2012CA 癌症幸存者的营养与运动指南
- 格式:pdf
- 大小:544.56 KB
- 文档页数:33
癌症患者的营养护理建议营养在癌症患者的治疗中起着至关重要的作用。
良好的营养摄入可以帮助患者增加免疫力、减轻治疗的不良反应、促进康复和提高生活质量。
下面是一些癌症患者营养护理的建议,旨在辅助治疗过程和提高患者的整体健康状况。
1. 多样化膳食成分癌症患者的膳食应该包含多种多样的食物,以确保摄入足够的各类营养素。
建议增加新鲜水果、蔬菜、全谷物、低脂肪乳制品、富含健康脂肪的坚果和种子等食物的摄入。
这些食物富含抗氧化剂、维生素、矿物质和纤维,有助于保护细胞免受伤害,并提供身体所需的营养素。
2. 均衡摄入蛋白质蛋白质是癌症患者康复和身体修复的重要组成部分。
鱼类、瘦肉、禽类、豆类和蛋类都是优质蛋白质的良好来源。
在蛋白质的选择上,应该避免高脂肪和高胆固醇的食物,例如炸鸡、油炸食品和红肉。
优质蛋白质的摄入有助于支持免疫系统的功能、促进治疗过程中的伤口愈合,并提供能量进行身体修复。
3. 补充足够的水分在癌症治疗过程中,患者往往会经历恶心、呕吐、腹泻等消化问题,这些都可能导致脱水。
饮食中摄入足够的水分对于保持身体水平平衡非常重要。
此外,透明的汤、果汁等也可以作为摄入水分的补充。
患者应保持饮食中水分的摄入,并避免过多摄入咖啡因或含糖饮料。
4. 控制食物中的症状性问题癌症患者在接受治疗过程中可能会经历不同的症状,例如口腔溃疡、便秘和恶心等。
针对这些症状性问题,我们可以采取一些措施来保证患者能够进食:- 对于口腔溃疡,建议选择温软而易于咀嚼的食物,如煮熟的蔬菜、软糯米饭和果泥等。
- 对于便秘问题,建议增加膳食中的纤维摄入,并保持足够的水分摄入。
可以选择食用水果、蔬菜和全谷物食品来促进肠道蠕动。
- 对于恶心和呕吐,建议选择清淡、易于消化的食物,并避免大量进食的同时饮水。
控制这些症状性问题有助于患者维持正常的饮食,增加身体所需营养的摄入。
5. 谨慎选择补充剂在选择补充剂时,应咨询医生或专业营养师的意见。
虽然补充剂可以提供额外的营养,但过量摄入某些营养素可能会对治疗产生负面影响。
如何靠营养&运动防癌?1、每周摄入猪肉、牛肉、羊肉等红肉的量要少于500克,尽可能少吃加工的肉类制品(包括熏肉、咸肉、火腿等)这里的500 g指的是摄入的熟肉的重量,即500 g煮熟的红肉相当于700-750 g生肉。
证据显示,红肉,尤其是加工肉类,是结肠、直肠癌发病的危险因素。
但是,专家也强调,由于肉类是蛋白质、锌和维生素B12的重要来源,所以不建议选择全素食膳食。
如果摄入量适当,许多动物源性食物也是有营养和有益健康的。
对那些吃肉的人来说,可以通过选择吃家禽肉和鱼肉来限制红肉的摄入量。
最好只吃红肉中的瘦肉。
最好避免加工肉类,包括火腿、熏牛肉、意大利香肠。
一般来说它们的能量密度高,也可能含有大量的盐。
它们通常通过烟熏、腌制或添加化学防腐剂来保存。
对那些不吃肉类膳食的人,也可以从混合的豆类和谷物中摄取足量的蛋白质。
2、不推荐过度依赖维生素等膳食补充剂预防肿瘤,但在某些营养素缺乏病或膳食摄入不足时应适当补充证据表明,高剂量营养素补充剂可以预防癌症,也可能诱发癌症。
最佳的营养来源是食物和饮品,而不是营养补充剂。
为了预防癌症,应该选择包含不同食物的均衡饮食,营养丰富的天然食物含有很多对健康有益的物质如纤维素、维生素和矿物质,膳食中的营养素通常与那些“多种”补充剂中没有的营养素及其他生物活性物质共存。
然而,除了各种膳食外,膳食补充剂在有些时候对特定人群有好处。
例如维生素B12对那些难吸收天然维生素B12的50岁以上的人,叶酸对准备或已经怀孕的妇女,以及维生素D补充剂对不能暴露充足的阳光的人或不能从阳光中合成充足维生素D的人。
3、维持健康体重在人的一生中维持健康体重可能是预防癌症的重要方法之一,对许多其他慢性病来说也有预防作用。
专家建议防癌把体重维持在正常范围,即到21岁时使体重处于正常BMI的低值,21岁起维持体重在正常范围,在整个成年期避免体重增长和腰围增加。
正常体重范围的标准:通常确定亚洲人群BMI介于18.4~23.9为正常体重范围,BMI等于24或超过28为超重或肥胖。
癌症康复饮食指南科学膳食增强免疫力癌症康复饮食指南——科学膳食增强免疫力导言:癌症是当今世界最为常见的疾病之一,它给患者和其家人带来了巨大的身心负担。
除了现代医学的治疗手段外,合理的饮食也被广泛认为是促进康复的重要因素之一。
本文旨在为癌症患者和康复者提供科学的饮食指南,帮助其增强免疫力,促进康复过程。
一、营养摄入与癌症康复1.1 碳水化合物的合理搭配碳水化合物是人体主要的能量来源,对于癌症患者而言尤为重要。
适量的碳水化合物摄入可以提供充足的能量,帮助患者更好地应对治疗和康复过程。
在选择碳水化合物食物时,应主要选择全谷物和粗粮,如糙米、全麦面包等,避免过量食用精制面粉和高糖食品。
1.2 强化蛋白质摄入蛋白质是维持身体功能和结构的重要组成部分,对于癌症康复具有重要意义。
适量的蛋白质摄入可以帮助患者修复和代谢,增强免疫力。
推荐食用优质蛋白,如鱼类、豆类、禽类、牛奶等,同时避免过度油炸和高脂肪处理方式。
1.3 多种维生素和矿物质的摄入维生素和矿物质是人体正常生理功能所必需的,对于癌症康复具有重要作用。
推荐摄入各类新鲜蔬菜、水果和浅色蔬菜,以获得更多的天然维生素和矿物质。
此外,鉴于癌症患者吸收能力可能减弱,可以适量选择维生素和矿物质的补充剂。
二、增强免疫力的饮食策略2.1 富含抗氧化物的食物抗氧化物可以中和自由基,减轻氧化应激对机体的伤害,从而增强免疫功能。
建议增加食用富含抗氧化物的食物,如花椰菜、蓝莓、西兰花等,并正确储存和烹饪以保留其抗氧化性能。
2.2 摄入足够的纤维膳食纤维对于促进肠道健康以及增强免疫力具有重要作用。
适量摄入膳食纤维可以促进胃肠蠕动,增强免疫细胞的活性。
推荐食用全谷物、蔬菜、水果等富含纤维的食物,避免过度烹饪和加工,以保留其纤维含量。
2.3 补充足够的液体充足的水分摄入对于维持机体正常功能和代谢具有关键作用。
癌症患者更容易出现脱水现象,因此应注意补充足够的液体,包括水、汤类、果汁等,同时避免过度饮用刺激性饮料。
癌症病人的营养支持和饮食建议癌症是一种严重并常见的疾病,其治愈和恢复过程往往需要综合性的治疗措施。
除了传统的医学治疗,良好的营养支持和科学合理的饮食也极为重要。
本文将介绍癌症患者所需的营养支持和饮食建议。
第一部分:营养支持提供足够的能量和蛋白质对于癌症患者非常重要,它们对于促进身体恢复、增加抵抗力以及减缓肿瘤发展起到关键作用。
以下是一些建议:1. 确保摄入足够的能量:癌症会导致机体代谢水平升高,使得能量消耗增加。
因此,患者需要更多的能量来源来满足其基础代谢需要以及肿瘤生长消耗。
富含碳水化合物(如米、面粉、土豆等)和脂肪(如橄榄油、坚果等)的食物是增加能量摄入的好选择。
2. 提供足够的蛋白质:蛋白质是组织修复和免疫功能所必需的。
患者需要摄入足够的蛋白质来支持身体修复和肿瘤治疗所需。
富含蛋白质的食物包括鱼肉、禽肉、豆类、乳制品以及坚果。
3. 补充足够的水分:癌症治疗可能导致口干舌燥,容易出现脱水情况。
癌症患者需要保持良好的水分摄入量,这有助于维持体液平衡,排除代谢产物并减少恶心和呕吐的发生。
4. 补充营养素:癌症患者往往需要额外补充一些营养素,如维生素D、钙镁等。
这些营养素有助于增强机体抵抗力和促进康复。
建议咨询专业营养师了解具体的适用量。
第二部分:饮食建议除了提供全面的营养支持外,科学合理的饮食也对癌症患者的康复至关重要。
以下是一些饮食建议:1. 多吃富含抗氧化物的食物:抗氧化物有助于清除体内自由基,减少细胞损伤。
癌症患者可以增加食用富含抗氧化物的食物,如水果(蓝莓、草莓等)、蔬菜(菠菜、甘蓝等)以及坚果。
2. 减少红肉和加工肉摄入量:大量研究表明,高红肉和加工肉摄入与某些癌症(如结直肠癌)的发生风险增加相关。
建议患者减少红肉和加工肉(如香肠、午餐肉等)的摄入,转而选择禽类、鱼类或豆制品作为主要蛋白质来源。
3. 增加水果和蔬菜的摄入量:水果和蔬菜富含维生素、矿物质和纤维素等营养素,有助于提高免疫力并降低某些癌症的发生风险。
癌症幸存者的长期健康管理癌症,这个令人闻之色变的词汇,当它被战胜,患者成为幸存者之后,并不意味着一切就结束了。
长期的健康管理对于癌症幸存者来说至关重要,它是确保生活质量、预防复发、促进全面康复的关键。
癌症治疗往往是一场艰苦的战役,手术、放疗、化疗等治疗手段在消灭癌细胞的同时,也给身体带来了巨大的创伤。
治疗后的身体就像经历了一场暴风雨的洗礼,需要精心的呵护和修复。
这时候,长期健康管理就像是一把保护伞,为幸存者遮风挡雨。
饮食管理是长期健康管理中的重要一环。
癌症幸存者的饮食应该均衡、多样化,富含蛋白质、维生素、矿物质等营养成分。
多吃新鲜的蔬菜和水果,为身体提供丰富的抗氧化物质和膳食纤维。
优质蛋白质的来源如鱼、禽、蛋、瘦肉、豆类等,有助于修复受损的组织和细胞。
同时,要控制脂肪和糖分的摄入,避免食用过多加工食品和高热量饮料。
规律的饮食时间和适量的进食量也非常重要,避免暴饮暴食和过度节食。
运动对于癌症幸存者的康复同样不可或缺。
适当的运动可以增强体质,提高免疫力,改善心肺功能,减轻焦虑和抑郁情绪。
可以选择适合自己身体状况的运动方式,如散步、慢跑、瑜伽、太极拳等。
开始运动时要循序渐进,逐渐增加运动的强度和时间。
运动前最好咨询医生的建议,确保身体状况允许进行相应的运动。
心理健康也是不容忽视的方面。
癌症的经历往往会给幸存者带来心理创伤,恐惧、焦虑、抑郁等情绪可能会长期困扰着他们。
这时候,寻求专业的心理支持是非常必要的。
可以通过心理咨询、参加心理支持小组等方式,与他人分享自己的感受,获得情感上的支持和理解。
同时,家人和朋友的陪伴和关爱也能给予幸存者巨大的精神力量,让他们感受到温暖和希望。
定期复查是长期健康管理的重要环节。
通过定期的检查,可以及时发现癌症是否有复发的迹象,以及治疗带来的副作用是否得到了有效的控制。
复查的项目包括血液检查、影像学检查等,具体的复查时间和项目应根据癌症的类型、治疗方式以及个体的身体状况来确定。
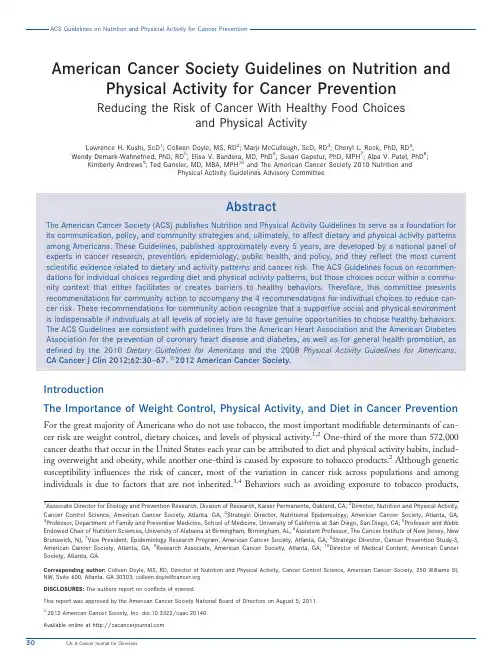
American Cancer Society Guidelines on Nutrition and Physical Activity for Cancer PreventionReducing the Risk of Cancer With Healthy Food Choicesand Physical ActivityLawrence H.Kushi,ScD1;Colleen Doyle,MS,RD2;Marji McCullough,ScD,RD3;Cheryl L.Rock,PhD,RD4;Wendy Demark-Wahnefried,PhD,RD5;Elisa V.Bandera,MD,PhD6;Susan Gapstur,PhD,MPH7;Alpa V.Patel,PhD8;Kimberly Andrews9;Ted Gansler,MD,MBA,MPH10and The American Cancer Society2010Nutrition andPhysical Activity Guidelines Advisory CommitteeAbstractThe American Cancer Society(ACS)publishes Nutrition and Physical Activity Guidelines to serve as a foundation for its communication,policy,and community strategies and,ultimately,to affect dietary and physical activity patterns among Americans.These Guidelines,published approximately every5years,are developed by a national panel of experts in cancer research,prevention,epidemiology,public health,and policy,and they reflect the most current scientific evidence related to dietary and activity patterns and cancer risk.The ACS Guidelines focus on recommen-dations for individual choices regarding diet and physical activity