英文病历书写
- 格式:doc
- 大小:812.50 KB
- 文档页数:94
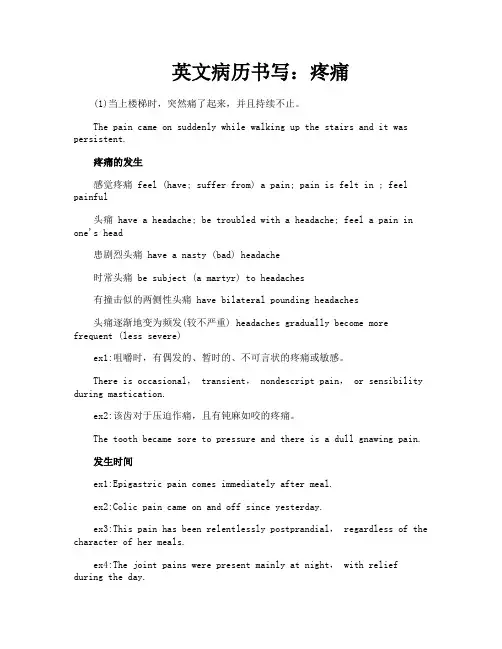
英文病历书写:疼痛(1)当上楼梯时,突然痛了起来,并且持续不止。
The pain came on suddenly while walking up the stairs and it was persistent.疼痛的发生感觉疼痛 feel (have; suffer from) a pain; pain is felt in ; feel painful头痛 have a headache; be troubled with a headache; feel a pain in one's head患剧烈头痛 have a nasty (bad) headache时常头痛 be subject (a martyr) to headaches有撞击似的两侧性头痛 have bilateral pounding headaches头痛逐渐地变为频发(较不严重) headaches gradually become more frequent (less severe)ex1:咀嚼时,有偶发的、暂时的、不可言状的疼痛或敏感。
There is occasional, transient, nondescript pain, or sensibility during mastication.ex2:该齿对于压迫作痛,且有钝麻如咬的疼痛。
The tooth became sore to pressure and there is a dull gnawing pain.发生时间ex1:Epigastric pain comes immediately after meal.ex2:Colic pain came on and off since yesterday.ex3:This pain has been relentlessly postprandial, regardless of the character of her meals.ex4:The joint pains were present mainly at night, with relief during the day.ex5:The mild frontal headaches were usually present upon awakening,but not severe enough to require analgesics.ex6:The pain usually commenced within 30 minutes after meals and lasted 1 to 3 hours.发生原因ex1:He described the pain as dull and aching, occurring approximately once a week, unrelated to food intake, and radiating to his back.(2)起初疼痛无变化,但数小时时变成发作性的'痛。
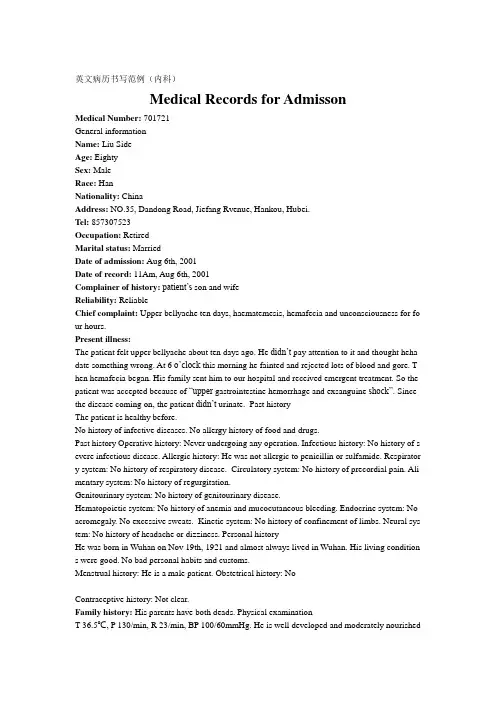
英文病历书写范例(内科)Medical Records for AdmissonMedical Number: 701721General informationName: Liu SideAge: EightySex: MaleRace: HanNationality: ChinaAddress: NO.35, Dandong Road, Jiefang Rvenue, Hankou, Hubei.Tel: 857307523Occupation: RetiredMarital status: MarriedDate of admission: Aug 6th, 2001Date of record: 11Am, Aug 6th, 2001Complainer of history:patient’s son and wifeReliability: ReliableChief complaint: Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for fo ur hours.Present illness:The patient felt upper bellyache about ten days ago. He didn’t pay attention to it and thought heha date something wrong. At 6 o’cloc k this morning he fainted and rejected lots of blood and gore. T hen hemafecia began. His family sent him to our hospital and received emergent treatment. So the patient was accepted because of “upper gastrointestine hemorrhage and exsanguine shock”. Since the disease coming on, the patient didn’t urinate. Past historyThe patient is healthy before.No history of infective diseases. No allergy history of food and drugs.Past history Operative history: Never undergoing any operation. Infectious history: No history of s evere infectious disease. Allergic history: He was not allergic to penicillin or sulfamide. Respirator y system: No history of respiratory disease. Circulatory system: No history of precordial pain. Ali mentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease.Hematopoietic system: No history of anemia and mucocutaneous bleeding. Endocrine system: No acromegaly. No excessive sweats. Kinetic system: No history of confinement of limbs. Neural sys tem: No history of headache or dizziness. Personal historyHe was born in Wuhan on Nov 19th, 1921 and almost always lived in Wuhan. His living condition s were good. No bad personal habits and customs.Menstrual history: He is a male patient. Obstetrical history: NoContraceptive history: Not clear.Family history: His parents have both deads. Physical examinationT 36.5℃, P 130/min, R 23/min, BP 100/60mmHg. He is well developed and moderately nourished.Active position. His consciousness was not clear. His face was cadaverous and the skin was not sta ined yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pi tting edema. Superficial lymph nodes were not found enlarged. HeadCranium: Hair was black and white, well distributed. No deformities. No scars. No masses. No ten derness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external au ditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nare s flaring. No tenderness in nasal sinuses. Eye: Bilateral eyelids were not swelling. No ptosis. No e ntropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or dep ressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect p upillary reactions to light were existent.Mouth: Oral mucous membrane was not smooth, and there were ulcer can be seen. Tongue was in midline. Pharynx was congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in mi dline. ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was nei ther narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities. Breast: Symmetric bilaterally.Lungs: Respiratory movement was bilaterally symmetric with the frequency of 23/min. thoracic e xpansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales. Heart: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum imp ulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardi al friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 150/min. Cardiac rhythm was not regular. No pathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal ty pe or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. T here was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular mur murs. Extremities: No articular swelling. Free movements of all limbs.Neural system: Physiological reflexes were existent without any pathological ones. Genitourinary system: Not examed. Rectum: not exanedInvestigationBlood-Rt: Hb 69g/L RBC 2.70T/L WBC 1. 1G/L PLT 120G/L History summary1. Patient was male, 80 years old2. Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.3. No special past history.4. Physical examination: T 37.5℃, P 130/min, R 23/min, BP 100/60mmHg Superficial lymph node s were not found enlarged. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill ne gative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs. No other positive signs. 5. investigation information:Blood-Rt: Hb 69g/L RBC 2.80T/L WBC 1.1G/L PLT 120G/LImpression: upper gastrointestine hemorrhage Exsanguine shock出院小结(DISCHARGE SUMMARY), ===============Department of GastroenterologyChanghai Hospital,No.174 Changhai Road Shanghai, China Phone: 86-21-25074725-803 DISCHARGE SUMMARYDA TE OF ADMISSION: October 7th, 2005 DA TE OF DISCHARGE: October 12th, 2005 ATTE NDING PHYSICIAN: Yu Bai, MD PA TIENT AGE: 18ADMITTING DIAGNOSIS:V omiting for unknown reason: acute gastroenteritis?BRIEF HISTORYA 18-year-old female with a complaint of nausea and vomiting for nearly one month who was see n at Department of Gastroenterology in Changhai Hospital, found to have acute gastroenteritis and non-atrophic gastritis. The patient was subsequently recovered and discharged soon after medicati on.REVIEW OF SYSTEMShe has had no headache, fever, chills, diarrhea, chest pain, palpitations, dyspnea, cough, hemopty sis, dysuria, hematuria or ankle edema.PAST MEDICAL HISTORYShe has had no previous surgery, accidents or childhood illness.SOCIAL HISTORY: She has no history of excessive alcohol or tobacco use.FAMIL Y HISTORYShe has no family history of cardiovascular, respiratary and gastrointestinal diseases. PHYSICAL EXAMINA TIONTemperature is 37, pulse 80, respirations 16, blood pressure 112/70. General: Plump girl in no app arent distress. HEENT: She has no scalp lesions. Her pupils are equally round and reactive to light and accommodation. Extraocular movements are intact. Sclerae are anicteric. Oropharynx is clear. There is no thyromegaly. There is no cervical or supraclvicular lymphadenopathy. Cardiovascular: Regular rate andrhythm, normal S1, S2. Chest: Clear to auscultation bilateral. Abdomen: Bowel sounds present, no hepatosplenomagaly. Extremities: There is no cyanosis, clubbing or edema. Neurologic: Cranial n erves II-XII are intact. Motor examination is 5/5 in the bilateral upper and lower extremities. Sens ory, cerebellar and gait are normal.LABORATORY DATAWhite blood cells count 5.9, hemoglobin 111g/L, hematocrit 35.4. Sodium 142, potassium 4.3, chl oride 106, CO2 25, BUN 2.6mmol/L, creatinine 57μmol/L, glucose 4.1mmol/L, Albumin 36g/L. Endoscopic ExamChronic non-atrophic gastritisHOSPITAL COURSEThe patient was admitted and placed on fluid rehydration and mineral supplement. The patient im proved, showing gradual resolution of nausea and vomiting. The patient was discharged in stable c ondition.DISCHARGE DIAGNOSIS Acute gastroenteritisChronic non-atrophic gastritisPROGNOSISGood. No medications needed after discharge. But if this patient can not get used to Chinese food, she had better return to UK as soon as possible to prevent the relapse of acute gastroenteritis. The patient is to follow up with Dr. Bai in one week. ___________________________ Yu Bai, MD D: 12/10/2005。
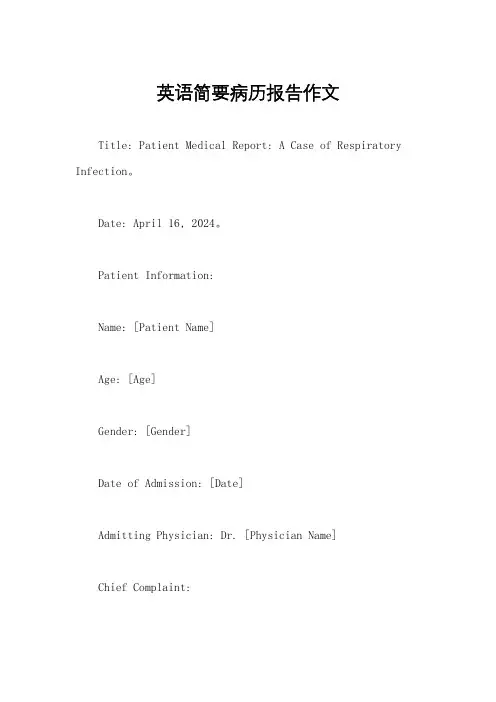
英语简要病历报告作文Title: Patient Medical Report: A Case of Respiratory Infection。
Date: April 16, 2024。
Patient Information:Name: [Patient Name]Age: [Age]Gender: [Gender]Date of Admission: [Date]Admitting Physician: Dr. [Physician Name]Chief Complaint:The patient presents with symptoms of cough, fever, shortness of breath, and fatigue.History of Present Illness:The patient, [Patient Name], a [Age]-year-old [Gender], presented to the emergency department with complaints of cough, fever, shortness of breath, and fatigue for the past five days. The cough was productive, with yellowish-green sputum. The fever was intermittent and associated with chills. The patient also reported experiencing mild chest pain exacerbated by coughing.Past Medical History:The patient has a past medical history significant for asthma, for which they use an inhaler as needed. There are no known allergies to medications.Medications:The patient takes [Medication Name] for asthma asneeded.Social History:The patient is a non-smoker and denies any history of alcohol or illicit drug use. They work as a [Occupation] and have no recent travel history.Family History:There is no significant family history of respiratory illnesses.Physical Examination:On physical examination, the patient was febrile with a temperature of [Temperature], tachycardic with a heart rate of [Heart Rate], and tachypneic with a respiratory rate of [Respiratory Rate]. Oxygen saturation was [Oxygen Saturation]% on room air. Lung auscultation revealed coarse crackles in the lower lung fields bilaterally. There was no evidence of cyanosis, clubbing, or peripheral edema. 。



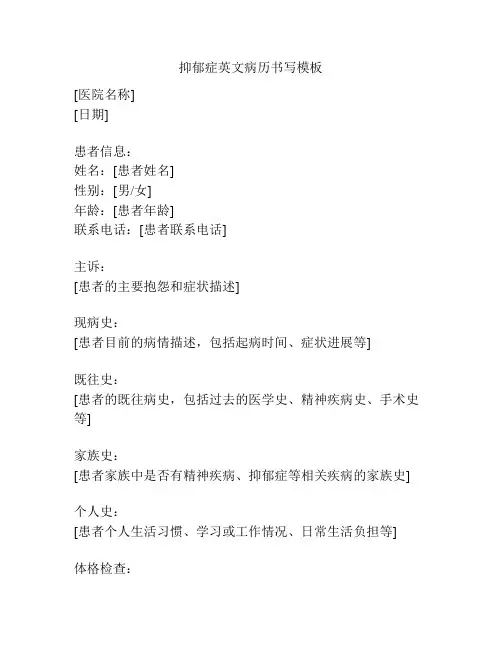
抑郁症英文病历书写模板
[医院名称]
[日期]
患者信息:
姓名:[患者姓名]
性别:[男/女]
年龄:[患者年龄]
联系电话:[患者联系电话]
主诉:
[患者的主要抱怨和症状描述]
现病史:
[患者目前的病情描述,包括起病时间、症状进展等]
既往史:
[患者的既往病史,包括过去的医学史、精神疾病史、手术史等]
家族史:
[患者家族中是否有精神疾病、抑郁症等相关疾病的家族史]
个人史:
[患者个人生活习惯、学习或工作情况、日常生活负担等]
体格检查:
- 一般情况:[患者的一般状态,如疲劳、食欲变化等]
- 精神状态:[患者的精神状态,如情绪低落、焦虑等]
- 神经系统检查:[对患者神经系统功能进行的检查结果]
辅助检查:
[患者曾进行的辅助检查,如血液化验、神经影像学检查等的结果]
诊断:
[医生对患者的初步诊断,如抑郁症、轻度抑郁发作等]
治疗计划:
