
European Medicines Agency
7 Westferry Circus, Canary Wharf, London, E14 4HB, UK London, 19 July 2007
Doc.
Ref.EMEA/CHMP/SWP/294648/2007
COMMITTEE FOR MEDICINAL PRODUCTS FOR HUMAN USE
(CHMP)
GUIDELINE ON STRATEGIES TO IDENTIFY AND MITIGATE RISKS FOR FIRST-IN-
HUMAN CLINICAL TRIALS WITH INVESTIGATIONAL MEDICINAL PRODUCTS
DRAFT AGREED BY CHMP EXPERT GROUP 6 March 2007
ADOPTION BY CHMP FOR RELEASE FOR CONSULTATION 22 March 2007
END OF CONSULTATION (DEADLINE FOR COMMENTS) 23 May 2007
AGREED BY CHMP EXPERT GROUP 4 July 2007
ADOPTION BY CHMP 19 July 2007
DATE FOR COMING INTO EFFECT 1 September 2007
KEYWORDS First-in-human, Phase I clinical trials, identification of risk, non-clinical
requirements, animal models, MABEL, risk mitigation strategies
GUIDELINE ON STRATEGIES TO IDENTIFY AND MITIGATE RISKS FOR FIRST-IN-HUMAN CLINICAL TRIALS WITH INVESTIGATIONAL MEDICINAL PRODUCTS
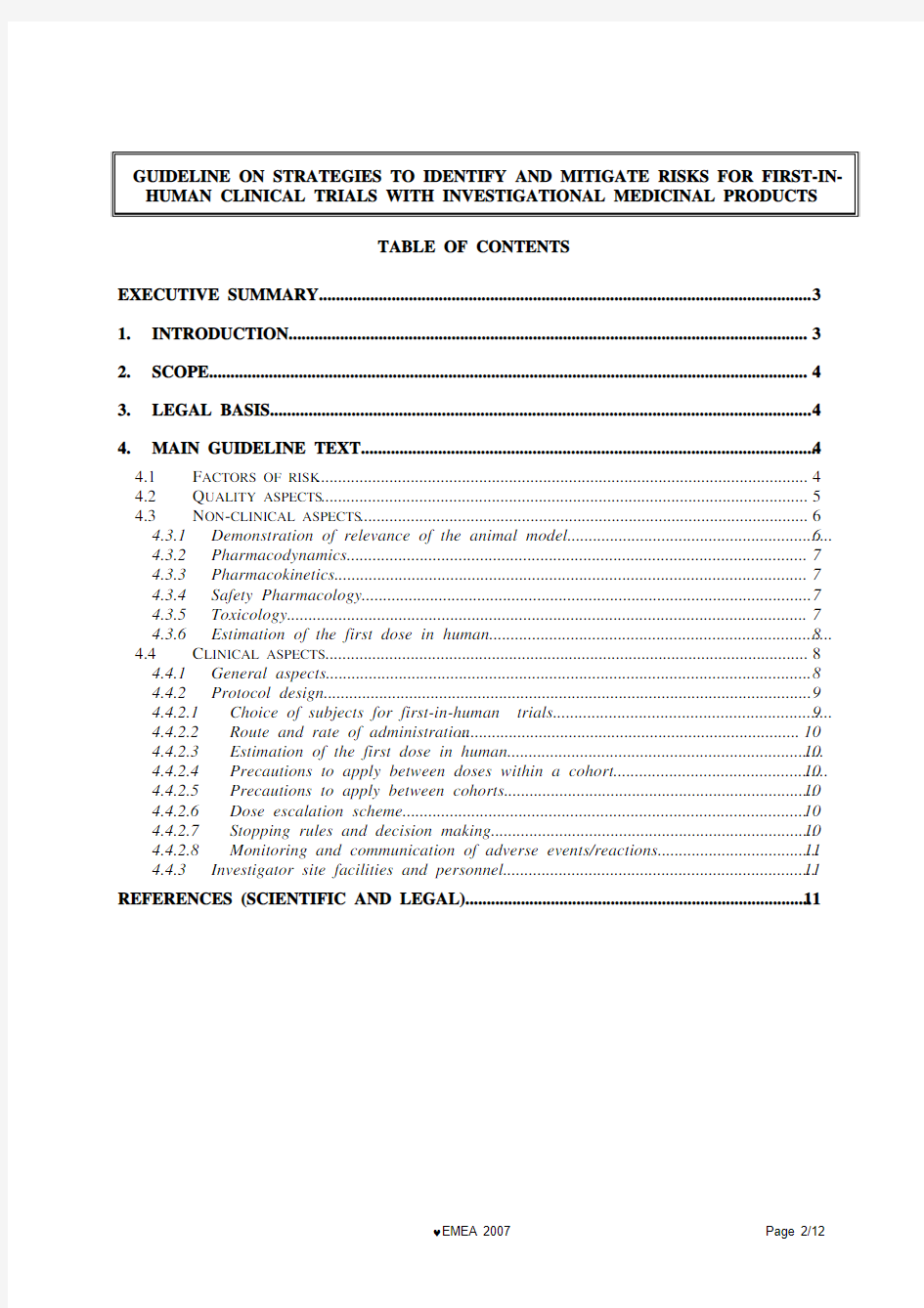
TABLE OF CONTENTS
EXECUTIVE SUMMARY (3)
1.INTRODUCTION (3)
2.SCOPE (4)
3.LEGAL BASIS (4)
4.MAIN GUIDELINE TEXT (4)
4.1F ACTORS OF RISK (4)
4.2Q UALITY ASPECTS (5)
4.3N ON-CLINICAL ASPECTS (6)
4.3.1Demonstration of relevance of the animal model (6)
4.3.2Pharmacodynamics (7)
4.3.3Pharmacokinetics (7)
4.3.4Safety Pharmacology (7)
4.3.5Toxicology (7)
4.3.6Estimation of the first dose in human (8)
4.4C LINICAL ASPECTS (8)
4.4.1General aspects (8)
4.4.2Protocol design (9)
4.4.2.1Choice of subjects for first-in-human trials (9)
4.4.2.2Route and rate of administration (10)
4.4.2.3Estimation of the first dose in human (10)
4.4.2.4Precautions to apply between doses within a cohort (10)
4.4.2.5Precautions to apply between cohorts (10)
4.4.2.6Dose escalation scheme (10)
4.4.2.7Stopping rules and decision making (10)
4.4.2.8Monitoring and communication of adverse events/reactions (11)
4.4.3Investigator site facilities and personnel (11)
REFERENCES (SCIENTIFIC AND LEGAL) (11)
EXECUTIVE SUMMARY
This guideline is intended to assist sponsors in the transition from non-clinical to early clinical development. It identifies factors influencing risk for new investigational medicinal products and considers quality aspects, non-clinical and clinical testing strategies and designs for first-in-human clinical trials. Strategies for mitigating and managing risk are given, including the calculation of the initial dose to be used in humans, the subsequent dose escalation, and the conduct of the clinical trial. 1. INTRODUCTION
The safety of subjects participating in first in human studies is the paramount consideration as they would not normally be expected to derive any therapeutic benefit.
Decisions on strategies for development of a new medicine and the experimental approaches used to assemble information relevant to the safety of first-in-human clinical trials must be science-based, and should be made and justified on a case-by-case basis.
Quality aspects should not, in themselves, be a source of risk for first-in-human trials. Nevertheless, special consideration should be given to certain factors which may add to the risk as described in this guideline.
The non-clinical testing and experimental approaches for first-in-human studies might identify potential factors influencing risk for investigational medicinal products. The ability of non-clinical studies to predict safety issues in humans may be limited because the nature of the target is more specific to humans or because of other factors.
The factors influencing the decision to proceed with the trial in healthy volunteers or patients and how to conduct the trials need to be carefully considered. Attention should be given to the estimation of the initial dose to be used in humans and to the subsequent dose escalations, intervals between doses to different individuals and the management of risk.
In defining an appropriate early development programme for an investigational medicinal product information on safety needs to be integrated from many sources and frequently reviewed in an iterative process.
This guideline is intended to assist sponsors in the transition from non-clinical to early clinical development by outlining factors influencing risk to be considered in the non-clinical testing strategy and designs of first-in-human clinical trials for investigational medicinal products.
Expert scientific advice on this topic may be requested from National Competent Authorities or the EMEA.
This guideline should be read in conjunction with the published EU guidelines (see also section references) and in particular the following:
Non-clinical aspects:
? Non-Clinical Safety Studies For The Conduct Of Human Clinical Trials For Pharmaceuticals (ICH M3), CPMP/ICH/286/95,
? Preclinical safety evaluation of biotechnology-derived pharmaceuticals (ICH S6) CPMP/ICH/302/95,
? The Non-clinical Evaluation of the Potential for delayed Ventricular Repolarisation (QT Interval Prolongation) by Human Pharmaceuticals (ICH S7B) CPMP/ICH/423/02 ? Safety pharmacology studies for human pharmaceuticals (ICH S7A)- CPMP/ICH/539/00
? Toxicokinetics: the assessment of systemic exposure in toxicity studies (ICH S3A) - CPMP/ICH/384/95
? Position Paper on the non-clinical safety studies to support clinical trials with a single micro dose (CPMP/SWP/2599/02)
Clinical aspects
? Guideline for Good Clinical Practice (ICH E6), CPMP/ICH/135/95
? General Considerations for Clinical Trials, (ICH E8) CPMP/ICH/291/95.
? EUDRALEX- Volume 10 – Clinical trials. In particular: Chapter I: Application and Application Form and Chapter II: Monitoring and Pharmacovigilance.
2. SCOPE
This guideline applies to all new chemical and biological investigational medicinal products except gene and cell therapy medicinal products. It covers non-clinical issues for consideration prior to the first administration in humans and the design and conduct of trials in the initial phase of single and ascending doses during the clinical development.