patterns,but those choices occur within a commu-nity context that either facilitates or creates barriers to healthy behaviors.Therefore,this committee presents recommendations for community action to accompany the4recommendations for individual choices to reduce can-cer risk.These recommendations for community action recognize that a supportive social and physical environment is indispensable if individuals at all levels of society are to have genuine opportunities to choose healthy behaviors.The ACS Guidelines are consistent with guidelines from the American Heart Association and the American Diabetes Association for the prevention of coronary heart disease and diabetes,as well as for general health promotion,as defined by the2010Dietary Guidelines for Americans and the2008Physical Activity Guidelines for Americans.CA Cancer J Clin2012;62:30–67.V C2012American Cancer Society.IntroductionThe Importance of Weight Control,Physical Activity,and Diet in Cancer Prevention For the great majority of Americans who do not use tobacco,the most important modifiable determinants of can-cer risk are weight control,dietary choices,and levels of physical activity.1,2One-third of the more than572,000 cancer deaths that occur in the United States each year can be attributed to diet and physical activity habits,includ-ing overweight and obesity,while another one-third is caused by exposure to tobacco products.2Although genetic susceptibility influences the risk of cancer,most of the variation in cancer risk across populations and among individuals is due to factors that are not inherited.3,4Behaviors such as avoiding exposure to tobacco products, 1Associate Director for Etiology and Prevention Research,Division of Research,Kaiser Permanente,Oakland,CA;2Director,Nutrition and Physical Activity, Cancer Control Science,American Cancer Society,Atlanta,GA;3Strategic Director,Nutritional Epidemiology,American Cancer Society,Atlanta,GA;4Professor,Department of Family and Preventive Medicine,School of Medicine,University of California at San Diego,San Diego,CA;5Professor and Webb Endowed Chair of Nutrition Sciences,University of Alabama at Birmingham,Birmingham,AL;6Assistant Professor,The Cancer Institute of New Jersey,New Brunswick,NJ;7Vice President,Epidemiology Research Program,American Cancer Society,Atlanta,GA;8Strategic Director,Cancer Prevention Study-3, American Cancer Society,Atlanta,GA;9Research Associate,American Cancer Society,Atlanta,GA;10Director of Medical Content,American Cancer Society,Atlanta,GA.Corresponding author:Colleen Doyle,MS,RD,Director of Nutrition and Physical Activity,Cancer Control Science,American Cancer Society,250Williams St, NW,Suite600,Atlanta,GA30303;colleen.doyle@DISCLOSURES:The authors report no conflicts of interest.This report was approved by the American Cancer Society National Board of Directors on August5,2011.V C2012American Cancer Society,Inc.doi:10.3322/caac.20140.Available online at 30CA:A Cancer Journal for Cliniciansmaintaining a healthy weight,staying physically active throughout life,and consuming a healthy diet can substantially reduce one’s lifetime risk of developing,5,6 or dying from,5,7cancer.2,8-11These same behaviors are also associated with a decreased risk of developing cardiovascular disease and diabetes.12Indeed,a recent study demonstrated that nonsmoking(former and never smokers)adult men and women whose lifestyles were most consistent with the2006American Cancer Society(ACS)cancer prevention guidelines for weight control,diet,physical activity,and alcohol had a significantly lower risk of dying from cancer,cardio-vascular disease,or all causes combined.7 Although these healthy choices are made by indi-viduals,they may be facilitated or impeded by the social,physical,economic,and regulatory environ-ment in which people munity efforts are therefore essential to create an environment that facilitates healthy food choices and physical activity. Overview of the GuidelinesThe ACS publishes Nutrition and Physical Activity Guidelines to advise health care professionals,policy-makers,and the general public about dietary and other lifestyle practices that reduce cancer risk.13 These Guidelines,updated in2012by the ACS Nutrition and Physical Activity Guidelines Advisory Committee,are based on synthesis of the current scientific evidence on diet and physical activity in relation to cancer risk.The Committee reviewed evi-dence from human population studies and laboratory experiments published since the last release of the Guidelines in2006.13The Committee also consid-ered other comprehensive reviews of diet,obesity, and physical inactivity in relation to cancer.For many aspects of nutrition and physical activity,the most thorough reviews were the2007World Cancer Research Fund/American Institute for Cancer Research(WCRF/AICR)report and the subsequent Continuous Update reports on breast cancer14and colorectal cancer15;other comprehensive reviews or meta-analyses that were published in recent years were also considered.16In weighing the evidence from randomized controlled trials(RCTs),the Committee considered thefindings in relation to the design of the trial,the specific question being addressed,and the importance of the trial results in the context of other evidence from human populations.Prospective cohort studies were weighted more heav-ily than case-control studies,especially when results were available from several cohorts.Population-based case-control