E?ect of carbocisteine on acute exacerbation of chronic obstructive pulmonary disease (PEACE Study): a randomised placebo-controlled study
Jin-Ping Zheng, Jian Kang, Shao-Guang Huang, Ping Chen, Wan-Zen Yao, Lan Yang, Chun-Xue Bai, Chang-Zheng Wang, Chen Wang,
Bao-Yuan Chen, Yi Shi, Chun-Tao Liu, Ping Chen*, Qiang Li, Zhen-Shan Wang, Yi-Jiang Huang, Zhi-Yang Luo, Fei-Peng Chen, Jian-Zhang Yuan, Ben-Tong Yuan, Hui-Ping Qian, Rong-Chang Zhi, Nan-Shan Zhong
Summary
Background Chronic obstructive pulmonary disease (COPD) is characterised by air? ow limitation, and has many components including mucus hypersecretion, oxidative stress, and airway in? ammation. We aimed to assess whether carbocisteine, a mucolytic agent with anti-in?ammatory and antioxidation activities, could reduce the yearly exacerbation rate in patients with COPD.
Methods We did a randomised, double-blind, placebo-controlled study of 709 patients from 22 centres in China. Participants were eligible if they were diagnosed as having COPD with a postbronchodilator forced expiratory volume
in 1 s (FEV
1) to forced vital capacity (FVC) ratio (FEV
1
/FVC) of less than 0·7 and an FEV
1
between 25% and 79% of the
predicted value, were aged between 40 and 80 years, had a history of at least two COPD exacerbations within the previous 2 years, and had remained clinically stable for over 4 weeks before the study. Patients were randomly assigned to receive 1500 mg carbocisteine or placebo per day for a year. The primary endpoint was exacerbation rate over 1 year, and analysis was by intention to treat. This trial is registered with the Japan Clinical Trials Registry (http://umin. ac.jp/ctr/index/htm) number UMIN-CRT C000000233.
Findings 354 patients were assigned to the carbocisteine group and 355 to the placebo group. Numbers of exacerbations per patient per year declined signi? cantly in the carbocisteine group compared with the placebo group (1·01 [SE 0·06] vs1·35 [SE 0·06]), risk ratio 0·75 (95% CI 0·62–0·92, p=0·004). Non-signi? cant interactions were found between the preventive e? ects and COPD severity, smoking, as well as concomitant use of inhaled corticosteroids. Carbocisteine was well tolerated.
Interpretation Mucolytics, such as carbocisteine, should be recognised as a worthwhile treatment for prevention of exacerbations in Chinese patients with COPD.
Funding Kyorin Pharmaceuticals.
Introduction
Chronic obstructive pulmonary disease (COPD) is characterised by air?ow limitation, and patho-physiologically involves many components including mucus hypersecretion, oxidative stress, and in? ammation in the airway and lungs.1 Therefore, agents active with mucolytic, anti-in?ammatory, and antioxidative e? ects could o? er promise for treatment.
In Europe and Asia, mucolytics such as carbocisteine have been widely used for treatment of respiratory diseases with phlegm production2 because of their capacity to facilitate sputum elimination.3,4 Furthermore, carbocisteine seems likely to have a role in antioxidation5,6 and anti-in? ammation7–9 that might be more important than mucolysis itself for long-term management of COPD. Clinical studies have shown bene?ts in preventing exacerbation of COPD with carbocisteine.10–12 H owever, these results have been inconclusive because of certain pitfalls in study design, such as small sample size, not being double-blinded, lack of placebo control, or short period of study.13 Poole and Black14 did a systematic review of mucolytics in COPD, which has been updated15 with
inclusion of the BRONCUS study16 using N-acetylcysteine.
Their results showed that mucolytics including carbo-
cisteine were e? ective in reducing the number of exacer-
bations in COPD and improving health status in all studies
except BRONCUS.16 Since evidence on long-term e? cacy
remains insu? cient, mucolytics are not recom m ended for
regular treatment by guidelines such as that of the Global
Initiative for Chronic Obstructive Lung Disease (GOLD).1
Clinical trials that closely follow reliable research study
designs are therefore warranted to clarify whether COPD
patients can bene? t from protracted mucolytic therapy.
The aim of this study was to assess the e? ectiveness in
preventing exacerbation, improving quality of life, as well
as the safety pro? les of long-term (1-year) carbocisteine
administration in patients with COPD.
Methods
Patients
Participants were eligible for inclusion if they were
diagnosed as having COPD with a postbronchodilator
Lancet 2008; 371: 2013–18
See Comment page 1975
Guangzhou Institute of
Respiratory Disease,
First A? liated Hospital of
Guangzhou Medical College,
Guangzhou,
China (Prof J-P Zheng MD,
Prof N-S Zhong MD);
First A? liated Hospital of China
Medical University, Shenyang,
China (Prof J Kang MD); Ruijing
Hospital, Shanghai Jiao Tong
University Medical School,
Shanghai, China
(Prof S-G Huang MD); Shenyang
PLA General Hospital, Shenyang,
China (P Chen MD); Peking
University Third Hospital,
Beijing, China (Prof W-Z Y ao MD);
First A? liated Hospital, Xi’An
Jiao Tong University, Xi’An, China
(Prof L Y ang MD); Zhongshan
Hospital, Fudan University,
Shanghai, China
(Prof C-X Bai MD); Xin Qiao
Hospital, Chongqing, China
(Prof C-Z Wang MD); Chao Y ang
Hospital, Beijing, China
(Prof C Wang MD); Tianjin General
Hospital, Tianjin, China
(B-Y Chen MD); Nanjing PLA
General Hospital, Nanjing, China
(Y Shi MD); Huaxi Hospital,
Chengdu, China (C-T Liu MD);
Second Xiangya Hospital,
Changsha, China
(*Prof P Chen MD); Changhai
Hospital, Shanghai, China
(Q Li MD); Second A? liated
Hospital of Dalian Medical
University, Dalian, China
(Z-S Wang MD); Hainan Province
Hospital, Haikou, China
(Y-J Huang MD); First Municipal
Hospital, Foshan, China
(Z-Y Luo MD); Second A? liated
Hospital of Guangzhou Medical
College, Guangzhou, China
(F-P Chen MD); Red Cross
Hospital, Guangzhou, China
(J-Z Y uan MD); Second Municipal
Hospital, Shenzhen, China
(B-T Y uan MD); Xinhai Hospital,
Guangzhou, China (H-P Qian MD);
and Panyu Hospital, Guangzhou,
China (R-C Zhi MD)
forced expiratory volume in 1 s (FEV?) to forced vital
capacity (FVC) ratio (FEV?/FVC) of less than 0·70 and an FEV? between 25% and 79% of predicted value. The severity of COPD was de? ned in accordance with GOLD criteria.1
Patients had to be aged between 40 and 80 years,
have a history of at least two COPD exacerbations within the previous 2 years, yet have remained clinically stable for over 4 weeks before the study, and have good oral and writing skills. Smoking status was recorded and veri? ed by history; non-smokers were also included in the study.Patients were excluded if they had a history of physician-diagnosed asthma, non-COPD respiratory disorders, lung volume reduction surgery or transplantation, other conditions likely to interfere with the study, a requirement for long-term oxygen therapy (12 h or more per day) or pulmonary rehabilitation, evidence of alcohol or drug misuse, known or suspected hypersensitivity to the study medication or part of its ingredients, current use of oral corticosteroids, involvement in an investigational drug trial during the previous 12 weeks, or onset of an exacerbation requiring systemic or oral corticosteroid therapy or hospitalisation during the run-in period. Those with a history of severe glaucoma or severe heart, liver, and kidney diseases, or di? use bilateral bronchiectasis, and those in pregnancy or lactation were also excluded from the study.Participants were enrolled from 22 medical centres in China, of which 20 were academic hospital-based centres and two were community-based pulmonary clinics; six were located in northern China, four in eastern China, nine in southern China, and three in western China.The study was approved by local ethics committees and was done in compliance with the Declaration of H elsinki (1996). All patients gave written in-formed consent.
Study design
This was a multicentre, randomised, double-blind, placebo-controlled, parallel-group study. The study protocol was designed by an investigator steering committee and transplanted to all study sites thereafter. All investigators were trained before the trial to ensure reliable study quality, with special emphasis on understanding of the protocol, how to do a spirometry test, blinding of allocation, drug management, and compliance with good clinical practice. Beijing Contract Research Organisation (Beijing, China) was exclusively responsible for data management, data analysis, and data quality control.Randomisation was done using the predetermined computer-generated randomisation list provided by a statis-tician from the Beijing Contract Research Organisation. The processing of ran d om i sation was strati? ed by study centre, based on a block size of four, to allow for a balanced number of participants in both groups at a centre level. At each centre, the enrolled participants were allocated in order of their assigned numbers to the carbocisteine group or the placebo group.Neither the investigator nor the patient knew the group allocation. The placebo was identical to the intervention drug in appearance, labelling, and packaging, but did not contain any active ingredients.Supplies of tablets for every patient were identi? ed with
a three-digit number. A sealed envelope that contained the randomisation code for any given patient was kept by the
investigator and was not to be broken during the study,
except in cases of a serious life-threatening adverse event.
Opening of a certain envelope, whether intentional or
accidental, had to be carefully recorded on the related
case-report form, and the patient had to be withdrawn from the study. The steering committee and the independent party who did the statistics analysis were
blocked from all information about treatment allocations during the study.
After a 2-week run-in period, eligible patients with COPD were randomly assigned to receive carbocisteine (2×250 mg, three times daily) or placebo (two tablets, three times daily) for 1 year. Both carbocisteine and placebo tablets were provided by Baiyunshan Pharmaceutical, China. No other medications were provided as part of the study.After randomisation, patients were interviewed every
3 months until the end of trial to con? rm their vital signs, record any unscheduled visits to a health-care provider, check their adherence to the study regimen by collecting and counting the number of remaining tablets, record adverse events, and re? ll study tablets for the next 3 months.Conventional treatment for COPD, such as short-acting
or long-acting bronchodilators and inhaled corticosteroids,
Figure 1: Trial pro? le Correspondence to:
Nan-Shan Zhong, State Key Laboratory of Respiratory Diseases, Guangzhou Institute of
Respiratory Disease, First A? liated Hospital of Guangzhou Medical College, Guangzhou 510120, China nanshan@https://www.doczj.com/doc/9718259282.html,
that had been started before the study, was permitted to continue but had to be sustained during the study period. Sys t emic administrations of corticosteroids, antibiotics, muco l ytics, or antitussive agents were not permitted unless con c omitant use of these agents were needed to treat exacerbation.
Outcome measures
The primary endpoint was exacerbation rate over 1 year. Exacerbation de? ned by Anthonisen17was used—ie, at least 2-day persistence of at least two major symptoms (worsening dyspnoea and an increase in sputum purulence, volume, or both), or of any single major symptom plus more than one minor symptom (upper airway infection, unexplained fever, and increased wheezing). Clinical data such as di? culty breathing, the amount and trait of sputum, fever, and presence of upper airway infection were followed-up using a patient diary card, and were reviewed between the patient and his or her attending physician at each interview before ? nal validation as an exacerbation by the steering committee. Secondary endpoints included covariance-adjusted exacerbation rate, quality of life, lung function and arterial oxygen saturation. Exacerbation rates strati? ed by months on treatment (3, 6, and 9 months) were also assessed. Quality of life was assessed by St George’s Respiratory Questionnaire (SGRQ) scores.18 The patients completed an SGRQ (using a validated Chinese version) before randomisation and at the end of study while they were clinically stable, under the supervision of clinical sta?trained on questionnaire administration.
