DNA virus and oncolgoy
- 格式:pdf
- 大小:433.08 KB
- 文档页数:15
【非细胞生物全系列—05】病毒—双链DNA病毒(上)作者:[美]Robert G.Webster当当病毒—双链DNA病毒(上)非细胞生物病毒双链DNA病毒双链DNA病毒(dsDNAvirus),这类病毒通常只有在进入宿主细胞核之后才能进行自我复制。
除此之外,这类病毒还需要宿主细胞核内的DNA聚合酶才能完成自我复制,因此它们很大程度上受宿主细胞的细胞周期影响。
有效的感染与子代的产生都需要在宿主细胞进行复制时才能进行,因为病毒所利用的核内DNA聚合酶在此时是活跃的。
此类病毒有可能诱发细胞快速裂解,导致细胞转变和癌变,如疱疹病毒、腺病毒和乳头多瘤空泡病毒。
1.DNA病毒脱氧核糖核酸病毒(英语:DNA virus)又称DNA病毒,其遗传物质为DNA,分为双链DNA病毒、单链DNA病毒两大类。
(1)特征DNA病毒,又名脱氧核苷酸病毒,即病毒核酸是DNA的一种生物病毒,属于一级病毒。
DNA病毒广泛存在于人、脊椎动物、昆虫体内以及多种传代细胞系中,每种病毒只能感染一种动物(个别例外),仅少数致病。
DNA由脱氧核苷酸组成的大分子聚合物。
脱氧核苷酸由碱基、脱氧核糖和磷酸构成。
其中碱基有4种:腺嘌呤(A)、鸟嘌呤(G)、胸腺嘧啶(T)和胞嘧啶(C)。
DNA 分子结构中,两条多脱氧核苷酸链围绕一个共同的中心轴盘绕,构成双螺旋结构。
脱氧核糖-磷酸链在螺旋结构的外面,碱基朝向里面。
两条多脱氧核苷酸链反向互补,通过碱基间的氢键形成的碱基配对相连,形成相当稳定的组合。
脱氧核糖核酸(DNA)是生物细胞内携带有合成RNA和蛋白质所必需的遗传信息的一种核酸,是生物体发育和正常运作必不可少的生物大分子。
DNA中的核苷酸中碱基的排列顺序构成了遗传信息。
该遗传信息可以通过转录过程形成RNA,然后其中的mRNA通过翻译产生多肽,形成蛋白质。
在细胞分裂之前,DNA复制过程复制了遗传信息,这避免了在不同细胞世代之间的转变中遗传信息的丢失。
在真核生物中,DNA存在于细胞核内称为染色体的结构中。
【产品推荐】新冠病毒相关蛋白和抗体来源:菲恩生物发布时间:2022-01-20 13:48 点击量:133自从2019年爆发新冠疫情以来,病毒已经出现了很多变异株,那么为什么新冠病毒会不断出现新变异株?新冠病毒是一个RNA病毒,而RNA病毒在病毒复制过程中普遍具有较高的突变频率。
即使冠状病毒具有一定的纠错功能,病毒的突变频率也大约有百万分之三左右,换个说法就是,每次病毒复制产生的新病毒中,每10个病毒中就可能会有一个病毒出现突变。
因此,新突变株的出现对于新冠病毒来说是一个正常现象。
2021年11月9日,南非首次从病例样本中检测到一种新冠病毒B.1.1.529变异株。
短短2周时间,该变异株即成为南非豪登省新冠感染病例的绝对优势变异株,增长迅猛。
11月26日,WHO将其定义为第五种“关切变异株”(variant of concern, VOC),取名希腊字母Ο(奥密克戎)变异株。
世卫组织根据危险程度将新冠变异毒株分成了两类:令人担忧的变异毒株(VOC,variant of concern)和值得关注的变异毒株(VOI,variant of interest)。
前者在世界范围内引发的病例多、范围广,并有数据证实其传播能力、毒性强,或导致疫苗和临床治疗有效性降低;后者在世界范围内确认出现社区传播病例,或在多个国家被发现,但尚未形成大规模传染。
目前,VOC是对疫情影响最大同时也是对全球威胁最大的变异毒株,包括:Alpha、Beta、Gamma和Delta、omecoron五种。
上图为5种变异株的氨基酸突变位点比较南非疫情应对与创新中心主任奥利维拉表示,B.1.1.529存在“不同寻常的突变群”,共有50个突变,刺突蛋白上有32个突变。
美国全国公共广播电台称,Omicron的突变数量是德尔塔病毒的两倍之多。
COVID-19 Genomics UK Consortium(COG-UK)公司的SARS-CoV-2基因组团队发布了Omicron变体32个突变(左)的新图像。

![[讲座]埃博拉病毒、流感病毒与人类的健康](https://uimg.taocdn.com/1be5b60d866fb84ae45c8daf.webp)
DNA疫苗的作用机制高晓佩;管晓燕;白国辉;刘建国【摘要】BACKGROUND: In 1990, Wolff et al. reported that DNA was examined as a gene therapy tool, and emerged as a promising therapy after observations that simple injection of naked plasmid DNA and RNA led to profound transgene expression in vivo.DNA vaccines are recognized for harboring several distinguishing characteristics and advantages (including low cost, ease and rapidity of manufacturing, and stability) making them a method for addressing global health threats in the future. OBJECTIVE: To review the status and research progress of DNA vaccines in the view of mechanism of action: innate immune signaling from bacterial DNA, transfecting somatic cell by DNA vaccines, cross-presentation and cross-activation, transfecting antigen presenting cells by DNA vaccines, and apoptosis. METHODS: The first author retrieved the databases of PubMed and CNKI for the articles concerning DNA vaccines published between January 2000 and June 2017 using the keywords of "DNA vaccine, gene vaccine, plasmid DNA, cross-presentation, transfection, apoptosis"in English and Chinese, respectively. A total of 105 literatures were searched, and 47 eligible articles were included in accordance with the inclusion criteria. RESULTS AND CONCLUSION: The immunogenicity of DNA vaccines in humans has been limited by low expression levels of antigen, in comparison with the conventional protein vaccines in the past two decades. Studies on the mechanism of action of DNA vaccines in terms ofantigen-presenting cell types able to cross-present DNA-encoded antigens, the activation of innate immune responses due to DNA itself and induction of cell apoptosis have suggested the opportunities to increase the immunogenicity of these vaccines.%背景:1990年Wolff 等发现将RNA和DNA表达载体直接注射小鼠骨骼肌,可以检测到相应的蛋白表达,这揭示DNA可以直接用于疾病的治疗和免疫,基因疗法和DNA疫苗应运而生.随着近年来的研究发展, DNA 疫苗迅速显示出了几个显著特点(包括低成本、生产制造的简单便捷、及稳定性),使其成为未来解决全球卫生问题的最有前景的方法之一.目的:从来自细菌DNA 的先天免疫信号、DNA 疫苗直接转染组织细胞、交叉激活和交叉呈递机制、DNA疫苗直接转染APCs及细胞凋亡机制5个方面综述DNA疫苗的作用机制.方法:第一作者通过电子计算机检索2000年1月至2017年6月为止PubMed数据库及CNKI中国期刊全文数据库收录的与 DNA 疫苗有关的文献.英文检索词"DNA vaccine、gene vaccine、DNA plasmid、cross-presentation、transfection、apoptosis",中文检索词"基因疫苗、DNA疫苗、DNA质粒、交叉呈递、细胞凋亡、细胞转染",总计得到中英文文献105篇,47篇文献符合标准.结果与结论:在DNA疫苗发展的20多年里,研究人员发现人类DNA疫苗与传统蛋白疫苗相比,只能获得有限的抗体表达水平.在DNA疫苗作用机制中DNA转染组织细胞或者专职抗原呈递细胞、专职抗原呈递细胞交叉激活及交叉呈递DNA编码的抗原,同时DNA激活先天的免疫应答、诱导细胞凋亡,基于这些理论的研究为将来改善DNA疫苗的免疫效果提供理论支持.【期刊名称】《中国组织工程研究》【年(卷),期】2018(022)008【总页数】6页(P1281-1286)【关键词】DNA疫苗;基因疫苗;DNA质粒;作用机制;交叉激活;组织构建;细胞凋亡【作者】高晓佩;管晓燕;白国辉;刘建国【作者单位】遵义医学院口腔医学院,贵州省遵义市 563099;遵义医学院口腔医学院,贵州省遵义市 563099;贵州省普通高等学校口腔疾病研究特色重点实验室遵义市口腔疾病研究重点实验室,贵州省遵义市 563006;贵州省普通高等学校口腔疾病研究特色重点实验室遵义市口腔疾病研究重点实验室,贵州省遵义市 563006;遵义医学院口腔医学院,贵州省遵义市 563099;贵州省普通高等学校口腔疾病研究特色重点实验室遵义市口腔疾病研究重点实验室,贵州省遵义市 563006【正文语种】中文【中图分类】R3180 引言 IntroductionDNA疫苗是编码抗原或抗原表位来构建的封闭环状DNA质粒[1]。
