
J Neurosurg 88:581–585, 1998
Multiple choroid plexus papillomas of the lateral ventricle distinct from villous hypertrophy
侧脑室多发脉络丛乳头状瘤
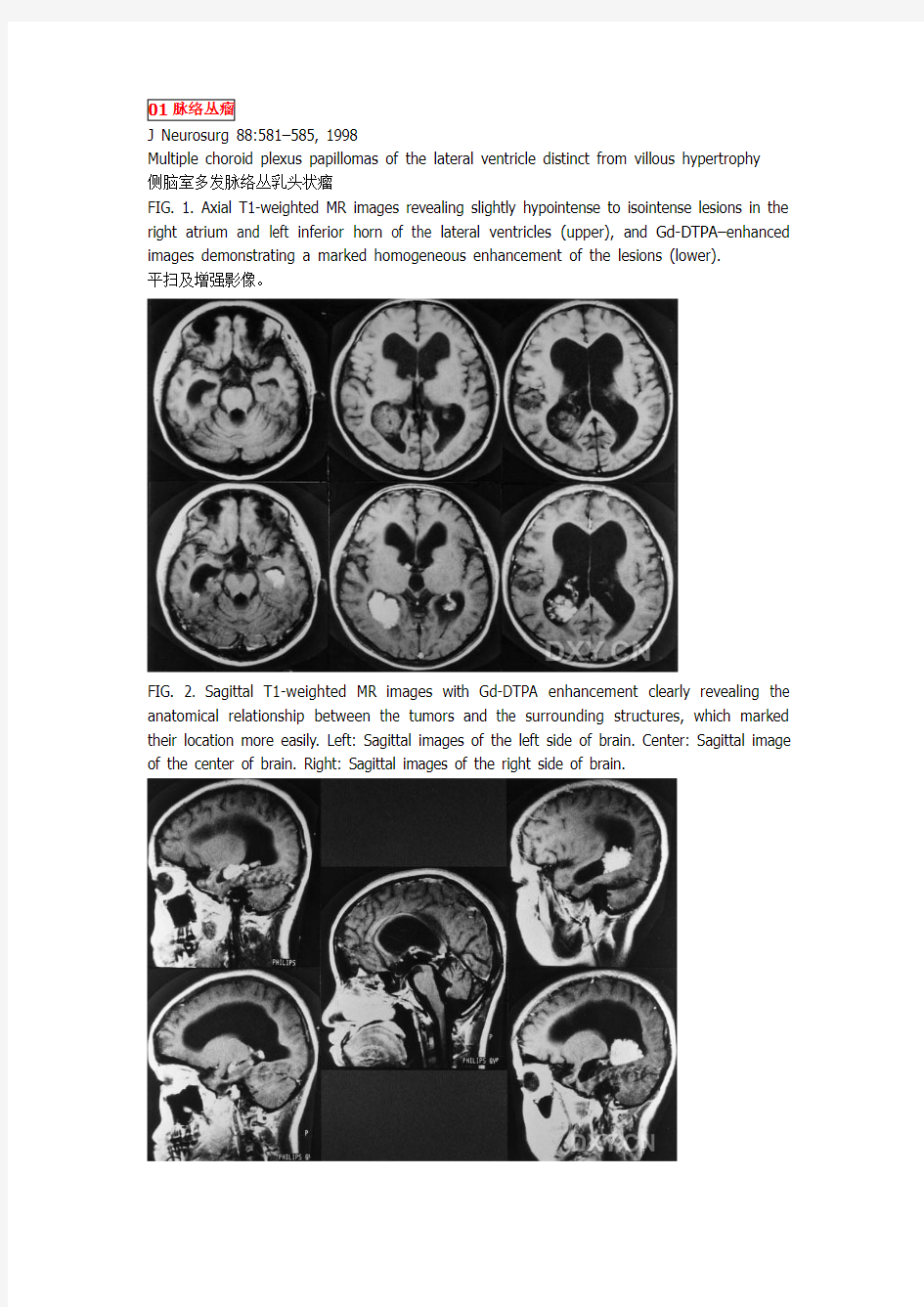
FIG. 1. Axial T1-weighted MR images revealing slightly hypointense to isointense lesions in the right atrium and left inferior horn of the lateral ventricles (upper), and Gd-DTPA–enhanced images demonstrating a marked homogeneous enhancement of the lesions (lower).
平扫及增强影像。
FIG. 2. Sagittal T1-weighted MR images with Gd-DTPA enhancement clearly revealing the anatomical relationship between the tumors and the surrounding structures, which marked their location more easily. Left: Sagittal images of the left side of brain. Center: Sagittal image of the center of brain. Right: Sagittal images of the right side of brain.
