原发性乳腺淋巴瘤
- 格式:pdf
- 大小:1.06 MB
- 文档页数:5
原发性乳腺淋巴瘤有哪些症状?*导读:本文向您详细介绍原发性乳腺淋巴瘤症状,尤其是原发性乳腺淋巴瘤的早期症状,原发性乳腺淋巴瘤有什么表现?得了原发性乳腺淋巴瘤会怎样?以及原发性乳腺淋巴瘤有哪些并发病症,原发性乳腺淋巴瘤还会引起哪些疾病等方面内容。
……*原发性乳腺淋巴瘤常见症状:乳房肿块、乳房肥大、乳房硬化、乳房胀痛*一、症状一、症状最常见的临床表现出现单侧乳腺的肿块,右侧侵犯多见。
只有一组报道见侵犯左侧,约5%~25%可见双侧侵犯。
只有少数发生于男性。
临床表现为无痛性、相对活动的增大的肿块,一般与皮肤不粘连,此肿块常在体检或乳腺扫描时发现,需要与浸润性乳腺癌鉴别。
不常见的表现是在怀孕的年轻妇女可见乳房短期内迅速增大,可触及双侧肿块。
组织学检查为Burkitt或Burkitt样淋巴瘤。
此病预后极差,因为肿瘤增长迅速,大范围播散,可侵犯卵巢和中枢神经系统。
这种临床表现在非洲多见,西方国家也偶见报道。
乳腺淋巴瘤好发于右侧,腋窝淋巴结受累者为30%~40%,其质地较实体瘤软。
二、诊断具备以下几条可诊断为原发性乳腺淋巴瘤:①临床上证实乳腺为首发或主要部位;②无其他部位淋巴瘤的证据,排除同侧腋窝淋巴结侵犯的存在;③局部淋巴结侵犯应是乳腺病变与淋巴结病变同时出现。
继发性乳腺淋巴瘤可定义为所有不符合上述标准的侵犯乳腺的淋巴瘤。
*以上是对于原发性乳腺淋巴瘤的症状方面内容的相关叙述,下面再看下原发性乳腺淋巴瘤并发症,原发性乳腺淋巴瘤还会引起哪些疾病呢?*原发性乳腺淋巴瘤常见并发症:乳房结核*一、并发病症也有文献报道合并其他自身免疫病,如Sj?gren综合征等。
*温馨提示:以上就是对于原发性乳腺淋巴瘤症状,原发性乳腺淋巴瘤并发症方面内容的介绍,更多疾病相关资料请关注疾病库,或者在站内搜索“原发性乳腺淋巴瘤”可以了解更多,希望可以帮助到您!。
乳腺原发性弥漫性大B细胞性淋巴瘤22例临床病理分析作者:司成来源:《中国保健营养·下旬刊》2014年第03期[摘要] 目的对乳腺原发性弥漫性大B细胞性淋巴瘤的诊断、治疗及预后进行探讨、分析,并对临床病理特征、免疫表型等进行观察。
方法随机抽取我院自2005年3月——2010年6月收治的按照世界卫生组织标准诊断为乳腺原发性弥漫性大B细胞性淋巴瘤的患者共22例,对其临床病理特征、免疫表型进行观察、分析,并实施随访。
结果乳腺原发性弥漫性大B细胞性淋巴瘤患者共22例,均为女性,年龄32-76岁,平均年龄53.2岁。
所有患者中肿块位于左侧乳房的有8例,肿块位于右侧乳房的有12例,肿块位于双侧乳房的有2例。
按照AnArbor分期,Ⅳ期的患者为1例,Ⅲ期的患者为2例,Ⅱ期的患者为9例,Ⅰ期的患者为10例。
最为常见的首发症状为乳腺单侧肿块。
大多表现为肿瘤性淋巴细胞弥漫浸润,中等大小或较大,部分呈列兵状排列,个别残留了部分乳腺结构,淋巴上皮可见部分病变,部分坏死。
非生发中心B细胞型患者可进行免疫分型。
对16例患者成功实施了随访,10例患者的存活期为20-83个月;6例患者于手术后6-16个月后死亡。
结论临床上,乳腺原发性弥漫性大B细胞性淋巴瘤较为少见,非生发中心B细胞型较为多见,免疫组化标记能够较好的利于患者病情的明确诊断。
对该病的治疗,以手术辅助联合放、化治疗为宜。
[关键词] 原发性;B细胞性淋巴瘤;病理分析;预后文章编号:1004-7484(2014)-03-1291-02原发性乳腺淋巴瘤较为少见,由Wiseman[1]等于上世纪七十年代首次发现并确定其诊断标准,以非霍奇金淋巴瘤为主,其中数量较多的为B细胞,以弥漫性大B细胞性淋巴瘤为主。
患者罹患该病后,一般治疗效果较差,且在临床诊断时容易发生误诊。
现为积累经验,达到与同行分享、交流的目的,随机抽取我院自2005年3月——2010年6月收治的乳腺原发性弥漫性大B细胞性淋巴瘤的患者共22例,进行回顾性分析,并报告如下。
原发性乳腺淋巴瘤怎样治疗?*导读:本文向您详细介绍原发性乳腺淋巴瘤的治疗方法,治疗原发性乳腺淋巴瘤常用的西医疗法和中医疗法。
原发性乳腺淋巴瘤应该吃什么药。
*原发性乳腺淋巴瘤怎么治疗?*一、西医*1、治疗尽管原发性乳腺淋巴瘤为一罕见病,但仍应作为乳腺肿瘤的一种独立疾病进行诊断,对于源于乳腺的淋巴瘤还没有统一的治疗方案,许多研究组报道它的治疗与具有相同组织学类型的全身性淋巴瘤相似。
最早采用单纯手术方式,后来放疗作为一种新手段与手术联合进行,20世纪70年代后则不采用根治术等这些致残性手术,而以切除活检,辅助放疗和(或)化疗取代,扩大性局灶切除也是不必要的,因为这些肿瘤细胞对于放疗和全身化疗特别敏感,一般不提倡乳腺切除,外科手术通常只用于在化疗和放疗不能控制时进行减少瘤负荷,De Blasio等对Ⅰ期患者应用40Gy照射乳腺区域淋巴结及手术活检区,取得了较好的局部控制,由于Ⅱ期患者有远处复发的危险性(70%),所以联合化疗很有必要。
Kim等(1999)报道ⅠAE期采用局部治疗可治率,但ⅡAE期病人应采用全身化疗后放疗,化疗方案仍以CHOP为标准方案,Ribrag等报道应用CHOP方案治疗20例局限性B细胞性淋巴瘤(16例为中心性弥漫大B细胞淋巴瘤),16例CR,2例PR,2例进展,中位随访54个月,6个病人在8~66个月后复发,其中2例复发病人累及中枢神经系统,2例PR病人在化疗后4或8个月也累及中枢神经系统,因此,此类病人应采用中枢神经系统预防治疗。
总之,该病发病率低,但恶性程度高,治疗宜采用综合手段,根治性乳房手术并不能有效提高生存率,Ⅱ期以上病人或恶性度高的组织亚型治疗倾向于使用联合方案,它需要多学科综合治疗。
*2、预后临床分期和组织学类型对于决定其预后特别重要,所有病例的5年总生存率为43%;Ⅰ期患者5年无复发生存率为50%,总生存率为61%;而Ⅱ期患者分别为26%和27%,组织学类型也可决定中位生存期:滤泡中心母细胞性/中心细胞性淋巴瘤为63个月,弥漫型中心母细胞性/中心细胞性淋巴瘤为52个月,中心母细胞性淋巴瘤为42个月,免疫母细胞性淋巴瘤为47个月,高度恶性的大细胞性或Burkitt淋巴瘤应该应用联合化疗加或不加放疗。
