胸外科英文文献汇报2017.11.23
- 格式:pptx
- 大小:774.75 KB
- 文档页数:10
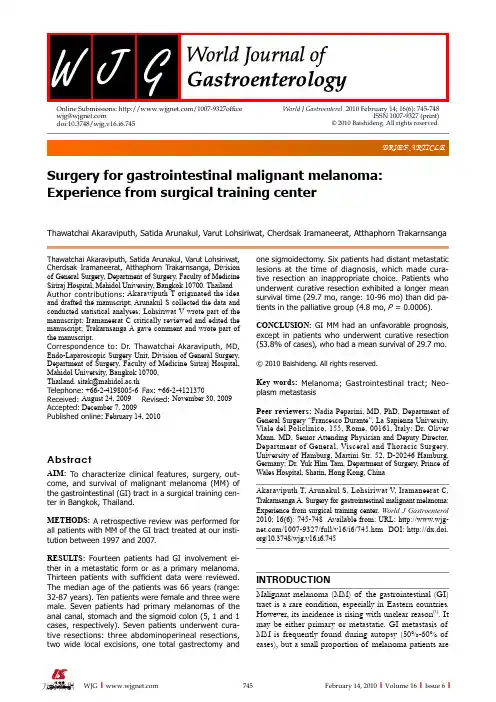
BRIEF ARTICLESurgery for gastrointestinal malignant melanoma: Experience from surgical training centerThawatchai Akaraviputh, Satida Arunakul, Varut Lohsiriwat, Cherdsak Iramaneerat, Atthaphorn TrakarnsangaThawatchai Akaraviputh, Satida Arunakul, Varut Lohsiriwat, Cherdsak Iramaneerat, Atthaphorn Trakarnsanga, Division of General Surgery, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand Author contributions: Akaraviputh T originated the idea and drafted the manuscript; Arunakul S collected the data and conducted statistical analyses; Lohsiriwat V wrote part of the manuscript; Iramaneerat C critically reviewed and edited the manuscript; Trakarnsanga A gave comment and wrote part of the manuscript.Correspondence to: Dr. Thawatchai Akaraviputh, MD, Endo-Laparoscopic Surgery Unit, Division of General Surgery, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok 10700, Thailand. sitak@mahidol.ac.thTelephone: +66-2-4198005-6 Fax: +66-2-4121370Received: August 24, 2009 Revised: November 30, 2009Accepted: December 7, 2009Published online: February 14, 2010AbstractAIM: To characterize clinical features, surgery, out-come, and survival of malignant melanoma (MM) of the gastrointestinal (GI) tract in a surgical training cen-ter in Bangkok, Thailand.METHODS: A retrospective review was performed for all patients with MM of the GI tract treated at our insti-tution between 1997 and 2007.RESULTS: Fourteen patients had GI involvement ei-ther in a metastatic form or as a primary melanoma. Thirteen patients with sufficient data were reviewed. The median age of the patients was 66 years (range: 32-87 years). Ten patients were female and three were male. Seven patients had primary melanomas of the anal canal, stomach and the sigmoid colon (5, 1 and 1 cases, respectively). Seven patients underwent cura-tive resections: three abdominoperineal resections, two wide local excisions, one total gastrectomy andone sigmoidectomy. Six patients had distant metastatic lesions at the time of diagnosis, which made cura-tive resection an inappropriate choice. Patients who underwent curative resection exhibited a longer mean survival time (29.7 mo, range: 10-96 mo) than did pa-tients in the palliative group (4.8 mo, P = 0.0006).CONCLUSION: GI MM had an unfavorable prognosis, except in patients who underwent curative resection (53.8% of cases), who had a mean survival of 29.7 mo.© 2010 Baishideng. All rights reserved.Key words: Melanoma; Gastrointestinal tract; Neo-plasm metastasisPeer reviewers: Nadia Peparini, MD, PhD, Department ofGeneral Surgery “Francesco Durante”, La Sapienza University, Viale del Policlinico, 155, Rome, 00161, Italy; Dr. Oliver Mann, MD, Senior Attending Physician and Deputy Director, Department of General, Visceral and Thoracic Surgery, University of Hamburg, Martini Str. 52, D-20246 Hamburg, Germany; Dr. Yuk Him Tam, Department of Surgery, Prince of Wales Hospital, Shatin, Hong Kong, ChinaAkaraviputh T, Arunakul S, Lohsiriwat V, Iramaneerat C, Trakarnsanga A. Surgery for gastrointestinal malignant melanoma: Experience from surgical training center. World J Gastroenterol 2010; 16(6): 745-748 Available from: URL: /1007-9327/full/v16/i6/745.htm DOI: /10.3748/wjg.v16.i6.745INTRODUCTIONMalignant melanoma (MM) of the gastrointestinal (GI) tract is a rare condition, especially in Eastern countries. However, its incidence is rising with unclear reason [1]. It may be either primary or metastatic. GI metastasis of MM is frequently found during autopsy (50%-60% of cases), but a small proportion of melanoma patients areWorld J Gastroenterol 2010 February 14; 16(6): 745-748ISSN 1007-9327 (print)© 2010 Baishideng. All rights reserved.Online Submissions: /1007-9327office wjg@doi:10.3748/wjg.v16.i6.745diagnosed with GI metastasis while living (2%-5% of patients)[2,3]. The most common sites of the metastasis are the stomach and small intestine. Meanwhile, pri-mary MM can arise in any GI mucosal site, but is most common in the anorectal region and esophagus.The prognosis of GI MM is very poor with a 5-year survival of< 10%[4]. Surgery is still the mainstay of treatment. Recent studies have reported a trend toward less radical resection because there is no significant ad-vantage of aggressive surgery over limited surgery in terms of local disease control, recurrence, and survival time[4,5].In Thailand, MM is less common than in western countries and the data are limited. This study, therefore, was conducted to evaluate clinical features, surgical op-tions, and outcome including recurrence and survival of MM of the GI tract in a surgical training center in Bang-kok, Thailand.MATERIALS AND METHODSA retrospective review was conducted on patients diag-nosed with MM of the GI tract who were admitted to Siriraj Hospital between 1997 and 2007. Patients were identified from the hospital computer database us-ing an ICD-10 system. Patients’ charts were reviewed retrospectively for patient characteristics, presenting symptoms, physical examination findings, imaging re-sults, operative records, presence of complications, recurrence, follow-up time, survival time, and cause of death. Diagnosis was confirmed in all patients by histo-logical study and immunochemistry for S-100 protein or HMB45 monoclonal antibody. Survival time was defined as the number of months from the time of diagnosis of GI MM to the time of death or the last follow-up evaluation. The long-term follow-up data were col-lected by direct contact with patients or their relatives.A Kaplan-Meier method was used for statistical analysis of survival outcome. This study was approved by Siriraj ethics committee, Mahidol University (EC1 2550/307).RESULTSBetween 1997 and 2007, there were 14 patients diag-nosed with MM of the GI tract in Siriraj Hospital. One patient was excluded from this study due to insufficient data in the medical records; thus, only 13 cases were in-cluded in this study. Ten patients were female and three were male. The median age of the patients at presenta-tion was 66 years (range: 32-87 years). Seven patients had a primary GI MM (anorectal, n = 5; sigmoid colon, n= 1; and stomach, n= 1), whereas the others (three patients, 23.1%) had metastatic MM of the GI tract. The primary melanoma sites of these three patients were ocular, thumb, and ovary. There were three patients who had advanced GI MM of unknown primary origin.The most common presenting symptom was ab-dominal pain (5 patients, 38.5%), followed by intra-ab-dominal mass in four patients (30.8%). Other presenting symptoms included obstructive jaundice, small bowel obstruction, bowel habit change, and tenesmus. The anorectal region was the most common site of GI MM (7 patients, 53.8%), followed by the stomach (3 patients, 23.1%) (Table 1).Seven patients (53.8%) underwent curative resection, which consisted of three abdominoperineal resections, two wide local excisions, one total gastrectomy, and one sigmoidectomy. There was no perioperative mortality in this study. Meanwhile, another six patients (46.2%) had distant metastatic lesions at the time of diagnosis. They therefore received only palliative surgical treatment such as colostomy, small bowel resection, and enteroenterostomy anastomosis. Patients who underwent curative resection exhibited a longer mean survival time (29.7 mo, range: 10-96 mo) than patients in the palliative group (4.8 mo, range: 4-12 mo) (Figure 1). Survival was significantly increased in patients who underwent curative resection (P = 0.0006).DISCUSSIONIn