Induced Pluripotent Stem Cells Chapter 8
- 格式:pdf
- 大小:1.70 MB
- 文档页数:19


Rapid CommunicationT lineage differentiation from induced pluripotent stem cellsFengyang Lei a,1,Rizwanul Haque a,1,Lauren Weiler a ,Kent E.Vrana b ,Jianxun Song a,*aDepartment of Microbiology &Immunology and Penn State Hershey Cancer Institute,The Pennsylvania State University College of Medicine,500University Dr.,Hershey,PA 17033,USA bDepartment of Pharmacology,The Pennsylvania State University College of Medicine,Hershey,PA 17033,USAa r t i c l e i n f o Article history:Received 7August 2009Accepted 10September 2009Available online 15September 2009Keywords:T cellsInduced pluripotent stem cells Notch signaling Differentiationa b s t r a c tInduced pluripotent stem (iPS)cells have potential to differentiate into T lymphocytes,however,the actual ability of iPS cells to develop into T lineages is not clear.In this study,we co-cultured iPS cells on OP9cells expressing the Notch ligand Delta-like 1(DL1),the iPS cells differentiated into T lympho-cytes.In addition,in vitro stimulation of iPS cell-derived T lymphocytes resulted in secretion of IL-2and IFN-c .Moreover,adoptive transfer of iPS cell-derived T lymphocytes into Rag -deficient mice recon-stituted their T cell pools.These results indicate that iPS cells are able to follow the normal program of T cell differentiation.Ó2009Elsevier Inc.All rights reserved.1.IntroductionInduced pluripotent stem (iPS)cells have been generated from mouse and human somatic cells by introducing Oct3/4and Sox2with either Klf4and c-Myc or Nanog and Lin28using retroviruses or lentiviruses 3years ago [1–3].Because the viruses inserted dur-ing the genomic alteration of the cells may potentially trigger the expression of tumorigenic genes or oncogenes,reprogramming of adult cells to obtain iPS cells poses significant risks that might limit their use in humans.However,recently,the new advancements of technology help to introduce target genes by non-integrative gene transduction [4,5]and remove oncogenes after the induction of pluripotency [6,7],thereby enhancing the potential use of iPS cells in the generation of individualized iPS cells [5,8–10]and the treat-ment of human diseases.In addition,patient-specific iPS cells would be useful in the terms of drug discovery and regenerative medicine [9,11].Previously,it has been demonstrated that human cord blood-derived hematopoietic stem cells (HSCs)cultured on Delta-like 1ligand (DL1)-expressing OP9stromal cells promote lineage commitment and differentiation of T lymphocytes [12–14].Also,it has been shown that the directed differentiation of ES cells into T lymphocytes required the engagement of Notch receptors to DL1expressed on the OP9-DL1stromal cells,whichwas capable of inducing ES cell differentiation into mature func-tional T lymphocytes after fetal thymic organ culture (FTOC)[15]or a subsequent transfer culture of ES-derived hematopoietic pre-cursor cells present in hematopoietic zones [16].Thus,the Notch signaling pathway plays a key role at several stages of T-lympho-cyte differentiation [17].To understand whether or not iPS cells are able to differentiate into T lymphocytes,we cultured mouse iPS cells on a monolayer of OP9-DL1cells over a period of approx-imately 3weeks following the subsequent addition of Flt-3ligand and IL-7,which provide signals for proliferation,survival/prolifer-ation and differentiation [18].We found that the iPS cells differen-tiated into T lymphocytes that expressed T cell receptor-b (TCR b ),and CD3on the surface.In addition,iPS cell-derived T lymphocytes secreted IL-2and IFN-c when stimulated with anti-CD3plus anti-CD28antibodies in vitro .Moreover,adoptive transfer of those iPS cell-derived T lymphocytes into Rag -deficient mice reconstituted their T cell pools.These data indicate that iPS cells are able to fol-low the normal program of T cell differentiation.2.Materials and methods 2.1.Cells and miceMouse iPS-MEF-Ng-20D-17cell line,which was induced from mouse embryonic fibroblasts (MEF)by retroviral transfection of Oct3/4,Sox2,Klf4,and c-Myc [1],was obtained from Dr.Shinya Yamanaka (Institute for Frontier Medical Sciences,Kyoto Univer-sity,Japan)through RIKEN Cell Bank (Ibaraki,Japan).C57BL/6J and B6.129S7-Rag 1tm 1Mom /J (Rag 1-deficient)mice were purchased0008-8749/$-see front matter Ó2009Elsevier Inc.All rights reserved.doi:10.1016/j.cellimm.2009.09.005Abbreviations:iPS cells,induced pluripotent stem cells;HSCs,hematopoietic stem cells;ES cells,embryonic stem cells;DL1,delta-like 1ligand;MEF,mouse embryonic fibroblasts;DP,double positive;DN,double negative;SP,single positive.*Corresponding author.Fax:+17175314600.E-mail address:jus35@ (J.Song).1These authors contributed equally to this work.Cellular Immunology 260(2009)1–5Contents lists available at ScienceDirectCellular Immunologyjournal homepage:www.else /locate/ycimmfrom Jackson Laboratory(Bar Harbor,ME).All experiments were in compliance with the regulations of the Pennsylvania State Univer-sity College of Medicine Animal Care committee in accordance with guidelines of the Association for the Assessment and Accred-itation of Laboratory Animal Care.2.2.AntibodiesAnti-CD3(2C11),anti-CD28(37.51),mouse IL-2and IFN-c were from BD PharMingen(San Diego,CA).PE,PerCP,Biotin,or APC con-jugated-CD3(17A2),CD4(GK1.5),CD8(53-6.7),CD25(3C7),CD44 (1M7),CD45(30-F11),CD117(2B8),TCR b H57597IL-2(JES6-5H4), IFN-c(XMG1.2),and isotype control antibodies were from Bioleg-end(San Diego,CA).2.3.Cell cultureiPS cells were maintained on feeder layers of irradiated SNL76/7 cells in6-well culture plates(Nunc)as previously described,and were passaged every3days.In brief,iPS cells were maintained in DMEM culture medium supplemented with15%fetal calf serum (FCS),0.1mmol/L nonessential amino acids,1mmol/L L-glutamine (all from Invitrogen),and0.1mmol/L b-mercaptoethanol(Sigma). Monolayers of OP9-DL1cells were cultured in a-MEM medium supplemented with20%FCS and2.2g/L sodium bicarbonate(all from Invitrogen).iPS cells were washed once in OP9-DL1medium before plating onto subconfluent OP9-DL1monolayers for T line-age differentiation in the presence of murine recombinant Flt-3li-gand(mrFlt3L;5ng/ml;Peprotech,Rocky Hill,NJ)and1ng/ml murine IL-7(mIL-7;Peprotech).2.4.Cytokine secretionOn day22of T lineage differentiation,2Â106iPS cell-derived progenitor T cells were isolated and stimulated with4l g plate-coated anti-CD3(2C11)plus4l g soluble anti-CD28(37.51)anti-bodies per ml in48-well plates containing1ml RPMI1640with 10%FCS(Invitrogen)with brefeldin A(Golgiplug;BD Biosciences) for5h at37°C at5%CO2.IL-2and IFN-c were analyzed by intra-cellular staining,after gating on live CD3+CD4+CD8+or CD3+ CD4ÀCD8+T cells.2.5.Adoptive cell transferOn Day22,3Â106iPS cell-derived CD3+cells were injected i.v. into4-week Rag1-deficient mice.After4weeks,single-cell suspen-sions from lymph nodes and spleen were analyzed for expression of CD4,CD8,CD3and TCR b usingflow cytometry.3.Results3.1.Notch signaling promotes iPS cell differentiationiPS cells are identical to natural pluripotent stem cells(e.g.,ES cells)in many respects,such as the morphology and growth.Undif-ferentiated mouse iPS cell colonies maintained on a feeder layer showed an appearance similar to that of mouse ES cells(Fig.1A). To determine whether iPS cells are capable of undergoing T-lym-phocyte differentiation,wefirst analyzed the morphologic growth of iPS cells in the presence of Notch signaling.After5-day culture with OP9-DL1cell,iPS cells differentiated into mesoderm-like col-onies,and became the lymphocyte-like cells on day12,which were associated with non-adherent grape-like clusters(Fig.1A).Inter-esting,on day22,lymphocyte-like cells spread fully in the plate. By calculating cell numbers of iPS cell-derived lymphocyte-like cells,we found approximately1000-fold increase in cell number (Fig.1B).In addition,before culture on OP9-DL1cells,the iPS cells did not express hematopoietic lineage markers,including CD117 and CD45,however,these markers were up-regulated after7days of culture,and then decreased(Fig1C).These data indicate that Notch signaling promotes iPS cell differentiation toward hemato-poietic lineage.3.2.iPS cells differentiated to T lymphocytesCD3and TCR b are used as markers of T lymphocytes.To deter-mine whether or not stimulation of iPS cells with Notch Signaling could contribute to T-lymphocyte differentiation,we assessedA2 F.Lei et al./Cellular Immunology260(2009)1–5expression of CD3and TCR b on iPS cell-derived cells.After 12-day co-culture with OP9-DL1cells,iPS cells lost CD117expression and retained CD4ÀCD8À,but expressed CD44and CD25on the surface of thymocyte-like populations (DN1and DN3.Fig.2A).From day 18,cells expressed both CD4and CD8,including CD4+CD8+,and CD4ÀCD8+populations (Day 22.Fig.2B),and expressed CD3and TCR b (Day 22.Fig.2C).By gating CD45+population on day 18(Fig.2D),we found the cells were CD4+CD8+(DP),CD4ÀCD8À(DN),and CD4ÀCD8+(SP)(Fig.2E).The majority of CD3+cells were located in CD4ÀCD8+population,however,approximately 5%of CD4+CD8+population also expressed CD3(Fig.2F),suggesting CD3+TCR b +cells were generated from CD4+CD8+population.These CD4+CD8+cells are thymocyte