SIMULTANEOUS TREATMENT EFFECTIVNESS OF DYSLIPIDEMIA, DIABETES MELLITUS AND ARTERIAL HYPERTENSION
- 格式:pdf
- 大小:213.44 KB
- 文档页数:12
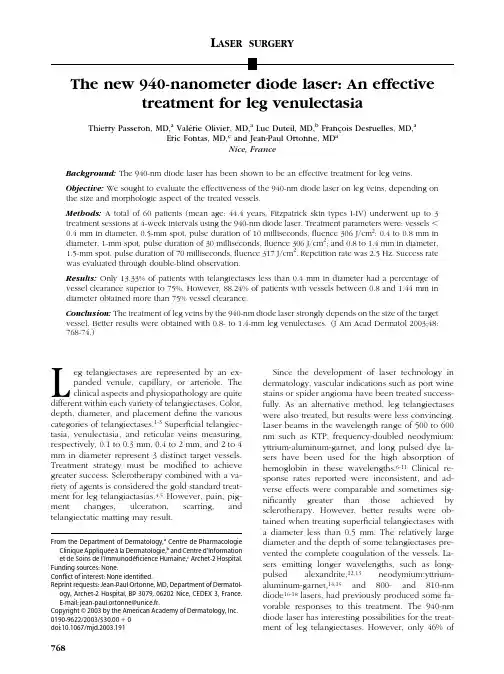
L ASERSURGERYThe new940-nanometer diode laser:An effective treatment for leg venulectasiaThierry Passeron,MD,a Vale´rie Olivier,MD,a Luc Duteil,MD,b Franc¸ois Desruelles,MD,aEric Fontas,MD,c and Jean-Paul Ortonne,MD aNice,FranceBackground:The940-nm diode laser has been shown to be an effective treatment for leg veins. Objective:We sought to evaluate the effectiveness of the940-nm diode laser on leg veins,depending on the size and morphologic aspect of the treated vessels.Methods:A total of60patients(mean age:44.4years,Fitzpatrick skin types I-IV)underwent up to3 treatment sessions at4-week intervals using the940-nm diode laser.Treatment parameters were:vesselsϽ0.4mm in diameter,0.5-mm spot,pulse duration of10milliseconds,fluence306J/cm2;0.4to0.8mm in diameter,1-mm spot,pulse duration of30milliseconds,fluence306J/cm2;and0.8to1.4mm in diameter, 1.5-mm spot,pulse duration of70milliseconds,fluence317J/cm2.Repetition rate was2.5Hz.Success rate was evaluated through double-blind observation.Results:Only13.33%of patients with telangiectases less than0.4mm in diameter had a percentage of vessel clearance superior to75%.However,88.24%of patients with vessels between0.8and1.44mm in diameter obtained more than75%vessel clearance.Conclusion:The treatment of leg veins by the940-nm diode laser strongly depends on the size of the target vessel.Better results were obtained with0.8-to1.4-mm leg venulectases.(J Am Acad Dermatol2003;48: 768-74.)L eg telangiectases are represented by an ex-panded venule,capillary,or arteriole.Theclinical aspects and physiopathology are quite different within each variety of telangiectases.Color, depth,diameter,and placement define the various categories of telangiectases.1-3Superficial telangiec-tasia,venulectasia,and reticular veins measuring, respectively,0.1to0.3mm,0.4to2mm,and2to4 mm in diameter represent3distinct target vessels. Treatment strategy must be modified to achieve greater success.Sclerotherapy combined with a va-riety of agents is considered the gold standard treat-ment for leg telangiactasias.4,5However,pain,pig-ment changes,ulceration,scarring,and telangiectatic matting may result.Since the development of laser technology in dermatology,vascular indications such as port wine stains or spider angioma have been treated success-fully.As an alternative method,leg telangiectases were also treated,but results were less convincing. Laser beams in the wavelength range of500to600 nm such as KTP,frequency-doubled neodymium: yttrium-aluminum-garnet,and long pulsed dye la-sers have been used for the high absorption of hemoglobin in these wavelengths.6-11Clinical re-sponse rates reported were inconsistent,and ad-verse effects were comparable and sometimes sig-nificantly greater than those achieved by sclerotherapy.However,better results were ob-tained when treating superficial telangiectases with a diameter less than0.5mm.The relatively large diameter and the depth of some telangiectases pre-vented the complete coagulation of the -sers emitting longer wavelengths,such as long-pulsed alexandrite,12,13neodymium:yttrium-aluminum-garnet,14,15and800-and810-nm diode16-18lasers,had previously produced some fa-vorable responses to this treatment.The940-nm diode laser has interesting possibilities for the treat-ment of leg telangiectases.However,only46%ofFrom the Department of Dermatology,a Centre de Pharmacologie Clinique Applique´e a`la Dermatologie,b and Centre d’Information et de Soins de l’Immunode´ficience Humaine,c Archet-2Hospital. Funding sources:None.Conflict of interest:None identified.Reprint requests:Jean-Paul Ortonne,MD,Department of Dermatol-ogy,Archet-2Hospital,BP3079,06202Nice,CEDEX3,France.E-mail:jean-paul.ortonne@unice.fr.Copyright©2003by the American Academy of Dermatology,Inc. 0190-9622/2003/$30.00ϩ0doi:10.1067/mjd.2003.191768patients in a recent study achieved75%clearing.19 The objective of this study was to evaluate the ef-fects of the940-nm diode laser on a large group of patients,depending on size and morphologic aspect of the treated vessels.Long-term results and occur-rence of side effects were also studied. MATERIALS AND METHODSA total of60patients seeking treatment for leg telangiectases were enrolled in the prospective study after obtaining written consent.Patients ranged in ages from25to75years with the mean age being44.4years and the minimum age being18 years.Of the patients,58were women.Fitzpatrick skin type among patients was I(4),II(18),III(35), and IV(3).Patients having Fitzpatrick skin type V and VI were excluded.All categories of telangiecta-ses were included(linear,arborized,and spider). Spider telangiectases were differentiated from ar-borized telangiectases by virtue of a perforating venule in the center.Treatment sites were varied to study different locations on the lower extremities. Calculating distances in millimeters,and the exact treatment sites for clinical,photographic,and Dopp-lerflow evaluations were noted for each patient from different anatomic marks.They were then pre-cisely located on tracing paper where the telangiec-tases,naevi,lentigo,and other selected natural marks were reproduced to allow precise identifica-tion of the treatment site during the course of the study.Personal history of sclerotherapy was noted. Pregnancy,lactation,poor healing,previous sclero-therapy,or other laser therapy for leg veins within the last2months,and a history of deep or superficial vein thrombosis were all criteria of exclusion.Pa-tients were instructed to shave their legs before each laser session and to avoid sun exposure until6 weeks after the last treatment.Patients were treated by a940-nm diode laser (Dornier Medilas D,SkinPulse).Bothfluence and pulse duration were selectable within a range of200 to1000J/cm2and10to100milliseconds,respec-tively.Three hand pieces allowed the delivery of laser energy with0.5-,1-,and1.5-mm diameter spot sizes.Telangiectases less than0.4mm in diameter were treated by a0.5-mm spot with a pulse duration of10milliseconds.For telangiectases between0.4 and0.8mm in diameter,a1-mm spot with a pulse duration of30milliseconds was used,and a1.5-mm spot with a pulse duration of70milliseconds was used for telangiectases between0.8to1.4mm in diameter.Repetition rate was2.5Hz.Each proce-dure involved afluence of306J/cm2when the0.5-or1-mm spot was used and317J/cm2with1.5-mm spot.Fluences were adapted to have complete ves-sel disappearance without blanching of the epider-mis.The study involved treatment of entire length of the vessels until they were no longer visible.No cooling device was used.Postlaser care consisted only of taping emollient cream.Patients returned for follow up treatment every4weeks,for a total of3 treatments.Afinal visit was scheduled4weeks after thefinal treatment.Patients were re-evaluated1year later to determine the long-term effectiveness of the treatment.Patients were instructed to rate the pain per-ceived during treatment on a visual scale of1to10, with1representing minimal discomfort and10rep-resenting severe plications including hy-perpigmentation,erythema,telangiectatic matting, purpura,crusting,and scarring were recorded be-fore each new laser se´ance and at thefinal visit.Photographs were taken before treatment,after each session,and at thefinal visit.A Polaroid Macro 5SLR magnifying X1and X3was used with identical parameters on each occasion.Evaluation was done by2physicians who reviewed in a blinded manner the photographs of each patient.For each patient, the percentage of vessel clearance was estimated and an average of these2evaluations was made.A laser Doppler perfusion imager(PIM1.0,Lisca De-velopment AB,Linko¨ping,Sweden)was used to scan the selected area(2.5ϫ2.5cm)before each laser se´ance and at thefinal visit to study the evo-lution of the spatial distribution of the skin perfu-sion.Finally,each patient who had previously un-dergone sclerotherapy was asked to compare the2 methods as to their effectiveness and level of pain. RESULTSOf the60patients,52returned for all posttreat-ment evaluations.A total of6patients were unable to tolerate the pain and2patients decided to stop after1se´ance because of no improvement.These patients were all considered to have had ineffective treatment(clearance rates0%-25%).The degree of concordance between the2observers was evalu-ated by linear weighted.Thewas very good (0.91).Only13.33%of patients with telangiectases less than0.4mm in diameter had a vessel clearance of more than75%.However,88.24%of patients with vessels between0.8and1.4mm in diameter ob-tained more than75%vessel plete vessel clearance(Ͼ95%)was obtained only in the group with vessels between0.8to1.4mm in diam-eter.In this group,35.3%(6of17)patients obtained complete vessel clearance.The results of the940-nm diode laser in60patients are summarized in Figs1to 3.Examples of pretreatment and posttreatment pho-tographs are shown in Figs4and5.Passeron et al769J A M A CAD D ERMATOL V OLUME48,N UMBER5For each perfusion image,4skin blood flow (SBF)parameters were calculated:mean value (Mean);minimum;maximum (Max);and SD.Table I summarizes the SBF parameters (mean ϮSD)ob-tained at each visit and grouped by diameter-vessel class.An analysis of variance was performed to as-sess the effects of time (visit)and vessel diameter on these parameters.The results of this analysis showed that a signi ficant diameter effect was detected (P ϭ.017).Indeed,whatever the visit,the minimum and Mean SBF were found higher in the small-vessel class (Ͻ0.4mm)compared with the 2other classes.Concerning the time effect,no signi ficant effect was found except for parameter Max SBF where the value measured at the last visit was higher (P ϭ.006)than for the former visits,whatever the diameter class.This last point was mainly true in the small-vessel class where Max SBF at the last visit was twice the baseline value.The descriptive analysis of Table I indicates that SBF parameters were quite compa-rable for the medium-and large-vessel classes.A variability of responses was observed in this study on the SBF parameters.At the final visit,an increase of Mean SBF was observed mainly in the small-vessel class (72%)whereas a decrease of Mean SBF was observed on the medium-(56%)and the large-(60%)vessel classes.Fig 6illustrates the decrease of Mean SBF after laser diode treatment observed on the perfusion images for 2patients belonging to medium-and large-vessel classes.The analysis of the relationship between SBF parameters and the percentage of clearance showed poor correlation (r Ͻ0.2).This was probably a result of the high variability of SBF parameters observed in this study.Nevertheless,the lower clearance rates observed for the small-vessel class compared with the 2others were probably related to the highest Mean and Max SBF values observed in thisclass.Fig 2.Effectiveness of treatment by type oftelangiectsias.Fig 1.Vein clearance rates by number of treatment.770Passeron et alJ A M A CAD D ERMATOLM AY 2003Pain during laser treatment was important (mean:6.09/10;range:1-10).Adverse effects were d erythema in the distribution of the treated veins was quite common immediately after laser treat-ment.Transitional crusting was observed in 21pa-tients for 1to 4weeks without permanent sequela.Minimal telangiectatic matting was noted in 3pa-tients.Hypopigmentation was observed in 4pa-tients,all of whom had Fitzpatrick skin type III,lasting 4to 8weeks before cleaning.No adverse effect was noted in the 3patients having Fitzpatrick skin type IV.No scarring occurred in any patient.A total of 46patients had a history of sclerother-apy treatment for leg veins.Of these,20patients found laser treatment more ef ficient,but 21patients found sclerotherapy had given better results.The remaining 5patients considered the treatment ser therapy was more painful than sclerotherapy for 31of the 46patients.In all,28patients were evaluated 1year beyond the treatment,of which only one had partial vessel recurrence.DISCUSSIONLasers with long wavelengths of light,within the visible spectrum,penetrate more deeply into the skin,making them more suitable for deeper ves-sels.20The 940-nm diode laser (Dornier Medilas D,SkinPulse)was expected to allow better penetration of the dermis as a result of its longer wavelength.In addition,this wavelength corresponds with the sec-ond absorption peak of hemoglobin,decreases in-terference of melanin,and covers the entire vascular volume.The large number of patients allowed for analysis of the results according to vessel type and diameter.About 80%of the patients had more than 50%vessel clearance and more than half had more than 75%vessel clearance when linear or arborized telangiec-tases were treated.However,none of the 6patients with spider telangiectases obtained more than 50%vessel clearance.When effectiveness is evaluated according to vessel diameter,the results are more conclusive.Only 13.33%of patients with telangiec-tases less than 0.4mm in diameter had a percent of vessel clearance more than 75%.However,88.24%Fig 4.Leg telangiectases before treatment (A )and 1month after the third session of laser diode treatment (B).Fig 3.Effectiveness of treatment by diameter of treated vessel.Passeron et al 771J A M A CAD D ERMATOL V OLUME 48,N UMBER 5of patients with vessels between 0.8and 1.4mm in diameter obtained more than 75%vessel clearance.Only 1patient obtained less than 50%vessel clear-ance but was among