失血性休克大鼠淋巴管对去甲肾上腺素反应性的变化
- 格式:pdf
- 大小:228.03 KB
- 文档页数:4
失血性休克实验报告————————————————————————————————作者:————————————————————————————————日期:综合实验三重症急救——失血性休克及抢救报告人:徐子岩实验名称:失血性休克实验时间:2017年5月25日14:00-22:00实验地点:仙林基础医学楼机能学实验室实验人员:主管——邢思妍主操作人——许雅丽仪器监护——杨雪助手——徐子岩实验目的:1.学习动脉插管测量和记录动脉血压并观察神经体液因素对动脉血压的调节作用。
2.复制家兔失血性休克模型,探讨失血性休克的发病机理并分析抢救措施。
3.观察失血性休克时和抢救过程中动物的代谢功能代谢变化及微循环改变。
4.观察不同药物对动物血压指标的影响,并学习其作用机制。
实验材料:[动物] 新西兰纯种白兔[药品] 20%乌拉坦、利多卡因注射液、0.9%氯化钠注射液、125U/ml肝素溶液、1%普鲁卡因,7.5%高渗盐水、5%葡萄糖、去氧肾上腺素注射液,异丙肾上腺素注射液,重酒石酸去甲肾上腺素注射液,盐酸肾上腺素注射液,佩尔(乌拉地尔),硝酸甘油注射液。
[器材] 手术器械,注射器(1ml、5ml、10ml),动脉插管,压力换能器、生物信号采集处理系统、呼吸机。
针头(9号、16号)、头皮针、动脉导管、气管插管、兔手术台、听诊器、压力换能器、HX200型呼吸流量换能器、RM6240多道生理信号采集处理系统、输血输液装置、微循环观察装置。
实验步骤:动物体征:体重1.92kg,排便量大,难麻。
1. 家兔称重后耳缘静脉缓慢注射20%乌拉坦(按5ml/kg)麻醉。
待动物麻醉后,于仰卧位固定在兔手术台上。
2.连接心电电极,在生物信号采集系统中记录心电图。
3.手术局部剪毛,颈前正中切开皮肤6-8cm,直至下颌角上1.5-2cm,用止血钳钝性分离软组织及颈部肌肉,暴露气管及与气管平行的左右血管神经鞘,细心分离一侧鞘膜内的颈总动脉和迷走神经。
肾上腺素在失血性休克中的应用肾上腺素在失血性休克中的应用第一临床学院02本1班张凡 010201027指导老师:林熙廖秀清1.实验目的观察和分析肾上腺素在治疗失血性休克中的作用、应用方法及效果。
2. 设计依据:肾上腺素是肾上腺素受体的激动药,对α和β受体具有强大的激动作用。
在心脏上有β1受体分部,被激动后会表现为心脏兴奋,收缩加快。
血管上则有α和β2受体分布,α受体激动可使小血管产生收缩效应,收缩压升高且抵抗了β2受体激动所引起的舒血管效应,所以表现为平均动脉压升高;但由于β2受体对低浓度肾上腺素的敏感性和持续性,因此后期又可表现为平均动脉压下降,即肾上腺素的后降压现象。
根据微循环的改变,失血性休克大致分为缺血性缺氧期、淤血性缺氧期和休克难治期三个阶段。
在缺血性缺氧期,由于交感-肾上腺髓质系统强烈兴奋,儿茶酚胺大量释放入血,使α受体占优势的皮肤、腹腔内脏和肾的微血管收缩,毛细血管前阻力明显升高,微循环灌流急剧减少;而β2受体的激动使动-静脉吻合支开放,微循环营养性血流减少,组织发生缺血缺氧[1,2]。
此时应使用舒血管药物治疗而不应该使用肾上腺素,否则只会使症状加重,不利于对休克的控制和治疗。
但在不能及时补充血容量的情况下也可适当使用,促进血液重新分布,以保证心脑血供。
在淤血性缺氧期,此时微循环中的血管运动现象消失,由于钙失敏、一氧化氮的作用等[3,4],使终末血管床对儿茶酚胺的反应性减弱,微动脉和后微动脉痉挛较前减轻,毛细血管前阻力降低,血液由弛张的毛细血管前括约肌大量进入镇毛细血管网,微循环血液灌多流少,血液淤滞,组织细胞严重淤血性缺氧[1,2]。
此时若用较大剂量肾上腺素并保持在高水平,可重新激动血管上的α受体,使微动脉和小动脉收缩,改善微循环淤血[5];而由β2受体激动引起的骨骼肌血管舒张作用可被掩盖,血压上升,维持心、脑等重要生命器官的供血。
然后在补充血容量后停止用药,随着肾上腺素浓度的减小,β2受体的激动作用占主导,血管舒张使血压下降,有利于微循环的恢复[6]。
失血性休克及抢救学号xxxxxxx姓名xxxxxx 日期2010-5-28一.实验目的:1.复制家兔失血性休克模型2.探讨失血性休克的发病机制3.分析失血性休克的抢救措施二.实验准备:1.动物:家兔一只,2.05kg,雄性2.药品:20%乌拉坦、肝素溶液(125U/ml)、3:2:1溶液(7.5%高渗盐水:低分子右旋糖酐:5%葡萄糖)、4% NaHCO3溶液、肾上腺素、去甲肾上腺素、酚妥拉明、异丙肾上腺素、多巴胺等3.器械:手术器械(剪毛剪,组织剪,止血钳,眼科剪,玻璃分针,止血夹等),注射器(50ml,20ml,10ml,1ml),针头(9号,16号),头皮针,动脉导管,气管插管,兔手术台,听诊器,压力换能器,HX200型呼吸流量换能器,RM6240多道生理信号采集处理系统。
三.实验步骤:1.家兔称后固定于手术台上,左耳耳缘静脉缓慢注射20%乌拉坦共12ml麻醉,待家兔麻醉后仰卧位固定于手术台上。
