兰索拉唑说明书
- 格式:docx
- 大小:32.59 KB
- 文档页数:3
兰索拉唑片(可意林)的说明书生活交际当中难免遇到吃喝聚会,因此一部分人的胃肠疾病也就接踵而至了。
目前治疗胃肠疾病最好的药物当属兰索拉唑片(可意林)了,它对于人体没有任何副作用,您可以放心使用。
针对胃肠疾病比较严重的患者,我们极力推荐您使用兰索拉唑片(可意林)进行治疗,其效果立竿见影。
【药品名称】通用名称:兰索拉唑片商品名称:兰索拉唑片(可意林)英文名称:Lansoprazole Tablets拼音全码:LanSuoLaZuoPian(KeYiLin)【主要成份】本品主要成份为兰索拉唑。
化学名:(+)-2[3—甲基—4—(2,2,2—三氟乙氧基)—2吡啶基]—1H—苯并咪唑。
【成份】分子式:C16H14F3N3O2S分子量:369.37【性状】该品为肠溶片,除去包衣后显白色或类白色。
【适应症/功能主治】胃溃疡、十二指肠溃疡、反流性食管炎、佐-艾(Zollinger-Ellison)综合征(胃泌素瘤)。
【规格型号】15mg*14s【用法用量】治疗胃溃疡和十二指肠溃疡,每日清晨口服1次,一次15~30mg。
或遵医嘱。
【不良反应】本品副作用轻微,主要表现为口干、头晕、恶心。
【禁忌】孕妇、哺乳期妇女忌用。
【注意事项】1、治疗过程中应注意观察,因长期使用的经验不足,暂不推荐用于维持治疗。
2、本品服用时请不要嚼碎,应整片用水吞服。
3、下列患者慎重用药。
(1)曾发生药物过敏症的患者。
(2)肝肾功能障碍的患者。
4、因本药会掩盖胃癌的症状,所以须先排除胃癌,方可给药。
【儿童用药】遵医嘱。
【老年患者用药】遵医嘱。
【孕妇及哺乳期妇女用药】孕妇、哺乳期妇女忌用。
【药物相互作用】如与其他药物同时使用可能会发生药物相互作用,详情请咨询医师或药师。
【药物过量】尚不明确。
【药理毒理】该品为新型的抑制胃酸分泌的药物,它作用于胃壁细胞的H+-K+-ATP酶,使壁细胞的H+不能转运到胃中去,以致胃液中胃酸量大为减少,临床上用于十二指肠溃疡、胃溃疡、反流性食管炎,佐-艾(Zollinger-Ellison)综合征(胃泌素瘤)的治疗,疗效显著,对幽门螺杆菌有抑制作用。
兰索拉唑肠溶胶囊(达克普隆)的说明
书
关于《兰索拉唑肠溶胶囊(达克普隆)的说明书》,是我们特意为大家整理的,希望对大家有所帮助。
饱一顿饿一顿的状况通常出現在工作中很忙的群体之中,平常吃饭没规律性是造成胃肠病症产生的关键原因。
日常生活大伙儿一定要培养按时吃饭的习惯性,不可以依据本身的爱好来饮食搭配。
现阶段发布了一种称为兰索拉唑肠溶胶囊(达克普隆)的肠胃药,它是一种天然中草药材做成的肠胃药,针对身体无毒性副作用,您能够安心使用。
生产药品名称疫苗
通用性名字:兰索拉唑肠溶胶囊
产品名称:兰索拉唑肠溶胶囊(达克普隆)
拼音字母全码:LanSuoLaZuoJiaoNang(DaKePuLong)
生产关键成分疫苗兰索拉唑。
化学名:(。
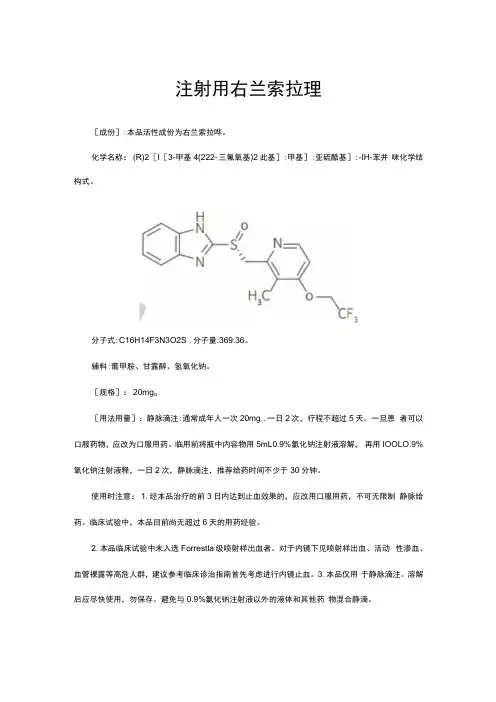
注射用右兰索拉理[成份]:本品活性成份为右兰索拉哗。
化学名称:(R)2[I[3-甲基4(222-三氟氧基)2此基]:甲基]:亚硫酷基]:-IH-苯并咪化学结构式。
分子式:C16H14F3N3O2S ,分子量:369.36。
辅料:葡甲胺、甘露醇、氢氧化钠。
[规格]:20mg o[用法用量]:静脉滴注:通常成年人一次20mg ,一日2次,疗程不超过5天。
一旦患者可以口服药物,应改为口服用药。
临用前将瓶中内容物用5mL0.9%氯化钠注射液溶解,再用IOOLO.9%氧化钠注射液释,一日2次,静脉滴注,推荐给药时间不少于30分钟。
使用时注意:1.经本品治疗的前3日内达到止血效果的,应改用口服用药,不可无限制静脉给药。
临床试验中,本品目前尚无超过6天的用药经验。
2.本品临床试验中未入选Forrestla级喷射样出血者。
对于内镜下见喷射样出血、活动性渗血、血管裸露等高危人群,建议参考临床诊治指南首先考虑进行内镜止血。
3.本品仅用于静脉滴注。
溶解后应尽快使用,勿保存。
避免与0.9%氯化钠注射液以外的液体和其他药物混合静滴。
4.使用本品时应使用专用的输液器,不得与其他药物共用。
万不得已需要通过其他药物的输液器侧管给予本品时应停止输注其他药物,并在本品给药之前和之后用0.9%氯化钠注射液冲管。
5.本品静消使用时应配有孔径为1.2um的过滤器,以便去除输液过程中可能产生的沉淀物。
这些沉淀物有可能引起小血管栓塞而产生严重后果。
[适应症]:用于口服疗法不适用的伴有出血的胃、十二指肠溃疡。
6禁忌症]:1.对本品中任何成份过敏的患者禁止使用本品。
2.正在使用硫酸阿扎那韦、盐酸利匹韦林的患者禁止使用本品。
[注意事项]:L以下患者慎重用药。
(1)有药物过敏症既往史的患者。
(2)肝功能障碍的患者(因本药的代谢、排泄延迟)。
2 .本品治疗可能会掩盖消化道肿瘤的症状,应排除恶性肿瘤后方可用药。
3 .本品治疗时密切观察病情,治疗无效时应改用其它疗法。
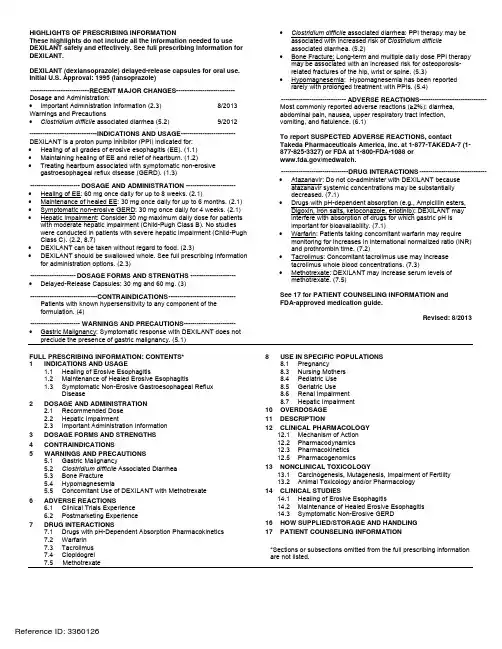
PRODUCT MONOGRAPHPr DEXILANT®Dexlansoprazoledelayed release capsules 30 mg and 60 mg H+, K+ - ATPase InhibitorTakeda Canada Inc. Oakville, Ontario, L6M 4X8 Date of Preparation: September 2, 2014Submission Control No: 176596Table of ContentsPART I: HEALTH PROFESSIONAL INFORMATION (3)SUMMARY PRODUCT INFORMATION (3)INDICATIONS AND CLINICAL USE (3)CONTRAINDICATIONS (3)WARNINGS AND PRECAUTIONS (4)ADVERSE REACTIONS (6)DRUG INTERACTIONS (9)DOSAGE AND ADMINISTRATION (11)OVERDOSAGE (12)ACTION AND CLINICAL PHARMACOLOGY (12)STORAGE AND STABILITY (16)DOSAGE FORMS, COMPOSITION AND PACKAGING (16)PART II: SCIENTIFIC INFORMATION (17)PHARMACEUTICAL INFORMATION (17)CLINICAL TRIALS (17)DETAILED PHARMACOLOGY (21)TOXICOLOGY (23)REFERENCES (26)PART III: CONSUMER INFORMATION (28)Pr DEXILANT®Dexlansoprazole delayed release capsules, 30 mg and 60 mgPART I: HEALTH PROFESSIONAL INFORMATION SUMMARY PRODUCT INFORMATIONINDICATIONS AND CLINICAL USEDEXILANT® is indicated for the following in adults 18 years of age and older:Healing of Erosive EsophagitisDEXILANT® is indicated for healing of all grades of erosive esophagitis for up to 8 weeks. Maintenance of Healed Erosive EsophagitisDEXILANT® is indicated for maintaining healing of erosive esophagitis for up to 6 months. Symptomatic Non-Erosive Gastroesophageal Reflux DiseaseDEXILANT® is indicated for the treatment of heartburn associated with symptomatic non-erosive gastroesophageal reflux disease (GERD) for 4 weeks.Geriatrics (> 65 years of age):No dosage adjustment is necessary for elderly patients.Pediatrics (< 18 years of age):Safety and effectiveness of DEXILANT® in pediatric patients have not been established. CONTRAINDICATIONSPatients who are hypersensitive to this drug or to any ingredient in the formulation. For a complete listing, see the DOSAGE FORMS, COMPOSITION AND PACKAGING. DEXILANT® should not be concomitantly administered with atazanavir (see DRUG INTERACTIONS, Drugs with pH-Dependent Absorption Pharmacokinetics).WARNINGS AND PRECAUTIONSGeneralSymptomatic response with DEXILANT® does not preclude the presence of gastric malignancy.Pseudomembranous colitis has been reported with nearly all antibacterial agents, including clarithromycin and amoxicillin, and may range in severity from mild to life threatening. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of antibacterial agents.Treatment with antibacterial agents alters the normal flora of the colon and may permit overgrowth of Clostridia. Studies indicate that a toxin produced by Clostridium difficile is a primary cause of “antibiotic-associated colitis”.After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to discontinuation of the drug alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation, and treatment with an antibacterial drug clinically effective against Clostridium difficile colitis.Decreased gastric acidity due to any means, including proton pump inhibitors, increases gastric counts of bacteria normally present in the gastrointestinal tract. Treatment with proton pump inhibitors (PPIs) may lead to slightly increased risk of gastrointestinal infections such as Salmonella and Campylobacter and possibly Clostridium difficile.Literature suggests that concomitant use of PPIs with methotrexate (primarily at high dose) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. A temporary withdrawal of the PPI may be considered in some patients receiving treatments with high dose methotrexate.Bone Fracture:Several published observational studies suggest that proton pump inhibitor (PPI) therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist, or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines (see DOSAGE AND ADMINISTRATION and ADVERSE REACTIONS). Carcinogenesis and MutagenesisDexlansoprazole was positive in the Ames test for mutagenicity in bacteria. In an in vitro chromosome aberration test using Chinese hamster lung cells, dexlansoprazole was considered positive based on equivocal data in which the percentage of cells with aberrant chromosomes increased slightly but did not reach the preset criteria for a positive response. Dexlansoprazole was negative in the in vivo mouse micronucleus test.Lansoprazole is a racemic mixture of R- and S-enantiomers. Following administration of lansoprazole in humans and animals, the major component circulating in plasma is dexlansoprazole, the R-enantiomer of lansoprazole. Therefore, the carcinogenic potential of dexlansoprazole was assessed using existing lansoprazole studies (see TOXICOLOGY). Lansoprazole treatment for 2-years was associated with hyperplasia and neoplasms (carcinoids) of enterochromaffin-like cells (ECL cells) in the stomach of conventional rats and mice. These proliferations are related to prolonged hypergastrinemia secondary to gastric acid suppression. Benign tumors of the testis (interstitial cell adenomas in rats and rete testis adenomas in mice) were secondary to an inhibitory effect on testosterone synthesis at high doses in these species. Hepatocellular adenomas and carcinomas were increased in the livers of mice related to induction of CYP enzymes leading to increased liver weights.Endocrine and MetabolismHypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically (see ADVERSE REACTIONS).The chronic use of PPIs may lead to hypomagnesaemia. Moreover, hypokalemia and hypocalcemia have been reported in the literature as accompanying electrolyte disorders. Cyanocobalamin (Vitamin B12) DeficiencyThe prolonged use of proton pump inhibitors may impair the absorption of protein-bound Vitamin B12 and may contribute to the development of cyanocobalamin (Vitamin B12) deficiency.GenitourinaryTesticular interstitial cell adenoma occurred in 1 of 30 rats treated with 50 mg/kg/day of lansoprazole (13 times the recommended human dose based on body surface area) in a one-year toxicity study (see TOXICOLOGY, Carcinogenicity).These changes are associated with endocrine alterations which have not been, to date, observed in humans.Special PopulationsPregnant Women:There are no adequate or well-controlled studies in pregnant women with DEXILANT®. Exposure in clinical trials was very limited. DEXILANT® should not be administered to pregnant women unless the expected benefits outweigh the potential risks. See TOXICOLOGY, Reproduction and Teratology.Nursing Women:It is not known whether dexlansoprazole is excreted in human milk. However, lansoprazole (the racemate) and its metabolites are excreted in the milk of rats. As many drugs are excreted in human milk, DEXILANT® should not be given to nursing mothers unless its use is considered essential.Pediatrics (< 18 years of age):Safety and effectiveness of DEXILANT® in pediatric patients have not been established. Geriatrics (> 65 years of age):In clinical studies of DEXILANT®, 11% of patients were aged 65 years and over. No overall differences in safety or effectiveness were observed between these patients and younger patients. No dosage adjustment is necessary for elderly patients. See ACTION AND CLINICAL PHARMACOLOGY, Special Populations and Conditions.Benefits of use of PPIs should be weighed against the increased risk of fractures as patients in this category (> 71 years of age) may already be at high risk for osteoporosis-related fractures. If the use of PPIs is required, they should be managed carefully according to established treatment guidelines (see DOSAGE AND ADMINISTRATION and ADVERSE REACTIONS) Hepatic Impairment:No dosage adjustment is necessary for patients with mild hepatic impairment (Child-Pugh Class A). A maximum daily dose of 30 mg should be considered for patients with moderate hepatic impairment (Child-Pugh Class B). No studies have been conducted in patients with severe hepatic impairment. See ACTION AND CLINICAL PHARMACOLOGY, Special Populations and Conditions.Renal ImpairmentNo dosage adjustment is necessary for patients with renal impairment. See ACTION AND CLINICAL PHARMACOLOGY, Special Populations and Conditions.ADVERSE REACTIONSClinical Trial Adverse Drug ReactionsBecause clinical trials are conducted under very specific conditions the adverse reaction rates observed in the clinical trials may not reflect the rates observed in practice and should not be compared to the rates in the clinical trials of another drug. Adverse drug reaction information from clinical trials is useful for identifying drug-related adverse events and for approximating rates.The safety of DEXILANT® was evaluated in 4548 patients in controlled and uncontrolled clinical studies (30 mg, 60 mg, and 90 mg), including 863 patients treated for at least 6 months and 282 patients treated for one year. Patients ranged in age from 18 to 90 years (median age 48 years), with 54% female, 85% Caucasian, 8% Black, 4% Asian and 3% other races. Six randomized controlled clinical trials were conducted for the treatment of erosive esophagitis, maintenance ofhealed erosive esophagitis, and symptomatic GERD, which included 896 patients on placebo, 2621 patients on DEXILANT® 30 mg or 60 mg and 1363 patients on lansoprazole 30 mg.The following adverse events were reported to have a possible or definite treatment-relationship to DEXILANT® in 1% or more of the treated patients in placebo and positive-controlled clinical trials (Tables 1 and 2, respectively). Numbers in parentheses indicate the percentage of the adverse events reported.In placebo-controlled studies, gastrointestinal adverse reactions other than constipation