18类常用抢救药品
- 格式:ppt
- 大小:207.50 KB
- 文档页数:58
急诊科18类常用抢救药品:18类常用抢救药品(急诊科专用)一、中枢神经兴奋药尼可刹米(可拉明)[药理及应用]直接兴奋延髓呼吸中枢,使呼吸加深加快。
对血管运动中枢也有微弱兴奋作用。
用于中枢性呼吸抑制及循环衰竭、麻醉药及其它中枢抑制药的中毒。
[用法]常用量:肌注或静注,0.25~0.5g/次,必要时1~2小时重复。
极量:1.25g/次。
[注意]大剂量可引起血压升高、心悸、出汗、呕吐、心律失常、震颤及惊厥。
山梗菜碱(洛贝林)[药理及应用]兴奋颈动脉体化学感受器而反射性兴奋呼吸中枢。
用于新生儿窒息、吸入麻醉药及其它中枢抑制药的中毒,一氧化碳中毒以及肺炎引起的呼吸衰竭。
[用法]常用量:肌注或静注,3mg/次,必要时半小时重复。
极量20mg/日。
[注意]不良反应有恶心、呕吐、腹泻、头痛、眩晕;大剂量可引起心动过速、呼吸抑制、血压下降、甚至惊厥。
二、抗休克血管活性药多巴胺[药理及应用]直接激动α和β受体,也激动多巴胺受体,对不同受体的作用与剂量有关:小剂量(2~5μg/kg?min)低速滴注时,兴奋多巴胺受体,使肾、肠系膜、冠状动脉及脑血管扩张,增加血流量及尿量。
同时激动心脏的β1受体,也通过释放去甲肾上腺素产生中等程序的正性肌力作用;中等剂量(5~10μg/kg?min)时,可明显激动β1受体而兴奋心脏,加强心肌收缩力。
同时也激动α受体,使皮肤、黏膜等外周血管收缩。
大剂量(>10μg /kg?min)时,正性肌力和血管收缩作用更明显,肾血管扩张作用消失。
在中、小剂量的抗休克治疗中正性肌力和肾血管扩张作用占优势。
用于各种类型休克,特别对伴有肾功能不全、心排出量降低、周围血管阻力增高而已补足血容量的患者更有意义。
[用法]常用量:静滴,20mg/次加入5%葡萄糖250ml中,开始以20滴/分,根据需要调整滴速,最大不超过0.5mg/分。
[注意]1.不良反应有恶心、呕吐、头痛、中枢神经系统兴奋等;大剂量或过量时可使呼吸加速、快速型心律失常。
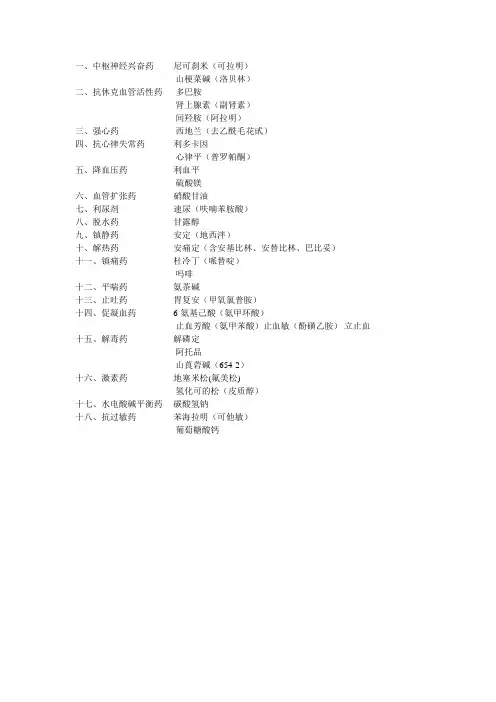
一、中枢神经兴奋药尼可刹米(可拉明)
山梗菜碱(洛贝林)
二、抗休克血管活性药多巴胺
肾上腺素(副肾素)
间羟胺(阿拉明)
三、强心药西地兰(去乙酰毛花甙)
四、抗心律失常药利多卡因
心律平(普罗帕酮)
五、降血压药利血平
硫酸镁
六、血管扩张药硝酸甘油
七、利尿剂速尿(呋喃苯胺酸)
八、脱水药甘露醇
九、镇静药安定(地西泮)
十、解热药安痛定(含安基比林、安替比林、巴比妥)
十一、镇痛药杜冷丁(哌替啶)
吗啡
十二、平喘药氨茶碱
十三、止吐药胃复安(甲氧氯普胺)
十四、促凝血药6-氨基己酸(氨甲环酸)
止血芳酸(氨甲苯酸)止血敏(酚磺乙胺)立止血十五、解毒药解磷定
阿托品
山莨菪碱(654-2)
十六、激素药地塞米松(氟美松)
氢化可的松(皮质醇)
十七、水电酸碱平衡药碳酸氢钠
十八、抗过敏药苯海拉明(可他敏)
葡萄糖酸钙。
常备急救药品急救药品的管理与使用要科学而又分秒必争。
力求准确、迅速、及时。
本文作用就病区抢救车上急救药品的贮存与保管中应注意的事项作一阐述,并按急救药品的药理分类对每一类急救药品中的常用药品在临床应用时的常见问题进行分析,下面是店铺为大家整理的常备急救药品相关资料,供大家参考!常备急救药品1、尼可刹米:剂量:0.375g 。
作用及用途:为最常见的呼吸兴奋剂,使呼吸加快加深,提高呼吸中枢对二氧化碳的敏感性,用于各种原因引起的中枢性呼吸循环衰竭。
不良反应:大剂量可兴奋整个中枢神经系统,引起心率加快、血压升高、咳嗽、呕吐、肌肉震颤,甚至引起惊厥。
2、洛贝林:剂量:3mg 。
作用及用途:能选择性兴奋中枢神经系统提高中枢神经系统功能活动的药物,主要用于抢救因芗中互或严重危害疾病,如严重感染、创作等所致的呼吸抑制或衰竭,主要用于新生儿窒息,小儿感染性疾病引起的呼吸衰竭和一氧化碳中毒。
不良反应:过量时可产生过度以兴奋而导致惊厥,严重惊厥随即转入抑制,甚至引起死亡。
3、肾上腺素:剂量:1mg 。
作用及用途:兴奋心血管系统,抑制支气管平滑肌和加强新陈代谢,使周围血管收缩,心率加快,血压长高,用于心脏复苏、过敏性休克、支气管哮喘及局部止血,或与局麻药配伍,延缓局麻药的吸收,延长局麻作用时间,并减少局麻药吸收中毒的可能性。
不良反应:心悸、头痛、激动不安、震颤、血压升高等到,有诱发脑溢血的危险,也能引起心律失常,甚至发展为心室纤颤。
4、去甲肾上腺素:剂量:1mg 。
作用与用途:主要表现为兴奋心血管系统,具有很强的血管收缩作用,使外周阴力增高,血压上升。
静滴用于各种原因引起的休克,且可用胆道与胃手术中止血。
不良反应:局部组织缺血坏死、急性肾功能衰竭,长期用药突然停药,可引起血压剧降。
5、异丙肾上腺素:剂量:1mg 。
作用及用途:可增强心肌收缩力,加快心率,扩张周围血管及支气管平滑肌,促进代谢。
用于支气管哮喘急性发作,房室传导阻滞及各种休克和心脏骤停。

18种常用的抢救药物急诊科长用药物有;肾上腺素、阿托品、利多卡因、胺碘酮、多巴胺、甘露醇、速尿、硝酸甘油、消心痛、西地兰、尼可刹米、纳洛酮、地塞米松、氨茶碱、吗啡、立止血、垂体后叶素、安定、碳酸氢钠、亚硝酸异戊脂、亚甲兰、氯磷定、二巯基丁二酸钠。
回一、中枢神经兴奋药:尼可刹米(可拉明)、山梗菜碱(洛贝林)二、抗休克血管活性药:多巴胺、肾上腺素(副肾素)间羟胺(阿拉明)三、强心药:西地兰(去乙酰毛花甙)四、抗心律失常药:利多卡因、心律平(普罗帕酮)乙胺碘呋酮五、降血压药:硝普钠、硫酸镁六、血管扩张药:硝酸甘油七、利尿剂:速尿(呋喃苯胺酸)八、脱水药:甘露醇九、镇静药:安定(地西泮)苯巴比妥(鲁米那)咪唑安定十、解热药:安痛定(含安基比林、安替比林、巴比妥)来比林十一、镇痛药:杜冷丁(哌替啶)吗啡十二、平喘药:氨茶碱喘啶甲强龙十三、止吐药:胃复安(甲氧氯普胺)异丙嗪十四、促凝血药:6-氨基己酸(氨甲环酸)止血芳酸(氨甲苯酸)止血敏(酚磺乙胺)立止血十五、解毒药:解磷定、阿托品备选药:山莨菪碱(654-2)十六、激素药:地塞米松(氟美松) 备选药:氢化可的松(皮质醇)十七、水电酸碱平衡药:碳酸氢钠氯化钾十八、抗过敏药:苯海拉明(可他敏)葡萄糖酸钙尼可刹米(可拉明)[药理及应用]直接兴奋延髓呼吸中枢,使呼吸加深加快,也可刺激颈动脉体和主动脉体化学感受器,提高呼吸中枢对CO2的敏感性。
对血管运动中枢也有微弱兴奋作用。
临床常用于中枢性呼吸抑制,对各种中枢抑制药如吗啡等过量引起的呼吸抑制疗效较好,对巴比妥类中毒者效果较差。
[用法]常用量:肌注或静注,0.375/次,必要时1~2小时重复。
剂量:1.25g/次。
[注意]大剂量可引起血压升高、心悸、出汗、呕吐、心律失常、震颤及惊厥。
山梗菜碱(洛贝林)[药理及应用]兴奋颈动脉体化学感受器而反射性兴奋呼吸中枢。
临床常用于用于新生儿窒息、小儿感染性疾病引起的呼吸衰竭以及一氧化碳中毒。
18 types of commonly used rescue drugs(For emergencydepartment only)1. Central nervous system stimulantsNicosame (Colamin)[Pharmacology andapplication] Directly excite the medulla oblongata respiratory center to deepen and speed up breathing. It also has a weak excitatory effect on the vascular movement center. Used for central respiratory depression and circulatory failure, poisoning of anesthetics and other central depressants.[Usage] Common dosage: intramuscularly or intravenously, 0.25-0.5g/time, repeat 1 to 2 hours if necessary. Maximum amount:1.25g/time.[Note] Large doses can cause elevated bloodpressure, palpitations, sweating, vomiting, arrhythmia, tremor and convulsions.Lobeline (Lobeline)[Pharmacology and application] Exciting carotid body chemoreceptors and reflex excitement of respiratory center. It is used for neonatal asphyxia, inhalation anesthetics and other central depressant poisoning, carbon monoxide poisoning and respiratory failure caused by pneumonia.[Usage] Common dosage: intramuscularly or intravenously, 3 mg/time,repeat in half an hour if necessary. The maximum amount is 20mg/day.