POSITION PAPER
Clinician ’s Guide to Prevention and Treatment of Osteoporosis
F.Cosman &S.J.de Beur &M.S.LeBoff &E.M.Lewiecki &B.Tanner &S.Randall &R.Lindsay
Received:12June 2014/Accepted:24June 2014/Published online:15August 2014#The Author(s)2014.This article is published with open access at https://www.doczj.com/doc/ce17552289.html,
Abstract The Clinician ’s Guide to Prevention and Treatment of Osteoporosis was developed by an expert committee of the National Osteoporosis Foundation (NOF)in collaboration with a multispecialty council of medical experts in the field of bone health convened by NOF.Readers are urged to consult current prescribing information on any drug,device,or pro-cedure discussed in this publication.
Keywords Diagnosis .Guide .Osteoporosis .Prevention .Treatment
Executive summary
Osteoporosis is a silent disease until it is complicated by fractures —fractures that occur following minimal trauma or,in some cases,with no trauma.Fractures are common and
place an enormous medical and personal burden on the aging individuals who suffer them and take a major economic toll on the nation.Osteoporosis can be prevented,diagnosed,and treated before fractures occur.Importantly,even after the first fracture has occurred,there are effective treatments to de-crease the risk of further fractures.Prevention,detection,and treatment of osteoporosis should be a mandate of primary care providers.
Since the National Osteoporosis Foundation (NOF)first published the Guide in 1999,it has become increasingly clear that many patients are not being given appropriate information about prevention and many patients are not receiving appro-priate testing to diagnose osteoporosis or establish osteoporo-sis risk.Most importantly,many patients who have osteoporosis-related fractures are not being diagnosed with osteoporosis and are not receiving any of the Food and Drug Administration (FDA)-approved,effective therapies.
This Guide offers concise recommendations regarding pre-vention,risk assessment,diagnosis,and treatment of osteopo-rosis in postmenopausal women and men age 50and older.It includes indications for bone densitometry and fracture risk thresholds for intervention with pharmacologic agents.The absolute risk thresholds at which consideration of osteoporo-sis treatment is recommended were guided by a cost-effectiveness analysis.
Synopsis of major recommendations to the clinician Recommendations apply to postmenopausal women and men age 50and older.
Universal recommendations &Counsel on the risk of osteoporosis and related fractures.&
Advise on a diet that includes adequate amounts of total calcium intake (1000mg/day for men 50–70;1200mg/day
F.Cosman (*):R.Lindsay
Helen Hayes Hospital,West Haverstraw,NY ,USA e-mail:cosmanf@https://www.doczj.com/doc/ce17552289.html,
S.J.de Beur
Johns Hopkins Bayview Medical Center,Baltimore,MD,USA M.S.LeBoff
Brigham and Women ’s Hospital,Boston,MA,USA E.M.Lewiecki
New Mexico Clinical Research and Osteoporosis Center,Albuquerque,NM,USA
B.Tanner
Vanderbilt University Medical Center,Nashville,TN,USA S.Randall
National Osteoporosis Foundation,Washington,DC,USA F.Cosman :R.Lindsay
Department of Medicine,Columbia University,New York,NY ,USA
Osteoporos Int (2014)25:2359–2381DOI 10.1007/s00198-014-2794-2
for women51and older and men71and older),incorpo-rating dietary supplements if diet is insufficient.
&Advise on vitamin D intake(800–1000IU/day),including supplements if necessary for individuals age50and older. &Recommend regular weight-bearing and muscle-strengthening exercise to improve agility,strength,pos-ture,and balance;maintain or improve bone strength;and reduce the risk of falls and fractures.
&Assess risk factors for falls and offer appropriate modifi-cations(e.g.,home safety assessment,balance training exercises,correction of vitamin D insufficiency,avoid-ance of central nervous system depressant medications, careful monitoring of antihypertensive medication,and visual correction when needed).
&Advise on cessation of tobacco smoking and avoidance of excessive alcohol intake.
Diagnostic assessment
&Measure height annually,preferably with a wall-mounted stadiometer.
