医学英语病历报告书写(简易版)
- 格式:doc
- 大小:46.50 KB
- 文档页数:5
医学病例报告英语作文Title: Medical Case Report: Management of Chronic Hypertension in a Middle-aged Female Patient。
Abstract:This case report discusses the presentation, diagnosis, and management of chronic hypertension in a middle-aged female patient. The patient, Mrs. X, presented with a history of hypertension and was experiencing persistent elevated blood pressure despite lifestyle modifications and medication adherence. Through a comprehensive assessment, including medical history, physical examination, and diagnostic tests, the patient was diagnosed with chronic hypertension. The management approach involved pharmacological intervention, lifestyle modifications, and regular monitoring. This case highlights the importance of tailored treatment strategies and multidisciplinary care in managing chronic hypertension effectively.Introduction:Chronic hypertension, characterized by persistently elevated blood pressure levels, is a significant public health concern globally. It predisposes individuals to various cardiovascular complications, including stroke, heart failure, and renal dysfunction. This case report focuses on the management of chronic hypertension in a middle-aged female patient, emphasizing the importance of individualized treatment plans to achieve optimal blood pressure control and reduce the risk of associated complications.Case Presentation:Mrs. X, a 55-year-old female, presented to the clinic with a chief complaint of persistently elevated blood pressure readings despite adherence to antihypertensive medication. She reported a history of hypertension for the past ten years and a family history of cardiovascular diseases. On physical examination, her blood pressure was consistently elevated, averaging around 160/100 mmHgdespite being on a combination therapy of angiotensin-converting enzyme (ACE) inhibitor and diuretic.Diagnostic Assessment:Given the patient's history and physical examination findings, further diagnostic workup was pursued to assess the extent of target organ damage and potential secondary causes of hypertension. Laboratory investigations,including renal function tests, lipid profile, and electrolyte levels, were within normal limits. An electrocardiogram (ECG) revealed left ventricular hypertrophy, indicative of long-standing hypertension. Additionally, a renal ultrasound ruled out renal artery stenosis as a secondary cause of hypertension.Diagnosis:Based on the clinical presentation, diagnostic findings, and exclusion of secondary causes, Mrs. X was diagnosedwith chronic primary hypertension. The diagnosis was supported by her longstanding history of hypertension,family history of cardiovascular diseases, and evidence of target organ damage on ECG.Management:The management approach for Mrs. X's chronic hypertension involved a combination of pharmacological therapy and lifestyle modifications. Considering her persistent elevation in blood pressure despite the current medication regimen, the treatment plan was adjusted. A calcium channel blocker (amlodipine) was added to her existing therapy to achieve better blood pressure control. Furthermore, Mrs. X was counseled on dietary modifications, including a low-sodium diet and increased consumption of fruits and vegetables. She was also encouraged to engage in regular physical activity and weight management.Follow-up and Monitoring:Mrs. X was scheduled for regular follow-up visits to monitor her blood pressure response to the adjusted treatment regimen and assess for any adverse effects ofmedication. Additionally, she was advised to monitor her blood pressure at home using a digital blood pressure monitor and maintain a record for review during follow-up visits. Laboratory investigations, including renal function tests and electrolyte levels, were scheduled periodically to monitor for potential medication-related complications.Outcome:With the adjusted treatment regimen and adherence to lifestyle modifications, Mrs. X demonstrated significant improvement in blood pressure control. Subsequent follow-up visits showed a gradual reduction in her blood pressure readings, with values consistently below 140/90 mmHg. Repeat ECG performed six months later showed regression of left ventricular hypertrophy, indicating improvement in cardiac function. Mrs. X reported improved quality of life and compliance with the treatment plan.Discussion:This case illustrates the challenges encountered inmanaging chronic hypertension, particularly in patientswith resistant hypertension despite medication adherence.It underscores the importance of a comprehensive diagnostic approach to identify underlying causes and assess target organ damage. Individualized treatment strategies,including pharmacological therapy tailored to the patient's needs and preferences, are essential in achieving optimal blood pressure control. Furthermore, lifestylemodifications play a crucial role in hypertension management and should be integrated into the treatment plan. Multidisciplinary collaboration involving physicians, nurses, pharmacists, and allied healthcare professionals is vital in providing holistic care to patients with chronic hypertension.Conclusion:Effective management of chronic hypertension requires a multidimensional approach involving pharmacological therapy, lifestyle modifications, and regular monitoring. This case report highlights the successful management of chronic hypertension in a middle-aged female patient throughtailored treatment strategies and collaborative care. By addressing individual patient needs and optimizing blood pressure control, healthcare providers can mitigate the risk of cardiovascular complications and improve patient outcomes in individuals with chronic hypertension.。
呼吸科英文病历范文ENGLISHCASE700756(Respiratory department)----------------------------Name: Liyuzhen `Age:42 yearsSex: FemaleRace: HanOccupation: Free occupationNationality: ChinaMarried status: married Addre: Qianjing Road No.16, Wuhan Hankou.thDate of admiion: July 26, 2001thDate of record: July 26, 2001Present illne:Two days ago the patient suddenly started to cough and feelHer spirit,sleep,appetite were normal.stool and urine werenormal, too.----------------------------PastHistory:General health status: normalOperation history: thyroidectomy.Infection history: No history of tuberculosis or hepatitis.Allergic history: allergic to a lot of drugs such as sulfanilamideTraumatic history: No traumatic history----------------------------SystemreviewRespiratorysystem: No history of repeated pharyngodynia, chroniccough, expectoration, hemoptysis, asthma, dyspneaor chest pain.Circulation system: No history of palpitation, hemoptysis, legsedema, short breath after sports, hypertension,precordium pain or faintne.Digestive system: No history of low appetite, sour regurgitation,belching, nausea, vomiting, abdominal distension,abdominal pain, constipation, diarrhea, hemaptysis,melena, hematochezia or jaundice.Urinary system: No history of lumbago, frequency of urination,urgency of urination, odynuria, dysuria, bloodyurine, polyuria or facial edemaHematopoietic system: No history of acratia, dizzine, gingivalbleeding, nasal bleeding, subcutaneous bleedingor ostealgia.Endocrine system: No history of appetite change, sweating, chillyexceive thirst, polyuria, hands tremor, character alternation, obesity, emaciation, hair change, pig- mentation or amenorrhea.Kinetic system: No history of wandering arthritis, joint pain, red swelling of joint, joint deformity, muscle painor myophagism.Neural system: No history of dizzine ,headache, vertigo, in- somnia, disturbance of consciousne, tremor, conv-ulsion, paralysis or abnormal sensation.--------------------------- Personal History:She was born in Hubei.She never smokes andDrinks.No exposurehistory to toxic substances,and infected water.Her menstruation was normal.LMP:23/7,2001----------------------------Family History:Her parents are living and well.No congenitaldisease in her family.