重叠综合征诊断和治疗-天津医科大学总医院-王邦茂共86页PPT资料
- 格式:ppt
- 大小:1.89 MB
- 文档页数:80
2024自身免疫性肝病重叠综合征的诊断和治疗肝脏的自身免疫性疾病主要包括自身免疫性肝炎(AlH)、原发性胆汁性胆管炎(PB原发性硬化性胆管炎(PSC)。
AlH是一种由针对肝细胞的自身免疫反应所介导的肝脏实质炎症以血清自身抗体阳性、高免疫球蛋白G(IgG)血症和/或Y-球蛋白血症、界面性肝炎等为特点,如不治疗常可导致肝硬化[1]oPBC是一种慢性炎症性自身免疫性胆汁淤积性肝病,以血清抗线粒体抗体(AMA)阳性、碱性磷酸酶(ALP)升高和非化脓性胆管炎为特征,部分患者也表现为AMA阴性/或抗sp100、gp210抗体阳性,晚期PBC可导致肝硬化和肝功能衰竭[2]。
PSC是一种以肝内和/或肝外胆管损伤为特征的慢性胆汁淤积性肝病,可导致胆管狭窄、胆汁淤积,最终是胆汁性肝硬化并伴有终末期肝病[3]。
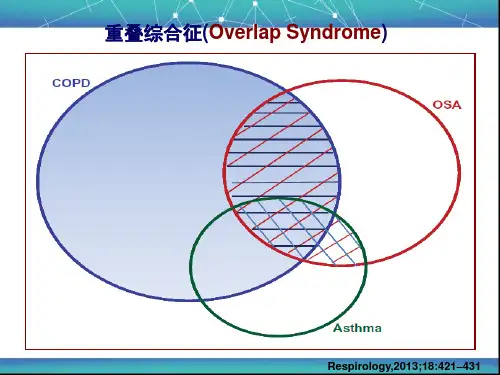
上述任何两种疾病的特征同时或连续出现称为重叠综合征其中以AIH-PBC重叠最常见。
AIH-PBC会快速进展为肝硬化,随后是肝功能衰竭,并且预后较差[4]。
但是对该疾病仍缺乏规范的诊断和治疗标准,因此,对于自身免疫性肝病重叠综合征的研究非常重要。
1、A IH-PBC1.1流行病学AIH以女性多见,男女比为1:4~1:6o发病年龄主要在50~60岁,在欧洲国家,AIH的时点患病率为10-25/10万人,新西兰2014—2016年的患病率为2.39/10万人,2016年日本的时点患病率为23.9/10万人[5]o我国一项包含1020例AIH患者的单中心回顾性观察研究⑹显示,AIH患者的峰值年龄为55(6~82)岁,男女比为1:5o PBC多见于50岁以上的女性,在丹麦,男女比约1:4.2,美国约为1:5.4,PBC的患病率为1.91~40∙2∕10万人,以北美和北欧国家最高。
我国尚缺乏基于人群的PBC流行病学数据具有AIH 特征的PBC是自身免疫性肝病中最常见的重叠形式,患病率为所有PBC患者的5%~15%o同样,在确诊为AIH的患者中,5.35%的患者也能检测到AMA[11]。

25 Efficacy of Noninvasive MechanicalVentilation in Obese Patients withChronic Respiratory FailureP.Piesiak,A.Brzecka,M.Kosacka,and R.JankowskaAbstractChronic respiratory failure(CRF)develops in a minority of obesepatients.Noninvasive mechanical ventilation(NIMV)is a new optionaltreatment for such patients.The aim of this study was to evaluate theeffectiveness of NIMV in obese patients with CRF.The material of thestudy consisted of34obese patients(body mass index47.3Æ7.9kg/m2)with CRF(PaO2¼6.40Æ0.93kPa and PaCO2¼8.67Æ2.13kPa)who were hypoxemic despite an optimal therapy.Thirteen patients hadan overlap syndrome(OS)–chronic obstructive pulmonary disease(COPD)coexisting with obstructive sleep apnea syndrome(OSAS)and21patients had obesity-hypoventilation syndrome(OHS).Ventilationparameters were determined during polysomnography.The efficacy ofNIMV was evaluated on thefifth day and after1year’s home treatment.We observed a significant increase in the mean blood oxygen saturationduring sleep in all patients;the increase was greater in patients with OHS(92.6Æ1.4%)than in patients with OS(90.4Æ1.8%).There was asignificant improvement of diurnal PaO2and PaCO2on thefifth day ofNIMV(mean PaO2increase2.1kPa and PaCO2decrease0.9kPa)andalso after1year of home NIMV(mean PaO2increase1.9kPa and PaCO2decrease2.4kPa).Only one patient stopped treatment because of lack oftolerance during the observation period(1–3years).In conclusion,NIMVis an effective and well tolerated treatment option in obese patients withCRF resulting in a rapid relief of respiratory disorders during sleep and agradual,long-term improvement of gas exchange during the day,particu-larly in patients with OHS.P.Piesiak(*) A.Brzecka M.Kosacka R.JankowskaDepartment of Pulmonology and Lung Cancer,WroclawMedical University,105Grabiszynska St.,Wroclaw,Polande-mail:ppiesiak@tlen.pl167M.Pokorski(ed.),Neurobiology of Respiration,Advances in Experimental Medicine and Biology788,DOI10.1007/978-94-007-6627-3_25,#Springer Science+Business Media Dordrecht2013KeywordsChronic respiratory failure Chronic obstructive pulmonary disease (COPD) Noninvasive mechanical ventilation(NIMV) Obesity Obesity-hypoventilation syndrome(OHS) Obstructive sleep apnea syndrome Overlap syndrome Polysomnography1IntroductionObesity is a social problem,reported globally. Current data suggests that the