patients who had stopped the study because of severe pain and,therefore,was considered as a treatment failure.Our study clearly demonstrated that results obtained with the diode laser strongly depend on type (P ϭ.011,Fisher chi-square)and diameter (P Ͻ.001,chi-square)of treated telangiectases.As type and diameter were not linked in our study,there was no confusion bias.The poor response of spider telangiectases is easilyTable I.Skin blood flow parameters (mean ϮSD)Vessel class<0.4mm 0.4-0.8mm 0.8-1.4mm GlobalMeanSDMeanSDMeanSDMeanSDDiameter 0.350.070.520.060.950.090.600.24Clearance 4126602576106025Mean SBF V00.450.290.370.190.340.250.380.23Mean SBF V10.400.180.320.240.300.180.340.21Mean SBF V20.530.250.370.280.280.220.380.27Min V00.120.150.050.060.060.090.070.10Min V10.070.060.060.110.060.070.060.09Min V20.130.110.080.110.050.100.090.11MaxV0 1.78 1.26 1.97 1.88 2.09 1.63 1.96 1.65MaxV1 2.00 1.66 1.71 1.26 2.08 1.31 1.89 1.36MaxV2 4.05 2.07 2.20 1.77 2.46 2.52 2.73 2.15SD V00.190.110.220.140.230.180.210.14SD V10.220.120.190.130.200.110.200.12SD V20.340.170.220.130.220.160.250.15Max ,Maximum;Min ,minimum;SBF ,skin blood flow;V0,baseline visit;V1,visit 1;V2,visit 2.The mean values of Min,Max,and Mean SBF,and SD of SBF were calculated for each vessel class at each visit and also for grouped vessel sizes(global).Fig 5.Leg telangiectases before (A )and just after first laser treatment (B ).C ,Clinical aspect after 1year.772Passeron et alJ A M A CAD D ERMATOLM AY 2003understandable as the laser,with the parameters used in this study,was not able to treat the central perforating venule.These types of telangiectases should be first treated by sclerotherapy.Moreover,this study corroborates and statistically proves the accepted results that deeper and larger vessels are best targeted by longer wavelengths,whereas these longer wavelengths are not suitable for super ficial and thin ser Doppler measure-ments indicated that small-vessel class showed higher Mean and Max SBF values compared with the 2other classes.This was probably a result of the fact that the vessel networks under investigation were different in size and depth.This difference of vessel classes was well identi fied by the SBF imaging mea-surements in the sense that,in the measured SBF,a vessel class stood out compared with 2others.Anal-ysis of the hemoglobin oxygenation in the different treated vessels could not be done.However,blue coloring was signi ficantly associated with the larger vessels (0.8-1.4mm),whereas red coloring was as-sociated with the smaller vessels.Flow rate was also proportional to vessel size.These 2important pa-rameters might play a role in treatment response.However,the statistical analysis could not indicate differences of results within the 3sized groups for each of these parameters.Three sessions were nec-essary to obtain effective pared with the results obtained by Kaudewitz et al 19with the same diode laser,our overall results were identical.This study demonstrated the interest in and necessity for analyzing results according to vessel type and diam-eter.For the 45patients who had prior treatment by sclerotherapy,the laser method was equally effec-tive but more painful.However,18of the 23patients who had telangiectases larger than 0.4mm in diam-eter and who were previously treated by sclerother-apy found the laser treatment more effective than sclerotherapy.Side effects were rare and disappeared within 8weeks.Patients having Fitzpatrick skin type IV did not present additional side effects compared with the patients with other Fitzpatrick skin types.Crust-ing of 21%is a high degree of epidermal effect for a laser that penetrates deeply into tissues and interacts less with super ficial cutaneous layers.As it was ob-served when super ficial red telangiectases were treated,it is believed that this was a result of feed-back diffusion to the epidermis of the thermalen-Fig 6.Images of skin blood flow perfusion (telangiectases)observed at baseline and during subsequent visits for 2patients.Top row ,Patient 1;bottom row ,patient 2.Passeron et al 773J A M A CAD D ERMATOL V OLUME 48,N UMBER 5ergy delivered to the superficial vessels.The recom-mendation is to wait5or6weeks between2 treatments because transitional crusting was ob-served up to4weeks after the laser se´ance.Pain sometimes curbed the treatment,but lengthening of the laser repetition rate allowed decrease in the pain with little loss of time.An open study was performed on two thirds of the patients where they were treated with prior application of EMLA cream.As this topical anesthetic could cause vasoconstriction of vessels and,therefore,interact with the results ob-tained,studies were made on the effects of the laser when using this cream on the other lower limb, similar to the one used for the central study.Indica-tions were that the use of EMLA cream an hour before the se´ance decreased the pain significantly, without apparent loss of effectiveness.Nevertheless, it should be noted that the measurements of vessel diameter were done just before each laser se´ance so it was impossible to determine if the EMLA cream had led to a vasoconstriction capable of decreasing the effectiveness of the laser.Cooling technology is the standard of care in laser treatment of leg vessels.A cooling devise was not used in the study,but it is likely that the use of cooling technology will appre-ciably decrease pain and crusting.Development of laser technology allows for many wavelengths with variation of pulse duration,fluence,and spot size.All these parameters should be adapted to the type of telangiectases of each patient.The940-nm diode laser is a useful treatment for leg veins with clinical response lasting1year in the segment of patients we could monitor for this period.The method is safe and can be afforded to patients having Fitzpatrick skin type III or IV.How-ever,a treatment plan should be clearly outlined according to the type of leg veins to afford the best treatment for the patient.For this,the940-nm diode laser should be used for simple and arborized leg veins with0.8-to1.4-mm diameter.Smaller telangi-ectases should be treated by a laser using shorter wavelengths.Our gratitude to Alexandra Charlesworth and Nadine Gentles for revising the manuscript.REFERENCES1.Sommer A,Van Mierlo PLH,Neumann HAM,Kessels AGH.Redand blue telangiectasias:differences in oxygenation?Dermatol Surg1997;23:55-9.2.Redisch W,Pelzer RH.Localized vascular dilatations of the hu-man skin:capillary microscopy and related studies.Am Heart J 1949;37:106-14.3.Weiss RA,Weiss MA.Painful telangiectasias:diagnosis and treat-ment.In:Goldman MP,Weiss RA,Bergan JJ,editors.Varicose veins and telangiectasias.Diagnosis and treatment.St Louis: Quality Medical Publishing;1999.p.498-517.4.Kauvar AN.The role of lasers in the treatment of leg veins.SeminCutan Med Surg2000;19:245-52.5.Goldman MP,Weiss RA.Treatment of leg telangiectasia withlaser and high-intensity pulsed light.Dermatol Ther2000;13:38-49.6.Massey RA,Katz BE.Successful treatment of spider leg veinswith a high-energy,long-pulse,frequency-doubled Neodymi-um:YAG laser(HELP-G).Dermatol Surg1999;25:677-80.7.West TB,Alster parison of the long-pulse dye(590-595nm)and KTP(532nm)lasers in the treatment of facial and leg telangiectasias.Dermatol Surg1998;24:221-6.8.Reichert D.Evaluation of the long-pulse dye laser for thetreatment of leg telangiectasias.Dermatol Surg1998;24:737-40.9.Alora MB,Stern RS,Arndt KA,Dover parison of the595nm long-pulse(1.5msec)and ultralong-pulse(4msec)lasers in the treatment of leg veins.Dermatol Surg1999;25:445-9. 10.Bernstein EF,Lee J,Lowery J,Brown DB,Geronimus R,Lask G,etal.Treatment of spider veins with the595nm pulsed-dye laser.J Am Acad Dermatol1998;39:746-50.11.Buscher BA,McMeekin TO,Goodwin D.Treatment of leg telan-giectasia by using a long-pulse dye laser at595nm with and without dynamic cooling sers Surg Med2000;27:171-5.12.McDaniel DH,Ash K,Lord J,Newman J,Adrian RM,Zukowkiser therapy of spider leg veins:clinical evaluation of a new long pulsed alexandrite laser.Dermatol Surg1999;25: 52-8.13.Kauvar AN,Lou WW.Pulsed alexandrite laser for the treatmentof leg telangiectasia and reticular veins.Arch Dermatol2000;136:1371-5.14.Weiss RA,Weiss MA.Early clinical results with a multiple syn-chronized pulsed1064nm laser for leg telangiectasias and re-ticular veins.Dermatol Surg1999;25:399-402.15.Sadick NS.Long-term results with a multiple synchronized-pulsed1064nm Nd:YAG laser for the treatment of leg venulec-tasias and reticular veins.Dermatol Surg2001;27:365-9.16.Dierickx CC,Duque V,Anderson RR.Treatment of leg telangiec-tasia with a pulsed diode sers Surg Med1998;10:40. 17.Garden JM,Bakus AD,Miller ID.Diode laser treatment of legsers Surg Med1998;21:32.18.Varma S,Lanigan ser therapy of telangiectatic leg veins:clinical evaluation of the810nm diode laser.Clin Exp Dermatol 2000;25:419-22.19.Kaudewitz P,Klo¨vekorn W,Rother W.Effective treatment of legvein telangiectasia with a new940nm diode laser.Dermatol Surg2001;27:101-6.20.Dover JS,Arndt KA.New approaches to the treatment of vascu-lar sers Surg Med2000;26:158-63.774Passeron et al J A M A CAD D ERMATOLM AY2003。
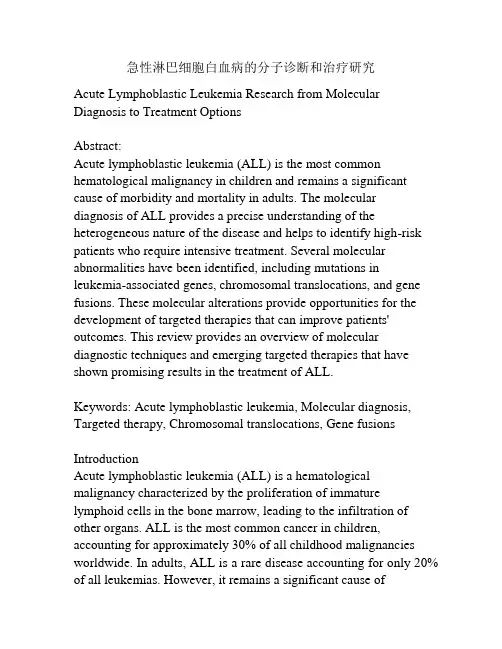
急性淋巴细胞白血病的分子诊断和治疗研究Acute Lymphoblastic Leukemia Research from Molecular Diagnosis to Treatment OptionsAbstract:Acute lymphoblastic leukemia (ALL) is the most common hematological malignancy in children and remains a significant cause of morbidity and mortality in adults. The molecular diagnosis of ALL provides a precise understanding of the heterogeneous nature of the disease and helps to identify high-risk patients who require intensive treatment. Several molecular abnormalities have been identified, including mutations in leukemia-associated genes, chromosomal translocations, and gene fusions. These molecular alterations provide opportunities for the development of targeted therapies that can improve patients' outcomes. This review provides an overview of molecular diagnostic techniques and emerging targeted therapies that have shown promising results in the treatment of ALL.Keywords: Acute lymphoblastic leukemia, Molecular diagnosis, Targeted therapy, Chromosomal translocations, Gene fusions IntroductionAcute lymphoblastic leukemia (ALL) is a hematological malignancy characterized by the proliferation of immature lymphoid cells in the bone marrow, leading to the infiltration of other organs. ALL is the most common cancer in children, accounting for approximately 30% of all childhood malignancies worldwide. In adults, ALL is a rare disease accounting for only 20% of all leukemias. However, it remains a significant cause ofmorbidity and mortality, particularly in patients with relapsed or refractory disease. The prognosis of ALL is influenced by several factors, including age, initial response to therapy, and the presence of specific genetic abnormalities. The development of molecular diagnostic techniques has led to a better understanding of the molecular heterogeneity of ALL and has paved the way for the development of targeted therapies.Molecular diagnosis of ALLThe diagnosis of ALL is based on the presence of blast cells in the bone marrow or peripheral blood, along with clinical manifestations. Molecular diagnosis techniques have been developed to provide a better understanding of the molecular basis of the disease and to identify high-risk patients who require aggressive treatment. These techniques include cytogenetic analysis, fluorescence in situ hybridization (FISH), polymerase chain reaction (PCR), and next-generation sequencing (NGS). Cytogenetic analysis is a classical technique that involves the visualization of chromosomal abnormalities using banding techniques. Chromosomal translocations involving the immunoglobulin and T-cell receptor genes are common in ALL and are associated with specific subtypes of the disease. For example, the t(9;22) Philadelphia chromosome is present in approximately 25% of adult ALL cases and is associated with a poor prognosis. FISH is a more sensitive technique that allows the detection of chromosomal translocations, gene fusions, and copy number variations using fluorescent probes. PCR is a highly sensitive technique that amplifies specific DNA sequences and is widely used to detect fusion genes and minimal residual disease(MRD) in ALL patients. NGS is a next-generation sequencing technique that allows the simultaneous detection of multiple mutations and copy number variations in a single assay, providing a comprehensive genomic analysis of the disease.Targeted therapies in ALLThe identification of specific molecular abnormalities in ALL has led to the development of targeted therapies that can improve patients' outcomes. The success of targeted therapies in ALL depends on the identification of patient subgroups that are likely to benefit from these therapies, as well as the development of drugs that can target the specific molecular abnormalities.Chromosomal translocations involving the B-cell receptor (BCR) and the T-cell receptor (TCR) genes are common in ALL and result in the formation of fusion proteins that drive leukemogenesis. Several drugs have been developed to target these fusion proteins, including imatinib and dasatinib, which target the BCR-Abl fusion protein, and ponatinib, which targets the T315I mutation in the BCR-Abl fusion protein.Gene fusions involving the mixed-lineage leukemia (MLL) gene are common in infant ALL and are associated with a poor prognosis. Several drugs have been developed to target MLL fusion proteins, including