Clinical Neurology and Neurosurgery108(2006)
549–552
Thrombolytic therapy in acute ischemic stroke in Asia:The?rst
prospective evaluation
Nijasri C.Suwanwela?,Kammant Phanthumchinda,Yuttachai Likitjaroen Neurological Unit,Department of Medicine,Faculty of Medicine,Chulalongkorn University,Rama IV Road,Bangkok10330,Thailand
Received30May2005;received in revised form21September2005;accepted27September2005
Abstract
Objective:Intravenous thrombolytic therapy has been widely recommended as a standard treatment for acute ischemic stroke in most clinical practice guidelines.However,the experience in Asia is still limited.We report the?rst prospective case series of thrombolytic therapy in a developing Asian country.
Patients and methods:Consecutive patients with acute ischemic stroke who presented within3h of onset were screened under stroke fast track program.Those who were eligible were treated with intravenous recombinant tissue plasminogen activator(rt-PA).General and neurological examinations together with the National Institute of Health stroke scale(NHISS)and modi?ed Rankin scale(MRS)were recorded prior to and after the treatment at1h,24h,on discharge and at3months.Hemorrhagic brain lesion and death within3months were also recorded. Results:Thirty-four patients or2.1%of patients with acute stroke received intravenous thrombolysis.The mean pretreatment NIHSS was 18.8and the majority of patients had stroke in the middle cerebral artery territory.The mean door-to-needle time was72.6min(ranged 20–150min).Major neurological improvement,de?ned as improving of the NIHSS>8points or NIHSS of0points at24h,was observed in 17patients(50%).Intracerebral hemorrhage was detected in four cases(11.8%),two of them were symptomatic(5.9%)and one was fatal. Conclusion:Intravenous thrombolysis can be given in patients with acute stroke in our population.Our cases were more severe than other studies.However,half of them experienced major neurological improvement.The risk of hemorrhagic brain lesion is not much higher than previously reported.
?2005Elsevier B.V.All rights reserved.
Keywords:Thrombolysis;Intravenous thrombolysis;Ischemic stroke;Acute stroke;Developing country;Asia
1.Introduction
Intravenous thrombolytic treatment has been used as a standard therapy in acute ischemic stroke and is recom-mended in various guidelines[1–6].However,in Asia throm-bolytic treatment has not been widely applied[7].The major obstacle behind is the limited short therapeutic window, which requires awareness of the public and special setting of emergency management.Limited knowledge and experi-ence of the physicians have also made the treatment even more sophisticated.Among those physicians who are knowl-edgeable for the treatment,there is also fear of serious ?Corresponding author.Tel.:+6622564655/6697998993;
fax:+6622564655.
E-mail address:fmednsu@md2.md.chula.ac.th(N.C.Suwanwela).complications especially intracerebral hemorrhage which is known to be more common among the Asian[8].This study was performed at a university hospital in Thailand.A com-prehensive stroke program which includes stroke fast track for hyperacute stroke patients,multidisciplinary acute stroke unit,neuroimaging and neurovascular ultrasound laboratory, and homecare treatment has been established since the year 2000.Here we report our experience on thrombolytic therapy under stroke fast track program in34patients.To our knowl-edge,this is the?rst ever report of the thrombolytic treatment outside the clinical trials in developing countries in Asia. 2.Methods
All acute ischemic strokes who presented at King Chu-lalongkorn Memorial Hospital during2001–2004were
0303-8467/$–see front matter?2005Elsevier B.V.All rights reserved. doi:10.1016/j.clineuro.2005.09.008
550N.C.Suwanwela et al./Clinical Neurology and Neurosurgery108(2006)549–552
screened for the eligibility for intravenous thrombolytic treat-ment under the stroke fast track program.Those who received the treatment were prospectively studied.In this stroke fast track program,the emergency room physicians and nursing staff,radiologists,laboratory team and the neurology team were educated to be aware of the potential of thrombolytic treatment and the importance of the prompt reaction and man-agement in patients who presented with hyperacute stroke. When emergency room physician encountered a patient with hyperacute stroke,s/he would activate the stroke fast track where essential blood tests and non-contrast CT scan were immediately performed.At the same time,an on-call neurol-ogist was noti?ed and promptly saw the patient and the CT scan result.Patients with evidence of intracranial hemorrhage were excluded.Ischemic stroke patients with CT evidence of early cerebral edema or clear evidence of infarction more than one-third of the middle cerebral artery territory were also excluded.Patient and family discussion about the throm-bolytic treatment would be done in the emergency room and if there was no contraindication and all agreed,intravenous recombinant tissue plasminogen activator(rt-PA)would be given within3h of the stroke onset.For inclusion and exclu-sion criteria,we adopted the criteria that were published in the NINDS rt-PA trial[1].The recommended dosage of rt-PA (Actilyse,Boehringer Ingelheim,Germany)was0.9mg/kg. However,in some special circumstances such as in patients who are older than80years,the dosage could be lowered to 0.6mg/kg[9].Ten percent of the dosage was given as a bolus dose and the remaining was infused intravenously within1h.
