英文病历(发热待查)
- 格式:doc
- 大小:52.00 KB
- 文档页数:7
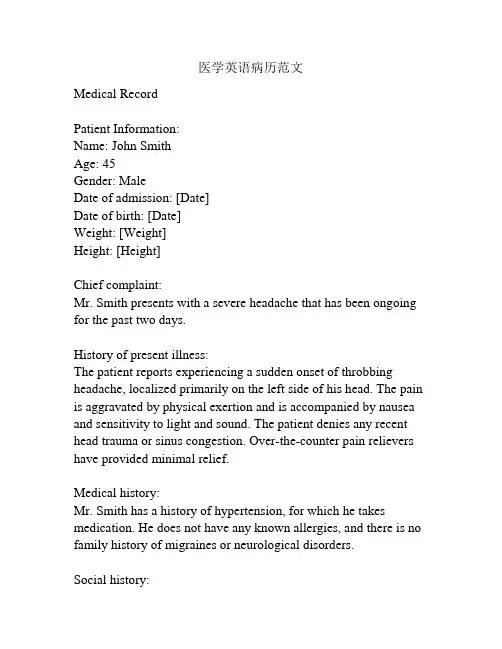
医学英语病历范文Medical RecordPatient Information:Name: John SmithAge: 45Gender: MaleDate of admission: [Date]Date of birth: [Date]Weight: [Weight]Height: [Height]Chief complaint:Mr. Smith presents with a severe headache that has been ongoing for the past two days.History of present illness:The patient reports experiencing a sudden onset of throbbing headache, localized primarily on the left side of his head. The pain is aggravated by physical exertion and is accompanied by nausea and sensitivity to light and sound. The patient denies any recent head trauma or sinus congestion. Over-the-counter pain relievers have provided minimal relief.Medical history:Mr. Smith has a history of hypertension, for which he takes medication. He does not have any known allergies, and there is no family history of migraines or neurological disorders.Social history:The patient is a smoker, consuming approximately 10 cigarettes per day. He drinks alcohol in moderation, primarily on social occasions. He denies any illicit drug use. His occupation involves long hours of computer work.Physical examination:On examination, the patient appears to be in mild distress due to the headache. His vital signs are within normal limits. Neurological examination reveals no focal deficits, and his cranial nerves appear to be intact. There is no evidence of meningeal irritation. His neck is supple, and there is no nuchal rigidity. The remainder of the physical examination is unremarkable. Laboratory tests:Blood tests, including a complete blood count and comprehensive metabolic panel, were performed. All results were within normal limits.Imaging studies:A brain MRI was ordered to rule out any structural abnormalities. The scan revealed no evidence of intracranial hemorrhage, mass, or other abnormalities.Assessment and plan:Mr. Smith is presenting with a severe headache consistent with a migraine without aura. He will be prescribed a triptan medication for acute management of his headache. He will also be counseled on lifestyle modifications, including smoking cessation and stress reduction techniques. A follow-up appointment will be scheduled in two weeks to evaluate the effectiveness of the treatment plan.Additionally, the patient is advised to seek immediate medical attention if his symptoms worsen or if he develops any new neurological symptoms.Signature: [Physician's Name]Date: [Date]。
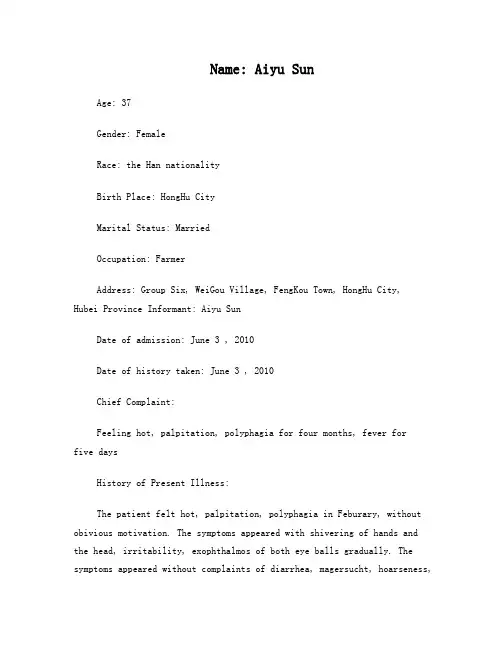
Name: Aiyu SunAge: 37Gender: FemaleRace: the Han nationalityBirth Place: HongHu CityMarital Status: MarriedOccupation: FarmerAddress: Group Six, WeiGou Village, FengKou Town, HongHu City,Hubei Province Informant: Aiyu SunDate of admission: June 3 , 2010Date of history taken: June 3 , 2010Chief Complaint:Feeling hot, palpitation, polyphagia for four months, fever forfive daysHistory of Present Illness:The patient felt hot, palpitation, polyphagia in Feburary, without obivious motivation. The symptoms appeared with shivering of hands and the head, irritability, exophthalmos of both eye balls gradually. The symptoms appeared without complaints of diarrhea, magersucht, hoarseness,blurred vision and so on. The patient did not go to receive any medical treatment. From April, the symptoms above became more severe, with powerless of limbs. The patient went to local hospital on 27th, April. Examination result: FT3>25pg/ml↑,FT4>8npg/dl↑,TSH<0.01uIU/ml↓;WBC6.11*109/L, N7.01*109/L; ALT 52u/L↑, AST 41u/L. The patient was diagnosed as “hyperthyroidism, cacergasia of liver”. The patient took Tapazole 5mg tid , propanolol, inosine, drugs for liver protection and WBC raising from then on. The symptoms described above was relievedafter taking these medicines. On 12nd, May, the bood routine was still normal: WBC 5.8*109/L, N 3.1*109/L. But five days ago, without obivious motivation, the patient had a pharynx ache, fever, which was highest at 38.7°C,with headache and catarrhus. The pati ent was diagnosed as “upper respiratory infection, hyperthyroidism, agranulemia” and gave antiinfection therapy. But the fever continued, the therapy effect was not well. The patient comes to our hospital today. The blood routine today is WBC 0.15*109/L↓, N0*109/L↓↓↓, and the outpatient department receives the patient to our ward as“hyperthyroidism, agranulemia”.During the course of disease, sleep and psyche were acceptable. Polyphagia lasted. Stool and urine were as usual. Physical strength descended. Weight was stable.Past History:General Health Status: good √moderate poorInfectious Disease: √no yes(if any, please write down date of onset, brief diagnostic and therapeutic, course )Typhoid fever Dysentery Malaria Schistosomiasis Leptospirosis Tuberculosis Epidemic hemorrhagic fever othersAllergic history: √no yes (clinical manifestation: allergen: ) Trauma and/or operation history: √no yes- 1 -Review of Symptoms:Respiratory system: √no yesRepeated pharyngeal pain:chronic cough: expectoration: Hemoptysis: asthma: dyspnea: chest pain:Circulatory system:√no yesPalpitation: exertional dyspnea: cyanosis: hemoptysis: Edema of lower extremities: chest pain: syncope: hypertension:Digestive system:√no yesAnorexia: dysphagia: sour regurgitation: eructation: nausea: Emesis: melena: abdominal pain: diarrhea: hematemesis: Hematochezia: jaundice:Urinary system:√no yesLumbar pain: urinary frequency: urinary urgency: dysuria: oliguria: Polyuria: retention of urine: incontinence of urine: hematuria: Pyuria: nocturia: puffy face:Hematopoietic system:√no yesFatigue: dizziness: gingival hemorrhage: epistaxis: subcutaneous hemorrhage:Metabolic and endocrine system:√no yesBulimia: anorexia: hot intolerance: hyperhidrosis: cold intolerance: Polydipsia: amenorrhea: tremor of hands: character change: Marked obesity: marked emaciation: hirsutism: alopecia: Hyperpigmentation: sexual function change: impotence: amenorrhea:Musculoskeletal system:√no yesMigrating arthralgia: arthralgia: artrcocele: arthremia: Dysarthrosis: myalgia: muscular atrophy:Neurological system:√no yesDizziness: headache: paresthesia: hypomnesis: Visual disturbance: Insomnia: somnolence: syncope: convulsion:Disturbance of consciousness: paralysis: vertigo:Personal history:Resident history in endemic disease area:√no yesSmoking: √no yes: about___yearsDrinking:√no occasional frequent: about____years average____ml/day Others:In April 2009, the patient was diagnosed as “polyp of vocal cord” in our hospital and got medicine thrapy.Menstrual history:Menarchal age: 21 years old duration__5__days/ interval_30_daysLast menstrual period: 2010.5.1 menopausal age: _13_years oldAmount of flow: small √moderate largedysmenorrheal: p resence √absenceMarital and obstetrical history:Married age: 21 years old