[Note] Adverse reactions include nausea, vomiting, diarrhea, headache, dizziness; large doses can cause tachycardia, respiratory depression, blood pressure drop, and even convulsions.2. Anti-shock vasoactive drugsDopamine[Pharmacology and application] Directactivation of α and β receptors, as well as dopamine receptors. The effect on different receptors is related to the dose: low-dose (2~5μg/kg•min) l ow-speed instillation, excites dopamine receptors, Dilate the kidneys, mesenteric, coronary arteries and cerebral vessels, increase blood flow and urine output. At the same time, it stimulates the β1 receptors of the heart, and also produces a moderately programmed positive inotropic effect by releasing norepinephrine; at a medium dose (5~10μg/kg•min), it can obviously activate β1 receptors to excite the heart and strengthen the myocardium. Contraction force. At thesame time, it also stimulates alpha receptors, causingperipheral blood vessels such as skin and mucous membranes to contract. At high doses (>10μg/kg•min), the positive muscle strength and vasoconstriction effect are more obvious, and the renal vasodilation effect disappears.Positive muscle strength and renal vasodilatation are dominant in medium and low-dose anti-shock therapy. It is used for various types of shock, especially for patients with renal insufficiency, decreased cardiac output, and increased peripheral vascular resistance that have already supplemented blood volume.[Usage] Common dosage: intravenous drip, add 20mg/time to 250ml of 5% glucose, start with 20 drops/min, adjust the drip rate as needed, and the maximum shall not exceed 0.5mg/min.[Note] 1. Adverse reactions include nausea, vomiting, headache, central nervous system excitement, etc.; large doses or overdose can accelerate breathing and rapid arrhythmia. 2.Disabled for patients with hypertension, myocardial infarction, hyperthyroidism, and diabetes. 3. Before use, blood volume should be supplemented and acidosis should be corrected. 4. No spillage during infusion.Adrenaline (Adrenaline)[Pharmacology and Application] It can excite the α and β receptors. Exciting the heart β1-receptors can increase myocardial contractility, increase heart rate, and increase myocardial oxygen consumption; excite α-receptors, which cancontract skin, mucosal blood vessels and small bloodvessels in internal organs, and increase blood pressure; excite β2-receptors Relax bronchial smooth muscles and relieve bronchospasm. Used for anaphylactic shock,cardiac arrest, bronchial asthma, local hemostasis of mucosa or gums, etc.[Usage] 1. Rescue anaphylactic shock: intramuscular injection of 0.5 to 1 mg/time, or slow intravenous injection with 0.9% saline diluted to 10 ml. If the curative effect is not good, use 2~4mg dissolved in 5% glucose solution 250~500ml intravenously instead. 2. Rescue cardiac arrest: 1 mg intravenously, the dose can be increased and repeated every 3 to 5 minutes (1 to 5 mg). 3. Combined with local anesthetics: add a small amount (about 1:200,000-500,000) in the local anesthetic (<300μg).[Note] 1. Adverse reactions include palpitations, headaches, and increased blood pressure. Excessive dosage or stray blood pressure during subcutaneous injection can cause a sudden increase in blood pressure, arrhythmia, and severe ventricular fibrillation and death. 2. Use with caution in hypertension, organic heart disease, diabetes, hyperthyroidism, digitalis poisoning, hypovolemic shock, cardiogenic asthma, etc.Alternative medicine: meta-hydroxylamine (alamin)Three, cardiotonicmedicineCedilan (desacetyl lanolin)[Pharmacology and application] Strengthen myocardial contractility, reflexly excite the vagus nerve, reduce the autonomy of the sinus node and atrium, slow down the heart rate and conduction, and increase the heart rate. Used for congestive heart failure, atrial fibrillation and paroxysmal supraventricular tachycardia.[Usage] Common dose: 0.4mg for the initial dose, if necessary, inject half the dose for 2 to 4 hours. Saturation amount is 1~1.2mg.