General and neurological examinations together with the National Institute of Health stroke scale(NIHSS)and mod-i?ed Rankin scale(MRS)were recorded prior to and after the treatment.Types of stroke were de?ned by the criteria used in TOAST study and the Oxfordshire Community Stroke Project[10,11].After thrombolysis,repeat measurements of the NIHSS were done at1h,24h and on daily basis until the patient was discharged or dead.Major neurological improve-ment was de?ned as improvement of NIHSS≥8points or an NIHSS score of0at24h.Repeat CT scan of the brain was scheduled at24h after the initiation of the treatment.In case of neurological worsening,CT scan would be performed soon after the detection of deterioration.Intracerebral hemor-rhage was diagnosed by CT scan.Symptomatic hemorrhage was de?ned as hemorrhagic lesion on CT scan with clinical worsening of NIHSS more than4points.Final evaluation of the NIHSS and MRS was performed at3months.Death within3months was also recorded.
3.Results
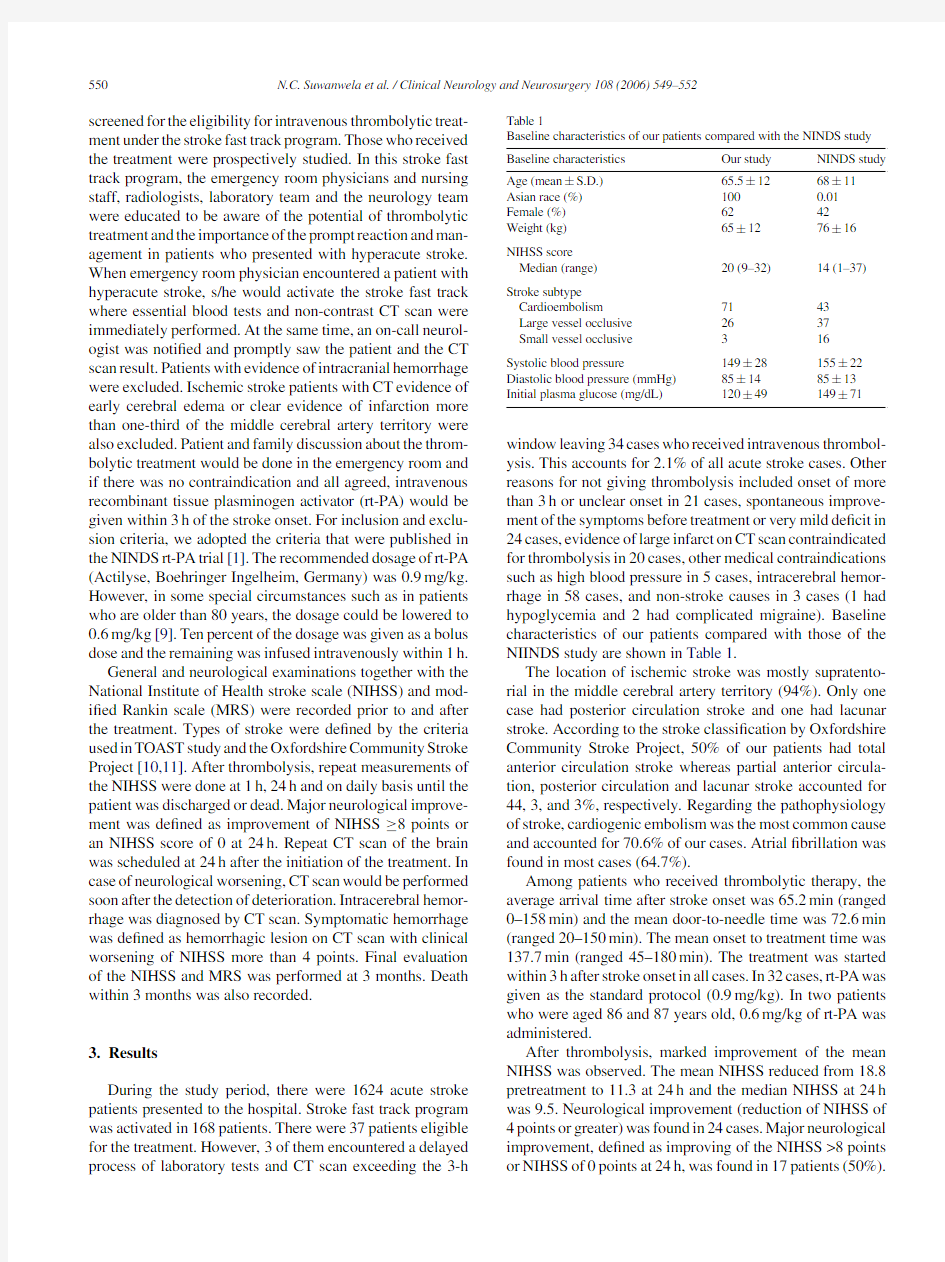
During the study period,there were1624acute stroke patients presented to the hospital.Stroke fast track program was activated in168patients.There were37patients eligible for the treatment.However,3of them encountered a delayed process of laboratory tests and CT scan exceeding the3-h Table1
Baseline characteristics of our patients compared with the NINDS study Baseline characteristics Our study NINDS study Age(mean±S.D.)65.5±1268±11 Asian race(%)1000.01 Female(%)6242
