Sterile Drug Insp CPGM 7356-002A_ORA_LAO-NM 9-10-15_EMc LAO FINAL
- 格式:pdf
- 大小:353.02 KB
- 文档页数:54
![精神神经疾病治疗药[发明专利]](https://uimg.taocdn.com/dba39e49b0717fd5370cdc43.webp)
专利名称:精神神经疾病治疗药专利类型:发明专利
发明人:熊谷裕生,内海润
申请号:CN02807257.X
申请日:20020329
公开号:CN1537016A
公开日:
20041013
专利内容由知识产权出版社提供
摘要:一种可用于神经疾病、特别是不安腿综合症的治疗的精神神经疾病治疗药。
本发明的精神神经疾病治疗药含有(-)-17-(环丙基甲基)-3,14β-二羟基-4,5α-环氧基-6β-[N-甲基-反式-3-(3-呋喃基)丙烯酰胺]吗啡喃盐酸盐这样的阿片样物质κ受体激动性化合物(喷他佐辛除外)作为有效成分。
申请人:东丽株式会社
地址:日本东京
国籍:JP
代理机构:中国国际贸易促进委员会专利商标事务所
代理人:陈昕
更多信息请下载全文后查看。
FDA检查员指导手册CP 7356.002:药品生产检查程序目录对现场报告的要求 (35)第一部分背景 (36)第二部分执行 (36)2.1.目的 (36)2.2.策略 (36)2.2.1.对生产企业两年一度的检查(包括重新包装商、合同实验室等) (36)2.2.2.系统性检查 (37)2.2.3.对原料药及制剂生产的系统性检查计划 (38)2.2.3.1.质量系统 (38)2.2.3.2.厂房设施与设备系统 (38)2.2.3.3.物料系统 (38)2.2.3.4.生产系统 (38)2.2.3.5.包装和贴签系统 (38)2.2.3.6.实验室控制系统 (39)2.3.程序管理指导 (39)2.3.1.定义 (39)2.3.1.1.监督性检查 (39)2.3.1.2.达标检查 (40)2.3.1.3.受控状态 (40)2.3.1.4.药品工艺 (40)2.3.1.5.药品生产检查 (41)第三部分检查 (41)3.1.检查活动 (41)3.1.1.总则 (41)3.1.2.检查方法 (42)3.1.2.1.全面性检查的选择 (43)3.1.2.2. 简略性检查的选择 (43)3.1.2.3.综合性检查围 (43)3.1.3.系统性检查围 (43)3.1.3.1.质量系统 (44)3.1.3.2. 厂房设施与设备系统 (44)3.1.3.3.物料系统 (45)3.1.3.4.生产系统 (46)3.1.3.5.包装和贴签系统 (47)3.1.3.6.实验室控制系统 (48)3.1.4.取样 (49)3.1.5.检查组组成 (49)3.1.6.报告 (49)第四部分分析 (50)第五部分法律性/行政性策略 (50)5.1.质量系统 (51)5.2.厂房设施和设备 (51)5.3.物料系统 (51)5.4.生产系统 (52)5.5.包装和贴签系统 (52)5.6.实验室控制系统 (52)对现场报告的要求作为法律行动的一部分,所有针对因在执行cGMP方面有缺陷而采取的检查,均要向药品评价和研究中心的达标办公室呈交一份现场检查报告(EIR)。
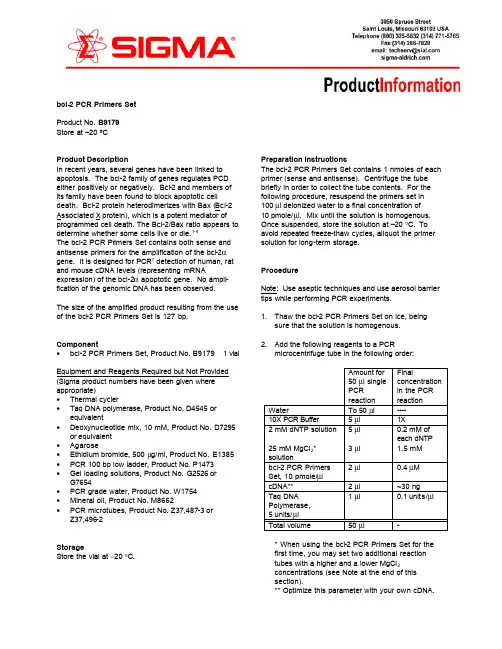
bcl-2 PCR Primers Set Product No. B9179 Store at –20 ºCProduct DescriptionIn recent years, several genes have been linked to apoptosis. The bcl-2 family of genes regulates PCD either positively or negatively. Bcl-2 and members of its family have been found to block apoptotic cell death. Bcl-2 protein heterodimerizes with Bax (Bcl-2 Associated X protein), which is a potent mediator of programmed cell death. The Bcl-2/Bax ratio appears to determine whether some cells live or die.1-4The bcl-2 PCR Pr imers Set contains both sense and antisense primers for the amplification of the bcl-2αgene. It is designed for PCR† detection of human, rat and mouse cDNA levels (representing mRNA expression) of the bcl-2α apoptotic gene. No ampli-fication of the genomic DNA has been observed.The size of the amplified product resulting from the use of the bcl-2 PCR Primers Set is 127 bp.Component• bcl-2 PCR Primers Set, Product No. B9179 1 vial Equipment and Reagents Required but Not Provided (Sigma product numbers have been given where appropriate)• Thermal cycler• Taq DNA polymerase, Product No. D4545 or equivalent• Deoxynucleotide mix, 10 mM, Product No. D7295 or equivalent• Agarose• Ethidium bromide, 500 µg/ml, Product No. E1385 • PCR 100 bp low ladder, Product No. P1473• Gel loading solutions, Product No. G2526 or G7654• PCR grade water, Product No. W1754• Mineral oil, Product No. M8662• PCR microtubes, Product No. Z37,487-3 or Z37,496-2StorageStore the vial at −20 °C.Preparation InstructionsThe bcl-2 PCR Primers Set contains 1 nmoles of each primer (sense and antisense). Centrifuge the tube briefly in order to collect the tube contents. For the following procedure, resuspend the primers set in100 µl deionized water to a final concentration of10 pmole/µl. Mix until the solution is homogenous. Once suspended, store the solution at –20 °C. To avoid repeated freeze-thaw cycles, aliquot the primer solution for long-term storage.ProcedureNote: Use aseptic techniques and use aerosol barrier tips while performing PCR experiments.1. Thaw the bcl-2 PCR Primers Set on ice, beingsure that the solution is homogenous.2. Add the following reagents to a PCRmicrocentrifuge tube in the following order:Amount for50 µl singlePCRreactionFinalconcentrationin the PCRreaction Water To 50 µl ----10X PCR Buffer 5 µl 1X2 mM dNTP solution 5 µl 0.2 mM ofeach dNTP25 mM MgCl2*solution3 µl 1.5 mMbcl-2 PCR PrimersSet, 10 pmole/µl2 µl 0.4 µM cDNA** 2 µl ~30 ngTaq DNAPolymerase,5 units/µl1 µl 0.1 units/µl Total volume50 µl -* When using the bcl-2 PCR Primers Set for thefirst time, you may set two additional reactiontubes with a higher and a lower MgCl2concentrations (see Note at the end of thissection).** Optimize this parameter with your own cDNA.3. Mix gently by finger tapping and centrifuge briefly to collect the mixture in the bottom of the tube. Overlay the reaction mixture with 2 drops (~30 µl) of mineral oil to cover the surface of the reaction mixture if not using a thermal cycler with a heated lid. Place the tube in the thermal cycler when the thermal cycler reaches 95 oC, and run the following PCR program. 95 oC for 2 min 94 oC for 45 sec 53 oC for 45 sec x 30 cycles 72 oC for 1.5 min 72 oC for 7 min The amplified DNA can be evaluated by agarose gel electrophoresis.Note: Using different thermal cyclers:For a better detection of the amplified product you may increase the number of amplification cycles. In case you do not see differences in the amount of the amplified DNA fragments, decrease the number of cycles to verify your results.In rare cases, some of the parameters should beoptimized for the specific thermal cycler or cDNA samples. The most frequently adjusted factors are MgCl 2 concentration and annealing temperature. You may prepare three different reactions using MgCl 2 at a concentration of 0.5-3 mM (e.g., 0.5-0.8 mM, 1.5 mM and 3 mM). Optimize the MgCl 2 and/or the annealing temperature on your instrument using the positive control cDNA provided before using your own cDNA.Troubleshooting GuideProblem Cause Solution A PCR component may be missing or degraded. Try to isolate the problematic reagent by replacing it with a fresh one. A checklist is also recommended when assembling reactions.No PCR products cDNA or MgCl 2concentration is not optimal .Optimize the cDNA and MgCl 2 concentrations.Highbackground, smearing or nonspecific bandsIncrease the annealing temperature or decrease the MgCl 2concentration. Another solution for avoiding high background is to decrease the amount of cDNA template used for amplification.Contamination with other DNAUse sterile techniques while performing PCR experiments. cDNA quality is not sufficientUse a different cDNA preparation.Amplifiedproducts are not the correct sizeNon-optimal PCR conditions Optimize PCR conditions especially cDNA and MgCl 2 concentrations and annealing temperature. Poor resolution of products in agarose gelUse 2% agarose gel and increase run time.References1. Oltavi, Z.N., et al ., Cell, 74, 609 (1993)2. Korsmeyer, S.J., Cancer Research (Suppl), 59,1693s (1999)3. Agarwal, N. and Metha, K., Biochem. Biophys.Res. Commun., 230, 251 (1997)4. Aggarwal, S. and Gupta, S., J. Immunol., 160,1627 (1998)†The PCR process is covered by patents owned by Hoffman-LaRoche, Inc. Purchase of this product does not convey a license under these patents.ya 6/00Sigma brand products are sold through Sigma -Aldrich, Inc.Sigma-Aldrich, Inc. warrants that its products conform to the information contained in this and other Sigma -Aldrich publications. Purchaser must determine the suitability of the product(s) for their particular use. Additional terms and conditions may apply.Please see reverse side of the invoice or packing slip.。
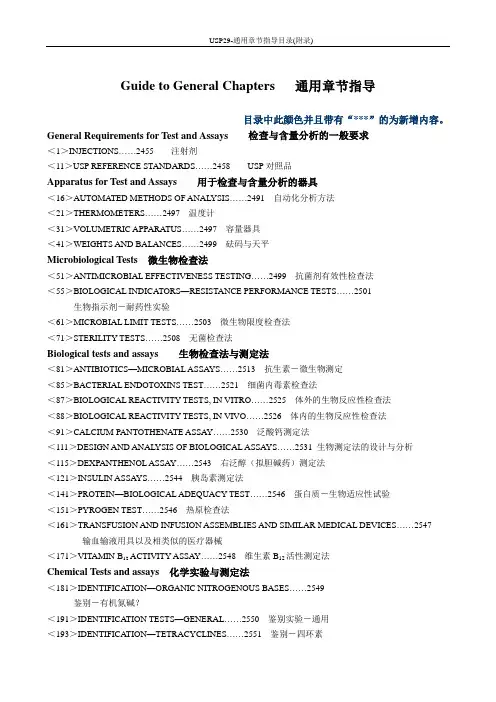
USP29-通用章节指导目录(附录)Guide to General Chapters 通用章节指导目录中此颜色并且带有“***”的为新增内容。
General Requirements for Test and Assays检查与含量分析的一般要求<1>INJECTIONS……2455注射剂<11>USP REFERENCE STANDARDS……2458USP对照品Apparatus for Test and Assays用于检查与含量分析的器具<16>AUTOMATED METHODS OF ANAL YSIS……2491自动化分析方法<21>THERMOMETERS……2497温度计<31>VOLUMETRIC APPARATUS……2497容量器具<41>WEIGHTS AND BALANCES……2499砝码与天平Microbiological Tests 微生物检查法<51>ANTIMICROBIAL EFFECTIVENESS TESTING……2499抗菌剂有效性检查法<55>BIOLOGICAL INDICATORS—RESISTANCE PERFORMANCE TESTS (2501)生物指示剂-耐药性实验<61>MICROBIAL LIMIT TESTS……2503微生物限度检查法<71>STERILITY TESTS……2508无菌检查法Biological tests and assays生物检查法与测定法<81>ANTIBIOTICS—MICROBIAL ASSAYS……2513抗生素-微生物测定<85>BACTERIAL ENDOTOXINS TEST……2521细菌内毒素检查法<87>BIOLOGICAL REACTIVITY TESTS, IN VITRO……2525体外的生物反应性检查法<88>BIOLOGICAL REACTIVITY TESTS, IN VIVO……2526体内的生物反应性检查法<91>CALCIUM PANTOTHENATE ASSAY……2530泛酸钙测定法<111>DESIGN AND ANAL YSIS OF BIOLOGICAL ASSAYS……2531 生物测定法的设计与分析<115>DEXPANTHENOL ASSAY……2543右泛醇(拟胆碱药)测定法<121>INSULIN ASSAYS……2544胰岛素测定法<141>PROTEIN—BIOLOGICAL ADEQUACY TEST……2546蛋白质-生物适应性试验<151>PYROGEN TEST……2546热原检查法<161>TRANSFUSION AND INFUSION ASSEMBLIES AND SIMILAR MEDICAL DEVICES (2547)输血输液用具以及相类似的医疗器械<171>VITAMIN B12 ACTIVITY ASSAY……2548维生素B12活性测定法Chemical Tests and assays化学实验与测定法<181>IDENTIFICATION—ORGANIC NITROGENOUS BASES (2549)鉴别-有机氮碱?<191>IDENTIFICATION TESTS—GENERAL……2550鉴别实验-通用<193>IDENTIFICATION—TETRACYCLINES……2551鉴别-四环素<197>SPECTROPHOTOMETRIC IDENTIFICATION TESTS......2552分光光度计鉴别实验<201>THIN-LAYER CHROMATOGRAPHIC IDENTIFICATION TEST.. (2553)薄层色谱鉴别实验Limit Test 限度检查法<206>ALUMINUM……2554铝<211>ARSENIC……2554砷<221>CHLORIDE AND SULFATE……2555氯和硫<223>DIMETHYLANILINE……2555二甲基苯胺<226>4-EPIANHYDRO-TETRACYCLINE……25564-?-四环素<231>HEA VY METALS……2556重金属<241>IRON……2557铁<251>LEAD……2558铅<261>MERCURY……2558汞<271>READIL Y CARBONIZABLE SUBSTANCES TEST……2560易碳化物检查法<281>RESIDUE ON IGNITION……2560灼烧残渣<291>SELENIUM……2560硒Other Tests and Assays 其它检查法与测定法<301>ACID-NEUTRALIZING CAPACITY……2561酸中和容量<311>ALGINATES ASSAY……2562藻酸盐测定法<331>AMPHETAMINE ASSAY……2562苯丙胺测定法<341> ANTIMICROBIAL AGENTS—CONTENT……2563 抗菌剂-含量<345> Assay for Citric Acid/Citrate and Phosphate……2565 柠檬酸/柠檬酸盐和磷酸盐的测定<351>ASSAY FOR STEROIDS……2565类固醇(甾类化合物)测定法<361> BARBITURATE ASSAY……2565 巴比妥类药物测定法<371>COBALAMIN RADIOTRACER ASSAY……2566钴铵素放射性跟踪剂测定法<381>ELASTOMERIC CLOSURES FOR INJECTIONS……2567 注射剂的弹性密封件<391>EPINEPHRINE ASSAY……2567肾上腺测定法<401>FATS AND FIXED OILS……2568脂肪与混合油<411>FOLIC ACID ASSAY……2571叶酸测定法<425>IODOMETRIC ASSAY—ANTIBIOTICS……2572碘量检查法-抗生素<429>LIGHT DIFFRACTION MEASUREMENT OF PARTICLE SIZE (2572)粒子尺寸的光衍射测量<431>METHOXY DETERMINA TION……2575甲氧基测定法<441>NIACIN OR NIACINAMIDE ASSAY……2576烟酰或烟酰胺测定法<451>NITRITE TITRATION……2578亚硝酸盐滴定<461>NITROGEN DETERMINA TION……2578氮测定法<466>ORDINARY IMPURITIES……2579一般杂质<467>ORGANIC VOLATILE IMPURITIES……2580有机的易挥发杂质<471>OXYGEN FLASK COMBUSTION……2590氧瓶燃烧法<481>RIBOFLAVIN ASSAY……2590核黄素测定法<501>SALTS OF ORGANIC NITROGENOUS BASES……2591有机氮盐<511>SINGLE-STEROID ASSAY……2591单一的类固醇测定法<521>SULFONAMIDES……2592磺胺制剂<531>THIAMINE ASSAY……2593硫胺素测定法<541>TITRIMETRY……2593滴定法<551>ALPHA TOCOPHEROL ASSAY……2596α-维生素E测定法<561>ARTICLES OF BOTANICAL ORIGIN……2596植物起源的药品<563>IDENTIFICATION OF ARTICLES OF BOTANICAL ORIGIN……2603植物药品的鉴别<565>BOTANICAL EXTRACTS……2609植物提取<571>VITAMIN A ASSAY……2611维生素A的测定法<581>VITAMIN D ASSAY……2612维生素D的测定法<591>ZINC DETERMINATION……2616锌的测定法Physical Test and Determinations物理检查与测定法INHALERS, AND DRY POWDER <601>AEROSOLS, NASAL SPRAYS,USP28METERED-DOSEINHALERS……2617气溶胶,鼻用喷雾剂,定量吸入器与干粉吸入器<611>ALCOHOL DETERMINATION……2637乙醇测定法<616>BULK DENSITY AND TAPPED DENSITY……2638堆密度与拍实密度<621>CHROMATOGRAPHY…….2639色谱法<631>COLOR AND ACHROMICITY……2651呈色与消色<641>COMPLETENESS OF SOLUTION……2652完全溶解<643>TOTAL ORGANIC CARBON……2652总有机碳<645>WA TER CONDUCTIVITY……2653水电导率<651>CONGEALING TEMPERA TURE……2654凝点温度<661>CONTAINERS……2655容器<671>CONTAINERS—PERMEATION……2663容器-渗透<691>COTTON……2664棉花<695>CRYSTALLINITY……2665结晶性<696>Crystallinity Determination By Solution Calorimetry……2666 通过溶液量热学测定结晶性<698>DELIVERABLE VOLUME……2667可转移的体积<699>DENSITY OF SOLIDS……2669固体密度<701>DISINTEGRATION……2670崩解时限***<701>Disintegration (Harmonized Chapter, Official April 1,2006)………..2671崩解时限(协调的章节,法定日期,2006.4.1)<711>DISSOLUTION……2673 溶出度***<711>Dissolution (Harmonized Chapter, Official April 1,2006)………..2675 溶出度(协调的章节,法定日期,2006.4.1)<721>DISTILLING RANGE……2682馏程<724>DRUG RELEASE……2682药物释放度***<724>Drug releasee (Harmonized Chapter, Official April 1,2006)………..2690药物释放度(协调的章节,法定日期,2006.4.1)<726>ELECTROPHORESIS……2694电泳<727>CAPILLARY ELECTROPHORESIS……2696毛细管电泳法***<730>Plasma Spectrochemistry….2700 血浆光谱化学<731>LOSS ON DRYING……2704干燥失重<733>LOSS ON IGNITION……2704灼烧失重<736>MASS SPECTROMETRY……2705 质谱<741>MELTING RANGE OR TEMPERATURE……2708熔距或熔点<751>METAL PARTICLES IN OPHTHALMIC OINTMENTS……2709眼用软膏中的金属粒子<755>MINIMUM FILL……2710最低装填量<761>NUCLEAR MAGNETIC RESONANCE……2710核磁共振<771>OPHTHALMIC OINTMENTS……2715眼用软膏<776>OPTICAL MICROSCOPY……2716光学显微镜<781>OPTICAL ROTATION……2718旋光<785>OSMOLALITY AND OSMOLARITY……2718同渗重摩与同渗容摩<786>PARTICLE SIZE DISTRIBUTION ESTIMATION BY ANAL YTICAL SIEVING (2720)通过筛分法估算粒子分布<788>PARTICULATE MATTER IN INJECTIONS……2722注射剂中的颗粒<789>PARTICULATE MATTER IN OPHTHALMIC SOLUTIONS……2729眼用溶液中的颗粒<791>pH (2730)<795>PHARMACEUTICAL COMPOUNDING—NONSTERILE PREPARATIONS (2731)药物混合-非无菌制剂<797>PHARMACEUTICAL COMPOUNDING—STERILE PREPARATIONS (2735)药物混合-无菌制剂<801>POLAROGRAPHY……2752极谱法<811>POWDER FINENESS……2754粉剂细度<821>RADIOACTIVITY……2755放射性<823>RADIOPHARMACEUTICALS FOR POSITRON EMISSION TOMOGRAPHY —COMPOUNDING……2763用于正电子发射断层摄影术的放射性药物<831>REFRACTIVE INDEX……2766折光率<841>SPECIFIC GRA VITY……2766比重<846>SPECIFIC SURFACE AREA……2767 比表面积<851>SPECTROPHOTOMETRY AND LIGHT-SCA TTERING……2770分光光度计与光散射<861>SUTURES—DIAMETER…2775缝线-直径<871>SUTURES—NEEDLE ATTACHMENT……2775缝线-穿孔实验<881>TENSILE STRENGTH…..2776张力<891>THERMAL ANAL YSIS……2776热分析<905>UNIFORMITY OF DOSAGE UNITS……2778制剂单位的含量均匀度<905>UNIFORMITY OF DOSAGE UNITS (Harmonized Chapter, Official April 1,2006)……2780制剂单位的含量均匀度(协调的章节2006.4.1)<911>VISCOSITY……2785粘度<921>WA TER DETERMINA TION……2785水测定法<941>X-RAY DIFFRACTION……2788X光衍射General Information通用信息<1010>ANAL YTICAL DATA—INTERPRETA TION AND TREATMENT (2790)分析数据-解释与处理<1015>AUTOMA TED RADIOCHEMICAL SYNTHESIS APPARATUS (2801)放射性自动合成装置<1031>THE BIOCOMPATIBILITY OF MATERIALS USED IN DRUG CONTAINERS, MEDICAL DEVICES, AND IMPLANTS (2802)用于药物容器、医疗设施和植入剂的材料的生物相容性<1035>BIOLOGICAL INDICATORS FOR STERILIZATION……2811灭菌用生物指示剂<1041>BIOLOGICS……2814生物制剂***<1043>Ancillary Material for Cell, Gene, and Tissue-Engineered Products…….2814 细胞,基因与组织设计产品的辅助材料<1045>BIOTECHNOLOGY-DERIVED ARTICLES……2821生物技术提取产品<1046>CELL AND GENE THERAPY PRODUCTS……2831细胞与基因治疗产品<1047>BIOTECHNOLOGY-DERIVED ARTICLES—TESTS……2858生物技术产品-检查法<1048>QUALITY OF BIOTECHNOLOGICAL PRODUCTS: ANAL YSIS OF THE EXPRESSION CONSTRUCT IN CELLS USED FOR PRODUCTION OF r-DNA DERIVED PROTEIN PRODUCTS1 (2883)生物产品质量:从蛋白质产品中提取的r-DNA产品在细胞中表达结构的分析<1049>QUALITY OF BIOTECHNOLOGICAL PRODUCTS: STABILITY TESTING OF BIOTECHNOLOGICAL/BIOLOGICAL PRODUCTS1 (2884)生物技术产品的质量:生物技术/生物产品的稳定性实验<1050>VIRAL SAFETY EV ALUA TION OF BIOTECHNOLOGY PRODUCTS DERIVED FROM CELL LINES OF HUMAN OR ANIMAL ORIGIN (2887)从人或动物细胞中提取的生物技术产品的病毒安全性评估<1051>CLEANING GLASS APPARATUS……2896玻璃容器的清洗<1061>COLOR—INSTRUMENTAL MEASUREMENT……2896显色-仪器测量***<1065>Ion Chromatography………2898 离子色谱法<1074>EXCIPIENT BIOLOGICAL SAFETY EV ALUA TION GUIDELINES (2900)赋形剂(辅料)生物安全性评估指导<1075>GOOD COMPOUNDING PRACTICES……2903好的混合操作<1078>GOOD MANUFACTURING PRACTICES FOR BULK PHARMACEUTICAL EXCIPIENTS (2906)批药品赋形剂的生产管理规范***<1079>Good Storage and Shipping Practices……2915 良好的贮存与船运规范<1081>GEL STRENGTH OF GELATIN……2920白凝胶的凝胶强度<1086>IMPURITIES IN OFFICIAL ARTICLES……2920药典物品中的杂质<1087>INTRINSIC DISSOLUTION……2923内部的溶出度<1088>IN VITRO AND IN VIVO EV ALUA TION OF DOSAGE FORMS (2924)体内与体外的剂型的评估<1090>IN VIVO BIOEQUIV ALENCE GUIDANCES……29291体内生物等效性指导<1091>LABELING OF INACTIVE INGREDIENTS……2968非活性成分的标示<1101>MEDICINE DROPPER……2969医用滴管<1111>MICROBIOLOGICAL ATTRIBUTES OF NONSTERILE PHARMACEUTICAL PRODUCTS (2969)非无菌药品中的微生物分布<1116>MICROBIOLOGICAL EV ALUA TION OF CLEAN ROOMS AND OTHER CONTROLLED ENVIRONMENTS……2969洁净的房间与其它可控环境的微生物评估<1118>MONITORING DEVICES—TIME, TEMPERATURE, AND HUMIDITY (2976)监控装置-时间、温度与湿度<1119>NEAR-INFRARED SPECTROPHOTOMETRY……2979近红外分光光度测定法***<1120>Raman Spectrophotometry……..2983 Raman分光光度测定法<1121>NOMENCLATURE……2988命名***<1136>Packaging-Unit-of-Use……2989包装-单元使用<1146>PACKAGING PRACTICE—REPACKAGING A SINGLE SOLID ORAL DRUG PRODUCT INTO A UNIT-DOSE CONTAINER……2990 包装操作-将单一固体口服药品产品再包装成单元剂量<1150>PHARMACEUTICAL STABILITY……2994药物稳定性<1151>PHARMACEUTICAL DOSAGE FORMS……2996药物剂型<1160>PHARMACEUTICAL CALCULATIONS IN PRESCRIPTION COMPOUNDING (3006)按处方混合的药物的计算<1171>PHASE-SOLUBILITY ANAL YSIS……3016相溶解分析***<1174>Powder Flow….3017 粉末流动性<1176>PRESCRIPTION BALANCES AND VOLUMETRIC APPARATUS….3020 处方天平与容量器具***<1177>Good Packaging Practices….3021 良好的包装操作***<1178>Good Repackaging Practices….3023 良好的再包装操作<1181>SCANNING ELECTRON MICROSCOPY……3025扫描电子显微镜<1191>STABILITY CONSIDERATIONS IN DISPENSING PRACTICE……3029 分装操作中稳定性考察<1196>PHARMACOPEIAL HARMONIZATION……3031药典的一致性<1207>STERILE PRODUCT PACKAGING—INTEGRITY EV ALUATION (3035)无菌产品包装-完整性评估<1208>STERILITY TESTING—V ALIDATION OF ISOLATOR SYSTEMS (3037)无菌实验-隔离系统的验证<1209>STERILIZATION—CHEMICAL AND PHYSICOCHEMICAL INDICATORS AND INTEGRATORS……3040灭菌-化学与物理化学的指示剂以及二者的综合<1211>STERILIZATION AND STERILITY ASSURANCE OF COMPENDIAL ARTICLES (3041)药典物品中的灭菌与灭菌保证<1216>TABLET FRIABILITY……3046片剂的脆碎度<1221>TEASPOON……3047茶匙<1222>TERMINALL Y STERILIZED PHARMACEUTICAL PRODUCTS—PARAMETRIC RELEASE……3047最终灭菌产品-放行参数<1225>V ALIDATION OF COMPENDIAL METHODS……3050药典方法的验证<1227>V ALIDATION OF MICROBIAL RECOVERY FROM PHARMACOPEIAL ARTICLES (3053)从药物中回收微生物的验证<1230>W ATER FOR HEALTH APPLICATIONS……3055健康用水<1231>W ATER FOR PHARMACEUTICAL PURPOSES……3056制药用水<1241>W ATER–SOLID INTERACTIONS IN PHARMACEUTICAL SYSTEMS (3074)在药物系统中水与固体的相互作用<1251>WEIGHING ON AN ANAL YTICAL BALANCE……3076关于分析天平的称重***<1265>Written Prescription Drug Information-Guidelines……….3078 书面的处方药信息-指南Dietary Supplements营养补充剂General Tests and Assays 一般检查法与测定法<2021>MICROBIAL ENUMERATION TESTS—NUTRITIONAL AND DIETARY SUPPLEMENTS (3080)微生物数量实验-营养与食品添加剂<2022>MICROBIOLOGICAL PROCEDURES FOR ABSENCE OF SPECIFIED MICROORGANISMS—NUTRITIONAL AND DIETARY SUPPLEMENTS (3083)不得检出特定微生物的程序-营养与营养补充剂<2023>MICROBIOLOGICAL A TTRIBUTES OF NONSTERILE NUTRITIONAL AND DIETARY SUPPLEMENTS……3087非无菌的营养与食品添加剂中的微生物分布<2040>DISINTEGRATION AND DISSOLUTION OF DIETARY SUPPLEMENTS (3089)食品添加剂的崩解与溶出<2091>WEIGHT VARIATION OF DIETARY SUPPLEMENTS……3092食品添加剂的重量差异<2750>MANUFACTURING PRACTICES FOR DIETARY SUPPLEMENTS (3093)食品添加剂的生产操作。