occurred at a higher incidence for DEXILANT® than placebo. In active-controlled studies, diarrhea occurred at a higher incidence for DEXILANT® than lansoprazole. The incidence of other common adverse reactions for DEXILANT® were similar to or lower than placebo or lansoprazole.Less Common Clinical Trial Adverse Drug Reactions(<1%)Other adverse reactions that were reported for DEXILANT® (30 mg, 60 mg or 90 mg) in controlled studies at an incidence of less than 1% are listed below by body system:Blood and Lymphatic System Disorders: anemia, lymphadenopathyCardiac Disorders: acute myocardial infarction, angina, arrhythmia, bradycardia, edema, palpitations, tachycardiaEar and Labyrinth Disorders: ear pain, tinnitus, vertigoEndocrine Disorders: goiterEye Disorders: eye irritation, eye swellingGastrointestinal Disorders: abdominal discomfort, abdominal tenderness, abnormal feces, anal discomfort, Barrett’s esophagus, bezoar, bowel sounds abnormal, breath odor, colitis microscopic, colonic polyp, dry mouth, duodenitis, dyspepsia, dysphagia, enteritis, eructation, esophagitis, gastric polyp, gastritis, gastroenteritis, gastrointestinal disorders, gastrointestinal hypermotility disorders, GERD, GI ulcers and perforation, hematemesis, hematochezia, hemorrhoids, impaired gastric emptying, irritable bowel syndrome, mucus stools, oral mucosal blistering, painful defecation, paresthesia oral, proctitis, rectal hemorrhage, vomitingGeneral Disorders and Administration Site Conditions: adverse drug reaction, asthenia, chest pain, chills, feeling abnormal, inflammation, mucosal inflammation, nodule, pain, pyrexia Hepatobiliary Disorders: biliary colic, cholelithiasis, hepatomegalyImmune System Disorders: hypersensitivityInfections and Infestations: candida infections, influenza, nasopharyngitis, oral herpes, pharyngitis, sinusitis, upper respiratory tract infection, viral infection, vulvo-vaginal infection Injury, Poisoning and Procedural Complications: overdose, procedural pain, sunburn Laboratory Investigations: ALP increased, ALT increased, AST increased, bilirubin decreased/increased, blood creatinine increased, blood gastrin increased, blood glucose increased, blood potassium increased, liver function test abnormal, platelet count decreased, total protein increased, weight increasedMetabolism and Nutrition Disorders: appetite changes, hypercalcemia, hypokalemia Musculoskeletal and Connective Tissue Disorders: arthralgia, arthritis, muscle cramps, musculoskeletal pain, myalgiaNervous System Disorders: altered taste, convulsion, dizziness, memory impairment, migraine, paresthesia, psychomotor hyperactivity, tremor, trigeminal neuralgiaPsychiatric Disorders: abnormal dreams, anxiety, depression, insomnia, libido changesRenal and Urinary Disorders: dysuria, micturition urgencyReproductive System and Breast Disorders: dysmenorrhea, dyspareunia, menorrhagia, menstrual disorderRespiratory, Thoracic and Mediastinal Disorders: aspiration, asthma, bronchitis, cough, dyspnoea, hiccups, hyperventilation, respiratory tract congestion, sore throatSkin and Subcutaneous Tissue Disorders: acne, dermatitis, erythema, pruritus, rash, skin lesion, urticariaVascular Disorders: deep vein thrombosis, hot flush, hypertensionAdditional adverse reactions that were reported for DEXILANT® (60 mg or 90 mg) in a long-term uncontrolled study included: anaphylaxis, auditory hallucination, B-cell lymphoma, bursitis, central obesity, cholecystitis acute, decreased hemoglobin, dehydration, diabetes mellitus, dysphonia, epistaxis, folliculitis, gout, herpes zoster, hyperglycemia, hyperlipidemia, hypothyroidism, increased neutrophils, MCHC decreased, neutropenia, oral soft tissue disorder, rectal tenesmus, restless legs syndrome, somnolence, thrombocythemia, tonsillitis.Post-Market Adverse Drug ReactionsAdverse reactions have been identified during post-marketing surveillance of DEXILANT®. As these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Blood and Lymphatic System Disorders: autoimmune hemolytic anemia, idiopathic thrombocytopenic purpuraEar and Labyrinth Disorders: deafnessEye Disorders: blurred visionGastrointestinal Disorders: oral edema, pancreatitisGeneral Disorders and Administration Site Conditions: facial edemaHepatobiliary Disorders: drug-induced hepatitisImmune System Disorders: anaphylactic shock (requiring emergency intervention), exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis (some fatal)Metabolism and Nutritional Disorders: hypomagnesemia, hyponatremiaMusculoskeletal and Connective Tissue: Osteoporosis and osteoporosis-related fractures Nervous System Disorders: cerebrovascular accident, transient ischaemic attackRenal and Urinary Disorders: acute renal failureRespiratory, Thoracic and Mediastinal Disorders: pharyngeal edema, throat tightnessSkin and Subcutaneous Tissue Disorders: generalized rash, leucocytoclastic vasculitis Withdrawal of long-term PPI therapy can lead to aggravation of acid related symptoms and may result in rebound acid hypersecretion.DRUG INTERACTIONSDrug-Drug InteractionsDrugs with pH-Dependent Absorption PharmacokineticsDEXILANT® causes inhibition of gastric acid secretion. DEXILANT® is likely to substantially decrease the systemic concentrations of the HIV protease inhibitor atazanavir, which is dependent upon the presence of gastric acid for absorption, and may result in a loss of therapeutic effect of atazanavir and the development of HIV resistance. Therefore, DEXILANT® should not be co-administered with atazanavir.It is theoretically possible that DEXILANT® may interfere with the absorption of other drugs where gastric pH is an important determinant of oral bioavailability (e.g., Ampicillin esters, digoxin, iron salts, ketoconazole).Cytochrome P 450 InteractionsDEXILANT® is metabolized, in part, by CYP2C19 and CYP3A4 (see ACTION AND CLINICAL PHARMACOLOGY, Metabolism).In vitro studies have shown that dexlansoprazole is not likely to inhibit CYP isoforms 1A1, 1A2, 2A6, 2B6, 2C8, 2C9, 2D6, 2E1 or 3A4. As such, no clinically relevant interactions with drugs metabolized by these CYP enzymes would be expected. Furthermore, in vivo studies showed that DEXILANT® did not have an impact on the pharmacokinetics of, coadministered phenytoin (CYP2C9 substrate) or theophylline (CYP1A2 substrate).1 The subjects’ CYP1A2 genotypes in the drug-drug interaction study with theophylline were not determined. Although in vitro studies indicated that DEXILANT® has the potential to inhibit CYP2C19 in vivo, an in vivo drug-drug interaction study in mainly CYP2C19 extensive and intermediate metabolizers has shown that DEXILANT® does not affect the pharmacokinetics of diazepam (CYP2C19 substrate). WarfarinIn a study of 20 healthy subjects, co-administration of DEXILANT® 90 mg once daily for 11 days with a single 25 mg oral dose of warfarin on day 6 did not result in any significant differences in the pharmacokinetics of warfarin or INR compared to administration of warfarin with placebo.1 However, there have been reports of increased INR and prothrombin time in patients receiving PPIs and warfarin concomitantly. Patients treated with PPIs and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time. Concomitant Use of Antacids with DEXILANT®No formal drug-drug interaction studies were conducted with DEXILANT® and antacids. Drug-drug interactions studies were performed with the racemate lansoprazole and antacids. Simultaneous administration of lansoprazole with aluminum and magnesium hydroxide or magaldrate results in lower peak plasma levels, but does not significantly reduce bioavailability. Antacids may be used concomitantly if required. In clinical trials, antacids were administered concomitantly with lansoprazole delayed-release capsules. In a single-dose crossover study when 30 mg of lansoprazole was administered concomitantly with one gram of sucralfate in healthy volunteers, absorption of lansoprazole was delayed and its bioavailability was reduced. The value of lansoprazole AUC was reduced by 17% and that for C max was reduced by 21%. In a similar study when 30 mg of lansoprazole was administered concomitantly with 2 grams of sucralfate, lansoprazole AUC and C max were reduced by 32% and 55%, respectively. When lansoprazole dosing occurred 30 minutes prior to sucralfate administration, C max was reduced by only 28% and there was no statistically significant difference in lansoprazole AUC. Therefore, lansoprazole should be administered at least 30 minutes prior to sucralfate. It would be expected that similar results would be seen with DEXILANT®.TheophyllineAlthough a study of the use of concomitant theophylline and dexlansoprazole did not reveal any changes in the pharmacokinetics or pharmacodynamics of theophylline, individual patients should monitor their theophylline level while taking the two drugs concomitantly.TacrolimusConcomitant administration of dexlansoprazole and tacrolimus may increase whole blood levels of tacrolimus, especially in transplant patients who are intermediate or poor metabolizers of CYP2C19.ClopidogrelConcomitant administration of dexlansoprazole and clopidogrel in healthy subjects had no clinically important effect on exposure to the active metabolite of clopidogrel or clopidogrel-induced platelet inhibition (see DETAILED PHARMACOLOGY).No dose adjustment of clopidogrel is necessary when administered with an approved dose of DEXILANT®. MethotrexateCase reports, published population pharmacokinetic studies, and retrospective analyses suggest that concomitant administration of PPIs and methotrexate (primarily at high dose) may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate. However, no formal drug interaction studies of methotrexate with PPIs have been conducted.Drug-Food InteractionsDEXILANT® can be taken without regard to food or timing of food (see ACTION AND CLINICAL PHARMACOLOGY).Drug-Herb InteractionsInteractions with herbal products have not been established.Drug-Laboratory TestsInteractions with laboratory tests have not been established.DOSAGE AND ADMINISTRATIONRecommended Dose and Dosage Adjustmentb Controlled studies did not extend beyond 6 months.No dosage adjustment for DEXILANT® is necessary for patients with mild hepatic impairment (Child-Pugh Class A). DEXILANT® 30 mg should be considered for patients with moderate hepatic impairment (Child-Pugh Class B). No studies have been conducted in patients with severe hepatic impairment (Child-Pugh Class C).No dosage adjustment is necessary for elderly patients or for patients with renal impairment. Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated.Missed DoseIf a capsule is missed at its usual time, it should be taken as soon as possible. But if it is too close to the time of the next dose, only the prescribed dose should be taken at the appointed time. A double dose should not be taken.AdministrationDEXILANT® can be taken without regard to food or the timing of food.DEXILANT® should be swallowed whole with plenty of water.