川崎病诊治专家共识
- 格式:docx
- 大小:16.01 KB
- 文档页数:4
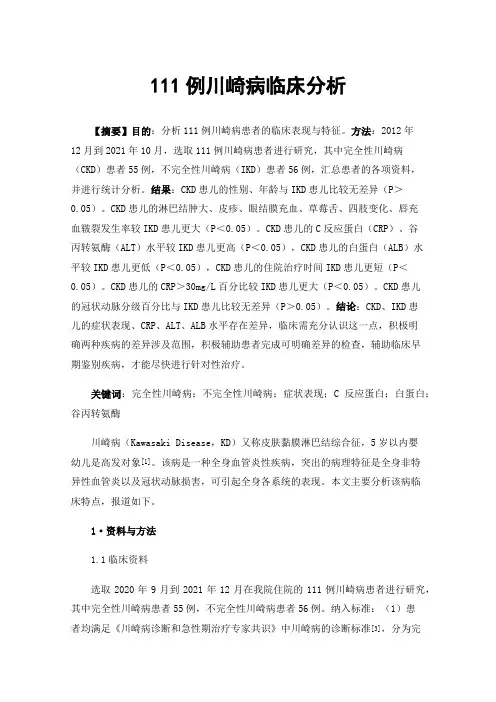
111例川崎病临床分析【摘要】目的:分析111例川崎病患者的临床表现与特征。
方法:2012年12月到2021年10月,选取111例川崎病患者进行研究,其中完全性川崎病(CKD)患者55例,不完全性川崎病(IKD)患者56例,汇总患者的各项资料,并进行统计分析。
结果:CKD患儿的性别、年龄与IKD患儿比较无差异(P>0.05)。
CKD患儿的淋巴结肿大、皮疹、眼结膜充血、草莓舌、四肢变化、唇充血皲裂发生率较IKD患儿更大(P<0.05)。
CKD患儿的C反应蛋白(CRP)、谷丙转氨酶(ALT)水平较IKD患儿更高(P<0.05),CKD患儿的白蛋白(ALB)水平较IKD患儿更低(P<0.05),CKD患儿的住院治疗时间IKD患儿更短(P<0.05)。
CKD患儿的CRP>30mg/L百分比较IKD患儿更大(P<0.05)。
CKD患儿的冠状动脉分级百分比与IKD患儿比较无差异(P>0.05)。
结论:CKD、IKD患儿的症状表现、CRP、ALT、ALB水平存在差异,临床需充分认识这一点,积极明确两种疾病的差异涉及范围,积极辅助患者完成可明确差异的检查,辅助临床早期鉴别疾病,才能尽快进行针对性治疗。
关键词:完全性川崎病;不完全性川崎病;症状表现;C反应蛋白;白蛋白;谷丙转氨酶川崎病(Kawasaki Disease,KD)又称皮肤黏膜淋巴结综合征,5岁以内婴幼儿是高发对象[1]。
该病是一种全身血管炎性疾病,突出的病理特征是全身非特异性血管炎以及冠状动脉损害,可引起全身各系统的表现。
本文主要分析该病临床特点,报道如下。
1·资料与方法1.1临床资料选取2020年9月到2021年12月在我院住院的111例川崎病患者进行研究,其中完全性川崎病患者55例,不完全性川崎病患者56例。
纳入标准:(1)患者均满足《川崎病诊断和急性期治疗专家共识》中川崎病的诊断标准[3],分为完全性川崎病(CKD)和不完全性川崎病(IKD)两种类型。
川崎病的诊断标准引言川崎病,又称混合性血管炎,是一种儿童常见的全身性疾病,起病急骤,可累及多个器官。
该病的早期诊断对预防并发症的发生至关重要。
本文将介绍川崎病的诊断标准和相关评估参数。
诊断标准川崎病的诊断标准通常基于国际儿科学会议上提出的川崎病诊断标准(The 5th Revised Indian and American Criteria)。
根据该标准,川崎病的诊断必须符合以下 5 个主要标准中的至少 4 个:1.持续发热:持续 5 天以上的高热(≥ 39℃),在使用抗生素治疗后热退或热型不符合抗生素反应。
2.蜜糖舌炎:舌黏膜出现鲜红的草莓状疹,伴随舌苔脱落。
3.双手掌红肿:双手掌红肿,可伴指甲剥脱;4.双脚足底红肿:双足足底红肿,足底可出现鲜红的草莓舌状疹;5.蜂窝组织炎:淋巴结炎性肿大,主要位于颈部区域。
在诊断川崎病时,如果孩子符合上述 4 个主要标准中的 3 个,但同时具备以下4 个附加标准中的至少 2 个,则也可被诊断为川崎病:1.口腔黏膜改变:咽炎、嘴唇炎、舌下疹等。
2.枕部淋巴结肿大:一侧或双侧颈部淋巴结肿大,直径大于 1.5 厘米。
3.皮疹:包括四肢上非特异性皮疹、躯干红斑或斑块,或是紫疹。
4.结膜炎:双侧结膜充血、结膜水肿、结膜红斑。
评估参数除了诊断标准,还有一些评估参数可以辅助川崎病的诊断和治疗:1.血液检查:包括白细胞计数、血清C反应蛋白(CRP)、血小板计数等。
这些指标在川崎病发病早期往往异常升高。
2.心肌炎标志物:心肌肌钙蛋白Ⅰ和肌钙蛋白T是诊断心肌炎的重要指标,其临床表现可能与川崎病相关。
3.心电图检查:心电图检查有助于评估心脏病变,例如冠状动脉或冠状动脉瘤形成。
4.足背动脉超声:足背动脉超声检查可用于早期评估年幼患者是否存在冠状动脉损害。
5.心脏超声:心脏超声检查是评估川崎病合并心血管并发症的首选方法,可以观察冠状动脉瘤、心功能降低等。
结论川崎病是一种全身性疾病,早期诊断对预防并发症的发生至关重要。

川崎病专题讨论会纪要《中华儿科杂志》编辑委员会中华医学会儿科学分会心血管学组中华医学会儿科学分会免疫学组川崎病(Kawasaki diseases,KD)是一种主要发生在5岁以下婴幼儿的急性发热出疹性疾病,属急性自限性血管炎综合征,其发病率有逐年增高趋势,在发达国家或地区,KD所致的冠状动脉病变(coronary artery lesions,CAL)已取代风湿热成为小儿最常见的后天性心脏病,并且可能成为成年后缺血性心脏病的危险因素之一。
KD病因及免疫发病机制仍未完全清楚,大量流行病学及临床观察提示KD可能是感染因素所致的急性免疫调节紊乱,遗传因素亦与KD发病相关。
已报道多种细菌、病毒、支原体及其代谢产物(如链球菌和葡萄球菌超抗原)等与KD发病有关,但目前仍未检测到致KD的单一病原微生物。
感染导致免疫活性细胞(如T细胞、单核/巨噬细胞)异常活化,所产生的细胞因子可能参与血管内皮损伤及干扰自身免疫耐受。
急性自限性血管炎症反应易导致冠状动脉病变,KD治疗的重点是尽快阻止促炎症细胞因子的产生和清除,降低炎症反应,预防和减轻冠状动脉病变。
《中华儿科杂志》编委会分别于2006年12月5日和2007年3月28日组织了川崎病专题讨论会,川崎病超声心动图诊断专题讨论会,儿科心血管和免疫的专家就KD的临床热点问题如不完全型(不典型)KD的诊断、IVIG无反应型(不敏感)KD处理等问题进行了十分热烈的讨论,现归纳如下。
一、KD诊断标准因缺乏特异诊断方法,KD的诊断主要靠临床表现,某些实验室检查可以协助临床诊断。
KD可分为典型和不典型两类。
1.典型KD:2002年日本川崎病研究组提出典型KD诊断标准,经第七届国际川崎病大会讨论通过后发表于Pediatrics International(2005)。
美国心脏病协会(AHA)亦提出典型KD诊断标准并发表于Pediatrics(2004)和Circulation(2004)上。
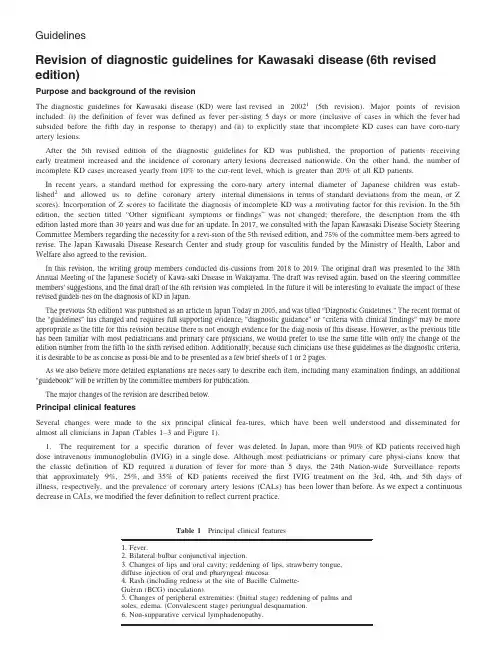