- 药物治疗:[针对患者的症状和病情制定的药物治疗方案,包括药物名称、剂量和用法]
- 心理治疗:[计划进行的心理治疗方法,如认知行为疗法、支持性治疗等]
- 生活指导:[针对患者日常生活习惯、行为方式等方面的指导建议]
随访计划:
[医生制定的患者随访计划,包括下次随访时间和内容]
备注:
[医生对患者病情的特殊说明和其他需要备注的信息]
医生签名:
[医生姓名]
[医生职称/科室]
以上即为抑郁症的英文病历书写模板,供参考使用。
请根据实际病情和诊疗需求进行调整。
口腔科英文病历书写范文Patient Information:The patient is a 35-year-old male, complaining of severe toothache in the lower right jaw for the past week. He reports that the pain has gradually worsened and is now affecting his sleep and daily routine.Initial Observation:Upon examination, I noticed a swollen area around the second molar on the patient's lower right side. The tooth appears to have a deep cavity, and the surrounding gums are red and inflamed. The patient states that he's had this toothache for some time now but ignored it, thinking it would go away.Symptoms:The patient complains of throbbing pain that radiatesto his jaw and ear. He says the pain is worse at night and when he eats or drinks anything cold or hot. He also mentions occasional sensitivity to air when he breathes through his mouth.Treatment Plan:Given the severity of the symptoms, I recommended an X-ray to assess the extent of the infection. Based on the X-ray results, we'll decide if a root canal treatment or extraction is necessary. Antibiotics will be prescribed to address the current infection.Advice:I advised the patient to avoid chewing on the affected side and to stick to soft, non-spicy foods for the time being. He should also avoid rinsing his mouth vigorously to prevent further irritation.。
心肌炎病历书写范文英文回答:Patient Name: [Patient's Name]Gender: [Patient's Gender]Age: [Patient's Age]Date of Admission: [Date of Admission]Chief Complaint:The patient presented with symptoms of fatigue, shortness of breath, and chest pain for the past week.History of Present Illness:The patient reported experiencing flu-like symptoms, including fever and body aches, two weeks prior to theonset of the current symptoms. The symptoms worsened gradually, leading to the patient seeking medical attention. The patient denied any recent travel, exposure to sick individuals, or history of cardiac diseases.Past Medical History:The patient has no significant past medical history and is not on any regular medication. No known allergies.Family History:No significant family history of cardiac diseases or autoimmune disorders.Social History:The patient is a non-smoker and denies alcohol orillicit drug use. The patient works as an office managerand denies any exposure to toxins or chemicals.Physical Examination:On examination, the patient appeared fatigued. Vital signs were stable. Auscultation of the heart revealed a regular rate and rhythm with no murmurs, rubs, or gallops. Lung examination showed decreased breath sounds in thelower lung fields. No peripheral edema or cyanosis noted.Laboratory Investigations:Complete blood count (CBC), liver function tests (LFTs), renal function tests (RFTs), and electrolyte levels were within normal limits. Cardiac enzymes, including troponin levels, were elevated. Echocardiogram showed reduced left ventricular ejection fraction (LVEF) and global hypokinesis.Diagnosis:Based on the clinical presentation, elevated cardiac enzymes, and echocardiographic findings, the patient was diagnosed with myocarditis.Treatment:The patient was started on supportive measures,including bed rest, adequate hydration, and pain management. Cardiac medications, including beta-blockers and ACE inhibitors, were initiated to manage heart failure symptoms. The patient was closely monitored for any signs of complications, such as arrhythmias or heart failure exacerbation.Prognosis:The prognosis for myocarditis varies depending on the severity of cardiac involvement and the promptness of treatment initiation. With appropriate management, the patient's symptoms are expected to improve gradually over time.中文回答:患者姓名,[患者姓名]性别,[患者性别]年龄,[患者年龄]入院日期,[入院日期]主诉:患者近一周以来出现疲劳、气短和胸痛等症状。