&Bone mineral density(BMD)testing should be performed:–In women age65and older and men age70and older –In postmenopausal women and men above age50–69, based on risk factor profile
–In postmenopausal women and men age50and older who have had an adult age fracture,to diagnose and determine degree of osteoporosis
–At dual-energy X-ray absorptiometry(DXA)facilities using accepted quality assurance measures
&Vertebral imaging should be performed:
–In all women age70and older and all men age80and older if BMD T-score is≤?1.0at the spine,total hip,or femoral neck
–In women age65to69and men age70to79if BMD T-score is≤?1.5at the spine,total hip,or femoral neck
–In postmenopausal women and men age50and older with specific risk factors:
&Low-trauma fracture during adulthood(age50and older) &Historical height loss(difference between the current height and peak height at age20)of1.5in.or more(4cm) &Prospective height loss(difference between the current height and a previously documented height measurement) of0.8in.or more(2cm)
&Recent or ongoing long-term glucocorticoid treatment
–If bone density testing is not available,vertebral imaging may be considered based on age alone.
&Check for secondary causes of osteoporosis.&Biochemical markers of bone turnover can aid in risk assessment and serve as an additional monitoring tool when treatment is initiated.
Monitoring patients
&Perform BMD testing1to2years after initiating medical therapy for osteoporosis and every2years thereafter.
–More frequent BMD testing may be warranted in certain clinical situations.
–The interval between repeat BMD screenings may be lon-ger for patients without major risk factors and who have an initial T-score in the normal or upper low bone mass range. &Biochemical markers can be repeated to determine if treatment is producing expected effect.
Pharmacologic treatment recommendations
&Initiate pharmacologic treatment:
–In those with hip or vertebral(clinical or asymptomatic) fractures
–In those with T-scores≤?2.5at the femoral neck,total hip,or lumbar spine by DXA
–In postmenopausal women and men age50and older with low bone mass(T-score between?1.0and?2.5, osteopenia)at the femoral neck,total hip,or lumbar spine by DXA and a10-year hip fracture probability≥3%or a 10-year major osteoporosis-related fracture probability ≥20%based on the USA-adapted WHO absolute fracture risk model(Fracture Risk Algorithm(FRAX?);www.
https://www.doczj.com/doc/ce17552289.html, and https://www.doczj.com/doc/ce17552289.html,/FRAX)
&Current FDA-approved pharmacologic options for osteo-porosis are bisphosphonates(alendronate,ibandronate, risedronate,and zoledronic acid),calcitonin,estrogen agonist/antagonist(raloxifene),estrogens and/or hormone therapy,tissue-selective estrogen complex(conjugated estrogens/bazedoxifene),parathyroid hormone1–34 (teriparatide),and receptor activator of nuclear factor kappa-B(RANK)ligand inhibitor(denosumab).
&No pharmacologic therapy should be considered indefi-nite in duration.After the initial treatment period,which depends on the pharmacologic agent,a comprehensive risk assessment should be performed.There is no uniform recommendation that applies to all patients and duration decisions need to be individualized.
&In adults age50and older,after a fracture,institute appropri-ate risk assessment and treatment measures for osteoporosis as indicated.Fracture liaison service(FLS)programs,where
patients with recent fractures may be referred for care coor-dination and transition management,have demonstrated im-provement in the quality of care delivered. Osteoporosis:impact and overview
Scope of the problem
Osteoporosis is the most common bone disease in humans, representing a major public health problem as outlined in Bone Health and Osteoporosis:A Report of the Surgeon General(2004)[1].It is characterized by low bone mass, deterioration of bone tissue and disruption of bone architec-ture,compromised bone strength,and an increase in the risk of fracture.According to the WHO diagnostic classification, osteoporosis is defined by BMD at the hip or lumbar spine that is less than or equal to2.5standard deviations below the mean BMD of a young-adult reference population.Osteopo-rosis is a risk factor for fracture just as hypertension is for stroke.The risk of fractures is highest in those with the lowest BMD;however,the majority of fractures occur in patients with low bone mass rather than osteoporosis,because of the large number of individuals with bone mass in this range.
Osteoporosis affects an enormous number of people,of both sexes and all races,and its prevalence will increase as the population ages.Based on data from the National Health and Nutrition Examination Survey III(NHANES III),NOF has estimated that more than9.9million Americans have osteopo-rosis and an additional43.1million have low bone density[2]. About one out of every two Caucasian women will experience an osteoporosis-related fracture at some point in her lifetime,as will approximately one in five men[1].Although osteoporosis is less frequent in African Americans,those with osteoporosis have the same elevated fracture risk as Caucasians.