At the start and end of the study, postbronchodilator spirometry was done according to American Thoracic Society recommendations for acceptability and repro-ducibility.19 FEV? was measured 20 min after inhalation of 400 μg salbutamol via a spacer. Predicted FEV? values were selected from the European Committee of Coal and Steel predictions20 and adjusted for Chinese ethnicity according to Zheng and Zhong’s recommen d ation21 to minimise variations from ethnic di? erences.
SpO? as measured by ? nger pulse oximetry was taken at the end of the run-in period and at 6 and 12 months of treatment. Adverse events were reviewed at each study interview.
Statistical analysis
Accurate calculation of sample size had been an issue of
great attention when planning the trial, but we were unable to do so because of a scarcity of reference data from previously published studies. Consequently, the sample size was determined on the basis of experiences of Chinese respiratory doctors and by the steering committee. The estimated sample size was deemed to be powered for this study.
All statistical analyses for baseline characteristics and outcomes were done on an intention-to-treat basis. Quanti-tative baseline characteristics and outcome measures were reported as means (SD) or as percentages within groups.
Exacerbation rate was analysed with a negative binomial
regression model including inter a ctions between treatment
and covariates (such as COPD stages, smoking status, and
concomitant medications). If interaction was not signi? -
cant, the treatment e? ect was assessed with a regression
model adjusted by covariant. Risk ratio and 95% CI in the
carbocisteine group versus placebo group were reported.
Log-rank test was used to compare the di? erence of
exacerbation in percentages between groups. SGRQ scores
Figure 2: Kaplan-Meier plot of probability of being exacerbation-free at each time point through the study
(total, symptom, activity, and impact score) and post-bronchodilator FEV
1
were analysed as changes from baseline values with Wilcoxon’s rank-sum test. χ2 test or Fisher’s exact test were used to compare the di? erence in percentages between groups.
Safety pro? les were assessed by safety set analysis. All hypothesis tests were two-sided, and p<0·05 was de? ned as signi?cant. No interim analysis was planned. All statistical analyses were done with a validated software package (SAS version 9.1).
Role of the funding source
The funding source had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had ? nal responsibility for the decision to submit for publication.
Results
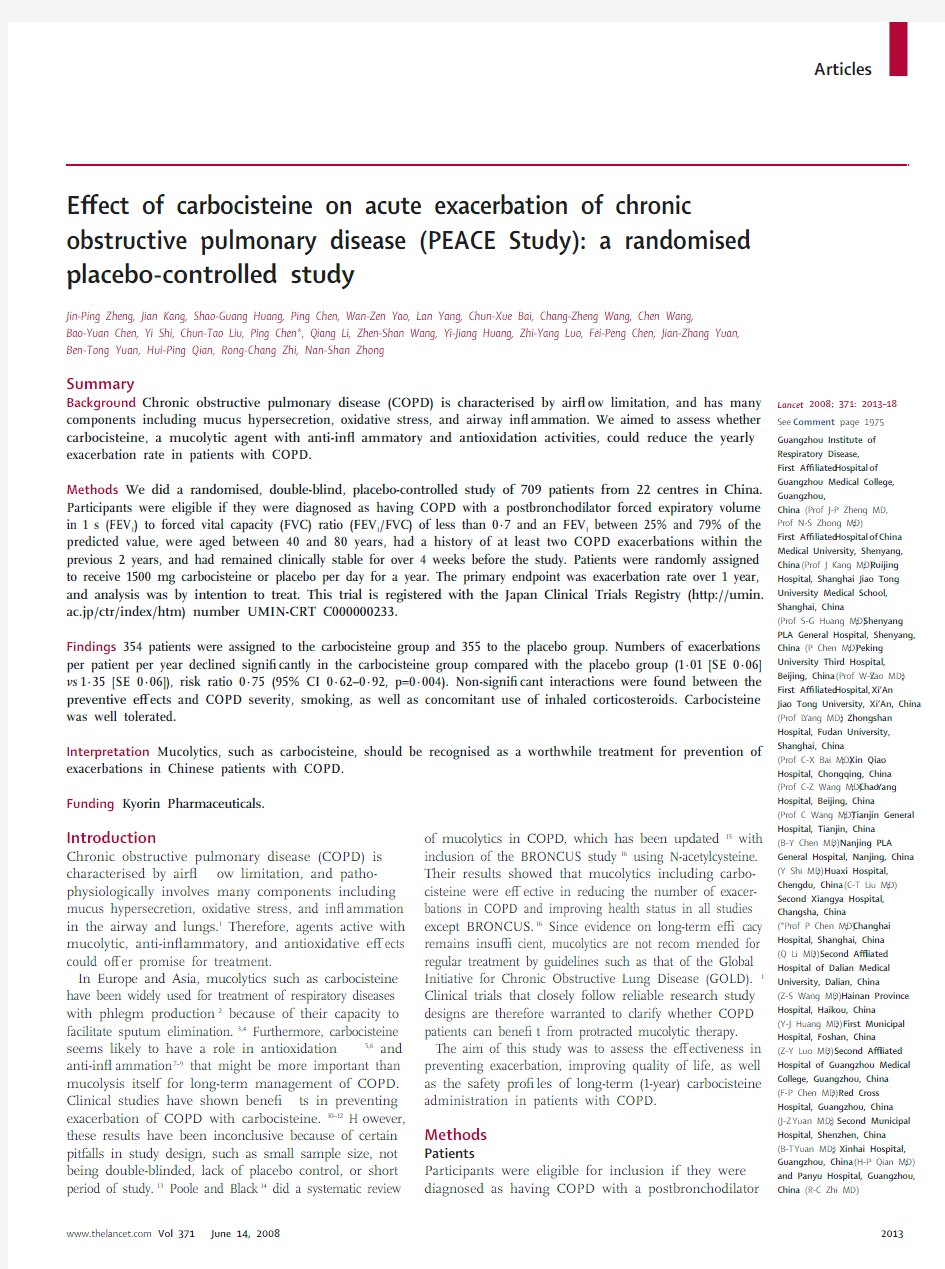
Recruitment ran from June 1 to Sept 30, 2005, and the study was completed by Oct 15, 2006. 709 patients underwent randomisation (? gure 1). Of these, two patients (one in each group) were excluded because of ineligibility, but were included in the safety analysis. Non-signi? cant di? erence was found in the withdrawal rate between these two groups (13·60% vs 12·15%, χ2=0·332; p=0·565).
The two groups were similar in patient demographics, including history of smoking, duration and severity of COPD, baseline pulmonary function, quality of life, and base l ine medication (table 1). COPD stages II and III accounted for 88·1% (623 of 707) of the patients, with the rest being stage IV. Before this study, the most common bronchodilator used was xanthines, followed by β agonists and anticholinergics, whereas inhaled cortico s teroids were prescribed in only 16·7% (118 of 707) of patients.
Patient compliance was similar between the groups. The mean treatment duration was 341·2 days (SD 71·5) in the carbocisteine group and 342·6 days (SD 71·3) in the placebo group, with non-signi? cant di? erence between each other (Z=–0·599, p=0·549).
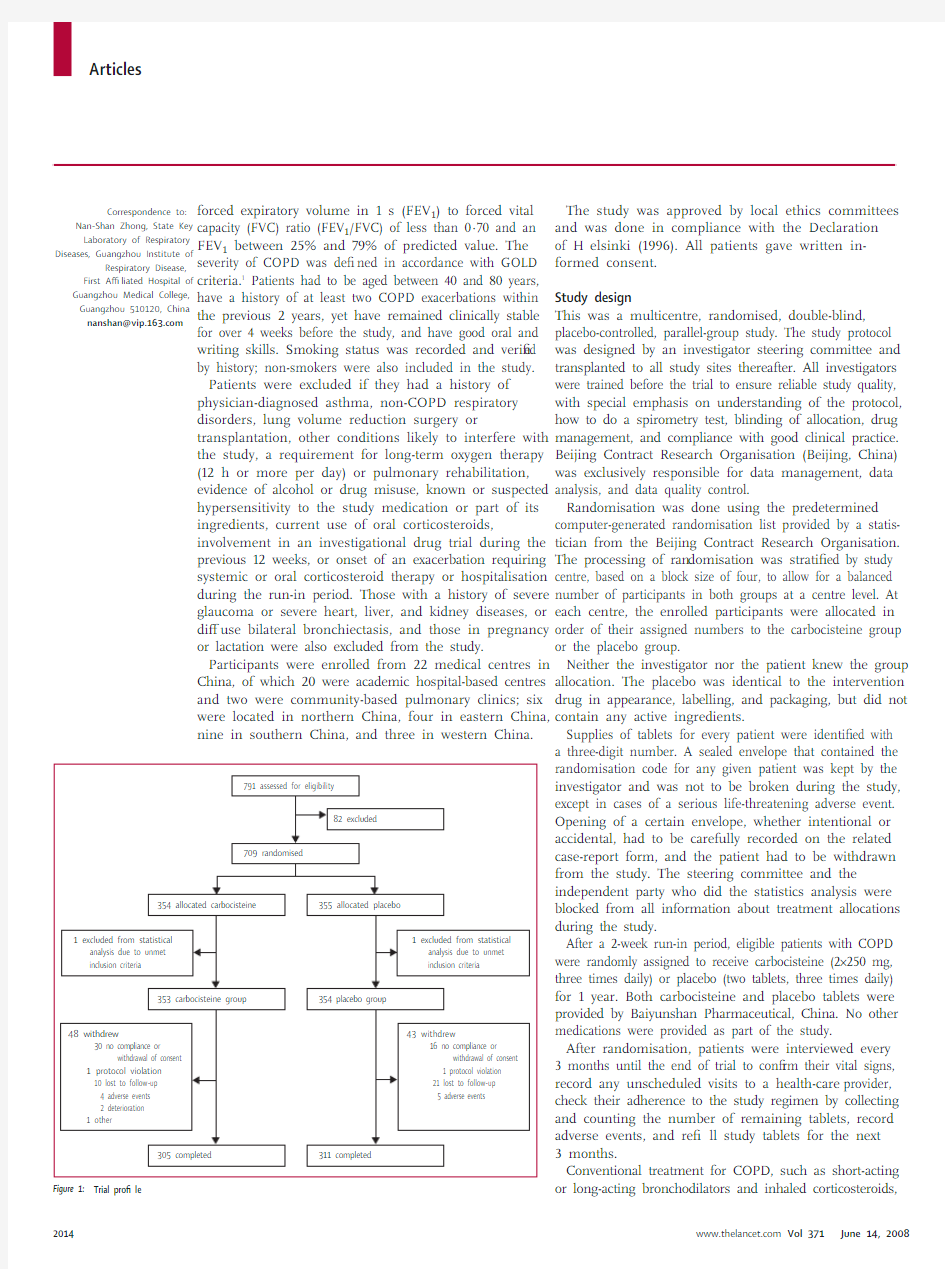
The 1-year cumulative number of exacerbations was 325 in the carbocisteine group and 439 in the placebo group, corresponding to 1·01 (SE 0·06) exacerbations per patient-year with carbocisteine treatment versus 1·35 (SE 0·06) with placebo (a 24·5% reduction). The risk ratio of exacerbation was 0·75 (95% CI 0·62–0·92, p=0·004). A Kaplan-Meier plot of the number of patients who were exacerbation-free at each time point through the study is shown in ? gure 2.
