欧洲肌骨超声检查指南 肩关节
- 格式:pdf
- 大小:2.54 MB
- 文档页数:8
血管和浅表器官超声检查指南图书信息作者:中国医师协会超声医师分会出版社:人民军医出版社; 第1版(2011年6月1日)平装: 172页正文语种:简体中文开本: 32ISBN: 9787509148358条形码: 9787509148358产品尺寸及重量: 20.8 x 14.2 x 1 cm ; 322 g内容简介《血管和浅表器官超声检查指南》由中国医师协会超声医师分会邀请众多专家参与讨论编写而成,是国内第一部规范超声科医师检查技术、规范血管和浅表器官疾病的超声诊断和鉴别诊断标准的指南。
内容包括:血管超声检查指南、甲状腺超声检查指南、乳腺超声检查指南、肌肉骨骼超声检查指南。
每篇指南包含检查目的、适应证和禁忌证、检查前准备、检查方法、正常超声表现、超声观察内容,以及各种疾病的超声图像表现和报告书写要点等,适合各年资医师学习阅读,是指导超声医师临床工作的规范性文本。
编辑推荐《血管和浅表器官超声检查指南》由中国医师协会超声医师分会起草,目的存于指导中国超声医师、超声检查技术或相关人员应用彩色多普勒超声进行血管和浅表器官的检查中国医师协会超声医师分会将根据学科发展适时进行修改,以保障其先进性。
欢迎对此指南提出修改建议并请与中国医师协会超声医师分会联系。
目录上篇血管超声检查指南第1章头颈部血管超声检查指南第一节经颅多普勒超声常规检查指南第二节经颅彩色多普勒超声检查指南第三节颈动脉、椎动脉及锁骨下动脉多普勒超声检查指南第2章腹部血管超声检查指南第一节腹主动脉瘤多普勒超声检查指南第二节腹腔干(CA)、肠系膜上动脉(SMA)和肠系膜下动脉(1MA)多普勒超声检查指南第三节下腔静脉(IVC)多普勒超声检查指南第叫节肝门静脉多普勒超声检查指南第五节肝移植术后并发症多普勒超声检查指南第六节肾动脉多普勒超声检查指南第七节移植肾多普勒超声检查指南第3章四肢血管超声检查指南第一节上肢动脉多普勒超声检查指南第二节上肢静脉血栓多普勒超声检查指南第三节髂动脉及下肢动脉多普勒超声检查指南第四节髂静脉及下肢静脉血栓多普勒超声检查指南第五节下肢静脉反流多普勒超声检查指南第六节下肢浅静脉超声评价与标记指南第七节动静脉造瘘术前上肢血管多普勒超声评价指南第八节血液透析及静脉内瘘多普勒超声检查指南附录外周动脉脉冲多普勒频谱采集下篇浅表器官超声检查指南第4章甲状腺超声检查指南第5章乳腺超声检查指南第6章肌肉骨骼系统超声检查指南第一节概述第二节肩关节及肩锁关节第三节肘关节第四节腕关节第五节膝关节第六节髋关节第七节距小腿关节(踝关节)第八节骨骼及软组织肿瘤第九节周围神经。
·经验交流·肱二头肌长头肌腱腱鞘积液对超声引导下治疗冻结肩疗效的影响韦宗凯胡彧彭晓静杭菁叶新华李奥摘要目的探讨肱二头肌长头肌腱腱鞘积液对超声引导下关节腔注射治疗冻结肩疗效的影响。
方法选取经临床诊断为冻结肩的患者81例,根据有无肱二头肌长头肌腱腱鞘积液分为腱鞘积液组42例和无腱鞘积液组39例,两组均行超声引导下关节腔注射治疗,并于治疗前和治疗后2周行高频超声检查,获得腋下关节囊(ARC)厚度,同时行Constant-Murley肩关节功能评分,并对两组结果进行比较分析。
ARC厚度与Constant-Murley肩关节功能评分间的相关性分析采用Pearson相关分析法。
结果与治疗前比较,两组患者治疗后ARC厚度均减少,Constant-Murley肩关节功能评分均增高,差异均有统计学意义(均P<0.05);治疗后与无腱鞘积液组比较,腱鞘积液组Constant-Murley肩关节功能评分降低,ARC厚度增大,差异均有统计学意义(均P<0.05)。
Pearson相关分析显示,Constant-Murley肩关节功能评分与ARC厚度呈负相关(r=-0.40,P<0.05)。
结论肱二头肌长头肌腱腱鞘积液会影响超声引导下关节腔注射治疗冻结肩的疗效;ARC厚度可作为超声引导下肩关节腔注射治疗冻结肩疗效评价的参考指标。
