病理考试名词解释与简答题最全
- 格式:pdf
- 大小:3.67 MB
- 文档页数:16
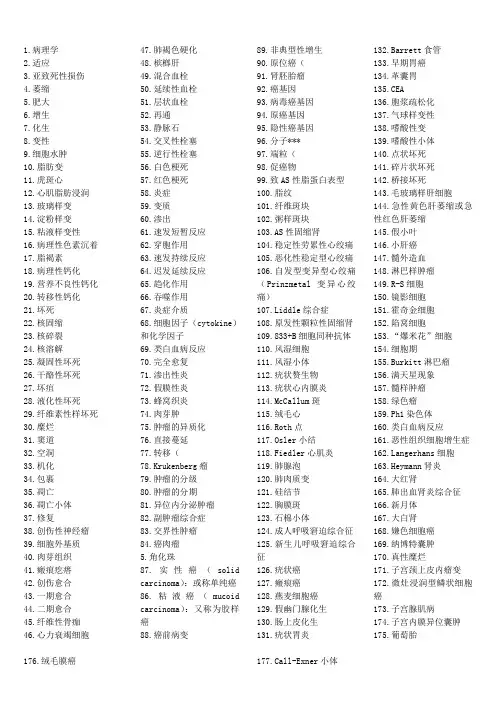
1.病理学2.适应3.亚致死性损伤4.萎缩5.肥大6.增生7.化生8.变性9.细胞水肿10.脂肪变11.虎斑心12.心肌脂肪浸润13.玻璃样变14.淀粉样变15.粘液样变性16.病理性色素沉着17.脂褐素18.病理性钙化19.营养不良性钙化20.转移性钙化21.坏死22.核固缩23.核碎裂24.核溶解25.凝固性坏死26.干酪性坏死27.坏疽28.液化性坏死29.纤维素性样坏死30.糜烂31.窦道32.空洞33.机化34.包裹35.凋亡36.凋亡小体37.修复38.创伤性神经瘤39.细胞外基质40.肉芽组织41.瘢痕疙瘩42.创伤愈合43.一期愈合44.二期愈合45.纤维性骨痂46.心力衰竭细胞47.肺褐色硬化48.槟榔肝49.混合血栓50.延续性血栓51.层状血栓52.再通53.静脉石54.交叉性栓塞55.逆行性栓塞56.白色梗死57.红色梗死58.炎症59.变质60.渗出61.速发短暂反应62.穿胞作用63.速发持续反应64.迟发延续反应65.趋化作用66.吞噬作用67.炎症介质68.细胞因子(cytokine)和化学因子69.类白血病反应70.完全愈复71.渗出性炎72.假膜性炎73.蜂窝织炎74.肉芽肿75.肿瘤的异质化76.直接蔓延77.转移(78.Krukenberg瘤79.肿瘤的分级80.肿瘤的分期81.异位内分泌肿瘤82.副肿瘤综合症83.交界性肿瘤84.癌肉瘤5.角化珠87.实性癌(solidcarcinoma):或称单纯癌86.粘液癌(mucoidcarcinoma):又称为胶样癌88.癌前病变89.非典型性增生90.原位癌(91.肾胚胎瘤92.癌基因93.病毒癌基因94.原癌基因95.隐性癌基因96.分子***97.端粒(98.促癌物99.致AS性脂蛋白表型100.脂纹101.纤维斑块102.粥样斑块103.AS性固缩肾104.稳定性劳累性心绞痛105.恶化性稳定型心绞痛106.自发型变异型心绞痛(Prinzmetal变异心绞痛)107.Liddle综合症108.原发性颗粒性固缩肾109.833+B细胞同种抗体110.风湿细胞111.风湿小体112.疣状赘生物113.疣状心内膜炎114.McCallum斑115.绒毛心116.Roth点117.Osler小结118.Fiedler心肌炎119.肺腺泡120.肺肉质变121.硅结节122.胸膜斑123.石棉小体124.成人呼吸窘迫综合征125.新生儿呼吸窘迫综合征126.疣状癌127.瘢痕癌128.燕麦细胞癌129.假幽门腺化生130.肠上皮化生131.疣状胃炎132.Barrett食管133.早期胃癌134.革囊胃135.CEA136.胞浆疏松化137.气球样变性138.嗜酸性变139.嗜酸性小体140.点状坏死141.碎片状坏死142.桥接坏死143.毛玻璃样肝细胞144.急性黄色肝萎缩或急性红色肝萎缩145.假小叶146.小肝癌147.髓外造血148.淋巴样肿瘤149.R-S细胞150.镜影细胞151.霍奇金细胞152.陷窝细胞153.“爆米花”细胞154.细胞期155.Burkitt淋巴瘤156.满天星现象157.髓样肿瘤158.绿色瘤159.Ph1染色体160.类白血病反应161.恶性组织细胞增生症ngerhans细胞163.Heymann肾炎164.大红肾165.肺出血肾炎综合征166.新月体167.大白肾168.嫌色细胞癌169.纳博特囊肿170.真性糜烂171.子宫颈上皮内瘤变172.微灶浸润型鳞状细胞癌173.子宫腺肌病174.子宫内膜异位囊肿175.葡萄胎176.绒毛膜癌177.Call-Exner小体178.前列腺特异性抗原179.硬化性腺病180.小叶原位癌181.APUD细胞,APUD瘤182.Simond综合征183.Sheehan综合征184.纤维性甲状腺炎185.许特尔细胞瘤186.砂粒体187.嗜铬细胞瘤188.沃-弗189.卫星现象190.噬神经细胞现象191.鬼影细胞192.PrP病193.缺血性脑病194.层状坏死195.Verocay小体196.神经原纤维缠结197.Hirano小体198.结核结节199.原发综合征200.开放性愈合201.结核瘤202.干性结核性胸膜炎203.伤寒细胞204.髓样肿胀期205.凹空细胞206.隐性梅毒207.树胶样肿208.白色肺炎209.Kaposi肉瘤210.嗜酸性脓肿211.假结核结节212.象皮肿213.干线性肝硬化214.腊样变性215.阿米巴肿216.含铁小结217.无反应性结核218.肿瘤219.肿瘤的实质220.肿瘤的间质221.肿瘤的异型性222.间变223.间变性肿瘤224.肿瘤的演进225.癌脐226.心内膜下心肌梗死227.心肌纤维化228.高血压脑病229.细支气管230.呼吸性细支气管231.小气道232.慢性阻塞性肺病233.慢性支气管炎234.肺气肿235.继发性颗粒固缩肾236.VonHippel-Lindan(VHL)病237.腹膜假粘液瘤238.迟发性神经原死亡239.软脑膜癌病240.老年斑241.含铁血黄素1.:是一门研究疾病的病因、发病机制、病理改变(包括代谢、机能和形态结构的改变)和转归的医学基础学科。
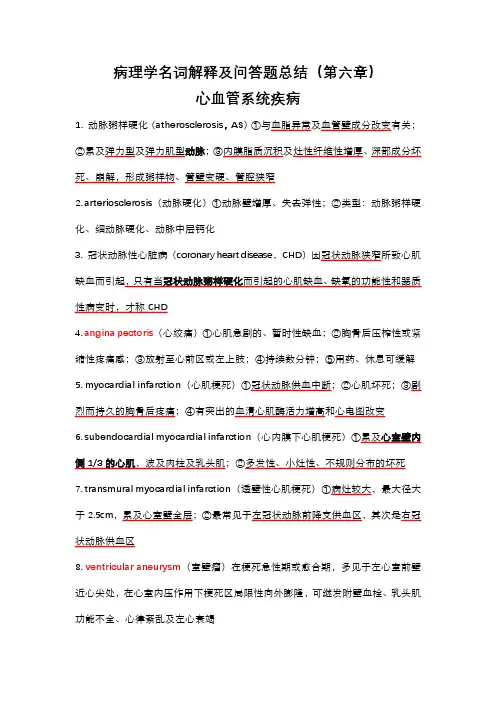
病理学名词解释及问答题总结(第六章)心血管系统疾病1. 动脉粥样硬化(atherosclerosis,AS)①与血脂异常及血管壁成分改变有关;②累及弹力型及弹力肌型动脉;③内膜脂质沉积及灶性纤维性增厚、深部成分坏死、崩解,形成粥样物、管壁变硬、管腔狭窄2. arteriosclerosis(动脉硬化)①动脉壁增厚、失去弹性;②类型:动脉粥样硬化、细动脉硬化、动脉中层钙化3. 冠状动脉性心脏病(coronary heart disease,CHD)因冠状动脉狭窄所致心肌缺血而引起,只有当冠状动脉粥样硬化而引起的心肌缺血、缺氧的功能性和器质性病变时,才称CHD4. angina pectoris(心绞痛)①心肌急剧的、暂时性缺血;②胸骨后压榨性或紧缩性疼痛感;③放射至心前区或左上肢;④持续数分钟;⑤用药、休息可缓解5. myocardial infarction(心肌梗死)①冠状动脉供血中断;②心肌坏死;③剧烈而持久的胸骨后疼痛;④有突出的血清心肌酶活力增高和心电图改变6. subendocardial myocardial infarction(心内膜下心肌梗死)①累及心室壁内侧1/3的心肌,波及肉柱及乳头肌;②多发性、小灶性、不规则分布的坏死7. transmural myocardial infarction(透壁性心肌梗死)①病灶较大,最大径大于2.5cm,累及心室壁全层;②最常见于左冠状动脉前降支供血区,其次是右冠状动脉供血区8.ventricular aneurysm(室壁瘤)在梗死急性期或愈合期,多见于左心室前壁近心尖处,在心室内压作用下梗死区局限性向外膨隆,可继发附壁血栓、乳头肌功能不全、心律紊乱及左心衰竭9. 冠状动脉性猝死(sudden coronary death)①多见于男性青、壮年;②常在某种诱因作用下或在睡眠中发病;③发病后迅速死亡;④冠状动脉病变及相应心肌病变10. primary hypertension(原发性高血压)①原因未明;②体循环动脉血压持续升高;③独立性全身性疾病;④基本病变为全身细动脉和肌性小动脉硬化;⑤常引起心、脑、肾和眼底病变11. concentric hypertrophy of heart(心脏向心性肥大)①压力性负荷增加;②左心室代偿性肥大;③心腔不扩张,甚至略缩小12. hypertensive encephalopathy(高血压脑病)①高血压患者;②脑血管病变及痉挛,血压骤升;③中枢神经系统功能障碍:头痛、呕吐、视力障碍及意识模糊;④脑水肿或伴点状出血13. accelerated hypertension(急进型高血压)①多见于青中年;②血压显著升高,舒张压常>17.3kPa(130mmHg);③病变进展迅速,病变:增生性小动脉硬化和细动脉纤维蛋白样坏死;④较早出现肾衰竭14. aneurysm(动脉瘤)指动脉壁因局部病变(薄弱或结构破坏)而向外膨出,形成永久性的局限性扩张,常见于弹性动脉及其主要分支。
植物病理学名词解释-简答题一、名词解释1.病状:植物得病后本身所表现的病态。
病征:病原物在植物病部表现出的特征性结构体。
症状:植物生病后的不正常表现。
病原:引起植物发病的原因。
2.喷菌现象在徒手切片中看到有大量细菌从病部喷出,这种现象称为喷菌现象(bacteria exudation,BE) 。
为细菌病害所特有,是区分细菌病害和其它病害的最简便的手段之一。
3.钝化温度(Thermal lnactivation Point,TIP) 将病组织汁液处理10min使病毒丧失活性的最低温度,用摄氏度表示。
4.病害循环病害循环(disease cycle) 也称作侵染循环(infection cycle):5.整体产果(Holocarpic)。
低等真菌繁殖时, 营养体全部转为繁殖体时叫整体产果分体产果(Eucarpic)。
高等真菌繁殖时, 营养体部分转为繁殖体时叫分体产果。
6.系统侵染:7.综合防治综合防治(综合治理IPM)(植物病害管理PDM):从农业生产的全局和农业生态系的总体观念出发,根据有害生物和环境之间的相互关系,充分发挥自然控制因素的作用,因地制宜地协调应用生物的、物理的、化学的等必要措施,将有害生物控制在经济损害允许水平之下,以获得最佳的经济、生态和社会效益。
同时要把防治过程中可能产生的有害副作用减少到最低限度。
8.局部侵染:系统侵染:9生理小种(Physiological race) :指在种内或变种内或专化型内,在形态上没有差异,但生理特性(培养性状、生理生化、病理、致病力或其他特性)有差异的生物型或生物型群。
9.单分体病毒;10侵染性病害:病原生物侵染植物引起的病害非侵染性病害:由植物自身及非生物因素引起的植物病害。
11、同宗配合:单个菌株生出的雌雄性器官能交配,自身亲合,如卵菌。
异宗配合: 异宗配合:同一菌株上生出的雌雄性器官不能交配,必须和另一有亲和力菌株上的才能交配,担子菌以此为主(接合、子囊两种方式都有)。
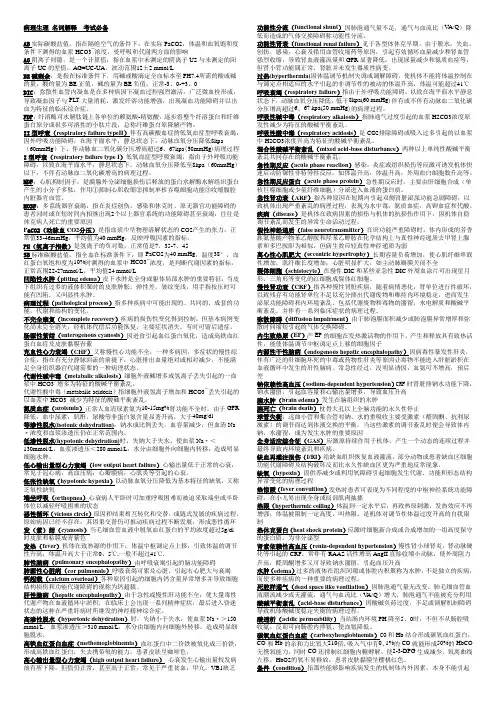
病理生理名词解释考试必备AB实际碳酸盐值,指在隔绝空气的条件下,在实际PaCO2,体温和血氧饱和度条件下测得的血浆HCO3¯浓度,受呼吸和代谢两方面的影响AG阴离子间隙,是一个计算值,指在血浆中未测定的阴离子US与未测定的阳离子UC的差值。
AG=UC-UA,波动范围12±2 mmol/LBE碱剩余,是指在标准条件下,用碱或酸滴定全血标本至PH7.4所需的酸或碱的量,酸的量为BE正值,碱的量为BE负值,正常-3、0-+3、0DIC:弥散性血管内凝血是在多种病因下凝血过程强烈激活,广泛微血栓形成,导致凝血因子与PLT大量消耗,激发纤溶功能增强,出现凝血功能障碍并以出血为特征的临床综合症。
FDP:纤溶酶可水解肽链上各单位的赖氨酸-精氨酸,逐步将整个纤溶蛋白和纤维蛋白原分成很多可溶性的小肽片段,总称纤维蛋白原降解产物。
II型呼衰(respiratory failure typeII)伴有高碳酸血症的低氧血症型呼吸衰竭,因外呼吸功能障碍,在海平面水平,静息状态下,动脉血氧分压降低8kpa(60mmHg)下,伴动脉血二氧化碳分压增高超过6、67kpa(50mmHg)病理过程I型呼衰(respiratory failure type I)低氧血症型呼吸衰竭,指由于外呼吸功能障碍,以致在海平面水平,静息状态下,动脉血氧分压降低至8kpa(60mmHg)以下,不伴有动脉血二氧化碳增高的病理过程。
MDF:心肌抑制因子,是胰腺外分泌细胞损伤后释放的蛋白水解酶水解组织蛋白产生的小分子多肽,作用①抑制心肌收缩②抑制单核吞噬细胞功能③收缩腹腔内脏器官血管。
MOSF:多系统器官衰竭,指在炎症创伤,感染和休克时,原无器官功能障碍的患者同时或在短时间内相继出现2个以上器官系统的功能障碍甚至衰竭,往往是休克病人死亡的重要原因P aCO2(动脉血CO2分压)是指血浆中呈物理溶解状态的CO2产生的张力,正常值33-46mmHg,平均值为40 mmHg,反映呼吸因素的指标。
1化生:为适应环境变化,一种已分化组织转变为另一种分化组织的过程。
2坏死:以溶酶性变化为特点的活体内局部组织中细胞的死亡3凋亡:是指机体细胞在某些因素作用下,通过细胞内基因及其产物的调控而发生的一种程序性的细胞死亡。
4肉芽组织:是新生的富含毛细血管的幼稚阶段的纤维结缔组织,由纤维母细胞、毛细血管及一定数量的炎性细胞等有形成分组成的。
栓塞:在循环血液中出现的不溶于血液的异常物质,随血流运行阻塞5血栓:在活体的心血管内,血液发生凝固或血液中某些有形成分析出、凝集形成固体质块的过程。
形成的固体质块称为血栓。
6梗死:局部组织因血流中断引起的缺血性坏死7、肉芽肿:炎症局部巨噬细胞及其衍生物增生形成境界清楚的结节状病灶为特征。
8异型性:无论在瘤细胞形态还是在组织学结构上,肿瘤都与其来源的正常组织有不同程度的差异,这种差异性称为异型性。
(反映了肿瘤分化程度)9:癌前病变:指具有癌变潜在可能性的病变,这些病变长期存在有可能转变为癌。
-10、假小叶:是肝硬化的特征性病变,是指由广泛增生的纤维在组织将原来的肝小叶和再生的肝细肝细胞团。
11、结核结节:是在细胞免疫的基础上形成的,由于上皮样细胞、朗格汉斯细胞加上外周局部聚集的淋巴细胞和少量反应性增生的纤维母细胞构成。
12、原发综合征:肺的原发病灶、淋巴管炎和肺门淋巴结结核称为~13风湿小体:风湿性肉芽肿,也称阿少夫小体。
多见于心肌间质、心内膜下及皮下结缔组织,是一种肉芽肿型病变,形状略呈梭行形。