细菌和病毒英文作文Bacteria and Viruses: Microscopic Entities with Macroscopic Impact.In the vast and intricate universe of microbiology, bacteria and viruses occupy a unique and fascinating niche. These microorganisms, though invisible to the naked eye,play a crucial role in the functioning of our planet andits inhabitants. From the soil to the human body, theyexist in various environments, sometimes beneficial and sometimes causing harm. Understanding their nature, functions, and interactions with their hosts is crucial for comprehending the delicate balance of life on Earth.Bacteria are single-celled microorganisms that canexist independently or in symbiosis with other organisms. They are diverse, ranging from harmful pathogens that cause diseases like cholera and tuberculosis to beneficial probiotics that aid in digestion and immune system function. Bacteria have a wide range of shapes and sizes, from rod-like bacteria called bacilli to spiral-shaped bacteria known as spirochetes. They reproduce rapidly through a process called binary fission, allowing them to adapt and thrive in various environments.On the other hand, viruses are much smaller than bacteria and consist of genetic material (DNA or RNA) surrounded by a protective protein shell. Unlike bacteria, viruses cannot replicate independently; they need to infect a host cell and hijack its machinery to produce more viruses. Viruses can infect a wide range of hosts, from animals to plants and even bacteria. Some viruses, like the influenza virus, can cause mild to severe illness, while others, such as the HIV virus, can lead to chronic andlife-threatening conditions.The impact of bacteria and viruses on human health is immense. Bacterial infections can range from minor skin infections to life-threatening sepsis, while viral infections can cause respiratory diseases, gastroenteritis, and even neurological disorders. The study of these microorganisms has led to the development of antibiotics,vaccines, and other therapeutic agents that have revolutionized medicine and saved millions of lives.However, the rise of antibiotic-resistant bacteria and the constant threat of new and emerging viruses pose significant challenges to global health. The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has highlighted the urgent need for more research and innovation in the field of microbiology. The development of new drugs, vaccines, and diagnostic tools is crucial for combating these microbial threats and safeguarding the health of future generations.Beyond human health, bacteria and viruses also play a crucial role in the environment. Bacteria help in the decomposition of organic matter, nutrient cycling, and the production of essential compounds like vitamins. They are also essential for the functioning of soil and aquatic ecosystems. On the other hand, viruses can affect the population dynamics of bacteria and other microorganisms, maintaining the balance of ecological systems.In conclusion, bacteria and viruses are fascinating and complex microorganisms that have a profound impact on our lives. They exist in every corner of the planet,interacting with and influencing the functioning of ecosystems, including our own bodies. The study of these microorganisms continues to yield valuable insights into the mechanisms of life and disease, leading to the development of new therapies and strategies for promoting health and well-being. As we face the challenges of antibiotic resistance and new microbial threats, it is crucial to invest in research and education to ensure a sustainable and healthy future for all.。
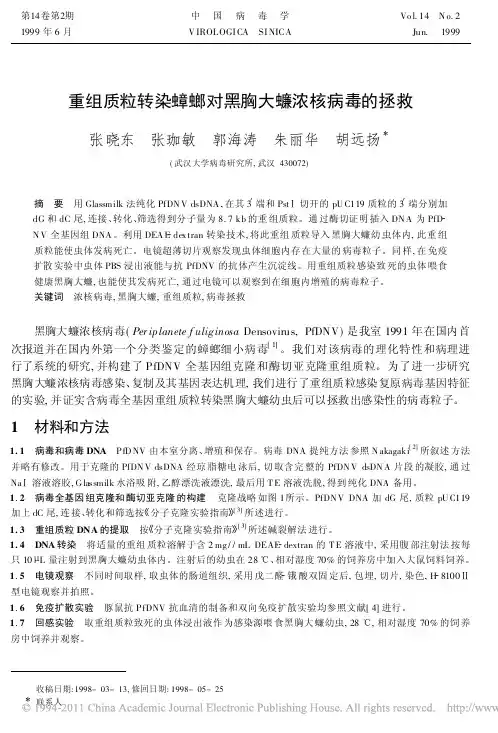
重组质粒转染蟑螂对黑胸大蠊浓核病毒的拯救张晓东 张珈敏 郭海涛 朱丽华 胡远扬(武汉大学病毒研究所,武汉430072)摘 要 用Glassmilk法纯化PfDN V dsDNA,在其3 端和Pst 切开的pU C119质粒的3 端分别加dG和dC尾,连接、转化、筛选得到分子量为8.7kb的重组质粒。
通过酶切证明插入DN A为PfDN V全基因组DNA。
利用DEA E dex tran转染技术,将此重组质粒导入黑胸大蠊幼虫体内,此重组质粒能使虫体发病死亡。
电镜超薄切片观察发现虫体细胞内存在大量的病毒粒子。
同样,在免疫扩散实验中虫体PBS浸出液能与抗PfDNV的抗体产生沉淀线。
用重组质粒感染致死的虫体喂食健康黑胸大蠊,也能使其发病死亡,通过电镜可以观察到在细胞内增殖的病毒粒子。
关键词 浓核病毒,黑胸大蠊,重组质粒,病毒拯救黑胸大蠊浓核病毒(Per ip lanete f uliginosa Densovirus,PfDNV)是我室1991年在国内首次报道并在国内外第一个分类鉴定的蟑螂细小病毒[1]。
我们对该病毒的理化特性和病理进行了系统的研究,并构建了PfDNV全基因组克隆和酶切亚克隆重组质粒。
为了进一步研究黑胸大蠊浓核病毒感染、复制及其基因表达机理,我们进行了重组质粒感染复原病毒基因特征的实验,并证实含病毒全基因重组质粒转染黑胸大蠊幼虫后可以拯救出感染性的病毒粒子。
1 材料和方法1.1 病毒和病毒DNA P fD NV由本室分离、增殖和保存。
病毒DNA提纯方法参照N akagaki[2]所叙述方法并略有修改。
用于克隆的PfDN V dsDNA经琼脂糖电泳后,切取含完整的PfDN V dsDN A片段的凝胶,通过Na 溶液溶胶,G lassmilk水浴吸附,乙醇漂洗液漂洗,最后用T E溶液洗脱,得到纯化DNA备用。
1.2 病毒全基因组克隆和酶切亚克隆的构建 克隆战略如图1所示。
PfDN V DNA加dG尾,质粒pU C119加上dC尾,连接、转化和筛选按 分子克隆实验指南 [3]所述进行。
dna病毒的讲解我们很多人都知道dna是一种遗传性的物质,那么你们知道dna病毒码,今天就为大家讲一种病毒,就是dna病毒,其实在生活中我们不经常遇到dna病毒,我们甚至都不知道dna病毒的存在,那么dna病毒到底是一种什么样的病毒呢DNA病毒是生物病毒的一种,属于一级病毒。
本病毒广泛存在于人、脊椎动物、昆虫体内以及多种传代细胞系中,每种病毒只能感染一种动物(个别例外),仅少数致病。
繁殖:是专性活细胞内寄生物。
它不可单独进行繁殖,必须在活细胞内才可。
繁殖方式:复制。
繁殖过程:吸附(病毒粒子借衣壳上的受体与宿主细胞“粘附”在一起,否则,病毒粒子将不能侵入宿主细胞。
)注入遗传物质, 接着就是利用寄主细胞的营养进行DNA的复制和蛋白质的翻译,然后就是装配,最后就释放.DNA病毒很少,基本上都是RNA病毒,噬菌体,天花病毒,花椰菜花叶病毒等。
对DNA检测,一个是定量检测,另外还有一个是基因分形和耐药的变异,定性检测比定量要求高。
还有定量的问题,强调用干扰素和核苷类似物进行抗病毒治疗,无论是哪一种药物的治疗,病毒的滴度和阴转都是考核抗病毒治如何疗的硬性指标,所以这项检测指标是非常重要的,而且在很多药物治疗过程中,乙肝病毒DNA下降的速度和幅度对于抗病毒治疗应达的疗效具有重要的预测价值。
对乙肝病毒进行基因分形和耐药变异问题测定,比如说有的病人服药之后从阴性转成阳性,还有乙肝病毒DNA的升高,这样的病人我们要充分重视是否产生了耐药变异,这个检测对医生更换药物或者更换治疗方案是非常有关系的。
乙肝病毒DNA阳性说明体内有活性病毒的复制,所有这样的病人都要进行治疗。
是否进行治疗主要取决于当时的转氨酶水平是正常还是升高的,如果是转氨酶升高,特别是转氨酶在80以上,400以内,这样的病人是非常适合抗病毒治疗的。
转氨酶水平是一个重要的指标,有人说乙肝病毒DNA阳性、转氨酶正常的病人是不是都不需要治疗呢?如果这么较真的话,我们要对这部分病人进行肝组织活检。
日本从鲑鱼科鱼中分离出一种新病毒
李凯年
【期刊名称】《畜牧兽医科技信息》
【年(卷),期】1996(000)011
【摘要】最近,日本从其北部养殖的一些鲑科鱼的脑和卵巢液中分离出一种以前未介绍过的病毒。
这种病毒分离自幼鱼和成鱼,病鱼表现异常的游水动作和没有生气。
在5—25℃下,该病毒复制,引起细胞病变作用和易感细胞系溶解。
在一些鱼细胞系中见有持续感染。
该病毒颗粒有包膜,形状为20面体,直径为80nm,有一个中心电
子稠密核心。
该病毒用IUdR和BVdU复制,感染细胞中的包涵体可被吖啶橙染色。
该病毒密度为1.155g/ml,病毒RNA长度为7.3kb。
该
【总页数】1页(P4-4)
【作者】李凯年
【作者单位】
【正文语种】中文
【中图分类】S941
【相关文献】
1.日本科学家从微型藻类中分离出抗高血压肽 [J], 汪开治
2.日本从番鸭中分离出鹅细小病毒 [J], 黄安国
3.日本从可燃冰中分离出天然气 [J],
4.韩国科学家从进口辐射松原木中分离出12种长喙壳科真菌 [J], 汪开治
5.从感染传染性皮下组织和造血器官坏死病毒的对虾中分离到一种新病毒 [J], Yuanan Lu;陈怀青
因版权原因,仅展示原文概要,查看原文内容请购买。