Weight(kg)65±1276±16 NIHSS score
Median(range)20(9–32)14(1–37) Stroke subtype
Cardioembolism7143
Large vessel occlusive2637
Small vessel occlusive316
Systolic blood pressure149±28155±22 Diastolic blood pressure(mmHg)85±1485±13 Initial plasma glucose(mg/dL)120±49149±71 window leaving34cases who received intravenous thrombol-ysis.This accounts for2.1%of all acute stroke cases.Other reasons for not giving thrombolysis included onset of more than3h or unclear onset in21cases,spontaneous improve-ment of the symptoms before treatment or very mild de?cit in 24cases,evidence of large infarct on CT scan contraindicated for thrombolysis in20cases,other medical contraindications such as high blood pressure in5cases,intracerebral hemor-rhage in58cases,and non-stroke causes in3cases(1had hypoglycemia and2had complicated migraine).Baseline characteristics of our patients compared with those of the NIINDS study are shown in Table1.
The location of ischemic stroke was mostly supratento-rial in the middle cerebral artery territory(94%).Only one case had posterior circulation stroke and one had lacunar stroke.According to the stroke classi?cation by Oxfordshire Community Stroke Project,50%of our patients had total anterior circulation stroke whereas partial anterior circula-tion,posterior circulation and lacunar stroke accounted for 44,3,and3%,respectively.Regarding the pathophysiology of stroke,cardiogenic embolism was the most common cause and accounted for70.6%of our cases.Atrial?brillation was found in most cases(64.7%).