关键词超声检查;冻结肩;腱鞘积液;腋下关节囊;关节腔注射[中图法分类号]R445.1;R687.2[文献标识码]AInfluence of biceps longus tendon sheath effusion on the treatment ofultrasound-guided for frozen shoulderWEI Zongkai,HU Yu,PENG Xiaojing,HANG Jing,YE Xinhua,LI AoDepartment of Ultrasound,the First Affiliated Hospital,Nanjing Medical University,Nanjing210000,ChinaABSTRACT Objective To explore the influence of biceps longus tendon sheath effusion on the treatment of ultrasound-guided intra-articular injections in patient with frozen shoulder.Methods A total of81patients with clinically diagnosed frozen shoulders were divided into group with tendon sheath effusion of biceps brachii longus and group without tendon sheath effusion of biceps brachii longus.All patients were underwent ultrasound-guided intra-articular injections,and high-frequency ultrasound examinations were performed to measure axillary recess capsule(ARC)thickness before and2weeks after the injection,and Constant-Murley shoulder score were evaluated.The results were compared and analyzed. Pearson correlation analysis was used to analyze the correlation between ARC thickness and Constant-Murley shoulder score. Results Compared with the results before treatment,the ARC thickness of the two groups was reduced and the Constant-Murley shoulder scores was increased after treatment.The differences were statistically significant(all P<0.05).Compared with the group without tendon sheath effusion after the treatment,the Constant-Murley shoulder score of group with tendon sheath effusion was significantly decreased,and the ARC thickness was increased.The difference were statistically significant(both P<0.05). Pearson