studies with at least200cases of cancer were considered more informative than smaller or hospital-based case-control studies.Studies that adjusted for total energy intake,considered other dietary factors,and controlled for other known risk factors were considered more credible than those that failed to meet these criteria.For many issues concerning nutrition and cancer,the evidence is not definitive because the published results are inconsistent or because the methods of studying nutrition and chronic disease in human populations continue to evolve.Part of the uncer-tainty has resulted from studies that focus on specific nutrients or foods in isolation,thereby oversimplify-ing the complexity of foods and dietary patterns;the importance of the dose,timing,and duration of exposure;and the large variations in nutritional sta-tus among human populations.Nutrition and physi-cal activity research is equally challenging in RCTs, generally considered the gold standard for scientific inference.Studies may fail tofind an effect if the intervention begins too late in life,is too small,or ifthe follow-up is too short for a benefit to appear.In addition,RCTs of lifestyle interventions cannot be blinded,and disease endpoints such as cancer require many years of follow-up.No single trial can resolve allof the questions that are relevant to the potential effects of nutrition throughout the lifespan.Moreover, many important questions about how diet,physical activity,and obesity relate to cancer cannot presentlybe addressed in RCTs.For example,while there is substantial interest in the effects of early-life body size and dietary patterns on the risk of adult cancer,it is practically not feasible to conduct RCTs to determinethe long-term consequences of interventions that begin in infancy and extend for many years.Inferences about the many complex interrelation-ships between body weight,physical activity,diet, and cancer risk are therefore based,for the most part,on a combination of shorter-term clinical trials and observational studies coupled with advancing understanding of the biology of cancer.These Guidelines are based on the totality of evidence from these sources,taking into account both the potential health benefits and possible risks from adopting them.No diet or lifestyle pattern can guarantee fullVOLUME62_NUMBER1_JANUARY/FEBRUARY201231protection against any disease;the potential health benefit represents a decreased likelihood that the disease will occur,not a guarantee of total protec-tion.These Guidelines provide a summary of the existing scientific information about weight control, physical activity,and nutrition in relation to cancer and are intended to be followed as a whole.The ACS Guidelines are consistent with guidelines established for cancer prevention by other governmental and non-governmental organizations2,10;those from the American Heart Association17and the American Diabetes Association18for the prevention of coro-nary heart disease and diabetes;and those for general health promotion,as defined by the2010Dietary Guidelines for Americans19and the2008Physical Activity Guidelines for Americans.20In addition to recommendations regarding indi-vidual choices,the ACS Guidelines underscore what communities can and should do to facilitate healthy eating and physical activity behaviors(Table1).The recommendations for community action recognize that a supportive social and physical environment is indispensable if individuals at all levels of society are to have genuine opportunities to choose and main-tain healthy behaviors.ACS Guidelines for Nutrition and Physical ActivityRecommendations for Community Action Social,economic,and cultural factors strongly influ-ence individual choices about diet and physical activ-ity.21-24Although many Americans would like to adopt a healthy lifestyle,many encounter substantial barriers that make it difficult to follow diet and activity guidelines.21,22,24Indeed,according to the Institute of Medicine,‘‘It is unreasonable to expectTABLE1.American Cancer Society Guidelines on Nutrition and Physical Activity for Cancer PreventionACS RECOMMENDATIONS FOR INDIVIDUAL CHOICESAchieve and maintain a healthy weight throughout life.l Be as lean as possible throughout life without being underweight.l Avoid excess weight gain at all ages.For those who are currently overweight or obese,losing even a small amount of weight has health benefits andis a good place to start.l Engage in regular physical activity and limit consumption of high-calorie foods and beverages as key strategies for maintaining a healthy weight.Adopt a physically active lifestyle.l Adults should engage in at least150minutes of moderate intensity or75minutes of vigorous intensity activity each week,or an equivalent combination, preferably spread throughout the week.l Children and adolescents should engage in at least1hour of moderate or vigorous intensity activity each day,with vigorous intensity activity occurring at least3days each week.l Limit sedentary behavior such as sitting,lying down,watching television,or other forms of screen-based entertainment.l Doing some physical activity above usual activities,no matter what one’s level of activity,can have many health benefits.Consume a healthy diet,with an emphasis on plant foods.l Choose foods and beverages in amounts that help achieve and maintain a healthy weight.l Limit consumption of processed meat and red meat.l Eat at least2.5cups