血药浓度及药动学参数
- 格式:pdf
- 大小:310.30 KB
- 文档页数:4
1实验一 血药浓度法测定扑热息痛静脉注射给药的药动学参数[实验目的]掌握静脉注射给药后用血药浓度法测定药物制剂的药物动力学参数的原理与方法,并加深对这些参数的理解。
[仪器与试剂]仪器:离心机,紫外分光光度计,离心试管,具塞刻度试管,涡旋混合器 试剂:对乙酰氨基酚、1%肝素溶液、0.12mol/L 氢氧化钡溶液、20g/L 硫酸锌溶液[实验原理]本实验以对乙酰氨基酚为模型药物,测定其在家兔体内的药物动力学参数。
若药物在体内分布符合单室模型,静脉注射给药时,药物按一级速度消除,则血药浓度经时变化公式为:kt e C C -=0式中C 为t 时间血药浓度;k 为表观一级消除速度常数。
两边同取对数,得:0log 303.2log C kt C +-=,k=-2.303×b ,a C 10lg -= 相关公式: kt 693.021=,00C X V =,kV Cl = Vk X k C Cdt AUC 000k t -00dt e C ====⎰⎰∞∞ kC t t C C AUC n i i n i i i +-+=+-=+∑)](2[1101[实验方法]1 标准曲线的制备1.1 标准溶液的配制精密称取105℃干燥恒重的扑热息痛1g (按含量计算称取)。
用热蒸馏水溶解于250ml容量瓶中,冷至室温后稀释至刻度,置冰箱保存备用(4000µg /ml)。
分别精密吸取上述4000µg /ml的浓贮备液1.25、2.5、3.75、5.0、6.25ml 于100ml容量瓶中,用蒸馏水稀释至刻度,得50、100、150、200、250µg /ml 的标准溶液。
1.2 空白(无药)血浆的制备将试验动物家兔耳静脉处毛拔掉,涂搽酒精,用100W 灯泡烤5min,再将耳静脉横向切开,用经1%肝素溶液处理并烤干的离心管采血约9ml。
然后将刀口贴上棉球,用夹子夹住。
将所取血样置37℃水浴中保温1h,离心(3000r/min)10min,得上清液(血浆)约4.5ml,制备标准曲线用3ml。
![[管理]血药浓度随时间变化的规律及药动学参数](https://uimg.taocdn.com/4efc5e3ae3bd960590c69ec3d5bbfd0a7956d576.webp)
血药浓度随时间变化的规律及药动学参数血药浓度随时间变化的规律及药动学参数(一)药时曲线用药后药物在体内的浓度可因转运或转化以致随时间而变化,药效也随着浓度而变化,如以曲线表示,则前者称时量关系曲线(Time-concentration Relationship Curve),后者为时效关系曲线(Time-response Relationship Curve)。
以非静脉一次给药为例,药物的时量关系和时效关系经历以下三个阶段:潜伏期-持续期-残留期。
潜伏期:用药后到开始出现作用的时间,反映药物的吸收和分布;持续期:药物维持有效浓度的时间;残留期:药物浓度已降至最小有效浓度以下时,但尚未从体内完全消除的时间。
(三)药物的消除动力学:血药浓度不断衰减的动态变化过程。
药物的消除:药物经生物转化和排泄使药理活性消失的过程。
药物的消除动力学有两种:1、一级消除动力学:指单位时间内药物按恒定的比例消除。
即血液中药物的消除速率与血中的药物浓度成正比,机体的血药浓度高,其单位时间内消除的药量多,消除速度随血药浓度下降而降低。
在血药浓度下降以后,药物的消除仍然按比率消除,故又称之为药物的恒比消除。
大多数药物按此方式消除。
如每小时消除1/2。
2、零级消除动力学:指单位时间内药物按恒定数量进行的消除。
即不论血浆药物浓度高低,单位时间内消除的药物量不变。
故又称之为药物的恒量消除。
常为药量过大,超过机体最大消除能力所致。
如每小时消除100mg/h。
(三)药物的消除动力学:血药浓度不断衰减的动态变化过程。
药物的消除:药物经生物转化和排泄使药理活性消失的过程。
药物的消除动力学有两种:1、一级消除动力学:指单位时间内药物按恒定的比例消除。
即血液中药物的消除速率与血中的药物浓度成正比,机体的血药浓度高,其单位时间内消除的药量多,消除速度随血药浓度下降而降低。
在血药浓度下降以后,药物的消除仍然按比率消除,故又称之为药物的恒比消除。
大多数药物按此方式消除。
生物药剂学与药动学——药动学概述一、药动学定义药动学是应用动力学的原理和数学处理方法,研究药物在体内的吸收、分布、代谢和排泄过程(即ADME 过程)的量变规律的学科,即药动学是研究药物体内过程动态变化规律的一门学科。
二、血药浓度与药物效应(一)治疗浓度范围治疗浓度范围即治疗窗,是指给药后产生药效的最低有效浓度和产生毒性的最低中毒浓度之间的浓度范围。
治疗窗窄的药物,其治疗浓度相对较难控制,易发生治疗失败或不良反应,常需进行治疗药物监测。
(二)血药浓度与药物效应的关系对于大多数药物及其制剂,药物进入体内后,血中的药物浓度与药物作用靶位的实际浓度呈正相关,从而间接反映药物的临床效应,包括治疗效果及不良反应。
药动学中常以血液中的药物总浓度作为观察指标。
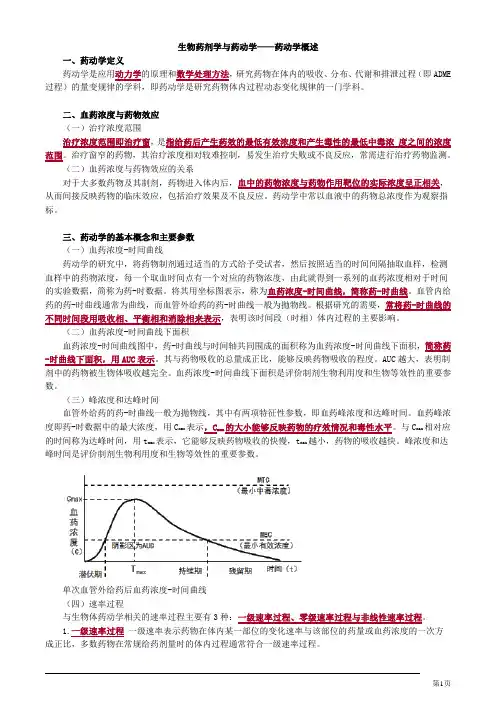
三、药动学的基本概念和主要参数(一)血药浓度-时间曲线药动学的研究中,将药物制剂通过适当的方式给予受试者,然后按照适当的时间间隔抽取血样,检测血样中的药物浓度,每一个取血时间点有一个对应的药物浓度,由此就得到一系列的血药浓度相对于时间的实验数据,简称为药-时数据。
将其用坐标图表示,称为血药浓度-时间曲线,简称药-时曲线。
血管内给药的药-时曲线通常为曲线,而血管外给药的药-时曲线一般为拋物线。
根据研究的需要,常将药-时曲线的不同时间段用吸收相、平衡相和消除相来表示,表明该时间段(时相)体内过程的主要影响。