角膜炎病历书写范文英文回答:Patient Name: John Smith.Age: 35。
Date of Admission: 10/15/2021。
Chief Complaint:The patient presents with redness, pain, and blurred vision in the right eye for the past 3 days.History of Present Illness:The patient reports a gradual onset of symptoms, including eye pain, light sensitivity, and excessive tearing. He denies any trauma or foreign body sensation in the eye. The symptoms have not improved with over-the-counter eye drops.Past Medical History:The patient has a history of seasonal allergies and occasional dry eye symptoms. He denies any previous eye infections or surgeries.Medications:The patient takes over-the-counter allergy medication as needed.Family History:Non-contributory.Social History:The patient is a non-smoker and denies alcohol or drug use.Review of Systems:Negative for fever, chills, headache, or changes in vision in the left eye.Physical Examination:Visual acuity 20/30 in the right eye, 20/20 in the left eye. Slit-lamp examination reveals corneal opacity, conjunctival injection, and decreased corneal sensation in the right eye. The left eye examination is unremarkable.Diagnosis:Right eye keratitis, likely due to bacterial or viral etiology.Plan:The patient will be started on topical antibiotic eye drops and will be scheduled for a follow-up appointment in 3 days to monitor the response to treatment.英文回答结束。
原文来自:湘雅医学翻译网MEDICAL RECORD DOCUMENTATIONIncomplete inpatient medical record documentation will be identified by UTMB staff. Y ou will receive written notification of your incomplete record documentation on a weekly basis through U.S. Postal Service mail. UTMB Bylaws and Rules & Regulations of the Medical Staff state that “no record shall remain incomplete, including signatures, greater than thirty (30) calendar days from discharge”.Final Discharge Note (Form 5346)The Final Discharge Note should be completed at the time of discharge. It should be signed (full signature) and dated by the attending physician. Abbreviations should not be used on this form. The following must be recorded on the form:Principal Diagnosis: The condition which, after study, caused admission to the hospital.Complications (if present): Conditions which developed after admission that may have extended the length of stay and required use of additional resources.Comorbidities (if existing): Conditions present prior to admission that could extend the length of stay or require additional resources.Principal Procedure: The definite/therapeutic procedure most closely related to the principal diagnosis.The discharge plan must be documented, and the availability of appropriate services to meet the patient’s needs after hospitalization must be addressed.History and Physical Examination (Form 2005)A complete history and physical examination shall, in all cases, be written and placed in the record within twenty-four (24) hours after admission of the patient. If a complete history and physical has been obtained within thirty (30) days prior to admission in a physician’s office, a durable legible copy of this report may be used in the patient’s hospital medical record, provided there have been no subsequent changes or if there were changes, the changes have been recorded