By analysing the covariance factors in our regression model, only two factors—COPD staging and concomitant therapy (theophylline and inhaled corticosteroids)—were found to signi? cantly a?ect COPD exacerbation. There were no signi?cant interactions between treatment and COPD stages (p=0·190 for treatment×COPD stage IV/ stage II; and p=0·159 for treatment×stage III/stage II). After adjusting for COPD stages, analysis of regression model excluding interaction showed favourable reduction
in the numbers of exacerbations in carbocisteine group compared with the placebo group (table 2). Similarly, no signi? cant interaction was noted between treatment and concomitant inhaled corticosteroids or inhaled corticosteroids naive. Fewer exacerbations were seen in the carbocisteine group than placebo group (risk ratio 0·75; 95% CI 0·63–0·91, p=0·004). The risk ratio adjusted by xanthines was 0·74 (95% CI 0·61–0·89, p=0·002). The advantage of carbocisteine over placebo in preventing an exacerbation was remarkable even after such adjustment. There were no signi?cant interactions between treatment and smoking status, and the risk ratio in exacerbation adjusted for smoking status was 0·74, 95% CI 0·64–0·86, p<0·0001.
Analysis of the length of treatment revealed that the prevention of exacerbation acted at month 6, when the risk ratio began to show statistical di? erences between the two groups (risk ratio 0·70 [95% CI 0·56–0·88], p=0·108 at 3 months; 0·79 [0·60–1·15], p=0·002 at 6 months; p=0·002 at 9 months 0·73 [0·60–0·89]).
Table 3 summarises the pretreatment and post-treatment quality of life in both groups. After a year of treatment, signi?cant changes from baseline in SGRQ total score (–4·06 units), symptom score (–11·34 units), and activity
score (–3·33 units) were detected in patients treated with carbocisteine but not placebo. The improvements in SGRQ total score and symptom score were regarded as clinically relevant. The SGRQ impact score did not show any change from baseline in either group. Postbronchodilator FEV? measurements were similar in each group before and after treatment, with no signi? cant di? erence between these two groups. as was di? erence in SpO? between the two treatments at each interview.
For the safety pro? les, 113 adverse events were reported during the study period (57 in the carbocisteine group and 56 in the placebo group). The most common adverse events reported (?ve events or more) were gastrointestinal and cardiac problems (14 cases and nine cases in the carbocisteine group vs?ve cases each in the placebo group). Table 4 summarises the adverse events. No deaths were reported in the study.
Discussion
The results of our study support previous ? ndings that long-term use of carbocisteine reduced the rate of exacerbations of COPD. The advantage of carbocisteine over placebo in prevention of an exacerbation was note-worthy, even after adjustment for COPD severity and concomitant therapy. We found no di? erence in exacerbation rate between the carbocisteine group and placebo group at early treatment (3 month), suggesting that longer use of carbocisteine was more e? ective for preventing exacerbations of COPD.
In addition to preventing COPD exacerbations, carbocisteine was shown to improve the patients’ quality of life. After 1 year of treatment with carbocisteine, signi? cant improvements over placebo were achieved in SGRQ (total and symptom scores). The activity score also seemed favourable with carbocisteine versus placebo.
The role of long-term mucolytic and antioxidation or anti-in? ammation therapy in COPD has attracted interest. Poole and Black15 did a systematic review in which 26 ran d omised, placebo-controlled studies recruiting 7335 par t icipants with COPD were included. Their data showed that treatment with mucolytics for at least 2 months sig n i?c antly reduced the number of exacerbations. The present study also showed preventive e?ects of carbo-cisteine on exacerbations when adjusted for concomitant use of inhaled corticosteroids. This ? nding di? ered from the BRONCUS study16 in which signi? cant reduction in exacerbation rate by N-acetylcysteine was shown only in patients without concomitant use of inhaled cortico-steroids. Several explanations might be reasonable for such di?erence. Firstly, inhaled corticosteroids were administered in only 16·7% of our study participants (table 1), compared with 70% of the BRONCUS16 partici-pants. Additionally, therapeutic inhaled cortico s teroids are generally prescribed in smaller doses to Chinese patients.22 As such, the e? ects of carbocisteine would be more readily identi? ed in our patients, with modest use of concomitant inhaled corticosteroids, than in the BRONCUS study. Secondly, carbocisteine showed a unique picture in terms of pharmacokinetics and drug actions (including probable inhibition of viral adherence to the airway11,23), and hence its di? erent e? cacy from N-acetylcysteine. Thirdly, the role of ethnicity in response to a treatment should be noted. The Chinese di?er from Europeans in dietary patterns, nutritional status, and lifestyle, which might speci? cally a?ect certain therapies. For instance, signi? cant di? erences in theophylline pharmaco k inetic constants were reported between American and Chinese children with asthma.24 Zhou and colleagues25 also showed that low-dose adminis-tration of theophylline signi?cantly reduced the time to ? rst exacer b ation and improved SGRQ scores in Chinese patients with COPD, which had not been reported in studies in white patients.
As the most important source of noxious, oxidant radical-rich gas, tobacco smoke represents a major risk factor for COPD. However, not all patients develop COPD because of smoking. In rural areas of developing countries like China, biomass fuel is also an important source of indoor air pollution.26 Unfortunately, non-smoking patients are excluded from many clinical studies related to COPD.27,28 Potential di?erences between smoking or non-smoking populations in the treatment of COPD were therefore not fully addressed. In a study by Zheng and co-workers,29 combination therapy with salmeterol and ? uticasone was seen to provide more bene? ts in COPD smokers than in non-smokers. We know of no study that has so far compared the e? ects of carbocisteine between smoking and non-smoking individuals. Our results showed signi?cantly fewer COPD exacerbations in carbocisteine-treated patients compared with placebo after adjustment for smoking status.
Prevention of acute exacerbations of COPD could lead to substantial savings in terms of healthcare use. Inhaled corticosteroids, long-acting β? agonists, and anti c holinergics would be preferable for better outcomes, yet mucolytics could be more a? ordable, and will continue to have a role in treatment of COPD, particularly for long-term use. For instance, the annualised cost per patient for carbocisteine therapy in China is 650 Yuan (US$90), but is about 4320 Yuan ($580) for combined treatment with inhaled
corticosteroids and long-acting β? agonists (more than six times higher). For many patients who cannot a? ord the combined t reatment f or c onventional t herapy, l ess-expensive mucolytics such as carbocisteine might be an important option, especially in low-income countries and regions. In our study, the direct cost of exacerbation was not analysed because of the incomplete data recorded from the study. Unlike in Europe and the USA, only a small percentage of people in China are covered by health insurance and reimbursement, and most have to pay for their medical services themselves. Since the uninsured group might not seek treatment because of ?nancial distress, we were unable to accurately calculate the medical costs.
There was no signi? cant improvement in lung function in the carbocisteine group compared with the placebo group after 1 year of treatment, which indicates that the reduced rates of of exacerbations and improvements in qual i ty of life were not due to bronchodilation e? ects. These ? nd i ngs were similar to those in other studies of mucolytics.15
Our study showed that the nature and incidence of adverse events were similar across the carbocisteine and placebo groups for 1 year, which were consistent with other studies using the same carbocisteine regimen. These results indicated that long term use of carbocisteine was well tolerated.
In conclusion, the 1-year management of carbocisteine was e? ective for COPD patients in terms of reductions in exacerbations and improvements in quality of life. There were no interactions between treatment and COPD severity, smoking status, and concomitant use of inhaled corticosteroids. Mucolytics, such as carbocisteine, should be recognised as a worthwhile treatment for the long-term management of COPD.
Contributors
N-SZ and JK chaired the steering committee, designed the study protocol, organised the study, and ensured the intrinsic quality of the study. All other authors enrolled participants, collected data, and took responsibility for
their own centres. All authors contributed equally to this paper.
Con? ict of interest statement
Jin-ping Zheng won a Best Poster Travel Grant for COPD research from European Respiratory Society annual conference 2007 due to this work. We declare that we have no other con? ict of interest.
Acknowledgments
We would like to thank Kyorin Pharmaceutical, Japan, for ? nancial
support for the study; Mei Jiang (Guangzhou Institute of Respiratory Disease) and Beijing Contract Research Organisation (Beijing, China) for the statistical analysis; and Guang-qiao Zeng (Guangzhou Institute of Respiratory Disease) for his help with the manuscript.
References
1 Global strategy for the diagnosis, management, and prevention of
chronic obstructive pulmonary disease. GOLD website.
https://www.doczj.com/doc/9718259282.html, (accessed June 23, 2007).
2 Braga PC, Allegra L, Rampoldi C, Ornaghi A, Beghi G. Long lasting
e? ects of theology and clearance of bronchial mucus after short-term
administration of high does of carbocisteine-lysine to patients with
chronic bronchitis. Respiration 1990; 57: 353–58.
3 Sakakura Y, Majima Y, Saida S, et al. Reversibility of mucociliary
clearance chronic sinusitis. Clin Otolaryngol 1985; 10: 79–83.
4 Boonyapiwat B, Forbes B, Steventon GB. Phenylalanine hydroxylase:
possible involvement in the S-oxidation of S-carboxymethyl-L-cysteine.
Anal Biochem 2004; 335: 91–97.5 Guizzardi F, Todighiero S, Binelli A, et al. S-CMC-Lys-dependent
stimulation of electrogenic glutathione secretion by human
respiratory epithelium. J Mol Med 2006; 84: 97–107.
6 Steventon GB, Mitchell SC. The sulphoxidation of
S-carboxymethyl-L-cysteine in COPD. Eur Respir J 2006; 27: 865–66.
7 Carpagnano GE, Resta O, Foschino-Barbaro MP, et al. Exhaled
Interleukine-6 and 8-isoprostane in chronic obstructive pulmonary
disease: e? ect of carbocysteine lysine salt monohydrate (SCMC-Lys)
Eur J Pharmacol 2004; 505: 169–75.
8 Brandolini L, Allegretti M, Berdini V, et al. Carbocysteine lysine salt
monohydrate (SCMC-LYS) is a selective scavenger of reactive oxygen intermediates (ROIs). Eur Cytoline Netw 2003; 14: 20–26.
9 Ishii Y, Kimura T, Morishima Y, et al. S-carboxymethylcysteine inhibits
neutrophil activation mediated by N-formyl-methyl-leucyl-phenylalanine.
Eur J Pharmacol 2002; 449: 183–89.
10 Allegra L, Cordaro CI, Grassi C. Prevention of acute exacerbations of
chronic obstructive bronchitis with carbocysteine lysine salt
monohydrate: a multicenter, double-blind, placebo-controlled trial.
Respiration 1996; 63: 174–80.
11 Yasuda H, Yamaya M, Sasaki T, et al. Carbocysteine reduces frequency
of common colds and exacerbations in patients with chronic
obstructive pulmonary disease. J Am Geriatr Soc 2006; 54: 378–80.
12 Tatsumi K, Fukuchi Y. Carbocisteine improves quality of life in
patients with chronic obstructive pulmonary disease. J Am Geriatr Soc 2007; 55: 1884–86.
13 Mitchell SC. Carbocysteine therapy in older people with chronic
obstructive pulmonary disease. J Am Geriatr Soc 2006; 54: 1792–93.
14 Poole PJ, Black PN. Oral mucolytic drugs for exacerbations of chronic
obstructive pulmonary disease: systematic review. BMJ 2001; 322: 1–6.
