妊娠期高血压指南
- 格式:doc
- 大小:197.50 KB
- 文档页数:27
·临床指南·妊娠期高血压疾病诊治指南(2015)中华医学会妇产科学分会妊娠期高血压疾病学组中华医学会妇产科学分会妊娠期高血压疾病学组组织有关专家根据国内外的最新研究进展,参考美国、加拿大、英国、澳大利亚等国家和地区学术组织的最新相关指南[1-4],并结合我国国情和临床实践经验,在2012年发表的“妊娠期高血压疾病诊治指南(2012版)[5]”的基础上,经反复讨论修改,最终形成“妊娠期高血压疾病诊治指南(2015)”修订版。
本指南遵循循证医学理念,对有关治疗方案给出证据评价(证据等级以罗马数字显示,推荐等级以英文字母表示)[6],以进一步规范我国妊娠期高血压疾病(hypertensive disorders of pregnancy)的临床诊治。
本指南循证证据等级及推荐等级评价:(1)证据等级:Ⅰ:证据来自至少1个高质量的随机对照试验;Ⅱ-1:证据来自设计良好的非随机对照试验;Ⅱ-2:证据来自设计良好的队列(前瞻性或回顾性)研究或者病例对照研究;Ⅱ-3:证据来自比较不同时间或地点干预措施效果差异的研究;Ⅲ:基于临床经验、描述性研究或者专家委员会报告等的专家意见。
(2)推荐等级:A:证据适合推荐应用于临床预防;B:证据较适合推荐应用于临床预防;C:现有的证据间不一致;D:有一定证据不推荐用于临床预防;E:有相当证据建议不推荐用于临床预防;Ⅰ:没有足够的证据。
一、分类妊娠期高血压疾病为多因素发病,可存在各种母体基础病理状况,也受妊娠期环境因素的影响。
妊娠期间病情缓急不同,可呈现进展性变化并可迅速恶化。
(一)妊娠期高血压(gestational hypertension)妊娠20周后首次出现高血压,收缩压≥140 mmHg(1mmHg=0.133kPa)和(或)舒张压≥90 mmHg,于产后12周内恢复正常;尿蛋白检测阴性。
收缩压≥160mmHg和(或)舒张压≥110mmHg 为重度妊娠期高血压。
2020年妊娠期高血压疾病诊治指南摘要妊娠期高血压疾病是全世界孕产妇和围产儿死亡的主要原因之一。
中华医学会妇产科学分会妊娠期高血压疾病学组在2015版指南的基础上进行修订,并颁发妊娠期高血压及子痫前期临床诊治指南2020版。
在2020版指南中,明确强调了妊娠期高血压疾病孕妇发病的背景复杂,尤其子痫前期‐子痫存在多因素‐多机制‐多通路致病的综合征发病性质。
不仅孕妇高血压的临床表现程度和表现形式复杂,子痫前期的首发症状也存在多样性。
于此基础上,本指南在强调各种风险因素识别同时,提出应重视妊娠期的临床预警信息,强化产前检查,提高早期识别和早期诊断能力,并在降压和预防抽搐等对症处理的基础上,注意各种诱发病因的诊治。
本指南旨在为妊娠期高血压及子痫前期的临床诊治提供指导,并扩展临床多方面诊治思路。
中华医学会妇产科学分会妊娠期高血压疾病学组在《妊娠期高血压疾病诊治指南(2015)》[1]的基础上,更新发布“妊娠期高血压疾病诊治指南(2020)”版本。
本指南根据对妊娠期高血压疾病的新的认识,参考了美国、加拿大、英国、澳大利亚、国际妇产科联盟(FIGO)、WHO等最新的相关指南[2‐10],并结合我国国情、临床研究及实践经验,遵循循证医学理念,对有关的治疗方案给出了证据评价[11]。
本指南更加强调对妊娠期高血压疾病的临床预警和早期识别能力,强调早预警、早发现和早干预,进一步规范和指导我国妊娠期高血压疾病的临床处理。
本指南的循证证据等级及推荐建议:(1)证据等级:①Ⅰ:证据来自至少1个高质量的随机对照试验;②Ⅱ‐1:证据来自设计良好的非随机对照试验;③Ⅱ‐2:证据来自设计良好的队列(前瞻性或回顾性)研究或者病例对照研究;④Ⅱ‐3:证据来自不同时间或地点干预措施效果的差异研究;⑤Ⅲ:基于临床经验、描述性研究或者专家委员会报告等的专家意见。
(2)推荐建议:①A:证据适合推荐应用于临床预防;②B:证据较适合推荐应用于临床预防;③C:现有的证据间不一致;④D:有一定的证据不推荐用于临床预防;⑤E:有相当证据不推荐用于临床预防;⑥L:没有足够的证据(数量或质量)可以提出建议,但是,其他因素可能会影响决策。