原发性乳腺弥漫大B细胞淋巴瘤临床和病理特征汪园园;杨喆;邓元;常红云;李晓锋;张冠军;刘希【摘要】目的探讨原发性乳腺弥漫大B细胞淋巴瘤(primary breast diffuse large B-cell lymphoma,PB-DLBCL)的临床病理特征和遗传学上MYC基因重排情况.方法回顾性分析西安交通大学第一附属医院收治的8例PB-DLBCL临床病理资料,术前均诊断为乳腺癌或炎症.肿瘤最大直径1.8~7.4 cm,平均3.3 cm,其中ⅠEA期5例,ⅡEA期2例,ⅣE期1例.行免疫组织化学染色进行免疫分型,采用原位杂交检测EBV感染状态,采用荧光原位杂交检测MYC重排情况.结果 PB-DLBCL的肿瘤细胞弥漫或略呈结节状浸润乳腺组织,可见残存的乳腺导管.肿瘤细胞呈中等-大的中心母或免疫母细胞样形态.根据Hans分型,非生发中心B细胞型7例(87.5%),生发中心B细胞型1例(12.5%).8例病例EBER原位杂交均为阴性,无EBV感染.MYC荧光原位杂交检测显示无MYC重排或扩增.结论PB-DLBCL临床表现难与乳腺癌、乳腺炎症区别,确诊需依靠病理组织学和免疫表型分析.PB-DLBCL免疫表型分型大部分为非生发中心型,目前研究尚未见PB-DLBCL中MYC重排阳性.【期刊名称】《分子诊断与治疗杂志》【年(卷),期】2018(010)005【总页数】6页(P295-300)【关键词】乳腺;弥漫大B细胞淋巴瘤;临床病理;免疫表型;MYC基因重排【作者】汪园园;杨喆;邓元;常红云;李晓锋;张冠军;刘希【作者单位】西安交通大学第一附属医院病理科,陕西,西安710061;西安交通大学第一附属医院病理科,陕西,西安710061;西安交通大学第一附属医院病理科,陕西,西安710061;西安交通大学第一附属医院病理科,陕西,西安710061;西安交通大学第一附属医院病理科,陕西,西安710061;西安交通大学第一附属医院病理科,陕西,西安710061;西安交通大学第一附属医院病理科,陕西,西安710061【正文语种】中文原发性乳腺弥漫大B细胞淋巴瘤(primary breast diffuse large B-cell lymphoma,PB-DLBCL)是恶性程度较高的淋巴瘤,约占原发性乳腺恶性肿瘤的0.5%,占非霍奇金淋巴瘤的1%,占结外淋巴瘤的3%[1]。
原发性乳腺恶性淋巴瘤怎样治疗?*导读:本文向您详细介绍原发性乳腺恶性淋巴瘤的治疗方法,治疗原发性乳腺恶性淋巴瘤常用的西医疗法和中医疗法。
原发性乳腺恶性淋巴瘤应该吃什么药。
*原发性乳腺恶性淋巴瘤怎么治疗?*一、西医*1、治疗:有学者认为根治术加术后放疗是本病的最好治疗方法。
但近来大多数作者认为对本病采取合理的综合治疗措施可以延长患者的生存期。
综合治疗要全面细致地了解病情,充分考虑各种治疗方法的利弊,制定出一套包括手术、化疗、放疗及免疫治疗等方法在内的科学合理的治疗方案。
1.手术治疗:在综合治疗中具有重要意义。
因为手术虽不能彻底治愈,但却可去除肿瘤负荷,为其他治疗方法创造有利条件。
术中应注意无瘤技术操作,并干净彻底地将肿瘤和乳腺所属淋巴结一并去除。
2.化疗:本病主要播散途径是经血行和临近淋巴结侵犯。
因此,化疗的作用是不可忽视的。
可采用标准的CHOP方案和MOPP、COPP、CVPP等方案进行化疗。
3.放疗:对早期病人很敏感,甚至有人提出单独放疗可取得长期生存。
但从大量文献报道看,手术加放疗对控制原发灶一般是成功的,对Ⅱa期病人给予放疗加化疗的综合治疗,治愈率可达90%以上。
有人统计1500例Ⅰ~Ⅱa期病人的放疗加化疗的资料,5年生存率可达88%~98%。
*2、预后:1.本病预后较差,组织学类型是影响预后的主要因素。
结节型比弥漫型预后好;分化好的小细胞型比分化差的大细胞型预后好;分化差的曲核细胞型预后更差。
它好发于年轻病人,常伴纵隔肿块,易侵犯骨髓并转为白血病。
2.分期亦是影响预后的关键因素,分期越晚预后则越差。
*温馨提示:上面就是对于原发性乳腺恶性淋巴瘤怎么治疗,原发性乳腺恶性淋巴瘤中西医治疗方法的相关内容介绍,更多更详尽的有关原发性乳腺恶性淋巴瘤方面的知识,请关注疾病库,也可以在站内搜索“原发性乳腺恶性淋巴瘤”找到更多扩展资料,希望以上内容对大家有帮助!。
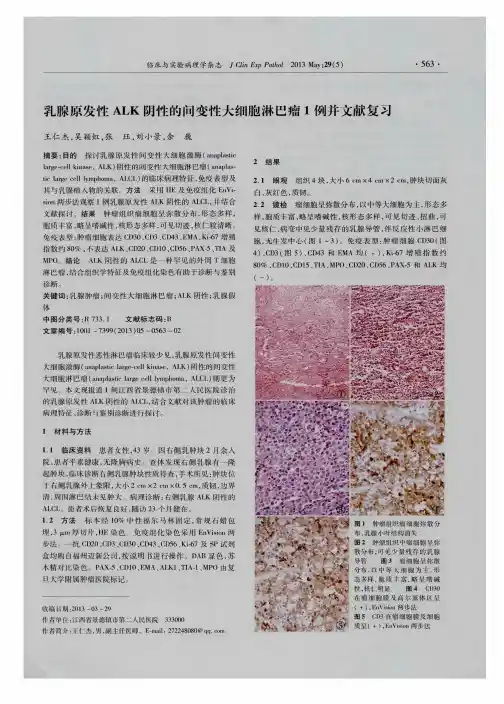
Mammographic and sonographic findings of primary breast lymphomaChae Yeon Lyou,Sang Kyu Yang 4,Du Hwan Choe,Byung Hee Lee,Kie Hwan KimDepartment of Radiology,Korea Cancer Center Hospital,Seoul,KoreaReceived 5December 2006;accepted 15February 2007AbstractThe objective of this study was to describe the mammographic and sonographic appearances of primary lymphoma of the breast.We retrospectively reviewed the mammographic and ultrasonographic images of 12patients with primary lymphoma of the breast.Descriptions of imaging findings were made according to the Breast Imaging Reporting and Data System lexicon by two radiologists.Mammography was performed on 11patients.Most of the lesions were shown to be oval-shaped (72.7%)and high-density (90.9%)masses on mammography.Ultrasound examination was performed on 8patients.The lymphomas were commonly single (75%),circumscribed (50%)or microlobulated (37.5%),and oval (50%)masses