progenitors,which have a large nucleus with dense heterochromatin and a thin rim of cyto-plasm.Collectively,these data suggest that iPS cells were able to differentiate to T lymphocytes.3.3.iPS cell-derived T lymphocytes were able to secrete cytokine and restored T cell pools of Rag1-deficient miceTo investigate whether iPS cell-derived T lymphocytes are func-tional T lymphocytes,we stimulated iPS cell-derived T lympho-cytes with plate-coated anti-CD3plus soluble ant-CD28antibodies.We observed that iPS cell-derived CD3+CD4ÀCD8+but not CD3+CD4+CD8+T lymphocytes were able to produce IL-2and IFN-c as detection by intracellular staining (Fig.3).In line with this,we adoptively transferred iPS cell-derived CD3+T lym-phocytes (H-2b )into Rag 1-deficient mice (H-2b )that had no ma-ture T lymphocytes,we found that the treatment of adoptive transfer reversed T-lymphocyte pools of Rag 1-deficient mice,and induced generation of CD4+and CD8+T lymphocytes in lymph nodes and spleen.The percentages of CD4+and CD8+T lympho-cytes in these transferred Rag 1-deficient mice are similar as those in wild type of C67BL/6J mice (16.7%single CD4+and 10.3%single CD8+verse 16.8%single CD4+and 14.8%single CD8+)(Fig.4A).After gating on CD4+(Fig.4B)or CD8+cells,we observed these cells were CD3+and TCR b +cells,suggesting adoptive transfer of iPS cell-de-rived T lymphocytes were capable of generating mature T lympho-cytes in Rag 1-deficient mice.4.DiscussionRecently,functional cardiomyocytes has been induced from both mouse and human iPS cells by various stimulations [19,20],however,whether or not T cells could be induced from iPS cells is still not determined.Here we reported for the first time that T lineage differentiation could be directionally induced from iPS cells by an efficient and simple system of Notch signaling.The Notch signaling pathway had already been demonstrated to play an important role in commitment to the T lymphocytes fate,and HSCs or ES cells/OP9-DL1co-cultures robust T lymphopoiesis [12,15].Recently,a protocol to the generation of T lymphocytes from human ES-derived hematopoietic zones has been developed,which could be clinically and scientifically relevant [16].Our data indicate that Notch signaling promotes iPS cell differentiation from hematopoietic progenitors (CD45+,CD117+),mostly of the DN2(CD25+CD44+)or DN3(CD25+CD44À)phenotypes [21],thymocyte progenitors (CD4+CD8+)and mature T cells (CD3+TCR b +CD4ÀCD8+).Over a period of approximately three weeks of co-culture,more than 1000-fold of T lineages in cell number were generated,including mature CD3+TCR b +CD4ÀCD8+cells (SP),which secreted IL-2and IFN-c when stimulated with anti-CD3plus CD28antibod-ies,and CD3+TCR b +CD4+CD8+cells (DP),which were still thymo-cyte progenitors.Similarly,we did not observed the generation of CD3+TCR b +CD4+CD8Àcells using this in vitro culture system,probably as a result of blocked development due to limited MHCII expression by OP9cells [22,23].However,if CD3+T cell progenitors (both CD4+CD8+and CD4ÀCD8+)were isolated from OP9-DL1co-cultures and transferred into Rag -deficient mice,the entire T cell repertoire could be reconstituted in vivo .This repopulation may be due to transfer of T cell precursors and subsequent differentia-tion in the thymus.Because of the plasticity and potentially unlimited capacity for self-renewal,iPS cell-derived T cells may be applied for T cell75.5%20.8%37.6%61.8%1001011021031041001011021031041010110210310410010110210310427.7%13.5%23.8%F.Lei et al./Cellular Immunology 260(2009)1–53adoptive immunotherapy,such as cancer,autoimmune disorders, and infectious or aging-related diseases.Our approach for genera-tion of T cells from iPS cells provides the necessary foundation for ultimately generating patient-and/or disease-specific iPS cell-de-rived T cell therapies.AcknowledgmentsWe thank Dr.Shinya Yamanaka(Institute for Frontier Medical Sciences,Kyoto University,Japan)for providing iPS-MEF-Ng-20D-17cell line,and Dr.Juan Carlos Zuniga-Pflucker(Department of Immunology,University of Toronto,Sunnybrook)for supporting OP9-DL1cells.This work was supported by grants from the Pennsylvania Department of Health and the St.Baldrick’s Foundation to J.S. References[1]K.Okita,T.Ichisaka,S.Yamanaka,Generation of germline-competent inducedpluripotent stem cells,Nature448(2007)313–317.[2]K.Takahashi,K.Tanabe,M.Ohnuki,M.Narita,T.Ichisaka,K.Tomoda,S.Yamanaka,Induction of pluripotent stem cells from adult humanfibroblasts by defined factors,Cell131(2007)861–872.[3]J.Yu,M.A.Vodyanik,K.Smuga-Otto,J.Antosiewicz-Bourget,J.L.Frane,S.Tian,J.Nie,G.A.Jonsdottir,V.Ruotti,R.Stewart,I.I.Slukvin,J.A.Thomson,Induced pluripotent stem cell lines derived from human somatic cells,Science318 (2007)1917–1920.[4]J.Yu,K.Hu,K.Smuga-Otto,S.Tian,R.Stewart,I.I.Slukvin,J.A.Thomson,Humaninduced pluripotent stem cells free of vector and transgene sequences,Science (2009).[5]F.Soldner,D.Hockemeyer,C.Beard,Q.Gao,G.W.Bell,E.G.Cook,G.Hargus,A.Blak,O.Cooper,M.Mitalipova,O.Isacson,R.Jaenisch,Parkinson’s disease patient-derived induced pluripotent stem cells free of viral reprogramming factors,Cell136(2009)964–977.[6]M.Nakagawa,M.Koyanagi,K.Tanabe,K.Takahashi,T.Ichisaka,T.Aoi,K.Okita,Y.Mochiduki,N.Takizawa,S.Yamanaka,Generation of induced pluripotent stem cells without Myc from mouse and humanfibroblasts,Nat.Biotechnol.26 (2008)101–106.[7]I.H.Park,R.Zhao,J.A.West,A.Yabuuchi,H.Huo,T.A.Ince,P.H.Lerou,M.W.Lensch,G.Q.Daley,Reprogramming of human somatic cells to pluripotency with defined factors,Nature451(2008)141–146.[8]I.H.Park,N.Arora,H.Huo,N.Maherali,T.Ahfeldt,A.Shimamura,M.W.Lensch,C.Cowan,K.Hochedlinger,G.Q.Daley,Disease-specific induced pluripotentstem cells,Cell134(2008)877–886.[9]Q.Zhou,J.Brown, A.Kanarek,J.Rajagopal, D.A.Melton,In vivoreprogramming of adult pancreatic exocrine cells to beta-cells,Nature455 (2008)627–632.[10]A.D.Ebert,J.Yu, F.F.Rose Jr.,V.B.Mattis, C.L.Lorson,J.A.Thomson, C.N.Svendsen,Induced pluripotent stem cells from a spinal muscular atrophy patient,Nature457(2009)277–280.[11]M.Wernig,C.J.Lengner,J.Hanna,M.A.Lodato,E.Steine,R.Foreman,J.Staerk,S.Markoulaki,R.Jaenisch,A drug-inducible transgenic system for direct reprogramming of multiple somatic cell types,Nat.Biotechnol.26(2008) 916–924.[12] Motte-Mohs, E.Herer,J.C.Zuniga-Pflucker,Induction of T-celldevelopment from human cord blood hematopoietic stem cells by Delta-like 1in vitro,Blood105(2005)1431–1439.[13]T.M.Schmitt,J.C.Zuniga-Pflucker,Induction of T cell development fromhematopoietic progenitor cells by delta-like-1in vitro,Immunity17(2002) 749–756.[14]A.C.Jaleco,H.Neves,E.Hooijberg,P.Gameiro,N.Clode,M.Haury,D.Henrique,L.Parreira,Differential effects of Notch ligands Delta-1and Jagged-1in human lymphoid differentiation,J.Exp.Med.194(2001)991–1002.[15]T.M.Schmitt,R.F.de Pooter,M.A.Gronski,S.K.Cho,P.S.Ohashi,J.C.Zuniga-Pflucker,Induction of T cell development and establishment of T cell competence from embryonic stem cells differentiated in vitro,Nat.Immunol.5(2004)410–417.[16]F.Timmermans,I.Velghe,L.Vanwalleghem,M.De Smedt,S.VanCoppernolle,T.Taghon,H.D.Moore,G.Leclercq, ngerak,T.Kerre, J.Plum,B.Vandekerckhove,Generation of T cells from human embryonic stem cell-derived hematopoietic zones,J.Immunol.182(2009)6879–6888.[17]B.A.Osborne,L.M.Minter,Notch signalling during peripheral T-cell activationand differentiation,Nat.Rev.Immunol.7(2007)64–75.[18]H.Wang,L.J.Pierce,G.J.Spangrude,Distinct roles of IL-7and stem cell factor inthe OP9-DL1T-cell differentiation culture system,Exp.Hematol.34(2006) 1730–1740.[19]G.Narazaki,H.Uosaki,M.Teranishi,K.Okita, B.Kim,S.Matsuoka,S.Yamanaka,J.K.Yamashita,Directed and systematic differentiation of cardiovascular cells from mouse induced pluripotent stem cells,Circulation 118(2008)498–506.Rag1-deficient+cell transfer14.8%16.7% 6.06%10.3%1031021011001031021011004 F.Lei et al./Cellular Immunology260(2009)1–5[20]J.Zhang,G.F.Wilson, A.G.Soerens, C.H.Koonce,J.Yu,S.P.Palecek,J.A.Thomson,T.J.Kamp,Functional cardiomyocytes derived from human induced pluripotent stem cells,Circ.Res.104(2009)e30–e41.[21]J.L.Zakrzewski,A.A.Kochman,S.X.Lu,T.H.Terwey,T.D.Kim,V.M.Hubbard,S.J.Muriglan,D.Suh,O.M.Smith,J.Grubin,N.Patel,A.Chow,J.Cabrera-Perez,R.Radhakrishnan, A.Diab,M.A.Perales,G.Rizzuto, E.Menet, E.G.Pamer,G.Heller,J.C.Zuniga-Pflucker,O.Alpdogan,M.R.van den Brink, Adoptive transfer of T-cell precursors enhances T-cell reconstitution afterallogeneic hematopoietic stem cell transplantation,Nat.Med.12(2006) 1039–1047.[22]T.M.Schmitt,M.Ciofani,H.T.Petrie,J.C.Zuniga-Pflucker,Maintenance of T cellspecification and differentiation requires recurrent notch receptor–ligand interactions,J.Exp.Med.200(2004)469–479.[23]M.Ciofani,G.C.Knowles,D.L.Wiest,H.von Boehmer,J.C.Zuniga-Pflucker,Stage-specific and differential notch dependency at the alphabeta and gammadelta T lineage bifurcation,Immunity25(2006)105–116.F.Lei et al./Cellular Immunology260(2009)1–55。
iPS细胞基本概念诱导多能干细胞(induced pluripotent stem cells, iPS cells)最初是日本人山中申弥(Shinya Yamanaka)于2006年利用病毒载体将四个转录因子(Oct4, Sox2, Klf4 和c-Myc)的组合转入分化的体细胞中,使其重编程而得到的类似胚胎干细胞的一种细胞类型[1]。
随后世界各地不同科学家陆续发现其他方法同样也可以制造这种细胞。
细胞可分为全能干细胞、多能干细胞和单能干细胞,诱导多能干细胞即通过向体细胞中导入诱导基因,使体细胞重编程获得具有胚胎干细胞样特性的多能干细胞,也称为去分化。