•Alternatively, DEXILANT® capsules can be opened and administered as follows: Open capsule;Sprinkle intact granules on one tablespoon of applesauce;Swallow immediately. Granules should not be chewed.OVERDOSAGEThere have been no reports of significant overdose of DEXILANT®. Dexlansoprazole is not expected to be removed from the circulation by hemodialysis.ACTION AND CLINICAL PHARMACOLOGYMechanism of ActionDEXILANT® is a PPI that suppresses gastric acid secretion by specific inhibition of the (H+, K+)-ATPase in the gastric parietal cell. By acting specifically on the proton pump, DEXILANT®blocks the final step of acid production.PharmacodynamicsAntisecretory ActivityThe effects of DEXILANT® 60 mg (n = 20) or lansoprazole 30 mg (n = 23) once daily for five days on 24-hour intragastric pH were assessed in healthy subjects in a multiple-dose crossover study.2 The results are summarized in Table 3.Table 3:Effect on 24-Hour Intragastric pH on Day 5 After®* p value <0.05 versus lansoprazole.PharmacokineticsThe formulation of DEXILANT® utilizing Dual Delayed Release technology results in a dexlansoprazole plasma concentration-time profile with two distinct peaks; the first peak occurs 1 to 2 hours after administration, followed by a second peak within 4 to 5 hours (see Figure 1).2,3Figure 1: Mean Plasma Dexlansoprazole Concentration – Time Profile Following Oral Administration of 60 mg DEXILANT® or 30 mg Lansoprazole Once Daily forDexlansoprazole is eliminated with a half-life of approximately 1 to 2 hours in healthy subjects (see Table 4) and in patients with symptomatic GERD. No accumulation of dexlansoprazole occurs after multiple, once daily doses of DEXILANT® 30 mg or 60 mg.Table 4: Mean (CV %) Pharmacokinetic Parameters for Healthy®After oral administration of DEXILANT® 30 mg or 60 mg to healthy subjects , mean C max and AUC values of dexlansoprazole increased approximately dose proportionally (see Figure 2).Figure 2: Mean Plasma Dexlansoprazole Concentration –Time Profile Following Oral Administration of DEXILANT® on Day 5Distribution:Plasma protein binding of dexlansoprazole ranged from 96.1% to 98.8% in healthy subjects and was independent of concentration from 0.01 to 20 mcg/mL. The apparent volume of distribution (Vz/F) after multiple doses in symptomatic GERD patients was 40.3 L.Metabolism:Dexlansoprazole is extensively metabolized in the liver by oxidation, reduction, and subsequent formation of sulfate, glucuronide and glutathione conjugates to inactive metabolites. Oxidative metabolites are formed by the cytochrome P450 (CYP) enzyme system including hydroxylation mainly by CYP2C19, and oxidation to the sulfone by CYP3A4.CYP2C19 is a polymorphic liver enzyme which exhibits three phenotypes in the metabolism of CYP2C19 substrates; extensive metabolizers (*1/*1), intermediate metabolizers (*1/mutant) and poor metabolizers (mutant/mutant). Systemic exposure of dexlansoprazole is generally higher in intermediate and poor metabolizers. Dexlansoprazole is the major circulating component in plasma4, regardless of CYP2C19 metabolizer status. In CYP2C19 intermediate and extensive metabolizers, the major plasma metabolites are 5-hydroxy dexlansoprazole and its glucuronide conjugate, while in CYP2C19 poor metabolizers dexlansoprazole sulfone is the major plasma metabolite.Excretion:Following the administration of DEXILANT®, no unchanged dexlansoprazole is excreted in urine. Following the administration of [14C]dexlansoprazole to 6 healthy male subjects, approximately 50.7% (standard deviation (SD): 9.0%) of the administered radioactivity was excreted in urine and 47.6% (SD: 7.3%) in the feces. Apparent clearance (CL/F) in healthy subjects was 11.4 to 11.6 L/h, respectively, after 5-days of 30 or 60 mg once daily administration. Effect of Food:DEXILANT® can be taken without regard to food or the timing of food. In food-effect studies in healthy subjects receiving DEXILANT®, increases in C max ranged from 12% to 55% and increases in AUC ranged from 9% to 37% under various fed conditions compared to fasting. However, no relevant differences with regard to intragastric pH were observed.5 An additional study showed that administration of 60 mg DEXILANT® prior to consumption of breakfast, lunch, dinner or an evening snack did not have an effect on dexlansoprazole exposure, or a clinically relevant effect on 24-hour intragastric pH control.6Special Populations and ConditionsPediatrics:The pharmacokinetics of dexlansoprazole in patients under the age of 18 years have not been studied.Geriatrics:In a study of 12 male and 12 female healthy subjects who received a single oral dose of DEXILANT® 60 mg, the terminal elimination half-life of dexlansoprazole was statistically significantly longer in geriatric subjects compared to younger subjects (2.23 and 1.5 hours, respectively). In addition, dexlansoprazole exhibited higher systemic exposure (AUC) in geriatric subjects (34.5% higher) than younger subjects. These differences were not clinically relevant.No dosage adjustment is necessary in geriatric patients (see WARNINGS AND PRECAUTIONS and DOSAGE AND ADMINISTRATION).Gender:In a study of 12 male and 12 female healthy subjects who received a single oral dose of DEXILANT® 60 mg, females had higher systemic exposure (AUC) (42.8% higher) than males. No dosage adjustment is necessary in patients based on gender.。
注射用兰索拉唑配伍禁忌分析1. 兰索拉唑是什么?兰索拉唑是继奥美拉唑之后研发的第2代质子泵抑制剂,可特异性作用于胃壁细胞H+,K+-ATP酶,阻断壁细胞分泌H+,抑制胃酸分泌其结构特点是在侧链中导入氟元素的取代苯并咪唑化合物,使其生物利用度较奥美拉唑提高了30%以上,亲脂性也强于奥美拉唑因此,该药物在酸性条件下可迅速透过壁细胞膜转变为次磺酸和次磺酰衍生物而发挥药效,对幽门螺杆菌的抑菌活性比奥美拉唑提高了4倍。
兰索拉唑具有治愈率高减轻症状速度更快生物利用度高不良反应价格低等优点,临床广泛用于治疗十二指肠溃疡胃溃疡反流性食管炎及佐埃综合征等消化道疾病,其配伍稳定性已成为临床用药中存在的危险因素,有关报道数量逐年递增现对国内发表的文献进行收集整理,并分析产生配伍禁忌的可能原因,评价药品的安全性,为临床合理用药提供参考。
2. 兰索拉唑有何配伍禁忌?2.1 与抗菌药物的配伍禁忌头孢替安:将1g注射用盐酸头孢替安溶入250mL0.9%氯化钠注射液,取出10mL 注入无菌玻璃试管中,再将30mg注射用兰索拉唑溶入100mL0.9%氯化钠注射液,取出10mL加入同一试管中,发现试管中液体立即变浑浊,10min后产生乳白色絮状物,放置24h后,乳白色絮状物形成沉淀[3]头孢哌酮舒巴坦钠:用10mL 注射器抽取注射用兰索拉唑稀释液和头孢哌酮舒巴坦钠稀释液各5mL,注射器立即出现乳白色浑浊,静置5min,可出现白色絮状物,经震荡后仍不消失。
头孢哌酮钠舒巴坦钠:将注射用兰索拉唑稀释液和头孢哌酮钠舒巴坦钠稀释液等体积混合后,溶液出现乳白色浑浊,静置可出现白色絮状物,经振荡后仍不消失,表明两种药物存在配伍禁忌。
氨曲南:用10ml无菌注射器抽取5ml灭菌注射用水将注射用兰索拉唑30mg充分溶解取2ml,同样用10ml无菌注射器抽取5ml灭菌注射用水将注射用氨曲南0.5g充分溶解取2ml,分别注入同一支5ml的一次性无菌针筒内,即出现乳白色混浊液体,静置30min后为混浊液体内有白色颗粒实验说明注射用兰索拉唑与注射用氨曲南存在配伍禁忌,两者不能同时使用。
兰索拉唑肠溶片的说明书肠胃不好,生活就不会好,人们的生活总是跟吃分不开关系。
目前患上胃肠疾病的人群很多,正确选择药物就成了您治愈疾病的重要选择了。
兰索拉唑肠溶片是如今治疗胃肠疾病非常好的药物,在众多的胃肠药物当中当属疗效最好的。
那么关于兰索拉唑肠溶片的各种药性和服药原则您了解吗。
【药品名称】通用名称:兰索拉唑片商品名称:兰索拉唑肠溶片拼音全码:LanSuoLaZuoPian【主要成份】本品主要成份为兰索拉唑。
化学名:2-[[[3-甲基-4-(2,2,2-三氟乙氧基)-2-吡啶基]甲基]亚磺酰基]-1H -苯并咪唑。
分子式:C16H14F3N3O2S分子量:369.37【性状】白色肠溶片,除去肠溶衣后显白色或类白色。
【适应症/功能主治】胃溃疡、十二指肠溃疡、反流性食管炎、佐-艾(Zollinger-Ellison)综合征(胃泌素瘤)。
【规格型号】15mg*12s【用法用量】每日清晨口服1次,一次15~30mg,或遵医嘱。
【不良反应】副作用轻微,主要表现为口干、头晕、恶心。
【禁忌】孕妇、哺乳期妇女忌用。
【注意事项】曾发生药物过敏症的患者及肝机能障碍的患者应慎重用药。
【儿童用药】对小儿的安全性尚未被确立(由于在小儿的临床经验极少)。
【老年患者用药】老年患者的胃酸分泌能力和其他生理机能均会降低,故用药期间请注意观察。
【孕妇及哺乳期妇女用药】孕妇、哺乳期妇女忌用。
【药物相互作用】会延迟安定(diazepam)及苯妥英钠(phenytoin Sodium)的代谢与排泄,资料已被发表于类似药物奥美拉唑的报告中。
【药物过量】未进行该项实验且无可靠文献。
【药理毒理】该品为新型的抑制胃酸分泌的药物,它作用于胃壁细胞的H+-K+-ATP酶,使壁细胞的H+不能转运到胃中去,以致胃液中胃酸量大为减少,临床上用于十二指肠溃疡、胃溃疡、反流性食管炎,佐-艾(Zollinger-Ellison)综合征(胃泌素瘤)的治疗,疗效显著,对幽门螺杆菌有抑制作用。
兰索拉唑片(泰左欣)的说明书
肠胃的重要性是不言而喻的,中国古代人对于肠胃的养生保健是非常重视的,只有大便通畅,脾胃安宁,才能更好的预防其他疾病,肠胃是为我们人类提供能量的重要场所。
如今推出了一种叫做兰索拉唑片(泰左欣)的肠胃药,它能有效治愈您的肠胃疾病,还能起到一定的预防保健作用。
【药品名称】
通用名称:兰索拉唑片
商品名称:兰索拉唑片(泰左欣)
【适应症/功能主治】胃溃疡、十二指肠溃疡、反流性食管炎、佐-艾(Zollinger-Ellison)综合征(胃泌素瘤)。
【规格型号】30mg*7s
【用法用量】治疗胃溃疡和十二指肠溃疡,每日清晨口服1次,一次15~30mg。
或遵医嘱。
【有效期】0 月
【批准文号】国药准字H20113166
【生产企业】南京海辰药业股份有限公司
综上所述,您对于兰索拉唑片(泰左欣)这种肠胃药有了一个全面的了解了吗?治疗肠胃疾病我们一定不能盲目用药,只有选择科学正规的药物,并且遵循医生的用药原则才能很好的治愈您的疾病,切勿讳疾忌医。
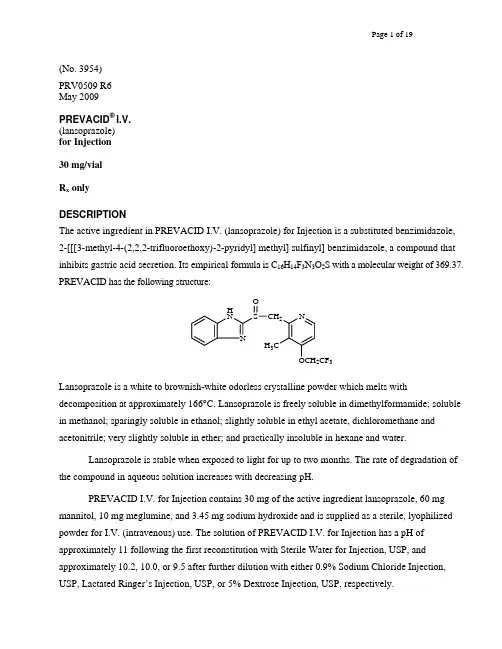
O N H NS CH 2 N H 3C2CF 3 (No. 3954)PRV0509 R6May 2009PREVACID ® I.V.(lansoprazole)for Injection30 mg/vialR x onlyDESCRIPTIONThe active ingredient in PREVACID I.V. (lansoprazole) for Injection is a substituted benzimidazole, 2-[[[3-methyl-4-(2,2,2-trifluoroethoxy)-2-pyridyl] methyl] sulfinyl] benzimidazole, a compound that inhibits gastric acid secretion. Its empirical formula is C 16H 14F 3N 3O 2S with a molecular weight of 369.37. PREVACID has the following structure:Lansoprazole is a white to brownish-white odorless crystalline powder which melts withdecomposition at approximately 166°C. Lansoprazole is freely soluble in dimethylformamide; soluble in methanol; sparingly soluble in ethanol; slightly soluble in ethyl acetate, dichloromethane and acetonitrile; very slightly soluble in ether; and practically insoluble in hexane and water.Lansoprazole is stable when exposed to light for up to two months. The rate of degradation of the compound in aqueous solution increases with decreasing pH.PREVACID I.V. for Injection contains 30 mg of the active ingredient lansoprazole, 60 mgmannitol, 10 mg meglumine, and 3.45 mg sodium hydroxide and is supplied as a sterile, lyophilized powder for I.V. (intravenous) use. The solution of PREVACID I.V. for Injection has a pH ofapproximately 11 following the first reconstitution with Sterile Water for Injection, USP, andapproximately 10.2, 10.0, or 9.5 after further dilution with either 0.9% Sodium Chloride Injection, USP, Lactated Ringer’s Injection, USP, or 5% Dextrose Injection, USP, respectively.CLINICAL PHARMACOLOGYPharmacokinetics and MetabolismFollowing the administration of 30 mg of lansoprazole by intravenous infusion over 30 minutes to healthy subjects, plasma concentrations of lansoprazole declined exponentially with a mean (+ standard deviation) terminal elimination half-life of 1.3 (± 0.5) hours. The mean peak plasma concentration of lansoprazole (C max) was 1705 (± 292) ng/mL and the mean area under the plasma concentration versus time curve (AUC) was 3192 (± 1745) ng⋅h/mL. The absolute bioavailability of lansoprazole following oral administration is over 80%, and C max and AUC of lansoprazole are approximately proportional in doses from 15 mg to 60 mg after single oral administration. The pharmacokinetics of lansoprazole did not change with time after 7-day once daily repeated oral or intravenous administration of 30 mg lansoprazole.DistributionThe apparent volume of distribution of lansoprazole is approximately 15.7 (± 1.9) L, distributing mainly in extracellular fluid. Lansoprazole is 97% bound to plasma proteins. Plasma protein binding is constant over the concentration range of 0.05 to 5.0 µg/mL.MetabolismLansoprazole is extensively metabolized in the liver. Two metabolites have been identified in measurable quantities in plasma (the hydroxylated sulfinyl and sulfone derivatives of lansoprazole). These metabolites have very little or no antisecretory activity. Lansoprazole is thought to be transformed into two active species which inhibit acid secretion by blocking the proton pump [(H+,K+)-ATPase enzyme system] at the secretory surface of the gastric parietal cell. The two active species are not present in the systemic circulation. The plasma elimination half-life of lansoprazole is less than 2 hours while the acid inhibitory effect lasts more than 24 hours. Therefore, the plasma elimination half-life of lansoprazole does not reflect its duration of suppression of gastric acid secretion. EliminationFollowing an intravenous dose of lansoprazole, the mean clearance was 11.1 (± 3.8) L/h. Following single-dose oral administration of lansoprazole, virtually no unchanged lansoprazole was excreted in the urine. In one study, after a single oral dose of 14C-lansoprazole, approximately one-third of the administered radiation was excreted in the urine and two-thirds was recovered in the feces. This implies a significant biliary excretion of the lansoprazole metabolites.Special PopulationsGeriatric UseFollowing oral administration, the clearance of lansoprazole is decreased in the elderly, with elimination half-life increased approximately 50% to 100%. Because the mean half-life in the elderly remains between 1.9 to 2.9 hours, repeated once daily dosing does not result in accumulation of lansoprazole. Peak plasma levels were not increased in the elderly. No intravenous dosage adjustment is needed.Pediatric UseThe pharmacokinetics of intravenous lansoprazole have not been studied in pediatric patients. For further information, please see the PREVACID package insert for the oral formulations.GenderThe pharmacokinetic data of intravenous lansoprazole in females is