[Note] 1. Adverse reactions include nausea, vomiting, loss of appetite, diarrhea,headache, hallucinations, green and yellow vision, arrhythmia and atrioventricular block. 2. Acute myocarditis, patients with myocardial infarction are forbidden; and it is forbidden to use it with calcium.Fourth, anti-arrhythmic drugsLidocaine[Pharmacology and application] At low doses, it promotes K+ outflow in myocardial cells, reduces the autonomy of myocardial conduction fibers, and has the effect of anti-ventricular arrhythmia. Used for ventricular tachycardia and premature ventricular.[Usage] Intravenous injection: 1~1.5mg/kg/time (usually 50~100mg/time) if necessary, repeat 1~2 times every 5 minutes. Intravenous infusion: Take 100mg and add 5% glucose 100~200ml forintravenous infusion, static speed is 1~2ml/min. The total amount is <300mg.[Note] 1. Adverse reactions are mainly central nervous system symptoms such as dizziness, drowsiness, paresthesia, muscle tremor, etc. Excessive amounts can cause convulsions, coma and respiratory depression. ccasionally, symptoms of cardiotoxicity such as hypotension, bradycardia, and conduction block are seen. 2. It is forbidden for patients with Alzheimer's syndrome, pre-excitation syndrome and conduction block.Use with caution in patients with liver insufficiency,congestive heart failure, glaucoma, epilepsy, and shock.Propafenone (Propafenone)[Pharmacology andapplication] Extend the time of action potential andeffective refractory period, reduce the spontaneous excitability of the myocardium, reduce the autonomy, and slow down the conduction velocity. In addition, it also blocks beta receptors and L-type calcium channels, and has a mildly negative inotropic effect. It is used for patients with supraventricular and ventricular tachycardia andpremature beats, and pre-excitation syndrome withtachycardia or atrial fibrillation.[Usage] Intravenous injection within 3 to 5 minutes after the first dilution of 70mg, and repeated once after 20 minutes of ineffective; or 1 intravenous injection followed by (20-40/hour) to maintain intravenous infusion. The total amount in 24 hours is less than 350mg.[Note] 1. Adverse reactions include nausea, vomiting, constipation, taste changes, headache, dizziness, etc. In severe cases, it can cause arrhythmia, such as conduction block, sinus node dysfunction. 2. Use with caution in patients with sick sinus syndrome, hypotension, heart failure, and severe CPD.Five, blood pressure lowering drugsReserpine[Pharmacology and application] It can empty the storage of norepinephrine, block the transmission of sympathetic nerve impulse, thus make blood vessels relax and blood pressure drop. It is characterized by slowness, gentleness and long-lasting; and has a calming and slowing heart rate effect. Suitable for patients with mild and moderate hypertension (especially effective for patients with mental stress).[Usage] Common dosage: intramuscularly or intravenously,1mg/time, repeat once after 6 hours of ineffective.[Note] 1.Common adverse reactions include nasal congestion, fatigue, lethargy, and diarrhea. Large doses can causeparalysis tremens. Long-term application can causedepression. 2. Avoid use for patients with gastric and duodenal ulcer.Magnesium Sulfate[Pharmacology and application] After injection, excessive magnesium ions relax the peripheral vascular smooth muscles, causing sympathetic nerve impulse transmission barriers, thereby dilating blood vessels and lowering blood pressure, characterized by rapid and strong antihypertensive effect. Used for convulsions, pregnancy-induced hypertension, eclampsia, tetanus, hypertension, acute renal hypertensive crisis, etc.[Usage] Common dosage: 25% magnesium sulfate 10ml/time, deep intramuscular injection (slow).