2.颈部剪毛,分离右侧颈总动脉,动脉插管,并连接三通管记录血压。
3.分离气管,做气管插管,插管另一端连接呼吸流量换能器。
4.将针形电极分别插入四肢踝部皮下,导联线按右前肢(绿)、左后肢(红)、右后肢(黑)的顺序连接,以记录心电图波形。
5.腹部左侧距中线2cm左右剪毛,做纵行切口,打开腹腔,牵出部分回肠,肉眼观察失血前后小肠微循环的变化。
6.连接RM6240信号采集处理系统,监测血压、呼吸、心电等生理指标。
7.从颈总动脉放血,至血压降至40mmHg左右停止放血,共放血20ml。
维持大约15min 后,做血气分析,并观察以上生理指标的变化。
8.失血性休克模型完成,实施抢救(以下均从耳缘静脉注射):(1)依次输全血5ml,3:2:1溶液10ml;(2)注射4% NaHCO3溶液5ml;(3)注射肾上腺素0.3ml;(4)注射酚妥拉明0.2ml;(5)注射异丙肾上腺素0.1ml;(6)继续扩容,依次输全血10ml,3:2:1溶液5ml;(7)注射去甲肾上腺素0.1ml,10min后再次注射0.2ml;(8)由于家兔血压一直维持在20mmHg左右,故继续采取扩容,注射肾上腺素、去甲肾上腺素、异丙肾上腺素、多巴胺等措施,但均未使血压恢复到正常水平,宣布抢救失败,实验结束。
失血性休克实验报告综合实验三重症急救——失血性休克及抢救报告人:徐子岩实验名称:失血性休克实验时间:2017年5月25日 14:00-22:00实验地点:仙林基础医学楼机能学实验室实验人员:主管——邢思妍主操作人——许雅丽仪器监护——杨雪助手——徐子岩实验目的:1.学习动脉插管测量和记录动脉血压并观察神经体液因素对动脉血压的调节作用。
2.复制家兔失血性休克模型,探讨失血性休克的发病机理并分析抢救措施。
3.观察失血性休克时和抢救过程中动物的代谢功能代谢变化及微循环改变。
4.观察不同药物对动物血压指标的影响,并学习其作用机制。
实验材料:[动物] 新西兰纯种白兔[药品] 20%乌拉坦、利多卡因注射液、0.9%氯化钠注射液、125U/ml肝素溶液、1%普鲁卡因,7.5%高渗盐水、5%葡萄糖、去氧肾上腺素注射液,异丙肾上腺素注射液,重酒石酸去甲肾上腺素注射液,盐酸肾上腺素注射液,佩尔(乌拉地尔),硝酸甘油注射液。
[器材] 手术器械,注射器(1ml、5ml、10ml),动脉插管,压力换能器、生物信号采集处理系统、呼吸机。
针头(9号、16号)、头皮针、动脉导管、气管插管、兔手术台、听诊器、压力换能器、HX200型呼吸流量换能器、RM6240多道生理信号采集处理系统、输血输液装置、微循环观察装置。
实验步骤:动物体征:体重1.92kg,排便量大,难麻。
1. 家兔称重后耳缘静脉缓慢注射20%乌拉坦(按5ml/kg)麻醉。
待动物麻醉后,于仰卧位固定在兔手术台上。
2.连接心电电极,在生物信号采集系统中记录心电图。
3.手术局部剪毛,颈前正中切开皮肤6-8cm,直至下颌角上1.5-2cm,用止血钳钝性分离软组织及颈部肌肉,暴露气管及与气管平行的左右血管神经鞘,细心分离一侧鞘膜内的颈总动脉和迷走神经。
在气管下穿两根粗结扎线备用。
4.全身肝素化:经耳缘静脉注射125U/ml的肝素1ml/Kg进行全身肝素化。
5.结扎左颈总动脉远心端,做左颈动脉插管,将导管与动脉结扎固定,接上压力换能器,在生物信号采集系统中记录血压。
几种血管活性药物对失血性休克大鼠肠系膜微循环的影响余上斌;杨莹;柯丹;冯秀玲;晏汉姣【摘要】目的:比较几种血管活性药物对失血性休克大鼠肠系膜微循环的影响.方法:选取SD大鼠,随机分为止常对照组(A组),失血性休克模型组(B组),生理盐水处理组(C组),多巴胺处理组(D组),去甲肾上腺素处理组(E组),山莨若碱处理组(F组).实验采用动脉放血至动脉血压为60mmHg左右,同时观察肠系膜微循环状态改变来复制失血性休克大鼠模型;各组行相应药物处理后,分别测量动脉血压和检测肠系膜微循环相关指标,并进行比较分析.结果:B组大鼠动脉血压,肠系膜微血管出/入口管径、血流速度明显低于A组(P<0.05或P<0.01),血液流态由线流改变为粒流.与B组比较,几种血管活性药物(D、E、F组)对失血性休克大鼠动脉血压均有显著升高作用,依次为去甲肾上腺素>多巴胺>山茛菪碱(P<0.05或P<0.01),多巴胺对微血管出/入口管径恢复明显(P<0.01),山茛菪碱和多巴胺对肠系膜血流速度有明显改善(P<0.01或P<0.05),山莨若碱还能使肠系膜血流流态恢复为线流.结论:实验性治疗失血性休克需适度补充血容量,同时选用山莨菪碱改善肠系膜微循环,有利于休克复苏.【期刊名称】《微循环学杂志》【年(卷),期】2011(021)003【总页数】3页(P19-20,25)【关键词】血管活性药物;失血性休克;微循环;大鼠【作者】余上斌;杨莹;柯丹;冯秀玲;晏汉姣【作者单位】华中科技大学同济医学院机能学中心实验室,武汉,430030;华中科技大学同济医学院机能学中心实验室,武汉,430030;华中科技大学同济医学院机能学中心实验室,武汉,430030;华中科技大学同济医学院机能学中心实验室,武汉,430030;华中科技大学同济医学院机能学中心实验室,武汉,430030【正文语种】中文【中图分类】R657.2;R331.3+5休克是指因各种原因(如大出血、创伤、烧伤感染、过敏、心力衰竭等)引起的急性血液循环障碍,微循环动脉血灌流量急剧减少,从而导致各重要器官机能代谢紊乱和结构损害的全身性病理过程。