FIG. 3. Upper: Photomicrograph of the tumor specimen obtained during the first operation in the right ventricular region. Note the papillary growth of a single and partly stratified layer of columnar epithelium, consistent with a typical choroid plexus papilloma. Lower: Photomicrograph of the tumor specimen obtained during the second operation in the left ventricular region. The histopathological characteristics are similar to those shown in the right ventricular region. H & E, original magnification 3 200.
病理结果。
Acta Neurochir (2003) 145: 139–143 DOI 10.1007/s00701-002-1047-x Acta Neurochirurgica Printed in Austria Case Report
Choroid plexus papilloma of bilateral lateral ventricle
T. Erman1, A. I˙. Go¨c?er1, S? . Erdog?an2, M. Tuna1, F. I˙ldan1, and S. Zorludemir2
1Department of Neurosurgery, C? ukurova University, School of Medicine, Adana, Turkey
2Department of Pathology, C? ukurova University, School of Medicine, Adana, Turkey
Fig. 1. (a) Axial non-contrast CT scan demonstrating tumour of the lateral ventricles bilaterally and hydrocephalus. (b) Axial contrast enhanced CT scan demonstrating an enhancing tumour of the lateral ventricle bilaterally with hydrocephalus
(b) Axial contrast enhanced CT scan demonstrating an enhancing tumour of the lateral ventricle bilaterally with hydrocephalus
Fig. 2. Axial enhanced MRI demonstrating a lobulated enhancing mass in the bilateral lateral ventricular trigone
Fig. 2. Axial enhanced MRI demonstrating a lobulated enhancing mass in the bilateral lateral ventricular trigone
Transient memory disturbance after removal of an intraventricular trigonal meningioma by a parieto-occipital interhemispheric precuneus approach:Case report
肿瘤切除后记忆暂时紊乱
Koji Tokunaga, MDa,T, Takashi Tamiya, MDb, Isao Date, MDa
aDepartment of Neurological Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Okayama 700-8558, Japan
bDepartment of Neurological Surgery, Faculty of Medicine, Kagawa University, Kagawa 700-8558, Japan
Received 15 December 2004; accepted 13 June 2005
Fig. 1. Left and center: Preoperative gadolinium-enhanced T1-weighted MR images demonstrating a homogeneously enhanced mass at the left trigonal region, extending predominantly in the anterior direction. Right: A T2-weighted MR image showing moderate
edema around the mass
Fig. 2. Left and right: Postoperative gadolinium-enhanced T1-weighted images demonstrating the route approaching the left trigone from the interhemispheric fissure and confirming complete removal of the tumor
Symptom Changes Caused by Movement of a Calcified Lateral Ventricular Meningioma CASE REPORT
Shigeki Imaizumi, M.D.,* Takehide Onuma, M.D.,* Motonobu Kameyama, M.D.,* and Kiyoshi Ishii, M.D.?
*Departments of Neurosurgery and ?Radiology, Sendai City Hospital, Sendai, Japan
Sequential CT studies over 16 years revealed no distinctive change in size of the calcified meningioma (A-D). CT taken 16 years before this admission (A). Hydrocephalus and peritumoral edema caused by a tumor in the ventricle were seen at admission (B). The ventricle size was normalized after ventriculoperitoneal shunt placement (C). The tumor was displaced beyond the ventricular midline five months later (D). Half of the tumor was resected during the 1st surgery using the trans callosal route (E) and the remaining mass was removed during the second surgery using the trans inferior temporal sulcus approach (F).
Hemangiopericytoma in the Trigone of the Lateral Ventricle—Case Report—
Fig. 1 Axial computed tomography scan showing a massive right tri gonalmass, with dilation of
the contralateral ventricle.
Fig. 2 (A) Preoperative axial T1-weighted magnetic resonance (MR) image showing a large, isointense trigonal tumor. (B) T2-weighted MR image showing the hypointense tumor. (C) Sagittal T1-weighted MR image with contrast medium showing intense enhancement of the tumor.
