糖尿病指南2016
- 格式:ppt
- 大小:9.51 MB
- 文档页数:143
ADA2016 指南:糖尿病血糖控制诊疗标准近日美国糖尿病学会(ADA)更新了2016 年糖尿病医学诊疗标准,于2015 年12 月22 日在线发表于2016 年1 月份增刊。
现将糖尿病血糖控制部分全文摘要如下:血糖控制的评估有两项措施可供医护人员和患者评估血糖控制的有效性:患者自我血糖监测(SMBG)、糖化血红蛋白(HbA1c)。
动态血糖监测(CGM)以及组织间隙葡萄糖测定可作为部分患者SMBG 的有益补充。
建议:1. 对于胰岛素注射次数较少或使用非胰岛素治疗的患者,SMBG 作为教育内容的一部分可能有助于指导治疗决策和/ 或患者自我管理。
2. 给予患者SMBG 处方后,应确保患者得到持续的SMB 技术指导、技术评估、结果评价及患者使用 SMBG 数据调整治疗的能力。
3. 大多数采用采用胰岛素强化治疗(每日多次胰岛素注射MDI 或胰岛素泵治疗)的患者应在餐前或加餐前行SMBG,偶尔在餐后、睡前、运动前、怀疑低血糖、低血糖治疗后直到血糖正常、在关键任务如驾驶操作前亦需行SMBG。
4. 对于部分成年(年龄≥ 25 岁)1 型糖尿病患者,正确使用CGM 并联合胰岛素强化治疗有助于降低HbA1c。
5. 虽然目前CGM 降低儿童、青少年及青年患者糖化血红蛋白的证据不足,但CGM 可能对这些人群有帮助,是否成功与坚持使用该装置的依从性相关。
6. CGM 可作为无症状低血糖和/ 或频发低血糖患者SMBG 的一个辅助方法。
7. 由于CGM 的依从性变异较大,给予患者CGM 处方前应评估患者持续使用GCM 的准备状态。
8. 给予患者CGM 处方时,应加强糖尿病教育、培训和支持,以获得最佳的CGM 实施方案和持续使用。
9. 成功使用CGM 的患者应该坚持使用到65 岁以后。
(译者注:此指南为2016 年新增)血糖监测MBGMBG 作为最基本的评价血糖控制水平的手段之一,可以反映实时血糖水平、评估餐前餐后血糖以及生活事件和降糖药物对血糖的影响、发现低血糖,有助于为患者制定个体化的治疗方案、提高治疗的有效性和安全性;同时SMBG 作为糖尿病自我管理的一部分,可使患者更好的了解自身疾病状态,使患者积极参与糖尿病管理、按需调整行为、及时向医务工作者咨询的手段,提高患者治疗的依从性。

84 ENDOCRINE PRACTICE Vol 22 No. 1 January 2016AACE/ACE Consensus StatementCONSENSUS STATEMENT BY THE AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY ON THE COMPREHENSIVE TYPE 2 DIABETES MANAGEMENT ALGORITHM – 2016 EXECUTIVE SUMMARYAlan J. Garber, MD, PhD, FACE 1; Martin J. Abrahamson, MD 2; Joshua I. Barzilay, MD, FACE 3; Lawrence Blonde, MD, FACP , FACE 4; Zachary T. Bloomgarden, MD, MACE 5; Michael A. Bush, MD 6;Samuel Dagogo-Jack, MD, DM, FRCP , FACE 7; Ralph A. DeFronzo, MD, BMS, MS, BS 8;Daniel Einhorn, MD, FACP , FACE 9; Vivian A. Fonseca, MD, FACE 10; Jeffrey R. Garber, MD, FACP , FACE 11; W. Timothy Garvey, MD, FACE 12;George Grunberger, MD, FACP , FACE 13; Yehuda Handelsman, MD, FACP , FNLA, FACE 14;Robert R. Henry, MD, FACE 15; Irl B. Hirsch, MD 16;Paul S. Jellinger, MD, MACE 17; Janet B. McGill, MD, FACE 18; Jeffrey I. Mechanick, MD, FACN, FACP , FACE, ECNU 19;Paul D. Rosenblit, MD, PhD, FNLA, FACE 20; Guillermo E. Umpierrez, MD, FACP , FACE 21From the 1Chair, Professor, Departments of Medicine, Biochemistry and Molecular Biology, and Molecular and Cellular Biology, Baylor College of Medicine, Houston, Texas, 2Beth Israel Deaconess Medical Center, Department of Medicine and Harvard Medical School, Boston, Massachusetts, 3Division of Endocrinology, Kaiser Permanente of Georgia and the Division of Endocrinology, Emory University School of Medicine, Atlanta, Georgia, 4Director, Ochsner Diabetes Clinical Research Unit, Department of Endocrinology, Diabetes and Metabolism, Ochsner Medical Center, New Orleans, Louisiana, 5Clinical Professor, Mount Sinai School of Medicine, Editor, Journal of Diabetes , New York, New York, 6Clinical Chief, Division of Endocrinology, Cedars-Sinai Medical Center, Associate Clinical Professor of Medicine, Geffen School of Medicine, UCLA, Los Angeles, California, 7A.C. Mullins Professor & Director, Division of Endocrinology, Diabetes and Metabolism, University of Tennessee Health Science Center, Memphis, Tennessee, 8Professor of Medicine, Chief, Diabetes Division, University of Texas Health Science Center at San Antonio, San Antonio, Texas, 9Immediate Past President, American College of Endocrinology, Past-President, American Association of Clinical Endocrinologists, Medical Director, Scripps Whittier Diabetes Institute, Clinical Professor of Medicine, UCSD, Associate Editor, Journal of Diabetes , Diabetes and Endocrine Associates, La Jolla, California, 10Professor of Medicine and Pharmacology, Tullis Tulane Alumni Chair in Diabetes, Chief, Section of Endocrinology, Tulane University Health Sciences Center, New Orleans, Louisiana, 11Endocrine Division, Harvard Vanguard Medical Associates, Boston, Massachusetts, Division of Endocrinology, Beth Israel Deaconess Medical Center, Boston, Massachusetts, 12Professor and Chair, Department of Nutrition Sciences, University of Alabama at Birmingham, Director, UABThis document represents the official position of the American Association of Clinical Endocrinologists and American College of Endocrinology. Where there were no randomized controlled trials or specific U.S. FDA labeling for issues in clinical practice, the participating clinical experts utilized their judgment and experience. Every effort was made to