15 Poole PJ, Black PN. Mucolytic agents for chronic bronchitis or chronic
obstructive pulmonary disease. Cochrane Database Syst Rev 2006;
3: CD001287. DOI:10.1002/14651858.CD001287.pub2.
16 Decramer M, Rutten-van Molken M, Dekhuijzen PN, et al. E? ects of
N-acetylcysteine on outcomes in chronic obstructive pulmonary disease (Bronchitis Randomized on NAC Cost-Utility Study, BRONCUS):
a randomised placebo-controlled trial. Lancet 2005; 365: 1552–60.
17 Anthonisen NR, Manfreda J, Warren CPW, et al. Antibiotic therapy in
exacerbation of chronic obstructive pulmonary disease.
Ann Intern Med 1987; 106: 196–204.
18 Jones PW. Health status measurement in chronic obstructive
pulmonary disease. Thorax 2001; 56: 880–87.
19 American Thoracic Society. Standardization of spirometry-1994
update. Am J Respir Crit Care Med 1995; 152: 1107–36.
20 Quanjer PH. Standardized lung function testing. O? cial Statement of
the European Respiratory Society. Eur Respir J Suppl 1993; 16: 5–40.
21 Zheng JP, Zhong NS. Normative values for pulmonary function
testing in Chinese adults. Chin Med J 2002; 115: 50–54.
22 Chen P, Zhao HT, Sun L, et al. The e? cacy of half of the Global
Initiative for Asthma recommended dose of inhaled corticosteroid in the management of Chinese asthmatics. Chin J Tuberc Respir Dis 2005;
28: 458–63.
23 Yasuda H, Yamaya M, Sasaki T, et al. Carbocisteine inhibis rhinovirus
infection in human trcheal epithelial cells. Eur Respir J 2006; 28: 51–58.
24 Zhong NS. Management of asthma in developing counties. In:
Barnes PJ, Grunstein MM, Le? AR, Woodcock AJ, eds. Asthma.
Philadelphia: Lippincott-Raven Publishers, 1997: 1869–81.
25 Zhou Y, Wang X, Zeng X. Positive bene? ts of theophylline in a
randomized, double-blind, parallel-group, placebo-controlled study of low-dose, slow-release theophylline in the treatment of COPD for
1 year. Respirology 2006; 11: 603–10.
26 Liu S, Zhou Y, Wang X, et al. Biomass fuels are the probable risk factor
for chronic obstructive pulmonary disease in rural South China.
Thorax 2007; 2000: 1–10.
27 Casaburi R, Mahler DA, Jones PW, et al. A long-term evaluation of
once-daily inhaled tiotropium in chronic obstructive pulmonary
disease. Eur Respir J 2002; 19: 217–24.
28 Calverley MA, Anderson JA, Celli B, Ferguson GT, Jenkins C, et al.
Salmeterol and ? uticasone propionate and survival in chronic
obstructive pulmonary disease. N Engl J Med 2007; 356: 775–89.
29 Zheng J, Y ang L, Wu YM, et al. The e? cacy and safety of combination
salmeterol (50 μg)/? uticasone propionate (500 μg) inhalation twice daily via accuhalar in Chinese patients with COPD. Chest 2007; 132: 1756–63.
一、DRGs简介
图 1 各国 DRGs 研究进展 图 1 中黄色的是已经开始运作 DRGs 的,已趋成熟;蓝色的是已经在做,处于成长过程中的;红色的是开始在做;绿色的是准备做的。从图中不难看出,进行 DRGs 研究的国家是很多的。 (三) DRGs 分组框架 DRGs 是由住院病例分为 25 个 MBC ( 主要诊断分类 ) ,再在 25 个 MBC 的基础上进行 DRGs 的分类。它的分组指标包括疾病的首要诊断、手术种类、并发症和合并症、出院状况(是否死亡)、年龄、昏迷时间和新生儿的体重,根据这些指标把 MBC 分为了若干个 DRGs 组,这些组在各个国家分组的数量不一样,它可以作为质量控制、费用补偿,易于管理。它依据资源消耗相近、临床特征相近进行分组。具体可见图 2 所示。 图 2 DRGs 分组框架 根据发病器官、系统和病因结构先划分成 25 个诊断分类组,详见表 1 。 表 1 25 个诊断分类组
图 3 DRGs 的形成 图 3 是在 25 个诊断相关分类以后分成的 DRGs ,它有手术室手术及操作和非手术室手术和操作,以及手术的分级、肿瘤症状,最后要按照年龄、伴随症和合并症进行分组。
DRGs的核心思想是将具有某一方面相同特征的病例归为一组,以方便管理。那么DRGs有哪些分组原则呢?
4. MCC (主要并发症 / 合并症) 对患者医疗资源消耗起到很大影响的并发症和合并症。 表 2 DRGs 分组情况 表 2 是 DRGs 的分组情况,美国 876 个,德国 986 个,法国 700 个,英国 583 个。 (六)应用效果 国外 20 余年的应用经验表明与现有的其他付费方式相比 DRGs 是一种相对合理的医疗费用管理方法和质量评价方法,既兼顾了政府、医院、患者等多方利益,又达到了医疗质量与费用的合理平衡。它可以兼顾各方利益达到质量与费用的合理平衡。 1. 效果一 能够控制医疗费用的增长。 DRGs 不再根据医院的投入,而是按照医院收治的病例及其诊断制定相应的补偿标准,使政府对医疗费用的控制更为直接有效。另一方面补偿标准的制定对医院起到了很好的约束作用,可以激励医院降低医疗成本从而节约卫生资源。 美国实施 DRGs 老年医疗保险住院总费用的增长速度从 1983 年的 18.5% ,降到 1990 年的 5.7%。手术费的增长率从 1984 年的 14.5% 降到 1992 年的 6.6% ,平均住院天数从 1980 年的 10.4 天降到 1990 年的 8.7 天, 1995 年已缩短到 6.7 天。 2. 效果二 提高医院的管理水平。 DRGs 定额预付制的实施给医院管理带来了一场深刻的变革,促进了医疗质量、经济、信息等方面管理学科的发展,涌现了临床路径、战略成本管理、数字化医院等先进管理手段,并且为医院进行同行间的评价和内部的管理提供了有效的手段。 3. 效果三 增加患者满意度。 DRGs 对医疗费用的控制,减轻了患者的就医负担,医院服务效率与服务质量的提
COPD患者的饮食指导 一.饮食指导的意义 慢性阻塞性肺病与高血压、糖尿病、以及恶性肿瘤等诸多慢性疾病一样,营养干预已成为疾病治疗环节中不可或缺的一部分。 1.改善能量负平衡 慢性阻塞性肺病患者因疾病所致的长期能量代谢失衡,普遍存在体质量下降及肌肉消耗。体质量下降,尤其是祛脂体质或称作瘦体群的下降,归根结底是能量的负平衡所致(韩锋锋,夏韶民,罗勇,2012)。瘦体群的下降直接影响患者的肌肉功能,包括呼吸肌的力量和运动耐力。而引起能量失衡的本质原因是热能摄入与消耗之间的不平衡(Schols AM, 2000)。过去的研究多集中于气道阻力增加引起的呼吸肌负荷和做功增加,而近期的一些报道认为由于慢性阻塞性肺病缓解期患者多存在骨骼肌形态的改变和代谢的异常,致使日常活动中无氧代谢的发生频率增加。而要限制活动量及降低静息能量消耗相对不易,故唯有通过营养干预,增加营养摄入来保证能量代谢平衡。 2.提高免疫功能, 营养失衡导致患者抗病能力的下降,免疫功能改变的结果易使患者的呼吸系统受到病原微生物的侵袭而发生肺炎,并使感染病程迁延,难以痊愈。免疫功能的下降影响了肺的防御机制。营养不良,呼吸道感染,呼吸衰竭等往往互为因果并形成恶性循环,有效的营养干预则有利于打破这种循环,改善患者的预后,降低住院率,提高生活质量(罗勇,徐卫国,杨玲,2003)。 3.平衡心理状态,利于康复 相比急性期患者,缓解期慢性阻塞性肺病患者精神紧张度高,焦虑、抑郁等负性情绪增多,厌食及恐惧进食的情绪障碍的发生率普遍高于一般人群。这与患者进食含碳水化合物较多的高热量食物期间所发生的缺氧和呼吸困难等表现有一定的关系,后者导致了患者就餐的恐惧心理(张鹏宇,陈文华,金先桥,2001)。因此,通过及时调整饮食结构和有效的营养干预有利于增进食欲,满足营养吸收和促进慢性阻塞性肺病的康复治疗。