妊娠期高血压疾病诊治指南(2012版)(一)妊娠期高血压:妊娠期出现高血压,收缩压≥140mmHg与(或)舒张压≥90mmHg,于产后12周恢复正常。
尿蛋白(一),产后方可确诊。
少数患者可伴有上腹部不适或血小板减少。
(二)子痫前期:轻度:妊娠20周后出现收缩压≥140mmHg与(或)舒张压≥90mmHg伴蛋白尿≥0、3g/24h。
重度:血压与尿蛋白持续升高,发生母体脏器功能不全或胎儿并发症。
子痫前期患者出现下述任一不良情况可诊断为重度子痫前期:①血压持续升高:收缩压≥160mmHg与(或)舒张压≥110mmHg;②蛋白尿≥2、0g/24h或随机蛋白尿≥(++);③持续性头痛或视觉障碍或其它脑神经症状;④持续性上腹部疼痛,肝包膜下血肿或肝破裂症状;⑤肝脏功能异常:肝酶ALT或AST水平升高;⑥肾脏功能异常:少尿(24h尿量<400ml或每小时尿量<17ml)或血肌酐>106μmol/L;⑦低蛋白血症伴胸水或腹水;⑧血液系统异常:血小板呈持续性下降并低于100×109/L;血管内溶血、贫血、黄疸或血LDH升高;⑨心力衰竭、肺水肿;⑩胎儿生长受限或羊水过少;⑾孕34周以前发病(II-2B)。
(三)子痫:子痫前期基础上发生不能用其它原因解释的抽搐。
(四)妊娠合并慢性高血压:妊娠20周前收缩压≥140mmHg与(或)舒张压≥90mmHg,妊娠期无明显加重;或妊娠20周后首次诊断高血压并持续到产后12周以后。
(五)慢性高血压并发子痫前期:慢性高血压孕妇妊娠前无蛋白尿,妊娠后出现蛋白尿≥0、3g/24h;或妊娠前有蛋白尿,妊娠后尿蛋白明显增加或血压进一步升高或出现血小板减少<100×109/L。
二诊断(一)病史:注意询问妊娠前有无高血压、肾病、糖尿病、抗磷脂综合征等病史,了解此次妊娠后高血压、蛋白尿等征象出现的时间与严重程度,有无妊娠期高血压疾病家族史。
(二)高血压的诊断血压的测量:测前被测者至少安静休息5分钟。
![妊娠期高血压疾病诊治指南_2016年[全文本]](https://uimg.taocdn.com/8cd7c79bb9f3f90f77c61b20.webp)
妊娠期高血压疾病诊治指南(2015)一、分类二、诊断三、处理四、预防五、管理附.HELLP综合征的诊断和治疗一、分类(一)妊娠期高血压(二)子痫前期----子痫(三)妊娠合并慢性高血压(四)慢性高血压并发子痫前期2012版妊娠期高血压子痫前期(轻度、重度)子痫妊娠合并慢性高血压慢性高血压并发子痫前期(一)妊娠期高血压妊娠20周后首次出现高血压,收缩压≥140mmHg和(或)舒张压≥90mmHg,于产后12周内恢复正常;尿蛋白检测阴性。
收缩压≥160 mmHg和(或)舒张压≥110 mmHg为重度妊娠期高血压。
2012版妊娠期首次出现高血压,收缩压≥140 mmHg(1 mm Hg=0.133 kPa)和(或)舒张压≥90 mm Hg。
于产后12周恢复正常。
尿蛋白阴性。
产后方可确诊。
少数患者可伴有上腹部不适或血小板减少。
(二)子痫前期----子痫1.子痫前期妊娠20周后出现收缩压≥140 mmHg和(或)舒张压≥90 mmHg,且伴有下列任一项:尿蛋白≥0.3 g/24 h,或尿蛋白/肌酐比值≥0.3,或随机尿蛋白≥(+)(无法进行尿蛋白定量时的检查方法);无蛋白尿但伴有以下任何一种器官或系统受累:心、肺、肝、肾等重要器官,或血液系统、消化系统、神经系统的异常改变,胎盘-胎儿受到累及等。
2012版轻度子痫前期【2015版已去除该项】:妊娠20周后出现收缩压≥140 mm Hg 和(或)舒张压≥90 mm Hg伴尿蛋白≥0.3 g/24 h或随机尿蛋白≥(+)。
重度子痫前期:血压和尿蛋白持续升高,发生母体脏器功能不全或胎儿并发症。
重度子痫前期子痫前期孕妇出现下述任一表现可诊断为重度子痫前期:(1)血压持续升高:收缩压≥160 mmHg和(或)舒张压≥110 mmHg;(2)持续性头痛、视觉障碍或其他中枢神经系统异常表现;(3)持续性上腹部疼痛及肝包膜下血肿或肝破裂表现;(4)肝酶异常:血丙氨酸转氨酶(ALT)或天冬氨酸转氨酶(AST)水平升高;(5)肾功能受损:尿蛋白>2.0 g/24 h;少尿(24 h尿量<400 ml、或每小时尿量<17 ml)、或血肌酐>106μmol/L;(6)低蛋白血症伴腹水、胸水或心包积液;(7)血液系统异常:血小板计数呈持续性下降并低于100×109/L;微血管内溶血(表现有贫血、黄疸或血乳酸脱氢酶(LDH)水平升高);(8)心功能衰竭;(9)肺水肿;(10)胎儿生长受限或羊水过少、胎死宫内、胎盘早剥等。