amount of persons in the highest body mass index(BMI)groups (>40kg/m2)is increasing at rates two and three times faster than those with a BMI of30kg/m2 (Sturm2007).Obesity affects significantly the respiratory system,decreasing lung volumes, increasing work of breathing,affecting respiratory muscle function and ventilatory control(Steier et al.2009).Most of the obese are able to maintain awake eucapnia,but some of them develop chronic respiratory failure(CRF).It is usually due to the chronic alveolar hypoventilation that causes an increase of arterial partial pressure of carbon diox-ide(PaCO2)above6kPa.This is usually a conse-quence of obstructive sleep apnea syndrome (OSAS)and/or obesity-hypoventilation syndrome (OHS)(Borel et al.2011;Leech et al.1991).Noninvasive mechanical ventilation(NIMV) used for home mechanical ventilation is a well-established and increasingly used therapeutic option for patients with chronic hypercapnic respiratory failure due to chronic obstructive pul-monary disease(COPD),neuromuscular or rib cage diseases(Lloyd-Owen et al.2005;Simonds 2003;Mehta and Hill2001;American College of Chest Physicians1999).There are few data presenting the effects of NIMV therapy in severe obese patients with CRF especially in a long period of time(Perez de Llano et al.2005; Janssens et al.2003).Therefore,the aim of this study was to evaluate the effectiveness of NIMV in obese patients with chronic alveolar hypoventilation in a short and long period of time.2MethodsThe study was approved by the Ethics Commit-tee of Wroclaw Medical University and writteninformed consent was obtained from all studypatients.2.1Patients and DiagnosesThe studied group consisted of34severely obesepatients of the mean age55Æ11years and BMI47.3Æ7.9kg/m2(F/M11/23)admitted to theDepartment of Pulmonology and Lung Cancer,Medical University of Wroclaw in a period of2008–2012.The patients were assessed either forstable chronic respiratory failure or treated fol-lowing an episode of acute decompensated respi-ratory failure.Study inclusion criteria wereBMI>30kg/m2;daytime stable respiratoryfailure with PaCO2>6kPa;hypoxemia despite optimal therapy,including oxygen therapy orCPAP(continuous positive airway pressure).The exclusion criterion was an inability to pro-vide written informed consent.Thefinal diagnoses of the studied34individuals are shown in Fig.25.1.We diagnosedCOPD with OSAS in13patients(overlapsyndrome-OS)and OHS in21patients.In thegroup of OHS patients,14of them had coexistingOSAS(OHS+OSA).According to Mokhlesi(2010)OHS was defined as a combination ofobesity(BMI!30kg/m2),daytime hypercapnia(PCO2!6kPa),and various types of sleep-disordered breathing after ruling out other disorders that may cause alveolar hypoventilation, such as like severe restrictive,obstructive168P.Piesiak et al.pulmonary diseases,chest wall disorders,severe hypothyroidism,or neuromuscular diseases. COPD and OSA were diagnosed according to the following guidelines:Global Strategy for Diagnosis,Management,and Prevention of COPD(2011)and The Report of an American Academy of Sleep Medicine Task Force(1999).2.2Study ProtocolAll patients underwent baseline assessments of spirometry,arterial blood gas measurement,full polysomnography(PSG)before treatment,on the fifth day of NIMV therapy and during