镜下中心见纤维素样坏死,周围有Aschoff细胞,外周有少量淋巴细胞、浆细胞浸润。
心衰细胞: 左心衰竭肺淤血时,有些巨噬细胞吞噬了红细胞并将其分解,胞浆内形成含铁血黄素,此时这种细胞称为心力衰竭细胞。
又称心衰细胞。
15. 原位癌(carcinoma in situ):原位癌一般指粘膜鳞状上皮层内或皮肤表皮层内的重度非典型增生几乎*累及或累及上皮的全层(上皮内瘤变Ⅲ级)但尚未侵破基底膜而向下浸润生长者。
一、名词解释(10题,每题3分,共计30分)1. 蜂窝织炎2. 脓细胞3. 疖4. 毒血症5. 肉芽肿6. 泡沫细胞7. 假小叶8. 空洞9. 大叶性肺炎10. 硅肺二、单项选择(30题,每题1分,共计20分)1.当尿路梗阻,尿液在肾盂中潴留,引起肾体积增大、肾实质变薄,称为A. 变性B. 肥大C. 萎缩D. 增生2.细胞内或间质中出现异常物质或正常物质显著增多,称为A. 代偿B. 适应C. 肥大D. 变形3.关于凋亡的叙述,下列哪项是错误的?A. 是基因调控的程序化细胞死亡B. 凋亡细胞核固缩、核染色质边集C. 凋亡细胞周围可有巨噬细胞存在D. 凋亡细胞周围可有中性粒细胞存在4.病毒性肝炎点状坏死后再生属于A. 完全再生B. 不完全再生C. 纤维性修复D. 瘢痕性修复5.完成瘢痕修复的物质基础是A. 上皮组织B. 肉芽组织C. 纤维蛋白网架D. 毛细血管网6.临床上一次抽取腹水量不能过大,是为了防止A. 静脉性充血B. 减压性充血C. 心力衰竭D. 肺淤血7.槟榔肝的典型病变是A. 肝小叶结构破坏B. 肝细胞坏死C. 门静脉分支扩张淤血D. 肝血窦扩张淤血,肝细胞脂肪变性8.血液从血管或心腔逸出,积聚在体腔内,称A. 出血B. 内出血C. 外出血D. 破裂性出血9.关于白色血栓的叙述,哪像不正确?A. 多发生在血流缓慢的心瓣膜上B. 多见于静脉血栓的起始部C. 不易脱落引起远端血管栓塞D. 主要由血小板和少量纤维蛋白组成10.血栓转归中不会发生的是A. 钙化B. 溶解C. 化生D. 机化11.至少多少毫升的空气一次性进入机体静脉就可以导致患者猝死A. 50B. 60C. 80D. 10012.男,14岁,右股深部巨大血管瘤,术后情况良好,伤口一期愈合。
拆线后下床活动5分钟后,突然晕倒,抢救无效死亡。
应考虑A. 脑血管意外B. 心肌梗死C. 脂肪栓塞D. 肺动脉栓塞13.易发生出血性梗死的器官是A. 心B. 肾C. 脾D. 肠14.贫血性梗死不常见于A. 脾梗死B. 肾梗死C. 心肌梗死D. 肺梗死15.下列哪一项不是炎症时实质细胞常出现的变质性变化?A. 细胞水肿B. 黏液变性C. 脂肪变性D. 凝固性坏死16.炎症时引起局部疼痛的主要因素是A. 炎症局部动脉扩张B. 炎症局部静脉阻塞C. 局部充血渗出D. 炎症渗出物和炎症介质的作用17.急性炎症时,组织变红的主要原因是A. 血管扩张,血流加速B. 炎症灶内血栓形成C. 炎性细胞浸润D. 组织间隙水肿18.炎症反应最重要的功能是A. 杀灭侵入人体的病原微生物B. 产生免疫反应C. 将炎性细胞输送到炎症灶D. 吞噬损伤因子19.不符合急性炎症时白细胞渗出叙述的是A. 白细胞黏附于血管内皮细胞是白细胞从血管游出的前提B. 游出血管外的白细胞可分泌胶原酶降解血管基底膜,进入周围组织C. 白细胞介素6具有阳性趋化作用D. 趋化因子通过与白细胞表面的特异性G蛋白偶联受体相结合而发挥作用20.急性蜂窝织炎的常见致病菌是A. 金黄色葡萄球菌B. 溶血性链球菌C. 大肠杆菌D. 多为混合感染21.浆液性炎常见于下列哪种疾病?A. 大叶性肺炎B. 小叶性肺炎C. 毒蛇咬伤D. 阑尾炎22.金黄色葡萄球菌感染最常引起A. 浆液性炎B. 化脓性炎C. 蜂窝织炎D. 脓肿23.炎症在局部蔓延时不会形成A. 糜烂B. 溃疡C. 瘘管D. 炎性假瘤24.对维持肿瘤生长起重要作用的肿瘤间质成分是A. 结缔组织B. 血管C. 淋巴细胞D. 间质细胞25.属于良性肿瘤的是A. 淋巴管瘤B. 精原细胞瘤C. Krukenberg瘤D. 黑色素瘤26.良性肿瘤对机体影响最大的因素是A. 生长部位B. 生长速度C. 组织来源D. 体积大小27.高分化鳞癌最典型的病理特点是A. 癌细胞核分裂象多见B. 形成癌巢C. 出现角化珠D. 细胞间可见细胞间桥28.动脉粥样硬化粥瘤的粥样物质的主要成分是A. LDLB. VLDLC. ox-LDLD. 胆固醇29.冠心病心肌梗死后肉眼能辨认病灶的最早时间是A. 1~2小时B. 4小时C. 5小时D. 6小时30.Mc Callum斑常见于A. 左心房后壁B. 左心房前壁C. 右心房D. 左心室三、简答题(4题,每题10分,共计40分)1 比较坏死和凋亡(20分)2. 简述胃良恶性溃疡的区别(12分)3.简述类白血病反应(8分)答案及评分标准一、名词解释(10题,每题3分,共计30分)1.蜂窝织炎:疏松结缔组织的弥漫性化脓性炎症,常发生于皮肤肌肉和阑尾。
病理生理学重点名词解释与简答题(Key terms of pathophysiology Interpretation and brief answer)First, the noun explanationThe basic pathological process: mainly refers to a variety of diseases may occur, common, complete sets of functions, metabolism and structural changes.Health: health means not only sickness or illness, but also a complete, physical, mental, and social state of being.Disease: disease is under certain conditions caused by the cause of damage, due to the body's self regulatory disorder and the occurrence of abnormal life process.Etiology: a cause of disease that is characteristic of the disease and is known as the cause of the disease.Incentives: factors that contribute to the development of disease are called triggers.Brain death (brain death): the permanent cessation of the function of the organism as a whole is a permanent loss of the function of the brain. At present, the standard of brain death above the foramen magnum is generally used.Hypotonic dehydration: also called hyponatremia of low volume, characterized by losing Na+ more than dehydration, serum Na+ concentration <130mmol/L, plasma osmotic pressure <280mmol/L, accompanied by a decrease in extracellular fluid volume.Hypertonic dehydration: also known as low volume hypernatremia, characterized by more water loss than loss of Na+, serum Na+ concentration of >150mmol/L, plasma osmolality, >310mmol/L, extracellular fluid volume and extracellular fluid volume are reduced.Water intoxication: high solubility hyponatremia, characterized by decreased serum sodium, serum Na+ concentration, <130mmol/L, plasma osmotic pressure <280mmol/L, but the total body sodium is normal or increased, the patient has water retention, so that the volume of fluid increases significantly.Dehydration fever: because of the decrease of water from the skin, the heat is affected, leading to elevated body temperature, called dehydration fever.Edema: excessive fluid that is called edema in the interstitial space or inside the body cavity.Hyperkalemia: serum potassium levels are higher than 5.5mmol/LHypokalemia: serum potassium levels below 3.5mmol/L.Disturbance of acid-base balance: the excessive acid base overload, serious deficiency or regulatory disturbance caused by pathological conditions lead to the PH abnormal condition caused by the destruction of acid-base homeostasis in the environment.Metabolic acidosis: a type of acid-base disturbance characterized by an increase in extracellular fluid H+ or a primary decrease in HCO3- and a decrease in PH.Respiratory acidosis: a CO2 disorder or excessive intake causes a disturbance of acid-base balance characterized by a primary increase in plasma [H2CO3] and a decrease in PH.Metabolic acidosis: extracellular liquid increase or loss of H+, [HCO3-] in plasma increased and PH increased primaryacid-base disorders characterized by type.Respiratory alkalosis: a type of acid-base disturbance characterized by hyperventilation of the lungs and primary decrease in plasma [H2CO3] and elevated PH.Mixed acid-base disturbance: there are two or three simple types of acid-base disturbances in the same patient.Hypoxia (hypoxia): pathological changes in cellular metabolism, function, and morphological structure resulting from reduced oxygen supply or impaired oxygen use.Cyanosis (cyanosis): when the uniform concentration of deoxygenated hemoglobin in the blood capillary of more than 5g/dl, the skin and mucous membranes were purple.Type four hypoxia: hypoxia hypoxia, blood type hypoxia, circulatory hypoxia, tissue hypoxia.Enterogenous cyanosis: methemoglobinemia due to eating leadsto a large number of hemoglobin oxidation caused by.Shock: this word by Shock, and English shock, various strong risk factors acting on the body, the circulation decreased dramatically, tissue and organ perfusion