at the time of admission. A durable, legible original or reproduction of the office or clinical prenatal record is acceptable.The history and physical examination includes at a minimum the patient’s chief complaint, present illness/injury, review of systems, past history, family history and physical examination. The patient’s biophysical, psychosocial, cultural, spiritual, developmental, educational, functional,nutritional, and pain/comfort needs will be addressed as appropriate. The physician H&P will be filed in the H&P section of the medical record.The attending physician must sign and date the History and Physical Examination.Inpatient Progress Note (Form 5300)Inpatient progress notes shall be written to provide a chronological record of the patient’s progress. Notes should be timely, legible, relevant, and sufficiently detailed to permit and justify continuity of care. Progress notes on procedures/operations should also include doctor number after the signature. All notes must be timed, dated and signed. A progress note should be written by a physician everyday and more often on critical patients.Operative ReportAn operative note must be written and dictated immediately after surgery and should include the items listed below. The report is signed by the appropriate physician(s).1.preoperative diagnosis;2.postoperative diagnosis; of procedure;4.description of findings;5.technical procedure used;6.specimens removed; of primary surgeon and any assistants; and8.condition of patient after surgery.Discharge SummaryA discharge summary is required on patients discharged from the hospital and should be completed at the time of discharge.The Discharge Summary must contain:, UH#, date of admission, date of discharge, and attending physician;2.chief complaint or reason(s) for admission;3.significant history and physical findings;4.pertinent laboratory and x-ray findings;5.treatment rendered;6.princ ipal and additional or associated diagnoses (indicate principal);7.surgical procedures; and8.disposition –include specific instructions given to the patient and/or family, aspertinent (including instructions relating to physical activity, medication, diet, andfollow-up care);9.prognosis.The physician is required to sign and date the discharge summary.Dictated/typed discharge summaries are not required in the following situations:1.normal obstetric deliveries, including uncomplicated cesarean sections;2.normal newborns.see:/Article/ShowArticle.asp?ArticleID=851。
病历书写英文单词现病史[History of present illness (HPI/PI)]现病史书写的重点包括:一、主诉中症状的详细描述;二、疾病的发展过程;三、诊疗经过;四、目前的一般情况。
1、诱因·无诱因下[With no inducing factors]·无明显诱因下[Under no obvious predisposing causes]·感冒一周后[After getting (catching) common cold for 1 week] 2、症状出现的叙述·有……症状▲suffer from▲have an attack of▲have(fell)▲begin to fell▲a feeling (sensation) of……▲complain (of)▲……sensation (feeling) in (of) ……▲[发热]have a temperature (become feverish)·在……情况下发生▲活动时呼吸困难[dyspnea on exertion]▲躺下后即出现咳嗽[Cough occurs soon after lying]·与……有(无)关▲与……有关[be associated with]▲与……有关[have (make) relation to]▲与……无关[have (make)no relation to]·在……情况下加重(减轻)▲餐后加重[become worse after taking meals]▲站立后缓解[be relieved by standing up]▲随呼吸和咳嗽而加重[become more severe with breathing and cough] ·伴有……▲be accompanied by3、起病方式·急性腹痛[acute abdominal pain]·慢性低热[chronic lower fever]·暴发性发病[the onset was fulminating]·骤起胸痛[an explosive onset of chest pain]·突然起病伴高热[the onset was sudden with high fever]·突发突止[attacks began and ended abruptly]·因……而突然起病[the attack is precipitated by……]·很快发生晕厥[syncope occured rapidly]·逐渐出现咳嗽咳痰[gradual