Medical impact
Fractures and their complications are the relevant clinical se-quelae of osteoporosis.The most common fractures are those of the vertebrae(spine),proximal femur(hip),and distal forearm (wrist).However,most fractures in older adults are due at least in part to low bone mass,even when they result from consid-erable trauma.A recent fracture at any major skeletal site in an adult older than50years of age should be considered a signif-icant event for the diagnosis of osteoporosis and provides a sense of urgency for further assessment and treatment.The most notable exceptions are those of the fingers,toes,face, and skull,which are primarily related to trauma rather than underlying bone strength.Fractures may be followed by full recovery or by chronic pain,disability,and death[3].
Hip fractures are associated with an8to36%excess mortality within1year,with a higher mortality in men than in women[4];additionally,hip fractures are followed by a2.5-fold increased risk of future fractures[5].Approximately20% of hip fracture patients require long-term nursing home care, and only40%fully regain their pre-fracture level of indepen-dence[1].Although the majority of vertebral fractures are initially clinically silent,these fractures are often associated with symptoms of pain,disability,deformity,and mortality [3].Postural changes associated with kyphosis may limit activity,including bending and reaching.
Multiple thoracic fractures may result in restrictive lung disease,and lumbar fractures may alter abdominal anatomy, leading to constipation,abdominal pain,distention,reduced appetite,and premature satiety.Vertebral fractures,whether clinically apparent or silent,are major predictors of future fracture risk,up to5-fold for subsequent vertebral fracture and2-to3-fold for fractures at other sites.Wrist fractures are less disabling but can interfere with some activities of daily living as much as hip or vertebral fractures.
Pelvic fractures and humerus fractures are also common and contribute to increased morbidity and mortality.Fractures can also cause psychosocial symptoms,most notably depres-sion and loss of self-esteem,as patients grapple with pain, physical limitations,and lifestyle and cosmetic changes.
Economic toll
Annually,two million fractures are attributed to osteoporosis, causing more than432,000hospital admissions,almost2.5 million medical office visits,and about180,000nursing home admissions in the USA[1].Medicare currently pays for approx-imately80%of these fractures,with hip fractures accounting for 72%of fracture costs.Due in part to an aging population,the cost of care is expected to rise to$25.3billion by2025[6].
Despite the availability of cost-effective and well-tolerated treatments to reduce fracture risk,only23%of women age67 or older who have an osteoporosis-related fracture receive either a BMD test or a prescription for a drug to treat osteo-porosis in the6months after the fracture[7].
Basic pathophysiology
Bone mass in older adults equals the peak bone mass achieved by age18–25minus the amount of bone subsequently lost. Peak bone mass is determined largely by genetic factors,with contributions from nutrition,endocrine status,physical activ-ity,and health during growth[8].
The process of bone remodeling that maintains a healthy skeleton may be considered a preventive maintenance pro-gram,continually removing older bone and replacing it with new bone.Bone loss occurs when this balance is altered, resulting in greater bone removal than replacement.The
imbalance occurs with menopause and advancing age.With the onset of menopause,the rate of bone remodeling increases,magnifying the impact of the remodeling imbalance.The loss of bone tissue leads to disordered skeletal architecture and an increase in fracture risk.