GuidelinesRevision of diagnostic guidelines for Kawasaki disease(6th revised edition)Purpose and background of the revisionThe diagnostic guidelines for Kawasaki disease(KD)were last revised in20021(5th revision).Major points of revision included:(i)the definition of fever was defined as fever per-sisting5days or more(inclusive of cases in which the fever had subsided before the fifth day in response to therapy)and(ii)to explicitly state that incomplete KD cases can have coro-nary artery lesions.After the5th revised edition of the diagnostic guidelines for KD was published,the proportion of patients receiving early treatment increased and the incidence of coronary artery lesions decreased nationwide.On the other hand,the number of incomplete KD cases increased yearly from10%to the cur-rent level,which is greater than20%of all KD patients.In recent years,a standard method for expressing the coro-nary artery internal diameter of Japanese children was estab-lished2and allowed us to define coronary artery internal dimensions in terms of standard deviations from the mean,or Z scores).Incorporation of Z scores to facilitate the diagnosis of incomplete KD was a motivating factor for this revision.In the5th edition,the section titled“Other significant symptoms or findings”was not changed;therefore,the description from the4th edition lasted more than 30 years and was due for an update. In 2017, we consulted with the Japan Kawasaki Disease Society Steering Committee Members regarding the necessity for a revi-sion of the 5th revised edition, and 75% of the committee mem-bers agreed torevise. The Japan Kawasaki Disease Research Center and study group for vasculitis funded by the Ministry of Health, Labor and Welfare also agreed to the revision.In this revision, the writing group members conducted dis-cussions from 2018 to 2019. The original draft was presented to the 38th Annual Meeting of the Japanese Society of Kawa-saki Disease in Wakayama. The draft was revised again, based on the steering committee members’ suggestions, and the final draft of the 6th revision was completed. In the future it will be interesting to evaluate the impact of these revised guideli-nes on the diagnosis of KD in Japan.The previous 5th edition1 was published as an article in Japan Today in 2005, and was titled “Diagnostic Guidelines.” The recent format of the “guidelines” has changed and requires full supporting evidence; “diagnostic guidance” or “criteria with clinical findings” may be more appropriate as the title for this revision because there is not enough evidence for the diag-nosis of this disease. However, as the previous title has been familiar with most pediatricians and primary care physicians, we would prefer to use the same title with only the change of the edition number from the fifth to the sixth revised edition. Additionally, because such clinicians use these guidelines as the diagnostic criteria, it is desirable to be as concise as possi-ble and to be presented