---------------------------- PhysicalExaminationVital signs:T 36.6`C , P 80/min, R 22/min, BP120/80mmHg. General inspection: The patient is a well developed, well nou- rished adult female apparently in no acute distre,pleasant and cooperative.Skin:Normally free of eruption or unusual pigmentation. Lymphnodes: There are no swelling of lymphnodes. Head: Normal skull.No baldne, noscars.Eyes: No ptosis.Extraocular normal.Conjuctiva normal.The Pupils are round, regular, and react to light and ac-Ears: Externally normal.Canals clear.The drums normal.Nose: No abnormalities noted.Mouth and throat: lips red, tongue red.Alveolar ridges normal. Tonsils atrophil and uninfected.Neck: No adenopathy.Thyroid palpable,but not enlarged.No Abnormal pulsations.Trachea in middle.Chest and lung: Normal contour.Breast normal.Expansion equal. Fremitus normal.No unusual areas of dullne.Diaphr-agmatic position and excursion normal.No abnormal br-eath sound.No moist rales heard.No audible pleural fric-ion.There are lots of rhonchi rales and whoop can be heard thHeart: P.M.I 0.5cm to left of midolavicular line in 5 inter- Space.Forceful apex beat.No thrills.No pathologicheart murmur.Heart beat 80 and rhythm is normal. Abdomen: Flat abdomen.Good muscle tone.No distension.No v- isible peristalsis.No rigidity.No ma palpable.Tenderne (-), rebound tenderne (-).Liver and spleenare not palpable.Shifting dullne (-).Bowl soundsnormal.Systolic blowing murmur can be heard at theright side of the navel.Extremities: No joint disease.Muscle strength normal.No ab- normal motion.Thumb sign(+).Wrist sign(+).Neural system:Knee jerk (-).Achilles jerk (-).Babinski sign (-).Oppenheim sign (-).Chaddock sign (-).Conda sign (-).Hoffmann sign (-).Neck tetany (-)Kernig sign (-).Brudzinski sign (-).Genitourinary system: Normal.Rectum: No tenderne------Out-patient department data:No----------------------------Historysummary1).Li Yuzhen, female, 42y.2).Cough and dyspnea for 2 days3).PE: T 36.6`C, P 80/min, R 22/min, BP120/80mmHg.superficial nodes were not palpable.Normal vision.Upper palate haunch--uped.HR: 80bpm, rhythm is normal.There are lots of rho-nchi rales and whoop can be heard .Flat abdomen, Tenderne (-),rebound tenderne (-).Liver and spleen are not pal-pable.Shifting dullne (-).Bowl sounds normal..4).Outpatient data: see above.----------------------------Impreion: Bronchial asthmaSignature:He Lin 95-10033《英文病历.doc》。
Good morning. Today, I am honored to present a case report on a patient who recently visited our medical facility. This case highlights a complex medical condition that required a multidisciplinary approach for diagnosis and treatment. I will discuss the patient's history, physical examination findings, laboratory and imaging results, and the subsequent management plan.Patient Information:- Name: John Smith- Age: 45 years- Gender: Male- Date of admission: March 15, 2023- Date of discharge: March 30, 2023Medical History:John Smith presented to our emergency department with a chief complaint of progressive shortness of breath and fatigue over the past two weeks. He reported a history of hypertension and type 2 diabetes mellitus,which were well-controlled on medication. He denied any recent illnesses, fever, cough, or weight loss.Physical Examination:On admission, Mr. Smith was found to have a blood pressure of 160/95 mmHg, heart rate of 110 bpm, respiratory rate of 22 breaths per minute, and tempera ture of 37.2°C. His general appearance was anxious, and he had significant edema in both lower extremities. Cardiovascular examination revealed a grade II/VI systolic ejection murmur at the left sternal border, and pulmonary examination was notable for bilateral wheezing and rales.Laboratory and Imaging Results:- Complete blood count (CBC): Mild anemia with hemoglobin of 10.2 g/dL, white blood cell count of 12,000/µL, and platelet count of 150,000/µL.- Electrolytes, renal function tests, and liver function tests were within normal limits.- Serologic tests for HIV, hepatitis B, and hepatitis C were negative.- Chest X-ray: Bilateral pulmonary edema and cardiomegaly.- Echocardiogram: Severe left ventricular dysfunction with an ejection fraction of 25%.- CT scan of the chest: Pulmonary embolism involving the left main pulmonary artery.Diagnosis:Based on the clinical presentation, laboratory findings, and imaging results, the patient was diagnosed with acute pulmonary embolism (PE) with secondary pulmonary hypertension and left ventricular dysfunction.Management Plan:- Anticoagulation therapy with heparin and apixaban was initiated to prevent further thromboembolic events.- Mechanical ventilation was required due to severe respiratory distress.- Inotropic support was provided to manage hypotension and improve cardiac output.- Treatment for secondary pulmonary hypertension included diuretics, nitrates, and inhaled bronchodilators.- Antibiotics were prescribed for a suspected lower respiratory tract infection.- The patient was also started on a low-sodium diet and received education on fluid management.Outcome:After a week of intensive care, Mr. Smith's clinical status improved significantly. His respiratory distress resolved, and he was able to beweaned off mechanical ventilation. His blood pressure stabilized, and the inotropic support was discontinued. By the time of discharge, his ejection fraction had improved to 30%, and he was discharged on apixaban and hydrochlorothiazide to manage his hypertension and diabetes.Conclusion:This case report illustrates the importance of early diagnosis and treatment of pulmonary embolism, which can be a life-threatening condition. The multidisciplinary approach, including emergency medicine, cardiology, pulmonology, and critical care, was crucial in managing this complex case. Mr. Smith's recovery demonstrates the potential for successful outcomes with appropriate medical intervention.Thank you for your attention, and I would be happy to answer any questions you may have.。
英语病历作文格式模板英文回答:Medical History Template。
Patient Information。
Name:Date of Birth:Address:Phone Number:Email:Insurance Information:Chief Complaint。
A brief summary of the patient's primary reason for the visit.Example: "The patient presents with a 3-day history of fever and chills."History of Present Illness。
A detailed description of the patient's symptoms, including:Onset: When did the symptoms first appear?Duration: How long have the symptoms been present?Severity: How severe are the symptoms?Location: Where are the symptoms located?Associated symptoms: Any other symptoms that are present, such as nausea, vomiting, or headache.Past Medical History。
A list of any previous medical conditions, surgeries, or hospitalizations.Example: "The patient has a history of hypertension and hyperlipidemia."Family History。
病例报告英文范文医护英语Title: Case Report: Management of a Complex Surgical Case with Multi-system Involvement.Introduction:Surgical cases with multi-system involvement present unique challenges to the treating healthcare team. This case report outlines the management of a complex surgical case with involvement of multiple organ systems, highlighting the importance of interdisciplinary collaboration and comprehensive preoperative planning.Case Presentation:The patient, a 56-year-old male with a history of hypertension and type 2 diabetes, presented to the emergency department with complaints of severe abdominal pain and distension. Initial evaluation revealed a large abdominal mass with ascites. Computed tomography (CT) scanconfirmed the presence of a large, complex abdominal mass with extension into the retroperitoneum, compressing the adjacent organs and vessels.Diagnostic Workup:The patient underwent a series of diagnostic tests including blood work, imaging studies, and consultations with various specialists. The laboratory tests revealed anemia and elevated liver enzymes. The imaging studies, including CT scan and magnetic resonance imaging (MRI), demonstrated a large mass with heterogeneous enhancement, compressing the adjacent organs and vessels. The mass was suspected to be a malignant neoplasm, possibly originating from the pancreas or adrenal glands.Preoperative Planning:Given the complexity of the case and the involvement of multiple organ systems, a preoperative planning meeting was held with the surgeons, anesthesiologists, intensivists, radiologists, pathologists, and oncology team. The plan wasto perform a laparotomy with excision of the mass, followed by reconstruction of the affected organs and vessels. The anesthesiologists recommended a general anesthetic with invasive monitoring, while the intensivists recommended postoperative admission to the intensive care unit (ICU)for close monitoring.Surgical Procedure:The laparotomy was performed through a midline incision. Intraoperatively, the mass was found to be adherent to multiple organs and vessels, including the