DOT1L inhibitors and CDK9 inhibitors, which target the epigenetic regulation of gene expression. ConclusionMolecular diagnosis techniques have provided a better understanding of the heterogeneous nature of ALL and haveidentified specific molecular abnormalities that can be targeted by drugs. The use of targeted therapies in ALL is still in its early stages, and more research is needed to identify patient subgroups that are likely to benefit from these therapies, as well as the development of new drugs that can target specific molecular abnormalities. The success of targeted therapies in ALL depends on a better understanding of the disease's biology and the development of personalized treatment strategies.Targeted therapies have revolutionized the treatment of several cancers, including ALL. These therapies provide a more precise approach to cancer treatment by targeting specific molecular abnormalities that drive tumor growth and spread, while sparing normal tissue. Successful targeted therapies in ALL have led to improved outcomes for many patients, particularly those with high-risk disease.Imatinib and dasatinib are two drugs that target the BCR-Abl fusion protein associated with the t(9;22) translocation. These drugs have improved outcomes in patients with Philadelphia-positive ALL, leading to increased survival rates and reduced chemotherapy toxicity. Ponatinib is a third-generation BCR-Abl inhibitor that has shown promise in treating patients with the T315I mutation, which confers resistance to imatinib and dasatinib. Gene fusions involving the MLL gene are common in infant ALL and are associated with a poor prognosis. These fusions result in the recruitment of histone-modifying enzymes that alter gene expression and drive leukemogenesis. Drugs targeting epigenetic regulators, such as DOT1L and CDK9 inhibitors, represent a promising approach to treating MLL-rearranged ALL.Other targeted therapies under investigation in ALL include immune checkpoint inhibitors, chimeric antigen receptor (CAR) T-cell therapy, and antibody-drug conjugates. Immune checkpoint inhibitors, such as nivolumab and pembrolizumab, release the brakes on T-cell function, allowing them to attack cancer cells more effectively. CAR T-cell therapy involves extracting a patient's own T-cells and genetically modifying them to target specific cancer antigens before infusing them back into the patient. Antibody-drug conjugates combine a targeted antibody that binds to a cancer cell surface antigen with a toxic payload, resulting in targeted cell death. Blinatumomab, a bispecific T-cell engager antibody, targets the CD19 antigen on leukemia cells and redirects T-cells to attack them.Despite the success of targeted therapies in ALL, there are still challenges to overcome. Many targeted therapies require specific molecular abnormalities to be present in order to be effective, which limits their use to certain patient subgroups. Additionally, the development of resistance to targeted therapies can lead to treatment failure and disease progression. Therefore, ongoing research efforts are needed to identify new targets and develop strategies to overcome resistance.In conclusion, targeted therapies have shown promising results in the treatment of ALL by targeting specific molecular abnormalities that drive leukemogenesis. The development of personalized treatment strategies based on the molecular profile of the disease holds great potential for improving outcomes and reducing treatment-related toxicity. Ongoing research efforts are needed tooptimize and expand the use of targeted therapies in the management of ALL.Targeted therapies have revolutionized cancer treatment and become an essential component of the standard of care for several cancers, including ALL. These therapies provide a more precise approach to cancer treatment by targeting specific molecular abnormalities that drive tumor growth and spread, while sparing normal tissues. In ALL, targeted therapies have dramatically improved outcomes for high-risk patients, and ongoing research is identifying new molecular targets and developing strategies to overcome resistance.One of the most successful targeted therapies in ALL is tyrosine kinase inhibitors (TKIs) that target the BCR-Abl fusion protein associated with the t(9;22) translocation. Imatinib was the first TKI approved for the treatment of Philadelphia-positive ALL, leading to improved outcomes in these patients. However, imatinib resistance can develop, and dasatinib and ponatinib are second and third-generation TKIs with increased potency and activity against imatinib-resistant mutations.The development of resistance to targeted therapies is also a significant challenge, limiting their long-term effectiveness. One strategy to overcome resistance is to use combination therapies that target multiple pathways simultaneously. For example, the combination of a TKI with a CDK9 inhibitor has shown preclinical efficacy in MLL-rearranged ALL. Another approach is to develop new drugs that target molecular mechanisms leading to resistance, such as the Bruton's tyrosine kinase inhibitor acalabrutinib, which blocks the activation of the PI3K/AKT signaling pathway and has shown efficacy against TKI-resistant ALL cells in preclinicalmodels.Immune checkpoint inhibitors have shown promising results in several cancers, including melanoma and lung cancer, by restoring T-cell function and enhancing anti-tumor immunity. In ALL, early-phase clinical trials are ongoing to assess the safety and efficacy of immune checkpoint inhibitors, and preliminary results suggest potential benefits in relapsed/refractory disease.CAR T-cell therapy is a rapidly evolving immunotherapy that uses genetically engineered T-cells to target cancer cells, offering a personalized approach to cancer treatment. In ALL, CAR T-cell therapy targeting the CD19 antigen has shown high response rates, leading to FDA approval of tisagenlecleucel and axicabtagene ciloleucel for relapsed/refractory Philadelphia-negative ALL. Ongoing research is optimizing the manufacturing process and developing novel CAR constructs to improve efficacy and reduce toxicity.In conclusion, targeted therapies have revolutionized the treatment of ALL by improving outcomes and reducing toxicity. However, challenges remain, including the development of resistance, the need for specific molecular abnormalities, and toxicities associated with some targeted therapies. Ongoing research is needed to optimize and expand the use of targeted therapies by identifying new targets and developing strategies to overcome resistance, improve efficacy, and reduce toxicity. Ultimately, the goal is to develop personalized treatment strategies that maximize the benefits of targeted therapies for all patients with ALL.。
demonstrate翻译过去式:demonstrated; 过去分词:demonstrated; 现在分词:demonstrating;demonstrate 基本解释及物动词论证; 证明,证实; 显示,展示; 演示,说明不及物动词示威游行demonstrate 相关例句及物动词1. demonstrate的反义词1. The doctor demonstrated the harmful effects of tobacco.医生用实例说明烟草的有害的影响。
2.2. This fully demonstrates their willingness to cooperate.这充分表明他们愿意合作。
3.3. The lawyer demonstrated that the witness was lying.律师证明证人在说谎。
4.4. How do you demonstrate that the earth is round?你怎样证明地球是圆的?不及物动词1. demonstrate的意思1. The workers demonstrated for higher wages.工人示威要求加薪。
demonstrate 网络解释1. 示范:店内服务人员顛峰銷售四大原則教育(EDUCATE) 示範(DEMONSTRATE) 推薦(RECOMMEND) 活動(ACTIVTY) 銷售Q and A Q1.油性不潔、滿臉痘痘皮膚還能美白? Q2.哪種情況下皮膚較易長斑? Q3.如何選擇合適的美白全系列產品?2.2. 论证:①例如他谈到维特根斯坦的二分法,即可知的事实与可直觉(shown)的神秘,以及罗素的逻辑结构之只能直觉而不能论证(demonstrate并认为以往的哲学大多是企图论证只能被直觉的东西,因而是无意义的,或者是什么也没有说.3. 説明:耶稣的天国观是藉着宣讲来传扬开去的,祂透过直接讲解和间接的比喻向听众阐明,神迹奇事是用来说明(demonstrate)祂的讲解,却永远不是取代讲道,与第三波人士重说明而轻讲道的做法颇不一样.demonstrate 双语例句1. demonstrate1. Our results along with those reported by Lin et al demonstrate reossification and stabilization of tumor size can be achieved on CT and MRI imaging following serial arterial embolization.我们和Lin等的结果都表明连续动脉栓塞术后在CT和MRI上可以见到重新骨化和肿瘤大小的稳定。
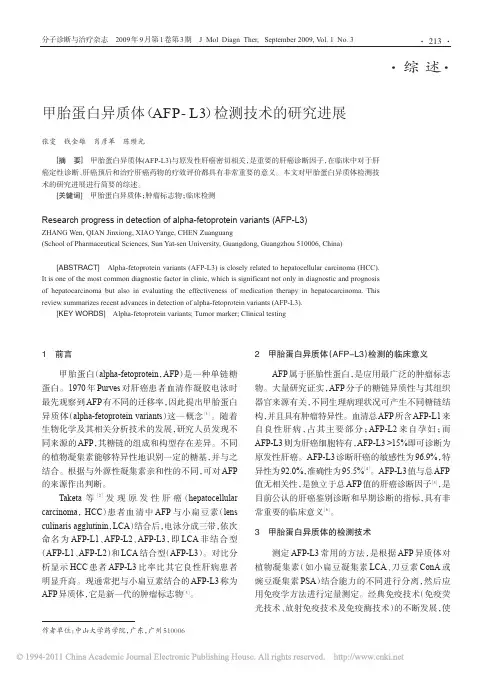
1前言甲胎蛋白(alpha-fetoprotein,AFP)是一种单链糖蛋白。
1970年Purves对肝癌患者血清作凝胶电泳时最先观察到AFP有不同的迁移率,因此提出甲胎蛋白异质体(alpha-fetoprotein variants)这一概念[1]。
随着生物化学及其相关分析技术的发展,研究人员发现不同来源的AFP,其糖链的组成和构型存在差异。
不同的植物凝集素能够特异性地识别一定的糖基,并与之结合。
根据与外源性凝集素亲和性的不同,可对AFP 的来源作出判断。
Taketa等[2]发现原发性肝癌(hepatocellular carcinoma,HCC)患者血清中AFP与小扁豆素(lens culinaris agglutinin,LCA)结合后,电泳分成三带,依次命名为AFP-L1、AFP-L2、AFP-L3,即LCA非结合型(AFP-L1、AFP-L2)和LCA结合型(AFP-L3)。
对比分析显示HCC患者AFP-L3比率比其它良性肝病患者明显升高。
现通常把与小扁豆素结合的AFP-L3称为AFP异质体,它是新一代的肿瘤标志物[3]。
2甲胎蛋白异质体(AFP-L3)检测的临床意义AFP属于胚胎性蛋白,是应用最广泛的肿瘤标志物。
大量研究证实,AFP分子的糖链异质性与其组织器官来源有关,不同生理病理状况可产生不同糖链结构,并且具有肿瘤特异性。
血清总AFP所含AFP-L1来自良性肝病,占其主要部分;AFP-L2来自孕妇;而AFP-L3则为肝癌细胞特有,AFP-L3>15%即可诊断为原发性肝癌。
AFP-L3诊断肝癌的敏感性为96.9%,特异性为92.0%,准确性为95.5%[4]。
AFP-L3值与总AFP 值无相关性,是独立于总AFP值的肝癌诊断因子[5],是目前公认的肝癌鉴别诊断和早期诊断的指标,具有非常重要的临床意义[6]。
3甲胎蛋白异质体的检测技术测定AFP-L3常用的方法,是根据AFP异质体对植物凝集素(如小扁豆凝集素LCA、刀豆素ConA或豌豆凝集素PSA)结合能力的不同进行分离,然后应用免疫学方法进行定量测定。
鼻内镜手术致眼内直肌损伤的临床特征和治疗思考宾蓉发布时间:2023-07-05T07:26:25.455Z 来源:《健康世界》2023年8期作者:宾蓉[导读] 目的通过总结鼻内镜鼻窦手术导致的严重眼眶并发症,特别是眼肌损伤的临床特征、处理经验及预后的评估,以期引起鼻内镜外科医生的重视,自我警醒,并探讨此类并发症的更佳治疗手段。
方法通过对相关病例的临床及影像学检查,分析判断眼眶并发症情况,包括眶内出血、眼外肌、视神经及眼球等组织有无损伤及其部位、程度,分别采用不同术式治疗眼内直肌损伤所致的特殊类型斜视。
结果 10例患者中4例因并发严重视神经损伤视力丧失或其他原因放弃后期的斜视矫正手术;6例接受斜视手术患者中,1例内直肌和下直肌同时损伤患者一期斜视术后眼位矫正不满意,放弃二期斜视手术,5例单纯内直肌损伤患者斜视术后第一眼位基本正位,外形上获得较好的改善,但是,患侧眼球的内转运动却不能完全恢复至正常,存留或轻或重的运动受限,侧方位注视仍有较明显复视。
结论鼻内镜手术导致的眼肌损伤复杂、严重,眼球运动受限、复视和眼位偏斜为最常见临床表现。
此手术为非常规斜视手术,处理比较棘手,没有标准的治疗方案,且由于缺乏对照研究,很难评价治疗方法的有效性。
即使患者术后第一眼位基本恢复至正位,但是都难以完全取得眼肌的功能复位要求,故重在预防。
成都市金牛区人民医院摘要:目的通过总结鼻内镜鼻窦手术导致的严重眼眶并发症,特别是眼肌损伤的临床特征、处理经验及预后的评估,以期引起鼻内镜外科医生的重视,自我警醒,并探讨此类并发症的更佳治疗手段。
方法通过对相关病例的临床及影像学检查,分析判断眼眶并发症情况,包括眶内出血、眼外肌、视神经及眼球等组织有无损伤及其部位、程度,分别采用不同术式治疗眼内直肌损伤所致的特殊类型斜视。
结果 10例患者中4例因并发严重视神经损伤视力丧失或其他原因放弃后期的斜视矫正手术;6例接受斜视手术患者中,1例内直肌和下直肌同时损伤患者一期斜视术后眼位矫正不满意,放弃二期斜视手术,5例单纯内直肌损伤患者斜视术后第一眼位基本正位,外形上获得较好的改善,但是,患侧眼球的内转运动却不能完全恢复至正常,存留或轻或重的运动受限,侧方位注视仍有较明显复视。
IAC九项教练精萃概述(中英文)(2012-04-15 08:31:20)转载▼分类:教练技术标签:iac教练技术精萃杂谈ICF(国际教练联合会)和IAC(国际教练协会)是目前世界上最大的两大教练组织,都是由Thomas J. Leonard所创建的。
ICF和IAC都提出了各自的教练能力标准,以建立行业标准,帮助推进教练行业在世界范围内的发展。
ICF提出的教练能力标准叫做“ICF11项教练能力”,IAC提出的叫做“IAC9项教练精萃”,目前已经有人把“ICF11项教练能力”翻译成中文,而互联网上我还没有看到中文版本的“IAC9项教练精萃”,因此我利用这个周末的休息时间,把“IAC9项教练精萃”翻译成中文,以方便国内的教练同仁门更容易的了解,也欢迎大家转载传播。
“ICF11项教练能力”与“IAC9项教练精萃”有很多相似的地方,同时也存在一些差异,我个人认为“IAC9项教练精萃”的标准要求更高,事实上IAC的CC(Cerificated Coach)认证难度比ICF的认证更难。
IAC九项教练精萃概述The IAC Coaching Masteries - Overview(翻译人博客:/coachnlp)英文原文地址:/index.php/get_certified/the_iac_coaching_masteries_overviewIAC(国际教练协会,)九项教练精萃的目的是为真正独立的教练认证培训机构提供一种基准和标准,同时这九项教练精萃并不隶属于任何的教练培训机构。
我们的目的在于为当今教练的效果提供一种测评手段,特别的是,IAC在认证教练的时候,评委通过观察教练与两个不同客户的半小时教练环节来测评教练的教练技术的熟练程度。
The purpose of the IAC Coaching Masteries™ is to provide the basis and standards for a truly independent certifying body, without allegiance to any coach training schools or organizations. Our goal is to create a vehicle for evaluating effective coaching in the moment. Specifically, the IAC® certification focuses on masterful coaching skills that are observable and can be measured by our certifiers during recorded, half-hour sessions with two different clients.IAC九项教练精萃由一个国际教练团队所开发,目的在于提供一个测评高水平教练的明确的标准,并且这个标准适用于全球的任何文化环境中。
《急危重症护理》课程教案课题:院前急救教学目的:1.识记紧急呼救、现场评估、检伤分类的内容和方法。
2.识记现场和途中救护的措施和要点。
3.理解检伤分类和现场救护的原则和意义。
4.理解途中运转的原则和注意事项。
5.学会应用伤情评估和检伤分类的常用方法。
6.学会应用急救技能现场救护院前常见疾病。
课型:新授课课时:本章6个项目,安排6个课时。
教学重点:认识现场呼救、现场评估、检伤分类、现场救护、伤病员转运以及途中救护的重要性;掌握现场呼救的内容和方法;熟悉有关急救通讯系统的相关知识;掌握伤情评估的方法;掌握常用检伤分类的方法;掌握各种院前急救的现场救护的重点;了解我国院外转运的现状及困难;掌握途中救护实施前的物品及伤病员准备。
教学难点:能写出重要概念的外文缩略语及中文意译;掌握伤情评估的流程;能为伤病员佩戴正确的标志;能有效实施各种院前现场救护措施;了解我国院外转运使用的工具及相关法律,常用的设备和药物;掌握途中救护的一般治疗和成批伤救护。
教学过程:1.教学形式:讲授课,教学组织采用课堂整体讲授和分组演示。
2.教学媒体:采用启发式教学、案例教学等教学方法。
教学手段采用多媒体课件、视频等媒体技术。
作业处理:完成每章后的思考题。
板书设计:药物,防治感染。
⑨对中毒的伤病员,及时注射解毒药物或给予排毒素药物处理。
2.现场救护的程序①根据现场伤病员情况,应协助医生对伤病员的伤情或病情进行初步评估,要求迅速、准确。
②立即实施最紧急的急救措施,如对气道梗阻的伤病员清理呼吸道,开放气道,对心搏骤停的伤病员立即实施心肺复苏术,必要时可在现场实施紧急手术,尽可能稳定伤情或病情。
③稳定伤病员的情绪,减轻或消除强烈刺激对其造成的心理反应。
对于创伤而言,急救5项技术是重点,它们分别为有效的通气、止血、包扎、固定和搬运。
二、常见的急症症状、体征及处理(一)休克1.判断要点引起休克的病因各有不同,但其病理生理变化大致相同,临床表现相似,主要为:①反应迟钝,意识异常,神志模糊和昏迷。
常用术语总结一、基本概念及用法债权人:obligee债务人:obligor一方:one party对方\相对人:the other party;善意相对人:the other party in good faith债权:creditor’s right; right to performance; right债务/义务: obligation标的物:subject matter责任:liability要约:offer;承诺:acceptance;要约邀请:invitation to offer;要约人:offeror受要约人:offeree收件人:recipient代理人:agent被代理人/本人:principle行为人:person performing (such) act代理权:agency authority应当:shall可以:may不能:may not不正当:improperly有权做. . 。
:may; is entitled to do履行义务:perform obligation, render performance订立合同:enter into a contract; conclude a contract; form a contract带来损失:cause loss to . 。
损害利益:harm somebody’s interest赔偿损失:indemnify the other party for its loss由某人承担费用:expenses shall be borne by sb。
承担损害赔偿责任:be liable for damages各自承担相应的责任:bear their respective liabilities accordingly要求承担违约责任:hold . 。
. liable for breach of contract享有权利、承担义务:assume right and obligation二、各个条文中的术语合同订立采取。
doi:10.3969/j.issn.1006-5725.2011.15.051作者单位:510180广州市第一人民医院呼吸内科通信作者:赵子文E-mail:zhaozw@yeah.net ·药物与临床·支气管哮喘(bronchial asthma)是呼吸系统的常见病、多发病。
吸入糖皮质激素方法由于具有使用药物剂量小,起效快,全身副作用少等优点,成为治疗支气管哮喘的最佳给药方式[1-2]。
理想的吸入糖皮质激素必须同时满足最大疗效和最大安全性要求,但目前临床评价最高和最常用的布地奈德和丙酸氟替卡松等药在高剂量或长期治疗时仍会产生肾上腺皮质功能抑制、骨质疏松、儿童患者生长发育受抑、肺炎发生率增高、咽部白色念珠菌感染和发音困难等不良反应。
因此,开发抗炎活性更强,不良反应较小的吸入糖皮质激素类药物仍然是临床支气管哮喘防治的需要。
环索奈德(CIC)作为新一代的吸入糖皮质激素是糖皮质激素前体药,其本身无活性,但能在靶器官肺内被内源性酯酶分解为活性代谢产物———去异丁酰基环索奈德(des-CIC)。
后者具有显著的抗炎活性,可抑制炎性环索奈德气雾剂治疗成人支气管哮喘的有效性和安全性评价张颖何桦赵子文摘要目的:评价环索奈德气雾剂治疗成人支气管哮喘的临床疗效和安全性。
方法:72例轻、中度支气管哮喘患者随机分成两组,进行单盲、平行、阳性药(布地奈德)对照试验,治疗12周,以晨间PEF值作为主要评价指标,辅以夜间PEF值、FEV1值、ACQ评分、哮喘症状评分、缓解症状所需的万托林剂量等评价环索奈德的有效性;通过心电图、口咽部检查、实验室检查及不良事件数据评价环索奈德的安全性。
结果:治疗前、后试验组和对照组的晨间PEF值变化差异均有显著性(P<0.05),但组间差异无统计学意义(P>0.05);试验组和对照组夜间PEF、FEV1和ACQ数据有明显改善,所需万托林的剂量显著减少,哮喘症状评分明显好转,但组间差异无统计学意义(P>0.05)。
