antihypertensive tablets and nifedipine, the blood pressure control at 130 / 80mmHg .He has history of smoking for 40 years , average40 pieces per day .And no history of drinking.4.Coronary angiography shows: multivessel coronary artery lesions.Impression: 1、Coronary heart diseaseUnstable anginaMultivessel coronary artery lesionsCardiac function in secondary(NYHA)2、Hypertension in level 3 (Very high risk)Signature:。
妇科英文病历模板篇一:妇产科英文模板CASEMedical Number: 756943General informationName: Yue Jun-rongAge: Forty- two years old Sex: FemaleRace: Han Occupation: UnemploymentNationality: ChinaMarital status: Married Address : Xiaochang county of Xiaogan cityin Hubei. Tel: 4835963Date of admission: Feb.27th, 2003Date of record: 3pm, Feb.27th, 2003 Complainer of history: the patient herselfReliability: ReliableChief complaint: The patient was found “myoma ofuterus” over two years ago and menometrorrhagia for 5 months.Present illness: In 1999, the patient was found “myoma ofuterus” in a physical examination. But she had nothing1uncomfortable and her catamenia was normal. She used some Chinese traditional medicine. About 5 months ago, she found the cycle of her catamenia was shorten from 30 days to 20 days and the period lasted from 2 days to 4 days. She felt no pain and the quantity was normal. She was accepted in our hospital and her diagnosis was “subserous myoma of uterus”.Since onset, her appetite was good, and both her spiritedness and physical energy are normal. Defecation and urination are normal, too.Past historyOperative history: Never undergoing any operation.Infectious history: No history of severe infectious disease.Allergic history: She was not allergic to penicillin or sulfamide.Respiratory system: No history of respiratory disease.Circulatory system: No history of precordial pain.Alimentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease. Hematopoietic system: No history of anemia andmucocutaneous bleeding. Endocrine system: Noacromegaly. No excessive sweats.2Kinetic system: No history of confinement of limbs.Neural system: No history of headache or dizziness.Personal historyShe was born in Hubei on July 16th, 1956 and almost always lived in Wuhan. She graduated from senior high school. Her living conditions were good. No bad personal habits and customs.Menstrual history: The first time when she was 14. Lasting 2 days every times and its cycle is about 30 days.Obstetrical history: Pregnacy 3 times, once nature production, induced abortion twice.Contraceptive history: Not clear.Family history: His parents are both alive.Physical examinationT 36.8?, P 80/min, R 20/min, BP 120/80mmHg. She is well developed and moderately nourished. Active position. The skin was not stained yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not enlarged.HeadCranium: Hair was black and well distributed. No deformities. No scars. No masses. No tenderness.3Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external auditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nares flaring. No tenderness in nasal sinuses.Eye: Bilateral eyelids were not swelling. No ptosis. No entropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or depressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect pupillary reactions to light were existent.Mouth: Oral mucous membrane was smooth, and of no ulcer or erosion. Tongue was in midline. Pharynx was not congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in midline.ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was neither narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities.4Breast: Symmetric bilaterally. Neither nipples nor skin were retracted. Elasticity was fine.Lungs: Respiratory movement was bilaterally symmetric with the frequency of 20/min. Thoracic expansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales.Heart: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum impulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardialfriction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 80/min. Cardiac rhythm was regular. Nopathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. There was not tenderness and rebound tenderness on abdomen or renal region. Liver was not reached. Spleen was not enlarged. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus 5/min. No vascular murmurs.Extremities: No articular swelling. Free movements of all5limbs.Neural system: Physiological reflexes were existent without any pathological ones. Genitourinary system: Not examed.Rectum: not exanedInvestigationBlood-Rt: Hb 127g/l RBC 3.93T/l WBC 3.9G/lUrine-Rt: SG 1.070 pH 6.0B-ultrasound: 1. subserous myoma of uterus2. position of loop is normalHepatic function: NormalPT & APTT: NormalProfessional ExaminationPudendum: Married typeVagina: unobstructed, secretion is excessive, white and ropy.Os of cervix: No bleeding, slight anabrosis.Body of uterus: Big like a fist of man, hard and its surface is smooth.Others: NormalHistory summary1. Patient was female, 45 years old2. The patient was found “myoma of uterus” over two6year ago and menometrorrhagia for 5 months..3. No special past history.4. Physical examination showed no abnormity in lung, heart and abdoman. Professional examination can been seen above.5. investigation information: see aboveImpression: subserous myoma of uterusSignature: He Lin (95-10033)来源:杨帆| 分享(7) | 浏览(49)篇二:妇产科英文病历Inpatient HistoryName: Yali ZhouSex: FemaleAge: 38year Ward: No.8 Bed: No.816 Marital status: Married Birthplace: ShanghaiNationality: Han Provider: Patient, reliable. Record date: 2005-12-13G & O History: GW: 30+5weeks, G2P0, LMP: 2005-5-10; EDC: 2006-2-17Chief Complaint: G2P0, GW: 30+5weeks. This patient presents hypertension for 3 months, and systemic edema for 2 weeks.7History of Present illness:The patient had regular menses previously. LMP: 2005-5-10; EDC:2006-2-17. Uric HcG test was positive after 40 days of amenorrhea. Fetal movements were felt in 4 months’ gestation. In 12+2weeks’ gestation, the patient’s blood pressure was found 160/90 mmHg when shecompleted her first ante-partum examination in Hospital of Women and Children’s Health in Huangpu District. Therewas no symptoms at that time, and she didn’t take anytreatment. Half a month ago, she presented edema on both the lower extremities, which expanded to the whole body gradually. She came to our hospital on Dec, 5th and took her sencond ante-partum examination. The bp was200/160mmHg, and uric protein(++) on dipstick test. She has occasional headaches, but no epigastric pain, no visual disturbances, no oliguria, no nausea or vomiting, no thoracic pain. She was admitted on 2005-12-6.After admission, she appears clear, with a good appetite, good sleeping, and normal urination and defecation.Past history: Patient denies history of hepatitis and tuberculosis. No history of allergies. Vaccinated regularly. Past medical history is uemarkable. Surgical history denied.8No history of severe trauma and transfusion.Review of systems:Respiratory system: No history of chronic cough or breathlessness. No hemoptysis or dyspnea.Cardiovascular system: No precordial pain. No palpation. No syncope. For details see present history.Gastroentestinal system: No history of chronic abdominal pain and diarrhea; No nausea or vomiting; No hematemesis and blood stool.Endocrinic system: No polydipsia or polyphasia or polyuria. No sudden change of character and intelligence.Hematologic system: No bruises or abnormal hemorrhage. No recurrent oral ulcer and gingival bleeding.Genitourinary system: No decreased libido; No vaginal dryness or vaginal bleeding; History of STD denied; No urinary frequency. No precipitant urination or dysuria. No hematuria or proteinuria.Neuropsychiatric system: No convulsion or anesthesia. No headaches. No abnormal orientation. No deterioration of memory or intelligence.Locomotor system: No arthralgia, no muscular atrophies or dystrophies.9Personal History:Born and grown up in Shanghai. Patient denied history of tobacco or alcohol use.Marital and Childbearing history: Married. 