肺功能检查指南(第二部分)––肺量计检查 肺量计检查是肺功能检查中最常用的方法,采用肺量计测量呼吸容积和流量,两者可通过呼吸时间的微分或积分相互转换。肺量计分为两种:容积型肺量计通过密闭系统直接测量呼吸气体的容积,直观易懂,但仪器体积大,易于交叉感染,且呼吸阻力高,测定参数少;流量型肺量计则测量气体流量,呼吸阻力低,操作简单,体积小,清洁和维护方便,已逐渐取代容量型肺量计。
(一)肺量计技术标准 见。
1.测试环境的校准: 由于气体容积受环境温度、压力、湿度等因素的影响而变化,故肺量计检查时需将测试环境校准为生理条件,即正常体温(37 ℃)、标准大气压(760 mmHg,1 mmHg=kPa)及饱和水蒸气状态(BTPS)。若仪器已内置温度计和压力计,需确认其可靠性。2.肺量计校准: 是对实际测量值与理论值之间的误差进行校准。用于校准肺量计的校准仪,常称为定标筒,须精确到总量程的±%。校准时应确保肺量计与定标筒的连接无漏气、无阻塞。若校准超出范围应及时查找原因,必要时请专业人员检修。关键措施见。
容量计的质量控制:①每天检查是否漏气:封闭容量计的出口,给予≥ cmH2O(1 cmH2O=kPa)的持续正压,若1 min后容积减少>30 ml则存在漏气。②每天用定标筒检查容积精确度,误差应≤±3%。③每个季度检查容积线性,方法有2种,一种以1 L 容积递增,连续注入肺量计,如0~1、1~2、2~3、……、7~8 L;另一种初始容积以1 L递增,以3 L容积分次注入肺量计,如0~3、1~4、2~5、3~6、4~7和5~8 L。比较相应的累积容积与实测容积的差异,若误差均符合容积精确性要求,则其容积线性可接受。 流量计的质量控制:①校准:每次启动流量计均需经定标筒校准,误差应≤±3%,校准后可获得一个校准系数。流量计检查的结果是以传感器计量的数值乘以校准系数所得的。②校准验证:每天都应用定标筒在~L/s范围内以不同流量进行校准验证,至少操作3次,误差应≤±3%。③线性验证:每周还需以低、中、高3种不同的流量~、~和~L/s)进行流量线性验证,每种流量至少操作3次,每种流量对应的容积误差均应≤±3%。 标准呼吸模拟器校准:某些肺功能实验室和厂家还会采用微机控制的气泵,称为标准呼吸模拟器,产生多种标准波形(如ATS 的24个FVC波形和26个PEF波形)的气流,气流通过肺量计,对比肺量计的测量值与模拟器的标准值之间的差异,即为肺量计的误差。我国的肺功能仪校准规范推荐定期用标准呼吸模拟器对肺功能仪进行质量检测,并可获得权威机构签发的证书。 1.检查前应详细询问受试者的病史,判断肺量计检查的适应证,排除禁忌证,并了解受试者的用药情况。 2.准确测量身高和体重:详见肺功能指南第一部分。 3.体位:取坐位,测试时应挺胸坐直不靠椅背,双脚着地不翘腿,头保持自然水平或稍微上仰,勿低头弯腰俯身。正确的坐姿有助于受试者获得最大的呼吸量。若采用站位或卧位,应在报告中说明。 4.检查动作的练习:检查前应先向受试者介绍及演示检查动作,并指导受试者进行练习。也可播放演示录像,有助于受试者更快地掌握动作要领。 肺量计检查主要包括慢肺活量、用力肺活量及最大自主通气量3部分内容,其中慢肺活量检查将在肺容量检查部分详细介绍,本章主要介绍用力肺活量和最大自主通气量检查。 (一)FVC FVC是指最大吸气至肺总量(TLC)位后,做最大努力、最快速度的呼气,直至残气量(RV)位所呼出的气量。用力呼气时单位时间内所呼出的气量又称为时间肺活量。 1.检查程序分为4个阶段()。 图1 FVC检查的程序 2.测试曲线和指标:容积-时间曲线(V-T曲线)是呼气时间与容积变化的关系曲线()。流量-容积曲线(F-V曲线)是呼吸气体流量随肺容积变化的关系曲线()。曲线形状和指标大小取决于呼气力量、胸肺弹性、肺容积及气道阻力对呼气流量的综合影响。在F-V曲线的起始部分,呼气肌的长度最长,收缩力最大,流量也最大,图形上表现为流量迅速增至峰值,其值与受试者的努力程度有关,故称为用力依赖部分。在曲线的终末部分,呼吸肌长度显着缩短,收缩力显着降低,呼气流量与用力无关,流量的大小与小气道的通畅程度密切相关,故称为非用力依赖部分。T-V曲线和F-V曲线上的常用指标:(1)FVC:指完全吸气至TLC 位后以最大的努力、最快的速度做呼气,直至残气量位的全部肺容积。在正常情况下,VC与FVC相等。但在气流阻塞的情况下,用力呼气可致气道陷闭,VC可略大于FVC。(2)t秒用力呼气容积(FEVt):指完全吸气至TLC位后在t秒以内的快速用力呼气量。按呼气时间,可分为、、FEV1、FEV3和FEV6等指标,分别表示完全吸气后在、、1、3、6 s的用力呼气量。(3)一秒率(FEV1/FVC ):是FEV1与FVC的比值,常用百分数(%)表示,是判断气流阻塞的主要指标。气流阻塞时,给予充足的呼气时间,受试者可充分呼
肺功能检查 肺功能检查肺功能检查是呼吸系统疾病的必要检查之一,对于早期检出肺、气道病变,评估疾病的病情严重程度及预后,评定药物或其它治疗方法的疗效,鉴别呼吸困难的原因,诊断病变部位、评估肺功能对手术的耐受力或劳动强度耐受力及对危重病人的监护等方面有重要的指导意义。项目肺功能检查包括通气功能、换气功能、呼吸调节功能及肺循环功能等,检查项目及测定指标众多.过去的肺功能仪主要以机械和化学方法检测为主,测定烦琐,费时费力,而且检测误差较大,限制了其在临床上的广泛应用,医务工作者对其知识也了解有限。近年来,随着科学技术的发展,新的检测技术的出现,尤其是电子计算机的应用,使肺功能检测技术得到了很大的发展,其在临床上的重要性也愈益受到重视。目的肺功能检查主要用于以下目的:1、早期检出肺、呼吸道病变。2、鉴别呼吸困难的原因,判断气道阻塞的部位。3、评估肺部疾病的病情严重程度。 4、评估外科手术耐受力及术后发生并发症的可能性。 5、健康体检、劳动强度和耐受力的评估; 6、危重病人的监护等。特点1、肺功能检查是一种物理检查方法,对身体无任何损伤,无痛苦和不适。2、肺功能检查具有敏感度高、重复检测方便和病人易于接受等优点。3、
与X线胸片、CT等检查相比,肺功能检查更侧重于了解肺部的功能性变化,呼吸系统疾病的重要检查手段。重要性 1、诊断患者呼吸功能状况,确诊肺功能损伤的性质与程度。 2、要确诊COPD必须进行肺功能检查。 3、肺功能检查有助于临床医生明确COPD的严重程度,并依据疾病严重程度制定相应的治疗方案。对象1、反复上呼吸道感染者——观察肺功能是否有损伤2、有吸烟史及长期咳嗽——看小气道功能是否改变3、季节性咳喘发作——看是否患有哮喘 4、慢性支气管炎定期复查——监控病程发展 5、胸片异常——判断肺功能损害程度 6、麻醉、外科手术的危险评估,以及术后恢复的预测哮喘病人典型哮喘发作时的肺功能检查首先表现为阻塞性病变,但并非所有阻塞性病变都是哮喘。进一步确诊可进行气道扩张试验来确诊哮喘。对于非典型哮喘或哮喘缓解期或气道扩张试验阴性者,可酌情进行气道激发试验来确诊哮喘。儿童1、反复咳嗽或伴有喘息;2、咳嗽持续2~3周以上,抗生素治疗无效;3、反复“感冒”发展到下呼吸道,持续10天以上;4、哮喘患儿病情评估;5、急性发作的呛咳、声音嘶哑、呼吸困难;6、婴幼儿急性支气管炎、肺炎与哮喘的早期鉴别; 7、其他呼吸系统疾病。表现呼吸系统疾病在肺功能检查中的表现主要有:1、阻塞性病变:指由于各种因素造成呼吸道狭窄而出现气流受阻的
呼吸系统疾病的营养支持 在所有呼吸系统疾病的治疗中,营养治疗是重要的治疗部分。营养不良可减弱呼吸肌强 度,改变通气能力及损害免疫功能,引起肺功能的下降。营养状况的恢复能改善受损肺功能、 可以提高疗效,当经口自然进食不足时,对有消化功能的病人来说,肠内营养比静脉更为常 用。COPD病人的营养治疗的一般原则同样适用于其他肺部疾病,现以COPD为例,讨论呼吸系 统疾病的营养支持问题。 C O P D患者发生营养不良的机制: ?机体能量消耗增加; ?胃肠道消化吸收功能障碍; ?机体分解代谢的增加; ?摄入减少; ?其他因素:如适应调节机制、抑郁、吸烟、缺乏营养知识。 一、营养不良的不利影响 在COPD病人中,有25%的门诊患者存在营养不良,有50%的住院病人存在明显的营养 不良,有急性呼吸衰竭的COPD危重病人存在营养不良的比例高达60%。无论自主呼吸或机 械通气的呼吸疾病病人,营养不良均损害呼吸肌功能、通气动力、肺防卫机制,最终削弱肺 功能。营养不良引起呼吸肌,尤其是膈肌强度下降。降低膈肌强度的其他因素包括矿物质和 电解质缺乏,如低磷、低镁或低钙血症。伴有营养不良的呼吸系统疾病病人,在自主呼吸时, 其呼吸强度和通气动力减弱,会引起咳嗽能力下降和肺不张,最后引起肺炎;在机械通气时, 可致撤机延迟。COPD患者的预后受到许多因素的影响,营养不良是其中之一,当血清白蛋 白低于2.6g/dl时,经常发生腹泻,加重营养不良,死亡率明显增高。 成人营养不良的评估见表1。 表1 成人营养不良程度估计指标 监测指标标准值正常轻度营养不良中度营养不良重度营养不良标准体重% 100 >90 80~90 60~80 <60 血清白蛋白(g/L)45 35~45 30~35 25~30 <25 血清转铁蛋白(g/L) 2.5~3.0 >2.0 1.5~2.0 1.0~1.5 <1.0 前白蛋白 (mg/L) 150~300 >150 100~150 50~100 <50 氮平衡(g/d) ±1 ±1 -5~-10 -10~-15 <-15 淋巴细胞总数(×109/L) >1.7 >1.7 1.2~1.7 0.8~1.2 <0.8 营养不良的类型 ?蛋白质-能量营养不良(消瘦型):总能量不足,内脏蛋白产生维持正常,体重下降。肿瘤病人。 ?蛋白质营养不良(恶性营养不良):分解代谢应激及营养素摄取量不足,内脏蛋白消耗,ALB、前白蛋白降低、免疫功能受损,人体测量值正常,严重应激。
肺功能检查判读(七大步骤 ) 肺功能检查判读 第 1. 首先需先区分正常与不正常数值 一般而言,以统计的 [平均值 +/- 1.65标准差] 作为分界点,正常值订为 TLC>80%, FVC>80%, FEV1>75%, FEV1 /FVC (%)>75%, Flow rate>60%。 RV/TLC<=35%(若>40%肺内充气过度,减少限制性通气障碍) 第 2. 判别为阻塞型式为限制型 第 3. 区分其严重度 第 4. 对照临床的相关性 步骤 (七大步骤 ) 1. 检视流量容积图 (FVC curve) 先检视 FVC 是否变小,再检视 F-V图,病人是否配合,曲线斜率,是否有呼吸道 阻塞。 2. FVC 每个人都有一唯一最大的呼气FV图形,重复性且高灵敏度。 FVC 的大小决定于肺的弹性,呼吸道的口径大小及其阻抗;且随着胸廓大小,性 别及年龄而变。 FVC 若是正常,则阻塞型式通气型障碍都有可能。 3. FEV1 重复性最高,最易获得,也是最有用得检查项目,属于 FVC 的一部份,与胸廓大 小无关 正常%FEV1介于75-85%之间 最快查出呼吸道阻塞的方法。 FEV1若是正常,任何有意义的阻塞型或局限型的通气障碍都可排除。反之,则两 者都有可能。 4. %FEV1 (FEV1 /FVC) 以绝对数值表示,若数值降低,表阻塞型通气障碍,若是正常或增加,可能为纯粹 的局限型通气障碍。 5. FEF25-75 或 Vmax50 Expiratory Flow value 通常与 FEV1 的变化相同; FEF25-75比FEV1更早能侦测出呼吸道阻塞病变(Small airway disease)。 6. 检查静态肺容积 假使肺容积降低,应为局限型通气障碍;肺容积增加,局限型通气障碍多为不可