Neurol Med Chir (Tokyo)
Child’s Nerv Syst (1998) 14:350–353
? Springer-Verlag 1998 BRIEF COMMUNICATION
Meningiomas of the lateral ventricles of the brain in children
Fig. 1 MRI showing intraventricular mass
Fig. 2 CT 2 weeks after operation, showing complete removal of tumour Fig. 3 CT scan showing intraventricular neoplasm in trigone region Fig. 4 CT 6 months after operation, showing complete removal of tumour
Acta Neuropathol (Berl) (1986) 71 : 167-- 170 Acta
Neuropathologlca
9 Springer-Verlag 1986
Central neurocytoma - a rare benign intraventricular tumor
j . j . Townsend I, 2 and J. P. Seaman 3
Department of Pathology, University of Utah
2 Salt Lake Veterans Administration Medical Center
3 LDS Hospital, Salt Lake City, UT, USA
Fig. 1. This picture demonstrates the well-circumscribed soft tumor mass (in the anterior right lateral ventricle) attached to the septum pellucidum and corpus callosum (case 1)
Fig. 2. The CT scan demonstrates the well-circumscribed mass in the right lateral ventricle anteriorly producing hydrocephalus (case 2)
Fig. 3. This print demonstrates the tumor to be composed of small dark nuclei forming occasional Homer Wright rosettes as seen in the center of the picture (case 1). Hematoxylin and eosin, x 800
Fig. 4. The tumor was composed of small round to oval nuclei which formed Homer Wright rosettes as seen in the center (case 2).Hematoxylin and eosin, x 375
Fig. 5. The neurosecretory granules can be seen in this electron micrograph, x 27,173
Fig. 6. Electron microscopy demonstrated numerous synapses with well-formed junctions as seen in the center, x 27,173
Journal of Clinical Neuroscience (1999) 6(4), 319-323
? 1999 Harcourt Brace & Co. Ltd
Clinical studies
Intraventricular neurocytoma: a clinicopathological study of 20 cases with review of the literature
Mehar Chand Sharma ~ MD, Chitra SarkaP MD, Asis Kumar Karak ~ MD PHD, Sailesh Gaikwad 2 MD,
Ashok Kumar Mahapatra a MCH, Veer Singh Mehta a MCH
Fig. 1 Contrast enhanced CT scan showing a well defined hyperdense mass, predominantly in the right lateral ventricle with cyst formation and secondary hydrocephalus (Case 16).
Fig. 2 Photomicrographs showing: (A) cellular areas separated by acellular fibdllary zones (H&E x 350); (B) thin walled dilated vascular channels within the tumour (H&E × 140); (C) diffuse
fibrillary immunostaining with synaptophysin antibody (x 200)
Case report
Epidermoid of the lateral ventricle: evaluation with diffusionweighted and diffusion tensor
imaging
表皮样囊肿
Radboud W. Koot a, Anuradha P. Jagtap b, Erik M. Akkerman b, Gerard J. Den
Heeten b, Charles B.L.M. Majoie b,*
a Department of Neurosurgery, Academic Medical Center, P.O. Box 22660, 1100 DD Amsterdam,
Netherlands
b Department of Radiology, Academi
c Medical Center, P.O. Box 22660, 1100 DD Amsterdam,
Netherlands
Received 4 March 2003; accepted 14 March 2003
Fig. 1. (A, B, C): (A) Axial T2-weighted (3500/90/1), and axial (B) and coronal (C), contrast
enhanced T1- weighted (570/40/2) MR images show enlarged left lateral ventricle with mass
effect and shift of midline structures to the right. Note widening of the left choroidal fissure (C;
arrow). A definite tumor cannot clearly be delineated. (D, E) Axial DWI shows a hyperintense
lesion in the left perimesencephalic cistern (D; arrow) and in the dilated left lateral ventricle (E).
The mass is surrounded by hypointense CSF. Findings are consistent with epidermoid tumor. (F) ADC map at the same level as (E) show ADC values in the lesion similar to brain parenchyma.
(G) FA maps of the lesion show areas of anisotropy, clearly demonstrate its relationship to neighboring white matter tracts and accentuate the lobulated structure of the lesion (tensor-imaging).
Fig. 1. (A, B, C): (A) Axial T2-weighted (3500/90/1), and axial (B) and coronal (C), contrast enhanced T1- weighted (570/40/2) MR images show enlarged left lateral ventricle with mass effect and shift of midline structures to the right. Note widening of the left choroidal fissure (C; arrow). A definite tumor cannot clearly be delineated. (D, E) Axial DWI shows a hyperintense lesion in the left peri mesencephalic cistern (D; arrow) and in the dilated left lateral ventricle (E). The mass is surrounded by hypointense CSF. Findings are consistent with epidermoid tumor. (F) ADC map at the same level as (E) show ADC values in the lesion similar to brain parenchyma.
(G) FA maps of the lesion show areas of anisotropy, clearly demonstrate its relationship to neighboring white matter tracts and accentuate the lobulated structure of the lesion
(tensor-imaging).