0-0-1-0; She had an abortion in 3 months’ gestation in Dec., 2004. Birthcontrol has been instructed.Family history: The patient’s Mother and a sister sufferedfrom hypertension. No family history of DM or stroke. No family history of nervous or mental diseases.Physical ExaminationT: 37? P: 89/minR: 20/minBP: 180/120mmHgGeneral appearance: Patient is a 38 years old female who appears pleasant, in no apperant distress, given her age, well developed andwell nourished. Oriented to person, place and time.Lymph nodes: Not enlarged.Skin: No jaundice or rashes. No cyanosis and bruises. No edema.Head: Skull and scalp normal. No tenderness. No loss of hair.Eyes: No edema in eyelids, no ptosis, no conjunctivalcongestion.Width of palpebral fissures is normal. No10jaundice. Pupil’s size and shape is normal. Corneal is clear. No exophthalmos.Ears: Auditory acuity is excellent. No ear purulent discharge.Nose: Shape is normal. No obstruction. No deviation of nasal septum.Mouth: No lips herpes. No cyanosis. No gums pyorrhea and bleeding. No tongue deviation. Tonsils not enlarged.Neck: Her neck is soft. Trachea is midline. No thyroid abnormality was found. Neck vein was not distended.Chest: Contour is normal. No sternum tenderness. The breasts are bilaterally symmetrical. No tenderness and mass.Lung:Inspection: Respiration regular. Degree of expansion is symmetry.Plapation: Tactile fremitus symmetrical.Percussion: extensive resonance to percussion.Ausculation: Clear to ausculation with no rubs noted.Heart:Inspection: No abnormal pulsation or retraction.Plapation: The apex beat can be felt in the 5th intercostal space 1 cm inside of the left mid-clavicular line.11Percussion: The border of cardiac is not enlarged.Ausculation: The heart sounds were of good quality and the rhythm was regular.Radial pulse is normal.Abdomen:Inspection: Universial abdominal bulge. Dilated veins observed.Palpation: Soft. Liver and spleen is not enlarged. Nontender. Murphy’s sign is negative. For details seeobstetric examination.Percussion: No shifting dullness. The upper border of the liver is in the 5th intercostal space.Ausculation: Bowl sound clear. 4/min.Spine and extremities: Severe edema in both lower extremities. No clubbed finger. No disorder of the movement of axial and appendicular bones.Reflex: Symmetrical, equal without pathological responses. Babinski sign and Kernig sign and hoffmann sign are all negative.Obstetric examinationPatient appears pleasant, given her age, well developed and12well nourished. No jaundice. No enlarged lymph nodes.Fetus: Abdominal girth: 93cm; height of fundus: 29cm; estimated fetal weight: 1600g; fetal position: LOA; point of fetal heart tone: ; fetal heart rate: 148/min; FM: active.Pelvis: 24-17-19-9 cm.Anorectal examination: fetal presentation: N/A; sincipital presentation: N/A; fetal membrane: not ruptured. Amniotic fluid: N/A;Flexion of knee: active.Laboratory and special examinationthDec. 6, Blood Rt: Hb: 121g/L; PLT 136×10e9Urine Rt: uric protein(++); occlude blood: (+++)Dec. 7th, Fetal Ultrasound: BPD: 78mm; HC: 259mm; AC: 238mm; FL:51mm; HL:49mm. fetal presentation: head; Position of placenta: right wall of uterus.Thickness of placenta: 23mm. Degree of placental maturity: ?; fetal heartbeat and fetal movement seen; amniotic fluid: 64mm. There is no hematocoelia or ascites. The lower edge of placenta is1323mm from thecervix.Umbilical A: P2: 0.87; R2: 0.59; S/D: 2.46.Fetal heart rate: 145/minDec. 8th, 24h uric protein: 7.5gDec.10th, serum potassium: 3.9mmol/LScr: 86umol/LALT: 25U/L ; AST: 30U/LFeatures of the case:1. Female, 38years old, G2P0, GW: 30+5weeks.2. This patient presents hypertension for 3 months, andsystemic edema for 2 weeks.3. PE: BP: 180/120mmHg. Obstetric exam: Fetus: Abdominal girth: 93cm; height offundus: 29cm; estimated fetal weight: 1600g; fetal position:LOA; point of fetal hearttone: ; fetal heart rate: 148/min; FM: active.Pelvis: 24-17-19-9 cm.Flexion of knee: active.4. Laboratory and special exam:Dec. 6th, Blood Rt: Hb: 121g/L; PLT 136×10e9Urine Rt: uric protein(++); occlude blood: (+++)14Dec. 7th, Fetal Ultrasound: BPD: 78mm; HC: 259mm; AC: 238mm; FL:51mm;Degree of placental maturity: ?; fetal heartbeat and fetalmovementseen; amniotic fluid: 64mm.Umbilical A: P2: 0.87; R2: 0.59; S/D: 2.46.Fetal heart rate: 145/minDec. 