achieve consensus among the committee members. Position statements are meant to provide guidance, but they are not to be consid -ered prescriptive for any individual patient and cannot replace the judgment of a clinician.Diabetes Research Center, Mountain Brook, Alabama, 13Grunberger Diabetes Institute, Clinical Professor, Internal Medicine and Molecular Medicine & Genetics, Wayne State University School of Medicine, Bloomfield Hills, Michigan, 14Medical Director & Principal Investigator, Metabolic Institute of America, President, American College of Endocrinology, Tarzana, California, 15Professor of Medicine, University of California San Diego, Chief, Section of Diabetes, Endocrinology & Metabolism, VA San Diego Healthcare System, San Diego, California, 16Professor of Medicine, University of Washington School of Medicine, Seattle, Washington, 17Professor of Clinical Medicine, University of Miami, Miller School of Medicine, Miami, Florida, The Center for Diabetes & Endocrine Care, Hollywood, Florida, 18Professor of Medicine, Division of Endocrinology, Metabolism & Lipid Research, Washington University, St. Louis, Missouri, 19Clinical Professor of Medicine, Director, Metabolic Support, Division of Endocrinology, Diabetes, and Bone Disease, Icahn School of Medicine at Mount Sinai, New York, New York, 20Clinical Professor, Medicine, Division of Endocrinology, Diabetes, Metabolism, University California Irvine School of Medicine, Irvine, California, Co-Director, Diabetes Out-Patient Clinic, UCI Medical Center, Orange, California, Director & Principal Investigator, Diabetes/Lipid Management & Research Center, Huntington Beach, California, and 21Professor of Medicine, Emory University School of Medicine, Director, Endocrinology Section, Grady Health System, Atlanta, Georgia.Address correspondence to American Association of ClinicalEndocrinologists, 245 Riverside Avenue, Suite 200, Jacksonville, FL 32202. E-mail: publications@. DOI: 10.4158/EP151126.CSTo purchase reprints of this article, please visit: /reprints.Copyright © 2016 AACE.85Abbreviations:A1C= hemoglobin A1C; AACE= American Association of Clinical Endocrinologists; ACCORD = Action to Control Cardiovascular Risk in Diabetes; ACCORD BP= Action to Control Cardiovascular Risk in Diabetes Blood Pressure; ACEI = angiotensin-converting enzyme inhibitor; AGI = alpha-glucosidase inhibitor; apo B = apolipoprotein B; ARB = angiotensin II receptor blocker; ASCVD= atherosclerotic cardio-vascular disease; BAS = bile acid sequestrant; BMI = body mass index; BP = blood pressure; CHD = coro-nary heart disease; CKD= chronic kidney disease; CVD = cardiovascular disease; DKA = diabetic ketoac-idosis; DPP-4 = dipeptidyl peptidase 4; EPA = eicosa-pentaenoic acid; FDA = Food and Drug Administration; GLP-1= glucagon-like peptide 1; HDL-C= high-density-lipoprotein cholesterol; LDL-C = low-density-lipoprotein cholesterol; LDL-P = low-density-lipopro-tein particle; Look AHEAD = Look Action for Health in Diabetes; NPH = neutral protamine Hagedorn; OSA = obstructive sleep apnea; SFU = sulfonylurea; SGLT-2 = sodium glucose cotransporter-2; SMBG = self-moni-toring of blood glucose; T2D = type 2 diabetes; TZD = thiazolidinedioneEXECUTIVE SUMMARYThis algorithm for the comprehensive management of persons with type 2 diabetes (T2D) was developed to provide clinicians with a practical guide that considers the whole patient, their spectrum of risks and complica-tions, and evidence-based approaches to treatment. It is now clear that the progressive pancreatic beta-cell defect that drives the deterioration of metabolic control over time begins early and may be present before the diagnosis of diabetes (1). In addition to advocating glycemic control to reduce microvascular complications, this document high-lights obesity and prediabetes as underlying risk factors for the development of T2D and associated macrovascular complications. In addition, the algorithm provides recom-mendations for blood pressure (BP) and lipid control, the two most important risk factors for cardiovascular disease (CVD).Since originally drafted in 2013, the algorithm has been updated as new therapies, management approach-es, and important clinical data have emerged. The 2016 edition includes