pregnancy_4__times natural labour: 3 timesAbortion: 2 times premature labour: 0 times still birth: 0 timesDystocia and its course:0Family history:(pay attention to the infectious and hereditary disease related to the present illness)Father: √healthy ill: deceased cause:Mother: √healthy ill: deceased cause:Others: noPhysical ExaminationGeneral conditions:Temperature: 37.3°C pulse:88 times per minute (√regular irregular)Blood pressure:139/84mmHg respiration: 20 times per minute(√regular irregular) Development: √normal HypoplasiaNutrition: good √moderate poor cachexiaFacial expression: √normal acute chronic other( )Posture: √active semi-reclining position other ( )Mental status:√clear confusion somnolence delirium comaGait: √normal abnormal cooperation: √yes noSkin and mucosa:Color:√normal pale cyanosis stained yellow pigmentationrash:√no yes: (type: distribution: )subcutan eous hemorrhage: √no yes (type: distribution: )Hair distribution: √normal hypertrichosis oligotrichosisalopecial(location: ) Temperature and moisture: √normal cold warm dry moist dehydrationEdema: √no yes ( location and degree )Liver palmar : √no yes spider angioma:√no yes (location: )Others: noLymph nodes:enlargement of superfacial lymph node: √no yes (location and description: ) Head: without abnormityCranium: without abnormityEye: exophthalmos: exophthalmos of both eye ballseyelid: without descensusconjunctiva: without edemasclera: without stained yellowCornea: √normal abnormal ( od os )Pupil:√equally round and equal in size: unequal (od os )Pupil reflex: √normal delayed (od os ) absent (od os ) others:Ear: di scharge of external auditory canal:√normal (left right quality: ) Mastoid tenderness : no (left right )disturbance of rough hearing test: yes √noNose: flaring of alae nasi:√no yesstuffy discharge:√no yestenderness over paranasal sinuses: √no ye s(location: )Mouth: lip: redMucosa: without ulcerationTongue: stretched tongue is in the middleGum: nomalTonsil: Ⅰ°enlargement of both sidesPharynx: congestionsound: √normal hoarseness teeth: √normal absent carieNeck:neck rigidit y √no yes (distance between sternum and mandible:______transvers fingers) Carotid artery: √normal pulsation increased pulsation marked distention Trachea:√middle deviation (leftward rightward )Hepatojugular vein reflux: negativeThyroid: normal √enla rged bruitChest:Chest wall: √normal barrel chest prominence or retraction: (left right ) Precordial prominence: √no yespercussion pain over sternum:√no yesBreast: normalLung:Inspection: normal respiratory movementPalpation:vocal tactile fremitus: normalpleural rubbing sensation: √no yesSubcutaneous crepitus sensation:√no yesPercussion: √resonanc dullness Flatness Hyperresonance tympany lower border of lung: (detailed percussion in respiratory disease) midclavicular line : right:_6__cm left:_6__cmmidaxillary line: right:_8__cm left:_8__cmscapular line: right:_10__cm left:_10__cmAuscultation: breathing sound :√normal abnormalRales: √no yes (moist dry ) location:Heart:Inspection:apical pulsation:√normal unseen increase diffuse sSubxiphoid pulsation: √no yesLocation of apex beat:√normal shift (distance away from leftMCL___cm) Palpation:apical pulsation: √normal lifting apex impulse negative pulsationThrill:√no yes (location: ) phase:Percussion:relative dullness border:√Normal decreased absent increaseR(cm) line L(cm)2 Ⅱ 22 Ⅲ 43 Ⅳ 6Ⅴ8Distance between anterior median line and MCL 8.5cm Auscultation: heart rate: 88bpm rhythm: regularheart sound:√normal abnormalextra s ound:√no S3 gallop S4 opening snap:murmur: √no yes:location timing quality intensity transmission:effects of position:effects of respiration:P2 = A2 pericardial friction sound:√no yesPeripheral vascular sign: √no yes: paradoxical pulse pu lsus alternansWater hammer pulse capillary pulsationpulse deficit Pistol shot sound Duroziez sign Abdomen:Inspection: shape: √normal distention scaphoid frog-bellygastric pattern:√no yes visible intestinal peristalsis:√no yesabdominal vein v aricose: √no yes (direction: )operation scar:√no yesPalpation: √soft guarding (location: )Tenderness: √no yes (location: )rebound tenderness:√no yes (location: )fluctuation succussion splash:√no yesliver: can’t be touch ed under the ribsgallbladder: can’t be touched under the ribsMurphy sign: negativespleen: can’t be touched under the ribskidneys: kidney zones without Percussion painabdominal mass :can’t be touchedPercussion: liver dullness border: √normal decreased absen tUpper hepatic border locates at right midclavicularline5_intercostal spaceShift dullness: negativePain on percussion in costovertebral area:√no yes R L Auscultation: bowel sounds : √normal hyperperistalsis hypoperistalsis absenceVascular bruit :√no yes (location )Genital organ: √unexamined normal abnormalAnus and rectum:√unexamined normal abnormalSpine and extremities:Spine: √normal deformity (kyphosis lordosis scoliosis )Tenderness (location )Extremities: √normal arthremia(loc ation ) arthrocele (location ) Ankylosis (location ) aropachy Muscular tenderness(location ) muscular atrophy (location )Neurological system:Abdominal reflex++ cremasteric reflex- knee reflex++Kernig`s sign(R- L- ) Brudzinski`s sign:(R- L- ) Babinski sign (R- L- )Opphenheim sign(R- L- )Gordon sign (R- L- ) Lasegue sign (R- L- ) Others: noImportant exam results from out-patient service: X-ray number:no27th, April, local hospital: FT3>25pg/ml↑,FT4>8npg/dl↑,TSH<0.01uIU/ml↓;WBC 6.11*109/L, N 7.01*109/L;ALT 52u/L↑, AST 41u/L.12nd, May, local hospital: Blood-rt: WBC 5.8*109/L, N 3.1*109/L3rd, June, our hospital: Blood-rt: WBC 0.15*109/L↓, N0*109/L↓↓↓Summary of case history:1 Patient Aiyu Sun, female, 37 years old.2 Chief Complaint: Feeling hot, palpitation, polyphagia for four months, fever for five days3 Past History: General health status was moderate. In April 2009, the patient was diagnosed as “polyp of vocal cord” in our hospital and got medicine thrapy. The patient deny history of TB, HBV, schistosome infection, DM, HBP, heart diseases and other special diseases. The patient deny history of allergy, trama, surgery operation and blood transfusion.4 Physical Examination: T37.3°C P88 times per minute BP:139/84mmHg R: 20 times per minute. Normal development, moderate nutrition, active posture, clear mental status, cooperated examination. There is no yellow stained in the skin and mucosa. There is no enlargement of superfacial lymph nodes. Head shape and cranium are normal. There is exophthalmos of both eye balls. Both tonsils are Ⅰ°enlarged. Pharynx is congestion. No neck rigidity. Trachea is in the middle. Thyroid of both sides isⅡ°enlarged, without vascular bruit. Breathing sound of the lung is normal. And there is no rale. Heart rhythm is regular, without any obvious murmur at each valve zone. Abdomen shape is normal. Abdomen is soft, without tenderness or rebound tenderness. Liver and spleen can’t be touched under the ribs. Kidney zones are without percussion pain. Both hands are shivering. There is no edema of both lower limbs.5 exam results:27th, April, local hospital: FT3>25pg/ml↑,FT4>8npg/dl↑,TSH<0.01uIU/ml↓;WBC 6.11*109/L,N 7.01*109/L; ALT 52u/L↑, AST 41u/L.12nd, May, local hospital: Blood-rt: WBC 5.8*109/L, N 3.1*109/L;3rd, June, our hospital: Blood-rt: WBC 0.15*109/L↓, N0*109/L↓↓↓Primary diagnosis:1 Hyperthyroidism2 Agranulemia:(1)Induced by drugs;(2)Hematopoietic system diseases?(such as aplastic anemia,MDS,leukemia etc.)3 Acute upper respiratory infection4 Other diseases which cause fever: such as other infections, connective tissue diseases etc.Corrected diagnosis (date 2010.6.4)1 Hyperthyroidism2 Agranulemia: Induced by drugs3 Acute upper respiratory infectionsignature:writer: Yanling LiangRevisor:。