(二)血药浓度-时间曲线下面积血药浓度-时间曲线图中,药-时曲线与时间轴共同围成的面积称为血药浓度-时间曲线下面积,简称药-时曲线下面积,用AUC表示。
其与药物吸收的总量成正比,能够反映药物吸收的程度。
AUC越大,表明制剂中的药物被生物体吸收越完全。
血药浓度-时间曲线下面积是评价制剂生物利用度和生物等效性的重要参数。
(三)峰浓度和达峰时间血管外给药的药-时曲线一般为拋物线,其中有两项特征性参数,即血药峰浓度和达峰时间。
血药峰浓度即药-时数据中的最大浓度,用C max表示,C max的大小能够反映药物的疗效情况和毒性水平。


吸入制剂评价参数吸入制剂是指通过呼吸道给药的药物制剂,适用于治疗各种呼吸系统疾病。
其评价参数相当重要,可以分为物理性质、生物利用度、性能及稳定性、药动学、安全性和有效性等方面。
下面是一些相关参考内容:一、物理性质评价参数:1. 粒径分布:吸入制剂的粒径分布对其沉积在目标部位的药物吸收和疗效具有直接影响。
可以通过激光粒度仪等检测仪器来测定粒径分布。
2. 重量:测量制剂的重量可以用来确定给药剂量的准确性。
3. 颗粒密度:粒子的颗粒密度能指示制剂的均匀性和稳定性。
二、生物利用度评价参数:1. 药物释放速率:药物释放速率是吸入制剂的重要参数之一,能反映吸入制剂的释药性能。
2. 肺部沉积率:通过评测肺部沉积率来评估药物在吸入后在呼吸道中的分布情况,了解药物与呼吸道的相互作用。
三、性能及稳定性评价参数:1. 温度和湿度敏感性:以及稳定性是评估吸入制剂稳定性的重要参数,可以通过暴露于不同温度和湿度条件下进行观察。
吸入制剂的稳定性能直接影响其药效。
2. 吸湿性:吸入制剂的吸湿性评价是一个重要的参数,吸湿性能能够影响药物的储存和附加物的准确性。
四、药动学评价参数:1. 血药浓度:通过检测给药后在血液中的药物浓度变化可以评估药物的吸收情况和血液清除速率。
2. 药物代谢:评估药物的代谢途径和代谢产物对其药理活性的影响。
五、安全性评价参数:1. 毒性:通过动物实验等方法评估药物对机体的毒性和副作用。
2. 致敏性:评估药物对宿主免疫系统的影响,是否会引起过敏反应。
六、有效性评价参数:1. 治疗效果:评估吸入制剂在临床应用中的治疗效果和疗效。
2. 目标部位浓度:评估吸入制剂在呼吸道中的沉积情况,以及药物在目标部位的浓度。
总之,吸入制剂的评价参数是多方面的,包括物理性质、生物利用度、性能及稳定性、药动学、安全性和有效性等方面。
通过综合评估这些参数,可以判断吸入制剂的质量、稳定性和疗效,为其发展提供指导和依据。

血药浓度随时间变化的规律及药动学参数(The regularity and pharmacokinetic parameters of serum concentration with time)The regularity and pharmacokinetic parameters of serum concentration with time(I) drug time curveAfter administration of drug concentration in vivo by transfer or transformation that is changing with time, effect also changes along with concentration, such as curve representation, the former is called curve relationship (Time-concentration Relationship Curve), the latter for the aging curve(Time-response Relationship Curve).Taking the non intravenous administration for example, the dose duration relationship and the time dependence of the drug pass through the following three stages: incubation period, duration, and residual period.Incubation period: the time after which medication starts to function, reflecting the absorption and distribution of drugs;Duration: the time at which an effective concentration of the drug is maintained;Residual period: the concentration of the drug has been reduced to below the minimum effective concentration, but has not yet been completely eliminated from the body.