[Note] 1. Too fast injection speed or excessive dosage can cause rapid hypotension, central nervous system depression, respiratory depression, etc. (calcium rescue); 2. Use digitalis with caution during menstruation.Six, vasodilatorsNitroglycerin[Pharmacology and application] It has the effect of relaxing smooth muscles, relaxing the veins and arteries of the whole body, and it is more obvious than the small arteries in thepost-capillary veins (volume vessels). It also has asignificant diastolic effect on coronary blood vessels, reduces peripheral resistance, and reduces heart load. It isused for the treatment and prevention of angina pectoris of coronary heart disease, and can also be used to lower blood pressure or treat congestive heart failure.[Usage] Dilute with 5% dextrose or sodium chloride solution and then intravenously, the starting dose is 5μg/min, it is best to use an infusion pump to input at a constant rate. There are great differences between patients and the drug. There is no fixed suitable dose for intravenous drip. The dose should be adjusted according to individual blood pressure, heart rate and other hemodynamic parameters.[Note] 1. Common adverse reactions include headache, dizziness, facial flushing, palpitations, orthostatic hypotension, and syncope. 2. It is contraindicated in patients with severe hypotension and tachycardia in the early stage ofmyocardial infarction, severe anemia, glaucoma, and increased intracranial pressure.Seven, diureticsFurosemide (furananiline)[Pharmacology and application] Inhibit the reabsorption of sodium and chlorine in the medulla of the ascending branch of the loop, promote the excretion of sodium, chloride, and potassium, and affect the formation of renal medulla hyperosmotic pressure, thereby interfering with the process of urineconcentration and diuresis Strong. It is used for theadjuvant treatment of various edema, reduction ofintracranial pressure, excretion of drug poisoning and hypertensive crisis.[Usage] Intramuscular or intravenous injection: 20mg~80mg/day, every other day or 1 to 2 timesa day, starting from a small dose.[Note] Long-termmedication has water and electrolyte disorders (hypokalemia, hyponatremia, hypochlorite), which can cause nausea, vomiting, diarrhea, thirst, dizziness, muscle cramps, etc.; occasionally skin rash, itching, blurred vision;sometimes Produce orthostatic hypotension, hearingimpairment, leukopenia and thrombocytopenia.Eight,dehydration medicineMannitol[Pharmacology and application] Causes high osmotic pressure in the renal tubules and diuresis, and at the same time increases blood osmotic pressure, which can dehydrate tissues and reduce intracranial pressure. It is used to treat cerebral edema and glaucoma. It is also used for early renal failure andprevention of acute oliguria.[Usage] Intravenous drip: 250~500ml/time of 20% solution, drip rate 10ml/min.[Note]1. Adverse reactions include water and electrolyteimbalance. ther headaches, blurred vision, dizziness,long-term use of large doses can cause renal tubulardamage. 2. Use with caution in patients with cardiac insufficiency, cerebral hemorrhage, and oliguria due to dehydration.Nine, sedativesValium (Diazepam)[Pharmacology and Application] It has sedative, hypnotic, anti-anxiety, anti-convulsant and skeletal muscle relaxation effects. It is used for anxiety and various neuroses, insomnia and anti-epilepsy, and relieves reflex muscle spasm caused by inflammation.[Usage] Common dosage: 10mg/time, then add 5-10mg every 3 to 4 hours as needed. The total amount in 24 hours is limited to40-50mg.[Note] 1. Adverse reactions include drowsiness, dizziness, ataxia, etc., occasionally respiratory depression and hypotension. 2. Use with caution in patients with acute alcoholism, myasthenia gravis, glaucoma, hypoproteinemia, and chronic obstructive pulmonary disease.Alternative medicine: Phenobarbital (lumina)10. AntipyreticsAntongding (including antipyrine, antipyrine, barbital)[Pharmacology and Application] It has antipyretic, analgesic and anti-inflammatory effects. Mainly used for fever, headache, migraine, neuralgia, toothache and rheumatic pain.[Usage] Common dosage: intramuscularinjection, 2~4ml/time.