病毒基因英语作文In the realm of biology, viruses are fascinating entitiesthat challenge our understanding of life. They are not considered living organisms by all definitions, as they cannot reproduce on their own and must hijack a host cell to replicate. However, their genetic material is a topic of great interest and study.Viruses possess genetic material in one of two forms: DNA or RNA. DNA viruses, such as the herpes virus, have a double-stranded DNA that is similar to the genetic material of their host cells. This similarity allows them to integrate their genetic material into the host's genome and remain dormant until activated.RNA viruses, on the other hand, like the influenza virus, have single-stranded RNA. Their genetic code is more prone to mutation, which is why these viruses can evolve rapidly and develop resistance to treatments. The RNA can be either positive-sense (+RNA), which can be directly translated into proteins, or negative-sense (-RNA), which requires an intermediate step to create a positive-sense RNA strand.The process of viral replication is a complex interaction between the virus and the host cell. Once inside the cell, the virus releases its genetic material, which then uses the host's cellular machinery to produce more viral particles. This process can lead to the destruction of the host cell, asit is overwhelmed by the production of viral components.Understanding the genetic makeup of viruses is crucial for developing vaccines and antiviral drugs. By targetingspecific genes or proteins essential for viral replication, scientists can create treatments that inhibit the virus's ability to infect and reproduce. For example, the development of vaccines for the human papillomavirus (HPV) has been successful due to the detailed knowledge of its DNA structure and the proteins it expresses.Furthermore, the study of viral genetics has led to the discovery of bacteriophages, viruses that infect bacteria. These bacteriophages have been found to have diverse genetic material and can be engineered to target specific bacteria, offering a potential alternative to antibiotics in the fight against antibiotic-resistant bacteria.In conclusion, the genetic makeup of viruses is a cornerstone of virology. It not only helps us understand how viruses function and evolve but also provides the foundation for developing strategies to combat viral infections. As we continue to unravel the mysteries of viral genetics, we gain a deeper appreciation for the intricate dance between viruses and their hosts, and the potential to harness this knowledge for the betterment of human health.。
病毒分类表国际微生物学会联合会(International Union of Microbiological Societies,IUMS)病毒学组设立的国际病毒分类委员会(The International Committee on Taxonomy of Viruses,ICTV)制定了《国际病毒分类与命名原则》(The International Code of Virus Classification and Nomenclature)。
病毒及类病毒的分类阶元(taxon)的规则简述如下:目:病毒的目以“-病毒目”(-virales)为词尾;科:病毒的科以“-病毒科”(-viridae)为词尾,类病毒的科以“-类病毒科”(-viroidae)为词尾;亚科:病毒的亚科以“-病毒亚科”(-virinae)为词尾;属:病毒的属以“-病毒属”(-virus)为词尾,类病毒的属以“-类病毒属”(-viroid)为词尾;种:病毒的种病毒分类不使用界、门、纲这几个阶层。
根据病毒的基因组组成及复制方式,病毒分为如下几类:•病毒(Viruses)o DNA病毒(DNA Viruses)▪第一组:双链DNA病毒(Group I:dsDNA Viruses)▪第二组:单链DNA病毒(Group II:ssDNA Viruses)o RNA病毒(RNA virus)▪第三组:双链RNA病毒(Group III:dsRNA Viruses)▪第四组:正链RNA病毒(Group IV:(+)ssRNA Viruses)▪第五组:负链RNA病毒(Group V:(-)ssRNA Viruses)o DNA与RNA逆转录病毒(DNA and RNA Reverse Transcribing Viruses)▪第六组:RNA逆转录病毒(GroupVI: RNA Reverse TranscribingViruses)▪第七组:DNA逆转录病毒(GroupVII: DNA Reverse TranscribingViruses)•亚病毒因子(Subviral Agents)o卫星(Satellites)o类病毒(Viroids)o朊毒体(Prions)也可以根据病毒的细胞生物宿主,分为“细菌病毒”、“真菌病毒”、“植物病毒”、“无脊椎动物病毒”、及“脊椎动物病毒”。
新近Cyclovirus的发现与研究近期,一种新的病毒——Cyclovirus,被科学家们发现并引起了研究者们广泛的关注。
这种病毒被发现在人类和其他动物身上,并且似乎能引起一些疾病。
Cyclovirus是一种环状病毒,它的基因组相当小,只有其他病毒的一小部分。
这种病毒被发现于2013年,当时科学家们正在研究何谓代表常见疾病的气喘。
他们发现,在气喘患者体内找到了Cyclovirus的存在。
随后,一系列的研究表明这种病毒在常见病和严重疾病的发展中起着至关重要的作用。
其中包括人类的心肌炎、肝病、以及如兔子病毒病等动物疾病。
此外,科学家们还发现,Cyclovirus不同于其他病毒,它的生命周期、菌株和特点均有所不同。
Cyclovirus的研究进展如何?科学家们目前已经意识到,Cyclovirus在人类和动物的身上都存在,且可能与一些疾病有关联。
但这种病毒的病理生理基础还需要进一步研究。
近年来,越来越多的有关病理生理基础的研究开始浮出水面。
这种病毒传播的方式还不完全清楚,但科学家们认为它可能通过空气或者其他途径传播,需要更多的研究。
目前,已有许多的实验室致力于Cyclovirus的研究,他们设法从多个样本中分离出了这种病毒,并且研究人员们正试图在动物和人类中重现Chyclovirus感染。
但由于缺乏足够的病例数量,这一过程变得异常困难。
关于Cyclovirus的前景,研究者们表示相当乐观。
首先,掌握所以事实并逐渐认识这种病毒的行为及其潜在的反应得以加速。
其次,Cyclovirus也有着理想的特点,这将使得在实验条件下满足众多要求变得容易。
最终,Cyclovirus的研究对于新型肺炎等疾病的研究也会起着积极的作用。
众多研究者们已经走上前线,将持续密切关注Chyclovirus的研究和发现,以寻求提供优异抗病毒性能的新药物改进方案,确保社会大众的健康和安全。
Mini-reviewDNA viruses in human cancer:An integrated overview on fundamental mechanisms of viral carcinogenesisDeilson Elgui de Oliveira*Department of Pathology,Botucatu School of Medicine,State University of Sao Paulo (UNESP),BrazilReceived 5January 2006;received in revised form 17May 2006;accepted 18May 2006AbstractThe first experimental data suggesting that neoplasm development in animals might be influenced by infectious agents were published in the early 1900s.However,conclusive evidence that DNA viruses play a role in the pathogenesis of some human cancers only emerged in the 1950s,when Epstein–Barr virus (EBV)was discovered within Burkitt lymphoma cells.Besides EBV,other DNA viruses consistently associated with human cancers are the hepatitis B virus (HBV),human pap-illomavirus (HPV),and Kaposi sarcoma herpesvirus (KSHV).Although each virus has unique features,it is becoming clearer that all these oncogenic agents target multiple cellular pathways to support malignant transformation and tumor development.