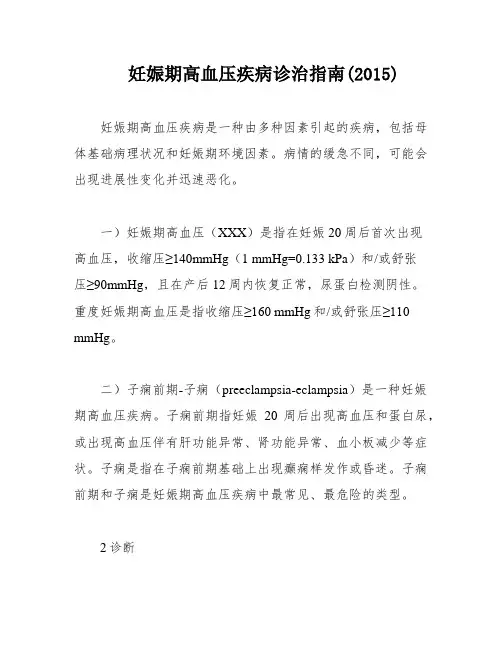
妊娠期高血压疾病诊治指南(2015)妊娠期高血压疾病是一种由多种因素引起的疾病,包括母体基础病理状况和妊娠期环境因素。
病情的缓急不同,可能会出现进展性变化并迅速恶化。
一)妊娠期高血压(XXX)是指在妊娠20周后首次出现高血压,收缩压≥140mmHg(1 mmHg=0.133 kPa)和/或舒张压≥90mmHg,且在产后12周内恢复正常,尿蛋白检测阴性。
重度妊娠期高血压是指收缩压≥160 mmHg和/或舒张压≥110 mmHg。
二)子痫前期-子痫(preeclampsia-eclampsia)是一种妊娠期高血压疾病。
子痫前期指妊娠20周后出现高血压和蛋白尿,或出现高血压伴有肝功能异常、肾功能异常、血小板减少等症状。
子痫是指在子痫前期基础上出现癫痫样发作或昏迷。
子痫前期和子痫是妊娠期高血压疾病中最常见、最危险的类型。
2诊断对于妊娠期高血压疾病的诊断,应该根据患者的临床表现、体征和实验室检查结果进行综合评估。
在诊断时,需要排除其他可能引起高血压的原因。
对于子痫前期和子痫,需要密切监测患者的病情变化,及时采取治疗措施。
3治疗治疗妊娠期高血压疾病的目标是保护母亲和胎儿的健康。
治疗方案应该根据患者的具体情况进行个体化制定。
对于轻度妊娠期高血压,常规措施包括定期随访、控制血压、监测尿蛋白等。
对于重度妊娠期高血压和子痫前期-子痫,应该及时采取药物治疗,如镁剂、降压药等。
在治疗过程中,需要密切监测患者的病情变化和胎儿的情况,及时采取必要的措施。
4预防预防妊娠期高血压疾病的关键是提高孕妇的健康素养和生活方式。
孕妇应该注意饮食、适当运动、保持心理健康等。
对于高危人群,应该进行定期检查和监测。
对于已经患有妊娠期高血压疾病的孕妇,需要及时采取治疗措施,预防病情恶化,保护母亲和胎儿的健康。
孕妇出现高血压和(或)蛋白尿等症状。
二)体格检查:测量血压、尿检等。
三)实验室检查:检测肝酶、肾功能、血小板计数、LDH等指标。
四)影像学检查:B超检查胎儿生长情况、胎盘位置等。
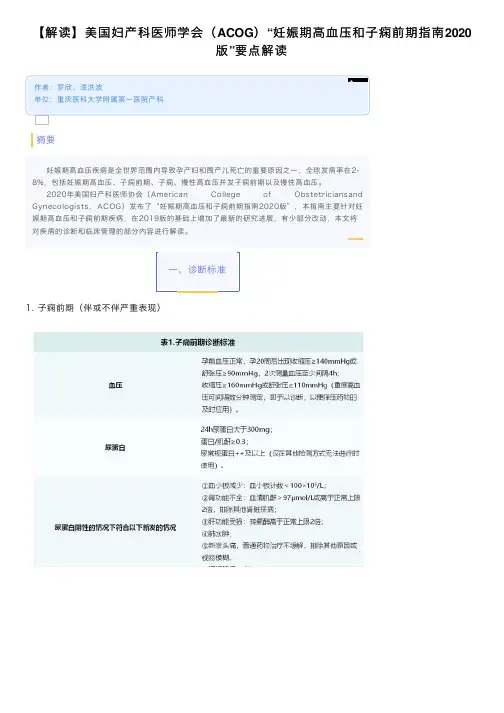
解读:对于⼦痫前期(伴或不伴严重表现)的诊断标准并⽆变动,本部分指南强调要辩证的看待临床症状,即不能轻视它们包括可能因门静脉周围或局灶性坏死、肝细胞⽔肿或胆道系统扩张所引起的持续性右上腹或中上腹疼痛,因为这些体征并不伴有实验室指标的异常;也不能太过依赖,⽐如头痛作为严重症状的诊断指标特异性是有所⽋缺的的,需要联合其他实验室指标来得到确凿的诊断。
指南还指出了尿蛋⽩仍然作为重要但⾮必要的诊断依据。
24⼩时尿蛋⽩结果虽然⽐较准确,但是获得结果的过程有些漫长,在这个过程中可能病情会进展到异常严重的地步,所以指南建议条件不允许的情况下将使⽤随机尿蛋⽩来评估蛋⽩尿,鉴于随机尿蛋⽩假阳性率过⾼,指南建议将随机尿蛋⽩⼤于++作为随机尿蛋⽩阳性的有效评估。
另外,指南指出⼦痫前期的诊断应当在20周以后,如果在20周以前发现类似症状更应该考虑⼦痫前期的替代诊断,如⾎栓性⾎⼩板减少性紫癜、溶⾎性尿毒症综合征、葡萄胎妊娠、肾病或⾃⾝免疫性疾病等。
指南还阐述了⼦痫前期诊断中肝酶升⾼的⼀个⼩细节,⼦痫前期诊断初期肝酶的升⾼特征应该是AST升⾼幅度⼤于ALT,如果这个趋势反过来,那么应该排除肝实质病变的可能才能诊断为⼦痫前期。
2. 妊娠期⾼⾎压妊娠期⾼⾎压定义为妊娠20周后新发的收缩压和/或舒张压≥140/90mmHg, 两次⾎压测量⾄少间隔4⼩时,产后⾎压可恢复正常。
重度⾼⾎压定义为收缩压和/或舒张压≥160/110mmHg,为便于降压药物的及时应⽤,间隔时间仅需数分钟⽽⾮4⼩时。
解读:本部分指南强调要重视妊娠期⾼⾎压,原因有三,⼀妊娠期⾼⾎压与不伴严重特征的⼦痫前期治疗⽅案相同;⼆有研究指出约半数的妊娠期⾼⾎压会进展为⼦痫前期,三即便是蛋⽩尿阴性的情况下,重度妊⾼依旧需要视为伴有严重特征的⼦痫前期进⾏管理。