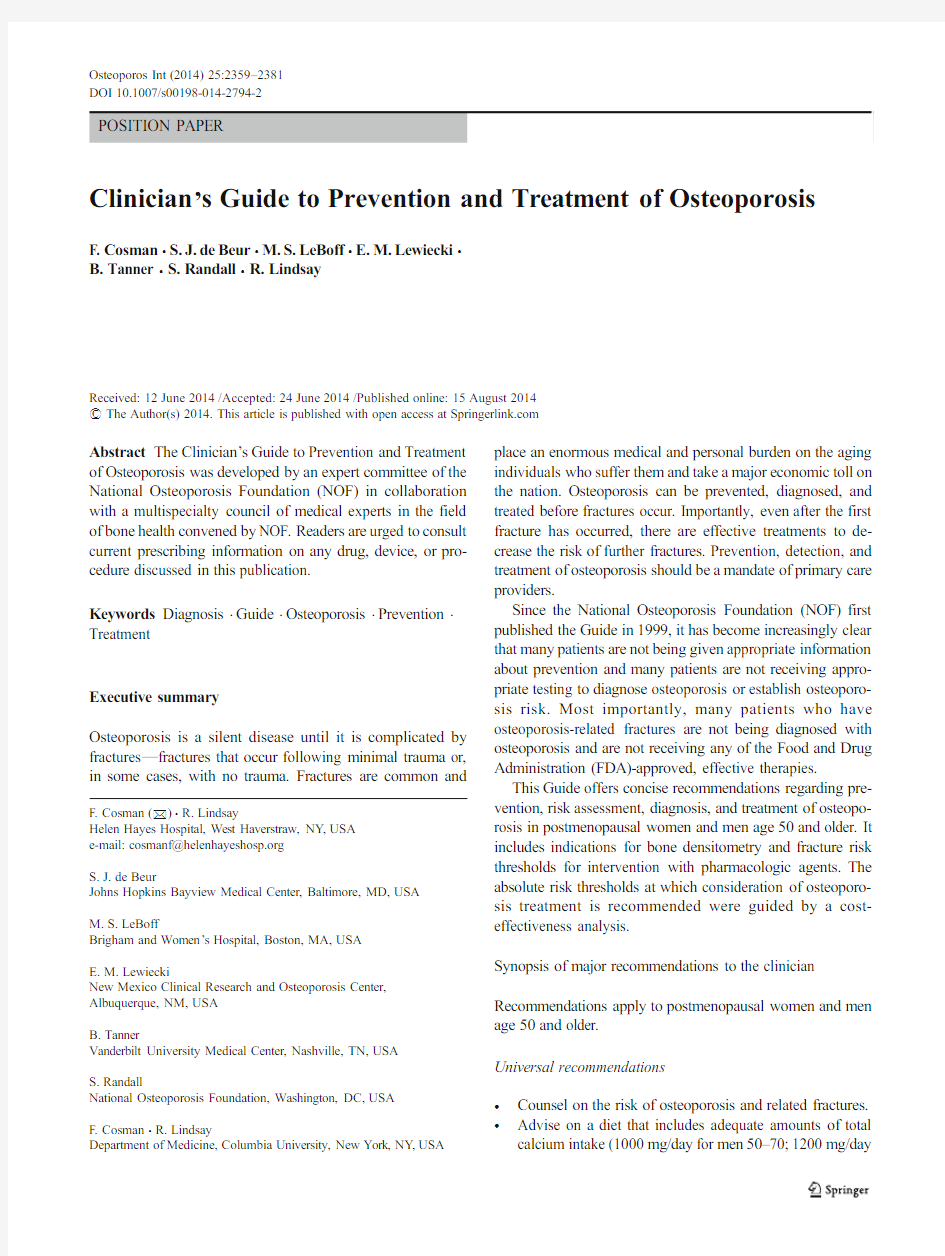
Figure 1shows the changes within cancellous bone as a consequence of bone loss.Individual trabecular plates of bone are lost,leaving an architecturally weakened structure with significantly reduced mass.Increasing evidence suggests that rapid bone remodeling (as measured by biochemical markers of bone resorption or formation)increases bone fragility and fracture risk.