as a few brief sheets of 1 or 2 pages.As we also believe more detailed explanations are neces-sary to describe each item, including many examination findings, an additional “guidebook” will be written by the committee members for publication.The major changes of the revision are described below.Principal clinical featuresSeveral changes were made to the six principal clinical fea-tures,which have been well understood and disseminated for almost all clinicians in Japan(Tables1–3and Figure1).1.The requirement for a specific duration of fever was deleted.In Japan,more than90%of KD patients received high dose intravenous immunoglobulin(IVIG)in a single dose.Although most pediatricians or primary care physi-cians know that the classic definition of KD required a duration of fever for more than5days,the24th Nation-wide Surveillance reports that approximately9%,25%,and35%of KD patients received the first IVIG treatment on the3rd,4th,and5th days of illness,respectively,and the prevalence of coronary artery lesions(CAL s)has been lower than before. As we expect a continuous decrease in CALs, we modified the fever definition to reflect current practice.Table1Principal clinical features1.Fever.2.Bilateral bulbar conjunctival injection.3.Changes of lips and oral cavity:reddening of lips,strawberry tongue,diffuse injection of oral and pharyngeal mucosa.4.Rash(including redness at the site of Bacille Calmette-Gu e rin(BCG)inoculation).5.Changes of peripheral extremities:(Initial stage)reddening of palms andsoles,edema.(Convalescent stage)periungual desquamation.6.Non-supparative cervical lymphadenopathy.Table 2Definition of complete or incomplete KDNumber of principalclinical featuresCoronary artery abnormalities (+)Coronary artery abnormalities (À)6Complete (a)Complete (a)5Complete (a)Complete (a)4Complete (b)Incomplete (d)3Incomplete (c)Incomplete (d)Table 3 Other significant demographic, clinical, echocardio-graphic, and laboratory features1. Kawasaki disease may be suspected in the presence of fewer than four principal clinical features when the following findings are observed:•Elevation of hepatic transaminases early in the course of the disease.•Increased leukocytes in the urine sediment of an infant.•Thrombocytosis in the convalescent phase •Elevation of BNP or NT-pro BNP •Mitral valve regurgitation or pericardial effusion by echocardiography •Enlargement of the gallbladder (hydrops of gallbladder)•Hypoalbuminemia or hyponatremia2. If a KD patient manifests the following findings, the patient should be considered for admission of a critical care unit.•Hemodynamically significant myocarditis •Hypotention (shock)•Paralytic ileus •Decreased level of consciousness3. Risk scores to predict intravenous immunoglobulin resistance may be applied to guide patient management. The following features are elements of the risk scores for predicting intravenous immunoglobulin resistance.