发展趋势自2008年开始,小鼠和人的ips细胞研究取得了极大的发展,并在体细胞的选择、转录因子的组合和数量、病毒载体、筛选条件和小分子化合物等方面进行了完善,还逐步向疾病的治疗方面深入,镰刀形红细胞贫血症治疗的研究,从理论和实践上为人类单基因遗传病的治疗奠定基础。
此外,猴、大鼠和猪ips细胞的建立在人类疾病研究上具有重大应用价值,既可构建人类疾病的动物模型,又能进行细胞移植实验,为将来的实验细胞替代治疗奠定基础。
2009年3月,Nagy小组和Kaji小组采用转座子法取代病毒载体的基因投递的方法,高效率制备了基因组无病毒整合的鼠iPS细胞,获得iPS细胞后,他们又成功将先前导入的转录因子基因从iPS细胞中移除。
随着越来越多研究模型的建立,越来越多的体细胞被成功诱导为多能干细胞,以及无病毒整合技术的发现和有害基因的成功敲除,使得诱导多能干细胞向更加系统,更加安全,更加高效的方向发展。
伴随着ips细胞被诱导分化成为多巴胺神经元、能分泌胰岛素的细胞、心脏实质细胞、视网膜的前驱细胞和神经前体细胞等的成功,越来越多的体细胞得意诱导分化成功,为患帕金森综合症、糖尿病、心血管疾病和视网膜病变等疾病的患者提供了治愈的可能。
面临问题第一,诱导体细胞重编程的分子机制至今仍不清楚。
诱导多能干细胞名词解释概述诱导多能干细胞(induced pluripotent stem cells,简称iPSCs)是一种在实验室中通过重新编程成熟细胞而获得的一类多能干细胞。
与胚胎干细胞相比,iPSCs具有相似的多能性和自我更新能力,但不涉及胚胎的形成过程,从而避免了伦理和法律争议。
iPSCs的发现被认为是一项重大突破,为疾病治疗、组织再生和药物筛选等领域带来了新的可能。
历史背景iPSCs的发现可以追溯到2006年,由日本科学家山中伸弥和他的团队首次成功地通过将成熟的人体皮肤细胞转录因子的表达方式,将其重新编程成具有胚胎干细胞样特征的细胞。
这项研究是在老鼠细胞中进行的,但随后的研究证实了在人体细胞中也可以实现这一转化。
山中伸弥因此成为首位获得诺贝尔生理学或医学奖的日本科学家。
iPSCs的制备方法iPSCs的制备方法通常包括以下几个关键步骤:1.选择原始细胞:可以使用多种类型的成熟细胞作为起始细胞,如皮肤细胞、血液细胞等。
起始细胞的选择在一定程度上会影响后续iPSCs的性质和应用。
2.重编程方法:通过引入转录因子或使用其他技术,将起始细胞中特定转录因子的表达重新激活,使其回到未分化状态。
这些转录因子通常包括Oct4、Sox2、Klf4和c-Myc等。
3.细胞培养和扩增:将重编程后的细胞进行培养和扩增,使其成为一个细胞系。
这个细胞系中的细胞具有类似于胚胎干细胞的特征,包括多能性和自我更新能力。
4.鉴定和纯化:通过特定的标志物或性状,对iPSCs进行鉴定和纯化。
这些标志物包括Oct4、Nanog、Sox2等。
纯化后的iPSCs可以用于进一步的应用研究。
iPSCs的特性iPSCs具有以下几个重要的特性:1.多能性:iPSCs具有向三个胚胎发层(内胚层、中胚层和外胚层)分化的潜能,从而有能力分化成各种类型的成熟细胞,如神经细胞、心肌细胞、肝细胞等。
这种多能性使得iPSCs在疾病治疗和组织再生方面具有巨大潜力。
Repeated infusions of donor-derived cytokine-induced killer cells in patients relapsing after allogeneic stem cell transplantation: a phase I studyMartino Introna,Gianmaria Borleri,Elena Conti,Marta Franceschetti,Anna Maria Barbui, Raewyn Broady,Erica Dander,Giuseppe Gaipa,Giovanna D’Amico,Ettore Biagi,Matteo Parma, Enrico M. Pogliani,Orietta Spinelli,Donatella Baronciani,Anna Grassi,Josée Golay,Tiziano Barbui,Andrea Biondi,Alessandro RambaldiFrom the Laboratory of Cellular and Gene Therapy “nzani”,Ospedali Riuniti di Bergamo,Bergamo,Italy (MI,GB,EC,MF,JG); Division of Hematology,Ospedali Riuniti di Bergamo,Bergamo,Italy (AMB,RB, OS,AG,TB,AR); Laboratory of Cellular and Gene Therapy “S.Verri”, University of Milano Bicocca, Ospedale S.Gerardo,Monza,Italy (ED,GG,GD,EB,AB); Institute of Internal Medicine,University of Milano Bicocca,Monza,Italy (MP, EMP); Division of Hematology and Bone Marrow Transplant Centre, Ospedale Businco,Cagliari,Italy (DB).Funding:this work was partially supported by grants from the Italian Association for Cancer Research (AIRC),to MI,AR and AB,the “Associazione Italiana contro le Leucemie,linfomi e mieloma (AIL) Bergamo-Sezione Paolo Belli”,the Comitato “S.Verri”,the Italian Ministry for Universities and Research (MIUR)to AB and FIRB project RBAU01H8SX to MI and by a generous personal donation from Dr. EC.Manuscript received December 6, 2006.Manuscript accepted May 5,2007. Correspondence:Martino Introna,Laboratory of Cellular and Gene Therapy “G. Lanzani”,c/o Presidio Matteo Rota, via Garibaldi 11-13,Ospedali Riuniti di Bergamo,24128 Bergamo,Italy. E-mail:mintrona@ospedaliriuniti.bergamo.it Background and ObjectivesCytokine-induced killer (CIK) cells have shown anti-leukemic activity and little graft-versus-host disease (GVHD) in several animal models. The safety of these cells in autologous settings has been shown. We performed a phase I study of allogeneic (donor’s) CIK cells in patients relapsing after allogeneic haematopoietic stem cell transplantation (HSCT).Design and MethodsEleven patients with acute myelogenous leukemia (n=4),Hodgkin’s disease (n=3), chronic myelomonocytic leukemia,(n=1),pre-B acute lymphoblastic leukemia (n=1) and myelodysplasia (n=2),all of whom had relapsed after sibling (n=6) or matched unrelated donor (n=5) HSCT,entered this study.ResultsBefore CIK administration,six patients had received other salvage treatments includ-ing chemotherapy(n=5),radiotherapy(n=1) and unmanipulated donor lymphocytes (n=6) without any significant tumor response. The median number of CIK infusions was two (range 1-7) and the median number of total CIK cells was 12.4 x106/kg (range 7.2-87.4). The infusions were well tolerated and no acute or late infusion-relat-ed reactions were recorded. Acute GVHD (grade I and II) was observed in four patients,30 days after the last CIK infusion,and progressed into extensive chronic GVHD in two cases. Disease progression and death occurred in six patients. One patient had stable disease,one had hematologic improvement and three achieved complete responses.Interpretation and ConclusionsThis study shows that the production of allogeneic CIK cells is feasible under clinical-grade conditions,well tolerated and may contribute to clinical responses.Key words: CIK,DLI,GVHD,allo HSCT.Haematologica 2007; 92:952-959©2007 Ferrata Storti FoundationOriginal ArticleABSTRACT|952|haematologica/the hematology journal | 2007; 92(07)Infusions of cytokine-induced killer cells in allo-HSCThaematologica/the hematology journal | 2007; 92(07) | 953|M. Introna et al.| 954| haematologica/the hematology journal | 2007; 92(07)Infusions of cytokine-induced killer cells in allo-HSCThaematologica/the hematology journal | 2007; 92(07) | 955|Administration of allogeneic CIK cells to patients and clinical responsesThe median time from allogeneic HSCT to relapse or progression was 250 days (range, 90 to 1182) while a median of 315 days (range 132-1224) elapsed from trans-plantion to the first CIK infusion. Table 2 shows the total amount of CIK cells infused and the number of infusionsfor each patient, with patients listed according to the total amount of cells infused from the lowest to the highest. On the basis of cell recovery at the end of in vitro expansion,the first administration of CIK cells in each patient ranged from 3.6 up to 12.4 x 106/kg (data not shown ). Three patients received only one CIK cell preparation (patients 2, 4 and 5).Three patients received two CIK infusions at an interval ofTable 1. Patients' characteristics.Pt No.Age at Diagnosis Lines of previous Previous Intensity of Donor bHLA mismatchesMonths from Best response and sexallogeneic chemotherapy aautologous conditioning (locus)diagnosis to after allogeneic HSCT HSCT regimenallogeneic HSCT HSCT (days)c1/ F24HD 3 + RT yes Reduced MUD 1 allelic class I (B)23PR (+41)2/F 38MDS 0no Myeloablative SIB 05CR (+29)3/M 58AML 1yes Reduced MUD 09 CR (+33)4/F 54AML 1n o Reduced SIB 0 5 CR (+80)5/M 54sMDS 2yes Reduced SIB 0 1 PD 6/F 57AML 2n o Reduced SIB 0 4 CR (+80)7/F 62AML 2no Reduced SIB 0 5 CR (+42)8/F 40Pre B ALL 1yes Myeloablative MUD 048 CR (+36)9/M 37HD 4 + RT yes Reduced MUD 1 antigenic class I ( C)128 CR (+77)10/M 53CMML 0n oReduced SIB 0 6 CR (+27)11/M 36HD3 + RTyes Reduced MUD 1 allelic class I (A)29 CR (+30)a RT: radiotherapy; bMUD: unrelated donor; SIB: sibling donor.c CR: complete response; PR: partial response; PD: progressive disease.Numbers in parentheses refer to days from the date ofthe allogeneic HSCT.Table 2. Patients' hematologic status,treatment and responses.PtDays fromAddi tionalStatus First CIK CIK cells Acute Chronic Best Further Last No.HSCT to therapy pre CIK infusioninfused GVHD GVHDClinical therapy follow-upprogression before CIK infusion ×106/kg response c relapse infusion b (n.of inf.)1(+167)NoneActive(+169)7.2 (2)No No NR DLI 10×106/kg Death (+314)2(+405)DLI 85×106/kg Cytogenetic relapse (+603)7.6 (1)II (+624)Extensive CRNoAlive (+880)(+411,+433,and mixed (+666)+466,+496,+559)chimerism 3(+103)Chemo (+157)Active (+165)9.6 (2)No No NR No Death (+188)4(+245)Chemo (+275)Active (+315)10 (1)No No NR No Death (+330) DLI 5×106/kg (+280)5NAa None Active (+147)12.4 (1)I (+157)No HI 2nd allo HSCT Death (+310)(+ 190)6(+180)Chemo (+205) Active (+270)14.5 (2) No No NR No Death (+345)7(+1182)DLI 10×106/kg Active (+1224)24 (3) No No NR No Death (+1327)(+1194)8(+637)ChemoActive(+741)26.4 (4)NoNoNRNoDeath (+829)DLI 10×106/kg (+663,+692)9(+257)RT (38 Gy) (+315)Active (+374)51 (7)No No SD Chemo (+640)Alive (+1000)10(+90)DLI 10×106/kg (+102)Cytogenetic relapse (+132)53 (6)II (+195)Extensive CR No Alive (+782)and mixed chimerism (+235)11(+455)Chemo (+462)Active(+537)87.4 (6)II (+525)NoCRChemo (+572)Alive (+979)DLI 1×106/kg (+516)aNA: not applicable (never achieved partial or complete response); b RT: radiotherapy; DLI: donor lymphocyte infusion;c CR: complete response; SD: stable disease; NR: no response;HI: hematologic improvement.35Numbers in parentheses refer to days from the date of the allogeneic HSCM. Introna et al.