on sonography.The echo pattern of the mass was hypoechoic in 7patients (87.5%)but hyperechoic in 1patient (12.5%).No mass had spiculated margins or calcifications.Ipsilateral axillary lymph node involvement was noted in 1patient.In conclusion,most primary lymphomas of the breast present as oval-shaped and high-density masses on mammography and as single and hypoechoic masses with circumscribed or microlobulated margins on sonography.D 2007Elsevier Inc.All rights reserved.Keywords:Breast;Lymphoma;Ultrasound;Mammography1.IntroductionThe breast is an uncommon site of development for malignant lymphomas despite the relative frequency of primary extranodal non-Hodgkin lymphomas.Breast lym-phomas can be either primary or secondary.Secondary breast lymphomas more commonly occur in association with extramammary non-Hodgkin lymphomas.Primary breast lymphomas are less common,accounting for only 0.05%–0.53%of all breast malignancies [1].There are few articles about the imaging findings of primary breast lymphoma in the radiology literature [2–7].Data on the sonographic appearance of primary breast lymphomas are even more limited than those on its mammographic appearance.We reviewed 12cases of primary lymphoma of the breast to determine the mammo-graphic and sonographic characteristics of this rare diseasewith the American College of Radiology Breast Imaging Reporting and Data System (BI-RADS)lexicon [8].2.Materials and methodsA retrospective review of medical records at our institution that date between January 1993and October 2006revealed 12patients with primary breast lymphoma.All cases were diagnosed based on pathological demonstration after surgical biopsy or ultrasound (US)-guided core needle biopsy and satisfied the specific diagnostic criteria described by Wise-man and Liao [9]for primary lymphoma of the breast,including histological evidence of a close association between the mammary tissue and the lymphomatous infiltrate as well as absence of disseminated lymphoma or preceding extramammary lymphoma at the time of diagnosis.Presence of homolateral axillary node involvement is acceptable provided that both lesions developed simultaneously.The patients’ages at the time of the diagnosis as well as their physical findings and clinical status were abstracted from the medical records.We reviewed the pathological0899-7071/07/$–see front matter D 2007Elsevier Inc.All rights reserved.doi:10.1016/j.clinimag.2007.02.0284Corresponding author.Department of Radiology,Korea Cancer Center Hospital,215-4Gongneung-Dong,Nowon-Gu,Seoul 139-706,Korea.Tel.:+8229701576;fax:+8229702433.E-mail address:twoscan@ (S.K.Yang).Clinical Imaging 31(2007)234–238reports of