Acute Myocardial Infarction With Normal Coronary Arteries
- 格式:pdf
- 大小:162.48 KB
- 文档页数:7
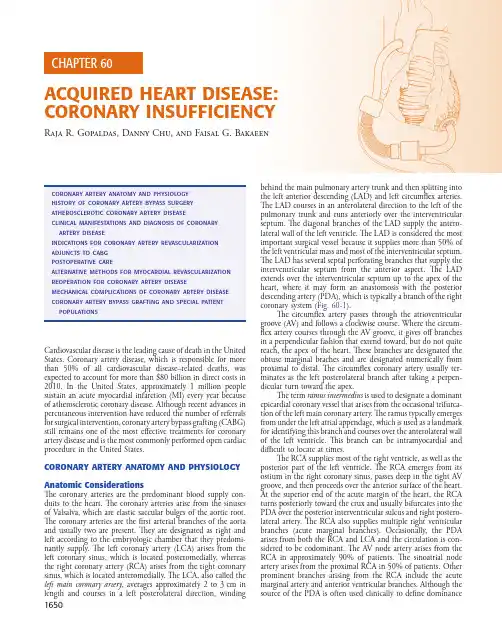
1650Cardiovascular disease is the leading cause of death in the United States. Coronary artery disease, which is responsible for more than 50% of all cardiovascular disease–related deaths, was expected to account for more than $80 billion in direct costs in 2010. In the United States, approximately 1 million people sustain an acute myocardial infarction (MI) every year because of atherosclerotic coronary disease. Although recent advances in percutaneous intervention have reduced the number of referrals for surgical intervention, coronary artery bypass grafting (CABG) still remains one of the most effective treatments for coronary artery disease and is the most commonly performed open cardiac procedure in the United States.CORONARY ARTERY ANATOMY AND PHYSIOLOGY Anatomic ConsiderationsThe coronary arteries are the predominant blood supply con-duits to the heart. The coronary arteries arise from the sinuses of Valsalva, which are elastic saccular bulges of the aortic root. The coronary arteries are the first arterial branches of the aorta and usually two are present. They are designated as right and left according to the embryologic chamber that they predomi-nantly supply. The left coronary artery (LCA) arises from the left coronary sinus, which is located posteromedially, whereas the right coronary artery (RCA) arises from the right coronary sinus, which is located anteromedially. The LCA, also called the left main coronary artery , averages approximately 2 to 3 cm in length and courses in a left posterolateral direction, winding behind the main pulmonary artery trunk and then splitting into the left anterior descending (LAD) and left circumflex arteries. The LAD courses in an anterolateral direction to the left of the pulmonary trunk and runs anteriorly over the interventricular septum. The diagonal branches of the LAD supply the antero-lateral wall of the left ventricle. The LAD is considered the most important surgical vessel because it supplies more than 50% of the left ventricular mass and most of the interventricular septum. The LAD has several septal perforating branches that supply the interventricular septum from the anterior aspect. The LAD extends over the interventricular septum up to the apex of the heart, where it may form an anastomosis with the posterior descending artery (PDA), which is typically a branch of the right coronary system (Fig. 60-1).The circumflex artery passes through the atrioventricular groove (AV) and follows a clockwise course. Where the circum-flex artery courses through the AV groove, it gives off branches in a perpendicular fashion that extend toward, but do not quite reach, the apex of the heart. These branches are designated the obtuse marginal braches and are designated numerically from proximal to distal. The circumflex coronary artery usually ter-minates as the left posterolateral branch after taking a perpen-dicular turn toward the apex.The term ramus intermedius is used to designate a dominant epicardial coronary vessel that arises from the occasional trifurca-tion of the left main coronary artery. The ramus typically emerges from under the left atrial appendage, which is used as a landmark for identifying this branch and courses over the anterolateral wall of the left ventricle. This branch can be intramyocardial and difficult to locate at times.The RCA supplies most of the right ventricle, as well as the posterior part of the left ventricle. The RCA emerges from its ostium in the right coronary sinus, passes deep in the right AV groove, and then proceeds over the anterior surface of the heart. At the superior end of the acute margin of the heart, the RCA turns posteriorly toward the crux and usually bifurcates into the PDA over the posterior interventricular sulcus and right postero-lateral artery. The RCA also supplies multiple right ventricular branches (acute marginal branches). Occasionally, the PDA arises from both the RCA and LCA and the circulation is con-sidered to be codominant. The AV node artery arises from the RCA in approximately 90% of patients. The sinoatrial node artery arises from the proximal RCA in 50% of patients. Other prominent branches arising from the RCA include the acute marginal artery and anterior ventricular branches. Although thesource of the PDA is often used clinically to define dominanceACQUIRED HEART DISEASE: CORONARY INSUFFICIENCYRaja R. Gopaldas, Danny Chu, and Faisal G. BakaeenAcquired HeArt diseAse: coronAry insufficiency Chapter 60 1651systems—the coronary sinus and its tributaries, the anterior right ventricular veins, and the thebesian veins. The coronary sinus predominantly drains the left ventricle and receives 85% of coronary venous blood. It lies within the posterior AV groove and empties into the right atrium. The anterior right ventricular veins travel across the right ventricular surface to the right AV groove, where they enter directly into the right atrium or form the small cardiac vein, which enters into the right atrium directly or joins the coronary sinus just proximal to its orifice. The the-besian veins are small venous tributaries that drain directly into the cardiac chambers and exit primarily into the right atrium and right ventricle. Understanding the anatomy of the coronary sinus is essential for placing the retrograde cardioplegia cannula during cardiopulmonary bypass.Physiology and Regulation of Coronary Blood FlowAortic pressure is a driving force in the maintenance of myocar-dial perfusion. During resting conditions, coronary blood flow is maintained at a fairly constant level over a wide range of aortic perfusion pressures (70 to 180 mm Hg) through the process of autoregulation.Because the myocardium has a high rate of energy use, normal coronary blood flow averages 225 mL/min (0.7 to 0.9 mL/g of myocardium/min) and delivers 0.1 mL/g/min of oxygen to the myocardium. Under normal conditions, more than 75% of the delivered oxygen is extracted in the coronary capillary bed, so any additional oxygen demand can only be met by increasing the flow rate. This highlights the importance of unobstructed coronary blood flow for proper myocardial func-tion. Box 60-1 summarizes the unique features of coronary blood flow.In response to increased load, such as that caused by strenu-ous exercise, the healthy heart can increase myocardial blood flow fourfold to sevenfold. Increased blood flow occurs through several mechanisms. Local metabolic neurohumoral factors cause coronary vasodilation when stress and metabolic demand increase, thereby lowering the coronary vascular resistance. This results in increased delivery of oxygen-rich blood, mimicking the phenomenon of reactive hyperemia. When a transient occlu-sion to the coronary artery is released (e.g., during the perfor-mance of a beating heart operation), blood flow immediately rises to exceed the normal baseline flow and then gradually returns to its baseline level. The autoregulatory mechanism responsible is guided by several metabolic factors, including CO 2, O 2 tension, hydrogen ions, lactate, potassium ions, and adenosine. Of these, adenosine is one of the leading candidates in the autoregulatory mechanism. Adenosine, a potent vasodila-tor and a degradation product of adenosine triphosphate (ATP),of circulation in the heart, anatomists define it according to where the sinoatrial node artery arises. Table 60-1 summarizes the hierarchy of the coronary artery anatomy.All the epicardial conductance vessels and septal perforators from the LAD give rise to a multitude of branches, termed resistance vessels, which traverse perpendicularly into the ven-tricular wall. These vessels play a crucial role in oxygen and nutrient exchange with the myocardium by forming a rich plexus capillary network. The rich capillary plexus offers a low-resistance sink to allow for unimpeded increase of arterial blood flow when oxygen demand rises. This is important because the myocardial vascular bed extracts oxygen at its full capacity, even in low-demand circumstances, thereby allowing no margin for further oxygen extraction when demand is high.An intricate network of veins drains the coronary circula-tion and the venous circulation can be divided into threeFIGURE 60-1 Anatomy of normal coronary artery vasculature.RCPDAcuteLM CALAD Diag.OM1652 SeCtION XI cHestEpidemiologic evidence suggests that coronary artery ath-erosclerosis is closely linked to the metabolism of lipids, specifi-cally LDLc. The development of lipid-lowering drugs has resulted in a significant reduction in mortality. In one observa-tional study of patients who received statin therapy and were known to have coronary artery disease (CAD), statin treatment was associated with improved survival in all age groups.1 The greatest survival benefit was found in those patients in the highest quartile of plasma levels of high-sensitivity C-reactive protein (hs-CRP), a biomarker of inflammation and CAD.2 Animal and human studies have demonstrated that statin therapy also modifies the lipid composition within plaques by lowering the amount of LDLc and stabilizing the plaque through various mechanisms, including reduction in macro-phage accumulation, collagen degradation, reduction in smooth muscle cell protease expression, and decrease in tissue factor expression.PathogenesisThe primary cause of atherosclerotic coronary disease is endo-thelial injury induced by an inflammatory wall response and lipid deposition. There is evidence that an inflammatory response is involved in all stages of the disease, from early lipid deposition to plaque formation, plaque rupture, and coronary artery throm-bosis. Vulnerable or high-risk plaques that are prone to rupture are characterized by the following:1. A large, eccentric, soft lipid core 2. A thin fibrous cap3. Inflammation within the cap and adventitia4. Increased plaque neovascularity5. Evidence of outward or positive vessel remodelingThinner fibrous caps are at a higher risk for rupture, prob-ably because of an imbalance between the synthesis and degrada-tion of the extracellular matrix in the fibrous cap that results in an overall decrease in the collagen and matrix components (Fig. 60-2). Increased matrix breakdown caused by matrix degrada-tion by an inflammatory cell-mediated metalloproteinase oraccumulates in the interstitial space and relaxes vascular smooth muscle. This results in vasomotor relaxation, coronary vasodila-tion, and increased blood flow. Another substance that plays an important role is nitric oxide (NO), which is produced by the endothelium. Without the endothelium, coronary arteries do not autoregulate, suggesting that the mechanism for vasodilation and reactive hyperemia is endothelium-dependent.Extravascular compression of the coronaries during systole also plays an important role in the regulation of blood flow. During systole, the intracavitary pressures generated in the left ventricular wall exceed intracoronary pressure and blood flow is impeded. Hence, approximately 60% of the coronary blood flow occurs during diastole. During exercise. increased heart rate and reduced diastolic time can compromise flow time but this can be offset by vasodilatory mechanisms of the coronary vessels. Buildup of atherosclerotic plaques and fixed coronary occlusion significantly impair coronary blood compensatory mechanisms during increased heart rates. This forms the basis for exercise-induced stress tests, in which increased activity or exercise unmasks underlying coronary disease.HISTORY OF CORONARY ARTERY BYPASS SURGERYOne of the first attempts at myocardial revascularization was made by Dr. Arthur Vineberg from Canada. He operated on a series of patients who presented with symptoms of myocardial ischemia and implanted the left internal mammary artery into the myocardium by creating a pocket. The operation did not entail a direct anastomosis to any coronary vessel and was performed on a beating heart through a left anterolateral thora-cotomy. Dr. Michael DeBakey performed a successful aortocoro-nary saphenous vein graft in 1964. Dr. Mason Sones, who is credited with inventing cardiac catheterization, helped establish coronary artery bypass