a new section on lifestyle therapy as well as discussion of all classes of obesity, antihyperglycemic, lipid-lowering, and antihypertensive medications approved by the U.S. Food and Drug Administration (FDA) through December 2015.This algorithm supplements the American Association of Clinical Endocrinologists (AACE) and A merican College of Endocrinology (ACE) 2015 Clinical Practice Guidelines for Developing a Diabetes Mellitus Comprehensive Care Plan (2) and is organized into discrete sections that address the following topics: the founding principles of the algo-rithm, lifestyle therapy, obesity, prediabetes, glucose control with noninsulin antihyperglycemic agents and insulin, management of hypertension, and management of dyslipidemia. In the accompanying algorithm, a chart summarizing the attributes of each antihyperglycemic class and the principles of the algorithm appear at the end. (Endocr Pract. 2016;22:84-113)PrinciplesThe founding principles of the Comprehensive Type 2 Diabetes Management Algorithm are as follows (see Comprehensive Type 2 Diabetes Management Algorithm—Principles):1. Lifestyle optimization is essential for all patientswith diabetes. Lifestyle optimization is multifac-eted, ongoing, and should engage the entire diabe-tes team. However, such efforts should not delayneeded pharmacotherapy, which can be initiatedsimultaneously and adjusted based on patientresponse to lifestyle efforts. The need for medicaltherapy should not be interpreted as a failure oflifestyle management, but as an adjunct to it.2. The hemoglobin A1C (A1C) target should beindividualized based on numerous factors, such asage, life expectancy, comorbid conditions, dura-tion of diabetes, risk of hypoglycemia or adverseconsequences from hypoglycemia, patient moti-vation, and adherence. An A1C level of ≤6.5% isconsidered optimal if it can be achieved in a safeand affordable manner, but higher targets maybe appropriate for certain individuals and maychange for a given individual over time.3. Glycemic control targets include fasting and post-prandial glucose as determined by self-monitor-ing of blood glucose (SMBG).4. The choice of diabetes therapies must be individu-alized based on attributes specific to both patientsand the medications themselves. Medication attri-butes that affect this choice include antihyper-glycemic efficacy, mechanism of action, risk ofinducing hypoglycemia, risk of weight gain, otheradverse effects, tolerability, ease of use, likelyadherence, cost, and safety in heart, kidney, orliver disease.5. Minimizing risk of both severe and nonseverehypoglycemia is a priority. It is a matter of safety,adherence, and cost.6. Minimizing risk of weight gain is also a priority.It too is a matter of safety, adherence, and cost.7. The initial acquisition cost of medications is onlya part of the total cost of care, which includesmonitoring requirements and risks of hypoglyce-86mia and weight gain. Safety and efficacy shouldbe given higher priority than medication cost.8. This algorithm stratifies choice of therapies basedon initial A1C level. It provides guidance as towhat therapies to initiate and add but respectsindividual circumstances that could lead to differ-ent choices.9. Combination therapy is usually required andshould involve agents with complementary mech-anisms of action.10. Comprehensive management includes lipid andBP therapies and treatment of related comorbidi-ties.11. Therapy must be evaluated frequently (e.g., every3 months) until stable using multiple criteria,including A1C, SMBG records (fasting and post-prandial), documented and suspected hypoglyce-mia events, lipid and BP values, adverse events(weight gain, fluid retention, hepatic or renalimpairment, or CVD), comorbidities, other rele-vant laboratory data, concomitant drug adminis-tration, diabetic complications, and psychosocialfactors affecting patient care. Less frequent moni-toring is acceptable once targets are achieved.12. The therapeutic regimen should be as simple aspossible to optimize adherence.13. This algorithm includes every FDA-approved classof medications for T2D (as of December 2015).Lifestyle TherapyThe key components of lifestyle therapy include medical nutrition therapy, regular physical