用 户 手 册 - 中科院自动化所 三博红外- SCIT红外测温仪红外
- 格式:pdf
- 大小:728.39 KB
- 文档页数:28
红外测温tn9工作原理红外测温TN9是一种使用红外光学技术来实现温度检测的仪器。
其工作原理可以分为三个部分,包括红外辐射、光学成像和温度计算。
红外辐射是物体发出的一种热辐射,其波长范围在0.7~1000微米之间,其中中红外波段(3~5微米)和远红外波段(8~14微米)是热辐射强度最高的两个波段。
红外测温TN9通过感知物体所发出的红外辐射来实现温度测量。
红外辐射通过物体表面的反射、散射和透过而传播。
在通过目标物体之前,红外辐射进入红外测温TN9的光学通道中,其中包括红外滤光片以及进入测温区域的镜头。
红外滤光片可以选择不同的波长,并将所选波长的红外辐射通过。
镜头将反射或透过物体表面的红外光成像于检测器上。
检测器所采用的技术是热电偶,在红外光经过滤光片和镜头后,将其转化为电信号,再经过放大后送至温度计算单元。
温度计算的计算原理是基于普朗克辐射定律、斯蒂芬·玻尔兹曼定律以及温度计算公式。
根据普朗克辐射定律,黑体的辐射功率密度与温度的四次方成正比,即E_λ=2hc ²/λ^5 x 1/(e^hc/λkT-1)。
斯蒂芬·玻尔兹曼定律则是指黑体辐射的总功率与温度的四次方成正比,即P=σAT⁴。
通过将上述两个公式联立可以得到温度计算公式T=(hc/σk)/(ln[(2hc²)/EP^5+1]),其中h为普朗克常数,c为光速,k为玻尔兹曼常数,σ为斯蒂芬·玻尔兹曼常数,E为检测器灵敏度,P为检测器输出。
红外测温TN9的工作原理基于红外辐射和光学成像原理,通过光学通道将目标物体表面的红外光成像于检测器上,并将其转化为电信号再进行温度计算。
由于其非接触式的检测方式,使得它在测量温度时具有方便、快速和安全等优点,广泛应用于冶金、化工、电力等领域的温度检测和控制。
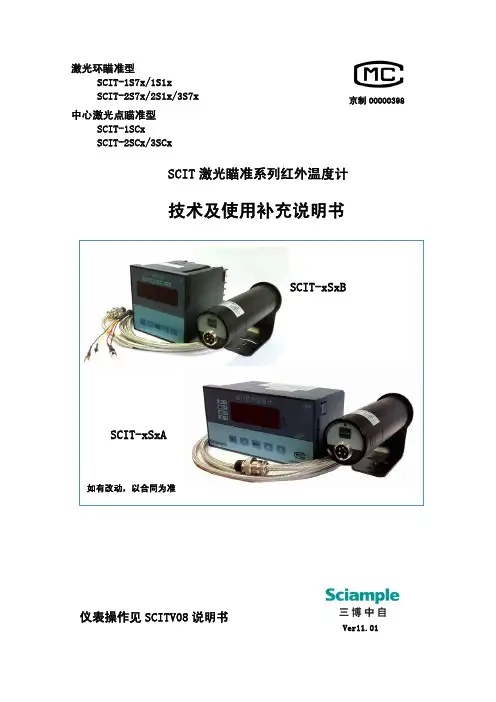
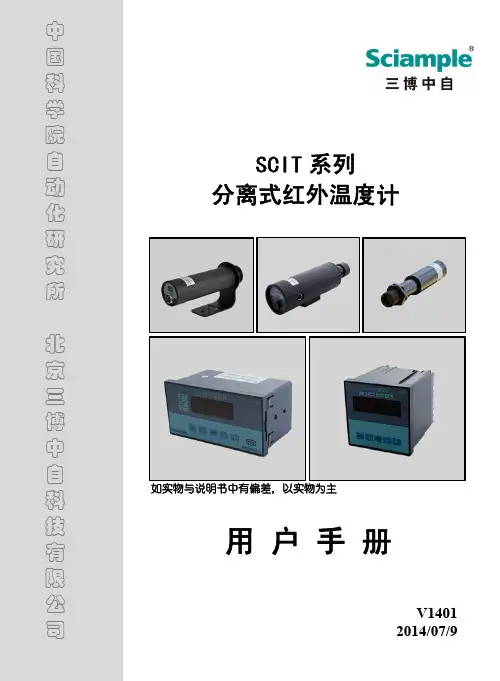
京制00000398激光环瞄准型SCIT-1S7x/1S1xSCIT-2S7x/2S1x/3S7x Ver11.01仪表操作见SCITV08说明书中心激光点瞄准型SCIT-1SCxSCIT-2SCx/3SCxSCIT 激光瞄准系列红外温度计技术及使用补充说明书SCIT-xSxBSCIT-S/SC 系列测温仪由SCIT-S/SC 测头配SCITV08A (A :160×80)或SCITV08B (B :96×96)仪表构成。
型号说明SC I T - 1 S 1 A1.技术指标*注1 :SCIT-3S7与SCIT-3SC原先型号为SCIT-2SL7与SCIT-2SCL。
3)SCITV08系列红外测温仪表技术规格型号SCITV08A SCITV08B 外形尺寸160mm ×80m 96mm ×96mm 开孔尺寸152 mm ×72m 92mm ×92m 发射率 0.10~1.10(调整步长0.01) 测温方式 实时值、最大值、平均值测量 计算间隔 最大值/平均值计算间隔:1~99秒,调整步长1秒操作与显示由 五键操作;4位LED 数码显示,4~6个LED 提示符指示报警和测温状态(可显测头环温)标准配置 接口 全隔离14bit 模拟信号输出:4mA~20mA 带继电器触点和声光指示的两个多模式报警点(,) 专用电缆 5m(可选配长至200m) 电源及功耗 AC220V±10% 小于6瓦工作环境环境温度0℃~60℃,湿度:0~80%(不结露);测头加水冷套时气冷:0~120℃;水冷:0~175℃储存温度 0℃~85℃选配件全隔离式数字接口:RS232,RS485微打接口,大屏,记录单元 2.外形安装图安装支架(标准配置为弯板支架)支架a. 外型图4-φ6φ30.51276039243258302-M3M1/4 inch φ30.5A.弯板支架B.直板支架3.瞄准本系列的测温仪用激光来进行瞄准,激光瞄准有两种: 1)激光环瞄准型; 2)激光点瞄准型(1)激光环瞄准型瞄准:中心空白圆孔为真实测温区域;用户可用激光环中心圆孔去瞄准被测目标。
双色红外测温仪使用说明1.准备工作在使用之前,确保双色红外测温仪处于正常工作状态。
检查电池电量,确认电池充足。
确保设备的红外测量窗口干净清晰,没有污垢或划痕,以保证准确测量。
2.开机和关机按下开机按钮,双色红外测温仪将开始自检程序。
在自检完成后,测温仪将进入待机模式,显示当前的环境温度。
在待机模式下,按下关机按钮可以关闭双色红外测温仪。
3.测量目标表面温度将双色红外测温仪对准目标表面,按下测量按钮。
双色红外测温仪将同时显示目标表面温度和环境温度。
确保准星对准目标表面,保持稳定不动,以获取准确的温度测量值。
4.温度单位切换使用双色红外测温仪时,可以根据需要切换温度单位。
按下单位切换按钮,可以在摄氏度(°C)和华氏度(°F)之间切换。
5.最大和最小测量值记录6.温度报警根据需要,可以设置温度报警功能。
按下报警设置按钮,可以进入温度报警设置模式。
根据双色红外测温仪的具体型号,可以设置上限温度和下限温度。
当目标表面的温度超过或低于设定的温度范围时,双色红外测温仪将发出声音或显示报警提示。
7.数据保存和传输在一些型号的双色红外测温仪中,可以保存测量的温度数据。
通过连接电脑或移动设备,可以将数据传输到电脑或移动设备进行进一步分析和处理。
8.使用注意事项-在使用双色红外测温仪之前,请阅读设备的使用说明书,并按照说明进行操作。
-在使用双色红外测温仪时,确保仪器的测量窗口清洁,没有遮挡物。
-在测量目标表面温度时,确保准星对准目标表面,保持稳定不动,以获得准确的测量值。
-双色红外测温仪测量到的温度是目标表面的温度,而非内部温度。
-在使用双色红外测温仪时,避免直接将仪器暴露在强烈的阳光下,以免影响测量精度。