BASIS
3. LEGAL
This guideline applies to relevant Clinical Trial Authorisation applications submitted in accordance with Directive 2001/20/EC and should be read in conjunction with Directive 2001/83 as amended and its Annex I. (See references)
TEXT
GUIDELINE
4. MAIN
For many new investigational medicinal products, the non-clinical safety pharmacology and toxicology programme provides sufficient safety data for estimating risk prior to first administration in humans. However, for some novel medicinal products this non-clinical safety programme might not be sufficiently predictive of serious adverse reactions in man and the non-clinical testing and the design of the first-in-human study requires special consideration.
When planning a first-in-human clinical trial, sponsors and investigators should identify the factors of risk and apply risk mitigation strategies accordingly as laid down in this guideline. In addition to the principles expressed in this guideline, some special populations such as paediatrics may deserve specific considerations.
4.1 Factors of risk
Predicting the potential severe adverse reactions for the first-in-human use of an investigational medicinal product, involves the identification of the factors of risk. Concerns may be derived from particular knowledge or lack thereof regarding (1) the mode of action, (2) the nature of the target, and/or (3) the relevance of animal models.
The Sponsor should discuss the following criteria for all first-in-human trials in their clinical trial authorisation application. These criteria should be taken into account on a case-by-case basis.
? Mode of action
While a novel mechanism of action might not necessarily add to the risk per se, consideration should be given to the novelty and extent of knowledge of the supposed mode of action. This includes the nature and intensity (extent, amplification, duration, reversibility) of the effect of the medicinal product on the specific target and non-targets and subsequent mechanisms, if applicable. The type and steepness of the dose response as measured in experimental systems, which may be linear within the dose range of interest, or non-linear (e.g. plateau with a maximum effect, over-proportional increase, U-shaped, bell-shaped), is of importance.
For example, the following modes of action might require special attention:
? A mode of action that involves a target which is connected to multiple signalling pathways (target with pleiotropic effects), e.g. leading to various physiological effects, or targets that are ubiquitously expressed, as often seen in the immune system.
? A biological cascade or cytokine release including those leading to an amplification of an effect that might not be sufficiently controlled by a physiologic feedback mechanism (e.g., in the immune system or blood coagulation system). CD3 or CD28 (super-) agonists might serve as an example.
When analysing risk factors associated with the mode of action, aspects to be considered may include: ? Previous exposure of human to compounds that have related modes of action.
? Evidence from animal models (including transgenic, knock-in or knock-out animals) for the potential risk of serious, pharmacologically mediated toxicity
? Novelty of the molecular structure of the active substance(s), for example a new type of engineered structural format, such as those with enhanced receptor interaction as compared to the parent compound.
? Nature of the target
The target in human should be discussed in detail. Beyond the mode of action, the nature of the target itself might impact on the risk inherent to a first administration to humans, and sponsors should discuss the following aspects, based on the available data:
? the extent of the available knowledge on the structure, tissue distribution (including expression in/on cells of the human immune system), cell specificity, disease specificity, regulation, level of expression, and biological function of the human target including “down-stream” effects, and how it might vary between individuals in different populations of healthy subjects and patients.
? If possible a description of polymorphisms of the target in relevant animal species and humans, and the impact of polymorphisms on the pharmacological effects of the medicinal product.
? Relevance of animal species and models
The Sponsor should compare the available animal species to humans taking into account the target, its structural homology, distribution, signal transduction pathways and the nature of pharmacological effects. (See also 4.3.1)
Where available animal species/models or surrogates are perceived to be of questionable relevance for thorough investigation of the pharmacological and toxicological effects of the medicinal product, this should be considered as adding to the risk.
aspects
4.2 Quality
The requirements are the same for all investigational medicinal products regarding physico-chemical characterisation and, additionally biological characterisation of biological products (see references). Quality attributes should not, in themselves, be a source of risk for first-in-human trials. However, these quality attributes are to be considered in a risk assessment preceding a first-in-human trial. Specific points to be considered are:
? Determination of strength and potency
To determine a safe starting dose, the methods used for determination of the strength and/or the potency of the product need to be relevant, reliable and qualified. As an example, where the dose is based on biological activity and is expressed in arbitrary units, and the assays are not qualified and/or validated to ensure their reliability, the doses used in non-clinical studies may be poorly defined and mislead the interpretation of what is a safe dose. Therefore it is important to have a representative defined reference material from early in the development programme to measure biological activity. For a biological medicinal product, the lack of a bioassay measuring the functional or biological activity should be justified.
? Qualification of the material used
The material used in non-clinical studies should be representative of the material to be used for first-in-human administration. It is important to have an adequate level of quality characterisation even at this early point of development. A characterisation of the product including its heterogeneity, degradation profile and process-related impurities should be performed. Particular attention should be given to impurities that could be pharmacologically active and/or toxic. Special consideration should be given to the suitability and qualification of methods to sufficiently characterise the active substance and drug product.
When moving from non-clinical studies to first-in-human administration, there should be sufficient assurance that product differences, should they occur, would not have an adverse impact on clinical
characteristics of the product, especially safety. Furthermore, during the early development of a product, significant modifications to the manufacturing process frequently occur. Particularly in the case of complex molecules, these modifications can potentially result in subtle changes to the active substance that may not be detectable in characterisation studies but can affect biological properties and could have clinical consequences.
Given the fact that major clinical decisions are based on the non-clinical data it is important to show that these data remain valid.
Further non-clinical studies may be needed with the product intended for use in the first-in-human trial in the following situations:
o Where there are differences in the product quality attributes of the non-clinical and clinical material and adverse clinical consequences may result from such differences.
o Where there are differences in the manufacturing process and the limitations of product characterisation, including biological assays, cannot assure that the material used in non-
clinical studies is representative of the material to be used in clinical studies.
? Reliability of very small doses
Applicants should demonstrate that the intended formulation of the doses to be administered provides the intended dose. There is a risk of reduced accuracy in cases where the medicinal product needs to be diluted, to prepare very small doses, or the product is provided at very low concentrations as the product could be adsorbed to the wall of the container or infusion system. This might lead to an over-estimation of the safety of the initial clinical doses and non-clinical safety data. Therefore, compatibility of the product with primary packaging materials and administration systems should be investigated, where relevant.
aspects
4.3 Non-clinical
4.3.1 Demonstration of relevance of the animal model
Qualitative and quantitative differences may exist in biological responses in animals compared to humans. For example, there might be differences in affinity for molecular targets, tissue distribution of the molecular target, cellular consequences of target binding, cellular regulatory mechanisms, metabolic pathways, or compensatory responses to an initial physiological perturbation.
Where there is evidence of species-specificity of action from in vitro studies with human cells compared with cells from a test species, the value of the in vivo response of the test species may be significantly reduced in terms of predicting the in vivo human response. It should be noted that a similar response in human and animal cells in vitro is not necessarily a guarantee that the in vivo response will be similar.
In practice this means that animal studies with highly species-specific medicinal products may: ? not reproduce the intended pharmacological effect in humans;
? give rise to misinterpretation of pharmacokinetic and pharmacodynamic results;
? not identify relevant toxic effects.
A weight-of-evidence approach should involve integration of information from in vivo,ex vivo and in vitro studies into the decision-making process.
High species-specificity of a medicinal product makes the non-clinical evaluation of the risk to humans much more difficult, but does not imply that there is always an increased risk in first-in-human trials.
The demonstration of relevance of the animal model(s) may include comparison with humans of: o Target expression, distribution and primary structure. However, a high degree of homology does not necessarily imply comparable effects;
o Pharmacodynamics
? Binding and occupancy, functional consequences, including cell signalling if relevant.
? Data on the functionality of additional functional domains in animals, if applicable,
e.g. Fc receptor system for monoclonal antibodies.
o Metabolism and other pharmacokinetic aspects
o Cross-reactivity studies using human and animal tissues (e.g. monoclonal antibodies).
The search for a relevant animal model should be documented and justified in detail.
Where no relevant species exists, the use of homologous proteins or the use of relevant transgenic animals expressing the human target may be the only choice. The data gained is more informative when the interaction of the product with the target receptor has similar physiological consequences to those expected in humans. The use of in vitro human cell systems could provide relevant additional information.
The relevance and limitations of all models used should be carefully considered and discussed fully in the supporting documentation.
4.3.2 Pharmacodynamics
Pharmacodynamic studies should address the mode of action, and provide knowledge on the biology of the target. These data will help to characterise the pharmacological effects and to identify the most relevant animal models. The primary and secondary pharmacodynamics, should be conducted in in vitro animal and human systems and in vivo in the animal models. These studies should include target interactions preferably linked to functional response, e.g. receptor binding and occupancy, duration of effect and dose-response.
A dose/concentration-response curve of the pharmacological effect(s) should be established with sufficient titration steps in order to increase the likelihood to detect significant pharmacological effects with low doses and to identify active substances with U-shaped or bell-shaped dose-response curves. Such significant or even reverse effects have been reported with biological compounds. Since a low dose is to be administered to humans in the first-in-human trial, this is of high importance.
Although GLP compliance is not mandatory for pharmacodynamic and pharmacokinetic studies, they should be of high quality and consistent with the principles of GLP.
4.3.3 Pharmacokinetics
Standard pharmacokinetic and toxicokinetic data should be available in all species used for safety studies before going into human (ICH S3, S6, M3).
Exposures at pharmacodynamic doses in the relevant animal models should be determined especially when pharmacodynamic effects are suspected to contribute to potential safety concerns.
4.3.4 Safety Pharmacology
Standard core battery data should be available before the first administration in humans (CHMP/ICH guidelines S7A, S7B, S6, M3).
Additional studies to investigate effects in other organ systems should be carried out on a case by case basis. In particular, for medicinal products targeting the immune system, potential unintended effects should be investigated, e.g. using in vitro studies, including human material.
4.3.5 Toxicology
The toxicology programme should be performed in relevant animal species and include toxico-kinetics.
When factors influencing risk are identified (see section 4.1), the inclusion of additional endpoints should be considered, on a case-by-case basis.
Toxicity studies in non-relevant species may give rise to misinterpretation and are discouraged. The use of homologous products or transgenic model approach or of in vitro human cell systems could provide relevant additional information.