activity, suffi-cient amounts of sleep, behavioral support, and smok-ing cessation and avoidance of all tobacco products (see Comprehensive Type 2 Diabetes Management Algorithm—Lifestyle Therapy). In the algorithm, recommendations appearing on the left apply to all patients. Patients with increasing burden of obesity or related comorbidities may also require the additional interventions listed in the middle and right side of the figure.Lifestyle therapy begins with nutrition counseling and education. All patients should strive to attain and maintain an optimal weight through a primarily plant-based diet high in polyunsaturated and monounsaturated fatty acids, with limited intake of saturated fatty acids and avoidance of trans fats. Patients who are overweight (body mass index [BMI] of 25 to 29.9 kg/m2) or obese (BMI ≥30 kg/ m2) should also restrict their caloric intake with the goal of reducing body weight by at least 5 to 10%. As shown in the Look AHEAD (Action for Health in Diabetes) and Diabetes Prevention Program studies, lowering caloric intake is the main driver for weight loss (3-6). The clini-cian or a registered dietitian (or nutritionist) should discuss recommendations in plain language at the initial visit and periodically during follow-up office visits. Discussion should focus on foods that promote health versus those that promote metabolic disease or complications and should include information on specific foods, meal plan-ning, grocery shopping, and dining-out strategies. In addi-tion, education on medical nutrition therapy for patients with diabetes should also address the need for consisten-cy in day-to-day carbohydrate intake, limiting sucrose-containing or high-glycemic-index foods, and adjusting insulin doses to match carbohydrate intake (e.g., use of carbohydrate counting with glucose monitoring) (2,7). Structured counseling (e.g., weekly or monthly sessions with a specific weight-loss curriculum) and meal replace-ment programs have been shown to be more effective than standard in-office counseling (3,6,8-15). Additional nutri-tion recommendations can be found in the 2013 Clinical Practice Guidelines for Healthy Eating for the Prevention and Treatment of Metabolic and Endocrine Diseases in Adults from AACE/ACE and The Obesity Society (16).After nutrition, physical activity is the main compo-nent in weight loss and maintenance programs. Regular physical exercise—both aerobic exercise and strength training—improves glucose control, lipid levels, and BP; decreases the risk of falls and fractures; and improves functional capacity and sense of well-being (17-24). In Look AHEAD, which had a weekly goal of ≥175 minutes per week of moderately intense activity, minutes of physi-cal activity were significantly associated with weight loss, suggesting that those who were more active lost more weight (3). The physical activity regimen should involve at least 150 minutes per week of moderate-intensity exer-cise such as brisk walking (e.g., 15- to 20-minute mile) and strength training; patients should start any new activity slowly and increase intensity and duration gradually as they become accustomed to the exercise. Structured programs can help patients learn proper technique, establish goals, and stay motivated. Patients with diabetes and/or severe obesity or complications should be evaluated for contrain-dications and/or limitations to increased physical activity, and an exercise prescription should be developed for each patient according to both goals and limitations. More detail on the benefits and risks of physical activity and the practi-cal aspects of implementing a training program in people with T2D can be found in a joint position statement from the American College of Sports Medicine and American Diabetes Association (25).Adequate rest is important for maintaining energy levels and well-being, and all patients should be advised to sleep approximately 7 hours per night. Evidence supports an association of 6 to 9 hours of sleep per night with a reduction in cardiometabolic risk factors, whereas sleep deprivation aggravates insulin resistance, hypertension, hyperglycemia, and dyslipidemia and increases inflamma-tory cytokines (26-31). Daytime drowsiness—a frequent