Ó2006Elsevier Ireland Ltd.All rights reserved.Keywords:Viral carcinogenesis;DNA viruses;Cancer;Epstein–Barr virus;Kaposi’s sarcoma-associated virus;Human papillomavirus;Simian Virus 40virus;Hepatitis B virus1.IntroductionIn 1908,Vilhelm Ellermann and Oluf Bang,two Danish pathologists doing research on leukemia in chickens,provided important evidence that malig-nant tumors in animals could be caused by the so-called ‘‘filterable agents’’[1].Three years later,Peyton Rous reported that another avian malignan-cy,a sarcoma developing in Plymouth Rock fowls,could be readily reproduced by inoculating cell-free tumor extracts in healthy animals [2].The ‘‘filterable agents’’are now recognized as retroviruses,and many others associated withtumors in a variety of animals were discovered in the last century.Because human tumors were not believed to be contagious,the first studies on viral carcinogenesis were received with skepti-cism.Additionally,the putative infectious neo-plasms of chickens were not considered to be valid models for analogous human diseases.More-over,in 1907Ciuffo reported that benign tumors could be,in fact,transmissible among humans [3].The debate about the association of infectious agents with human tumors remained in a ‘‘latent state’’until 1964,when the Epstein–Barr virus (EBV)was discovered within malignant cells from Burkitt lymphoma (BL)[4].In 1990,it was estimated that 15.6%of cancer inci-dence (about 1,450,000cases)would be associated0304-3835/$-see front matter Ó2006Elsevier Ireland Ltd.All rights reserved.doi:10.1016/j.canlet.2006.05.010*Fax:+551438152348.E-mail address:elgui@.Cancer Letters 247(2007)182–196/locate/canletwith microbial and parasitic agents[5].Developing countries have higher incidences of virus-induced cancers,which can actually represent a remarkable public health issue.Besides its epidemiological rele-vance,as elegantly stated previously,‘‘viral carcino-genesis provided the breakthroughs that crystallized current concepts of cancer development,and revealed mechanisms for the orchestration of normal cell growth control’’[6].Here,we aim to review the state-of-art of DNA virus-induced carcinogenesis,focusing on major concerns addressed in the literature.The role of RNA viruses in human carcinogenesis has been dis-cussed elsewhere[6].2.Cancer in briefThe term cancer encompasses a great variety of entities,many with unique etiology,pathogenesis, natural history,treatment response,and cure rates. According to Hanahan and Weinberg,most cancers are seldom self-sufficient in growth stimuli;they become insensitive to anti-growth signals;they are capable of causing tissue invasion(and few will be able to cause metastasis as well);their proliferative potential is unrestricted,they cause sustained angio-genesis locally,and their cells are resistant to apop-tosis.Noteworthy,these‘‘hallmarks of cancers’’are present in variable degrees in different diseases con-sidered,among different cases of the same cancer, and even in a given malignant tumor after time[7].When transformed cells develop into malignant tumors,they have already had acquired some of the above-mentioned hallmarks,which will be strengthened during tumor progression.Besides, new features will be acquired,and malignant tumors will become more heterogeneous and aggressive as a consequence.Interestingly,some of the above fea-tures are also required for efficient viral replication, and few viruses become very skilled in providing them to infected cells.As these features impair cell stability and tissue homeostasis,infection by onco-genic viruses offers a prone-to-transformation sce-nario,in which the development of a malignant tumor is likely to happen or,at least,it is boosted.3.DNA viruses in human cancerTo date,few DNA viruses are consistently asso-ciated with human neoplasms,notably the hepatitis B virus(HBV),human papillomavirus(HPV),EBV, and Kaposi sarcoma herpesvirus(KSHV).General information about these pathogens is provided in Table1.Chronic infection with HBV is an important risk factor for development of hepatocellular carcinoma, a malignant tumor frequently observed in some countries of Asia and Africa[16].On the other hand,specific HPV genotypes are responsible for benign neoplasms and some carcinomas,including cancer of uterus[17],some penile and upper aerodi-gestive tract carcinomas[18,19].Major achieve-ments in the prevention of virus-induced cancers may be attributable to strategies to control infection in human populations.For instance,HBV vaccina-tion has dramatically decreased the number of hepa-tocellular carcinomas,and it is expected that a new HPV vaccine will have a profound impact on the prevention of cervical cancer[20],and perhaps a sig-nificant decrease in other HPV-related neoplasms.EBV and KSHV are members of the Herpesviridae family of viruses,which encompass many of the most complex animal viruses described so far.Both can establish long-term viral infections in theirTable1DNA viruses with well-documented association with human cancersVirus Viral taxonomy Discovery Genome Associated human cancers Review Hepatitis B virus Hepadnaviridae1967[8,9]dsDNA(partial)3.2kb,4genesHepatocellular carcinoma[10]Human papillomavirus Papillomaviridae1983[11]DsDNA8kb Squamous cell carcinomas in anogenitaland head and neck sites[12]Epstein–Barr virus/ human herpesvirus4Herpesviridae(gammaherpesvirus;lymphocryptovirus)1964[4]DsDNA172kb,90genesBurkitt lymphoma,undifferentiatednasopharyngeal carcinoma,Hodgkinlymphoma,non-Hodgkin lymphoma inimmunosuppressed patients[13]Kaposi sarcoma-associated herpesvirus/human herpesvirus8Herpesviridae(gammaherpesvirus;radnovirus)1994[14]DsDNA165kb,90genesKaposi sarcoma,primary effusionlymphoma,[15]D.Elgui de Oliveira/Cancer Letters247(2007)182–196183target cells.EBV is