•Leukocytosis with left shift •thrombocytopenia •hypoalbuminemia •hyponatremia •hyperbilirubinemia (jaundice)•elevation of CRP •Age <1year4. Other non-specific findings which may be observed in Kawasaki Disease and should not exclude the diagnosis.•Irritability •Cardiovascular: abnormal extra heart sounds, electrocardio-gram changes, aneurysm of peripheral arteries other than coronary (axillary etc.),•Gastrointestinal: abdominal pain, vomiting, diarrhea •Hematologic: increased erythrocyte sedimentation rate, ane-mia •Dermatologic: micropustular rash, transverse grooves across the finger nails.•Respiratory: cough, rhinorrhea, retropharyngeal edema, infiltrate on chest radiograph.•Rheumatologic: pain, swelling.•Neurologic: cerebrospinal fluid pleocytosis, seizures, facial nerve palsy, paralysis of the extremities.BNP, brain natriuretic protein; KD, Kawasaki disease; NT-pro BNP, N terminal pro-brain natriuretic protein.1.Mortality in the acute phase: <0.1%.2.Recurrence rate: 3–4%; proportion of siblings’ cases, 1–2%.3.Nonsuppurative cervical lymphadenopathy (multiple hypoe-choic, enlarged nodes observed on ultrasound) is less fre-quently encountered (approximately 65%) compared with other principal clinical features during the acute phase. Non-suppurative cervical lymphadenopathy is observed in approxi-mately 90% of older children and often can be the firstclinical feature of KD with fever.To diagnose complete or incomplete KD, the exclusion of other febrile illnesses is essential.a: A patient who fulfills the criteria with five or six signs is diagnosed as complete KD.b: A patient who fulfills the criteria with four signs and coro-nary artery abnormality by echocardiography (Figure 1-h) is diag-nosed with complete KD.c: A patient who has three principal clinical features with coro-nary artery abnormality by echocardiography (Figure 1-h) and in whom other febrile illnesses have been excluded fulfills the crite-ria in “c.”d: When the patients who fulfill three or four signs in the the principle clinical features without coronary artery dilation but with some features from the list of ‘Other significant clinical fea-tures’ can be diagnosed as incomplete KD, if other diseases are ruled out.e: Incomplete KD may also be considered in the presence of only one or two principal clinical features after excluding other diagnoses.2. The clinical feature of “Polymorphous exanthema” was changed to “Rash” and now includes “redness at the site of Bacille Calmette-Gu e rin (BCG) inoculation”. Japanese pediatricians have recognized that redness at the site of BCG inoculation is a specific clinical sign that appears at the onset of KD. In the present revision, we included