-在长时间不使用时,请关闭双色红外测温仪,以节省电池电量。
以上是双色红外测温仪的使用说明,希望能对您有所帮助。
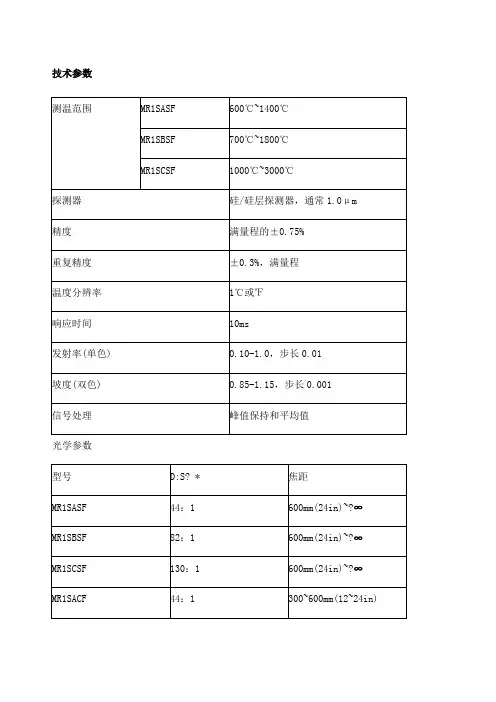
技术参数光学参数*?? 95%能量时,CF=近焦,SF=标准焦距??? 最小焦距时的最小光点尺寸*? 最小的光点尺寸直径=最小焦距/最小的D:S 一般参数电气参数仪器特点Marathon FA?红外测温仪技术参数:1、温度测量范围: 250℃到 3000℃(482°F to 5432°F)2、光学分辨率最高可达 100:13、特别适用于现场安装空间狭小的安装条件4、精度高,测量值的± 0.3%5、更快速响应时间 10 毫秒,可选到10秒6、提供模拟量和数字量输出技术参数Marathon FA 红外测温仪介绍雷泰马拉松 FA 系列红外测温仪使用光纤技术可克服测量过程中各种极端的环境条件。
FA 系列红外测温仪由电子盒和光纤探头、光缆组成,探测器和信号处理部分集成在一电子盒中,此电子盒可远距离放置,光纤探头和光缆可安装在强电磁场中的环境中,并且可耐的最高环温达200℃。
雷泰马拉松 FA 系列光纤测温仪的测温范围为250℃到3000℃(482°F to 5432°F) ,FA 光纤探头由耐用光缆将光学探头连接到电路盒上,电路盒包括:探测器、电子线路、内置用户接口、LED 显示及连接电缆的接线端子。
FA1 和FA2 系列尤其适用于目标不能接近的、恶劣的工业环境,安装空间狭小的现场测温应用。
雷泰 FA 系列单色光纤式测温仪的固定焦距的光学探头包括一个小的不锈钢圆柱形外壳和透镜,其可承受的环境温度高达200℃,并且符合NEMA-4的标准。
雷泰 FA 系列的光纤探头可装一空气吹扫器以防止透镜被污染,光缆由金属套保护,并由VITON 保护套所密封,以防止水和油的流入,这种装配可使光缆以很小的半径弯曲以便其方便地穿过狭小的空间。
雷泰 FA 系列单色光纤式测温仪还提供可在PC 上使用的WINDOWS下的马拉松软件,以实现远程进行参数设置、数据读取、数据的图形显示及RS485的多点网络配置。
红外测温仪PT300概述红外测温仪是一种能够无接触测量物体表面温度的仪器,它使用红外线辐射技术来检测物体放射出的热量。
红外测温仪PT300是一款高精度、可靠性高、操作简单的测温仪器,广泛应用于工业自动化、家庭安全等领域。
特点1.高精度测量:红外测温仪PT300采用高精度传感器和先进的算法,能够准确地测量物体表面温度,误差范围仅为±0.2℃。
2.无接触测量:红外测温仪PT300采用红外线辐射技术,不需要与被测物体直接接触,避免了接触传感器的磨损和污染问题。
3.多功能显示:红外测温仪PT300的显示屏可以同时显示实时温度、最大/最小/平均温度、温度差、发射率、测温单位等信息,提供了更丰富的测量数据。
4.大测量范围:红外测温仪PT300的测量范围为-32℃~760℃,能够满足常见物体的测量需求。
5.光标对准:红外测温仪PT300的光标可以对准被测物体的目标区域,在操作上更加便捷。
应用红外测温仪PT300具有广泛的应用领域,包括但不限于以下几个方面:1.工业自动化:PT300可用于生产线上的温度监控,如炉温控制、玻璃熔化、金属冶炼等。
2.建筑监测:PT300可用于测量建筑内墙体、天花板等物体的表面温度,以检测出是否存在能量损失和隐蔽问题。
3.家庭安全:PT300可用于检测家庭用具的温度变化,以避免烫伤、火灾等安全问题。
操作使用红外测温仪PT300非常简单,以下是具体步骤:1.开机:按下PT300的开关按钮,仪器即开始运行。
2.设定测量单位:PT300的测量单位默认为摄氏度,如果需要更改单位为华氏度,请按下设定键,然后使用增加/减少键来选择单位。
3.设定发射率:被测物体的发射率是测量温度的重要参数,需要在开始测量前设置。
可以使用设定键设置发射率,然后使用增加/减少键来调整数值。
4.对准被测物体:使用红外测温仪PT300的光标对准被测物体的目标区域,确保仪器从正确的区域测量温度。
5.开始测量:按下PT300上的测量按钮,仪器会通过红外线辐射技术进行测量,然后在显示屏上显示测量结果。
显微红外光谱法测定电路板不良焊点处的残留物黄涛宏1 吴天明21岛津国际贸易(上海)有限公司上海分析中心 200020 上海2中科院上海有机化学研究所 200032上海摘要 焊点焊接不良造成电路板缺陷。
在显微镜观察下,发现了造成焊点不良的残留物。
使用傅立叶红外显微镜分析了该残留物。
选择典型的表面喷涂有助焊剂的单面覆铜板,用工具刀刮去部分助焊剂,以露出的铜箔做为红外测量的背景,使用红外显微镜的反射模式测定了助焊剂的红外光谱。
和对照品比较,确定该助焊剂为松香。
在红外显微镜测量模式下,设定测量区域,得到污染物和助焊剂的混合光谱图。
通过差谱的方法,给出污染物的红外光谱图,谱图中出现1731 cm-1,1458 cm-1 1384 cm-1和1014 cm-1等强峰。
对照含有PCB生产工艺中涉及的助剂、基板、粘胶剂、固化剂和阻焊剂等成分的红外光谱库,确认该污染物是一种阻焊剂。
主题词红外显微镜,电路板,不良焊点,残留异物引言目前,我国的印刷电路板产业已成为世界第二大印制电路板生产大国,年销售收入已超过60亿美元。
当代电器的电路板制作中,电路板与元器件之间的焊接至关重要。
现代化的制作工艺需要保证这两者高质量的焊接,目前通常都采用波峰焊锡工艺,以流水线方式进行大批量制造。
在制作过程中,一旦出现不良焊点,就会造成原材料的大量报废和误工损失。
焊点的失效分析在电子产品质量控制中扮演着重要的角色。
傅里叶变换红外显微镜通常用于固体样品微区分析[1-3],同时也是电子及工业产品失效分析的强有力工具[4-7]。
红外显微镜获取微区样品的红外光谱能够直接显示样品的成分特征或分子结构信息。
用红外显微镜法检测不良焊点处的残留异物,可迅速判断导致焊接不良的原因,并指导改进印刷电路板的制作工艺。