A large arachnoid cyst of the lateral ventricle extending from the supracerebellar cistern—case report
Seoung Woo Park, MDa, Soo Han Yoon, MDb,*, Ki Hong Cho, MDb, Yong Sam Shin, MDb
aDepartment of Neurosurgery, Kangwon National University, College of Medicine, Chunchon 200-701, South Korea bDepartment of Neurosurgery, Ajou University School of Medicine, Suwon 443-721, South Korea
Received 23 May 2005; accepted 30 July 2005
Fig. 1. Initial MRimaging shows that the arachnoid cyst had developed from the supracerebellar space in the posterior fossa and extended into the antrum and temporal horn of the left lateral ventricle. A and B: Axial MR imaging shows that the intraventricular cyst displaces the left choroidal vessels anteriorly (small arrow heads), the right choroid plexus laterally (smallarrow), the midline vessels to the right (large arrow), and an enlarged velum interpositum. C: Axial MR imaging shows that the left choroid plexus (small arrow) was severely displaced anteriorly and the thin cystic wall (arrow head)
crossed the right lateral ventricle. D and E: CoronalMRimages show that the cyst (small arrow heads) displaces the left choroids plexus contralaterally (arrow) and the right choroid plexus and choroidal vessels laterally (large arrow head). F: Coronal MR images shows displaced and collapsed right choroids plexus (small arrow), branching portion of choroidal vessels (large arrow), and left choroidal vessels (arrow head). G: Sagittal MR imaging shows that the cyst of the posterior fossa depressing the cerebellum downwardly (arrows) extending into and dilating the velum interpositum (small arrow heads) with anteriorly displaced contralateral choroid plexus (large arrow). H: Sagittal MR imaging shows the herniation of cerebellum (arrow) with visualization of the central canal of the cervical spinal cord (arrow heads).
Clinical Study
Intraventricular tanycytic ependymoma: case report and review of the literature
Brian T. Ragel1, Jeannette J. Townsend2, Adam S. Arthur1 and William T. Couldwell1
1Department of Neurosurgery; 2Department of Pathology, University of Utah Health Sciences Center, Salt Lake City,
UT, USA
Key words: supratentorial tumors, tanycytic ependymoma
Figure 1. Brain MRI depicting 2.8 · 2.6 · 2.3 cm (height · transverse · anterior–posterior) lesion arising from the region of the left superolateral third ventricle and septum pellucidum. Mass extends superolaterally into the left frontal horn of the lateral ventricle. (A) Axial T1 with contrast, showing minimal enhancement. (B) Axial T2, showing heterogenous signal. (C) Coronal T1 with contrast, with incidental left sphenoid wing meningioma (arrow). (D) Coronal FLAIR sequence.
Figure 2. (A) Low-power H&E stain (150·) showing moderately cellular tissue with areas of well-differentiated streaming tumor cells set in a vague fascicular architecture and faint perivascular pseudorosettes (black arrow). (B) High-power H&E photomicrograph (300X) depicting tumor cells arranged radially around a blood vessel, typical of the perivascular pseudorosettes of ependymomas (black arrow). (C) High-power photomicrograph (600X) of GFAP immunohistochemistry reactivity, depicting the delicate GFAP-positive processes of ependymal cells radiating towards the blood vessel wall (black arrow).