肺功能检查指南概述及一般要求 一、概述 肺功能检查是运用呼吸生理知识和现代检查技术探索人体呼吸系统功能状态的检查。临床上常用的检查包括肺容积检查、肺量计检查、支气管激发试验、支气管舒张试验、肺弥散功能检查、气道阻力检查及运动心肺功能检查等。肺功能检查是临床上对胸肺疾病诊断、严重程度、治疗效果和预后评估的重要检查手段,目前已广泛应用于呼吸内科、外科、麻醉科、儿科、流行病学、潜水及航天医学等领域。 二、肺功能检查在我国的发展历程 在我国,呼吸功能检查的研究与临床应用已有70多年历史。1939年,蔡翘等首先报告大学生及中学生肺活量的检测。195 1年,吴锦秀等检测了6 414名健康学生的肺活量。1956年,吴绍青等发表了通气功能检查方法以及中国人通气功能的数据。此后,吴绍青、张仲扬、汪士、高启文、何国钧、薛汉麟、王鸣歧、陈民孝、朱蕾、郑劲平等许多医学工作者对肺功能的研究和临床应用做了大量的工作。 1961年,吴绍青等编著了我国第一部肺功能检查的专著——《肺功能测验在临床上的应用》,对我国肺功能的研究和临床应用起到了很好的促进作用。 1992年穆魁津等编写了《全国肺功能正常值汇编》和《肺功能检测原理与临床应用》,2004年朱蕾等编写了《临床肺功能》,2007年郑劲平和陈荣昌编写了《肺功能学——基础与临床》;2009年郑劲平和高怡编写了《肺功能检查实用指南》,2010年赵立军和李强编写了《实用肺功能临床解读手册》,同年贺正一等编写了《简明临床肺功能检查与应用》,2012年周怡编写了《肺功能检查临床病例分析》等,这些肺功能专著的陆续出版进一步推动了我国肺功能检查的发展。 近30多年来,国内召开了多次肺功能学术专题会议。1979年卫生部在杭州举办了“第一届全国肺功能学术讲座”,1986年《中华结核和呼吸杂志》与《解放军医学杂志》在杭州举办了“血气分析与肺功能座谈会”,1992年中华医学会呼吸病学分会肺功能学组和上海分会肺科学会在上海主办了“第三届全国肺功能学术交流会议”,1994年在天津召开了“第四届全国肺功能学术会议”,1997年中华医学会在西安召开了“第五届全国肺功能与呼吸监护学术会议”,2004年《中华结核和呼吸杂志》编委会在内蒙古包头市召开了“第六届全国肺功能(临床呼吸生理)学术研讨会”,2013年中华医学会呼吸病学分会肺功能专业组在广州召开了“全国肺功能学术会议",同时成立了中国肺功能联盟。 这些肺功能学术会议的召开为肺功能检查提供了很好的学术交流平台,展示了我国呼吸生理及肺功能领域的研究进展以及取得的成果。随着计算机技术的发展及我国医疗科研水平的提高,呼吸生理的研究取得了巨大进展,肺功能检查仪器不断更新,检测技术不断改进,检查项目不断增加,应用范围日趋扩大。
临床路径模式在医院病案管理中的应用 临床路径在病案管理中不断发展与壮大得到越来越多的关注,与发达国家医疗卫生机构相比较,我国临床路径在管理模式中的运用还不是很成熟,但随着交流的频繁与社会选择的需要与必要性,临床路径在我国医疗机构病案管理的道路会越来越宽敞。文章先描述临床路径的要素,然后分析我国病案管理中临床路径中存在的问题有:意识淡薄、临床路径病种资料准确性欠缺,针对存在的问题提出相应的对策。 标签:临床路径;病案管理;模式 临床路径是针对患有某一固有疾病的一组病人,临床医务工作的人员在时限要求范围内通过流程顺序对患者的疾病做出最适宜的医疗照顾方案以及医疗服务程序。临床路径做为质量效益型医疗管理模式中非常重要的一种类型,其目的是为了改进质量管理,有效控制医疗资源的过度消费,帮助患者尽早远离病痛,将医疗资源的消耗降至最低[1]。临床路径通过规范临床医疗治疗与护理的行为,提高医疗效率,让患者平均住院天数有效减少,减轻患者病痛,节约医疗卫生资源,适应了社会的需要[2]。卫生部已经颁布了112种疾病的临床路径,在2009年又展开了100种疾病的临床路径的制订,作为医院病案管理模式中的一项重要内容,临床路径迎来了机遇,同时也面对着许多挑战。 1 临床路径的构成要素 科学的程序化要求中,临床路径的构成要素有八个,分别是:目的与目标、范围与项目、岗位职责、临床路径的每日流程、临床路径的实施控制、变异分析、医疗信息归集。病案管理模式旨在为某个病种的患者提供高效、优质、费用低的医疗卫生服务,通过制订制、实施临床路径方案,满足平均住院人数、平均住院费用、医疗质量特性综合满足率的需求与预定的目标。临床路径的范围涉及从入院到出院的整个过程,一些疾病需要对出院病人的随访或者门诊预约服务也包括在内。临床路径的项目有病例评估、医嘱类诊疗护理项目、医嘱类医疗服务项目、医患沟通、健康教育、变异监测记录。 临床路径的岗位职是让医护人员尽职尽责的进行医疗行为,是管理者对被管理者进行管理的一种工作模式,严格要求医护人员掌握的职业操守的一种规范,包括主治医师及医师职责、主任医生职责、个案答理者职责、护士职责、住院医师职责等。临床路径要求每天一个流程表单,内容不仅包括医嘱类诊疗护理项目,也包括非医嘱类诊疗护理项目,以及每个项目的服务规范、技术标准、操作规程、执行要求、执行结果等记录。 临床路径实施控制是针对每一个病种或者病例的表单实施过程的控制,包括三级医生查房逐级检控、会诊过程、病案讨论、手术诊疗过程、护理过程、临床药学控制控制等。变异分析的内容包括:患者个体差异、患者病理改变、患者年龄与体质变异、病情变异、医疗决策变异、院内感染变异、医疗行为与规范不一
使用功率踏车进行运动试验 测试前的准备 完成流量传感器定标Flow Sensor Calibration[1],[F1],[F3]存储定标结果。 进入新的测试New Study [2],输入病人信息资料。[F3]存储。 选择肺功能测试Pulmonary Function[5],然后[1]Flow Volume Loop流速容量环。这是为了采集静态基础数据,以便与运动流速容量环作比较,并且在没有 MVV 实测数据的情况下计算VE 的预计最大值。必须完成两次具有重复性的测试 (FVC,FEV1 重复性在5%以内 )。如果FEV1实/预百分比低于80%,需要记录下来。 Exit[鼠标或ALT-X]退出,然后进入MVV [2]测定最大自主通气量。这项结果将用作VE 的预计最大值。按[F1]开始测定。指导病人开始快速而用力的深呼吸后,再次按[F1]开始采集数据。 12秒后测试自动结束。重复测定,直到两次MVV 结果在10% 以内(“f” 呼吸频率正常人应在90 – 130,阻塞病人应在60 – 90次/分)。Exit[鼠标或ALT-X]退出,返回主菜单。 运动测试 运动及代谢测试Exercise/Metabolic Test [4]。 在屏幕左下选择[F2] Reference Values运动预计值。如果使用功率车,需要计算斜坡方案(Ramp)的功率,可用VO2预计最大值先减去0.5 L/min,再乘以10,即可得到斜坡方案(Ramp)每分钟增加的功率。 VO2 Max predicted 2.000 - .5 1.5 x 10 Protocol 15 watt ramp 功率车的功率增量为5 watts。如果通过以上计算,得到的结果为17,可以选择15或20 watt的方案。如果病人FEV1实/预百分比低于80%,要用病人的FEV1实/预百分比去乘上面得到的结果。如果病人FEV1实/预百分比为50%,则用50%乘以上面得到的结果。病人肺部的状态会影响到运动方案的选择。[Esc]返回上一级菜单。 选择合适的运动方案,再按下[F10]。确认以下选项: Measurement Mode Breath by Breath Exercise(每次呼吸法运动测试) (测试方式) Bike根据病人情况,参考上述方法选择斜坡方案(Ramp protocol) (功率踏车) ECG SMC 3 Lead或none (运动心电) Left Graph HR vs. VO2 (左显示图形)
健康宣教与疾病认识 COPD是一种具有气流受限特征的可以预防和治疗的疾病,气流受限不完全可逆、呈进行性发展,与肺部对香烟烟雾等有害气体或有害颗粒的异常炎症反应有关。COPD主要累及肺脏,但也可引起全身(或称肺外)的不良效应。 二、避免环境污染 避免各种致病因素,尤其是吸烟、环境污染、感冒等,避免粉尘、刺激性气体的吸入;注意保暖,改变不良的生活方式,有条件者改善生活环境。 三、药物治疗 1.支气管舒张剂:与口服药物相比,吸入剂不良反应小,因此多首选吸入治疗。2.糖皮质激素:这一治疗可减少急性加重频率,改善生活质量。联合吸入糖皮质激素和β2受体激动剂,比各自单用效果好。对COPD患者不推荐长期口服糖皮质激素治疗。 3.其他药物:(1)祛痰药(黏液溶解剂) (2)抗氧化剂(3)免疫调节剂(4)疫苗(5)中药治疗。 四、长期家庭氧疗 长期家庭氧疗对于缺氧的人非常重要,缺氧就需要补充氧气,什么时间段缺氧就要什么时间段补充氧气。血氧饱和度低于90%必须长期家庭氧疗,低于91-95%最好长期家庭氧疗,长期家庭氧疗一般是经鼻导管吸入氧气,流量1.0~2.0 L/min(遵医嘱),吸氧持续时间段覆盖缺氧时间段,睡眠期间一定要吸氧。长期家庭氧疗要使用氧疗用的氧气机,而不是普通氧气机。 五、呼吸机治疗 当有CO2潴留二氧化碳分压高或需要呼吸支持改善呼吸窘迫降低心脏负荷的情况,或者有睡眠呼吸暂停综合征(打鼾症),可以使用双水平带后备频率的无创呼吸机治疗,降低二氧化碳分压,如果仅合并有睡眠呼吸暂停综合征(打鼾症),单纯吸氧是不能改善睡眠时的缺氧问题,这种情况可以使用单水平呼吸机,解决憋气缺氧,从而控制和稳定病情。 七、康复治疗 康复治疗可以使进行性气流受限、严重呼吸困难而很少活动的患者改善活动能力、提高生活质量,是COPD患者一项重要的治疗措施。它包括呼吸生理治疗,肌肉训练,营养支持、精神治疗与教育等多方面措施。在呼吸生理治疗方面包括帮助患者咳嗽,用力呼气以促进分泌物清除;使患者放松,进行缩唇呼吸以及避免快速浅表的呼吸以帮助克服急性呼吸困难等措施。在肌肉训练方面有全身性运动与呼吸肌锻炼,前者包括步行、登楼梯、踏车等,后者有腹式呼吸锻炼等。在营养支持方面,应要求达到理想的体重;同时避免过高碳水化合物饮食和过高热卡摄人,以免产生过多二氧化碳。 八、定期医院检查