of vegetables and fruits each day.l Choose whole grains instead of refined grain products.If you drink alcoholic beverages,limit consumption.l Drink no more than1drink per day for women or2per day for men.ACS RECOMMENDATIONS FOR COMMUNITY ACTIONPublic,private,and community organizations should work collaboratively at national,state,and local levels to implement policy and environmentalchanges that:l Increase access to affordable,healthy foods in communities,worksites,and schools,and decrease access to and marketing of foods and beveragesof low nutritional value,particularly to youth.l Provide safe,enjoyable,and accessible environments for physical activity in schools and worksites,and for transportation and recreation in communities.ACS indicates American Cancer Society.32CA:A Cancer Journal for Cliniciansthat people will change their behavior easily when so many forces in the social,cultural,and physical envi-ronment conspire against such change.’’25Access to and affordability of healthy foods,the availability and extensive marketing of high-calorie foods and beverages of low nutritional value,and barriers to the ability of individuals to be physi-cally active for recreation and transportation in communities have all been implicated as contribu-tors to obesity trends in the United States.24,26 Avoiding unhealthy weight gain,therefore,goes beyond‘‘personal responsibility’’and an individual’s ability to achieve healthy diet and physical activity habits.Reversing obesity trends will require a broad range of multilevel strategies that include policy and environmental changes.These Guidelines therefore emphasize the impor-tance of public,private,and community organiza-tions working collaboratively at national,state,and local levels to implement policy and environmental changes that:Increase access to affordable,healthy foods in com-munities,worksites,and schools,and decrease access to and marketing of foods and beverages of low nutritional value,particularly to youth.Provide safe,enjoyable,and accessible environments for physical activity in schools and worksites,and for transportation and recreation in communities. Current trends toward increasing portion sizes27-29; the consumption of high-calorie convenience foods, sugar-sweetened beverages,and restaurant meals;and declining levels of physical activity are contributing to an obesity epidemic among Americans of all ages and across all population segments.30-32Longer workdays and more households with multiple wage earners reduce the amount of time available for the prepara-tion of meals,with a resulting shift toward the increased consumption of high-calorie foods outside the home,which are frequently less nutritious than foods prepared at home.33Large portion sizes, calorie-dense foods,and sugar-sweetened beverages are extensively marketed by restaurants,supermarkets, and food and beverage companies.29,32,34,35Reduced leisure time,increased amounts of time spent sitting, increased reliance on automobiles for transportation, and increased availability of electronic entertainment and communications media all contribute to reduced levels of physical activity.36-38There is increasing evi-dence of associations between the built environment and obesity and physical activity levels.36,39,40Poor access to sidewalks,parks,and recreation facilities is associated with greater obesity risk,41whereas neigh-borhoods that facilitate walking and safe physical recreation have lower obesity prevalence.21-24The increase in overweight and obesity noted among Americans is of particular concern for a num-ber of population groups,including children,whoare establishing lifelong behavioral patterns that affect health,and people who live in lower income neighborhoods,which are often characterized by nearby stores that lack affordable,high-quality healthy foods,and increased safety concerns that may limit opportunities for physical activity.Evidence suggests that obese children are more likely than normal-weight children to become obese adults,and that their obesity in adulthood is likely tobe more severe.42-44Promoting the establishment of healthy behaviors among youth is more effective, and often easier,than efforts to change unhealthy behaviors already established in adult populations. Therefore,creating environments that make it easierfor children to establish positive eating and physical activity habits early in life are critical.45Improvingthe school environment through policies that require daily,quality physical education and healthier food and beverage choices,and that limit the availabilityof and access to foods and beverages of low nutri-tional value;limiting advertising and marketing of less healthy foods and beverages;and ensuring com-munities have safe places to play,as well as routes that facilitate bicycling and walking to school,are important strategies to consider in addressing youth obesity trends.24,46While all Americans face obstacles to making healthy choices,the challenges are compounded for lower income and racial/ethnic minority groups,who frequently face additional barriers to making healthy food and physical activity choices.Access to super-markets has been associated with more healthful diets, greater consumption of vegetables and fruits,and lower rates of obesity,47,48and numerous studies have shown that communities with a greater proportion of ethnic minority and low-socioeconomic status resi-dents can be characterized