the most important etiological factor in classic BL,and it is also detected in undif-ferentiated nasopharyngeal carcinomas(NPC)[21], in a subset of Hodgkin lymphomas(HL),and in some cases of non-Hodgkin lymphomas,notably in immunosuppressed patients[22].Few other puta-tive associations between EBV infection and human cancers are currently under evaluation[23].On the other side,in the last10years much effort has been devoted to the study of KSHV,the last human DNA tumor virus identified so far.KSHV is now consistently detected in all forms of Kaposi sarcoma (KS),in HIV-positive primary effusion lymphomas (PEL),and in Multicentric Castleman disease (MCD)[24].Despite the lack of conclusive data about other DNA tumor viruses in the development of human cancers,studies on adenoviruses and two small DNA viruses,the simian virus40(SV40)and poly-omaviruses,have been providing fundamental information to clarify the molecular mechanisms of virus-induced cell transformation.Adenoviruses are widespread in the human population,and the infection is often asymptomatic.However,it may cause respiratory illnesses in children,conjunctivitis, and gastroenteritis.More than50serotypes of human adenoviruses have been described,but none is consistently associated with cancer in humans. However,few human adenoviruses do cause malig-nant tumors in rodents(e.g.,Ad12,Ad18,and Ad31),and their oncogenic properties rely on two main viral genes:E1A,which disrupts the function of important tumor suppressing proteins,and E1B,which inhibits apoptosis in many different ways[25].SV40and the polyomavirus,on the other hand, usually infect monkeys and mice,respectively. Because cells from SV40or polyomaviruses natural hosts are very permissive to the lytic viral cycle,they are not transformed during infection.However,in non-permissive or semi-permissive animal cells,the expression of viral products–namely the large T antigen of SV40and the middle T antigen of poly-omaviruses–can be sufficient to produce malignant cells.In fact,SV40may transform humanfibro-blasts in vitro,and it was demonstrated that this virus also transforms human mesothelial cells[26]. The association between SV40infection and the development of pleural mesotheliomas is currently under debate due to conflicting data in the literature [27–29].Noteworthy,important epidemiological evidence that the virus at least act as a co-factor in the development of asbestos-associated human mesotheliomas has recently emerged[30].It is not surprising that thefirst successful attempt to convert human normal cells into pheno-typically malignant ones with a minimum set of genetic elements employed components of a DNA virus(namely,SV40-encoded proteins),in addition to the H-RAS oncogene and the hTERT gene, which encodes the catalytic subunit of human telo-merase[31].As will be discussed in the following sections,DNA tumor viruses developed many dif-ferent strategies to control key cellular processes, including cell proliferation,differentiation,cell sig-naling,senescence,and apoptosis(Fig.1).4.Viral infection and genetic instabilityGenetic instability is one of the foremost charac-teristics shared by cancers,observed either at the chromosomal or gene levels in malignant cells. Chromosomal imbalances,namely aneuploidy,have long been detected in malignant cells using conven-tional microscopy and karyotyping.On the other hand,a lesson has been taken from studies on inher-ited cancer syndromes in which dysfunction of DNA-repair genes causes genome-wide mutational events.Whether gene mutations or aneuploidy is the leading phenomenon in carcinogenesis remains an unsolvable dilemma,since both play a variable role in the development of different cancers.Lately,aneuploidy has caught more attention due to new data suggesting that it could be one of the earliest events in the development of some inher-ited as well as sporadic cancers.Aneuploidy itself was proposed as the leading gear in the genetic instability engine[32].In this regard,disruption of the mitotic spindle apparatus may be responsible for the establishment of chromosomal imbalances, which allows further mutations in critical genes to happen.Noteworthy,chromosomal abnormalities are well-known consequences of telomere dysfunc-tion,and it seems that,at least in some cancers,neo-plastic cells experience a variable period of telomere shortening before they become immortal.This results in progressive genetic instability,which becomes more and more severe after cell transfor-mation.The genetic instability also plays a role in tumor progression,providing cell heterogeneity that allows the emergence of malignant clones that have acquired advantageous features,such as low nutri-ent demand,auto-sufficiency in growth signals,high proliferation rate,low immunogenicity,etc.184 D.Elgui de Oliveira/Cancer Letters247(2007)182–196HPV-infected cells from precancerous lesions of the cervix often show aberrant mitotic figures [33].The HPV E7oncoprotein from high-risk HPV genotypes contributes to the induction of genomic instability by inducing centrosome duplication errors [34].Interestingly,recurrent gains of 3q were observed in cervical and vaginal mucosa during the transition of high-risk HPV-associated severe dys-plasia to invasive carcinoma [35].HBV X protein is responsible for a similar mechanism of genetic instability:it causes the formation of abnormal cen-trioles,followed by multipolar mitosis and