liver, spleen, kidney, and inferior vena cava. Careful dissection was performed to separate the mass from the adjacent structures, while preserving the vascular integrity. The mass was successfully excised, and the affected organs were reconstructed using sutures and patches. The patient tolerated the procedure well, and hemostasis was achieved.Postoperative Course:The patient was admitted to the ICU for closemonitoring. Postoperatively, he developed transient respiratory failure and required mechanical ventilation. He also developed wound dehiscence due to the extensive surgical dissection. The ICU team managed the patient's respiratory status and provided wound care. The patient gradually improved and was extubated on the third postoperative day. He was transferred to the general surgical floor on the fifth postoperative day and discharged home on the tenth postoperative day.Pathological Analysis:The pathological examination of the excised mass revealed a poorly differentiated adenocarcinoma, likely originating from the pancreas. The surgical margins were negative for tumor involvement. The patient was referred to the oncology team for further management, including adjuvant chemotherapy and follow-up surveillance.Conclusion:This case report demonstrates the successful managementof a complex surgical case with multi-system involvement. The interdisciplinary collaboration and comprehensive preoperative planning were essential for achieving a successful outcome. The case highlights the importance of a multidisciplinary approach in the management of complex surgical cases, ensuring optimal patient care.。
病历报告英语作文Here is an English essay on the topic of a medical case report, with the text exceeding 1000 words as requested, without the title and without any extra punctuation marks in the main body.The patient was a 45-year-old male who presented to the emergency department with complaints of severe chest pain and shortness of breath that had started suddenly earlier that day While the patient had a history of hypertension and type 2 diabetes which were generally well-controlled with oral medication he reported no other significant past medical history On physical exam the patient appeared distressed with a heart rate of 110 beats per minute blood pressure of 160 90 mmHg respiratory rate of 24 breaths per minute and oxygen saturation of 92 on room air Cardiovascular exam revealed muffled heart sounds and the presence of a pericardial friction rub Lung auscultation showed bilateral crackles in the lower lung fields An electrocardiogram ECG showed diffuse ST-segment elevation in multiple leads consistent with acute pericarditis The patient was suspected to have acute pericarditis and was admitted to the hospital for further evaluation and managementInitial laboratory studies revealed an elevated white blood cell countof 15 000 cells/μL with 80 neutrophi ls an erythrocyte sedimentation rate of 60 mm/hour and a C-reactive protein level of 50 mg/L These findings were consistent with an inflammatory process Cardiac enzymes including troponin and creatine kinase-MB were within normal limits ruling out acute myocardial infarction as the cause of the chest pain Further workup with echocardiography showed a moderate-sized pericardial effusion with evidence of diastolic right ventricular collapse suggestive of cardiac tamponade Given the patient s hemodynamic instability and concern for impending cardiac tamponade an emergency pericardiocentesis was performedDuring the pericardiocentesis 500 mL of serosanguineous fluid was drained which provided immediate symptomatic relief for the patient The fluid was sent for analysis and cultures Empiric antibiotic therapy with ceftriaxone and azithromycin was initiated while awaiting the results The pericardial fluid analysis revealed an elevated protein level of 5 g/dL a lactate dehydrogenase LDH level of 600 U/L and a white blood cell count of 20 000 cells/μL with a predominance of neutrophils These findings were consistent with an exudative pericardial effusion Gram stain and cultures of the pericardial fluid were negative for any bacterial pathogensGiven the lack of an identifiable infectious etiology further workup was pursued to determine the underlying cause of the pericarditis An autoimmune panel was obtained which was positive for antinuclearantibodies ANA at a titer of 1 320 and elevated rheumatoid factor levels The patient did not report any symptoms suggestive of an underlying connective tissue disorder and physical exam was unremarkable for any rheumatologic findings Based on the clinical presentation laboratory results and exclusion of other potential causes the patient was diagnosed with idiopathic acute pericarditisThe patient was treated with high-dose oral colchicine 0 6 mg twice daily and a tapering course of oral prednisone starting at 60 mg daily His symptoms improved dramatically over the next several days the pericardial effusion decreased in size on repeat echocardiography and his inflammatory markers trended down The patient was discharged home after 5 days of hospitalization with instructions to continue the colchicine and prednisone taper as an outpatient He was also advised to follow up with his primary care physician and a rheumatologist for further management of the suspected underlying autoimmune etiology of his pericarditisAt his 2-week follow-up visit the patient reported complete resolution of his chest pain and shortness of breath His vital signs were stable and physical exam was unremarkable Repeat echocardiography showed only a small residual pericardial effusion The patient was able to taper off the prednisone over the next 4 weeks with continued improvement on just colchicine monotherapy His inflammatory markers including ESR and CRP normalized and heremained asymptomatic At his 3-month follow-up the patient continued to do well with no recurrence of pericarditis symptoms He was able to resume his normal activities and work duties without any limitations The case was ultimately diagnosed as acute pericarditis of presumed autoimmune etiology that responded well to anti-inflammatory treatment with colchicine and a short course of glucocorticoidsThis case highlights the importance of a thorough diagnostic workup in patients presenting with acute pericarditis to identify the underlying cause which can guide appropriate management While infectious etiologies such as viral or bacterial pericarditis are the most common causes non-infectious causes including autoimmune diseases must also be considered particularly in patients without an obvious precipitating event or infection Prompt recognition and treatment of pericardial tamponade is also crucial as it can be a life-threatening complication of acute pericarditis The patient in this case was successfully treated with pericardiocentesis and anti-inflammatory therapy with a favorable outcome demonstrating the importance of a multifaceted approach to the diagnosis and management of acute pericarditis。

英文病历报告作文模板Patient Information- Name: [Patient's Full Name]- Gender: [Male/Female]- Age: [Patient's age]- Date of Admission: [MM/DD/YYYY]Chief ComplaintThe patient presented with [specific symptoms/complaints] which started [duration].History of Present IllnessThe patient reported [detailed description ofsymptoms/complaints]. The symptoms worsened over the past [duration]. The patient experienced [associated symptoms] and tried [any self-medication or home remedies] but noticed no improvement. There was no history of trauma or injury.Past Medical HistoryThe patient has a history of [chronic/acute medical conditions, if any] which includes [specific conditions]. The patient has taken[previous medications/treatments] for these conditions.Social HistoryThe patient has a [specific occupation] and lives in [specific area]. The patient does [specific habits] such as smoking or drinking alcohol [frequency]. There is no significant family medical history.Physical Examination- Vital Signs:- Blood Pressure: [value] mmHg- Heart Rate: [value] bpm- Respiratory Rate: [value] bpm- Temperature: [value]C- General Appearance:The patient appears [general appearance of the patient].