Shunji Nishio · Takato Morioka · Futoshi Mihara
Masashi Fukui
Subependymoma of the lateral ventricles
Fig. 1 Case 1. Enhanced CT scan shows a low density tumor in the right lateral ventricle
Fig. 2A–C Case 3. On contrast enhanced axial T1-weighted image, a hypointense
intraventricular tumor shows no tumor enhancement. Note cystic areas within the tumor and associated hydrocephalus (A). While the tumor is indistinguishable from the cerebrospinal fluid in the ventricle on T2-weighted image (B), it is clearly distinguished on heavily T2-weighted image (C)
Fig. 3A–C Case 4. Axial T1-weighted precontrast MRI shows a hypointense tumor filling the anterior horn of the right lateral ventricle (A). A T2-weighted MRI shows peritumoral edema in the right frontal lobe (B). Axial T1-weighted postcontrast MRI shows heterogeneous enhancement of the tumor (C)
Massive symptomatic subependymoma星状细胞增生性室管膜瘤of the lateral ventricles: case report and review of the literature
大的症状性瘤
Fig. 1 Axial pre- (a) and post- (b) contrast-enhanced computed tomography (CT) of the head shows a large symmetric isodense intraventricular mass without calcifications filling the lateral ventricles and extending into the temporal horns
Fig. 2 Axial T2-weighted and fluid attenuation inversion recovery (FLAIR) images (b, c) show a large symmetric hyperintense intraventricular mass that fills the lateral ventricles (a, b) and the temporal horns
Fig. 3 Axial (a) and coronal T1-weighted (b) post-contrastenhanced images demonstrate an intraventricular mass with minimal enhancement occupying the lateral ventricles and extending into the temporal horns
Fig. 5 Axial T2-weighted (a),FLAIR (b), and T1-weighted(c) post-contrast-enhanced
images demonstrate a slight debulking of the tumor after surgery with CSF present in the frontal horns of the lateral ventricle. The patient has a right frontal ventriculoperitoneal shunt catheter in place and is presently asymptomatic
Fig. 4 Resection specimen reveals a subependymoma, as characterized by nests of tumor cell nuclei and microcysts in a fibrillary stroma
Multicentric juvenile pilocytic astrocytoma occurring primarily in the trigone of the lateral ventricle
Fig. 1 A Pre- and B post-contrast enhancement computerized tomography showing a
7′6′6 cm mixed-density mass in the trigone of the left lateral ventricle entrapping the ipsilateral occipital horn. The solid compartment and cystic wall are well enhanced. There were conglomerate calcifications in the posteromedial portion of the mass. Hydrocephalus is also noted Fig. 2A–D Preoperative magnetic resonance images (MRIs). A Axial T1-weighted MRI showing a mixed-intensity mass with sharp demarcation from the adjacent structures except the posteromedial portion of the mass. B–D Gadoliniumenhanced MRIs showing that the cystic wall and solid component are well enhanced and that the septum pellucidum and lateral ventricular wall, the perimesencephalic cistern, and the anterior meninges or ventral aspect of the brain stem are enhanced, suggesting leptomeningeal spread. Small enhanced nodules are also seen in the right anterior temporal and occipital lobes as nodular disease. Tonsillar herniation and mild distortion of the brain stem with enlargement of the IV ventricle are also shown