of microcirculation is seriously insufficient, and systemic critical pathological process of vital organs function, metabolic disorder serious.MODS (multiple organ dysfunction syndrome): refers to the severe trauma, infection, shock, the original organ dysfunction of patients at the same time or within a short period of time have appeared more than two organ system dysfunction that homoiostasis must rely on clinical intervention to maintain syndrome.Systemic inflammatory response (SIRS): a systemic inflammatory response syndrome that results from uncontrolled, self sustained enlargement and self destruction caused by infection or non infectious agents acting on the body.Compensatory anti-inflammatory response syndrome (CARS): when an infection or trauma occurs, the organism produces an endogenous anti-inflammatory response that is associated with an increased immune response and an increased susceptibility to infection.DIC (disseminated intravascular bleeding): a role in the pathogenic factor, the coagulation system was activated and induced by micro thrombosis, or secondary fibrinolysis, resulting in bleeding, shock, organ dysfunction and microangiopathic hemolytic anemia in a pathological process.FDP fibrin degradation products: plasmin hydrolyze various fragments produced by Fbg and Fbn.Split cell: a special variant of the shape of red blood cells,Called schistocyte, shape, star, moon shaped helmet, referred to as the red cell debris. The fragment is high in brittleness and susceptible to hemolysis.Heart failure: cardiac pump dysfunction caused by various causes, and a negative or relatively reduced cardiac output that fails to meet the metabolic needs of tissue.Myocardial tension (muscle) derived dilatation:The source of expansion: reduce the myocardial tension due to stroke volume, the ventricular end diastolic volume increased, pre load led to the increase of the initial length of the muscle fibers increased, then enhance myocardial contractility, metabolism increases stroke volume, heart cavity enhanced myocardial contractility with this expansion called heart source expansion.Myogenic expansion: long-term volume overload and heart failure caused by dilated cardiomyopathy, mainly caused by excessive sarcomere stretch, the heart cavity enlargement, heart cavity with the excessive stretch and decreased myocardial contractility with expansion called myogenic expansion.Respiratory failure: a pathological process in which the arterial blood oxygen pressure is below normal and accompanied by or without elevated carbon dioxide partial pressure due to severe external respiratory dysfunction.Restrictive hypoventilation: alveolar ventilation caused by restricted expansion of the alveoli during inspiration. Obstructive hypoventilation: a ventilatory disorder caused by narrowing or obstruction of the airways.Functional shunt: part of alveolar ventilation lesions significantly reduced blood flow and weight, not less, even because of inflammatory hyperemia to increase blood flow (such as lobar pneumonia, early) ratio of alveolar minute ventilation and pulmonary blood flow per minute was significantly reduced, so that the flow through this part of alveolar venous blood without sufficient artery can mixed with arterial blood, the similar arteriovenous short circuit, called functional shunt, also known as blood doping.Dead space ventilation: under certain etiological factors, partial alveolar blood flow can be reduced, VA/Q can be significantly increased, less alveolar blood flow and ventilation, alveolar ventilation can not be fully utilized, become dead cavity like ventilation.Pulmonary encephalopathy: because of respiratory failure caused by brain dysfunction, patients can show a series of neuropsychiatric symptoms, such as directional, memory disorders, confusion, headache, drowsiness, coma and so on.ARDS (acute respiratory distress syndrome): respiratory dysfunction caused by alveolar capillary membrane injury caused by various reasons and the occurrence of acute respiratory failure syndrome clinical characteristics, is characterized by progressive dyspnea and hypoxemia.Hepatic encephalopathy: neuropsychiatric syndrome secondary to severe liver disease.False neurotransmitter: phenylethanolamine and octopamine in chemical structure and normal neurotransmitter norepinephrine and dopamine are similar, but can not complete the authenticity of neurotransmitter function, known as false neurotransmitter.Hepatorenal syndrome: acute renal tubular necrosis associated with functional renal failure and severe hepatitis in decompensated cirrhosis.Acute renal failure due to GFR decreased rapidly, or renal tubular degeneration and necrosis in a pathological process caused by acute severe, often oliguria, azotemia, hyperkalemia, metabolic acidosis and water intoxication syndrome.Chronic renal failure:Any disease of renal unit destruction, in the months and years or longer after the remaining nephron cannot fully remove metabolic waste and environment, thus to maintain the constant in the gradual emergence of metabolic waste retention and water electrolyte and acid-base balance disorders and renal endocrine dysfunction.The levels of non protein nitrogen (NPN) in blood, including uremia, creatinine, uric acid, and so on, are called azotemia. The NPN in normal blood is 25~35mg%, and the urea nitrogen is 10-15mg%.Renal hypertension: hypertension caused by renal parenchymal disease is called renal hypertension.Uremia: refers to acute or chronic renal failure to severe stage, metabolites and toxins accumulate in the body, water, electrolyte and acid-base balance disorders and some endocrine disorders caused by a series of systemic function and metabolic disorder syndrome.Two, Jane answer1. briefly describe the diagnostic criteria for brain deathAccording to the determination of brain death is the irreversible coma and brain response; second, stop breathing for 15 minutes, artificial respiration still no spontaneous breathing; the cranial nerve reflex; the pupil or fixed; the brain waves disappeared; the complete cessation of cerebral blood circulation (cerebral angiography).2. which type of dehydration is prone to loss of fluid shock? Why?Hyponatremia with low volume (hypotonic glue) is liable to cause fluid shock. (1) the extracellular fluid Bian through thepressure drop, no thirst, drinking water reducing. (2) the extracellular fluid Bian through pressure reduction, ADH reflex secretion decreased, no significant decrease in urine volume.