另外指南还指出妊⾼进展为⼦痫前期的特征:在⾼⾎压孕妇中,有蛋⽩尿症状的妇⼥进展为重度⾼⾎压的频率更⾼,早产和围产期死亡率更⾼;⽽没有蛋⽩尿的⼥性发⽣⾎⼩板减少或肝功能障碍的频率更⾼。

2021妊娠期高血压疾病诊治指南(下)(四)硫酸镁防治子痫硫酸镁是治疗子痫和预防抽搐复发的一线药物(Ⅰ‐A),也是对于重度子痫前期预防子痫发作的用药[31‐34](Ⅰ‐A);硫酸镁控制子痫再次发作的效果优于地西泮、苯巴比妥和冬眠合剂等镇静药物[34‐37](Ⅰ‐A);除非存在硫酸镁应用禁忌证或者硫酸镁治疗效果不佳,否则不推荐使用苯巴比妥和苯二氮卓类药物(如地西泮)用于子痫的预防或治疗;对于非重度子痫前期孕妇也可酌情考虑应用硫酸镁(Ⅰ‐C)。
1. 用法:(1)子痫抽搐:静脉用药负荷剂量为4~6 g,溶于10% 葡萄糖溶液20 ml 静脉推注15~20 min,或溶于5%葡萄糖溶液100 ml 快速静脉滴注,继而1~2 g/h静脉滴注维持。
或者夜间睡眠前停用静脉给药,改用肌内注射,用法为25%硫酸镁20 ml+2%利多卡因2 ml臀部深部肌内注射。
24 h硫酸镁总量为25~30 g(Ⅰ‐A)。
(2)预防子痫发作:适用于重度子痫前期和子痫发作后,负荷剂量2.5~5.0 g,维持剂量与控制子痫处理相同。
用药时间根据病情需要调整,一般每天静脉滴注6~12 h,24 h总量不超过25 g。
(3)子痫复发抽搐:可以追加静脉负荷剂量用药2~4 g,静脉推注2~3 min,继而1~2 g/h静脉滴注维持。
(4)若为产后新发现高血压合并头痛或视力模糊,建议启用硫酸镁预防产后子痫前期‐子痫。
(5)控制子痫抽搐24 h后需要再评估病情,病情不稳定者需要继续使用硫酸镁预防复发抽搐。
用药期间应每天评估病情变化,决定是否继续用药;引产和产时可以持续使用硫酸镁,尤其对于重度子痫前期;若剖宫产术中应用,要注意孕产妇的心脏功能;产后继续使用24~48 h,注意再评估病情;硫酸镁用于重度子痫前期预防子痫发作以及重度子痫前期的期待治疗时,为避免长期应用对胎儿(或新生儿)的血钙水平和骨质的影响,建议及时评估病情,如孕妇病情稳定,应在使用5~7 d后停用硫酸镁;在重度子痫前期的期待治疗中,必要时可间歇性应用。
妊娠期高血压疾病执行摘要Hypertension in Pregnancy: Executive Summary(ACOG 2013)The American College of Obstetricians and Gynecologists (the College) convened a task force of experts in the management of hypertension in pregnancy to review available data and publish evidence-based recommendations for clinical practice. The Task Force on Hypertension in Pregnancy comprised 17 clinician-scientists from the fields of obstetrics, maternal-fetal medicine, hypertension, internal medicine, nephrology, anesthesiology, physiology, and patient advocacy. This executive summary includes a synopsis of the content and task force recommendations of each chapter in the report and is intended to complement, not substitute, the report.美国妇产科学会组织专家通过回顾现有的研究数据及基于证据的建议颁布了妊娠期高血压疾病的临床指南。
妊高病专家组成员由的17位专家组成,他们来自临床专家,产科学、母胎医学、高血压疾病、内科学、肾脏学、麻醉学、生理学和患方维权者。
这个执行摘要包括内容概要和每章节的专家组推荐。