Thailand, MM is a rare disease. The estimated incidence rate of cutaneous melanoma in Thailand is 0.4 and 0.1 per 100 000 in men and women, respectively[5]. Incidence of MM of the GI tract is exceedingly rare[6]. There haveMM: Malignant melanoma; GI: Gastrointestinal; CT: Computed tomo-graphy.Akaraviputh T et al. Malignant melanoma of gastrointestinal tractbeen only a few reported cases of documented anorectal MM in Thailand [7]. MM of the GI tract can be either primary or metastatic. Primary GI melanoma must be differentiated from metastatic disease by previous history of melanoma and complete physical examination.Patients often present with bleeding, pain or intestinal obstruction. If the patients present with GI bleeding, an endoscopy with magnification might be the procedure of choice to diagnose MM of the GI tract [8-10]. Multiple black, depressed lesions (1 ± 5 mm in diameter) with a “bull’s eye” appearance are usually viewed in the GI mucosa [9]. In the present study, approximately half of the patients presented with pain. A lower number of patients presented with gross GI bleeding and obstruction.MM of the GI tract remains a fatal disease. Patients often present with advanced disease. In our study, almost half of the patients had metastatic disease at the time of presentation. The prognosis of GI MM is poor. The mean survival time of patients with a local or locoregional disease who underwent curative resection was only 29.7 mo. Several investigators have reported that the overall survival varies from 12 to 18 mo, with a 5-year survival of < 10%[11]. When systemic metastasis has occurred, mean survival is only 6-8 mo [12,13].As a result of the poor prognosis of this disease, operative intervention has been discouraged. However, several recent studies have demonstrated better survival outcome in the patients who had complete surgical resection [14-19]. Our experiences compare favorably with those of other centers. Our study demonstrated seven patients with GI MM who underwent curative resection with a mean survival comparable to that in other centers. Several adjuvant treatment of GI MM such as chemotherapy, radiotherapy and immunotherapy have been utilized in many countries, but no such treatment was given in our center because of their unclear effectiveness. One recent randomized trial has demonstrated no survival benefit of adjuvant therapy [20].In conclusion, patients with GI MM had a poor prog-nosis, especially in nonoperable cases. Surgical resection of the tumor resulted in a longer survival time. In selected patients with local or locally advanced disease, surgery should be performed where possible.BackgroundGastrointestinal (GI) malignant melanoma (MM) is a rare malignancy. As a result of the paucity of cases, the available data about its clinical features, treat-ment options, and outcomes are very limited, especially in Eastern countries.Research frontiersAs a result of the poor prognosis of GI MM, improvement of its treatment op-tions is an area that is in need of research. However, in order to reach that point, some basic understanding of the clinical characteristics and treatment outcomes of current surgical approaches is required. This study provides a picture of clinical experience with this rare disease from one surgical training center in Thailand.Innovations and breakthroughsThis study revealed that the nature of MM of the GI tract and its treatment out-comes in Thailand were similar and comparable to those from other centers.ApplicationsWith a better understanding of GI MM and its poor prognosis, future research should look at how to improve the treatment outcome, through early diagnosis, selection of patients undergoing surgery, and improvement of surgical tech-niques.Peer reviewThis is a retrospective study