correlation analysis showed that Constant-Murley shoulder score was negatively correlated with ARC thickness(r=-0.40,P<0.05).Conclusion Tendon sheath effusion of biceps brachii longus can affect the efficacy of ultrasound-guided intra-articular injections for frozen shoulder.ARC thickness can be used as a reference index for evaluation of ultrasound-guided intra-articular injections for frozen shoulder.KEY WORDS Ultrasonography;Frozen shoulder;Tendon sheath effusion;Axillary recess capsule;Intra-articular injection基金项目:国家自然科学基金青年科学基金项目(81401427)作者单位:210000南京市,南京医科大学第一附属医院超声诊断科通讯作者:李奥,Email:****************冻结肩是一种以肩关节疼痛和活动受限为特征的疾病,好发于50岁左右人群,女性多见[1]。

肌骨超声引导下PRP肩袖间隙注射治疗冻结肩的临床疗效及机制研究郑苏;王刚;赵磊;解嘉阳;谢谨;郭爽【期刊名称】《湖北医药学院学报》【年(卷),期】2024(43)2【摘要】目的:观察肌骨超声(MSKUS)引导下富血小板血浆(PRP)肩袖间隙注射治疗冻结肩的临床疗效,并探讨其机制。
方法:60例冻结肩患者随机分为对照组和治疗组,每组各30例,治疗组采取PRP注射治疗,对照组采取倍他米松+9%氯化钠溶液注射治疗。
治疗2个疗程后,比较两组患者Constant-Murley肩关节功能评分、肩周后方关节囊厚度(PCT)、盂肱距离(GHD)和TNF-α、IL-6含量及临床疗效等。
结果:治疗后两组患者Constant-Murley肩关节功能评定疼痛、ADL、ROM、MMT评分较治疗前均有提升(P<0.05),且治疗组改善更明显(P<0.05)。
两组患者TNF-α和IL-6含量较治疗前均有所降低(P<0.05),且治疗组降低更明显(P<0.05)。
两组患者治疗后PCT均降低,GHD均提高,较治疗前差异有统计学意义(P<0.05),且治疗组改善更明显(P<0.05)。
治疗组总有效率为96.6%,对照组总有效率为93.1%,差异有统计学意义(P<0.05)。
结论:MSKUS引导下PRP肩袖间隙注射治疗冻结肩,可减轻患者疼痛,改善肩关节功能,提高临床疗效,可能与调节TNF-α、IL-6含量水平,修复PCT和GHD组织损伤有关。
【总页数】5页(P147-151)【作者】郑苏;王刚;赵磊;解嘉阳;谢谨;郭爽【作者单位】十堰市太和医院·湖北医药学院附属医院医务处;湖南中医药大学【正文语种】中文【中图分类】R72【相关文献】1.超声引导下肩袖三角间隙注射结合常规康复技术治疗部分及全层小撕裂型肩袖损伤2.超声引导下多次肩袖间隙糖皮质激素注射治疗疼痛期粘连性肩关节囊炎的短期疗效3.超声引导脉冲射频肩胛上神经调控复合臭氧肩袖间隙注射应用于肩袖损伤治疗效果观察4.超声引导下肩袖间隙注射及肩胛上神经阻滞联合触发点针刺治疗粘连性肩关节囊炎的疗效分析5.超声引导下肩袖间隙注射配合“肩三针”针灸治疗冈上肌腱炎的疗效观察因版权原因,仅展示原文概要,查看原文内容请购买。
肌肉骨骼超声技术指南2.肘关节注释:系统扫描技术如下所述。
考虑到肘关节的检查,多集中在基于临床发现的关节的一个象限这一事实,该指南只是操作上理论性的指导。