symptom of sleep disorders such as sleep apnea—is asso-ciated with increased risk of accidents, errors in judgment,87and diminished performance (32). The most common type of sleep apnea, obstructive sleep apnea (OSA), is caused by physical obstruction of the airway during sleep. The resulting lack of oxygen causes the patient to awaken and snore, snort, and grunt throughout the night. The awaken-ings may happen hundreds of times per night, often with-out the patient’s awareness. OSA is more common in men, the elderly, and persons with obesity (33,34). Individuals with suspected OSA should be referred to a sleep specialist for evaluation and treatment (2).Behavioral support for lifestyle therapy includes the structured weight loss and physical activity programs mentioned above as well as support from family and friends. Patients should be encouraged to join commu-nity groups dedicated to a healthy lifestyle for emotional support and motivation. In addition, obesity and diabetes are associated with high rates of anxiety and depression, which can adversely affect outcomes (35,36). Healthcare professionals should assess patients’ mood and psycho-logical well-being and refer patients with mood disorders to mental healthcare professionals. Cognitive behavior-al therapy may be beneficial. A recent meta-analysis of psychosocial interventions provides insight into successful approaches (37).Smoking cessation is the final component of lifestyle therapy and involves avoidance of all tobacco products. Structured programs should be recommended for patients unable to stop smoking on their own (2).ObesityObesity is a disease with genetic, environmental, and behavioral determinants that confers increased morbidity and mortality (38,39). An evidence-based approach to the treatment of obesity incorporates lifestyle, medical, and surgical options, balances risks and benefits, and empha-sizes medical outcomes that address the complications of obesity rather than cosmetic goals. Weight loss should be considered in all overweight and obese patients with prediabetes or T2D, given the known therapeutic effects of weight loss to lower glycemia, improve the lipid profile, reduce BP, and decrease mechanical strain on the lower extremities (hips and knees) (2,38).The AACE Obesity Treatment Algorithm emphasizes a complications-centric model as opposed to a BMI-centric approach for the treatment of patients who have obesity or are overweight (see Comprehensive Type 2 Diabetes Management Algorithm—Complications-Centric Model for Care of the Overweight/Obese Patient). The patients who will benefit most from medical and surgical interven-tion have obesity-related comorbidities that can be clas-sified into 2 general categories: insulin resistance/cardio-metabolic disease and biomechanical consequences of excess body weight (40). Clinicians should evaluate and stage patients for each category. The presence and severity of complications, regardless of patient BMI, should guide treatment planning and evaluation (41,42). Once these factors are assessed, clinicians can set therapeutic goals and select appropriate types and intensities of treatment that will help patients achieve their weight-loss goals. Patients should be periodically reassessed (ideally every 3 months) to determine if targets for improvement have been reached; if not, weight loss therapy should be changed or intensi-fied. Lifestyle therapy can be recommended for all patients with overweight or obesity, and more intensive options can be prescribed for patients with comorbidities. For exam-ple, weight-loss medications can be used in combination with lifestyle therapy for all patients with a BMI ≥27 kg/ m2 and comorbidities. As of 2015, the FDA has approved 8 drugs as adjuncts to lifestyle therapy in patients with over-weight or obesity. Diethylproprion, phendimetrazine, and phentermine are approved for short-term (a few weeks) use, whereas orlistat, phentermine/topiramate extended release (ER), lorcaserin, naltrexone/bupropion, and liraglutide 3 mg may be used for long-term weight-reduction therapy. In clinical trials, the 5 drugs approved for long-term use were associated with statistically significant weight loss (placebo-adjusted decreases ranged