It should be noted that human specific proteins are likely to be immunogenic in animal species. Therefore repeat dosing studies in animals may not predict the effects of such substances in humans (e.g. presence of neutralising antibodies).
Animal models that are thought to be similar to the human disease may provide further insight in the pharmacological action, the pharmacokinetics, (e.g. disease-related expression of the target) as well as dosing in patients and safety (e.g., evaluation of undesirable promotion of disease progression). Therefore, in certain cases, studies performed in animal models of disease may be used as an acceptable alternative to toxicity studies in normal animals. The scientific justification for the use of these animal models of disease to support safety should be provided.
4.3.6 Estimation of the first dose in human
The estimation of the first dose in human is an important element to safeguard the safety of subjects participating in first-in-human studies. All available information has to be taken in consideration for the dose selection and this has to be made on a case-by-case basis. Different methods can be used.
In general, the No Observed Adverse Effect Level (NOAEL) determined in non-clinical safety studies performed in the most sensitive and relevant animal species, adjusted with allometric factors (see references “Other guidelines”) or on the basis of pharmacokinetics gives the most important information. The relevant dose is then reduced/adjusted by appropriate safety factors according to the particular aspects of the molecule and the design of the clinical trials.
For investigational medicinal products for which factors influencing risk according to section 4.1 have been identified, an additional approach to dose calculation should be taken. Information about pharmacodynamics can give further guidance for dose selection. The ‘Minimal Anticipated Biological Effect Level’ (MABEL) approach is recommended. The MABEL is the anticipated dose level leading to a minimal biological effect level in humans. When using this approach, potential differences of sensitivity for the mode of action of the investigational medicinal product between humans and animals, need to be taken into consideration e.g. derived from in-vitro studies. A safety factor may be applied for the calculation of the first dose in human from MABEL as discussed below.
The calculation of MABEL should utilise all in vitro and in vivo information available from pharmacokinetic/pharmacodynamic (PK/PD) data such as:
i) target binding and receptor occupancy studies in vitro in target cells from human and the relevant
animal species;
ii) concentration-response curves in vitro in target cells from human and the relevant animal species and dose/exposure-response in vivo in the relevant animal species.
iii) exposures at pharmacological doses in the relevant animal species.
Wherever possible, the above data should be integrated in a PK/PD modelling approach for the determination of the MABEL.
In order to further limit the potential for adverse reactions in humans, a safety factor may be applied in the calculation of the first dose in human from the MABEL. This should take into account criteria of risks such as the novelty of the active substance, its biological potency and its mode of action, the degree of species specificity, and the shape of the dose-response curve and the degree of uncertainty in the calculation of the MABEL. The safety factors used should be justified.
When the methods of calculation (e.g. NOAEL, MABEL) give different estimations of the first dose in man, the lowest value should be used, unless justified.
Other approaches may also be considered in specific situations, e.g. for studies with conventional cytotoxic IMPs in oncology patients. (See references “Other guidelines”)
4.4 Clinical aspects
4.4.1 General aspects
The safety of participants in first-in-human clinical trials can be enhanced by identification and planned mitigation of factors associated with risk. Key aspects of the trial should be designed to mitigate those risk factors, including:
? study population;
? trial sites;
? first dose;
? route and rate of administration;
? number of subjects per dose increment (cohort);
? sequence and interval between dosing of subjects within the same cohort;
? dose escalation increments;
? transition to next dose cohort;
? stopping rules;
? allocation of responsibilities for decisions with respect to subject dosing and dose escalation.
In general, the higher the potential risk associated with an investigational medicinal product (IMP) and its pharmacological target, the greater the precautionary measures that should be exercised in the design of the first-in-human study. The protocol should describe the strategy for managing risk including a specific plan to monitor for and manage likely adverse events or adverse reactions as well as the procedures and responsibilities for modifying or stopping the trial if necessary. The sponsor should arrange for peer review of the protocol and the associated risk factors and to assure that they have been properly considered and planned for.
It is recognised that placebo is often included as part of the design of Phase I studies. The study design including randomisation schemes should take this into account. Any decisions taken with respect to subsequent dosing at the same dose level and or to dose escalation, should take into account the number of subjects that might have received either placebo or the active medicinal product. There should always be rapid access to the treatment allocation codes when relevant.
For first-in-human trials where there is uncertainty about the risk it is recommended that a confirmatory pharmacodynamic measure is identified that can show the pharmacological effect and link with the preclinical experience.
4.4.2 Protocol design
4.4.2.1 Choice of subjects for first-in-human trials
Subjects are not generally expected to derive any therapeutic benefit from a first-in-human trial.
The paramount factors should always be the safety, rights and well-being of the volunteers, whether patients or healthy individuals, and the value of what can be learned from the clinical trial.
The choice of the study population, i.e. healthy subjects or patients, including special populations, should be fully justified by the sponsor on a case-by-case basis. Several factors should be considered, such as:
(a) the risks inherent in the type of medicinal product - it is important that those risks (and
uncertainty about them) be quantified and justified;
(b) its molecular target,
(c) immediate and potential long term toxicity;
(d) the lack of a relevant animal model;
(e) the relative presence of the target in healthy subjects or in patients; e.g. cancer patients;
(f) the possible higher variability in patients;
(g) the ability of healthy volunteers to tolerate any potential side effects;
(h) the potential pharmacogenomic difference between the targeted patient group and healthy
subjects;
(i) the patients’ ability to benefit from other products or interventions; and
(j) the predicted therapeutic window of the IMP.
Where practicable concurrent medication in patients should be avoided as it, together with the disease state may give rise to greater variability in response and interactions, with the possibility for adverse reactions and/or difficulties in the interpretation of results.
Healthy subjects or patients should not be included in first-in-human clinical trials if they are in another clinical trial or have participated recently in another clinical trial unless justified. It is important to include clear exclusion criteria to prevent concomitant or immediate consecutive exposure to investigational medicinal products.
4.4.2.2 Route and rate of administration
The choice of route and rate of administration of the first dose in humans should be justified based on the non-clinical data. In the case of an intravenous administration, a slow infusion, may be more appropriate than a slow bolus. This would allow monitoring for an adverse reaction and, if clinically indicated, timely discontinuation of the infusion to mitigate a serious outcome.
4.4.2.3 Estimation of the first dose in human
The estimation of the first dose in humans has been discussed above in detail (see section 4.3.6).
4.4.2.4 Precautions to apply between doses within a cohort
It will usually be appropriate to design the administration of the first dose so that a single subject receives a single dose of the active IMP. Further dose administration should be sequential within each cohort to mitigate the risk. Any non-sequential dose administration within each cohort should be justified. There must be an adequate period of observation between the administration of the medicinal product to the first, second and subsequent subjects in a cohort to observe and interpret reactions and adverse events. The duration of the interval of observation should be justified and will depend on the properties of the product and the data available, including non-clinical PK and PD. Experience and identified risk factors from trials with comparable medicinal products should also be considered.
The number of subjects per dose increment (the cohort size) depends on the variability of both pharmacokinetic and pharmacodynamic parameters and the trial objectives such as justifying progression to the next cohort. While larger cohorts are likely to provide more precise data, they may not be necessary to fulfil the objectives of the study.
4.4.2.5 Precautions to apply between cohorts
Where risk factors from section 4.1 are identified for the IMP there should be a precautionary approach to progressing to a subsequent cohort. Criteria should be pre-specified in the protocol that will be used to identify and mitigate the risk of progressing to a subsequent cohort. Administration in the next cohort should not occur before participants in the previous cohort have been treated and data/results from those participants are reviewed in accordance with the protocol. This may include comparison of PK, PD or PK/PD data from any previous cohorts with known non-clinical data and safety information to inform the decision. Any observed pharmacological responses should be compared to the responses that were anticipated. Unanticipated pharmacological responses may require a revised dose escalation. Time intervals between cohorts should be guided by non-clinical and clinical PK and PD data and if available, data from comparable medicinal products.
4.4.2.6 Dose escalation scheme
Dose increases should proceed with caution taking into account identified risk factors from non-clinical studies such as a steep dose-response curve, exposure-response and dose-toxicity curves.
The dose increment between two dose levels should be guided by the dose/toxicity or dose/effect relationship defined in non-clinical studies, depending on whichever is steeper where this information is available. The steeper the increase in the dose/toxicity or dose/effect curves, the lower the dose increment that should be selected. The choice of the next dose level should include some estimate of the potential pharmacodynamic effects and adverse effects (if any).
Information on exposure, effect, and safety from the preceding dose in human should be taken into account. Since the initial doses may be very low, it is anticipated that early cohorts may not show any pharmacological effects. Where there is no response in a cohort the precautions for the next cohort should be the same as for the previous cohort.
4.4.2.7 Stopping rules and decision making
The protocol should define stopping rules for the cohort and trial. It should define processes and responsibilities for making decisions about dosing of subjects, dose escalation and stopping the cohort or trial. In the case of multicentre trials it is particularly important to define processes for immediate communications between sites.
4.4.2.8 Monitoring and communication of adverse events/reactions
The trial design should provide a specific plan for monitoring for adverse events or adverse reactions. The mode of action of the investigational medicinal product,findings in the non-clinical toxicity studies and any anticipated responses should be used to identify likely adverse reactions. All clinical staff should be trained to identify those reactions and how to respond to those or any other adverse events or reactions. There should be constantly available rapid access to the treatment allocation codes when relevant.
In cases where there is a predictable risk of a certain type of adverse reaction occurring in humans, a treatment strategy should be described in the protocol. This should include the availability of specific antidotes where they exist, a clear plan of availability of supportive treatment emergency facilities and medical staff.
The length of the monitoring period and nature of monitoring within and if deemed appropriate outside the research site should be justified on the grounds of pharmacokinetics, pharmacodynamics and safety endpoints as part of the strategy to manage risks in the clinical trial. Special consideration should be given to potential long-term consequences on physiological systems and potential long-term safety problems.