临床路径与病案信息管理相互作用的研究进展 摘要】临床路径作为一种新的医护模式,具有与病案信息管理相互作用的关系。本文主要将主要介绍病案信息管理对临床路径实施的作用与临床路径对病案信息 管理的相关影响。采用完善的电子病案及信息系统,提高病案信息管理人员的业 务水平、服务意识,是促进临床路径有效实施及推广的有力措施。 【关键词】临床路径;病案信息;病案管理;电子病案 【中图分类号】R197.32 【文献标识码】A 【文章编号】1007-8231(2016)10-0243-02 临床路径是在能确保医护质量的基础上,减少医护工作的成本,减少病人的 医疗费用。随着我国医疗制度改革的不断进行,临床路径开始越加受到社会各界 的重视。而随着临床路径工作模式的推广,病案信息管理定会的面临更高要求。 故是有需要讨论病案信息管理与临床路径间的相互作用。 1.病案信息管理对临床路径实施的作用 1.1 在临床路径实施前的作用 病案信息管理者需要进行临床路径病种的选择与表格设计等工作。病案管理 人员需要据对应的《疾病和有关健康问题的国际统计分类》第10次修订本(ICD-10)编码分析近年病例数,从高费用、高容量、变异少病源充足和治疗效果等特点中探寻可控性,最后将总的资料上交给有关科室选择实施临床路径的病种。因病 案统计人员有较多为丰富的统计分析工作的经验,能够利用简单的表格能有效提 取数据。故病案统计人员需要收集并筛选临床路径患者的相关信息,同临床科室 为开展临床路径的病种设计科学的表格,以便分析临床路径的相关数据。临床路 径是一种医院新的管理模式,综合了各方面的知识,所以有必要在开展临床路径 前相关培训。病案室则负责培训医护人员,让相关医护人员掌握符合我国纳入标 准的112种疾病的ICD-10编码与手术编码。 1.2 在临床路径实施中的作用 实施临床路径便会有相应资料的产生,而这些资料便需要病案信息管理人员 控制和保管。且在临床路径的实施中,病案科要负责收集与审核临床路径患者的 各种信息。临床路径主要由临床路径标准住院流程及临床路径表组成,这两者的 内容大多都同病案的书写有着紧密的联系;病案是医疗行为的重要载体,以患者 为中心的任何医疗行为都要体现在病案中。故能够通过病案监督临床路径是否正 确实施,是否按照住院流程标准执行。患者出院后,病案信息管理人员需要收集 与分析临床路径的各种数据,以得出床路径进展情况,给临床决策与医院决策提 供重要依据。 2.临床路径对病案信息管理的影响 2.1 影响医院病案质量 马国胜在二零零三年研究了两千八百八十六份同期病案的终末质量,其发现 在实施临床路径管理模式之后,甲级病案率较普通病案高,而乙、丙级病案率则 较普通病案低;同时在临床路径管理模式下,出院患者病案在三天内归档的率与 病案的完整率都比对照组高。其也就证明了临床路径管理模式可以明显提升病案 管理的水平。医院在管理病案期间可以依据临床路径的工作内容等制定统一临床 路径管理治疗考核标准,从而加强对护理病案质量的管理的监控,以此提高医护 人员的水平,提高病案质量,避免医患纠纷。 2.2 影响病案标准
病案信息管理和临床路径相互作用的研究 发表时间:2017-04-18T15:36:49.490Z 来源:《医师在线》2017年2月上第3期作者:向波 [导读] 临床路径的实质,是一种具有实践性、顺序性的医护计划,有医生、忽视等医护人员按照既定的路线与方法进行临床操作。 皖南医学院第二附属医院241000 摘要:目的:主要研究病案信息管理与临床路径相互作用的相关问题。方法:我院于2015年1月将病案信息管理与临床路径结合方法应用到临床工作中,收集病案信息管理和临床路径结合后我院临床工作质量,并与实施前进行比较。结果:在实施病案信息管理与临床路径相互结合的管理模式后,我院临床工作质量有了明显提高,比较实施前后我院出现医疗信息差错情况,实施后明显优于实施前,组间数据差异相比具有统计学意义(P<0.05);比较实施前后相关患者的住院时间、住院花费情况,实施后优于实施前(P<0.05)。结论:将病案信息管理和临床路径相结合的工作模式应用到临床上,有助于进一步提高医院临床工作质量,避免出现医疗信息数据差错问题,值得在临床上做就进一步推广。 关键词:病案信息管理;临床路径;相互作用 前言:临床路径的实质,是一种具有实践性、顺序性的医护计划,有医生、忽视等医护人员按照既定的路线与方法进行临床操作,其主要目的是进一步改善患者预后。随着临床路径被进一步推广,病案信息管理也发生一定的变化,并且也面临着更高的要求,了解病案信息管理与临床路径相互作用的关系、实现两者的顺利结合,已经成为相关人员关注的重点。为此,本文分析我院自2015年1月份实施病案信息管理与临床路径结合以来临床工作的相关资料,具体研究内容如下。 1.资料与方法 1.1一般资料 我院自2015年1月实施病案信息管理和临床路径思想,所涉及科室覆盖全医院,本文选取该时间段内来我院就诊的1346例患者,包括男性患者833例,女性患者513例。同时回顾性分析我院实施病案信息管理和临床路径之前就诊的1524例患者临床资料,包括男性患者856例,女性患者668例。两组患者性别等一般资料数据差异无统计学意义,可以进行组间比较。 1.2方法 收集实施病案信息管理和临床路径前后相关患者的临床信息,并做好组间比较。 1.3统计学处理 采用SPSS 20.0软件对本次研究的相关数据进行处理,以X2值、t值检验数据间的差异,当P<0.05时,认为数据差异具有统计学意义。 2.结果 在实施病案信息管理和临床路径后,我院临床工作质量进一步提高,通过比较实施前后我院在临床工作中出现的医疗信息差错情况后发现,实施后仅出现3例信息错误案例,与实施前的64例相比,数据差异具有统计学意义(P<0.05),相关资料如表1所示。 3.讨论 临床路径的主要目的是在医疗质量得到保证的情况下,试图寻找效益更高的医护模式,我国最早在1996年引入临床路径概念,随着现代医疗技术的进一步发展,临床路径概念得到了人们的普遍关注。在这种背景下,病案信息管理作为医院日常管理的重点内容,时刻受到临床路径思想的影响,临床路径也对病案信息管理提出了更高的要求。 3.1病案信息管理对临床路径实施的影响 在临床路径工作中,开展病案信息管理的中的重点,就是要做好临床路径病种的选择与报表设计等前期工作。在具体操作中,工作人员将按照《疾病和有关健康问题的国际统计分类》的相关内容,对近几年发生的病例数进行回顾性分析,在综合考虑不同治疗方法费用、疗效的基础上,按照模式可循、并发症少等方面寻求相关方法的可控性,最终汇总资料后,交由相关科室选择临床路径病种。 临床路径的实施必然会产生相对应的资料,这些资料的保管、储存都是有病案信息管理部门完成。如果不能及时有效的采取管理办法,会导致管理效果达不到预期,影响临床路径的实施效果。同时,由于临床路径主要由临床路径标准、住院流程、临床路径表三方面组
呼吸科必备基本功:全面解读肺功能检查(系列视频教程) 如果你此时此刻处于一脸懵圈儿的状态,那你就该好好思考一下,你是否是一名优秀的呼吸科医生了。(答案在下方试播视频中) 呼吸科必备基本功:肺功能检查的临床解读。 肺功能检查是一种必要的呼吸系统疾病的检查,对于早期气肺疾病、气道病变诊断,评估疾病及预后、临床疗效等具有重要的意义。临床中所使用的肺功能检查方法多样,选择合适的方法对于诊断思路具有重要的意义。 然而就这一项基本功,现实中却存在着各种问题:开展普及程度不够;检查流程的标准化亟待提高;检查项目不完整。学习氛围不足。 医院不开展,医生拿着病人外院带来的报告单,好尴尬,看不懂啊;医院开展了,医生不重视,拿着报告单却要去追问检验技师,试问多少技师具有临床思维。 因此,丁香园特邀杭州市第一人民医院呼吸科副主任医师沈凌开设《手把手教你读懂肺功能测定》系列课程!结合大量真实临床案例,让大家在临床上可以灵活通过临床思维去运用及解读肺功能检查。肺功能检查的临床意义 早期检出肺、气道病变鉴别呼吸困难和咳嗽的原因评估病情的严重程度评估疾病的病情进展评定药物和其它治疗方法
的疗效劳动强度、耐受力的评估危重病人的监护评估胸肺外科手术耐受力通过系列课程,你将学习 概述:肺功能检查现状、临床应用及肺功能评估注意事项。肺通气功能内容及其临床解读:每分钟通气量;最大通气量;气速指数;时间肺活量。 不同类型通气功能障碍特征及病因:阻塞性通气功能障碍;限制性通气功能障碍;真、假性限制性通气功能障碍如何鉴别;阻塞性和限制性病变如何区别?混合型通气功能障碍。肺通气功能异常的特殊类型:小气道阻塞;上气道阻塞;如何区分胸内、外上气道阻塞;如何量化上气道阻塞。 肺通气功能检测的几个问题:正常值范围如何确定;肺功能损害程度的分类法与COPD 分级为什么不同;PEF%与FEV1%有何关系。 肺容积测定:测定指标、计算指标及相互关系;如何把肺容积和肺通气图形相结合;肺容积的影响因素;肺容量异常的程度评价;肺容积的测定方法及临床解读。 肺弥散功能测定:气血屏障的特性;检查的适应症和禁忌症;检查方法步骤及临床应用解读;影响因素及注意事项。气道反应性:临床解读、增高的机制、影响因素。 支气管激发试验:临床解读、适应症、禁忌症、操作步骤、注意事项。 支气管舒张试验:适应症、禁忌症、试验流程、临床解读、
慢性阻塞性肺疾病患者营养及代谢支持的应 用 【关键词】慢性阻塞性肺疾病,营养,代谢支持 慢性阻塞性肺疾病(COPD)发展过程中往往伴有营养不良,其发生率为24%~71%〔1,2〕,其中,肺气肿、肺心病尤为突出,呈蛋白热量营养不良状态。营养不良的程度与气流阻塞程度有关,有发生急性呼吸衰竭和死亡的倾向,因而被视为重要的预后指标〔3〕。因此,营养及代谢支持治疗也成为COPD治疗的重要手段,加强营养及代谢支持治疗能纠正患者的代谢紊乱,降低感染的发生率,改善患者预后。 1 COPD营养及代谢的特点和胃肠道功能的变化 营养不良使呼吸肌贮备下降及易于疲劳,能量供应不足和肌纤维结构的改变减弱呼吸肌的收缩力和耐力,损害呼吸肌的功能,从而诱发或加重呼吸衰竭。营养不良影响通气驱动力,降低呼吸中枢对氧的反应。由于蛋白营养不足,肺泡及支气管上皮的修复功能受损,使气管插管套管压迫的部位更易发生溃疡及出血,增加了合并症的几率。除了蛋白及能量供应不足以外,某些电解质及微量元素的不足亦可引起呼吸肌无力。COPD患者伴发呼吸衰竭时,低磷血症使膈肌功能受到明显损害〔4〕,是较常见的并发症。