1实验部分1.1实验仪器和测试参数红外光谱仪:岛津FTIR-8400S傅立叶变换红外光谱仪红外显微镜:岛津AIM-8800多媒体红外显微镜光谱测量范围:4000-720cm-1分辨率:8 cm-1采集次数:50次检测器:1型MCT检测器1.2样品对照样品:同批原材料的敷铜板一块,无孔无锡,正面铜光可见(图中右半测,下称“空白电路板”)。
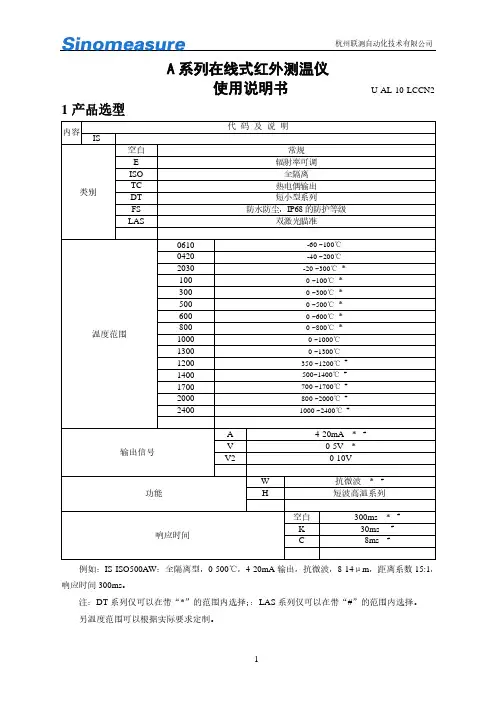
使用说明书U-AL-10-LCCN2 1产品选型内容代码及说明IS-类别空白常规E 辐射率可调ISO 全隔离TC 热电偶输出DT 短小型系列FS 防水防尘,IP68的防护等级LAS 双激光瞄准温度范围0610 -60 ~100℃0420 -40 ~200℃2030 -20 ~300℃* 100 0 ~100℃* 300 0 ~300℃* 500 0 ~500℃* 600 0 ~600℃* 800 0 ~800℃* 1000 0 ~1000℃1300 0 ~1300℃1200 350 ~1200℃# 1400 500~1400℃# 1700 700 ~1700℃# 2000 800 ~2000℃# 2400 1000 ~2400℃#输出信号A 4-20mA *# V 0-5V * V2 0-10V功能W 抗微波*# H 短波高温系列响应时间空白300ms *# K 30ms # C 8ms #例如:IS-ISO500AW:全隔离型,0-500℃,4-20mA输出,抗微波,8-14μm,距离系数15:1,响应时间300ms。
注:DT系列仅可以在带“*”的范围内选择;:LAS系列仅可以在带“#”的范围内选择。
另温度范围可以根据实际要求定制。
感谢您选择A系列红外测温仪。
红外测温仪可以不接触目标而通过测量目标发射的红外辐射强度计算出物体的表面温度。
非接触测温是红外测温仪最大的优点,使用户可以方便地测量难以接近或移动的目标。
A系列红外测温仪为一体化集成式红外测温仪,传感器、光学系统与电子线路共同集成在不锈钢壳体内;A系列易于安装,金属壳体上的标准螺纹可与安装部位快速连接;同时,A系列还有各型选件(例如吹扫器、安装支架、可调安装支架、吹扫保护套等)以满足各种工况场合要求。
3参数描述3.1基本性能保护等级 IP65 (NEMA-4)环境温度 0 ~60℃存储温度 -20 ~ 80℃相对湿度 10 – 95%(不结露)材料不锈钢电缆长度2m (标准) 默认定制长度:3.2电气参数工作电源 12~24 VDC默认 6~24 VDC3.1VDC最大电流电流系列20mA 电压系列8mA输出信号 0-5V/0-10V/4-20mA可选3.3测量参数光谱范围 8 ~ 14 µm(1.0µm 1.6µm仅为LAS系列)温度范围 -60-2400℃分段光学分辨率 4:1 25:130:1 50:1100:1注:(AW系列为15:1 DT系列为:20:1)响应时间 300ms默认 50ms8ms测温精度测量值的±1%或±1℃,取大值(环境温度23±5℃时)境温度23±5℃时)*重复精度测量值的±0.5%或±1℃,取大值(环境温度23±5℃时)测量值的±1%或±1℃,取大值(环境温度23±5℃时)*发射率 0.95 1.0默认(IS-E500A辐射率0.10-1.00可调)4外型尺寸A系列常规:L1=40mm;L2=106mmLAS 系列:L1=50mm;L2=145mm特殊定制:L1= mm;L2= mm 5光路图D:S=15:1D:S=25:1D:S=30:1D:S=50:1D:S=100:16工作原理及注意事项6.1红外测温原理任何物体都向外辐射红外能量,辐射强度随着温度的变化而变化。
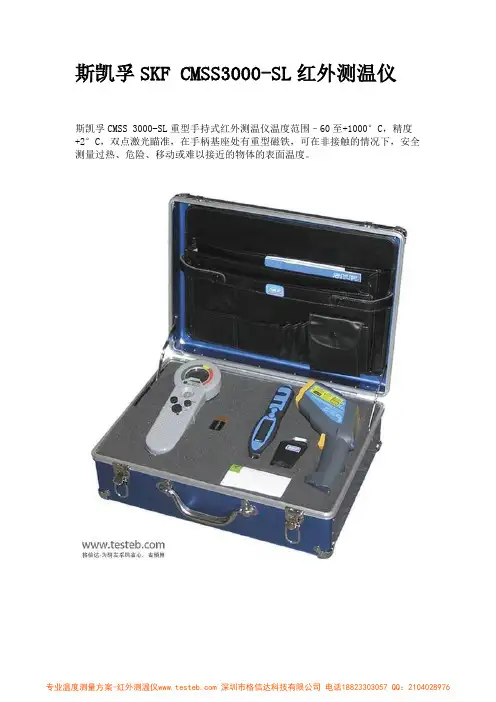
斯凯孚SKF CMSS3000-SL红外测温仪
斯凯孚CMSS 3000-SL重型手持式红外测温仪温度范围–60至+1000°C,精度+2°C,双点激光瞄准,在手柄基座处有重型磁铁,可在非接触的情况下,安全测量过热、危险、移动或难以接近的物体的表面温度。
SKF CMSS3000-SL红外测温仪特点
手持式非接触式测温,坚固耐用使用方便
可在不接触的情况下,安全测量过热、危险、移动或难以接近的物体的表面温度
双点激光瞄准,可调节的辐射率,距离比率50:1
温度范围–60至+1000°C(–75至+1800°F)
最大值、最小值、温差、平均温度显示
CMSS 3000-SL红外测温仪在手柄基座处有重型磁铁
LCD背光显示,高强度白色LCD手电筒
超长电池寿命,高和低警报级别
斯凯孚SKF CMSS3000-SL重型手持式红外测温仪技术参数
格信达科技专注于:电学测试、温度测量、无损检测及环境测量,配套电子焊台、测量工具、手动工具,以及进口机电之通讯器、编码器、传感器等产品的选型方案及供应。
致力于通过合理的渠道,为用户提供最佳的服务与最快的响应、最优的价格、最快的交货和放心保障。

optris®CSlaser LT/ 2M ¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯¯红外测温仪操 作 手 册•北京时代瑞资科技有限公司网 址:北京时代瑞资科技有限公司 网 址:CE认证本产品符合下列标准:电磁兼容性 EN 61326-1:2006(基本要求)EN 61326-2-3:2006安全规则EN 61010-1:2001激光安全 EN 60825-1:2007本产品满足:电子兼容性要求2004/108/EG低电压要求2006/95/EG使用之前仔细阅读此手册。