limited; however, in a study with oral lansoprazole comparing 12 male and 6 female human subjects who received lansoprazole, no gender differences were found in pharmacokinetics and intragastric pH results. No intravenous dosage adjustment is needed (also refer to Use in Women).Renal InsufficiencyIn patients with severe renal insufficiency, plasma protein binding decreased by 1.0%-1.5% after oral administration of 60 mg of lansoprazole. Patients with renal insufficiency had a shortened elimination half-life and decreased total AUC (free and bound). The AUC for free lansoprazole in plasma, however, was not related to the degree of renal impairment; and the C max and T max (time to reach the maximum concentration) were not different than the C max and T max from subjects with normal renal function. No intravenous dosage adjustment is necessary in patients with renal insufficiency. Hepatic InsufficiencyIn patients with various degrees of chronic hepatic disease, the mean plasma half-life of lansoprazole was prolonged from 1.5 hours to 3.2-7.2 hours after oral administration. An increase in the mean AUC of up to 500% was observed at steady state in hepatically-impaired patients compared to healthy subjects. Intravenous dose reduction in patients with severe hepatic disease should be considered. RaceThe pooled mean pharmacokinetic parameters of orally administered lansoprazole from twelve U.S. Phase 1 studies (N=513) were compared to the mean pharmacokinetic parameters from two Asianstudies (N=20). The mean AUCs of lansoprazole in Asian subjects were approximately twice those seen in pooled U.S. data; however, the inter-individual variability was high. The C max values were comparable. Information for intravenous dosing is not available.PharmacodynamicsMechanism of ActionPREVACID (lansoprazole) belongs to a class of antisecretory compounds, the substituted benzimidazoles, that suppress gastric acid secretion by specific inhibition of the (H+, K+) -ATPase enzyme system at the secretory surface of the gastric parietal cell. Because this enzyme system is regarded as the acid (proton) pump within the parietal cell, lansoprazole has been characterized as a gastric acid-pump inhibitor, in that it blocks the final step of acid production. This effect is dose-related and leads to inhibition of both basal and stimulated gastric acid secretion for at least 24 hours irrespective of the stimulus. Lansoprazole does not exhibit anticholinergic or histamine type-2 antagonist activity.Antisecretory ActivityAcid OutputAn open-label, single-center, two period study was conducted to evaluate the pharmacodynamics of 30 mg of intravenous lansoprazole and 30 mg of oral lansoprazole in 29 healthy subjects. The primary pharmacodynamic endpoints were pentagastrin stimulated maximum acid output (MAO) and basal acid output (BAO). Subjects received oral lansoprazole for 7 days in Period 1 and then were immediately switched to intravenous lansoprazole for 7 days in Period 2. MAO and BAO were measured at baseline and 21 hours following the last oral dose and the last intravenous dose of lansoprazole. This study demonstrated that 7 days of oral lansoprazole followed by 7 days of intravenous lansoprazole administration significantly suppressed gastric acid output as compared with baseline. Seven days of 30 mg of intravenous lansoprazole was equivalent to 30 mg of oral lansoprazole in the ability to maintain gastric acid output suppression (Table 1).Table 1: Acid Output (mEq/hr)PREVACID 30 mgBaseline After 7 Days ofOral Dosing After 7 Days of I.V. DosingMaximum Acid Output (Median) 11.26n=27 4.76*n=285.13*n=28Basal Acid Output (Median) 1.42n=28 0.42*n=280.27*n=28* Significantly (p ≤ 0.05) less acid output as compared to baseline.24-Hour Intragastric pHA multiple-dose study was conducted in 36 healthy subjects comparing the pharmacokinetics and pharmacodynamics of lansoprazole after intravenous administration and oral administration. During the first-hour post-dosing interval, intravenous lansoprazole resulted in significantly higher mean intragastric pH than did oral lansoprazole. There were no statistically significant differences between oral and intravenous regimens in 24-hour mean intragastric pH for the percentage of time that the intragastric pH was above 3 and 4 after 1-day or 5-day once daily repeated administration of 30 mg lansoprazole. Gastric acid suppression was maintained throughout each treatment period. The pharmacodynamic results are summarized in Table 2.Table 2: Mean Antisecretory Effects after Single and Multiple Daily DosingParameter BaselineValuePREVACID30 mg daily Orallyx 5 days30 mg I.V. Infusion daily x5 DaysDay 1 Day 5 Day 1 Day 5Mean 24-Hour pH Mean first hour pH % Time Gastric pH>3 % Time Gastric pH>4 3.334.4445.2731.074.752.7474.0867.185.254.7983.9277.614.864.64*78.3670.515.365.91*85.5479.68*Significantly (p≤ 0.05) higher than the oral lansoprazoleRefer to CLINICAL PHARMACOLOGY for pharmacokinetic results.Enterochromaffin-like (ECL) Cell EffectsDuring lifetime exposure of rats with up to 150 mg/kg/day of lansoprazole dosed orally seven days per week, marked hypergastrinemia was observed followed by ECL cell proliferation and formation of carcinoid tumors, especially in female rats (refer to PRECAUTIONS, Carcinogenesis, Mutagenesis, Impairment of Fertility).Gastric biopsy specimens from the body of the stomach from approximately 150 patients treated continuously with lansoprazole for at least one year did not show evidence of ECL cell effects similar to those seen in rat studies. Longer term data are needed to rule out the possibility of an increased risk of the development of gastric tumors in patients receiving long-term therapy with lansoprazole. Other Gastric Effects In HumansLansoprazole did not significantly affect mucosal blood flow in the fundus of the stomach. Due to the normal physiologic effect caused by the inhibition of gastric acid secretion, a decrease of about 17% in blood flow in the antrum, pylorus, and duodenal bulb was seen. Lansoprazole significantly slowed the gastric emptying of digestible solids. Lansoprazole increased serum pepsinogen levels and decreased pepsin activity under basal conditions and in response to meal stimulation or insulin injection. As with other agents that elevate intragastric pH, increases in gastric pH were associated with increases in nitrate-reducing bacteria and elevation of nitrite concentration in gastric juice in patients with gastric ulcer. No significant increase in nitrosamine concentrations was observed.Serum Gastrin EffectsIn over 2,100 patients, median fasting serum gastrin levels increased 50% to 100% from baseline but remained within normal range after treatment with 15 to 60 mg of oral lansoprazole. These elevations reached a plateau within two months of therapy and returned to pretreatment levels within four weeks after discontinuation of therapy.Endocrine EffectsHuman studies for up to one year have not detected any clinically significant effects on the endocrine system. Hormones studied include testosterone, luteinizing hormone (LH), follicle stimulating hormone (FSH), sex hormone binding globulin (SHBG), dehydroepiandrosterone sulfate (DHEA-S), prolactin, cortisol, estradiol, insulin, aldosterone, parathormone, glucagon, thyroid stimulating hormone (TSH), triiodothyronine (T3), thyroxine (T4), and somatotropic hormone (STH). Lansoprazole in oral doses of 15 to 60 mg for up to one year had no clinically significant effect on sexual function. In addition, lansoprazole in oral doses of 15 to 60 mg for two to eight weeks had no clinically significant effect on thyroid function.In 24-month carcinogenicity studies in Sprague-Dawley rats with daily lansoprazole dosages up to 150 mg/kg, proliferative changes in the Leydig cells of the testes, including benign neoplasm, were increased compared to control rates; these findings are rat specific.Other EffectsNo systemic effects of lansoprazole on the central nervous system, lymphoid, hematopoietic, renal, hepatic, cardiovascular or respiratory systems have been found in humans. Among 56 patients who had extensive baseline eye evaluations, no visual toxicity was observed after lansoprazole treatment (up to 180 mg/day) for up to 58 months.After lifetime lansoprazole exposure in rats, focal pancreatic atrophy, diffuse lymphoid hyperplasia in the thymus and spontaneous retinal atrophy were seen.CLINICAL STUDIESErosive EsophagitisA multicenter, double-blind, two-period placebo-controlled, pharmacodynamic study was conductedto assess the ability of PREVACID I.V. for Injection to maintain gastric acid suppression in patients switched from the oral dosage form of lansoprazole to the intravenous dosage form. Erosive esophagitis patients (n=87; 18 to 78 years of age; 28 female; 69 Caucasian/non-Hispanic, 14 Hispanic, 3 African-American, and 1 Native American) received 30 mg of oral lansoprazole for 7 days in Period 1. Patients were then immediately switched to receive either 30 mg of intravenous lansoprazole or intravenous placebo (normal saline) for 7 days in Period 2. MAO and BAO were determined 21 hours following the last dose of oral medication and the last dose of intravenous administration. MAO was calculated from two hours of continuous collection of gastric contents following a subcutaneous injection of 6.0 μg/kg of pentagastrin. BAO was calculated from one hour of continuous collection of gastric contents.This study demonstrated that, after seven days of repeated oral administration followed by 7 days of intravenous administration, the oral and intravenous dosage forms of PREVACID were similar in their ability to suppress MAO and BAO in patients with erosive esophagitis (refer to Table 3). Also, patients receiving oral PREVACID, who were switched to intravenous placebo, experienced a significant increase in acid output within 48 hours of their last oral dose.Table 3: Acid Output (mEq/h) in Erosive Esophagitis PatientsPREVACID Oral PREVACID I.V. Placebo I.V.