redness at the site of BCG inoculation as a clinical feature that counts as “rash,” even in the absence of more diffuse dermatologic changes.In particular, this sign is observed in more than 70% of the patients whose ages are from 6 to 20 months old3. When the patient do not show polymorphous exanthema but shows the redness of BCG scar and other 4 principle sign, that patient can be diagnosed as not incomplete KD, but (com-plete) KD. The impact of this change to the principal diagnostic clini-cal features will require further study and should be moni-tored.a bc de fg hFig.1(a)Bulbar conjunctival injection;(b)reddening of lips,strawberry tongue;(c)rash;(d)redness at the site of Bacille Calmette-Gu e rin (BCG)inoculation;(e)reddening of palms with edema;(f)periungual desquamation;(g)non-supparative cervical lymphadenopa-thy;(h)Echocardiographic finding of coronary artery aneurysm.3.Non-suppurative cervical lymphadenopathy(multiple hypoechoic,enlarged nodes observed by ultrasound)is lessfrequently encountered(approximately65%)than other principal clinical features during the acute phase.Nonsuppurative cervical lymphadenopathy is observed in approximately90%of older children and often can be the first clinical feature of KD with fever.This phenomenon is described as“Remark”1at the last part.4.The precise clinical definitions of complete and incom-plete KD are now clearly delineated as outlined in the appendixand are based on the number of principal clini-cal features and the presence of coronary artery abnormalities.A patient who fulfills the criteria in“a”or“b”is diagnosed as complete KD.A patient who has three prin-cipal clinical features with coronary artery abnormality by echocardiography and in whom other febrile illnesses have been excluded fulfills the criteria in“c”and is diag-nosed as incomplete KD.Patients who fulfill the criteria in“d”are also diagnosed as incomplete Kawasaki disease defined as the presence of three or four principal clinical features without coronary artery dilation but with features from the list of“Other significant clinical features”.Incomplete Kawasaki disease may also be considered in the presence of only one or two principal clinical features after very careful,sufficient observation and excluding other diagnoses.For these patients,particularly careful consideration of the differential diagnosis is essential.For reference,in the24th nationwide survey,0.7%and 5.4%of all KD patients were reported as incomplete KD with only one or two clinical features,respectively.However,the possibilities of other disease are higher than for incomplete KD,if the coronary artery is not involved and the principal signs are limited to less than two.Evaluation of the coronary arteries using Z scoresThe revised guidelines recommend the use of Z scores for