(three) elimination kinetics of drugs: the dynamic process ofcontinuous attenuation of serum concentration.Elimination of drugs: the process of biotransformation and excretion of drugs that results in the disappearance of pharmacological activity. There are two kinds of the kinetics of the elimination of drugs:1, first-order elimination kinetics: the elimination of drugs at a constant rate per unit time.That is, the rate of elimination of drugs in the blood is directly proportional to the concentration of drugs in the blood, the blood concentration of the body is high, the amount of drugs is eliminated in unit time, and the elimination rate decreases with the decrease of serum concentration. After the decrease in serum concentration, the elimination of the drug is still eliminated at a rate. Therefore, it is also called the constant ratio elimination of drugs. Most drugs are eliminated this way.Such as the elimination of 1/2 per hour.2. Zero elimination kinetics: the elimination of a constant amount of drugs per unit time. That is, regardless of the level of plasma drug concentration, the amount of drugs removed per unit time. It is also known as the quantity of drug elimination. Often too much, more than the maximum elimination capacity caused by the body.Such as the elimination of 100mg/h per hour.(three) elimination kinetics of drugs: the dynamic process of continuous attenuation of serum concentration.Elimination of drugs: the process of biotransformation and excretion of drugs that results in the disappearance of pharmacological activity. There are two kinds of the kinetics of the elimination of drugs:1, first-order elimination kinetics: the elimination of drugs at a constant rate per unit time.That is, the rate of elimination of drugs in the blood is directly proportional to the concentration of drugs in the blood, the blood concentration of the body is high, the amount of drugs is eliminated in unit time, and the elimination rate decreases with the decrease of serum concentration. After the decrease in serum concentration, the elimination of the drug is still eliminated at a rate. Therefore, it is also called the constant ratio elimination of drugs. Most drugs are eliminated this way.Such as the elimination of 1/2 per hour.2. Zero elimination kinetics: the elimination of a constant amount of drugs per unit time. That is, regardless of the level of plasma drug concentration, the amount of drugs removed per unit time. It is also known as the quantity of drug elimination. Often too much, more than the maximum elimination capacity caused by the body.Such as the elimination of 100mg/h per hour.Four 、 pharmacokinetic parameters of commonly used drugs(a) bioavailability (Bioavailability):.The speed and extent of absorption