治疗的方法英语作文Title: Effective Treatments for Various Conditions。
Introduction:In recent years, the field of medicine has made significant advancements in developing effective treatments for various conditions. These treatments haverevolutionized healthcare, providing hope and relief to millions of people worldwide. This essay will explore some of the most popular and successful treatment methods, highlighting their benefits and impact on patients' lives.1. Pharmaceutical Treatments:Pharmaceutical treatments involve the use of medications to manage and cure diseases. These treatments have proven to be highly effective in combating a wide range of conditions. For instance, antibiotics are commonly used to treat bacterial infections, while antiviral drugsare effective against viral infections such as influenza. Furthermore, advancements in cancer research have led to the development of targeted therapies and immunotherapies, which have shown promising results in treating various types of cancer.2. Surgical Interventions:Surgical interventions are often necessary for conditions that cannot be managed through medication alone. Modern surgical techniques have greatly improved patient outcomes and recovery times. For example, minimally invasive surgeries, such as laparoscopic procedures, have become increasingly popular due to their reduced post-operative pain, shorter hospital stays, and quicker recovery periods. Additionally, organ transplantation has become a lifesaving treatment option for patients with end-stage organ failure.3. Physical Therapy:Physical therapy plays a vital role in therehabilitation of individuals with physical injuries or disabilities. It involves the use of exercises and techniques to improve mobility, strength, and overall function. Physical therapy is commonly employed after surgeries, accidents, or strokes. This treatment method helps patients regain their independence and enhance their quality of life. It can also alleviate chronic pain and prevent further complications.4. Psychological Therapies:Psychological therapies focus on addressing mental health conditions and improving emotional well-being. These therapies encompass various approaches, includingcognitive-behavioral therapy, psychoanalysis, and group therapy. They provide individuals with a safe space to explore their emotions, develop coping mechanisms, and overcome psychological challenges. Psychological therapies have proven to be highly effective in treating conditions such as depression, anxiety disorders, and post-traumatic stress disorder.5. Complementary and Alternative Medicine (CAM):Complementary and alternative medicine refers to treatment methods that are used alongside conventional medicine. These include practices such as acupuncture, herbal medicine, and yoga. While the effectiveness of CAM treatments may vary, many individuals find them beneficial in managing chronic pain, reducing stress, and improving overall well-being. However, it is important to note that CAM treatments should be used in conjunction with, rather than as a replacement for, evidence-based medical treatments.Conclusion:The development of effective treatments has significantly improved healthcare outcomes and provided hope to countless individuals. Pharmaceutical treatments, surgical interventions, physical therapy, psychological therapies, and complementary and alternative medicine all play crucial roles in managing and curing various conditions. By combining these approaches, healthcareprofessionals can provide comprehensive and personalized care to patients, ensuring the best possible outcomes.。
Blood Purif 2009;27:114–126 DOI:10.1159/000167018T he Cardiorenal Syndrome Claudio Ronco a Chang-Yin Chionh a Mikko Haapio b Nagesh S. Anavekar cAndrew House e Rinaldo Bellomo da D epartment of Nephrology, Ospedale San Bortolo, V icenza , Italy;b H UCH Meilahti Hospital, Division of Nephrology, H elsinki , Finland;c D epartment of Cardiology, The Northern Hospital, and d Department of IntensiveCare, Austin Hospital, M elbourne , Vic., Australia; eL ondon Health Sciences Centre, Division of Nephrology,London,Ont.,Canadadisease (e.g. chronic glomerular disease) contributing to de-creased cardiac function, cardiac hypertrophy and/or in-creased risk of adverse cardiovascular events. Type V CRS re-flects a systemic condition (e.g. diabetes mellitus, sepsis) causing both cardiac and renal dysfunction. Biomarkers can help to characterize the subtypes of the CRS and to indicatetreatment initiation and effectiveness. The identification of patients and the pathophysiological mechanisms underly-ing each syndrome subtype will help to understand clinicalderangements, to make the rationale for management strat-egies and to design future clinical trials with accurate selec-tion and stratification of the studied population. C opyright © 2009 S. Karger AG, Basel IntroductionA large proportion of patients admitted to hospital, especially in the critical care setting, have various degrees of heart and kidney dysfunction [1] . Primary disorders of one of these two organs often result in secondary dys-function or injury to the other [2] . Such pathophysiolog-ical interactions represent the pathophysiological basis for a clinical entity often referred to as the cardiorenal syndrome (CRS) [3] . Although generally defined as a con-dition characterized by the initiation and/or progression of renal insufficiency secondary to heart failure [4],the term ‘cardiorenal syndrome’ is also often used to describeKey Words A cute kidney injury ؒ Acute heart failure ؒ Chronic kidney disease ؒ Cardiorenal syndrome ؒ Renocardiac syndrome ؒHeart-kidney interaction ؒ Cardiovascular risk Abstract T he term ‘cardiorenal syndrome’ (CRS) has increasingly been used in recent years without a constant meaning and a well-accepted definition. To include the vast array of interrelatedderangements, and to stress the bidirectional nature of the heart-kidney interactions, the classification of the CRS today includes 5 subtypes whose etymology reflects the primary and secondary pathology, the time frame and simultaneous cardiac and renal codysfunction secondary to systemic dis-ease. The CRS can generally be defined as a pathophysiolog-ical disorder of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chron-ic dysfunction in the other organ. Type I CRS reflects an abrupt worsening of cardiac function (e.g. acute cardiogen-ic shock or decompensated congestive heart failure) leading to acute kidney injury. Type II CRS describes chronic abnor-malities in cardiac function (e.g. chronic congestive heart failure) causing progressive and permanent chronic kidney disease. Type III CRS consists in an abrupt worsening of renal function (e.g. acute kidney ischemia or glomerulonephritis) causing acute cardiac disorder (e.g. heart failure, arrhythmia, ischemia). Type IV CRS describes a state of chronic kidneyP ublished online: January 23, 2009the negative effects of reduced renal function on the heartand circulation (more appropriately named renocardiacsyndrome)[5] . Unfortunately, despite the frequent use of these terms in the literature, there is no consensus defini-tion or classification for this condition or cluster of con-ditions. The absence of a clear definition and the com-plexity of heart and kidney interactions contribute to alack of clarity with regard to diagnosis and management[6] . This is unfortunate as recent advances in basic and clinical sciences have changed our understanding of or-gan crosstalk and interactions and have demonstrated that some therapies can have efficacy in attenuating both cardiac and renal injury [7] . All these considerations sug-gest the need for a more clearly articulated definition of the subtypes of the CRS in terms of clinical presentation,pathophysiology, diagnosis and management[5, 6].In this article, we examine the nature of this complex clini-cal entity and discuss salient aspects of this condition and potential interventions based on a logical approach to thedefinition of its different clinical subtypes.C RS: A Proposed DefinitionT he common understanding of the CRS is that a rela-tively normal kidney is dysfunctional because of a dis-eased heart [8] with the assumption that in the presence of a healthy heart, the same kidney would likely function relatively normally[9] . This concept, however, has re-cently been challenged and a more articulated definition for the CRS has been proposed [5, 6] .Heart-kidney inter-actions include a variety of conditions, either acute or chronic, where the primary failing organ can be eitherthe heart or the kidney ( f ig. 1, 2 )[10] . For this reason, we discuss the different heart-kidney interactions, which fallunder the umbrella of the CRS, using the definition struc-ture summarized in t able 1[5, 6] .Cardiovascular mortality increased by end-stage renal dysfunction Cardiovascular risk increased by kidney dysfunction Chronic HF progression due to kidney dysfunction •Uremia-related HF •Volume-related HFHF due to acute kidney dysfunction •Volume/uremia-induced HF •Renal ischemia-induced HF •Sepsis/cytokin-induced HFCKD secondary to HFAKI secondary to contrast-induced nephropathy AKI secondary to cardiopulmonary bypass AKI secondary to heart valve replacement AKI secondary to HFF ig . 1. Heart and kidney interactions.HF = Heart failure; CKD = chronic kidney disease.F ig. 2. The bidirectional nature of the CRS and the acute or chron-ic temporal characteristics of the syndrome.C o l o r v e r s i o n a v a i l a b l e o n l i n eA major problem with previous terminology is that it does not allow clinicians or investigators to identify and fully characterize the relevant pathophysiological inter-actions. This is important because such interactions dif-fer according to the type of combined heart/kidney disorder[11] . F or example, while a diseased heart has n umerous negative effects on kidney function, renal in-sufficiency can also significantly impair cardiac function [10] . Thus, a large number of direct and indirect effects of each organ dysfunction can initiate and perpetuate the combined disorder of the two organs through a complex combination of neurohumoral feedback mechanisms.F or this reason, a subdivision into different subtypes seems to provide a more concise and logically correct ap-proach to this condition. We will use such a subdivision to discuss several issues of importance in relation to this syndrome.C RS Type I (Acute CRS)T ype I CRS or acute CRS is characterized by a rapid worsening of cardiac function, which leads to acute kid-ney injury (AKI) ( f ig. 3 ). Acute heart failure (AHF) may then be divided into 4 main subtypes [12]:hypertensive pulmonary edema with preserved left ventricular systol-ic function, acute decompensated chronic heart failure (ADCHF), cardiogenic shock, and predominant right ventricular failure. Type I CRS is common. More than one million patients in the USA alone are admitted to hospital every year with either de novo AHF or with ADCHF[12] . Among patients with ADCHF or de novo AHF, premorbid chronic renal dysfunction is common and predisposes to AKI [13, 14] . The mechanisms by which the onset of AHF or ADCHF leads to AKI are mul-tiple and complex [4] . They are broadly described in a previous publication [6] . The clinical importance of each of these mechanisms is likely to vary from patient to pa-tient (e.g. acute cardiogenic shock vs. hypertensive pul-monary edema) and situation to situation (AHF second-ary to perforation of a mitral valve leaflet from acute bac-terial endocarditis vs. worsening right heart failure secondary to noncompliance with diuretic therapy). In AHF, AKI seems to be more severe in patients with im-paired left ventricular ejection fraction (LVEF) compared to those with preserved LVEF [15] and increasingly worse when LVEF is further impaired. It achieves an incidence of 170% in patients with cardiogenic shock [16].F urther-more, impaired renal function is consistently found as an independent risk factor for 1-year mortality in AHF pa-tients, including in patients with ST-elevation myocar-dial infarction [16, 17] . A plausible reason for this inde-pendent effect might be that an acute decline in renal function does not simply act as a marker of illness sever-ity, but also carries an associated acceleration in cardio-vascular pathobiology leading to a higher rate of cardio-vascular events both acutely and chronically, possibly through the activation of inflammatory pathways [9, 18] .T he salient clinical issues of type I CRS relate to how the onset of AKI (de novo or in the setting of chronic re-nal impairment) induced by primary cardiac dysfunction impacts on diagnosis, therapy and prognosis and how its presence can modify the general approach to the treat-ment of AHF or ADCHF. The first important clinical principle is that the onset of AKI in the setting of AHF or ADCHF implies inadequate renal perfusion until proven otherwise. This should prompt clinicians to consider the diagnosis of a low cardiac output state and/or marked in-crease in venous pressure leading to kidney congestion and take the necessary diagnostic steps to either confirm or exclude the diagnosis (careful physical examination looking for ancillary signs and laboratory findings of a low cardiac output state such as absolute or relative hypo-tension, cold extremities, poor postcompressive capillaryTable 1. Proposed definitions of CRS(1) CRS general definition: a pathophysiological disorder