Fig. 3 Photomicrograph of the trigonal juvenile pilocytic astrocytoma showing the typical histological features, including pilocytic, stellate, and oligodendroglial cells, microcysts, cytoid or granular bodies, and Rosenthal fibers with loose and compact areas. Vascular proliferation
and pleomorphism are absent. (H & E, ′250)
Intraventricular Hemangiopericytoma
Nabeel Al-Brahim, MD, Rocco Devilliers, MD, FRCS(C), and
John Provias, MD, FRCP(C)
Figure 1. Axial T1-weighted magnetic resonance image shows a well delineated tumor in the right lateral ventricle.
Figure 2. Contrast-enhanced T1-weighted image shows homogenous enhancement of the tumor.
关于侧脑室脑膜瘤手术治疗情况的分析 发表时间:2013-08-06T09:32:56.090Z 来源:《中外健康文摘》2013年第26期供稿作者:王彬王文华 [导读] 操作空间足够大、减少皮层牵拉、尽可能暴露肿瘤的供血动脉是侧脑室三角区手术入路的选择原则。 王彬王文华(中国人民武装警察部队上海市总队医院201103) 【中图分类号】R739.45 【文献标识码】A【文章编号】1672-5085(2013)26-0219-02 【摘要】目的结合临床实践经验,探讨侧脑室脑膜瘤的手术治疗。方法选取收治的侧脑室脑膜瘤患者46例为研究对象,采用总结回顾分析法,将研究对象的病例资料、临床治疗资料等搜集整理,并与经治医师、责任护士共同探讨病例,探讨侧脑室脑膜瘤的手术治疗的方法以及临床应用价值。结果患者临床症状:头痛、恶心、呕吐、肢体运动障碍、记忆力下降等。结论采用显微手术的方式进行治疗侧脑室脑膜瘤疗效显著,具有一定的优越性,值得临床推广应用。 【关键词】显微镜手术侧脑室脑膜瘤治疗分析 在颅内脑膜瘤中,脑室内脑膜瘤约占0.5%~5%,多发于额、顶、枕区大脑凸面、蝶骨嵴、颅前窝嗅沟等位置,其中侧脑室脑膜瘤约占侧脑室肿瘤的20.0%~30.0%[1.2]。对于此种疾病的治疗方法,手术为主要治疗手段。随着医学科技的发展以及显微镜技术的成熟,显微外科切除术也在不断进步,笔者选取中国人民武装警察部队上海市总队医院患者为研究对象,现报告如下。 1、资料与方法 1.1 一般资料:选取2011年1月~2012年12月期间,我院收治的侧脑室脑膜瘤患者46例为研究对象,其中男27例,女19例,年龄19~73岁,平均(41.12±9.32)岁。 1.2 研究方法:采用总结回顾分析法,将研究对象的病例资料、临床治疗资料等搜集整理,并与经治医师、责任护士共同探讨病例,探讨侧脑室脑膜瘤的手术治疗的方法以及临床应用价值。采用Microsoft Excel建立数据库,运用SPSS 13. 0统计软件进行统计分析。 2、结果 2.1 辅助检查结果:全部患者均行头颅CT扫描,结果表现为侧脑室内高密度占位病变,其中31例患者有钙化、9例患者肿瘤明显强化、6例患者瘤周脑组织有低密度水肿影。14例患者行MRI检查,32例脑血管造影检查,显示脉络膜前动脉供血10例,脉络膜后动脉供血13例,脉络膜前及脉络膜后动脉供血12例,回流至大脑内静脉15例,大脑大静脉15例。 2.2 手术治疗结果:采用显微神经外科技术对患者肿瘤进行全切除,肿瘤大小(2.2cm×2.5cm)~(8cm×8cm),并在术后常规行脑室外引流3~5d。手术入路方式,颞中回入路8例,顶枕入路29例,经胼胝体入路9例。本组所欲患者无手术死亡或重残。其中,命名性失语和阅读障碍9例,经1个月治疗后恢复正常;轻偏瘫4例,经治疗3个月后均恢复正常;癫痫发作6例,经抗癫痫治疗得到控制;对患者进行3个月~6年的随访,平均随访 3.5年,患者均未出现肿瘤复发,CT复查见扩大的侧脑室均恢复正常,并恢复正常工作和生活,对治疗效果表示满意。术后病理诊断,患者病理类型:纤维型15例,纤维母细胞型8例,上皮细胞型12例,血管内皮型4例,混合型7例。 3、讨论 侧脑室脑膜瘤病程较长,因肿瘤多数为良性,且在侧脑室内缓慢生长,而且侧脑室的空间相对较大,对肿瘤的生长有代偿作用,患者局灶性症状出现较少,且进行早期诊断比较困难[3]。而当患者肿瘤增大堵塞室间孔出现慢性梗阻性脑积水或对周围脑组织产生压迫时,才会有相应的临床症状而就诊。对于该病的诊断主要依靠CT、MRI检查明确诊断。通过全脑血管造影,对定性和手术有一定帮助,可使医生明确肿瘤的血供、脉络膜前动脉或(和)脉络膜后动脉异常,包括血管增粗、迂曲和肿瘤染色等,以为进一步治疗提供详细信息。 由于侧脑室脑膜瘤位置深在,质地多较韧,同时临近脑功能区及较多动静脉,血供多丰富,而且多数肿瘤体积往往较大,进行普通的手术切除较为困难,并发症较多,患者康复效果不佳。而采用显微手术切除肿瘤,则是治疗侧脑室脑膜瘤最有效的方法。本次研究中,患者采用了显微手术的方式进行治疗,取得了良好的效果,3年生存率达100%,且患者均对治疗结果表示满意。笔者认为,侧脑室肿瘤手术入路较多,分别有经顶叶、纵裂叶、颞枕叶、颞中回入路等。进行显微镜手术时,应根据患者术前神经功能障碍情况、脑室的大小、肿瘤的大小与位置、肿瘤是否位于优势半球、供血动脉走行、引流静脉的去向及术后可能出现的神经功能缺失等因素选择合适的手术入路,并且应避开大脑皮层主要功能区(如中央前回、中央后回、优势半球的角回等),以使手术更好的进行。操作空间足够大、减少皮层牵拉、尽可能暴露肿瘤的供血动脉是侧脑室三角区手术入路的选择原则。皮肤切口以颞顶偏后弧形切开为佳,皮瓣切口应较大,并选择以偏后下的颞顶瓣或颞顶枕瓣入颅。便于接近肿瘤,且可避免过分牵拉(或撕裂)大脑外侧裂血管与皮肤血管,即使患者的肿瘤体积过大、深在,亦可处理好肿瘤根部、血管与脉络丛的关系。 参考文献 [1]李建华,张俊和,等.经楔前叶入路显微手术切除侧脑室三角区脑膜瘤3例[J].中国微侵袭神经外科杂志,2010,12(11):571. [2]祝斐,黄新,陈谦学,等.神经内镜在侧脑室脑膜瘤显微手术中的应用[J].中国临床神经外科杂志,2008,13(3):146. [3]杨东波,蒋传路,李永利,等.侧脑室脑膜瘤的显微外科治疗(附22例报告)[J].中国微侵袭神经外科杂志,2009,10(4):186.