of drugs into the body circulation.Notation: F= (A/D) * 100% (oral: <100%; vein: 100%)Divided into: absolute bioavailability: F= (PO equal amount of drugs, AUC/iv equal amount of drugs AUC) * 100%The relative bioavailability of F= (equivalent to the reagent AUC/ with standard drug AUC * 100%)(two) apparent volume of distributionThe volume of fluid required for the distribution of plasma drug levels in vivo after the distribution of plasma and tissue is balanced. Vd=A/C0, theoretical capacity)Significance:1, the distribution volume of a given drug is measured to produce the desired dosage of the drug concentration: D = C, Vd2. Predict the distribution of drugs:Vd small drugs are mainly distributed in organs with large bloodflow;Vd large, low blood concentration and wide distribution of drugs;(three) half-life: generally refers to the half-life of plasma (T1/2), that is, the time required for the plasma concentration to fall by half. Since most drugs are eliminated in afirst-order kinetic manner, their half-life is a constant, T1/2=0.693/ke.Significance: reflects the rate of drug elimination. T1/2 long to eliminate slow and maintain long time(1) drug classification according to: short effect, medium effect, long effect;(2) determine the interval between dosing(3) the steady-state concentration time was predicted: 4-5 t1/2;(4) predict the basic elimination time of drugs: 4-5 t1/2 after the last dose(four) the steady blood concentration (CSS/ / Ping Ping concentration value): continuous constant drug dosages, gradually accumulated, through 5 half-life, blood concentration reached a stable level. The serum concentration at this time is called steady-state serum concentration, CSS. At this point the amount of drugs removed and the amount of drugsentering the body is equal, drugs are no longer accumulated in the body.Significance: (1) the plateau concentration is directly proportional to the total quantity of the day.(2) the fluctuation range of plateau concentration, high limit and low limit is proportional to each dose.(five) clearance rate:The rate of clearance of the drug is how many liters of blood can be removed per unit time. Each drug has its own fixed CL.CL=ke/Vd.Four 、 the change of serum concentration and the regimen of administrationIn clinical, most drugs need to be repeatedly given in order to achieve the desired level of serum concentration. Therefore, the time curve of the administration is zigzag.