(last oral dose) (last I.V. dose) (last I.V. dose)Maximum Acid Output (Median) 7.16n=807.64n=5626.90**n=17Basal Acid Output (Median) 0.77n=810.51n=553.19*n=16*, ** Significantly different from PREVACID I.V. at p=0.005 and p<0.001 levels, respectivelyINDICATIONS AND USAGEWhen patients are unable to take the oral formulations, PREVACID I.V. for Injection is indicated as an alternative for the short-term treatment (up to 7 days) of all grades of erosive esophagitis. Once the patient is able to take medications orally, therapy can be switched to an oral formulation of PREVACID for a total of 6 to 8 weeks. The safety and efficacy of PREVACID I.V. for Injection as an initial treatment of erosive esophagitis have not been demonstrated. Refer to full prescribing information for the oral formulations of PREVACID.CONTRAINDICATIONSPREVACID I.V. for Injection is contraindicated in patients with known severe hypersensitivity to any component of the formulation.PRECAUTIONSGeneralSymptomatic response to therapy with lansoprazole does not preclude the presence of gastric malignancy.Treatment with PREVACID I.V. for Injection should be discontinued as soon as the patient is able to resume treatment with PREVACID oral formulations.Drug InteractionsLansoprazole is metabolized through the cytochrome P450 system, specifically through the CYP3A and CYP2C19 isozymes. Studies have shown that lansoprazole does not have clinically significant interactions with other drugs metabolized by the cytochrome P450 system, such as warfarin, antipyrine, indomethacin, ibuprofen, phenytoin, propranolol, prednisone, diazepam, or clarithromycin in healthy subjects. These compounds are metabolized through various cytochrome P450 isozymes including CYP1A2, CYP2C9, CYP2C19, CYP2D6, and CYP3A. When lansoprazole was administered concomitantly with theophylline (CYP1A2, CYP3A), a minor increase (10%) in the clearance of theophylline was seen. Because of the small magnitude and the direction of the effect on theophylline clearance, this interaction is unlikely to be of clinical concern. Nonetheless, individual patients may require additional titration of their theophylline dosage when lansoprazole is started or stopped to ensure clinically effective blood levels.In a study of healthy subjects neither the pharmacokinetics of warfarin enantiomers nor prothrombin time were affected following single or multiple 60 mg doses of lansoprazole. However, there have been reports of increased International Normalized Ratio (INR) and prothrombin time in patients receiving proton pump inhibitors, including lansoprazole, and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with proton pump inhibitors and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time.Concomitant administration of lansoprazole and tacrolimus may increase whole blood levels of tacrolimus, especially in transplant patients who are intermediate or poor metabolizers of CYP2C19.Lansoprazole causes a profound and long-lasting inhibition of gastric acid secretion; therefore, it is theoretically possible that lansoprazole may interfere with the absorption of drugs where gastric pH is an important determinant of bioavailability (eg, ketoconazole, ampicillin esters, iron salts, digoxin). Carcinogenesis, Mutagenesis, Impairment of FertilityIn two 24-month carcinogenicity studies, Sprague-Dawley rats were treated with oral lansoprazole doses of 5 to 150 mg/kg/day - about 1 to 40 times the exposure on a body surface (mg/m2) basis of a 50-kg person of average height [1.46 m2 body surface area (BSA)] given the recommended human dose of 30 mg/day. Lansoprazole produced dose-related gastric enterochromaffin-like (ECL) cell hyperplasia and ECL cell carcinoids in both male and female rats. It also increased the incidence of intestinal metaplasia of the gastric epithelium in both sexes. In male rats, lansoprazole produced a dose-related increase of testicular interstitial cell adenomas. The incidence of these adenomas in rats receiving doses of 15 to 150 mg/kg/day (4 to 40 times the recommended human dose based on BSA) exceeded the low background incidence (range = 1.4 to 10%) for this strain of rat.In a 24-month carcinogenicity study, CD-1 mice were treated orally with doses of 15 to600 mg/kg/day, 2 to 80 times the recommended human dose based on BSA. Lansoprazole produced a dose-related increased incidence of gastric ECL cell hyperplasia. It also produced an increased incidence of liver tumors (hepatocellular adenoma plus carcinoma). The tumor incidences in male mice treated with 300 and 600 mg/kg/day (40 to 80 times the recommended human dose based on BSA) and female mice treated with 150 to 600 mg/kg/day (20 to 80 times the recommended human dose based on BSA) exceeded the ranges of background incidences in historical controls for this strainof mice. Lansoprazole treatment produced adenoma of rete testis in male mice receiving 75 to600 mg/kg/day (10 to 80 times the recommended human dose based on BSA).A 26-week p53 (+/-) transgenic mouse carcinogenicity study was not positive.Lansoprazole was not genotoxic in the Ames test, the ex vivo rat hepatocyte unscheduled DNA synthesis (UDS) test, the in vivo mouse micronucleus test, or the rat bone marrow cell chromosomal aberration test. It was positive in in vitro human lymphocyte chromosomal aberration assays.Lansoprazole at intravenous doses of up to 30 mg/kg/day (approximately 8 times the recommended human dose based on BSA) was found to have no effect on fertility and reproductive performance in male and female rats.Pregnancy: Teratogenic EffectsPregnancy Category BTeratology studies have been conducted in rats and rabbits using intravenous lansoprazole doses of up to 30 mg/kg/day (approximately 8 times in rats and 16 times in rabbits of the recommended human dose based on BSA). Treatment with lansoprazole did not result in any impairment of fertility or harm to the fetus.However, there are no adequate and well-controlled studies in pregnant women using the intravenous route. Because animal reproduction studies are not always predicative of human response, PREVACID I.V. for Injection should be used during pregnancy only if clearly needed.Nursing MothersLansoprazole or its metabolites are excreted in the milk of rats. It is not known whether lansoprazole is excreted in human milk. Because many drugs are excreted in human milk, because of the potential for serious adverse reactions in nursing infants from lansoprazole, and because of the potential for tumorigenicity shown for lansoprazole in rodent carcinogenicity studies, a decision should be made whether to discontinue nursing or to discontinue PREVACID I.V. for Injection, taking into accountthe importance of PREVACID I.V. for Injection to the mother.Pediatric UseThe safety and effectiveness of PREVACID I.V. for Injection have not been established for pediatric patients. For further information, please see the PREVACID package insert for the oral formulations.Use in WomenAmong intravenous PREVACID treated subjects, similar percentages of adverse events were reported in males and females.Over 4,000 women were treated with oral PREVACID. Ulcer healing rates in females were similar to those in males. The incidence rates of adverse events in females were also similar to those seen in males.Use in Geriatric PatientsData in elderly patients administered intravenous lansoprazole is limited; however, with oral lansoprazole, ulcer healing rates in elderly patients are similar to those in a younger age group. The incidence rates of PREVACID-associated adverse events and laboratory test abnormalities are similar to those seen in younger patients. For geriatric patients, dosage and administration of PREVACID need not be altered for a particular indication.ADVERSE REACTIONSClinical Safety Experience with PREVACID I.V. for InjectionMore than 1,000 patients and subjects have participated in domestic and foreign clinical trials. Treatment with PREVACID I.V. for Injection was well-tolerated.In four U.S. trials involving 161 subjects exposed to PREVACID I.V. for Injection, the following treatment-related adverse events were reported in >1% of subjects: headache (1.0%), injection site pain (1.0%), injection site reaction (1.0%) and nausea (1.3%). Treatment-related adverse events occurring in less than 1% of subjects included abdominal pain, vasodilatation, diarrhea, dyspepsia, vomiting, dizziness, paresthesia, rash, and taste perversion. No additional adverse drug reactions were reported with the intravenous formulation that had not been reported previously with the oral formulations.Clinical Safety Experience with Oral Formulations of PREVACIDWorldwide, over 10,000 patients have been treated with oral PREVACID in Phase 2 or Phase3 clinical trials involving various dosages and durations of treatment. In general, PREVACID treatment has been well-tolerated in both short-term and long-term trials.The following adverse events were reported by the treating physician to have a possible or probable relationship to drug in 1% or more of PREVACID-treated patients and occurred at a greater rate in PREVACID-treated patients than placebo-treated patients in Table 4.Table 4: Incidence of Possibly or Probably Treatment-Related Adverse Events in Short-Term,Placebo-Controlled PREVACID StudiesBody System/Adverse Event PREVACIDOral(N= 2768)%Placebo(N= 1023)%Body as a WholeAbdominal Pain Digestive SystemConstipation DiarrheaNausea 2.11.03.81.31.20.42.31.2Headache was also seen at greater than 1% incidence but was more common on placebo. The incidence of diarrhea was similar between patients who received placebo and patients who received 15 mg and 30 mg of PREVACID, but higher in the patients who received 60 mg of PREVACID (2.9%, 1.4%, 4.2%, and 7.4%, respectively).Additional adverse experiences occurring in less than 1% of patients or subjects who received PREVACID in domestic trials are shown below:Body as a Whole - abdomen enlarged, allergic reaction, asthenia, back pain, candidiasis, carcinoma, chest pain (not otherwise specified), chills, edema, fever, flu syndrome, halitosis, infection (not otherwise specified), malaise, neck pain, neck rigidity, pain, pelvic pain; Cardiovascular System - angina, arrhythmia, bradycardia, cerebrovascular accident/cerebral infarction, hypertension/ hypotension, migraine, myocardial infarction, palpitations, shock (circulatory failure), syncope, tachycardia, vasodilation; Digestive System - abnormal stools, anorexia, bezoar, cardiospasm, cholelithiasis, colitis, dry mouth, dyspepsia, dysphagia, enteritis, eructation, esophageal stenosis, esophageal ulcer, esophagitis, fecal discoloration, flatulence, gastric nodules/fundic gland polyps, gastritis, gastroenteritis, gastrointestinal anomaly, gastrointestinal disorder, gastrointestinal hemorrhage, glossitis, gum hemorrhage, hematemesis, increased appetite, increased salivation, melena, mouth ulceration, nausea and vomiting, nausea and vomiting and diarrhea, gastrointestinal moniliasis, rectal disorder, rectal hemorrhage, stomatitis, tenesmus, thirst, tongue disorder, ulcerative colitis, ulcerative stomatitis; Endocrine System - diabetes mellitus, goiter, hypothyroidism; Hemic and Lymphatic System - anemia, hemolysis, lymphadenopathy; Metabolic and Nutritional Disorders -avitaminosis, gout, dehydration, hyperglycemia/hypoglycemia, peripheral edema, weight gain/loss; Musculoskeletal System - arthralgia, arthritis, bone disorder, joint disorder, leg cramps,musculoskeletal pain, myalgia, myasthenia, ptosis, synovitis; Nervous System - abnormal dreams, agitation, amnesia, anxiety, apathy, confusion, convulsion, dementia, depersonalization, depression, diplopia, dizziness, emotional lability, hallucinations, hemiplegia, hostility aggravated, hyperkinesia, hypertonia, hypesthesia, insomnia, libido decreased/increased, nervousness, neurosis, paresthesia, sleep disorder, somnolence, thinking abnormality, tremor, vertigo; Respiratory System - asthma, bronchitis, cough increased, dyspnea, epistaxis, hemoptysis, hiccup, laryngeal neoplasia, lung fibrosis, pharyngitis, pleural disorder, pneumonia, respiratory disorder, upper respiratoryinflammation/infection, rhinitis, sinusitis, stridor; Skin and Appendages -acne, alopecia, contact dermatitis, dry skin, fixed eruption, hair disorder, maculopapular rash, nail disorder, pruritus, rash, skin carcinoma, skin disorder, sweating, urticaria; Special Senses -abnormal vision, amblyopia, blepharitis, blurred vision, cataract, conjunctivitis, deafness, dry eyes, ear/eye disorder, eye pain, glaucoma, otitis media, parosmia, photophobia, retinal degeneration/disorder, taste loss, taste perversion, tinnitus, visual field defect; Urogenital System - abnormal menses, breast enlargement, breast pain, breast tenderness, dysmenorrhea, dysuria, gynecomastia, impotence, kidney calculus, kidney pain, leukorrhea, menorrhagia, menstrual disorder, penis disorder, polyuria, testis disorder, urethral pain, urinary frequency, urinary retention, urinary tract infection, urinary urgency, urination impaired, vaginitis.PostmarketingAdditional adverse experiences have been reported since oral PREVACID has been marketed. The majority of these cases are foreign-sourced and a relationship to PREVACID has not been established. Because these events were reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These events are listed below by COSTART body system.Body as a Whole –anaphylactic/anaphylactoid reactions; Digestive System - hepatotoxicity, pancreatitis, vomiting; Hemic and Lymphatic System - agranulocytosis, aplastic anemia, hemolytic anemia, leukopenia, neutropenia, pancytopenia, thrombocytopenia, and thrombotic thrombocytopenic purpura; Musculoskeletal System – myositis; Skin and Appendages – severe dermatologic reactions including erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis (some fatal); Special Senses -speech disorder; Urogenital System – interstitial nephritis, urinary retention.。