J Neurosurg 88:581–585, 1998 Multiple choroid plexus papillomas of the lateral ventricle distinct from villous hypertrophy 侧脑室多发脉络丛乳头状瘤 FIG. 1. Axial T1-weighted MR images revealing slightly hypointense to isointense lesions in the right atrium and left inferior horn of the lateral ventricles (upper), and Gd-DTPA–enhanced images demonstrating a marked homogeneous enhancement of the lesions (lower). 平扫及增强影像。 FIG. 2. Sagittal T1-weighted MR images with Gd-DTPA enhancement clearly revealing the anatomical relationship between the tumors and the surrounding structures, which marked their location more easily. Left: Sagittal images of the left side of brain. Center: Sagittal image of the center of brain. Right: Sagittal images of the right side of brain.
侧脑室囊肿是什么 相信有些准妈妈在产检的时候会发现胎儿侧脑室囊肿,这听起来很令人害怕,准妈妈们总是会想得比较多,长期这样,准妈妈会精神过于紧张,为了防止这种现象的发生,我们为大家介绍一下侧脑室囊肿是什么,准妈妈们也可以有个心理准备,保持乐观的心态,积极产检,才能给胎儿最好的保护。 目前认为侧脑室囊肿病理分型有:神经上皮样囊肿(包括脉络丛囊肿和室管膜囊肿)和蛛网膜囊肿,其中大多数为脉络丛囊肿。脉络丛囊肿是最常见的神经上皮样囊肿,多见于儿童,在整个脑室系统均可发生,最多见于侧脑室三角区,其次为侧脑室体部、枕角和颞角,额角罕见,与脉络丛的解剖分布有关。脉络丛囊肿常在胎儿时就已经发生,与第18号染色体三体有关,也可能和21号染色体变异有关,但是大多数在出生后2年内消失,并不影响婴幼儿的生长发育。 侧脑室囊肿可单发,也可多发.本病一般无任何症状,一旦囊肿阻塞脑脊液循环,则可以造成胎儿脑室扩张.脉络膜囊肿多在
早期妊娠晚期或中期妊娠早期发现,孕24~26周后明显缩小或消失. 侧脑室有囊性肿块一般对胎儿没有直接影响。如果囊肿比较小,而且在左侧侧脑室一般不会堵塞脑脊液循环,不造成颅内压 增高等。暂时可以先不处理这个囊肿的问题,如果胎儿未发现合并其他畸形,则可嘱孕妇随访观察,至妊娠结束。 检查中若发现胎儿脉络膜囊肿,不要立即认为是病理性或生理性的,应同时仔细检查胎儿是否合并有其他畸形,如果胎儿合 并有其他畸形时应建议孕妇行羊膜腔穿刺抽羊水作染色体检查,以尽早排除染色体疾病.如果胎儿未发现合并其他畸形,则可嘱 孕妇随访观察,至妊娠结束. 等生产完后,可以到神经外科就诊,可能需要定期复查,确定此囊肿的性质是良性的还是恶性的,然后确定治疗方案。 通过上面的介绍,对于侧脑室囊肿是什么,相信准妈妈们心中也有自己的理解了,其实,每个宝宝都是上天赋予我们的天使,作为准妈妈千万要放松自己的心情,如果发现侧脑室囊肿就要坚持复检,最后确定情况如何,这是为宝宝未来的健康保障,也是为每个家庭的幸福保障。