(1) continuous constant dose, total dose increases, CSS increases; administration of the same amount, change the number of drug CSS invariant. A total of conventional drugs in children, the same day the total number of drug, the more each use less, smaller fluctuations in safety range of small, multiple service, Ping concentration maintained at the minimum effective dose and minimum dose.(2) dose volume maintenance method: doubling the first dose, then rapidly reaching CSS in a half life, and then using maintenance dose. This method is suitable for emergency treatment, and requires rapid treatment.(3) intermittent administration: according to the needs of clinical treatment, the medication regimen with interval of more than half time can be used to reduce the incidence of adverse reactions. Such as glucocorticoids.(4) the regimen should be individualized, such as liver and kidney dysfunction, the half-life is longer than normal, and the time to CSS is longer. Therefore, the dosage should be reduced and the interval between doses should be extended.。

药动学的参数药物动力学是研究药物在体内吸收、分布、代谢和排泄过程的科学。
正确认识和掌握药物动力学的参数对于合理用药、临床治疗以及新药开发都具有重要意义。
本文将从吸收、分布、代谢和排泄四个方面分别介绍药物动力学的主要参数。
一、吸收参数1. 生物利用度(bioavailability):药物经口给药后进入体内的总吸收量与直接注射的总吸收量的比值。
一般通过体内外药物浓度随时间的变化曲线来计算。
2. 最大血浓度(Cmax):药物在给药之后血浆中达到的最高浓度。
该参数反映了药物吸收的速度和程度。
3. 时间到达峰浓度(Tmax):最大血浓度出现所需要的时间。
4. 血药浓度-时间曲线(AUC):药物在体内的总曝露量,通过血浆药物浓度随时间的变化曲线下的面积来计算。
AUC值越大,表示总体内曝露量越大。
二、分布参数1. 分布容积(Vd):反映药物在体内分布的广泛程度。
Vd值越大,说明药物在体内的分布范围越广。
2. 血浆蛋白结合率(protein binding):部分药物在体内主要以结合蛋白的形式存在,该参数反映了药物与蛋白质结合的程度。
3. 大脑-血浆分布系数(BBB):反映了药物能否越过血脑屏障进入脑组织,对于中枢神经系统药物很重要。
三、代谢参数1. 代谢速率(metabolic clearance):单位时间内从血浆中清除药物的速率。
代谢速率越大,药物代谢越快。
2. 代谢半衰期(t1/2):药物浓度下降到初始浓度的一半所需要的时间。
代谢半衰期可间接反映药物在体内停留的时间。
四、排泄参数1. 肾脏清除率(renal clearance):药物在单位时间内通过肾脏清除的速率。
2. 肝脏清除率(hepatic clearance):药物在单位时间内通过肝脏清除的速率。
药物动力学参数反映了药物在体内的代谢、分布、排泄等过程。
了解这些参数有助于合理用药,指导临床用药,也有助于评价新药的临床前药代动力学特性。
对于药物研究、开发和用药安全有着重要的意义。
反映药物吸收的药动学参数药物吸收是药物在体内进入血液循环的过程,是药物治疗效果的关键环节之一。
药物吸收的药动学参数是评价药物吸收速度和程度的指标,对于合理用药和优化药物疗效具有重要意义。
药物吸收的药动学参数主要包括吸收速度常数(Ka)、吸收半衰期(t1/2a)、绝对生物利用度(F)和相对生物利用度(Frel)等。
吸收速度常数(Ka)是衡量药物从给药部位进入血液的速度的指标。
它反映了药物在给药部位的吸收速度,通常用一级动力学方程来描述。
吸收速度常数越大,说明药物吸收越快,反之则说明吸收较慢。
吸收半衰期(t1/2a)是指药物从给药部位进入血液后,血浆中药物浓度下降到初始浓度一半所需的时间。
吸收半衰期的长短直接影响到药物的疗效和给药频率。
吸收半衰期越短,说明药物吸收速度越快,血浆中药物浓度下降得越快,需要更频繁地给药。
绝对生物利用度(F)是指药物经口给药后进入血液循环的百分比。
它反映了口服给药后肠道吸收和首过效应对药物生物利用度的影响。
绝对生物利用度越高,说明药物口服后更容易被吸收并发挥作用。
相对生物利用度(Frel)是指某种给药途径相对于其他给药途径的生物利用度。
相对生物利用度常用来比较不同给药途径的吸收差异,如口服与静脉注射。
相对生物利用度大于1表示该途径的生物利用度高于参比途径,小于1表示生物利用度低于参比途径。