from 2.9% with orlistat to 9.7% with phentermine/topiramate ER) after 1 year of treatment. These agents improve BP and lipids, prevent progression to diabetes during trial periods, and improve glycemic control and lipids in patients with T2D (43-60). Bariatric surgery should be considered for adult patients with a BMI ≥35 kg/ m2 and comorbidities, especially if therapeutic goals have not been reached using other modalities (2,61).PrediabetesPrediabetes reflects failing pancreatic islet beta-cell compensation for an underlying state of insulin resistance, most commonly caused by excess body weight or obesity. Current criteria for the diagnosis of prediabetes include impaired glucose tolerance, impaired fasting glucose, or metabolic syndrome (see Comprehensive Type 2 Diabetes Management Algorithm—Prediabetes Algorithm). Any one of these factors is associated with a 5-fold increase in future T2D risk (62).The primary goal of prediabetes management is weight loss. Whether achieved through lifestyle therapy, pharma-cotherapy, surgery, or some combination thereof, weight loss reduces insulin resistance and can effectively prevent progression to diabetes as well as improve plasma lipid profile and BP (44,48,49,51,53,60,63). However, weight loss may not directly address the pathogenesis of declining beta-cell function. When indicated, bariatric surgery can be highly effective in preventing progression from prediabe-tes to T2D (62).No medications (either weight loss drugs or antihy-perglycemic agents) are approved by the FDA solely for the management of prediabetes and/or the prevention of T2D. However, antihyperglycemic medications such as metformin and acarbose reduce the risk of future diabetes88in prediabetic patients by 25 to 30%. Both medications are relatively well-tolerated and safe, and they may confer a cardiovascular risk benefit (63-66). In clinical trials, thia-zolidinediones (TZDs) prevented future development of diabetes in 60 to 75% of subjects with prediabetes, but this class of drugs has been associated with a number of adverse outcomes (67-69). Glucagon-like peptide 1 (GLP-1) receptor agonists may be equally effective, as demon-strated by the profound effect of liraglutide 3 mg in safely preventing diabetes and restoring normoglycemia in the vast majority of subjects with prediabetes (59,60,70,71). However, owing to the lack of long-term safety data on the GLP-1 receptor agonists and the known adverse effects of the TZDs, these agents should be considered only for patients at the greatest risk of developing future diabetes and those failing more conventional therapies.As with diabetes, prediabetes increases the risk for atherosclerotic cardiovascular disease (ASCVD). Patients with prediabetes should be offered lifestyle therapy and pharmacotherapy to achieve lipid and BP targets that will reduce ASCVD risk.T2D PharmacotherapyIn patients with T2D, achieving the glucose target and A1C goal requires a nuanced approach that balances age, comorbidities, and hypoglycemia risk (2). The AACE supports an A1C goal of ≤6.5% for most patients and a goal of >6.5% (up to 8%; see below) if the lower target cannot be achieved without adverse outcomes (see Comprehensive Type 2 Diabetes Management Algorithm—Goals for Glycemic Control). Significant reductions in the risk or progression of nephropathy were seen in the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADV ANCE) study, which targeted an A1C <6.5% in the intensive therapy group versus standard approaches (72). In the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, inten-sive glycemic control significantly reduced the risk and/ or progression of retinopathy, nephropathy, and neuropathy (73,74). However, in ACCORD, which involved older and middle-aged patients with longstanding T2D who were at high risk for or had established CVD and a baseline A1C >8.5%, patients randomized to intensive glucose-lowering therapy (A1C target of <6.0%) had increased mortality (75). The excess mortality occurred only in patients whose A1C remained >7% despite intensive therapy, whereas in the standard therapy group (A1C target 7 to 8%), mortality followed a U-shaped curve with increasing death rates at both low (<7%) and high (>8%) A1C