8th, 24h uric protein: 7.5gDec.10th, serum potassium: 3.9mmol/LScr: 86umol/LALT: 25U/L ; AST: 30U/LDiagnosis and differential diagnosis:Diagnosis: 1. Severe pre-eclampsia. This patient is a 38-year-old woman, who presents with hypertension and edema. Pre-eclampsia is hypertension associated with proteinuria and edema, occurring primarily in nulliparas after the 20th gestational week and most frequently near term. Other clinical findings of the patient include uric protein (++),etc. These lead to the diagnosis of pre-eclampsia, which feature the clinic status of the latter. The patient has (1) blood pressure 180/120mmHg(160/110mmHg);15(2)proteinuria(++) on dipstick testing and 7.5g (5g)in a 24-hour period. Conclusively, she can be classified as severe pre-eclampsia.Pre-eclampsia is a multisystemic syndrome, primary investigations reveal that she has occasional headaches, but no epigastric pain, no visual disturbances, no oliguria, no nausea or vomiting, no thoracic pain, indicating that there are no many complications at present. Further evaluations are indispensable, which requires more careful investigations.2. Chronic essential hy pertension. The patient’shypertension began from the 12w of gestation, which indicate thatshe has chronic hypertension. Besides, she has a family history of hypertension. After all, she doesn’tpresent severe complaints when her blood pressure were as high as 200/160mmHg. All these lead to the diagnosis of chronic hypertension. To confirm the diagnosis, the blood pressure after delivery should be evaluated.Differential diagnosis: 1. chronic essential hypertension associated with pregnancy. Essential hypertension associated with pregnancy can also cause a very high blood pressure. However, given the age,proteinuria and edema are possibly not complications of hypertension, indicating that she has16superimposed pre-eclampsia. Besides, the symptoms of proteinuria and edema are temporally associated with gestation.2. Chronic hypertension due to renal disease. This includes chronic hypertension due to interstitial nephritis, chronic glomerulonephritis, SLE, diabetic glomerulosclerosis, and so on. In these occasions, the patient would also possibly present hypertension, proteinuria and edema, but her proteinuria was found recently and she didn’t have any symptoms associated with renal diseases previously. In addition, her serum creatinine is in the normal scale (Scr: 86umol/L), which contradicts the hypothesis that she has a renal disease. So the diagnosis of chronic hypertension due to renal disease is not considered at present.Further investigations and treatments:1. Close observation and monitoring, plus quick evaluation: daily weighing; q4-6h monitoring of blood pressure; daily monitoring ofprotein in urine; Regular liver and kidney function testing; Ultrasound of the abdomen; Fetus heartbeat monitor; Conduct ophthalmoscopy examination to evaluat e the severity of the patient’s condition; Conduct PT,APTT, FDP, 3P test to evaluate the coagulant function.172. Rests: Lie in bed on left side.3. Magnesium sulfate administration with close observation offlexion of knee, respiratory rate and urine.4. Control hypertension with Labetalol or Nitroglycerin. The goal of bp control is diastolic pressure《110mmHg andMAP《140mmHg.5. Administer furosemide to control edema.6. Cautious evaluation of the maternal and fetal complications and take action correspondingly. Severe maternal complications include edema of the brain, pulmonary edema; DIC; HELLP syndrome; renal failure. Indicative symptoms include headache, epigastric pain, visual disturbances, oliguria, nausea and vomiting, thoracic pain, etc.7. Use corticosteroids to accelerate fetal lung maturity.8. Delivery. In an effort to reduce perinatal morbidity and mortality, delivery should be delayed. If the patient develops into the following conditions: 1.Blood pressure consistently higher than 100mmHg diastolic in a 24h period or confirmed higher than 110mmHg; 2. Rising serum creatinine; 3. Persistent severe headache; 4. epigastric pain; 4. abnormal liver function tests; 5: Thrombocytopnia; 6: HELLP18syndrome; 7: Eclampsia; 8: Pulmonary edema; 9: Abnormal antepartum fetal heart rate testing; 10: SGA fetus with failure to grow on serial ultrasound examinations.Clinic diagnosis: 1. Severe pre-eclampsia2. Chronic essential hypertension Signiture: /Jacky Luo 篇三:妇科英文病历CASEMedical Number: 756943General informationName: Yue Jun-rongAge: Forty- two years oldSex: FemaleRace: HanOccupation: UnemploymentNationality: ChinaMarital status: MarriedAddress: Xiaochang county of Xiaogan city in Hubei. Tel: 4835963 Date of admission: Feb.27th, 2003 Date of record: 3pm, Feb.27th, 2003 Complainer of history: the patient herself Reliability: Reliable Chief complaint: The patient was