surgery as a planned and consistent therapy in patients with angiographically documented coronary artery disease.The development of the heart-lung machine and demon-stration of successful clinical use by Dr. John Heysham Gibbon in the 1950s and the advancement of cardioplegia techniques in later years by Dr. Gerald Buckberg allowed surgeons to perform coronary anastomosis on an arrested (nonbeating) heart with a relatively bloodless field, thus increasing the safety and accuracy of the coronary bypass. In the 1990s, the advent of devices that could atraumatically stabilize the heart provided another pathway for the development of off-pump techniques of myocardial revascularization. T oday, an armamentarium of techniques, ranging from conventional on-pump CABG to minimally inva-sive robotic and percutaneous approaches, is available to manage coronary artery disease. Table 60-2 summarizes the timeline of major historical events in the development of surgery for myo-cardial revascularization.ATHEROSCLEROTIC CORONARY ARTERY DISEASE Coronary atherosclerosis is a process that begins early in the patient’s life. Epicardial conductance vessels are the most suscep-tible and intramyocardial arteries, the least. Risk factors for atherosclerosis include elevated plasma levels of total cholesterol and low-density lipoprotein cholesterol (LDLc), cigarette smoking, hypertension, diabetes mellitus, advanced age, low plasma levels of high-density lipoprotein cholesterol (HDLc), and a family history of premature coronary artery disease.Acquired HeArt diseAse: coronAry insufficiency Chapter 60 1653CLINICAL MANIFESTATIONS AND DIAGNOSIS OF CORONARY ARTERY DISEASEClinical PresentationThe most common presenting symptom of CAD is angina. It may be accompanied by dyspnea or mistaken for a gastrointes-tinal disturbance. The symptoms typically are exacerbated or incited by effort but subsequently resolve with rest. Unstable angina encompasses resting angina, new-onset angina, and accel-erated angina and is usually indicative of severe ischemia and impending MI. However, not all cases of angina are necessarily indicative of CAD, because disease processes from other systems can closely mimic those of angina. Approximately 15% of patients with CAD do not present with angina.The term acute coronary syndrome (ACS) has evolved to refer to a constellation of clinical symptoms that represent myo-cardial ischemia. It encompasses both ST-segment elevation MI (STEMI) and non–ST-segment elevation MI (NSTEMI). MI often presents as crushing chest pain that may be associated with nausea, diaphoresis, anxiety, and dyspnea. Symptoms of hypo-perfusion may also include dizziness, fatigue, and vomiting. Heart rate and blood pressure may be initially normal, but both increase in response to the duration and severity of pain. Loss of blood pressure is indicative of cardiogenic shock and indicates a poorer prognosis. At least 40% of the ventricular mass mustreduced production of extracellular matrix results in thinner fibrous caps. Not all plaque ruptures are symptomatic; whether they are is dependent on the thrombogenicity of the plaque’s components. Tissue factor within the lipid core of the plaque, secreted by activated macrophages, is one of the most potent thrombogenic stimuli. Rupture of a vulnerable plaque may be spontaneous or caused by extreme physical activity, severe emotional distress, exposure to drugs, cold exposure, or acute infection.Fixed Coronary ObstructionsMore than 90% of patients with symptomatic ischemic heart disease have advanced coronary atherosclerosis caused by a fixed obstruction. Atherosclerotic plaques of the coronary arteries are concentric (25%) or eccentric (75%). Eccentric lesions compro-mise only a portion of the lumen; through vascular remodeling, the arterial lumen may remain patent until late in the disease process. The impact of an arterial stenosis on coronary blood flow can be appreciated in the context of Poiseuille’s law. Reduc-tions in luminal diameter up to 60% have minimal impact on flow but when the cross-sectional area of the vessel has decreased by 75% or more, coronary blood flow is significantly compro-mised. Clinically, this loss of flow often coincides with the onset of exertional angina. A 90% reduction in luminal diameter results in resting angina.FIGURE 60-2 components of atherosclerotic plaque. thinning of the fibrous cap eventually results in plaque rupture with extrusion of highly thrombogenic lipid laden material into the coronary artery. this causes an acute occlusion of the coronary artery resulting in myocardial infarc-tion. (Adapted from choudhury rP, fuster V, fayad ZA. Molecular, cellular and functional imaging of atherothrombosis. nature rev drug discov 3:913–925, 2004.)Modality TargetProcess MRIUltrasound PET ++––++++Flow-mediated vasodilation Endothelial dysfunctionAdhesion molecules Endothelial activation++++MacrophagesInflammation +–++++++++++MMPs Cathepsin +±––Lipid core Fibrous capαv β3 integrinFibrinPlatelets αIIb β3 integrin Tissue factor Proteolysis ApoptosisAngiogenesisThrombosis ThrombusFibrous capLipid-rich necrotic coreMonocyte recruitment↓NO productionAngiogenesisInternal elasticlaminaLDLFoam cell Fibrin Endothelial cell VCAM1, ICAM, selectinsCollagen fibril Smooth muscle cellApoptotic cell PlateletMMPApproximate American HeartAssociation lesion stage I II III IV V VIαv β3 integrin1654 SeCtION XI cHestChest RadiographyThe chest radiograph is helpful in identifying causes of chest discomfort or pain other than CAD. Chest radiography does not detect CAD directly; it only identifies sequelae, such as cardiomegaly, pulmonary edema, and pleural effusions, that are indicative of heart failure. Evidence of calcification in the coro-nary arteries, although suggestive of CAD, is not reflective of the severity of the disease.Resting ElectrocardiographyA 12-lead resting electrocardiogram (ECG) should be obtained in patients suspected of having CAD or its sequelae. The ECG is evaluated for evidence of left ventricular hypertrophy, ST-segment depression or elevation, ectopic beats, or Q waves. In addition, arrhythmias (atrial fibrillation or ventricular tachy-cardia) and conduction defects (left anterior fascicular block, right bundle branch block, left bundle branch block) are sug-gestive of CAD and MI. Persistent ST-segment elevation or an evolving Q wave is consistent with myocardial injury and ongoing ischemia. Fifty percent of patients have normal electro-cardiographic results despite having significant CAD, and 50% of ECGs obtained during chest pain at rest will be normal, indicating the inaccurate nature of the test.Risk Stratification and Further TestingBased on age, clinical history, symptomatology, physical signs, and diagnostic tests, CAD patients are classified as low, interme-diate, or high risk. Such stratification enables the clinician to determine the intensity of medical therapy and timing of coro-nary angiography.Low- to intermediate-risk patients treated early and with a conservative strategy may undergo stress testing for further risk stratification. The choice to conduct stress testing depends on the patient’s resting ECG and ability to perform exercise.An exercise stress ECG is helpful in unmasking underlying CAD and is a more reliable screening test than a resting ECG in patients older than 40 years. The Bruce protocol is the most commonly used standardized treadmill exercise protocol. The protocol involves five 3-minute bouts of treadmill exercise, each designed to elicit greater myocardial oxygen demand than the last, to determine the patient’s ischemic threshold. A typical protocol requires the patient to expend about 12 metabolic equivalents (METs) of energy to ensure a complete test. A posi-tive exercise ECG may show progressive flattening of the ST segment or ST-segment depression as exercise progresses. During the recovery phase, ST depression may persist, with downslop-ing segments and T wave inversion. Additional findings associ-ated with an adverse prognosis and the presence of multivessel occlusive disease include a duration of symptom-limited exercise of less than 6 METs, the failure of systolic blood pressure to increase to more than 120 mm Hg, and the appearance of ven-tricular arrhythmias. For detection of CAD, the sensitivity and specificity of an exercise ECG approach 70% and 80%, respec-tively (Box 60-3).Conditions that preclude accurate interpretation of the stress ECG include digoxin therapy, widespread resting ST- segment depression (≥1 mm), left ventricular hypertrophy, left bundle branch block, and other conduction abnormalities. For patients with these conditions and those unable to exercise, a pharmacologic stress test with an imaging modality using a radionuclide agent such as thallium or sestamibi, multiple-gatedbe involved for cardiogenic shock to occur. The first manifesta-tion of CAD in 40% of patients is sudden onset of a nonper-fusing ventricular rhythm, such as ventricular tachycardia or fibrillation.The prehospital mortality rate for an acute MI (AMI) is approximately 50%. Of those patients who reach the hospital, another 25% die during the hospital stay and another 25% die in the first year afterward.3,4 Mechanical complications of MI include acute ventricular septal defect (VSD), papillary muscle rupture, and free ventricular rupture. They usually occur approx-imately 7 to 10 days after the initial MI.Physical ExaminationSome clinical findings are generic and are related to the systemic manifestations of atherosclerosis. Eye examination may reveal a copper wire sign, retinal hematoma or thrombosis secondary to vascular occlusive disease, and hypertension. Corneal arcus and xanthelasma are features noticed in cases of hypercholesterol-emia. Other clinical manifestations are caused by sequelae of CAD, as noted in Box 60-2.A thorough vascular evaluation is essential for any patient who presents with coronary disease because atherosclerosis is a systemic process. In addition, if surgery is being planned, the extremities should be evaluated for any previous surgical scars or fractures that could potentially preclude vein harvest.Diagnostic TestingBiochemical StudiesPatients suspected of having an ACS should undergo appropri-ate blood testing. Levels of creatinine kinase muscle and brain subunits (CK-MB) and troponin T or I should be assessed at least 6 to 12 hours apart. Additional laboratory tests include a complete blood count (CBC), comprehensive metabolic panel, and lipid profile (total cholesterol, triglycerides, LDLc, HDLc). Elevated brain natriuretic peptide (BNP) and CRP levels suggest a worse outcome.Acquired HeArt diseAse: coronAry insufficiency Chapter 60 1655Multidetector Computed TomographyMultidetector computed tomography (MDCT), one of the most recent imaging modalities, allows imaging of the coronary arter-ies, especially of coronary artery bypass grafts. Studies have indicated that the sensitivity and specificity MDCT approach or exceed those of other noninvasive methods of visualizing the coronary artery anatomy.5 MDCT is especially useful for imaging proximal CAD and coronary artery bypass grafts. More recent technology improves on conventional MDCT by adding more arrays to the imaging process; 128-slice MDCT arrays are cur-rently available. These scanners can acquire myocardial images within 1 second while exposing the patient to less radiation than traditional scanners. Although it is still preferable that patients have relatively low heart rates during imaging (to reduce arti-fact), the technology has significantly advanced and produces images on par with those generated by the gold standard, con-ventional angiography.6Magnetic Resonance Imaging and Gadolinium Magnetic Resonance ImagingMyocardial first-pass perfusion magnetic resonance imaging (MRI) has been considered a good alternative to nuclear cardiac ischemia and viability testing. However, the procedure has not gained widespread popularity because special training and exper-tise are required to perform this type of imaging and interpret the results.Cardiac Catheterization and InterventionCardiac catheterization remains the gold standard for evaluating the anatomy of the coronary arteries. High-quality coronary angiography is essential for identifying CAD and