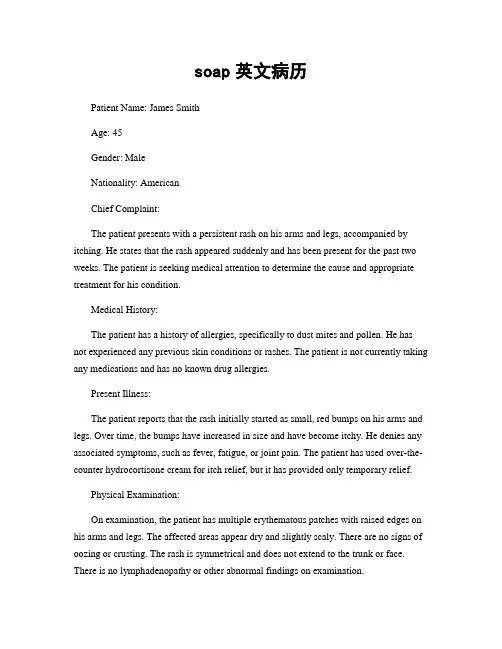
soap英文病历Patient Name: James SmithAge: 45Gender: MaleNationality: AmericanChief Complaint:The patient presents with a persistent rash on his arms and legs, accompanied by itching. He states that the rash appeared suddenly and has been present for the past two weeks. The patient is seeking medical attention to determine the cause and appropriate treatment for his condition.Medical History:The patient has a history of allergies, specifically to dust mites and pollen. He has not experienced any previous skin conditions or rashes. The patient is not currently taking any medications and has no known drug allergies.Present Illness:The patient reports that the rash initially started as small, red bumps on his arms and legs. Over time, the bumps have increased in size and have become itchy. He denies any associated symptoms, such as fever, fatigue, or joint pain. The patient has used over-the-counter hydrocortisone cream for itch relief, but it has provided only temporary relief.Physical Examination:On examination, the patient has multiple erythematous patches with raised edges on his arms and legs. The affected areas appear dry and slightly scaly. There are no signs of oozing or crusting. The rash is symmetrical and does not extend to the trunk or face. There is no lymphadenopathy or other abnormal findings on examination.Differential Diagnosis:1. Contact dermatitis: Contact with an irritant or allergen may cause a localized rash with itching and erythema.2. Atopic dermatitis: Chronic inflammatory skin condition characterized by itching, redness, and dryness of the skin.3. Psoriasis: Autoimmune disorder causing thick, scaly patches on the skin.4. Scabies: Infestation of the skin by microscopic mites causing intense itching and a characteristic rash.Investigations:1. Skin scraping and microscopic examination: To rule out scabies infestation.2. Allergy testing: To determine if the rash is related to an allergic reaction.Treatment Plan:1. Topical steroid cream: Prescribe a stronger topical steroid cream to reduce inflammation and relieve itching. Instruct the patient to apply a thin layer to the affected areas twice daily for two weeks.2. Moisturizers: Recommend using non-fragrance, hypoallergenic moisturizers to keep the skin hydrated and prevent dryness.3. Avoid triggers: Advise the patient to avoid known allergens or irritants that may exacerbate the rash.4. Follow-up: Schedule a follow-up appointment in two weeks to evaluate the effectiveness of the treatment and make any necessary adjustments.Patient Education:1. Review proper application of the topical steroid cream and discuss potential side effects, such as skin thinning and discoloration.2. Emphasize the importance of avoiding scratching to prevent infection and further skin damage.3. Discuss the potential triggers for allergic reactions and provide recommendations for allergen avoidance, such as using fragrance-free products and washing clothes with mild detergents.Prognosis:With appropriate treatment and adherence to the prescribed regimen, the prognosis for this patient is good. The symptoms should improve within two weeks with resolution of the rash and relief from itching. However, it is important to monitor the patient for any signs of exacerbation or recurrence.。

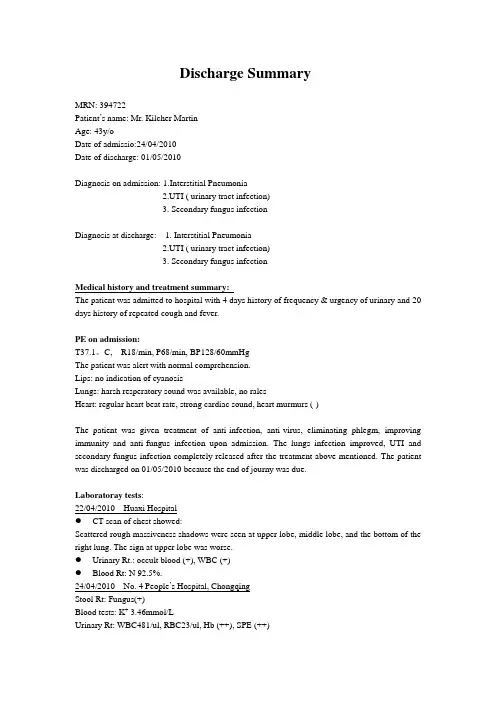
Discharge SummaryMRN: 394722Patient’s name: Mr. Kilcher MartinAge: 43y/oDate of admissio:24/04/2010Date of discharge: 01/05/2010Diagnosis on admission: 1.Interstitial Pneumonia2.UTI ( urinary tract infection)3. Secondary fungus infectionDiagnosis at discharge: 1. Interstitial Pneumonia2.UTI ( urinary tract infection)3. Secondary fungus infectionMedical history and treatment summary:The patient was admitted to hospital with 4 days history of frequency & urgency of urinary and 20 days history of repeated cough and fever.PE on admission:T37.1。
C, R18/min, P68/min, BP128/60mmHgThe patient was alert with normal comprehension.Lips: no indication of cyanosisLungs: harsh resperatory sound was available, no ralesHeart: regular heart beat rate, strong cardiac sound, heart murmurs (-)The patient was given treatment of anti-infection, anti-virus, eliminating phlegm, improving immunity and anti-fungus infection upon admission. The lungs infection improved, UTI and secondary fungus infection completely released after the treatment above mentioned. The patient was discharged on 01/05/2010 because the end of journy was due.Laboratoray tests:22/04/2010 Huaxi Hospital●CT scan of chest showed:Scattered rough massiveness shadows were seen at upper lobe, middle lobe, and the bottom of the right lung. The sign at upper lobe was worse.●Urinary Rt.: occult blood (+), WBC (+)●Blood Rt: N 92.5%.24/04/2010 No. 4 People’s Hospital, ChongqingStool Rt: Fungus(+)Blood tests: K+ 3.46mmol/LUrinary Rt: WBC481/ul, RBC23/ul, Hb (++), SPE (++)30/04/2010 No. 4 People’s Hospital, ChongqingUrinary Rt: normalStool Rt: normalBlood Rt: normalCT scan of chest showed a sign of inflammation at right lung with mild pleural effusion, which indicated that the lung infection was at the stage of absorbtion.Ultrasound of heart: no indication of pericardial effusion.Others: normalOn the date of discharge, the patient had cough occationally. No fever, chest pain, no urinary frequency and urgency. The patient stayed in a normal mental staus with good appetite. Normal bowels movement and passing water. The patient was allawed to leave hospital on account of the end of the journey was due.Suggestions by treating doctor:Dringking WaterAvoid tiredRecieptName: Kilcher Martin。
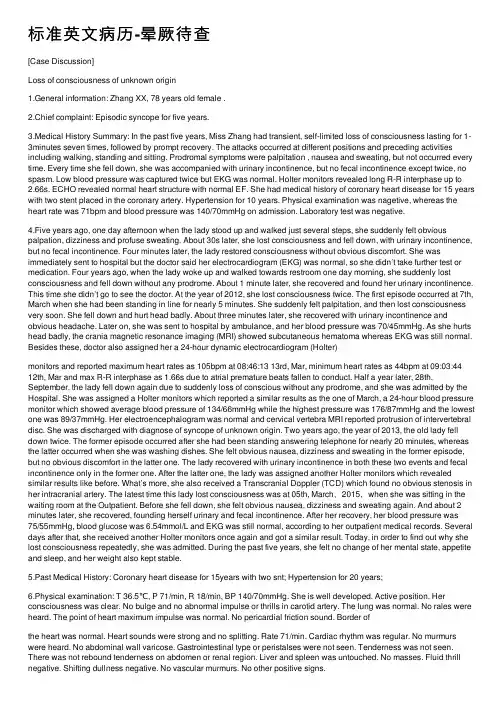