Communication of serious adverse events and suspected unexpected serious adverse reactions (SUSARs) is particularly important. Sponsors should ensure that processes are in place, before the trial starts, for expedited reporting of any SUSARs to the national competent authority (ies), ethics committee(s) and investigator(s). The sponsor needs to ensure that these processes include the necessary steps for reporting of the SUSARs to the EudraVigilance Clinical Trial Module. (see Directive 2001/20/EC and Chapter II of Volume 10 of the Rules Governing Medicinal Products in the European Community)
4.4.3 Investigator site facilities and personnel
First-in-human trials should take place in appropriate clinical facilities and be conducted by trained investigators who have acquired the necessary expertise and experience in conducting early phase trials (i.e. phase I-II) and medical staff with appropriate level of training and previous experience of first-in-human studies. They should also understand the investigational medicinal product, its target and mechanism of action.
Units should have immediate access to equipment and staff for resuscitating and stabilising individuals in an acute emergency (such as cardiac emergencies, anaphylaxis, cytokine release syndrome, convulsions, hypotension), and ready availability of Intensive Care Unit facilities. Procedures should be established between the clinical research unit and its nearby Intensive Care Unit regarding the responsibilities and undertakings of each in the transfer and care of patients.
First-in-human trials should preferably be conducted as a single protocol at a single site. When different sites are involved this should be justified and an appropriate plan needs to be in place to assure the well-being of all trial participants and to assure an adequate information communication system. This information system should ensure that new safety findings are transmitted to all participating sites and that the integrity of the study design is not compromised.
REFERENCES (scientific and legal)
Legal basis
? Directive 2001/20/EC of the European Parliament and of the Council of 4 April 2001 on the approximation of the laws, regulations and administrative provisions of the Member States relating to the implementation of good clinical practice in the conduct of clinical trials on medicinal products for human use (Official Journal L 121, 1/5/2001 p. 34 - 44).
? Directive 2001/83/EC of the European Parliament and of the Council of 6 November 2001 on the Community code relating to medicinal products for human use (Official Journal L 311, 28/11/2001 p. 67 - 128).
Consolidated Directive 2001/83/EC of the European Parliament and of the Council of 6 November 2001 on the Community code relating to medicinal products for human use as amended by
Directive 2002/98/EC, Directive 2004/24/EC and Directive 2004/27/EC. (Official journal l – 311, 28/11/2004, p. 67 – 128)
? Detailed guidance for the request for authorisation of a clinical trial on a medicinal product for human use to the competent authorities, notification of substantial amendments and declaration of the end of the trial. October 2005 Revision 2
Detailed guidances in Volume 10 of the Rules Governing Medicinal Products in the European Community
? Detailed guidance on the application format and documentation to be submitted in an application for an Ethics Committee opinion on the clinical trial on medicinal products for human use February 2006 Revision 1
? Detailed guidance on the collection, verification and presentation of adverse reaction reports arising from clinical trials on medicinal products for human use April 2006 Revision 2.
? Detailed guidance on the European database of Suspected Unexpected Serious Adverse Reactions (Eudravigilance – Clinical Trial Module) as required by Article 11, Article 17 and Article 18 of Directive 2001/20/EC Revision 1. April 2004.
Guidance on quality aspects
? EUDRALEX -Volume 4 - Medicinal Products for Human and Veterinary Use: Good Manufacturing Practice. In particular, Annex 13: Manufacture of Investigational Medicinal Products.
? Guideline on Virus Safety Evaluation of Biotechnological Investigational Medicinal Products - Draft- EMEA/CHMP/BWP/398498/2005-corr.
? Guideline on the Requirements to the Chemical and Pharmaceutical Quality Documentation concerning Investigational Medicinal Products in Clinical Trials. CHMP/QWP/185401/2004
Other guidelines
? Guidance for Industry Estimating the Maximum Safe Starting Dose in Initial Clinical Trials for Therapeutics in Adult Healthy Volunteers. FDA/CDER, July 2005