附录一:英文技术资料翻译英文原文:Emerg Infect Dis. 2008 August; 14(8): 1255–1258.doi: 10.3201/eid1408.080059PMCID: PMC2600390Cutaneous Infrared Thermometry for Detecting Febrile PatientsPierre Hausfater, Yan Zhao, Stéphanie Defrenne, Pascale Bonnet, and Bruno Riou* Author information Copyright and License informationThis article has been cited by other articles in PMC.AbstractWe assessed the accuracy of cutaneous infrared thermometry, which measures temperature on the forehead, for detecting patients with fever in patients admitted to an emergency department. Although negative predictive value was excellent (0.99), positive predictive value was low (0.10). Therefore, we question mass detection of febrile patients by using this method.Keywords: Fever, mass detection, cutaneous infrared thermometry, infectious diseases, emergency, dispatchRecent efforts to control spread of epidemic infectious diseases have prompted health officials to develop rapid screening processes to detect febrile patients. Such screening may take place at hospital entry, mainly in the emergency department, or at airports to detect travelers with increased body temperatures (1–3). Infrared thermal imaging devices have been proposed as a noncontact and noninvasive method for detecting fever (4–6). However, few studies have assessed their capacity for accurate detection of febrile patients in clinical settings. Therefore, we undertook a prospective study in an emergency department to assess diagnostic accuracy of infrared thermal imaging.The StudyThe study was performed in an emergency department of a large academic hospital (1,800 beds) and was reviewed and approved by our institutional review board (Comitéde Protection des Personnes se Prêtant àla Recherche Biomédicale Pitié-Salpêtrière, Paris, France). Patients admitted to the emergency department were assessed by a trained triage nurse, and several variables were routinely measured, including tympanic temperature by using an infrared tympanic thermometer (Pro4000; Welch Allyn, Skaneateles Falls, NY, USA), systolic and diastolic arterial blood pressure, and heart rate.Tympanic temperature was measured twice (once in the left ear and once in the right ear). This temperature was used as a reference because it is routinely used in our emergency department and is an appropriate estimate of central core temperature (7–9). Cutaneous temperature was measured on the forehead by using an infrared thermometer (Raynger MX; Raytek, Berlin, Germany) (Figure 1). Rationale for an infrared thermometer device instead of a larger thermal scanner was that we wanted to test a method (i.e., measurement of forehead cutaneous temperature