1、肘部前侧 anterior elbow为了检查前肘,患者面对检查者就座,肘部处于桌子上方的伸展位置。
要求患者伸展肘部并将前臂旋转,手心向上,患者身体朝向被检查侧稍微弯曲,使得完全旋转,并且更容易对前房进行评估。
通过在关节下放置枕头可以获得完全的肘部伸展。
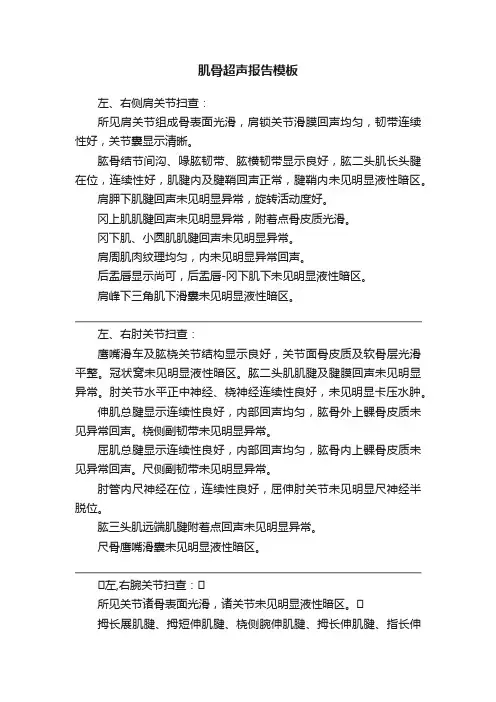
横向超声图像的获得,将探头垂直于肱骨干,从滑车-尺骨关节下方大约5cm上下进行扫描,获得髁上区域的图像,示浅表二头肌和深肱肌。
在这些肌肉的旁边和内侧,走形着肱动脉和正中神经:神经位于动脉的内侧。
图例:a,肱动脉; 箭头,正中神经;箭头,远端肱二头肌腱; 星号,肱骨滑车关节软骨; Br,肱肌; Pr,旋前肌2、远端二头肌肌腱 distal biceps tendon检查远端肱二头肌肌腱,同时保持患者的前臂处于最大旋后,以使腱插入桡骨结节进入视野。
由于从表面到深度的倾斜过程,如果探针不与其保持平行,则该肌腱的部分可能出现人为低回声。
因此,必须将探针的远端半部轻轻地推向患者的皮肤,以确保US探头和远端二头肌腱之间的平行,从而允许其纤维图案的充分可视化。
他的远端二头肌肌腱最好在其长轴上进行检查。
短轴平面检查肱二头肌的远端部分不太有用,因为探针取向的轻微变化可能产生肌腱回声的显着变化并在肌腱和邻近动脉之间产生混淆。
沿着长轴平面上的短肱肌腱跟随其在冠突上的插入。
图例:箭头,远端肱二头肌腱; 星号,冠状窝和前脂肪垫; Br,肱肌; HC,肱骨头; RH,径向头; s,旋后肌3、前侧关节凹部 anterior joint recess:使用内侧矢状平面检查冠状窝,其显示为充满前脂肪垫的肱骨前表面的凹面。
在正常状态下,在脂肪垫和肱骨之间可以看到少量的液体。
在横向扫描中,前肱骨远端骨骺表现为由低回声关节软骨薄层覆盖的波状高回声线:其外侧三分之一对应于肱骨头(圆形),而其内侧三分之一对应于肱骨滑车(V- 形)。
肌骨超声报告模板左、右侧肩关节扫查:所见肩关节组成骨表面光滑,肩锁关节滑膜回声均匀,韧带连续性好,关节囊显示清晰。
肱骨结节间沟、喙肱韧带、肱横韧带显示良好,肱二头肌长头腱在位,连续性好,肌腱内及腱鞘回声正常,腱鞘内未见明显液性暗区。
肩胛下肌腱回声未见明显异常,旋转活动度好。
冈上肌肌腱回声未见明显异常,附着点骨皮质光滑。
冈下肌、小圆肌肌腱回声未见明显异常。
肩周肌肉纹理均匀,内未见明显异常回声。
后盂唇显示尚可,后盂唇-冈下肌下未见明显液性暗区。
肩峰下三角肌下滑囊未见明显液性暗区。
左、右肘关节扫查:鹰嘴滑车及肱桡关节结构显示良好,关节面骨皮质及软骨层光滑平整。
冠状窝未见明显液性暗区。
肱二头肌肌腱及腱膜回声未见明显异常。
肘关节水平正中神经、桡神经连续性良好,未见明显卡压水肿。
伸肌总腱显示连续性良好,内部回声均匀,肱骨外上髁骨皮质未见异常回声。
桡侧副韧带未见明显异常。
屈肌总腱显示连续性良好,内部回声均匀,肱骨内上髁骨皮质未见异常回声。
尺侧副韧带未见明显异常。
肘管内尺神经在位,连续性良好,屈伸肘关节未见明显尺神经半脱位。
肱三头肌远端肌腱附着点回声未见明显异常。
尺骨鹰嘴滑囊未见明显液性暗区。
左,右腕关节扫查:所见关节诸骨表面光滑,诸关节未见明显液性暗区。
拇长展肌腱、拇短伸肌腱、桡侧腕伸肌腱、拇长伸肌腱、指长伸肌腱、尺侧腕伸肌腱连续性良好,厚度正常,内部回声均匀,伸肌支持带未见增厚,腱鞘内未见明显液性暗区。
尺侧腕屈肌腱、掌长肌腱、指长屈肌腱、拇长屈肌腱、桡侧腕屈肌腱连续性良好,厚度正常,内部回声均匀,腕横韧带未见增厚,腱鞘内未见明显液性暗区。
腕管水平正中神经、Guyon管尺神经连续性良好,形态正常。
大鱼际肌、小鱼际肌、骨间肌、蚓状肌纤维回声良好,内未见明显异常回声。
左、右髋关节扫查所见关节显示可,关节囊未见明显液性暗区。
缝匠肌及阔筋膜张肌髂前上棘起点未见明显异常。
股直肌髂前下棘起点、髂腰肌小转子止点未见明显异常。