as‘‘food deserts’’(ie,they tend to have fewer supermarkets that carry healthy, affordable,high-quality foods).49-51Limited access to supermarkets frequently results in residents shoppingfor food at local convenience stores,where healthyVOLUME62_NUMBER1_JANUARY/FEBRUARY201233food options tend to be fewer,of lesser quality,and more expensive.52Even in neighborhoods where supermarkets are available,low-income residents may more frequently purchase a diet of less expensive, higher-calorie foods;studies have suggested that lower cost foods comprise a greater proportion of the diet of lower income individuals.53Studies also sug-gest that these neighborhoods,as compared with more affluent areas,have greater access to fast food restaurants and other restaurants that are less likely to offer healthier options.50,54,55Research also points to disparities in the built environment,which likely contribute to differences in physical activity.Access to parks,gyms,and other opportunities for physical activity,such as the avail-ability of sidewalks and the close proximity of resi-dential areas to stores,jobs,schools,and recreation centers,have been shown to contribute to more physi-cally active lifestyles.56,57However,studies have found significantly fewer sports areas,parks,greenways, and bike paths in high-poverty areas when compared with areas with lower poverty rates.Even when these facilities are available,cost factors,distance from physical activity facilities,and transportation avail-ability may still affect access among low-income populations.58,59Heavy traffic,lack of street light-ing,unleashed dogs,high crime rates,and a lack of sidewalks and traffic calming measures are other factors that may present barriers to physical activity, particularly in low-income areas.Ensuring that all Americans have access to afford-able,healthy food choices and opportunities for safe physical activity will require multiple strategies and bold action,ranging from the implementation of community,worksite,school,and other health pro-motion programs to policies that affect community planning,transportation,school-based physical edu-cation,food advertising and marketing,and food services.Public,private,and community organiza-tions at local,state,and national levels will need to implement new policies and reallocate or expand resources to facilitate necessary changes.Health care professionals;school,business,faith group,and other community leaders;and policy makers all have opportunities to provide leadership and to promote purposeful changes in public policy and in commu-nity environments that are necessary to help individ-uals maintain a healthy body weight and remain physically active throughout life.Recommendations for Individual Choices Although the previously rapid increases in obesity prevalence appear to be leveling off in women and possibly in men,approximately two-thirds of Ameri-cans are overweight or obese.60The percentage of children,adolescents,and adult men who are over-weight or obese has continued to increase through 2004,although the trend has now stabilized in adult women and youth.60-62In addition,many Americans are less physically active than is optimal for health. Obesity increases the risk of many cancers,and also has adverse effects on coronary heart disease,stroke, type2diabetes,and other health outcomes,including premature mortality.Thus,while there continues to be scientific uncertainty about how specific aspects of excess adiposity,excessive energy intake,and physical inactivity relate to cancer,there is no debate that these contribute to an increased risk of many types of cancer and that they constitute a serious and growing health problem.These Guidelines therefore emphasize the importance of achieving or maintain-ing a healthy body weight;adopting a physically active lifestyle;consuming a healthy diet that emphasizes plant foods,particularly within the con-text of weight management;and limiting consump-tion of alcoholic beverages.1.Achieve and Maintain a Healthy Weight Throughout Life•Be as lean as possible throughout life without being underweight.•Avoid excess weight gain at all ages.For those who are currently overweight or obese,losing even a small amount of weight has health ben-efits and is a good place to start.•Engage in regular physical activity and limit consumption of high-calorie foods and beverages as key strategies for maintaining a healthy weight. Body Weight and Cancer RiskIn the United States,it has been estimated that over-weight and obesity contribute to14%to20%of all cancer-related mortality.63Overweight and obesity are clearly associated with an increased risk of devel-oping many cancers,including cancers of the breast in postmenopausal women,14colon and rectum,15 endometrium,kidney and adenocarcinoma of the esophagus,and pancreas2,64;are probably associated with an increased risk of cancer of the gallbladder2; and may also be associated with an increased risk34CA:A Cancer Journal for Cliniciansof cancer of the liver,non-Hodgkin lymphoma, multiple myeloma,cancer of the cervix,cancer of the ovary,and aggressive prostate cancer.63,65-70In addition,abdominal fatness is convincingly associ-ated with colorectal cancer,and probably related to a higher risk of pancreatic,endometrial,and post-menopausal breast cancer.2Overweight and obesity are thought to affect the risk of these cancers through a variety of mecha-nisms,some of which are specific to