follow-up visit1year later.The PSG was performed with an Aura setup(Grass Technologies;West Warwick,RI)and spirometry with a Lung test 1,000system(MES,Krakow,Poland)according to guidelines recommended by Quanjer and the European Respiratory Society(1993).NIMV parameters were established duringfirst night under PSG control to avoid apneas and snoring and to achieve the adequate nocturnal respiratory control.Supplementary oxygen was provided to patients who were hypoxemic despite NIMV treatment(PaO2<7.3kPa).After establishing parameters of NIMV and achieving an improve-ment,the patients were discharged from the hos-pital and followed up at12months.Ventilation parameters were determined dur-ing the polysomnography under the medical supervision.Most of the subjects(83%)received NIMV via a Trilogy ventilator(Philips-Respironics,USA)in a pressure support,sponta-neous/timed mode(PS-S/T).The patients used the optional AVAPS(average volume assured pressure support)mode that automatically adapts pressure support–inspiratory positive airway pressure(IPAP)to provide the preset patient’s average tidal volume(VT).In that mode,IPAP was than titrated during ventilation in steps of 1mbar/min to achieve a desired VT In the pres-ent study,the IPAP was set between expiratory positive airway pressure(EPAP)and30mbar. AVAPS was set to7–10ml/kg of ideal body weight.Ventilator settings were changed according to the patient’s daytime and nocturnal tolerance,and to the maximal decrease of PaCO2.During1year’s treatment,the settings13 patients (38%) with COPD and OSAS (overlap syndrome)AHI>5 (mean 45±22) FEV1/VC<70% (mean61±8)34 obese patientswith CRF21 patients (62%)with OHSFEV1/VC≥70%(mean 78±7)14 patients with OSASAHI>5 (mean49±26)7 patients without OSASAHI≤5 (mean 3±2)Fig.25.1Final diagnosis as a reason of chronic respira-tory failure in the studied population,based on polysomnography and spirometry.CRF chronic respira-tory failure,COPD chronic obstructive pulmonary disease,OS overlap syndrome,OHS obesity hypoventilation syndrome,AHI apnea/hypopnea index, FVC forced vital capacity,FEV1forced expiratory vol-ume in1s.Values are meansÆSD25Efficacy of Noninvasive Mechanical Ventilation in Obese Patients with Chronic Respiratory Failure169for EPAP,respiratory rate,and inspiratory/expi-ratory ratio were kept at the same level.Twenty six received supplemental oxygen(Table25.1).The differences between groups were assessed by a paired t-test.Statistical significance was assumed with at a p<0.05.3ResultsIn the group of34patients we diagnosed the OS coexisting with of COPD and OSAS in 13patients and OHS in21patients(Fig.25.1). The analysis of different clinical variables of both groups(OS and OHS)showed a sig-nificantly lower FEV1/VC ratio in the OS patients(65Æ8%vs.78Æ7%,p<0.05). The patients with both OS and OHS suffer-ed from severe sleep apnea syndrome with similar high apnea/hypopnea(45.0Æ21.1vs.47.9Æ28.1,p>0.05)and desaturation indexes(67.2Æ25.6vs.64.3Æ24.8,p>0.05) (Table25.2).After the initiation of NIMV we observed an improvement of the clinical status of the patients soon after the onset of treatment and 1year afterward.On thefifth day of NIMV, there was an increase in the mean SaO2during sleep in all patients,but it was greater in the patients with obesity-hypoventilation syndrome (92.6Æ1.4%)than in those with the overlap syndrome(90.4Æ1.8%,p<0.05).We observed a significant improvement of diurnal PaO2and PaCO2soon after the beginning of NIMV(mean PaO2increase of 2.1kPa and PaCO2decrease of0.9kPa on thefifth day of NIMV)and then after a year’s home NIMV (mean PaO2increase of 1.9kPa and PaCO2 decrease of2.4kPa)(Table25.3).During the observation period,two patients died(one patient with the overlap syndrome and one with the obesity-hypoventilation syndrome coexisting with OSA),and one patient stopped treatment because of lack of tolerance.After12months’NIMV treatment we did not observe any significant changes in spirometry results.There was a small decrease of BMI after12months of NIMV(before:47.3Æ7.9 kg/m2and after:44.7Æ6.6kg/m2,p>0.05), but it did not reach statistical significance (Table25.4).4DiscussionThe prevalence of respiratory failure is estimated between20and30%in hospitalized obese adult patients(Borel et al.2011).The presence of hypercapnia and hypoxemia in patients with severe obesity is a consequence of complex interactions between a lot of factors associated with obesity itself,respiratory drive and sleep disordered breathing and in some cases coexisting chronic lung disease(Piper and Grunstein2010). One of the most common reasons of respiratory failure in obesity is the obesity-hypoventilation syndrome.There is a dose–response relationship between obesity as expressed by BMI and OHS prevalence(Nowbar et al.2004).There are data showing that70–90%of patients with OHS also exhibit OSAS(Resta et al.2000).It is in accor-dance to our study,where62%of patients had OHS and79%had OSAS.Most obese patient with respiratory failure can be treated effectively with oxygen or CPAP therapy.But for some seriously ill patients this approach is insufficient.Our trial demonstrated that in such patients NIMV has high efficacy in aTable25.1NIMV parametersVariablesIPAP(mbar)19.2Æ4.0EPAP(mbar)8.5Æ3.0VT(ml)583.2Æ68.1Vleak(ml)55.1Æ14.1f(breaths/min)16.5Æ3.1PS-S/T AVAPS mode(%of patients)84.1Æ7.2Oxygen(l/min) 2.6Æ0.9Patient-triggered breaths(%)45Æ27Compliance(h:min/day)5:23Æ02:45Supplemental oxygen therapy(n)26Values are meansÆSDIPAP inspiratory positive airway pressure,EPAP expira-tory positive airway pressure,VT tidal volume,Vleakleakage volume,f breathing frequency,PS-S/T pressuresupport-spontaneous/timed mode,AVAPS Average vol-ume assured pressure support mode170P.Piesiak et al.short and long period of time.In severe obese patients with chronic and complete respiratory failure,NIMV improved the ventilation during sleep by preventing apneas and hypopneas and increasing the minute ventilation.The control polysomnography performed on thefifth day of NIMV treatment showed significantly higher mean nocturnal oxygen saturation.Interestingly, the daytime gas exchange improved as well,with a significant increase of oxygen saturation and a reduction of carbon dioxide level.Our study demonstrates that after1year’s nocturnal NIMV performed at home these positive changes were still present and the reduction of carbon dioxide level was even more noticeable.Long term positive effects of NIMV were independent from spirometry changes and loosing weight. Our results confirm thefindings of previous small studies of patients who were not as obese, which