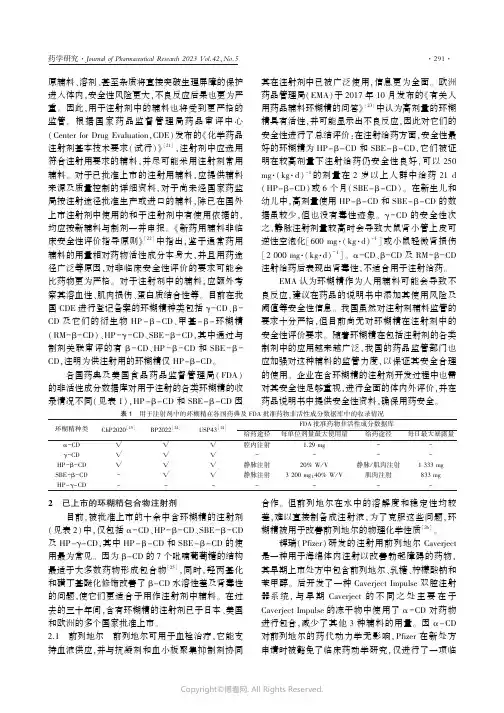
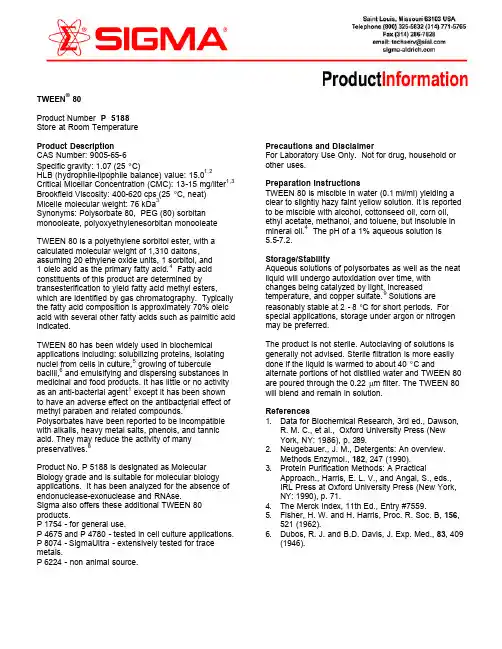
原辅料㊁溶剂㊁甚至杂质将直接突破生理屏障的保护进入体内ꎬ安全性风险更大ꎬ不良反应后果也更为严重ꎮ因此ꎬ用于注射剂中的辅料也将受到更严格的监管ꎮ根据国家药品监督管理局药品审评中心(CenterforDrugEvaluationꎬCDE)发布的«化学药品注射剂基本技术要求(试行)»[21]ꎬ注射剂中应选用符合注射用要求的辅料ꎬ并尽可能采用注射剂常用辅料ꎮ对于已批准上市的注射用辅料ꎬ应提供辅料来源及质量控制的详细资料ꎬ对于尚未经国家药监局按注射途径批准生产或进口的辅料ꎬ除已在国外上市注射剂中使用的和于注射剂中有使用依据的ꎬ均应按新辅料与制剂一并申报ꎮ«新药用辅料非临床安全性评价指导原则»[22]中指出ꎬ鉴于通常药用辅料的用量相对药物活性成分本身大ꎬ并且用药途径广泛等原因ꎬ对非临床安全性评价的要求可能会比药物更为严格ꎮ对于注射剂中的辅料ꎬ应额外考察其溶血性㊁肌肉损伤㊁蛋白质结合性等ꎮ目前在我国CDE进行登记备案的环糊精种类包括γ-CD㊁β-CD及它们的衍生物HP-β-CD㊁甲基-β-环糊精(RM-β-CD)㊁HP-γ-CD㊁SBE-β-CDꎬ其中通过与制剂关联审评的有β-CD㊁HP-β-CD和SBE-β-CDꎬ注明为供注射用的环糊精仅HP-β-CDꎮ各国药典及美国食品药品监督管理局(FDA)的非活性成分数据库对用于注射的各类环糊精的收录情况不同(见表1)ꎬHP-β-CD和SBE-β-CD因其在注射剂中已被广泛使用ꎬ信息更为全面ꎮ欧洲药品管理局(EMA)于2017年10月发布的«有关人用药品辅料环糊精的问答»[23]中认为高剂量的环糊精具有活性ꎬ并可能显示出不良反应ꎬ因此对它们的安全性进行了总结评价:在注射给药方面ꎬ安全性最好的环糊精为HP-β-CD和SBE-β-CDꎬ它们被证明在较高剂量下注射给药仍安全性良好ꎬ可以250mg (kg d)-1的剂量在2岁以上人群中给药21d(HP-β-CD)或6个月(SBE-β-CD)ꎮ在新生儿和幼儿中ꎬ高剂量使用HP-β-CD和SBE-β-CD的数据虽较少ꎬ但也没有毒性迹象ꎮγ-CD的安全性次之ꎬ静脉注射剂量较高时会导致大鼠肾小管上皮可逆性空泡化[600mg (kg d)-1]或小鼠轻微肾损伤[2000mg (kg d)-1]ꎮα-CD㊁β-CD及RM-β-CD注射给药后表现出肾毒性ꎬ不适合用于注射给药ꎮEMA认为环糊精作为人用辅料可能会导致不良反应ꎬ建议在药品的说明书中添加其使用风险及阈值等安全性信息ꎮ我国虽然对注射剂辅料监管的要求十分严格ꎬ但目前尚无对环糊精在注射剂中的安全性评价要求ꎮ随着环糊精在包括注射剂的各类制剂中的应用越来越广泛ꎬ我国的药品监管部门也应加强对这种辅料的监管力度ꎬ以保证其安全合理的使用ꎮ企业在含环糊精的注射剂开发过程中也需对其安全性足够重视ꎬ进行全面的体内外评价ꎬ并在药品说明书中提供安全性资料ꎬ确保用药安全ꎮ表1 用于注射剂中的环糊精在各国药典及FDA批准药物非活性成分数据库中的收录情况环糊精种类ChP2020[15]BP2022[24]USP43[14]FDA批准药物非活性成分数据库给药途径每单位剂量最大使用量给药途径每日最大暴露量α-CDɿɿɿ腔内注射1.29mg--γ-CDɿɿɿ----HP-β-CDɿɿɿ静脉注射20%W/V静脉/肌肉注射1333mgSBE-β-CD-ɿɿ静脉注射3200mgꎻ40%W/V肌肉注射833mgHP-γ-CD-------2 已上市的环糊精包合物注射剂目前ꎬ被批准上市的十余中含环糊精的注射剂(见表2)中ꎬ仅包括α-CD㊁HP-β-CD㊁SBE-β-CD及HP-γ-CDꎬ其中HP-β-CD和SBE-β-CD的使用最为常见ꎮ因为β-CD的7个吡喃葡萄糖的结构最适于大多数药物形成包合物[25]ꎬ同时ꎬ羟丙基化和磺丁基醚化修饰改善了β-CD水溶性差及肾毒性的问题ꎬ使它们更适合于用作注射剂中辅料ꎮ在过去的三十年间ꎬ含有环糊精的注射剂已于日本㊁美国和欧洲的多个国家批准上市ꎮ2.1㊀前列地尔㊀前列地尔可用于血栓治疗ꎬ它能支持血液供应ꎬ并与抗凝剂和血小板聚集抑制剂协同合作ꎮ但前列地尔在水中的溶解度和稳定性均较差ꎬ难以直接制备成注射液ꎬ为了克服这些问题ꎬ环糊精被用于改善前列地尔的物理化学性质[26]ꎮ辉瑞(Pfizer)研发的注射用前列地尔Caverject是一种用于海绵体内注射以改善勃起障碍的药物ꎬ其早期上市处方中包含前列地尔㊁乳糖㊁柠檬酸钠和苯甲醇ꎮ后开发了一种CaverjectImpulse双腔注射器系统ꎬ与早期Caverject的不同之处主要在于CaverjectImpulse的冻干物中使用了α-CD对药物进行包合ꎬ减少了其他3种辅料的用量ꎮ因α-CD对前列地尔的药代动力学无影响ꎬPfizer在新处方申请时被豁免了临床药动学研究ꎬ仅进行了一项临床安全性和有效性研究证明新处方的安全性和有效性与原处方相当[27]ꎮ此外ꎬ添加α-CD可增强冻干物的固态稳定性ꎬ特别是抑制前列地尔分解为PGA1(一种水解产物)ꎮ早期的Caverject只能保存在20~25ħ环境中ꎬ其中40mg规格制剂25ħ以下的保质期仅3个月ꎬ而CaverjectImpulse在室温下(15~30ħ)的保质期可以达到至少两年[28]ꎬ稳定性显著提高ꎮ表2 已上市的含环糊精的注射剂环糊精种类药物名称剂型/给药途径商品名公司上市国家HP-β-CD丝裂霉素注射剂/静脉输液MitoExtraꎬMitozytrexNovartis美国盐酸特拉万星冻干粉/静脉输液VibativCumberlandPharms美国㊁欧盟丁苯酞注射剂/静脉注射恩必普石药集团中国双氯芬酸钠注射剂/静脉注射DylojectJavelinPharmsInc.英国㊁美国来特莫韦溶液/静脉注射PrevymisMerckSharpDohme美国黄体酮注射剂/肌肉或皮下注射LubionIBSA英国㊁欧盟SBE-β-CD阿立哌唑注射剂/肌肉注射AbilifyOtsuka美国㊁欧盟甲磺酸齐拉西酮注射剂/肌肉注射GeodonPfizer美国伏立康唑冻干粉/静脉输液VfendPfizer美国㊁欧盟㊁日本瑞德西韦溶液或冻干粉/静脉注射VekluryGileadSciencesInc.美国㊁欧盟㊁日本盐酸胺碘酮注射剂/静脉注射NexteroneBaxterHealthcare美国泊沙康唑溶液/静脉注射NoxafilMerckSharpDohme美国㊁欧盟㊁日本卡非佐米冻干粉/静脉输液KyprolisOnyxTherap美国㊁欧盟㊁日本德拉沙星葡甲胺冻干粉/静脉输液BaxdelaMelinta美国HP-γ-CD替肟锝[99mTc]注射剂/静脉注射CardioTecBracco美国㊀㊀还有多家前列地尔-α-CD包合物注射剂上市ꎬ如Auxilium的Edexꎬ处方中辅料为α-CD及乳糖ꎬ其临床研究[29]已证明ꎬ前列地尔-α-CD包合物在注射后可几乎完全解离ꎻOno的Prostavasinꎬ为冻干粉针剂ꎬ处方中辅料为α-CD及麦芽糖水合物ꎬ除海绵体内注射外ꎬ还可用于复溶后动脉注射以治疗慢性动脉闭塞症ꎬ或静脉滴注ꎬ用于血管移植术后的抗栓治疗等ꎮ2.2㊀双氯芬酸钠㊀双氯芬酸是最常用的非甾体抗炎药之一ꎬ具有解热和镇痛特性ꎮ自1974年以来ꎬ双氯芬酸已被证明对风湿病㊁急性关节炎症和轻度至中度疼痛极为有效ꎮ由于其溶解度低ꎬ双氯芬酸通常以其钠盐或钾盐形式使用[30]ꎮ使用丙二醇和苯甲醇作为溶剂制备的双氯芬酸钠注射剂Voltarol虽然增加了双氯芬酸钠的溶解性ꎬ但静脉刺激性大ꎬ必须在使用前稀释至100mL以上ꎬ并控制输液速度ꎮ而用HP-β-CD作为增溶剂的双氯芬酸钠注射剂Dyloject有效解决了这些问题ꎬ起效更快(30min内镇痛效果更好)且血栓性静脉炎的发生率更低[31]ꎮ这与HP-β-CD优越的增溶作用和安全性有关ꎬHP-β-CD-双氯芬酸钠注射剂静脉更刺激小ꎬ对血小板破坏效果小ꎬ且不会引发心律失常[32]ꎬ使Dyloject可以以1mL/支的小剂量在15s内完成静脉推注ꎬ迅速达到有效血药浓度ꎬ发挥效果ꎮJavelin公司还对临床给予37.5mgDyloject后HP-β-CD的安全性和药代动力学情况进行了研究[33]ꎬ约80%~90%的HP-β-CD经肾脏排出ꎬ总血浆清除率为(98.0ʃ22.7)mL min-1ꎬ终末半衰期为(2.7ʃ1.4)hꎬ连续每日剂量给药后HP-β-CD无累积ꎮ虽然肾损害程度会影响HP-β-CD的代谢情况ꎬ但与双氯芬酸钠的消除无关ꎬ且无安全性风险ꎬ故在轻度至中度肾损伤患者中无需进行剂量调整ꎮ2.3㊀来特莫韦㊀人类巨细胞病毒(humancytomega ̄lovirusꎬHCMV)疾病常见于免疫功能低下的个体ꎬ尤其是移植受者ꎮ除严重的肺炎外ꎬHCMV疾病的临床表现包括胃肠道并发症ꎬ导致口服药物的摄入和吸收困难ꎬ使治疗更加复杂[34]ꎮ目前的抗HCMV药物ꎬ如更昔洛韦㊁膦甲酸钠和西多福韦ꎬ都有显著的副作用ꎬ且出现了耐药性ꎮ来特莫韦是一种新开发的抗病毒药物ꎬ通过抑制巨细胞病毒末端酶复合物发挥作用[35]ꎬ其不良反应更小ꎬ更不易产生耐药性ꎬ且对异基因造血干细胞移植的成年HCMV血清阳性患者能起到预防作用[36]ꎮ目前上市的来特莫韦制剂有薄膜包衣片和静脉注射液两种剂型ꎬ其中静脉注射的给药方式适用范围更广ꎬ在有HCMV疾病的胃肠道并发症及移植物抗宿主病[37]的患者中均可使用ꎬ并且可以在移植后立即使用ꎬ作用更及时[38]ꎮ早期研发过程中曾开发一种来特莫韦的精氨酸磷酸盐缓冲注射剂ꎬ但其临床研究中出现局部不耐受现象ꎬ受试者输液部位存在疼痛ꎮ出于增溶性能和减少注射部位刺激性的角度考虑ꎬ一种新型基于HP-β-CD的制剂被设计用于来特莫韦静脉注射[34]ꎬHP-β-CD在来特莫韦注射液中作为赋形剂的可行性已得到证实[39]ꎬ在两种规格(240mgꎻ480mg)的注射剂中用量分别为1800mg和3600mgꎬ临床试验中未发现与HP-β-CD相关的肾损伤ꎬ且无局部不耐受现象发生ꎬ证明其在注射剂中安全性良好[40]ꎮ2.4㊀瑞德西韦㊀瑞德西韦是GileadSciences在十多年前研发的一种单磷酸酰胺前药ꎬ对RNA病毒有广泛抑制作用ꎬ被用于治疗埃博拉病毒和其他几种冠状病毒引起的感染ꎬ如中东呼吸综合征(MiddleEastrespiratorysyndromeꎬMERS)和严重急性呼吸综合征(severeacuterespiratorysyndromeꎬSARS)等[41]ꎮ它也是FDA批准的第一种用于治疗2019冠状病毒病的药物(Veklury)ꎮ由于瑞德西韦的肝脏首过效应高ꎬ不能经口服使用[42]ꎬ因此以肠外溶液的形式静脉输注是其唯一经批准的给药途径ꎮVeklury包含注射液和注射用粉末两种形式ꎬ均以SBE-β-CD为赋形剂ꎬ用量分别为瑞德西韦的60倍(6g)和30倍(3g)ꎬ虽然其中SBE-β-CD浓度较大ꎬ但各项安全性数据中均未发现其毒性作用[43]ꎮ瑞德西韦难溶于水(溶解度:0.028mg mL-1)ꎬ因此制剂中必须使用增溶剂[44]ꎮSBE-β-CD具有很好的增溶和稳定作用ꎬ永久带负电荷的SBE-β-CD能够通过非共价分子间相互作用对瑞德西韦进行包合ꎬ从而显著提高其溶解度ꎬSBE-β-CD上的磺丁基基团也对增强包合物的稳定性起到了关键作用[45]ꎮ研究显示ꎬ瑞德西韦在20%(W/W)的聚山梨酯80的水溶液中溶解度为3.9mg mL-1ꎬPEG-400溶液中为3.3mg mL-1ꎬ而在该浓度的SBE-β-CD中ꎬ溶解度可达8.5mg mL-1[46]ꎮ2.5㊀盐酸胺碘酮㊀盐酸胺碘酮是一种Ⅲ类抗心律失常药物ꎬ能阻断心脏组织中的心肌钙㊁钾和钠通道ꎬ还可以抑制α和β肾上腺素能受体[47]ꎮ除了具有抗心律失常的功效外ꎬ胺碘酮几乎没有负性肌力活性ꎬ这使其成为心血管功能受损患者的理想药物[48]ꎮ目前ꎬ胺碘酮是治疗 广谱 房性和室性心律失常的最有效㊁最常用的抗心律失常药ꎬ约占世界市场的30%[49]ꎮ最常用的胺碘酮注射剂Cordarone中使用聚山梨酯80作为稀释剂ꎬ聚山梨酯80可引起低血压ꎬ导致使用这种注射剂的患者出现低血压和心动过缓等不良反应的概率增加ꎬ1836例使用Cordarone治疗的患者中ꎬ288例(16%)发生了药物相关性低血压[50]ꎮ而新开发的胺碘酮注射剂Nexterone中ꎬ用一种没有任何血流动力学效果的稀释剂Captisol(一种磺丁基醚-β-环糊精)代替聚山梨酯80ꎬ有效改善了其副作用[51-52]ꎮ其非临床药理学与毒理学研究证明ꎬ在相同剂量下ꎬCordarone会使麻醉犬只出现低血压ꎬ而Nexterone无此不良反应[53]ꎮ临床研究表明ꎬNexterone与Cordarone在健康志愿者中生物等效ꎬ环糊精包合物的形成不影响胺碘酮的药代动力学[50]ꎮ3 环糊精注射剂的发展前景近年来ꎬ随着对环糊精的聚集特性㊁结构修饰㊁包合过程等方面研究ꎬ发现了它在新型注射剂中应用的更多可能:环糊精可以单独或与其他赋形剂组合形成聚集体ꎻ环糊精结构的结合能力也可用于修饰共轭聚合物的性质ꎬ添加靶向配体㊁生物相容性增强剂或附加疗法ꎬ用于靶向癌组织和输送各种治疗药物ꎻ通过控制环糊精环结构本身的水解ꎬ还可用于控制其内包封的药物释放[54]ꎮ这些新型改性环糊精和环糊精聚合物已经在纳米颗粒的制备㊁基因递送㊁水凝胶的形成等多方面证明了其发展前景ꎮ3.1㊀基于环糊精的注射用纳米粒㊀环糊精改善药物水溶性㊁增加载药量的能力以及纳米粒靶向给药的潜力ꎬ为环糊精和纳米粒在制剂中的联合使用提供了巨大机遇ꎬ可以在改善药物的溶解性㊁提高稳定性和包封效率㊁防止药物降解方面发挥效果ꎮ包含环糊精的纳米系统可分为仅由聚集CD和/或包合物组成的纳米粒ꎬ以及还含有其他成分的纳米粒ꎬ如聚合物纳米粒㊁基于脂质的纳米粒㊁金属纳米粒等[55]ꎮ3.1.1㊀仅由聚集CD和/或包合物组成的纳米粒㊀环糊精可在水溶液中自组装形成瞬时团簇㊁纳米粒子和小的低聚糖微粒ꎮ天然α-CD㊁β-CD和γ-CD在纯水溶液中的临界聚集浓度(criticalaggregationconcentrationꎬCAC)分别为25㊁8和9mg mL-1ꎬHP-β-CD异构体混合物的CAC估计可达到118mg mL-1或更高ꎮ药物/CD包合物的形成会使CAC发生改变ꎬ与胶束一样ꎬ水溶性聚合物可以增强环糊精的增溶效果ꎮ药物/CD包合物纳米粒的形成可以对环糊精的药物递送能力产生显著影响ꎬ增加环糊精通过某些黏膜增强药物输送的能力[56]ꎬ还可将药物输送到特定器官[57]ꎮ3.1.2㊀聚合物纳米粒㊀Ahmed等[58]合成了一种由L-赖氨酸交联琥珀酰-β-CD组成的纳米药物载体ꎬ该载体通过超分子主客体相互作用与胺碘酮结合ꎬ并具有高巨噬细胞亲和力ꎮ纳米颗粒辅助胺碘酮给药使药物靶向心肌巨噬细胞ꎬ对心脏组织的选择性递送效果提高了250%ꎬ并减少了肺部蓄积ꎬ降低了非靶向毒性ꎮJadhav等[59]采用双乳液溶剂蒸发法制备了负载地塞米松磷酸钠(dexamethasonesodiumphosphateꎬDSP)的长链脂肪酸氯化物棕榈酸疏水改性环糊精纳米颗粒ꎬ纳米颗粒粒径<120nmꎬ包封率高ꎬ稳定性好ꎮ体外溶血和体内急性毒性研究证明该改性环糊精安全性好ꎬ能作为一种可行的注射给药纳米载体系统ꎮ包封后DSP的药代动力学曲线显示AUC增加2.3倍ꎬ平均滞留时间延长ꎬ这增加了纳米粒通过高通透性和滞留(enhancedpermeabilityandretentionꎬEPR)效应外渗到炎症部位的可能性ꎮ佐剂诱导关节炎大鼠模型的药效学研究和安全性评估显示ꎬ与市售制剂相比ꎬ其抗关节炎活性极佳ꎬ且副作用显著减少ꎮ这些结果表明ꎬDSP-CD纳米粒可作为治疗类风湿关节炎的一种有前途的药物递送系统ꎮ3.1.3㊀金属纳米粒㊀含有环糊精包裹的抗癌药物的金属纳米载体在有效癌症治疗中具有巨大潜力ꎬ将药物包裹在金㊁银和金属氧化物(磁性)等金属纳米颗粒中有助于克服化疗的局限性ꎬ将抗癌药物有效地运送到靶点ꎮ此外ꎬ这些金属可以通过近红外辐射或磁场从外部触发ꎬ从而改善药物释放动力学ꎮ一些常用的化疗药物ꎬ如阿霉素㊁紫杉醇㊁甲氨蝶呤等ꎬ由于其疏水性而迅速降解ꎬ并表现出体内不稳定性ꎮ环糊精为包裹此类疏水性药物提供结构相容性ꎬ并在不显示任何全身毒性的情况下提高其负载能力㊁溶解性和稳定性[5]ꎮShelley等[60]开发了用α-CD和柠檬酸修饰的pH响应型氧化铁纳米粒ꎬ用于递送抗癌剂槲皮素ꎮ该纳米粒在肿瘤细胞的酸性环境中大量释放槲皮素ꎬ而在正常NIH-3T3细胞的细胞活力极小ꎮ这种刺激性响应的纳米粒可能会产生一种有效的抗癌分子药物递送系统ꎮ3.1.4㊀用于siRNA递送的纳米粒㊀使用阳离子改性的环糊精和核酸之间的静电力可使之相互作用聚集成纳米颗粒ꎬ用于递送siRNA[61]ꎮ由于纳米结构的产生ꎬ环糊精聚阳离子显示出两亲特性ꎬsiRNA被浓缩并封装在该结构中形成大分子ꎬ从而改善肿瘤细胞血管EPR效应ꎮ环糊精还可以导致膜破裂ꎬ从而提高siRNA的渗透性ꎮ这种破坏比单独的质子海绵效应更优ꎬ因为它不仅可以通过增加摄取ꎬ还可以通过增加核内体逃逸来改善向细胞质的输送ꎮ因此ꎬ环糊精的多功能阳离子纳米载体无论是在作为siRNA转染的合适载体ꎬ还是增加特异性靶向配体的功能后作为特定癌症治疗中的有效siRNA纳米载体ꎬ或是同时递送siRNA和化疗药物等方面均具有广泛前景[62]ꎮMonique等[63]制备了一种用于治疗亨廷顿病(HuntingtonᶄsdiseaseꎬHD)的基于修饰环糊精纳米粒的新型递送系统ꎬ该纳米粒装载有针对亨廷顿(huntingtinꎬhtt)基因的siRNAꎬ并与血脑屏障穿梭肽狂犬病病毒糖蛋白复合ꎮ体外血脑屏障模型显示ꎬ该制剂成功穿过脑内皮细胞ꎬ将包裹的siRNA释放到神经元细胞的细胞质中ꎬ并介导htt基因的部分沉默ꎬ靶向纳米粒的沉默效率比非靶向制剂高20%ꎮ证明了环糊精平台是一个用于提供基于siRNA的HD治疗药物的有希望的选择ꎬ并具有更广泛的潜力ꎬ可以治疗中枢神经系统中具有基因验证靶点的其他疾病ꎮ3.2㊀基于环糊精的注射用水凝胶㊀可注射水凝胶以液体形式注入ꎬ并通过原位化学/酶聚合或快速溶胶-凝胶相变转化为固体形式ꎬ而不需要有毒或变性交联剂ꎮ这类水凝胶的溶胶形式可以结合药物㊁蛋白质甚至细胞ꎬ实现其局部或全身应用和控制释放[64]ꎮ环糊精是一种非常有前途的柔性水凝胶构建材料ꎬ其与客体分子之间的超分子相互作用下形成的超分子水凝胶可以定义为由物理相互作用产生的高度有序的网络ꎮ由于这一特点ꎬ超分子水凝胶通常比更无序或化学交联网络的系统表现出更强的物理性能(即稳定性㊁对外部环境的响应性㊁机械性能和可逆性)ꎬ更易调节ꎬ并且能够自我修复[65]ꎮ目前已有大量基于环糊精的注射用水凝胶投入研究ꎮ环糊精的包合过程受到温度的影响ꎬ部分包合过程可在低温下形成ꎬ加热后解离ꎮ利用这一性质ꎬOkubo等[66]开发了一种缓释热响应性注射水凝胶ꎮ通过向疏水改性羟丙甲纤维素(HM-HPMC)水凝胶中加入β-CDꎬ发生包合作用ꎬ可使高黏度的HM-HPMC转变为低黏度溶胶ꎮHM-HPMC/β-CD水凝胶在接近体温时发生解离ꎬ黏度增大ꎬ转变为凝胶ꎮ向该水凝胶载体中载入胰岛素后ꎬ可使胰岛素在大鼠体内的平均滞留时间延长1.6倍ꎬ证明HM-HPMC/β-CD水凝胶是一种成功的热响应性可注射缓释水凝胶载体ꎮ可局部定位注射在肿瘤内或肿瘤周围的原位水凝胶是一种可以降低全身毒性反应㊁精准调节药物释放的有效的局部化疗载体ꎮFiorica等[67]利用透明质酸胺衍生物和乙烯砜功能化β-CD中氨基和乙烯基之间的偶氮型Michael反应ꎬ使其在37ħ的水环境中发生快速自发的交联过程ꎬ开发了一种可注射原位形成水凝胶ꎮ该载体中阿霉素被β-CD包合ꎬ可于注射部位缓慢释放ꎮ体内研究表明ꎬ该药物水凝胶可有效减小小鼠实体瘤体积ꎬ且不对其他组织造成细胞毒性副作用ꎬ证明该载体可以成为实体瘤局部化疗的有效手段ꎮ4 总结环糊精及其衍生物因其优越的增溶及稳定性能ꎬ以及良好的生物相容性和低毒性ꎬ已经在多种上市注射剂中得到应用ꎮ并且ꎬ环糊精形成聚集体的特性及其结构结合多种功能性配体的能力使其能参与纳米粒㊁水凝胶等药物递送载体的形成ꎬ实现靶向递送㊁pH响应㊁热响应㊁药物控释等多种功能ꎬ具有广阔的发展前景ꎮ但由于环糊精存在一定活性ꎬ部分环糊精具有肾毒性ꎬ在其使用过程ꎬ尤其是用于注射剂中时ꎬ必须对其安全性进行全面评价ꎮ随着溶解性更优㊁安全性更好㊁功能性更强的环糊精衍生物的开发ꎬ相信环糊精将成为难溶性药物注射剂和新型注射载体开发过程中更受青睐的选择ꎮ参考文献:[1]㊀SHEORANRꎬKHOKRASLꎬCHAWLAVꎬetal.RecentPatentsꎬFormulationTechniquesꎬClassificationandChar ̄acterizationofLiposomes[J].RecentPatNanotechnolꎬ2019ꎬ13(1):17-27.[2]SARKARAꎬFATIMAIꎬJAMALQMSꎬetal.NanoparticlesasaCarrierSystemforDrugDeliveryAcrossBloodBrainBarrier[J].CurrDrugMetabꎬ2017ꎬ18(2):129-137.[3]WONGCYꎬAL-SALAMIHꎬDASSCR.Microparticlesꎬmicrocapsulesandmicrospheres:Areviewofrecentdevel ̄opmentsandprospectsfororaldeliveryofinsulin[J].IntJPharmꎬ2018ꎬ537(1/2):223-244.[4]LOFTSSONTꎬSTEFáNSSONE.Cyclodextrinsandtopicaldrugdeliverytotheanteriorandposteriorsegmentsoftheeye[J].IntJPharmꎬ2017ꎬ531(2):413-423. [5]GANDHISꎬSHENDEP.Cyclodextrins-modifiedmetallicnanoparticlesforeffectivecancertherapy[J].JControlReleaseꎬ2021(339):41-50.[6]LIJꎬGAOHꎬYEZꎬetal.Insilicoformulationpredictionofdrug/cyclodextrin/polymerternarycomplexesbymachinelearningandmolecularmodelingtechniques[J].CarbohydrPolymꎬ2022(275):118712.[7]JICSINSZKYLꎬMARTINAKꎬCRAVOTTOG.Cyclodextrinsintheantiviraltherapy[J].JDrugDelivSciTechnolꎬ2021(64):102589.[8]何仲贵.环糊精包合物技术[M].北京:人民卫生出版社ꎬ2008.[9]LIUJꎬDINGXꎬFUYꎬetal.Cyclodextrinsbaseddeliverysystemsformacrobiomolecules[J].EurJMedChemꎬ2021(212):113105.[10]SRIPETCHSꎬPRAJAPATIMꎬLOFTSSONT.CyclodextrinsandDrugMembranePermeation:Thermody ̄namicConsiderations[J].JPharmSciꎬ2022ꎬ111(9):2571-2580.[11]CONCEIÇÃOJꎬADEOYEOꎬCABRAL-MARQUESHMꎬetal.Cyclodextrinsasexcipientsintabletformulations[J].DrugDiscovTodayꎬ2018ꎬ23(6):1274-1284. [12]JAMBHEKARSSꎬBREENP.Cyclodextrinsinpharma ̄ceuticalformulationsII:solubilizationꎬbindingconstantꎬandcomplexationefficiency[J].DrugDiscovTodayꎬ2016ꎬ21(2):363-368.[13]LIPꎬSONGJꎬNIXꎬetal.Comparisonintoxicityandsol ̄ubilizingcapacityofhydroxypropyl-β-cyclodextrinwithdifferentdegreeofsubstitution[J].IntJPharmꎬ2016ꎬ513(1/2):347-356.[14]TheUnitedStatesPharmacopeialConvention.U.S.Phar ̄macopeia43/NationalFormulary38[M].Baltimore:U ̄nitedBookPressꎬ2020.[15]国家药典委员会.中华人民共和国药典2020年版(四部)[S].北京:中国医药科技出版社ꎬ2020.[16]SERNOTꎬGEIDOBLERRꎬWINTERG.Proteinstabiliza ̄tionbycyclodextrinsintheliquidanddriedstate[J].AdvDrugDelivRevꎬ2011ꎬ63(13):1086-1106.[17]LOFTSSONT.CyclodextrinsinParenteralFormulations[J].JPharmSciꎬ2021ꎬ110(2):654-664.[18]LOFTSSONTꎬJARHOPꎬMÁSSONMꎬetal.Cyclodextrinsindrugdelivery[J].ExpertOpinDrugDelivꎬ2005ꎬ2(2):335-351.[19]SUVARNAPꎬCHAUDHARIPꎬLEWISSA.Cyclodextrin-BasedSupramolecularTernaryComplexes:EmergingRoleofTernaryAgentsonDrugSolubilityꎬStabilityꎬandBioavailability[J].CritRevTherDrugCarrierSystꎬ2022ꎬ39(5):1-50.[20]RINC N-L PEZJꎬALMANZA-ARJONAYCꎬRIASCOSAPꎬetal.Technologicalevolutionofcyclodex ̄trinsinthepharmaceuticalfield[J].JDrugDelivSciTechnolꎬ2021(61):102156.[21]国家药品监督管理局药品审评中心.化学药品注射剂基本技术要求(试行)[EB/OL].(2008-01-10)[2023-01-12].https://www.cde.org.cn/zdyz/downloadAtt?idCODE=96341bbd4a5efa390d9223e6d8202c1b.[22]国家药品监督管理局药品审评中心.新药用辅料非临床安全性评价指导原则[EB/OL].(2012-05-15)[2023-01-12].https://www.cde.org.cn/zdyz/domes ̄ticinfopage?zdyzIdCODE=9320dbe8ae0bdb1f798ad9971bcd0dc1.[23]EMA.Questionsandanswersoncyclodextrinsusedasex ̄cipientsinmedicinalproductsforhumanuse[EB/OL].(2017-10-09)[2023-01-12].https://www.ema.europa.eu/en/documents/report/cyclodextrins-used-ex ̄cipients-report-published-support-questions-answers-cyclodextrins-used_en.pdf.[24]OfficeBPC.BritishPharmacopoeia2022[S].London:TheStationeryOfficeꎬ2022.[25]STELLAVJꎬRAJEWSKIRA.Sulfobutylether-β-cyclo ̄dextrin[J].IntJPharmꎬ2020(583):119396.[26]WIESEMꎬCORDESHPꎬCHIHꎬetal.InteractionofprostaglandinE1withalpha-cyclodextrininaqueoussys ̄tems:stabilityoftheinclusioncomplex[J].JPharmSciꎬ1991ꎬ80(2):153-156.[27]FDA.ClinicalPharmacologyBiopharmaceuticsReview[EB/OL].(2002-06-11)[2023-01-12].https://www.accessdata.fda.gov/drugsatfda_docs/nda/2002/21-212_Caverject_biopharmr.pdf.[28]SHEEHYPMꎬRAMSTADT.Determinationofthemolec ̄ularcomplexationconstantbetweenalprostadilandalpha-cyclodextrinbyconductometry:implicationsforafreeze-driedformulation[J].JPharmBiomedAnalꎬ2005ꎬ39(5):877-885.[29]FDA.ClinicalPharmacologyBiopharmaceuticsReview[EB/OL].(1997-06-12)[2023-01-12].https://www.accessdata.fda.gov/drugsatfda_docs/nda/97/20649_EDEX_BIOPHARMR.PDF.[30]BOUMYAWꎬTAOUFIKNꎬACHAKMꎬetal.Electro ̄chemicalsensorsandbiosensorsforthedeterminationofdiclofenacinpharmaceuticalꎬbiologicalandwatersamples[J].TalantaOpenꎬ2021(3):100026.[31]LEESONRMꎬHARRISONSꎬERNSTCCꎬetal.Dylojectꎬanovelinjectablediclofenacformulationꎬoffersgreatersafetyandefficacythanvoltarolforpostoperativedentalpain[J].RegAnesthPainMedꎬ2007ꎬ32(4):303-310. [32]HOYSM.DiclofenacSodiumBolusInjection(Dyloject(TM)):AReviewinAcutePainManagement[J].Drugsꎬ2016ꎬ76(12):1213-1220.[33]FDA.ClinicalPharmacologyBiopharmaceuticsReview[EB/OL].(2014-12-23)[2023-01-12].https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/022396Orig1s000ClinPharmR.pdf.[34]ERB-ZOHARKꎬKROPEITDꎬSCHEUENPFLUGJꎬetal.IntravenousHydroxypropylβ-CyclodextrinFormulationofLetermovir:APhaseIꎬRandomizedꎬSingle-AscendingꎬandMultiple-DoseTrial[J].ClinTranslSciꎬ2017ꎬ10(6):487-495.[35]LJUNGMANPꎬSCHMITTMꎬMARTYFMꎬetal.AMortalityAnalysisofLetermovirProphylaxisforCytomega ̄lovirus(CMV)inCMV-seropositiveRecipientsofAlloge ̄neicHematopoieticCellTransplantation[J].ClinInfectDisꎬ2020ꎬ70(8):1525-1533.[36]KOMATSUTEꎬHODOWANECACꎬCOLBERG-POLEYAMꎬetal.In-depthgenomicanalysesidentifiednovelle ̄termovirresistance-associatedsubstitutionsinthecyto ̄megalovirusUL56andUL89geneproducts[J].AntiviralResꎬ2019(169):104549.[37]MARTYFMꎬLJUNGMANPꎬCHEMALYRFꎬetal.Leter ̄movirProphylaxisforCytomegalovirusinHematopoietic-CellTransplantation[J].NEnglJMedꎬ2017ꎬ377(25):2433-2444.[38]PIRETJꎬBOIVING.Clinicaldevelopmentofletermovirandmaribavir:Overviewofhumancytomegalovirusdrugre ̄sistance[J].AntiviralResꎬ2019(163):91-105.[39]GARRIDOPFꎬCALVELOMꎬBLANCO-GONZáLEZAꎬetal.TheLordoftheNanoRings:CyclodextrinsandthebattleagainstSARS-CoV-2[J].IntJPharmꎬ2020(588):119689.[40]FDA.ClinicalPharmacologyBiopharmaceuticsReview[EB/OL].(2017-11-08)[2023-01-12].https://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/209939Orig1s000ꎬ209940Orig1s000ClinPharmR.pdf. [41]PIÑEIROÁꎬPIPKINJꎬANTLEVꎬetal.Aggregationversusinclusioncomplexestosolubilizedrugswithcyclo ̄dextrins.Acasestudyusingsulphobutylether-β-cyclodex ̄trinsandremdesivir[J].JMolLiqꎬ2021(343):117588. [42]CAOYCꎬDENGQXꎬDAISX.Remdesivirforsevereacuterespiratorysyndromecoronavirus2causingCOVID-19:Anevaluationoftheevidence[J].TravelMedInfectDisꎬ2020(35):101647.[43]FDA.ClinicalPharmacologyBiopharmaceuticsReview[EB/OL].(2020-10-22)[2023-01-12].https://www.accessdata.fda.gov/drugsatfda_docs/nda/2020/214787Orig1s000ClinpharmR.pdf.[44]SZENTELꎬPUSKáSIꎬSOHAJDATꎬetal.Sulfobutylether-beta-cyclodextrin-enabledantiviralremdesivir:Character ̄izationofelectrospun-andlyophilizedformulations[J].CarbohydrPolymꎬ2021(264):118011.[45]VÁRNAIBꎬMALANGAMꎬSOHAJDATꎬetal.Molecularinteractionsinremdesivir-cyclodextrinsystems[J].JPharmBiomedAnalꎬ2022(209):114482.