assessing its extent and severity.Cardiac catheterization is commonly performed by insert-ing a short, self-sealing vascular sheath into either femoral artery. Vascular access may also be obtained via a brachial or radial artery. Angiography is done by using hollow preshaped catheters (5 or 6 Fr), which are placed under fluoroscopic guidance ret-rograde through the aorta into the ostia of the coronary arteries and coronary bypass grafts. A solution of radiographic contrast material is injected through the catheter to opacify the lumen. Images are recorded in rapid succession onto film or in a digital format. The surgeon typically uses the coronary angiography images to determine the number and location of coronary targets where bypass anastomoses are to be constructed (Figs. 60-3, 60-4, and 60-5).Other information obtained from cardiac catheterization includes coronary and aortic calcification, ventricular function, and, if ventriculography is performed, mitral regurgitation. Injection of contrast into the aortic root provides useful root and ascending aortic images when indicated.Right heart catheterization is used to measure central venous, right atrial, right ventricular, pulmonary artery, and pulmonary wedge pressures, as well as cardiac output. It can also be used to identify intracardiac shunts, assess arrhythmias, and initiate temporary cardiac pacing. Preoperative right heart catheterization is used selectively and is generally not necessary unless right ventricular dysfunction or pulmonary vascular disease is suspected.Percutaneous coronary intervention (PCI) techniques in current use include balloon dilation, stent-supported dilation, atherectomy, and plaque ablation with a variety of devices,acquisition [MUGA] scanning, or positron emission tomogra-phy (PET) should be considered. Echocardiography may be considered as an alternative. Pharmacologic stress agents include adenosine, dobutamine, and dipyridamole.EchocardiographyMany patients undergoing CABG also undergo transthoracic echocardiography by the evaluating cardiology team to estimate ventricular wall abnormalities and the ejection fraction. Common indications for a resting echocardiogram include heart murmurs and a suspicion of a structural problem, such as aortic stenosis or insufficiency, hypertrophic cardiomyopathy, mitral valve stenosis or regurgitation, and congestive heart failure. Ven-tricular dilation and wall thinning are other features noted on the echocardiogram in patients with chronic ischemic CAD or prior infarcts.1656 SeCtION XI cHestinsignificant problems, the greatest cause of lumen loss in stented coronary arteries is neointimal hyperplasia. This is the principal mechanism of in-stent stenosis and results from inappropriate cell proliferation—hence, the advent of cytotoxic drug-eluting stents.INDICATIONS FOR CORONARY ARTERY REVASCULARIZATIONBox 60-4 summarizes the indications for myocardial revascular-ization. The first four indications are managed preferably by PCI, whereas indications 5 through 7 are managed preferably by surgical revascularization. The last two indications constitute surgical emergency. Although this stratification is broad and provides a bird’s eye view of the management approach, each patient should be risk-stratified before an appropriate strategy is initiated. When possible, proper risk stratification is absolutely essential to determine the balance of risks and benefits of medical management, PCI, and CABG.Chronic Stable AnginaCardiovascular risk reduction strategy is essential to treating patients with chronic stable angina. In the 2007 focused update of the 2002 American Heart Association (AHA)/American College of Cardiology (ACC) guidelines 7 for managing chronic stable angina, cardiovascular risk reduction strategies includedFIGURE 60-3 Left coronary angiogram demonstrating hemodynami-cally severe lesions in the left anterior descending artery (small arrow) and the circumflex artery (large arrow).FIGURE 60-4 right coronary angiogram demonstrating hemodynam-ically significant lesions (arrow). the right coronary artery terminatesas a posterior descending artery in the right dominant system.thrombectomy with aspiration devices, specialized imaging, and physiologic assessment with intracoronary devices.Coronary artery stents were the first substantial break-through in the prevention of restenosis after angioplasty. Although stent recoil or compression are not completelyFIGURE 60-5 coronary angiogram demonstrating critical left main coronary artery stenosis (arrow).。
心梗后室间隔穿孔的治疗进展张亮;刘东海;罗宏;谌启辉;乔晨辉【期刊名称】《河南医学研究》【年(卷),期】2013(022)001【总页数】3页(P144-146)【作者】张亮;刘东海;罗宏;谌启辉;乔晨辉【作者单位】郑州大学第一附属医院心血管外科河南郑州450052;郑州大学第一附属医院心血管外科河南郑州450052;郑州大学第一附属医院心血管外科河南郑州450052;郑州大学第一附属医院心血管外科河南郑州450052;郑州大学第一附属医院心血管外科河南郑州450052【正文语种】中文室间隔穿孔是急性心梗后少见的严重并发症,在急性心梗病人中继发室间隔穿孔的发病率大约为1%~2%[1],从心梗发生到发生穿孔平均时间为2~4 d,最早可发生于心梗后几小时,最迟见于心梗后2周[2,3]。
但随着积极的药物治疗、迅速有效的控制患者血压和急诊溶栓技术、介入治疗技术的临床应用,心梗后室间隔穿孔的总体发病率降低至0.24%[4],但值得注意的是,在开展溶栓治疗之后室间隔穿孔平均发生时间提前到心肌梗死后的1 d左右[5]。
一旦发病,短时间内会导致心功能衰竭、心源性休克而致死,预后极差。
及时闭合穿孔是改善这类患者预后的唯一有效方法。
本文就近些年急性心梗后室间隔穿孔的治疗方法及时机进行综述。
1 自然病程在保守治疗的心梗后室间隔穿孔的病人中,将近24%的患者死于发病后的24 h内,46%死于1周内,67%~82%死于2月内,只有5%~7%的患者能够存活超过 1 a[6]。
据 Lemery 等[7]人报道,25 例心梗后室间隔穿孔病人经内科保守治疗,其中19人在1月内死亡。
有报道称极少数的室间隔穿孔患者未经治疗存活14 a[8]。
一项多中心的研究跟踪了55例由于心梗后室间隔穿孔伴发心源性休克的患者。
其中24例患者行内科保守治疗,剩下的31例患者构成了高危手术组。
最终只有7例患者存活,其中6例为手术修复了缺损的病人[9]。
心肌梗塞的英语English:A myocardial infarction, commonly known as a heart attack, occurs when the blood flow to a part of the heart is blocked, leading to damage or death of the heart muscle cells. This blockage is typically caused by a buildup of plaque in the coronary arteries, which restricts the flow of oxygen-rich blood to the heart. The symptoms of a heart attack can vary but often include chest pain or discomfort, shortness of breath, nausea, and lightheadedness. Immediate medical treatment is crucial to prevent further damage to the heart, and may include medications to dissolve the clot, angioplasty to open the blocked artery, or coronary bypass surgery to restore blood flow to the heart muscle. Long-term management may involve lifestyle changes, such as diet modification and exercise, as well as medications to control blood pressure and cholesterol levels.中文翻译:心肌梗塞,通常称为心脏病发作,是指心脏部分区域的血流被阻塞导致心肌细胞受损或死亡。
血浆脑钠肽在急性冠状动脉综合征的诊断及预后评估中的作用观察陈军;徐任璇【摘要】Objective: To study the roles of brain natriuretic peptide (BNP) in diagnosis and prognostic evaluation of patients with acute coronary syndrome(ACS). Methods:The levels of BNP were detected in 54 patients with acute myocardial infarction(AMI),35 patients with unstable angina pectoris(UAP) ,20 patients with stable angina pectoris(SAP) and 20 healthy volunteers as controls.The correlations were compared between the number of impaired coronary arteries, the lesions of left main coronary artery, the Gensini scores of coronary artery and the levels of BNP respectively. The mortality of the patients with ACS in hospital at 30 days and 3 months,and the major adverse cardiac events ( MACE ), cardiogenic death, re - myocardial infarction, recurrent angina, consequential heart failure and the composite endpoint rates of readmission were analyzed. Results:The levels of BNP in group AMI and group UAP were significantly higher than those in group SAP and controls(P <0. 01 ) ,and the level of BNP in group AMI was significantly higher than it in group UAP( P < 0. 01 ). Multivariate logistic regression analysis showed that, the level of plasma BNP was independent with the risk factors of coronary heart disease, such as age, gender, family history, smoking, hyperlipidemia, high blood pressure, diabetes, and so on,but it was associated with mortality and rates MACE ( P < 0. 05 - P < 0.01 ). Conclusions: The levels of BNP inpatients with ACS increase significantly and are associated with degrees of coronary artery disease and myocardial ischemia. The change of plasma BNP is an independent predictor for mortality and incidence of MACE in hospital at 30 days and 3 months among ACS patients.%目的:探讨血浆脑钠肽(BNP)水平变化在急性冠状动脉综合征(ACS)诊断及预后评估中的作用.方法:检测54例急性心肌梗死(AMI组)患者、35例不稳定型心绞痛(UAP组)患者、20例稳定型心绞痛(SAP组)患者以及20名健康体检者(对照组)血浆BNP水平;比较冠状动脉病变支数、左主干病变及冠状动脉Gensini评分与BNP的相关性,并随访患者住院期间及出院后30天、3个月病死率,以及主要心脏不良事件(MACE)、心源性死亡、再次心肌梗死、再发心绞痛、继发心力衰竭和再入院的复合终点发生率.结果:AMI组、UAP组的BNP水平显著高于SAP组和对照组(P<0.01),AMI组BNP 水平显著高于UAP组(P<0.01);冠状动脉3支或左主干病变患者BNP水平均显著高于1支和2支病变(P<0.01),2支病变与3支或左主干病变差异亦有统计学意义(P<0.01).血浆BNP水平独立于年龄、性别、家族史、吸烟、高脂血症、高血压、糖尿病等冠心病危险因素,与出院后30天、3个月病死率独立相关(P<0.01).结论:ACS患者BNP水平明显升高,并与其冠状动脉病变及心肌缺血程度密切相关.血浆BNP水平变化可能独立于各因素预测ACS患者30天和3个月病死率及MACE 发生率.【期刊名称】《蚌埠医学院学报》【年(卷),期】2011(036)006【总页数】4页(P621-624)【关键词】急性冠状动脉综合征;脑钠肽;诊断;预后评估【作者】陈军;徐任璇【作者单位】上海市杨浦区安图医院,心内科,200093;上海市杨浦区安图医院,心内科,200093【正文语种】中文【中图分类】R541.4急性冠状动脉综合征(acute coronary syndrome,ACS)是严重威胁人类健康的一类急性心血管事件,包括不稳定性心绞痛(unstable angina pectoris,UA)、非ST段抬高性心肌梗死(non-ST segment elevationmyocardial infarction,NSTEMI)和ST段抬高性心肌梗死(ST segment elevationmyocardial infarction,STEMI),以及以上各病症导致的猝死。
急性冠脉综合征患者血清降钙素原、D-二聚体水平测定张晋东;杨海波;赵晓燕;赵荫涛;王小芳;李凌【期刊名称】《郑州大学学报(医学版)》【年(卷),期】2015(000)002【摘要】目的:检测急性冠脉综合征(ACS)患者血清降钙素原、D-二聚体水平,探讨二者与ACS患者冠状动脉病变程度的关系。
方法:根据病情严重程度将因ACS入院的患者分为不稳定型心绞痛组( UAP组,72例)、急性心肌梗死组( AMI组,30例),另选取同期行冠状动脉造影、结果正常的20例患者作为对照组。
采用ELISA法测定血清降钙素原、D-二聚体水平。
分析血清降钙素原、D-二聚体水平与病变支数、Gensini积分的关系。
结果:AMI组血清降钙素原、D-二聚体水平高于UAP组及对照组(F=3.298、5.082,P<0.05),UAP组与对照组血清降钙素原、D-二聚体水平差异无统计学意义(P>0.05)。
UAP组血清降钙素原、D-二聚体水平与Gensini积分无关(P>0.05),AMI组血清D-二聚体水平与Gensini积分呈正相关(r=0.523,P<0.05)。
结论:ACS患者血清降钙素原水平与冠状动脉内的炎症反应及斑块的稳定性有关,而D-二聚体水平与冠状动脉狭窄的严重程度有关。
%Aim:To determine the serum levels of procalcitonin and D-dimer in patients with acute coronary syndrome (ACS) and investigate the association between ACS and the 2 parameters.Methods:All patients with ACS were classified into unstable angina pectoris(UAP)group(n=72) and acute myocardial infarction(AMI) group(n=30),and individuals without coronary heart disease were chosenas the control group ( n =20 ) .Serum procalcitonin and D-dimer levelswere measured by ELISA .The correlations between serum procalcitonin , D-dimer levels and the numbers of impaired coronary arteries,Gensini scores of coronary stenosis were analyzed respectively .Results:The levels of serum procalcitonin and D-dimer in AMI group were significantly higher than those in UAP group and control group (F=3.298 and 5.082,P<0.05), and there was no significant difference between UAP group and control group .There was positive correlation between the D-dimer level and Gensini scores in the AMI group (r=0.523,P<0.05),while there were no correlations between the levels of procalcitonin or D-dimer with Gensini scores in the UAP group (P>0.05).Conclusion:In patients with ACS, the lev-el of serum procalcitonin correlates with the inflammatory response of coronary artery and the stability of plaques , and serum D-dimer level relates to the stenosis severity of coronary artery .【总页数】4页(P267-270)【作者】张晋东;杨海波;赵晓燕;赵荫涛;王小芳;李凌【作者单位】郑州大学第一附属医院心内科郑州450052;郑州大学第一附属医院心内科郑州450052;郑州大学第一附属医院心内科郑州450052;郑州大学第一附属医院心内科郑州450052;郑州大学第一附属医院心内科郑州450052;郑州大学第一附属医院心内科郑州450052【正文语种】中文【中图分类】R543.3【相关文献】1.慢性阻塞性肺疾病合并不成比例肺动脉高压患者血浆D-二聚体水平测定及分析[J], 李晶;孙俊生;卓宋明;申严2.急性早幼粒细胞白血病患者血浆D-二聚体水平测定 [J], 杨艳辉3.胃癌患者手术前后外周血D-二聚体与CA724水平测定及意义 [J], 彭方兴;袁三英;吴宸;陈进;罗亮;陈汇4.急性生理学与慢性健康状况评分Ⅱ联合血清D-二聚体、肌钙蛋白Ⅰ及脑钠肽水平测定对慢性阻塞性肺疾病患者预后评估价值 [J], 罗玉爱;王捷;李贤英5.类风湿关节炎患者血浆D-二聚体水平测定及其临床意义 [J], 付利然;杜转敏;杨毛吉因版权原因,仅展示原文概要,查看原文内容请购买。
出现心绞痛,但冠脉没阻塞?3步搞定这种临床常见难点!冠脉造影发现无明显阻塞的胸痛该做哪些检查?如何治疗?看国际大咖发言。
出现胸痛、心绞痛,但到医院做冠脉造影检查发现没有出现明显阻塞,之后又反复出现这些症状,该怎么办?是不是得考虑去看其他科室。
未必,这时你可能有必要做进一步检查。
近日,Udo Sechtem教授在2020年欧洲心脏病学会(ESC)年会上提出了胸痛伴非阻塞性冠状动脉疾病的诊断、治疗与预后。
这个病很常见,发病占比超过阻塞性冠脉疾病在2019年ESC慢性冠状动脉综合征指南中提到,根据常见症状如胸痛和/或呼吸困难的发生,可以预测阻塞性冠状动脉疾病的发生率。
但是,我们看到即便有典型的胸痛,其实大部分年龄段人群出现冠状动脉疾病的发生率都不到50%,因此,Udo Sechtem教授表示非阻塞性冠状动脉疾病引起的胸痛占了更主要的原因。
表1 不同年龄阶段心绞痛、呼吸困难与冠状动脉疾病发生的关系这该如何解释?首先来了解一下冠状动脉微血管的概念。
它是直径在10-300 μm 的血管,是内皮细胞调节冠脉血流和心肌细胞营养交换的部位,是心脏行使正常生理功能的基本保证。
不过,由于目前冠脉造影只能检测到约500 μm直径的血管,所以不同于大中型冠状动脉,这些冠状动脉微小血管不能被冠脉造影所检测。
这些微小血管出现功能障碍而导致胸痛,现有的冠脉造影无法发现时,就是我们今天要谈的“非阻塞性冠脉疾病”。
图1 冠状动脉微血管的结构图微血管功能障碍和/或心外膜冠状动脉痉挛导致心肌需氧量和血液供应不匹配,是非阻塞性冠状动脉疾病的主要病理机制。
冠脉造影都无法发现,我们要如何诊断?根据今年7月欧洲经皮心血管介入协会(EAPCI)联合欧洲心脏病学会(ESC)发布首部关于缺血伴非阻塞性冠状动脉疾病(INOCA)的专家共识,目前评估缺血的无创技术为心肌单光子发射CT或多巴胺负荷超声心动图,但如果缺血影响到整个心室则以上方法无效。
因此,Udo Sechtem教授推荐使用有创评估法,分为以下三步:①冠状动脉造影;②基于导丝的诊断及腺苷测试。
血引起传导障碍也可使QRS波轻微增宽及QT间期相应延长,David等在犬实验性超急性期心肌缺血模型中,从 Frank导联记录R波振幅及心室内传导时间,在结扎冠状动脉后开始 2~3min内缺血区传导速度呈同步双相反应,初始30s缺血区心室传导加速,R波振幅之和(∑RWA)降低,于第二相时缺血区心室传导减慢,∑RWA增大,提示急性心肌缺血时,R波振幅取决于心室内的传导速度,而不单是血流动力学改变。