on surgical management of MM of the GI tract. Patients who underwent curative resection exhibited a longer mean survival time than patients in the palliative group. Survival was significantly increased in patients who underwent curative resection.REFERENCES1 Klaase JM , Kroon BB. Surgery for melanoma metastatic to the gastrointestinal tract. Br J Surg 1990; 77: 60-612 Dasgupta T , Brasfield R. Metastatic melanoma. A clinico-pathological study. Cancer 1964; 17: 1323-13393 Cagir B , Whiteford MH, Topham A, Rakinic J, Fry RD. Changing epidemiology of anorectal melanoma. Dis Colon Rectum 1999; 42: 1203-12084 Bullard KM , Tuttle TM, Rothenberger DA, Madoff RD, Baxter NN, Finne CO, Spencer MP. Surgical therapy for anorectal melanoma. J Am Coll Surg 2003; 196: 206-2115 Promtatvethi V , Gojaseni P, Buri P, Censarn N. Malignant melanoma: a clinical experience in a Thai hospital. J Med Assoc Thai 1978; 61: 210-2166 Crombie IK . Racial differences in melanoma incidence. Br J Cancer 1979; 40: 185-1937Somran J , Kanngurn S, Porncharoenpong S, Lertkajornsin O. Anorectal malignant melanoma: report of two cases from Buddhachinnaraj Hospital. J Med Assoc Thai 2005; 88: 1128-11338 Pommer B , Probst A, Messmann H. Gastric metastases from malignant melanoma. Endoscopy 2008; 40 Suppl 2: E30-E31 9Tanaka K , Toyoda H, Hamada Y, Aoki M, Kosaka R, Noda T, Katsurahara M, Nakamura M, Ninomiya K, Inoue H, Imoto I. Duodenal metastasis of malignant melanoma observed by magnification endoscopy. Endoscopy 2008; 40 Suppl 2: E6-E7 10Galloro G , Inzirillo A, Magno L, Diamantis G, Inzirillo M, Pastore A, Ruggiero S, Mosella G. Multiple nodular lesions by colonic metastatic malignant melanoma. Dig Liver Dis 2009; 41: 16911 Yang JI , Byun HJ, Kang JM. Education and imaging. Gastrointestinal: anorectal malignant melanoma. J Gastroenterol Hepatol 2009; 24: 69712Liang KV , Sanderson SO, Nowakowski GS, Arora AS.1.00.90.80.70.60.50.40.30.20.10.0C u m s u r v i v a l0 12 24 36 48 60 72 84 96t /moFigure 1 Kaplan-Meier curve demonstrating survival of patients with malignant melanoma of the gastrointestinal tract, who underwent curative resection and palliative resection.Akaraviputh T et al . Malignant melanoma of gastrointestinal tractMetastatic malignant melanoma of the gastrointestinal tract.Mayo Clin Proc 2006; 81: 511-51613 Lens M, Bataille V, Krivokapic Z. Melanoma of the smallintestine. Lancet Oncol 2009; 10: 516-52114 Berger AC, Buell JF, Venzon D, Baker AR, Libutti SK.Management of symptomatic malignant melanoma of the gastrointestinal tract. Ann Surg Oncol 1999; 6: 155-16015 Agrawal S, Yao TJ, Coit DG. Surgery for melanomametastatic to the gastrointestinal tract. Ann Surg Oncol 1999; 6: 336-34416 Ishizone S, Koide N, Karasawa F, Akita N, Muranaka F,Uhara H, Miyagawa S. Surgical treatment for anorectal malignant melanoma: report of five cases and review of 79Japanese cases. Int J Colorectal Dis 2008; 23: 1257-126217 Sanki A, Scolyer RA, Thompson JF. Surgery for melanomametastases of the gastrointestinal tract: indications and results. Eur J Surg Oncol 2009; 35: 313-31918 Huang YJ, Wu MH, Lin MT. Multiple small-bowelintussusceptions caused by metastatic malignant melanoma.Am J Surg 2008; 196: e1-e219 Slaby J, Suri U. Metastatic melanoma with multiple smallbowel intussusceptions. Clin Nucl Med 2009; 34: 483-48520 Spitler LE, Grossbard ML, Ernstoff MS, Silver G, JacobsM, Hayes FA, Soong SJ. Adjuvant therapy of stage III and IV malignant melanoma using granulocyte-macrophage colony-stimulating factor. J Clin Oncol 2000; 18: 1614-1621S- Editor Tian L L- Editor Kerr C E- Editor Ma WHAkaraviputh T et al. Malignant melanoma of gastrointestinal tractSurgery for gastrointestinal malignant melanoma:Experience fromsurgical training center作者:Thawatchai Akaraviputh, Satida Arunakul, Varut