(3) the extracellular fluid transferred to the intracellular fluid, and the extracellular fluid decreased further.3. to analyze the influence of water intoxication on the body.Extracellular fluid was diluted due to excessive water, so the blood sodium concentration decreased and osmotic pressure decreased. In addition, the kidney can not discharge too much water in time, the water is transferred to the relatively high osmotic pressure cells, causing edema. The result is that both the intracellular and external fluid volume are increased, and the osmotic pressure is decreased. Because the cell liquid capacity greater than the extracellular fluid retention capacity, so most of the moisture accumulation in the cells, therefore in mild water intoxication, interstitial water retention degree is still not enough to cause recessive edema of the concave. Acute water intoxication, the nerve cells in the brain edema and intracranial pressure, the cerebral symptoms appeared earliest and prominent, can occur in various neuropsychiatric symptoms, such as gaze, aphasia, confusion, lethargy, irritability and other directional arrhythmia, and papilloedema, severe cases can occur due to cerebral hernia caused by respiratory and cardiac arrest patients with mild, chronic or water poisoning is slow, symptoms are often not obvious, many covered by the symptoms and signs of primary disease, can have drowsiness, headache, nausea, vomiting,muscle spasms and pain symptoms such as weak and feeble.4. to discuss the mechanism of edema caused by imbalance of fluid exchange inside and outside the blood vessel.The force that drives the flow out of the intravascular fluid is the average effective hydrostatic pressure. The force that causes the fluid to flow back into the capillaries is effective colloid osmotic pressure. Normally, the tissue fluid is slightly larger than the reflux. Lymph reflux, tissue fluid reflux, the remaining part of the lymphatic system through the backflow into the blood circulation, normal adults in quiet state, enzyme hours about 120ml liquid through the lymphatic system into the blood circulation. The interstitial fluid increased hydrostatic pressure, and the rate of lymph formation was accelerated. In addition, the permeability of the lymphatic wall is higher and the protein is easy to pass. Therefore, lymph reflux can not only send a little more of the tissue fluid back into the body, but also the proteins that leak out of the capillaries, and the large molecules produced by cell metabolism absorb the circulation of the body. One or more of these factors at the same time or one after another disorders may be an important cause of edema.5. hypokalemia and hyperkalemia can cause muscle paralysis. What is the mechanism of this?Hypokalemia is mainly due to hyperpolarized block. The ratio of [K+ /[K+]e] the increase of hypokalemia, and muscle cell negative resting potential, the resting potential and threshold potential interval increases, cell excitability anddecreased, even not serious when excited, i.e. cells in the hyperpolarized state block. Hyperkalemia results in inactivation of the fast sodium channel because of the small resting potential of the skeletal muscle and is unable to be excited by extracellular depolarization.6. what kinds of acid-base disorders are caused by severe vomiting? To analyze the mechanism of its occurrence.Severe vomiting easily leads to metabolic alkalosis:H+ lost the gastric juice, the digestive tract of HCO3- H+ is not neutralized and absorbed into the blood; the loss of Cl- in gastric juice, can cause hypochloremic alkalisis; K+ lost the gastric juice, can cause hypokalemic alkalosis; the loss caused by a large amount of gastric juice, effective circulating blood volume reduction, secondary aldehyde solid ketone the increase caused by metabolic alkalosis.7. what types of acid-base disturbances can occur in the oliguria stage of acute renal failure? Why? What are the changes in the acid-base balance index?Can occur because of metabolic acidosis, renal function and acid alkali, in severe renal failure, can not be fixed in acid by urinary excretion, especially sulfuric acid and phosphoric acid accumulation in the body, resulting in the increase of H+ concentration HCO3- concentration decreased, due to reduced HCO3-, so AB, SB and BB significantly decreased. Negative BE increased, PH decreased by Paco2 secondary respiratory compensation, down AB<SB.8. what type of hypoxia can be caused by hemorrhagic shock?.Hemorrhagic shock, due to a large number of blood loss and lack of tissue blood, resulting in inadequate oxygen supply, can lead to circulatory hypoxia.9. what kind of hypoxia can pulmonary edema cause? Its hypoxia mechanism?Can cause hypoxic hypoxia, due to pulmonary edema, ventilation function of fertilizer limited caused by alveolar PO2 decreased, pulmonary ventilation dysfunction by alveolar diffuse into the blood oxygen reduction, PaO2 and lack of oxygen, caused by hypoxic hypoxia.10. to analyze the mechanism of red blood cell growth during chronic hypoxia.When the number of red blood cells in chronic hypoxia is mainly due to the increase in renal production and release of erythropoietin EPO; hypoxia can increase the activity of HIF-1 in cytoplasm, HIF-1 gene and