all lesions and then determined the histological subtypes of lymphoma according to the classification by the World Health Organization.Mammograms were available for11patients.Mammog-raphy was performed using dedicated film-screen equipment (Senographe600T,GE Health Care)and single-emulsion film.Images were obtained in two standard planes(medio-lateral oblique and craniocaudal).US of the breast was also performed before biopsy in eight images were obtained using HDI5000 (Advanced Technology Laboratories,Bothell,WA,USA) and SSD-5500(Aloka,Tokyo,Japan)with a5-to12-MHz linear array.Mammograms and US images were reviewed by two radiologists,and the imaging appearances were determined by consensus.Descriptions of imaging findings were made according to the BI-RADS lexicon.Mammograms were reviewed to determine the presence of focal masses,the shape,margin,and density of the masses,calcifications,and axillary images were assessed for the presence of masses,the number and size of the masses,shape,margins,echo pattern,orientation,posterior acoustic features,and presence of calcifications.3.ResultsAll12patients were women;at the time of their diagnosis,their ages ranged from23to62years(mean age=46years).Breast symptoms in all patients were present as palpable lumps.Pain was present in only1patient. Clinical evidence of skin retraction and nipple discharge were absent in all patients.The right breast was involved in 5patients(41.7%),whereas the left was involved in 7(58.3%).All patients were diagnosed as having non-Hodgkin lymphoma,with the most common subtype being diffuse large B-cell lymphoma(83.4%,n=10/12)(Fig.1C and1D). One patient had a small lymphocytic B-cell lymphoma (8.3%,n=1/12),and another had a Burkitt-like high-grade B-cell lymphoma(8.3%,n=1/12).On mammography,all breast lesions presented as masses (100%,n=11/11).Eight of the masses were oval(72.7%, n=8/11),two were round(18.2%,n=2/11),and one was irregular(9.1%,n=1/11)(Table1).All except one were high-density masses(90.9%,n=10/11),and one was isodense to the adjacent glandular tissue(9.1%,n=1/11). Four masses had indistinct margins(36.3%,n=4/11),three had circumscribed margins(27.3%,n=3/11),and another three had obscured margins(27.3%,n=3/11).No mass had calcifications(Figs.1A,2A,and3A).Ipsilateral axillary lymphadenopathy was noted in one patient.On US,most patients presented with a single mass(75%, n=6/8),but two patients had multiple masses.The diameter of masses ranged from0.7to 5.9cm(mean diame-ter=2.3F1.7cm).The long axis of all masses paralleled the skin line(wider-than-tall or horizontal orientation).The shape of masses appeared as oval(50%,n=4/8),irregular (37.5%,n=3/8),or