COPD患者年龄偏大,咀嚼功能低下等致使热卡摄入下降。此外,COPD患者进餐时加重呼吸负荷,血氧饱和度下降,造成患者气促厌食、摄入减少。膈肌下降使胃容量减少,心力衰竭、缺氧及高碳酸血症造成胃肠淤血,抗生素和氨茶碱类药物对胃黏膜刺激等因素导致胃肠功能紊乱,亦可使患者厌食、摄入减少。COPD患者由于气道阻力增加,肺顺应性下降,而使呼吸肌做功增加,导致静息能量消耗(REE)增加20%~40%〔5,6〕。COPD是不完全可逆的气流受限、呈进行性发展的疾病〔7〕,长期的低氧血症和/或二氧化碳潴留,影响消化系统对营养物质的吸收。呼吸肌作功和氧耗量增加,使机体的静息能量消耗与活动时热能消耗不断增加,为满足能量消耗的需要,贮存的脂肪和肌肉蛋白质分解代谢增强,长期营养不良引起呼吸肌结构和功能发生改变,导致呼吸肌力减弱〔8〕。同时,热量摄入相对不足、缺氧、感染等因素又引起呼吸肌能量代谢改变,有氧氧化减弱,无氧酵解增强,最终导致能量负平衡,营养状况逐渐下降。Sahebjami等〔9〕的研究表明COPD的营养状况往往与气道阻塞的严重程度呈平行关系。 2 营养支持治疗的目的 目的主要是:(1)纠正已经出现的营养不良,改善营养状态,提高对疾病和治疗的耐受性。(2)阻止进行性蛋白质和热量的消耗,改善负氮平衡。(3)调整和改善病人的代谢状态,减少并发症。(4)缩短病程,降低死亡率。近年来随着代谢支持、代谢调理和生态免疫营
COPD患者注意事项 据了解,COPD患者一次急性加重的住院费用会高于日常使用支气管扩张剂思力华(噻托溴铵)一年的用药花费,而通过长期坚持规范用药,可大大降低慢阻肺的死亡率。 预防感冒 根据天气变化及时增减衣物,避免受凉。 深呼吸运动 采用鼻吸口呼的方式,进行深长呼吸,每天早晚各做1次,每次15~20分钟左右,体质稍好者还可配合呼吸操或慢步行、登楼梯、太极拳等练习。 家庭氧疗 每天吸氧15个小时以上,吸氧浓度为1~2升/分钟。 药物治疗 慢阻肺缓解期治疗的药物主要有支气管扩张剂(如舒利迭、思力华等)、化痰药(如氨溴素等)、提高免疫力药物(如微卡等),必要时应用抗生素,但最好在专科医生指导下使用。 良好的生活习惯 必须戒烟;注意休息。 合理饮食 慢阻肺患者一般比较消瘦,抵抗力较差。因此,应补充优质蛋白;避免碳水化合物类饮料;忌吃羊肉、狗肉等湿热上火的食物;宜吃百合、梨、木耳、芝麻、萝卜、蜂蜜、莲有两种方法不仅能延长慢阻肺患者的寿命,而且能提高慢阻肺患者的生活质量,那就是戒烟(针对吸烟患者)和氧疗。国内外的研究显示,长期家庭氧疗是惟一能提高慢阻肺患者生存率的治疗手段。 对于慢性阻塞性肺疾病(COPD,简称“慢阻肺”)的治疗,以保护残存肺功能、延缓肺功能下降为主要目的。需从以下几方面努力:如防治感染,采用化痰、解痉及扩张支气管的药物,治疗并发症,如心功能衰竭、电解质紊乱等。而患者积极配合医生治疗,注重自我管理,对减轻慢阻肺急性加重起到非常重要的作用。 要诀1积极关注
患者应积极向医生或医务工作者咨询,了解引起病情急性加重的因素,加以避免。例如,吸烟、感冒、着凉、下呼吸道反复感染等。吸烟可导致呼吸道免疫功能下降,易受外来微生物的侵袭和破坏。 要诀2经常使用支气管扩张药物 这是控制慢阻肺患者症状的中心药物。病情比较重的患者可能要终身应用支气管扩张剂,这些药物包括β2-受体激动剂、M受体阻断剂和茶碱等。目前,对中、重度患者主张长效β2 -受体激动剂和激素同时吸入使用,可减缓肺功能下降,改善呼吸困难的症状。但每一位患者情况不同,如何递增或递减这些药物,都应咨询有经验的专科医生。 要诀3适量运动 在身体情况允许时,要加强运动锻炼,包括呼吸肌锻炼。例如,进行腹式呼吸锻炼,以发挥腹肌作用,同时也增强膈肌功能,增加运动时最大通气量,减少呼吸功耗,改善机体氧合度。稳定期患者可做一些节奏较慢、较温和的体育运动,如打太极拳,可使骨骼肌得到锻炼。每天锻炼数十分钟,持之以恒,可提高呼吸肌的耐力和机体的生理功能,促进食欲和睡眠。 要诀 4 长程氧疗 多个临床观察表明,对于动脉血氧分压(PO2)<55毫米汞柱的患者每天吸氧>15小时,可明显延长患者寿命,改善生活质量。 所有治疗慢阻肺的药物,如抗感染、扩张支气管类等,都不能逆转疾病进展,只能改善症状、减少并发症、控制病程。但是有两种方法不仅能延长慢阻肺患者的寿命,而且能提高患者的生活质量,那就是戒烟(针对吸烟患者)和氧疗。国内外的研究显示,长期家庭氧疗是惟一能提高慢阻肺患者生存率的治疗手段。 长期家庭氧疗的主要目的是纠正低氧血症,减少呼吸功以及减轻心脏负荷,防止和逆转缺氧所致的组织损伤和器官功能障碍,同时尽量保持患者的活动能力。对伴有慢性低氧血症的慢阻肺患者,需要长期低流量吸氧,每天连续吸氧时间不得少于15小时。 (白春学教授每周一、四上午有专家门诊) 什么是“慢阻肺” 慢性阻塞性肺疾病(COPD)简称“慢阻肺”,是一种严重危害人们健康而又易被忽视的慢性进行性加重的呼吸道疾病,也就是老百姓常说的慢性支气管炎和肺气肿到了“一定程度”的总称。这个“程度”就是进出肺部的气流出现限制。 慢阻肺的主要症状是长期咳嗽、反复咯痰,每年出现一次到数次的咳嗽、咯痰加重(即急性加重),出现活动性气急,并逐渐加重。慢阻肺病程呈进行性加重,
临床路径模式在医院病案管理中的应用 发表时间:2016-07-18T11:10:13.553Z 来源:《中华临床医师杂志》(电子版)2016年2月第4期作者:郑桂华1 周旭文2 郑烈辉1 张业金2 黄曼芬2 [导读] 临床路径(Clinical Pathway,CP)模式是一种十分先进的医疗管理模式,其理念主要是不断的改进质量管理。 郑桂华1 周旭文2 郑烈辉1 张业金2 黄曼芬2 【摘要】临床路径模式顺应医疗卫生改革的趋势,逐步在病案管理中被广泛应用,我国临床路径管理模式刚刚起步,其工作的开展运用还不是十分成熟,这也给医院病案管理人员带来了很大的挑战。因此,改变先前的管理模式,更新病案管理人员的相关理念,学会并运用崭新的临床路径管理模式为医院病案管理服务是当前医院的一项重点。随着社会的需要和技术的不断革新,临床路径模式将不断提高医疗质量,规范临床病案管理,减少医疗资源的浪费,成为病案管理的不二之选。 【关键词】临床路径管理;病案管理;应用效果 临床路径(Clinical Pathway,CP)模式是一种十分先进的医疗管理模式,其理念主要是不断的改进质量管理,有效的控制并减少医疗费用的无效支出,减少医疗资源的浪费,规范医院的临床治疗和护理,提高医疗效果,减少患者的病痛和经济负担,使患者更快的恢复健康。临床路径模式适应社会的相关需求[1-3],作为一种效益质量管理模式被应用到医院管理工作中受到了医院管理人员的关注,为医院的医疗工作带来变革。 临床路径模式的基本理念 从上世界80年代开始,临床路径模式最早在美国的一些医院开始研究应用[4,5],随着时间推移,医疗科技的进步,临床路径模式也几经变化,现逐渐在我国医院中应用开来。临床路径模式是医护人员对一些特殊的手术及诊断,实施一些有针对性的、计划性的及时间性的管理计划,这样可以减少医疗资源的不必要浪费,加快患者康复的速度,提升医疗效率,使得患者获得最佳的护理。临床路径模式体现了以人为本的护理理念,依照其既定的管理计划,培养和提高医护人员的临床护理品质,为医院病案管理带来方便和提升。 临床路径模式在医院病案管理中应用的要求 1.临床路径模式对病案实施的要求 临床路径模式强调诊疗过程的规范性和标准性,要求诊疗过程要有计划,避免了出现传统诊疗中的多变引起的不稳定因素。当对临床路径模式的病种进行选择的时候,主要有以下要求:(1)突出重点,一些代表专科水平的病种要加以重视;(2)病种选择应针对当下的主要多发病和常见病;(3)每一种病种的病例数要达到一定的要求。依照临床路径模式选择相关病例,针对患者的病情病况、住院天数等相关指标进行统计分析比较,选择组内患者各指标变化差异较小的病种进行探究,这样可以降低临床路径模式的实施难度,提高其成功率,为该模式的患者切实提供有效的服务[6-7]。针对医院一些医嘱类型的项目,实施临床路径模式的过程中应对整个的医疗过程进行评价,随机抽取相关病例并采用回顾性分析,依照循证医学的思路施行有标准的医嘱内容。 2.临床路径模式的评估对病案管理的要求 依照临床路径模式,病案的首页位置应当几种记录患者最原始、最重要的资料信息。通过这些信息可以了解患者的基本信息,为医学统计和治疗信息提供必要的数据来源。另外通过病案管理系统,可以对患者的诊疗信息统计分析和研究,汇总临床路径的开展情况。 3.临床路径模式中监控对病案的要求 临床路径的实施过程中各项流程的执行是否符合既定标准可以通过病案一一展现出来,病案信息能够对医疗过程及效果进行反应。在病案管理过程中,对病案的每个环节做好质量检查能够有效的对临床路径模式的整个流程和执行情况进行监督,通过病案的检查和统计可以检测和评价实施效果[8],分析特殊病案发生变异的原因,为临床路径的改善提供依据。 临床路径模式在病案管理中实施中存在的主要问题 1.病案管理人员的综合素质较弱 临床路径实施过程中,病案管理人员普遍意识较为淡薄,在病案管理方便存在着发展不平衡的现象,病案管理人员缺乏工作积极性,对自身工作不够重视,综合素质、业务能力及思想水平等方面较为薄弱。第二,病案管理的团队结构没有科学性。医院的大部分病案管理人员多是从医生、护士等转变而来,缺乏病案管理的专业人士,这些人多数缺乏专业的知识,专业技能参差不齐,随着网络技术在病案管理中的应用,给这些病案管理人员带来了很大的困难。科学技术在不断飞速发展,医院的信息化也不断加快,现有的病案管理人员已很难满足医院信息化的基本需要,对于医学知识及医院管理知识兼备的人员现在非常少。 2.信息化应用起步难 病案管理工作在我国起步较晚,实施过程中受到各种因素的影响,当前医院信息化临床路径的发展并不十分顺利[9]。在病案管理中,由于没有统一的标准,病案管理受人为影响的因素较大,给病案的再次调用和长期保存带来了较大困难。当前,医院的病案资源不能够在临床诊疗中作为依据应用。病案记录仍以手工书写为主,且主要是文本格式,无法形成结构化的数据,不利于临床路径的发展。 病案管理缺乏统一的信息管理软件和病案规范。虽然现在已经有一些电子病案信息软件,但是各系统之间不兼容,无法形成统一的网络进行共享交流,很难形成全国性的统一系统,医疗信息资源重复且浪费。 适应临床路径实施的病案管理对策 1.提升病案管理人员的综合素质,更新病案管理人员的理念 普及现代医院的服务模式和建设职能,将其结构观念深入每个档案管理人员的心中,鼓励病案管理人员主动地学习相关知识。在工作过程中可以建立临床路径模式管理小组,使得病案管理人员积极参与其中,带头依照新路径进行工作。相关人员应当树立循证医学的理念,开展临床路径知识的教育培训,将临床路径知识与医院内的工作结合在一起[10]。病案管理人员的专业素质和编码水平越高,越能掌握好患者的病案信息变化情况,工作人员应当严谨、认真的学习,积极搜集有用的资料,保障临床路径模式的顺利实施。 2.统一疾病分类编码标准 统一疾病分类编码标准有助于保障临床路径病种资料的统一性。应设立相关病案管理的综合管理委员会[11],协调统一各地区的病案信息标准,对国际上疾病最新信息及时传达和完善。使得地区范围内的病案编码的一致,临床路径病种的资料能够统一。