of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction in the other or-gan(2) CRS type I (acute CRS): abrupt worsening of cardiac function(e.g. acute cardiogenic shock or decompensated congestive heart failure) leading to AKI(3) CRS type II (chronic CRS): chronic abnormalities in cardiac function (e.g. chronic congestive heart failure) causing progres-sive and permanent chronic kidney disease(4) CRS type III (acute renocardiac syndrome): abrupt worsening of renal function (e.g. acute kidney ischemia or glomerulone-phritis) causing acute cardiac disorder (e.g. heart failure, arrhyth-mia, ischemia)(5) CRS Type IV (chronic renocardiac syndrome): chronic kidney disease (e.g. chronic glomerular disease) contributing to de-creased cardiac function, cardiac hypertrophy and/or increased risk of adverse cardiovascular events(6) CRS type V (secondary CRS): systemic condition (e.g. diabetes mellitus, sepsis) causing both cardiac and renal dysfunctionrefill, confusion, persistent oliguria, distended jugular veins, elevated or rising lactate). The second important consequence of the development of type I CRS is that it may decrease diuretic responsiveness. In a congestive state (peripheral edema, increased body weight, pulmo-nary edema, elevated central venous pressure), decreased response to diuretics can lead to failure to achieve the de-sired clinical goals. The physiological phenomena of d i-uretic breaking(diminished diuretic effectiveness sec-ondary to postdiuretic sodium retention) [19]and postdi-uretic sodium retention[20] may also play an enhanced part in this setting. In addition, concerns of aggravating AKI by the administration of diuretics at higher doses or in combination are common among clinicians. Such con-cerns can also act as an additional, iatrogenic mechanism equivalent in its effect to that of diuretic resistance (less sodium removal). Accordingly, diuretics may best be giv-en in AHF patients with evidence of systemic fluid over-load with the goal of achieving a gradual diuresis. Furo-semide can be titrated according to renal function, sys-tolic blood pressure and history of chronic diuretic use. High doses are not recommended and a continuous di-uretic infusion might be helpful [21] . In parallel, mea-surement of cardiac output and venous pressure may also help ensure continued and targeted diuretic therapy. Ac-curate estimation of cardiac output can now be easily achieved by means of arterial pressure monitoring com-bined with pulse contour analysis or by Doppler ultra-sound [22–25] . Knowledge of cardiac output allows phy-sicians to develop a physiologically safer and more logical approach to the simultaneous treatment of AHF and AD-CHF and AKI. If diuretic resistant fluid overload exists despite an optimized cardiac output, removal of isotonic fluid can be achieved by ultrafiltration ( f ig. 4 ). This ap-proach can be efficacious and clinically beneficial [26]. The presence of AKI with or without concomitant hyper-kalemia may also affect patient outcome by inhibiting the prescription of angiotensin-converting enzyme (ACE) inhibitors and aldosterone inhibitors (drugs that have been shown in large randomized controlled trials to in-crease survival in the setting of heart failure and myocar-dial infarction) [27] . This is unfortunate because, provid-ed there is close monitoring of renal function and potas-sium levels, the potential benefits of these interventions likely outweigh their risks even in these patients.T he acute administration of -blockers in the setting of type I CRS is generally not advised. Such therapy should wait until the patient has stabilized physiologi-cally and concerns about a low cardiac output syndrome have been resolved. In some patients, stroke volume can-not be increased and relative or absolute tachycardia sus-tains the adequacy of cardiac output. Blockade of such compensatory tachycardia and sympathetic system-de-pendent inotropic compensation can precipitate cardio-genic shock and can be lethal [28] . Particular concern applies to -blockers excreted by the kidney such as aten-olol or sotalol, especially if combined with calcium an-tagonists [29] . These considerations should not inhibit the slow, careful and titrated introduction of appropriate treatment with -blockers later on, once patients are he-modynamically stable.T his aspect of treatment is particularly relevant in pa-tients with the CRS where evidence suggests that under-treatment after myocardial infarction is common [30]. Attention should be paid to preserving renal function, perhaps as much attention as is paid to preserving myo-cardial muscle. Worsening renal function (WRF) during admission for ST-elevation myocardial infarction is a Humorally mediated damageExogenous factorsDrugsHormonal factorsF ig. 3.Diagram illustrating and summa-rizing the major pathophysiological inter-actions between the heart and kidney in type I CRS.powerful and independent predictor of in-hospital and 1-year mortality [16, 17] . In a study involving 1,826 pa-tients who received percutaneous coronary intervention, even a transient rise in serum creatinine ( 125% com-pared to baseline) was associated with increased hospital stay and mortality [31] . Similar findings have also been shown among coronary artery bypass graft cohorts [32]. In this context, creatinine rise is not simply a marker of illness severity but it rather represent a causative factor for cardiovascular injury acceleration through the activa-tion of hormonal, immunological and inflammatory pathways [9, 18] .G iven that the presence of type I CRS defines a popu-lation with high mortality, a prompt, careful, systematic, multidisciplinary approach involving invasive cardiolo-gists, nephrologists, critical care physicians and cardiac surgeons is both logical and desirable.C RS Type II (Chronic CRS)T ype II CRS or chronic CRS is characterized by chron-ic abnormalities in cardiac function (e.g. chronic conges-tive heart failure) causing progressive chronic kidney in-sufficiency ( f ig. 5 ).W RF in the context of heart failure is associated with significantly increased adverse outcomes and prolonged hospitalizations [33] . The prevalence of renal dysfunction in chronic heart failure has been reported to be approxi-mately 25% [33] . Even limited decreases in estimated glo-merular filtration rate (GF R) of 19 ml/min appear to confer a significantly increased mortality risk [33].Some researchers have considered WRF a marker of severity of generalized vascular disease [33].Independent predictors of WRF include: old age, hypertension, diabetes mellitus and acute coronary syndromes.PbF ig. 4.Diagram presenting the technical features of ultrafiltration as applicable to patients with AHF and di-uretic-resistant fluid overload.T he mechanisms underlying WRF likely differ based on acute versus chronic heart failure. Chronic heart fail-ure is characterized by a relatively stable long-term situ-ation of probably reduced renal perfusion, often predis-posed by both micro- and macrovascular disease in the context of the same vascular risk factors associated with cardiovascular disease. However, although a greater pro-portion of patients with a low estimated GFR have a worse New York Heart Association class, no evidence of an as-sociation between LVEF and estimated GFR can be con-sistently demonstrated. Thus, patients with chronic heart failure and preserved LVEF appear to have a similar esti-mated GFR to patients with impaired LVEF ( !45%)[34].Neurohormonal abnormalities are present with excessive production of vasoconstrictive mediators (epinephrine, angiotensin, endothelin) and altered sensitivity and/or release of endogenous vasodilatory factors (natriuretic peptides, nitric oxide). Pharmacotherapies used in the management of heart failure have been touted as contrib-uting to WRF. Diuresis-associated hypovolemia, earlyi ntroduction of renin-angiotension-aldosterone system blockade, and drug-induced hypotension have all beensuggested as contributing factors[4] . However, their role remains highly speculative. More recently, there has been increasing interest in the pathogenetic role of relative or absolute erythropoietin deficiency contributing to a more pronounced anemia in these patients than might be ex-pected for renal failure alone[35] . Erythropoietin recep-tor activation in the heart may protect from apoptosis, fibrosis and inflammation. In keeping with such experi-mental data, preliminary clinical studies show that eryth-ropoietin administration in patients with chronic heart failure, chronic renal insufficiency and anemia leads to improved cardiac function, reduction in left ventricularsize and lowering of B-type natriuretic peptide[36].Pa-tients with type II CRS are more likely to receive loop diuretics and vasodilators and also to receive higher dos-es of such drugs compared to those with stable renalfunction[37] . Treatment with these drugs may partici-pate in the development of renal injury. However, such therapies may simply identify patients with severe hemo-dynamic compromise and thus a predisposition to renal dysfunction rather than being responsible for worsening renal dysfunction. Regardless of the cause, reductions inChronic hypoperfusionIncreased renal vasc. resist.Increased venous pressureLow cardiac outputSclerosis-fibrosisChronic hypoperfusion Necrosis-apoptosisLow cardiac outputSubclinical inflammation Endothelial dysfunction Accelerated atherosclerosisF ig. 5. Diagram illustrating and summarizing the major pathophysiological interactions between the heart and kidney in type II CRS. CKD = Chronic kidney disease.renal function in the context of heart failure are associ-ated with increased risk for adverse outcomes.T he Impact of the CRS on MedicationsT he proportion of individuals with chronic kidney dis-ease (CKD) receiving appropriate risk factor modification and/or interventional strategies is lower than the general population, a concept termed ‘therapeutic nihilism’ [38]. Many databases and registries have repeatedly shown that these therapeutic choices seem to parallel WRF [39–41]. Among patients with end-stage kidney disease (ESKD; CKD stage V), who are known to be at extreme risk, less than 50% are on a combination of aspirin, -blockers, ACE inhibitors and statins [42] . In a cohort involving over 140,000 patients, 1,025 with documented ESKD were less likely to receive aspirin, -blockers or ACE inhibitors af-ter myocardial infarction. Yet those ESKD patients who did receive the aspirin, -blocker and ACE inhibitor com-bination had similar risk reductions in 30-day mortality when compared to non-ESKD patients who had received conventional therapy [41] . This failure to treat is not just limited to ESKD patients. Patients with less severe forms of CKD are also less likely to receive risk-modifying med-ications following myocardial infarction compared to their normal renal function counterparts.P otential reasons for this therapeutic failure include concerns about WRF, and/or therapy-related toxic effects due to low clearance rates [43, 44].Bleeding concerns with the use of platelet inhibitors and anticoagulants are especially important with reduced renal function and ap-pear to contribute to the decreased likelihood of patients with severe CKD receiving aspirin and/or clopidrogrel despite the fact that such bleeding is typically minor and the benefits sustained in these patients [45].However, several studies have shown that when appropriately ti-trated and monitored, cardiovascular medications used in the general population can be safely administered to those with renal impairment and with similar benefits [42, 44, 46] .N ewer approaches to the treatment of cardiac failure such as cardiac resynchronization therapy have not yet been studied in terms of their renal functional effects, although preserved renal function after cardiac resyn-chronization therapy may predict a more favorable out-come [47] . Vasopressin V2 receptor blockers have been reported to decrease body weight and edema in patients with chronic heart failure [48] , but their effects in pa-tients with the CRS have not been systematically studied and a recent large randomized controlled trial showed no evidence of a survival benefit with these agents [49] .C RS Type III (Acute Renocardiac Syndrome)T ype III CRS or acute renocardiac syndrome is char-acterized by an abrupt and primary worsening of renal function (e.g. AKI, ischemia or glomerulonephritis) which then causes or contributes to acute cardiac dys-function (e.g. heart failure, arrhythmia, ischemia). The pathophysiological aspects are summarized in f igure 6 .T he development of AKI as a primary event leading to cardiac dysfunction (type III CRS) is considered less common than type I CRS. This is partly because, unlike type I CRS, it has not been systematically considered or studied. However, AKI is a condition with a growing in-cidence in hospital and intensive care unit patients. Using the recent RIF LE consensus definitions and its Injury and Failure categories, AKI has been identified in close to 9% of hospital patients [50] and, in a large intensive care unit database, AKI was observed in more than 35% of critically ill patients [51] . AKI can affect the heart through several pathways whose hierarchy is not yet es-tablished. Fluid overload can contribute to the develop-ment of pulmonary edema. Hyperkalemia can contribute to arrhythmias and may cause cardiac arrest. Untreated uremia affects myocardial contractility through the ac-cumulation of myocardial depressant