round(12.5%,n=1/8).Circumscribed and microlobulated margins were common—in50%(n=4/ 8)and37.5%(n=3/8)of the masses,respectively(Table2). The echo pattern of the mass was hypoechoic in seven patients(87.5%)(Fig.1B and Fig.2B)but hyperechoic in one patient(12.5%)(Fig.3B).Posterior enhancement was observed in six patients(75%),no posterior acoustic feature was observed in two(25%),and posterior acoustic shadowing was not observed in any patient.No mass had spiculated margins or calcifications.4.DiscussionPrimary lymphomas of the breast are rare,accounting for only1.7%–2.2%of extranodal lymphomas and for only 0.4%–0.7%of all non-Hodgkin lymphomas[10].To our knowledge,there are only few articles about breast lymphomas,except for case reports,in the radiology literature.We tried to describe the characteristics of the mammographic and sonographic features of primary breast lymphomas with the BI-RADS lexicon.A primary breast lymphoma may be very well defined and may be mistaken for a benign process,most notably in patients younger than35years[2],in whom cysts and fibroadenomas are more common.The key in the evaluation of these cases remains to be adequate tissue biopsy for histopathological evaluation and immunophe-notyping[11].The original diagnostic criteria for primary breast lymphoma were suggested by Wiseman and Liao [9]in1972.In our series,diffuse large B-cell lymphoma was the most frequent histological subtype.This result is consistent with the findings of another study[10]. Table1Mamographic findings of primary breast lymphomas(n=11) Mammographic finding Sample distribution[n(%)] ShapeRound2(18.2)Oval8(72.7)Lobular0(0)Irregular1(9.1)MarginCircumscribed3(27.3) Microlobulated1(9.1)Obscured3(27.3)Indistinct4(36.3)Spiculated0(0)DensityHigh10(90.9)Equal1(9.1)Low0(0)Fat containing0(0)CalcificationsPresent0(0)Absent11(100)C.Y.Lyou et al./Clinical Imaging31(2007)234–238235Lieberman et al.[7]reported that the imaging pattern of mammary non-Hodgkin lymphoma was unrelated to its histopathological subtype.Symptoms of mammary lymphomas may mimic those of carcinoma and cause difficulties in differential diagnosis.Breast lymphomas usually present as solitary painless lumps in younger patients as compared with breast carcinomas [12].This most likely reflects the relatively rapid growth of these lesions,as compared with breast carcinomas,especially in younger patients.The literature reveals that breast lymphomas can occasionally present as a diffuse rapid breast enlargement in the younger age group or as breast skin thickening caused by lymphatic blockage by lymphomas,resulting in retrograde edema [3].In our series,the age range of the patients at diagnosis was 23–62years (mean age=46years).All patients had a palpable lump.Pain was present in one patient.The right breast was involved in five patients (41.7%),whereas the left was involved in seven (58.3%).An unexplained right-sided predominance,in contrast to left-sided predominance documented in breast carcinomas,was classically described in primary lymphomas of the breast [1,8,13,14],but this was not noted in our series.Several studies had been performed to confirm the mammographic appearance of breast lymphomas.Lieber-man et al.[7]reviewed among 29women 32cases of non-Hodgkin lymphoma,of which 21(66%)were classified as primary breast non-Hodgkin lymphomas;mammograms revealed solitary and uncalcified masses in 69%of the cases,multiple masses in 9%,and diffuse increased opacity with skin thickening in 9%.Four cases (13%)had normal findings.Paulus [3]presented 31patientswithFig.1.Images for a 47-year-old woman with diffuse large B-cell lymphoma.(A)Craniocaudal mammogram of the right breast showing a high-density and oval mass (white arrows)with partially obscured margins (black arrows).(B)US image showing a 3-cm-diameter,hypoechoic,and oval mass (white arrows)with microlobulated margins (black arrows)and posterior acoustic enhancement.(C)Low-power view of surgical biopsy specimen showing that lymphocytic infiltrates replaced the normal architecture of the underlying breast parenchyma (hematoxylin–eosin,original magnification Â40).(D)High-power view showing that the mass is composed of medium-sized to large lymphoid cells with oval-to-round vesicular nuclei with fine chromatin.The cytoplasm is scanty and amphophilic to basophilic (hematoxylin–eosin,original magnification Â200).C.Y.Lyou et al./Clinical Imaging 31(2007)234–238236mammographic changes of proven reticuloendothelial system disease in which the masses in breast lymphomas were of homogeneous density and did not contain tumor calcifications and noted that there was no stromal distortion of the surrounding breast parenchyma as is recognized and often found in breast carcinomas.A less common mammographic finding of lymphomas is diffuse increased parenchyma density with or that without skin thickening.This pattern of involvement is predominantly observed in patients with a high-grade lymphoma [5].Axillary lymphadenopathy may be associated with primary lymphoma of the breast,but this is not a prominent feature of most reported cases [2,15–18].Mammographically,a solitary mass was the most common radiological pattern in our study.Most masses had an oval shape and were of high density.Margins were variable.Calcifications present in up to half of thecarcinomas were not seen in our series of lymphomas,in agreement