particular cancer types.These mechanisms include effects on immune function and inflammation;levels and metabolism of several hormones,including insulin and estradiol; factors that regulate cell proliferation and growth, such as insulin-like growth factor(IGF)-1;and pro-teins that make hormones more or less available to tissues,such as sex hormone-binding globulin and IGF-binding proteins.71-73Overweight and obesity may increase the risk of adenocarcinoma of the esophagus by increasing the risk of gastroesophageal reflux disease and Barrett esophagus.74,75Most research on energy imbalance and cancer focuses on increased risks associated with overweight and obesity.Some studies exploring intentional weight loss suggest that losing weight may reduce the risk of postmenopausal breast cancer76-78and possibly other cancers.79Results from large studies of lifestyle and behavioral weight loss interventions have shown that modest weight loss improves insulin sensitivity and biochemical measures of hormone metabolism, which have been postulated to contribute to the rela-tionship between obesity and certain cancers.79,80 Examples include the Diabetes Prevention Program Study81and the Action for Health in Diabetes (Look AHEAD)study,82,83both of which used life-style interventions to promote weight loss.Even though our knowledge about the relationship between weight loss and cancer risk is incomplete,individuals who are overweight or obese should be encouraged and supported in their efforts to reduce their weight. Achieving and Maintaining a Healthy WeightA healthy weight depends on a person’s height,so rec-ommendations for a healthy weight are often expressed in terms of a body mass index(BMI)(Table2). Although BMI is not a direct measure of adiposity, it is simple to measure and widely used clinically and in research studies.BMI is calculated as body weight in kilograms(kg)divided by height in meters,squared(m2).84Exact cutoffs for a healthy BMI are somewhat arbitrary,but for most adults,experts con-sider a BMI within the range of18.5to25.0kg/m2to be healthy,a BMI between25.0and29.9kg/m2tobe overweight,and a BMI of30.0kg/m2and overto be obese.The World Health Organization has modified this range,based on differential body com-position across various racial/ethnic groups.85For example,individuals with Asian ancestry are con-sidered to be overweight with a BMI greater than 23.0kg/m2.86Individuals should strive to maintain healthy weights as illustrated in Table2.The way to achieve a healthy body weight is to balance energy intake(food and beverage intake) with energy expenditure(physical activity).19,20 Excess body fat can be reduced by decreasing caloric intake and increasing physical activity.For most adults,a reduction of50to100calories per day may prevent gradual weight gain,whereas a reduction of 500calories or more per day is a common initial goalin weight loss programs.Similarly,300minutes or more of moderate to vigorous intensity physical activity per week may be needed to prevent weight gain or to sustain weight loss for previously over-weight people.19,20,30Caloric intake can be reducedby decreasing the size of food portions;limiting between-meal snacks;and limiting the intake of foods and beverages that are high in calories,fat, and/or added sugars,and that provide few nutrients (eg,many fried foods,cookies,cakes,candy,ice cream, and sugar-sweetened beverages).Such foods and bev-erages should be replaced with choices such as vegeta-bles and fruits,beans,whole grains,and lower calorie beverages.87Meals served in many fast food establish-ments and restaurants typically exceed the serving sizes needed to meet daily caloric needs and are often highin hidden fats and sugars.87They also are often low in vegetables,fruits,beans,and whole grains.33Keeping track of food intake and physical activity has been shown to be effective in weight management.87,88The health of young people,and the adults theywill become,is critically linked to the establishmentof healthy behaviors in childhood.50,89,90Risk factors such as excess weight gain,unhealthy dietary pat-terns,and physical inactivity during childhood and adolescence can result in an increased risk of developing cancer,cardiovascular disease and stroke, diabetes,hypertension,and osteoporosis later in life.91 Children who adopt healthy lifestyle habits at an earlyVOLUME62_NUMBER1_JANUARY/FEBRUARY201235age are more likely to continue these behaviors throughout life.Research suggests that the majority of children and adolescents who are overweight will remain overweight in adulthood.92,93For these rea-sons,efforts to establish healthy weight and patterns of weight gain should begin in childhood,but are no less important in adulthood and throughout life.2.Adopt a Physically Active Lifestyle •Adults should engage in at least150minutes of moderate intensity or75minutes of vigorous intensity activity each week,or an equivalent com-bination,preferably spread throughout the week.•Children and adolescents should engage in at least1hour of moderate or vigorous intensity activity each day,with vigorous intensity activ-ity occurring at least3days each week.•Limit sedentary behavior such as sitting,lying down,watching television,or other forms of screen-based entertainment.