[46]LARSONN.CompositionscomprisinganRNApolymeraseinhibitorandcyclodextrinfortreatingviralinfections:UnitedStatesofAmerica:US2019083525[P].2019-03-21.[47]MHOUMADIAꎬELKHASHABMꎬPRILLIEUXSꎬetal.Characterizationoftheheatbehaviorofamiodaronehydro ̄chloride[J].ThermochimicaActaꎬ2022(708):179121. [48]FEDUSKAETꎬTHOMABNꎬTORJMANMCꎬetal.AcuteAmiodaronePulmonaryToxicity[J].JCardiothoracVascAnesthꎬ2021ꎬ35(5):1485-1494.[49]MUJOVIC'NꎬDOBREVDꎬMARINKOVIC'Mꎬetal.Theroleofamiodaroneincontemporarymanagementofcomplexcardiacarrhythmias[J].PharmacolResꎬ2020(151):104521.[50]FDA.MedicalReview(s)-Nexterone[EB/OL].(2008-12-24)[2023-01-12].https://www.accessdata.fda.gov/drugsatfda_docs/nda/2008/022325s000_MedR.pdf. [51]CHOWDHURYAꎬFERNANDESBꎬMELHUISHTMꎬetal.AntiarrhythmicsinCardiacArrest:ASystematicReviewandMeta-Analysis[J].HeartLungCircꎬ2018ꎬ27(3):280-290.[52]SOARJꎬPERKINSGDꎬMACONOCHIEIꎬetal.EuropeanResuscitationCouncilGuidelinesforResuscitation:2018Update-Antiarrhythmicdrugsforcardiacarrest[J].Re ̄suscitationꎬ2019(134):99-103.[53]FDA.SummaryReview(s)-Nexterone[EB/OL].(2008-12-24)[2023-01-12].https://www.accessdata.fda.gov/drugsatfda_docs/nda/2008/022325s000_SumR.pdf. [54]WEBSTERDMꎬSUNDARAMPꎬBYRNEME.Injectablenanomaterialsfordrugdelivery:carriersꎬtargetingmoietiesꎬandtherapeutics[J].EurJPharmBiopharmꎬ2013ꎬ84(1):1-20.[55]MENEZESPDPꎬANDRADETAꎬFRANKLAꎬetal.Ad ̄vancesofnanosystemscontainingcyclodextrinsandtheirapplicationsinpharmaceuticals[J].IntJPharmꎬ2019(559):312-328.[56]LOFTSSONTꎬSAOKHAMPꎬARSC.Self-associationofcyclodextrinsandcyclodextrincomplexesinaqueoussolu ̄tions[J].IntJPharmꎬ2019(560):228-234.[57]KONRÁDSD TTIRFꎬOGMUNDSDÓTTIRHꎬSIGURDSSONVꎬetal.Drugtargetingtothehairfollicles:acyclodextrin-baseddrugdelivery[J].AAPSPharmSciTechꎬ2009ꎬ10(1):266-269.[58]AHMEDMSꎬRODELLCBꎬHULSMANSMꎬetal.ASu ̄pramolecularNanocarrierforDeliveryofAmiodaroneAnti-ArrhythmicTherapytotheHeart[J].BioconjugChemꎬ2019ꎬ30(3):733-740.[59]JADHAVDꎬVAVIAP.DexamethasoneSodiumPhosphateLoadedModifiedCyclodextrinBasedNanoparticles:AnEfficientTreatmentforRheumatoidArthritis[J].JPharmSciꎬ2021ꎬ110(3):1206-1218.[60]SHELLEYHꎬBABURJ.RoleofCyclodextrinsinNanop ̄article-BasedDrugDeliverySystems[J].JPharmSciꎬ2018ꎬ107(7):1741-1753.[61]DAVISME.ThefirsttargeteddeliveryofsiRNAinhumansviaaself-assemblingꎬcyclodextrinpolymer-basednanoparticle:fromconcepttoclinic[J].MolPharmꎬ2009ꎬ6(3):659-668.[62]MOUSAZADEHHꎬPILEHVAR-SOLTANAHMADIYꎬDADASHPOURMꎬetal.Cyclodextrinbasednaturalnano ̄structuredcarbohydratepolymersaseffectivenon-viralsiRNAdeliverysystemsforcancergenetherapy[J].JControlReleaseꎬ2021(330):1046-1070.[63]MENDONÇAMCPꎬCRONINMFꎬCRYANJFꎬetal.Modifiedcyclodextrin-basednanoparticlesmediatedde ̄liveryofsiRNAforhuntingtingenesilencingacrossaninvitroBBBmodel[J].EurJPharmBiopharmꎬ2021(169):309-318.[64]MOHAMMADIMꎬKARIMIMꎬMALAEKEH-NIKOUEIBꎬetal.Hybridinsitu-forminginjectablehydrogelsforlocalcancertherapy[J].IntJPharmꎬ2022(616):121534.[65]TORCHIOAꎬCASSINOCꎬLAVELLAMꎬetal.Injectablesupramolecularhydrogelsbasedoncustom-madepoly(e ̄therurethane)sandα-cyclodextrinsasefficientdeliveryvehiclesofcurcumin[J].MaterSciEngCMaterBiolAp ̄plꎬ2021(127):112194.[66]OKUBOMꎬIOHARADꎬANRAKUMꎬetal.Athermore ̄sponsivehydrophobicallymodifiedhydroxypropylmethyl ̄cellulose/cyclodextrininjectablehydrogelforthesustainedreleaseofdrugs[J].IntJPharmꎬ2020(575):118845.[67]FIORICACꎬPALUMBOFSꎬPITARRESIGꎬetal.Ahy ̄aluronicacid/cyclodextrinbasedinjectablehydrogelforlocaldoxorubicindeliverytosolidtumors[J].IntJPharmꎬ2020(589):119879.(收稿日期:2023-02-03)实验研究㊀基金项目:新疆维吾尔自治区自然科学基金-杰出青年科学基金(No.2021D01E32)ꎻ乌鲁木齐市科学技术局优秀青年科技人才培养项目作者简介:娜迪热 艾尔肯ꎬ女ꎬ硕士生ꎬ研究方向:新药与医院制剂研发ꎬE-mail:1324264211@qq.com通信作者:李茜ꎬ女ꎬ博士ꎬ主任药师ꎬ研究员ꎬ研究方向:新药与医院制剂研发ꎬTel:0991-5814127ꎬE-mail:reallynana@163.com洋甘菊活性组分对LPS诱导人支气管上皮细胞的保护作用及机制研究娜迪热 艾尔肯1ꎬ2ꎬ彭军1ꎬ2ꎬ3ꎬ范芳芳1ꎬ2ꎬ李茜1ꎬ2(1.新疆医科大学第四临床医学院ꎬ新疆乌鲁木齐830000ꎻ2.新疆中药炮制研究重点实验室ꎬ新疆乌鲁木齐830000ꎻ3.新疆理化技术研究所干旱区植物资源与化学重点实验室ꎬ新疆乌鲁木齐830000)摘要:目的㊀基于驱动蛋白家族3A基因(Kif3a)和Sonichedgehog(SHH)信号通路探讨洋甘菊活性组分对脂多糖(LPS)诱导的人支气管上皮细胞(16HBE)的保护作用及机制ꎮ方法㊀用脂多糖诱导人支气管上皮细胞建立哮喘炎症细胞模型ꎮCCK-8法检测不同浓度洋甘菊活性组分对脂多糖诱导人支气管上皮细胞的增殖的抑制作用ꎬ筛选出最佳洋甘菊活性组分给药浓度ꎮ将细胞分为空白对照组㊁脂多糖模型组㊁阳性药物组(1μmol L-1地塞米松干预2h)㊁洋甘菊活性组分组(200μg mL-1ꎬ48h)ꎮAnnexinV/PI结合流式细胞术检测各组的凋亡率ꎮ实时荧光PCR法和Westernblot法检测Kif3a㊁SHH㊁Ptch1和Gli1的mRNA和蛋白表达变化ꎮ结果㊀脂多糖干预后ꎬ可显著降低人支气管上皮细胞活力(P<0.05)ꎬ并诱导其细胞凋亡(P<0.01)ꎮ洋甘菊活性组分在浓度200μg mL-1处理48h时ꎬ可以显著逆转脂多糖对细胞的损伤并促进增殖(P<0.01)ꎬ减弱脂多糖诱导的细胞凋亡(P<0.01)ꎮ与空白对照组比较ꎬ脂多糖诱导的人支气管上皮细胞内Kif3a在mRNA水平和蛋白表达水平显著降低(P<0.05)ꎬSHH㊁Ptch1㊁Gli1在mRNA水平和蛋白表达水平显著升高(P<0.05)ꎻ与脂多糖模型组相比较ꎬ洋甘菊活性组分处理后可显著逆转mRNA水平和蛋白表达(P<0.05)ꎬ增加Kif3a的mRNA水平和蛋白表达水平ꎬ并降低SHH㊁Ptch1㊁Gli1的mRNA水平和蛋白表达(P<0.05)ꎮ结论㊀脂多糖诱导人支气管上皮细胞损伤ꎬ下调Kif3a水平从而上调SHH㊁Ptch1㊁Gli1水平ꎬ调控SHH信号通路处于异常激活状态ꎮ洋甘菊活性组分可显著逆转脂多糖诱导的细胞炎症损伤ꎬ上调Kif3a水平ꎬ下调SHH㊁Ptch1㊁Gli1水平ꎬ通过Kif3a调控SHH信号通路ꎬ对脂多糖诱导的人支气管上皮细胞发挥保护作用ꎬ改善哮喘气道炎症ꎮ关键词:洋甘菊活性组分ꎻ哮喘ꎻ人支气管上皮细胞ꎻKif3aꎻSHH信号通路中图分类号:R285.5㊀文献标识码:A㊀文章编号:2095-5375(2023)05-0298-006doi:10.13506/j.cnki.jpr.2023.05.002TheprotectiveeffectandmechanismoftheactivecomponentsofMatricariachamomillaL.onLPS-inducedhumanbronchialepithelialcellsNADIRE Aierken1ꎬ2ꎬPENGJun1ꎬ2ꎬ3ꎬFANFangfang1ꎬ2ꎬLIQian1ꎬ2(1.FourthClinicalCollegeꎬXinjiangMedicalUniversityꎬUrumqi830000ꎬChinaꎻ2.XinjiangKeyLaboratoryofProcessingandResearchofTraditionalChineseMedicineꎬUrumqi830000ꎬChinaꎻ3.KeyLaboratoryofXinjiangIndigenousMedicinalPlantsResourceUtilizationꎬXinjiangTechnicalInstituteofPhysicsandChemistryꎬChineseAcademyofSciencesꎬUrumqi830000ꎬChina)Abstract:Objective㊀ToinvestigatetheprotectiveeffectandmechanismoftheactivecomponentsofMatricarlacham ̄omillaL.onLPS-induced(lipopolysaccharide)humanbronchialepithelialcells(16HBE)basedonKif3aandSHHsigna ̄lingpathway.Methods㊀LPS-induced16HBEwereestablishedastheasthmainflammatorycellmodelꎬCCK-8assaywasusedtodetecttheinhibitoryeffectoftheactivecomponentsofM.chamomileon16HBEinducedbyLPSatdifferentconcen ̄trationsꎬandtheoptimalconcentrationoftheactivecomponentsofM.chamomilewasselected.ThecellsweredividedintonormalcontrolgroupꎬLPSmodelgroupꎬpositivedruggroup(1μmol L-1dexamethasoneinterventionfor2h)ꎬandtheac ̄tivecomponentsofM.chamomilegroup(200μg mL-1ꎬ48h).CellapoptosisratewasanalyzedbyAnnexinV/PIstainingandflowcytometry.mRNAandproteinexpressionofKif3aꎬSHHꎬPtch1andGlilwereevaluatedbyreal-timePCRandWesternblotꎬrespectively.Results㊀AfterLPSinterventionꎬ16HBEcellviabilitywasreduced(P<0.05)andapoptosiswasinduced(P<0.01)ꎬsignificantly.TheactivecomponentsofM.chamomileat200μg mL-1for48hcanreversethedamageof16HBEinducedbyLPSꎬincreasedcellsproliferativeactivity(P<0.01)andreducedLPS-inducedapoptosis(P<0.01)ꎬsignificantly.ComparedwithnormalcontrolgroupꎬthemRNAlevelandproteinexpressionlevelofKif3ain16HBEinducedbyLPSweredecreased(P<0.05)ꎬandthemRNAlevelandproteinexpressionlevelofSHHꎬPtc1andGli1weresignifi ̄cantlyincreased(P<0.05)ꎻComparedwithLPSmodelgroupꎬtheactivecomponentsofM.chamomilegroupcansignificantlyreverseLPS-inducedcellsdamageꎬincreaseKif3amRNAlevelandproteinexpressionlevel(P<0.05)ꎬandreduceSHHꎬPtch1ꎬGli1mRNAlevelandproteinexpression(P<0.05).Conclusion㊀LPSinducedtheinjuryin16HBEꎬdown-regulatedthelevelofKif3aandup-regulatedthelevelsofSHHꎬPtch1andGli1ꎬwhichmakestheSHHsignalingpathwayinanabnormalstateofactivation.TheactivecomponentsofM.chamomilecansignificantlyreversetheLPS-inducedcelldamageꎬup-regulatethelevelofKif3aꎬanddown-regulatethelevelofSHHꎬPtch1ꎬandGli1.ItcanregulatetheSHHsigna ̄lingpathwaythroughKif3atoplayaprotectiveroleonLPS-induced16HBEandimproveasthmaairwayinflammation.Keywords:TheactivecomponentsofMatricarlachamomillaL.ꎻAsthmaꎻHumanbronchialepithelialcellsꎻKif3aꎻSHHsignalingpathway㊀㊀支气管哮喘(哮喘)是一种常见的慢性炎症性呼吸道疾病ꎬ影响着超过3.3亿儿童和成人ꎬ预计到2025年受影响的人口将增加到4亿[1]ꎮ随哮喘患病率的升高ꎬ已成为我国的一项重大公共卫生挑战ꎮ驱动蛋白家族3A基因(Kif3a)是哮喘的易感性位点之一ꎬ在Kif3a敲除的哮喘小鼠模型中小鼠气道反应明显增高[2]ꎮHedgehog(HH)基因家族共包括3个成员Sonichedgehog(SHH)㊁Indianhedgehog(IHH)和Deserthedgehog(DHH)ꎬSHH信号通路的上调诱导过敏性哮喘[3-4]ꎮKif3a的敲除或者突变会阻断Hedgehog信号的传导[5]ꎮ因此ꎬKif3a可通过调控SHH信号通路改善哮喘气道炎症ꎬ有效缓解哮喘症状ꎮ目前临床治疗中ꎬ常用药物是抗炎糖皮质激素及支气管扩张剂等ꎬ但长期使用引起不良反应[6]ꎮ近年来ꎬ中药在减轻哮喘症状㊁控制哮喘发作㊁防止哮喘复发等方面具有治疗优势[7]ꎮ洋甘菊又名母菊ꎬ拉丁名MatricarlachamomillaL.ꎬ«中华本草»中记载其具有散气消炎㊁软坚消肿㊁祛风止痛等功效ꎮ现代研究表明ꎬ洋甘菊具有抗氧化㊁抗炎㊁抗菌㊁抗抑郁㊁抗癌㊁保肝㊁抗糖尿病等多种药理活性[8]ꎮ洋甘菊作为新疆地区习用药材ꎬ是新疆传统名方祖卡木颗粒的主要药材之一ꎬ治疗呼吸系统疾病历史悠久[9]ꎮ洋甘菊醇提取物通过调节Th1/Th2的平衡对Balb/c小鼠巨噬细胞和淋巴细胞产生影响ꎬ发挥抗炎作用[10]ꎮ在一项关于短期服用传统草药的临床试验中ꎬ发现洋甘菊可以显著改善儿童普通感冒的哮喘症状[11]ꎮ然而ꎬ洋甘菊在改善和缓解哮喘症状的作用机制仍不清楚ꎮ前期ꎬ我们已通过工艺优化获得洋甘菊的活性组分ꎬ总黄酮含量为30.55mg g-1ꎬ其主要活性成分为黄酮(芹菜素㊁木犀草素)或类黄酮醇衍生物(槲皮素)[12]ꎮ本实验将进一步研究洋甘菊活性组分改善脂多糖(LPS)诱导人支气管上皮细胞(16HBE)的损伤ꎬ并探讨其保护作用机制ꎮ1㊀材料与方法1.1㊀细胞株㊀16HBE购自上海雅吉生物ꎮ1.2㊀仪器与试剂㊀SmartCellHF-90CO2细胞培养箱(上海力康仪器有限公司)ꎻTDL-60B台式低速离心机(上海安亭仪器厂)ꎻLSRFortessa流式细胞仪(BD)ꎻMyCyclerThermalCyclerPCR仪(Bio-Rad)ꎻ7500FastRealTimePCRinstrument(ABI)ꎻMini-PROTEANTetrasystem蛋白转膜仪(Bio-Rad)ꎻxMarkTM酶标仪(Bio-Rad)ꎮ角质细胞培养基KM(Sciencellꎬ批号:2101)ꎻ青霉素-链霉素双抗(10000U)(Gibcoꎬ批号:15070-063)ꎻPBS磷酸盐缓冲液粉剂(北京中杉金桥生物ꎬ批号:ZLI-9062)ꎻCCK-8细胞增殖/毒性检测试剂盒(全式金生物ꎬ批号:FC101-03)ꎻ脂多糖(Sigmaꎬ批号:L2630)ꎻ乳酸脱氢酶(LDH)试剂盒(南京建成ꎬ批号:A020-2-2)ꎻ地塞米松(Sigmaꎬ批号:D4902)ꎻAnnexinV-PE/7AADKit(BDꎬ批号:559763)ꎮ一抗:beta-Actin(批号:100166-MM10)购自义翘神州ꎻSHH(C9C5)抗体(批号:#2207)和KIF3A(D7G3)抗体(批号:#8507)购自美国CST公司ꎻAnti-Gli1抗体(批号:ab273018)购自Abcam公司ꎻPtch1抗体(批号:PA5-87508)购自赛默飞ꎮ二。
J Apoplexy and Nervous Diseases, Nov. 2023, Vol 40,No. 11溴吡斯的明引起重症肌无力患者心肌梗死的1例报告并文献复习周丽枝, 胡云, 周礼鑫, 童理, 杨剑文摘要: 重症肌无力是一种自身免疫性疾病,通常由针对神经肌肉接头处的乙酰胆碱受体的抗体介导,其常见的治疗有胆碱酯酶抑制剂,例如溴吡斯的明。
该药物在治疗过程中出现心血管事件较少见,但在临床中早期识别病情变化并警惕重症肌无力患者可能出现的心血管事件非常重要。
因此,我们报道重症肌无力老年女性患者继发于抗胆碱酯酶治疗导致急性心肌梗死并发心源性猝死的病例,并基于此病例对发生心血管不良事件的可能原因进行讨论。
关键词: 重症肌无力; 急性心肌梗死; 溴吡斯的明; 胆碱酯酶抑制剂中图分类号:R741 文献标识码:APyridostigmine bromide causes myocardial infarction in myasthenia gravis : a case report and literature reviewZHOU Lizhi ,HU Yun ,ZHOU Lixin , et al.(The First Affiliated Hospital of Hunan Normal University , Changsha 410005, China )Abstract : Myasthenia gravis is an autoimmune disease ,which is usually mediated by antibodies to acetylcholine re⁃ceptors at the neuromuscular junction. It is commonly treated with cholinesterase inhibitors such as pyridostigmine bro⁃mide. Although cardiovascular events with the drug are rare ,it is very important to early recognize disease changes and be alert to potential cardiovascular events in patients with myasthenia gravis. Therefore , we report a case of an elderly female patient with myasthenia gravis developing acute myocardial infarction and then sudden cardiac death following anticholines⁃terase therapy , and discuss the possible causes of adverse cardiovascular events based on this case.Key words : Myasthenia gravis ; Myocardial infarction ; Pyridostigmine bromide ; Cholinesterase inhibitor重症肌无力(myasthenia ,MG )是一种自身免疫性疾病,通常由针对神经肌肉接头处的乙酰胆碱受体的抗体介导,其特征临床表现为骨骼肌无力和易疲劳[1]。

![FDA官员灭菌药物检查指南手册7356[1].002A](https://uimg.taocdn.com/a6330113866fb84ae45c8d4e.webp)
CHAPTER 56 - DRUG QUALITY ASSURANCESUBJECT:STERILE DRUG PROCESS INSPECTIONS IMPLEMENTATION DATE *Upon Receipt*COMPLETION DATE9/30/93DATA REPORTINGPRODUCT CODES PRODUCT/ASSIGNMENT CODESIndustry codes 560O2A 54, 56,and 60-66 inclusive.FIELD REPORTING REQUIREMENTSForward a copy of each Establishment Inspe ction Report to H#-30O Attention: Division of Drug Quality Evaluation. Copies of Samples of Collection Reports and Analyst Worksheet for all samplesexcept those which are classified "1"should also be sub m itted.(This material will be used in evaluating the program).*As soon as the district becomes aware of any significant adverse inspectional, analytical, or other information which could orshould affect the agency's new product approval decisions withrespect to a firm, the district should i mm ediately notify HFC-120, Medical Products Quality Assurance Staff, via EMS or fax,and they will, i n turn, convey the information by fax orequivalent expeditious means to the appropriate Center regulatory units.*NOTE: Districts should assure that each operation performed bydirection of of this program circular is entered against thecorrect Product Code and Program/Assignment Code (P/AC).*Current Changes*TRANSMITTAL N#.90-68 (03/05/90)PARTI-BACKGOUND*This program is intended to cover the manufacture of all sterile drug products, including sterile bulk drugs, ophthalmic and o phthalm tic dosage forms, S mall Volume Parenteral (SVP) products, La rge Volume Parenteral ( LVP) products, and any other drug products required to be sterile.Biologicals, veterinary drug products, and bioassay drugs are excluded from coverage under this program.**Current Change*PART II - IMPLEMENTATIONOBJECTIVES*To provide guidance for conducting inspections of manufacturers of sterile bulk and finished dosage form drug products todetermine compliance with the Food, Drug, and Cosmetic Act andthe Good Manufacturing Practice Regulations (GMPs), Title 21, CFR Parts 210 and 211.*To initiate appropriate action against those manufacturers found to be out of compliance.To obtain information on key practices, to identify practiceswhich need correction or improvement, and to evaluate currentgood manufacturing practices in the #sterile drugs industry.PROGRAM #AGEMENT INSTRUCTIONS*I nspections of sterile product manufacturing firms will beperformed as either Full Inspections or Abbreviated inspections.In the Abbreviated Inspection, coverage will be directed to keypoints in the major systems affecting the production of thesterile drug product. If the information collected indicatesthat the firm's practices are in compliance with C GM Ps, theinspection may be concluded at this point.It should be pointed out that inspectional coverage under thisoption is not intended to limit the investigator ' s initiativein any way. If questionable practices are observed in areasoutside of the systems delineated under this option, theinvestigator is urged to expand the inspection to cover theseareas to his/her satisfaction.The Full Inspection Option involves an in depth inspection of key manufacturing systems and processes and their validation in order to maintain surveillance over the firm's activities.See Part III - inspectional and Attachment A for a completediscussion of the coverage requested under these inspectionoptions.*Current Change*This program is to be carried out when firms are inspected aspart of the regular statutory inspection cycle in accordance with the current ORA workplan. If the sterile drug products to beinspected are radioactive drugs, then CP735G.OO2C, "Radioactive Drugs", should be followed as supplementary guidance.*o Consider using a team approach in conducting theseinspections, utilizing investigators familiar with theseprocesses, and chemists, microbiologists, and engineers, asappropriate.o*Investigators or team members should be well qualified in sterile product production experience and preferably havecompleted formal training courses in parenteral drugmanufacture, sterilization methods, procedures andequipment. Microbiologists involved should have experiencein sterility/pyrogen testing and some experience in sterileproduct inspections.**Current Change*PART III - INSPECTIONAL*Refer to CP 7356.002, Drug Process inspections, for generalinformation on CGMP inspections. Refer to CP 7356.OO2C,"Radioactive Drugs" for supplemental instructions specific tora d iopharmaceutical drug products.Foreign inspections should be conducted using the guidance inthis program, taking into account the time limitation on theseinspections.This program provides two inspectional options: an Abbreviatedinspectional Option and a Full Inspectional Option. To determine which option should be used an evaluation of the following isappropriate:1. Review and EvaluationA full inspection should be conducted for initial inspections andmay also be conducted on a surveillance basis at the District 's discretion. Although it is not anticipated that full inspections will be conducted every two years, they should be conducted atless frequent intervals, perhaps at every third or fourthinspection. Also, whenever information becomes known which would question the firm's ability to produce quality products, anappropriate in-depth inspection should be performed.An abbreviated inspection should not be conducted for the initial inspection of a facility, nor when the firm has a past history of fluctuating into and out of compliance. The District shouldutilize all information at their disposal such as past historyresults of sample analyses, complaints, recalls, etc. todetermine if coverage under the abbreviated inspectional optionis appropriate for the specific firm.a. Determine if changes have occurred by comparing currentoperations against the EIR for the previous full inspection.The following type of changes are typical of those thatwould warrant the Full Inspection Option:1.New potential for cross-c ontamination arising throughchange in process or product line.e of new technology requiring new expertise,significantly new equipment or new facilities.