factors [52]and can cause pericarditis [53] . Partially corrected or uncorrected acidemia produces pulmonary vasoconstriction [54], which, in some patients, can significantly contribute to right-sided heart failure. Acidemia appears to have a neg-ative inotropic effect [55] and may, together with electro-lyte imbalances, contribute to an increased risk of ar-rhythmias [56] . Finally, as discussed above, renal isch-emia itself may precipitate activation of inflammation and apoptosis at cardiac level [9] .T he development of AKI, especially in the setting of chronic renal failure, can affect the use of medications that normally would maintain clinical stability in pa-tients with chronic heart failure. For example, an increase in serum creatinine from 1.5 mg/dl (130 m ol/l) to 2 mg/ dl (177 m ol/l), with diuretic therapy and ACE inhibi-tors, may provoke some clinicians to decrease or even stop diuretic prescription; they may also decrease or even temporarily stop ACE inhibitors. In some, maybe many cases, this may not help the patient. An acute decompen-sation of chronic heart failure may occur because of such changes in medications. When this happens the patient may be unnecessarily exposed to an increased risk of acute pulmonary edema or other serious complications of undertreatment.F inally, if AKI is severe and renal replacement therapy is necessary, cardiovascular instability generated by rap-id fluid and electrolyte shifts secondary to conventional dialysis can induce hypotension, arrhythmias, and myo-cardial ischemia [57] . Continuous techniques of renal re-placement, which minimize such cardiovascular insta-bility appear physiologically safer and more logical in thissetting[58] . C RS Type IV (Chronic Renocardiac Syndrome)Type IV CRS or chronic renocardiac syndrome is characterized by primary CKD (e.g. diabetes or chronic glomerular disease) contributing to decreased cardiac function, ventricular hypertrophy, diastolic dysfunction and/or increased risk of adverse cardiovascular events ( f ig. 7 ).T he National Kidney Foundation divides CKD into 5 stages based on a combination of severity of kidney dam-age and GF R[59] . Individuals with CKD, particularly those receiving renal replacement therapies, are at ex-tremely high cardiovascular risk[60] . About 50% of deaths in CKD stage V cohorts are attributed to cardio-vascular disease; namely coronary artery disease and itsassociated complications[54] . The 2-year mortality rate following myocardial infarction in patients with CKDstage V is high and estimated to be 50%[61].In compar-ison, the 10-year mortality rate after myocardial infarc-tion for the general population is 25%.T ype IV CRS is becoming a major public health prob-lem. A large population of individuals entering the tran-sition phase towards ESKD is emerging. National Kidney Foundation guidelines define these individuals as havingCKD[62] . CKD, which also encompasses ESKD, is de-fined as persistent kidney damage (confirmed by renal biopsy or markers of kidney damage) and/or a GF R!60ml/min/1.73m 2 for more than 3 months [59].This translates into a serum creatinine level of 61.3 mg/dl which would ordinarily be dismissed as not being repre-sentative of significant renal dysfunction. Using these criteria, current estimates of CKD account for at least 11million individuals and rising[63] . T he association between increased cardiovascular risk and renal dysfunction originally stemmed from data arising from ESKD or stage V CKD cohorts. The leading cause of death in such patients is cardiovascular with 1 40% of mortality being cardiovascular event related. This observation is supported by the Australian and New Zealand Dialysis and Transplant Registry, the United States Renal Data System and the Wave 2 Dialysis Mor-bidity and Mortality Study. Based on these findings, it is now well established that CKD is a significant risk factor for cardiovascular disease, such that individuals with ev-idence of CKD have between a 10- to 20-fold increased risk for cardiac death compared to age-matched and sex-matched controls without CKD[63] . As discussed, part of this problem may be related to the fact that such indi-viduals are also less likely to receive risk-modifying inter-ventions compared to their non-CKD counterparts[61, 64, 65].F ig. 6. Diagram illustrating and summa-rizing major pathophysiological interac-tions between the heart and kidney in type III CRS. RAA = Renin-angiotensin-aldo-sterone.。
肠道菌群对天然药物活性成分的生物转化郑艺璇;李国玉【摘要】目的:探究肠道菌群与天然药物生物转化及其代谢产物的关系,为研制生物利用度高的药物提供参考.方法:通过总结人肠道菌群及天然药物生物转化的研究情况,简述天然药物肠道菌群作用下的代谢和生物转化过程,总结不同种类天然药物的生物转化规律.结果:列举了苷类,黄酮类,苯丙素类,有机酸类等成分肠道菌代谢的研究,总结了肠道菌群对天然药物成分的生物转化规律.结论:肠道菌群对天然药物的生物转化主要以水解为主,大多数苷类成分经肠菌代谢为苷元或小分子物质后提高了生物利用度.【期刊名称】《中医药信息》【年(卷),期】2016(033)005【总页数】4页(P122-125)【关键词】肠道菌群;天然药物代谢产物;生物转化;微生物发酵【作者】郑艺璇;李国玉【作者单位】哈尔滨医科大学药学院,黑龙江哈尔滨150081;哈尔滨医科大学药学院,黑龙江哈尔滨150081【正文语种】中文【中图分类】R28肠道菌群构成了肠道的微生物环境,肠道菌群在不同个体中存在着差异性。
近年来的研究表明[1-2],个体肠道菌群的差异性有时与疾病存在相关性。
更重要的是,个体肠道菌群的差异性还会影响人体对药物的吸收利用,体现在对药物的生物转化方面,直接影响药物的生物利用度,进而影响药物对疾病的治疗。
随着天然药物在临床应用的愈加广泛,加之天然药物成分复杂,阐明肠道菌群与天然药物活性成分的生物转化关系,对天然药物的临床应用及天然药物的研发具有一定的参考价值。
生物转化,实质上是一种酶催化反应[3],具有成本较低、污染较小、条件温和以及副产物少的优点,同时它还有较高的立体选择性,能够获得很难通过化学合成得到的产物[4]。
药物在机体内发生化学结构的转变称为药物生物转化,即药物代谢[5]。
研究表明[6],人体肠道菌群的代谢活性与药物发挥疗效之间存在着密切的联系。
人体的肠道菌群对于天然药物的生物转化是复杂而又多样的,包括脱甲基[7]、脱羟基[8]、水解反应[9]、氧化还原反应[10-11]等,详见图1。
1.Define the following terms briefly.With example if you need.2.action researchAction research is a mode of inquiry undertaken by teachers and is more oriented to instructor and learner development than it is to theory building, although it can be used for the latter.‘Action research’is a generic term for a family of related methods that share some important common principles.Action research is conducted by or in cooperation with teachers for the purpose of gaining a better understanding of their educational environment and improving the effectiveness of their teaching.2.construct validityThis is perhaps the most complex of the validity types discussed so far.In research, construct validity refers to the degree to which the research adequately captures the construct of interest.Construct validity can be enhanced when multiple estimates of a construct are used.3.criterion-referenced test标准参照测验(Criterion-Referenced Test)又称准则参照测验。
USP30-1211翻译-灭菌(miè jūn)和无菌保证USP30-1211翻译(fānyì)-灭菌和无菌保证1211 STERILIZATION AND STERILITY ASSURANCE OF COMPENDIAL ARTICLES灭菌(miè jūn)和无菌保证纲要条款This informational chapter provides a general description of the concepts and principles involved in the quality control of articles that must be sterile. Any modifications of or variations in sterility test procedures from those described under Sterility Tests 71 should be validated in the context of the entire sterility assurance program and are not intended to be methods alternative to those described in that chapter.报告章节规定涉及到条款质量控制总的概念(gàiniàn)描述和原则是必须是无菌的.从无菌测试<71>的章节描述中,无菌保证程序的整个上下文中规定没有可选择的方法,任何有关无菌测试程序变更或修改应该(yīnggāi)得到验证.Within the strictest definition of sterility, a specimen would be deemed sterile only when there is complete absence of viable microorganisms from it. However, this absolute definition cannot currently be applied to an entire lot of finished compendial articles because of limitations in testing. Absolute sterility cannot be practically demonstrated without complete destruction of every finished article.在最严格的无菌定义里,仅当它不含有任何可存的微生物,样品才被认为无菌.然而, 因为测试的局限性,这个绝对的定义不能普遍应用到整个纲要条款中。
第42 卷第 5 期2023 年5 月Vol.42 No.5641~646分析测试学报FENXI CESHI XUEBAO(Journal of Instrumental Analysis)高效液相色谱法同时测定化妆品中辣椒碱等9种热感剂吴志珊1,2,吴姣娇1,2,尹伟成1,2,殷帅1,2,李卓芳2,姜成君1*(1.湖南省药品检验检测研究院,湖南长沙410001;2.岳阳市食品药品检验所,湖南岳阳414000)摘要:建立了测定化妆品中辣椒碱等9种热感剂的高效液相色谱法。
样品经80%甲醇超声提取后,过滤,以乙腈-0.5%甲酸水溶液为流动相,采用SymmetryShield TM RP18色谱柱(250 mm × 4.6 mm,5 μm)分离,液相色谱分离,二极管阵列检测器进行检测。
在优化实验条件下,9种热感剂的分离度好,专属性高,其质量浓度在0.2 ~ 100 μg/mL范围内与峰面积呈良好线性关系,相关系数(r2)均不小于0.999 5,检出限(LOD)为0.001 0 ~ 0.003 4 mg/kg。
以水基类、乳剂类、膏霜类3种阴性样品作为空白基质,9种热感剂在0.004、0.02、1 mg/kg 3种加标水平下的回收率为75.6% ~ 115%,相对标准偏差(RSD)为0.083% ~ 7.0%。
该方法专属性强、灵敏度高、准确度好,可用于化妆品中9种热感剂含量的测定。
关键词:热感剂;化妆品;高效液相色谱法(HPLC)中图分类号:O657.72;S641.3文献标识码:A 文章编号:1004-4957(2023)05-0641-06Simultaneous Determination of 9 Self-heating Compounds Including Capsaicin in Cosmetics by High PerformanceLiquid ChromatographyWU Zhi-shan1,2,WU Jiao-jiao1,2,YIN Wei-cheng1,2,YIN Shuai1,2,LI Zhuo-fang2,JIANG Cheng-jun1*(1.Hunan Institute for Drug Control,Changsha 410001,China;2.Food andDrug Inspection in Yueyang,Yueyang 414000,China)Abstract:A high performance liquid chromatographic(HPLC) method was established for the determi⁃nation of 9 self-heating compounds,including capsaicin in cosmetics.The samples were ultrasonically extracted with 80% methanol,and then filtered.The target compounds were separated on a Symme⁃tryShield TM RP18(250 mm × 4.6 mm,5 μm) with a mobile phase consisting of acetonitrile and 0.5% formic acid by gradient elution,and analyzed by HPLC with a PDA detector.Under the optimal condi⁃tions,good linear relationships were obtained for nine compounds in the concentration range of 0.2-100 μg/mL,with correlation coefficients(r2) not less than 0.999 5.The limits of detection(LODs)were in the range of 0.001 0-0.003 4 mg/kg.The spiked recoveries for water,lotion and cream ma⁃trixes at three levels of 0.004,0.02,1 mg/kg ranged from 75.6% to 115%,with relative standard de⁃viations(RSDs,n = 3) of 0.083%-7.0%.This method is accurate and sensitive,and is suitable for the qualitative and quantitative analysis of 9 self-heating compounds in cosmetics.Key words:self-heating compounds;cosmetics;high performance liquid chromatography(HPLC)近年来,随着人们审美要求的提高,消费者越来越注重自身形象和外表,具有健美功效的化妆品越来越受青睐。
与此同时的英语短语高级表达Simultaneously, concurrently, at the same time, in tandem, side by side, contemporaneously, in parallel, interchangeably, hand in hand, synchronously, in unison, coincidentally, mutually, and in the meantime are all advanced English phrases that can be used to express the idea of "at the same time" or "simultaneously."Choosing the most appropriate phrase depends on the context and the tone of the writing. For example, "simultaneously" and "concurrently" are often used in scientific or technical writing to describe events that occur together. "At the same time" is a more informal and widely used phrase that can be used in most contexts. "In tandem" and "side by side" suggest a协作 or并进的关系, while "contemporaneously" and "in parallel" suggest a parallel or simultaneous occurrence.Here are a few examples of how these phrases can be used in sentences:1. The researchers conducted multiple experiments simultaneously to test the effectiveness of the new drug.2. The company launched its new product and updated its website concurrently to maximize exposure.3. She was studying for her exams and working on apart-time job at the same time.4. The two organizations worked in tandem to organize the event.5. The runners sprinted side by side, neck and neck until the final stretch.6. The artist created several paintings contemporaneously, each reflecting a different mood.7. The two research teams are working in parallel on similar projects but with different approaches.8. The government implemented new policies interchangeably to address the economic crisis.9. The dancers moved hand in hand, gracefully choreographed in perfect sync.10. The clock's hands moved synchronously, marking the passing of time.11. The choir sang in unison, their voices blending harmoniously together.12. The accident occurred coincidentally with the start of the new traffic regulations.13. The two companies entered into a mutual agreement to share resources and expertise.14. In the meantime, the team continued to brainstorm new ideas for the project.These phrases add sophistication and variety to yourwriting, allowing you to express complex ideas and relationships more precisely. However, it's important to use them appropriately and not overuse them, as excessive use can make the writing sound unnatural or contrived.。