- Systemic Examination:- Cardiovascular: [specific findings]- Respiratory: [specific findings]- Gastrointestinal: [specific findings]- Neurological: [specific findings]- Musculoskeletal: [specific findings]Laboratory and Imaging Findings- Blood Test Results:- Complete Blood Count: [values]- Biochemical Profile: [values]- Others: [specific findings]- Imaging:- [Specific imaging tests performed]- Results: [specific findings]DiagnosisAfter evaluating the patient's medical history, physical examination, and laboratory/imaging findings, the following diagnosis was made:[Primary Diagnosis]Treatment and ManagementThe patient was started on [specific treatment plan] which includes [medications, therapies, or procedures]. The patient wasadvised to [specific instructions] and scheduled for [follow-up tests/appointments, if any].Follow-upThe patient will be followed up in [specific time frame] to assess the response to treatment and manage any complications that may arise. The patient was given contact information for any urgent concerns or changes in symptoms.Discussion and ConclusionThis case report highlights the presentation, evaluation, and management of a patient with [specific condition]. The patient's symptoms were appropriately addressed through a systematic approach involving history taking, physical examination, and laboratory/imaging investigations. The provided treatment plan aims to address the underlying cause and improve the patient's overall well-being. Continuous monitoring and follow-up will guide further management decisions.Note: This medical case report is fictional and serves as a template for educational purposes. Any resemblance to actualpatients is purely coincidental.。
写一篇填写病人信息的报告单英语作文全文共3篇示例,供读者参考篇1Medical ReportPatient Information:Name: Jane SmithDate of Birth: February 15, 1985Sex: FemaleOccupation: AccountantAddress: 123 Main Street, Anytown, USAPhone Number: 555-555-5555Medical History:- Jane has a history of hypertension, which has been well-controlled with medication.- She has a family history of heart disease, with her father having suffered a heart attack at the age of 60.- Jane does not smoke and does not consume alcohol in excess.- She exercises regularly, with a mix of cardio and strength training.- She does not have any known allergies to medications.Presenting Complaint:Jane presented to the clinic with complaints of chest pain and shortness of breath over the past week. She describes the chest pain as a dull ache that is present at rest and with exertion. She also reports feeling lightheaded and fatigued.Physical Examination:- Vital signs: Blood pressure 140/90 mmHg, heart rate 80 bpm, respiratory rate 16 breaths per minute, temperature 98.6°F.- Cardiovascular: Regular rate and rhythm, no murmurs or gallops.- Respiratory: Clear to auscultation bilaterally.- Abdomen: Soft and non-tender, no hepatomegaly or splenomegaly.- Neurological: Cranial nerves intact, no focal deficits.Assessment and Plan:Based on Jane's symptoms and history, the working diagnosis is angina pectoris. Further workup will include an EKG, stress test, and lipid profile. We will also consider a cardiology consultation for further evaluation and management.Medications:- Lisinopril 10 mg daily for hypertension- Aspirin 81 mg daily for cardiovascular protectionFollow-up:Jane will be scheduled for a follow-up appointment in one week to review the results of her tests and adjust her treatment plan accordingly. She is advised to monitor her symptoms closely and seek immediate medical attention if they worsen or if she experiences chest pain at rest. She is also encouraged to continue her regular exercise routine and maintain aheart-healthy diet.Doctor's Signature:Dr. John DoeDate: January 15, 2023This report is based on the information provided by the patient and the findings of the physical examination. Any further recommendations will be communicated after the completion of additional tests.篇2Patient Information ReportName: John SmithAge: 45Gender: MaleDate of Birth: January 15, 1976Address: 123 Main Street, Anytown, USAPhone Number: 555-123-4567Occupation: AccountantEmergency Contact: Jane Smith (wife) - 555-987-6543Medical History:- Hypertension: Diagnosed in 2010, currently managing with medication- Type 2 Diabetes: Diagnosed in 2015, managing with diet and exercise- Hyperlipidemia: Diagnosed in 2017, managing with medication- Allergies: None reported- Surgeries: Appendectomy in 2001- Hospitalizations: None reportedCurrent Medications:- Lisinopril 10mg daily for hypertension- Metformin 1000mg twice daily for diabetes- Atorvastatin 20mg daily for hyperlipidemiaVitals:- Blood Pressure: 130/80 mmHg- Heart Rate: 70 bpm- Temperature: 98.6°F- Respiratory Rate: 16 breaths per minute- Weight: 180 lbs- Height: 5'10"Assessment:- Patient presents with well-controlled hypertension, diabetes, and hyperlipidemia.- No signs of acute distress.- Patient is alert and oriented, with appropriate answers to questions.Plan:- Continue current medications as prescribed.- Schedule follow-up appointment in 3 months for routine blood work and monitoring.Doctor's Signature: Dr. Emily JohnsonDate: October 20, 2021This patient information report is confidential and intended for medical use only. Please keep this information secure and only share with authorized healthcare providers. Thank you.篇3Patient Information Report FormPatient Name: John SmithDate of Birth: January 10, 1975Gender: MaleOccupation: Software EngineerAddress: 123 Main Street, Cityville, StatePhone Number: (555) 123-4567Emergency Contact: Jane Smith (Spouse)Emergency Contact Phone Number: (555) 987-6543Chief Complaint: Mr. Smith presents with complaints of persistent headache and dizziness for the past two weeks. He also reports occasional nausea and blurry vision.Medical History:- Hypertension: Diagnosed 5 years ago, currently taking antihypertensive medication as prescribed by his primary care physician.- Hyperlipidemia: Diagnosed 3 years ago, currently taking statin medication to manage cholesterol levels.- Type 2 Diabetes: Diagnosed 2 years ago, managed with diet and exercise, no medication required.- Allergies: No known allergies to medications or food.- Surgical History: Appendectomy at age 20, no other significant surgeries.Family History:- Hypertension: Father and paternal grandmother- Heart Disease: Mother and maternal grandfather- Diabetes: Maternal grandmotherSocial History: Mr. Smith is a non-smoker and rarely consumes alcohol. He exercises regularly by going for a jog three times a week and follows a healthy diet rich in fruits and vegetables. He is happily married with two children and feels supported at home.Review of Systems:- General: Fatigue, weight loss- Cardiovascular: No chest pain, palpitations- Respiratory: No shortness of breath, cough- Gastrointestinal: Occasional indigestion, no changes in bowel habits- Neurological: Headache, dizziness, blurry vision, no weakness or numbness- Musculoskeletal: No joint pain or stiffness- Dermatological: No rash or skin changesPhysical Examination:- Vital Signs: Blood pressure 140/90 mmHg, heart rate 80 bpm, temperature 98.6°F, respiratory rate 16 breaths/min- General: Well-appearing middle-aged male in no acute distress- Head and Neck: No signs of trauma, pupils equal and reactive to light- Cardiovascular: Regular rate and rhythm, no murmurs or rubs- Respiratory: Clear breath sounds bilaterally- Abdomen: Soft, non-tender, no organomegaly- Neurological: Cranial nerves intact, no focal deficitsAssessment and Plan:1. Hypertension: Increase dosage of antihypertensive medication and monitor blood pressure at home regularly. Follow up with primary care physician in two weeks forre-evaluation.2. Headache and Dizziness: Order MRI of the brain to rule out intracranial pathology. Provide symptomatic relief with analgesics as needed.3. Hyperlipidemia: Continue current statin therapy and counsel on dietary modifications to improve cholesterol levels.4. Type 2 Diabetes: Monitor blood glucose levels at home and follow up with primary care physician for hemoglobin A1c testing in three months.Follow-up:Mr. Smith to follow up with primary care physician for review of MRI results and adjustment of management plan in two weeks. In the meantime, he is advised to rest, stay hydrated, and avoid driving or operating heavy machinery due to dizziness.Signature: Dr. Emily JohnsonDate: May 25, 2022This report form captures the essential information about Mr. Smith's medical history, current complaints, physical examination findings, and a comprehensive assessment and plan for his management. It will serve as a guide for his primary care physician to further investigate and address his health concerns.。