Among patients who received thrombolytic therapy,the average arrival time after stroke onset was65.2min(ranged 0–158min)and the mean door-to-needle time was72.6min (ranged20–150min).The mean onset to treatment time was 137.7min(ranged45–180min).The treatment was started within3h after stroke onset in all cases.In32cases,rt-PA was given as the standard protocol(0.9mg/kg).In two patients who were aged86and87years old,0.6mg/kg of rt-PA was administered.
After thrombolysis,marked improvement of the mean NIHSS was observed.The mean NIHSS reduced from18.8 pretreatment to11.3at24h and the median NIHSS at24h was9.5.Neurological improvement(reduction of NIHSS of 4points or greater)was found in24cases.Major neurological improvement,de?ned as improving of the NIHSS>8points or NIHSS of0points at24h,was found in17patients(50%).
N.C.Suwanwela et al./Clinical Neurology and Neurosurgery108(2006)549–552551
Table2
Complications after thrombolytic treatment
Complications Cases(%) Hemorrhagic brain lesion4(11.8) Symptomatic2(5.9) Death2(5.9) Intracerebral hemorrhage1 Massive infarction1
There were nine cases who NIHSS did not improve for more than2points after treatment.The mean NIHSS at3months was6.9.Regarding the treatment complications,intracere-bral hemorrhage was found in4cases(11.8%).Two patients died during acute phase of treatment.The complications are shown in Table2.
4.Discussion
We report our experience on rt-PA treatment in acute ischemic stroke.According to our knowledge,this is the?rst report of prospective case series in Asia.In Thailand,the cost of thrombolytic treatment of all patients is paid either by the government under the National program for universal cover-age or private insurance.Therefore,the treatment is available for all eligible patients in this study.Although the use of intra-venous thrombolysis has been known to be effective in acute stroke patients for almost a decade,we only treated seven cases with intravenous thrombolysis during4years before the establishment of stroke fast track protocol.The number of treated patients increased to34after the program.This accounted only for2.1%of our acute stroke patients and the rate was still much lower than those reported in developed countries[12,13].
In this study,we treated34out of37eligible patients presented within3h of onset.This suggests that with well-organized in-hospital process,more than90%of patients who presented in time can be treated successfully.Hence, our major obstacle for getting more patients is the delayed in hospitalization.Since the ambulance system in Thailand is still not well organized,we had only cases who presented to the emergency room by themselves.We strongly believe that public health initiatives and education are essential to increase the number of patients eligible for treatment in the future.
Among patients who were treated with thrombolytic agent,the NIHSS prior to treatment in this study was much higher than the NINDS studies.Moreover,most of our patients clinically had large stroke in the MCA territory which usually has severe focal de?cits.In this study,94% of the cases had ischemic stroke in the middle cerebral artery territory and50%of them had total anterior circulation infarc-tion.Regarding the cause of stroke,cardiogenic embolism accounts for71%of the cases.This may re?ect the sudden onset and the severity of the symptoms of cardiac emboli.Moreover,the cardioembolic nature might in?uence the out-come since patients with cardiogenic embolism are more likely to have migration of embolus resulting in sponta-neous improvement[14].On the other hand,the prognosis of patients with large hemispheric stroke in the MCA terri-tory is relatively poor despite any conventional treatment due to the high rate of spontaneous hemorrhagic transformation and malignant brain edema[15].
In this study,we were able to administer thrombolytic agent within3h in all cases.Our mean door-to-needle time was comparable to other studies performed in developed countries[11,16–18].In two extreme elderly patients,only 0.6mg/kg of rt-PA were administered.This is mainly due to attending physician preference since older patients were more likely to develop bleeding complications.The rt-PA dosage of0.6mg/kg was also used in a study of thrombolysis from Japan[9].Despite the severe symptoms and possible large area of ischemia at presentation,50%of our patients had major neurological improvement.A recent study using the data from the NINDS trial found that the major neurological improvement was noted in32.5%of the cases[19].