Lohsiriwat, Cherdsak Iramaneerat,Atthaphorn Trakarnsanga作者单位:Division of General Surgery, Department of Surgery, Faculty of Medicine Siriraj Hospital,Mahidol University, Bangkok 10700, Thailand刊名:世界胃肠病学杂志(英文版)英文刊名:WORLD JOURNAL OF GASTROENTEROLOGY年,卷(期):2010,16(6)1.Klaase JM;Kroon BB Surgery for melanoma metastatic to the gastrointestinal tract[外文期刊] 19902.Dasgupta T;Brasfield R Metastatic melanoma.A clinicopathological study[外文期刊] 19643.Cagir B;Whiteford MH;Topham A;Rakinic J Fry RD Changing epidemiology of anorectal melanoma[外文期刊] 19994.Bullard KM;Tuttle TM;Rothenberger DA;Madoff RD Baxter NN Finne CO Spencer MP Surgical therapy for anorectal melanoma [外文期刊] 2003(2)5.Promtatvethi V;Gojaseni P;Buri P;Censarn N Malignant melanoma:a clinical experience in a Thai hospital 19786.Crombie IK Racial differences in melanoma incidence[外文期刊] 19797.Somran J;Kanngurn S;Porncharoenpong S;Lertkajornsin O Anorectal malignant melanoma:report of two cases from Buddhachinnaraj Hospital 20058.Pommer B;Probst A;Messmann H Gastric metastases from malignant melanoma 2008(z 2)9.Tanaka K;Toyoda H;Hamada Y;Aoki M Kosaka R Noda T Katsurahara M Nakamura M Ninomiya K Inoue H Imoto I Duodenal metastasis of malignant melanoma observed by magnification endoscopy[外文期刊] 2008(z 2)10.Galloro G;Inzirillo A;Magno L;Diamantis G Inzirillo M Pastore A Ruggiero S Mosella G Multiple nodular lesions by colonic metastatic malignant melanoma[外文期刊] 200911.Yang JI;Byun HJ;Kang JM Education and imaging.Gastrointestinal:anorectal malignant melanoma[外文期刊] 200912.Liang KV;Sanderson SO;Nowakowski GS;Arora AS Metastatic malignant melanoma of the gastrointestinal tract[外文期刊] 200613.Lens M;Bataille V;Krivokapic Z Melanoma of the small intestine[外文期刊] 2009(5)14.Berger AC;Buell JF;Venzon D;Baker AR Libutti SK Management of symptomatic malignant melanoma of the gastrointestinal tract[外文期刊] 199915.Agrawal S;Yao TJ;Coit DG Surgery for melanoma metastatic to the gastrointestinal tract[外文期刊] 199916.Ishizone S;Koide N;Karasawa F;Akita N Muranaka F Uhara H Miyagawa S Surgical treatment for anorectal malignant melanoma:report of five cases and review of 79 Japanese cases[外文期刊] 2008(12)17.Sanki A;Scolyer RA;Thompson JF Surgery for melanoma metastases of the gastrointestinal tract:indications and results [外文期刊] 2009(3)18.Huang YJ;Wu MH;Lin MT Multiple small-bowel intussusceptions caused by metastatic malignant melanoma 200819.Slaby J;Suri U Metastatic melanoma with multiple small bowel intussusceptions[外文期刊] 200920.Spitler LE;Grossbard ML;Ernstoff MS;Silver G Jacobs M Hayes FA Soong SJ Adjuvant therapy of stage III and IV malignant melanoma using granulocyte-macrophage colony-stimulating factor 2000本文链接:/Periodical_wjg201006013.aspx。
手术室心胸外科护理论文心胸外科手术作为风险性较高的手术,这种手术存在创伤大、术后并发症多、手术所用时间长等特征,容易引发肺不张、呼吸道感染等并发症,直接影响患者术后康复效果及正常生活[1]。
优质护理就是利用包干责任的方法对患者执行责任制护理,从基础护理入手,逐步提升护理质量,从而为心胸外科患者提供最优质的服务[2]。
本文以100例接受心胸外科手术患者展开研究,探究进行优质护理的效果,具体情况如下。
1资料与方法1.1一般资料:挑选我院2015年9月至2016年11月所收治的胸外科手术患者为对象(100例),采用随机分配法将其划分为2组,研究组与对照组均有50例。
研究组患者中包括男性26例,2女性4例,患者的年龄22~79岁,平均(59±6)岁;对照组中男性27例,女性23例,年龄24~78岁,平均(58±6)岁。
2组患者年龄、性别等资料差异无统计学意义,具有可比性(P>0.05)。
1.2方法:对照组给予常规护理,研究组患者接受优质护理,主要内容为:(1)心理护理:护理人员必须耐心与患者交流、沟通,向患者讲解我院心胸外科发展状况、医院环境等,帮助患者快速适应陌生的环境,及时消除患者内心的陌生感及不适感。
在担心治疗效果方面,临床护理人员可以将相似的成功治疗病例经历介绍给患者,将患者战胜疾病的信心激发出来外,护患进行交流环节,及时掌握患者的心理状态,明确患者的实际需求,并尽可能给予满足。
(2)基础护理:告知患者要食用高蛋白、高维生素且容易消化的食物,多食用新鲜的水果、蔬菜,遵循少食多餐的原则饮食,保证患者摄入所需的营养。
加之,有规律的饮食,也有利于患者养成良好的排便习惯,确保大便通畅。
(3)训练指导:因开胸手术存在一定的特殊性,术后极易发生一系列呼吸并发症。
因此,患者入院后,要接受一系列呼吸训练,主要内容如下:①缩唇呼吸法:指导患者用鼻子吸气,随之闭口,使用缩唇呼气,训练时间控制为3次/d,,每次时间约为15min。
胸外科护理论文范文一:胸外科手术病人的舒适护理舒适护理是使人在生理、心理、灵性、社会上达到最愉快的状态,或降低其不愉快的程度。
病人来院就诊,其需求重点不外乎是医疗服务的有效及舒适。
虽然医疗有效,但病人并不一定感到满意,反之,若在治疗过程中得到应有的尊重、关心、爱护及帮助,病人必然会觉得舒适,即使病情没有得到改善,也会觉得医疗服务的有效。
我院将舒适护理模式与整体护理相结合,运用于胸外科手术病人,使病人在接受治疗的同时,在护理人员协助下,达到一个人的身、心、社会、心灵的舒适状态。