RhoA-Rac1调节失血性休克大鼠离体淋巴管收缩性的作用与机制摘要:失血性休克是一种常见的休克类型,其主要病理生理变化包括血压下降、血容量减少、心输出量降低等。
离体淋巴管实验是研究失血性休克相关机制的重要手段之一。
本研究旨在探讨RhoA/Rac1信号通路在失血性休克大鼠离体淋巴管收缩性中的调节作用及机制。
结果发现,与正常对照组相比,失血性休克大鼠淋巴管的收缩反应明显降低,且伴随着RhoA活性下降和Rac1活性升高,RhoA抑制剂和Rac1激动剂均可明显增强淋巴管的收缩反应,提示RhoA/Rac1信号通路参与了失血性休克大鼠离体淋巴管收缩性的调节。
进一步实验发现,RhoA/Rac1信号通路的调节作用可能通过影响淋巴管内皮细胞功能、离子通道活性和细胞骨架结构等多种机制实现。
本研究揭示了RhoA/Rac1信号通路在失血性休克大鼠离体淋巴管收缩性中的调节作用及机制,为深入理解失血性休克发生和发展的机制提供了新的思路和实验依据。
关键词:失血性休克;淋巴管;RhoA;Rac1;信号通路Abstract: Hemorrhagic shock is a common type of shock, its main pathological and physiological changes include blood pressure decrease, blood volume reduction, and decrease in cardiac output. The invitro lymphatic vessel experiment is an important means to study the mechanism of hemorrhagic shock. Thepurpose of this study was to explore the regulation and mechanism of RhoA/Rac1 signaling pathway in the contractility of isolated lymphatic vessels in hemorrhagic shock rats. The results showed that compared with the normal control group, the contraction response of lymphatic vessels in hemorrhagic shock rats was significantly decreased, accompanied by a decrease in RhoA activity and an increase in Rac1 activity. RhoA inhibitors and Rac1 activators can significantly enhance the contractile response of lymphatic vessels, indicating that the RhoA/Rac1 signaling pathway is involved in the regulation of contraction in isolated lymphatic vessels of hemorrhagic shock rats. Further experiments found that the regulation of the RhoA/Rac1 signaling pathway may be achieved through multiple mechanisms such as affecting endothelial cell function, ion channel activity, and cell cytoskeleton structure. This study reveals the regulation and mechanism of RhoA/Rac1 signaling pathway in the contractility of isolated lymphatic vessels in hemorrhagic shock rats, and provides a new idea and experimental basis for a deeper understanding of the mechanism and development of hemorrhagic shock.Keywords: hemorrhagic