**Current Change**b.Review the firm's complaint file, DPPRs, annual product reviews, etc. and determine if the pattern of complaints(or other information available to the District) as well asthe firm's records of internal rejection or reworking ofbatches warrant expanding the inspection to the pu11Inspection Option to look for weaknesses in the firm'sprocesses, systems or controls.c. If no significant changes have occurred and no violativeconditions are observed, the Abbreviated Inspection Optionmay be adequate.d. If significant changes have occurred, or if violative orpotentially violative conditions are noted, the inspectionshould be expanded to the Full Inspection Option to provideappropriate coverage.e. If an inspection needs to be expanded to the Full InspectionOption, it need be expanded only for the applicable generalproduct or process area in question.2.Abbreviated Inspection OptionThis option involves a more limited inspection of themanufacturer to maintain surveillance over the firm'sactivities. An Abbreviated Inspection as described below isadequate for routine coverage and will satisfy the biennialinspection requirement. The use of this option will saveinspectional and clerical resources.a. Inspections performed under this option should cover thoseitems delineated under the Fu11 Inspection Option with theexception that validation need not be covered for thosesystems and processes that have previously been coveredunder the Full Inspection Option.Perform an inspection of the firm's manufacturing facilityincluding a review of a representative number of Master andBatch Production Records (minimum of 5 batches) on productsmanufactured by the firm. Products that appear in thefirm's inspectional history of previous problems should beincluded. A brief inspection of the laboratory shouldinclude a spot c heck of a limited number of test records (atleast 10) to assure that batches are being subjected toadequate testing for conformance to specifications.**Current Changes**Special note should be taken of the firm's packaging andlabeling controls. Any observation of inadequate controlswill indicate that a Full inspectional Option should beperformed. If the following type of procedures areencountered, in-depth inspectional coverage should be givento the firm's Labeling systems:- The use of labels which are similar in size, shape,and color for different products.- The use of cut labels which are similar in appearancewithout some type of 100 percent electronicverification system for the finished product.- If the use of gang printing of cut labels is notminimized as required by current regulations.- If the firm has had more than one mislabeling recallin the past two years.- If the firm fills product into unlabeled containerswhich are later labeled under multiple private labels.If the abbreviated inspection reveals no significantobjectionable conditions, and there are no other factorsrequiring the use of the Full Inspection Option, use of theAbbreviated Inspection Option 18 adequate.Refer to the "Guide to Inspection of Bulk Pharmaceutical Chemical Manufacturing" for guidance on the applicability of CGMPs to bulk operations.3. Full Inspection OptionThe Full Inspection Option will be implemented when: (1) this is the initial inspection of the drug firm; (2) this is the firstinspection performed following a regulatory action against thefirm; or (3) the information collected under the AbbreviatedInspection indicates that the firm's practices are or may bedeficient in one or more system areas. An in-d epth inspection of all manufacturing, support, and documentation systems at the firm in question should be initiated. However, this in-depthinspection may be limited - at the discretion of the investigator - to only that system area that appears to be deficient.It is not expected that inspections performed under this optionwill necessarily result in the preparation of regulatory actionrecommendations. **INSTRUCTIONSThe inspection will focus on the major systems that impact on the safety and effectiveness of all sterile products manufactured by the firm:-sterilization procedures applied to the drug product;components; container/closures; product contact equipmentand surfaces- water systems- air handling- environmental monitoring- handling of incoming components- packaging and labeling- laboratory- lyophili z ation (where applicable)2.It is suggested that one drug product be selected and followedthroughout; if the firm utilizes more than one type of drugproduct sterilization process, one drug product representing each type of sterilization process should be selected.When selecting a drug product for review, drugs that are thesubject of DPPRs or listed in the firm's complaint files shouldbe considered.Drug product information to be reported:A. Name of Selected DrugB. Dosage SizeC. StrengthD. itch sizesE. Nu mber of batches per yearDescribe what type of sterile drug products are manufactured bythis firm:F. SVP6. LVP#. O p hthalmicsI. Sterile OticsJ. Sterile BulkK. Other (identify)Please indicate whether any of these products are lyophilized.The report should include separate sections for each unique drug product and sterilization process investigated.3.Attachment A has been provided as a reference guide for the typeof information that should be evaluated in a sterile processinspection.SAMPLE COLLECTIONCollect *documentary or physical* samples, including 'in-process samples where possible, to document any suspected adulterationand misbranding problems encountered during the inspection.If microbiological contamination is suspected, document wherepossible the conditions which could contribute microbiologicalcontamination to the product *both by collecting records andphysical samples taken aseptically at points where suchcontamination might occur, such as from the WFI system. Products found positive on initial sterility testing should also beconsidered for sampling.Physical samples should not be collected if the estimated levelof microbial contamination is low.*Collect samples for particulate matter contamination whereinspectional observations indicate poor manufacturing practiceshave possibly contributed to the introduction of particulatematter into these products or where finished product controls are inadequate to assure rejection of such units.Sample SizeFor guidance in determining sample sizes for endotoxin andsterility evaluation, refer to the respective Drug SurveillanceRequest (DSR). Such sampling may be accomplished to meet District obligations under that program, a s appropriate.Reporting*The investigator will utilize sections 590, 591, and 592 of the IOM for guidance in reporting inspectional findings.For inspections made pursuant to specific assignments from HFD-33G, all appropriate program areas should be fully reviewed andreported for all firms inspected, regardless of EIclassification.Attachment of standard operating procedures (SOPs),specifications, or other documentation in response to a question and/or to illustrate a deficiency is acceptable provided theresponse/deficiency is clearly described in all accompanyingnarrative.*Notify supervisors immediately if potentially serious healthhazards exist.*Current ChangePART IV - ANALYTI CA L*ANALYZING LABORATORIES1.Routine chemical analyses : all District laboratories exceptW#C and M L MI.2.Sterility Testing:Region Examining LaboratoryNE, MA NYK-RLSE SE-RLMW MLMISW, PA SAN-DO3.Other microbiological examinations : WEAC, NYK-RL (FOR NYKand BUF), SJN, BLT, SE-RL, CIN (for NWK and CIN), LOS, SAN,SEA, DAL and DEN (for DAL and DEN).Salmonella Serotyping Lab : MLMI.4.Chemical cross-contamination analyses by mass spectrometry(MS) : NYK-RL, DAL, SE-RL, DET, DEN, and LOS. Non-massspectrometry laboratories should call one of their ownregional MS labs and/or Division of Field Science (HFC-142)to determine the most appropriate MS lab for thedeterminations to be performed.5.Chemical cross-contamination analyses by Nuclear MagneticResonance (NMR) spectroscopy : SE-RL, NYK-RL, PHI and DET.Non-NMR laboratories should call one of their own regionalNMR labs and/or Division of Field Science (HFC-142) todetermine the most appropriate NMR lab for thedeterminations to be performed.6.Antibiotic Analyses:Examining Laboratory Drug ProductDEN-DO TetracyclinesErythromycinsNYK-RL PenicillinsCephalosporinsDivision of Drug All Other AntibioticsBiology, AntimicrobialDrugs Branch, HFD-178*7.Bioassys : Division of Research and Testing (HFD-470)8.Particulate Matter in Injectables: MLMI (HFD-470).**Current Change*ANALYSIS1.Samples are to be examined for compliance with applicablespecifications. Check analyses will be by the officialmethod, or when no official method exists, by othervalidated procedures. See CPG 7152.012.The presence of cross-contamination must be confirmed by asecond method. Spectroscopic methods, such as MS, NMR, UV-visible, or infrared are preferred. However, a secondchromatographic method may be employed, provided thechromatographic mechanisms are different (e.g., ion-pairingvs. conventional reverse phase HPLC).3.Sterility testing methods should be based on USP XXI and theSterility Analytical Manual, 1981. Other microbiologicalexaminations should be based on appropriate sections of USPXXI and BAM, 6th Edition, Chapter VII, Salmonella andcurrent supplement*Current Change*PART V - REGULATORY/ADMINISTRATIVE S#TEGYThe therapeutic significance of the drug product and thepotential adverse effect of the GMP deviation on the finishedproduct must be considered in determining whether or not aregulatory action and/or administrative action (e.g., withholding NDA/##, G#QAP non-acceptance) is indicated.When the nature of the deviations is considered in relation tothe therapeutic significance of the product(s) and it isdetermined that they pose a minimal risk to the consumer,voluntary correction by management should be sought as theprimary action. *However, this is not to imply that regulatoryaction will never be taken in such cases.* The district shouldrequire that all comm u nications for achieving voluntarycompliance by firm management be submitted in writing and containa time schedule for completion. *The field should determine ifthe schedule is a reasonable time frame and should monitor their progress.*When voluntary action is not accomplished or when the deviations observed pose a threat to the consumer, formal regulatory and/or administrative action should be recommended. When deciding thetype of action to recommend, the initial decision should be based on the seriousness of the problem and the most effective way toprotect the consumer (i.e., when non-sterile injectables arefound, injunction/recall would be the action(s ) of choice ).Outstanding instructions in the Regulatory Procedures Manual(RPM) should be followed.NOTE:The lack of a violative physical sample is not a bar to pursuing regulatory and/or administrative action providingthe GMP deficiencies have been well documented. Physicalsamples found to be in compliance likewise are not a bar topursuing action under UP charges.*The following list represents examples of deficient practiceswhich the Center believes could warrant regulatory and/oradministrative action:1.Contamination with filth, objectionable microorganisms,toxic chemicals or other drug chemicals ; or a reasonablepotential for contamination by same, with demonstratedavenues of contamination such as contact with uncleanequipment or through airborne contamination.2.Failure to assure that each batch conforms to establishedspecifications, such as NDA, USP, customer specifications,and label claims.3.Distribution of product which does not conform toestablished, specifications.**e of test methodology which is not adequate or validated.5.Deliberate blending for the purpose of diluting and hidingpyrogenic, microbiological or other noxious contamination, or where blending of a non-standard batch with one meeting specifications results in one blended batch meeting minimum specifications.6.Failure to assure that each batch is of uniform characterand quality (homogeneous).7.Conducting packaging and labeling operations in such amanner as to introduce a significant risk of mislabeling,for example, the use of cut labels which are similar inappearance without some type of 100 percents electronicverification system for the finished product.8. Failure to keep adequate records, including:o Date(s) of manufactureo QU antity manufacturedo Lot numbero T e st results and dateso L a beli i ng records and specimen of label usedo signature of person(s) responsible for accomplishing significant steps including:(1) determining yield(2)examining labeled containers for correctness oflabel(3)testing for conformance to specifications(4)blending, if required(5)assuring conformance with established manufacturingproc e dure(6)reviewing production and testing records andauthorizing release for distribution9.Failure to record distribution by lot n umb er in a mannerwhich would permit prompt recall.10.Failure to have any information which would establishstability for the intended period of use.*PART VI - REFERENCES, ATPACHMENTS, AND PROGRAM CONTACTS REFERENCES OR AIDSA.Inspection Operations Manual, Chapter 5, Part 542.58 - SterileProducts.B.Proposed CGMP's For Large Volume Parenterals published in theFederal Register, June 1, 1976.C.United States Pharmacopeia, latest revision and its supplements.D.*"Guideline on Validation of the Limulus Amebo cy te Lysate T e st asan End-Product Endotoxin T e st for Human and Animal ParenteralDrugs, Biological Products, and Medical Devices," December,1987.*E.Inspectors T e chnical Guide, Number 1, 1/9/13, "SterilizingSymbols (D, z,F."Understanding and Utilizing Values", Akers, Attia and Avis,"Pharmaceutical Technology", May 1978, pages 31-35.G.*Inspectors T e chnical Guide, Number 5, 6/9/72, "Ethylene Oxide aSterilizations, I. Calculation of Initial Gas Concentration". H.*Principles and Methods of Sterilization in Health Sciences,Charles C. Thomas Co., (1969), p. 508.*I.*Inspectors T e chnical Guide, Number 6, 4/28/72, "Leak-TestingSealed Am puls of Parenteral Solutions"*J.*"Parenteral Preparations", Avis, Chapter 36, pp. 498-524 in Remington's Pharmaceutical Sciences; Edit. Martin; MackPublishing Co., (1965).*K.*Inspectors Technical Guide, Number 24, 7/30/76, "Air Velocity Meters".*L.*Inspectors Technical Guide, Number 25, 9/1/76, "Ethylene Oxide Sterilizations, II. Graphical Aid to Determine GasConcentration".*M.*Inspectors Technical Guide, Number 32, 1/12/79, "Pyrogens, Stilla Danger".*N.Inspectors Technical Guide, Number 36, 10/21/80, "Reverse Osmosis".0.*Inspectors Technical Guide, Number 41, 10/18/85, "ExpirationDating and Stability Testing for Human Drug Products".*P.*Inspectors Technical Guide, Number 43, 4/18/86,."Lyophilization of Parenterals".*Q.Federal Standard 209, #current revision,*R.Remington's Pharmaceutical Sciences, *Current Edition*S.*"Guideline on Sterile Drug Products Produced by Aseptic Processing, # June 1987.*T.*"Guideline on General Principles of Process Validation," May 1987.*U.*Regulatory Procedures Manual, Part 8.*V."Guideline to Inspection of Bulk Pharmaceutical Chemical Manufacturing, Revised November 1987.ATTACHMENTSA-Reference points to be covered as appropriate to thetype of inspection being performed, and the type ofproduct and/or manufacturing system being evaluated.B-To be completed for each type of Biological Indicator and/or Product.CONTACTS*The area code for commercial calls to all headquarters contacts is 301.* A. ORA1.Jay S. AllenInvestigations Operations Branch/DFI/ORO (HFC-l33) Telephone: FTS 443-33402.Methods InquiryDivision of Field Science/ORO (HFC-l40), #lephone: FTS443-*3007*B. CDER*Manufacturing Surveillance Branch (HFD-336)Division of Drug Quality EvaluationTelephone: 8-295-8107**Current Change*PART VII - CENTER RESPONSIBILITIESThe Division of Drug Quality Evaluation (HFD-330) will evaluate all reports. Results 0f these evaluations will be shared with the field, ORA, and interested headquarters units.*Current Change*GUIDE TO EVALUATION OF STERILE PROCESS INSPECTIONSThe following reference questions are provided for evaluation of specific drug products, manufacturing systems, and quality control procedures.The points have been numbered for easier reference in the EIR narrative.COMPONENT STORAGE AND PREPARATION1.Does the firm have adequate written procedures describing thereceipt, handling, that are represented to be sterile and/orpyrogen free? (per 21 CFR 211.80 - 211.94; 211.184)2.Have these procedures been followed for the selected drugproduct?3. Are any colorants used (none are permitted)?4.Does the firm have written control procedures that adequatelydescribe the receipt, storage, sampling, issuance, andreconciliation of labeling and packaging materials? (per 21 CFR211.122 - 130; 211.134 and 211.137).5.Does the firm use cut or rol1 labels?6.Are the labels similar in color, shape, size and format fordifferent products or potencies?7.Does the firm use any type of electronic label verificationsystem (bar codes, machine vision systems, etc.)