by using a simple infrared thermometer) and not a specific device. The forehead region was chosen because it is more reliable than the region behind the eyes (5,10). The latter region may not be appropriate for mass screening because one cannot accurately measure temperature through eyeglasses, which are worn by many persons. Outdoor and indoor temperatures were also recorded.Figure 1Measurement of cutaneous temperature with an infrared thermometer. A) The device is placed 20 cm from the forehead. B) As soon as the examiner pulls the trigger, the temperature measured is shown on the display. Used with permission.The main objective of our study was to assess diagnostic accuracy of infrared thermometry for detecting patients with fever, defined as a tympanic temperature >38.0°C. The second objective was to compare measurements of cutaneous temperature and tympanic temperature, with the latter being used as a reference point. Data are expressed as mean ± standard deviation (SD) or percentages and their 95% confidence intervals (CIs). Comparison of 2 means was performed by using the Student t test, and comparison of 2 proportions was performed by using the Fisher exact method. Bias, precision (in absolute values and percentages), and number of outliers (defined as a difference >1°C) were also recorded. Correlation between 2 variables was assessed by using the least square method. The Bland and Altman method was used to compare 2 sets of measurements, and the limit of agreement was defined as ±2 SDs of the differences (11). We determined the receiver operating characteristic (ROC) curves and calculated the area under the ROC curve and its 95% CI. The ROC curve was used to determine the best threshold for the definition of hyperthermia for cutaneous temperature to predict a tympanic temperature >38°C. We performed multivariate regression analysis to assess variables associated with thedifference between tympanic and infrared measurements. All statistical tests were 2-sided, and a p value <0.05 was required to reject the null hypothesis. Statistical analysis was performed by using Number Cruncher Statistical Systems 2001 software (Statistical Solutions Ltd., Cork, Ireland).A total of 2,026 patients were enrolled in the study: 1,146 (57%) men and 880 (43%) women 46 ± 19 years of age (range 6–103 years); 219 (11%) were >75 years of age, and 62 (3%) had a tympanic temperature >38°C. Mean tympanic temperature was 36.7°C ± 0.6°C (range 33.7°C–40.2°C), and mean cutaneous temperature was 