侧脑室脑膜瘤的MRI诊断 作者:马春艳,芦苇,归俊,归云荣 【摘要】目的分析侧脑室脑膜瘤的MRI表现,以提高认识,为影像诊断提供依据。方法回顾分析26例经手术、病理证实的侧脑室脑膜瘤的MRI资料,分析其MRI表现。26例病人中21例做MRI平扫及增强扫描,5例只行平扫检查。结果 9例位于左侧侧脑室三角区,3例位于右侧侧脑室三角区且合并右侧额叶脑转移瘤,6例位于左侧侧脑室三角区及体部,8例位于右侧侧脑室三角区,其中3例合并脑实质转移瘤,5例合并肿瘤内出血;侧脑室脑膜瘤好发于中年人,多见于侧脑室三角区,肿瘤体积较大,形态不规则,信号不均匀,平扫时T1WI呈等或稍低信号,T2WI呈稍低、等或略高信号,边界清楚,增强后呈不均匀强化。结论侧脑室脑膜瘤MRI表现具有一定的特异性,提高对侧脑室脑膜瘤的认识,提高对脑膜瘤术前诊断水平,对临床制定正确的手术方案有重要的意义。 【关键词】脑膜瘤;侧脑室;磁共振成像 脑膜瘤是颅内最常见的良性脑肿瘤,其发病率仅次于胶质瘤,好发于35~70岁人群,其中女性发病率是男性的2倍[1]。多数脑膜瘤位于大脑凸面,并具有典型MRI表现,一般容易诊断,诊断符合率可高达95%[2],但侧脑室内脑膜瘤较少见,占脑膜瘤的0.5%~4.5%
[3],其部位特殊,导致其定性诊断有一定的困难。笔者对经手术、病理证实的26例侧脑室内脑膜瘤的MRI表现进行分析,并结合文献进行讨论,以期提高对其认识。
1 资料与方法 1.1 临床资料本组病例中男 12例,女14例,年龄22~58岁,平均38.6岁;所有患者均经手术病理证实。临床表现均有不同程度的头痛、头晕,其中8例合并恶心、呕吐;13例合并视力下降,6例伸舌右偏、右侧鼻唇沟变浅。 1.2 扫描方法使用Siemens Novus 0.35T核磁共振室扫描仪,扫描的层厚6mm,层间距1.5mm;26例病人中21例行MRI平扫和增强扫描,5例行平扫扫描,造影剂为钆喷酸匍胺注射液,用量为0.2ml/kg;均行自旋回波和快速自旋回波的T1WI、T2WI、液体衰减反转恢复(FLAIR)的轴位、矢状位及冠状位扫描。 2 结果 2.1 病灶部位 9例位于左侧侧脑室三角区,3例位于右侧侧脑室三角区且合并右侧额叶脑转移瘤(见图1~图3),6例位于左侧侧脑室三角区及体部(见图4~图6),8例位于右侧侧脑室三角区。
侧脑室肿瘤 【概述】 侧脑室左右各有一个,形状不规则,位于额叶、顶叶、枕叶及颞叶内。分为前角、下角、后角、体部和三角区5个部分,内含脑脊液,是由侧脑室内的脉络膜组织所分泌侧脑室内肿瘤是指来源于侧脑室壁、脉络膜组织及异位组织的肿瘤。常见者有脑膜瘤、室管膜瘤、脉络膜乳头状瘤及上皮样囊肿,其中以脑膜瘤为最多。根据大量病例的统计侧脑室的前部以胶质瘤为多见,后部多发生脑膜瘤,脉络膜乳头状瘤则多发生于三角区,并可向脑室的其它部位延伸,有时可通过室间孔而长入第三脑室。但总的看来侧脑室肿瘤多发生于侧脑室的前部及三角区。可见于任何年龄,但以20岁以前发病者较多,左侧似多于右侧,男多于女。 【临床表现】 脑室为脑内的空腔,内含脑脊液,因此其临床表现取决于肿瘤的大小和部位,只有当肿瘤阻塞了脑脊液循环通路,或当肿瘤压迫其周围脑组织时才出现相应的症状和体征。如颅内压增高症和病灶症状。 1.颅内压增高侧脑室内肿瘤当其体积很小或未引起脑脊液循环受阻时,病人可完全没有任何明显症状。当脑脊液循环发生障碍后(室间孔阻塞、脑室部分梗阻),而出现颅内压增高症,在临床上则表现为头痛。头痛也是大部分病人的首发症状,据资料统计,以头痛为首发症状者约占侧脑室肿瘤病人的9 2.5%。头痛常呈发作
性、间歇性或阵发性加重。当室间孔或脑室的一部分(上角或下角)被阻塞时则造成梗阻性脑积水,因脑室的急剧扩张,病人头痛常难以忍受,头痛严重时病人出现恶心与呕吐。有的病人可因突然的颅内压增高产生脑疝导致昏迷甚至死亡。肿瘤在侧室内有一定的活动度,常呈活瓣状而突然阻塞脑脊液循环通路,造成急性颅内压上升,这也是发作性头痛产生的原因。当因体位或头位发生变动使脑室受阻的情况解除时,病人头痛可很快停止。如再次阻塞,随之头痛再次发生,如此可反复多次发作。因此有少数病人于每次发作时常以前额撞地或呈屈膝俯卧位。 病人在头痛剧烈时常出现强直性痉挛或因脑疝形成而死亡。由于长期颅内压增高病人出现视力减退,小儿可有头颅的增大,叩之呈“破壶音”。 2.局灶症状局灶症状或称为定位体征,当肿瘤体积较小未压迫或未侵犯周围脑组织时不产生任何定位体征。由于肿瘤的不断生长对各不同部位的周围脑结构产生压迫或破坏,而出现各种不同的脑损害症状和体征。肿瘤可累及内囊、基底节,也可向脑实质内生长,从而病人出现半身或单肢型的瘫痪和感觉障碍,以及病灶对侧较轻的中枢性面瘫,同向性偏盲等。如果左侧颞、顶、枕交界区受到侵犯,病人将出现失认及失语症。脑室周围组织受累及所产生的临床症状的严重程度常随颅内压力的变化而变化。当颅内压严重升高时,症状变得明显,颅内压下降时可暂时得到缓解。