Barnhil等对5例变异型心绞痛患者于心绞痛发作时记录正交导联心电图,同时对7只实验性急性心肌缺血模型犬进行电生理检查,观察缺血区R波振幅变化。
结果发现,QRS波振幅变化与心肌内传导速度密切相关,强烈提示变异型心绞痛发作时,缺血区心肌传导速度减慢,引起心室终末除极延迟,最终导致QRS波终末 40ms电压增高。
图 1 急性心肌梗死超急性期,心电图表现缺血周围传导阻滞。
IABP在PCI中的临床应用现状刘相勇【摘要】主动脉内球囊反搏(IABP)是一种重要的机械循环支持装置,能有效增加心排血量、降低后负荷、增加冠状动脉灌注,改善缺血性胸痛和限制心肌梗死的范围.随着主动脉内气囊泵的器械和装置不断更新,质量不断改善与提高,应用范围不断扩大,并发症显著下降,对行经皮冠状动脉介入治疗(PCI)的高危患者,尤其是PCI术前、术中及术后出现血流动力学不稳定者尤为重要,但对于在PCI患者中应用IABP的时机及疗效存在分歧.%Intra aortic balloon pump( IABP )is a kind of important mechanical circulation support device , which can effectively increase the blood discharge, reduce aiterload , increase the coronary artery perfu-sion, improve the ischemic chest pain and limit the scope oi myocardial infarction. Along with intiaaoitic balloon pumps equipment and device constantly updating and continuous impiovementin the quality,the application scope has been expanding unceasingly, and the complications have decreased significantly. As to the percutaneous coronary intervention(PCI )high-iisk patients,especially in patients with PCI preoperative, in-tiaopeiative and postoperative hemodynamic instability, IABP is particularly important, while there are still controversies in timing and therapeutic effect oi IABP in PCI patients.【期刊名称】《医学综述》【年(卷),期】2012(018)012【总页数】3页(P1861-1863)【关键词】主动脉内球囊反搏;循环支持;介入治疗【作者】刘相勇【作者单位】河南科技大学第一附属医院心内科,河南,洛阳,471003【正文语种】中文【中图分类】R473主动脉内球囊反搏(intra aortic balloon pump,IABP)是一种重要的机械循环辅助装置,在临床工作中已应用多年。
Original paperCorresponding author:Ferhat Ozyurtlu MD, Special Grand Medical Hospital, 45030 Manisa, Turkey, phone: +90 530 543 61 06, e-mail: fozyurtlu@ Received: 31.12.2013, accepted: 13.02.2014.The association between coronary slow flow and platelet distribution width among patients with stable angina pectorisFerhat Ozyurtlu 1, Veysel Yavuz 2, Nurullah Cetin 3, Halit Acet 4, Erkan Ayhan 5, Turgay Isik 51Special Grand Medical Hospital, Manisa, Turkey 2Akhisar State Hospital, Manisa, Turkey 3Ercis State Hospital, Van, Turkey 4Department of Cardiology, Dicle University Faculty of Medicine, Diyarbakır, Turkey 5Department of Cardiology, Balıkesir University Faculty of Medicine, Balıkesir, TurkeyPostep Kardiol Inter 2014; 10, 3 (37): 161–165DOI: 10.5114/pwki.2014.45142A bs t r a c tIntroduction: Coronary slow flow (CSF) is an angiographic phenomenon characterised by the delay of distal vessel opacification in the absence of significant stenosis of the epicardial coronary arteries. Some of the factors playing a role in CSF pathophysiology are increased thrombogenic activity and inflammation.Aim: To examine the relationship between platelet distribution width (PDW) and CSF.Material and methods: Taking into consideration the exclusion criteria, 136 patients with CSF and 152 patients with normal coronary angiographies (control group) were included in the study. The association between thrombolysis infarction frame count (TFC) in myocardial and laboratory and other clinical parameters were evaluated.Results: The stated parameters were significantly higher in the group with CSF than in the normal coronary angiography group (control group). The PDW (16.6 ±0.7 vs. 16.4 ±0.6, p = 0.002), neutrophil lymphocyte ratio (NLR) (3.1 ±3.4 vs. 2.4 ±1.1, p = 0.027), haemoglobin (Hb) (14.1 ±1.3 vs. 14.7 ±1.1, p < 0.001), and red cell distribution width (RDW) (13.6 ±0.7 vs. 14.1 ±2.8, p = 0.026) were significantly higher in the CSF group than in the control group. Moreover, our study showed that PDW > 16.15 and Hb > 1 3.75 were predictors of the presence of CSF with sensitivities of 83% and 73% and specificities of 40% and 42%, respectively.Conclusions: This study has demonstrated that compared to normal coronary flow, PDW, Hb, NLR, and RDW are significantly higher in CSF patients. We believe that further studies are needed to clarify the role of PDW and Hb in patients with CSF.Key words: coronary slow flow, platelet distribution width.IntroductionThe phenomenon of coronary slow flow (CSF) is an angiographic clinical entity characterised by delayed dis-tal vessel opacification in the absence of significant epi-cardial coronary stenosis [1]. Diagnostic criteria for CSF include the absence of coronary atherosclerosis. What is important here is the atherosclerosis plaque, which visually forms significant or non-significant stenosis. Clinical data indicates that CSF is present in approxi-mately 1–7% of coronary angiography screenings [2], and although not a particularly rare condition, the underlying pathophysiological mechanisms of CSF are poorly under-stood. Proposed aetiologies for CSF include small vessel disease, microvascular vasomotor dysfunction, diffuse atherosclerosis, endothelial dysfunction, inflammation,increased platelet aggregation, and factors related to anatomic variation [1, 3–6]. Recently-published data as-sociates CSF with poor prognostic outcomes, including cardiac dysfunction, acute coronary syndrome, fatal ar-rhythmias, and sudden cardiac death [5–8]. Platelet dis-tribution width (PDW) is a direct measure of the variation in platelet size and a marker of platelet activation [9]. A recent study demonstrated a significant association between coronary artery disease (CAD) and PDW. Inter-estingly, PDW has also been linked to saphenous vein graft patency among patients who underwent coronary artery bypass [10]. Haemoglobin (Hb) is a key determi-nant of blood viscosity [11]. Red cell distribution widthFerhat Ozyurtlu et al. The association between coronary slow flow and platelet distribution width in patients with stable CAD(RDW) is a direct measure of the variation in erythrocyte size that is easily measured as a component of routine blood counts [12]. The RDW is a well recognised indica-tor of chronic inflammation and oxidative stress, and elevated RDW is strongly associated with poor clinical outcomes among patients with CAD [13, 14]. Neutrophil/ lymphocyte ratio (NLR), derived from the white blood cell count (WBC), is a common prognostic indicator in cardio-vascular disease [15, 16].AimThe aim of the present study is to evaluate the rela-tionships between CSF, PDW, and other haematological parameters in an effort to identify useful clinical indica-tors in patients undergoing coronary angiography. Material and methodsPatient selectionA retrospective evaluation of consecutive patients undergoing coronary angiography was conducted. All pa-tients enrolled in the study underwent coronary angiog-raphy as a result of chest pain and objective signs of isch-aemia during treadmill exercises or myocardial SPECT testing. Routine laboratory and clinical parameters (e.g. diabetes mellitus (DM), hypertension (HT), hypercholes-terolemia, tobacco use, family history of cardiovascular disease) were obtained from the patient medical re-cords. Study exclusion criteria included coronary ectasia, mild-severe valve disease, heart failure, anaemia, renal failure, inflammatory diseases, malignancy, peripheral and cerebral arterial disease, thyroid gland dysfunctions (hypo-hyperthyroidism), and LV (left ventricle).EchocardiographyAll patients underwent transthoracic echocardiogra-phy performed using a system V (Vingmed, G E) device and a 2.5 MHz phased-array transducer. Recordings were made with the patients in the left lateral decubitus posi-tion. LV ejection fraction was measured using the modi-fied Simpson’s rule according to the most recent guide-lines.Coronary angiographyCoronary angiography was performed using a GE im-aging system (General Electric Advantx LC +, Milwkuee, Wisconsin, US). The standard selective coronary angiog-raphy procedure in our clinic includes at least four views of the left coronary system and two views of the right coronary artery using the Judkins technique and 6-French right and left heart catheters and no nitroglycerin. Iohex-ol (GE Healthcare Omnipaque 350 ml, Ireland) was used as the contrast agent for all patients and control subjects. Coronary flow rates were measured using the Myocardial Infarction (TIMI) frame count (TFC) method, with cinean-giography at 30 frames per second. Coronary angiograms included at least four images of the left cardiac system and two images of the right cardiac system. These are in the form of cranial and caudal angulations of the left and right oblique images. Images with the best resolution were used for TFC evaluations of the left coronary artery system, and TFC evaluations of the right coronary artery were performed with the left anterior image with cranial angulation. In the cases, invasive haemodynamic evalu-ations were performed during the coronary angiography. Therefore, haemodynamic changes resulting from cath-eterisation and vasovagal syndrome could be evaluated with pressure trace; data indicating slow flow as a result of catheterisation and vasovagal syndrome were exclud-ed. Coronary angiograms were assessed independently for objective quantification of coronary flow by two inva-sive cardiologists blinded to the clinical findings.Laboratory parametersPrior to coronary angiography, eight-hour postprandi-al venous blood was collected from all patients for rou-tine laboratory testing. Haematological measurements were made using a Mindray Haematology Analyser (BC-6800, China) and were evaluated for complete blood count (CBC). LDL cholesterol analysis was performed us-ing an Olympus AU 2700 Plus Chemistry-ImmunoAnaly-ser (USA).DefinitionsStable angina was defined as discomfort in the chest, jaw, shoulder, back, or arms, typically elicited by exer-tion or emotional stress, and relieved by rest or nitro-glycerin. In accordance with World Health Organization criteria, anaemia was defined as a baseline haemoglo-bin concentration < 13 mg/dl in men or < 12 mg/dl in women. Glomerular filtration rate (GFR) was estimated using the simplified Modification of Diet in Renal Disease Equation [17]. Renal insufficiency was defined as G FR < 60 ml/min/1.732 m2. The TFC was derived according to the methods of G ibson et al. [18]. The first frame was defined as the frame in which radiocontrast agent was first visualised in the ostial region of the coronary artery. The last frame was defined as the frame in which the radiocontrast agent reaches the distal index point of the relevant coronary artery. The LAD is longer than all other coronary arteries; therefore, the corrected TFC (cTFC) is the LAD frame number divided by 1.7. SCF was defined as cTFC greater than two standard deviations from the normal range (40.8 frames for LAD, 29.8 frames for LCx, and 27.3 frames for RCA), while normal coronary was defined as cTFC within two standard deviations of the normal range reported for a particular vessel. All study parameters were reviewed and approved by the Local Ethics Committee.Ferhat Ozyurtlu et al. The association between coronary slow flow and platelet distribution width in patients with stable CADStatistical analysisThe statistical package for social sciences (SPSS, ver-sion 15) was used for all data analysis. Continuous data are expressed as mean ± standard deviation (SD), and categorical data are reported as percentages. The Stu-dent’s t -test was used to compare continuous parametric variables. The χ2 test was used to compare distributions of categorical variables. Cut-off values of PDW and Hb concentration for the prediction of SCF and their re-spective sensitivity and specificity values were estimat-ed using receiving operating characteristic (ROC) curve analysis. The threshold of statistical significance was es-tablished at p < 0.05.ResultsThe study population consisted of 6280 consecu-tive patients undergoing coronary angiography. Out of the total population, 136 patients with SCF were includ-ed in the study group. The control group consisted of 152 age-matched subjects with normal coronary angio-grams selected consecutively during the same study pe-riod as the study group. The same exclusion criteria were applied to the study and control groups. The distribution of cardiovascular risk factors, demographic character-istics, and laboratory parameters in the two groups are shown in Table I. The mean age of the CSF group was 53 ±9 years with a male gender dominance of 61.03%. Among known CAD risk factors, diabetes mellitus and smoking history were more prevalent in the CSF group than in the control