36.7°C ± 1.7°C (range 32.0°C–42.6°C). Mean systolic arterial blood pressure was 130 ± 19 mm Hg, mean diastolic blood pressure was 79 ± 13 mm Hg, and mean heart rate was 86 ± 17 beats/min. Mean indoor temperature was 24.8°C ± 1.1°C (range 20°C–28°C), and mean outdoor temperature was 10.8°C ± 6.8°C (range 0°C–32°C). Reproducibility of infrared measurements was assessed in 256 patients. Bias was 0.04°C ± 0.35°C, precision was 0.22°C ± 0.27°C (i.e., 0.6 ± 0.7%), and percentage of outliers >1°C was 2.3%.Diagnostic performance of cutaneous temperature measurement is shown in Table 1. For the threshold of the definition of tympanic hyperthermia definition used (37.5°C, 38°C, or 38.5°C), sensitivity of cutaneous temperature was lower than that expected and positive predictive value was low. We attempted to determine the best threshold (definition of hyperthermia) by using cutaneous temperature to predict a tympanic temperature >38°C (Figure 2, panel A). Area under the ROC curve was 0.873 (95% CI 0.807–0.917, p<0.001). The best threshold for cutaneous hyperthermia definition was 38.0°C, a condition already assessed in Table 1. Figure 2, panels B and C shows the correlation between cutaneous and tympanic temperature measurements (Bland and Altman diagrams). Correlation between cutaneous and tympanic measurements was poor, and the infrared thermometer underestimated body temperature at low values and overestimated it at high values. Multiple regression analysis showed that 3 variables (tympanic temperature, outdoor temperature, and age) were significantly (p<0.001) and independently correlated with the magnitude of the difference between cutaneous and tympanic measurements (Table 2).Table 1Assessment of diagnostic performance of cutaneous temperature inpredicting increased tympanic temperature*Figure 2A) Comparison of receiver operating characteristic (ROC) curves showing relationship between sensitivity (true positive) and 1 – specificity (true negative) in determining value of cutaneous temperature for predicting various thresholds of hyperthermia ...Table 2Variables correlated with magnitude of the difference between cutaneous and tympanic temperature measurements*ConclusionsInfrared thermometry does not reliably detect febrile patients because its sensitivity was lower than that expected and the positive predictive value was low, which indicated a high proportion of false-positive results. Ng et al. (5) studied 502 patients, concluded that an infrared thermal imager can appropriately