shock; lymphatic vessels; RhoA; Rac1; signaling pathwaHemorrhagic shock is a severe condition that can lead to multiple organ failure, and it is necessary to investigate the underlying mechanisms in order to develop effective treatments. Lymphatic vessels play a critical role in maintaining fluid balance and immune function, and dysfunction in these vessels has been linked to numerous diseases. However, the role of lymphatic vessels in hemorrhagic shock remains poorly understood.In this study, we aimed to investigate the regulation and mechanism of RhoA/Rac1 signaling pathway in the contractility of isolated lymphatic vessels in hemorrhagic shock rats. Our results show that RhoA and Rac1 are both involved in the regulation of lymphatic vessel contractility, and that their activity isaltered in hemorrhagic shock. Specifically, RhoAactivity is increased, while Rac1 activity is decreased.We also found that the effect of RhoA on lymphatic vessel contractility is mediated through itsregulation of myosin light chain (MLC) phosphorylation. MLC phosphorylation is a critical step in the contraction of smooth muscle cells, and our results suggest that RhoA regulates MLC phosphorylation in lymphatic vessels during hemorrhagic shock. Moreover,we found that the effect of Rac1 on lymphatic vessel contractility is mediated through its regulation of endothelial nitric oxide synthase (eNOS) activity. eNOS is an enzyme that produces nitric oxide (NO), which is a potent vasodilator. Our results suggestthat Rac1 regulates eNOS activation in lymphatic vessels during hemorrhagic shock, leading to decreased vessel contractility.Overall, our findings provide new insights into the regulation and mechanism of RhoA/Rac1 signaling pathway in the contractility of isolated lymphatic vessels in hemorrhagic shock rats. Our study suggests that RhoA and Rac1 may be potential targets for the treatment of hemorrhagic shock, and that modulation of their activity may have beneficial effects on lymphatic vessel functionHemorrhagic shock is a condition that occurs when the body loses a significant amount of blood, resulting in decreased blood flow