demonstrated that NIMV causes improvements in daytime gas exchange,daytime somnolence and HRQL(Murphy et al.2012). Another trial showed that bi-level pressure ven-tilation improves nocturnal ventilatory control and daytime gas exchange,quality of life,day-time symptoms and daytime physical activity in OHS patients(de Lucas-Ramos et al.2004);the improvements being associated with subsequent weight loss.However,in contrast to previous data,our study showed that nocturnal treatmentTable25.2Baseline spirometry,blood gas analysis and polysomnography in patients with overlap syndrome(OS)and obesity hypoventilation syndrome(OHS)OS OHS pVC(ml)2,487Æ642,290Æ868NS VC(%)68Æ1364Æ17NS FEV1(ml)1,680Æ2001,870Æ630NS FEV1(%)49Æ661Æ14NS FEV1/VC%65Æ878Æ7<0.05 SaO2(%)80.3Æ4.975.8Æ11.1NS PaO2(kPa) 6.49Æ0.60 6.04Æ1.01NS PaCO2(kPa)9.28Æ2.418.02Æ1.47NS pH7.347.37NS AHI45.0Æ21.147.9Æ28.1NS DI67.2Æ25.664.3Æ24.8NS Mean minimal nocturnal SaO2(%)71.0Æ5.066.3Æ10.8NS Values are meansÆSDOS overlap syndrome,OHS obesity hypoventilation syndrome,AHI apnea/hypopnea index,DI desaturation index,FVC forced vital capacity,FEV1forced expiratory volume in1s,NS non-significantTable25.3Daytime blood gasometry results at baseline,on the fifth day of NIMV,and at12months’follow-up NIMVBaseline5th day12months PaO2(kPa) 6.19Æ1.358.49Æ1.79*8.12Æ1.21* PaCO2(kPa)8.44Æ1.887.48Æ1.28* 6.08Æ0.95* SaO2(%)76.8Æ10.191.8Æ3.3*90.6Æ3.4* pH7.36Æ0.057.38Æ0.047.41Æ0.04 Values are meansÆSD*p<0.05compared with baselineTable25.4Clinical variables at baseline and at12-month follow-up visitBaseline12-month follow-upBMI(kg/m2)47.3Æ7.944.7Æ6.6FVC%pred65.1Æ15.571.9Æ21.4FEV1%pred58.3Æ13.864.2Æ20.8FEV1/FVC%74.5Æ10.170.4Æ11.0Values are meansÆSDFVC forced vital capacity,FEV1forced expiratory vol-ume in1s25Efficacy of Noninvasive Mechanical Ventilation in Obese Patients with Chronic Respiratory Failure171of chronic respiratory failure in patients with severe obesity was not associated with weight loss.We observed some weight reduction,but the change did not reach statistical significance, due likely to a small number of individuals.During NIMV we observed an increase in the average SaO2during sleep,greater in patients with obesity-hypoventilation syndrome than with overlap syndrome(92.5Æ1.3vs.90.5Æ1.9%,p<0.05).There was a significant improvement of the daytime blood gasometry (Table25.3).There are several trials that included OHS and COPD patients that showed similar results of NIMV(Murphy et al.2012; Oscroft et al.2010).But in some trials nocturnal hypoventilation was better controlled in patient with OHS(Windish and Storre2012;Storre et al. 2006).Our study also shows that coexistance of COPD in patient with respiratory failure was a prognostic factor of worse efficacy of NIMV.The duration of the nocturnal NIMV adher-ence is very important for the treatment efficacy. In our group the mean daily time of NIMV was longer than5h.It is in accordance to publication of Murphy et al.