EPO 3 enhancer binding, enhanced the expression of EPO gene, the EPO increased, the molecular weight of EPO was 34000 of the egg white sugar, can promote stem cell the original red blood cell differentiation, and promote the differentiation, proliferation and maturation, accelerate the synthesis of hemoglobin, the bone marrow reticulocyte and red blood cells released into the blood.11. try to describe the mechanism of shortness of breath inpeople on the upper plateau.The air in the plateau is thin and low in oxygen,At the beginning of the plateau, hypoxia induced PAO2 below 60mmHg and stimulated the peripheral chemoreceptor of the carotid body and the aortic body. The impulses were introduced into the medulla via the sinus nerve and the vagus nerve, which caused the respiration to accelerate gradually.12. can arterial blood pressure be used as a marker for the occurrence of shock? Why?No, because the shock early sympathoadrenomedullary excitement, heart rate, contractility increased, blood transfusion and infusion through their own, as well as increased renal reabsorption of sodium and water, increase the turn output, so that the increased cardiac output, plus the peripheral resistance increased, so the blood pressure was not obvious.13. to describe the characteristics and compensatory significance of microcirculatory changes in early stage of shock.Is the early stage of shock shock compensatory, the sympathetic nervous excitement, increased catecholamine, some organs of small vascular contraction or spasm, especially micro artery, after arterioles and precapillary sphincter contraction, the precapillary resistance increased, capillary closure, true capillary network reduced blood flow, blood flow slows down; beta adrenergic receptor the stimulated arteriovenousanastomoses are open, blood through the direct pathway and open the arteriovenous anastomosis reflux, microcirculation of non nutritive blood flow increase, reduce nutrient flow, severe hypoxic ischemic tissue. The above changes of microcirculation, on the one hand, cause ischemia and hypoxia of organs such as skin, abdomen, viscera and kidneys, on the other hand, they have compensatory significance to the whole. The main manifestations are: blood redistribution, autotransfusion, and self infusion.14. the mechanism of microcirculatory changes in shock stage II.The mechanism of microcirculatory changes in progressive stage is related to the effects of prolonged microvascular contraction and ischemia, hypoxia, acidosis, and various humoral factors.Acidosis: hypoxia leads to the decrease of tissue oxygen partial pressure, accumulation of CO2 and lactic acid and acidosis. Acidosis causes a decrease in the responsiveness of vascular smooth muscle to catecholamines and causes vasodilation.The local vasodilator metabolites increased: long-term ischemia and hypoxia, acidosis stimulates the release of histamine from mast cells increased, ATP decomposition products of adenosine accumulation, kinins generation increases, can cause vascular smooth muscle relaxation and telangiectasia.The changes of blood rheology: shock progression blood flow decreased obviously, micro slow blood flow in erythrocyte aggregation and easy; the effect of histamine on capillary permeability, plasma extravasation, blood viscosity increased; perfusion pressure decreased, resulting in leukocyte rolling, adhesion and adhesion to endothelial cells, blood blocked postcapillary resistance increased.IV: the role of endotoxin: the relaxation of vascular smooth muscle, resulting in persistent hypotension.15. what is the most common cause of multiple organ dysfunction syndrome (MODS)? Its pathogenesis?80% of the MODS patients had significant shock when they entered the hospital.Infectious causes, such as sepsis and severe infection, can affect approximately 70% of MODS, especially sepsis caused by severe infections.Non infectious causes such as major surgery and severe trauma, major surgery and severe trauma, whether or not infections are pure, can occur in MODS.Pathogenesis: (1) the general inflammatory response is out of control. Promoting the imbalance between anti-inflammatory and anti-inflammatory mediators. Other factors that cause organ dysfunction: organ microcirculation perfusion disorder, high metabolic state, ischemia-reperfusion injury.What is the mechanism of 16.DIC?The release of tissue factor, the activation of exogenous coagulation system, the initiation of blood coagulation system, the damage of vascular endothelial cells, the imbalance of coagulation and anticoagulant regulation, the destruction of blood cells, the activation of platelets, and the introduction of procoagulant substances into the blood.What is the mechanism by which 17.DIC leads to shock?Because of the large amount of micro thrombus in blood vessel, the microcirculation is blocked and the blood volume is reduced obviously. Extensive bleeding can reduce the volume of blood. The injury of cardiac muscle leads to decrease of cardiac output. The activation of coagulation factor XII may activate the kallikrein system, complement system and fibrinolytic system, and produce some vasoactive substances, such as bradykinin and complement components. The complement component can make the basophils and mast cells release histamine, etc. the peptide and histamine can relax the microvascular smooth muscle, increase the permeability, reduce the peripheral resistance and reduce the blood volume. Some components of FDP can enhance the action of histamine, bradykinin and promote the expansion of microvessels.18. try to explain the compensatory response of the heart when the heart function is incomplete.Heart rate increased, heart tension dilated, myocardial contraction increased, ventricular remodeling19. cardiac insufficiency after the type of compensatory cardiac hypertrophy and its mechanism, sarcomere replication.Hypertrophy