identify febrile patients, and reported a high area under the ROC curve value (0.972), which is similar to the area we found in the present study (0.925). However, such global assessment is of limited value because of low incidence of fever in the population. Rather than looking at positive predictive value or accuracy, one should determine negative predictive value. This determination might be of greater consequence if one considers an air traveler population or a population entering a hospital.Ng et al. (5) identified outdoor temperature as a confounding variable in cutaneous temperature measurement. Our study identified age as a variable that interferes with cutaneous measurement, but the role of gender is less obvious. Older persons showed impaired defense (stability) of core temperatures during cold and heat stresses, and their cutaneous vascular reactivity was reduced (12,13).Use of a simple infrared thermometry, rather than sophisticated imaging, should not be considered a limitation because this method concerns the relationship between cutaneous and central core temperatures. We can extrapolate our results to any devices that estimate cutaneous temperature and the software used to average it. Our study attempted to detect febrile patients, not infected patients. For mass detection of infection, focusing on fever means that nonfebrile patients are not detected. This last point is useful because fever is not a constant phenomenon during an infectious disease, antipyretic drugs may have been taken by patients, and a hypothermic ratherthan hyperthermic reaction may occur during an infectious process.In conclusion, we observed that cutaneous temperature measurement by using infrared thermometry does not provide a reliable basis for screening outpatients who are febrile because the gradient between cutaneous and core temperatures is markedly influenced by patient’s age and environmental characteristics. Mass detection of febrile patients by using this technique cannot be envisaged without accepting a high rate of false-positive results.AcknowledgmentWe thank David Baker for reviewing the manuscript.This study was supported by the Direction Générale de la Santé, Ministère de la Santé et de la Solidarité, Paris, France.Biography• Dr Hausfater is an internal medicine specialist in the emergency department of Centre Hospitalier Universitaire Pitié-Salpêtrière in Paris. His primary research interests are biomarkers of infection and inflammatory and infectious