•Doing some physical activity above usual activ-ities,no matter what one’s level of activity,can have many health benefits.Benefits of Physical ActivityPhysical activity may reduce the risk of several types of cancer,including cancers of the breast,colon,and endo-metrium,as well as advanced prostate cancer,and possi-bly,pancreatic cancer.2,69,94,95Although evidence for many other cancers is limited,associations may exist. Physical activity acts in a variety of ways to affect cancer risk.96Regular physical activity helps maintain a healthy body weight by balancing caloric intake with energy expenditure,and may help to prevent certain cancers via both direct and indirect effects,including regulating sex hormones,insulin,and prostaglandins,and having various beneficial effects on the immune system.97,98 A physically active lifestyle is also associated with a reduced risk of other chronic diseases,such as heart disease,diabetes,osteoporosis,and hypertension.20TABLE2.Adult BMI ChartBMI1920212223242526272829303132333435 HEIGHT WEIGHT IN POUNDS4010009196100105110115119124129134138143148153158162167 4011009499104109114119124128133138143148153158163168173 5097102107112118123128133138143148153158163168174179 50100100106111116122127132137143148153158164169174180185 50200104109115120126131136142147153158164169175180186191 50300107113118124130135141146152158163169175180186191197 50400110116122128134140145151157163169174180186192197204 50500114120126132138144150156162168174180186192198204210 50600118124130136142148155161167173179186192198204210216 50700121127134140146153159166172178185191198204211217223 50800125131138144151158164171177184190197203210216223230 50900128135142149155162169176182189196203209216223230236 501000132139146153160167174181188195202209216222229236243 501100136143150157165172179186193200208215222229236243250 60140147154162169177184191199206213221228235242250258 60100144151159166174182189197204212219227235242250257265 600200148155163171179186194202210218225233241249256284272 60300152160168176184192200208216224232240248256264272279 HEALTHY WEIGHT OVERWEIGHT OBESE BMI indicates body mass index.Source:US Department of Health and Human Services,National Institutes of Health,National Health,Lung,and Blood Institute.The Clinical Guidelines on the Identification,Evaluation and Treatment of Overweight and Obesity in Adults:Evidence Report.N1H Pub.No.98-4083.Bethesda,MD:US Department of Health and Human Services,National Institutes of Health,National Health,Lung,and Blood Institute;1998.36CA:A Cancer Journal for Clinicians。
癌症患者的日常饮食指南癌症是一种严重的疾病,对患者的身体和精神状态都带来很大的影响。
饮食在癌症患者的康复和治疗中起着至关重要的作用。
本文将为癌症患者提供一份日常饮食指南,帮助他们合理调配食物,提高抵抗力,促进康复。
一、食物选择1. 增加蔬菜和水果的摄入:蔬菜和水果富含维生素、矿物质和抗氧化剂,对于癌症患者的康复非常重要。
建议每天摄入至少5种不同颜色的蔬菜和水果,如红色(西红柿、红椒)、橙色(胡萝卜、南瓜)、黄色(柠檬、香蕉)、绿色(菠菜、西兰花)和紫色(葡萄、紫甘蓝)。
2. 选择高纤维食物:高纤维食物有助于促进消化系统的正常功能,降低患者便秘的风险。
常见的高纤维食物包括全麦面包、糙米、燕麦、豆类、坚果和种子等。
3. 适量摄入蛋白质:蛋白质对于癌症患者的康复至关重要,可以帮助修复组织和细胞。
建议选择瘦肉、鱼、家禽、乳制品和豆类等富含蛋白质的食物,并合理控制摄入量,避免过量摄入对肾脏造成负担。
4. 避免加工食品和高糖食物:加工食品和高糖食物含有较多的添加剂和糖分,对癌症患者的康复不利。
因此,应避免食用过多的糖果、甜点、碳酸饮料等。
二、饮食技巧1. 分食多餐:癌症患者可能因为治疗过程中的不适感而食欲不振,此时可以采用分食多餐的方式来增加进食量。
每天五至六餐,分量适中,避免过饱。
2. 食用易消化的食物:癌症患者体力消耗较大,消化功能可能有所减弱,因此食用易消化的食物能更好地被吸收。
例如,煮熟的蔬菜、软煮的鸡蛋、烤鳕鱼等都是不错的选择。
3. 多饮水:癌症患者在进行放疗或化疗时身体可能处于脱水状态,因此要确保充足的水分摄入。
建议每天喝6至8杯水,可以适量饮用鲜榨果汁、汤类等补充营养。
4. 避免辛辣刺激:辛辣食物可能会导致胃肠道不适,癌症患者需要避免摄入过多的辣椒、葱、姜、蒜等调料。
三、注意事项1. 个体差异:每个癌症患者的病情和身体状况不同,饮食需求也会有所不同。
因此,在制定饮食计划之前,最好咨询专业医生或营养师的建议。
癌症患者的营养支持与饮食建议引言:癌症是当今世界上最常见的致死性疾病之一,而合理的饮食对于癌症患者来说尤为重要。
科学的饮食可以帮助患者提高免疫力、减轻治疗的副作用、促进康复。
本文将介绍癌症患者所需的营养支持和饮食建议。
一、补充足够的蛋白质蛋白质是人体生长、修复组织以及产生免疫抗体所必需的重要营养素。
在罹患癌症时,身体会消耗大量蛋白质,因此摄取足够的蛋白质非常重要。
但是,并不是所有类型的蛋白质对于癌症患者都适用。
应该选择易消化又富含氨基酸和必需脂肪酸的高质量蛋白质来源,如禽肉、鱼类、豆类和坚果。
二、增加碳水化合物摄入癌症患者的机体会出现异常代谢和能量消耗增加,因此需要摄取足够的碳水化合物来提供能量。
建议选择复杂碳水化合物,如全麦面包、糙米、蔬菜和水果等,而不是简单碳水化合物(如糖和白面包),以减少血糖波动。
三、多摄入富含纤维的食物富含纤维的食物可以促进肠道蠕动、预防便秘,并帮助清除废物及毒素。
同时,它们还有助于降低胆固醇和控制体重。
建议癌症患者摄入充足的蔬菜、水果、全谷类以及豆类等富含纤维的食品。
四、迅速补充流失的液体癌症患者往往由于治疗副作用或恶心而导致食欲不振或呕吐。
这样会使身体缺乏水分并容易出现脱水问题。
因此,患者应该每天喝足够的液体来保持身体正常运作。
最好选择无咖啡因的饮品、纯净水或混合蔬果汁,以满足身体对液体的需求。
五、注意补充维生素和矿物质由于癌症治疗可能导致维生素和矿物质的丧失,患者需要特别关注这些营养素的摄入。
维生素C、维生素E、维生素D和锌等有抗氧化作用,可以增强免疫力。
此外,钙和镁也是非常重要的矿物质,有助于骨骼健康。
可以通过饮食多样化来摄取各种维生素和矿物质,如食用新鲜水果、蔬菜、全谷类、奶制品以及适量坚果。
六、避免过度油腻的食物在癌症治疗期间,消化系统可能会受到影响,患者应尽量避免过度油腻或高脂肪的食物,因为这些食物会增加胃肠道反应。
建议选择低脂肪和低胆固醇的食物,并采用健康的加工方法(如蒸、煮或烤),而不是油炸。
美国癌症协会指南:营养和运动对癌症的预防选择健康食品和运动减少癌症风险翻译:舒琳摘要美国癌症协会(ACS)出版了营养和运动指南,将其作为交流、制定政策、社区活动的一个依据,最终影响美国人的饮食和运动模式。
这些指南大约每5年发表一次,是由一个在癌症研究、预防、流行病学、公共卫生和政策的国家专家小组发展起来的,并且反映了饮食和运动模式与癌症风险关系的最新的科学证据。
美国癌症协会指南重点推荐了关于饮食和运动模式的个人选择,但是这些选择发生在群体环境,既不促进健康行为方式也不对其进行阻碍。
因此,该协会提出了对于社区活动的建议和4条个人选择的建议来减少癌症风险。
这些对社区活动的建议显示,如果社会各阶层的人们有真正的机会来选择健康的行为方式,一个支持的社会和物质环境是必不可少的。
美国癌症协会指南与美国心脏协会和美国糖尿病协会关于预防冠心病和糖尿病是一致的,还有由2010年美国膳食指南和2008年美国居民健身指南对促进健康的定义。
前言控制体重、运动和饮食对癌症预防的重要性对绝大多数不吸烟的美国人来说,癌症风险最重要的可变决定因素就是控制体重、饮食的选择和身体活动水平1,2。
每年发生在美国的癌症死亡的三分之一超过572000例可以归因于饮食和身体活动习惯,包括超重和肥胖,而另外三分之一是由于接触烟草产品2。
虽然遗传易感性会影响患癌症的风险,在种群和个人中癌症风险大部分的变异并不是取决于遗传因素3,4。
一些行为例如避免接触烟草产品、保持标准体重、坚持运动、健康饮食,可以大大减少人一生患癌症5,6或死于5,7癌症2,8-11的风险,这些相同的行为也同样能够降低发展成心血管疾病和糖尿病的风险12。
事实上,一项最新的研究显示,那些不吸烟(以前吸烟或从不吸烟)的成年男性或女性,他们的生活方式,与2006年美国癌症协会癌症预防指南中提出的关于体重控制、饮食、运动和酒精摄入相一致,能够显著降低死于癌症、心血管疾病或各种原因组合的风险7。
阴茎癌的饮食锻炼技巧增强身体抵抗力的锻炼方法阴茎癌是男性生殖系统中罕见但致命的一种恶性肿瘤。
除了接受规范的治疗措施外,饮食和锻炼也是预防和帮助恢复的重要因素。
本文将探讨饮食锻炼技巧,帮助增强身体抵抗力。
一、保持均衡的饮食1. 增加蔬菜和水果摄入量蔬菜和水果是富含维生素、矿物质和抗氧化剂的良好来源。
其中的维生素C和维生素E被认为对预防癌症具有一定的保护作用。
建议每日摄入五种不同颜色的蔬菜和水果,如番茄、胡萝卜、菠菜、蓝莓和柿子等。
2. 控制红肉摄入量红肉摄入过多与多种癌症的发生风险增加相关。
建议将红肉的摄入控制在适量范围内,并选择瘦肉或鱼类作为蛋白质的替代来源。
3. 增加纤维素摄入高纤维食物有助于维持胃肠道健康,并且可能降低患上某些癌症的风险。
全麦面包、燕麦片、豆类、水果和蔬菜都是良好的纤维素来源。
建议每日至少摄入25克纤维素。
4. 适量摄入膳食脂肪膳食脂肪是身体所需,但过多的脂肪摄入可能增加患上癌症的风险。
建议选择健康的脂肪来源,如橄榄油、鱼油、坚果和种子等,并限制食用高脂肪和高热量的食品。
二、选择合适的锻炼方法1. 有氧运动有氧运动如快走、慢跑、游泳等可以增强心肺功能,改善全身的氧气供应。
这些运动不仅有助于维持健康体重,还可以促进血液循环,提高免疫力。
建议每周进行至少150分钟的有氧运动。