chromo-somal imbalances,which are assumed consequences of crm1sequestration,a nuclear export protein that keeps proper centrosome synthesis and segregation [36].Additionally,DNA tumor viruses cause genetic instability other than aneuploidy.For instance,HPV E6protein downregulates the enzyme O 6-methylguanine-DNA methyltransferase (MGMT),which participates in DNA repair and prevents mutation in many critical genes,including TP53[37].On the other hand,HBV X protein was found to interact with XAP-1/UVDDB,a putative DNA-repair protein that binds damaged DNA during nucleotide excision repair (NER)[38].In time,EBV LMP-1protein inhibits DNA repair in both p53-deficient and p53-competent cells,and H1299p53-deficient epithelial cells expressing LMP-1are more sensitive to UV radiation and bleomycin,two important DNA-damaging agents [39].Fig.1.Overview of some critical cellular pathways and cellular proteins targeted by known human DNA oncoviruses.Multiple cellular processes are modified by viral products before malignant transformation takes place.For instance,infected cells may become genetically instable over time because viral proteins interfere with DNA repair,cause unattended cell cycle progression or disrupt the mitotic spindle.Besides,imbalance towards antiapoptotic signals by oncoviruses makes infected cells resistant to death,and stabilization of telomeres provides them limitless replicative potential.Altogether,these phenomena favor the development and progression of virus-associated cancers.Refer to text for more details.D.Elgui de Oliveira /Cancer Letters 247(2007)182–1961855.Cell immortalization by DNA virusCell immortalization is another pivotal phenom-enon in carcinogenesis,also one of the major char-acteristics shared by malignant neoplasms.In order to produce malignant tumors,cells must have to bypass apoptosis deflagrated during cell crisis, the endpoint of cellular senescence,observed when a critical level of telomere shortening is reached. Moreover,major mechanisms that grant an increased lifespan to malignant cells are related to telomere maintenance and suppression of apoptosis, which will be discussed later.Most human cancer cells have their telomeres lengthened by de novo expression of telomerase,an enzymatic complex formed by three major compo-nents:an RNA template of telomeric repeats (TTAGGG in vertebrates),the telomerase-associated protein(hTep-1),and a catalytic subunit that shows reverse transcriptional activity–the human telome-rase reverse transcriptase(hTert).Expression of TERT gene is rate limiting for telomerase activity, which is usually restricted to stem cells and germinal cells in non-neoplastic tissues.The RNA component is expressed constitutively and ubiquitously in nor-mal cells.Besides telomerase reactivation,telomeres may be subjected to the alternative lengthening of telomeres(ALT)pathway,a recombination-based mechanism for telomere lengthening.Although ALT activation may not share the same frequency of telomerase de novo expression during cancer development,ALT has gained considerable atten-tion due its anticipated role on cancer resistance to the new generation of drugs that target telomerase activity[40,41].EBV has long been recognized for its ability to produce B-lymphoblastoid cell lines(BLCL)with increased lifespan in vitro.The virus uses the CD21transmembrane protein(C3d complement receptor)to infect B-lymphocytes,which allow both lytic and latent viral cycles.A subset of BLCL that has become immortalized by EBV in vi-tro is named post-immortal BLCL.EBV-infected BLCL generated from patients with accelerated ageing due to Werner’s Syndrome(WS)display impaired telomeres dynamics and fail to become immortalized[42].On the other hand,expression of WRN gene,which encodes the Wrn DNA heli-case(which is non-functional in WS),is often verified in post-immortal EBV-infected BLCL. Therefore,active Wrn DNA helicase,which seems to work along telomerase for telomere lengthening,seems to be required for immortalization of EBV-infected BLCL[43].It was proposed that EBV plays a role in the pathogenesis of classical BL because it causes intense proliferation of infected B cells,which remains unnoticed due to impaired immune surveil-lance.Immunological dysfunction has been attributed to Plasmodium infection in BL cases arising in the so-called Malaria belt area in Equatorial Africa. This scenario is favorable to accumulation of genetic abnormalities,including the t(8;14)translo-cations,which are frequently found in BL[44,45]. They cause juxtaposition of c-myc proto-oncogene (located on8q24)to one of the immunoglobulin heavy chain genes loci at14q.Consequently, EBV-infected B cells disclose upregulation of c-myc oncoprotein,and auto-sustained cell-prolifer-ation signals.Interestingly,it was previously reported that c-myc cooperates with the ubiquitous transcrip-tion factor Sp1to enhance TERT expression[46]. Indeed,telomerase activity is increased in nasopha-ryngeal carcinomas(NPC),and it can be achieved in vitro in NPC cells via c-myc transactivation by EBV latent membrane protein1(LMP-1)[47]. Additionally,increased telomerase activity in NPC cell lines may be due to LMP-1-mediated nuclear translocation of the reverse transcriptase subunit of human telomerase bound to NF-j B [48].KSHV,on the other hand,transforms primary human endothelial cells in vitro,and only KSHV-infected cell cultures express telomerase,as accessed by the