found “myoma ofuterus” over two years ago and menometrorrhagia for 519months.Present illness: In 1999, the patient was found “myoma ofuterus” in a physical examination. But she had nothing uncomfortable and her catamenia was normal. She used some Chinese traditional medicine. About 5 months ago, she found the cycle of her catamenia was shorten from 30 days to 20 days and the period lasted from2 days to 4 days. She felt no pain and the quantity was normal. She was accepted in our hospital and her diagnosis was “subserous myoma of uterus”.Since onset, her appetite was good, and both her spiritedness and physical energy are normal. Defecation and urination are normal, too.Past historyOperative history: Never undergoing any operation.Infectious history: No history of severe infectious disease.Allergic history: She was not allergic to penicillin or sulfamide. Respiratory system: No history of respiratory disease.Circulatory system: No history of precordial pain.Alimentary system: No history of regurgitation. Genitourinary system: No history of genitourinary disease.20Hematopoietic system: No history of anemia and mucocutaneous bleeding.Endocrine system: No acromegaly. No excessive sweats.Kinetic system: No history of confinement of limbs.Neural system: No history of headache or dizziness.Personal historyShe was born in Hubei on July 16th, 1956 and almost always lived in Wuhan. She graduated from senior high school. Her living conditions were good. No bad personal habits and customs.Menstrual history: The first time when she was 14. Lasting 2 days every times and its cycle is about 30 days.Obstetrical history: Pregnacy 3 times, once nature production, induced abortion twice.Contraceptive history: Not clear.Family history: His parents are both alive.Physical examinationT 36.8?, P 80/min, R 20/min, BP 120/80mmHg. She is well developed and moderately nourished. Active position. The skin was not stained yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not21enlarged. HeadCranium: Hair was black and well distributed. No deformities. No scars. No masses. No tenderness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external auditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nares flaring. No tenderness in nasal sinuses.Eye: Bilateral eyelids were not swelling. No ptosis. No entropion.Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or depressed. Movement was normal. Bilateral pupils wereround and equal in size. Direct and indirect pupillary reactions tolight were existent.Mouth: Oral mucous membrane was smooth, and of no ulcer or erosion. Tongue was in midline. Pharynx was not congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in midline.ChestChestwall: Veins could not be seen easily. No subcutaneous22emphysema. Intercostal space was neither narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities.Breast: Symmetric bilaterally. Neither nipples nor skin were retracted. Elasticity was fine.Lungs: Respiratory movement was bilaterally symmetric with the frequency of 20/min. Thoracic expansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales.Heart: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum impulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardialfriction sound. Border of the heart was normal. Heart sounds were strongand no splitting. Rate 80/min. Cardiac rhythm was regular. Nopathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Therewas not tenderness and rebound tenderness on abdomen or renal region. Liver was not reached. Spleen was not enlarged. No masses. Fluidthrill23negative. Shifting dullness negative. Borhorygmus 5/min. No vascular murmurs. Extremities: No articular swelling. Free movements of all limbs.Neural system: Physiological reflexes were existent without anypathological ones.Genitourinary system: Not examed.Rectum: not exanedInvestigationBlood-Rt: Hb 127g/l RBC 3.93T/l WBC 3.9G/lUrine-Rt: SG 1.070 pH 6.0B-ultrasound: 1. subserous myoma of uterus2. position of loop is normalHepatic function: NormalPT & APTT: NormalProfessional ExaminationPudendum: Married typeVagina: unobstructed, secretion is excessive, white and ropy.Os of cervix: No bleeding, slight anabrosis.Body of uterus: Big like a fist of man, hard and its surface is smooth. Others: Normal24History summary1. Patient was female, 45 years old2. The patient was found “myoma of uterus” over twoyear ago and menometrorrhagia for 5 months..3. No special past history.4. Physical examination showed no abnormity in lung, heart and abdoman. Professional examination can been seen above.5. investigation information: see aboveImpression: subserous myoma of uterusSignature: He Lin (95-10033)25。