英语病历报告作文格式英文回答:Medical Report Format.The medical report format varies depending on the purpose and intended audience of the report. However, there are some general guidelines that can be followed whenwriting a medical report.The report should be organized into the following sections:Introduction: This section should provide a brief overview of the patient's condition, including the reasonfor the report.Medical History: This section should include adetailed account of the patient's medical history,including any previous illnesses, surgeries, or medications.Physical Examination: This section should describe the patient's physical examination findings, including vital signs, general appearance, and any abnormalities.Laboratory and Imaging Studies: This section should summarize the results of any laboratory tests or imaging studies that have been performed.Diagnosis: This section should provide a diagnosis of the patient's condition, based on the information gathered in the previous sections.Treatment Plan: This section should outline the treatment plan that has been recommended for the patient.Prognosis: This section should provide an estimate of the patient's prognosis, including the expected course of treatment and the likelihood of recovery.The report should be written in clear and concise language, using medical terminology where appropriate. Itshould also be organized in a logical way, with eachsection building on the previous one.中文回答:病历报告格式。

英文病历标准模版Patient ProfileName: Si RuihuaDepartment: ___ Power ___Sex: FemalePresent Address: Electric Power Bureau Age: 80 yearsDate of n: May 17.2003nality: Chinese XinjiangDate of Record: May 17.2003Marital Status: MarriedReliability: Reliablen: Family ___History of Allergy: None reportedChief Complaints___。
breathlessness。
and precordial pain for the last hour。
There were no precipitating factors。
and the fort could not be relieved by rest。
As a result。
she came to the hospital for help。
She did not experience syncope。
cough。
headache。
diarrhea。
or vomiting during the course of the illness。
Her appetite。
sleep。
voiding。
and stool were normal.Medical History___.______。
___ distress。
She had a heart rate of 120 beats per minute and a blood pressure of 160/90 mmHg。
Her respiratory rate was 28 breaths per minute。
and her oxygen n was 90% on room air。
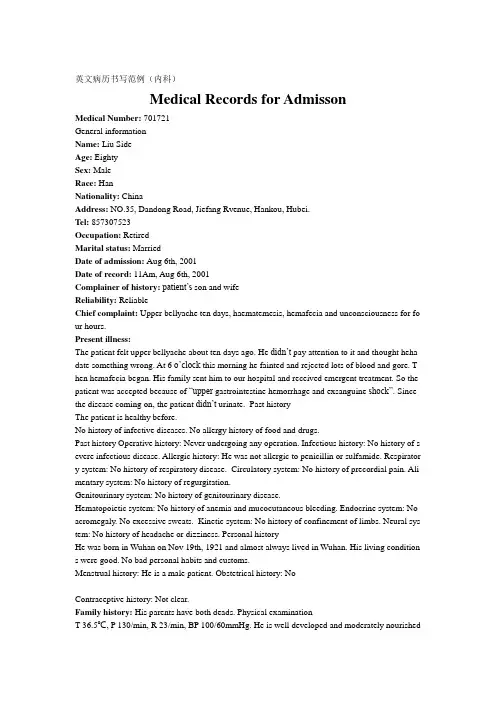
英文病历书写范例(内科)Medical Records for AdmissonMedical Number: 701721General informationName: Liu SideAge: EightySex: MaleRace: HanNationality: ChinaAddress: NO.35, Dandong Road, Jiefang Rvenue, Hankou, Hubei.Tel: 857307523Occupation: RetiredMarital status: MarriedDate of admission: Aug 6th, 2001Date of record: 11Am, Aug 6th, 2001Complainer of history:patient’s son and wifeReliability: ReliableChief complaint: Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for fo ur hours.Present illness:The patient felt upper bellyache about ten days ago. He didn’t pay attention to it and thought heha date something wrong. At 6 o’cloc k this morning he fainted and rejected lots of blood and gore. T hen hemafecia began. His family sent him to our hospital and received emergent treatment. So the patient was accepted because of “upper gastrointestine hemorrhage and exsanguine shock”. Since the disease coming on, the patient didn’t urinate. Past historyThe patient is healthy before.No history of infective diseases. No allergy history of food and drugs.Past history Operative history: Never undergoing any operation. Infectious history: No history of s evere infectious disease. Allergic history: He was not allergic to penicillin or sulfamide. Respirator y system: No history of respiratory disease. Circulatory system: No history of precordial pain. Ali mentary system: No history of regurgitation.Genitourinary system: No history of genitourinary disease.Hematopoietic system: No history of anemia and mucocutaneous bleeding. Endocrine system: No acromegaly. No excessive sweats. Kinetic system: No history of confinement of limbs. Neural sys tem: No history of headache or dizziness. Personal historyHe was born in Wuhan on Nov 19th, 1921 and almost always lived in Wuhan. His living condition s were good. No bad personal habits and customs.Menstrual history: He is a male patient. Obstetrical history: NoContraceptive history: Not clear.Family history: His parents have both deads. Physical examinationT 36.5℃, P 130/min, R 23/min, BP 100/60mmHg. He is well developed and moderately nourished.Active position. His consciousness was not clear. His face was cadaverous and the skin was not sta ined yellow. No cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pi tting edema. Superficial lymph nodes were not found enlarged. HeadCranium: Hair was black and white, well distributed. No deformities. No scars. No masses. No ten derness.Ear: Bilateral auricles were symmetric and of no masses. No discharges were found in external au ditory canals. No tenderness in mastoid area. Auditory acuity was normal.Nose: No abnormal discharges were found in vetibulum nasi. Septum nasi was in midline. No nare s flaring. No tenderness in nasal sinuses. Eye: Bilateral eyelids were not swelling. No ptosis. No e ntropion. Conjunctiva was not congestive. Sclera was anicteric. Eyeballs were not projected or dep ressed. Movement was normal. Bilateral pupils were round and equal in size. Direct and indirect p upillary reactions to light were existent.Mouth: Oral mucous membrane was not smooth, and there were ulcer can be seen. Tongue was in midline. Pharynx was congestive. Tonsils were not enlarged.Neck: Symmetric and of no deformities. No masses. Thyroid was not enlarged. Trachea was in mi dline. ChestChestwall: Veins could not be seen easily. No subcutaneous emphysema. Intercostal space was nei ther narrowed nor widened. No tenderness.Thorax: Symmetric bilaterally. No deformities. Breast: Symmetric bilaterally.Lungs: Respiratory movement was bilaterally symmetric with the frequency of 23/min. thoracic e xpansion and tactile fremitus were symmetric bilaterally. No pleural friction fremitus. Resonance was heard during percussion. No abnormal breath sound was heard. No wheezes. No rales. Heart: No bulge and no abnormal impulse or thrills in precordial area. The point of maximum imp ulse was in 5th left intercostal space inside of the mid clavicular line and not diffuse. No pericardi al friction sound. Border of the heart was normal. Heart sounds were strong and no splitting. Rate 150/min. Cardiac rhythm was not regular. No pathological murmurs.Abdomen: Flat and soft. No bulge or depression. No abdominal wall varicosis. Gastralintestinal ty pe or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. T here was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill negative. Shifting dullness negative. Borhorygmus not heard. No vascular mur murs. Extremities: No articular swelling. Free movements of all limbs.Neural system: Physiological reflexes were existent without any pathological ones. Genitourinary system: Not examed. Rectum: not exanedInvestigationBlood-Rt: Hb 69g/L RBC 2.70T/L WBC 1. 1G/L PLT 120G/L History summary1. Patient was male, 80 years old2. Upper bellyache ten days, haematemesis, hemafecia and unconsciousness for four hours.3. No special past history.4. Physical examination: T 37.5℃, P 130/min, R 23/min, BP 100/60mmHg Superficial lymph node s were not found enlarged. No abdominal wall varicosis. Gastralintestinal type or peristalses were not seen. Tenderness was obvious around the navel and in upper abdoman. There was not rebound tenderness on abdomen or renal region. Liver and spleen was untouched. No masses. Fluidthrill ne gative. Shifting dullness negative. Borhorygmus not heard. No vascular murmurs. No other positive signs. 