它不是替代而是补充说明该报告。
Hypertensive disorders of pregnancy remain a major health issue for women and their infants in the United States. Preeclampsia, either alone or superimposed on preexisting (chronic) hypertension, presents the major risk. Although appropriate prenatal care, with observation of women for signs of preeclampsia and then delivery to terminate the disorder, has reduced the number and extent of poor outcomes, serious maternal-fetal morbidity and mortality still occur. Some of these adverse outcomes are avoidable, whereas others can be ameliorated. Also, although some of the problems that face neonates are related directly to preeclampsia, a large proportion are secondary to prematurity that results from the appropriate induced delivery of the fetuses of women who are ill. Optimal management requires close observation for signs and premonitory findings and, after establishing the diagnosis, delivery at the optimal time for both maternal and fetal well-being. More recent clinical evidence to guide this timing is now available. Chronic hypertension is associated with fetal morbidity in the form of growth restriction and maternal morbidity manifested as severely increased blood pressure (BP). However, maternal and fetal morbidity increase dramatically with the superimposition of preeclampsia. One of the major challenges in the care of women with chronic hypertension is deciphering whether chronic hypertension has worsened or whether preeclampsia has developed. In this report, the task force provides suggestions for the recognition and management of this challenging condition.在美国、妊高病是一种严重威胁母胎健康的疾病。
子痫前期或慢性高血压并发子痫前期是主要危险因素。
尽管通过恰当的产前管理、子痫前期的监测以及适时终止妊娠来减少发病率以及不利的结局,但是严重的母胎发病率及死亡率依然存在。
一些不良结局是可以避免的、还有一些是可以改善的。
尽管一些新生儿面临的问题与子痫前期直接相关、但是大部分继发于因母体疾病导致的医源性早产。
优化管理需要严密监测疾病征兆、建立诊断、以及分娩时机的选择(考虑母胎因素)。