defining coronary artery dilation.When Z-score of internal coronary artery diameter≥2.5SD units,it is defined as coro-nary artery dilation.However,in case that the examiner has a difficulty to use Z score, conventional criteria using traditional measurements of inner diameter≥3mm(<5years old)or≥4mm(≥5years old)can be used for the diagnosis of coronary artery dilation.While Z scores are a more quantitative assess-ment,we realize that they have not been adopted by all centers in Japan.This change of definition may affect the incidence of coronary artery dilation,especially transient dilation and small aneurysm.Assessment of the impact of this change will there-fore be important in future epidemiologic surveys. Other significant demographic,clinical,echocardiographic,and laboratory featuresIn this section,we substantially revised the description of specific clinical features that can be associated with KD.1.Seven clinical features are described that may be helpful in the recognition of incomplete KD cases.We hope that futureclinical research will provide more accurate diag-nostic tools including the optimum cut-off values for these variables.Although it is expected that the quantitative cut-off values of all findings in these items will be deter-mined,there have been very few Japanese studies of suffi-cient quality.In the future,an algorithm using such cut-off values is expected to be constructed.2.Clinical findings that warrant referral to a tertiary medical center with experience in treating critically ill pediatric patientsare outlined.3.Risk scores to predict intravenous immunoglobulin resis-tance may be applied to guide patient management.We definedseven features that are elements of risk scores pre-dicting intravenous immunoglobulin resistance.These fea-tures may be useful in risk stratification of patients.4.Other non-specific findings that may be observed in KD and should not exclude the diagnosis have been added.Theseeight features may support the diagnosis of KD.This summary describes the major changes to the6th revised edition of the KD diagnostic guidelines.We hope that this revision will lead to standardization of the definition of incomplete KD and diagnostic approaches,and will further reduce number of coronary artery lesions suffered by KD patients.。
2022年ACR/VF川崎病管理指南(全文)川崎病(KD)又称皮肤黏膜淋巴结综合征,1967年由日本川崎富作医生首次报道。
2022年4月,美国风湿病学会(ACR )和血管炎基金会(VF)发布了川崎病(KD )的管理指南,包括诊断、治疗和管理,并更侧重于为临床诊疗过程中遇到的问题提供治疗建议。
本次2022年ACR年会上,美国华盛顿特区国家儿童医院风湿科主任Sangeeta Sule 教授以02021 ACR/VF Kawasaki Disease GUidelineS〃为题,分享ACR与VF共同制定的2021年版川崎盛KD )指南1, Karen James 博士以n CIinicaI Scenarios: Practical application of the 2021 American College of Rheumatology/ Vasculitis Foundation Kawasaki Disease Guidelines”为题,结合临床病例探讨了该指南的实际应用场景2OKD的诊断KD的诊断主要依靠临床表现并结合实验室检查,并排除其他疾病。