5. investigation information:Blood-Rt: Hb 69g/L RBC 2.80T/L WBC 1.1G/L PLT 120G/LImpression: upper gastrointestine hemorrhage Exsanguine shock出院小结(DISCHARGE SUMMARY), ===============Department of GastroenterologyChanghai Hospital,No.174 Changhai Road Shanghai, China Phone: 86-21-25074725-803 DISCHARGE SUMMARYDA TE OF ADMISSION: October 7th, 2005 DA TE OF DISCHARGE: October 12th, 2005 ATTE NDING PHYSICIAN: Yu Bai, MD PA TIENT AGE: 18ADMITTING DIAGNOSIS:V omiting for unknown reason: acute gastroenteritis?BRIEF HISTORYA 18-year-old female with a complaint of nausea and vomiting for nearly one month who was see n at Department of Gastroenterology in Changhai Hospital, found to have acute gastroenteritis and non-atrophic gastritis. The patient was subsequently recovered and discharged soon after medicati on.REVIEW OF SYSTEMShe has had no headache, fever, chills, diarrhea, chest pain, palpitations, dyspnea, cough, hemopty sis, dysuria, hematuria or ankle edema.PAST MEDICAL HISTORYShe has had no previous surgery, accidents or childhood illness.SOCIAL HISTORY: She has no history of excessive alcohol or tobacco use.FAMIL Y HISTORYShe has no family history of cardiovascular, respiratary and gastrointestinal diseases. PHYSICAL EXAMINA TIONTemperature is 37, pulse 80, respirations 16, blood pressure 112/70. General: Plump girl in no app arent distress. HEENT: She has no scalp lesions. Her pupils are equally round and reactive to light and accommodation. Extraocular movements are intact. Sclerae are anicteric. Oropharynx is clear. There is no thyromegaly. There is no cervical or supraclvicular lymphadenopathy. Cardiovascular: Regular rate andrhythm, normal S1, S2. Chest: Clear to auscultation bilateral. Abdomen: Bowel sounds present, no hepatosplenomagaly. Extremities: There is no cyanosis, clubbing or edema. Neurologic: Cranial n erves II-XII are intact. Motor examination is 5/5 in the bilateral upper and lower extremities. Sens ory, cerebellar and gait are normal.LABORATORY DATAWhite blood cells count 5.9, hemoglobin 111g/L, hematocrit 35.4. Sodium 142, potassium 4.3, chl oride 106, CO2 25, BUN 2.6mmol/L, creatinine 57μmol/L, glucose 4.1mmol/L, Albumin 36g/L. Endoscopic ExamChronic non-atrophic gastritisHOSPITAL COURSEThe patient was admitted and placed on fluid rehydration and mineral supplement. The patient im proved, showing gradual resolution of nausea and vomiting. The patient was discharged in stable c ondition.DISCHARGE DIAGNOSIS Acute gastroenteritisChronic non-atrophic gastritisPROGNOSISGood. No medications needed after discharge. But if this patient can not get used to Chinese food, she had better return to UK as soon as possible to prevent the relapse of acute gastroenteritis. The patient is to follow up with Dr. Bai in one week. ___________________________ Yu Bai, MD D: 12/10/2005。
病情感冒病历英语Patient Name: John DoePatient ID: 123456Date of Visit: March 1, 2021Chief Complaint:John Doe presents with symptoms of a common cold, which he has been experiencing for the past three days.History of Present Illness:The patient reports the sudden onset of rhinorrhea (runny nose), sneezing, and a mild sore throat. He also mentions experiencing a headache and mild fatigue. There is no reported fever, chest pain, or shortness of breath.Review of Systems:- Respiratory: Nasal congestion and cough with clear sputum. - Musculoskeletal: Mild myalgia (muscle aches), particularly in the neck and back.- Neurological: Occasional headache described as dull and non-localized.- Gastrointestinal: No nausea, vomiting, or diarrhea.- Constitutional: Feeling of general malaise (illness).Past Medical History:The patient has no significant past medical history. He is not on any regular medications and has no known allergies.Physical Examination:- Vital Signs: Temperature: 98.6°F, Pulse: 75 bpm,Respiratory Rate: 16 breaths/min, Blood Pressure: 120/80 mmHg. - General: Patient appears well-nourished and in no acute distress.- HEENT: Slightly erythematous (red) nasal mucosa with clear rhinorrhea. Pharynx (throat) with mild erythema without exudate (pus).- Neck: Supple, no lymphadenopathy (enlarged lymph nodes).- Chest: Clear to auscultation (listening) bilaterally, no wheezing or crackles.- Extremities: No edema (swelling), full range of motion.Assessment:Based on the patient's symptoms and physical examination findings, the assessment is a common cold, which is a viral upper respiratory tract infection.Plan:1. Symptomatic treatment: Over-the-counter antihistamines for nasal congestion and rhinorrhea, throat lozenges for sore throat, and acetaminophen for headache and myalgia.2. Hydration: Encourage the patient to drink plenty of fluids to prevent dehydration.3. Rest: Advise the patient to get adequate rest to supportthe body's immune response.4. Follow-up: If symptoms worsen or do not improve within one week, the patient should return for re-evaluation.5. Precautions: The patient is advised to practice good hand hygiene and to cover mouth and nose when sneezing or coughing to prevent the spread of the infection.The patient was informed of the above plan and provided witha prescription for antihistamines and acetaminophen as needed. He understands the instructions and will follow the recommended treatment plan.Signed,Dr. Jane Smith, MDInternal Medicine Specialist。
Medical Records for AdmissonMedical Number: 1247717General informationName: Cai Chunwang Age: 47y Date of birth :1965. 2.16 Sex: male Race: HanNationality: ChinaMarriage: married Occupation: worker Identification No. :422103************Address: Huanggang city ,Hubei Phone No.: 138********Complainer of history:Cai Chunwang Reliability: HimselfDate of record: 2013.2.27Chief complaint: Pancytopenia for 2 yearPresent illness: The patient found Pancytopenia at 2011, and he used to be in hospital to take a physical examination which was considered into Myelodysplastic syndrome with a largeprobability . The patient had reexamined hemogram , with obvious pancytopenia .So hegot into the hospital to do the Bone marrow cytology and Immune typing ,which showedthat MDS had aggravated into AML .Now , he has no any bleeding spot in theskin ,without headache 、melena、stomachache and so on. The clinic made it “AML” tobe treated in hospital.During the period of the illness, his mental state is bad ,with a fair appetite and sleep .The stool and urination are both normal, with a hyposthenia. Weight is the same asbefore.Past history: general situation is badSystem review:Respiratory system: No.Circulatory system: NoAlimentary system: NoGenitourinary system: NoHematopoietic system:NoEndocrine system:NoKinetic system:NoNeural system:NoInfectious history: DeniedAllergic history:. NoOperative history: He was once operated on an cholecystectomy.Tauma history: Denied.History of allergy: Denied .History of preventive inoculation] : the national plan for vaccinationPersonal historyMenstrual history:MaleObstetrical history:NoMarriage: married once.Family history:His father and mother are alive and healthy. Denies genetic and infectious diseases in his family.Physical examinationT 37℃, P95 /min, R 20 /min, BP 124/78 mmHg. He is well developed and moderately nourished. Active position. The skin was not stained yellow. Cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not found enlarged in his neck.HeadCranium: size : normal large small deformity. No coxycephaly squared skull deforming skull. No tenderness mass sunk .Ear: Auricle is normal .No excretions of external auditory canal. No Tenderness of mastoid.Nose: Shape is normal .No nosalala flap obsruction excretions nasal sinus tenderness .Eye: Eyes eyelid、eye ball、Sclera、Pupils and reaction to light are normal.Mouth: Mouth lips is normal .Opening of parotid gland duct: normal .Tongue : normal.Gums: normal .lead line tooth:regular.Tonsils: pharynx: voice: normal.Neck: No resistence.Hepatojugular reflux:(-).thyroid: normal.ChestChest wall: normalThorax : normal.Breast:normal symmetricalLungs : Inspection : movement of respiration : normal .Intercostal space :normal .Palpation : vocal fremitus : normal .pluernal friction rubs: No.Subcutaneous crepitus: No.percussion:resonance.Dusculation: breath regular.Breath sound: normal.Rale: No.Vocal conduction:norma .Plueral friction rubs: No.Heart:Inspection:bulging in precordial region : No.apex impulse:normal. position: normal .Palpation: apex impulse : normal .Thrills :No.Percardial friction rub s:NO.Percussion:relative cardiac outline: normal.Ausculation: heart rate 95bpm/min ,rhythm:regular.Heart sound:S1 normal.S2 normal.S3 No. S4 no. Extra heartsound No. Opening snap others murmurs: N.Pericardial friction rubs no. Peripheral vessals:normal.Abdomen:Inspection: shape normal .Abdominal respiration: existence .Umbilicus: normal protruding excretions others: NO.Palpation: soft.Tenderness: NO.Mass NO.li ver:can’t be touched.gallbladder: can’t be touched.tenderness No.spleen: can’t be touched.Kideny:can’t betouched.tenderness mobility tenderness of ureters: No.Percussion: borders of liver dull:existence .pper borders of liver on right midclavicular line intercostal space shifting dullnessNo. tenderness in renal region