1 临床资料随机抽取38例病人,年龄17-68岁,其中食管手术23例,肺癌5例,自发性气胸2例,贲门手术7例,纵隔肿瘤1例。
2 护理2.1 术前舒适护理2.1.1 创造舒适的环境完善的卫生淋浴,中央空调,热水供应等设施,利用壁橱、床头柜妥善放置病人生活用品,利用艺术壁挂装点美化病区,适宜的声响、光线、温湿度,使病区清洁、明亮、安静、舒适,饮食每日配餐员预定,开展点菜业务,饭菜、开水、药品送至床边,合理安排护理流程,减少清扫消毒工作与病人就餐、治疗时间的冲突。
病人感官受到良性刺激,有利于治疗。
2.1.2 营造良好的气氛重视服饰美及护理人员仪表风范,入院接待热情主动,作好入院宣教,帮助病人处理好同室病友关系,使病人从新人际关系中获得舒适感,并因受到重视、关怀,使不愉快的程度降到最低,从而对本次治疗充满信心。
2.1.3 做好心理干预提倡情感服务,面对面交流,灵活运用沟通技巧,因人而异讲解疾病有关知识,交代注意事项,评估心理状况,满足病人心理需求。
来自家庭、学校、工作单位等社会关系对病人的支持与关怀也可使病人减轻或消除精神压力。
2.1.4 饮食指导认真评估,指导合理进食,改善营养状况,提高对手术的耐受性。
2.1.5 练习肺功能和有效咳嗽向患者和家属说明开胸术后咳嗽排痰的目的和必要性,指导病人深呼吸,取半卧位或坐位,每日3次,每次10分钟,以增加肺活量,减少术后呼吸系统并发症的发生。


肺癌纵隔淋巴结转移与预后的关系分析来源:医学论文发表——创新医学网/ 作者:刘泗军,龙鸿川,阚奇伟,石勇作者单位:四川省眉山市人民医院胸心外科,四川眉山612100【摘要】目的:研究肺癌中不同形式的纵隔淋巴结转移与预后之间的关系。
方法:收集术后病检证实伴有纵隔淋巴结转移的肺癌病例56例,统计纵隔淋巴结的具体转移情况并分为:(1)隆突下淋巴结转移组与非隆突下淋巴结转移组;(2)跳跃式转移组与非跳跃式转移组;(3)1组淋巴结转移组、2组淋巴结转移组及3组淋巴结转移组。
比较各相应组的生存情况。
结果:隆突下淋巴结转移组与非隆突下淋巴结转移组的生存曲线比较,差异无统计学意义(P>0.05)。
跳跃式转移组生存情况较非跳跃式转移组差(P<0.05)。
纵膈淋巴结转移组数越多预后越差,尤其是伴有3组以上淋巴结转移的患者预后更差(P<0.01)。
结论:肺癌纵隔淋巴结的转移形式与预后相关,跳跃式转移及转移组数多的病例预后更差。
【关键词】肺癌;纵隔淋巴结;转移;预后Relationship between mediastinal lymph node metastasis and prognosis of lung cancerLIU Si jun, LONG Hong chuan, KAN Qi wei, SHI Yong(Department of Cardiothoracic Surgery, People′s Hospital in Meishan City, Meishan 612100, China)[ABSTRACT] Objective: To investigate the relationship between different forms of mediastinal lymph node metastasis and prognosis of lung cancer. Methods:Fifty six lung caner cases, with mediastinal lymph node metastasis confirmed by postoperative pathologic examination, were included. Made a comparison of survival of corresponding groups divided according to the forms of mediastinal lymph node metastasis, namely carinal lymph metastasis group and non carinal lymph metastasis group, skip metastasis group and non skip metastasis group and the groups according to the number of metastasis from 1 to 3. Rsults:Comparison of survival curves, between carinal lymph metastasis group and non carinal lymph metastasis group, showed no significant difference(P>0.05). Lifetime of skip metastasis group was significantly longer than non skip metastasis group(P<0.05). The more regional mediastinal lymph node metastasis, the worse the prognosis of lung cancer, especially prognosis of cases with three regional mediastinal lymph node metastasis was the worst(P<0.01). Conclusions: Forms of mediastinal lymph node metastasis relates with prognosis of lung cancer, prognosis of cases with skip metastasis or more regional lymph node metastasis is worse.[KEY WORDS] Lung cancer; Mediastinal lymph node; Metastasis; Proyhosis肺癌发病率逐年呈明显的增加趋势,其预后差,5年生存率低。
胸外科护士札记范文英文回答:As a nurse in the thoracic surgery department, I have encountered numerous cases and gained valuable experience. In this journal entry, I would like to share some of my observations and reflections.First and foremost, communication skills are crucial in providing effective care to thoracic surgery patients. Many of these patients may be anxious or in pain, and it is important for nurses to establish a rapport and provide reassurance. Clear and concise communication can help alleviate their fears and ensure they understand the treatment plan and post-operative instructions.Additionally, attention to detail is essential in thoracic surgery nursing. From pre-operative assessments to post-operative care, nurses must carefully monitor vital signs, drainage, and wound healing. Any deviation from theexpected progress should be promptly reported to the surgical team. Timely intervention can prevent complications and promote faster recovery.Furthermore, thoracic surgery patients often require specialized care, such as chest tube management and respiratory support. Nurses should be knowledgeable about the different types of chest tubes, their indications, and potential complications. Regular