to organs and tissues. One of the key consequences of hemorrhagic shock is impaired lymphatic vessel function, which can lead to fluid accumulation and tissue swelling. Understanding the mechanisms that regulate lymphatic vesselcontractility in hemorrhagic shock is therefore essential for developing effective treatments for thiscondition.The endothelial nitric oxide synthase (eNOS) pathway has been shown to play a critical role in regulating blood vessel tone and contractility, but its role in lymphatic vessels is not well understood. In a recent study, researchers investigated the role of eNOS in the regulation of lymphatic vessel contractility during hemorrhagic shock in rats.The researchers used an isolated vessel preparation to examine the contractility of lymphatic vessels from rats subjected to hemorrhagic shock. They found that eNOS was activated in the lymphatic vessels during hemorrhagic shock, leading to decreased vessel contractility. This effect was mediated by theRhoA/Rac1 signaling pathway, which is known to regulate cytoskeletal dynamics and contractility in cells.To further investigate the role of RhoA and Rac1 in lymphatic vessel function during hemorrhagic shock, the researchers used pharmacological inhibitors and found that inhibition of both RhoA and Rac1 improved lymphatic vessel contractility. These findings suggest that RhoA and Rac1 may be potential targets for the treatment of hemorrhagic shock.Overall, this study provides new insights into the regulation and mechanism of RhoA/Rac1 signaling pathway in the contractility of lymphatic vessels in hemorrhagic shock rats. By identifying eNOS andRhoA/Rac1 as key regulators of lymphatic vessel contractility, this study lays the groundwork for future research aimed at developing new treatments for hemorrhagic shockIn addition to the potential implications for hemorrhagic shock treatment, this study also has broader implications for lymphatic vessel function and regulation. Understanding the underlying mechanisms of lymphatic vessel contractility can lead to the development of treatments for a range of medical conditions that involve abnormal