[Note] ccasionally skin rash orexfoliative dermatitis, a very small number of allergic patients have agranulocytosis; weak physique to prevent collapse; anemia, hematopoietic dysfunction patients are not used.11. AnalgesicsDulantin (Meperidine)[Pharmacology and application] The opioid receptor acting on the central nervous system produces sedation and analgesia. Used for all kinds of severe pain, cardiogenic asthma, and pre-anaesthetic administration.[Usage] Common dosage: intramuscular injection 25~100mg/time, 100~400mg/day. Maximum amount: 150mg/time, 600mg/day. The interval between two medications should not be less than 4 hours.[Note] This product is dependent. Adverse reactions include nausea, vomiting, dizziness, headache, sweating, and dry mouth. verdose can cause dilated pupils, drop in blood pressure, tachycardia, respiratory depression, hallucinations, convulsions, coma, etc.Alternative medicine:Morphine12. Antiasthmatic drugsAminophylline[Pharmacology and Application] It has a relaxing effect on bronchial smooth muscle, intermittentlyinhibits the release of histamine and other allergicsubstances, and relieves congestion and edema of tracheal mucosa. It also relaxes the smooth muscle of the biliary tract, dilates the coronary arteries and has mild diuretic, cardiac and central excitatory effects. Used for bronchial asthma, also can be used for cardiogenic asthma, biliary colic, etc.[Usage] Common dosage: intravenous injection, intravenous drip. 0.25~0.5g/time, diluted with 5% glucose for use. The maximum amount is 0.5g/time, 1g/day.[Note] Too fast intravenous injection or too high concentration can cause nausea, vomiting, palpitations, drop in blood pressure and convulsions. Contraindicated in patients with acute myocardial infarction, hypotension, and severe coronary atherosclerosis.13.AntiemeticsMetoclopramide (Metoclopramide)[Pharmacology and Application] It can block the dopamine receptors, inhibit the emetic chemoreceptors of the brain to exert antiemetic effect, promote gastric peristalsis, and accelerate the emptying of gastric contents. It is used for uremia, vomiting caused by tumor chemotherapy and radiotherapy, and gastrointestinal dyskinesia caused by chronic functional dyspepsia.[Usage] Common dosage: intramuscularinjection, 10mg~20mg/time, no more than 0.5mg/kg per day.[Note] 1. Adverse reactions include orthostatic hypotension, constipation, etc. Large doses can causeextrapyramidal reactions and hyperlactemia. 2. It is contraindicated in pheochromocytoma, epilepsy, breast cancer patients undergoing radiotherapy or chemotherapy.14. Procoagulant drugs6-aminocaproic acid (tranexamic acid)[Pharmacology and application] Byinhibiting fibrinolysis, it can stop bleeding. Used for hemorrhage caused by elevated plasmin activity, such as postpartum hemorrhage, postoperative hemorrhage of prostate, liver, pancreas, lung and other internal organs.[Usage] Common dosage: intravenous infusion, the initial dosage is 4~6g, after dilution, the maintenance amount is 1g/h.[Note] 1. Adverse reactions include nausea, diarrhea, dizziness, skin rash, muscle pain, etc. Too fast intravenous injection can cause hypotension and bradycardia. verdose can cause thrombosis. 2. Those who have a tendency to thrombosis or have a history of thrombotic vascular disease are prohibited. Reduce or use with caution in patients with renal insufficiency.Alternative medicine: Hemostatic acid (aminomethyl methanoic acid),hemostatic allergic (sulphur ethyl amine), reptilase15. AntidotePralidoxime[Pharmacology and application] In the body, it can combine with the phosphoryl group inphosphorylated cholinesterase to form a non-toxicsubstance and be excreted in urine to restorecholinesterase activity. Used for the rescue of organophosphorus pesticides.[Usage] Common dosage: intravenous drip or slow intravenous injection. 1. Mildpoisoning: 0.4g/time, repeat once in 2 to 4 hours if necessary. 2. Moderate poisoning: 0.8~1.2g for the first time, then 0.4~0.8g every 2 hours, 2~3 times; 3. Severe poisoning: 1~1.2g for the first time, 0.4g per hourthereafter.