levels (76). In contrast, in the Veterans Affairs Diabetes Trial (V ADT), which had a higher A1C target for intensively treated patients (1.5% lower than the standard treatment group), there were no between-group differences in CVD endpoints, cardiovas-cular death, or overall death during the 5.6-year study period (75,77). After approximately 10 years, however, V ADT patients participating in an observational follow-up study were 17% less likely to have a major cardiovascu-lar event if they received intensive therapy during the trial (P<.04; 8.6 fewer cardiovascular events per 1,000 person-years), whereas mortality risk remained the same between treatment groups (78). Severe hypoglycemia occurs more frequently with intensive glycemic control (72,75,77,79). In ACCORD, severe hypoglycemia may have account-ed for a substantial portion of excess mortality among patients receiving intensive therapy, although the hazard ratio for hypoglycemia-associated deaths was higher in the standard treatment group (80). Cardiovascular auto-nomic neuropathy may be another useful predictor of cardiovascular risk, and a combination of cardiovascular autonomic neuropathy (81) and symptoms of peripheral neuropathy increase the odds ratio to 4.55 for CVD and mortality (82).Taken together, this evidence supports individualization of glycemic goals (2). In adults with recent onset of T2D and no clinically significant CVD, an A1C between 6.0 and 6.5%, if achieved without substantial hypoglycemia or other unacceptable consequences, may reduce lifetime risk of microvascular and macrovascular complications. A broader A1C range may be suitable for older patients and those at risk for hypoglycemia. A less stringent A1C of 7.0 to 8.0% is appropriate for patients with history of severe hypoglycemia, limited life expectancy, advanced renal disease or macro-vascular complications, extensive comorbid conditions, or long-standing T2D in which the A1C goal has been diffi-cult to attain despite intensive efforts, so long as the patient remains free of polydipsia, polyuria, polyphagia, or other hyperglycemia-associated symptoms. Therefore, selection of glucose-lowering agents should consider a patient’s ther-apeutic goal, age, and other factors that impose limitations on treatment, as well as the attributes and adverse effects of each regimen. Regardless of the treatment selected, patients must be followed regularly and closely to ensure that glyce-mic goals are met and maintained.The order of agents in each column of the Glucose Control Algorithm suggests a hierarchy of recommended usage, and the length of each line reflects the strength of the expert consensus recommendation (see Comprehensive Type 2 Diabetes Management Algorithm—Glycemic Control Algorithm). Each medication’s properties should be considered when selecting a therapy for individual patients (see Comprehensive Type 2 Diabetes Management Algorithm—Profiles of Antidiabetic Medications), and healthcare professionals should consult the FDA prescrib-ing information for each agent.• Metformin has a low risk of hypoglycemia, can promote modest weight loss, and has good antihyper-glycemic efficacy at doses of 2,000 to 2,500 mg/day.Its effects are quite durable compared to sulfonylureas (SFUs), and it also has robust cardiovascular safety relative to SFUs (83-85). Owing to risk of lactic acido-。
![糖尿病分级诊疗指南[2016版]](https://uimg.taocdn.com/790757bca0116c175e0e480a.webp)
安徽省糖尿病分级诊疗指南(2015年版)糖尿病(diabetes mellitus,DM)是最常见的慢性病之一,危害主要是其并发症,如糖尿病肾病、糖尿病视网膜病变、大血管病变等。
循证医学研究证明,严格控制血糖、血脂、血压和抗凝等多种危险因素,可显著降低糖尿病患者发生并发症的危险性,对早期糖尿病肾病、视网膜病变和糖尿病足的患者采取特殊的干预措施,可以显著降低其致残率和病死率,有效降低国家的疾病负担。
一、我国糖尿病的现状(一)、患病率 2007至2008年中华医学会糖尿病学分会(CDS)在我国部分地区开展的糖尿病流行病学调查显示,在20岁以上的人群中,糖尿病患病率为9.7%,糖尿病前期的比例为15.5%,糖尿病患者中仅有40%获得诊断。
最近发表的全国性流行病学调查也进一步验证了这一发现。
糖尿病分型包括1型糖尿病、2型糖尿病、特殊类型糖尿病、妊娠糖尿病4种类型,其中,2型糖尿病约占糖尿病患者的90%,其治疗和管理多数可以在基层医疗卫生机构(乡镇卫生院、村卫生室、城市社区卫生服务机构)开展。
(二)、发病率我国糖尿病的发病率尚无权威数据,根据历年数据推算,我国每年新发2型糖尿病患者680万。
(三)、糖尿病患者的就诊情况按照就诊率60%推算,全国范围内在各级医疗卫生机构接受医疗服务的糖尿病患者数约为2000余万人。
目前,2型糖尿病指南所推荐的糖尿病基本诊疗措施和适宜技术中,一些已在基层医疗卫生机构实施。
随着疾病筛查水平提高,未来所有未出现严重并发症的2型糖尿病患者均可以下沉基层医疗机构进行管理。
二、糖尿病定义及分型(一)、糖尿病是一组由多病因引起的以慢性高血糖为特征的代谢性疾病,是由于胰岛素分泌不足和(或)作用缺陷引起。
长期碳水化合物以及脂肪、蛋白质代谢紊乱可引起多系统损害,导致眼、肾、神经、心脏、血管等组织器官慢性进行性病变、功能减退及衰竭;病情严重或应激时可发生急性严重代谢紊乱,如糖尿病酮症酸中毒、高血糖高渗状态。