| 956| haematologica/the hematology journal | 2007; 92(07)19-21 days according to the study protocol (patients 1, 3,and 6). Patients 7 and 8 received three and four CIK infu-sions, respectively. Two patients (10 and 11) received six CIK infusions and finally one patient (n. 9) received seven CIK infusions. Each infusion was well tolerated and no immediate adverse effects were observed.Six patients (1, 3, 4, 6, 7 and 8) showed no evidence of clinical response, had rapidly progressive disease and died.One patient (n. 5) with secondary MDS (following previ-ous non-Hodgkin’s lymphoma treated with high dose chemotherapy and autologous transplantation), was elect-ed to CIK treatment because of early relapse after a reduced intensity allogeneic transplant. At the time of infusing CIK cells, a trilinear dysplasia was documented in the bone marrow showing a normal cellularity of full patient origin. CIK cells induced a hematologic improve-ment,30as documented by the induction of marrow apla-sia, with cytogenetic analysis showing 50% donor chimerism. A subsequent infusion of donor allogeneic PBSC was performed to rescue the hematologic function but disease progression occurred and the patient died on day + 310 (Table 2). One patient with HD (n.9) received a total of 51×106/kg CIK cells and the disease did not require further treatment for almost 1 year. On day +640 disease progression occurred (supraclavicular and axillary lymph nodes) so that chemotherapy was given (11 cycles of gem-citabine). This patient remains alive at day + 1000 with stable disease. In another HD patient (n. 11), disease relapse after transplantation was documented on day +455, so six cycles of gemcitabine followed by one unma-nipulated donor lymphocyte infusion (1×106/kg) were given. Given the lack of clinical response and massive dis-ease involvement of bone marrow, lung and mediastinalFigure 1.In vitro CIK expansion. A. The percentages of CD3+and CD3+/CD56+cells at the start (striped bars) and at the end (black bars) of culture are indicated.The results are the mean and standard deviations of 18 preparations. B. Absolute numbers of CD3+and CD3+/CD56+cells at the start (striped bars) and at the end (black bars) of cultures are indicated. The results are the mean and standard devia-tions of 18 preparations. C. Fold increase of absolute numbers of CD3+and CD3+/CD56+cells are shown as circles for each single expansion. The horizontal bars indicate the median fold increases for the two populations.Figure 2.In vitro cytotoxic activity by CIK cells. A.CIK cells from nine bone marrow donors were prepared in experimental conditions and tested against K562 or leukemic samples from the HLA-matched allogeneic recipients at the indicated effector:target (E:T) ratios. B.CIK cells from 16 healthy donors were prepared in experimental conditions and tested against normal autologous or HLA-mis-matched allogeneic T-PHA blasts at the indicated E:T ratios.A BC %p o s i t i v i t yF o l d i n c r e a s e (o f a b s . n u m b e r s )A b s o l u t e n u m b e r o f c e l l s ×106)1201008060402001000100101Start End Start End % CD3+% CD3+CD56+CD3+CD3+CD56+%l y s i s30:110:11:1K562Patients’ leukemiccellsK562Autologous Allogeneic T-PHA blastsT-PHA blasts30:110:1%l y s i s806040200806040200Start End Start End CD3+CD3+CD56+500040003000200010000ABInfusions of cytokine-induced killer cells in allo-HSCThaematologica/the hematology journal | 2007; 92(07) | 957|Figure 3.Post-transplant chimerism in the CD3+cell fraction of patients n. 10 and 2. Chimerism in the peripheral blood of CD3+cells of patients n. 10 and n. 2 was analyzed by polymerase chain reaction at different times after transplantation. The molecular pro-files of the donor’s and patient’s CD3+cells are shown in the upper panels. The measured precentages of donor CD3+cells are shown in each panel. The timing of DLI and CIK infusions is indicated on the right hand side.100%0%77%22%6%25%45%97%100%90%95%97%95%100%0%53%64%43%94%100%2790120132155147377491504595711DLI (+102)CIK (+132)CIK (+174)CIK (+509, +530)CIK (+610, +629)DLI (+411, +433)DLI (+466, +496)DLI (+559)CIK (+603)454522586628704Pt 10Donor RecipientDonor RecipientDays post transplantDays post transplantPt 2M. Introna et al.| 958| haematologica/the hematology journal | 2007; 92(07)antitumor activity.31More recently, two phase I studies have shown the feasibility and clinical safety of infusions of huge amounts of autologous CIK cells, with some pre-liminary evidence of antitumor activity.26-28Several differ-ent animal models have shown that allogeneic CIK cells of both human and animal origin do not mediate a significant GVHD effect but can retain a remarkable antitumor activ-ity.15-17,19,23-25In this study we have shown that large num-bers of allogeneic CIK cells can be produced in a 3-week time period and safely given to patients who have relapsed after allogeneic transplantation. This is the first report, to our knowledge, on the use of CIK cells in an allogeneic context for hematologic malignancies.We have demonstrated that CIK cells could be obtained for 18 out of 18 consecutive batches to treat the 11 patients enrolled into this study, which was open for enrollment for 8 months. The feasibility of the laboratory procedure is also documented by the fact that the total amount of start-ing nucleated cells was relatively modest (a mean of less than 1×109TNC obtained by donor leukapheresis) and in one case a small 30 mL peripheral blood sample was suffi-cient. It is important to note that the final yields and rela-tive purity of CIK cells are comparable with those report-ed previously by others.26-28The concomitant administration of other antineoplastic treatments such as chemotherapy or radiotherapy and the infusion of unmanipulated donor lymphocytes substan-tially prevents the possibility of evaluating the therapeutic activity of the allogeneic CIK cells that were infused, a problem also encountered in similar studies.32Within the limits of the study design, we can report the achievement of three complete responses (1 MDS, 1 CMML and 1 HD)and stable disease in one patient with HD. In one addition-al patient with secondary MDS, however, the infusion of CIK cells was the sole clinical intervention so that in this case the hematologic improvement,30documented by mar-row aplasia with 50% donor chimerism, could be directly ascribed to the infused CIK cells.Patients enrolled into this phase I study received variable amounts of CIK cells and despite the fact that some patients received more than 10×106/kg CIK cells as a first single infusion, acute toxicity was never observed. All patients received CIK cells after complete withdrawal of CsA and corticosteroids;acute G VHD developed in four patients but never exceeded grade II. However, progres-sion to extensive chronic G VHD occurred in the two patients who showed the most significant clinical respons-es. Therefore, although the interpretation of chronic G VHD may be hindered by the preceeding infusions of unmanipulated DLI, the administration of allogeneic CIK cells may be associated with the development of GVHD.In this regard it is interesting to note that in the two docu-mented cases, CIK administration was rapidly followed by the disappearance of host T lymphocytes. Since the patients who showed a clinical response as well as acute and chronic G VHD, were those who were also treated with unmanipulated DLI, the role of these latter in gaininga maximal therapeutic effect from CIK cells remains to be determined. Therefore, we cannot provide certain evi-dence of the antineoplastic activity of CIK cells in vivo , nor we can show that CIK cells are more effective than con-ventional DLI in rescuing patients experiencing disease recurrence after allografting. However, the degree of the toxicity of the observed G VHD may allow, in the near future, the planning of clinical studies with higher doses and repeated infusions of CIK cells in less clinically com-promised HSCT patients. On the other hand, the use of allogeneic MHC-unrestricted cytotoxic effector cells has been recently suggested for haploidentical NK cells 33and could also be explored with CIK cells, which share key molecules, such as NKG 2D, crucial for effective target recognition and killing.34In this report we confirm and extend previous observa-tions on the in vitro antitumor activity of CIK cells against leukemic samples of host origin. Furthermore, our data support the idea that these cells have limited toxicity against normal cells, as evidenced by the resistance of T-PHA blasts of autologous or allogeneic origin.All in all, the following comments can be made about the clinical results we observed in this small cohort of patients. First, the most interesting clinical results were recorded in patients with indolent diseases (MDS, HD,CMML) rather than in those with acute leukemias.Second, it seems unlikely that CIK cells alone can induce a major clinical response when a massive leukemia or lym-phoma relapse is occurring. Finally, our results are in keep-ing with previous observations by Slavin and co-workers 35who showed that, in patients resistant to DLI, remissions can be accomplished by adding donor peripheral blood lymphocytes activated in vivo or in vitro with IL-2.Nonetheless, a direct comparison in terms of efficacy and safety between the two studies is difficult to perform due to the different in vitro treatment protocols. Rather, cytore-ductive chemotherapy or radiotherapy should usually pre-ceed the administration of CIK cells given finally as a form of adoptive immunotherapy with the intention to treat minimal residual disease. Along the same lines, the pre-emptive use of CIK cells to treat a cytogenetic or molecu-lar relapse also seems rational. Determining the effective-ness of this strategy will obviously be a major aim of a future clinical study with CIK cells.Authors’ContributionsMI:responsible of the project, writer of the manuscript;GB:pro-duction of cells in GMP in Bergamo;E C:production of cells in GMP in Bergamo;MF:experimental data CIK cells;AMB:clini-cal administration of CIK cells;RB:experimental data CIK cells;E D, GG:production of CIK cells in GMP in Monza;GD'A:experimental data CIK cells;EB, MP , EMP , EMP , MP , DB: clin-ical administration CIK cells;OS: molecular analysis of chimerism;AG:clinical administration of CIK cells and patients registry;JG: quality control GMP facility;TB: responsible Department;AB:responsible Clinical Unit;AR:responsible Clinical Unit and CIK clinical design and writer of the manuscript.Conflict of InterestThe authors reported no potential conflicts of interest.Infusions of cytokine-induced killer cells in allo-HSCThaematologica/the hematology journal | 2007; 92(07) | 959|References1.Bleakley M, Riddell SR. Molecules and mechanisms of the graft-versus-leukaemia effect. Nat Rev Cancer 2004;4:371-80.2.Talmadge JE. Hematopoietic stem cell graft manipulation as a mechanism of immunotherapy. Int Immunopharma-col 2003;3:1121-43.3.Campbell JD, Cook G, Holyoake TL.Evolution of bone marrow transplanta-tion-the original immunotherapy.Trends Immunol. 