标准英⽂病历-晕厥待查[Case Discussion]Loss of consciousness of unknown origin1.General information: Zhang XX, 78 years old female .2.Chief complaint: Episodic syncope for five years.3.Medical History Summary: In the past five years, Miss Zhang had transient, self-limited loss of consciousness lasting for 1-3minutes seven times, followed by prompt recovery. The attacks occurred at different positions and preceding activities including walking, standing and sitting. Prodromal symptoms were palpitation , nausea and sweating, but not occurred every time. Every time she fell down, she was accompanied with urinary incontinence, but no fecal incontinence except twice, no spasm. Low blood pressure was captured twice but EKG was normal. Holter monitors revealed long R-R interphase up to 2.66s. ECHO revealed normal heart structure with normal EF. She had medical history of coronary heart disease for 15 years with two stent placed in the coronary artery. Hypertension for 10 years. Physical examination was nagetive, whereas the heart rate was 71bpm and blood pressure was 140/70mmHg on admission. Laboratory test was negative.4.Five years ago, one day afternoon when the lady stood up and walked just several steps, she suddenly felt obvious palpation, dizziness and profuse sweating. About 30s later, she lost consciousness and fell down, with urinary incontinence, but no fecal incontinence. Four minutes later, the lady restored consciousness without obvious discomfort. She was immediately sent to hospital but the doctor said her electrocardiogram (EKG) was normal, so she didn’t take further test or medication. Four years ago, when the lady woke up and walked towards restroom one day morning, she suddenly lost consciousness and fell down without any prodrome. About 1 minute later, she recovered and found her urinary incontinence. This time she didn’t go to see the doctor. At the year of 2012, she lost consciousness twice. The first episode occurred at 7th, March when she had been standing in line for nearly 5 minutes. She suddenly felt palpitation, and then lost consciousness very soon. She fell down and hurt head badly. About three minutes later, she recovered with urinary incontinence and obvious headache. Later on, she was sent to hospital by ambulance, and her blood pressure was 70/45mmHg. As she hurts head badly, the crania magnetic resonance imaging (MRI) showed subcutaneous hematoma whereas EKG was still normal. Besides these, doctor also assigned her a 24-hour dynamic electrocardiogram (Holter)monitors and reported maximum heart rates as 105bpm at 08:46:13 13rd, Mar, minimum heart rates as 44bpm at 09:03:44 12th, Mar and max R-R interphase as 1.66s due to atrial premature beats fallen to conduct. Half a year later, 28th, September, the lady fell down again due to suddenly loss of conscious without any prodrome, and she was admitted by the Hospital. She was assigned a Holter monitors which reported a similar results as the one of March, a 24-hour blood pressure monitor which showed average blood pressure of 134/66mmHg while the highest pressure was 176/87mmHg and the lowest one was 89/37mmHg. Her electroencephalogram was normal and cervical vertebra MRI reported protrusion of intervertebral disc. She was discharged with diagnose of syncope of unknown origin. Two years ago, the year of 2013, the old lady fell down twice. The former episode occurred after she had been standing answering telephone for nearly 20 minutes, whereas the latter occurred when she was washing dishes. She felt obvious nausea, dizziness and sweating in the former episode, but no obvious discomfort in the latter one. The lady recovered with urinary incontinence in both these two events and fecal incontinence only in the former one. After the latter one, the lady was assigned another Holter monitors which revealed similar results like before. What’s more, she also received a Transcranial Doppler (TCD) which found no obvious stenosis in her intracranial artery. The latest time this lady lost consciousness was at 05th, March,2015,when she was sitting in the waiting room at the Outpatient. Before she fell down, she felt obvious nausea, dizziness and sweating again. And about 2 minutes later, she recovered, founding herself urinary and fecal incontinence. After her recovery, her blood pressure was75/55mmHg, blood glucose was 6.54mmol/L and EKG was still normal, according to her outpatient medical records. Several days after that, she received another Holter monitors once again and got a similar result. Today, in order to find out why she lost consciousness repeatedly, she was admitted. During the past five years, she felt no change of her mental state, appetite and sleep, and her weight also kept stable.5.Past Medical History: Coronary heart disease for 15years with two snt; Hypertension for 20 years;6.Physical examination: T 36.5℃, P 71/min, R 18/min, BP 140/70mmHg. She is well developed. Active position. Her consciousness was clear. No bulge and no abnormal impulse or thrills in carotid artery. The lung was normal. No rales were heard. The point of heart maximum impulse was normal. No pericardial friction sound. Border ofthe heart was normal. Heart sounds were strong and no splitting. Rate 71/min. Cardiac rhythm was regular. No murmurs were heard. No abdominal wall varicose. Gastrointestinal type or peristalses were not seen. Tenderness was not seen. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluid thrill negative. Shifting dullness negative. No vascular murmurs. No other positive signs.7.Investigation information: EKG(08th,May.2015): sinus rhythm, heart rate 71/min, QS waveform was seen at III and A VF leads.Impression: Loss of consciousness (unknown origin)Coronary heart diseaseHypertensionHyperlipidemiaFatty liver。



英语病历范文Patient Information:- Name: [Not Specified]- Age: [Not Specified]- Date: [Not Specified]- Doctor: [Not Specified]Chief Complaint:The patient presents with a persistent cough, accompanied by mild fever and body aches for the past three days.History of Present Illness:The patient first noticed the symptoms on [Date], with a dry cough that gradually worsened. The fever started as low-grade but has been increasing, reaching up to 38.5 degrees Celsius.Past Medical History:The patient has no significant past medical history. No previous hospitalizations or chronic illnesses are reported.Medications:The patient has not taken any medications for the current illness, nor are they on any regular medication.Allergies:No known allergies to medications or environmental factors.Physical Examination:Vital signs: Temperature 38.3°C, Puls e 92 bpm, Respiratory rate 20 breaths per minute, Blood pressure 120/80 mmHg. The patient appears fatigued but in no acute distress. Lungs are clear to auscultation with no wheezing or crackles. The throat is slightly red without exudates.Assessment:Based on the symptoms and physical examination, the patient is likely suffering from a viral upper respiratory infection.Plan:1. Hydration and rest are recommended.2. Over-the-counter fever reducers and cough suppressants may be used as needed for symptomatic relief.3. If symptoms persist or worsen, the patient should return for further evaluation and potential testing for influenza or COVID-19.Follow-up:The patient is advised to follow up in one week if symptoms have not improved or if new symptoms develop.Instructions:- Increase fluid intake to prevent dehydration.- Avoid contact with others to prevent the spread of the infection.- Monitor for signs of worsening condition, such as difficulty breathing, persistent high fever, or chest pain.Note: This is a hypothetical patient case and should not be used as a substitute for professional medical advice, diagnosis, or treatment.。