with previous series [2,4,5,7].Desmoplastic or fibrotic reaction with architectural distortion often seen surrounding breast carcinomas was not demonstrated in the masses.Diffuse increased parenchymal density was not observed in any patient.Not much has been written about US findings of breast lymphomas [4–7].A hypoechoic,homogeneous,or hetero-geneous well-defined mass is the most common US finding among patients with malignant lymphoma of the breast [6,7].However,a wide spectrum of appearances,ranging from well defined to poorly defined,focal to diffuse [4–7],and hypoechoic to hyperechoic [4],has been described in previously reported series.Primary breast lymphoma can be present as an elongated cystic structure or an ellipsoid,well-defined,and complex lesion on US [11,17].There is one case of primary breast lymphoma that mimicked acute mastitis in a young woman [18].In our study,most masses showed an oval shape with circumscribed or microlobulated margins and a hypoechoic echo pattern,and one case showed a hyperechoic echo pattern on US.All masses had a horizontal orientation to the skin line.Most of themassesFig. 2.Images for a 56-year-old woman with diffuse large B-cell lymphoma.(A)Mediolateral oblique mammogram of the left breast showing a high-density and oval mass (white arrows)with partially indistinct margins (black arrows).(B)US image showing a large and hypoechoic mass (arrows)with irregularmargins.Fig. 3.Images for a 50-year-old woman with diffuse large B-cell lymphoma.(A)Craniocaudal mammogram of the right breast showing a high-density and round mass (arrows)in the outer part of the breast.(B)US image showing a circumscribed hyperechoic mass (arrows).C.Y.Lyou et al./Clinical Imaging 31(2007)234–238237showed posterior acoustic enhancement.No mass had spiculated or angulated margins.The greatest limitations of our study are caused by the small sample size,which is a direct reflection of the rarity of this lesion.Characterization of a larger number of primary breast lymphoma cases would be necessary to draw conclusions of any meaningful significance.Although the small study population with this rare disease clearly limits the value of the data obtained,certain tendencies were observed.In conclusion,most primary breast lymphomas present as oval-shaped and high-density masses on mammography and as single and hypoechoic masses with circumscribed or microlobulated margins on US.References[1]Brustein S,Filippa DA,Kimmel M,Lieberman PH,Rosen PP.Malignant lymphoma of the breast:a study of 53patients.Ann Surg 1987;205:144–50.[2]Meyer JE,Kopans DB,Long JC.Mammographic appearance ofmalignant lymphoma of the breast.Radiology 1980;135:623–6.