? Pre-clinical evaluation of anti- cancer medicinal products (CPMP/SWP/997/96)
? Evaluation of Anticancer Medicinal Products in Man (CPMP/EWP/205/95 Rev. 3)
药物临床试验的一般考虑指导原则 一、概述 药物临床试验的一般考虑指导原则(以下称指导原则),是目前国家食品药品监督管理总局关于研究药物在进行临床试验时的一般考虑。制定本指导原则的目的是为申请人和研究者制定药物整体研发策略及单个临床试验提供技术指导,同时也为药品技术评价提供参考。另外,已上市药品增加新适应症等进行临床试验时,可参照本指导原则。本指导原则主要适用于化学药物和治疗用生物制品。 二、临床试验基本原则 (一)受试者保护 1.执行相关法律法规 药物临床试验必须遵循世界医学大会赫尔辛基宣言,执行国家食品药品监督管理总局公布的《药物临床试验质量管理规范》等相关法律法规。 2.应具备的安全性基础 开展任何临床试验之前,其非临床研究或以往临床研究的结果必须足以说明药物在所推荐的人体研究中有可接受的安全性基础。 在整个药物研发过程中,应当由药理毒理专家和临床专家等动态地对药理毒理数据和临床数据进行评价,以评估临床试验可能给受试者带来的安全性风险。对于正在或将要进行的临床试验方案,也应进行必要的调整。 参与药物临床试验的有关各方应当按各自职责承担保护受
试者职责。 (二)临床试验基本方法 1.临床试验一般规律 药物研发的本质在于提出有效性、安全性相关的问题,然后通过研究进行回答。临床试验是指在人体进行的研究,用于回答与研究药物预防、治疗或诊断疾病相关的特定问题。通常采用两类方法对临床试验进行描述。 按研发阶段分类,将临床试验分为Ⅰ期临床试验、Ⅱ期临床试验、Ⅲ期临床试验和Ⅳ期临床试验。 按研究目的分类,将临床试验分为临床药理学研究、探索性临床试验、确证性临床试验、上市后研究。 两个分类系统都有一定的局限性,但两个分类系统互补形成一个动态的有实用价值的临床试验网络(图1)。 图1. 临床研发阶段与研究类型间的关系 (实心圆代表在某一研发阶段最常进行的研究类型,空心圆代表某些可能但较少进行的研究类型)概念验证(Proof of Concept,POC)是指验证候选药物的药理效应可以转化成临床获益,一般在早期临床研究阶段进行,用以探索安全耐受剂量下有效性的信号,降低临床开发风险。 本指导原则采用以研究目的分类为主线对临床试验进行描述。 临床药理学研究的目的是评价耐受性,明确并描述药代动力学及药效学特征,探索药物代谢和药物相互作用,以及评估药物活性。 探索性临床试验的研究目的是探索目标适应症后续研究的给药方案,为有效性和安全性确证的研究设计、研究终点、方法
北京市第二类体外诊断试剂临床试验 指导原则 由于体外诊断试剂产品具有发展快、专业跨度大、临床使用目的各异的特点,不同使用目的的产品,临床研究方法及内容不尽相同。申请人应在完成产品分析性能评估,拟定产品标准后,方可申请体外诊断试剂产品的临床评价。临床评价开始前,申请人应根据产品特点及使用目的,确定临床评价的项目、方法,制定合理的临床评价方案,合理、系统地评价申报产品的临床性能。本方案仅用于指导体外诊断试剂检测方法一致性临床研究,并对临床试验机构的选择、样本要求、检测前的准备、临床试验数据的分析等具体操作提出了一般性要求。 申请人应根据国家法律、法规、标准及技术指导原则的要求建立更加可靠、可重复的临床评价方案,合理评价产品的安全性、有效性。 一、临床试验机构的选择 临床评价开始前,申请人应根据申报产品特点选择临床试验机构。临床试验机构应当具有与申报产品相适应的人员、场地、设备、仪器和管理制度,试验机构的选择应符合以下标准要求:
本方案将申报产品的检测系统称为试验系统,所选择的对照检测系统称为对照系统。 (一)应选择至少2家(含两家)省级卫生医疗机构,特殊使用的产品可在市级以上的疾病控制中心、专科医院或检验检疫所、戒毒中心等临床机构。临床机构的检验实验室(简称实验室)应符合《医疗机构临床实验室管理办法》要求;应优先考虑经CNAS-CL02《医学实验室能力认可准则》(ISO 15189:2007)认可或GB17025标准认可的实验室。 (二)实验室所釆用的检测系统应为完整、有效的, 检测系统包括申报产品的检测系统和所选择的对照检测系统。对照检测系统的试剂、校准品、仪器等应是经注册批准的;其主要分析性能指标(如准确性、精密度、线性范围、参考区间、测量范围等)满足临床要求。 申报产品的检测系统与所选择的对照检测系统最好为同一类型的检测方法(如同为酶联免疫反应、同为化学发光免疫反应等),如为非同一类型的检测方法,尽可能选择分析性能较近似的方法。 (三)实验室应有完善的室内质控程序;应优先选择连续两年以上室间质量评价结果为满意的实验室。 (四)实验室的该项目检测人员应具有相应资质(项目
中成药临床应用指导原则 一、中成药安全性 中成药的历史悠久,应用广泛,大量研究和临床实践表明,在合理使用的情况下,中成药的安全性是较高的。合理使用包括正确的辨证选药、用法用量、使用疗程、禁忌症、合并用药等多方面,其中任何环节有问题都可能引发药物不良事件。合理用药是中成药应用安全的重要保证。药物的两重性是药物作用的基本规律之一,中成药也不例外,中成药既能起到防病治病的作用,也可引起不良反应。 1.中成药使用中出现不良反应的主要原因 (1)中药自身的药理作用或所含毒性成分引起的不良反应 (2)特异性体质对某些药物的不耐受、过敏等。 (3)方药证候不符,如辨证不当或适应证把握不准确 (4)长期或超剂量用药,特别是含有毒性中药材的中成药,如朱砂、雄黄、蟾酥、附子、川乌、草乌、北豆根等,过量服用即可中毒(5)不适当的中药或中西药的联合应用。 2.中成药使用中出现的不良反应有多种类型 临床可见以消化系统症状、皮肤粘膜系统症状、泌尿系统症状、神经系统症状、循环系统症状、呼吸系统症状、血液系统症状、精神症状或过敏性休克等为主要表现的不良反应,可表现为其中一种或几种症状。 3.临床上预防中成药不良反应,要注意以下几个方面: (1)加强用药观察及中药不良反应监测,完善中药不良反应报告制
度。 (2)注意药物过敏史。对有药物过敏史的患者应密切观察其服药后的反应,如有过敏反应,应及时处理,以防止发生严重后果。(3)辨证用药,采用合理的剂量和疗程。尤其是对特殊人群,如婴幼儿、老年人、孕妇以及原有脏器损害功能不全的患者,更应注意用药方案。 (4)注意药物间的相互作用,中、西药并用时尤其要注意避免因药物之间相互作用而可能引起的不良反应。 (5)需长期服药的患者要加强安全性指标的监测。 二、中成药临床应用基本原则 1.辨证用药:依据中医理论,辨认、分析疾病的证候,针对证候确定具体治法,依据治法,选定适宜的中成药。辨病辨证结合用药辨病用药是针对中医的疾病或西医诊断明确的疾病,根据疾病特点选用相应的中成药。临床使用中成药时,可将中医辨证与中医辨病相结合、西医辨病与中医辨证相结合,选用相应的中成药,但不能仅根据西医诊断选用中成药。 2.剂型的选择应根据患者的体质强弱、病情轻重缓急及各种剂型的特点,选择适宜的剂型。 3.使用剂量的确定对于有明确使用剂量的,慎重超剂量使用。有使用剂量范围的中成药,老年人使用剂量应取偏小值。 4.合理选择给药途径能口服给药的,不采用注射给药;能肌内注射给药的,不选用静脉注射或滴注给药。
附件1 证候类中药新药临床研究技术指导原则 证候(简称证)是对疾病(泛指非健康)发展到一定阶段的病因、病性、病位及病势等的高度概括,具体表现为一组有内在联系的症状和体征,是中医临床诊断和治疗的依据。为了更好地传承和发扬中医药特色和优势,国家药品监督管理局根据药品注册相关法规,特制定《证候类中药新药临床研究技术指导原则》(以下简称《指导原则》)。 证候类中药新药是指主治为证候的中药复方制剂新药。《指导原则》旨在为证候类中药新药临床试验的开展和有效性、安全性评价提供基础性指导,其正文内容中的每一个原则性要求都可以随着后续研究的不断深入,进一步丰富和发展为更详实具体的技术标准。 一、证候类中药新药的处方来源及基本要求 证候类中药新药的处方应来源于临床实践,符合中医药理论,体现理、法、方、药相一致的原则。证候类中药新药申请临床试验应有充分的人用历史证明性文献材料,包括处方来源、组方合理性、临床应用情况(包括提供临床实践完善处方的演变过程)、功能主治、用法用量等相关内容。如拟开发的证候类中药新药是来源于中医临床经验的积累,针对临床常见基本证候的,应提供相关证明;如是源于医案中对比分析研究所发现的相对成
熟有效的处方,应提供典型医案和系列医案;如具有一定临床研究基础且有相应数据证明的成熟有效的处方,应提供相关临床研究总结报告,该总结报告应明确具体中医证候、疗效特点和安全性信息;如是源于国家科技立项的临床研究成果,应提供临床研究部分的总结资料及相关的成果鉴定材料。 证候类中药新药立项开发时,应注意评估与已上市同类药品的临床价值差异,以明确其是否具备临床开发价值。 二、证候类中药新药的临床定位 证候类中药新药临床应定位于消除、改善或控制具有内在关联性的一组疾病的主要临床症状、体征等,也可定位于通过证候改善达到疾病治疗等目的。 三、证候类中药新药的证候诊断 拟开发新药的中医证候确定应有与之相关的临床实践基础,并应遵循中医药理论。 中医证候诊断标准可以参照有关国家标准、行业标准或团体标准等进行制定,如无适用的诊断标准,可自行制定并经专家论证达成共识。证候诊断构成要素可采用定性或半定量方式,或主次症的方法,鼓励制定具有中医特色的证候诊断量表,并可根据具体研究内容辅以客观诊断指标。 四、证候类中药新药的基本研究思路及试验设计 (一)基本研究思路 证候类中药新药临床研究可有多种模式,如单纯中医证候研究模式、中医病证结合研究模式或中医证统西医病的研究模式,
中成药临床应用指导原则 2010年6月
目录 前言 (2) 第一部分中成药概述 (3) 一、中成药的剂型 (3) 二、中成药分类 (7) 三、中成药安全性 (9) 第二部分中成药临床应用原则 (11) 一、中成药临床应用基本原则 (11) 二、联合用药原则 (12) 三、孕妇使用中成药的基本原则 (13) 四、儿童使用中成药的基本原则 (14) 第三部分各论 (16) 一、解表剂 (16) 二、泻下剂 (17) 三、和解剂 (18) 四、清热剂 (19) 五、祛暑剂 (20) 六、温里剂 (21) 七、表里双解剂 (22) 八、补益剂 (23) 九、安神剂 (24) 十、开窍剂 (25) 十一、固涩剂 (25) 十二、理气剂 (26) 十三、理血剂 (27) 十四、治风剂 (28) 十五、治燥剂 (29) 十六、祛湿剂 (30) 十七、祛痰剂 (31) 十八、止咳平喘剂 (32) 十九、消导化积剂 (33) 二十、杀虫剂 (34) 第四部分中成药临床应用的管理 (35) 一、含毒性中药材的中成药临床应用的管理 (35) 二、中成药不良反应的监测 (36) 三、开展中成药临床应用监测、建立中成药应用点评制度 (37)