lymphatic vessel function, such as lymphedema, cancer metastasis, and inflammation.Future research could investigate the effects of modulating eNOS and RhoA/Rac1 signaling in other models of lymphatic vessel dysfunction, such as lymphedema, to determine if similar mechanisms are involved. Additionally, studies could examine the effects of pharmacological agents that target these pathways on lymphatic vessel contractility in vivo andin vitro.Furthermore, this study raises intriguing questions about the role of the lymphatic system in regulating blood pressure and volume during hemorrhagic shock. Future studies could investigate how lymphatic vessel contractility may impact the flow and return of interstitial fluid to the circulatory system, and how this may contribute to the overall response to hemorrhagic shock.In conclusion, this study provides novel insights into the mechanisms underlying lymphatic vesselcontractility in hemorrhagic shock. By identifying eNOS and RhoA/Rac1 as key regulators, this study sets the stage for future research aimed at developing new treatments for hemorrhagic shock and other conditions that involve abnormal lymphatic vessel functionIn summary, the circulation of interstitial fluid plays a crucial role in maintaining fluid balance in the body. In the event of hemorrhagic shock, lymphatic vessel contractility is essential for the return of interstitial fluid to the circulatory system, which contributes to the overall response to shock. This study's new findings highlight potential targets for developing innovative treatments for hemorrhagic shockand other conditions that impact lymphatic vessel function。
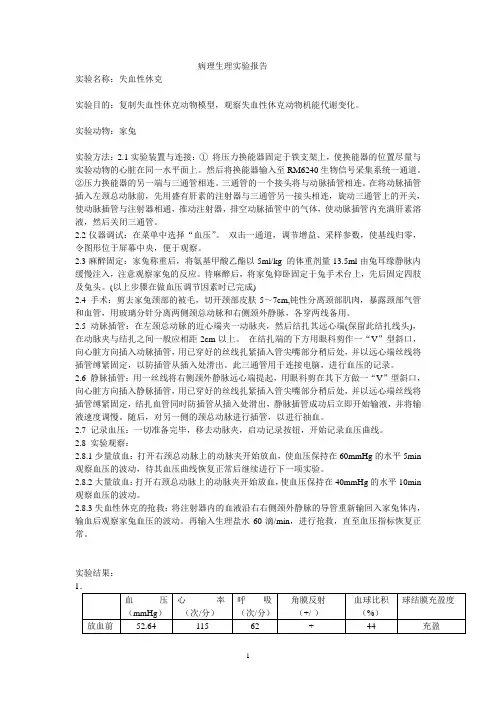
病理生理实验报告实验名称:失血性休克实验目的:复制失血性休克动物模型,观察失血性休克动物机能代谢变化。
实验动物:家兔实验方法:2.1实验装置与连接:①将压力换能器固定于铁支架上,使换能器的位置尽量与实验动物的心脏在同一水平面上。
然后将换能器输入至RM6240生物信号采集系统一通道。
②压力换能器的另一端与三通管相连。
三通管的一个接头将与动脉插管相连。
在将动脉插管插入左颈总动脉前,先用盛有肝素的注射器与三通管另一接头相连,旋动三通管上的开关,使动脉插管与注射器相通,推动注射器,排空动脉插管中的气体,使动脉插管内充满肝素溶液,然后关闭三通管。
2.2仪器调试:在菜单中选择“血压”。
双击一通道,调节增益、采样参数,使基线归零,令图形位于屏幕中央,便于观察。
2.3麻醉固定:家兔称重后,将氨基甲酸乙酯以5ml/kg 的体重剂量13.5ml由兔耳缘静脉内缓慢注入,注意观察家兔的反应。
待麻醉后,将家兔仰卧固定于兔手术台上,先后固定四肢及兔头。