[3]Paulus DD.Lymphoma of the breast.Radiol Clin North Am1982;20:561–8.[4]Jackson FI,Lalani ZH.Breast lymphoma:radiologic imaging andclinical appearance.Can Assoc Radiol J 1991;42:48–54.[5]Sabate JM,Gomez A,Torrubia S,Camins A,Rosen N,De Las HerasV ,Villalba-Nuno V .Lymphoma of the breast:clinical and radiologic features with pathologic correlation in 28patients.Breast J 2002;8:294–304.[6]Pope TL,Brenbridge AN,Sloop FB,Morris JR,Carpenter J.Primaryhistiocytic lymphoma of the breast:mammographic,sonographic and pathologic correlation.J Clin Ultrasound 1985;13:667–70.[7]Lieberman L,Giess CS,Dershaw DD,Louie DC,Deutch BM.Non-Hodgkin lymphoma of the breast:imaging characteristics and cor-relation with histopathologic findings.Radiology 1994;192:157–60.[8]American College of Radiology.Breast Imaging Reporting and DataSystem:BI-RADS atlas.4th ed.Reston (Va)7American College of Radiology;2003.[9]Wiseman C,Liao KT.Primary lymphoma of the breast.Cancer1972;29:1705–12.[10]Topalovski M,Crisan D,Mattson JC.Lymphoma of the breast Aclinicopathological study of primary and secondary cases.Arch Pathol Lab Med 1999;123:1208–18.[11]Mason HS,Johari V ,March DE,Crisi GM.Primary breast lymphoma:radiologic and pathologic findings.Breast J 2005;11:495–6.[12]Giardini R,Piccolo C,Rilke F.Primary non-Hodgkin’s lymphomas ofthe female breast.Cancer 1992;69:725–35.[13]Mambo NC,Burke JS,Butler JJ.Primary malignant lymphomas ofthe breast.Cancer 1977;39:2033–40.[14]Schouten JT,Weese JL,Carbone PP.Lymphoma of the breast.AnnSurg 1981;194:749–53.[15]Assaly T,Palayew MJ,Lisbona A,Alpert L.General case of the day.Radiographics 1992;12:602–5.[16]Watson AP,Fraser SE.Primary lymphoma of the breast.AustralasRadiol 2000;44:234–6.[17]Gal-Gombos EC,Esserman LE,Poniecka AW,Poppiti RJ.Is apseudocystic serpentine mass a sonographic indicator of breast lymphoma?Radiologic–histologic correlation of an unusual finding.AJR Am J Roentgenol 2001;176:734–6.[18]Grubstein A,Givon-Madhala O,Morgenstern S,Cohen M.Extranodalprimary B-cell non-Hodgkin lymphoma of the breast mimicking acute mastitis.J Clin Ultrasound 2005;33:140–2.Table 2Ultrasonographic findings of primary breast lymphomas (n =8)Ultrasonographic finding Sample distribution [n (%)]Shape Oval 4(50)Round 1(12.5)Irregular 3(37.5)Orientation Parallel 8(100)Not parallel 0(0)MarginCircumscribed 4(50)Indistinct 1(12.5)Angular0(0)Microlobulated 3(37.5)Spiculated 0(0)Echo pattern Anechoic 0(0)Hyperechoic 1(12.5)Complex 0(0)Hypoechoic 7(87.5)Isoechoic0(0)Posterior acoustic feature No posterior acoustic feature 2(25)Enhancement 6(75)Shadowing 0(0)Combined 0(0)Calcifications Present 0(0)Absent8(100)C.Y.Lyou et al./Clinical Imaging 31(2007)234–238238。