(2012)which showed that!4h nocturnal ventilation is required to achieve a reduction in daytime carbon dioxide.A careful adjustment of ventilator settings during the noc-turnal monitoring is essential for proper control of nocturnal hypoventilation.In our study, NIMV settings were adjusted under the polysomnographic control performed by an experienced technician and a patient was discharged after the optimal treatment had been established.Another reason of high efficacy of NIMV in our study could be more intensive mode of the NIMV treatment.The average per-centage of patient-triggered breaths was45%, indicating that patients were treated mostly by the controlled mode of NIMV.This is in an agreement with studies of Murphy et al.(2012) and Dreher et al.(2010a,b)showing that the intensive mode of ventilation is more effective in both OHS and COPD patients.In28out of the34patients we performed NIMV with ventilator in a pressure preset venti-lation mode with the addition of average volume assured pressure support(AVAPS)mode.Treatment tolerance was very high in our study, with only one patient who stopped NIMV because of intolerance in1year’s observation period.Storre et al.(2006)showed that NIMV conducted with AVAPS mode results in a better control of nocturnal ventilation compared with the pure pressure-preset NIMV in OHS patients. But there are also another data showing no supe-riority of the AVAPS option over standard pressure-preset NIMV devices(Murphy et al. 2012).5ConclusionsOHS and OS belong to the two most common reasons of respiratory failure in severely obese patients.In such a group of patients,NIMV is an effective and well tolerated treatment option resulting in a rapid relief of respiratory disorders during sleep and gradual improvement of gas exchange during the day especially in patients with OHS.The long-term positive effects of NIMV are independent from spirometry changes and loosing weight.Conflicts of Interest The authors declare no conflicts of interest in relation to this article.ReferencesAmerican College of Chest Physicians.(1999).Clinical indications for noninvasive positive pressure ventila-tion in chronic respiratory failure due to restrictive lung disease,COPD,and nocturnal hypoventilation:A consensus conference report.Chest,116,521–534. Borel,J.C.,Borel,A.L.,Monneret,D.,Tamisier,R., Levy,P.,&Pepin,J.L.(2011).Obesity hypoventilation syndrome:From sleep disordered breathing to systemic comorbidities and the need to offer combined treatment strategies.Respirology,17(4),601–610.de Lucas-Ramos,P.,de Miguel-Diez,J.,Santacruz-Siminiani,A.,Gonza´lez-Moro,J.M.,Buendı´a-Garcı´a, M.J.,&Izquierdo-Alonso,J.L.(2004).Benefits at1 year of nocturnal intermittent positive pressure venti-lation in patients with obesity-hypoventilation syn-drome.Respiratory Medicine,98,961–967. Dreher,M.,Kabitz,H.,Burgardt,V.,Walterspacher,S.,& Windisch,W.(2010a).Proportional assist ventilation172P.Piesiak et al.improves exercise capacity in patients with obesity.Respiration,80,106–111.Dreher,M.,Storre,H.,Schmoor,C.,&Windish,W.(2010b).High-intensity versus low-intensity non-invasive ventilation in stable hypercapnic COPD patients:A randomized cross-over trial.Thorax,65, 303–308.Global Strategy for Diagnosis,Management,and Preven-tion of COPD.(2011).Updated December2011./.Accessed22Oct2012. Janssens,J.P.,Derivaz,S.,Breitenstein,E.,De Muralt,B.,Fitting,J.W.,Chevrolet,J.C.,&Rochat,T.(2003).Changing patterns in long-term noninvasive ventilation:A7-year prospective study in the Geneva lake area.Chest,123,67–79.Leech,J.,Onal,E.,Aronson,R.,&Lopata,M.