of the heart can be caused by a variety of reasons. When partial myocardial cells are lost, reactive myocardial hypertrophy may occur in the residual myocardium. Prolonged overload can cause excessive cardiac hypertrophy,According to the cause of overload and cardiac reaction of different forms can be divided into overload cardiac hypertrophy: concentric hypertrophy, cardiac function in long-term excessive load pressure, systolic wall tension increase myocardial sarcomere parallel type hyperplasia, thickening of myocardial cells. Eccentric hypertrophy, heart in the long-term excessive load capacity, diastolic wall tension increase myocardial sarcomere was series hyperplasia, myocardial cell growth, ventricular volume increases; while the heart enlargement and systolic wall stress increases, and thus stimulate the proliferation of sarcomere parallel.20. briefly describe the mechanism and significance of heart rate reduction during heart failure.The mechanism of heart rate is: due to decreased cardiac output, heart rate caused by the intracardiac residual blood volume is increased; reduce the heart pump blood, ventricular end diastolic volume and pressure, can stimulate the right atrium and vena cava volumereceptor, via vagal afferent fibers in the vagus nerve to pivot, inhibition, sympathetic stimulation. If the combined hypoxia can stimulate the aortic body and carotidbody chemoreceptor, reflex excitability causes heart rate to accelerate. Significance: cardiac output is the product of stroke volume and heart rate, in a certain range, can improve the heart rate, cardiac output, and can improve the diastolic blood pressure, blood perfusion to the coronary artery, to maintain arterial blood pressure, which is of positive significance to the blood supply to vital organs.21. what is the mechanism of dyspnea caused by heart failure? What types of dyspnea do you have?Mechanism: lung congestion and pulmonary edema lead to lower lung compliance. To breathe the same amount of air, it is necessary to increase the work done by the respiratory muscle and consume more energy, so the patient feels labored. The bronchial mucosal hyperemia, swelling and airway secretions lead to airway resistance increases; the pulmonary capillary pressure and interstitial edema of pulmonary interstitial pulmonary capillary pressure increased, stimulation of fat receptors, causing reflex rapid shallow breathing. Types include exertional dyspnea, dyspnea, and paroxysmal nocturnal dyspnea.22. the severe hypokalemia (or excessive anesthetics, sedatives, hypnotics, severe pneumothorax, pleural effusion, obstruction of trachea, bronchial asthma, chronic bronchitis) the pathogenesis of respiratory failure caused by.The main effects of hypokalemia on the body is the membrane potential caused by the abnormal effect of nerve muscle, muscle relaxation of skeletal muscle weakness and even paralysis,leading to respiratory muscle contraction diastolic dysfunction caused by restrictive ventilation due to insufficient pulmonary dysfunction, which is outside the alveolar gas and gas exchange in extracellular potassium ion concentration in cell metabolism disorder caused by the disturbance of acid-base balance disorders, hypokalemia decreased, intracellular potassium concentration gradient transfer to the outside of the cell and extracellular hydrogen ion transfer to the cells increased, the hydrogen potassium exchange; the renal ammonia (hydrogen ions).23. to discuss the pathogenesis of pulmonary heart disease.The alveolar hypoxia and CO2 retention caused by blood H+ concentration is too high, can cause pulmonary arteriolar constriction, the pulmonary arterial pressure increased, thereby increasing the right ventricular afterload; pulmonary arteriole contraction and hypoxia can cause non muscular arterioles in muscle, pulmonary vascular smooth muscle cells to fibroblast cell hyperplasia, collagen and elastin synthesis increase, lead to pulmonary vascular wall thickening and lumen narrowing, hardening, resulting in chronic pulmonary hypertension lasting and stable due to the long-term hypoxia; compensatory polycythemia can increase blood viscosity, will also increase the resistance of pulmonary blood flow and increased right heart load; and some abdominal diseases such as pulmonary arteritis, small the destruction of a large number of pulmonary capillary and pulmonary embolism can be a cause of pulmonary hypertension; the hypoxia and acidosis family cardiac contractility and dyspnea, Forced expiratory intrathoracic pressure can cause abnormal increase of cardiaccompression effect of cardiac diastolic function, abnormal inspiratory intrathoracic pressure is reduced, the negative pressure outside the heart increases, increased right ventricular systolic load to right heart failure.24. to discuss the pathogenesis of pulmonary encephalopathyEffects of hypoxia, acidosis and hypercapnia on cerebral blood vessels:1, hypoxia and acidosis to cerebral vascular dilation; 2, hypoxia and acidosis leads to vascular endothelial injury: one is to increase vascular permeability, aggravate brain edema, while promoting intravascular coagulation; 3, hypoxia and acidosis reduced the formation of ATP: dysfunction of sodium pump, cell edema, cerebral vascular compression increased intracranial pressure, intracranial pressure, cerebral vascular compression, increased hypoxia, and forming a vicious spiral.Two. The effects of hypoxia, acidosis and hypercapnia on neurons:1, on the one hand, hypoxia can directly inhibit brain function, on the other hand can cause dysfunction of sodium pump, make the brain edema, increased intracranial pressure; 2, hypercapnia easily lead to intracellular acidosis, on the one hand, the glutamic acid decarboxylase activity increased, the increasing production of GABA, inhibit the function of central nervous system,On the other hand, it can enhance