group (29% vs. 17%, p = 0.019 and 58% vs. 46%, p = 0.028, respectively, Table I). The PDW (16.6 ±0.7% vs. 16.4 ±0.6%, p = 0.002), NLR (3.1 ±3.4 vs. 2.4 ±1.1, p = 0.027), haemoglobin (14.1 ±1.3 g/dl vs. 14.7 ±1.1 g/dl, p < 0.001), and RDW (13.6 ±0.7% vs. 14.1 ±2.8%, p = 0.026) were significantly increased in the CSF group relative to the control group (Table II). A PDW of 16.15 predicted CSF with a sensitivity of 83% and a specificity of 40% (ROC AUC: 0.618, 95% CI: 0.554–0.683, p = 0.001) (Figure 1 A)Table I. Distribution of baseline characteristic ofall patientsic blood pressure, DBP – diastolic blood pressure, LAD – left anterior descend-ing coronary artery, LCx – left circumflex coronary artery, RCA – right coronary artery, TFC – TIMI frame count, cTFC – corrected TIMI frame countTable II . Distribution of the haematological para-meters of all casesblood cell distribution width, MPV – mean platelet volume, PDW – platelet dis-tribution width, NLR – neutrophil/lymphocyte ratioFigure 1. Receiver operating characteristics (ROC) analysis of PDW (A ) and Hb (B ) concentrationS e n s i t i v i t y1.00.80.60.40.20.00.00.2 0.4 0.60.8 1.0A1-SpecificityS e n s i t i v i t y1.00.80.60.40.20.00.00.2 0.4 0.60.8 1.0B1-SpecificityFerhat Ozyurtlu et al. The association between coronary slow flow and platelet distribution width in patients with stable CADand an Hb concentration of 13.75 g/dl predicted CSF witha sensitivity of 73% and a specificity of 42% (ROC AUC:0.625, 95% CI: 0.561–0.690, p < 0.001) (Figure 1 B). DiscussionIn this study we examined the relationship between CSF, PDW, and other haematological parameters. The CSF was independently associated with PDW, Hb, NLR, and RDW. Moreover, our study data demonstrate that PDW > 16.15% and Hb > 13.75 g/dl predict the presence of CSF with sensitivities and specificities of 83% and 73%, and 40% and 42%, respectively.A limited number of studies have been performed examining the pathophysiology of CSF since the first description of the disease by Tambe et al. in 1972. Sev-eral competing hypotheses explaining the aetiology of CSF have emerged. These include atherosclerosis and increased thrombogenic activity. Inflammation plays an important role in the onset, development, and progres-sion of atherosclerosis. Atherosclerosis is itself consid-ered an inflammatory disease. Microvascular atheroscle-rosis may contribute to the development of CSF. Recent studies have demonstrated the relationship between CSF and inflammation.Vagdatli et al. [19] have proposed that PDW is a more specific indicator of platelet activation than MPV in the absence of platelet swelling. Elevated PDW directly mea-sures the variability in platelet size during platelet dis-tension and serves as a marker of platelet activation [20]. Increased platelet number, size, and the presence of pseudopodia may influence PDW. Khandekar et al. reported a significant elevation of PDW among patients with acute myocardial infarction and unstable angina pectoris [21]. Our study data demonstrate a significant association between PDW and CSF. A study conducted by Jindal et al. identified a significant association between PDW and microvascular dysfunction among diabetic pa-tients [22]. The CSF may be a symptom of microvascular and circulatory dysfunction. Numerous factors contribute to microvascular and circulatory dysfunction, including coronary microvascular imbalance and increased tonus, endothelial thickening of small vessels and endothelial nitric oxide imbalance, and blood viscosity. Hb concentra-tion is a determinant of blood viscosity, and a significant relationship between CSF and Hb concentration has been demonstrated previously [11]. The SCF patients frequently present with elevated blood viscosity [23]. Similar to ath-erosclerosis, blood viscosity is elevated in SCF patients as a result of increased platelet adhesion to the suben-dothelium, elevated protein infiltration into the arterial wall, and alterations to local shear forces [24]. Our data supports a significant relationship between CSF and hae-moglobin concentration, a component of blood viscosity.The NLR is associated with the onset and progression of atherosclerosis in the coronary arteries [25], and re-cent studies suggest that NLR is an excellent indicator of cardiovascular disease [15, 16, 26]. As a result, NLR has emerged as a new prognostic indicator [16, 27]. Among patients with acute coronary syndrome, neutrophils are functionally activated, and the presence of localised neu-trophil infiltration in atherosclerotic lesions has been documented, suggesting that neutrophils play a role in the mediation and destabilisation of atherosclerotic plaques [28]. The present study demonstrates a signifi-cant correlation between the presence of CSF and NLR, an inflammatory marker linked to CAD and atheroscle-rosis.Chronic inflammation and neuro-humoral activation can act synergistically to elevate RDW, enhancing the atherosclerotic process [29]. The RDW is an independent predictor of mortality and coronary morbidity among pa-tients with myocardial infarction [13, 14]. Similar to the report by Kalay et al. [25], the present study confirms a significant association between CSF and RDW. A recent study by Akpinar et al. involving a comparable number of patients reported elevated PDW, RDW, and NLR similar to our CSF study group [30].The relationship between cardiovascular disease and increased platelet activity is well known. In this study, we found a significant relationship between CSF and PDW, an established indicator of platelet activity. In addition, we detected a significant relationship between CSF and NLR, an indicator of systemic inflammation, and Hb con-centration, a component of blood viscosity. These predic-tive parameters are easily measured and are inexpensive in routine clinical practice. In case, it is supported in other studies; in patient with chest pain care the high value of PDW can be ranked in CSF diagnosis algorithm.In this study we evaluated the coronary arteries us-ing coronary angiography. Although it is well known that IVUS provides a more precise evaluation of coronary ath-erosclerosis, we were unable to perform intravascular ul-trasound (IVUS) assessment. In addition, the study data is reflective of the cross-sectional design and may not reflect the long-term clinical status of the patients. ConclusionsOur study data support a statistically significant as-sociation between PDW and CSF. Further studies of CSF will continue to advance our understanding of its etio-pathology.References1. Wang X, Nie SP. The coronary slow flow phenomenon: charac-teristics, mechanisms and implications. Cardiovasc Diagn Ther 2011; 1: 37-43.2. Mangieri E, Macchiarelli G, Ciavolella M, et al. Slow coronaryflow: clinical and histopathological features in patients with otherwise normal epicardial coronary arteries. Cathet Cardio-vasc Diagn 1996; 37: 375-81.Ferhat Ozyurtlu et al. The association between coronary slow flow and platelet distribution width in patients with stable CAD3. Sezgin AT, Sigirci A, Barutcu I, et al. Vascular endothelial func-tion in patients with slow coronary flow. Coron Artery Dis 2003;14: 155-61.4. Gokce M, Kaplan S, Tekelioglu Y, et al. Platelet function disorderin patients with coronary slow flow. Clin Cardiol 2005; 28: 145-8.5. Pekdemir H, Cin VG, Cicek D, et al. Slow coronary flow may bea sign of diffuse atherosclerosis. Contribution of FFR and IVUS.Acta Cardiol 2004; 59: 127-33.6. Beltrame JF, Limaye SB, Horowitz JD. The coronary slow flowphenomenon – a new coronary microvascular disorder. Cardi-ology 2002; 97: 197-202.7. Nurkalem Z, Gorgulu S, Uslu N, et al. Longitudinal left ventricu-lar systolic function is impaired in patients with coronary slow flow. Int J Cardiovasc Imaging 2009; 25: 25-32.8. Saya S, Hennebry TA, Lozano P, et al. Coronary slow flow phe-nomenon and risk for sudden cardiac death due to ventricular arrhythmias: a case report and review of literature. Clin Cardiol 2008; 31: 352-5.9. Herve P, Humbert M, Sitbon O, et al. Pathobiology of pulmonaryhypertension: the role of platelets and thrombosis. Clin Chest Med 2001; 22: 451-8.10. Ege MR, Guray U, Guray Y, et al. Platelet distribution width andsaphenous vein disease in patients after CABG: association with graft occlusion. Herz 2013; 38: 197-201.11. Wang S, Zhang Y, Cheng Y, et al. Correlation between the hema-tocryte and slow coronary flow. Clin Hemorheol Microcirc 2013 Jan 2.12. Tonelli M, Sacks F, Arnold M, et al. Relation between red bloodcell distribution width and cardiovascular event rate in people with coronary disease. Circulation 2008; 117: 163-8.13. Dabbah S, Hammerman H, Markiewicz W, et al. Relation be-tween red cell distribution width and clinical outcomes after acute myocardial infarction. Am J Cardiol 2010; 105: 312-7. 14. Polat N, Yildiz A, Oylumlu M, et al. Relationship between redcell distribution width and the GRACE Risk score with in-hospi-tal D eath in patients with acute coronary syndrome. Clin Appl Thromb Hemost 2014; 20: 577-82.15. Kaya H, Ertas F, Islamoglu Y, et al. Association between neutro-phil to lymphocyte ratio and severity of coronary artery disease.Clin Appl Thromb Hemost 2014; 20: 50-4.16. Acet H, Ertaş F, Akıl MA, et al. New inflammatory predictors fornon-valvular atrial fibrillation: echocardiographic epicardial fat thickness and neutrophil to lymphocyte ratio. Int J Cardiovasc Imaging 2014; 30: 81-9.17. Stevens LA, Coresh J, Greene T, et al. Assessing kidney functionmeasured and estimated glomerular filtration rate. N Engl J Med 2006; 354: 2473-83.18. G ibson CM, Cannon CP, Daley WL, et al. TIMI frame count:a quantitative method of assessing coronary artery flow. Circu-lation 1996; 93: 879-88.19. Vagdatli E, G ounari E, Lazaridou E, et al. Platelet distributionwidth: a simple, practical and specific marker of activation of coagulation. Hippokratia 2010; 14: 28-32.20. Herve P, Humbert M, Sitbon O, et al. Pathobiology of pulmonaryhypertension: the role of platelets and thrombosis. Clin Chest Med 2001; 22: 451-8.21. Khandekar MM, Khurana AS, Deshmukh SD, et al. Platelet vol-ume indices in patients with coronary artery disease and acute myocardial infarction: an Indian scenario. J Clin Pathol 2006; 59: 146-9. 22. Jindal S, G upta S, G upta R, et al. Platelet indices in diabetesmellitus: indicators of diabetic microvascular complications.Hematology 2011; 16: 86-9.23. Ergun-Cagli K, Ileri-Gurel E, Ozeke O, et al. Blood viscosity chang-es in slow coronary flow patients. Clin Hemorheol Microcirc 2011; 47: 27-35.24. Lowe G D. Blood rheology in arterial disease. Clin Sci (Lond)1986; 71: 137-46.25. Kalay N, Dogdu O, Koc F, et al. Hematologic parameters and an-giographic progression of coronary atherosclerosis. Angiology 2012; 63: 213-7.26. Hansson GK. Inflammation, atherosclerosis, and coronary arterydisease. N Engl J Med 2005; 352: 1685-95.27. Gibson PH, Cuthbertson BH, Croal BL, et al. Usefulness of neu-trophil/lymphocyte ratio as predictor of new-onset atrial fibril-lation after coronary artery bypass grafting. Am J Cardiol 2010;105: 186-91.28. Naruko T, Ueda M, Haze K, et al. Neutrophil infiltration of cul-prit lesions in acute coronary syndromes. Circulation 2002; 106: 2894-900.29. Packard RR, Libby P. Inflammation in atherosclerosis: from vas-cular biology to biomarker discovery and risk prediction. Clin Chem 2008; 54: 24-38.30. Akpinar I, Sayin MR, Gursoy YC, et al. Plateletcrit and red celldistribution width are independent predictors of the slow coro-nary flow phenomenon. J Cardiol 2014; 63: 112-8.。