前言 为加强中成药临床应用管理,提高中成药应用水平,保证临床用药安全,国家中医药管理局会同有关部门组织专家制定了《中成药临床应用指导原则》(以下简称《指导原则》)。《指导原则》由四部分组成,第一部分为中成药概述;第二部分为中成药临床应用基本原则;第三部分为各类中成药的特点、适应证及注意事项;第四部分为中成药临床应用的管理。 《指导原则》是为适应中成药临床应用管理需要而制定的,是临床应用中成药的基本原则。每种中成药临床应用的具体要求,还应以药品说明书、最新版本的《中华人民共和国药典》、《中华人民共和国药典-临床用药须知-中药卷》为准。在医疗工作中,临床医师应遵循中医基础理论,根据患者实际情况,选用适宜的药物,辨证辨病施治。 第三部分各论中为更好地说明各类中成药的特点,列举了部分中成药,列举的药物是《国家基本药物目录》中的药物和《国家基本药物目录》未包括但又属临床常用的中成药。 中药注射剂的临床应用及使用管理,《指导原则》提出了具体要求,同时还应遵照《卫生部关于进一步加强中药注射剂生产和临床使用管理的通知》(卫医政发〔2008〕71号)执行。
中成药临床应用指导原则 Prepared on 22 November 2020
中成药临床应用指导原则 一、中成药临床应用基本原则 1.辨证用药依据中医理论,辨认、分析疾病的证候,针对证候确定具体治法,依据治法,选 定适宜的中成药。 2.辨病辨证结合用药辨病用药是针对中医的疾病或西医诊断明确的疾病,根据疾病特点选用 相应的中成药。临床使用中成药时,可将中医辨证与中医辨病相结合、西医辨病与中医辨证相结合, 选用相应的中成药,但不能仅根据西医诊断选用中成药。 3.剂型的选择应根据患者的体质强弱、病情轻重缓急及各种剂型的特点,选择适宜的剂型。 4.使用剂量的确定对于有明确使用剂量的,慎重超剂量使用。有使用剂量范围的中成药,老 年人使用剂量应取偏小值。 5.合理选择给药途径能口服给药的,不采用注射给药;能肌内注射给药的,不选用静脉注射 或滴注给药。 6.使用中药注射剂还应做到: (1)用药前应仔细询问过敏史,对过敏体质者应慎用。 (2)严格按照药品说明书规定的功能主治使用,辨证施药,禁止超功能主治用药。 (3)中药注射剂应按照药品说明书推荐的剂量、调配要求、给药速度和疗程使用药品,不超剂量、过快滴注和长期连续用药。 (4)中药注射剂应单独使用,严禁混合配伍,谨慎联合用药。对长期使用的,在每疗程间要有一定的时间间隔。 (5)加强用药监护。用药过程中应密切观察用药反应,发现异常,立即停药,必要时采取积极救治措施;尤其对老人、儿童、肝肾功能异常等特殊人群和初次使用中药注射剂的患者应慎重使用,加强监测。 二、联合用药原则 (一)中成药的联合使用 1.当疾病复杂,一个中成药不能满足所有证候时,可以联合应用多种中成药。 2.多种中成药的联合应用,应遵循药效互补原则及增效减毒原则。功能相同或基本相同的中成药原则上不宜叠加使用。 3.药性峻烈的或含毒性成分的药物应避免重复使用。 4.合并用药时,注意中成药的各药味、各成分间的配伍禁忌。 5.一些病证可采用中成药的内服与外用药联合使用。 中药注射剂联合使用时,还应遵循以下原则: 两种以上中药注射剂联合使用,应遵循主治功放互补及增放减毒原则,符合中医传统配伍理论的要求,无配伍禁忌。
●中成药安全性 ●中成药的历史悠久,应用广泛,大量研究和临床实践表明,在合理使用的情况下, 中成药的安全性是较高的。合理使用包括正确的辨证选药、用法用量、使用疗程、禁忌症、合并用药等多方面,其中任何环节有问题都可能引发药物不良事件。合理用药是中成药应用安全的重要保证。 ●药物的两重性是药物作用的基本规律之一,中成药也不例外,中成药既能起到防病 治病的作用,也可引起不良反应。 ● 1.中成药使用中出现不良反应的主要原因 ●(1)中药自身的药理作用或所含毒性成分引起的不良反应; ●(2)特异性体质对某些药物的不耐受、过敏等; ●(3)方药证候不符,如辨证不当或适应证把握不准确; ●(4)长期或超剂量用药,特别是含有毒性中药材的中成药,如朱砂、雄黄、蟾酥、 附子、川乌、草乌、北豆根等,过量服用即可中毒; ●(5)不适当的中药或中西药的联合应用。 ● 2.中成药使用中出现的不良反应 有多种类型 ●临床可见以消化系统症状、皮肤粘膜系统症状、泌尿系统症状、神经系统症状、循 环系统症状、呼吸系统症状、血液系统症状、精神症状或过敏性休克等为主要表现的不良反应,可表现为其中一种或几种症状。 ● 3.临床上预防中成药不良反应,要注意以下几个方面: ●(1)加强用药观察及中药不良反应监测,完善中药不良反应报告制度。 ●(2)注意药物过敏史。对有药物过敏史的患者应密切观察其服药后的反应,如有 过敏反应,应及时处理,以防止发生严重后果。 ●(3)辨证用药,采用合理的剂量和疗程。尤其是对特殊人群,如婴幼儿、老年人、 孕妇以及原有脏器损害功能不全的患者,更应注意用药方案。 ●(4)注意药物间的相互作用,中、西药并用时尤其要注意避免因药物之间相互作 用而可能引起的不良反应。 ●(5)需长期服药的患者要加强安全性指标的监测。 ●一、中成药临床应用基本原则(1) ● 1.辨证用药 ●依据中医理论,辨认、分析疾病的证候,针对证候确定具体治法,依据治法,选定 适宜的中成药。 ● 2.辨病辨证结合用药 ●辨病用药是针对中医的疾病或西医诊断明确的疾病,根据疾病特点选用相应的中成 药。临床使用中成药时,可将中医辨证与中医辨病相结合、西医辨病与中医辨证相结合,选用相应的中成药,但不能仅根据西医诊断选用中成药。 ●一、中成药临床应用基本原则(2) ● 3.剂型的选择 ●应根据患者的体质强弱、病情轻重缓急及各种剂型的特点,选择适宜的剂型。 ● 4.使用剂量的确定对于有明确使用剂量的,慎重超剂量使用。有使用剂量范围的 中成药,老年人使用剂量应取偏小值。 ●一、中成药临床应用基本原则(3) ● 5.合理选择给药途径能口服给药的,不采用注射给药;能肌内注射给药的,不选 用静脉注射或滴注给药。 ● 6.使用中药注射剂还应做到:
药物I期临床试验管理指导原则(试行) 第一章总则 第一条为加强药物I期临床试验(以下简称I期试验)的管理,有效地保障受试者的权益与安全,提高I期试验的研究质量与管理水平,根据《中华人民共和国药品管理法》、《药品注册管理办法》、《药物临床试验质量管理规范》等相关规定,参照国际通行规范,制定本指导原则。 第二条本指导原则适用于I期试验,旨在为I期试验的组织管理和实施提供指导。人体生物利用度或生物等效性试验应参照本指导原则。 第二章职责要求 第三条申办者应建立评价药物临床试验机构的程序和标准,选择、委托获得资格认定的I期试验研究室进行I期试验。 第四条申办者应建立质量保证体系,对I 期试验的全过程进行监查和稽查,确保临床试验的质量,保障受试者的权益与安全。 第五条申办者可以委托合同研究组织(CRO执行I期试验中的某些工作和任务。委托前对合同研究组织的研究条件、能力、经验以及相应的质量管理体系进行评价。当合同研究组织接受了委托,则本指导原则中规定的由申办者履行的责任,合同研究组织应同样履行。申办者对临床试验的真实性及质量负最终责任。 第六条I期试验研究室负责I期试验的实施。研究者应遵循临床试验相关法律法规、规范性文件和技术指导原则,执行临床试验方案,保护受试者的权益与安全,保证临床试验结果的真实可靠。 第七条药物临床试验生物样本分析应在符合《药物临床试验生物样本分析实验室管理指南》(以下简称《实验室管理指南》)的实验室进行。从事药物临床试验生物样本分析的实验室均应接受药品监督管理部门的监督检查。 第八条伦理委员会应针对I期试验的特点,加强对受试者权益与安全的保护,重点关注:试验风险的管理与控制,试验方案设计和知情同意书的内容,研究团队的人员组成、资 质、经验,受试者的来源、招募方式,实施过程中发生的意外情况等。 第三章实施条件 第九条I期试验研究室应设有足够的试验病房,也可以设有临床试验生物样本分析实 验室(以下简称实验室)。试验病房应符合本指导原则的要求,实验室应符合《实验室管理指南》的要求。均应具备相应的组织管理体系、质量管理体系及能满足I 期试验需要的场所和设施设备等。 第十条I 期试验研究室应配备研究室负责人、主要研究者、研究医生、药师、研究护士及其他工作人员。所有人员应具备与承担工作相适应的专业特长、资质和能力。实验室人员应符合《实验室管理指南》的要求。 (一)研究室负责人。研究室负责人总体负责I 期试验的管理工作,保障受试者的权益 与安全。研究室负责人应具备医学或药学本科以上学历并具有高级职称,具有5 年以上药物 临床试验实践和管理经验,组织过多项I期试验。 (二)主要研究者。研究室负责人和主要研究者可以是同一人。主要研究者负责I 期试 验的全过程管理,熟悉与临床试验有关的资料与文献,确保试验顺利进行。主要研究者应具备医学或药学本科或以上学历、高级技术职称,具有系统的临床药理专业知识,至少5 年以 上药物临床试验经验,有负责过多项I期试验的经历。 (三)研究医生。研究医生协助主要研究者进行医学观察和不良事件的监测与处置。研究医生应具备执业医师资格,具有医学本科或以上学历,有参与药物临床试验的经历,具备急诊和急救等方面的能力。
抗肿瘤药物临床试验技术指导原则 一、概述 恶性肿瘤是严重威胁人类生命的一类疾病,尽管现有治疗手段取得了一定疗效,但多数肿瘤患者生存时间有限,缺乏有效的可以治愈的药物,亟需开发新的药物来满足需要。在抗肿瘤药物的风险效益评估中,医护人员和患者可能愿意承受相对较大的安全性风险,所以抗肿瘤药物的临床研究除遵循一般药物临床研究原则外,还应考虑其特殊性。由于肿瘤生物学研究的进展,一些新的作用机制、作用靶点的抗肿瘤药物不断涌现,呈现出不同于以往传统细胞毒类药物的安全性和有效性特点;肿瘤疾病的药物治疗也从以往的单纯追求肿瘤缩小向延长患者的生存期、提高生存质量转变,这些改变使抗肿瘤药物临床疗效评价终点指标也出现较大改变。因此,传统的抗肿瘤药物开发模式已经变得不适宜,需要更多地探索能加快和促进开发进程的临床研究策略。 本指导原则将对抗肿瘤药物临床研究一般考虑进行阐述,重点阐述在不同临床研究阶段中需要重点考虑的问题,旨在为抗肿瘤药物临床研究的设计、实施和评价提供方法学指导。申请人在进行临床研究时,还应当参照国家食品药品监督管理局(以下简称SFDA)既往发布的相关指导原则和《药物临床试验质量管理规范》(GCP)要求进行,对于一般药物临床研究需要遵从的原则以及与其他指导原则重复内容在本文中不再赘述。 本指导原则主要适用于抗肿瘤新化合物的临床研究,抗肿瘤生物制品也可参考部分内容,不适用于中药制剂。药物类别上主要针对细胞毒