2001;22:88-92.4.Slavin S, Morecki S, Weiss L, Shapira MY, Resnick I, Or R. Nonmyelo-ablative stem cell transplantation:reduced-intensity conditioning for can-cer immunotherapy-from bench to patient bedside. Semin Oncol 2004;31:4-21.5.Kolb HJ, Schmid C, Barrett AJ,Schendel DJ. G raft-versus-leukemia reactions in allogeneic chimeras. Blood 2004;103:767-76.6.Falkenburg JH, Willemze R. Minor his-tocompatibility antigens as targets of cellular immunotherapy in leukaemia.Best Pract Res Clin Haematol 2004;17:415-25.7.Introna M, Barbui AM, G olay J,Rambaldi A. Innovative cell-based therapies in onco-hematology: what are the clinical facts? Haematologica 2004;89:1253-60.8.Ruggeri L, Capanni M, Mancusi A,Aversa F , Martelli MF , Velardi A.Natural killer cells as a therapeutic tool in mismatched transplantation. Best Pract Res Clin Haematol 2004;17:427-38.9.Rosenberg SA, Lotze MT, Muul LM,Leitman S, Chang AE, Ettinghausen SE, et al. Observations on the systemic administration of autologous lym-phokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N Engl J Med 1985;313:1485-92.10.Siegel JP , Puri RK. Interleukin-2 toxici-ty. J Clin Oncol 1991;9:694-704.11.Klingemann HG . Natural killer cell-based immunotherapeutic strategies.Cytotherapy 2005;7:16-22.12.Hercend T, G riffin JD, Bensussan A,Schmidt RE, Edson MA, Brennan A, et al. Generation of monoclonal antibod-ies to a human natural killer clone.Characterization of two natural killer-associated antigens, NKH1A and NKH2, expressed on subsets of large granular lymphocytes. J Clin Invest 1985;75:932-43.13.G riffin JD, Hercend T, Beveridge R,Schlossman SF . Characterization of an antigen expressed by human natural killer cells. J Immunol 1983;130:2947-51.nier LL, Testi R, Bindl J, Phillips JH.Identity of Leu-19 (CD56) leukocyte differentiation antigen and neural cell adhesion molecule. J Exp Med 1989;169:2233-8.15.Schmidt-Wolf IG, Negrin RS, Kiem HP ,Blume KG , Weissman IL. Use of a SCID mouse/human lymphoma model to evaluate cytokine-induced killer cells with potent antitumor cell activity. J Exp Med 1991;174:139-49.16.Lu PH, Negrin RS. A novel population of expanded human CD3+CD56+cells derived from T cells with potent in vivo antitumor activity in mice with severe combined immunodeficiency. J Immunol 1994;153:1687-96.17.Hoyle C, Bangs CD, Chang P , Kamel O, Mehta B, Negrin RS. Expansion of Philadelphia chromosome-negative CD3(+) CD56(+)cytotoxic cells from chronic myeloid leukemia patients: in vitro and in vivo efficacy in severe combined immunodeficiency disease mice. Blood 1998;92:18-27.18.Alvarnas JC, Linn YC, Hope EG ,Negrin RS. Expansion of cytotoxic CD3+CD56+cells from peripheral blood progenitor cells of patients undergoing autologous hematopoietic cell transplantation. Biol Blood Marrow Transplant 2001;7:16-22.19.Baker J, Verneris MR, Ito M, Shizuru JA, Negrin RS. Expansion of cytolytic CD8(+)natural killer T cells with limit-ed capacity for graft-versus-host dis-ease induction due to interferon gamma production. Blood 2001;97: 23-31.20.Schmidt-Wolf IG , Lefterova P , Mehta BA, Fernandez LP , Huhn D, Blume KG et al. Phenotypic characterization and identification of effector cells involved in tumor cell recognition of cytokine-induced killer cells. Exp Hematol 1993;21:1673-79.21.Linn YC, Lau LC, Hui KM. Generation of cytokine-induced killer cells from leukaemic samples with in vitro cyto-toxicity against autologous and allo-geneic leukaemic blasts. Br J Haematol 2002;116:78-86.22.Sconocchia G, Lau M, Provenzano M,et al. The antileukemia effect of HLA-matched NK and NK-T cells in chronic myelogenous leukemia involves NKG2D-target-cell interactions. Blood 2005;106:3666-72.23.Verneris MR, Ito M, Baker J, Arshi A,Negrin RS, Shizuru JA. Engineering hematopoietic grafts: purified allo-geneic hematopoietic stem cells plus expanded CD8+NK-T cells in the treatment of lymphoma. Biol Blood Marrow Transplant 2001;7:532-42.24.Edinger M, Cao YA, Verneris MR,Bachmann MH, Contag CH, Negrin RS. Revealing lymphoma growth and the efficacy of immune cell therapies using in vivo bioluminescence imag-ing. Blood 2003;101:640-8.25.Sweeney TJ, Mailander V , Tucker AA,et al. Visualizing the kinetics of tumor-cell clearance in living animals. Proc Natl Acad Sci USA 1999;96:12044-9.26.Leemhuis T, Wells S, Scheffold C,Edinger M, Negrin RS. A phase I trial of autologous cytokine-induced killer cells for the treatment of relapsed Hodgkin disease and non-Hodgkin lymphoma. Biol Blood Marrow Transplant 2005;11:181-7.27.Wang FS, Liu MX, Zhang B, Shi M, LeiZY, Sun WB, et al. Antitumor activities of human autologous cytokine-induced killer (CIK) cells against hepa-tocellular carcinoma cells in vitro and in vivo. World J G astroenterol 2002;8:464-8.28.Shi M, Zhang B, Tang ZR, Lei ZY,Wang HF , Feng YY, et al. Autologous cytokine-induced killer cell therapy in clinical trial phase I is safe in patients with primary hepatocellular carcino-ma. World J Gastroenterol 2004;10:1146-51.29.Kubat M, Skavic J, Behluli I, Nuraj B,Bekteshi T, Behluli M, et al. Population genetics of the 15 AmpF lSTR Identifiler loci in Kosovo Albanians. Int J Legal Med 2004; 118: 115-8.30.Cheson BD, Bennett JM, Kantarjian H,Pinto A, Schiffer CA, Nimer SD, et al.Report of an international working group to standardize response criteria for myelodysplastic syndromes. Blood 2000;96:3671-4.31.Verneris MR, Baker J, Edinger M,Negrin RS. Studies of ex vivo activated and expanded CD8+NK-T cells in humans and mice. J Clin Immunol 2002; 22:131-6.32.Porter DL, Levine BL, Bunin N,Stadtmauer EA, Luger SM, G oldstein S, et al. A phase 1 trial of donor lym-phocyte infusions expanded and acti-vated ex vivo via CD3/CD28 costimu-lation. Blood 2006;107:1325-31.ler JS, Soignier Y, Panoskaltsis-Mortari A, McNearney SA, Yun G H,Fautsch SK, et al. Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in patients with cancer. Blood 2005;105:3051-7.34.Verneris MR, Karami M, Baker J,Jayaswal A, Negrin RS. Role of NKG 2D signaling in the cytotoxicity of activated and expanded CD8+ T cells. Blood 2004;103:3065-72.35.Slavin S, Naparstek E, Nagler A,Ackerstein A, Samuel S, Kapelushnik J,et al. Allogeneic cell theraphy with donor peripheral blood cells and recombinant human interleukin-2 to treat leukemia relapse after allogenic bone marrow transplantation. Blood 1996;87:2195-204.。
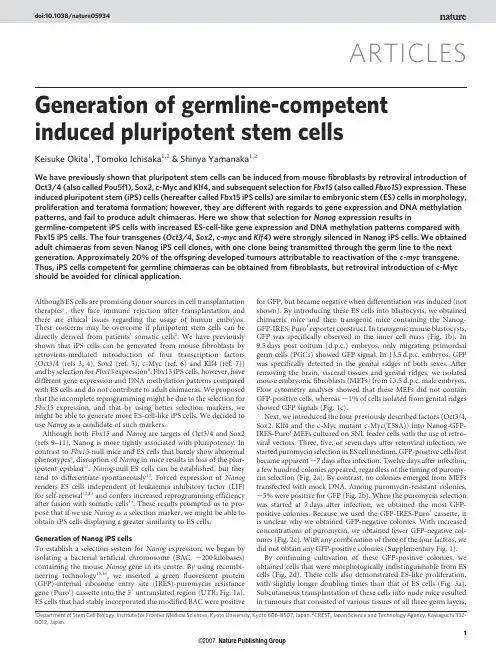
187G. Steinhoff (ed.), Regenerative Medicine: From Protocol to Patient,DOI 10.1007/978-90-481-9075-1_8, © Springer Science+Business Media B.V . 2011Abstract Nearly 50 years have passed since the concept of nuclear r eprogramming was proposed for the first time. Since then, several approaches have been developed to convert somatic cells to a pluripotent state. Direct reprogramming with defined factors, is the newest of these approaches. This method requires just a few genes, and it also has a great reproducibility. Applying this method to humans seems to open the door to cell transplantation therapy without immune rejection, drugd iscovery, and elucidation of the pathogenesis of intractable diseases. However, this concept still faces some issues which must be overcome before application due to a shortage of experience. This chapter introduces an overview of direct reprogram-ming as well as a special focus on its potentials and challenges.8.1 I ntroductionPluripotent stem cells such as embryonic stem (ES) cells may be a hopeful resource for regenerative medicine to repair degenerative or damaged tissues. ES cells have the potential to differentiate into all cell types in the body including germ cells. Not only pluripotency but also their growth properties are substantially superior. In conventional conditions, ES cells can grow infinitely while maintaining K. Takahashi and S. Yamanaka ( )Center for iPS cell Research and Application, Institute for Integrated Cell-Material Sciences, Kyoto University, Kyoto 606-8507, Japane-mail: takahash@cira.kyoto-u.ac.jpS. YamanakaDepartment of Stem Cell Biology, Institute for Frontier Medical Sciences,Kyoto University, Kyoto 606-8507, JapanandYamanaka iPS Cell Special Project, Japan