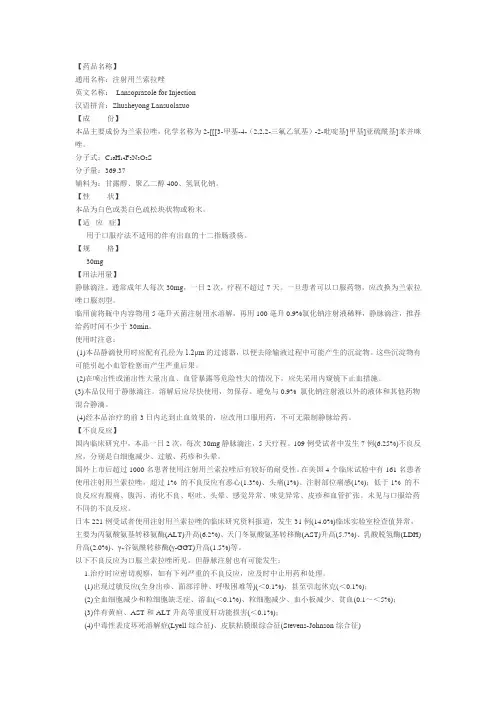
通用名称:注射用兰索拉唑英文名称:Lansoprazole for Injection汉语拼音:Zhusheyong Lansuolazuo【成份】本品主要成份为兰索拉唑,化学名称为2-[[[3-甲基-4-(2,2,2-三氟乙氧基)-2-吡啶基]甲基]亚硫酰基]苯并咪唑。
分子式:C16H14F3N3O2S分子量:369.37辅料为:甘露醇、聚乙二醇400、氢氧化钠。
【性状】本品为白色或类白色疏松块状物或粉末。
【适应症】用于口服疗法不适用的伴有出血的十二指肠溃疡。
【规格】30mg【用法用量】静脉滴注。
通常成年人每次30mg,一日2次,疗程不超过7天。
一旦患者可以口服药物,应改换为兰索拉唑口服剂型。
临用前将瓶中内容物用5毫升灭菌注射用水溶解,再用100毫升0.9%氯化钠注射液稀释,静脉滴注,推荐给药时间不少于30min。
使用时注意:(1)本品静滴使用时应配有孔径为1.2μm的过滤器,以便去除输液过程中可能产生的沉淀物。
这些沉淀物有可能引起小血管栓塞而产生严重后果。
(2)在喷出性或涌出性大量出血、血管暴露等危险性大的情况下,应先采用内窥镜下止血措施。
(3)本品仅用于静脉滴注。
溶解后应尽快使用,勿保存。
避免与0.9% 氯化钠注射液以外的液体和其他药物混合静滴。
(4)经本品治疗的前3日内达到止血效果的,应改用口服用药,不可无限制静脉给药。
【不良反应】国内临床研究中,本品一日2次,每次30mg静脉滴注,5天疗程。
109例受试者中发生7例(6.25%)不良反应,分别是白细胞减少、过敏、药疹和头晕。
国外上市后超过1000名患者使用注射用兰索拉唑后有较好的耐受性。
在美国4个临床试验中有161名患者使用注射用兰索拉唑,超过1% 的不良反应有恶心(1.3%)、头痛(1%)、注射部位痛感(1%);低于1% 的不良反应有腹痛、腹泻、消化不良、呕吐、头晕、感觉异常、味觉异常、皮疹和血管扩张。
未见与口服给药不同的不良反应。
日本221例受试者使用注射用兰索拉唑的临床研究资料报道,发生31例(14.0%)临床实验室检查值异常,主要为丙氨酸氨基转移氨酶(ALT)升高(6.2%)、天门冬氨酸氨基转移酶(AST)升高(5.7%)、乳酸脱氢酶(LDH)升高(2.0%)、γ-谷氨酰转移酶(γ-GGT)升高(1.5%)等。

兰索拉唑肠溶片(兰悉多)的说明书民以食为天,身体是革命的本钱,肠胃不好的话容易造成身体各方面出现病变。
饮食不合理容易导致肠胃疾病的发生,肠胃不好的话对于食物的吸收也是个问题。
所以我们一定要保证肠胃的健康,今天,我们为您介绍一种叫做兰索拉唑肠溶片(兰悉多)的药物,该药物就是肠胃特效药当中比较好的一种,下面来看看介绍。
【药品名称】通用名称:兰索拉唑肠溶片商品名称:兰索拉唑肠溶片(兰悉多)拼音全码:LanSuoLaZuoPian(LanXiDuo)【主要成份】本品主要成份为兰索拉唑。
化学名:2-[[[3-甲基-4-(2,2,2-三氟乙氧基)-2-吡啶基]甲基]亚磺酰基]-1H -苯并咪唑。
分子式:C16H14F3N3O2S分子量:369.37【性状】本品为肠溶片,除去肠溶衣后显白色至淡黄褐色。
【适应症/功能主治】胃溃疡、十二指肠溃疡、反流性食管炎、佐-艾(Zollinger-Ellison)综合征(胃泌素瘤)。
【规格型号】15mg*7s【用法用量】口服,不可咀嚼。
1.通常成人口服兰索拉唑片,每日一次,一次1至2片(12-30mg)。
2.十二指肠溃疡,需连续服用4-6周。
3.胃溃疡、反流性食管炎、卓-艾综合征,需连续服用6-8周;或遵医嘱。
【不良反应】副作用轻微,主要表现为口干、头晕、恶心。
【禁忌】对本品过敏者禁用。
【注意事项】曾发生药物过敏症的患者及肝机能障碍的患者应慎重用药。
【儿童用药】对小儿的安全性尚未被确立(由于在小儿的临床经验极少)。
【老年患者用药】老年患者的胃酸分泌能力和其他生理机能均会降低,故用药期间请注意观察。
【孕妇及哺乳期妇女用药】孕妇、哺乳期妇女忌用。
【药物相互作用】会延迟安定(diazepam)及苯妥英钠(phenytoin Sodium)的代谢与排泄,资料已被发表于类似药物奥美拉唑的报告中。
【药物过量】未进行该项实验且无可靠文献。
【药理毒理】该品为新型的抑制胃酸分泌的药物,它作用于胃壁细胞的H+-K+-ATP酶,使壁细胞的H+不能转运到胃中去,以致胃液中胃酸量大为减少,临床上用于十二指肠溃疡、胃溃疡、反流性食管炎,佐-艾(Zollinger-Ellison)综合征(胃泌素瘤)的治疗,疗效显著,对幽门螺杆菌有抑制作用。
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use PREVACID safely and effectively. See full prescribing information for:PREVACID (lansoprazole) Delayed-Release Capsules PREVACID SoluTab (lansoprazole) Dela y ed-Release Orally Disintegrating TabletsFor oral administrationInitial U.S. Approval: 1995 ---------------------------RECENT MAJOR CHANGES--------------------------- WARNINGS AND PRECAUTIONS• Bone Fracture (5.2)8/2010• Hypoma g nesemia (5.3)5/2011----------------------------INDICAT I ONS AN D USAGE----------------------------PREVACID is a proton pump inhibitor (PPI). Refer to DOSAGE AND ADMINISTRATION table (belo w ) for indications and usage.-----------------------DOSAGE AND ADMINISTRATION------------------------Indication Dose FrequencyDuodenal Ulcers (1.1, 1.3) Short-Term Tre a tment Maintenance of Healed 15 mg 15 mg y for 4 wksOnce dail Once daily H. pylori Erad duce Rec o l Ulcer (1.2)ication to Re urrence f Duodena Triple Therapy: PREVACID Amoxicil Clarithro lin mycin Dual Therapy: PREVACID Amoxicillin 0 mg3 1 gram500 mg 30 mg 1 gram rTwice daily for 10 o 14 days Three times daily for 14 days Benign Gastric Ulcer (1.4) Short-Term Treatment 30 mg Once daily up to 8wksNSAID-associated Gastric Ulcer (1.6)Healing Risk Reduction 30 mg 15 mg Once daily for 8 wks Once daily up to 12 wks GERD (1.7)Short-Term Treatment of Symptomatic GERDShort-Term Treatment of EE 15 mg30 mg Once daily up to 8 wksOnce daily up to 8wksPediatric (8.4) (1 to 11 years of age) Short-Term Tre f S matic GERD atment o ympto and Short-Term Treatment of EE ≤ 30 kg 15 mg Once daily up to 12wks> 30 kg 30 mg Once daily up to 12wks(12 to 17 years of age) Short-Term Treatment of Symptomatic GERDNonerosive GERD EE15 mg 30 mg Once daily up to 8wksOnce daily up to 8 wks Maintenance of Healing of EE (1.8)15 mg Once daily Pathological Hypersecretory Conditions (i.e., ZES) (1.9) 60 mgOnce daily -------------------DOSAGE FORMS AND STRENGTHS------------------Capsules and Tablets: 15 mg and 30 mg. (3)-----------------------------CONTRAINDICATIONS--------------------------- Contraindicated in patients with known severe hypersensitivity to any component of the PREVACID formulation. (4)---------------------WARNINGS AND PRECAUTIONS--------------------• Symptomatic response with PREVACID does not preclude th epresence of gastric maligna n cy. (5.1) • Bone Fracture: Long-term and multiple daily dose PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. (5.2) • Hypomagnesemia has been reported rarely with prolonged treatment with PPIs. (5.3) ---------------------------ADVERSE REACTIONS----------------------------Most commonly reported adverse reactions (≥1%): diarrhea, d ab ominal pain, nausea and constipation. (6) To report SUSPECTED ADVERSE REACTIONS, contact Taked aPharmaceuticals America Inc. at 1-877-TAKEDA-7 (1-877-825-3327) or FDA at 1-800-FDA-1088 or /medwatch. -----------------------------DRUG INTE R ACTIONS---------------------------• Do not co-administer with atazanavir. (7)• May interfere with th e absorption of drugs where gastric pH isimportant for bioavailability. (7)• Concomitant warfarin use may require mo n itoring for increases inINR and prothrombin time. (7) • Concomitant tacrolimus use may increase tacrolimus whole blood concentrations. (7) • Titration of theophylline dosage may be required when concomitan tPREVACID use is started or stopped. (7) ----------------------USE IN SPECIFIC POPULATIONS-------------------• Consider dose adjustment in patients with severe liver impairm e nt.(8.7)• PREVACID is not effective in patients with symptom a tic GERD 1month to less than 1 year of age. (8.4) See 17 for PATIENT COUNSELIN G INFORMATION and FDA -Approved Patient LabelingRevised: May 2011 FULL PRESCRIBING INFORMATION: CONTENTS* 1 INDICATIONS AND USAGE 1.1 Short-Term Treatment of Active Duodenal Ulcer 1.2 H. pylori Eradication to Reduce the Risk of Duodenal UlcerRecurrence 1.3 Maintenance of Healed Duodenal Ulcers 1.4 Short-Term Treatment of Active Benign Gastric Ulcer 1.5 Healing of NSAID-Associa t ed Gastric Ulcer1.6 Risk Reduction of NSAID-Associated Gastric Ulcer 1.7 Gastroesophageal Ref l ux Disease (GERD) 1.8 Maintenance of Heali n g of Erosive Esophagitis (EE) 1.9 Pathological Hypersecretory Condition s Including Zollinger-Ellison Syndrome (ZES) 2 DOSAGE AND ADMINISTRA T ION2.1 R ecommended Dose 2.2 Special Populations 2.3 Important Administration Information 3 DOSAGE FORMS AND STRENGTHS 4 CONTRAINDICATIONS5WARNINGS AND PRE C AUTIONS 5.1 Gastric Malignancy 5.2 Bone Fracture 5.3 Hypomagn e semia 6 A DVERSE RE A CTIONS6.1 C linical6.2 Postmarketing Experience 6.3 Combination Therapy with Amoxicillin and Clarithromycin 6.4 L aboratory Values 7 DRUG INTERACTIONS 8 USE IN SPECIFIC POPULA T IONS8.1 P regnancy 8.3 N ursing Mothers 8.4 P ediatric Use 8.5 G eriatric Use 8.6 R enal Impairment 8.7 H epatic Impairment 8.8 G ender 8.9 R ace10 OVERDOSAGE11 DESCRIPTION12 CLINICAL PHARMACOLOGY12.1 Mechanism of Action12.2 Pharmacodynamics12.3 Pharmacokinetics12.4 Specific Populations12.5 Drug-Drug Interactions13 NONCLINICAL TOXICOLOGY13.1 Carcinogenesis, Mutagenesis, Impairment of FertilityPage 2 of 2413.2 Animal Toxicology and/or Pharmacology14 CLINICAL STUDIES15 REFERENCES16 HOW SUPPLIED/STORAGE AND HANDLING17 PATIENT COUNSELING INFORMATION*Sections or subsections omitted from the full prescribing information are not listed.FULL PRESCRIBING INFORMATION1 INDICATIONSANDUSAGE1.1 Short-Term Treatment of Active Duodenal UlcerPREVACID is indicated for short-term treatment (for 4 weeks) for healing and symptom relief of active duodenal ulcer [see Clinical Studies (14)].1.2 H. pylori Eradication to Reduce the Risk of Duodenal Ulcer RecurrenceTriple Therapy: PREVACID/amoxicillin/clarithromycinPREVACID in combination with amoxicillin plus clarithro m ycin as triple therapy is indicated for the treatment of patients with H. pylori infection and duodenal ulcer disease (active or one-year history of a duoden a l ulcer) to eradicate H. pylori. Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence [see Clinical Studies (14)].Please refer to the full prescribing information for amoxicillin and cla r ithromycin.Dual Therapy: PREVACID/amoxicillinPREVACID in combination with amoxicillin as dual therapy is indicated for the treatment of patients with H. pylori infection and duodenal ulcer disease (active or one-year history of a duodenal ulcer) who are either allerg i c or intolerant to clarithromycin or in whom resistance to clarithromycin is known or suspected (see the clarithromycin package insert, MICROBIOLOGY section). Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence [see Clinical Studies (14)].Please refer to the full prescribing information for amoxicilli n.1.3 Maintenance of Healed Duodenal UlcersPREVACID is indicated to maintain healing of duodenal ulcers. Controlled studies do not extend beyond 12 months [see Clinical Studies (14)].1.4 Short-Term Treatment of Active Benign Gastric UlcerPREVACID is indicated for short-term treatment (up to 8 weeks) for healing and symptom relief of a c tive benign gastric ulcer [see Clinical Studies (14)].1.5 Healing of NSAID-Associated Gastric UlcerPREVACID is indicated for the treatment of NSAID-associated gastric ulcer in patients who continue NSAID use. Controlled studies did not extend beyond 8 weeks [see Clinical Studies (14)].1.6 Risk Reduction of NSAID-Associated Gastric UlcerPREVACID is indicated for reducing the risk of NSAID-associated gastric ulcers in patients with a history of a documented gastric ulcer who require the use of an NSAID. Controlled studies did not extend beyond 12 weeks [see Clinical Studies (14)].1.7 Gastroesophageal Reflux Disease (GERD)Short-Term Treatment of Symptomatic GERDPREVACID is indicated for the treatment of heartburn and other symptoms associated with GERD [see Clinical Studies (14)].Short-Term Treatment of Erosive EsophagitisPREVACID is indicated for short-term treatment (up to 8 weeks) for healing and symptom relief of all grades of erosive esophagitis. For patients whodo not heal with PREVACID for 8 weeks (5 to 10%), it may be helpful to give an additional 8 weeks of treatment. If there is a recurrence of erosive esophagitis an additional 8-week course of PREVACID may be considered [see Clinical Studies (14)].1.8 Maintenance of Healing of Erosive Esophagitis (EE)PREVACID is indicated to maintain healing of erosive esophagitis. Controlled studies did not extend beyond 12 months [see Clinical Studies (14 )].1.9 Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome (ZES)PREVACID is indicated for the long-term treatment of pathological hypersecretory conditions, including Zollinger-Ellison syndrome [see Clinical Studies (14)].2 DOSAGEANDADMINISTRATIONPREVACID is available as a capsule and an orally disintegrating tablet, and is available in 15 mg and 30 mg strengths. Directions for use specific to the route and available methods of administration for