类抗肿瘤药物临床研究,由于非细胞毒类药物(如信号传导抑制剂,生物反应调节剂,激素类等)是目前新药开发的主要方向,本指导原则也将尽可能对此类别药物临床研究的不同之处进行阐述。 本指导原则中的观点仅代表SFDA当前对抗肿瘤药物临床研究的一般性认识,不能涵盖在新药研发中遇到的所有情况,申请人在研究中应始终坚持具体问题具体分析的原则。尤其应注意的是,抗肿瘤药物研究理论和技术的快速发展,很可能对将来抗肿瘤药物开发模式产生影响,因此申请人可以积极探索更为科学合理的研究方法,并及时寻求SFDA 药品注册部门的建议。 二、临床研究的总体考虑 抗肿瘤药物的临床研究过程通常分为Ⅰ期、Ⅱ期和Ⅲ期临床试验。Ⅰ期临床试验主要目的是对药物的耐受性、药代动力学进行初步研究,为后期研究给药方案的设计提供数据支持;Ⅱ期临床试验主要是探索性的研究,如给药剂量探索、给药方案探索、瘤肿有效性探索等,同时也观察安全性;Ⅲ期临床试验则在Ⅱ期基础上进一步确证肿瘤患者临床获益情况,为获得上市许可提供足够证据。 需要指出,这种临床研究的分期并不是固定的开发顺序。在本指导原则中,尽管对Ⅰ、Ⅱ期探索性试验和Ⅲ期确证性试验区别对待,但统计假设的建立和检验也可以成为Ⅱ期临床试验的一部分,同样,部分探索性研究也可能成为Ⅲ期临床试验的一部分。 由于Ⅲ期临床试验需要提供生存获益的疗效数据,试验周期较长,因此可以采用探索的开发模式,按照预定的中期分析计划,依据不断积累的信息,对临床试验方案进行调整。
《中成药临床应用指导原则》 为加强中成药临床应用管理,提高中成药应用水平,保证临床用药安全,国家中医药管理局会同有关部门组织专家制定了《中成药临床应用指导原则》(以下简称《指导原则》)。《指导原则》由四部分组成,第一部分为中成药概述;第二部分为中成药临床应用基本原则;第三部分为各类中成药的特点、适应证及注意事项;第四部分为中成药临床应用的管理。 《指导原则》是为适应中成药临床应用管理需要而制定的,是临床应用中成药的基本原则。每种中成药临床应用的具体要求,还应以药品说明书、最新版本的《中华人民共和国药典》、《中华人民共和国药典-临床用药须知-中药卷》为准。在医疗工作中,临床医师应遵循中医基础理论,根据患者实际情况,选用适宜的药物,辨证辨病施治。 第三部分各论中为更好地说明各类中成药的特点,列举了部分中成药,列举的药物是《国家基本药物目录》中的药物和《国家基本药物目录》未包括但又属临床常用的中成药。 中药注射剂的临床应用及使用管理,《指导原则》提出了具体要求,同时还应遵照《卫生部关于进一步加强中药注射剂生产和临床使用管理的通知》(卫医政发〔2008〕71号)执行。第一部分中成药概述 中成药是在中医药理论指导下,以中药饮片为原料,按规定的处 方和标准制成具有一定规格的剂型,可直接用于防治疾病的制剂。中成药有着悠久的历史,应用广泛,在防病治病、保障人民群众健康方面发挥了重要作用。 中成药的处方是根据中医理论,针对某种病证或症状制定的,因此使用时要依据中医理论辨证选药,或辨病辨证结合选药。
中成药具有特定的名称和剂型,在标签和说明书上注明了批准文号、品名、规格、处方成分、功效和适应证、用法用量、禁忌、注意事项、生产批号、有效期等内容。相对于中药汤剂来说,中成药无需煎煮,可直接使用,尤其方便急危病症患者的治疗及需要长期治疗的患者使用,且体积小,有特定的包装,存贮、携带方便。 一、中成药的常用剂型 中成药剂型种类繁多,是我国历代医药学家长期实践的经验总结,近几十年,中成药剂型的基础研究取得了较大进展,研制开发了大量新剂型,进一步扩大了中成药的使用范围。 中成药的剂型不同,使用后产生的疗效、持续的时间、作用的特点会有所不同。因此,正确选用中成药应首先了解中成药的常用剂型。 (一)固体制剂 固体剂型是中成药的常用剂型,其制剂稳定,携带和使用方便。 1.散剂系指药材或药材提取物经粉碎、均匀混合而制成的粉末状制剂,分为内服散剂和外用散剂。散剂粉末颗粒的粒径小,容易分散,起效快。外用散剂的覆盖面积大,可同时发挥保护和收敛作用。散剂制备工艺简单,剂量易于控制,便于婴幼儿服用。但也应注意散 剂由于分散度大而造成的吸湿性、化学活性、气味、刺激性等方面的影响。 2.颗粒剂系指药材的提取物与适宜的辅料或药材细粉制成具有一定粒度的颗粒状剂型。颗粒剂既保持了汤剂作用迅速的特点,又克服了汤剂临用时煎煮不便的缺点,且口味较好、体积小,但易吸潮。根据辅料不同,可分为无糖颗粒剂型和有糖颗粒剂型,近年来无糖颗粒剂型的品种逐渐增多。
药物Ⅰ期临床试验管理指导原则(试行) 第一章总则 第一条为加强药物Ⅰ期临床试验(以下简称I期试验)的管理,有效地保障受试者的权益与安全,提高Ⅰ期试验的研究质量与管理水平,根据《中华人民共和国药品管理法》、《药品注册管理办法》、《药物临床试验质量管理规范》等相关规定,参照国际通行规范,制定本指导原则。 第二条本指导原则适用于Ⅰ期试验,旨在为Ⅰ期试验的组织管理和实施提供指导。人体生物利用度或生物等效性试验应参照本指导原则。 第二章职责要求 第三条申办者应建立评价药物临床试验机构的程序和标准,选择、委托获得资格认定的I期试验研究室进行Ⅰ期试验。 第四条申办者应建立质量保证体系,对I期试验的全过程进行监查和稽查,确保临床试验的质量,保障受试者的权益与安全。 第五条申办者可以委托合同研究组织(CRO)执行I期试验中的某些工作和任务。委托前对合同研究组织的研究条件、能力、经验以及相应的质量管理体系进行评价。当合同研究组织接受了委托,则本指导原则中规定的由申办者履行的责任,合同研究组织应同样履行。申办者对临床试验的真实性及质量负最终责任。
第六条Ⅰ期试验研究室负责Ⅰ期试验的实施。研究者应遵循临床试验相关法律法规、规范性文件和技术指导原则,执行临床试验方案,保护受试者的权益与安全,保证临床试验结果的真实可靠。 第七条药物临床试验生物样本分析应在符合《药物临床试验生物样本分析实验室管理指南》(以下简称《实验室管理指南》)的实验室进行。从事药物临床试验生物样本分析的实验室均应接受药品监督管理部门的监督检查。 第八条伦理委员会应针对Ⅰ期试验的特点,加强对受试者权益与安全的保护,重点关注:试验风险的管理与控制,试验方案设计和知情同意书的内容,研究团队的人员组成、资质、经验,受试者的来源、招募方式,实施过程中发生的意外情况等。 第三章实施条件 第九条Ⅰ期试验研究室应设有足够的试验病房,也可以设有临床试验生物样本分析实验室(以下简称实验室)。试验病房应符合本指导原则的要求,实验室应符合《实验室管理指南》的要求。均应具备相应的组织管理体系、质量管理体系及能满足I期试验需要的场所和设施设备等。 第十条I期试验研究室应配备研究室负责人、主要研究者、研究医生、药师、研究护士及其他工作人员。所有人员应具备与承担工作相适应的专业特长、资质和能力。实验室人员应符合《实验室管理指南》的要求。 (一)研究室负责人。研究室负责人总体负责I期试验的管理工作,保障受试者的权益与安全。研究室负责人应具备医学或药学本科以上学历并具有高级职称,具有5年以上药
中成药临床应用指导原则
目录 前言 (2) 第一部分中成药概述 (3) 一、中成药的剂型 (3) 二、中成药分类 (4) 三、中成药安全性 (5) 第二部分中成药临床应用原则 (6) 一、中成药临床应用基本原则 (6) 二、联合用药原则 (6) 三、孕妇使用中成药的基本原则 (7) 四、儿童使用中成药的基本原则 (7) 第三部分各论 (8) 一、解表剂 (8) 二、泻下剂 (8) 三、和解剂 (8) 四、清热剂 (9) 五、祛暑剂 (9) 六、温里剂 (9) 七、表里双解剂 (10) 八、补益剂 (10) 九、安神剂 (10) 十、开窍剂 (11) 十一、固涩剂 (11) 十二、理气剂 (11) 十三、理血剂 (12) 十四、治风剂 (12) 十五、治燥剂 (12) 十六、祛湿剂 (13) 十七、祛痰剂 (13) 十八、止咳平喘剂 (13) 十九、消导化积剂 (14) 二十、杀虫剂 (14) 第四部分中成药临床应用的管理 (15) 一、含毒性中药材的中成药临床应用的管理 (15) 二、中成药不良反应的监测 (15) 三、开展中成药临床应用监测、建立中成药应用点评制度 (15)
前言 为加强中成药临床应用管理,提高中成药应用水平,保证临床用药安全,国家中医药管理局会同有关部门组织专家制定了《中成药临床应用指导原则》(以下简称《指导原则》)。《指导原则》由四部分组成,第一部分为中成药概述;第二部分为中成药临床应用基本原则;第三部分为各类中成药的特点、适应证及注意事项;第四部分为中成药临床应用的管理。 《指导原则》是为适应中成药临床应用管理需要而制定的,是临床应用中成药的基本原则。每种中成药临床应用的具体要求,还应以药品说明书、最新版本的《中华人民共和国药典》、《中华人民共和国药典-临床用药须知-中药卷》为准。在医疗工作中,临床医师应遵循中医基础理论,根据患者实际情况,选用适宜的药物,辨证辨病施治。 第三部分各论中为更好地说明各类中成药的特点,列举了部分中成药,列举的药物是《国家基本药物目录》中的药物和《国家基本药物目录》未包括但又属临床常用的中成药。 中药注射剂的临床应用及使用管理,《指导原则》提出了具体要求,同时还应遵照《卫生部关于进一步加强中药注射剂生产和临床使用管理的通知》(卫医政发…2008?71号)执行。
新药I 期临床试验申请技术指南 (草案) 国家食品药品监督管理总局(CFDA) 2016年9月
目录 一、前言 (1) 二、背景 (2) 三、与药审中心沟通交流 (3) 四、IND提交所需的特定信息 (4) (一)规定的表格 (4) (二)文件目录 (4) (三)介绍性说明和总体研究计划 (5) (四)研究者手册 (6) (五)方案 (8) (六)化学、生产和控制信息 (9) (七)药理毒理信息 (13) (八)研究药物既往在人体使用的经验 (16) (九)其他重要信息 (16) (十)相关信息 (17) 五、提交信息 (17) 六、IND过程和审评过程 (17) (一)临床试验暂停要求 (19) (二)IND修订 (20) 七、申请人的其他责任 (21)
(一)遵守法规伦理要求 (21) (二)监测正在进行的研究 (22) (三)研究药物的推销或付费 (22) (四)记录和报告 (22) (五)IND安全性报告 (22) (六)IND年度报告 (23) 八、撤回、终止、暂停或者重新启动IND (24) 附件 (26) 附件1:药品注册临床试验申报资料信息表 (26) 附件2:研究者声明表 (29) 附件3: 化药Ⅰ期临床研究CMC资料表 (32)