(以上步骤在做血压调节因素时已完成)2.4 手术:剪去家兔颈部的被毛,切开颈部皮肤5~7cm,钝性分离颈部肌肉,暴露颈部气管和血管,用玻璃分针分离两侧颈总动脉和右侧颈外静脉,各穿两线备用。
2.5 动脉插管:在左颈总动脉的近心端夹一动脉夹,然后结扎其远心端(保留此结扎线头),在动脉夹与结扎之间一般应相距2cm以上。
在结扎端的下方用眼科剪作一“V”型斜口,向心脏方向插入动脉插管,用已穿好的丝线扎紧插入管尖嘴部分稍后处,并以远心端丝线将插管缚紧固定,以防插管从插入处滑出。
此三通管用于连接电脑,进行血压的记录。
2.6 静脉插管:用一丝线将右侧颈外静脉远心端提起,用眼科剪在其下方做一“V”型斜口,向心脏方向插入静脉插管,用已穿好的丝线扎紧插入管尖嘴部分稍后处,并以远心端丝线将插管缚紧固定,结扎血管同时防插管从插入处滑出,静脉插管成功后立即开始输液,并将输液速度调慢。
随后,对另一侧的颈总动脉进行插管,以进行抽血。
失血性休克大鼠肠淋巴管压力的变化牛春雨;赵自刚;陈瑞华;刘艳凯;樊贵;张静【期刊名称】《微循环学杂志》【年(卷),期】2002(012)004【摘要】@@ 近年来,作为血液循环辅助系统的淋巴循环及其病理生理意义,引起愈来愈多的学者重视[1,2].国外学者及本室过去的工作发现,失血性休克大鼠肠淋巴管的自主收缩活性降低,而且报道了淋巴流量及蛋白输出量的变化及其调节[3,4].但有关休克时肠淋巴管压力的变化,尚未见报道.本文旨在观察失血性休克、补液及干预治疗中肠淋巴管压力的变化,以及其与血压变化的关系.【总页数】3页(P1-3)【作者】牛春雨;赵自刚;陈瑞华;刘艳凯;樊贵;张静【作者单位】张家口医学院病理生理教研室,张家口,075029;张家口医学院病理生理教研室,张家口,075029;张家口医学院病理生理教研室,张家口,075029;张家口医学院病理生理教研室,张家口,075029;张家口医学院病理生理教研室,张家口,075029;张家口医学院病理生理教研室,张家口,075029【正文语种】中文【中图分类】R5【相关文献】1.肠淋巴管结扎对失血性休克大鼠重要器官ATP含量及膜泵功能的影响 [J], 焦丽强2.肌球蛋白轻链激酶在失血性休克大鼠离体淋巴管收缩性双相变化中的作用 [J], 张玉平;牛春雨;赵自刚;秦立鹏;司永华;张立民;张静3.肠淋巴管结扎对失血性休克大鼠肺组织基因表达谱的影响 [J], 牛春雨;赵自刚;邱景富;韩瑞;张玉平;张静4.失血性休克大鼠淋巴管对去甲肾上腺素反应性的变化 [J], 刘志权;牛春雨;赵自刚;魏艳玲;张静;秦立鹏;张玉平5.失血性休克大鼠淋巴管及血管压力对去甲肾上腺素反应的相关性研究 [J], 刘志权;牛春雨;赵自刚;张玉平;魏艳玲;张静因版权原因,仅展示原文概要,查看原文内容请购买。
MLCK在失血性休克大鼠淋巴管收缩性与血管反应性变化中的作用及其机制的开题报告
一、研究背景:
失血性休克是一种全身性灌流障碍状态,严重时可导致多器官功能
衰竭甚至死亡。
在失血性休克中,淋巴液的输注可以改善器官灌注、恢
复心输出量等,但其机制不十分清楚。
MLCK是一种具有重要生理功能的酶,其与淋巴液输注在失血性休克中的相互作用尚需探究。
二、研究目的:
本研究旨在探究MLCK在失血性休克大鼠淋巴管收缩性与血管反应
性变化中的具体作用及其机制,为深入理解失血性休克中淋巴液输注机
制提供一定的参考。
三、研究方案:
1.建立失血性休克大鼠模型,将动物随机分为对照组、失血性休克
组与淋巴液输注组。
2.通过测定淋巴管大小、内径压与淋巴排出量,观察失血性休克对
淋巴管收缩性及血管反应性的影响。
3.引入MLCK抑制剂,观察其对失血性休克大鼠淋巴管收缩性与血管反应性的改变。
4.应用ELISA法和Western Blot法检测MLCK的表达水平。
5.通过上述实验结果,进一步探讨MLCK在失血性休克大鼠淋巴管收缩性与血管反应性变化中的机理。
四、预期结果:
本研究预期通过实验结果,确定MLCK在失血性休克中的确切作用,进而深入探究其机制,为淋巴液输注在临床治疗上的应用提供理论基础。
去甲肾上腺素和肾上腺素对大鼠急性重度失血性休克的作用比较黎渝;于飞;陈序【摘要】目的:比较去甲肾上腺素及肾上腺素对大鼠急性重度失血性休克的作用,寻找合适的血管活性药物.方法:建立急性重度失血性休克大鼠模型,将大鼠分为3组,生理盐水组(NS组,n=20)、去甲肾上腺素组(NE组,n=20)及肾上腺素组(E组,n=20),复苏期初期NE组与E组分为4个剂量阶段给药(A=10 μg/kg,B=50μg/kg,C=l00 μg/kg,D=500 μg/kg),NS组则推注与E组,NE组相同容积的生理盐水,记录这3组大鼠的血流动力学的变化.结果:①在特定观察时间(90 min)末,E组大鼠存活例数(n=6)较NE组(n=0)、NS组(n=0)存活例数多,差异有统计学意义(P<0.05).②大鼠模型失血量大于50%并逐渐增大时,NS组大鼠很快死亡,NE组血压较E组下降更明显,E组用药仍然可以维持有效血压低值.结论:在急性重度失血性休克期,大剂量肾上腺素能更好的维持有效血压低值.【期刊名称】《广西医科大学学报》【年(卷),期】2014(031)006【总页数】3页(P923-925)【关键词】失血性休克;去甲肾上腺素;肾上腺素;大鼠【作者】黎渝;于飞;陈序【作者单位】广西医科大学第一附属医院麻醉科南宁 530021;广西医科大学第一附属医院麻醉科南宁 530021;广西医科大学第一附属医院麻醉科南宁 530021【正文语种】中文【中图分类】R605.971据文献报道,严重创伤引起的大量失血的死亡率高达50%[1]。