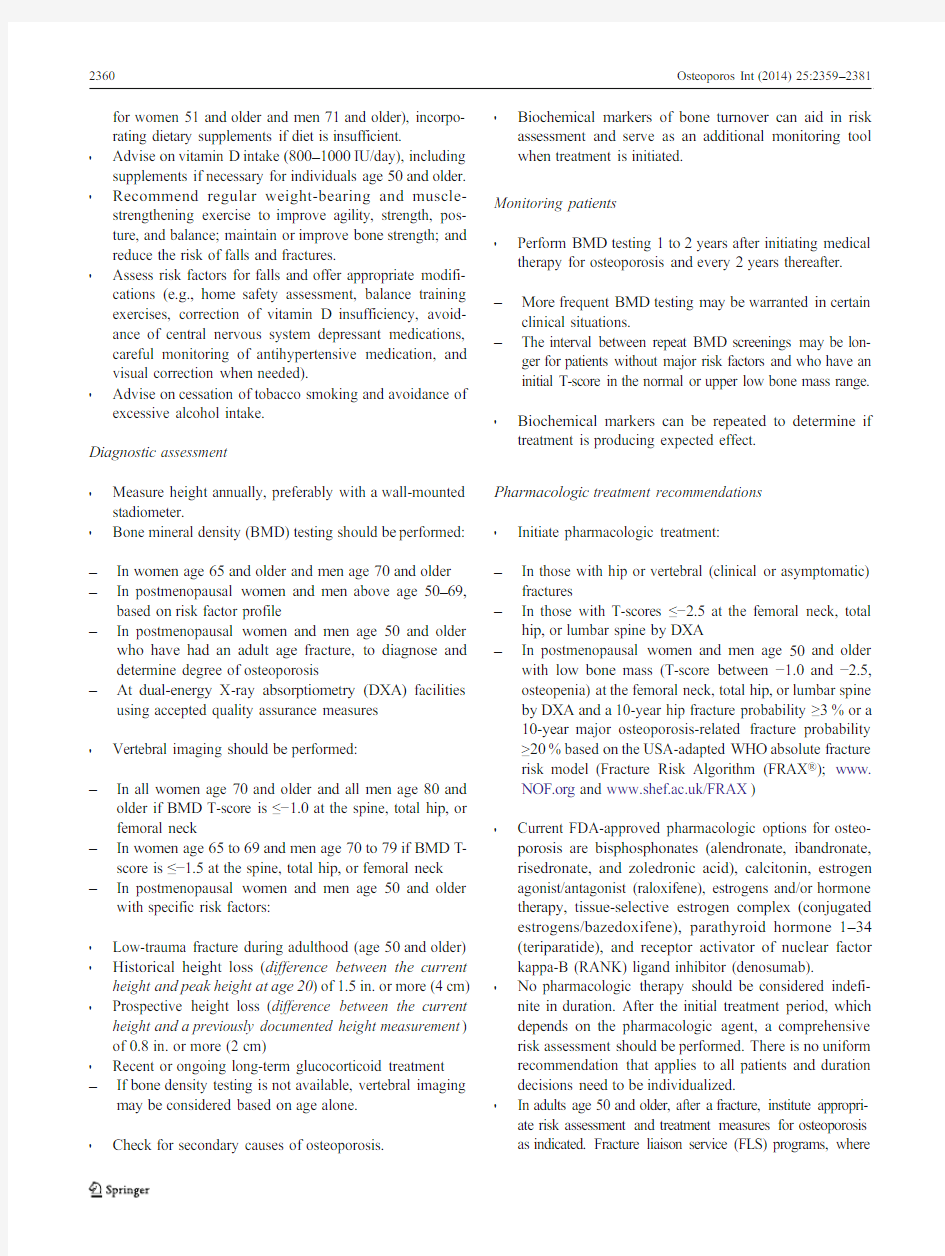
Bone loss leads to an increased risk of fracture that is magnified by other aging-associated declines in functioning.Figure 2shows the factors associated with an increased risk of osteoporosis-related fractures.These include general factors that relate to aging and sex steroid deficiency,as well as specific risk factors,such as use of glucocorticoids,which cause decreased bone formation and bone loss,reduced bone quality,and disruption of microarchitectural integrity.Frac-tures result when weakened bone is overloaded,often by falls or certain activities of daily living.
Approach to the diagnosis and management of osteoporosis
NOF recommends a comprehensive approach to the diagnosis and management of osteoporosis.A detailed history and physical examination together with BMD assessment,verte-bral imaging to diagnose vertebral fractures,and,when ap-propriate,the WHO 10-year estimated fracture probability are utilized to establish the individual patient ’s fracture risk [11].Therapeutic intervention thresholds are based on NOF ’s eco-nomic analysis that takes into consideration the cost-effectiveness of treatments and competition for resources in the USA [12,13].The clinician ’s clinical skills and past experience,incorporating the best patient-based research available,are used to determine the appropriate therapeutic intervention.The potential risks and benefits of all osteoporo-sis interventions should be reviewed with patients and the
unique concerns and expectations of individual patients con-sidered in any final therapeutic decision.Risk assessment
All postmenopausal women and men age 50and older should be evaluated for osteoporosis risk in order to determine the need for BMD testing and/or vertebral imaging.In general,the more risk factors that are present,the greater is the risk of fracture.Osteoporosis is preventable and treatable,but be-cause there are no warning signs prior to a fracture,many people are not being diagnosed in time to receive effective therapy during the early phase of the disease.Many factors have been associated with an increased risk of osteoporosis-related fracture (Table 1).