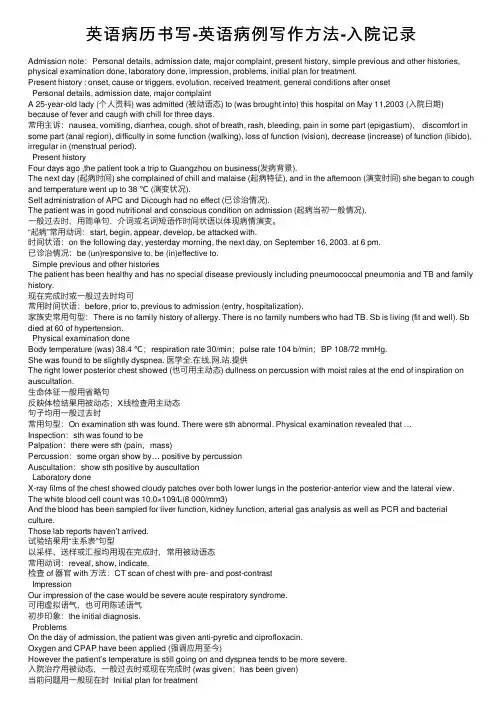
英语病历书写-英语病例写作⽅法-⼊院记录Admission note:Personal details, admission date, major complaint, present history, simple previous and other histories, physical examination done, laboratory done, impression, problems, initial plan for treatment.Present history : onset, cause or triggers, evolution, received treatment, general conditions after onsetPersonal details, admission date, major complaintA 25-year-old lady (个⼈资料) was admitted (被动语态) to (was brought into) this hospital on May 11,2003 (⼊院⽇期) because of fever and caugh with chill for three days.常⽤主诉:nausea, vomiting, diarrhea, cough, shot of breath, rash, bleeding, pain in some part (epigastium), discomfort in some part (anal region), difficulty in some function (walking), loss of function (vision), decrease (increase) of function (libido), irregular in (menstrual period).Present historyFour days ago ,the patient took a trip to Guangzhou on business(发病背景).The next day (起病时间) she complained of chill and malaise (起病特征), and in the afternoon (演变时间) she began to cough and temperature went up to 38 ℃ (演变状况).Self administration of APC and Dicough had no effect (已诊治情况).The patient was in good nutritional and conscious condition on admission (起病当初⼀般情况).⼀般过去时,⽤简单句,介词或名词短语作时间状语以体现病情演变。
发一份英文病历格式,希望对大家有用。
CASE HISTORYName……………..Age…………….Sex……………………..Maritalstatus ……………Race …………….Nationality …………………. Occupation …………Residence: ……………………………………………………………………………………………………………………………Chiefcomplaint: ……………………………………………………………………………………………………………………….Presentillness: …………………………………………………………………………………………………………………………Past history:General health up to onset of present illness, immunization, exposure to tuberculosis and other infections.Previous illness: Influenza, scarlet fever, diphtheria, typhoid fever, bronchitis, asthma, pneumonia, pleurisy, tonsillitis, rheumatism or sheumatic fever, cholera, tuberculosis, malaria or any other severe disorders. Operations: Date of each operation, nature, anesthetics used, complications and length of time patient incapacilted.Injuries: Details concerning any severe injuries .Personal history: Birth place, former places of residence, habits.Marital history:Family history:Social history:Physical examination:Temperature………… pulse rate……….respiratory rate …………blood pressure……….height ………… weight …………..General appearance:Appearance …………physicaldevelopment ……………..nutrition………………..status………….posture…………..gait…Tremors or other abnormal movements.Mental status:degree of consciousness…………….cooperation…………….orientation…………emotional state…………………Skincolor…………..texture…………….moisture………..hair-distribution…………character of scalp………………..Face:appearance…………color………..tenderness………………abnormal movements………………Eyes:Brows……….lids………..vision…………….eyeballmotion ………….prominence……………..tension……conjunctivae………sclerae……..corneae………..irises………….pupils……………..size……………shape………….regularity ……………….reactions……………fields………………fundi……………Ears:appearance……hearing…….tenderness………….discharge……….drums ……………canals…………….postauricular swelling or tenderness………………………..Nose:appearance ……..discharge………………nasal cavity …………septum………….transillumination……………..smell…….Mouth:Breath……………lips …………color…………fissure………….lesions…………………Tongue:tremor…..deviation………..color……..moisture……….texture……………..Gingivae:color…………….texture……….recession…………bleeding…………….Lesions:Teeth-number………….condition…………dentures…………….buccal mucus color………….eruptions…….lesions……Throat:palate and uvula ……………….pillars………..tonsils…………poster ior pharynx………larynx…………..Neck:lymphnodes…………….scars………thyroid……….salivaryglands……….position……….motion………veins…..pulsation…edema……..trachea……………..Shoulder girdle:deformity……….swelling………….tenderness………….freedom of movements………….muscle spasm……………….supraclavicular or infraclavicular lymphnodes………………………Arms and Hands:position……..deformities…………color………………….tenderness……………muscle strength………………. abnormal motions……………..joints: edema………… freedom of movements…….temperature…………moisture………..local swellings……….vessels ………….epitrochlear lymphnodes………fingers………….nails …………..reflexes………………..Breasts:size………contour……….tenderness…………….masses……….glandular consistency………nipples…………skin color……………texture……………retraction………..Axillae:skin……….hair……..lymphnodes……….Back:deformities………freedom of movements…….skin ……….swelling…….tenderness…………muscle spasm………..scapulae………..Thorax:shape……..respiratory movements……….swelling….pulsation……………Heart:apex impulse location…………character………..thrill…………..measurements: right border…….left border……….supracardiac dullness………..mid clavicular ilne………souds-rate…..rhythm………..intensity……..quality of murmurs………..pulses………..character……….condition of temporal, brachial, radial vessels……………….Lungs:resonance………..diaphragmatic excursion……………tactile fremitus……….. breath sounds………….whispered voic sounds……..spoken voice sounds……rales………..Abdomen:size………shape…….scars …………tension…….percussion note……………masses tenderness……….spasm………….pulsation……….umbilicus…….fluid wave………..shifting dullness………liver-dulness……….edge……..spleen ………….kidneys………..costovertebral tenderness………herniae ……………peristalsis: audible …..visible……bladder-dulness………..palpable distension……inguinal lymphnodes…..reflexes……Legs and Feet:Position…………deformities……….color……………..tenderness…………muscle strength………….abnormal motions………..freedom of movements….joints ……edema……..temperature…………moisture…………local swellings………ulcerations…………vessels…………arches……….toes..Nails…….reflexes……..clonus………Kerning…….Romberg…….Male Genitalia:Pubic hair………penis………..scrotum………testicles…….epididymis……….cords………………..Female Genitalia:pubic hair…..vulva……..vagina…….perineum……..cervix………..fundus…………..vaults…….Rectum:anal orifice….sphincter tone…..fissures…………hemorrhoids………..tenderness……………internal obstruction …..masses…….prostate…..tenderness….Other abnormal findings:…………Recapitulation of important variants:……….Impression…….Signature………………。