telomeric-repeat amplification protocol (TRAP)[49].The KSHV latency-associated nuclear antigen1(LANA-1)binds Sp1to form a complex with an increased transcriptional activity in vivo. The LANA-1/Sp1complex transactivates the TERT promoter,thus contributing to telomere elongation and consequent cell immortalization due to increased telomerase expression in KSHV-infected cells[50].In the context of HPV-associated malignancies, Zhang et al.evaluated the size of telomeres in cells from cervical pre-neoplastic lesions from16patients with high-risk HPV infection in a sequential fash-ion.Telomere shortening was predominantly found in early cervical intraepithelial neoplasia(CIN), whereas TERT expression was more evident in high grade CIN and invasive cervical carcinomas.These observations strongly suggest that cell immortaliza-tion and the acquisition of a malignant phenotype are closely associated phenomena,and indicate that186 D.Elgui de Oliveira/Cancer Letters247(2007)182–196the progressive genetic instability acquired during the telomere erosion phase in precancerous lesions may enhance the transformation of high-risk HPV-infected cervical cells[51].In the last decade,it was demonstrated that the HPV-16E6protein induces TERT expression in human foreskin keratinocytes(HFK)[52].This abil-ity was originally described as independent of E6-mediated p53degradation.However,when HPV E6and E7oncoproteins are co-expressed in HFK cells,although they do show telomere losses,they still bypass crisis and become immortal.In a recent paper,McMurray and McCance[53]demonstrated that,regardless of telomerase activity,degradation of p53by HPV E6protein is a key event for immor-talization of keratinocytes in the presence of HPV E7.The combination of p53dominant negative mutant with HPV E7alone successfully produced immortalized cells,stressing the role of p53dysfunc-tion in this phenomenon[53].Although HPV-16-infected keratinocytes had their lifespan extended by E6alone,pRb/p16INK4a inactivation is required in addition to TERT expres-sion for cells to become immortal[54].Interestingly, it seems that even such immortalized keratinocytes retain growth and differentiation control[55]. Therefore,although virus-induced cell immortaliza-tion provides the necessary progressive genetic instability that drives the acquisition of a malignant phenotype,additional oncogenic events are often needed(e.g.,activation of protoncogenes and inac-tivation of other tumor suppressor genes driven by the progressive genetic instability),in order for immortalized cells to transform.6.DNA virus-induced malignant transformationThe expression of many proteins encoded by tumor suppressor genes is known to be critical for the maintenance of genomefidelity and regulation of cell signaling and proliferation.When critical genes are disrupted,or became abnormally activated (e.g.,tumor suppressor genes and protoncogenes, respectively),the defective cells may evade biologi-cal security systems that avoid the emergence of transformed clones.Although difficult to be identified in vivo,transformed cells are characterized in vitro by low nutrient demand,morphological changes,high and unrestricted proliferation rate, anchorage-independent growth,and eventually tumorigenesis and metastasis capabilities,which can be assessed in animal models.It seems reasonable that,during their evolutionary interaction with host cells,DNA tumor viruses whose products could target some key cellular regulatory proteins achieved an important adaptative advantage over those that could not.In this regard,many differ-ent strategies for inhibition of p53tumor suppressor protein have been identified in DNA tumor viruses so far.Noteworthy,p53was discovered in co-precip-itation experiments with the SV40large T antigen [56].Inactivation of p53-dependent pathways in virus-infected cells may have many consequences, notably unchecked cell cycle progression,progressive genetic instability and resistance to apoptosis.E6proteins from high-risk HPV genotypes(e.g., HPV-16and HPV-18)cause proteasomal degrada-tion of p53,but E6proteins from low-risk geno-types(e.g.,HPV-6and HPV-11)fail to do it efficiently.High-risk HPV E6proteins form a com-plex with the E6-AP protein,a member of the E3 family of ubiquitin ligases that only binds p53when it is associated with HPV E6.The E6/E6-AP com-plex drives p53to ubiquitin-mediated degradation, thus decreasing functional levels of p53in the infected cell[57].Additional cell transformation properties of high-risk HPV E6proteins rely on their ability to target host PDZ domain-containing proteins for degradation[58].On the other hand, the retinoblastoma gene(RB)product(pRb), another important tumor suppressor protein,is also targeted by HPV E7proteins.The HPV E7protein disrupts pRb control over E2F proteins,an impor-tant family of transcription factors,allowing the activation of cyclin–CDK complexes,which ulti-mately causes unrestricted cell progression through-out G1to S phases of the cell cycle[52].The p53protein is also targeted by KSHV pro-teins LANA1and LANA2.The former is constitu-tively expressed in spindle-shaped cells of KS,as well as in latently infected endothelial cells and monocytes.The latter have a more stringent expres-sion profile,and it was described as a B-cell-specific latent viral protein[59].LANA-1represses p53 transcriptional activity,and inhibits the p53-depen-dent cell death in different