[Note] Because of iodine, it can sometimes cause sore throat and parotid gland swelling. Excessive injection can cause dizziness, blurred vision, nausea, vomiting, and tachycardia. In severe cases, convulsions and even respiratory depression can occur. Avoid compatibility with alkaline drugs.atropine[Pharmacology and application] M cholinergic receptor blocker. In addition to the general anti-M choline effect, such as relief ofgastrointestinal smooth muscle spasm, inhibition of glandular secretion, pupil dilation, increase of intraocularpressure, paralysis of vision adjustment, heart rate increase, etc., large doses can act on vascular smooth muscle and make blood vessels dilate , Relieve vasospasm, improve microcirculation. Used to relieve various visceral colic. 2. Sinus block, atrioventricular block and other slow arrhythmias caused by excessive vagus nerve excitement. 3. Anti-infective toxic shock. 4. Rescue organophosphate poisoning. 5. Administer before general anesthesia.[Usage] Common dosage: intramuscular or intravenous injection, 0.5-1 mg/time, total amount<2mg/day. When used for organophosphorus poisoning, 1-2 mg (5-10 times in severe cases), repeat every 10-20 minutes, and sometimes need 2 to 3 days to maintain.[Note] 1. The adverse reactions caused by the dose from small to large are as follows: 0.5mg, slight heart rate slowdown, slightly dry mouth and less sweat; 1mg, dry mouth, accelerated heart rate, slightly dilated pupils; 2mg, palpitations, significant Dry mouth, dilated pupils, and sometimes blurred vision; 5 mg, the above symptoms are aggravated, and there are slurred speech, irritability, dry skin, fever, difficulty urinating, and decreased bowel movements; above 10 mg, the above symptoms are moresevere, and the pulse is weak. , The central excitement phenomenon is serious, breathing speeds up and deepens, delirium, hallucinations, convulsions, etc.; severepoisoning can be turned from central excitement to inhibition, resulting in coma and respiratory paralysis. The lowest lethal dose is about 80-130 mg for adults and 10 mg for children. 2. High fever, tachycardia, diarrhea and the elderly should be used with caution. Those with glaucoma, pyloric obstruction and prostatic hypertrophy are disabled.Alternative medicine: Anisodamine (654-2)16. HormonesDexamethasone (flumethasone)[Pharmacology and Application] Anti-inflammatory, anti-toxic, anti-allergic, anti-shock and immunosuppressive effects. Used for the treatment of various inflammations and allergies.[Usage] Intramuscular injection, intravenous drip. 2~20mg/time.[Note] Adverse reactions: Inducing or aggravating infection, osteoporosis, muscle atrophy, slow wound healing, etc.; when used in large quantities, it is easy to cause Cushings syndrome (full moon face, buffalo back, central obesity, skin thinning, low Potassium, high blood pressure, urine sugar, etc.); long-term use can easily cause mental symptoms (insomnia, agitation, euphoria)and mental illness. People with a history of hysteria and mental illness are not used. Use with caution in patients with ulcer disease, thrombophlebitis, active tuberculosis, and postoperative intestinal anastomosis.Alternativemedicine: Hydrocortisone (cortisol)17. Hydropoweracid-base balance medicineSodium bicarbonate[Pharmacology and Application] It can increase the body's alkali reserve. Used to prevent and correct metabolic acidosis, septic shock, etc.[Usage] Metabolic acidosis: 1.4% 20ml/kg/time, intravenously. Infectious shock acidosis: 5% 5ml/kg/time, intravenously. All of the above can increase the C2 binding capacity by 10% (V), and correct it in stages until the symptoms disappear.[Note] A large amount of intravenous injection in a short time cancause metabolic alkalosis, hypokalemia, and hypocalcemia. It should be used with caution in patients with congestive heart failure and renal insufficiency.18.Anti-allergic drugsDiphenhydramine (Ketamine)[Pharmacology and application] H1 receptor antagonist. It can compete with the histamine released from the tissues for H1 receptors on effector cells, thereby eliminating allergic symptoms; and has central nervoussystem inhibitory effects such as sedation and hypnosis;also has antiemetic, local anesthesia and anti-M-choline-like effects. It is used to treat allergic diseases, motion sickness and vomiting.[Usage] Common dosage: intramuscular injection, 20 mg/time, 1 to 2times/day.[Note] 1. Adverse reactions include fatigue, dizziness, drowsiness, dry mouth, nausea, etc. ccasionally, it can cause skin rash and neutropenia. 2. Contraindicated in patients with glaucoma, enlarged prostate, pyloric obstruction and intestinal obstruction.Alternative medicine: calcium gluconate【翻译失败,可能限速延时太小!】。