Science and Technology Agency,Kawaguchi 332-0012, JapanandGladstone Institute of Cardiovascular Disease, San Francisco, CA 94158, USAChapter 8Induced Pluripotent Stem CellsKazutoshi Takahashi and Shinya Yamanaka188K. Takahashi and S. Yamanaka an undifferentiated state. Combined with the techniques of gene targeting and transgenes, these characters have allowed the generation of genetically modified animals (Robertson et al. 1986; Thomas and Capecchi 1987; Doetschman et al. 1987). To this end, the mechanisms or causes of many diseases have been eluci-dated. Reports on the establishment of human ES cells brought great expectations to regenerative medicine of various diseases (Thomson et al. 1998). In the last decade, scientists have established appropriate culture conditions, differentiation protocols and guidelines for users.On the other hand, ES cells face two big issues that need to be overcome before successful medical application can be achieved. One is immune rejection caused by the mismatching of human leukocyte antigen (HLA) haplotypes between ES cells and patient. Another is the usage of human embryos. Although the response to e thical issues may vary depending on regions and civilizations, it should be ear-nestly addressed in any case.One of the solutions to overcome these issues is to reprogram a patient’s own somatic cells directly to pluripotent stem cells. The reprogramming of the somatic nucleus was firstly demonstrated by Sir John Gurdon in 1958 (Gurdon et al. 1958). He developed cloned frogs by injecting the nucleus of a tadpole somatic cell into an egg. This report suggested that frog eggs have some reprogramming factor(s) that could initialize somatic state back to totipotency. In 1997, the group of Sir Ian Wilmut and Dr. Keith Campbell with their famous sheep, Dolly, showed that not only flexible species such as amphibians but also mammals have the reprogram-ming factor(s) in their eggs by using nuclear transfer technology (Wilmut et al. 1997). In the last year of the twentieth century, Dr. Takashi Tada and his colleagues showed that the nucleus of somatic cell also could be reset to the pluripotent state by electrical-fusion with mouse ES cells (Tada et al. 2001). All these findings and following associated reports suggested that ES cells as well as eggs have such reprogramming factor (s). At a later date, the same phenomenon was confirmed in human cells (Cowan et al. 2005).What is the reprogramming factor? People have hypothesized that factors playing important roles in ES cell identities, such as differentiation potentials and tumor-like growth properties, play a crucial role in the induction of pluripotency in somatic cells. The concept that the genes expressed specifically in stem cells p rovided multipotency to the cells has been established and called stemness (Ramalho-Santos et al. 2002). Therefore, the genes expressed predominantly in eggs and/or ES cells, and some non-ES cell specific genes which are important for the character of pluripotent cells can be candidates of reprogramming factor(s).The importance of pluripotent cell-associated genes has been proposed in s everal studies (Boiani and Schöler 2005; Niwa 2007).Oct3/4 (also known as Pou5f1) one of the most famous ES cell-specific genes, is an octamer sequence binding transcription factor (Okamoto et al. 1990; Schöler et al. 1990). Deletion of Oct3/4 gene caused the loss of pluripotency in both ES cells and early embryos (Nichols et al. 1998). Oct3/4-null embryos die at around the implantation stage. The inner cell mass (ICM) of Oct3/4-deficient embryo can no longer outgrow. Detailed analyses have shown that Oct3/4 prevents the d ifferentiation8 Induced Pluripotent Stem Cells189 into trophectoderm by suppressing the function of Cdx2 which plays essential role in trophectoderm development (Niwa et al. 2005). On the other hand, only a 1.5-fold increase of Oct3/4 expression in ES cells is sufficient to trigger differentiation into either mesoderm or primitive endoderm (Niwa et al. 2000). These data indicated that Oct3/4 is one of the most important regulators to prevent differentiation into specific lineages and maintain ES cells in a pluripotent state.The other important player is Sox2. The expression of Sox2 is restricted in nerve tissue and pluripotent cells including germ cells (Kamachi et al. 2000). Structural and biochemical analyses demonstrated that Sox2 binds directly to Oct3/4 and acts as a regulator of ES cell-specific gene expression such as Utf1, Fgf4 and Lefty1 (Ambrosetti et al. 1997; Reményi et al. 2003; Nishimoto et al. 1999). Homozygous deletion of Sox2 gene leads to embryo death immediate after implantation with the lack of epiblast formation (Avilion et al. 2003). Blastocysts carrying a null mutation of Sox2 gene looked normal, but the ICM could not expand in vitro whereas tropho-blasts and primitive endoderm cells can continue to proliferate. In addition, Sox2-deficient ES cells cannot maintain an undifferentiated state in conventional conditions (Masui et al. 2007). Taken together, Sox2 is crucial for the maintenance of pluripotent cells in both ES cells and early embryos.However, the functions of Oct3/4 and Sox2 are not sufficient to explain the molecular mechanisms underlying pluripotent stem cell identity. The presence of other co-factors has been speculated. Many exhaustive analyses were performed in the early 2000s, and databases of gene expression profiles were advanced rapidly such as expressed sequence tags (ESTs) and microarray technology (Kawai et al. 2001). To this end, hundreds of stemness-relating genes were found as candidates to define the stem cell phenotype (Tokuzawa et al. 2003; Takahashi et al. 2003). An in silico analysis and functional screening identified a novel stemness gene, designated Nanog at the same time (Mitsui et al. 2003). Nanog is a transcription factor which contains a paired-like homeobox. The expression pattern of Nanog in early development is more restricted than that of Oct3/4 or Sox2. Embryos carrying a null-mutation of Nanog gene die during the post-implantation period lacking epiblasts (Mitsui et al. 2003). Outgrowth of Nanog-deficient ICM is also defective, although primitive endoderm-like cells can proliferate. On the other hand, ES cells carrying homozygous deletion of the Nanog gene can proliferate in vitro although morphologies and gene expression patterns were changed to primitive endoderm-like state (Mitsui et al. 2003). In addition, forced expression of the Nanog gene allows cells to maintain pluripotency even without leukemia inhibitory factor (LIF) which is an essential component for self-renewal of mouse ES cells in serum- containing medium (Chambers et al. 2003; Mitsui et al. 2003). Therefore, these data suggested that Nanog acts as a switch between the pluripotent state and primi-tive endoderm.ChIP on chip analyses, which combine chromatin immunoprecipitation, microarray, and a transcriptome, revealed global target genes of Oct3/4, Sox2 and Nanog in ES cells (Chew et al. 2005; Loh et al. 2006; Boyer et al. 2005). More than 300 genes were categorized as common targets of these three transcription factors, including both expressed (Oct3/4, Sox2, Nanog, Stat3, Zic3) and not expressed190K. Takahashi and S. Yamanaka genes (Hoxb1, Pax6, Lhx5, Myf5) in ES cells. These data suggested that a circuit consisting of Oct3/4, Sox2 and Nanog promotes the expression of genes supporting the self-renewal of ES cells, suppresses those genes required for differentiation into three germ layers such as homeobox genes, and thus maintains pluripotency.On the other hand, several studies reported that some oncogenes also played important roles in ES cell identity (Chambers and Smith 2004; Cheng et al. 1998). The most famous oncogene related to self-renewal of mouse ES cells is Stat3. L IF-mediated Stat3 activation is essential and sufficient for the maintenance of pluripotency (Niwa et al. 1998). One of its downstream targets in LIF/Stat3 signal-ing pathway is c-Myc (Cartwright et al. 2005). An overexpression of c-Myc in mouse ES cells allows LIF-independent self-renewal. On the other hand, another well known oncogenic pathway, Ras/MAPK, negatively regulates the maintenance of pluripotency. Inhibition of the Ras/MAPK pathway by a small molecule or gene targeting blocks differentiation (Cheng et al. 1998; Burdon et al. 1999). It is not always true that these factors are expressed specifically in pluripotent cells. ES cells display tumor-like properties with regard to their growth including anchorage independence, infinite expansion and tumorigenicity. As a result, it is no wonder that tumor-related genes join the network of pluripotency.In 2006, direct reprogramming of mouse somatic cells was accomplished by introducing the combination of just four transcription factors: Oct3/4, Sox2, Klf4 and c-Myc (Takahashi and Yamanaka 2006). These reprogrammed cells artificially induced by the defined factors were named induced Pluripotent Stem (iPS) cells. In 1 year, human iPS cells were also generated from adult dermal fibroblasts (Fig. 8.1) (Takahashi et al. 2007; Yu et al. 2007). Since the first announcement of these findings, this field