phospholipase activity, decompose membrane phospholipids, dissolve lysosomes, and aggravate the damage of nerve cells.What is the cause of elevated blood ammonia in 25. hepatic encephalopathy? What are the toxic effects of ammonia intoxication on the brain?.The reasons for the increase of blood ammonia include: the decrease of urea synthesis and the lack of ammonia clearance. Toxicity: 1, ammonia to neurotransmitters in the brain changes, brain cell energy metabolism and ammonia the interference effect on the nerve cell membrane pump: NA-K interference on the nerve cell membrane; competition of K ion and ion distribution of membrane.26. what are the metabolic changes in acute renal failure and oliguria? Explain its mechanism.The change of urine: oliguria, anuria, low proportion of urine, hematuria, proteinuria, urinary tube; functional ARF, renal function is not damaged, the oliguria is mainly due to GFR significantly reduced by, and the organic ARF and glomerular and renal tubular dysfunction.Water intoxication: ARF, for reasons of oliguria, catabolism caused by increased intake of water, in the water too much, resulting in water retention, dilutional hyponatremia and cell edema at.The hyperkalemia: potassium with the urine reduced urine volume;。
临床医学病理学问答题、名词解释练习题及答案*萎缩的定义和病理性萎缩有哪些?★~P7萎缩:已发育正常的组织和器官,实质细胞体积减少,而致组织或器官缩小。
一、生理性:退化-动脉导管、脐带血管;胸腺,老年性萎缩。
二、病理性:1、全身性营养不良性萎缩,如:长期饥饿者、恶性肿瘤者2、神经性萎缩,如:脊髓前角灰貭炎者3、废用性萎缩,如:肢体骨折石膏固定后,肢体长期不活动4、压迫性萎缩,如:尿路结石,尿排泄不畅,而积在肾盂,引起肾实质发生压迫性萎缩5、内分泌性萎缩,如:垂体功能低下引起肾上腺、甲状腺、性腺等器官萎缩6、缺血性萎缩,如:冠状动脉粥样硬化引起心肌萎缩、脑动脉硬化引起脑萎缩*化生的定义,常见类型?★~P8化生:为适应环境变化,一种以分化成熟的组织转变为另一种分化成熟的组织的过程常见类型:1.上皮组织化生(1)鳞状上皮化生~常见部位:气管、支气管黏膜,如:长期吸烟者、慢性炎症者(2)肠上皮化生~常见部位:胃体、胃窦部,如:胃溃疡、慢性萎缩性胃炎2.间叶组织化生:结缔组织化生为骨,软骨或脂肪组织如:骨化性肌炎,纤维组织增生,并发生骨化生*心脏萎缩有哪些改变,以心肌为例?★~P81.大体改变:(1)心肌褐色(2)心尖锐尖(3)包膜皱缩(4)冠状动脉蛇样弯曲2.镜下改变:(1)心肌纤维变细窄(2)肌间距变宽(3)心肌细胞中可见脂褐素颗粒*病理性钙化的概念,种类~p.17正常机体内仅在骨和牙齿内含有固体钙盐,如在骨和牙齿以外的其它组织内有固体钙盐沉积,称之病理性钙化种类-营养不良性钙化(变性,坏死组织或义务的钙盐沉积)转移性钙化(全身性钙,磷代谢障碍引起血钙或血磷增高,导致钙盐在未受伤组织内沉积)。
*坏死的结局★(1)溶解吸收(2)分离排出(3)机化(4)包裹,钙化*坏疽比较:★*细胞凋亡与坏死的区别*再生性修复与纤维性修复的区别由耗损的同种实质细胞再生进行修复,可完全恢复原有细胞、组织的结构和功能。
由结缔组织来修补填空缺损,并形成瘢痕,只能恢复组织的完整性,不能完全恢复原有的结构和功能。
三、名词解释化生(Metaplasia):一种分化成熟的细胞,为适应环境的改变而转化为另一种性质相似并分化成熟细胞的过程。
;变性指由于物质代谢障碍细胞或间质内出现异常物质或正常物质的量显著增多,并伴有不同程度的功能障碍。
;虎斑心心肌脂肪变性最显著的发生部位是乳头肌和心内膜下心肌。
重者呈黄色条纹,轻者呈暗红色,两者相间排列,状似虎皮,故称为“虎斑心”;萎缩发育正常的细胞、组织和器官体积的缩小。
;酶解性组织坏死急性胰腺炎时细胞释放胰酶分解脂肪酸,乳房创伤时脂肪细胞破裂,可分别引起酶解性或创伤性脂肪坏死,属于液化坏死范畴;机化新生肉芽组织长入并取代坏死组织、血栓、脓液、异物等的过程;肉芽组织由新生薄壁毛细血管以及增生成纤维细胞构成,并伴有炎性细胞浸润,肉眼表现为鲜红色,颗粒状,柔软湿润,形似鲜嫩的肉芽而得名。
;坏死是以酶溶性变化为特点的活体内局部组织细胞的死亡。
细胞核的改变是细胞坏死的主要标志,有三种形式核固缩、核碎裂、核溶解。
瘢痕组织(iscar tissue);坏疽大片组织坏死后继发腐败菌感染,使其呈黑色、污绿色等特殊的颜色和气味。
分干性坏疽、湿性坏疽和气性坏疽三种。
;水变性细胞损伤后钠水的过多积聚;肥大与增生:肥大:由于功能增加,合成代谢旺盛,使细胞、组织或器官体积增大,可由于实质细胞体积增大,也可伴有实质细胞数量增加。
;增生:组织或器官内实质细胞数目增多。
常导致组织或器官的体积增大:再生损伤周围的同种细胞修复缺损;Mallory小体肝细胞内出现的红染玻璃样物质,是由中间丝的前角蛋白堆积成的;凝固性坏死蛋白质变性凝固且溶酶体酶水解作用较弱时,坏死区呈灰黄、干燥、质实状态。
细胞微细胞坏消失,组织结构轮廓尚存;干酪样坏死凝固性坏死的一种特殊类型。
在结核病时,因病灶中含脂质较多,坏死区呈黄色,状似干酪。
坏死彻底,不见组织结构轮廓。
;核碎裂(karyopyknosis)由于核染色质崩解和核膜破裂,细胞核发生碎裂,使核物质分散于细胞质中,也可有核固缩裂解城碎片而来;气球样变性(ballooning degeneration)肝细胞受损后,细胞浆水分增多,多角形细胞变大变圆,胞浆透明淡染;肉芽肿是由渗出的单核细胞和以局部增生的巨噬细胞形成的境界清楚的结节状病灶;栓塞性脓肿由栓塞于毛细血管的化脓菌引起的脓肿;脓性卡他粘膜化脓性炎又称脓性卡他。
病理学名词解释及问答题总结(第一章)细胞和组织的适应与损伤*病理学(pathology)是研究疾病的病因、发病机制、病理变化、结局和转归的医学基础学科。
*适应(adaptation) 细胞和由其构成的组织、器官,对内外环境中各种有害因子和刺激作用而产生的非损伤性应答反应,形态学上表现为萎缩、肥大、增生、化生*Atrophy(萎缩)已发育正常的细胞、组织或器官体积缩小,包括实质细胞的体积缩小和数量减少*Hypertrophy(肥大)由于功能增加,合成代谢旺盛,使细胞、组织或器官体积增大,包括实质细胞体积增大、常伴数量增加*pseudo hypertrophy (假性肥大) 实质细胞萎缩的同时,间质细胞增生,以维持器官的体积,甚至造成器官组织的体积增大*hyperplasia (增生) 组织或器官内实质细胞数目增多,常导致体积增大*metaplasia(化生) 一种分化成熟的细胞类型被另一种分化成熟的细胞所取代的过程;不可能发生于神经纤维组织*squamous metaplasia (鳞状上皮化生) 慢支时,支气管纤毛柱状上皮被鳞状上皮取代的过程*intestinal metaplasia (肠上皮化生) 慢性胃炎时,胃粘膜上皮转化为含有潘氏细胞或杯状细胞的小肠或大肠上皮组织*degeneration (变性) 又称可逆性损伤,是指细胞或间质受损伤后,由于代谢障碍,导致细胞内或间质内出现异常物质或正常物质异常蓄积的现象,常伴细胞功能低下。
*cellular swelling (细胞水肿) 又称水变性,是细胞损伤时最早出现的改变。
系因线粒体受损,ATP生成减少,Na-K泵功能障碍,导致细胞内Na-K过多。
无机盐、乳酸等蓄积,导致渗透压升高,加重水肿*fatty degeneration or fatty change (脂肪变性) 中性脂肪特别是甘油三脂蓄积于非脂肪细胞中*tigroid heart (虎斑心)心肌脂肪变性时,脂肪心肌呈黄色,与正常心肌的暗红色相间,形成黄红色斑纹*myocardial fatty infiltration (心肌脂肪浸润) 心外膜增生的脂肪组织沿间质深入心肌细胞间*hyaline degeneration (透明变性) 又称玻璃样变hyalinization,细胞内或间质中出现半透明状蛋白质蓄积,HE染色呈嗜依红均质状;Rusell小体由于粗面内质网中免疫球蛋白蓄积而形成。
兽医病理学:是研究动物的原因、发生、发展和转归规律及患病动物物质代谢、机能活动和形态结构变化的一门学科。
家畜病理学主要研究方法:1 尸体剖检:大体观察,组织学观察,细胞学观察,组织化学观察,超微结构观察,核酸技术2 动物实验3 临床病理学4 活体组织检查5 组织、细胞培养疾病:在致病因素的损伤与机体的抗损伤作用下,因自稳调节紊乱而发生的异常生命活动过程动脉性充血:因小动脉和毛细血管扩张,使局部组织和器官中血量增多的现象,简称充血静脉性充血:动脉输入正常,但静脉回流受阻,血液淤积在小静脉和毛细血管里,引起局部组织中静脉血含量增多的现象,简称淤血。
出血:血液流出心脏或血管之外。
血栓:在活体的心血管内,从血液成分形成固体物质的过程。
梗死:局部组织或器官因血流断绝而引起的坏死栓塞:循环血流中出现异常物质阻塞血管腔的过程,称为栓塞,这些异常物质被称为栓子。
脱水:各种原因引起的体液容量的明显丢失称为脱水。
水肿:体液在组织间隙蓄积过多。
高渗性脱水:以水分丧失为主,盐类丧失较少的脱水。
低渗性脱水(缺盐性脱水):盐类丧失多于水分丧失。
等渗性脱水:水及电解质同时大量丧失,血浆渗透压基本保持不变代谢性酸中毒:血浆内NaHCO3原发性减少,CO2结合力(CO2CP)降低,血液PH值低于正常范围。
呼吸性酸中毒:血液中H2CO3原发性增高,PCO2增高,pH值低于正常范围萎缩:发育正常的组织器官或细胞,由于物质代谢障碍而使其实质细胞体积缩小、数量减少,导致器官组织体积缩小、功能减退的过程。
变性:指在细胞和组织损伤时,在细胞或间质内出现异常物质或异常量的正常物质。
细胞肿胀:是指细胞内水分增多,胞体增大,胞浆内出现微细颗粒或大小不等的水泡。
玻璃样变性:是指在间质或细胞内出现一种光镜下呈均质、无结构、半透明的玻璃样物质的现象。
脂肪变性:在变性细胞内出现大小不等的游离脂肪小滴。
坏死:活体内局部组织或细胞的死亡。
为一种不可逆的病理变化。
病理病生最全名词解释(英汉俱全)1.疾病(disease)是指机体在一定原因作用下,自稳调节机制发生紊乱而出现的异常生命活动过程。
2.病理生理学(pathophysiology)是一门侧重从功能和代谢角度,阐明疾病发生、发展和转归规律的学科。
3.发热(fever)是指在致热源的作用下使体温调节中枢调定点上移而引起的调节性体温升高(超过0.5'C。
)4.病理过程(pathologic process)是指不同器官、系统在许多不同疾病中可能出现的共同的、成套的功能代谢的变化。
5.病因(etiology agents)是指作用于机体引起疾病并赋予该疾病特征性的因素。
6.过热(hyperthermia)由于体温调节障碍或散热障碍及产热器官功能异常等,体温调节机构不能将体温控制在与调定点相适应的水平上的被动性体温升高。
7.疾病发生的条件(predisposing factors)是指在病因作用于机体的前提下,影响疾病发生发展的各种体内外因素。
8.诱发因素(precipitating factor)是指能够促进和加强某一疾病原因作用的条件因素称为诱发因素,简称诱因。
9.氧自由基(oxygen free radical)由氧诱发的自由基称为氧自由基,例如超氧阴离子自由基、羟自由基。
10.应激(stress)是指机体受到强烈刺激而发生的以交感—肾上腺髓质系统和垂体—肾上腺皮质系统兴奋为特征的一种非特异性全身适应性反应。
11.急性期反应蛋白(acute phase protein)应激时由于感染、炎症或组织损伤等原因可使血浆中某些蛋白质浓度迅速升高,这种反应称为急性期反应,,这些蛋白则被称为急性期反应蛋白(AP)。
12.调定点(set piont,SP):调定点理论认为体温调节类似于恒温器的调节,在体温调节中枢内有一个调定点,体温调节机构围绕着这个调定点来调控体温。
当体温偏离调定点时,可有反馈系统(温度感受器)将偏差信息送到控制系统,后者将这些信息综合分析,与调定点比较,然后通过对效应器(产热和散热)的调控吧中心温度维持在与调定点相适应的水平。
2010年级临床医学专业名词解释1.萎缩与肥大:萎缩是已发育正常的细胞、组织或器官的体积缩小。