KD 包括完全性KD和不完全性KD两种类型,急性KD定义为KD 发热初期。
完全性KD不明原因的发热≥5d ,且具有以下5项中至少4项主要临床特征:1 )非渗出性双眼球结膜充血2 )口唇及口腔变化:口唇干红、皴裂,草莓舌,口咽部黏膜弥漫性充血3)四肢末梢改变:急性期手足发红、肿胀,恢复期甲周脱皮4)皮疹,常见弥漫性斑丘疹、猩红热样或多形红斑样皮疹,还包括单独出现的卡疤红肿5 )非化脓性颈部淋巴结肿大(至少1个淋巴结直径>1.5Cm ),通常为单侧不完全性KD不明原因的发热N 5d ,但上述主要临床特征不足4项的患儿按图1 流程评估。
诊断性影像学1 )对于疑似不完全性KD 和发热的儿童,强烈建议进行冠状动脉超声 心动图检查。
与典型KD 患者相比,不完全性KD 患者的冠状动脉病变风险增加。
川崎病治疗方案川崎病,也被称为Mucocutaneous Lymph Node Syndrome(黏膜淋巴结综合征),是一种儿童常见的急性全身性血管炎疾病。
该疾病最常发生在儿童年龄段,尤其是在5岁以下的儿童中。
川崎病病因尚不明确,但早期诊断和及时治疗非常关键,以避免出现严重并发症,特别是对心脏的影响。
目前,川崎病的治疗主要侧重于控制病情、减轻炎症反应,并防止并发症的发生。
以下是常用的川崎病治疗方案:1. 高剂量免疫球蛋白(IVIG)治疗:IVIG是目前最主要的川崎病治疗药物之一。
通常以2g/kg剂量通过静脉注射给药,疗程为单次给药。
IVIG的主要作用是降低体内炎症反应,减轻血管壁炎症,并预防冠状动脉病变的发生。
该药物常与其他治疗手段结合使用,以取得更好的治疗效果。
2. 高剂量阿司匹林治疗:阿司匹林通常在IVIG治疗后开始使用,剂量为80-100mg/kg/日分次服用。
该药物主要通过抗炎和抗血小板聚集作用,减轻川崎病患儿的症状,降低冠状动脉病变的风险。
在恢复期,剂量逐渐减少,以防止副作用,但需根据患儿体重和临床情况进行调整。
3. 丙种球蛋白治疗:对于IVIG无效或临床症状持续存在的患儿,丙种球蛋白治疗是一种备选方案。
通常以1-2g/kg剂量通过静脉注射给药,疗程可根据疾病进展进行调整。
丙种球蛋白可中和体内炎症介质,改善病情,预防并发症。
4. 其他治疗措施:除上述主要治疗方案外,川崎病患儿还可以接受其他治疗措施,如局部皮肤护理、镇痛药物、降温措施等,以缓解疾病症状和不适。
川崎病的治疗过程中,以下几点需要注意:1. 早期诊断和治疗:川崎病的症状与其他感染性疾病相似,因此早期诊断非常重要。
一旦怀疑川崎病,应立即就诊,并尽早启动治疗以避免并发症的发生。
2. 专业医生的指导:治疗川崎病应由经验丰富的小儿科医生或专科医生进行指导。
他们可以根据患儿年龄、病情严重程度和其他相关因素,制定个体化的治疗方案。
3. 长期随访和监测:川崎病的治疗通常需要长期随访和监测,以确保患儿的病情得到有效控制,并及时发现并预防任何可能的后遗症,尤其是对心脏的影响。
川崎病专题讨论会纪要《中华儿科朵忐》编辑委员会中华医学会儿科学分会心血管学组中华医学会儿科学分会免疫学组川崎^(Kawasaki diseases,KD)就是一种主要发生在5岁以下婴幼儿得急性发热出疹性疾病祸急性自限件血管炎综合征,其发病率有逐年増岛趋势准发达国家或地区,KD所致得冠状动脉病变(coronary artery lesions,CAL)已取代风湿热成为小儿最常见得后天性心脏病,并且可能成为成年后缺血性心脏病得危险因素之一・KD病因及免疫发筋机制仍未完全晴楚,大虽流行病学及临床观察提示KD可能就是感染因素所致得急性免疫调节紊乱,遗传因素亦与KD发病相关。
已报道釣中细菌、病瓠支原体及其代谢产物(如链球菌与葡萄球菌超抗廉)等与KD发病有关,但目前仍未检测到致KD得,丫i一病原微生物°感染导致免疫活性细胞(如T细胞.的核/巨噬细胞)异常活化,所产生得細胞因子可能参与血管内皮损伤及干扰自身免疫耐受。
急性自限性血管炎症反应易导致冠状动脉病变,KD治疗得重点就是尽快阻止促炎症细胞因子得产生与淸除,降低炎症反应,预防与减轻冠状动脉橋变。
《中华儿科朵志》編委会分别于2006年12月5日与2007年3月28日组织了川崎病专题讨论会丿1|崎病超声心动图诊断专题讨论会JL科心血管与免疫得专家就KD得临床热点问题如不完全型(不典型)KD得诊断、IVIG 无反应型(不敏感)KD处理尊问题进彳亍了十分热烈得讨论,现归纳如下。
一、KD诊断标准因缺乏特界诊断方法,KD得诊I析主要靠临床表现,某些实验室检查可以协助临床诊断° KD可分为典型与不典型两类。
1•典型KD:2002年日木川崎病研尤组提出典型KD诊断标准,经第七屈国际川崎病大会讨论通过后发表于Pediatrics International(2005). 国心脏病协会(AHA)亦提出典型KD诊断标准并发表于Pediatrlcs(2004) 与Circulation(2004)±o与会代表认为日木与英国得典型KD诊断标准大致相同,但有一些微小差界:日本标准将发热与其她5项主要临床表现整合在一起,而美国标准则将发热单列为必备诊断条件;日本标准认为具备6项主要临床表现中4项,超声心动图发现冠状动脉瘤或冠状动脉扩张者亦可诊断典型KD,而美国标准则认为如果具备除发热以外得4项主要临床表现,发热4(1时亦可明确典型KD诊断。
与会专家认为不具发热表现得KD患儿比例极低,北京KD流行病学调査结果仅有0、3%患儿无发热」対此提岀我国典型KD诊斷建议:发热5 d或以上(部分病例受治疗干扰发热可不足5d),具有以下5项中得4项者:双侧球结膜充血、口唇及口腔黏膜发红、肢端改变(急性期表现为肿胀,恢复期表现为脱屑)、皮疹与非化脓性颈淋巴结肿大即可确诊为KD。
如具备除发热以外3项表现并证实冇冠状动脉瘤或冠状动脉扩张者,亦可诊断典型KD。
须强调任何KD诊断标准并非特异,一定耍除外引起各项临床表现得其她疾病。
还应注意,各项临床表现并非同时出现,应动态观察,以助诊断。
2•不完全型KD:约10%患儿(尤其就是婴儿)为不完全型KD:该型名称混乱,有不典型KD.不完全型KD 与延迟诊断性KD等。
不典型KD尤抬具有少见临床表现者(如无菌性脑膜炎、肾脏受累等),延迟诊断世KD 就是抬各项诊断指标先后于10d左右才表现出來」刘而延迟了诊断。
与会代表认为我国宜采用、、不完全型KD"这一统一名称•不完全型KD并非轻型KD,其冠状动脉受累风险与实验室检査结果与典型KD类似」刘此不完全型KD诊断就是木次会议讨论得焦点间題之一。
与会专家强调尤应注总卡介苗接种处红斑、碘结、前葡萄膜炎、胆套肿大、恢复期肛周脱屑等重要表现以助诊断。
脑利钠肽上升可作为KD诊断得参考指标。