onset of cough and sputum]·偶而[occasionally (sporadically, accidentally)]·反复胸闷心悸[recurrent (bouts of) chest discomfort and palpitation] ·一过性发作[transitory attack]·连续胸痛[chest pain continually]·时重时轻[waned and waxed]·时好时坏[hang in the balance]·不停地咳嗽[have a fit of cough]·发作性呼吸困难[paroxysmal short of breath]·频繁咳嗽[cough frequently (very often)]·持续性(间歇性)[persistent (intermittent)]·频发胸痛[frequent episodes of chest pain]·持续不变[be steady]4、病情变化描述·[症状好转] ▲fell better than before▲take a favorable turn▲take a turn for the better ▲improve▲make favorable progress ▲turn for the better▲change for the better▲be better·[症状减轻] ▲alleviate▲reduce▲palliate▲diminish▲ease(lighten)▲mitigate·[症状消失] ▲disappear▲subside▲regress▲clear up▲vanish▲dissolve▲die (fade) away ▲relieve·[症状加重] ▲be (make,become,get) worse▲worsen▲become more severe▲take a turn for the worse▲be aggravated▲increase in severity▲take a bad turn▲make (become) more serious▲make (become) heavier·[无变化] ▲remain the same as……▲continue without change▲be identical▲be alike▲be similar▲resemble·[时好时坏] ▲wane and wax▲hang in the balance·[体温/血压升降]▲升至[rise (go up) to ]▲已升至[have risen (gone up) to ]▲从……升至……[go up from ……to……]▲升至[be elevated to]▲迅速下降[fall (decline, abate) abruptly]▲骤降(升)[sudden drop (elevation)]▲渐降(升)[fall (elevate) gradually]▲缓慢下降[slow crisis (lysis) of ]▲一天天下降[be (become) lower day by day]▲开始降低[begin to remit]▲降至正常[drop (was reduced) to normal]▲已降至[have gone down (dropped) to]▲回复到正常[return (revert) to normal]▲由……降(升)至……[fall (elev ate) from……to……]▲维持在……水平[maintain at a level of……]▲稳定在……[stabilize at……]▲热退了[fever disappeared]▲不超过[do not go up over (exceed)……]▲在……和……之间波动[fluctuate (vary) between……and……]▲在……至……范围内[range from……to……]▲平均38.5℃[an average temperature of 38.5℃]▲有39.2℃的体温[have fever (a temperature) of 39.2℃]5、症状的时间表示·持续▲lasted for 2 days▲have gone on for 1 month▲have continued for 10 hours▲lasted on the average 3-5 hours▲lasted a variable time from 5 minutes to several hours ▲lasted about half an hour·超过(不到)[move than (less than)]·……以前[two years ago]·多在……时发生[usually between 3 and 5 PM]·未发作过[be free of onsets (attacks) for 2 weeks]6、症状的严重程度·轻度[mild (slight)]·中度[moderate]·重度[severe (serious)]7、症状的其他描述方法·[部位] ▲be located (situated) in (over)[位于] ▲There is localized pain in……[疼痛位于]▲near……[在……附近]▲be localized to (in, over)[局限于]▲be limited (confined) to[局限于]·[表示部位的介词]▲心尖部,表示小的部位或点[at the apex]▲上腹部,表示大的部位[in the upper abdomen]▲在左下肢,表示皮肤表面上(下)的病变[on (beneath) the left lower limb]▲在右肺,表示正上方的相应体表部位[over the right lung]▲嘴上(下)方,表示高低或上下的位置关系[above (below)the mouth]▲左乳皮下[under the skin of the left breast]·[转移/放射]▲转移到……[shift (migrate) to……]▲放射到……[radiate (travel,go,refer)to……]▲从……放射到……[radiate from……to……]·[耳鼻咽喉及口腔症状]▲耳痛[otalgia (pain of ears)]▲耳鸣[tinnitus (ears ring)]▲耳鸣[a buzzing (ringing,singing) in the ears]▲左耳有耳鸣感[a buzzing sensation in the left ear]▲耳聋[deafness (loss in hearing)]▲左耳聋[be deaf of the left ear]▲耳流脓[otorrhea (otopyorrhea)]▲耳出血[otorrhagia]▲耳垢[cerumen (earwax)]▲耳血肿[othematoma]▲鼻塞[nasal obstruction]▲不能用鼻呼吸[be unable to breathe through (by) the nose (nasal dyspnea)]▲打喷涕和流涕[sneezing and nasal discharge]▲水样鼻涕[watery rhinorrhea]▲鼻出血[nosebleed]▲咽喉痛[sore throat]▲口吃[stuttering]▲口臭[ozostomia (saburra,halitosis)]▲张口困难[difficult (inability) to open the mouth]▲张口(吞咽、嚼)困难[difficult in opening the mouth (swallowing,masticating)]▲咽下困难[dysphagia]▲流涎多[have excessive salvation]·[眼科及牙科症状]▲眼睑浮肿[eyelid edema]▲眼痛[pain in the eyes]▲视边模糊[blurring of vision (blurred vision)]▲过度流泪[excessive tearing (watering)]▲视疲劳[asthenopia (visional tired)]▲视力减退[hypopsia (diminution of vision)]▲视力衰弱[o。