diseases. References1. Kaydos-Daniels SC, Olowokure B, Chang HJ, Barwick RS, Deng JF, Kuo SH, et al. ; SARS International Field Team. Body temperature monitoring and SARS fever hotline. Emerg Infect Dis2004;10:373–6. [PMC free article] [PubMed]2. Chng SY, Chia F, Leong KK, Kwang YPK, Ma S, Lee BW, et al. Mandatory temperature monitoring in schools during SARS. Arch Dis Child 2004;89:738–9. doi: 10.1136/adc.2003.047084. [PMC free article][PubMed] [Cross Ref]3. St John RK, King A, de Jong D, Brodie-Collins M, Squires SG, Tam TW Border screening for SARS.Emerg Infect Dis 2005;11:6–10. [PMC free article] [PubMed]4. Hughes WT, Patterson GG, Thronton D, Williams BJ, Lott L, Dodge R Detection of fever with infrared thermometry: a feasibility study. J Infect Dis 1985;152:301–6. [PubMed]5. Ng EY, Kaw GJ, Chang WM Analysis of IR thermal imager for mass blind fever screening. Microvasc Res 2004;68:104–9. doi: 10.1016/j.mvr.2004.05.003. [PubMed] [Cross Ref]6. Erickson RS, Meyer LT Accuracy of infrared ear thermometry and other temperature methods in adults. Am J Crit Care 1994;3:40–54. [PubMed]中文译文:新发传染性疾病.2008八月;14(8):1255–1258.DOI:10.3201/eid1408.080059PMCID: PMC2600390 红外测温仪检测发热患者的皮肤彼埃尔侯司法特,赵岩,史蒂芬妮德弗雷纳,帕斯卡尔,和布鲁诺里乌摘要我们评估皮肤红外测温的准确性,通过病人的额头检测温度,发热病人进入急科室进行检测。
红外测温仪H4 PLUS说明书红外测温的使用方法比较的简单和安全,可以快速提供温度测量,并且可以安全地读取难以接近的或不可到达的目标温度。
1、右手握住测温仪手柄,食指扣动一下开关,将听到“BI-BI”的声音,电源接通,屏幕将显示你正对物体的温度,测量时要注意距离系数K,本机KD:S12:1,通俗理解为测量范围为12m远时,被测物体面积为直径1米的圆,如果大于12m处存在一个1m直径的物体,测量的物体温度将不准确。
2、要测量物体,将镜头正对被测物体,按住开关将进行测量,这时屏幕左上侧将出现扫描(SCAN)符号,表示正在测量,松开开关,屏幕左上侧将出现保持(HOLD)符号,这是屏幕上显示的即是被测物体温度。
3、在视线不清或者黑暗的环境中使用该仪器,先松开电源开关按钮,然后按一下镭射/背光灯(LASER/BACKLIT)按键,这是屏幕上将显示镭射/背光灯符号,这是按下开关测量,将会看到被测物体上出现红色小点,表明正在对该区域进行测温。
不用时,松开电源开关键,再按镭射/背光灯按钮,按一下无镭射,按两下无背光灯,按三下没有背光灯和镭射。
4、在检测一个面(如密闭)时,可用定点法,每次测定时必须及时记录。
测量数据自动保持7秒,没有操作,30秒自动关机。
背光灯延迟十秒后自动关闭。
二、红外线测温仪使用注意事项1、必须准确确定被测物体的发射率。
只测量表面温度,红外测温仪不能测量内部温度。
2、波长在5um以上不能透过石英玻璃进行测温,玻璃有很特殊的反射和透过特性,不允许精确红外温度读数。
但可通过红外窗口测温。
红外测温仪最好不用于光亮的或抛光的金属表面的测温(不锈钢、铝等)。
3、定位热点,要发现热点,仪器瞄准目标,然后在目标上作上下扫描运动,直至确定热点。
4、注意环境条件:蒸汽、尘土、烟雾等。
它阻挡仪器的光学系统而影响精确测温。
5、环境温度,如果测温仪突然暴露在环境温差为20℃或更高的情况下,允许仪器在20分钟内调节到新的环境温度。
中科院推出红外测温仪
佚名
【期刊名称】《上海生物医学工程》
【年(卷),期】2003(24)2
【摘要】中科院上海技术物理研究所已于日前研制出两台红外测温仪样机。
该仪器通过接受人体红外线辐射来检测人体表面温度,可在一到两秒内完成测试,快速、有效地筛查出公共场所人流中的高体温人员。
【总页数】1页(P34-34)
【关键词】中科院;红外测温仪;体温;人体;测试
【正文语种】中文
【中图分类】R443.5
【相关文献】
1.红外测温仪进入创新时代--德国欧普士荣誉推出LS红外测温仪 [J],
2.红外测温仪进入创新朝代——德国欧普士荣誉推出LS红外测温仪 [J],
3.美国理想推出新型非接触式红外测温仪 [J], 无
4.美国菲力尔公司(FLIR Systems)推出创新性TG165红外成像测温仪 [J],
5.美国理想推出新型非接触式红外测温仪——新型红外测温仪经济实用,灵活多用,使用简便 [J],
因版权原因,仅展示原文概要,查看原文内容请购买。