除了以上常见的参数外,还有一些其他的药动学参数也可以用来评价药物吸收情况,如峰浓度(Cmax)、时间达到峰浓度(Tmax)等。
峰浓度表示药物在给药后达到的最高浓度,反映了给药途径和剂量对血浆浓度的影响。
时间达到峰浓度则是指从给药到达峰浓度所需的时间。
药物吸收的药动学参数可以通过体内外试验、人体实验和计算模型等方法进行研究和评价。
这些参数对于合理用药、优化给药方案以及预测药物疗效都具有重要意义。
在新药研发和临床应用中,了解和掌握药物吸收的药动学参数是十分必要的。
药动学之
药时曲线及意义
药物的体内过程
药物的体内过程
吸收分布代谢排泄
单次给药的药-时曲线图
线图
横坐标:时间(单位:h)
纵坐标:血药浓度(单位:mg/L)
中的参数
单次给药药-时曲线中的参
单次给药药时曲线中的参数
1.药时曲线分为吸收分布相和消除相;峰浓度(Cmax)
指药物吸收速率与消除速率相等时曲线的最高点
2.药时曲线的时间段分为:潜伏期、持续期、残留期
3.起效时间(Tmin):药物刚产生疗效或刚达到最小
有效浓度时间;峰时间;峰时间(Tmax):药物在体
内达到峰浓度的时间
4.曲线下面积(AUC):药时曲线下所覆盖的面积
多次给药的药-时曲线
多次给药药时曲线中的参数
1.稳态浓度(Css):药物在连续恒速或分次
恒量给药后,当给药速度等于消除速度时,
血药浓度维持在一个相对稳定的水平
2.峰浓度(Css,max)与谷浓度(Css,min)
多次给药的稳态血药浓度浓度
多次给药的稳态血药浓度
1.在等剂量等间隔的给药方法中,如果间隔一个半衰
期给药一次,经过4~6个半衰期可达到稳态血药浓度;
2.在负荷量+维持量的给药方法中,如果需要立即达到
稳态浓度,可采取负荷量用药,即按照半衰期为给药
间隔时,首次给药剂量加倍的方法,可在用药后一个
半衰期内达到问题血药浓度。
常用的药物代谢动力学参数包括那些药物代谢动力学(Pharmacokinetics,PK)是研究药物在体内的吸收、分布、代谢和排泄过程的科学。
常用的药物代谢动力学参数通常包括生物利用度(Bioavailability)、血药浓度峰值(Cmax)、时间-浓度曲线下面积(Area Under the Concentration-Time Curve,AUC)、药物半衰期(Half-life)、总体清除率(Clearance)、体积分布(Volume of Distribution)等。
1. 生物利用度(Bioavailability):指药物在体内经过吸收后进入体循环的程度,以百分比表示。
常用的计算方法包括静脉给药和口服给药后药物浓度的比较。
2. 血药浓度峰值(Cmax):指药物在给药后血浆或血清中达到的最高浓度。
Cmax的高低可以反映药物的吸收速度和经历的代谢和排泄过程。
3.时间-浓度曲线下面积(AUC):是反映药物在体内总体曝露程度的参数,表示血药浓度与时间的关系。
AUC值越大,说明药物在体内停留时间越长。
4. 药物半衰期(Half-life):指药物浓度降至初始浓度的一半所需的时间。
半衰期可以用来估计药物的消除速度。
5. 总体清除率(Clearance):指药物从体内完全清除的速度。
体内清除药物的总速率等于药物的剂量除以血浆中的平均浓度。
所以清除率可以用来估计药物在体内的排泄速度。
6. 体积分布(Volume of Distribution):描述药物在体内分布的广泛程度,计算方法是将药物剂量除以血浆中的初始浓度。
体积分布越大,说明药物在体内的分布范围越广。
此外,药物代谢动力学还可以进一步计算出其他参数,如药物清除率(Drug Clearance)、血浆蛋白结合率(Plasma Protein Binding),以及药物在肝脏的代谢率等。
这些参数可以帮助评估药物的药代动力学特征,并在药物治疗中确定剂量、调整给药方案等方面有重要的指导意义。
掌握药动学基本概念及其重要参数之间的相互关系:药-时曲线下面积、生物利用度、药峰时间、药峰浓度、消除半衰期、表观分布容积、清除率等。
一、一次性血管外给药三个时期1、潜伏期(短:吸收快)------有效期------残留期(长:蓄积中毒)2、时量关系:血药浓度随时间的变化过程。
3、房室概念与房室模型1)、一室模型:假定身体由一个房室组成,给药后药物立即均匀地分别于整个房室,并以一定的速率从该室消除。
单次静注给药时,时量(对数浓度)曲线呈单指数消除。
2)、二室模型:假定身体由两个房室组成,即中央室(血流丰富的器官如心、肝、肾)和周边室(血流量少的器官如骨、脂肪)。
给药后药物立即分布到中央室,然后缓慢分布到周边室。
单次静注给药时,时量(对数浓度)曲线呈双指数衰减即分为分布相和消除相。
二、药动学重要参数1、消除半衰期及意义:血药浓度下降一半所需的时间。
是决定给药间隔时间的重要参数之一。
2、生物利用度:药物吸收速度与程度的一种量度。
可药时曲线下面积AUC 计算,F=口服AUC/注射AUC 。
3、表观分布容积Vd :是指血药浓度与体内药物量间的一个比值,Vd=A/C=体内药量/血药浓度。
可反映药物分布的广泛程度或药物与组织结合的程度。
4、药-时曲线下面积AUC 代表一次用药后的吸收总量,反映药物的吸收程度。
三、药物消除动力学1.一级消除动力学(恒比消除):多数药消除半衰期恒定,与血药浓度无关。
血浆清除率(Cl):即单位时间内多少容积血浆中的药物被消除干净(单位用L&#8226;h-1 )。
消除速率:单位时间内被机体消除的药量。
常用表观分布容积(Vd)计算。
Vd及Cl的区别:①是两个独立的药动学指标,各有其固定的数值,互不影响,也不因剂量大小而改变其数值。
②Vd是表观数值,不是实际的体液间隔大小。
多数药的Vd值均大于血浆容积。
③Cl不是药物的实际排泄量。
Cl是肝肾等消除能力的总和。
④与组织亲和力大的脂溶xing药物其Vd可能比实际体重的容积还大。