assessment of the drainage system and maintaining aseptic technique during dressing changes are crucial to prevent infections.In addition to technical skills, compassion and empathy are vital in thoracic surgery nursing. Patients undergoing thoracic surgery may experience significant pain, discomfort, and emotional distress. Nurses should provide adequate pain management, offer emotional support, and encourage patients to express their concerns and fears. A caring and empathetic approach can greatly enhance the patient's overall experience and facilitate their recovery.Lastly, teamwork plays a pivotal role in the thoracicsurgery department. Nurses collaborate closely with surgeons, anesthesiologists, respiratory therapists, and other healthcare professionals to provide comprehensive care. Effective communication, mutual respect, and a shared goal of patient-centered care are essential for achieving successful outcomes.In conclusion, working as a nurse in the thoracic surgery department has taught me the importance of communication, attention to detail, specialized knowledge, compassion, and teamwork. These skills are essential in providing high-quality care to thoracic surgery patients.中文回答:作为胸外科护士,我遇到了许多病例并积累了宝贵的经验。
胸外科患者术后UEX原因分析及导管管理胸外科患者以手术治疗为主,但手术创面大、危险系数高,术后为了促进伤口的愈合、进行营养治疗等,使患者术后常需要各种管道,包括:经鼻胃肠减压管、十二指肠营养管、颈部伤口引流管、胸腔引流管、纵隔引流管、腹部伤口引流管、胃造瘘管、空肠造瘘管、经鼻(口)气管插管、深静脉导管、尿管等。
根据患者病情不同,所携带的管道数量达到3-8根不等。
为了使患者治疗更安全,减少医生的抱怨,减轻患者的痛苦,作为护理人员应做出更好的护理质量指标和护理品质。
非计划拔管(unplanned extubation UEX)是指未经医护人员同意,患者将导管自行拔出,或其他原因(包括医护人员操作不当)造成的导管脱落,又称意外拔管【1】。
据文献报道【2-3】,UEX的发生率2.8%-20.6%,一旦发生UEX,可能对患者造成伤害,延长住院天数,增加费用甚至导致死亡【4】,尤其是高危导管,如气管插管、胃肠减压管、胸腔引流管等,是常见的严重的护理不良事件。
临床资料:我科从2012年8月至2013年9月手术共659人,非计划拔管40例,发生率5.01%。
其中男性34例,女性6例;年龄在46-76岁。
非计划拔管导管种类包括气管切开导管1例占3%,空肠造瘘管1例占2%,颈部伤口引流管2例占5%,胸部引流管5例占12%,颈内静脉导管9例占22%,鼻肠管2例5%,胃管19例合并鼻肠管7例占45%,气管插管1例占3%。
1 原因分析1.1胸外科患者术后非计划拔管的直接原因分析活动时管道滑脱14例占34%,患者自行拔管12例占29%,在睡眠中拔管2例占5%,因缝线脱落致管道滑脱2例占5%,因咳嗽致管道滑出2例占5%,患者烦躁时拔管1例占3%,患者误拔1例占3%,管道自行脱出1例占3%,因汗液渗透致管道固定不牢脱出1例占2%,患者活动牵拉使管道脱出1例占2%,因暴力牵拉使管道脱出1例占2%,擤鼻涕使管道脱出1例占2%,因护士操作不当致拔管1例占5%。
胸外科手术后医院获得性肺炎危险因素分析崔海峰【摘要】Objective To analyze the hospital-acquired pneumonia-relatedrisk factors in postthoracic surgery. Methods Selected 200 cases of thoracic surgery ambulatory surgery patients in our hospital from April 2013 to April 2015 admitted to the investigation of hospital-acquired pneumonia,and analyzed risk factors. Results Long-term heavy smoking history,postoperative wound pain significantly,emphysema,chronic bronchitis and a history of intubation/mechanical ventilation,as risk factors,OR values were 1.887,4.598,2.496,2.328,P< 0.05. Conclusion Seriesof risk factors for hospital-acquired pneumonia occurred after the induction of thoracic surgery at the expanded analysis,and targeted prevention,can reduce the incidence of adverse events,clinical safety significance of the safeguards significantly.%目的:探讨胸外科手术后引发医院获得性肺炎的相关危险因素。
临床与病理杂志J Clin Pathol Res2015, 35(1) 27收稿日期(Date of reception):2015–01–05通信作者(Corresponding author):王斌,Email: wenwunj@AME国际病例001 | 胸壁滑膜肉瘤:病例报告及文献综述Emna Braham 1, Slim Aloui 1, Samira Aouadi 2, Ikram Drira 2, Tarek Kilani 3, Faouzi El Mezni 1(1. Department of pathology, Abderrahmen Mami Hospital, Ariana, Tunisia; 2. Department of Pneumology, Abderrahmen Mami Hospital,Ariana, Tunisia; 3. Departmernt of Thoracic Surgery, Abderrahmen Mami Hospital, Ariana, Tunisia)[摘 要]滑膜肉瘤是一种恶性软组织肿瘤,多发生于青壮年的四肢。
然而,胸壁滑膜肉瘤则非常少见,文献中仅有数例报道。
一名57岁老年女性因胸痛就诊。
影像学检查发现,右胸壁肿瘤破坏了第8肋骨中部,胸肌和胸膜外脂肪出现不均匀增强信号表明其亦受到累及。
行胸壁切除术。
组织学和免疫组化结果显示滑膜肉瘤。
对患者进行辅助化疗,然而治疗过程中失访。
6个月后,患者再次就诊时发现,胸壁出现复发的巨大肿瘤。
[关键词]滑膜肉瘤;胸壁;外科;组织学·AME 科研时间专栏·专栏导读:AME Groups 旗下出版了Journal of Thoracic Disease (《胸部疾病杂志》)、Annals of Cardiothoracic Surgery(《心胸外科年鉴》)、Chinese Journal of Cancer Research (《中国癌症研究》)和Annals of Translational Medicine (《转化医学年鉴》)等近20本英文医学学术期刊。