(1991).Voluntary hyperventilation in obesity hypoventilation.Chest,100,1334–1338.Lloyd-Owen,S.J.,Donaldson,G.C.,Ambrosino,N., Escarabill,J.,Farre,R.,Fauroux, B.,Robert, D., Schoenhofer,B.,Simonds,A.K.,&Wedzicha,J.A.(2005).Patterns of home mechanical ventilation use in Europe:Results from the Eurovent survey.European Respiratory Journal,25,1025–1031.Mehta,S.,&Hill,N.S.(2001).Noninvasive ventilation.American Journal of Respiratory and Critical Care Medicine,163,540–577.Mokhlesi,B.(2010).Obesity hypoventilation syndrome:A state-of-the-art review.Respiratory Care,55, 1347–1362.Murphy,P.B.,Davidson,C.,Hind,M.D.,Simonds,A., Williams,A.J.,Hopkinson,N.S.,Moxham,J.,Polkey, M.,&Hart,N.(2012).Volume targeted versus pressure support non-invasive ventilation in patients with super obesity and chronic respiratory failure:A randomised controlled trial.Thorax,67(8),727–734.Nowbar,S.,Burkart,K.M.,Gonzales,R.,Fedorowicz,A., Gozansky,W.S.,Gaudio,J.C.,Taylor,M.R.,&Zwillich,C.W.(2004).Obesity-associated hypoventilation inhospitalized patients:Prevalence,effects,and outcome.American Journal of Medicine,116,1–7.Oscroft,N.S.,Ali,M.,Gulati,A.,Davies,M.G.,Quinnell,T.G.,Shneerson,J.M.,&Smith,I.E.(2010).A randomisedcrossover trial comparing volume assured and pressure preset noninvasive ventilation in stable hypercapnicCOPD.Chronic Obstructive Pulmonary Disease, 7,398–403.Perez de Llano,L. A.,Golpe,R.,Ortiz,P.M., Veres Racamonde, A.,Va´zquez Caruncho,M., Caballero Muinelos,O.,&Alvarez Carro,C.(2005).Short-term and long-term effects of nasal intermittent positive pressure ventilation in patients with obesity-hypoventilation syndrome.Chest,128,587–594. Piper,A.J.,&Grunstein,R.R.(2010).Big breathing:The complex interaction of obesity,hypoventilation, weight loss,and respiratory function.Journal of Applied Physiology,108,199–205.Quanjer,P.H.,Tammeling,G.I.,Cotes,J.E.,Pedersen, O.F.,Peslin,R.,&Yernault,J.C.(1993).Lung volumes and forced ventilatoryflows.Report working party standardization of lung function tests.European Community of Steel and Coal.Official Statement of the European Respiratory Society.European Respira-tory Journal,6(Suppl16),5–40.Resta,O.,Foschino-Barbaro,M.P.,Bonfitto,P.,Talamo, S.,Legari,G.,De Pergola,G.,Minenna, A.,& Giorgino,R.(2000).Prevalence and mechanisms of diurnal hypercapnia in a sample of morbidly obese subjects with obstructive sleep apnoea.Respiratory Medicine,94,240–246.Simonds,A.K.(2003).Home ventilation.The European Respiratory Journal.Supplement,47,38s–46s. Steier,J.,Jolley,C.J.,Seymour,J.,Roughton,M.,Polkey, M.I.,&Moxham,J.(2009).Neural respiratory drive in obesity.Thorax,64,719–725.Storre,J.H.,Seuthe, B.,Fiechter,R.,Milioglou,S., Dreher,M.,Sorichter,S.,&Windisch,W.(2006).Average volume-assured pressure support in obesity hypoventilation:A randomized crossover trial.Chest, 130,815–821.Sturm,R.(2007).Increases in morbid obesity in the USA: 2000–2005.Public Health,121,492–496.The Report of an American Academy of Sleep Medicine Task Force.(1999).Sleep-related breathing disorders in adults:Recommendations for syndrome definition and measurement techniques in clinical research.Sleep,21,667–689.Windish,W.,&Storre,J.H.(2012).Target volume settings for home mechanical ventilation:Great prog-ress or just a gadget?Thorax,67,727–734.25Efficacy of Noninvasive Mechanical Ventilation in Obese Patients with Chronic Respiratory Failure173。