发热病历书写模板范文英文回答:Chief Complaint:The patient presents with a chief complaint of fever and chills for the past 5 days.History of Present Illness:The patient reports that the fever started suddenly and has been persistent, with temperatures ranging from 38.5°C to 39.5°C. The fever is associated with chills and sweating. There is no reported cough, sore throat, or runny nose. The patient denies any recent travel or exposure to sick contacts.Past Medical History:The patient has a past medical history of hypertensionand diabetes, which are well-controlled with medications. There is no history of similar episodes in the past.Medications:The patient is currently taking metformin for diabetes and amlodipine for hypertension.Allergies:The patient has no known drug allergies.Review of Systems:Apart from the fever and chills, the patient denies any other symptoms such as headache, body aches, nausea, vomiting, diarrhea, or urinary symptoms.Physical Examination:On examination, the patient appears ill and is febrile with a temperature of 39.2°C. There are no obvious sourcesof infection on initial examination, and the rest of the physical examination is unremarkable.Laboratory and Diagnostic Findings:Initial laboratory investigations reveal leukocytosis with a white blood cell count of 12,000/mm3 and a left shift. The rest of the complete blood count and metabolic panel are within normal limits. A chest X-ray is ordered to rule out pneumonia.Assessment and Plan:The patient is diagnosed with a febrile illness of unknown origin. Empiric antibiotic therapy is initiated while awaiting further diagnostic studies. The patient is advised to continue antipyretic medications and to follow up in 48 hours for reassessment.中文回答:主诉:患者主诉为发热和寒战,持续5天。
英语病历书写范文五年级以下是一个简化的英语病历书写范文,适用于五年级学生的理解水平:Patient Information (患者信息)Name: John SmithAge: 10 years oldGender: MaleDate of Visit: May 20, 2024Chief Complaint (主诉)John's mother reports that he has had a fever and sore throat for the past two days.History of Present Illness (现病史)John started feeling sick two days ago. He has had a fever, ranging from 38°C to 39°C. He also complains of a sore throat, making it difficult to swallow. He has been drinking plenty of fluids but has had little appetite.Past Medical History (既往病史)John has no known allergies and has been healthy in the past. He has had no surgeries or hospitalizations.Physical Examination (体格检查)General: John appears tired but alert. Temperature: 38.5°CThroat: Erythematous (red) and swollen, with tonsillar enlargement.Respiratory: No difficulty breathing.Abdomen: Soft, non-tender.Diagnosis (诊断)Acute pharyngitis (sore throat) with feverTreatment Plan (治疗计划)1.Prescribe antibiotics (for 5 days)2.Advise rest and plenty of fluids3.Check back in 2 daysPatient Education (患者教育)Explain to John's mother the importance of completing the antibiotic course as prescribed. Advise her to monitor John's temperature and report any worsening symptoms.Follow-up (随访)Schedule a follow-up visit for 2 days from today.请注意,这个病历是一个简化的版本,旨在帮助学生理解病历的基本结构和内容。
英文病历范文Title: English Medical Record Sample (Creating and Expanding on a Matching Content)Medical RecordNa John SmithDate of Birth: February 15, 1985Gender: MaleNationality: AmericanOccupation: AccountantChief Complaint:The patient presented with a complaint of persistent cough, shortness of breath, and chest pain for the past week.History of Present Illness:The symptoms initially started as a mild cough, which gradually worsened over the week. The patient also experienced shortness of breath, especially during physical activities. He reported occasional chest pain, which was sharp in nature and intensified during deep breaths. The patient denied any fever, night sweats, or weight loss.Past Medical History:The patient has a history of asthma since childhood and has been using an inhaler as needed. He had a similar episode ofpersistent cough and shortness of breath six months ago, which resolved with a course of oral steroids. No other significant medical history was reported.Social History:The patient is a non-smoker and denies any alcohol or illicit drug use. He lives with his wife and two children in a smoke-free environment. The patient works as an accountant and does not have any known occupational exposures.Family History:There is no significant family history of respiratory diseases or any chronic illnesses.Review of Systems:The review of systems was unremarkable except for the respiratory symptoms mentioned above.Physical Examination:On examination, the patient appeared to be in no acute distress. Vital signs were within normal limits. Auscultation of the lungs revealed mild wheezing bilaterally. Heart sounds were normal, and there were no signs of peripheral edema or cyanosis. Other systemic examinations were within normal limits.Investigations:Laboratory investigations, including complete blood count, liver and kidney function tests, and electrolyte levels, were all within normal range. Chest X-ray showed hyperinflation of lungs and no evidence of infiltrates or consolidation.Assessment and Plan:Based on the history, clinical findings, and investigations, the patient's symptoms and past medical history suggest asthma exacerbation. Initial management includes a trial of short-acting bronchodilators, oral corticosteroids, and close monitoring of symptoms. The patient was educated about proper inhaler technique and advised to follow up in one week for reassessment.Education and Counseling:The patient was counseled on the importance of adherence to the prescribed medication and the need to avoid triggers for asthma exacerbation, such as allergens and respiratory infections. He was also provided with a written asthma action plan for self-management and advised to seek medical attention if symptoms worsen or do not improve within a week.Follow-up:The patient will be scheduled for a follow-up visit in one week to reassess symptoms, evaluate response to treatment, andadjust the management plan accordingly.This medical record documents the patient's chief complaint, history of present illness, past medical history, social and family history, physical examination findings, investigations, diagnosis, and treatment plan. It serves as a comprehensive guide for healthcare professionals involved in the patient's care.。