? Describe8.Is the label verification on receipt, on line, or both?9.Is any printing done on line of label text, lot number,expiration date, etc.?10.Does the firm use dedicated packaging lines?11.Are the samples of labels used for acceptance (proofing) oflabels from vendors based on a statistical plan? Describesampling plan.12.Are labels printed by the firm or by an outside vendor?13.Have these procedures been completely and accurately followed forthe subject drug product?EVALUATION SYSTEMS14.Does the firm have an SOP on vendor audits?15.Has the firm audited the (a) component, (b) container, (c) closure, and (d) label vendors? Report the dates of last audits.16.Does the firm have written procedures for the production andprocess control of drug products? (per 21 CFR 211.100, - 211.115;211.186; 211.188; 211.192)17.Have these production and process control records been approvedby the firm's quality control unit and by designatedorganizational units?18.Have these process control records been completely and accuratelyprepared for the subject drug product?19.Briefly describe the firm's procedures for changing any of thestandard operating procedure documents described above.20.Does the firm have written procedures for the review and approvalof all drug production and control records before release of the batch for distribution? (21 CFR 211.192)21.Were these procedures followed in the review of the selected drugproduct?22.What are the firm's procedures for the investigation to be madefollowing any unexplained discrepancy found in batch productionrecords, or the failure o f a batch or any of its components tomeet specifications? (21 CFR 211.192)23.Were these procedures followed accurately and thoroughlyconcerning any batch discrepancies/failures of the selected drug?24.Does the firm have written laboratory control mechanisms,including change control procedures, which describe conformanceto established specifications and standards for the selected drug product? (21 CFR 211.160-167)25.Were all specified in-process and end product tests performed onthe selected drug product?26.Were all specifications met?*Current Change*MAJOR SYSTEMS AND PROCESSESMonitoring of Environment27.Is the air supplied to critical areas (exposed product/fillingareas) filtered through HEPA filters under positive pressure? 28.Is the air flow in critical areas laminar when delivered to thepoint of use? At what velocity? Is velocity determined at thecritical area or at the filter face?29.How is the air filtered that is s upplied to controlled areas(where unsterilized product, in-process materials, andcontainer/closures are prepared)?30.What are the firm's air quality classifications for:a.exposed product areasb.filling areac.surrounding plant areas31.Is room classification system based upon Federal Standard 209d orother?32.Are HEPA filters efficiency tested?33.How often are HEPA filters integrity tested? What test method isused?34.How often are air flow velocities checked for each HEPA filter?35.Does the firm have a written monitoring program for classifiedareas that included a scientifically sound sampling schedule that describes sampling locations, their relation to the workinglevel, and frequency? Describe the basis for the samplingprogram. (21 CFR 211.160)36.Are both viable and non-viable particulate samplings performed inall classified areas during production?37.Report the frequency of viable sampling using "active" samplingmethods for:a.exposed product areasb.filling areasc.surrounding areas38.Report the limits used, length of sampling period, and ifsampling is done during production or at rest.39.Report the type of viable sampling equipment use (STA,Centrifugal sampler, etc.)。
TWEEN® 80Product Number P 5188 Store at Room TemperatureProduct DescriptionCAS Number: 9005-65-6Specific gravity: 1.07 (25 °C)HLB (hydrophile-lipophile balance) value: 15.01,2 Critical Micellar Concentration (CMC): 13-15 mg/liter1,3 Brookfield Viscosity: 400-620 cps (25 °C, neat) Micelle molecular weight: 76 kDa3Synonyms: Polysorbate 80, PEG (80) sorbitan monooleate, polyoxyethylenesorbitan monooleate TWEEN 80 is a polyethylene sorbitol ester, with a calculated molecular weight of 1,310 daltons, assuming 20 ethylene oxide units, 1 sorbitol, and1 oleic acid as the primary fatty acid.4 Fatty acid constituents of this product are determined by transesterification to yield fatty acid methyl esters, which are identified by gas chromatography. Typically the fatty acid composition is approximately 70% oleic acid with several other fatty acids such as palmitic acid indicated.TWEEN 80 has been widely used in biochemical applications including: solubilizing proteins, isolating nuclei from cells in culture,5 growing of tubercule bacilli,6 and emulsifying and dispersing substances in medicinal and food products. It has little or no activity as an anti-bacterial agent1 except it has been shownto have an adverse effect on the antibacterial effect of methyl paraben and related compounds.7 Polysorbates have been reported to be incompatible with alkalis, heavy metal salts, phenols, and tannic acid. They may reduce the activity of many preservatives.8Product No. P 5188 is designated as Molecular Biology grade and is suitable for molecular biology applications. It has been analyzed for the absence of endonuclease-exonuclease and RNAse.Sigma also offers these additional TWEEN 80 products.P 1754 - for general use.P 4675 and P 4780 - tested in cell culture applications. P 8074 - SigmaUltra - extensively tested for trace metals.P 6224 - non animal source. Precautions and DisclaimerFor Laboratory Use Only. Not for drug, household or other uses.Preparation InstructionsTWEEN 80 is miscible in water (0.1 ml/ml) yielding a clear to slightly hazy faint yellow solution. It is reported to be miscible with alcohol, cottonseed oil, corn oil, ethyl acetate, methanol, and toluene, but insoluble in mineral oil.4 The pH of a 1% aqueous solution is5.5-7.2.Storage/StabilityAqueous solutions of polysorbates as well as the neat liquid will undergo autoxidation over time, with changes being catalyzed by light, increased temperature, and copper sulfate.9 Solutions are reasonably stable at 2 - 8 °C for short periods. For special applications, storage under argon or nitrogen may be preferred.The product is not sterile. Autoclaving of solutions is generally not advised. Sterile filtration is more easily done if the liquid is warmed to about 40 °C and alternate portions of hot distilled water and TWEEN 80 are poured through the 0.22 µm filter. The TWEEN 80 will blend and remain in solution.References1. Data for Biochemical Research, 3rd ed., Dawson,R. M. C., et al., Oxford University Press (NewYork, NY: 1986), p. 289.2. Neugebauer., J. M., Detergents: An overview.Methods Enzymol., 182, 247 (1990).3. Protein Purification Methods: A PracticalApproach., Harris, E. L. V., and Angal, S., eds.,IRL Press at Oxford University Press (New York,NY: 1990), p. 71.4. The Merck Index, 11th Ed., Entry #7559.5. Fisher, H. W. and H. Harris, Proc. R. Soc. B, 156,521 (1962).6. Dubos, R. J. and B.D. Davis, J. Exp. Med., 83, 409(1946).7. Disinfection, Sterilization & Preservation, 4th Ed.,Block, S.S. (Lea & Febiger Pub., 1991) Chapter 4.8. Martindale: The Extra Pharmacopoeia, 30th Ed.,Reynolds, J. E. F., ed., PharmaceuticalPress(London, England: 1993) p. 1030. 9. Donbrow, M., et al., Autoxidation of polysorbates.J. Pharm. Sci., 67, 1676-1681 (1978).TWEEN is a registered trademark of Uniqema, a business unit of ICI Americas Inc.RLG 11/05Sigma brand products are sold through Sigma-Aldrich, Inc.Sigma-Aldrich, Inc. warrants that its products conform to the information contained in this and other Sigma-Aldrich publications. Purchaser must determine the suitability of the product(s) for their particular use. Additional terms and conditions may apply. Please see reverse side ofthe invoice or packing slip.。
CPGM 7356.002A 无菌药品生产检查2015/09/11现场报告要求:企业检查报告(Establishment Inspection Reports ,EIRs)通过应用TurboEIR中的特定模块或可被监管事务办公室(Office of Regulatory Affairs,ORA)和药品审评和研究中心(Center for Drug Evaluation and Research,CDER)同时查看的替代性系统,以电子形式进行创建及存档。
对于因未能遵守适用于无菌药品工艺检查的美国联邦法规21卷第210和211部CGMP,而被归为官方行动指示(Official Action Indicated,OAI)的例行商业生产检查,依照监管程序手册(Regulatory Procedures Manual,RPM)的要求,通过MARCS-CMS递交通知、行政或司法行动的建议书。
各区分局需根据现行现场活动合规追踪系统(Field Activities Compliance Tracking System,FACTS)、全景图和CMS程序,立刻报告重大问题,包括快速提交和变更OAI通知。
检查过程中,当获取到有关不恰当的不良事件(Adverse Drug Experience,ADE)报告、未获批药物问题,或批准后报告违规行为(补充申请、现场警示报告(Field Alert Reports,FARs)等)的信息时,应按照适用的合规项目提供的指示以及EIR中单独的说明进行报告。
与这些检查活动相关的数据系统信息应根据单独的项目任务代码(Program Assignment Codes,PACs)报告。
在这些项目中,如扩大覆盖范围进行CGMP检查,应根据此合规项目进行报告。
要求各区分局应用此合规项目进行所有无菌药品工艺检查。
注:各区分局需保证按照此项目通知的指示执行的各项操作,需输入正确的产品编码和项目/任务代码(Program/Assignment Code ,P/AC)。
Food and Drug AdministrationCompliance Program Guidance Manual PROGRAM 7356.002F*Current Changes*FORM FDA 2438g (Computer Generated, 05/98)PAGE 1 of 30CHAPTER 56 - DRUG QUALITY ASSURANCE SUBJECT:*ACTIVE PHARMACEUTICAL INGREDIENTS (APIs)*IMPLEMENTATION DATE Upon ReceiptCOMPLETION DATEContinuingDATA REPORTINGPRODUCT CODES PRODUCT/ASSIGNMENT CODESIndustry Codes: 54 and 56 See Below56002F -Active Pharmaceutical Ingredient Process Inspections (Drug Quality Assurance)56008A -Drug Product Surveillance, CDER Initiated 56008H -Drug Product Surveillance, Imported Drugs, CDER and District Initiated Surveys 56R806-Foreign Routine Drug Surveillance Inspections*FIELD REPORTING REQUIREMENTSOAI ALERTSWhen the district becomes aware of any significant adverse inspectional, analytical, or other information that could or should affect the agency's new product approval decisions with respect to an *activepharmaceutical ingredient manufacturer referenced in an application, *the district should immediately notify HFC-240, Medical Products Quality Assurance Staff, via EMS or FAX. HFC-240 will thenconvey the information by FAX or equivalent expeditious means to the *Division of Manufacturing and Product Quality (HFD-320) in CDER's Office of Compliance.*PROCESS PROFILE REPORTING*In December 1995, at the request of CDER, the Medical Products Quality Assurance Staff (HFC-240) added profile classes CSN (Non Sterile API by Chemical Synthesis) and CSS (Sterile API by Chemical Synthesis) to the drug profile classification system. This change was requested because separate profile classes existed for nonsterile and sterile active pharmaceutical ingredients produced by fermentation processes, but the same did not hold true for active pharmaceutical ingredients produced by chemical synthesis processes. In implementing the change, however, MPQAS did not eliminate the profile class "CCS" because deleting the latter would have caused a loss of history in the GWQAP profiling system. Therefore, effective with this program circular, discontinue using Profile class CCS (Chemical Synthesis Crude Drug) and use only the following seven bulk profile classes to report the processes covered during API inspections:*FULL DESCRIPTION PROFILE CLASSNon Sterile API by Chemical Synthesis CSNSterile API by Chemical Synthesis CSSNon Sterile API by Fermentation CFNSterile API by Fermentation CFSPlant/Animal Extraction API CEXBiotechnology API CBICrude Bulk Not Elsewhere Classified (i.e., producers CRU*of bulk intermediates, and contract micronizers of APIs)*Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE 2 of 30REPORTING TO FORENSIC CHEMISTRY CENTER (FCC):*In order to assure that foreign firms supply the requested profile samples and documentation (See Page 12, Items 1 & 2), the Forensic Chemistry Center (FCC) should receive a copy of the coversheet for all inspections of foreign active pharmaceutical ingredient manufacturers. The coversheet endorsement should include a phone and fax number of the contact person at the firm. If a sample is not collected by the investigator during the inspection, the coversheet should also state that the manufacturer was instructed to collect and ship a sample and applicable records directly to FCC as per Appendix B. This will permit proper follow-up by FCC and also serve to identify the investigator who will receive a copy of the annotated collection report prepared by FCC. On a quarterly basis, FCC will send a summary of sample testing results to the Foreign Inspection Team (FIT), HFD-322.The container/closure and product information obtained from Appendix B will be included in the Active Pharmaceutical Ingredient Databases and made available to District Import Offices to help prevent counterfeit APIs from entering the United States market.*REPORTING TO CDER S DIVISION OF MANUFACTURING AND PRODUCT QUALITY: For domestic inspections of active pharmaceutical ingredient manufacturers, submit a copy of the EIR coversheet, FD-483, and District issued copy of Warning Letters (after CDER review and concurrence) to CDER's Division of Manufacturing and Product Quality, HFD-320, for review and trend analysis.*Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE 3 of 30*Current Changes*FORM FDA 2438g (Computer Generated, 05/98)PAGE 4 of 30PART I - BACKGROUND*Since the late 1980's, the U.S. Food and Drug Administration has intensified its inspectional coverage of active pharmaceutical ingredient (API) manufacturers. This is due, in part, to an increased awareness that API quality plays a potentially significant role in the quality, efficacy, and safety of finished dosage form pharmaceuticals. For example, physical properties of APIs formulated into solid oral dosage forms,suspensions, and topicals may adversely affect drug product dissolution/bioavailability. In addition,extremely small quantities of unidentified or uncharacterized impurities in drugs may cause serious patient side effects.FDA has long recognized that CGMP concepts, embodied in the good manufacturing practice regulations for finished pharmaceuticals (21 CFR 210 and 211), are valid and can be applied to API processes. These concepts include, among others, building quality into the product, employing appropriately qualified and trained personnel, establishing adequate written procedures and controls, establishing a system of in-process and end product tests, process validation, and ensuring stability of APIs for the intended period of use.*The *September 1991 FDA Guide to Inspections of Bulk Pharmaceutical Chemicals, reformatted in May 1994 with minor editorial changes, contains general guidance as to the extent and application ofGMP/validation concepts to API production and agency expectations regarding tests for impurities and impurity profiles. This guide must be used for inspection of both foreign and domestic facilities to promote inspectional consistency and uniformity.**At present, FDA expects API manufacturers to apply CGMPs to all steps of an API process, beginning with the use of starting materials, and to validate critical process steps that impact the quality and purity of the final API. This approach recognizes that the control needed is highly dependent on themanufacturing process and that the level of control increases throughout the synthesis as the processproceeds from early intermediate steps to final isolation and purification steps. This approach also allows appropriate levels of control, depending on the process itself (i.e., fermentation process vs. chemical synthesis) and the risk or criticalness associated with the specific process step being performed.This "control all manufacturing steps, validate critical process steps " approach is embodied in the draft FDA Guidance for Industry on the Manufacture, Processing or Holding of Active Pharmaceutical Ingredients, which was released for public discussion on September 20, 1996. The latter can be obtained from CDER s Drug Information Branch, HFD-210, or can be downloaded from CDER s Home Page at /cder/api.htm.