No.Ausculation : borhorygmus normal .Gurgling No.vessalbruits No.Extremities: Spine : normal.Spinous process :no.Mobility : normal. Extremeties: normal.Neural system:not found any abnormality.Genitourinary system: not examined.Rectum:not examinedHistory summary1.General information: Cai Chunwang ,male ,47y.2.Chief complaint: Pancytopenia for 2 year.3. past history: general situation is bad, Infectious history: Denied. Allergic history:. No.Operative history:He was once operated on an cholecystectomy. Tauma history: Denied. History of allergy:Denied . Historyof preventive inoculation] : the national plan for vaccination4. Physical examination: T 37℃, P95 /min, R 20 /min, BP 124/78 mmHg. his mental state is bad.Superficial lymph nodes were not found enlarged in his neck. heart rate 95 bpm/min ,rhythm:regular.Heart sound:S1 normal. S2 normal. S3 No. S4 no. shape normal . Abdominal respiration: existence .Umbilicus: normal protruding excretions others: NO. Palpation: soft. Tenderness: NO. Mass NO.liver:can’t be touched. gallbladder: can’t be touched. tenderness No. spleen: can’t be touched.Kideny:can’t be touched. tenderness mobility tenderness of ureters: No. Percussion: borders of liver dull: existence . pper borders of liver on right midclavicular line intercostal space shifting dullness No.tenderness in renal region No. Ausculation : borhorygmus normal . Gurgling No. vessal bruits No.movement of respiration : normal . Intercostal space :normal . Palpation : vocal fremitus : normal .pluernal friction rubs: No. Subcutaneous crepitus: No. percussion: resonance. Dusculation: breath regular. Breath sound: normal. Rale: No. Vocal conduction: norma .5.Specialist case:serious anemia. The skin was not stained yellow. Cyanosis. No pigmentation. No skin eruption. Spider angioma was not seen. No pitting edema. Superficial lymph nodes were not found enlarged in his neck.No tenderness of sternum. Ausculation of the heart and lung has not obvious abnormality. Abdomen is soft . Tenderness: NO. Mass NO. liver:can’t be touched. gallbladder: can’t be touched. tenderness No. spleen: can’t be touched. Extremeties are normal .6 . investigation information: one medical record of 2013 year.Impression: AMLSignature: Huang QiulanDate: 2013.2.27。
医学英语病历写作范文Chief Complaint: Patient presents with chest pain and shortness of breath for 3 days.History of Present Illness: The patient, a 55-year-old male, reports experiencing sudden onset of chest pain 3 days ago. The pain is described as sharp and crushing, radiating to the left arm. He also reports associated shortness of breath and diaphoresis. The symptoms are aggravated with physical activity and alleviated with rest. There is no history of similar episodes in the past.Past Medical History: The patient has a history of hypertension and hyperlipidemia. He is on regular medications including amlodipine and atorvastatin.Family History: The patient's father had a history of myocardial infarction at the age of 60. His mother has hypertension and diabetes.Social History: The patient is a non-smoker and denies alcohol or recreational drug use. He is currently employed as a manager and reports moderate stress at work.Review of Systems: The patient denies any recent weight changes, fever, or chills. There is no history of cough, sputum production, or hemoptysis. He denies any gastrointestinal symptoms such as nausea, vomiting, or abdominal pain.Physical Examination:- Vital signs: Blood pressure 140/90 mmHg, heart rate 90 bpm, respiratory rate 20 breaths per minute, oxygen saturation 96% on room air.- General: The patient appears uncomfortable and diaphoretic.- Cardiovascular: Regular rhythm, no murmurs, rubs, or gallops. Capillary refill time is less than 2 seconds.- Respiratory: Clear breath sounds bilaterally, no wheezing or crackles.Assessment and Plan:1. Rule out acute coronary syndrome: The patient's presentation is concerning for acute coronary syndrome given the symptoms of chest pain, shortness of breath, anddiaphoresis. ECG and cardiac enzymes will be obtained to evaluate for myocardial ischemia.2. Blood pressure management: The patient's blood pressure is elevated, and optimization of antihypertensive medications will be addressed.3. Lipid management: Given the patient's history of hyperlipidemia, lipid panel will be obtained to assess for dyslipidemia and adjust medications as needed.4. Stress management: The patient's moderate stress at work will be addressed through counseling and potential referral to a stress management program.中文病历:主诉:患者因胸痛和呼吸急促已3天。
英语病历书写范文五年级以下是一个简化的英语病历书写范文,适用于五年级学生的理解水平:Patient Information (患者信息)Name: John SmithAge: 10 years oldGender: MaleDate of Visit: May 20, 2024Chief Complaint (主诉)John's mother reports that he has had a fever and sore throat for the past two days.History of Present Illness (现病史)John started feeling sick two days ago. He has had a fever, ranging from 38°C to 39°C. He also complains of a sore throat, making it difficult to swallow. He has been drinking plenty of fluids but has had little appetite.Past Medical History (既往病史)John has no known allergies and has been healthy in the past. He has had no surgeries or hospitalizations.Physical Examination (体格检查)General: John appears tired but alert. Temperature: 38.5°CThroat: Erythematous (red) and swollen, with tonsillar enlargement.Respiratory: No difficulty breathing.Abdomen: Soft, non-tender.Diagnosis (诊断)Acute pharyngitis (sore throat) with feverTreatment Plan (治疗计划)1.Prescribe antibiotics (for 5 days)2.Advise rest and plenty of fluids3.Check back in 2 daysPatient Education (患者教育)Explain to John's mother the importance of completing the antibiotic course as prescribed. Advise her to monitor John's temperature and report any worsening symptoms.Follow-up (随访)Schedule a follow-up visit for 2 days from today.请注意,这个病历是一个简化的版本,旨在帮助学生理解病历的基本结构和内容。
英文病历范文Title: English Medical Record Sample (Creating and Expanding on a Matching Content)Medical RecordNa John SmithDate of Birth: February 15, 1985Gender: MaleNationality: AmericanOccupation: AccountantChief Complaint:The patient presented with a complaint of persistent cough, shortness of breath, and chest pain for the past week.History of Present Illness:The symptoms initially started as a mild cough, which gradually worsened over the week. The patient also experienced shortness of breath, especially during physical activities. He reported occasional chest pain, which was sharp in nature and intensified during deep breaths. The patient denied any fever, night sweats, or weight loss.Past Medical History:The patient has a history of asthma since childhood and has been using an inhaler as needed. He had a similar episode ofpersistent cough and shortness of breath six months ago, which resolved with a course of oral steroids. No other significant medical history was reported.Social History:The patient is a non-smoker and denies any alcohol or illicit drug use. He lives with his wife and two children in a smoke-free environment. The patient works as an accountant and does not have any known occupational exposures.Family History:There is no significant family history of respiratory diseases or any chronic illnesses.Review of Systems:The review of systems was unremarkable except for the respiratory symptoms mentioned above.Physical Examination:On examination, the patient appeared to be in no acute distress. Vital signs were within normal limits. Auscultation of the lungs revealed mild wheezing bilaterally. Heart sounds were normal, and there were no signs of peripheral edema or cyanosis. Other systemic examinations were within normal limits.Investigations:Laboratory investigations, including complete blood count, liver and kidney function tests, and electrolyte levels, were all within normal range. Chest X-ray showed hyperinflation of lungs and no evidence of infiltrates or consolidation.Assessment and Plan:Based on the history, clinical findings, and investigations, the patient's symptoms and past medical history suggest asthma exacerbation. Initial management includes a trial of short-acting bronchodilators, oral corticosteroids, and close monitoring of symptoms. The patient was educated about proper inhaler technique and advised to follow up in one week for reassessment.Education and Counseling:The patient was counseled on the importance of adherence to the prescribed medication and the need to avoid triggers for asthma exacerbation, such as allergens and respiratory infections. He was also provided with a written asthma action plan for self-management and advised to seek medical attention if symptoms worsen or do not improve within a week.Follow-up:The patient will be scheduled for a follow-up visit in one week to reassess symptoms, evaluate response to treatment, andadjust the management plan accordingly.This medical record documents the patient's chief complaint, history of present illness, past medical history, social and family history, physical examination findings, investigations, diagnosis, and treatment plan. It serves as a comprehensive guide for healthcare professionals involved in the patient's care.。