四年级英语病历范文Patient Name: Zhang SanAge: 10 years oldDate of Visit: October 10th, 2023Chief Complaint:The patient complains of a sore throat, cough, and runny nose for the past three days.History of Present Illness:The patient's symptoms started three days ago with a sore throat, followed by a cough and runny nose. The cough is dry and persistent, and the patient has been experiencing some difficulty swallowing due to the sore throat. There is no history of fever, chills, or ear pain. The patient's appetite has decreased, and there is a mild decrease in energy levels.Past Medical History:The patient has a history of seasonal allergies, with symptoms of sneezing and itchy eyes during the spring andfall seasons. There is no history of asthma or other chronic respiratory conditions.Family History:There is no significant family history of respiratory illnesses or other chronic conditions.Medications:The patient is not currently taking any medications.Allergies:The patient has no known drug allergies.Review of Systems:- Constitutional: Decreased appetite and energy levels - Respiratory: Sore throat, cough, runny nose- Gastrointestinal: No nausea, vomiting, or diarrhea - Musculoskeletal: No joint pain or swellingPhysical Examination:- Vital Signs: Temperature 98.6°F, pulse 80 beats per minute, respiratory rate 20 breaths per minute, blood pressure 110/70 mmHg- General: The patient appears fatigued, but alert and oriented- Head and Neck: Erythematous pharynx, no tonsillar exudates, clear nasal discharge- Respiratory: Lungs clear to auscultation bilaterally - Cardiovascular: Regular rate and rhythm, no murmurs or gallops- Abdomen: Soft, non-tender, non-distendedAssessment:Based on the patient's history and physical examination, the likely diagnosis is an upper respiratory tract infection, possibly viral in nature.Plan:1. Symptomatic treatment for sore throat and cough, including acetaminophen for pain and discomfort2. Encourage increased fluid intake and rest3. Monitor for any signs of worsening symptoms, such as persistent high fever or difficulty breathing4. Follow up in three days if symptoms do not improve or worsen中文回答:患者张三,10岁,主诉三天来咽喉痛、咳嗽和流鼻涕。
Name: Aiyu SunAge: 37Gender: FemaleRace: the Han nationalityBirth Place: HongHu CityMarital Status: MarriedOccupation: FarmerAddress: Group Six, WeiGou Village, FengKou Town, HongHu City, Hubei Province Informant: Aiyu SunDate of admission: June 3 , 2010Date of history taken: June 3 , 2010Chief Complaint:Feeling hot, palpitation, polyphagia for four months, fever for five daysHistory of Present Illness:The patient felt hot, palpitation, polyphagia in Feburary, without obivious motivation. The symptoms appeared with shivering of hands and the head, irritability, exophthalmos of both eye balls gradually. The symptoms appeared without complaints of diarrhea, magersucht, hoarseness, blurred vision and so on. The patient did not go to receive any medical treatment. From April, the symptoms above became more severe, with powerless of limbs. The patient went to local hospital on 27th, April. Examination result: FT3>25pg/ml↑,FT4>8npg/dl↑,TSH<0.01uIU/ml↓;WBC 6.11*109/L, N 7.01*109/L; ALT 52u/L↑, AST 41u/L. The patient was diagnosed as “hyperthyroidism, cacergasia of liver”. The patient took Tapazole 5mg tid , propanolol, inosine,drugs for liver protection and WBC raising from then on. The symptoms described above was relieved after taking these medicines. On 12nd, May, the bood routine was still normal: WBC 5.8*109/L, N 3.1*109/L. But five days ago, without obivious motivation, the patient had a pharynx ache, fever, which was highest at 38.7°C,with headache and catarrhus. The patient was diagnosed as “upper respiratory infection, hyperthyroidism, agranulemia” and gave antiinfection therapy. But the fever continued, the therapy effect was not well. The patient comes to our hospital today. The blood routine today is WBC 0.15*109/L↓, N0*109/L↓↓↓, and the outpatient department receives the patient to our ward as“hyperthyroidism, agranulemia”.During the course of disease, sleep and psyche were acceptable. Polyphagia lasted. Stool and urine were as usual. Physical strength descended. Weight was stable.Past History:General Health Status: good √moderate poorInfectious Disease: √no yes(if any, please write down date of onset, brief diagnostic and therapeutic, course )Typhoid fever Dysentery Malaria Schistosomiasis Leptospirosis Tuberculosis Epidemic hemorrhagic fever othersAllergic history: √no yes (clinical manifestation: allergen: ) Trauma and/or operation history: √no yesReview of Symptoms:Respiratory system: √no yesRepeated pharyngeal pain:chronic cough: expectoration: Hemoptysis: asthma: dyspnea: chest pain:Circulatory system:√no yesPalpitation: exertional dyspnea: cyanosis: hemoptysis: Edema of lower extremities: chest pain: syncope: hypertension:Digestive system:√no yesAnorexia: dysphagia: sour regurgitation: eructation: nausea: Emesis: melena: abdominal pain: diarrhea: hematemesis: Hematochezia: jaundice:Urinary system:√no yesLumbar pain: urinary frequency: urinary urgency: dysuria: oliguria: Polyuria: retention of urine: incontinence of urine: hematuria: Pyuria: nocturia: puffy face:Hematopoietic system:√no yesFatigue: dizziness: gingival hemorrhage: epistaxis: subcutaneous hemorrhage:Metabolic and endocrine system:√no yesBulimia: anorexia: hot intolerance: hyperhidrosis: cold intolerance: Polydipsia: amenorrhea: tremor of hands: character change: Marked obesity: marked emaciation: hirsutism: alopecia: Hyperpigmentation: sexual function change: impotence: amenorrhea:Musculoskeletal system:√no yesMigrating arthralgia: arthralgia: artrcocele: arthremia: Dysarthrosis: myalgia: muscular atrophy:Neurological system:√no yesDizziness: headache: paresthesia: hypomnesis: Visual disturbance: Insomnia: somnolence: syncope: convulsion:Disturbance of consciousness: paralysis: vertigo:Personal history:Resident history in endemic disease area:√no yesSmoking: √no yes: about___yearsDrinking:√no occasional frequent: about____years average____ml/day Others:In April 2009, the patient was diagnosed as “polyp of vocal cord” in our hospital and got medicine thrapy.Menstrual history:Menarchal age: 21 years old duration__5__days/ interval_30_daysLast menstrual period: 2010.5.1 menopausal age: _13_years oldAmount of flow: small √moderate largedysmenorrheal: presence √absenceMarital and obstetrical history:Married age: 21 years old pregnancy_4__times natural labour: 3 timesAbortion: 2 times premature labour: 0 times still birth: 0 timesDystocia and its course:0Family history:(pay attention to the infectious and hereditary disease related to the present illness)Father: √healthy ill: deceased cause:Mother: √healthy ill: deceased cause:Others: noPhysical ExaminationGeneral conditions:Temperature: 37.3°C pulse:88 times per minute (√regular irregular)Blood pressure:139/84mmHg respiration: 20 times per minute (√regular irregular) Development: √normal HypoplasiaNutrition: good √moderate poor cachexiaFacial expression: √normal acute chronic other( )Posture: √active semi-reclining position other ( )Mental status:√clear confusion somnolence delirium comaGait: √normal abnormal cooperation: √yes noSkin and mucosa:Color:√normal pale cyanosis stained yellow pigmentationrash:√no yes: (type: distribution: )subcutaneous hemorrhage: √no yes (type: distribution: )Hair distribution: √normal hypertrichosis oligotrichosis alopecial(location: ) Temperature and moisture: √normal cold warm dry moist dehydrationEdema: √no yes ( location and degree )Liver palmar : √no yes spider angioma:√no yes (location: )Others: noLymph nodes:enlargement of superfacial lymph node: √no yes (location and description: ) Head: without abnormityCranium: without abnormityEye: exophthalmos: exophthalmos of both eye ballseyelid: without descensusconjunctiva: without edemasclera: without stained yellowCornea: √normal abnormal ( od os )Pupil:√equally round and equal in size: unequal (od os )Pupil reflex: √normal delayed (od os ) absent (od os ) others:Ear: discharge of external auditory canal:√normal (left right quality: ) Mastoid tenderness : no (left right )disturbance of rough hearing test: yes √noNose: flaring of alae nasi:√no yesstuffy discharge:√no yestenderness over paranasal sinuses: √no yes(location: )Mouth: lip: redMucosa: without ulcerationTongue: stretched tongue is in the middleGum: nomalTonsil: Ⅰ°enlargement of both sidesPharynx: congestionsound: √normal hoarseness teeth: √normal absent carieNeck:neck rigidity √no yes (distance between sternum and mandible: ______transvers fingers) Carotid artery: √normal pulsation increased pulsation marked distention Trachea:√middle deviation (leftward rightward )Hepatojugular vein reflux: negativeThyroid: normal √enlarged bruitChest:Chest wall: √normal barrel chest prominence or retraction: (left right ) Precordial prominence: √no yespercussion pain over sternum:√no yesBreast: normalLung:Inspection: normal respiratory movementPalpation:vocal tactile fremitus: normalpleural rubbing sensation: √no yesSubcutaneous crepitus sensation:√no yesPercussion: √resonanc dullness Flatness Hyperresonance tympanylower border of lung: (detailed percussion in respiratory disease)midclavicular line : right:_6__cm left:_6__cmmidaxillary line: right:_8__cm left:_8__cmscapular line: right:_10__cm left:_10__cmAuscultation: breathing sound :√normal abnormalRales: √no yes (moist dry ) location:Heart:Inspection:apical pulsation:√normal unseen increase diffuse sSubxiphoid pulsation: √no yesLocation of apex beat:√normal shift (distance away from left MCL___cm) Palpation:apical pulsation: √normal lifting apex impulse negative pulsationThrill:√no yes (location: ) phase:Percussion:relative dullness border:√Normal decreased absent increaseR(cm) line L(cm)2 Ⅱ 22 Ⅲ 43 Ⅳ 6Ⅴ8Distance between anterior median line and MCL 8.5cm Auscultation: heart rate: 88bpm rhythm: regularheart sound:√normal abnormalextra sound:√no S3 gallop S4 opening snap:murmur: √no yes:location timing quality intensity transmission:effects of position:effects of respiration:P2 = A2 pericardial friction sound:√no yesPeripheral vascular sign: √no yes: paradoxical pulse pulsus alternansWater hammer pulse capillary pulsationpulse deficit Pistol shot sound Duroziez sign Abdomen:Inspection: shape: √normal distention scaphoid frog-bellygastric pattern:√no yes visible intestinal peristalsis:√no yesabdominal vein varicose: √no yes (direction: )operation scar:√no yesPalpation: √soft guarding (location: )Tenderness: √no yes (location: )rebound tenderness:√no yes (location: )fluctuation succussion splash:√no yesliver: can’t be touch ed under the ribsgallbladder: can’t be touched under the ribsMurphy sign: negativespleen: can’t be touched under the ribskidneys: kidney zones without Percussion painabdominal mass :can’t be touchedPercussion: liver dullness border: √normal decreased absentUpper hepatic border locates at right midclavicular line5_intercostal spaceShift dullness: negativePain on percussion in costovertebral area:√no yes R L Auscultation: bowel sounds : √normal hyperperistalsis hypoperistalsis absence Vascular bruit :√no yes (location )Genital organ: √unexamined normal abnormalAnus and rectum:√unexamined normal abnormalSpine and extremities:Spine: √normal deformity (kyphosis lordosis scoliosis )Tenderness (location )Extremities: √normal arthremia(location ) arthrocele (location ) Ankylosis (location ) aropachy Muscular tenderness(location ) muscular atrophy (location )Neurological system:Abdominal reflex++ cremasteric reflex- knee reflex++Kernig`s sign(R- L- ) Brudzinski`s sign:(R- L- ) Babinski sign (R- L- )Opphenheim sign(R- L- )Gordon sign (R- L- ) Lasegue sign (R- L- ) Others: noImportant exam results from out-patient service: X-ray number:no27th, April, local hospital: F T3>25pg/ml↑,FT4>8npg/dl↑,TSH<0.01uIU/ml↓;WBC 6.11*109/L, N 7.01*109/L;ALT 52u/L↑, AST 41u/L.12nd, May, local hospital: Blood-rt: WBC 5.8*109/L, N 3.1*109/L3rd, June, our hospital: Blood-rt: WBC 0.15*109/L↓, N0*109/L↓↓↓Summary of case history:1 Patient Aiyu Sun, female, 37 years old.2 Chief Complaint: Feeling hot, palpitation, polyphagia for four months, fever for five days3 Past History: General health status was moderate. In April 2009, the patient was diagnosed as “polyp of vocal cord” in our hospital and got medicine thrapy. The patient deny history of TB, HBV, schistosome infection, DM, HBP, heart diseases and other special diseases. The patient deny history of allergy, trama, surgery operation and blood transfusion.4 Physical Examination: T37.3°C P88 times per minute BP:139/84mmHg R: 20 times per minute. Normal development, moderate nutrition, active posture, clear mental status, cooperated examination. There is no yellow stained in the skin and mucosa. There is no enlargement of superfacial lymph nodes. Head shape and cranium are normal. There is exophthalmos of both eye balls. Both tonsils are Ⅰ°enlarged. Pharynx is congestion. No neck rigidity. Trachea is in the middle. Thyroid of both sides is Ⅱ°enlarged, without vascular bruit. Breathing sound of the lung is normal. And there is no rale. Heart rhythm is regular, without any obvious murmur at each valve zone. Abdomen shape is normal. Abdomen is soft, without tenderness or rebound tenderness. Liver and spleen can’t be touched under the ribs. Kidney zones are without percussion pain. Both hands are shivering. There is no edema of both lower limbs.5 exam results:27th, April, local hospital: F T3>25pg/ml↑,FT4>8npg/dl↑,TSH<0.01uIU/ml↓;WBC 6.11*109/L,N 7.01*109/L; ALT 52u/L↑, AST 41u/L.12nd, May, local hospital: Blood-rt: WBC 5.8*109/L, N 3.1*109/L;3rd, June, our hospital: Blood-rt: WBC 0.15*109/L↓, N0*109/L↓↓↓Primary diagnosis:1 Hyperthyroidism2 Agranulemia:(1)Induced by drugs;(2)Hematopoietic system diseases?(such as aplastic anemia, MDS,leukemia etc.)3 Acute upper respiratory infection4 Other diseases which cause fever: such as other infections, connective tissue diseases etc.Corrected diagnosis (date 2010.6.4)1 Hyperthyroidism2 Agranulemia: Induced by drugs3 Acute upper respiratory infectionsignature:writer: Yanling LiangRevisor:。