It is generally believed that risk of intracerebral hemor-rhage is higher among the Asian than the Caucasian.This is mainly based on the incidence of hypertensive cerebral hemorrhage.However,the risk of hemorrhagic transforma-tion in patients with ischemic stroke among the Asian is not well documented.In general,the occurrence of hem-orrhagic complications after ischemic stroke is associated with large infarcts especially proximal MCA occlusion due to cardioembolic stroke as in our study population[20–23]. In this study,however,the overall rate of intracerebral hem-orrhage was11.8%and the symptomatic hemorrhage was found in5.9%.Although it is little higher than the rate of hemorrhage in the NINDS study(6.7%),we believed that it is mainly due to the severity of our patients.In this study,more than50%of the cases had the pretreatment NIHSS score of more than20.It was shown in the NINDS study that hem-orrhages were likely to occur in patients with very severe strokes(NIHSS scores>20).However,these patients with severe stroke would probably have died or been left disabled without thrombolytic treatment[24,25].
In conclusion,our experience on the rt-PA treatment in Asian stroke patients showed that it is feasible to set up a spe-cial stroke fast track program in order to identify hyperacute stroke patients.With this program we were able to effec-tively treat2.1%of our cases with intravenous thrombolytic therapy.Although we treated more severe patients,the rate of major improvement was as high as those previously reported. More importantly,the rate of symptomatic and asymptomatic intracerebral hemorrhages were only little higher than other studies.Therefore,we recommend that thrombolytic treat-ment in acute ischemic stroke in our selected Asian popula-tion is at least as useful and not more harmful when compare to the Caucasian.We are aware that we have limited number of cases in this series and further studies in Asia are needed to con?rm our?ndings.
552N.C.Suwanwela et al./Clinical Neurology and Neurosurgery108(2006)549–552
References
[1]The National Institute of Neurological Disorders and Stroke rt-PA
Stroke Study Group.Tissue plasminogen activator for acute ischemic stroke.N Engl J Med1995;333:1581–7.
[2]Hacke W,Kaste M,Fieschi C,Toni D,Lesaf?re E,von Kum-
mer R,et al.Intravenous thrombolysis with recombinant tissue plasminogen activator for acue hemispheric stroke:the European Cooperative Acute Stroke Study(ECASS).JAMA1995;274:1017–
25.
[3]Hacke W,Kaste M,Fieschi C,von Kummer R,Davalos A,Meier
D,et al.Randomised double-blind placebo-controlled trial of throm-bolytic therapy with intravenous alteplase in acute oischemic stroke (ECASS II).Lancet1998;352:1245–51.
[4]Klijn CJM,Hankey G.Management of acute ischemic stroke:new
guidelines from the American Stroke Association and European Stroke https://www.doczj.com/doc/c08797126.html,ncet Neurol2003;2:698–701.
[5]Adams Jr HP,Adams RJ,Brott T,del Zoppo GJ,Furlan A,Gold-
stein LB,et al.,Stroke Council of the American Stroke Association.
Guidelines for the early management of patients with ischemic stroke.A scienti?c statement from the Stroke Council of the Amer-ican stroke Association.Stroke2003;34:1056–83.
[6]European Stroke Initiative Executive Committee and Writing Com-
mittee.The European Stroke Initiative recommendation for stroke management update.Cerebrovasc Dis2003;16:311–8.
[7]Yamaguchi T,Japanese Thrombolysis Study Group.Intravenous tis-
sue plasminogen activator in acute carotid artery territory stroke:a placebo controlled,double blind trial.In:del Zoppe GJ,Mori E, Hacke W,editors.Thrombolytic Therapy in Acure Ishcmic Strije II.
New York,NY:Springer Verlag;1993.p.59–65.
[8]The Asian Acute Stroke Advisory Panel.Stroke epidemiological
data of nine Asian https://www.doczj.com/doc/c08797126.html,n Acute Stroke Advisory Panel (AASAP).J Med Assoc Thai2000Jan;83(1):1–7.
[9]Minematsu K,Yamaguchi T,Hashi K,Shinohara Y,Saito I,Mori
E,et al.Results of clinical trial of intravenous rt-PA(Alteplase)for acute ischemic stroke:Japan Alteplase Clinical Trial(J-ACT).In: Presented at5th World Stroke Congress.2004(abstract).