2. 肌力训练肌力训练包括举重、俯卧撑、仰卧起坐等,可以增强肌肉力量和耐力。
通过肌力训练可以提高身体的抵抗力,减少发病风险。
建议每周进行两到三次的肌力训练,每次包括全身主要肌群的练习。
3. 柔韧性锻炼柔韧性锻炼如瑜伽、拉伸等可以改善身体的灵活性和平衡能力。
这些锻炼有助于减轻压力、促进睡眠,并提高免疫系统的功能。
建议每周进行三到五次的柔韧性锻炼,每次持续15到30分钟。
4. 放松和休息适当的放松和休息对身体具有重要作用。
压力和焦虑会削弱免疫系统,增加罹患癌症的风险。
建议学习一些放松技巧,如深呼吸、冥想、按摩等,以帮助恢复身心的平衡。
2012 年ACS《癌症预防的营养与运动指南》解读浙江大学医学院附属邵逸夫医院肿瘤内科陈薇潘宏铭最近,美国癌症协会(ACS)下属的营养与运动指导委员会发布了2012 年版《癌症预防的营养与运动指南》。
这是继2006 年版后,美国肿瘤学、预防与流行病学及公共卫生学专家通过再次系统回顾相关循证学证据,面向美国社区及广大民众推出的最新癌症防控建议。
证据显示,在美国每年57 万余癌症死亡病例中,有近1/3 病例与饮食及运动习惯相关,另1/3 则死于烟草制品暴露。
由于人口、环境、饮食习惯及地域文化背景等诸多差异,指南中部分内容并不完全适用于我国。
但研究已证实,不论是在欧美等发达地区,还是在亚非等欠发达地区,恶性肿瘤高发均与某一种或一些不良的生活方式相关。
因此,ACS 2012 年版《癌症预防的营养与运动指南》在我国亦有重要现实意义,本文将结合我国实际情况,对该指南重点部分进行解读,希望能对我国肿瘤学临床医生有所裨益。
饮食、运动:多种恶性肿瘤的明确危险因素乳腺癌乳腺癌的发病率在我国正逐年攀升。
已知的非饮食相关危险因素:绝经后激素替代疗法、青年时期接受电离辐射、月经初潮早于12岁、绝经时间推迟、30 岁以后生育第一胎以及明确的家族史等。
目前认为,绝经后体重增加及饮酒也与乳腺癌发病率升高有关,如以蔬菜、水果、禽肉及鱼为主的食谱或可降低罹患乳腺癌风险。
专家建议,最佳预防方法是坚持日常运动、终生控制体重在合理水平及不饮酒或限制饮酒。
肺癌肺癌是全世界致死率最高的恶性肿瘤,超过85% 的肺癌由吸烟引起。
不仅如此,吸烟还与许多不良生活习惯相关联,如缺少运动、不健康的饮食模式等,这些肺癌风险相关因素很难分开。
在美国,得益于近20 年来的禁烟措施,肺癌发生率已有所下降;但在我国,烟民比率仍旧居高不下。
因此,戒烟是预防肺癌的重中之重。
此外,研究还发现多摄入水果有助于降低肺癌发生率。
胃癌虽然在美国胃癌发病率较低,但其仍是仅次于肺癌的全世界第二高致死率的恶性肿瘤。
癌症病人的营养支持与膳食建议随着现代医学和治疗技术的发展,癌症的治疗效果有了很大的提升。
然而,治疗并不仅仅依赖于放化疗等方法,患者的营养状态也起着至关重要的作用。
合理的营养支持和膳食建议能够增强患者体力、提高免疫力,并降低治疗带来的副作用。
本文将介绍癌症患者营养支持所需的各种营养素以及适宜的饮食建议。
一、蛋白质蛋白质是组成身体组织和维持身体正常功能必不可少的营养素。
对于癌症患者来说,蛋白质尤为重要,因为肿瘤可以消耗大量蛋白质。
1. 摄入足够量的优质蛋白质:优质蛋白质主要来自于鱼、禽肉、乳制品、大豆等食物。
保证摄入足够量的蛋白质,有利于患者维持肌肉质量和增加免疫力。
2. 分散进餐:建议将一天所需的蛋白质分成几个小份进食,如3-5餐。
这样可以提高蛋白质吸收率,并减轻消化系统的压力。
二、碳水化合物癌症患者通常会经历恶心、呕吐等副作用,这些都可能导致摄入能量不足。
碳水化合物是获得能量的重要来源。
1. 选择低糖指数食物:低糖指数食物能够更稳定地提供能量,避免血糖波动过大。
建议选择全谷类食物(如全麦面包)、淀粉类食品(如土豆、红薯)作为主要的碳水化合物来源。
2. 多次少量进食:如果患者很难在一顿餐中摄入足够的碳水化合物,可以尝试多次少量进食。
例如,每隔两小时就摄入一些容易消化的碳水化合物食物(如水果)来补充能量。
三、脂肪脂肪是提供能量和维持正常机体功能所必需的。
然而,选择合适的脂肪类型对于癌症患者尤为重要。
1. 选择健康脂肪:建议避免摄入过多饱和脂肪酸(如动物脂肪)以及反式脂肪酸(如快餐食品中的人造黄油)。
相反,应该选择富含不饱和脂肪酸的食物,如橄榄油、花生油、坚果等。
2. 控制摄入量:尽管脂肪是必需的,但是对于已经超重或有代谢性疾病(如高血压、糖尿病)的患者来说,需要控制总摄入量。
咨询专业营养师以确定适宜的摄入量。
四、维生素和矿物质维生素和矿物质在维持身体正常功能方面起着至关重要的作用。
然而,由于治疗过程中可能出现食欲不振等问题,患者往往无法从普通食物中获取足够的维生素和矿物质。
癌症患者的营养补充护理指南营养对于癌症患者来说是至关重要的。
癌症患者的身体常常处于消耗状态,免疫系统受损,需要额外的营养支持来维持机体的功能。
因此,制定一个科学合理的营养补充护理指南对于帮助癌症患者保持良好的营养状态至关重要。
本文将介绍一些适用于癌症患者的营养补充护理指南,以及注意事项。
一、主食选择癌症患者在选择主食时,应以高纤维、易消化、低脂肪、高蛋白的食物为主。
例如,可以选择全麦面包、糙米、粗粮等富含纤维的主食。
同时,患者还应合理控制碳水化合物的摄入量,以防止肥胖和血糖波动。
二、蛋白质摄入蛋白质是身体修复和恢复的重要营养素之一。
癌症患者的身体往往处于恶性代谢状态,蛋白质的需求量也相应增加。
可以通过摄入鸡肉、瘦肉、鱼类、低脂奶制品、豆类等富含蛋白质的食物来满足需求。
三、蔬菜水果摄入蔬菜水果富含多种维生素和矿物质,能够提供充足的抗氧化物质和纤维。
患者应该多样化摄入不同颜色的蔬菜水果,以确保获得全面丰富的营养物质。
此外,患者可以选择一些富含维生素C的水果,如柑橘类水果,以增强免疫力。
四、脂肪摄入适量的脂肪摄入对于癌症患者是必要的,但需要注意选择健康脂肪。
例如,可以选择植物油、坚果、鱼油等富含不饱和脂肪酸的食物。
同时,患者应避免高脂肪、高热量的食物,以免增加肥胖风险。
五、小餐多餐癌症患者常常因为治疗原因导致食欲不振,进食困难。
此时,可以通过多吃少量的方式来增加营养摄入。
患者可以将一天的食物分为多次进食,保证充足的营养吸收并减轻饱腹感。
六、饮食卫生癌症患者的免疫系统通常较弱,容易感染。
因此,在饮食过程中要保持饮食器具的清洁卫生,避免食物被污染。
同时,患者应避免生吃刺激性食物,并注意饮食安全和食物卫生。
七、补充营养剂如果患者因为治疗或食欲不振等原因无法满足身体所需的营养摄入,可以考虑适量的营养补充剂。
但应在医生指导下使用,并遵循剂量指导。
总结起来,癌症患者的营养补充护理是一个相对复杂的过程。
在制定指南时,应根据患者的实际情况进行个体化的营养安排。
癌症患者的营养支持和膳食安排癌症是一种罕见的疾病,它通常与人体免疫系统的失调有关。
据世界卫生组织的统计数据,2018年有超过90万人因癌症死亡。
良好的营养摄入对于癌症患者来说极为重要,因为营养失调会削弱免疫系统,从而加重病情,甚至影响治疗的效果。
本篇文章将详细介绍癌症患者的营养支持和膳食安排。
1. 营养支持癌症患者需要良好的营养支持,以维持免疫系统的功能和身体健康的状况。
由于癌症本身会导致身体的代谢水平增加,因此患者的能量需求也会增加。
以下是癌症患者需要注意的营养素:1.1 蛋白质癌症患者需要大量的蛋白质来维持身体的能量需求和修复受损的组织。
建议食用富含蛋白质的食物,如肉类、鱼类、家禽等。
患者还可以通过口服高蛋白质营养补充剂来获取足够的蛋白质。
1.2 脂肪脂肪虽然是令人担忧的营养素,但它在癌症患者的健康中也起着重要的作用。
脂肪可以提供重要的能量来源,并保护身体脏器不受损伤。
患者应该避免饮食中的饱和脂肪酸,而是选择富含单不饱和脂肪酸的食物,如橄榄油、坚果和鱼类。
1.3 碳水化合物碳水化合物是人体的主要能量来源,因此患者需要保证足够的碳水化合物供给。
建议食用淀粉类食品,如米、面、土豆和豆类。
此外,患者也需要避免高糖分的食物,如糖果、饮料等。
1.4 维生素和矿物质癌症患者需要大量的维生素和矿物质,以保证身体免疫系统的正常运转。
建议食用富含维生素和矿物质的食物,如新鲜水果、蔬菜、瘦肉、鱼和豆类等。
2. 膳食安排在癌症患者的膳食安排中,需要满足以下要求:2.1 避免高温烹饪在烹饪过程中,高温可能会导致蛋白质和维生素的分解,从而降低食物的营养价值。
患者应避免高温烹饪,如煎炸等,而是选择低温烹饪,如蒸、煮、炖等。
2.2 均衡饮食患者需要摄取足够的营养素,以保持身体健康和缓解病情。
每天应摄取适量的蛋白质、碳水化合物、脂肪、维生素和矿物质。
建议将每天的饮食分为三餐和三个小的零食,以保证营养的均衡摄取。
2.3 避免口腔疼痛癌症患者常常会经历口腔疼痛、口干和味觉改变等症状,这些症状会影响他们的饮食。
肿瘤科病人营养支持指南营养在肿瘤科病人的治疗过程中起着重要的作用。
合理的营养支持可以帮助提高病人的生活质量,增强免疫力,并为治疗提供必要的能量和营养物质。
本文旨在为肿瘤科病人提供全面的营养支持指南,以助其更好地应对治疗过程中的营养需求。
一、肿瘤科病人的营养需求肿瘤科病人的能量消耗通常较高,其基础代谢率可能增加。
此外,肿瘤本身、手术创伤、化疗和放疗等治疗手段都会对营养摄取和吸收造成一定影响。
因此,病人的营养需求也较为特殊。
1. 蛋白质摄取蛋白质是肿瘤科病人营养支持中的重要组成部分。
足够的蛋白质摄取可以维持或修复组织,促进伤口愈合,增强免疫力。
建议肿瘤科病人每天摄取1.0-1.5克/公斤的蛋白质。
瘦肉、鱼类、豆类及奶制品都是良好的蛋白质来源。
2. 脂肪摄取脂肪是提供人体能量的重要来源。
肿瘤科病人的脂肪摄取应适量,过多的脂肪可能导致体重增加和消化不良。
选择健康的脂肪源,如橄榄油、亚麻籽油等,并减少摄入含高饱和脂肪的食物,如猪肉、黄油等。
3. 碳水化合物摄取碳水化合物是人体主要的能量来源,特别是来自全谷物的碳水化合物,含有丰富的维生素、矿物质和膳食纤维。
建议肿瘤科病人选择全谷物米饭、面粉和面包等作为主要的碳水化合物摄取来源。
二、肿瘤科病人的饮食原则除了合理的营养摄取,肿瘤科病人在日常饮食中,还需遵循一些饮食原则以保障其营养摄入的效果。
1. 多样化的饮食均衡多样化的饮食可以提供丰富的营养物质,包括维生素、矿物质和膳食纤维。
建议肿瘤科病人在食用主食、蔬菜、水果、蛋白质和脂肪时保持多样性,避免偏食。
2. 适度控制食量合理控制饮食量可避免过度的能量摄取,预防肥胖及其带来的不良影响。
建议肿瘤科病人根据个人情况选择适当的饮食量,并注意饮食频次与强度。
3. 注意饮食安全在治疗过程中,肿瘤科病人的免疫力可能下降,因此需要格外注意饮食安全性。
避免生食、剩菜剩饭,选择新鲜食材,保证食物的煮熟和储存过程的卫生。
三、营养支持治疗对于需要营养支持的肿瘤科病人,医生可能会采取营养支持治疗的方式来满足其特殊的营养需求。
肿瘤科病人营养支持与指导随着肿瘤发病率的不断上升,肿瘤科的病人群体也越来越庞大。
与此同时,人们对于肿瘤科病人的营养支持与指导也越来越关注。
良好的营养状况对于肿瘤病人的治疗和康复非常重要。
本文将就肿瘤科病人的营养支持与指导进行探讨。
一、肿瘤病人的营养需求肿瘤病人的身体状态通常较为虚弱,而治疗过程中的副作用也对病人的食欲和消化功能造成了一定的影响。
因此,肿瘤病人的营养需求与一般人群有所不同。
在制定营养支持计划时,需综合考虑病人的病情、治疗方案以及个体差异等因素。
1. 蛋白质摄入肿瘤病人需要额外补充足够的蛋白质,以满足身体对于修复和代谢的需求。
在摄入蛋白质时,应优先选择优质蛋白,如鱼、禽肉、蛋类等。
同时,也可通过适量的乳制品和豆制品来保证蛋白质的摄入。
2. 脂肪摄入脂肪是病人的重要能量来源之一,对于细胞膜的修复以及各种生理功能起着重要作用。
合理的脂肪摄入有助于提高病人的免疫力,并减少肿瘤的恶化风险。
建议选择富含不饱和脂肪酸的食物,如鱼类、坚果和橄榄油等。
3. 碳水化合物摄入碳水化合物是病人能量的主要来源,合理的碳水化合物摄入能够满足身体的能量需求,同时避免出现肌肉消耗情况。
建议选择富含膳食纤维的碳水化合物,如全谷类食物、蔬菜和水果等。
二、营养支持的实施对于在肿瘤科进行治疗的病人来说,营养支持是非常重要的一环。
适当的营养支持可以增强病人的免疫力,减少治疗过程中的副作用,促进康复。
在实施营养支持时,需要遵循以下原则:1. 制定个性化的膳食方案根据病人的具体情况制定个性化的膳食方案,包括能量、蛋白质、脂肪和碳水化合物的摄入量。
应与病人进行沟通,了解其口味喜好、饮食禁忌等,以便于制定更符合病人实际情况的膳食方案。
2. 重视口腔护理肿瘤病人往往出现食欲不振、口干舌燥等情况,因此,重视口腔护理是非常必要的。
病人可以经常用淡盐水漱口,保持口腔清洁;还可以尝试一些温热、软烂、适口的食物,增加进食的兴趣。
3. 结合药物治疗在肿瘤病人的营养支持中,还需要结合药物治疗进行综合干预。