18种抢救药品中枢神经兴奋药一、0.375mg /支尼可刹米(可拉明)直接兴奋延髓呼吸中枢,使呼吸加深加快。
对血管运动中枢也有药理及应用] [微弱兴奋作用。
用于中枢性呼吸抑制及循环衰竭、麻醉药及其它中枢抑制药的中毒。
小时重复。
极量:2次,必要时1~用法]常用量:肌注或静注,0.25~0.5g/ [ 1.25g/次。
注意]大剂量可引起血压升高、心悸、出汗、呕吐、心律失常、震颤及惊厥。
[ 支8mg /山梗菜碱(洛贝林)兴奋颈动脉体化学感受器而反射性兴奋呼吸中枢。
用于新生儿窒][药理及应用吸入麻醉药及其它中枢抑制药的中毒,一氧化碳中毒以及肺炎引起的呼吸衰竭。
息、20mg/日。
]常用量:肌注或静注,3mg/次,必要时半小时重复。
极量[用法[注意]不良反应有恶心、呕吐、腹泻、头痛、眩晕;大剂量可引起心动过速、呼吸抑制、血压下降、甚至惊厥。
二、抗休克血管活性药多巴胺20mg/支[药理及应用]直接激动α和β受体,也激动多巴胺受体,对不同受体的作用与剂量有关:小剂量(2~5μg/kg?min)低速滴注时,兴奋多巴胺受体,使肾、肠系膜、冠状动脉及脑血管扩张,增加血流量及尿量。
同时激动心脏的β1受体,也通过释放去甲肾上腺素产生中等程序的正性肌力作用;中等剂量(5~10μg/kg?min)时,可明显激动β1受体而兴奋心脏,加强心肌收缩力。
同时也激动α受体,使皮肤、黏膜等外周血管收缩。
大剂量(>10μg /kg?min)时,正性肌力和血管收缩作用更明显,肾血管扩张作用消失。
在中、小剂量的抗休克治疗中正性肌力和肾血管扩张作用占优势。
用于各种类型休克,特别对伴有肾功能不全、心排出量降低、周围血管阻力增高而已补足血容量的患者更有意义。
[用法]常用量:静滴,20mg/次加入5%葡萄糖250ml中,开始以20滴/分,根据需要调整滴速,最大不超过0.5mg/分。
[注意]1.不良反应有恶心、呕吐、头痛、中枢神经系统兴奋等;大剂量或过量时可使呼吸加速、快速型心律失常。
抢救药品规格和作用口诀一肾二异三阿托四洛五可六利多七多八阿九西地十尿一去地氨钙我科抢救药物(主要18种,次要8种):一、肾上腺素(1mg/ml/支)1、药理作用:可兴奋心脏,收缩血管,能解除支气管平滑肌痉挛,减轻支气管粘膜充血水肿。
2、适应症:过敏性休克,支气管哮喘,心跳骤停的抢救。
3、注意事项:不良反应有面色苍白,心慌,头痛,心律失常,停药后消失,剂量过大注射入血管使血压骤升,反复局部注射易引起局部坏死。
4、禁用于高血压,心脏病,糖尿病,甲亢,洋地黄中毒,心源性哮喘,出血性休克等患者。
二、异丙肾上腺素(1mg/ml/支)1、药理作用:为拟肾上腺素药,对β1与β2受体都有很强的作用,对α受体无作用,加快心率。
2、适应症:用于急性重症支气管哮喘,心跳骤停,抗休克与房室传导阻滞以及尖端扭转性室速。
3、注意事项:不良反应有心悸,头痛,头晕,喉干,恶心,软弱无力,出汗,可产生耐药性,剂量过大可引起心律失常。
禁与碱性药物合用。
甲亢,洋地黄中毒,心肌炎患者禁用。
舌下含服应咬碎。
三、阿托品(0.5mg/ml/支)1、药理作用:抗胆碱药,能解除迷走神经对心脏的抑制作用,加快心率,消除心脏传导阻滞,可解除痉挛抑制腺体分泌,散大瞳孔。
2、适应症:用于窦性心动过缓,房室传导阻滞,阿斯综合症,胃肠道,胆绞痛,散瞳,有机磷农药中毒。
3、注意事项:心动过速,青光眼者禁用。
四、洛贝林(3mg/ml/支)1、药理作用:本品刺激颈动脉和主动脉弓化学感受器,反射性兴奋呼吸中枢。
2、适应症:用于新生儿窒息,各种原因引起的早期呼吸衰竭。
3、注意事项:大剂量可兴奋迷走神经而导致心动过缓,传导阻滞,特大剂量可引起惊厥,呼吸麻痹,不良反应有恶心,呕吐,头痛,心悸。
五、可拉明(0.375/2ml/支)又名尼可刹米1、药理作用:本品可兴奋延髓呼吸中枢,也可通过外周化学感受器反射性兴奋呼吸中枢,对大脑皮质血管运动中枢和脊髓有微弱的兴奋作用。
2、适应症:中枢性呼吸麻醉药和中枢神经抑制药中毒,新生儿高胆红素血症辅助治疗。
18 类常用抢救药品(急诊科专用)18 类常用抢救药品(急诊科专用)18 类常用抢救药品急诊科专用)尼可刹米(可拉明)[药理及应用]直接兴奋延髓呼吸中枢,使呼吸加深加快。
对血管运动中枢也有微弱兴奋作用。
用于中枢性呼吸抑制及循环衰竭、麻醉药及其它中枢抑制药的中毒。
[用法]常用量:肌注或静注,0.25―― 0.5g/次,必要时1――2小时重复。
极量:1.25g/次。
[注意]大剂量可引起血压升高、心悸、出汗、呕吐、心律失常、震颤及惊厥。
山梗菜碱(洛贝林)[药理及应用]兴奋颈动脉体化学感受器而反射性兴奋呼吸中枢。
用于新生儿窒息、吸入麻醉药及其它中枢抑制药的中毒,一氧化碳中毒以及肺炎引起的呼吸衰竭。
[用法]常用量:肌注或静注,3mg/次,必要时半小时重复。
极量20mg/日。
[注意]不良反应有恶心、呕吐、腹泻、头痛、眩晕;大剂量可引起心动过速、呼吸抑制、血压下降、甚至惊厥。
、抗休克血管活性药多巴胺[药理及应用]直接激动a和3受体,也激动多巴胺受体,对不同受体的作用与剂量有关:小剂量(2 ------ 5卩g/kg?min )低速滴注时,兴奋多巴胺受体,使肾、肠系膜、冠状动脉及脑血管扩张,增加血流量及尿量。
同时激动心脏的3 1 受体,也通过释放去甲肾上腺素产生中等程序的正性肌力作用;中等剂量(5―― 10卩g/kg?min )时,可明显激动[3 1受体而兴奋心脏,加强心肌收缩力。
同时也激动a受体,使皮肤、黏膜等外周血管收缩。
大剂量(>10卩g /kg?min )时,正性肌力和血管收缩作用更明显,肾血管扩张作用消失。
在中、小剂量的抗休克治疗中正性肌力和肾血管扩张作用占优势。
用于各种类型休克,特别对伴有肾功能不全、心排出量降低、周围血管阻力增高而已补足血容量的患者更有意义。
[用法]常用量:静滴,20mg/次加入5%葡萄糖250ml 中, 开始以20滴/分,根据需要调整滴速,最大不超过0.5mg/分。
急救药品大全急救药品是指在紧急情况下用于救治病患的药物。
它们的使用可以迅速缓解症状、稳定病情,并为患者争取到更多的时间等待进一步的医疗救治。
以下是一份急救药品大全,列举了常用的急救药品及其作用、用法和注意事项。
1. 心肺复苏药物- 肾上腺素:用于心跳骤停时的心肺复苏,促进心脏收缩,增加心肌供血。
- 硝酸甘油:用于心绞痛急性发作时的紧急救治,扩张冠状动脉,增加血流。
- 阿托品:用于心脏骤停时的心肺复苏,增加心率,扩张气道。
2. 呼吸急救药物- 氧气:用于缺氧状态下的急救,提供充足的氧供给,维持呼吸功能。
- 布地奈德:用于哮喘急性发作时的紧急救治,缓解气道痉挛。
3. 抗过敏急救药物- 氯雷他定:用于过敏反应急性发作时的紧急救治,抑制组织释放的过敏介质。
- 甲氨蝶呤:用于严重过敏反应时的急救,阻断过敏反应链。
4. 抗感染急救药物- 青霉素:用于严重感染时的急救,抑制细菌细胞壁的合成,杀灭细菌。
- 利奈唑胺:用于真菌感染急性发作时的紧急救治,抑制真菌生长。
5. 止血急救药物- 云南白药:用于外伤出血时的急救,促进血液凝固,止血。
- 维生素K1:用于凝血因子缺乏时的急救,促进血液凝固。
6. 解热镇痛急救药物- 对乙酰氨基酚:用于发热、头痛等症状的急救,降低体温,缓解疼痛。
7. 抗心绞痛急救药物- 硝酸甘油:用于心绞痛急性发作时的紧急救治,扩张冠状动脉,增加血流。
8. 抗中毒急救药物- 对乙酰氨基酚:用于中毒引起的发热、头痛等症状的急救,降低体温,缓解疼痛。
- 活性炭:用于中毒时的急救,吸附有毒物质,减少毒物吸收。
以上列举的急救药品只是部份常用药品,具体使用时应遵循医生的指导和处方要求。
在急救过程中,应注意以下事项:1. 注意药品的适应症和禁忌症,不要滥用或者误用药物。
2. 了解药品的使用方法和剂量,按照医生的建议正确使用。
3. 注意药品的保存条件和有效期,避免使用过期或者受损的药品。
4. 急救过程中应注意观察患者的反应和病情变化,及时调整急救措施。
急诊常用药18类常用抢救药品(急诊科专用)一、中枢神经兴奋药尼可刹米(可拉明)[药理及应用]直接兴奋延髓呼吸中枢,使呼吸加深加快。
对血管运动中枢也有微弱兴奋作用。
用于中枢性呼吸抑制及循环衰竭、麻醉药及其它中枢抑制药的中毒。
[用法]常用量:肌注或静注,0.25~0.5g/次,必要时1~2小时重复。
极量:1.25g/次。
[注意]大剂量可引起血压升高、心悸、出汗、呕吐、心律失常、震颤及惊厥。