each of these dosage forms is presented below. PREVACID should be taken before eating. PREVACID products SHOULD NOT BE CRUSHED OR CHEWED. In the clinical trials, antacids were used concomitantly with PREVACID.2.1 Recommended DoseDoseFrequency Indication RecommendedDuodenal UlcersShort-Term Treatment 15 mg Once daily for 4 weeksMaintenance of Healed 15 mg Once dailyH. pylori Eradication to Reduce the Risk ofDuodenal Ulcer Recurrence*Triple Therapy:PREVACID 30 mg Twice daily (q12h) for 10 or 14 daysAmoxicillin 1 gram Twice daily (q12h) for 10 or 14 daysClarithromycin 500 mg Twice daily (q12h) for 10 or 14 daysDual Therapy:PREVACID 30 mg Three times daily (q8h) for 14 daysAmoxicillin 1 gram Three times daily (q8h) for 14 days Benign Gastric UlcerShort-Term Treatment 30 mg Once daily for up to 8 weeksNSAID-associated Gastric UlcerHealing 30 mg Once daily for 8 weeks†Risk Reduction 15 mg Once daily for up to 12 weeks†Gastroesophageal Reflux Disease (GERD)Short-Term Treatment of Symptomatic GERD 15 mg Once daily for up to 8 weeksShort-Term Treatment of Erosive Esophagitis 30 mg Once daily for up to 8 weeks‡Pediatric(1 to 11 years of age)Short-Term Treatment of Symptomatic GERD and Short-Term Treatment of Erosive Esophagitis≤ 30 kg 15 mg Once daily for up to 12 weeks§> 30 kg 30 mg Once daily for up to 12 weeks§(12 to 17 years of age)Short-Term Treatment of Symptomatic GERDNonerosive GERD 15 mg Once daily for up to 8 weeksErosive Esophagitis 30 mg Once daily for up to 8 weeksMaintenance of Healing of Erosive Esophagitis 15 mg Once dailyPathological Hypersecretory Conditions Including60 mg Once daily¶Zollinger-Ellison Syndrome*Please refer to amoxicillin and clarithromycin full prescribing information for CONTRAINDICATIONS and WARNINGS, and forinformation regarding dosing in elderly and renally-impaired patients.†Controlled studies did not extend beyond indicated duration.‡For patients who do not heal with PREVACID for 8 weeks (5 to 10%), it may be helpful to give an additional 8 weeks of treatment. Ifthere is a recurrence of erosive esophagitis, an additional 8 week course of PREVACID may be considered.§The PREVACID dose was increased (up to 30 mg twice daily) in some pediatric patients after 2 or more weeks of treatment if theyremained symptomatic. For pediatric patients unable to swallow an intact capsule please see Administration Options.¶Varies with individual patient. Recommended adult starting dose is 60 mg once daily. Doses should be adjusted to individual patientneeds and should continue for as long as clinically indicated. Dosages up to 90 mg twice daily have been administered. Daily dose ofgreater than 120 mg should be administered in divided doses. Some patients with Zollinger-Ellison Syndrome have been treatedcontinuously with PREVACID for more than 4 years.Populations2.2 SpecialRenal impairment patients and geriatric patients do not require dosage adjustment. However, consider dose adjustment in patients with severe liver impairment [see Use in Specific Populations (8.5, 8.6 and 8.7)].InformationAdministration2.3 ImportantAdministration OptionsPREVACID Delayed-Release Capsules – Oral Administration• PREVACID Delayed-Release Capsules should be swallowed whole.• Alternatively, for patients who have difficulty swallowing capsules, PREVACID Delayed-Release Capsules can be opened and administered as follows:capsule.o Openo Sprinkle intact granules on one tablespoon of either applesauce, ENSURE pudding, cottage cheese, yogurt or strained pears.immediately.o Swallow• PREVACID Delayed-Release Capsules may also be emptied into a small volume of either apple juice, orange juice or tomato juice and administered as follows:capsule.o Openo Sprinkle intact granules into a small volume of either apple juice, orange juice or tomato juice (60 mL – approximately 2 ounces).o Mix briefly.o Swallow immediately.o To ensure complete delivery of the dose, the glass should be rinsed with two or more volumes of juice and the contents swallowed immediately.PREVACID Delayed-Release Capsules – Nasogastric Tube (≥16 French) Administration• For patients who have a nasogastric tube in place, PREVACID Delayed-Release Capsules can be administered as follows:capsule.o Openo Mix intact granules into 40 mL of apple juice. DO NOT USE OTHER LIQUIDS.o Inject through the nasogastric tube into the stomach.o Flush with additional apple juice to clear the tube.USE IN OTHER FOODS AND LIQUIDS HAS NOT BEEN STUDIED CLINICALLY AND IS THEREFORE NOT RECOMMENDED.PREVACID SoluTab Delayed-Release Orally Disintegrating Tablets• PREVACID SoluTab should not be broken or cut.• PREVACID SoluTab should not be chewed.o Place the tablet on the tongue and allow it to disintegrate, with or without water, until the particles can be swallowed.o The tablet typically disintegrates in less than 1 minute.o Alternatively, for children or other patients who have difficulty swallowing tablets, PREVACID SoluTab can be delivered in two different ways.PREVACID SoluTab – Oral SyringeFor administration via oral syringe, PREVACID SoluTab can be administered as follows:Place a 15 mg tablet in oral syringe and draw up 4 mL of water, or place a 30 mg tablet in oral syringe and draw up 10 mL of water.Shake gently to allow for a quick dispersal.After the tablet has dispersed, administer the contents within 15 minutes.Refill the syringe with approximately 2 mL (5 mL for the 30 mg tablet) of water, shake gently, and administer any remaining contents.PREVACID SoluTab – Nasogastric Tube (≥ 8 French) AdministrationFor administration via a nasogastric tube, PREVACID SoluTab can be administered as follows:Place a 15 mg tablet in a syringe and draw up 4 mL of water, or place a 30 mg tablet in a syringe and draw up 10 mL of water.Shake gently to allow for a quick dispersal.After the tablet has dispersed, inject through the nasogastric tube into the stomach within 15 minutes.Refill the syringe with approximately 5 mL of water, shake gently, and flush the nasogastric tube.3 DOSAGE FORMS AND STRENGTHS• 15 mg capsules are opaque, hard gelatin, colored pink and green with the TAP logo and “PREVACID 15” imprinted on the capsule.• 30 mg capsules are opaque, hard gelatin, colored pink and black with the TAP logo and “PREVACID 30” imprinted on the capsule.• 15 mg tablets are white to yellowish white, uncoated, colored orange to dark brown speckles with “15” debossed on one side of the tablet.• 30 mg tablets are white to yellowish white, uncoated, colored orange to dark brown speckles with “30” debossed on one side of the tablet.4 CONTRAINDICATIONSPREVACID is contraindicated in patients with known severe hypersensitivity to any component of the formulation of PREVACID. For information on contraindications for amoxicillin or clarithromycin, refer to their full prescribing information, CONTRAINDICATIONS sections.PRECAUTIONS5 WARNINGSAND5.1 Gastric MalignancySymptomatic response to therapy with lansoprazole does not preclude the presence of gastric malignancy.5.2 Bone FractureSeveral published observational studies suggest that proton pump inhibitor (PPI) therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines [see Dosage and Administration (2) and Adverse Reactions (6.2)].For information on warnings and precautions for amoxicillin or clarithromycin, refer to their full prescribing information, WARNINGS and PRECAUTIONS sections.5.3 HypomagnesemiaHypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically [see Adverse Reactions (6.2)].6 ADVERSE REACTIONS6.1 ClinicalWorldwide, over 10,000 patients have been treated with PREVACID in Phase 2 or Phase 3 clinical trials involving various dosages and durations of treatment. In general, PREVACID treatment has been well-tolerated in both short-term and long-term trials.Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.The following adverse reactions were reported by the treating physician to have a possible or probable relationship to drug in 1% or more of PREVACID-treated patients and occurred at a greater rate in PREVACID-treated patients than placebo-treated patients in Table 1.Table 1: Incidence of Possibly or Probably Treatment-Related Adverse Reactionsin Short-Term, Placebo-Controlled PREVACID StudiesBody System/Adverse Event PREVACID(N= 2768)%Placebo(N= 1023)%Body as a WholeAbdominal Pain 2.1 1.2 Digestive SystemConstipation Diarrhea Nausea 1.03.81.30.42.31.2Headache was also seen at greater than 1% incidence but was more common on placebo. The incidence of diarrhea was similar between patients who received placebo and patients who received 15 mg and 30 mg of PREVACID, but higher in the patients who received 60 mg of PREVACID (2.9%, 1.4%, 4.2%, and 7.4%, respectively).The most commonly reported possibly or probably treatment-related adverse event during maintenance therapy was diarrhea.In the risk reduction study of PREVACID for NSAID-associated gastric ulcers, the incidence of diarrhea for patients treated with PREVACID, misoprostol, and placebo was 5%, 22%, and 3%, respectively.Another study for the same indication, where patients took either a COX-2 inhibitor or lansoprazole and naproxen, demonstrated that the safety profile was similar to the prior study. Additional reactions from this study not previously observed in other clinical trials with PREVACID included contusion, duodenitis, epigastric discomfort, esophageal disorder, fatigue, hunger, hiatal hernia, hoarseness, impaired gastric emptying, metaplasia, and renal impairment.Additional adverse experiences occurring in less than 1% of patients or subjects who received PREVACID in domestic trials are shown below:Body as a Whole – abdomen enlarged, allergic reaction, asthenia, back pain, candidiasis, carcinoma, chest pain (not otherwise specified), chills, edema, fever, flu syndrome, halitosis, infection (not otherwise specified), malaise, neck pain, neck rigidity, pain, pelvic painCardiovascular System – angina, arrhythmia, bradycardia, cerebrovascular accident/cerebral infarction, hypertension/hypotension, migraine, myocardial infarction, palpitations, shock (circulatory failure), syncope, tachycardia, vasodilationDigestive System – abnormal stools, anorexia, bezoar, cardiospasm, cholelithiasis, colitis, dry mouth, dyspepsia, dysphagia, enteritis, eructation, esophageal stenosis, esophageal ulcer, esophagitis, fecal discoloration, flatulence, gastric nodules/fundic gland polyps, gastritis, gastroenteritis, gastrointestinal anomaly, gastrointestinal disorder, gastrointestinal hemorrhage, glossitis, gum hemorrhage, hematemesis, increased appetite, increased salivation, melena, mouth ulceration, nausea and vomiting, nausea and vomiting and diarrhea, gastrointestinal moniliasis, rectal disorder, rectal hemorrhage, stomatitis, tenesmus, thirst, tongue disorder, ulcerative colitis, ulcerative stomatitisEndocrine System – diabetes mellitus, goiter, hypothyroidismHemic and Lymphatic System – anemia, hemolysis, lymphadenopathyMetabolism and Nutritional Disorders – avitaminosis, gout, dehydration, hyperglycemia/hypoglycemia, peripheral edema, weight gain/loss Musculoskeletal System – arthralgia, arthritis, bone disorder, joint disorder, leg cramps, musculoskeletal pain, myalgia, myasthenia, ptosis, synovitis Nervous System – abnormal dreams, agitation, amnesia, anxiety, apathy, confusion, convulsion, dementia, depersonalization, depression, diplopia, dizziness, emotional lability, hallucinations, hemiplegia, hostility aggravated, hyperkinesia, hypertonia, hypesthesia, insomnia, libidodecreased/increased, nervousness, neurosis, paresthesia, sleep disorder, somnolence, thinking abnormality, tremor, vertigoRespiratory System – asthma, bronchitis, cough increased, dyspnea, epistaxis, hemoptysis, hiccup, laryngeal neoplasia, lung fibrosis, pharyngitis, pleural disorder, pneumonia, respiratory disorder, upper respiratory inflammation/infection, rhinitis, sinusitis, stridorSkin and Appendages – acne, alopecia, contact dermatitis, dry skin, fixed eruption, hair disorder, maculopapular rash, nail disorder, pruritus, rash, skin carcinoma, skin disorder, sweating, urticariaSpecial Senses – abnormal vision, amblyopia, blepharitis, blurred vision, cataract, conjunctivitis, deafness, dry eyes, ear/eye disorder, eye pain, glaucoma, otitis media, parosmia, photophobia, retinal degeneration/disorder, taste loss, taste perversion, tinnitus, visual field defectUrogenital System – abnormal menses, breast enlargement, breast pain, breast tenderness, dysmenorrhea, dysuria, gynecomastia, impotence, kidney calculus, kidney pain, leukorrhea, menorrhagia, menstrual disorder, penis disorder, polyuria, testis disorder, urethral pain, urinary frequency, urinary retention, urinary tract infection, urinary urgency, urination impaired, vaginitis.6.2 Postmarketing ExperienceAdditional adverse experiences have been reported since PREVACID has been marketed. The majority of these cases are foreign-sourced and a relationship to PREVACID has not been established. Because these reactions were reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These events are listed below by COSTART body system.Body as a Whole - anaphylactic/anaphylactoid reactions; Digestive System -hepatotoxicity, pancreatitis, vomiting; Hemic and Lymphatic System - agranulocytosis, aplastic anemia, hemolytic anemia, leukopenia, neutropenia, pancytopenia, thrombocytopenia, and thrombotic thrombocytopenic purpura; Metabolism and Nutritional Disorders – hypomagnesemia; Musculoskeletal System – bone fracture, myositis; Skin and Appendages - severe dermatologic reactions including erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis (some fatal); Special Senses -speech disorder; Urogenital System - interstitial nephritis, urinary retention.6.3 Combination Therapy with Amoxicillin and ClarithromycinIn clinical trials using combination therapy with PREVACID plus amoxicillin and clarithromycin, and PREVACID plus amoxicillin, no adverse reactions peculiar to these drug combinations were observed. Adverse reactions that have occurred have been limited to those that had been previously reported with PREVACID, amoxicillin, or clarithromycin.Triple Therapy: PREVACID/amoxicillin/clarithromycinThe most frequently reported adverse reactions for patients who received triple therapy for 14 days were diarrhea (7%), headache (6%), and taste perversion (5%). There were no statistically significant differences in the frequency of reported adverse reactions between the 10- and 14-day triple therapy regimens. No treatment-emergent adverse reactions were observed at significantly higher rates with triple therapy than with any dual therapy regimen.Dual Therapy: PREVACID/amoxicillinThe most frequently reported adverse reactions for patients who received PREVACID three times daily plus amoxicillin three times daily dual therapy were diarrhea (8%) and headache (7%). No treatment-emergent adverse reactions were observed at significantly higher rates with PREVACID three times daily plus amoxicillin three times daily dual therapy than with PREVACID alone.For information on adverse reactions with amoxicillin or clarithromycin, refer to their full prescribing information, ADVERSE REACTIONS sections.6.4 Laboratory ValuesThe following changes in laboratory parameters in patients who received PREVACID were reported as adverse reactions:Abnormal liver function tests, increased SGOT (AST), increased SGPT (ALT), increased creatinine, increased alkaline phosphatase, increased globulins, increased GGTP, increased/decreased/abnormal WBC, abnormal AG ratio, abnormal RBC, bilirubinemia, blood potassium increased, blood urea increased, crystal urine present, eosinophilia, hemoglobin decreased, hyperlipemia, increased/decreased electrolytes, increased/decreased cholesterol, increased glucocorticoids, increased LDH, increased/decreased/abnormal platelets, increased gastrin levels and positive fecal occult blood. Urine abnormalities such as albuminuria, glycosuria, and hematuria were also reported. Additional isolated laboratory abnormalities were reported.In the placebo controlled studies, when SGOT (AST) and SGPT (ALT) were evaluated, 0.4% (4/978) and 0.4% (11/2677) patients, who received placebo and PREVACID, respectively, had enzyme elevations greater than three times the upper limit of normal range at the final treatment visit. None of these patients who received PREVACID reported jaundice at any time during the study.In clinical trials using combination therapy with PREVACID plus amoxicillin and clarithromycin, and PREVACID plus amoxicillin, no increased laboratory abnormalities particular to these drug combinations were observed.For information on laboratory value changes with amoxicillin or clarithromycin, refer to their full prescribing information, ADVERSE REACTIONS sections.INTERACTIONS7 DRUGDrugs with pH-Dependent Absorption KineticsPREVACID causes long-lasting inhibition of gastric acid secretion. PREVACID and other PPIs are likely to substantially decrease the systemic concentrations of the HIV protease inhibitor atazanavir, which is dependent upon the presence of gastric acid for absorption, and may result in a loss of therapeutic effect of atazanavir and the development of HIV resistance. Therefore, PREVACID and other PPIs should not be co-administered with atazanavir [see Clinical Pharmacology (12.5)].It is theoretically possible that PREVACID and other PPIs may interfere with the absorption of other drugs where gastric pH is an important determinant of oral bioavailability (e.g., ampicillin esters, digoxin, iron salts, ketoconazole) [see Clinical Pharmacology (12.5)].WarfarinIn a study of healthy subjects, co-administration of single or multiple 60 mg doses of PREVACID and warfarin did not affect the pharmacokinetics of warfarin nor prothrombin time [see Clinical Pharmacology (12.5)]. However, there have been reports of increased INR and prothrombin time in patients receiving PPIs and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. Patients treated with PPIs and warfarin concomitantly may need to be monitored for increases in INR and prothrombin time [see Clinical Pharmacology (12.5)]. TacrolimusConcomitant administration of lansoprazole and tacrolimus may increase whole blood levels of tacrolimus, especially in transplant patients who are intermediate or poor metabolizers of CYP2C19.TheophyllineA minor increase (10%) in the clearance of theophylline was observed following the administration of PREVACID concomitantly with theophylline. Although the magnitude of the effect on theophylline clearance is small, individual patients may require additional titration of their theophylline dosage when PREVACID is started or stopped to ensure clinically effective blood levels [see Clinical Pharmacology (12.5)].For information on drug interactions for amoxicillin or clarithromycin, refer to their full prescribing information, DRUG INTERACTIONS sections.8 USE IN SPECIFIC POPULATIONS8.1 PregnancyTeratogenic effectsPregnancy Category B. Reproduction studies have been performed in pregnant rats at oral doses up to 40 times the recommended human dose and in pregnant rabbits at oral doses up to 16 times the recommended human dose and have revealed no evidence of impaired fertility or harm to the fetus due to lansoprazole. There are, however, no adequate or well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed [see Nonclinical Toxicology (13.2)].See full prescribing information for clarithromycin before using in pregnant women.。
兰索拉唑一基本情况化学名称:(+)-2【3—甲基—4—(2,2,2—三氟乙氧基)—2吡啶基】—1H—苯并咪唑。
分子结构:主要剂型:片剂、胶囊、注射剂适应症:胃溃疡、十二指肠溃疡、反流性食管炎、佐-艾(Zollinger-Ellison)综合征(胃泌素瘤)。
不良反应:1.过敏反应:偶有皮疹、瘙痒等症状,如出现上述症状时请停止用药。
2.血液系统:偶有贫血、白细胞减少,嗜酸球增多等症状,血小板减少之症状极少发生3.消化系统:偶有便秘,腹泻,口渴,腹胀等症状。
偶有GOT、GPT、ALP、LDH、γ-GTP上升等现象,所以须细心观察,如有异常现象就应采取停药等适当的处置。
4.精神神经系统:偶有头痛、嗜睡等症状。
失眠,头晕等症状极少发生。
5.其他:偶有发热,总胆固醇上升,尿酸上升等症状。
用法与用量:十二指肠溃疡,通常成人每日一次,口服兰索拉唑15mg~30mg,连续服用4~6周;胃溃疡、反流性食道炎、Zollinger-Ellison症候群、吻合口部溃疡,通常成人每日一次,口服兰索拉唑30mg,连续服用6~8周。
但用做维持治疗、高龄者、有肝功能障碍、肾功能低下的患者,每日一次,口服兰索拉唑15mg。
.对小儿的用药:对小儿的安全性尚未被确立(由于在小儿的临床经验极少)二、市场情况1.全国共有92家生产厂家,天津武田制药公司生产,商品名为“ 达克普隆”兰索拉唑肠溶胶囊,国内兰索拉唑原料和肠溶片由汕头经济特区鮀滨制药厂研究开发,于1994年1月获得二类新药证书和生产批文。
价格从5元多到30多不等,天津武田进口的兰悉多和汕头鮀滨制药的达克普隆占据很大的市场,超过98%(2005年)。
生产厂家主要有:兰索拉唑胶囊湖北潜龙药业有限公司国药准字H20066197兰索拉唑胶囊天津武田药品有限公司国药准字H10980036兰索拉唑胶囊天津武田药品有限公司国药准字H10980035兰索拉唑肠溶片汕头经济特区鮀滨制药厂国药准字H10980136兰索拉唑肠溶片郑州瑞康制药有限公司国药准字H20083439兰索拉唑肠溶片河南帅克制药有限公司国药准字H20065318兰索拉唑片扬子江药业集团有限公司国药准字H20054142兰索拉唑片上海信谊有限公司国药准字H20067605兰索拉唑片昆明源瑞制药有限公司国药准字H20103669兰索拉唑片湖北科益药业股份有限公司国药准字H200738622.同类产品还有:奥美拉唑肠溶胶囊(片剂、注射剂)(评价较高,兰索拉唑是其第二代产品),埃索美拉唑、雷尼替丁、阿莫西林、胃灵颗粒、康复新液(溶液剂)、诺森(进口药,比较贵)、甲磺酸左氧氟沙星、枸橼酸铋钾胶囊(丽珠得乐)、铝碳酸镁片、等。
兰索拉唑肠溶胶囊(达克普隆)的说明书饱一顿饿一顿的情况往往出现在工作比较忙的人群当中,平时吃饭没规律是导致肠胃疾病发生的重要原因。
生活中大家一定要养成按时吃饭的习惯,不能根据自身的喜好来饮食。
目前推出了一种叫做兰索拉唑肠溶胶囊(达克普隆)的肠胃药,这是一种纯天然中草药制成的肠胃药,对于人体无毒副作用,您可以放心使用。
【药品名称】通用名称:兰索拉唑肠溶胶囊商品名称:兰索拉唑肠溶胶囊(达克普隆)拼音全码:LanSuoLaZuoJiaoNang(DaKePuLong)【主要成份】兰索拉唑。
化学名:(&plusmn;)-2[[[3-甲基-4-(2,2,2-三氟乙氧基)-2-吡啶基]甲基]亚硫酰基]苯并咪唑。
分子式:C16H14F3N3O2S分子量:369.37【性状】本品为白色胶囊,内容物为白色或类白色肠溶球状颗粒。
【适应症/功能主治】胃溃疡、十二指肠溃疡、返流性食道炎、卓-艾综合征(Zollinger-Ellison症候群)、吻合口溃疡。
【规格型号】30mg*14s【用法用量】1.胃溃疡,十二指肠溃疡,吻合口溃疡,卓-艾综合征:通常成人每日一次,口服兰索拉唑30mg。
胃溃疡和吻合口溃疡,连续服用8周。
十二指肠溃疡需连续服用6周。
2.返流性食管炎:通常成人每日一次,口服兰索拉唑30mg,连续服用8周。
对反复发和复发性返流性食管炎的维持治疗,每日一次,口服15mg,如症状缓解不明显可加量至30mg。
【不良反应】1.过敏症:偶有皮疹、瘙痒等症状,如出现上述症状时请停止用药。
2.肝脏:偶有GOT、GPT、AL-P、LDH、γ-GTP 上升等现象,所以须细心观察,如有异常现象应采取停药等适应的处置。
3.血液:偶有贫血、白细胞减少,嗜酸球增多等症状,血小板减少之症状极少发生。
4.消化器:偶有便秘,腹泻,口渴,腹胀等症状。
5.精神神经系:偶尔头痛、嗜睡等症状。
失眠,头晕等症状极少发生。
6.其他:偶有发热,总胆固醇上升,尿酸上升等症状。
兰索拉唑
成份
本品主要成份为:兰索拉唑。
化学名称:2-[[[3-甲基-4-(2,2,2-三氟乙氧基)-2-吡啶基]甲基]-亚磺酰基]-1H-苯并咪唑。
化学结构式:
分子式:C16H14F3N3O2S
分子量:369.37
性状
本品为肠溶片,除去包衣后显白色或淡黄褐色。
适应症
胃溃疡、十二指肠溃疡、反流性食管炎、卓-艾(Zollinger-Ellison)综合征(胃泌素瘤)。
用法用量
口服,不可咀嚼,通常成人口服兰索拉唑片,每日一次,一次1至2片(15-30mg)。
十二指肠溃疡,需连续服用4-6周;胃溃疡反流性食管炎、卓-艾综合征,需连续服用6-8周;或遵医嘱。
不良反应
1.过敏反应:偶有皮疹、瘙痒等症状,如出现上述症状时请停止用药。
2.血液系统:偶有贫血、白细胞减少,嗜酸球增多等症状,血小板减少之症状极少发生
3.消化系统:偶有便秘,腹泻,口渴,腹胀等症状。
偶有GOT、GPT、ALP、LDH、γ-GTP 上升等现象,所以须细心观察,如有异常现象就应采取停药等适当的处置。
4.精神神经系统:偶有头痛、嗜睡等症状。
失眠,头晕等症状极少发生。
5.泌尿生殖系统:可出现尿频、蛋白尿、阳瘘等。
6.其他:偶有发热,总胆固醇上升,尿酸上升等症状.
禁忌
对本品过敏者禁用。
注意事项
(1)治疗过程中应注意观察,因长期使用的经验不足,暂不推荐用于维持治疗。
(2)本品服用时请不要嚼碎,应整片用水吞服。
(3)肝功能障碍者及高龄者须慎用。
(4)使用本品有时会掩盖胃癌的症状,所以要在排除胃癌可能性的基础上方可给药。
孕妇及哺乳期妇女用药
1.有报道,在动物实验中胎仔的药物血浆浓度高于母体的血浆浓度,所以对于孕妇或有怀孕可能的妇女,只有在判定治疗的益处超过危险性的情况下方可使用。
2.动物实验显示兰索拉唑会分布于乳汁中,故哺乳期妇女最好避免用药,必须应用时应避免哺乳。
儿童用药
对儿童用药的安全性尚未被确立(小儿的临床经验极少)。
老年用药
一般而言,老年患者的胃酸分泌能力和其他生理机能均会降低,用药期间请注意观察。
药物相互作用
兰索拉唑会延迟安定(diazepam)及苯妥英钠(phenytoin)的代谢与排泄,使对乙酰氨基酚的血药浓度峰值升高,达峰时间缩短。
药物过量
未进行该项试验且无可参考文献。
药理毒理
药理作用:
本品为苯并咪唑类化合物,口服吸收后转移至胃黏膜,在酸性条件下转化为活性代谢体,该活化体特异性地抑制胃壁细胞H[sup]+[/sup]/K[sup]+[/sup]-ATP酶系统而阻断胃酸分泌的
最后步骤。
本品以剂量依赖方式抑制基础胃酸分泌以及刺激状态下的胃酸分泌。
本品对胆碱和组胺H2受体无拮抗作用。
毒理研究:
遗传毒性:Ames试验、大鼠肝细胞程序外DNA合成试验以及小鼠微核试验、大鼠骨髓细胞染色体畸形试验结果均为阴性。
体外人淋巴细胞染色体畸形试验结果为阳性。
生殖毒性:口服本品150mg/kg/天(按体表面积换算,相当于人用剂量的40倍),对大鼠生殖能力和生殖行为没有影响。
致畸研究显示,妊娠大鼠口服本品150mg/kg/天,妊娠兔口服本品30mg/kg/天(按体表面积换算,相当于人用剂量的16倍),对胎仔没有致畸作用,本品及其代谢产物可以通过大鼠乳汁分泌。
致癌研究:SD大鼠连续24个月口服本品5~150mg/kg/天,结果显示本品以剂量依赖方式诱发胃肠嗜铬样(ECL)细胞增生和良性ECL细胞瘤:受试动物胃出现肠上皮化生的频率增加。
雄性大鼠睾丸间质细胞腺瘤发生率以剂量方式增加。
CD-1小鼠连续24个月口服本品15~600mg/kg/天(按体表面积换算,相当于人用剂量的2~80倍),结果本品以剂量依赖方式诱发ECL细胞增生,给药小鼠肝脏肿瘤发生率升高、300和600mg/kg/天组雄性小鼠和150和600mg/kg/天组雌性小鼠肿瘤发生率超过了该品系小鼠历史肿瘤的发生率范围。
给予本品75~600mg/kg/天小鼠发生睾丸网腺瘤。
药代动力学
兰索拉唑的生物利用度具有个体差异性。
健康成人空腹单次口服30mg,Tmax为
1.5~
2.2h,Cmax为0.75~1.15mg/l,T1/2为1.3~1.7h。
兰索拉唑在肝内被代谢为火星的代谢产物,主要经胆汁和尿排泄,尿中测不出原形药物,全部为代谢产物,至服用后24小时为止,其尿中排泄率为1
3.1~1
4.3%。
兰索拉唑在体内无蓄积性。