—598 —介人放射学杂志2019 年6 月第28 卷第6 期J Intervent Radiol 2019, V〇1.28, No.6[J]. J Nucl Med, 2008, 49:541-545.[20] Kunos CA, Resnick MI, Kinsella TJ, et al. Migration ofimplanted free radioactive seeds for adenocarcinoma of the prostate using a Mick applicator[J]. Brachytherapy, 2004, 3:71-77.[21 ] Gacci M, Semi S, Lapini A, et al. PSA recurrence afterbrachytherapy for seed misplacement:a double-blind radiologic and pathologic work-up after salvage prostatectomy [J ]. Prostate Cancer Prostatic Dis, 2008, 11 :99-101.[22] Franca CA, Vieira SL, Carvalho AC, et al. Radioactive seedmigration after prostate brachytherapy with iodine-125 using loose seeds versus stranded seeds [J]. Intemat Braz J Urol, 2009, 35:573-579.[23] Gao M, Wang JZ, Nag S, et al. Effects of seed migration onpost-implant dosimetry of prostate brachytherapy [J]. Med Phys, 2007, 34:471-480.[24] El-Bared N, Sebbag N, Beliveau-Nadeau D, et al. Seed loss inprostate brachytherapy operator dependency and impact on dosimetry [J ]. Strahlenther Onkol, 2016, 192:305-311.[25] Choi YW, Munden RF, Erasmus JJ, et al. Effects of radiationtherapy on the lung:radiologic appearances and differential diagnosis[J]. Radiographics, 2004, 24:985-997.[26] Miura N, Kusuhara Y, Numata K, et al. Radiation pneumonitiscaused by a migrated brachytherapy seed lodged in the lung [J].Jpn J Clin Oncol, 2008, 38:623-625.[27] Chen WC, Katcher J, Nunez C, et al. Radioactive seed migrationafter transperineal interstitial prostate brachytherapy and associateddevelopment of small-cell lung cancer[J]. Brachytherapy, 2012,11 :354-358.[28] Calvert AD, Dyer AW, Montgomery VA. Montgomery embolizationof prostatic brachytherapy seeds to pulmonary arteries:a casestudy [J]. Radiol Case Rep, 2016, 12:34-38.[29] Zhu AX, Wallner KE, Frivold GP, et al. Prostate brachytherapyseed migration to the right coronary artery associated with anacute myocardial infarction [J ]. Brachytherapy, 2006, 5: 262-265.[30] Davis BJ, Pfeifer EA, Wilson TM, et al. Prostate brachytherapyseed migration to the right ventricle found at autopsy followingacute cardiac dysrhythmia [J]. J Urol, 2000,164: 1661.[31] Nguyen BD, Schild SE, Wong WW, et al. Prostate brachytherapyseed embolization to the right renal artery [ J Brachytherapy,2009, 8:309-312.(收稿日期:2018-07-03)(本文编辑:俞瑞纲)•书讯•《介入护理实践指南(2019版)》出版由中国医师协会介人医师分会介人围手术专业委员会编写的《介人护理实践指南(2019 版)》一书日前出版发行。
PROCARDIA XL® (nifedipine)Extended Release TabletsFor Oral UseDESCRIPTIONNifedipine is a drug belonging to a class of pharmacological agents known as the calciumchannel blockers. Nifedipine is 3,5-pyridinedicarboxylic acid, 1,4-dihydro-2,6-dimethyl-4(2-nitrophenyl)-, dimethyl ester, C17H18N2O6, and has the structural formula: HN CH 3H 3C H 3COCCOCH 3 H NO 2OO Nifedipine is a yellow crystalline substance, practically insoluble in water but soluble in ethanol. It has a molecular weight of 346.3. Procardia XL is a registered trademark for Nifedipine GITS. Nifedipine GITS (Gastrointestinal Therapeutic System) Tablet is formulated as a once-a-day controlled-release tablet for oral administration designed to deliver 30, 60, or 90 mg ofnifedipine.Inert ingredients in the formulations are: cellulose acetate; hydroxypropyl cellulose; hypromellose; magnesium stearate; polyethylene glycol; polyethylene oxide; red ferric oxide; sodium chloride; titanium dioxide.System Components and PerformanceProcardia XL Extended Release Tablet is similar in appearance to a conventional tablet. It consists, however, of a semipermeable membrane surrounding an osmotically active drug core. The core itself is divided into two layers: an “active” layer containing the drug, and a “push” layer containing pharmacologically inert (but osmotically active) components. As water fromthe gastrointestinal tract enters the tablet, pressure increases in the osmotic layer and “pushes”against the drug layer, releasing drug through the precision laser-drilled tablet orifice in the active layer.Procardia XL Extended Release Tablet is designed to provide nifedipine at an approximately constant rate over 24 hours. This controlled rate of drug delivery into the gastrointestinal lumen is independent of pH or gastrointestinal motility. Procardia XL depends for its action on the existence of an osmotic gradient between the contents of the bi-layer core and fluid in the gastrointestinal tract. Drug delivery is essentially constant as long as the osmotic gradient remains constant, and then gradually falls to zero. Upon swallowing, the biologically inert components of the tablet remain intact during gastrointestinal transit and are eliminated in the feces as an insoluble shell.CLINICAL PHARMACOLOGYNifedipine is a calcium ion influx inhibitor (slow-channel blocker or calcium ion antagonist) and inhibits the transmembrane influx of calcium ions into cardiac muscle and smooth muscle. The contractile processes of cardiac muscle and vascular smooth muscle are dependent upon the movement of extracellular calcium ions into these cells through specific ion channels. Nifedipine selectively inhibits calcium ion influx across the cell membrane of cardiac muscle and vascular smooth muscle without altering serum calcium concentrations.Mechanism of ActionA) AnginaThe precise mechanisms by which inhibition of calcium influx relieves angina have not been fully determined, but includes at least the following two mechanisms:1) Relaxation and Prevention of Coronary Artery SpasmNifedipine dilates the main coronary arteries and coronary arterioles, both in normal and ischemic regions, and is a potent inhibitor of coronary artery spasm, whether spontaneous or ergonovine-induced. This property increases myocardial oxygen delivery in patients with coronary artery spasm, and is responsible for the effectiveness of nifedipine in vasospastic (Prinzmetal’s or variant) angina. Whether this effect plays any role in classical angina is not clear, but studies of exercise tolerance have not shown an increase in the maximum exercise rate-pressure product, a widely accepted measure of oxygen utilization. This suggests that, in general, relief of spasm or dilation of coronary arteries is not an important factor in classical angina.2) Reduction of Oxygen UtilizationNifedipine regularly reduces arterial pressure at rest and at a given level of exercise by dilating peripheral arterioles and reducing the total peripheral vascular resistance (afterload) against which the heart works. This unloading of the heart reduces myocardial energy consumption and oxygen requirements, and probably accounts for the effectiveness of nifedipine in chronic stable angina.B) HypertensionThe mechanism by which nifedipine reduces arterial blood pressure involves peripheral arterial vasodilatation and the resulting reduction in peripheral vascular resistance. The increased peripheral vascular resistance that is an underlying cause of hypertension results from an increase in active tension in the vascular smooth muscle. Studies have demonstrated that the increase in active tension reflects an increase in cytosolic free calcium.Nifedipine is a peripheral arterial vasodilator which acts directly on vascular smooth muscle. The binding of nifedipine to voltage-dependent and possibly receptor-operated channels in vascular smooth muscle results in an inhibition of calcium influx through these channels. Stores of intracellular calcium in vascular smooth muscle are limited and thus dependent upon the influx of extracellular calcium for contraction to occur. The reduction in calcium influx by nifedipine causes arterial vasodilation and decreased peripheral vascular resistance which results in reduced arterial blood pressure.Pharmacokinetics and MetabolismNifedipine is completely absorbed after oral administration. Plasma drug concentrations rise at a gradual, controlled rate after a Procardia XL Extended Release Tablet dose and reach a plateau at approximately six hours after the first dose. For subsequent doses, relatively constant plasma concentrations at this plateau are maintained with minimal fluctuations over the 24-hour dosing interval. About a four-fold higher fluctuation index (ratio of peak to trough plasma concentration) was observed with the conventional immediate-release Procardia capsule at t.i.d. dosing than with once daily Procardia XL Extended Release Tablet. At steady-state, the bioavailability of the Procardia XL Extended Release Tablet is 86% relative to Procardia capsules. Administration of the Procardia XL Extended Release Tablet in the presence of food slightly alters the early rate of drug absorption, but does not influence the extent of drug bioavailability. Markedly reduced gastrointestinal retention time over prolonged periods (i.e., short bowel syndrome), however, may influence the pharmacokinetic profile of the drug which could potentially result in lower plasma concentrations. Pharmacokinetics of Procardia XL Extended Release Tablets are linear over the dose range of 30 to 180 mg in that plasma drug concentrations are proportional to dose administered. There was no evidence of dose dumping either in the presence or absence of food for over 150 subjects in pharmacokinetic studies. Nifedipine is extensively metabolized to highly water-soluble, inactive metabolites, accounting for 60 to 80% of the dose excreted in the urine. The elimination half-life of nifedipine is approximately two hours. Only traces (less than 0.1% of the dose) of unchanged form can be detected in the urine. The remainder is excreted in the feces in metabolized form, most likely as a result of biliary excretion. Thus, the pharmacokinetics of nifedipine are not significantly influenced by the degree of renal impairment. Patients in hemodialysis or chronic ambulatory peritoneal dialysis have not reported significantly altered pharmacokinetics of nifedipine. Since hepatic biotransformation is the predominant route for the disposition of nifedipine, the pharmacokinetics may be altered in patients with chronic liver disease. Patients with hepatic impairment (liver cirrhosis) have a longer disposition half-life and higher bioavailability of nifedipine than healthy volunteers. The degree of serum protein binding of nifedipine is high (92–98%). Protein binding may be greatly reduced in patients with renal or hepatic impairment.HemodynamicsLike other slow-channel blockers, nifedipine exerts a negative inotropic effect on isolated myocardial tissue. This is rarely, if ever, seen in intact animals or man, probably because of reflex responses to its vasodilating effects. In man, nifedipine decreases peripheral vascular resistance which leads to a fall in systolic and diastolic pressures, usually minimal in normotensive volunteers (less than 5-10 mm Hg systolic), but sometimes larger. With Procardia XL Extended Release Tablets, these decreases in blood pressure are not accompanied by any significant change in heart rate. Hemodynamic studies in patients with normal ventricular function have generally found a small increase in cardiac index without major effects on ejection fraction, left ventricular end diastolic pressure (LVEDP), or volume (LVEDV). In patients with impaired ventricular function, most acute studies have shown some increase in ejection fraction and reduction in left ventricular filling pressure.Electrophysiologic EffectsAlthough, like other members of its class, nifedipine causes a slight depression of sinoatrial node function and atrioventricular conduction in isolated myocardial preparations, such effects have not been seen in studies in intact animals or in man. In formal electrophysiologic studies, predominantly in patients with normal conduction systems, nifedipine has had no tendency to prolong atrioventricular conduction or sinus node recovery time, or to slow sinus rate. INDICATIONS AND USAGEI. Vasospastic AnginaProcardia XL is indicated for the management of vasospastic angina confirmed by any of the following criteria: 1) classical pattern of angina at rest accompanied by ST segment elevation, 2) angina or coronary artery spasm provoked by ergonovine, or 3) angiographically demonstrated coronary artery spasm. In those patients who have had angiography, the presence of significant fixed obstructive disease is not incompatible with the diagnosis of vasospastic angina, provided that the above criteria are satisfied. Procardia XL may also be used where the clinical presentation suggests a possible vasospastic component, but where vasospasm has not been confirmed, e.g., where pain has a variable threshold on exertion, or in unstable angina where electrocardiographic findings are compatible with intermittent vasospasm, or when angina is refractory to nitrates and/or adequate doses of beta blockers.II. Chronic Stable Angina(Classical Effort-Associated Angina)Procardia XL is indicated for the management of chronic stable angina (effort-associated angina) without evidence of vasospasm in patients who remain symptomatic despite adequate doses of beta blockers and/or organic nitrates or who cannot tolerate those agents.In chronic stable angina (effort-associated angina), nifedipine has been effective in controlled trials of up to eight weeks duration in reducing angina frequency and increasing exercise tolerance, but confirmation of sustained effectiveness and evaluation of long-term safety in these patients is incomplete.Controlled studies in small numbers of patients suggest concomitant use of nifedipine and beta-blocking agents may be beneficial in patients with chronic stable angina, but available information is not sufficient to predict with confidence the effects of concurrent treatment, especially in patients with compromised left ventricular function or cardiac conduction abnormalities. When introducing such concomitant therapy, care must be taken to monitor blood pressure closely, since severe hypotension can occur from the combined effects of the drugs (See WARNINGS).III. HypertensionProcardia XL is indicated for the treatment of hypertension. It may be used alone or in combination with other antihypertensive agents.CONTRAINDICATIONSKnown hypersensitivity reaction to nifedipine.WARNINGSExcessive HypotensionAlthough in most angina patients the hypotensive effect of nifedipine is modest and well tolerated, occasional patients have had excessive and poorly tolerated hypotension. These responses have usually occurred during initial titration or at the time of subsequent upward dosage adjustment, and may be more likely in patients on concomitant beta blockers.Severe hypotension and/or increased fluid volume requirements have been reported in patients receiving nifedipine together with a beta-blocking agent who underwent coronary artery bypass surgery using high dose fentanyl anesthesia. The interaction with high dose fentanyl appears to be due to the combination of nifedipine and a beta blocker, but the possibility that it may occur with nifedipine alone, with low doses of fentanyl, in other surgical procedures, or with other narcotic analgesics cannot be ruled out. In nifedipine-treated patients where surgery using high dose fentanyl anesthesia is contemplated, the physician should be aware of these potential problems and, if the patient’s condition permits, sufficient time (at least 36 hours) should be allowed for nifedipine to be washed out of the body prior to surgery.The following information should be taken into account in those patients who are being treated for hypertension as well as angina:Increased Angina and/or Myocardial InfarctionRarely, patients, particularly those who have severe obstructive coronary artery disease, have developed well documented increased frequency, duration and/or severity of angina or acute myocardial infarction on starting nifedipine or at the time of dosage increase. The mechanism of this effect is not established.Beta Blocker WithdrawalIt is important to taper beta blockers if possible, rather than stopping them abruptly before beginning nifedipine. Patients recently withdrawn from beta blockers may develop a withdrawalsyndrome with increased angina, probably related to increased sensitivity to catecholamines. Initiation of nifedipine treatment will not prevent this occurrence and on occasion has been reported to increase it.Congestive Heart FailureRarely, patients, usually receiving a beta blocker, have developed heart failure after beginning nifedipine. Patients with tight aortic stenosis may be at greater risk for such an event, as the unloading effect of nifedipine would be expected to be of less benefit, owing to the fixed impedance to flow across the aortic valve in these patients.Gastrointestinal Obstruction Requiring SurgeryThere have been rare reports of obstructive symptoms in patients with known strictures in association with the ingestion of Procardia XL. Bezoars can occur in very rare cases and may require surgical intervention.Cases of serious gastrointestinal obstruction have been identified in patients with no known gastrointestinal disease, including the need for hospitalization and surgical intervention.Risk factors for a gastrointestinal obstruction identified from post-marketing reports of Procardia XL (GITS tablet formulation) include alteration in gastrointestinal anatomy (severe gastrointestinal narrowing, colon cancer, small bowel obstruction, bowel resection, gastric bypass, vertical banded gastroplasty, and colostomy), hypomotility disorders (constipation, gastroesophageal reflux disease, ileus, obesity, hypothyroidism, and diabetes) and concomitant medications (H2-histamine blockers, nonsteroidal anti-inflammatory drugs, laxatives, anticholinergic agents, and levothyroxine).PRECAUTIONSGeneral-Hypotension: Because nifedipine decreases peripheral vascular resistance, careful monitoring of blood pressure during the initial administration and titration of nifedipine is suggested. Close observation is especially recommended for patients already taking medications that are known to lower blood pressure (See WARNINGS).Peripheral Edema: Mild to moderate peripheral edema occurs in a dose dependent manner with an incidence ranging from approximately 10% to about 30% at the highest dose studied(180 mg). It is a localized phenomenon thought to be associated with vasodilation of dependent arterioles and small blood vessels and not due to left ventricular dysfunction or generalized fluid retention. With patients whose angina or hypertension is complicated by congestive heart failure, care should be taken to differentiate this peripheral edema from the effects of increasing left ventricular dysfunction.Information for Patients: Procardia XL Extended Release Tablets should be swallowed whole. Do not chew, divide or crush tablets. Do not be concerned if you occasionally notice in your stool something that looks like a tablet. In Procardia XL, the medication is contained within a nonabsorbable shell that has been specially designed to slowly release the drug for your body to absorb. When this process is completed, the empty tablet is eliminated from your body.Laboratory Tests: Rare, usually transient, but occasionally significant elevations of enzymes such as alkaline phosphatase, CPK, LDH, SGOT and SGPT have been noted. The relationship to nifedipine therapy is uncertain in most cases, but probable in some. These laboratory abnormalities have rarely been associated with clinical symptoms; however, cholestasis with or without jaundice has been reported. A small (5.4%) increase in mean alkaline phosphatase was noted in patients treated with Procardia XL. This was an isolated finding not associated with clinical symptoms and it rarely resulted in values which fell outside the normal range. Rare instances of allergic hepatitis have been reported. In controlled studies, Procardia XL did not adversely affect serum uric acid, glucose, or cholesterol. Serum potassium was unchanged in patients receiving Procardia XL in the absence of concomitant diuretic therapy, and slightly decreased in patients receiving concomitant diuretics.Nifedipine, like other calcium channel blockers, decreases platelet aggregation in vitro. Limited clinical studies have demonstrated a moderate but statistically significant decrease in platelet aggregation and an increase in bleeding time in some nifedipine patients. This is thought to be a function of inhibition of calcium transport across the platelet membrane. No clinical significance for these findings has been demonstrated.Positive direct Coombs test with/without hemolytic anemia has been reported, but a causal relationship between nifedipine administration and positivity of this laboratory test, including hemolysis, could not be determined.Although nifedipine has been used safely in patients with renal dysfunction and has been reported to exert a beneficial effect, in certain cases, rare, reversible elevations in BUN and serum creatinine have been reported in patients with preexisting chronic renal insufficiency. The relationship to nifedipine therapy is uncertain in most cases but probable in some.Drug Interactions: Beta-adrenergic blocking agents: (See INDICATIONS AND USAGE and WARNINGS) Experience in over 1400 patients with Procardia capsules in a noncomparative clinical trial has shown that concomitant administration of nifedipine and beta-blocking agents is usually well tolerated, but there have been occasional literature reports suggesting that the combination may increase the likelihood of congestive heart failure, severe hypotension, or exacerbation of angina.Long-acting Nitrates: Nifedipine may be safely coadministered with nitrates, but there have been no controlled studies to evaluate the antianginal effectiveness of this combination.Digitalis: Administration of nifedipine with digoxin increased digoxin levels in nine of twelve normal volunteers. The average increase was 45%. Another investigator found no increase in digoxin levels in thirteen patients with coronary artery disease. In an uncontrolled study of over two hundred patients with congestive heart failure during which digoxin blood levels were not measured, digitalis toxicity was not observed. Since there have been isolated reports of patients with elevated digoxin levels, it is recommended that digoxin levels be monitored when initiating, adjusting, and discontinuing nifedipine to avoid possible over- or under-digitalization.Coumarin Anticoagulants: There have been rare reports of increased prothrombin time in patients taking coumarin anticoagulants to whom nifedipine was administered. However, the relationship to nifedipine therapy is uncertain.Cimetidine: A study in six healthy volunteers has shown a significant increase in peak nifedipine plasma levels (80%) and area-under-the-curve (74%), after a one week course of cimetidine at 1000 mg per day and nifedipine at 40 mg per day. Ranitidine produced smaller, non-significant increases. The effect may be mediated by the known inhibition of cimetidine on hepatic cytochrome P-450, the enzyme system probably responsible for the first-pass metabolism of nifedipine. If nifedipine therapy is initiated in a patient currently receiving cimetidine, cautious titration is advised.Carcinogenesis, Mutagenesis, Impairment of Fertility: Nifedipine was administered orally to rats for two years and was not shown to be carcinogenic. When given to rats prior to mating, nifedipine caused reduced fertility at a dose approximately 30 times the maximum recommended human dose. There is a literature report of reversible reduction in the ability of human sperm obtained from a limited number of infertile men taking recommended doses of nifedipine to bind to and fertilize an ovum in vitro. In vivo mutagenicity studies were negative.Pregnancy: Pregnancy Category C: Nifedipine has been shown to produce teratogenic findings in rats and rabbits, including digital anomalies similar to those reported for phenytoin. Digital anomalies have been reported to occur with other members of the dihydropyridine class and are possibly a result of compromised uterine blood flow. Nifedipine administration was associated with a variety of embryotoxic, placentotoxic, and fetotoxic effects, including stunted fetuses (rats, mice, rabbits), rib deformities (mice), cleft palate (mice), small placentas and underdeveloped chorionic villi (monkeys), embryonic and fetal deaths (rats, mice, rabbits), and prolonged pregnancy/decreased neonatal survival (rats; not evaluated in other species). On a mg/kg basis, all of the doses associated with the teratogenic embryotoxic or fetotoxic effects in animals were higher (3.5 to 42 times) than the maximum recommended human dose of120 mg/day. On a mg/m2 basis, some doses were higher and some were lower than the maximum recommended human dose, but all are within an order of magnitude of it. The doses associated with placentotoxic effects in monkeys were equivalent to or lower than the maximum recommended human dose on a mg/m2 basis.There are no adequate and well-controlled studies in pregnant women. Procardia XL Extended Release Tablets should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.Pediatric Use: Safety and effectiveness in pediatric patients have not been established.ADVERSE EXPERIENCESOver 1000 patients from both controlled and open trials with Procardia XL Extended ReleaseTablets in hypertension and angina were included in the evaluation of adverse