疾病英文作文模板Possible Disease Essay Template:Paragraph 1: Introduction。
Disease can be defined as an abnormal condition that affects the body or mind and impairs normal functioning. There are many types of diseases, including infectious, genetic, autoimmune, and lifestyle-related diseases. Some diseases are acute, while others are chronic. Diseases can have various symptoms, such as pain, fever, fatigue, rash, cough, and difficulty breathing. Diseases can also have different causes, risk factors, treatments, and outcomes. In this essay, I will discuss some common diseases and their impact on individuals and society.Paragraph 2: Infectious Diseases。
Infectious diseases are caused by pathogens such as bacteria, viruses, fungi, and parasites. Examples ofinfectious diseases include influenza, tuberculosis, malaria, HIV/AIDS, and COVID-19. Infectious diseases can spread through direct or indirect contact, such as coughing, sneezing, touching, or sharing contaminated objects. Infectious diseases can be prevented by vaccination, hygiene, isolation, and treatment. Infectious diseases can also have social, economic, and political consequences,such as quarantine, travel restrictions, and stigma.Paragraph 3: Genetic Diseases。
英语病历模板范文Chief Complaint:The patient presents with a persistent cough and chest tightness for the past 2 weeks. He also reports feeling fatigued and experiencing shortness of breath during physical activities.History of Present Illness:The patient reports a history of smoking for 20 years, with a 10-pack-year smoking history. He denies any recent travel or exposure to sick contacts. He has been taking over-the-counter cough medicine for symptomatic relief withlimited improvement.Past Medical History:The patient has a history of hypertension and hyperlipidemia, for which he takes medication regularly. Healso reports a past history of seasonal allergies and occasional sinus infections.Family History:There is a family history of cardiovascular disease, with the patient's father suffering from a heart attack at the age of 55.Physical Examination:Vital signs on presentation were stable with a blood pressure of 130/80 mmHg, pulse rate of 80 beats per minute, respiratory rate of 18 breaths per minute, and oxygen saturation of 98% on room air. Lung auscultation revealed bilateral scattered wheezes and diminished breath sounds in the lower lung fields.Assessment and Plan:Based on the patient's presenting symptoms and physical examination findings, the working diagnosis is exacerbationof chronic obstructive pulmonary disease (COPD). The plan includes initiating bronchodilators, corticosteroids, and supplemental oxygen therapy. A chest X-ray will be ordered to rule out any acute pathology. Patient education on smoking cessation will be provided, and a follow-up appointment in 2 weeks for reassessment of symptoms will be scheduled.。
英文大病例写作示例
撰写大病例是实习医师与住院医师的日常工作,也是上级医师作进一步诊断治疗的原始依据,国外的英文大病例并无统一格式,但是基本内容大致相仿,本节介绍的许多医疗记录的词汇值得借鉴。
Details个人资料
Name: Joe Bloggs(姓名:乔。
伯劳格斯)
Date: 1st January 2000(日期:2000年1月1日)
Time: 0720(时间:7时20分)
Place: A&E(地点:事故与急诊登记处)
Age: 47 years(年龄:47岁)
Sex: male(性别:男)
Occupation: HGV(heavy goods vehicle )driver(职业:大型货运卡车司机)
PC(presenting complaint)(主诉)
4-hour crushing retrosternal chest pain(胸骨后压榨性疼痛4小时)HPC(history of presenting complaint)(现病史)
Onset: 4 hours of “crushing tight” retrostern al chest pain,radiating to neck and both arms,gradual onset over 5-10 minutes.(起病特征:胸骨后压榨性疼痛4小时,向颈与双臂放,
5-10分钟内渐起病)
Duration: persistent since onset(间期:发病起持续至今)
Severe: “worst pain ever had”(严重性:“从未痛得如此厉害过)
Relieving/exacerbating factors缓解与恶化因素
GTN(glyceryl trinitrate)provided no relief although normally relieves pain in minutes,no other relieving/exacerbating factors.(硝酸甘油平时能在数分钟内缓解疼痛,但本次无效,无其它缓解和恶化因素。
)Associated symptoms相关症状
Nausea,vomiting×2,sweating,dizzy(恶心、呕吐2次、出汗、眩晕)
1997:external chest tightness and dyspnea initially controlled atenolol.