has rapidly expanded and developed in various directions.In this chapter, I will introduce the expected potential and possible problems of iPS cells based on the latest findings.Fig. 8.1iPS cells derived from adult human dermal fibroblasts191 8 Induced Pluripotent Stem Cells8.2 D erivation8.2.1 R eprogramming Factors and SubstitutesMouse iPS cells were initially established by forced-expression of Oct3/4, Sox2, Klf4 and c-Myc in mouse embryonic fibroblasts (MEFs) or tail-tip fibroblasts (TTFs) from adult mice (Takahashi and Yamanaka 2006). Some of these factors can be replaced with related genes. For example, Klf2 or Klf5 can mimic Klf4 func-tions, and Sox1, Sox3, Sox15, Sox17 and Sox18 are also able to substitute for Sox2 (Nakagawa et al. 2008). Estrogen-related receptor, beta (Esrrb), can contribute to direct reprogramming with Oct3/4 and Sox2 (Feng et al. 2009). In addition, treat-ment with kenpaullone along with transduction of Oct3/4 and Sox2 also can p roduce ES-like colonies from MEFs (Lyssiotis et al. 2009).All of the Myc family genes in mammals, c-Myc, N-Myc and L-Myc, dramati-cally enhance the efficiency of iPS cell generation (Nakagawa et al. 2008). Although Myc is dispensable for direct reprogramming, the number of iPS cell colonies gener-ally diminishes to approximately 150 without Myc (Nakagawa et al. 2008; Wernig et al. 2008b). The effects of Myc on iPS cell generation can be mimicked by the activation of the canonical Wnt pathway (Marson et al. 2008). Myc proteins are substrates of Glycogen synthase kinase-3 (GSK3) which is activated by Wnt signals (Cohen et al. 2001). Phosphorylated Myc proteins by GSK3 are rapidly degraded by proteasomes. These data suggest that Myc acts as a booster of direct reprogramming.8.2.2 S election of Reprogrammed CellsGenerally, mice carrying a reporter system of fluorescent proteins and/or drug resistance genes driven by the promoters of pluripotent cell-associated genes are used for the establishment of mouse iPS cells. First, iPS cells are generated from MEFs or TTFs carrying b geo, which is a beta-galactosidase and neomycin resis-tance fusion gene knocked into the Fbx15 locus (Takahashi and Yamanaka 2006). Thereafter, other reporter systems have been designed for this purpose. Nanog or Oct3/4 can also work as selection markers of reprogramming (Okita et al. 2007; Wernig et al. 2007; Maherali et al. 2007). For example, green fluorescence protein (GFP) and puromycin resistance gene controlled by Nanog or Oct3/4 promoter are widely used in the field. The other indicator of reprogramming is the silencing of the retrovirus promoter (Nakagawa et al. 2008). The long terminal repeat (LTR) of mouse molony-leukemia virus (MMLV) can act as a strong promoter. In contrast, the activity of MMLV LTR is effectively silenced in pluripotent cells such as ES cells and iPS cells. Although some researchers have tried to elucidate this phenom-enon, the underlying mechanisms still remain unclear (Wolf and Goff 2007, 2009). Nevertheless, when a retrovirus encoding fluorescent protein is transduced along192K. Takahashi and S. Yamanaka with the reprogramming factors into somatic cells, the disappearance of the f luorescence suggests that reprogramming has been completed.These reporters are employed because it is quite hard to distinguish r eprogrammed cells from the non-reprogrammed cells just by morphology in mice. In contrast, there is little unrest for human cells. Human iPS cells form distinctive flat, tightly packed and clear edged colonies like human ES cells, whereas non-reprogrammed cells show granular morphologies and tend to form rough colonies (Takahashi et al. 2007; Lowry et al. 2008).8.2.3 E pigeneticsSome reports have shown that treatment with histone deacetylase (HDAC) inhibi-tors, such as Trichostatin A (TSA), valproic acid (VPA), DNA methyltransferase (DNMT) inhibitor, and 5-Aza-2¢-deoxycytidine can improve the frequency of iPS cell establishment (Huangfu et al. 2008a; b; Mikkelsen et al. 2008). Inhibition of histone methyltransferase G9a by treatment with a small molecule, BIX-01294, is also effective. These data suggest that epigenetic modifications are closely linked to nuclear reprogramming (Shi et al. 2008).8.2.4 O ther ElementsIn addition to the above, some other factors which can improve the reprogramming efficiency were identified. The transduction of microRNAs such as miR-291-3p, miR-294, miR-295 elevates the number of iPS cell colonies by about 10-fold (Judson et al. 2009). In addition, RNA-related protein LIN28 enhances the efficiency of human iPS cells generation (Yu et al. 2007; Liao et al. 2008). The inhibition of both Mitogen-Activated Protein Kinase (MEK) and GSK3, which is generally called 2i in serum-free culture, increases the reprogramming efficiency (Silva et al. 2008). The overexpression of Spalt-like 4 (Sall4) or the suppression of transformation related protein 53 (Trp53) increase the reprogramming efficiency both in mouse and human (Tsubooka et al. 2009; Hong et al. 2009; Kawamura et al. 2009; Li et al. 2009; Marión et al. 2009; Utikal et al. 2009; Banito et al. 2009). In the case of human cells, telomerase reverse transcriptase (TERT) and Simian virus 40 large T (SV40LT) antigen that promote the immortalization of human primary fibroblasts, can enhance the reprogramming efficiency (Park et al. 2008b; Mali et al. 2008).8.2.5 C ell SourcesIn mouse, MEFs and TTFs are commonly used as sources of iPS cells in many reports. Various other cell types were demonstrated to be sources of iPS cells, such193 8 Induced Pluripotent Stem Cellsas neural progenitors, adrenal glands, keratinocytes, muscular cells, intestinal e pithelium cells, mesenchymal stem cells and hematopoietic cells can be (Aoi et al. 2008; Wernig et al. 2008a; Silva et al. 2008; Kim et al. 2008; Eminli et al. 2008, 2009). In addition, terminally differentiated cells such as mature B cells, T cells and pancreatic b-cells can also be reprogrammed into iPS cells (Hong et al. 2009; Hanna et al. 2008; Stadtfeld et al. 2008a).In human, fibroblasts derived from a fetus, neonatal foreskin and adult dermis are widely used (Takahashi et al. 2007; Yu et al. 2007). Human iPS cells were also generated from keratinocytes, mesenchymal stroma cells and hematopoietic cells (Aasen et al. 2008; Loh et al. 2009). The efficiency of iPS cell generation from these cell types thus seems to be similar, although direct comparisons among them still need to be carried out.8.3 P ropertiesThe characteristics of mouse iPS cells are almost completely equivalent to those of mouse ES cells. The morphology of both mouse ES cells and iPS cells is identical. Those two cells types can grow in serum-containing medium in the presence of leukemia inhibitory factor (LIF) and/or feeder cells (Okita et al. 2007). They can also be maintained in serum-free medium supplemented 2i (Silva et al. 2008).The expression levels of pluripotent cell marker genes such as ERas, Rex1 and Esg1are indistinguishable between ES cells and iPS cells. Microarray analyses have also shown the global gene expression patterns of mouse iPS cells to be very similar to those of mouse ES cells (Okita et al. 2007; Wernig et al. 2007; Maherali et al. 2007). In addition, iPS cells also have the potential to undergo homologous recombination that is a useful property of ES cells in biology (Hanna et al. 2007).Not only the transcripts but the epigenetic status of iPS cells and ES cells, including DNA methylation and histone modification, are quite similar (Meissner et al. 2008). CpG methylation in the promoter regions of pluripotent cell marker genes such as Oct3/4, Rex1and Nanog are highly unmethylated in iPS cells, whereas those of MEFs or TTFs were steadily methylated. Previous reports d emonstrated that both the 4th (K4) and 27th (K27) lysine residues of histone H3 are methylated around the locus of differentiation-associated genes such as Gata4, Pax6 and Msx2 in mouse ES cells (Bernstein et al. 2006). Generally, K4 is methy-lated in the regions transcriptionally activated. In contrast, methylation of K27 reflects silencing in the vicinity. These bivalent patterns of histone methylation may imply that ES cells are always ready and waiting to initiate differentiation. In addi-tion, mouse iPS cells also show bivalent patterns of histone methylation in differ-entiation marker genes as similar to mouse ES cells (Maherali et al. 2007). Therefore, in the broad view of both external and inner aspects, it seems that iPS and ES cells have a striking resemblance. However, detailed analyses suggest that194K. Takahashi and S. Yamanaka the epigenetic patterns are not completely identical between ES cells and iPS cells (Mikkelsen et al. 2008). On the other hand, differences in these properties can be found among iPS clones.These similarities and differences are also found in human cells. In particular, the patterns of global DNA methylation differ between human iPS cells and human ES cells (Chin et al. 2009). On the other hand, various differences such as gene expres-sion patterns, statuses of X-chromosome inactivation and differentiation capacities have been reported even among human ES clones (International Stem Cell Initiative 