胸外科规培生读书报告范文英文回答:Title: The Importance of Reading in Cardiothoracic Surgery Residency.Introduction:Reading is an essential component of medical education, particularly for surgical residents. In cardiothoracic surgery, staying abreast of the latest research and techniques is crucial for providing optimal patient care. This reading report aims to delve into the significance of reading in cardiothoracic surgery residency, exploring its benefits and providing guidance on effective reading strategies.Benefits of Reading:Enhanced Knowledge and Skills: Reading medicaljournals, textbooks, and articles allows residents to expand their knowledge base, stay informed about advancements in the field, and develop specialized expertise in cardiothoracic surgery.Improved Patient Care: By staying up-to-date with the latest research, residents can incorporate evidence-based practices into their patient care, resulting in better outcomes and improved patient safety.Increased Critical Thinking Skills: Critical reading involves analyzing and evaluating information, which strengthens residents' ability to make sound clinical judgments and engage in meaningful discussions with colleagues.Enhanced Communication Skills: Through reading, residents can develop their writing skills, improve their communication with patients and families, and enhance their ability to present medical information effectively.Preparation for Board Certification: Reading isessential for preparing for the board certification exams, which assess residents' knowledge and skills in cardiothoracic surgery.Effective Reading Strategies:Identify Needs: Determine the areas in which you need to enhance your knowledge or skills, and focus your reading efforts accordingly.Set Realistic Goals: Break down large reading assignments into smaller, manageable chunks to avoidfeeling overwhelmed.Utilize Multiple Resources: Utilize a variety of resources, including textbooks, journals, online repositories, and peer-reviewed articles, to gain a comprehensive understanding of topics.Active Reading: Engage in active reading by highlighting, note-taking, and summarizing key points to improve comprehension and retention.Discuss and Share: Share your readings with colleagues and engage in discussions to foster knowledge sharing and reinforce concepts.Conclusion:Reading is indispensable in cardiothoracic surgery residency. It provides residents with the knowledge, skills, and abilities necessary to deliver exceptional patient care, make evidence-based decisions, and excel in their careers. By adopting effective reading strategies, residents can maximize the benefits of this essential component ofmedical education.中文回答:胸外科规培医师读书报告。
优质护理服务在胸外科、肿瘤外科的实践与体会朱俊风【摘要】Objective : To explore of development " high quality nursing service demonstration project" activities in thoracic , tumor surgery practice and effect. Methods : Actions include, increase human resources, improve the responsibility of the position, implement the responsihility total - crop - shaving,formulate satisfaction questionnaire. While conducting regular quality inspection and satisfaction survey. Results : Create a " high quality nursing service demonstration ward" , improve the patient satisfaction and clinical nursing quality. Conclusion : High quality nursing service can improve nursing quality , improve patient satisfaction, strengthened the nurse sense of achievement and honor.%目的:探讨开展"优质护理服务示范工程"活动在胸外科、肿瘤外科的做法与效果.方法:采取的措施包括,加大人力资源配置,健全岗位职责,实行责任大包干,制定满意度调查表.同时开展定期质量检查和满意度调查.结果:创建"优质护理服务示范病房",提高了患者的满意度和临床护理质量.结论:优质护理服务可提高护理质量,提高患者满意度,增强了护士的成就感和荣誉感.【期刊名称】《护理实践与研究》【年(卷),期】2011(008)019【总页数】2页(P79-80)【关键词】优质护理服务;基础护理;护理质量【作者】朱俊风【作者单位】225200,江苏省扬州大学医学院附属扬州洪泉医院【正文语种】中文为了使护理服务更加贴近患者、贴近病房、贴近社会,提升护理形象,达到患者满意、社会满意、政府满意,还有护士满意、医师满意、医院满意的目标。