Since the majority of osteoporosis-related fractures result from falls,it is also important to evaluate risk factors for falling (Table 2).The most important of these are personal history of falling,muscle weakness and gait,selected medi-cations,balance,and visual deficits [15].Dehydration is also a risk factor for falls.
Several of these risk factors have been included in the WHO 10-year fracture risk model (Table 3).As suggested by the WHO [11],this set of risk factors increases fracture risk inde-pendently of BMD and can be combined with BMD measure-ments to assess an individual patient ’s risk of future fracture.Diagnostic assessment
Consider the possibility of osteoporosis and fracture risk based on the presence of the risk factors and conditions outlined in Tables 1and 3.Metabolic bone diseases other than osteoporosis,such as hyperparathyroidism or osteomalacia,may be associat-ed with low BMD.Many of these diseases have very specific therapies,and it is appropriate to complete a history and phys-ical examination before making a diagnosis of osteoporosis on the basis of a low BMD alone.In patients in whom a specific secondary,treatable cause of osteoporosis is being considered (Table 1),relevant blood and urine studies (see below)should be obtained prior to initiating therapy.Any adulthood fracture may be an indication of osteoporosis and should be evaluated ac-cordingly.Consider hip and vertebral fractures as indications
of
Normal bone Osteoporo?c bone
Fig.1Micrographs of normal vs.osteoporotic bone [9],from Dempster et al.,with permission of The American Society for Bone and Mineral Research [9]
osteoporosis unless excluded by the clinical evaluation and imaging.Fractures present a sense of urgency as they signify increased fracture risk over the subsequent 5years [16].Patients with recent fractures,multiple fractures,or very low BMD should be evaluated for secondary etiologies.
Osteoporosis affects a significant number of men,yet the condition often goes undetected and untreated.The evaluation of osteoporosis in men requires special consideration as some of the laboratory testing to assess underlying causes in men differs from those in women.Screening BMD and vertebral imaging recommendations for men are outlined in Table 8.The 2012Endocrine Society ’s Osteoporosis in Men:An Endocrine So-ciety Clinical Practice Guideline provides a detailed approach to the evaluation and treatment of osteoporosis in men [17].Diagnosis
The diagnosis of osteoporosis is established by measurement of BMD or by the occurrence of adulthood hip or vertebral fracture in the absence of major trauma (such as a motor vehicle accident or multiple story fall).Laboratory testing is indicated to exclude secondary causes of osteoporosis [1,14,17](Table 4).
BMD measurement and classification
DXA measurement of the hip and spine is the technology used to establish or confirm a diagnosis of osteoporosis,predict future fracture risk,and monitor patients.Areal BMD is expressed in absolute terms of grams of mineral per square centimeter scanned (g/cm 2)and as a relationship to two norms:compared to the BMD of an age-,sex-,and ethnicity-matched reference population (Z-score)or compared to a young-adult reference population of the same sex (T-score).The difference between the patient ’s BMD and the mean BMD of the reference population,divided by the stan-dard deviation (SD)of the reference population,is used to calculate T-scores and Z-scores.Peak bone mass is achieved in early adulthood,followed by a decline in BMD.The rate of bone loss accelerates in women at menopause and continues to progress at a slower pace in older postmenopausal women (see Fig.3)and in older men.An individual ’s BMD is
presented as the standard deviation above or below the mean BMD of the reference population,as outlined in Table 5.The BMD diagnosis of normal,low bone mass (osteopenia),oste-oporosis,and severe or established osteoporosis is based on the WHO diagnostic classification (Table 5)[18].
BMD testing is a vital component in the diagnosis and management of osteoporosis.BMD has been shown to corre-late with bone strength and is an excellent predictor of future fracture risk.Instead of a specific threshold,fracture risk increases exponentially as BMD decreases.Although avail-able technologies measuring central (lumbar spine and hip)and peripheral skeletal sites (forearm,heel,fingers)provide site-specific and global (overall risk at any skeletal site)as-sessment of future fracture risk,DXA measurement at the hip is the best predictor of future hip fracture risk.DXA measure-ments of the lumbar spine and hip must be performed by appropriately trained technologists on properly maintained instruments.DXA scans are associated with exposure to triv-ial amounts of radiation.