2007). One of the conceivable reasons for this is the variety of genetic backgrounds among humans, unlike the situation regarding experimental animals. In fact, ES clones derived from different blastocysts provided by the same couple have been shown to have a strong resemblance to each other (Chen et al. 2009).8.4 D ifferentiation Capacity and Their PrecursorsMany protocols for in vitro differentiation of mouse ES cells have been estab-lished. Most of them can be applied to iPS cells. The traditional method with embryoid body formation allows iPS cells to differentiate into all three germ layers of endoderm, mesoderm and ectoderm (Takahashi and Yamanaka 2006; Wernig et al. 2007; Maherali et al. 2007). In vitro differentiations of iPS cells into specific cell types such as cardiac cells, bloods, adipocytes and retinal epitheliums has also been achieved (Schenke-Layland et al. 2008; Narazaki et al. 2008; Tashiro et al. 2009; Senju et al. 2009). The gold standard to test the pluripotency is the genera-tion of chimeric mice and the subsequent germ-line transmission. Similar to ES cells, mouse iPS cells are able to contribute to the development of chimeric mice including germ cells (Okita et al. 2007; Wernig et al. 2007; Maherali et al. 2007). The successful rate of germ-line transmission for iPS cells is no less than that for ES cells. In addition, mouse iPS cells have hurdled the stricter challenge of tetra-ploid complementation (Kang et al. 2009; Zhao et al. 2009; Boland et al. 2009). The tetraploid embryos generated by the fusion of two eggs can contribute only to the placenta instead of the pup body. When iPS cells are injected into a tetraploid blastocyst, the entire body of the pup should be derived from the injected iPS cells. The pups only from iPS cells are then successfully born. These results suggest that mouse iPS cells have already reached the pluripotency of ES cells.Most of the protocols for human ES cell differentiation are also applicable to human iPS cells. Random differentiation of human iPS cells can be achieved by embryoid body formation in vitro or teratoma experiments in vivo (Takahashi et al. 2007; Yu et al. 2007). Directed differentiation into specific cell lineages has also succeeded, such as differentiation into retinal cells, vascular cells, pancreatic i nsulin-producing cells, hepatocyte-like cells, functional cardiomyocytes and neuronal cells (Osakada et al. 2009; Viczian et al. 2009; Taura et al. 2009; Zhang et al. 2009a, b; Song et al. 2009; Gai et al. 2009; Karumbayaram et al. 2009; Chambers et al. 2009).195 8 Induced Pluripotent Stem Cells8.5 P otential Applications for TherapiesOne of the potentially useful applications of iPS cell technology is that the source of regenerative medicine using a patient’s own pluripotent stem cells (Yamanaka 2009). These order-made iPS cells would thus make it possible to achieve autolo-gous transplantation. The first study for therapeutic application of iPS cells was reported with the mouse model of sickle-cell anemia, a blood disease caused by a defect in the b-globin gene (Hanna et al. 2007). They established iPS cells from the diseased mouse, and then repaired their genetic defects by homologous recombina-tion. The injection of hematopoietic progenitors derived from genetically-corrected iPS cells could cure the diseased donor mouse. Another report showed the injection of iPS-derived cells directly into the liver of irradiated hemophilia A mice to improve their phenotypes (Xu et al. 2009). These are examples of ideal models for regenerative medicine. In human case, the idea of iPS cell therapy was also brought up by Raya and colleagues (Raya et al. 2009). At first, they corrected genes by introducing a lentiviral vector encoding FANCA or FANCD2in keratinocytes derived from Fonconi anemia patients. iPS cells derived from the patients with genetic correction can be differentiated into the hematopoietic lineage.Moreover, dopaminergic neurons differentiated from iPS cells were able to improve the behavior of a Parkinson’s disease model rat through transplantation into the brain (Wernig et al. 2008c). On the other hand, however, they found that residual undifferentiated iPS cells included in the cells for transplantation caused a teratoma. Undifferentiated cells and the subsequent tumor formation after trans-plantation remain to be a major complication of pluripotent cell therapies, not only with iPS cells, but also with ES cells.The depletion of SSEA-1 positive cells, which means undifferentiated cells, from the cultures by fluorescence-activated cell sorter (FACS) can reduce the risk of teratoma formation after cell transplantation (Wernig et al. 2008a). This issue was analyzed with a different point of view in the work of Miura and colleagues (Miura et al. 2009). They differentiated 36 mouse iPS cell lines derived from embryonic or adult cells as well as ES cells into neural progenitor cells using the sphere culture method (Miura et al. 2009). They found that residual undifferenti-ated cells existed in less than 0.5% of ES cells or MEF-derived iPS cell lines. In contrast, TTF-derived iPS cell lines reproducibly produced a significantly higher ratio of undifferentiated cells. Interestingly, such differences showed no clear rela-tionship with the presence or absence of Myc transgenes.8.6 C onclusion and PerspectiveHuman iPS cells have another potential utility as a tool for drug discovery or under-standing the pathogenesis of diseases. Over the last couple of years, iPS cells were established from somatic cells of patients with refractory diseases such as Amyotrophic lateral sclerosis (ALS), Duchenne muscular dystrophy, Down s yndrome and196K. Takahashi and S. Yamanaka Parkinson’s disease, milial dysautonomia, type I diabetes, beta-thalassemia and Fanconi anemia (Park et al. 2008a; Maehr et al. 2009; Ye et al. 2009; Soldner et al. 2009). Heretofore, it was difficult to analyze the pathogenesis of specific diseases in vitro because large amount of the patient’s cells are needed. iPS cells established from the patients may overcome the issue with their indefinite self-renewal ability. Combining the proliferation of undifferentiated iPS cells and the differentiation of specific cell types can yield an enormous amount of cells carrying the causal factors of diseases as associated with genetic mutations can be obtained, and used for large-scale screening or analyses.If pathological conditions can be recapitulated in vitro using iPS cells from the patients, they could be used for screening therapeutically-effective molecules, and/ or for the evaluation of medicine side-effects for each individual patient. For example, Long-QT syndromes (LQTS) are congenital or acquired types of diseases with delayed repolarization and subsequent depolarization of the heart. This can lead to a risk of ventricular fibrillation and unexpected death. A mutation in one of several disease-causing genes can bring on LQTS, and the effective medication is different among each type of LQTS. An epinephrine-loading test seems to be effec-tive to determine if a patient has LQTS. However, this test may carry a certain degree of risk. Functional cardiomyocytes derived from patient’s iPS cells can be used for the in vitro diagnosis of LQTS, thus reducing the burden and risk for the patient.However, recapitulation pathogenesis with disease-specific iPS cells does not always work well. Dimos et al. established iPS cells derived from an ALS patient (Dimos et al. 2008). They successfully differentiated ALS-iPS cells into both glial cells and motor neurons. However, although the glial cells of ALS patient produce toxins and result in destroying motor neurons, they failed to show the phenomenon in vitro with iPS cells. In contrast, Ebert and colleagues generated iPS cells carrying spinal muscular atrophy (SMA) which is a neurological disorder developed during infancy and causes death. Motor neurons derived from SMA patient’s iPS cells showed a defect in the maturation of motor neurons (Ebert et al. 2009). Another paper also reported the success of reproducing a pathological condition. They choose Familial dysautonomia (FD) as a model of pathogenesis, which shows peripheral neuropathy induced by a reduction in the expression of the IKBKAP gene. They developed neural crest precursor cells from FD-iPS cells. As result, they observed a defect of cell migration and spontaneous differentiation into TuJ1 or ASCL1 positive neurons. In addition, they treated the cells with kinetin which could correct the expression of IKBKAP in mutant cells, and it markedly improved the phenotypes required for cell migration. Therefore, although not in all cases, these data indicate that the recapitulation of the pathogenesis and subsequent tests for drug effects are feasible.First iPS cells were generated by transduction with four reprogramming factors with retroviral vectors (Takahashi and Yamanaka 2006). This method has proven to be the most effective. However, viral integration into the genome should be avoided for clinical applications, because of destruction or unexpected activation of adjacent genes, which may result in tumor formation. Many attempts have been。