新药I期临床试验申请技术指南 一、前言 国家食品药品监督管理总局(CFDA)发布本技术指南旨在帮助新药研发申请人提交足够的临床试验研究申请(Investigational new drug,IND)材料,以提高新药研发与审评效率,并同时能保证药品的安全性、有效性和质量可控性。 本指导原则阐述了在中国将研究药品(包括已进行结构确证的治疗性生物工程类产品)开始用于人体研究时,所需要提供的数据。将申报资料的要求按照新药不同的研究阶段加以分类,在满足向CFDA提供评估拟进行研究所需要数据的同时,建立对同一类别IND申报的统一标准,增加IND申报要求的透明度、标准化,减少模糊性和不一致性,将有助于缩短新药批准进入临床试验的时间。 本指导原则的目的是:(1)针对I期临床试验确保有充足的数据提交给监管机构,以评价拟进行的临床研究的安全性和可行性;(2)结合IND阶段的沟通交流制度,优化IND申报流程。(3)通过规I期临床资料的数据要求,加快新药研发。通过优化申报流程与细化申报资料标准,本技术指南将促进申请人成功地提交IND。
附件 兽用中药、天然药物临床试验技术指导原则等 5个技术指导原则 兽用中药、天然药物临床试验技术指导原则 一、概述 临床试验是指在一定控制条件下科学地考察和评价兽药治疗或预防靶动物特定疾病或证候的有效性和安全性的过程。充分、可靠的临床研究数据是证明所申报产品安全性和有效性的依据。 兽用中药、天然药物的研制过程,与西兽药相比,既有相同点,也有其特殊性。首先,中药新药的发现或立题,多来源于临床的直接观察及经验获得的提示;其次,中药内在成分及其相互作用的复杂性致使其药学、药效及毒理的研究面临更多的困难;再者,影响研究结论客观性和准确性的因素也相对较多。因此,临床试验对中药有效性和安全性的评价具有更加特殊的意义。 为了保证兽用中药、天然药物临床试验结论的确实可靠,规范临床研究行为,根据《兽药注册办法》和《新兽药研制管理办法》制定本指导原则。本指导原则旨在阐述兽用中药、天然药物临床试验设计和实施过程中应把握的一般性原则及关键性问题,为兽用中药、天然药物新产品研发提供技术指导。 二、兽用中药、天然药物临床试验的基本内容 根据试验目的的不同,兽用中药、天然药物的临床试验一般包括靶动物安全性试验、实验性临床试验和扩大临床试验。申请注册新兽药时,应根据注册分类的要求和具体情况的需要,进行一项或多项临床试验。 (一)靶动物安全性试验 靶动物安全性试验是观察不同剂量受试兽药作用于靶动物后从有效作用到毒性作用,甚至到致死作用的动态变化的过程。该试验旨在考察受试兽药使用于靶动物的安全性及安全剂量范围,为进一步临床试验给药方案的制定提供依据。 (二)实验性临床试验 实验性临床试验是以符合目标适应证的自然病例或人工发病的试验动物为研究对象,确证受试兽药对靶动物目标适应证的有效性及安全性,同时为扩大临床试验合理给药剂量及给药方案的确定提供依据。实验性临床试验的目的在于对新兽药临床疗效进行确证,保证研究结论的客观性和准确性。 (三)扩大临床试验 扩大临床试验是对受试兽药临床疗效和安全性的进一步验证,一般应以自然发病的动物作为研究对象。 三、兽用中药、天然药物临床试验的共性要求 (一)以中兽医学理论为指导 中药用于防治动物疾病及提高生产性能有着悠久的历史,并已形成了一套完整的理论体系。基于对生命活动规律和疾病发生学的整体观,中兽医学对疾病的治疗通常立足于通过调节脏腑、经络、气血等机能建立机体内环境的稳态,维持机体气机出入升降、功能活动的有序性,提高机体对外环境的适应能力。因此,中药的特点和优势在于“整体调节",这与化学药品“对抗疗法”有着本质的不同。 兽用中药、天然药物临床试验中评定治疗结局指标的确立,不应只从单纯生物医学模式出发,仅着眼于外来致病因子,或生物学发病机理的微观改变和局部征象,而应从整体水平上选择与功能状态、证候相关的多维结局指标。在中药临床试验设计时,将治疗效能定位于对病因或某一疾病环节的直接对抗,或仅仅对用药后短期内的死亡率等极少指标的考察,显
业务学习培训2016年3月25日 中成药临床应用指导原则 第二部分中成药临床应用原则 一、中成药临床应用基本原则 1.辨证用药依据中医理论,辨认、分析疾病的证候,针对证候确定具体治法,依据治法,选定适宜的中成药。 2.辨病辨证结合用药辨病用药是针对中医的疾病或西医诊断明确的疾病,根据疾病特点选用相应的中成药。临床使用中成药时,可将中医辨证与中医辨病相结合、西医辨病与中医辨证相结合,选用相应的中成药,但不能仅根据西医诊断选用中成药。 3.剂型的选择应根据患者的体质强弱、病情轻重缓急及各种剂型的特点,选择适宜的剂型。 4.使用剂量的确定对于有明确使用剂量的,慎重超剂量使用。有使用剂量范围的中成药,老年人使用剂量应取偏小值。 5.合理选择给药途径能口服给药的,不采用注射给药;能肌内注射给药的,不选用静脉注射或滴注给药。 6.使用中药注射剂还应做到: (1)用药前应仔细询问过敏史,对过敏体质者应慎用。 (2)严格按照药品说明书规定的功能主治使用,辨证施药,禁止超功能主治用药。 (3)中药注射剂应按照药品说明书推荐的剂量、调配要求、给药速度和疗程使用药品,不超剂量、过快滴注和长期连续用药。 (4)中药注射剂应单独使用,严禁混合配伍,谨慎联合用药。对长期使用的,在每疗程间要有一定的时间间隔。 (5)加强用药监护。用药过程中应密切观察用药反应,发现异常,立即停药,必要时采取积极救治措施;尤其对老人、儿童、肝肾功能异常等特殊人群和初次使用中药注射剂的患者应慎重使用,加强监测。 二、联合用药原则 (一)中成药的联合使用 1.当疾病复杂,一个中成药不能满足所有证候时,可以联合应用多种中成药。 2.多种中成药的联合应用,应遵循药效互补原则及增效减毒原则。功能相同或基本相同的中成药原则上不宜叠加使用。 3.药性峻烈的或含毒性成分的药物应避免重复使用。 4.合并用药时,注意中成药的各药味、各成分间的配伍禁忌。 5.一些病证可采用中成药的内服与外用药联合使用。 中药注射剂联合使用时,还应遵循以下原则: 1.两种以上中药注射剂联合使用,应遵循主治功效互补及增效减毒原则,符合中医传统配伍理论的要求,无配伍禁忌。 2.谨慎联合用药,如确需联合使用时,应谨慎考虑中药注射剂的间隔时间以及药物相互作用等问题。
医疗器械临床试验设计指导原则 (征求意见稿) 二〇一七年十一月
目录 一、适用范围 ..................... 错误!未定义书签。 二、临床试验的开展原则 ........... 错误!未定义书签。 三、医疗器械临床试验的设计原则和特点错误!未定义书签。(一)临床试验目的 ............... 错误!未定义书签。(二)器械临床试验设计需考虑的特殊因素错误!未定义书签。 1.器械的工作原理 ................ 错误!未定义书签。2.使用者技术水平和培训 .......... 错误!未定义书签。3.学习曲线 ...................... 错误!未定义书签。4.人为因素 ...................... 错误!未定义书签。(三)临床试验设计的基本类型和特点错误!未定义书签。1.平行对照设计 ................... 错误!未定义书签。(1)随机化 ...................... 错误!未定义书签。(2)盲法 ........................ 错误!未定义书签。(3)对照 ........................ 错误!未定义书签。 2.配对设计 ....................... 错误!未定义书签。 3.交叉设计 ....................... 错误!未定义书签。 4.单组设计 ....................... 错误!未定义书签。(1)与OPC比较 .................. 错误!未定义书签。(2)与PG比较 ................... 错误!未定义书签。
附件 体外诊断试剂临床试验技术指导原则 一、概述 体外诊断试剂的临床试验(包括与已上市产品进行的比较研究试验)是指在相应的临床环境中,对体外诊断试剂的临床性能进行的系统性研究。 申请人应在符合要求的临床单位,在满足临床试验最低样本量要求的前提下,根据产品临床预期用途、相关疾病的流行率和统计学要求,制定能够证明其临床性能的临床试验方案,同时最大限度地控制试验误差、提高试验质量并对试验结果进行科学合理的分析。临床试验报告是对临床试验过程、结果的总结,是评价拟上市产品有效性和安全性的重要依据,是产品注册所需的重要文件之一。 本指导原则仅对体外诊断试剂临床试验提出了一般性的要求。由于体外诊断试剂产品具有发展快、专业跨度大、临床预期用途各异的特点,不同临床预期用途产品的临床试验方法及内容不尽相同。申请人应根据产品特点及临床预期用途,制定合理的临床试验方案。国家食品药品监督管理总局也将根据体外诊断试剂发展的需要,适时修订本指导原则。 二、临床试验的基本原则 (一)基本要求 1.临床试验必须符合赫尔辛基宣言的伦理学准则,必须获得临床试验机构伦理委员会的同意。研究者应考虑临床试验用样本,如血液、羊水、胸水、腹水、组织液、胸积液、组织切片、骨髓等的获得或试验结果对受试者的风险性,应提交伦理委员会的审查意见及受试者的知情同意书。对于例外情况,如客观上不可能获得受试者的知情同意或该临床试验对受试者几乎没有风险,可经伦理委员会审查和批准后免于受试者的知情同意。 2.受试者的权益、安全和健康必须高于科学和社会利益。 3.为受试者保密,尊重个人隐私。防止受试者因检测结果而受到歧视或伤害。 4.临床前研究结果支持进行临床试验。 (二)临床试验机构及人员的要求 1. 第三类体外诊断试剂申请人应当选定不少于3家(含3家)、第二类体外诊断试剂申请人应当选定不少于2家(含2家)临床试验机构,按照有关规定开展临床试验。 2.体外诊断试剂的临床试验机构应获得国家食品药品监督管理总局资质认可。 3.申请人应根据产品特点及其预期用途,综合不同地区人种、流行病学背景、病原微生物的特性等因素选择临床试验机构。临床试验机构必须具有与试验用体外诊断试剂相适应的专业技术人员及仪器设备,并能够确保该项试验的实施。 4. 申请人应当在临床试验前制定文件明确各方的职责分工,与各临床试验机构协商制定统一的临床试验方案,按照临床试验方案组织制定标准操作规程,并组织对参加试验的所有研究者进行临床试验方案和试验用体外诊断试剂使用的培训,以确保临床试验方案和试验用体外诊断试剂操作的一致性,并在临床试验过程中促进各研究者之间的沟通。 5.在临床试验开始前,申请人应与临床试验工作人员进行临床试验的预试验,