1997年:出现胸外疼痛与呼吸困难,最终经服atenolol控制。
4/12 symptoms worse,exercise tolerance 200 yards on flat,limited by chest pain
4月12日,症状加重,受胸痛限制,仅耐受平地行走200码
No rest pain,no orthopnoea,no PND
无静息时疼痛,无端坐呼吸、无阵发性夜间呼吸困难
Risk factors危险因素
Hypertension-no高血压:无
Smoking-20 cigarettes per day for 16 years吸烟:16年来每天20支
Diabetes-no糖尿病:无
Cholesterol-never checked胆固醇:未查
Ischemic heart disease-angina,previous MI缺血性心脏病:心绞痛、有心肌梗死病史
PMH(past medical history)过去史
1963: appendectomy1963年:阑尾切除手术
1972: duodenal ulcer,no symptoms since1972年:十二指肠溃疡,之后无症状
1986: myocardial infarction,full recovery / No subsequent investigation1986年:
心肌梗死,完全恢复,无随访
1989: gout quiescent on treatment1989年:痛风治疗期间症状静止No diabetes,hypertension,rheumatic heart disease,tuberculosis,epilepsy,asthma,jaundice,cerebrovascular disease.无糖尿病、高血压、风湿性心脏病、结核病、癫痫、哮喘、黄疸、脑血管疾病S/E(systems inquiry)系统回顾
General 一般情况
Fatigue lately,appetite unchanged,weight stable,no sweats or pruritus,sleeping well
最近有疲劳感,食欲无改变,体重稳定,无出汗或骚痒,睡眠佳。
RS呼吸系统
Dyspnea on exertion,particularly uphill,but not limiting;no cough sputum/wheeze
劳累时呼吸困难,上坡尤其如此,但无呼吸限制,无咳嗽咳痰、哮喘。
GIT gastrointestinal tract胃肠道
No current indigestion现无消化不良。
No symptoms lile previous duodenal ulcer过去无十二指肠溃疡症状。
No vomiting/dysphagia/abdominal pain无呕吐、吞咽困难、腹部疼痛。
GUS genitourinary system生殖泌尿道
No urinary systems无泌尿道症状。
NS神经系统
No headache/syncope无头痛、晕厥。
No dizziness/limb weakness/sensory loss无眩晕、肢体麻木、感觉丧失。
No disturberd bision/hearing/smell/speech无视觉、听力、味觉、嗅觉、语言障碍。
MS运动系统
No painful gout for 5 years无痛性痛风5年。
No joint pain/stiffness/swelling无关节痛、僵硬、肿胀。
No disability无伤残。
Skin皮肤
No rash/pruritus/bruising无皮疹、瘙痒、青肿。
Drug history药物史
Atenolol 100 mg once daily(Atenolol100mg每天1次)
GTN as required需要服用硝酸甘油。
Not taking aspirin无服用过阿斯匹林。
Allergies: penicillin-skin rash过敏反应:青霉素――皮疹。
FH(family history)家族史
Father died of “heart attack” at age 53.
父亲53岁死于“心脏病”。
Mother died of old age at 76.
母亲于76岁去世。
SH(social history)社会史
Lives with wife who fit and well.妻子健在,与其共同生活。
Own house私宅。
Completely independent生活全部自理。
Smoking 20 cigs/day for many years多年每天抽烟20支。
Alcohol: 24 units per week饮酒:每周24个单位。
Sexual history: not appropriate性生活:未评价。
Overseas travel: not appropriate海外旅游:未评价。
Pets: not appropriate宠物:未评价。
Occupation: heavy goods vehicle driver职业:大型货车卡车司机。
O/E(on examination)体检结果
General 一般情况
Unwell,sweaty,clammy,no cyanosis/jaundice
一般情况不佳,出汗、皮肤湿冷,无青紫、黄疸。
temperature: 37.5℃
体温37.5℃。
cigarette-stained fingers
烟熏手指。
no arcus / xanthomas / xanthelasma
无老人弓环、黄瘤、黄斑瘤。
CVS心血管系统
Pluse 104 bpm regular,normal character
脉搏每分钟104次,规则,心音正常。
BP110/70 mmHg (right),112/74 mmHg (left)
血压110/70 mmHg右,112/74 mmHg左。
JVP(jugular venous pulse)normal
颈静脉博动正常。
No precordial scars /chest deformities
无心前区疤痕、胸廓畸形。
Apex beat displaced to anterior axillary’s line 6th intercostals space
心尖博动向腋前线第6肋间移位。
No parasternal heave /thrills
无胸骨旁隆起、震颤。
Auscultation: heart sounds normal,but soft pan systolic murmur at apex radiating to axilla。