山梗菜碱(洛贝林)[药理及应用]兴奋颈动脉体化学感受器而反射性兴奋呼吸中枢。
用于新生儿窒息、吸入麻醉药及其它中枢抑制药的中毒,一氧化碳中毒以及肺炎引起的呼吸衰竭。
[用法]常用量:肌注或静注,3mg/次,必要时半小时重复。
极量20mg/日。
[注意]不良反应有恶心、呕吐、腹泻、头痛、眩晕;大剂量可引起心动过速、呼吸抑制、血压下降、甚至惊厥。
二、抗休克血管活性药多巴胺[药理及应用]直接激动α和β受体,也激动多巴胺受体,对不同受体的作用与剂量有关:小剂量(2~5μg/kg?min)低速滴注时,兴奋多巴胺受体,使肾、肠系膜、冠状动脉及脑血管扩张,增加血流量及尿量。
同时激动心脏的β1受体,也通过释放去甲肾上腺素产生中等程序的正性肌力作用;中等剂量(5~10μg/kg?min)时,可明显激动β1受体而兴奋心脏,加强心肌收缩力。
同时也激动α受体,使皮肤、黏膜等外周血管收缩。
大剂量(>10μg /kg?min)时,正性肌力和血管收缩作用更明显,肾血管扩张作用消失。
在中、小剂量的抗休克治疗中正性肌力和肾血管扩张作用占优势。
用于各种类型休克,特别对伴有肾功能不全、心排出量降低、周围血管阻力增高而已补足血容量的患者更有意义。
[用法]常用量:静滴,20mg/次加入5%葡萄糖250ml中,开始以20滴/分,根据需要调整滴速,最大不超过0.5mg/分。
[注意]1.不良反应有恶心、呕吐、头痛、中枢神经系统兴奋等;大剂量或过量时可使呼吸加速、快速型心律失常。
[药理学]18类常用抢救药品18类常用抢救药品(急诊科专用)一、中枢神经兴奋药尼可刹米(可拉明)[药理及应用]直接兴奋延髓呼吸中枢,使呼吸加深加快。
对血管运动中枢也有微弱兴奋作用。
用于中枢[用法]常用量:肌注或静注,0.25~0.5g/次,必要时1~2小时重复。
极量:1.25g/次。
[注意]大剂量可引起血压升高、心悸、出汗、呕吐、心律失常、震颤及惊厥。
山梗菜碱(洛贝林)[药理及应用]兴奋颈动脉体化学感受器而反射性兴奋呼吸中枢。
用于新生儿窒息、吸入麻醉药及其它中[用法]常用量:肌注或静注,3mg/次,必要时半小时重复。
极量20mg/日。
[注意]不良反应有恶心、呕吐、腹泻、头痛、眩晕;大剂量可引起心动过速、呼吸抑制、血压下降、甚二、抗休克血管活性药多巴胺[药理及应用]直接激动α和β受体,也激动多巴胺受体,对不同受体的作用与剂量有关:小剂量(2~5μ[用法]常用量:静滴,20mg/次加入5%葡萄糖250ml中,开始以20滴/分,根据需要调整滴速,最大不超过0 [注意]1.不良反应有恶心、呕吐、头痛、中枢神经系统兴奋等;大剂量或过量时可使呼吸加速、快速型肾上腺素(副肾素)[药理及应用]可兴奋α、β二种受体。
兴奋心脏β1-受体,使心肌收缩力增强,心率加快,心肌耗氧量[用法]1.抢救过敏性休克:肌注0.5~1mg/次,或以0.9%盐水稀释到10ml缓慢静注。
如疗效不[注意]1.不良反应有心悸、头痛、血压升高,用量过大或皮下注射时误入血管后,可引起血压突备选药:间羟胺(阿拉明)三、强心药西地兰(去乙酰毛花甙)[药理及应用]增强心肌收缩力,并反射性兴奋迷走神经,降低窦房结及心房的自律性,减慢心率与传导[用法]常用量:初次量0.4mg,必要时2~4小时再注半量。
饱和量1~1.2mg。
[注意]1.不良反应有恶心、呕吐、食欲不振、腹泻,头痛、幻觉、绿黄视,心律失常及房室传导阻滞。
四、抗心律失常药利多卡因[药理及应用]在低剂量时,促进心肌细胞内K+外流,降低心肌传导纤维的自律性,而具有抗室性[用法]静注:1~1.5mg/kg/次(一般用50~100mg/次)必要时每5分钟后重复1~2次。
18类常用抢救药品(急诊科专用)18类常用抢救药品(急诊科专用)18类常用抢救药品(急诊科专用)一、中枢神经兴奋药尼可刹米(可拉明)[药理及应用]直接兴奋延髓呼吸中枢,使呼吸加深加快。
对血管运动中枢也有微弱兴奋作用。
用于中枢性呼吸抑制及循环衰竭、麻醉药及其它中枢抑制药的中毒。
[用法]常用量:肌注或静注,0.25~0.5g/次,必要时1~2小时重复。
极量:1.25g/次。
[注意]大剂量可引起血压升高、心悸、出汗、呕吐、心律失常、震颤及惊厥。
山梗菜碱(洛贝林)[药理及应用]兴奋颈动脉体化学感受器而反射性兴奋呼吸中枢。
用于新生儿窒息、吸入麻醉药及其它中枢抑制药的中毒,一氧化碳中毒以及肺炎引起的呼吸衰竭。
[用法]常用量:肌注或静注,3mg/次,必要时半小时重复。
极量20mg/日。
[注意]不良反应有恶心、呕吐、腹泻、头痛、眩晕;大剂量可引起心动过速、呼吸抑制、血压下降、甚至惊厥。
二、抗休克血管活性药多巴胺[药理及应用]直接激动α和β受体,也激动多巴胺受体,对不同受体的作用与剂量有关:小剂量(2~5μg/kg?min)低速滴注时,兴奋多巴胺受体,使肾、肠系膜、冠状动脉及脑血管扩张,增加血流量及尿量。
同时激动心脏的β1受体,也通过释放去甲肾上腺素产生中等程序的正性肌力作用;中等剂量(5~10μg/kg?min)时,可明显激动β1受体而兴奋心脏,加强心肌收缩力。
同时也激动α受体,使皮肤、黏膜等外周血管收缩。
大剂量(>10μg /kg?min)时,正性肌力和血管收缩作用更明显,肾血管扩张作用消失。
在中、小剂量的抗休克治疗中正性肌力和肾血管扩张作用占优势。
用于各种类型休克,特别对伴有肾功能不全、心排出量降低、周围血管阻力增高而已补足血容量的患者更有意义。
[用法]常用量:静滴,20mg/次加入5%葡萄糖250ml中,开始以20滴/分,根据需要调整滴速,最大不超过0.5mg/分。
[注意]1.不良反应有恶心、呕吐、头痛、中枢神经系统兴奋等;大剂量或过量时可使呼吸加速、快速型心律失常。
18类急诊科常用药品及用法用量一、中枢神经兴奋药尼可刹米〔可拉明〕[药理及应用]直接兴奋延髓呼吸中枢,使呼吸加深加快。
对血管运动中枢也有微弱兴奋作用。
用于中枢性呼吸抑制及循环衰竭、麻醉药及其它中枢抑制药的中毒。
[用法]常用量:肌注或静注,0.25~0.5g/次,必要时1~2小时重复。
极量:1.25g/次。
[注意]大剂量可引起血压升高、心悸、出汗、呕吐、心律失常、震颤及惊厥。
山梗菜碱〔洛贝林〕[药理及应用]兴奋颈动脉体化学感受器而反射性兴奋呼吸中枢。
用于新生儿窒息、吸入麻醉药及其它中枢抑制药的中毒,一氧化碳中毒以及肺炎引起的呼吸衰竭。
[用法]常用量:肌注或静注,3mg/次,必要时半小时重复。
极量20mg/日。
[注意]不良反响有恶心、呕吐、腹泻、头痛、眩晕;大剂量可引起心动过速、呼吸抑制、血压下降、甚至惊厥。
二、抗休克血管活性药多巴胺[药理及应用]直接冲动α和β受体,也冲动多巴胺受体,对不同受体的作用与剂量有关:小剂量〔2~5μg/kg?min〕低速滴注时,兴奋多巴胺受体,使肾、肠系膜、冠状动脉及脑血管扩X,增加血流量及尿量。
同时冲动心脏的β1受体,也通过释放去甲肾上腺素产生中等程序的正性肌力作用;中等剂量〔5~10μg/kg?min〕时,可明显冲动β1受体而兴奋心脏,加强心肌收缩力。
同时也冲动α受体,使皮肤、黏膜等外周血管收缩。
大剂量〔>10μg /kg?min〕时,正性肌力和血管收缩作用更明显,肾血管扩X作用消失。
在中、小剂量的抗休克治疗中正性肌力和肾血管扩X作用占优势。
用于各种类型休克,特别对伴有肾功能不全、心排出量降低、周围血管阻力增高而已补足血容量的患者更有意义。
[用法]常用量:静滴,20mg/次参加5%葡萄糖250ml中,开场以20滴/分,根据需要调整滴速,最大不超过0.5mg/分。
[注意]1.不良反响有恶心、呕吐、头痛、中枢神经系统兴奋等;大剂量或过量时可使呼吸加速、快速型心律失常。
Revolt191118类常用抢救药品(急诊科专用)一、中枢神经兴奋药尼可刹米(可拉明)[药理及应用]直接兴奋延髓呼吸中枢,使呼吸加深加快。
对血管运动中枢也有微弱兴奋作用。
用于中枢性呼吸抑制及循环衰竭、麻醉药及其它中枢抑制药的中毒。
[用法]常用量:肌注或静注,0.25~0.5g/次,必要时1~2小时重复。
极量:1.25g/次。
[注意]大剂量可引起血压升高、心悸、出汗、呕吐、心律失常、震颤及惊厥。
山梗菜碱(洛贝林)[药理及应用]兴奋颈动脉体化学感受器而反射性兴奋呼吸中枢。
用于新生儿窒息、吸入麻醉药及其它中枢抑制药的中毒,一氧化碳中毒以及肺炎引起的呼吸衰竭。
[用法]常用量:肌注或静注,3mg/次,必要时半小时重复。
极量20mg/日。
[注意]不良反应有恶心、呕吐、腹泻、头痛、眩晕;大剂量可引起心动过速、呼吸抑制、血压下降、甚至惊厥。
二、抗休克血管活性药多巴胺[药理及应用]直接激动α和β受体,也激动多巴胺受体,对不同受体的作用与剂量有关:小剂量(2~5μg/kg?min)低速滴注时,兴奋多巴胺受体,使肾、肠系膜、冠状动脉及脑血管扩张,增加血流量及尿量。
同时激动心脏的β1受体,也通过释放去甲肾上腺素产生中等程序的正性肌力作用;中等剂量(5~10μg/kg?min)时,可明显激动β1受体而兴奋心脏,加强心肌收缩力。
同时也激动α受体,使皮肤、黏膜等外周血管收缩。
大剂量(>10μg /kg?min)时,正性肌力和血管收缩作用更明显,肾血管扩张作用消失。
在中、小剂量的抗休克治疗中正性肌力和肾血管扩张作用占优势。
用于各种类型休克,特别对伴有肾功能不全、心排出量降低、周围血管阻力增高而已补足血容量的患者更有意义。
[用法]常用量:静滴,20mg/次加入5%葡萄糖250ml中,开始以20滴/分,根据需要调整滴速,最大不超过0.5mg/分。
[注意]1.不良反应有恶心、呕吐、头痛、中枢神经系统兴奋等;大剂量或过量时可使呼吸加速、快速型心律失常。