因此,对严重创伤后出现大量出血的患者采取适当的治疗措施成为近年来的一个研究热点[2,3]。
在严重创伤导致失血性休克时,血管活性药物的使用能有效地维持血压,可为外科医生止血及液体复苏争取时间。
去甲肾上腺素被认为是抗休克治疗的一线血管活性药物,但在临床工作中发现[4],在一些创伤大、止血困难,输血输液供给不足的紧急情况下,肾上腺素能更好地维持有效血压,其作用和机制有待评估。
一、实验名称——动脉血压调节和失血性休克(二)二、实验目的1. 建立失血性休克的动物模型并观察失血性休克过程中心脏、肾及微循环的变化2. 了解抢救失血性休克时扩容血容量的意义,在扩容基础上的应用不同的血管活性药物治疗失血性休克,并进行疗效比较。
3. 观察肠系膜微循环,了解休克的机理。
三、合作同学朱骞、徐灵驰、陈霁云、胡蝶四、实验原理1. 失血性休克的原理微循环障碍致微循环动脉血灌流不足,重要的生命器官因缺氧而发生功能和代谢障碍,是各型休克的共同规律。
休克时微循环的变化,大致可分为三期,即微循环缺血期、微循环淤血期和微循环凝血期。
1)正常情况⑴动静脉吻合支是关闭的。
⑵只有20%毛细血管轮流开放,有血液灌流。
⑶毛细血管开放与关闭受毛细血管前括约肌的舒张与收缩的调节。
2)微循环缺血期⑴交感神经兴奋和肾上腺素、去甲肾上腺素分泌增多,小动脉、微动脉、后微动脉,毛细血管前括约肌收缩。
⑵动静脉吻合支开放,血液由微动脉直接流入小静脉。
⑶毛细血管血液灌流不足,组织缺氧。
3)微循环淤血期⑴小动脉和微动脉收缩,动静脉吻合支仍处于开放状态,进入毛细血管的血液仍很少。
⑵由于组织缺氧,组织胺、缓激肽、氢离子等舒血管物质增多,后微动脉和毛细血管前括约肌舒张,毛细血管开放,血管容积扩大,进入毛细血管内的血液流动很慢。
⑶由于交感神经兴奋,肾上腺素和去甲肾上腺素分泌增多,使微静脉和小静脉收缩,毛细血管后阻力增加,结果毛细血管扩张淤血。
4)微循环凝血期⑴由于组织严重缺氧、酸中毒,毛细血管壁受损害和通透性升高,毛细血管内血液浓缩,血流淤滞;另外血凝固性升高,结果在微循环内产生播散性血管内凝血。
⑵由于微血栓形成,更加重组织缺氧和代谢障碍,细胞内溶酶体破裂,组织细胞坏死,弓I起各器官严重功能障碍。
⑶由于凝血,凝血因子和血小板大量被消耗,纤维蛋白降解产物增多,又使血液凝固性降低;血管壁又受损害,继而发生广泛性出血。
2. 阿拉明和多巴胺治疗失血性休克的机理阿拉明是a -受体激动剂,具有显著地收缩血管的作用,能够快速升高血压;小剂量的多巴胺能够扩张血管。
休克的病理生理变化?一、微循环变化各种休克虽然由于致休克的动因不同,在各自发生发展过程中各有特点,但微循环障碍(缺血、淤血、播散性血管内凝血)致微循环动脉血灌流不足,重要的生命器官因缺氧而发生功能和代谢障碍,是它们的共同规律。
休克时微循环的变化,大致可分为三期,即微循环缺血期、微循环淤血期和微循环凝血期。
下面以低血容量性休克为例阐述微循环障碍的发展过程及其发生机理。
低血容量性休克常见于大出血、严重的创伤、烧伤和脱水。
其微循环变化发展过程比较典型(图10-1)。
(一)微循环缺血期(缺血性缺氧期)此期微循环变化的特点是:①微动脉、后微动脉和毛细血管前括约肌收缩,微循环灌流量急剧减少,压力降低;②微静脉和小静脉对酚胺敏感性较低,收缩较轻;③动静脉吻合支可能有不同程度的开放,血液从微动脉经动静脉吻合支直接流入小静脉。
引起微循环缺血的关键性变化是交感神经——肾上腺髓质系统强烈兴奋。
不同类型的休克可以通过不同机制引起交感——肾上腺髓质性休克和心源性休克时,心输出量减少和动脉血压降低可通过窦弓反射使交感——肾上腺髓质系统兴奋;在大多数内毒素性休克时,内毒素可直接剌激交感——肾上腺髓质系统使之发生强烈兴奋。
交感神经兴奋、酚胺释放增加对心血管系统的总的效应是使外周总阻力增高和心输出量增加。
但是不同器官血管的反应却有很大的差别。
皮肤、腹腔内脏和肾的血管,由于具有丰富的交感缩血管纤维支配,。
而且α受体又占有优势,因而在交感神经兴奋、酚胺增多时,这些部位的小动脉、小静脉、微动脉和毛细血管前括红肌都发生收缩,其中由于微动脉的交感缩血管纤维分布最密,毛细血管前括约肌对酚胺的反应性最强,因此它们收缩最为强烈。
结果是毛细血管前阻力明显升高,微循环灌流量急剧减少,毛细血管的平均血压明显降低,只有少量血液经直捷通路和少数真毛细血管流入微静脉、小静脉,组织因而发生严重的缺血性缺氧。
脑血管的交感缩血管纤维分布最少,α受体密度也低,口径可无明显变化。