*PART II - IMPLEMENTATIONOBJECTIVEThe primary objective of this compliance program is to provide comprehensive CGMP inspectional coverage of the domestic and foreign active pharmaceutical ingredient (API) industry in all profile classes (processes).PROGRAM MANAGEMENT INSTRUCTIONS*This program circular applies only to active pharmaceutical ingredients intended for use in drug products. An active pharmaceutical ingredient is defined as any substance that is represented for use in a drug and that, when used in the manufacturing, processing, or packaging of a drug, becomes an active ingredient or a finished dosage form of the drug. Although the agency has used the terms bulk pharmaceutical chemicals and bulk drug substances to describe these materials, FDA is aware that the term active pharmaceutical ingredient has international recognition. In light of this and for added clarity, the agency is adopting the term active pharmaceutical ingredient for use in this compliance program.**Owners or operators of all domestic drug establishments, to include APIs, not exempt under section510(g) of the Federal Food, Drug, and Cosmetic Act, as amended, or 21 CFR 207.10 are required to register and to submit a list of every drug in commercial distribution. Foreign drug manufacturers are not required to register, although they are required to list all drugs imported or offered for import into the United States. Refer to 21 CFR 207.40 for additional information on drug listing requirements for foreign drug establishments.*Although the current good manufacturing practice (CGMP) regulations, 21 CFR 210 and 211, do not apply to APIs, active pharmaceutical ingredients are subject to the broad requirement of Section501(a)(2)(B) of the Act in that they must be prepared in conformance with current good manufacturing practice. *No distinction is made between APIs and finished pharmaceuticals in the Act, and failure of either to comply with CGMP constitutes a violation of the Act.* Therefore, in this document, the term CGMP refers to the latter, rather than 21 CFR 210 and 211 provisions.*Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE 5 of 30EXCLUSION*This program circular does not apply to the sterilization and aseptic processing steps of sterile active pharmaceutical ingredients, which are covered by Compliance Program 7356.002A, Sterile Drug Process Inspections. The FDA has long maintained that sterile APIs are finished drug products subject to the CGMP regulation for finished pharmaceuticals (21 CFR 210 and 211) because these are repacked as finished dosage forms under aseptic conditions without further purification or processing.**Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE 6 of 30PART III - INSPECTIONAL*Inspections of active pharmaceutical ingredient manufacturers, whether foreign or domestic, should be conducted by experienced investigators with education and/or training in fermentation, chemical synthesis, recombinant DNA, and other biotechnology manufacturing methods. Use of chemists and/or microbiologists during API inspections is recommended, particularly for evaluating laboratory operations (e.g., analytical methods evaluation, analytical data, lab procedures and instrumentation), analytical review of methods used to establish impurity profiles, fermentation manufacturing processes, and complex multi-step chemical synthesis processes.**Investigators conducting API inspections must understand the basic differences between the processes used for the production of APIs and those used for finished dosage forms. APIs are usually produced by chemical synthesis, recombinant DNA technology, fermentation, enzymatic reactions, recovery from natural materials, or combinations of these processes. The production of APIs typically involves significant changes of starting materials or intermediates by various chemical, physical, and biological processing steps. Purification is the ultimate objective.In contrast, finished drug products are formulated from bulk raw materials that are usually subjected to some degree of quality control by the users (dosage form manufacturers). Most important, the manufacturing processes for finished pharmaceuticals typically do not involve purification steps.For these reasons, the manufacturing and quality controls employed in API production and their application throughout the process (i.e., stringency of controls, written instructions, in-process controls, sampling, testing, monitoring, and documentation employed in early processing steps vs. later isolation and purification steps) differ somewhat from those found in finished dosage form plants. These differences, however, are simply reflections of different manufacturing processes, not inherent differences in the importance of GMPs for the two types of production.**Since manufacturers of active pharmaceutical ingredients are often referenced in many drug applications, each inspection should cover as many API processes as is feasible. This strategy will maximize the use of agency resources and avoid repeated visits to the same manufacturing site to cover different API profile classes referenced in subsequent applications. Thus, effective with this CP revision, all inspections of API manufacturers, regardless of how these are initiated, will be "GMP qualifying inspections." Inspections should cover the specific API profile classes referenced in the assignment and all other API profile classes not inspected in the last two years.*Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE7 of 30For foreign API firms, investigators should only cover profile classes for APIs intended to be marketed or already marketed in the United States.APIs selected for coverage should include those referenced in drug applications, are therapeutically significant, are intended for use in parenteral drug products, are difficult to manufacture, or those on record as having past compliance problems. However, this does not preclude the selection of less therapeutically significant active pharmaceutical ingredients to evaluate specific API processes (profile classes) not previously given in-depth coverage at the facility.Investigators conducting API inspections should understand the general inspection strategy set forth in Part II of this program. Recognizing that API firms vary greatly in size, diversity of operations, and quality assurance systems, investigators should carefully plan their inspectional strategy at each firm. Of particular concern are API manufacturing operations located in developing countries. *Impurities and contaminants present in components, process water, and solvents used in the production of APIs may carry over into the active pharmaceutical ingredient and may not be detected by analytical tests conducted by either the API manufacturer or the dosage form manufacturer. During inspections, investigators should review the quality of process water and solvents used in isolation and purification steps, the firm's procedures for preventing API contamination/cross-contamination, procedures for controlling impurities, and the procedures and test methods for establishing a complete impurity profile for each API process.* These are covered in detail in the September 1991 FDA Guide to Inspection of Bulk Pharmaceutical Chemicals and its "Appendix A."During inspections, investigators should review the batches manufactured during the last year to determine not only those released, but any rejections. The firm s policy on reprocessing and reworking of APIs should also be examined. Some batches start off as a pharmaceutical grade and then become technical grade. This could indicate a problem with the validated process. In addition, equipment cleaning validation should be reviewed to assure that the firm can remove residues, microbial contamination, and endotoxins to acceptable levels when the end product is intended for parenteral or liquid dosage forms.*For API inspections initiated by a preapproval assignment, review guidance provided in CP 7346.832, Pre-Approval Inspections/Investigations, and assess the authenticity and accuracy of data contained in drug applications and drug master files. Report inspectional time under the appropriate program assignment codes (PACs) referenced in both compliance programs, based on coverage afforded to each program.**Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE8 of 30*CHANGES IN THE FOREIGN DRUG INSPECTION PROGRAMBeginning in FY 97, ORA and CDER agreed to implement several changes to the foreign drug inspection program to streamline the compliance review process. The Division of Emergency and Investigational Operations (ORO/DEIO), will continue to work with foreign governments in scheduling foreign inspections, making travel arrangements for inspection teams, and resolving logistical problems. However, new procedures are in effect for handling a foreign firm's response to an FD-483, submitting establishment inspection reports, and commenting on a foreign firm's response to an FD-483. Investigators should instruct management at foreign firms to submit the original written response to an FD-483 directly to CDER's Office of Compliance with a copy to the lead investigator. The original response with appropriate documentation should be submitted to the following address: Food and Drug AdministrationForeign Inspection Team, HFD-322Division of Manufacturing and Product QualityCenter for Drug Evaluation and Research7520 Standish PlaceRockville, Maryland 20855-2737Investigators and analysts will submit written comments regarding a foreign firm's response to an FD-483 directly to CDER's Foreign Inspection Team (FIT). After appropriate district office review and endorsement, all foreign establishment inspection reports (EIRs) will be promptly forwarded to FIT for review and final classification. FIT will continue to issue Warning Letters, Untitled Letters and other correspondence to foreign firms. FIT will also recommend automatic detention of foreignfirms/products, make recommendations to review units, and request follow-up inspections, as appropriate.*INSPECTIONReview the September 1991 FDA Guide to Inspections of Bulk Pharmaceutical Chemicals, (Reformatted May 1994) to become familiar with the various areas and topics that must be considered when conducting API inspections. Appendix A of this CP program is a summary of areas to be covered during API inspections. Photocopy this appendix and take with you*Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE9 of 30during inspections. Also obtain a copy of the drug application and/or Drug Master File (DMF), as applicable, and review these before initiating the inspection.Third (field) copies of applications, *supplements and annual reports* are now required (Refer to 21 CFR 314.440) and such copies are submitted by domestic firms directly to the applicant's home FDA district office. Foreign *applicants* are required to submit third copies of applications to the same headquarters units receiving the first and second copies. These are made available by DEIO to investigators before initiation of foreign inspections.*Investigators should review all available information including prior inspectional information, FD-483s and responses, any Warning Letters, the firm's compliance history, sample analysis results, complaints, recalls, etc., to prepare for the inspection. For domestic inspections, the information is available from the Pre-Approval Monitors (PAMs) at each District Office. For foreign inspections, the information is available from DEIO or FIT.**Additional suggested references that Investigators and Chemists should be familiar with include: the draft Guidance for Industry - Manufacture, Processing or Holding of Active Pharmaceutical Ingredients; USP <1086> Impurities in Official Articles; and the recent changes in tests for the presence of foreign substances and impurities, contained in Page 3636 of USP-NF Supplement 6, effective May 15, 1997. In addition, the Investigator should contact the Forensic Chemistry Center (FCC) to determine which APIs should be sampled, so that duplicates are not collected during different inspections.**The Investigator should consult the CDER Case Officer for clarification of the assignment to assure that they are aware of the previous deficiencies at the firm. During the inspection, assure that all the firm s promised actions are effective at correcting the problems. If the inspection determines that the firm has resolved all the deficiencies, submit the information for input into the CARS computer system.**Conduct a "GMP qualifying inspection" at each API manufacturer covering the products and processes specified in the assignment. In addition, cover in as far as possible, API processes that have not been inspected in the last two years. Also, conduct an in-depth inspection, to include examining pertinent systems and processes, whenever the District receives adverse information regarding a firm's ability to produce APIs of acceptable quality.*During inspections of API manufacturers:*Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE10 of 301.*Determine if the firm has made process changes by comparing current operations against the Establishment Inspection Report (EIR) for the previous inspection. Also compare the current operations with those filed in the Drug Master File or the drug application to determine whether the firm is complying with commitments made to the agency. The following changes are typical of those that would warrant *extensive coverage* during the inspection:a.New potential for cross-contamination arising through changes in API processes orproduct lines, to include processing numerous APIs of varying therapeutic significance incommon equipment and/or facilities.e of new technology requiring new expertise, significantly new equipment or newfacilities.c.*Recent changes in starting materials, intermediates, equipment, facilities, supportsystems, processing steps, packaging materials, and computer software that are not referenced in the DMF or application.*2.Verify that the size of the largest batch does not exceed the maximum working capacity of the firm's largest blender that is used for blending of API batches.3.Review the firm's complaint file. Determine whether the pattern of complaints (or other information available to the District) and the firm's records of internal rejection or*reprocessing/reworking* of API batches warrant expanding the inspection. Look for weaknesses in the firm's processes, systems or controls.4.Investigate the return of APIs for any reason. Determine whether the firm conducts investigations on returned products to find out if these APIs failed to meet specifications or were contaminated. Also determine the final disposition of returned APIs, i.e., whether reprocessed or destroyed.5.If the inspection is initiated because the firm *is referenced as an API supplier in a drug application (NDA, ANDA, AADA), evaluate operations against commitments in the application and/or drug master file. Also, verify the authenticity and accuracy of data submitted in the application and/or DMF.**Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE11 of 306.*Obtain a copy of the impurity profile for each active pharmaceutical ingredient process covered during the inspection and compare these to the impurity profiles submitted in the Drug Master File.*All Establishment Inspection Reports for API manufacturers must include:1.History of business, and any corporate affiliations.s, titles, *and complete mailing address of most responsible officials who should receive correspondence from FDA.*3. A list of APIs manufactured (or categories of products if many) along with the general manufacturing process for each (for example, chemical synthesis non-sterile, fermentation, extraction of natural products, etc.).4.*For foreign API manufacturers, the names, titles, complete mailing address, telephone and Fax number of the firm's U.S. Agent, Regulatory Agent, and/or Importer/Broker.*5.*For foreign API manufacturers, a report of all active pharmaceutical ingredients imported into the United States in the last three years, their consignees, and an estimate of the frequency and quantity of shipments to these consignees.*6. A description of areas/processes inspected (i.e., what areas, systems and processes were inspected, who was interviewed, what manufacturing activities were ongoing during the inspection).7. A description of any non-drug manufacturing activities conducted by the firm, such as processing pesticides or other toxic chemicals. If non pharmaceuticals are processed in the same facility and/or equipment with APIs, report precautions taken by the firm to prevent or minimize the potential for cross-contamination.8. A description of all API micronizing or milling operations, whether conducted in-house or by a contract micronizer. Fully describe the precautions taken by the firm to prevent or minimize the potential for cross-contamination. During inspections of contract micronizers,*Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE12 of 30obtain a complete list of all active pharmaceutical ingredients micronized and report the source (owners) of these materials.9.