年龄小于6个丿咸•儿,KD表现更不典型,与会专家一致建议参考芙国心脏病协会标准,即:发热持续不退,排除其她疾病,实验室检査有炎症反应证据存在(红细胞沉降率与c反应蛋白明显升高),虽无KD临床表现,应反复超声心动图检査,以了解有无冠状动脉损伤。
一旦发现明确宛状动脉病变,可诊断不完全型KD并采用标准治疗方案.然而对于年龄大于6个丿]患儿,发热5d或以上,需具备几项KD主要临床表现才疑诊KD尚有争议。
标准设置过严,可能导致部分患儿漏诊或延迟诊断,错失IVIG治疗最佳时机;诊断标准过松,则可能导致过度诊断与过度治疗。
经充分讨沦最后建议:除发热5 d或以I:外,应具有至少2项KD主要临床表现,并具备炎症反应抬标明显升臥在除外其她疾病时,可疑珍不完全型KD:应复育超声心动I轧监测冠状动脉与其她心脏改变,如出现冠状动脉病变者可确诊■并及时使用标准治疗方案,如无冠状动脉病变,建议暂不使用IVIGc如发热持续又不满足超声心动图与实验室抬标者,应除外其她疾病,包括病讶感染、猩红热、術萄球菌烫伤样综合征、中毒休克综合征、细菌性颈淋巴结炎、药物过敏、Stevens-Johnson综合征与全身型幼年特发性关节炎引起得类似临床表现等。
二、KD其她表现与实验室检査KD除6条主要临床表现外,还会出现以下症状与体征:1•心血管系统何以表现心肌炎、心包炎及心内膜炎,听诊可有心脏余音、奔马律或心音低钝,心电图检査可以有P・R. Q・T间期延长、界常Q波、QRS低电压.ST・T波改变或心律失常;胸部X线检査可有心影增大; 超声心动图除冠状动脉改变外,还可见心包枳液、二尖瓣反流等。
血管造影检査可见体循环动脉瘤(发生率约0. 8%)。
2•非心血管系统:消化系统:腹泻.呕吐、腹痛.胆囊肿大、麻痹性肠梗阻、轻度黄疸、血清转氨酶值上升; 血液系统:白血球讣数増多伴核左移、血小板增蚩(病程7d后人红细胞沉降率加快.C反应蛋白升商、低白蛋白血症、血脂片常(血清舟密度脂蛋白与胆固酹水平下降)、轻度贫血等;泌尿系统:泌尿道感染、蛋白尿.沉渣中白血球增多;呼吸系统:咳嗽.流涕、肺野出现界常阴影;神经系统:无菌性脑膜炎、惊臥意识障碍.面神经麻痹.四肢瘫.听神经障碍,个别患儿在恢复期可以岀现颅内出血;骨胳肌肉系统咲节炎.关节与(或)肌肉疼痛、肿胀。
KD得其她表现虽不能作为确诊得依据,但可以协助临床诊断,尤其就是实验室检査中得红细胞沉降率明显増快、CRP iyjW.升隊血小板增女(3岁以下得男孩,ESR. CRP、PLT升岛就是冠状动脉病变得商危因素)等。
三. KD得超声心动图诊断心血管系统并发症以冠状动脉病变巌常见,往往就是KD致死或致残得主要原坎In未经IVIG治疗患儿冠状动脉病变发生率达20%〜25%,正规IVIG治疗后降至5%左右。
KD急性期冠状动脉病变往往发生在冠状动脉近端,二维超声心动图检查容易发现,另外,超声心动图还可以检测心功能、瓣膜反流及心包积液°因此超声心动图对KD得诊断、病悄估测及治疗选择均显重要,所Y J KD患儿均应进行超肃心动图检金。
超術心动图检査应使用频率较高(5〜7、5MHZ)得探头,以提岛图像分辨率朋加冠状动脉病变检测得可靠性。
冠状动脉超声心动图检查H常分为冠状动脉扩张(coronary artery ectasia).狭窄与冠状动脉瘤(coronary artery aneurysm,CAA):冠状动脉病变发生频率依次为左冠状动脉前降支、右甩状动脉近端.左冠状动脉近端、左冠状动脉回旋支及右冠状动脉远段超声心动图检査应在胸骨旁.心尖部、剑下及胸骨上窝部位多种切面探查冠状动脉得幹段(冠状动脉左主干、回旋支、前降支及右冠状动脉近.中.远段)。
观察冠状动脉扩张部位及程度,冠状动脉瘤数目、部位、大小及形状。
测址舒张期冠状动脉内径,即血管内缘至内缘得距离,应避免在分支处测量°由于小儿冠状动脉内径得正常范困目前尚不统一,冠状动脉病变得诊断标准不一致。
从前主要采用日木川崎橋研尤组提岀得冠状动脉病变诊断标准,即小于5岁儿童冠状动脉内径>3 mm;5岁或5岁以上者>4mm; 冠状动脉局部内径较邻近处明显扩大,大于或等于1. 5倍.近年來已有一些报道用休表面积校正得左、右冠状动脉内空正常值°关国de Zorzi等提出冠状动脉内径z 值艺2、5为冠状动脉扩张。
日木Kurotobi等及新加坡Tan等均提岀冠状动脉内径Z值>2. 0为冠状动脉扩勲日木及新加坡学者提岀体表面积校正得冠状动脉内径正常值略低干茨国得资料,可能比较接近中国儿童。
我国目前仅有用年龄校正得冠状动脉正常值标准,该正常值得样木虽小(188名正常儿童),且提出年代早°中国儿童得体表面积校正冠状动脉正常范用需要重新建立。
已有研处证明尿用日木川崎橋研处组得冠状动脉病变诊断标准会低估川崎柄冠状动脉病变得发生率° Tan等报道得资料中,正常冠状动脉内径与主动脉瓣环内径比值范围较窄丄CA/AoA=0、15±0. 02(0、09〜th 21),RCA/AoA=0. 13±0. 02(0. 09〜0、20),比值与年龄.性别、身高.体里及体表面积无关,也可作为评价冠状动脉扩张得参考。
冠状动脉瘤指冠状动脉扩张段内径与相邻段内径比值超过1、5,且内径超过4mm。
冠状动脉内径v5mm 为小型CAA,5〜8 mm之间为中等CAA, >8 mm为巨大CAA。
中等以上冠状动脉瘤应注慰瘤内有无血栓形成。
在检査冠状动脉得过程中还要注意:观察左室功能.痂膜反流及心包积液情况。
冠状动脉扩张或CAA就是KD冠状动脉并发症得主要客观依据,近來有学者提出尅状动脉壁挥度(回声)增咏血管内壁不光滑就是KD血管或血管周鬧炎得表现,尤其就是对缺乏冠状动脉扩张或冠状动脉瘤得KD诊断有参考意义,临床应提尚警惕•对患儿加强随诊。
左室室壁节段运动只常、主动脉根部扩张、心功能减低、新出现得二尖瓣反流、心包积液对KD诊断也有帮助。
除冠状动脉以外,少数患儿可并发体循环动脉瘤,体循环动脉瘤以腋动脉瘤最常见,发生率0. 8%〜2. 2%。
其她依次为股动脉.肠系膜上动脉、肾动脉cKD冠状动脉病变呈动态发展过程,可从发病第5天开始,对怀疑KD者应尽早进行超声心动图检査作为参考基础。
建议于病程第2、4>8周复査超声心动图。
对合并持续岛如冠状动脉瘤、心功能减低、瓣膜反流及中虽:以上心包积液病例,可増加检査次数,严密观察,以抬导治疗。
研究发现4〜8周超声心动图显示冠状动脉正常者」年复査再次发现冠状动脉改变得可能性极小,但有专家建议有条件者1年还应复査超声心动图。
超声心动图对诊断冠状动脉远端病变及狭窄有局限性,选择性冠状动脉造影仍然就是其最准确得诊断方法。
近來有学者报道藝层螺旋CT冠状动脉造影、磁共振冠状动脉造影等新技术可以无创检测冠状动脉远段及狭窄病变。