experiences. Allside effects reported during Procardia XL Extended Release Tablet therapy were tabulatedindependent of their causal relation to medication. The most common side effect reported withProcardia XL was edema which was dose related and ranged in frequency from approximately10% to about 30% at the highest dose studied (180 mg). Other common adverse experiencesreported in placebo-controlled trials include:Procardia XL (%) Placebo (%)Adverse Effect (N=707) (N=266)Headache15.8 9.85.9 4.1 Fatigue4.1 4.5 DizzinessConstipation 3.3 2.3 Nausea 3.3 1.9Of these, only edema and headache were more common in Procardia XL patients than placebopatients.The following adverse reactions occurred with an incidence of less than 3.0%. With theexception of leg cramps, the incidence of these side effects was similar to that of placebo alone.Body as a Whole/Systemic: asthenia, flushing, painCardiovascular: palpitationsCentral Nervous System: insomnia, nervousness, paresthesia, somnolenceDermatologic: pruritus, rashGastrointestinal: abdominal pain, diarrhea, dry mouth, dyspepsia, flatulenceMusculoskeletal: arthralgia, leg crampsRespiratory: chest pain (nonspecific), dyspneaUrogenital: impotence, polyuriaOther adverse reactions were reported sporadically with an incidence of 1.0% or less. Theseinclude:Body as a Whole/Systemic: face edema, fever, hot flashes, malaise, periorbital edema, rigorsCardiovascular: arrhythmia, hypotension, increased angina, tachycardia, syncopeCentral Nervous System: anxiety, ataxia, decreased libido, depression, hypertonia,hypoesthesia, migraine, paroniria, tremor, vertigoDermatologic: alopecia, increased sweating, urticaria, purpuraGastrointestinal: eructation, gastroesophageal reflux, gum hyperplasia, melena, vomiting,weight increaseMusculoskeletal: back pain, gout, myalgiasRespiratory: coughing, epistaxis, upper respiratory tract infection, respiratory disorder,sinusitisSpecial Senses: abnormal lacrimation, abnormal vision, taste perversion, tinnitusUrogenital/Reproductive: breast pain, dysuria, hematuria, nocturiaAdverse experiences which occurred in less than 1 in 1000 patients cannot be distinguished from concurrent disease states or medications.The following adverse experiences, reported in less than 1% of patients, occurred underconditions (e.g., open trials, marketing experience) where a causal relationship is uncertain: gastrointestinal irritation, gastrointestinal bleeding, gynecomastia.Gastrointestinal obstruction resulting in hospitalization and surgery, including the need forbezoar removal, has occurred in association with Procardia XL, even in patients with no priorhistory of gastrointestinal disease.In multiple-dose U.S. and foreign controlled studies with nifedipine capsules in which adverse reactions were reported spontaneously, adverse effects were frequent but generally not seriousand rarely required discontinuation of therapy or dosage adjustment. Most were expected consequences of the vasodilator effects of nifedipine.Procardia(%)Capsules(%) PlaceboAdverse Effect (N=226) (N=235)Dizziness, lightheadedness,giddiness 27 15 Flushing, heat sensation 25 8Headache23 2012 10 WeaknessNausea, heartburn 11 8Muscle cramps, tremor 8 3Peripheral edema 7 1Nervousness, mood changes 7 47 5 PalpitationsDyspnea, cough, wheezing 6 3Nasal congestion, sore throat 6 8There is also a large uncontrolled experience in over 2100 patients in the United States. Most ofthe patients had vasospastic or resistant angina pectoris, and about half had concomitanttreatment with beta-adrenergic blocking agents. The relatively common adverse events weresimilar in nature to those seen with Procardia XL.In addition, more serious adverse events were observed, not readily distinguishable from thenatural history of the disease in these patients. It remains possible, however, that some or manyof these events were drug related. Myocardial infarction occurred in about 4% of patients and congestive heart failure or pulmonary edema in about 2%. Ventricular arrhythmias orconduction disturbances each occurred in fewer than 0.5% of patients.In a subgroup of over 1000 patients receiving Procardia with concomitant beta blocker therapy, the pattern and incidence of adverse experiences was not different from that of the entire group of Procardia-treated patients (See PRECAUTIONS).In a subgroup of approximately 250 patients with a diagnosis of congestive heart failure as well as angina, dizziness or lightheadedness, peripheral edema, headache, or flushing each occurred in one in eight patients. Hypotension occurred in about one in 20 patients. Syncope occurred in approximately one patient in 250. Myocardial infarction or symptoms of congestive heart failure each occurred in about one patient in 15. Atrial or ventricular dysrhythmias each occurred in about one patient in 150.In post-marketing experience, there have been rare reports of exfoliative dermatitis caused by nifedipine. There have been rare reports of exfoliative or bullous skin adverse events (such as erythema multiforme, Stevens-Johnson Syndrome, and toxic epidermal necrolysis) and photosensitivity reactions. Gastrointestinal obstruction resulting in hospitalization and surgery, including the need for bezoar removal, has occurred in association with Procardia XL, even in patients with no prior history of gastrointestinal disease.OVERDOSAGEExperience with nifedipine overdosage is limited. Generally, overdosage with nifedipine leading to pronounced hypotension calls for active cardiovascular support, including monitoring of cardiovascular and respiratory function, elevation of extremities, judicious use of calcium infusion, pressor agents, and fluids. Clearance of nifedipine would be expected to be prolonged in patients with impaired liver function. Since nifedipine is highly protein-bound, dialysis is not likely to be of any benefit.There has been one reported case of massive overdosage with Procardia XL Extended Release Tablets. The main effects of ingestion of approximately 4800 mg of Procardia XL in a young man attempting suicide as a result of cocaine-induced depression was initial dizziness, palpitations, flushing, and nervousness. Within several hours of ingestion, nausea, vomiting, and generalized edema developed. No significant hypotension was apparent at presentation, 18 hours post-ingestion. Electrolyte abnormalities consisted of a mild, transient elevation of serum creatinine, and modest elevations of LDH and CPK, but normal SGOT. Vital signs remained stable, no electrocardiographic abnormalities were noted, and renal function returned to normal within 24 to 48 hours with routine supportive measures alone. No prolonged sequelae were observed.The effect of a single 900 mg ingestion of Procardia capsules in a depressed anginal patient also on tricyclic antidepressants was loss of consciousness within 30 minutes of ingestion, and profound hypotension, which responded to calcium infusion, pressor agents, and fluid replacement. A variety of ECG abnormalities were seen in this patient with a history of bundle branch block, including sinus bradycardia and varying degrees of AV block. These dictated the prophylactic placement of a temporary ventricular pacemaker, but otherwise resolved spontaneously. Significant hyperglycemia was seen initially in this patient, but plasma glucose levels rapidly normalized without further treatment.。
1260 Rev Esp Cardiol. 2009;62(11):1260-6 Non-ST-Elevation Acute Myocardial Infarction With Normal Coronary Arteries: Predictors and Prognosis
Alejandro Cortell, Juan Sanchis, Vicente Bodí, Julio Núñez, Luis Mainar, Mauricio Pellicer, Gema Miñana, Enrique Santas, Eloy Domínguez, Patricia Palau, and Ángel Llácer
Servicio de Cardiología, Hospital Clínico Universitario de Valencia, Valencia, Spain
ORIGINAL ARTICLE
This study was supported by a grant from the HERACLES Cardiovascular Research Network (RD06/0009 Ministry of Science and Innovation, Instituto de Salud Carlos III, Madrid, Spain). Drs Juan Sanchis, Vicent Bodí, Julio Núñez, Luis Mainar, and Ángel Llácer also received support from a grant FIS PI070640 (Instituto de Salud Carlos III, Madrid, Spain).
Correspondence: Dr. J. Sanchis. Servicio de Cardiología. Hospital Clínico Universitario. Blasco Ibáñez, 17. 46010 Valencia. España. E-mail: Sanchis_juafor@gva.es
Manuscript received November 28, 2008. Accepted for publication July 7, 2009.
Introduction and objectives. Occasionally, coronary arteries without significant stenosis are observed during invasive treatment of acute non-ST-elevation myocardial infarction (NSTEMI). The aim was to investigate predictive factors and prognosis in these patients.Methods. The study involved 504 patients admitted for NSTEMI who underwent cardiac catheterization. The primary end-point was the observation of coronary arteries without significant stenosis, and the secondary end-point was death or myocardial infarction within a median of 3 years. In evaluating the secondary end-point, a control group of 160 patients with a normal troponin level and no significant coronary artery stenosis who were admitted for chest pain during the same period was included. Results. Overall, 64 patients (13%) had coronary arteries without significant lesions. The predictors were: female sex (odds ratio [OR] = 6.6; P=.0001), age <55 years (OR=3.0; P=.001), and the absence of diabetes (OR=2.4, P=.02), previous antiplatelet treatment (OR=3.9, P=.007) or ST-segment depression (OR=2.4, P=.008). The composite variable of female sex plus at least 2 additional predictive factors had a specificity of 85% and a sensitivity of 53% for coronary angiography showing no significant stenosis. The absence of coronary artery stenosis decreased the probability of death or myocardial infarction during follow-up (hazard ratio = 0.3, 95% confidence interval, 0.2-0.9; P=.03). Among all patients without significant stenosis (n=224), there was no difference in the event rate between those with elevated and normal troponin levels.Conclusions. In NSTEMI, female sex, age <55 years and the absence of diabetes, previous antiplatelet treatment, or ST-segment depression were all associated with coronary angiography showing no significant stenosis. The long-term prognosis in these patients was good.
Key words: Myocardial infarction. No significant stenosis on coronary angiography. Predictors. Prognosis.
Infarto de miocardio sin elevación del ST con coronarias normales: predictores y pronóstico
Introducción y objetivos. El manejo invasivo del infar-to agudo de miocardio sin elevación del ST (IAMSEST) detecta en ocasiones arterias coronarias sin estenosis significativas. Nuestro objetivo fue evaluar los factores asociados y el pronóstico de esta población. Métodos. Estudiamos a 504 pacientes ingresados por IAMSEST y sometidos a cateterismo cardiaco. El objetivo primario fue el hallazgo de coronarias sin estenosis signi-ficativas y el secundario, la mortalidad o el infarto a una mediana de 3 años. Para evaluar el objetivo secundario, se utilizó un grupo control de 160 pacientes ingresados por dolor torácico durante el mismo periodo con troponi-na normal y coronarias sin estenosis significativas. Resultados. Encontramos coronarias sin lesiones sig-nificativas en 64 (13%) pacientes. Los predictores fue-ron: ser mujer (odds ratio [OR] = 6,6; p = 0,0001), edad < 55 años (OR = 3,0; p = 0,001) y ausencia de diabe-tes (OR = 2,4; p = 0,02), tratamiento antiagregante pre-vio (OR = 3,9; p=.007) o descenso del ST (OR = 2,4; p = 0,008). La variable ser mujer con al menos dos va-riables adicionales identificó una coronariografía sin estenosis significativas con especificidad del 85% y sensibilidad del 53%. La ausencia de estenosis corona-rias significativas disminuyó la probabilidad de muerte o infarto durante el seguimiento (hazard ratio = 0,3; in-tervalo de confianza del 95%, 0,2-0,9; p = 0,03). En el total de pacientes sin estenosis coronarias significativas (n = 224), no hubo diferencias en la tasa de sucesos en-tre los pacientes con troponina elevada y normal. Conclusiones. El sexo femenino, la edad < 55 años y la ausencia de diabetes, tratamiento antiagregante previo o descenso del ST se asociaron a una coronariografía sin estenosis significativas en el IAMSEST. El pronóstico a largo plazo de esta población fue bueno.