*A copy of the firm's process validation protocol. Report the status of all validation efforts. If not completed, obtain and submit the firm's written timetable showing when process validation will be completed.*10. A report of any adverse findings as required by the Investigations Operations Manual (IOM). SAMPLING1.*A profile sample of the active pharmaceutical ingredient should be collected for analysis by the Forensic Chemistry Center, FCC (HFR-MA500) and Northeast Regional Lab (NRL). These samples of the API should not be confused with profile samples of actives collected together with finished product samples under the Pre-Approval Inspections/Investigations Compliance Program, CP 7346.832.Depending upon the cost, the sample should consist of 25 - 50 grams of active drug substance from three different lots, collected in duplicate. Documentation that should accompany the sample must include:- A flowchart and brief narrative description of the API manufacturing process;- A material safety data sheet for the active pharmaceutical ingredient;- A Certificate of Analysis *(COA)* for each lot; *in addition, a description of the computer system that was utilized to generate the COA and the precautions taken by the firm to safeguard the integrity of the computer data against employee manipulation.*- A copy of any potential/established impurity profiles and applicable methodologies;-The analytical methodology (if the inspection involves a new chemical entity).**Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE13 of 302.*During foreign inspections, it is often difficult for the investigator to collect profile samples of APIs. If a sample is not collected, the investigator should identify the lot (s) to be sampled and instruct the manufacturer to collect and ship the sample and applicable records directly to the FCC. The FCC will prepare an annotated collection report and forward the duplicate portion and copy of records to the NRL. An information copy will also be sent to the lead investigator.*3.*When collecting samples for profile analysis, protect these from trace contamination. In all instances, avoid using metal spatulas. Use a plastic container and closure for sampling and submit an empty container as a control sub. If a plastic spatula is used, also submit an unused spatula as asub-sample. Identify each container with the sample number, the product name and lot number, manufacturer, date and initials of the sampler. Wear disposable, talc-free, polyethylene gloves during the sampling activity. The preferred sampling method is by direct transfer and replacing the gloves between each subsample. Multiple product lots may be submitted under one collection report.*4.To establish a labeling/container forensic data base, obtain the following information during inspections of foreign API firms. Identify this information with the firm's name, central file number (CF Number), and street address and send to *FDA/FCC, Bulk Drug Group, HFR-MA500, 1141 Central Pkwy., Cincinnati, Ohio 45202.*plete telephone and FAX number;b.Contact person with title;c.*Decoding of the *lot/batch numbering system;d.*List* of the actual quantities of each lot of API produced for the last three years. Explainany difference between the batch and lot number. The records should reflect the total quantity*produced* and the amount shipped to the U.S.e.Description *and/or* specimen of the container closure systems *(if easily obtained)* forAPIs intended for U.S. distribution, as domestic packaging is often different:*Current Changes*FORM FDA 2438g (Computer Generated, 05/98) PAGE14 of 30。
FOOD AND DRUG ADMINISTRATIONPROGRAM 7356.002A COMPLIANCE PROGRAM GUIDANCE MANUALCHAPTER 56 – DRUG QUALITY ASSURANCEFIELD REPORTING REQUIREMENTS:Establishment Inspection Reports (EIRs) are to be created and filed electronically using the specific module in TurboEIR or replacement system that is accessible to both ORA and CDER.For inspections of routine commercial manufacturing classified as Official Action Indicated (OAI) due to failure to comply with 21 CFR Part 210 and 211 Current Good Manufacturing Practice (CGMP) as they apply to sterile drug process inspections, submit advisory, administrative, or judicial action recommendations via MARCS-CMS in accordance with the Regulatory Procedures Manual (RPM). Districts should immediately report significant issues according to current FACTS, Panorama and CMS procedures. This includes promptly filing and changing OAI notifications.During an inspection, if you obtain information pertaining to inadequate adverse drug experience (ADE) reporting, unapproved drug issues, or post-approval reporting violations (application supplements, Field Alert Reports (FARs), etc.), report in accordance with directions provided in the applicable compliance programs and under separate captions in the EIR. Data system information about these inspectional activities should be reported under separate Program Assignment Codes (PACs). Expansion of coverage under these programs into a CGMP inspection should be reported under this compliance program.The Districts are requested to use this compliance program for all sterile drug process inspections. NOTE: Districts should assure that each operation performed by direction of this program circular is entered against the correct Product Code and Program/Assignment Code (P/AC).TABLE OF CONTENTSPART I BACKGROUND (4)PART II IMPLEMENTATION (5)2.1 Objective (5)2.2 Program Management Instructions (5)A. Strategy (5)B. Inspection Planning (6)C. Profile Reporting (6)PART III INSPECTIONAL (7)3.1 Types of Sterilization (7)A. Terminal sterilization (7)B. Aseptic processing (7)3.2 Reporting (8)3.3 Inspection Approaches (9)3.4 System Inspection Coverage (11)3.5 Quality System (11)3.6 Facilities and Equipment System (13)A. Facilities (13)B. Equipment (14)3.7 Materials System (19)3.8 Production System (21)3.9 Packaging and Labeling System (27)3.10 Laboratory Control System (27)3.11 Sampling (29)PART IV ANALYTICAL (30)PART V REGULATORY/ADMINISTRATIVE STRATEGY (31)PART VI REFERENCES, ATTACHMENTS AND PROGRAM CONTACTS (33)6.1 References (33)6.2 Attachments (34)6.2 Contacts (34)PART VII CENTER RESPONSIBILITIES (36)ATTACHMENT A .................................................................................................................A[end Cover Page]PART I - BACKGROUNDThis program covers the manufacture and testing of all sterile drug products, including drugs that are sterilized by filtration or other means and aseptically processed, and drug products that are terminally sterilized. The type of products covered by this program include sterile bulk drugs, ophthalmic drugs, otic dosage forms, small volume parenteral (SVS) products for small molecule and licensed biological therapeutic drug products, large volume parenteral (LVP) products, and any other drug products required to be sterile or labeled as sterile. Center for Biologics Evaluation and Research (CBER) regulated products and veterinary drug products are excluded from coverage under this program.The guidance information in this program is tailored to sterile manufacturing operations and should be used in conjunction with the Compliance Program for Drug Manufacturing Inspections (CP 7356.002).In 2004, Food and Drug Administration (FDA) published the Guidance for Industry Sterile Drug Products Produced by Aseptic Processing-- Current Good Manufacturing Practice, which is referred to throughout this Compliance Program as FDA’s “2004 Aseptic Processing Guidance.” The document represents FDA’s current thinking on Current Good Manufacturing Practices (CGMPs) for aseptically processed drugs.The Guidance for Industry does not establish mandatory requirements and should not be referred to as the justification for an inspectional observation. Justification for inspectional observations originates from the CGMP regulations, 21 CFR Parts 210 and 211.Manufacturers who follow the 2004 Aseptic Processing Guidance are generally considered compliant with CGMP regulations. However, alternate approaches may be used if such approaches satisfy the requirements of 21 CFR Parts 210 and 211.For technical questions and unusual circumstances encountered during an inspection, investigators are encouraged to contact their District, ORA Office of Medical Products and Tobacco Operations/Division of Medical Products and Tobacco Program Operations and/or CDER for consultation. For questions concerning microbiological analysis, sterility and related sampling concerns, contact ORA Office of Regulatory Science/Medical Products and Tobacco Scientific Staff.[end Part I]PART II - IMPLEMENTATION2.1 OBJECTIVESThe primary objective of this program is to provide guidance for conducting inspections of manufacturers of sterile bulk1 and sterile finished dosage drug products to determine compliance with the Food, Drug, and Cosmetic Act and the Current Good Manufacturing Practice Regulations (CGMPs), Title 21, CFR Parts 210 and 211.Other objectives include:•Obtain information on operations impacting on sterility, to identify areas for improvement and correction.•Evaluate current good manufacturing practices in the sterile drug industry.•Initiate appropriate action against manufacturers observed to be out of compliance.2.2 PROGRAM MANAGEMENT INSTRUCTIONSA. STRATEGY(1) Inspection of SystemsInspections of drug manufacturers should be made and reported using the system definitions and organization in this compliance program. Focusing on systems will increase inspection efficiency because the systems are often applicable to multiple profile classes. The selection of the system(s) for coverage will be made by the District Office based on the firm’s specific operation, previous coverage, compliance history, or other priorities determined by the District Office.The inspection should normally result in a determination of acceptability or non-acceptability for all profile classes. Coverage of a system should be sufficiently detailed, i.e., select an example of each profile class, so that the conclusion about the system’s state-of-control applies to all the profiles classes. However, the determination that a system is adequately controlled for one profile class can be extended to another profile class(es) even if that other profile class(es) was not specifically reviewed. The lead Investigator must consider the uniqueness of the various manufacturing situations at the plant and use their best judgment when selecting profile classes to review.Selecting specific areas unique functions within a system will be at the discretion of the lead Investigator.The options for system coverage are described in CPGM 56002. Any given inspection need not cover every system. See P art III - Inspectional.Complete inspection of one system may necessitate further follow up of some items within the activities of another system(s) to fully document the findings. Such follow up does not constitute full coverage of the other system (and cannot be reported as such in FACTS); nor does that follow up obligate the investigator to perform full coverage of the other system.1 “Sterile bulk” refers to sterile active pharmaceutical ingredients (APIs).(2) Inspectional ScopeInspections of sterile product drug manufacturers are performed as either Full Inspections or Abbreviated Inspections using the systems strategy outlined in Part II –Implementation, of Compliance Program 7356.002, Drug Manufacturing Inspections.See Part III – Inspectional, of this program for a complete discussion of the coverage requested under these inspection options.B. INSPECTION PLANNINGImplement this program when sterile drug manufacturers are inspected as part of a regular statutory inspection. CDER will identify firms for inspection based on the risk-based prioritization model on annual performance goals, as part of the initiative to ensure risk-based prioritization of inspection coverage.Consider using a team approach for conducting inspections when appropriate. Utilize investigators familiar with sterile drug manufacturing and aseptic processing and consider the participation of a microbiologist with expertise in microbial controls. Specifically,•All team members should be very familiar with FDA’s Guidance for Industry Sterile Drug Products Produced by Aseptic Processing – Current Good Manufacturing Practice (September2004).•Investigators or team members should be well qualified in sterile product manufacturing, and have completed formal training courses in parenteral drug manufacture, aseptic technique,sterilization methods, and related procedures and equipment. Microbiologists involved shouldhave experience in sterility, endotoxin testing, and evaluation of microbial controls inmanufacturing.C. PROFILE REPORTINGUpdate all applicable profile classes in the profile screen of the FACTS coversheet based on inspection findings. The following is a list of sterile product profile classes effective at the time this program was implemented. Use the codes corresponding to the product and process type covered.FULL DESCRIPTIONPROFILECLASSLVP Large Volume Parenterals are sterile injectable drugs packaged in containers labeled as containing more than 100 mL. Most are terminally sterilized, but some can be sterilized byfiltration and aseptically processed.SVT Small Volume Parenterals are sterile injectable drugs packaged in containers labeled as containing less than 100 mL that are terminally sterilized.SVS Small Volume Parenterals are sterilized by filtration and aseptically processed.SVL Small Volume Parenteral are sterilized by filtration, aseptically filled and lyophilized.SLQ Sterile liquid (other than suspensions and emulsions)SON Sterile ointmentSPW Sterile powderCSS Sterile bulk drugs that are made by chemical synthesis.CFS Sterile crude drugs made by fermentation.CRX API sterile or API intermediate/NEC inorganic/mineral[end Part II]PART III - INSPECTIONAL3.1 TYPES OF STERILIZATIONThere are two broad methods to produce a sterile drug product:•Terminal Sterilization•Aseptic Processing of sterilized unit componentsThere are basic differences between the production of sterile drug products using aseptic processing and production using terminal sterilization. Terminal sterilization should be utilized when the product and container/closure system are able to withstand the terminal sterilization process.A. TERMINAL STERILZATION - The terminal sterilization process usually involves filling and sealing product containers under high quality environmental conditions designed to minimize microbial and particulate contamination of the product. This minimization of upstream bioburden reduces the challenge to the subsequent sterilization process. In most cases, the product, container, and closure have low bioburden, but are not sterile at the time of filling. The product is then subjected to a sterilization process in its final container.There are various methods of terminal sterilization including:•Moist Heat Sterilization•Irradiation•Ethylene Oxide (typically for assembled components/kits)Types of sterilization cycles include:1. Overkill method:o Generally used for heat stable materials.o Designed to provide a significant level of sterility assurance regardless of the number and resistance of the actual bioburden organisms in the load.o Results in greater heat/exposure input to the product or items being sterilized.2. Bioburden Based cycle:o Requires studies to determine the number and resistance of the microorganisms found in the product and the bioburden load of the incoming components and containers/closures.o Cycle development to destroy the microbial load, but not degrade the product.o Routine bioburden monitoring of batches and ongoing knowledge of the heat/exposure resistance of organisms found in product bioburden, container/closure bioburden andenvironmental monitoring samples.Reference to terminal sterilization: PDA Technical Report No. 1 (Revised 2007) Validation of Moist Heat Sterilization Processes: Cycle Design, Development, Qualification and Ongoing Control.B. ASEPTIC PROCESSING - Aseptic processing presents a higher risk of microbial contamination of the product than terminal sterilization. In