KSHV-infected cell types. However,this effect is caused neither by modifica-tions in p53DNA-binding properties nor by protein degradation[60].On the other hand,suppression of p53activity by LANA-2confers increased survival of B cells,and this mechanism has a suspected role in KSHV-induced lymphomagenesis[53].Contrary to the above mentioned,EBV oncopro-teins do not seem to interact directly with tumorD.Elgui de Oliveira/Cancer Letters247(2007)182–196187suppressor proteins.In fact,EBV nuclear antigen2 (EBNA-2),which is critical for EBV-induced immortalization of B-lymphocytes,upregulates wild-type(wt)p53through the activation of NF-j B transcription factor,and this effect can be achieved by EBNA-2alone or in combination with LMP-1[61].Such upregulation of wt p53may have different consequences in vivo,since it was demon-strated that its levels in EBV-infected BL cells deter-mine whether they would be impelled to unrestricted proliferation,cell cycle arrest or apoptosis[62].In addition to their unique viral oncoproteins,a set of KSHV and EBV products shares variable structural and functional similarities with human cell proteins.Interestingly,herpesviral genes that encode cellular homologues generally do not con-tain intronic sequences,which suggests that they were potentially acquired from host cells with the participation of mRNA intermediates,and perhaps retroviral cooperation[63].Another possibility is that some viral products acquired a variable,usually low,degree of similarity with human proteins by means of functional and structural convergence dur-ing evolution.From our knowledge,this hypothesis has not been properly addressed yet.In the past years,the viral mimicry of key cellular proteins(usually referred to as‘‘molecular piracy’’) provided many valuable insights into the mecha-nisms of viral carcinogenesis.For instance,it was demonstrated that the sole constitutive expression of the KSHV G protein-coupled receptor gene (v-GPCR)in an engineered transgenic mouse model (but none of other KSHV genes that encode onco-proteins,including v-cyclin,v-flip,and kaposin) promotes the formation of vascular tumors in vivo which resemble KS lesions in humans[64].Interest-ingly,v-GPCR was recognized as a lytic cycle gene, raising new questions about the importance of de novo expression of lytic genes in virus-induced carci-nogenesis,as well as the putative role of these genes in early phases of cancer development.It was later reported that the v-GPCR-mediated sarcomagenesis could be dramatically affected by drugs which inhibit the Akt-signaling pathway,prompting new promising strategies for treatment of KS[65].The role of viral homologues of cellular proteins will be discussed further in the following sections.In time,it has been recently reported that the EBV and KSHV genomes encode micro RNAs (miRNAs)that may have important cellular genes as targets for silencing during latent infection[66, 67].These very promisingfindings open a new mechanistic perspective of viral participation in malignant transformation,since the downregulation of critical regulatory proteins in infected cells might, in part,be explained by viral miRNAs activity.7.Viral control of apoptosisApoptosis is crucial for tissue homeostasis.Cell number in tissues is primarily dependent on cell pro-liferation and cell death by apoptosis.Both phenom-ena are usually dysfunctional in malignant tumors.The two main mechanisms of apoptosis converge at the level of activation of effector caspases.The first mechanism that causes caspase activation is triggered when apoptotic ligands(e.g.,Fas ligand and TNFs)bind to their receptors on the cell surface (CD95and TNFR,respectively).The death domains in the intracytoplasmatic portion of these receptors activate caspase8and initiate the caspase cascade.Moreover,this pathway is triggered by extrinsic signals.On the other hand,the second pathway is triggered by intrinsic signals,including telomere overshortening,DNA damage,disruption of mitochondrial membrane,etc.Ultimately,they cause cytochrome c release from mitochondria and the formation of the apoptosome complex,which proteolytically activates downstream caspases. Caspases are responsible for most of the phenomena observed in the apoptotic cell,including chromatin cleavage,breakdown of structural nuclear and cyto-skeleton proteins,membrane changes,cell shrinkage and cell fragmentation into apoptotic bodies,etc. Activation and function of these cysteine-rich enzymes are tightly regulated by different mecha-nisms,including post-translational modifications and direct inhibition by a family of inhibitory apop-totic proteins(IAPs).An alternative apoptotic cas-pase-independent pathway is described,and it is based on the release of apoptosis-inducing factor (AIF),a mitochondrial oxyreductase that causes DNA cleavage and chromatin condensation when it translocates to the cell nucleus[68].Although EBV-infected BCBL are sensitive to apoptosis due to the scarcity of serum and growth factors in culture,actually they seem to be more resistant than antigen-stimulated primary B-lym-phocytes.In EBV latently infected cells,LMP-1is an important factor that confers resistance to apop-tosis.It has recently been reported that LMP-1 inhibits apoptosis of infected B-lymphocytes partly due to the inhibition of antiapoptotic BAX gene [69].EBV LMP-1mimics a constitutively activated188 D.Elgui de Oliveira/Cancer Letters247(2007)182–196。