ORIGINAL ARTICLEPrevalence of hypertension and dyslipidemia and their associations with micro-and macrovascular diseases in patients with diabetes in Taiwan:An analysis of nationwide data for 2000e 2009Li-Nien Tseng a ,b ,i ,Yao-Hsien Tseng a ,i ,Yi-Der Jiang c ,Chia-Hsuin Chang c ,d ,Ching-Hu Chung e ,Boniface J.Lin f ,Lee-Ming Chuang c ,d ,Tong-Yuan Tai g ,**,Wayne H.-H.Sheu a ,b ,h ,*aDepartment of Internal Medicine,Taichung Veterans General Hospital,Taichung,Taiwan bSchool of Medicine,Chung Shan Medical University,Taichung,Taiwan cDepartment of Internal Medicine,National Taiwan University Hospital,Taipei,Taiwan dGraduate Institute of Preventive Medicine,National Taiwan University,School of Public Health,Taipei,Taiwan eDepartment of Pharmacology,Tzu Chi University,Hualien,Taiwan fSt.Mary’s Hospital,Taitung,Taiwan gTaipei Jen-Chi Relief Institute,Taipei,Taiwan hSchool of Medicine,National Yang-Ming University,Taipei,TaiwanReceived 16August 2012;received in revised form 5September 2012;accepted 6September 2012KEYWORDScardiovascular disease;cerebrovascular disease;diabetes;dyslipidemia;microvascular diseasesBackground/Purpose:Cardiovascular complication is the leading cause of mortality in patients with diabetes.Dyslipidemia and hypertension are the major risk factors contributing to cardio-vascular disease (CVD).This study was carried out to investigate the prevalence of dyslipide-mia and hypertension and their associations with microvascular and macrovascular complications in patients with type 2diabetes in Taiwan.Methods:Health-care data and diagnostic codes were retrieved from the Taiwan Bureau of National Health Insurance claims files for the years 2000e 2009.Based on these data the annual prevalences of dyslipidemia and hypertension were calculated and patients were stratified by age,gender,and diabetic complications.*Corresponding author.Department of Internal Medicine,Taichung Veterans General Hospital,Number 160,Section 3,Chung Kang Road,Taichung 407,Taiwan.**Corresponding author.Taipei Jen-Chi Relief Institute,200Guangzhou Street,Taipei,Taiwan.E-mail addresses:tytai@.tw (T.-Y.Tai),whhsheu@.tw (W.H.-H.Sheu).iThese authors contributed equally to this study.0929-6646/$-see front matter Copyright ª2012,Elsevier Taiwan LLC &Formosan Medical Association.All rights reserved./10.1016/j.jfma.2012.09.010Available online atjournal homepage:Journal of the Formosan Medical Association (2012)111,625e 636IntroductionThe number of people with diabetes mellitus worldwide is soaring with the largest number,an estimated131.9 million,reported in the Western Pacific region.1The number of cases with diabetes in Taiwan is also increasing. According to the claims database of the Taiwan National Health Insurance(NHI)program,the age-standardized prevalence of diabetes in Taiwan increased from4.7%to 6.5%for men and from5.3%to6.6%for women between 1999and2004.2Type2diabetes is associated with significant morbidity and mortality due to cardiovascular complications.3Dysli-pidemia,an established risk factor for cardiovascular disease(CVD),affects almost50%of the patients with type 2diabetes in the United States.4In addition to hypergly-cemia and hypertension,dyslipidemia is a modifiable CVD risk factor that remains largely uncontrolled in patients with type2diabetes.5Hypertension is another major modifiable risk factor of CVD.In Taiwan,more than50%of the elderly people are hypertensive.6In the United States,approximately75%of patients with diabetes have concomitant hypertension.7 There is a significant amount of overlap between the complications of diabetes and hypertension,namely, systemic vascular diseases.Although advances have been made in the treatment of diabetic complications,cardiovascular complications are still the leading cause of mortality in people with diabetes. Macrovascular complications,including CVD,cerebrovas-cular disease(cerebrovascular accident or CVA),and peripheral vascular disease(PVD),are the most common causes of mortality in patients with diabetes.8Because different methodologies are used to access the complica-tions,there are wide demographic and geographical differences in the prevalence of macrovascular complica-tions among cohorts of patients with diabetes.8 To better understand the prevalence of dyslipidemia and hypertension along with macrovascular and microvascular complications in patients with diabetes and their trends in recent years,data from the claims database of the Taiwan NHI program from2000to2009were retrieved and analyzed.MethodsPatients and methodsData sourceA universal compulsory NHI program was initiated by the Taiwanese government in March1995.9It provided coverage for95%of the total population of22.3million in Taiwan in2000,with the coverage increasing to98%in2005 and99.6%rge computerized administrative and claims data sets derived from this program have been maintained on an ongoing basis by the Collaboration Center of Health Information Application,the Department of Health(DOH),Executive Yuan,and are made available to investigators for research purposes after personal health information is scrambled.The DOH Mortality Registry also scrambles personal data to link them with the NHI claimsdata.In this study,inpatient and outpatient claims data sets from2000to2009were used.This study was approved by the Institutional Review Board of National Taiwan University Hospital.Selection of casesThe diagnostic code250used for diabetes mellitus was based on the International Classification of Diseases,9th Revision with Clinical Modification(ICD-9-CM)coding system.Before June2000,an A code(A181)was used for outpatients only.For privacy reasons,NHRI provided data for only one-third of the randomly sampled patients who were identified as having been hospitalized or having made an ambulatory visit for diabetes(ICD-9-CM code250and A code A181)from2000to2009.Patients were classified as having diabetes and included in the analysis if they had at least one admission code of diabetes or three or more outpatient codes of diabetes within365calendar days.To avoid the inclusion of misdiagnosed patients,we used the aforementioned selection criteria every year.10The definition of dyslipidemia and hypertensionIf the eligible patients with diabetes had also prescribed an Anatomical Therapeutic Chemical code C10(lipid modifying agents)drug for disease treatment for either outpatient or inpatient care in index year,they were considered to have a diagnosis of dyslipidemia.If the eligible patients with diabetes who also had at least two diagnosis of hyperten-sion(ICD-9-CM:401e405and A code A26)for either outpatient or inpatient care within365calendar days,then they were considered to have a diagnosis of hypertension. Demographic characteristicsDemographic information such as patient’s age and gender were obtained directly from the Bureau of NHIfiles.The patient’s age was divided into three categories:<40, 40e65,and>65years.Diabetes-related complications defined using ICD-9,op,or A codes are listed below: (1)Eye diseases(1a)All kinds of eye disease:362.01,362.02,362.53,362.83, 364.42,379.23,369.xx,14.2x-14.5x,14.7(A232)(1b)Blindness and low vision:369.xx/photocoagulation14.23,14.24,14.25,14.33,14.34,14.35,14.53,14.54,14.55/surgery:14.21,14.22,14.26,14.27,14.29,14.31,14.32,14.39,14.4,14.51,14.52,14.59,14.7 (2)PVD(2a)All kinds of PVD:440.2x,443.9,84.1x,39.25,39.29,39.50,39.59(A300,A301,A302)(2b)Amputation of lower limb:84.1x(nontraumatic, excluding ICD800-999)/blood vessel bypass surgery:39.25,39.29,39.59/percutaneous transluminal angio-plasty(PTA)39.50(3)CVD(3a)All kinds of CVD:398.91,402,404,410,411,412,413, 414,428,36.xx,(A260,A27,A270,A25,A250,A251) (3b)Myocardial infarction(MI):410(acute MI),412(old MI)/coronary artery bypass graft(CABG)36.1x/percu-taneous transluminal coronary angioplasty(PTCA)36.01,36.02,36.05,00.66/stent36.06,36.07(4)Stroke (4a)All kinds of stroke:430,431,432,433,434,435,436, 785.9(A290e A294)(5)Kidney disease(5a)All kinds of nephropathy:250.4,403,404,585,586, 581.8x,791.0,593.9,v42.0,v45.1,v56.0,v56.8,39.27,39.42,39.43,39.49,39.50,39.53,39.93,39.94,39.95(A350)(5b)Chronic renal failure:585/renal transplantation V42.0/ dialysis39.95,v45.1,v56.0,v56.8,[CURE_ITEM_NO1-4]: D8(hemodialysis),D9(peritoneal dialysis)(6)Foot disease(6a)All kinds of foot infection:foot gangrene040.0, 440.24,785.4with250.7or440.2,440.21,440.22,and 440.23/foot osteomyelitis:730.07,730.17,730.27, 730.97,440.23,707.14,707.15,707.1/cellulitis or abscess of the foot:680.7,682.7,681.1,681.10(6b)Foot amputation(ICD-9-CM codes):V49.71e77;V52.1 and(ICD-9procedure codes):84.11e17Statistical analysisWe performed a trend analysis to investigate the trends of prevalence of hypertension and/or dyslipidemia among patients with type2diabetes stratified by gender and age from2000to2009.We also used Kendall tau-c coefficient to measure the strength of associations across the years2000, 2004,and2008in diabetic patients with hypertension/ dyslipidemia,and those with macrovascular and microvas-cular complications stratified by gender and age. ResultsAnalysis of claims data from the Taiwan NHI database showed that the prevalence of both hypertension and dys-lipidemia in patients with type2diabetes increased year by year from2000to2008(p for trend<0.001).The preva-lence of diabetes with hypertension plus dyslipidemia increased by more than twofold,from13.52%to31.01%in women and from10.47%to25.65%in men from2000to2008 (Table1).In both genders,the peak age for dyslipidemia was40e65years,while the peak age for hypertension was >65years(p for all trends<0.001)(Table1).Approximately10%of the patients with diabetes suffered from CVA between2000and2009with men having slightly predominant rates(Table2).The prevalence of stroke showed a steady decrease in both genders in the past 10years.The prevalence of CVD gradually decreased from 38.14%in2000to33.43%in2009(p for trend<0.001),but was higher in diabetic women(34.7%)than in diabetic men (32.2%)(Table3).The prevalence of PVD increased from 1.87%in2000to 2.47%in2009.There was no gender difference,and PVD was more likely to occur in elderly patients(Table4).For patients with diabetes who are diagnosed with several microvascular complications,including eye disease, low vision/blindness,all kinds of nephropathy,chronic renal failure/transplantation/dialysis,and all kinds of dialysis,the prevalence of dyslipidemia was relatively stable during the2000e2009study period,except in patients with eye disease and those in both genders whoPrevalence of hypertension and dyslipidemia in Taiwan diabetic patients627underwent dialysis (Table 5).Although the prevalence of diabetes plus dyslipidemia decreased in patients with CVD,including those with MI and CVA,it increased in patients with PVD from 2000to 2009(p for all trends <0.001)(Table 6).The prevalence of hypertension increased in patients with microvascular complications,including all kinds of retinopathy,patients (in both genders)on dialysis,and in men with nephropathy (Table 7),while it decreased in patients with macrovascular complications,except those with PVD in both genders (Table 7).The prevalence of hypertension plus dyslipidemia increased in patients with all kinds of retinopathy,patients on dialysis,and in men with nephropathy.In contrast,the prevalence of hyper-tension plus dyslipidemia decreased in patients with all macrovascular complications in both genders except in those with PVD (Table 7).DiscussionMetabolic syndrome is characterized by obesity,glucose intolerance,elevated blood pressure (BP),and dyslipide-mia.Each component of metabolic syndrome predisposes people to atherosclerosis,and when clustered together,these components promote atherosclerosis even more prominently.Dai and colleagues studied 1494healthy Taiwanese patients aged >40years in 1992e 1993at Taipei City and San-Tze village,and found that the prevalence of each component of metabolic syndrome was as follows:obesity,29.7%;high triglyceride (TG)levels,21.7%;low high-density lipoprotein cholesterol (HDL-c)level,35.9%;high BP,56.9%;and impaired fasting glucose,13.1%.11Our present study showed that there was an obvious trend of increased prevalence of hypertension,dyslipidemia,and combined hypertension and dyslipidemia in patients with diabetes from 2000to 2009.Until 2009,64.47%of patients with diabetes had hypertension,42.22%of patients with diabetes had dyslipidemia,and 30.09%of them had both (Table 1).In both genders,the peak age for dyslipidemia was 40e 65years,while the peak age for hypertension was >65years.Dyslipidemia is a major risk factor for macrovascular complications in patients with type 2diabetes.12Further-more,type 2diabetes increases the risk for CVD mortality independent of low-density lipoprotein cholesterol (LDL-c)levels,adding to the greater overall cardiovascular risk in this population.13The dyslipidemia associated with insulin resistance is characterized by moderately increased TG levels carried in very-low-density lipoprotein particles,and reduced HDL-c carried in small HDL particles.5In patients with type 2diabetes,LDL particles are small and dense,and carry less cholesterol per particle;therefore,at any given LDL-c concentration,more LDL particles are present in an individual with type 2diabetes compared with those without the disease.5Data from the United States National Health and Nutri-tional Examination Survey (NHANES)1999e 2000showed that <50%of adults having diabetes had total cholesterol (TC)levels <200mg/dL despite >50%of these patients receiving medication for dyslipidemia.12Also,among the patients with type 2diabetes receiving treatment for628L.