[10]Bamford J,Sandercock P,Dennis M,Warlow C,Jones L,McPher-
son K,et al.A prospective study of acute cerebrovascular disease in the community:the Oxfordshire Community Stroke Project.1.
Methodology,demography and incident cases of?rst-ever stroke.J Neurol Neurosurg Psychiatry1988;51:1373–80.
[11]Adams Jr HP,Bendixen BH,Kappelle LJ,Biller J,Love BB,
Gordon DL,et al.Classi?cation of subtype of acute ischemic stroke.De?nitions for use in a multicenter clinical trial.TOAST.
Trial of Org10172in Acute Stroke Treatment.Stroke1993;24: 35–41.[12]Kapral MK,Laupacis A,Phillips SJ,Silver FL,Hill MD,Fang J,et
al.,for the investigators of the registry of the Canadian Stroke Net-work.Stroke care delivery in institutions participating in the registry of the Canadian stroke network.Stroke2004;35:1756–62.
[13]Grotta JC,Burgin WS,El-Mitwalli A,Long M,Campbell M,Mor-
genstern LB,et al.Intravenous tissue-type plasminogen activator therapy for ischemic stroke:Houston experience1996to2000.Arch Neurol2001;58(12):2009–13.
[14]Minematsu K,Yamaguchi T,Omae T.Spectacular shrinking de?cit:
rapid recovery from a major hemispheric syndrome by migration of an embolus.Neurology1992;42(1):157–62.
[15]Hacke W,Schwab S,Horn M,Spranger M,De Georgia M,von Kum-
mer R.Malignant middle cerebral artery territory infarction:clinical course and prognostic signs.Arch Neurol1996;53(4):309–15. [16]Szoeke CE,Parsons MW,Butcher KS,Baird TA,Mitchell PJ,Fox
SE,et al.Acute stroke thrombolysis with intravenous tissue plas-minogen activator in an Australian tertiary hospital.Med J Aust 2003;178(7):324–8.
[17]Merino JG,Silver B,Wong E,Foell B,Demaerschalk B,Tamayo
A,et al.Southwestern Ontario Stroke Program.Extending tissue plasminogen activator use to community and rural stroke patients.
Stroke2002;33(1):141–6.
[18]Koennecke HC,Nohr R,Leistner S,Marx P.Intravenous tPA for
ischemic stroke team performance over time,safety,and ef?cacy in
a single-center,2-year experience.Stroke2001;32(5):1074–8.
[19]Brown DL,Johnston KC,Wagner DP,Haley EC.Predicting major
neurological improvement with intravenous recombinant tissue plas-minogen activator treatment of stroke.Stroke2004;35:147–50. [20]Rimdusid P,Wardlow J,Lindley RI,Sandercock P,on behalf of the
International Stroke Tiral Collaboration Group.Hemorrhagic infarc-tion in acute ischemic stroke patients:International Stroke Trial Pilot Study.Cerebrovasc Dis1995;5:264.
[21]Pessin MS,Teal PA,Caplan LR.Hemorrhagic transformation:guilt
by association?Am J Neuroradiol1992;12:1123–6.
[22]Caplan LR,Mohr JP,Kistler JP,Koroshetz WJ.Should thrombolytic
therapy be the?rst-line treatment for acute ischemic stroke?N Engl J Med1997;337:1309–13.
[23]Schneweis S,Grond M,Neveling M,Schmulling S,Rudolf J,Heiss
WD.Intravenous thrombolysis in proximal middle cerebral artery occlusion.Cerebrovasc Dis2001;11(3):212–5.
[24]Grotta J.t-PA—the best current option for most patients.N Engl J
Med1997;337:1309–13.
[25]Tanne D,Kasner SE,Demchuk AM,Koren-Morag N,Hanson S,
Grond M,et al.Markers of increased risk of intracerebral hem-orrhage after intravenous recombinant tissue plasminogen activator therapy for acute ischemic stroke in clinical practice,the multicenter rt-PA acute stroke survey.Circulation2002;105:1679–85.