an aseptic filling process, the drug product, containers andclosures are sterilized separately and then brought together under an extremely high quality environmental condition designed to reduce the possibility of a non-sterile unit. Aseptic processing involves more variables than terminal sterilization. Any manual or mechanical manipulation of the sterilized drug, containers, or closures prior to or during aseptic filling and assembly poses the risk of microbial contamination.Some types of aseptic processing involve manual manipulations of sterile components, containers, and closures in addition to routine operator interventions in the critical area. Humans are a significant source of contamination in traditional aseptic processing, especially in production lines that require operators to routinely enter critical areas (Class 100, ISO 5, or Grade A) of the filling line. Aseptic processing systems based on more advanced control-based technologies, such as Restricted Access Barrier Systems (RABS) and Blow-Fill-Seal systems, are designed to reduce human interventions in the critical areas of the fill line while an isolator system completely separates the aseptic filling line from the external environment and minimizes employee interaction with the critical area.Note: More information about Isolator Technology and Blow-Fill-Seal systems is foundin FDA’s 2004 Aseptic Processing Guidance.When conducting inspections of sterile drug manufacturers, it is important to cover systems and areas within systems that present the greatest risk of product contamination and/or require strict control of processing parameters. For example, if a firm has several aseptic processing lines, cover the line(s) that require the most manual manipulations in the Class 100 (ISO 5) areas. If the firm terminally sterilizes a number of products, review one that is sensitive to heat and requires a product specific (bioburden based) sterilization cycle.Note: For terminal sterilized products that are aseptically filled prior to terminal sterilization, less rigorous aseptic controls can be considered.Because of the time limitations often associated with foreign inspections, careful inspection planning is particularly important. Prioritize areas for coverage based upon their potential impact on product quality.3.2 REPORTINGFollow instructions in the current editions of the IOM (Investigations Operations Manual) and Guide to International Inspection and Travel in preparing the inspection report.Use Turbo EIR for all reports, both domestic and international, even if a FDA-483 was not issued or was issued outside of Turbo EIR. The “Manufacturing / Design Operations” section of the report should be organized by the systems described in this program that were covered during the inspection. Briefly summarize your review of each covered system in accordance with the key elements outlined in this Compliance Program. Add more details and supporting evidence for the systems found to be deficient.3.3 INSPECTION APPROACHESIf the sterile drug products to be inspected are radioactive drugs, then Compliance Program 7356.002C, Radioactive Drugs, should be followed as supplementary guidance. This program should not be used for the inspection of Positron Emission Tomography (PET) Drug. Compliance Program 7356.002P is specific for PET drugs.This program (CP 7356.002A) should also be used in conjunction with Compliance Program7356.002M, Inspection of Licensed Biological Therapeutic Drug Products for the inspection of sterile licensed biological products.The CGMP Compliance Program 7356.002 provides general information on the system based approach to conducting inspections of drug manufacturers. It describes the six systems (Quality, Facilities and Equipment, Materials, Production, Packaging and Labeling, and Laboratory) and the two inspection options (Full Inspection and Abbreviated Inspection). It also provides guidance on when each option should be selected and discusses what “state of control” means in relation to the systems inspected. Inspections of sterile drug manufacturers are performed as either Full or Abbreviated inspections using the systems strategy outlined below.Full Inspections include surveillance or compliance inspections and provide a comprehensive evaluation of the firm’s compliance with CGMP. A Full Inspection will normally include an inspection of at least four systems, one of which must be the Quality System. Under this program, a Full Inspection should include the Facilities & Equipment, and Production Systems due to the critical role these systems play in the sterility assurance of finished product.Full Inspections (PAC 56002A) are conducted•when initial inspection of the drug firm is to be conducted;•when it is the first inspection conducted as a follow-up to a Warning Letter, regulatory action, or significant FDA 483 findings;•when information obtained during the Abbreviated Inspection reveals significant deficiencies with the firm’s practices and procedures in one or more system areas;•when there have been significant changes in the firm’s operations since the last inspection; or •for surveillance purposes at the District’s discretion because the firm has a history of recurring violations, fluctuating in and out of compliance, or when other information (samples,complaints, Field Alerts, recalls, etc.) calls into question the firm’s ability to produce qualityproducts.Abbreviated Inspections (PAC 56002I) may be appropriate if the following two conditions are satisfied:1. the firm has implemented a formal risk management program that assures effective design andcontrol (including maintenance). This includes a risk mitigating design of their processing lines that incorporates a modern separation and automation approach (e.g., isolators, closed RABS), and upstream bioburden controls. The responsiveness of the firm’s quality system to potentialhazards is also part of the evaluation, including whether the firm’s program provides robustdaily assurance and effective consumer protection through a formal lifecycle quality riskmanagement program that proactively uncovers and corrects issues in accord with ICH Q9.2. the firm has a record of sustained acceptable compliance history and a strong risk managementprogram.o the firm produces finished drug products that are terminally sterilized using robust sterilization methods. (Note: Terminal sterilization provides a much more robust process toensure sterility); or,o the firm has implemented robust risk management that provides daily assurance through their overall design and control program;o at the start of the inspection, conduct an extensive review of sterility assurance data since the last Full Inspection. The review of media fills, sterility testing data, recalls,defect/adverse event complaints, and reports reveals no findings of sterility failure of adistributed batch, ando the firm has a record of satisfactory CGMP compliance (e.g., two consecutive NAI or no more than one VAI inspection), with no Class 1 recalls.Microbial controls and sterility assurance should be the main focus of an abbreviated sterile drug inspection. The following critical elements of each system (other than the Quality System) should be covered in an Abbreviated Inspection under this program:•Facilities and Equipment:o cleaning and disinfectiono facility/equipment layout and air handling system for preventing viable and non-viable contaminationo material flowo quality control of classified areas, including air pressure balance and HEPA filtrationo trending data supporting the adequacy of clean room qualityo documented investigation into discrepancy•Materials:o microbial and bacterial endotoxin control of incoming materials and componentso quality of water supply, maintenance, qualificationo operation of the systems that provide the requisite water and process gaseso documented investigations into OOS, deviations, and discrepancies•Production:o observation of adequacy of operator behavior and aseptic techniques during manufacturing o production line operations and interventionso personnel training in aseptic techniqueso major production line repair or maintenance issueso risk assessment on microbial and bacterial endotoxin controls, including hold times of critical stepso validation of sterilization of equipment, container-closures and supplieso media fills design and resultso documented investigations into, deviations, discrepancies, and OOS results•Laboratory:o investigations into OOS, deviations, and discrepancieso test methods and controls, including adherence to validated methodso training and qualifications of laboratory personnelo trending of water system test resultso systems used for recovery, identification and trending of environmental monitoring isolates 3.4 SYSTEM INSPECTION COVERAGECompliance Program 7356.002, Drug Manufacturing Inspections, lists the areas that should be covered when inspecting each of the six systems. This program provides additional guidance, by system, for areas of specific concern for sterile drug products.Attachment A is a list of questions intended to be an aid in conducting inspections and obtaining information needed to assess a firm’s operations. The answers do not have to be reported in the EIR unless they are relevant. The list of questions covers: moist heat sterilization; dry heatsterilization/depyrogenation; aseptic filling; lyophilization; isolators; environmental monitoring; and biological indicators.3.5 QUALITY SYSTEMAs noted in Compliance Program 7356.002, the inspection of the quality system is two-phased. The first phase is to evaluate whether the Quality Unit has fulfilled their responsibility regarding the review and approval of procedures and assured their suitability for use. The second phase is to assess the data collected by the firm to identify potential quality problems. For sterile manufacturing operations, this latter objective involves large amounts of data that link to the other inspectional systems. The comprehensive review of such data by the firm is an essential element in assuring that products are produced with a high degree of sterility assurance. It is therefore important to review the firm’s system for using the data to assess the state of control of their manufacturing operations and facility. The data summaries and trend reports maintained by the Quality Unit should be reviewed during every inspection. During a routine CGMP inspection, this review can help determine which option (Full or Abbreviated) to select.The inspection of the Quality System should include the areas listed in CP7356.002. For this program, the inspection should include a review of all data and reports that may indicate product contamination and sterility assurance issues.Records pertaining to quality consist of the following:1. Periodic product evaluations, complaints, adverse events, investigations, Field Alert Reports,product retain evaluations, complaints, rejected lots, stability, and returned goods that indicatepossible product contamination or risks to patients (for example, hazy or cloudy product,foreign matter/particulates in injectable products, cracked, and leaky containers).2. Discrepancy and failure investigations, such as:o All initial positive sterility tests and endotoxin and media fill failures regardless of final disposition.o Unexpected results or trends.o All failures that occurred during validation or revalidation of sterilization / depyrogenation processes.o All investigations involving media fills / process simulations.o Environmental (microbial/viable and particle/non-viable counts) and personnel monitoring results that exceed alert or action levels.o Process deviations or equipment malfunctions that involve critical equipment, such as sterilizers and lyophilizers.o Out of Specification (OOS) results for assay, impurities, particulate matter, or reconstitution time, if applicable.o Product rejects (rejects determined during manufacturing and Quality Control test)3. Trends reports/ summaries of quality indicators:o For aseptic processing, summary of all media fills performed since last inspection.o Environmental monitoring trend data (microbial and particle counts).o Personnel monitoring trend data.o Summary of water system test results.4. Summary of change controls for critical utilities and equipment implemented since the lastinspection, for example:o Sterilizers, lyophilizers, depyrogenation equipmento Aseptic processing lineo Clean steam generator, process gas systemo WFI and / or Purified Water systemo Air handling systemso Automated building management systemEvery inspection of a sterile drug manufacturer should include a review of the type of information listed above and observation of the manufacturing operations occurring in the critical areas. The information can be used to select other system(s) to be covered during the inspection.In addition, the review of summary data and observation of operations can focus the inspection on potential problem areas and provides an overview of the effectiveness of the Quality System. The inspection of the Quality System may necessitate follow-up within another system. However, this coverage does not constitute or require complete coverage of these systems.3.6 FACILITIES AND EQUIPMENT SYSTEMCompliance Program 7356.002 lists the general areas to cover when inspecting the Facilities and Equipment System. The areas are applicable to sterile drug products and should be covered if this system is selected. The principle objective of an effective sterile drug manufacturing operation from a facility and equipment standpoint is to provide suitable protection of product. The inspectional evaluation of this objective is again two-part:•Review and evaluate the firm’s rationale for, and adequacy of, the facility and equipment design (Reference: Section IV of FDA’s 2004 Aseptic Processing Guidance).•Evaluate the data that provide information relevant to the state of control of the facility and equipment.In addition to the review of design elements and data, investigators should look for visible deficiencies in the facility and equipment, such as cleanliness, equipment deterioration (e.g., warping, corrosion), inaccessible and/or difficult to clean surfaces, and changes to critical equipment or systems that have not been qualified which may impact product quality. Investigator should look for aberrant events due to facility deterioration, a pattern of recurring and uncorrected maintenance issues, and increase or changes in production output that exceed the capacity of the facility and equipment.A. FACILITIESEvaluate the design and layout of the facility (e.g., personnel/material flow, cleanroom design). Specifications for clean room areas (layout, air filtration, appropriate air classification, pressure differentials between rooms and areas, temperature, and humidity) should be appropriate, and based on the risk of product contamination with particulate matter and microorganisms. Review the certification and qualification of the clean room areas to verify the areas meet design criteria and specifications. Certification and qualification typically includes data in support of the following: air flow pattern studies, HEPA (High Efficiency Particulate Air) filter integrity testing, air velocity measurement, non- viable particle, and verification of appropriate pressure differentials, temperature and humidity setpoints. Evaluate the airflow pattern (smoke studies) conducted under dynamic conditions to verify the unidirectional airflow and air turbulence within the critical area where sterilized drug product, containers, and closures are exposed to environmental conditions.•Reference: Section IV of FDA’s 2004 Aseptic Processing Guidance.•Routine monitoring and maintenance to assure air handling systems continue to operate within established parameters (microbiological monitoring is discussed under the Laboratory Control System).o Afford special attention to facilities that are performing construction in the clean areas, or at the vicinity of cleanroom. Because microbes (e.g., fungal spores) can be liberated from themovement of walls and other construction activities, determine if the facility is returned toacceptable environmental control through proper measures (environmental monitoring,media fills) before production can resume.o Verify that environmental monitoring of non-viable particle is occurring during operations including sites where there is the most risk to exposed product, container and closures.。