-N.Tseng et al.dyslipidemia,control of LDL-c was only achieved in 29.7%.12Consistent with the data from the NHANES 1999e 2000,data from the United Kingdom Prospective Diabetes Study in 3713patients newly diagnosed with type 2diabetes showed that HDL-c levels were lower (by 9%in men and 23%in women),while TG levels were 50%higher in patients with type 2diabetes than in nondiabetic patients.This kind of dyslipidemia pattern was more pronounced in females,so it was suggested to contribute to the greater cardiovascular risk in females compared with males.3Lin et al investigated 408drug-naı¨ve patients with type 2diabetes in central Taiwan,and found that among diabetic men,the plasma TG level was positively correlated with the waist-to-hip ratio (WHR)and alcohol consumption,whereas HDL-c was negatively correlated with age and body mass index.14A nationwide survey to evaluate the status of diabetes control in 7542patients with diabetes in 114accredited diabetes health promotion centers in Taiwan revealed that only 30.9%of patients met the goal of both systolic BP (SBP)and diastolic BP (DBP)less than 130/80mmHg,while 35.3%of patients met the goal of TC less than 160mg/dL or LDL-c less than 100mg/dL.15In the Western Pacific region,countries with large pop-ulations (China and Indonesia)and countries with a high prevalence of diabetes (10%in Malaysia,Hong Kong,and Singapore)contributed to the growing burden of this disease,16but the benefits of lowering lipid levels have not been systematically demonstrated in the Asian pop-ulation.17The Asia Pacific Cohort Studies Collaboration meta-analysis examined lipid associations with coronary heart disease (CHD)and CVD death from 17Asian cohorts including Taiwan.They found that the associations of TC,TG,and HDL-c with CVD were similar to those seen with CHD,but with a lesser magnitude.17Data from the Joint Asia Diabetes Evaluation (JADE)program from eight areas in Asia including Taiwan also showed that dyslipidemia and hypertension affected 76.8%and 84.6%of the patients,respectively.18In a study conducted by Xu et al in Beijing,China,the prevalence of lipid disorder was as high as 63.8%in the Chinese population in the Beijing area.19From our analysis of nationwide data,the highest prevalence was in females aged 40e 65years (46.15%),but this prevalence was lower than that reported in the JADE program or in the study by Xu and colleagues in China.18,19In our analysis,the prevalence of dyslipidemia in patients with microvascular complications remained stable.In patients with macrovascular complications,including all CVD and CVA,the prevalence of associated dyslipidemia decreased in both genders from 2000to 2009.These results may be attributable to an improved health-care system and promotion of health education in Taiwan.20In support of our findings,a diabetic study using data from the Taiwan NHI database showed that the proportion of statin use among all lipid-lowering drugs increased from 20.8%in 1997to 69.0%in 2003.21Hypertension is one of the most important risk factors for atherosclerosis-related morbidity and mortality.The prevalence rate of hypertension is also growing worldwide,and the rampant increase in prevalence is most serious in Asia.22It is predicted that there will be a 65.4%increase in hypertensive men in Asia by 2025compared with a 54.4%increase in the rest of the world.It will be even more632L.-N.Tseng et al.severe in women,with an81.6%increase in Asia compared with a54.4%increase in the rest of the world.22In a recent survey in Taiwan,the nationwide prevalence rates of hypertension were25%in men and18%in women,and the rate increased to47%among individuals aged 60years.23 The community-based data from a10-year follow-up cohort in Taiwan showed that the incidence rates have increased among individuals with prehypertension,obesity, and metabolic syndrome.24In our study,we found that for patients>65years of age with diabetes,the prevalence of hypertension even reached76.9%in women,and72.03%in men.These prevalence rates were similar to those reported by Long and Dagogo-Jack in the United States.7According to a nationwide survey conducted by Yu and colleagues (2006)in7541patients with diabetes in Taiwan,only30.9% of patients met the American Diabetes Association goal of BP maintenance(SBP and DBP less than130/80mmHg),but the percentage of patients with diabetes who fulfilled the ABC goals was only4.1%.15These data reflect the chal-lenges of treating diabetic patients with hypertension and dyslipidemia.Ourfindings showed that prevalence of CVD was more markedly increased in women who are aged40e65and >65years than in men in the same age group.Data from the Strong Heart Study indicated that diabetic women had a higher prevalence of MI and CHD than did diabetic men. The prevalence ratios of MI were3.8(1.4e10.1)for diabetic women and1.9(1.2e2.9)for diabetic men.25The authors of the study further demonstrated that diabetic women have increased WHR and have more adverse lipoprotein change,including greater decreases in HDL-c,apoA1,and LDL-c size,than do diabetic men.26Thiazolidinediones, which are agonists of peroxisomal proliferator-activated receptor-g,were shown to have cardioprotective effects and can modify lipid profile.They were introduced in Taiwan since the early2000s.Chen and colleagues found that rosiglitazone significantly reduces plasma levels of inflammatory biomarkers and restores global endothelial dysfunction,independently from insulin sensitization in healthy smokers.27However,whether the use of glitazones has some contribution to the overall decreased prevalence of CHD in patients with diabetes in the past10years needs further large-scale studies.Mortality from CVA was approximately2.8-folds higher in men with diabetes compared with men without diabetes.13 Approximately80%of strokes result from ischemic cerebral infarction in the nondiabetic population and cerebral hemorrhage occurs in the remaining20%of cases.28Studies in diabetic patients have shown a decreased prevalence of hemorrhagic stroke when compared with nondiabetic patients.29,30Our study showed that around70%of stroke cases were of the ischemic type.In the Framingham study, there was a fourfold tofivefold excess risk of hemorrhagic stroke in patients with diabetes compared with those without diabetes.31However,diabetes did not seem to have any effect on hemorrhagic stroke in a cohort of the Honolulu Heart Program.32The younger population had different risk factors and etiologies of stroke than the older population.Traditional cardiovascular risk factors,such as dyslipidemia and hypertension,were common in older patients,while the major risk factors in younger patients were congenital or acquired heart disease,or cervical artery dissection.33The difference in gender proportion was larger in the young stroke population,predominantly with men,than in the older stroke population.34A similar effect was found in our study.In our study,prevalence of PVD in diabetes increased from1.87%in2000to2.47%in2009with female predomi-nance and a rapid increase with age.The prevalence of PVD was approximately two times as high for patients with diabetes,among whom10%had lower extremities PVD, compared with nondiabetic patients.35The prevalence of PVD in diabetes might be underestimated because many people are asymptomatic.35The causes of increased PVD in diabetes might be attributable to aging,increased duration of diabetes,and associated risk factors.36In conclusion,we observed a progressively increasing rate of dyslipidemia,hypertension,and dyslipidemia plus hypertension in patients with diabetes from2000to2009 in Taiwan.However,prevalence of stroke and CVD decreased from2000to2009.Prevalence of diabetic dyslipidemia remained stable in those with microvascular complications and,indeed,it decreased gradually in patients with macrovascular complications except those with PVD.In diabetic patients with various macrovascular complications,the prevalence of hypertension decreased in the10-year interval except in those with PVD.As a result,prevalence of hypertension plus dyslipidemia slightly decreased in diabetic patients with macrovascular complications except those with PVD.Although these trends may be attributable to Taiwan’s recent efforts in advocating practice guidelines for diabetic care,estab-lishing diabetes mellitus care institutions and fostering shared care networks,a certain percentage of patients remain at the suboptimal control.More aggressive management of the comorbidities in patients with dia-betes is clearly warranted.AcknowledgmentsThe authors thank Ms Kang-Ning Hsu for her excellent help in data management.This work was supported by the Dia-betes Association of the R.O.C.,the Collaboration Center of Health Information Application,the Department of Health, Executive Yuan,Taiwan,and the National Health Research Institutes,Taiwan.References1.Whiting DR,Guariguata L,Weil C,Shaw J.IDF diabetes atlas:global estimates of the prevalence of diabetes for2011and 2030.Diabetes Res Clin Pract2011;94:311e21.2.Chang CH,Shau WY,Jiang YD,Li HY,Chang TJ,Sheu WH,et al.Type2diabetes prevalence and incidence among adults in Taiwan during1999e2004:a national health insurance data set study.Diabet Med2010;27:636e43.3.U.K.Prospective Diabetes Study27.Plasma lipids and lipo-proteins at diagnosis of NIDDM by age and sex.Diabetes Care 1997;20:1683e7.4.Saydah SH,Fradkin J,Cowie CC.Poor control of risk factors forvascular disease among adults with previously diagnosed dia-betes.JAMA2004;291:335e42.5.Vijayaraghavan K.Treatment of dyslipidemia in patients withtype2diabetes.Lipids Health Dis2010;9:144e55.Prevalence of hypertension and dyslipidemia in Taiwan diabetic patients6356.Chiu YH,Wu SC,Tseng CD,Yen MF,Chen TH.Progression ofpre-hypertension,stage1and2hypertension(JNC7):a pop-ulation-based study in Keelung,Taiwan(Keelung Community-based Integrated Screening No.9).J Hypertens2006;24: 821e8.7.Long AN,Dagogo-Jack orbidities of diabetes andhypertension:mechanisms and approach to target organ protection.J Clin Hypertens(Greenwich)2011;13:244e51. 8.Rastenyle D.Epidemiology of macrovascular disease andhypertension in diabetes mellitus.In:Alberti KGMM,Zimmet P, DeFronzo RA,editors.International textbook of diabetes mellitus.2nd ed.New York,Chichester,England:John Wiley& Sons;1997.p.146.9.Wen CP,Tsai SP,Chung WS.A10-year experience withuniversal health insurance in Taiwan:measuring changes in health and health disparity.Ann Intern Med2008;148:258e67.10.Lin CC,Lai MS,Syu CY,Chang SC,Tseng FY.Accuracy of dia-betes diagnosis in health insurance claims data in Taiwan.J Formos Med Assoc2005;104:157e63.11.Dai DF,Hwang JJ,Chen CL,Chiang FT,Lin JL,Hsu KL,et al.Effect of physical activity on the prevalence of metabolic syndrome and left ventricular hypertrophy in apparently healthy adults.J Formos Med Assoc2010;109:716e24.12.Farmer JA.Diabetic dyslipidemia and atherosclerosis:evidence from clinical trials.Curr Diab Rep2008;8:71e7. 13.Stamler J,Vaccaro O,Neaton JD,Wentworth D.Diabetes,other risk factors,and12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial.Dia-betes Care1993;16:434e44.14.Lin SD,Tu ST,Hsu SR,Lin KC,Sheu WH.Characteristics pre-dicting dyslipidemia in drug-naı¨ve type2diabetes patients.J Chin Med Assoc2006;69:404e8.15.Yu NC,Su HY,Tsai ST,Lin BJ,Shiu RS,Hsieh YC,et al.ABCcontrol of diabetes:survey data from National Diabetes Health Promotion Centers in Taiwan.Diabetes Res Clin Pract2009;84: 194e200.16.International Diabetes Federation,IDF Diabetes Atlas.http://;2011.17.Chan JC,Chan SP,Deerochanawong C,Go RT,Lee KO,Ma RC,et al.Diabetic dyslipidaemia in Asian populations in the Western Pacific Region:what we know and don’t know.Dia-betes Res Clin Pract2011;94:1e13.18.So WY,Raboca J,Sobrepena L,Yoon KH,Deerochanawong C,Ho LT,et prehensive risk assessments of diabetic patients from seven Asian countries:the Joint Asia Diabetes Evaluation(JADE)program.J Diabetes2011;3:109e18.19.Xu ZR,Wang YZ,Jing H,Liu YJ,Huang LJ,Wu CR,et al.[Lipidsdisorder,macrovascular diseases,and insulin resistance in Chinese diabetic patients].Zhongguo Yi Xue Ke Xue Yuan Xue Bao2002;24:457e61[article in Chinese].20.Cheng SH,Lee TT,Chen CC.A longitudinal examination ofa pay-for-performance program for diabetes care:evidencefrom a natural experiment.Med Care2012;50:109e16.21.Chiang CW,Chiu HF,Chen CY,Wu HL,Yang CY.Trends in theuse of lipid-lowering drugs by outpatients with diabetes inTaiwan,1997e2003.Pharmacoepidemiol Drug Saf2008;17: 62e9.22.Kearney PM,Whelton M,Reynolds K,Muntner P,Whelton PK,He J.Global burden of hypertension:analysis of worldwide ncet2005;365:217e23.23.Su TC,Bai CH,Chang HY,You SL,Chien KL,Chen MF,et al.Evidence for improved control of hypertension in Taiwan: 1993e2002.J Hypertens2008;26:600e6.24.Chien KL,Hsu HC,Sung FC,Su TC,Chen MF,Lee YT.Incidenceof hypertension and risk of cardiovascular events among ethnic Chinese:report from a community-based cohort study in Taiwan.J Hypertens2007;25:1355e61.25.Howard BV,Lee ET,Cowan LD,Fabsitz RR,Howard WJ,Oopik AJ,et al.Coronary heart disease prevalence and its relation to risk factors in American Indians.The Strong Heart Study.Am J Epidemiol1995;142:254e68.26.Howard BV,Cowan LD,Go O,Welty TK,Robbins DC,Lee ET.Adverse effects of diabetes on multiple cardiovascular disease risk factors in women.The Strong Heart Study.Diabetes Care 1998;21:1258e65.27.Chen IC,Chao TH,Tsai WC,Li YH.Rosiglitazone reducesplasma levels of inflammatory and hemostatic biomarkers and improves global endothelial function in habitual heavy smokers without diabetes mellitus or metabolic syndrome.J Formos Med Assoc2010;109:113e9.28.Gilman S.Advances in neurology(2).N Engl J Med1992;326:1671e6.29.Adams Jr HP,Putman SF,Kassell NF,Torner JC.Prevalence ofdiabetes mellitus among patients with subarachnoid hemor-rhage.Arch Neurol1984;41:1033e5.30.Megherbi SE,Milan C,Minier D,Couvreur G,Osseby GV,Tilling K,et al.Association between diabetes and stroke subtype on survival and functional outcome3months after stroke:data from the European BIOMED Stroke Project.Stroke 2003;34:688e94.31.Dawber TR,Kannel WB,Lyell LP.An approach to longitudinalstudies in a community:the Framingham Study.Ann NY Acad Sci1963;107:539e56.32.Rodriguez BL,D’Agostino R,Abbott RD,Kagan A,Burchfiel CM,Yano K,et al.Risk of hospitalized stroke in men enrolled in the Honolulu Heart Program and the Framingham Study:a compar-ison of incidence and risk factor effects.Stroke2002;33:230e6.33.Putaala J,Metso AJ,Metso TM,Konkola N,Kraemer Y,Haapaniemi E,et al.Analysis of1008consecutive patients aged 15to49withfirst-ever ischemic stroke:the Helsinki young stroke registry.Stroke2009;40:1195e203.34.Fromm A,Waje-Andreassen U,Thomassen L,Naess H.Comparison between ischemic stroke patients<50years and 50years admitted to a single centre:the Bergen Stroke Study.Stroke Res Treat2011;2011:183256.35.Mohler3rd ER.Peripheral arterial disease:identification andimplications.Arch Intern Med2003;163:2306e14.36.Tseng CH.Prevalence and risk factors of peripheral arterialobstructive disease in Taiwanese type2diabetic patients.Angiology2003;54:331e8.636L.-N.Tseng et al.。