最新的临床证据提供了研究的可能。
慢性高血压对胎儿的影响主要是胎儿生长受限、对母体的影响主要是严重的高血压。
慢性高血压面临的问题之一是鉴别疾病是否加重或是否并发子痫前期。
在这个报告中、专家组提供了建议及管理办法。
In the past 10 years, there have been substantial advances in the understanding of preeclampsia as well as increased efforts to obtain evidence to guide therapy. Nonetheless, there remain areas on which evidence is scant. The evidence is now clear that preeclampsia is associated with later-life cardiovascular (CV) disease; however, further research is needed to determine how best to use this information to help patients. The task force also has identified issues in the management of preeclampsia that warrant special attention. First, is the failure by health care providers to appreciate the multisystemic nature of preeclampsia. This is in part due to attempts at rigid diagnosis, which is addressed in the report. Second, preeclampsia is a dynamic process, and a diagnosis such as “mild preeclampsia” (which is discouraged) applies only at the moment the diagnosis is established because preeclampsia by nature is progressive, although at different rates. Appropriate management mandates frequent reevaluation for severe features that indicate the actions outlined in the recommendations (which are listed after the chapter summaries). It has been known for many years that preeclampsia can worsen or present for the first time after delivery, which can be a major scenario for adverse maternal events. In this report, the task force provides guidelines to attempt to reduce maternal morbidity and mortality in the postpartum period.过去十年、大量研究加深了对子痫前期的理解同时提供证据指导治疗。
然而、这一领域的研究证据依然缺乏。
目前研究显示,子痫前期与随后的心血管疾病相关。
但是、进一步的研究需要充分利用这一信息为病人提供指导帮助。
同样、专家组在子痫前期管理上提供了特别关注点。
首先、医疗工作者没有理解子痫前期发病的多系统性。
这部分是由严格的诊断标准造成的、这个标准将在这个报告中阐述。
其次、子痫前期是一种动态的过程、轻度子痫前期的诊断只适用在诊断建立时、因为子痫前期具有渐进性、尽管进展速度不一。