2016 AACEACE 共识声明:糖尿病综合管理方案2016 年1 月,美国临床内分泌医师协会(AACE )和美国内分泌学会(ACE )共同更新了2 型糖尿病综合管理方案,指南内容涵盖生活方式干预、总体指导原则及相关药物组合。
指南发表于《Endocrine Practice 》。
指南要点概括如下。
基本原则1、生活方式治疗,包括药物辅助减重,是治疗 2 型糖尿病的关键。
2、应根据个体化制定A1C 目标。
3、血糖控制目标包括空腹血糖和餐后血糖。
4、根据患者个体特征、医疗费用对患者的影响、处方限制以及患者的个人喜好选择个体化治疗方式。
5、优先选择低血糖风险最小化的治疗方案。
6、优先选择体重增加风险最小化的治疗方案。
7、初始药物费用只是总医疗费用的一部分,后者还包括必要的监测费用、控制低血糖风险以及体重增加风险的费用、保证治疗安全性的费用等。
8、本方案的分层治疗基于初始A1C 水平。
9、联合用药治疗时应选择具有互补作用机制的药物。
10、综合治疗包括血脂、血压以及相关并发症的治疗。
11、治疗期间需要经常评估治疗效果(如每 3 个月一次)直至病情稳定,之后可降低评估频率。
12、治疗方案应尽可能简单以提高依从性。
13、本方案包含的糖尿病治疗药物均经过FDA 批准。
血糖控制根据个体化制定A1C目标• A1C三6.5% :针对无严重疾病并存及低血糖发生风险较低的患者。
• A1C > 6.5% :针对合并严重疾病以及有低血糖发生风险的患者。
生活方式治疗生活方式治疗从营养咨询和教育开始。
所有患者应保持以植物类为基础的饮食习惯;增加多不饱和脂肪酸和单不饱和脂肪酸的摄入,避免反式脂肪酸和饱和脂肪酸摄入,以努力达到并保持最佳体重。
超重/肥胖患者应限制热量摄入以达到减重5%-10% 的目标。
结构化咨询(每周或每月一次的特定减肥课程)以及替代饮食已被证明比标准的办公室咨询更有效。
体力活动是减肥和维持计划的主要组成部分。
·指南与共识·中国糖尿病药物注射技术指南(2016年版)纪立农郭晓蕙黄金姬秋和贾伟平李玲陆菊明单忠艳孙子林田浩明翁建平邢秋玲袁莉章秋张明霞周智广朱大龙邹大进中华糖尿病杂志指南与共识编写委员会序根据2010年全国性糖尿病流行病学调查情况汇总,中国18岁以上成人糖尿病估测患病率为11.6%,而接受治疗的糖尿病患者仅有25.8%,其中能够达到有效血糖控制的患者仅约39.7%[1]。
可见,我国糖尿病患病率虽高,但血糖达标率却较低。
尽管有众多因素影响血糖达标,但即使是已使用胰岛素治疗后3个月及6个月的患者其血糖达标率也仅有36.2%及39.9%[2],而患者对胰岛素注射技术掌握不到位可能是重要原因之一。
胰岛素治疗是实现良好血糖控制的重要手段之一。
胰岛素注射装置、注射技术是使用胰岛素治疗的重要环节。
“2014-2015全球糖尿病患者胰岛素注射技术调查问卷”是第三次全球糖尿病患者胰岛素注射技术近况调查。
该研究从2014年2月持续到2015年6月,共纳入来自41个国家的13298例患者,其中包括3853例中国大陆患者,100例中国台湾患者。
调查结果显示,全球范围内,不规范注射现象普遍存在,而我国糖尿病患者的注射现状更是不容乐观。
与第二次注射技术调查相比,包括注射部位轮换不规范、注射笔用针头的重复使用、注射时手法错误及患者教育不充分等现象依然存在。
这些问题影响了胰岛素治疗的效果,从而导致部分患者血糖控制不达标。
另一方面,在我国,即使是医务人员,对于胰岛素注射技术对血糖控制影响的认识也有限;对于如何规范胰岛素注射,中国的医护工作者和患者在认识上还有较多不足之处。
幸运的是,目前注射技术在糖尿病管理中的重要作用越来越受到全球糖尿病专家的关注。
2015年10月,我有幸参加了在罗马召开的注射与治疗专家推荐论坛,与来自全球54个国家的183名专家共同讨论制订了《胰岛素注射与输注新推荐》[3],大会围绕在解剖学、生理学、病理学、心理学和注射技术等方面展开讨论。
第7卷 第6期2016年11月器官移植OrganTransplantationVol 7 No 6Nov 2016·指南与共识·DOI:10 3969/j issn 1674 7445 2016 06 001基金项目:国家自然科学基金(81370578、81570680)通讯作者:石炳毅,解放军第309医院,Email:shibingyi@medmail com cn中国器官移植术后糖尿病诊疗指南(2016版)中华医学会器官移植学分会 中国医师协会器官移植医师分会 【摘要】 实体器官移植后新发糖尿病(NODAT)增加移植物相关并发症的风险,如排斥反应、移植物功能减退或丧失以及感染,最终影响受者的长期生存。
此外,NODAT也是导致移植后心血管并发症的主要原因。
本指南组织国内器官移植和糖尿病专家在总结器官移植术后血糖异常国内外最新进展的基础上,参考《器官移植术后糖尿病临床诊疗指南(2010版)》并结合我国的临床实践,提出相关的诊疗建议。
内容包括NODAT的流行病学、危险因素和发病机制、移植术前筛查和预防措施、术后筛查和治疗策略等。
本指南提出早期保护胰腺分泌功能是重要的防治理念,有利于提高NODAT的预防和治疗质量,改善器官移植受者的预后。
【关键词】 器官移植;糖尿病;诊断;治疗;指南 【中图分类号】R617,R587 1 【文献标志码】A 【文章编号】1674 7445(2016)06 0001 101 前 言血糖异常是实体器官移植后常见的并发症。
器官移植受者接受免疫抑制剂与移植后新发糖尿病(newonsetdiabetesaftertransplantation,NODAT)直接相关。
现已明确,NODAT能增加移植物相关并发症的风险,如排斥反应、移植物功能减退或丧失以及感染[1 2],最终影响受者的长期生存[3]。
此外,NODAT也是导致移植后心血管并发症的主要原因[4 5]。
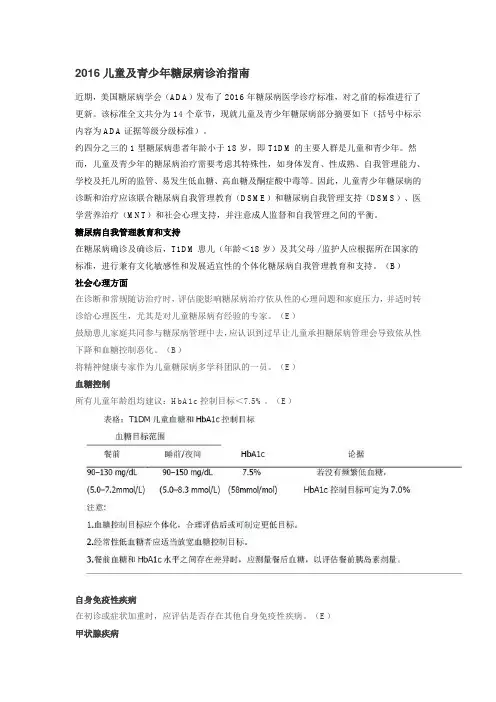
2016儿童及青少年糖尿病诊治指南近期,美国糖尿病学会(ADA)发布了 2016 年糖尿病医学诊疗标准,对之前的标准进行了更新。
该标准全文共分为 14 个章节,现就儿童及青少年糖尿病部分摘要如下(括号中标示内容为 ADA 证据等级分级标准)。
约四分之三的 1 型糖尿病患者年龄小于 18 岁,即 T1DM 的主要人群是儿童和青少年。
然而,儿童及青少年的糖尿病治疗需要考虑其特殊性,如身体发育、性成熟、自我管理能力、学校及托儿所的监管、易发生低血糖、高血糖及酮症酸中毒等。
因此,儿童青少年糖尿病的诊断和治疗应该联合糖尿病自我管理教育(DSME)和糖尿病自我管理支持(DSMS)、医学营养治疗(MNT)和社会心理支持,并注意成人监督和自我管理之间的平衡。
糖尿病自我管理教育和支持在糖尿病确诊及确诊后,T1DM 患儿(年龄<18 岁)及其父母 / 监护人应根据所在国家的标准,进行兼有文化敏感性和发展适宜性的个体化糖尿病自我管理教育和支持。
(B)社会心理方面在诊断和常规随访治疗时,评估能影响糖尿病治疗依从性的心理问题和家庭压力,并适时转诊给心理医生,尤其是对儿童糖尿病有经验的专家。
(E)鼓励患儿家庭共同参与糖尿病管理中去,应认识到过早让儿童承担糖尿病管理会导致依从性下降和血糖控制恶化。
(B)将精神健康专家作为儿童糖尿病多学科团队的一员。
(E)血糖控制所有儿童年龄组均建议:HbA1c 控制目标<7.5%。
(E)自身免疫性疾病在初诊或症状加重时,应评估是否存在其他自身免疫性疾病。
(E)甲状腺疾病1 型糖尿病确诊后即检查患儿的甲状腺过氧化物酶抗体和甲状腺球蛋白抗体。
(E)1 型糖尿病确诊后即测定患儿的 TSH 水平。
结果正常可 1-2 年复查一次,一旦出现甲状腺功能失调的症状、甲状腺肿、生长状态异常、血糖异常变化,应立即复查。
(E)乳糜泻1 型糖尿病确诊后应检查患儿组织型转谷氨酰胺酶水平和脱酰胺基麦胶蛋白抗体。
(E)具有乳糜泻阳性家族史或出现生长障碍、体重降低、体重不增、腹泻、腹胀、腹痛等症状及频繁发生不能解释的低血糖、血糖控制恶化的患儿,应进行筛查。


2016版中国糖尿病药物注射技术指南解读贾芸【期刊名称】《上海护理》【年(卷),期】2018(018)004【总页数】5页(P5-9)【关键词】糖尿病;胰岛素;注射技术;指南【作者】贾芸【作者单位】上海交通大学医学院附属仁济医院,上海 200127【正文语种】中文【中图分类】R47·指南解读·编者按:作为糖尿病治疗的重要手段之一,胰岛素药物的使用在我国已经相当广泛,胰岛素注射装置和注射技术作为胰岛素治疗的重要环节也受到临床护理人员的广泛重视。
2011年出台的第1版《中国糖尿病药物注射技术指南》,针对糖尿病药物注射装置、注射技术等多方面给出了指导性的规范。
近年来,随着全球及中国循证医学证据的增加,中华医学会糖尿病学分会对指南进行了第2次修订。
本期特邀上海市护理学会内科专业委员会糖尿病护理学组组长、资深糖尿病护理专家贾芸老师,就新指南的相关内容进行详尽解读,旨在帮助广大护理人员更好地掌握注射技术规范,使更多患者受益。
2010年全国性糖尿病流行病学调查报告显示:中国18岁以上成人糖尿病估测患病率为11.6%,而接受治疗的糖尿病患者仅有25.8%,其中血糖达标的人数只有39.7%[1]。
胰岛素治疗是实现良好血糖控制的重要措施之一。
然而,已经接受胰岛素治疗3个月和6个月的患者,血糖达标率仅为36.2%及39.9%,患者注射技术的不规范是重要原因之一[2]。
2008—2009年开展的全球糖尿病患者胰岛素注射技术调查发现:患者的注射技术现状不容乐观,其中注射部位轮换不规范、注射笔用针头重复使用率高、注射手法错误、所接受的注射相关教育不充分等问题较为突出。
这反映出医护人员对于“注射技术对患者血糖控制的影响”等方面认识存在一定局限性,提示无论医护人员还是患者对于如何规范注射胰岛素均存在误区[3]。
来自全球医疗护理、心理、教育领域的专家根据大量循证医学证据制定了“全球糖尿病药物注射技术新推荐”。