由于功能增加,合成代谢旺盛,使细胞、组织或器官体积增大,称为肥大。
2.化生与机化:一种分化成熟的细胞类型被另一种分化成熟的细胞类型所取代的过程,称为化生。
新生肉芽组织长入并取代坏死组织、血栓、脓液、异物等的过程,称为机化。
3.变性与脂肪变:细胞可逆性损伤,旧称变性。
中性脂肪特别是甘油三醇蓄积于非脂肪细胞的细胞质中,称为脂肪变。
4.凋亡与坏死:坏死是以酶溶性变化为特点的活体内局部组织细胞的死亡。
凋亡,是活体内个别细胞程序性细胞死亡的表现形式,是由体内外因素触发细胞内预存的死亡程序而导致的细胞主动性死亡方式。
5.空洞与溃疡:肺、肾等内脏坏死物液化后,经支气管、输尿管等自然管道排出,所残留的空腔称为空洞。
坏死灶较大不易被完全溶解吸收时,表皮黏膜的坏死物可被分离,形成组织缺损;浅者称为糜烂,深者称为溃疡。
10.窦道与瘘管:组织坏死后形成的只开口于皮肤黏膜表面的深在性盲管,称为窦道。
连接两个内脏器官或从器官通向体表的通道样缺损,称为瘘管。
11.完全再生与纤维性修复:由损伤周围的同种细胞来修复,称为再生,如果完全恢复了院组织的结构及功能,则称为完全再生。
由纤维结缔组织来修复,称为纤维性修复。
12.充血与淤血:器官或组织因动脉输入血量的增多而发生的充血,称动脉性充血。
器官或局部组织静脉血流回流受阻,血液淤积于小静脉和毛细血管内,称淤血,又称静脉性充血。
13. 血栓形成与附壁血栓:在活体的心脏和血管内,血液发生凝固或血液中某些有形成分凝集形成固体质块的过程,称为血栓形成。
发生于心腔或动脉瘤内的混合血栓称为附壁血栓。
14. 血栓的机化与再通:由肉芽组织逐渐取代血栓的过程,称为血栓机化。
在血栓机化过程中,由于水分被吸收,血栓干燥收缩或部分溶解而出现裂隙,周围新生的血管内皮细胞长入并被覆于裂隙表面形成新的血管,并相互吻合沟通,使被阻塞的血管部分地重建血流,这一过程称为再通。
适应、损伤、修复1、肥大:由于功能增强、合成代谢旺盛,细胞、组织和器官体积的增大。
可分为代偿性肥大和内分泌性肥大两类。
细胞肥大通常具有功能代偿意义。
2、化生:一种已分化成熟的细胞因受刺激因素的作用转化成另一种分化成熟细胞的过程。
常见的化生有鳞状上皮化生、肠上皮化生、结缔组织或支持组织化生。
3、肠上皮化生:由于炎症、溃疡病、肿瘤或其他原因,使胃黏膜上皮或腺体被肠上皮或腺体取代;其主要特征是胃黏膜内出现了杯状细胞、潘氏细胞和吸收绒毛上皮,这种现象称为“肠上皮化生”。
4、变性:由于细胞非致死性损伤导致的细胞形态学改变,细胞内或细胞间质内出现异常物质或正常物质蓄积的状态,常伴有细胞、组织、器官的功能低下。
一般是可恢复的,但严重的变性往往是不能恢复而发展成坏死。
(可逆性损伤)5、脂肪变性:非脂肪细胞的实质细胞中脂肪的过度蓄积,出现了异常的脂滴和正常脂滴数目显著增多,这种形态学改变称为脂肪变性。
常出现在肝肾心等组织。
6、虎斑心:心肌严重贫血、脂肪变性时,可见心内膜下,尤其是乳头肌处出现成排的黄色条纹(脂变的心肌纤维),与正常心肌纤维(暗红色)相间排列,状似虎皮斑纹,称为虎斑心。
7、病理性钙化:在骨和牙之外的组织中有固态的钙盐沉积,其可位于细胞内和细胞间质。
8、坏死:以酶溶性变化为主的活体局部组织和细胞的死亡称为坏死。
其主要表现是死亡细胞的质膜崩解、结构自溶,细胞的核浓缩、碎裂、溶解等细胞和组织的自溶性变化,坏死组织周围常有炎症反应。
9、纤维素样坏死:发生于结缔组织和小血管壁,是风湿病和急进性高血压的特征性病变。
镜下,坏死组织呈细丝状、颗粒状的红染的纤维素样。
10、坏疽:伴有腐败菌感染的较大块组织坏死,分为干性坏疽、湿性坏疽和气性坏疽。
11、干性坏疽:常继发于肢体、水分容易蒸发的体表组织坏死。
动脉阻塞、经脉通畅,坏死组织干燥,腐败菌感染较轻,故坏死部分与周围正常组织分界清楚。
12、凋亡:主要指活体内单个或小团细胞的死亡,死亡细胞质膜不破裂,不自溶,无炎症反应。
病理学肿瘤名词解释1 肿瘤(tumor)2 间变(anaplasia)3 转移(metastasis)4 异型性(atypia)5 癌前疾病或癌前病变(precancerous disease or precancerous lesion)6 不典型增生(atypical hyperplasia)7 原位癌(carcinoma in situ)8 癌珠(carcinoma pearl or keratin pearl)9 癌基因(oncogene)10 肿瘤抑制基因(tumor suppressor gene)问答题1 简述异型性、分化程度及与肿瘤良恶性的关系。
2 试比较肿瘤性增生与炎性或修复性增生的区别。
3 简述肿瘤的命名原则。
4 试比较良性瘤与恶性瘤的区别。
5 试比较癌与肉瘤的区别。
6 简述恶性瘤对机体的影响。
7 简述食管癌、胃癌、大肠癌的共同点(或相似点)。
8 简述肿瘤的分级、分期及与肿瘤发生发展的关系。
指出其在肿瘤防治中的意义。
9 何谓癌前病变,请列举5种癌前病变或癌前疾病,并说明应如何正确对待癌前病变。
10 患者男,48岁,因发热、咳嗽、咳黏液脓痰5天,痰中带血2天入院。
既往患者有吸烟、饮洒史。
曾于五年前被诊断为“慢性支气管炎”、“慢性胃炎”等,自述“心窝”、腹上区(上腹部)经常性疼痛,近来咳嗽时加重。
体格检查:体温38.30C,脉搏82次/分,呼吸21次/分,血压17.3/10.1kPa(130/76mmHg),消瘦,左锁骨上淋巴结肿大,质稍硬,动度差。
实验室检查:外周血白细胞0.85×109/L,血红蛋白90g/L。
X线胸片:左下肺近肺门处见一3cm×2.5cm边缘不整之阴影。
纤维胃镜:胃窦小弯侧有2cm×1.8cm的糜烂面伴灶性出血,余无特殊。
请拟定诊断的步骤和方法,并作出可能的诊断。
11 患者女,41岁,右乳腺乳头外上方皮下有肿块,你准备采取哪些方法来确定肿块的性质(包括采集病史,物理检查和病理检查)?12 患者女,37岁,腹上区不适伴明显消瘦3月,大便次数增多二周,食欲缺乏,最近10天内3次大便检查潜血阳性。
组损活检对活体组织采用局部切除、钳取、针吸、搔刮等方法,进行病理检查。
病理学是用自然科学的方法研究疾病的形态结构、代谢和功能等方面的改变,从而揭示疾病的病因、发病机制和转归的医学基础学科。
萎缩发育正常的器官、组织或细胞体积缩小。
肥大细胞、组织或器官体积的增大。
化生一种已分化组织转化为另一种相似性质的分化组织的过程。
变性由于物质代谢障碍,在细胞内或间质中出现异常物质,或正常物质数量增多。
水变性细胞内水分增多,造成细胞水肿。
脂肪变性除脂肪细胞外,细胞内出现脂滴或脂滴明显增多。
凝固性坏死组织细胞坏死后,蛋白质变性凝固且酶性分解作用较弱时,坏死区形成灰黄、干燥、质实的状态。
液化性坏死由于坏死组织中可凝固的蛋白质少,或坏死细胞自身及浸润的中性粒细胞释放大量水解酶,或组织富含水分和磷脂,组织坏死后易发生溶解液化。
玻璃样变细胞内或间质中出现均质红染、半透明的玻璃样物质。
(透明变性)干酪样坏死是一种特殊类型的凝固性坏死,由于坏死组织中含较多的脂质,外观呈淡黄色,松软,均匀细腻,似奶酪,称之。
常见于结核病。
干性坏疽发生于四肢末端,多见于足,由动脉阻塞和静脉回流通畅引起,腐败菌感染轻,坏死组织干燥,黑褐色,与周围正常组织分界清楚的特点。
湿性坏疽发生于肺、肠、阑尾、子宫、四肢,由动脉阻塞静脉回流受阻引起,坏死组织肿胀,乌黑色,与健康组织分界不清的特点。
坏疽肢体或与外界相通的内脏较大范围的坏死,同时伴有不同程度的腐败菌感染,呈黑色改变。
损伤修复不稳定细胞是一类再生能力相当强的细胞,如表皮细胞、呼吸道和消化道粘膜被覆细胞、淋巴及造血细胞、间皮细胞等。
稳定细胞又称静止细胞,这类细胞在生理情况下较稳定,一旦受到刺激和损伤后则表现出较强的再生能力。
永久细胞这类细胞无再生能力,属于这类细胞的有神经细胞、心肌细胞、骨骼肌细胞。
机化由新生肉芽组织逐渐取代坏死组织(血栓、脓液或其它异物等)的过程。
肉芽组织由新生的成纤维细胞和毛细血管组成,是一种幼稚的纤维结缔组织。
《病理学与病理生理学》期末复习题及答案一、名词解释1、疾病:是指机体在一定病因的作用下,自稳调节紊乱而发生的异常生命活动过程。
2、健康:不仅是没有疾病或病痛,而且是一种躯体上,精神上和社会适应上的完好状态。
3、缺氧:是指组织供氧不足或用氧障碍,从而引起组织代谢,功能以及形态结构发生异常变化的病理过程。
4、萎缩:是指发育正常的细胞、组织、器官体积的缩小。
5、化生:一种分化成熟细胞类型被另一种分化成熟的细胞类型所取代的过程。
6、肉芽组织:是指由新生的毛细血管和成纤维细胞组成的幼稚纤维结缔组织,可伴炎细胞浸润。
7、异型性:肿瘤组织无论在细胞形态还是组织结构上都与其起源的正常组织有不同程度的差异,这种差异称为异型性。
8、肿瘤:是指机体在各种致瘤因子的作用下,局部组织细胞发生基因突变或基因表达异常,导致克隆性异常增生而形成的新生物。
二、填空题1、疾病的经过包括潜伏期、前驱期、疾病明显期、转归期四个阶段。
2、传统意义上,死亡包括濒死期(临终状态)、临床死亡期、生物学死亡期三个时期。
3、常见的细胞和组织的适应性改变有萎缩、肥大、增生、化生四种。
4、细胞坏死的基本病理变化是细胞核的改变,表现为核固缩、核碎裂、核溶解。
5、淤血的后果有水肿、出血、组织损伤、硬化。
6、血栓的类型有白色血栓、混合血栓、红色血栓、透明血栓。
7、炎症的局部临床表现为红、肿、热、痛、功能障碍。
8、炎症的基本病理变化为变质、渗出、增生。
9、肿瘤转移途径可分为淋巴道转移、血道转移、种植性转移。
10、缺氧的类型包括低张性缺氧、血液性缺氧、循环性缺氧、组织性缺氧。
三、单项选择1、病理学应用最广泛的研究方法是EA.尸体剖验B.细胞培养和组织培养C.动物实验D.电镜E.活检2、病理学与病理生理学的任务是研究疾病EA.临床表现B.诊断与鉴别诊断C.防治措施D.流行病学特点E.发生与发展规律3、影响动脉血氧分压高低的主要因素是DA.血红蛋白的含量 B.组织供血能力 C.血红蛋白与氧气的亲和力D.肺的通气功能 E.线粒体磷酸脱氢酶活性4、一种分化成熟的组织变成另一种分化成熟组织的过程称为 DA.机化 B.钙化 C.分化 D.化生 E.适应5、坏死组织逐渐被肉芽组织取代的过程称为BA.纤维化B.机化C.钙化D.分化E.再生6、细动脉壁玻璃样变最常发生于哪种疾病BA.风湿性心脏病B.缓进性高血压C.急性肾小球肾炎D.嗜铬细胞瘤E.急性肾盂肾炎7、细胞坏死时,具有标志性的改变是EA.核溶解、胞质浓缩和胞膜破裂 B.核碎裂、核膜破裂和核质浓缩 C.核溶解、核质少和胞膜破裂D.核固缩、胞质浓缩和细胞膜皱缩 E.核固缩、核碎裂和核溶解8、全身营养不良时,首先发生萎缩的组织是BA.骨骼肌B.脂肪组织C.心肌D.肝实质E.脑组织9、肠扭转可导致肠管发生以下哪种病理变化BA.干性坏疽 B.湿性坏疽 C.气性坏疽 D.液化性坏死 E.干酪样坏死10、干酪样坏死好发于下列哪种疾病CA.风湿病 B.伤寒 C.结核 D.麻风 E.梅毒11、槟榔干的病理变化为 EA.中央静脉淤血 B.肝窦扩张 C.肝细胞萎缩D.肝细胞脂肪变性 E.中央静脉、肝窦扩张淤血及肝小叶周边肝细胞脂肪变性12、左心衰竭首先引起淤血的器官是BA.肝 B.肺 C.脾 D.肠 E.四肢13、右下肢血栓脱落主要栓塞于DA.肠系膜动脉 B.门静脉 C.肾动脉 D.肺动脉 E.脑动脉14、炎症最常见的原因是DA.机械性损伤 B.高温和低温 C.强酸和强碱 D.细菌和病毒 E.支原体和立克次体15、急性化脓性炎症早期,浸润的炎细胞主要是AA.中性粒细胞 B.单核巨噬细胞 C.淋巴细胞 D.嗜碱性粒细吧 E.嗜酸性粒细胞16、下述炎症改变中,最有防御意义的是 CA.渗出液的产生 B.氧自由基释放 C.白细胞渗出 D.血液停滞 E.炎症介质形成17、炎症局部组织早期呈鲜红色是由于AA.充血 B.淤血 C.炎细胞浸润 D.分解代谢增强 E.变性和坏死18、溶血性链球菌感染最常引起( A )A.蜂窝织炎 B.脓肿 C.纤维素性炎 D.伪膜性炎 E.出血性炎19、右心衰竭主要引起( B)A.慢性脾淤血 B.慢性肝淤血 C.胃肠淤血 D.下肢淤血 E.慢性肺淤血20、最常见的栓子是( C )A.脱落的肿瘤细胞团 B.空气 C.血栓 D.羊水 E.寄生虫21、下列哪项是原位癌的主要特征EA.是一种早期癌症 B.未发生转移 C.发生于子宫颈黏膜上皮D.可长期保持原来的结构,甚至消退 E.癌变波及上皮全层,但未浸润至黏膜下层22、诊断恶性肿瘤的重要依据是( D )A.肿块迅速长大 B.病理性核分裂象 C.恶病质 D.细胞的异型性 E.局部淋巴结肿大23、肿瘤的实质是指DA.神经组织B.纤维组织C.血管D.肿瘤细胞E.浸润的炎细胞24、低分化肿瘤的分化程度是BA.恶性程度低B.恶性程度高C.对放射治疗效果差D.对化疗效果差E.异型性小25、下列不属于癌前疾病的是 CA.肝硬化B.慢性萎缩性胃炎C.子宫平滑肌瘤D.结肠多发性息肉E.纤维性囊性乳腺病26、下列哪项条件易产生二期愈合(E)A.组织缺损大、创缘整齐、创面对合紧密 B.组织缺损少、创缘整齐、创面对合紧密 C.组织缺损大、无感染、创缘整齐 D.创缘整齐、创面对合紧密、有感染 E.创缘不整齐、创面对合不紧密、有感染27、下列哪种细胞是稳定细胞( D)A.皮肤表皮细胞 B.移行上皮细胞 C.造血细胞 D.平滑肌细胞 E.胃、肠道黏膜上皮细胞28、妇女分娩时死亡,尸体解剖发现肺小动脉内有角化上皮细胞、毛发等物质,其死亡原因可能是( D )A.脂肪栓塞 B.气体栓塞 C.肿瘤细胞栓塞 D.羊水栓塞 E.血栓栓塞29、引起炎症的因素中最常见的是( D )A.机械性损伤 B.物理性损伤 C.化学性损伤 D.生物性损伤 E.遗传性缺陷30、某人患阑尾炎,术后,伤口感染,一个月后才愈合,则属于(B)A.一期愈合 B.二期愈合 C.三期愈合 D.四期愈合 E.五期愈合四、简答题1.简述三种的坏疽的区别。