Case HistoryDefinitionA case history is a medical record of a patient’s illness. It records the whole medical case and functions as the basis for medical practitioners to make an accurate diagnosis and proposes effective treatment or preventive measures.Case histories fall into two kinds:in-patient case histories and out-patient case histories.Language FeaturesHistory and Physical usually involves past tense ( for history of present illness, past medical history, family history and review of systems concerning past information), and present tense ( review of system, physical examination, laboratory data, and plans ).Structurally, noun phrases are frequently used in physical examination, and ellipsis of subject is very common in review of system.In-patient Case HistoriesAn in-patient case history is also termed as History and Physical. It is an account of a patient’s present complaints with descriptions of his past medical history,and the description of the present conditions as well as physical examinations and impression about theIt usually consists of chief complaint, history of present illness, past medical history, review of systems, physical examination, impression, family history, social history, medications, allergies, laboratory on admission, and plan. However, what parts are included depends on the needs.住院病人病历完整模式病历(Case History)姓名(Name) 职业(Occupation)性别(Sex) 住址(Address)年龄(Age or DOB) 供史者(Supplier of history)婚姻(Marital status) 入院日期(Date of admission)籍贯(Place of birth) 记录日期(Date of record)民族(Race)主述.)现病史(HPI or .)过去史(PMH or .)社会活动史/个人史(SHx or .)家族史(FHx or .)曾用药物(Meds)过敏史(All)To be continued系统回顾(ROS)体格检查(PE or .)体温(T) 呼吸(R)血压(BP) 脉搏(P)一般状况(General status)皮肤黏膜(Skin & mucosa)头眼耳鼻喉(HEENT)颈部(Neck)胸部与心肺(Chest, Heart and Lungs)腹部(Abdomen)肛门直肠(Anus & rectum)外生殖器(External genitalia)四肢脊柱(Extremities & spine)神经反射(Nerve reflex)To be continued化验室资料(Lab data)(Blood test, Chem-7, EKG, EEG, X-ray examinations or X-ray slides, CT and NMR…)印象与诊断(Impression and diagnosis, or Imp)住院治疗情况记录(Hospital course)出院医嘱(Discharge instructions or recommendations)出院后用药(Discharge medications)医师签名(Signature)Patterns and contents of an out-patient case historyContents: general data (GD), chief complaint (CC), present illness (PI), physical examination (PE), tentative diagnosis (TD) or impression (Imp), treatment (Rp), etc.An out-patient case history should be written in brief and to the very point. More abbreviations and noun phrases are used.Sample of an out-patient case historyMale, 39 year oldCC: Fever, headache and cough for two days.PE: . looks fair. Pharynx congested and tonsils enlarged. Chest and abdomen negative.Imp:Rp: Penicillin 400,000u. .) . x 3 days.Aspirin 1 tab. x 2 days.Vit C 100 mg x 3 daysSignature ______Chief Complaint .)1. Sentence patterns in chief complaint症状+for+时间症状+of+时间+duration症状+时间+in duration时间+of+症状症状+since+时间Chief Complaint .)2. Commonly-used complaints:weakness, malaise, chills, fever, pain, headache, nausea and vomiting, diarrhea, neuro-psychiatric disorders, shortness of breath, bleeding or discharge, insomnia, stomachache, dyspepsia, no appetite, dysuria, cough, difficulty in coughing up sputum, sore throat, dizziness, palpitation, restlessness, etc. •弱点,不适感,发冷、发烧、疼痛、头痛、恶心、呕吐、腹泻、neuro-psychiatric紊乱、气短、出血或排放、失眠、胃痛,消化不良,没有胃口,排尿困难、咳嗽、咳痰、困难、喉咙痛、头晕、心悸、不安等。
Present Illness .)简明病历书写手册.docThe course of onsetDate of onsetMode of onsetProdromal symptomsThe cardinal symptomsThe attack of illnessThe development of symptomsDiagnosis and treatmentGeneral conditionExampleSpecial language structures in presenting present illness1. Describing the course of onset… started / began having / feeling …… first noticed / noted / perceived / recognized the onset of …… are the prodrome of …,… herald …Special language structures in presenting present illness2. Describing the mode and regularity of onsetexplosively / suddenly / acutely / abruptlygradually / chronically / increasingly / insidiouslyoccasionally / accidentallyoften / frequently / in frequency / recurrentlypersistently / intermittently爆炸性/突然/强烈•/突然长期/越来越多•逐渐/ /在不知不觉之中•偶尔/偶经常/经常在%的频率/的循环•持久/断断续续的Special language structures in presenting present illness3. Describing the cardinal symptoms… had / presented / developed / showed / manifested …… characterized by …… admits to …… states that …… feels …… denies …, … without / free of symptoms…Special language structures in presenting present illness4. Describing the attack of illness… appeared / occurred / came on …… had / developed episodes / attacks of …… was associated with …, …was accompanied by …, … was followed by …, … had relation to …… was preceded / heralded by …Special language structures in presenting present illness5. Describing the development of symptoms… disappeared / ceased / subsided …… took a favorable turn …., …took a turn for the better …, …relieved / improved / alleviated …… took a bad / unfavorable turn …, … took a turn for the worse …, …was aggravated / intens ified / exacerbated by …… remained the same as …, … continued, … persisted without changePast History .)简明病历书写手册.docHistory of vaccination and infectious diseasesHistory of allergy to drugs and other substancesHistory of surgical operation and external injurySystematic review of the past history and diseaseSpecial language structures in presenting past history… had enjoyed good health until… / … had been sound / well / healthy until…… had never been ill before … / had no illness of any kind before …… denied any history of / had no related history of / … denied experiencing / having attack of …No history of … / No history suggestive of / indicative of …… suffered from … / … had an attack of … / … was attacked / troubled by / … had a past history of …Except for … had no … / … no … apart from / but …Common diseases mentioned in past historymeasles, mumps, chicken-pox, smallpox, pertussis, influenza, scarlet fever, diphtheria, typhoid fever, bronchitis, pneumonia, encephalitis, meningitis, tetanus, poliomyelitis, dysentery, cholera, pleurisy, tonsillitis, rheumatism, malaria, tuberculosis, jaundice, allergy, sexually transmitted diseases, gonorrhea, syphilis, sequela, complication, hospitalization…麻疹,腮腺炎,chicken-pox氮、天花、百日咳、流行性感冒、猩红热、白喉、伤寒、支气管炎、肺炎、脑炎、脑膜炎、破伤风、脊髓灰质炎(小儿麻痹)、痢疾、霍乱、胸膜炎、扁桃体炎、风湿、疟疾、肺结核、黄疸、过敏、性传播疾病、淋病、梅毒、后遗症、并发症、住院…Personal History .) /Social History简明病历书写手册.docLife style and habitOccupation and working environmentMarital & childbearing historyMenstrual historyTraveling historySpecial language structures in presenting personal habits…have a long history of smoking / drinking…have a lifelong like / dislike for……admitted to excessive use of……denies the use of alcoholic beveragesSpecial language structures in presenting occupational history…work / act / serve as……be engaged in……practice one’s profession in ……be exposed to industrial poisons / dust / radioactive substances / hazards / toxic substances…Special language structures in presenting marital & childbearing history简明病历书写手册.doc… have been married for … years without conception… have a history of abortion or premature births… delivered one normal / abnormal infant… delivered … days before / prior to the expected date of confinementFamily History .)简明病历书写手册.docTerms mentioned in family historyfamily tendency, presence of hereditary disorders, cancer, tuberculosis, mental disorder and nervous affection, rheumatism, diabetes, hypertension, cerebral vascular accident, hemophilia, syphilis, tumor, epilepsy, allergy, etc. any contact with diseased individuals, relationship of patient’s childhood and adult life; age, health condition, and cause of death of parents, grandparents, self, spouse, siblings or relatives. 家庭的倾向,存在•遗传疾病、癌症、肺结核、精神障碍和紧张的感情、风湿、糖尿病、高血压、脑血管意外、血友病、梅毒、肿瘤、癫痫、过敏等任何接触患病的个人关系,病人的童年和成年生活;年龄、健康状况、和死亡原因的父母、祖父母、本人,配偶、兄弟姐妹或不相关的亲戚(联系)。