In postmenopausal women and men age 50and older,the WHO diagnostic T-score criteria (normal,low bone mass,and osteoporosis)are applied to BMD measurement by central DXA at the lumbar spine and femoral neck [18].BMD mea-sured by DXA at the one-third (33%)radius site can be used for diagnosing osteoporosis when the hip and lumbar spine cannot be measured or are unusable or uninterpretable [19].In premenopausal women,men less than 50years of age,and children,the WHO BMD diagnostic classification should not be applied.In these groups,the diagnosis of osteoporosis should not be made on the basis of densitometric criteria alone.The International Society for Clinical Densitometry (ISCD)recommends that instead of T-scores,ethnic or race-adjusted Z-scores should be used,with Z-scores of ?2.0or lower defined as either “low bone mineral density for chrono-logical age ”or “below the expected range for age ”and those above ?2.0being “within the expected range for age ”[19].Who should be tested?
The decision to perform bone density assessment should be based on an individual ’s fracture risk profile and skeletal health assessment.Utilizing any procedure to measure
bone
Fig.2Pathogenesis of
osteoporosis-related fractures,from Cooper and Melton,with modification [10]
density is not indicated unless the results will influence the patient’s treatment decision.The US Preventive Services Task Force recommends testing of all women age65and older and younger women whose fracture risk is equal to or greater than that of a65-year-old white woman who has no additional risk factors[20].
Table1Conditions,diseases,and medications that cause or contribute to osteoporosis and fractures
Lifestyle factors
Alcohol abuse Excessive thinness Excess vitamin A
Frequent falling High salt intake Immobilization
Inadequate physical activity Low calcium intake Smoking(active or passive) Vitamin D insufficiency
Genetic diseases
Cystic fibrosis Ehlers-Danlos Gaucher’s disease
Glycogen storage diseases Hemochromatosis Homocystinuria Hypophosphatasia Marfan syndrome Menkes steely hair syndrome Osteogenesis imperfecta Parental history of hip fracture Porphyria
Riley-Day syndrome
Hypogonadal states
Androgen insensitivity Anorexia nervosa Athletic amenorrhea Hyperprolactinemia Panhypopituitarism Premature menopause(<40years) Turner’s and Klinefelter’s syndromes
Endocrine disorders
Central obesity Cushing’s syndrome Diabetes mellitus(types1and2) Hyperparathyroidism Thyrotoxicosis
Gastrointestinal disorders
Celiac disease Gastric bypass Gastrointestinal surgery Inflammatory bowel disease Malabsorption Pancreatic disease
Primary biliary cirrhosis
Hematologic disorders
Hemophilia Leukemia and lymphomas Monoclonal gammopathies Multiple myeloma Sickle cell disease Systemic mastocytosis Thalassemia
Rheumatologic and autoimmune diseases
Ankylosing spondylitis Other rheumatic and autoimmune diseases
Rheumatoid arthritis Systemic lupus
Neurological and musculoskeletal risk factors
Epilepsy Multiple sclerosis Muscular dystrophy Parkinson’s disease Spinal cord injury Stroke
Miscellaneous conditions and diseases
AIDS/HIV Amyloidosis Chronic metabolic acidosis Chronic obstructive lung disease Congestive heart failure Depression
End-stage renal disease Hypercalciuria Idiopathic scoliosis
Post-transplant bone disease Sarcoidosis Weight loss
Medications
Aluminum(in antacids)Anticoagulants(heparin)Anticonvulsants
Aromatase inhibitors Barbiturates Cancer chemotherapeutic drugs
Depo-medroxyprogesterone(premenopausal contraception)Glucocorticoids(≥5mg/day prednisone or equivalent
for≥3months)
GnRH(gonadotropin-releasing
hormone)agonists
Lithium cyclosporine A and tacrolimus Methotrexate Parental nutrition
Proton pump inhibitors Selective serotonin reuptake inhibitors
Tamoxifen?(premenopausal use)Thiazolidinediones(such as Actos?and Avandia?)Thyroid hormones(in excess) From:The Surgeon General’s Report[1],with modification
Table6outlines the indications for BMD testing.BMD measurement is not recommended in children or adolescents and is not routinely indicated in healthy young men or pre-menopausal women unless there is a significant fracture his-tory or there are specific risk factors for bone loss.
Vertebral imaging
A vertebral fracture is consistent with a diagnosis of osteopo-rosis,even in the absence of a bone density diagnosis,and is an indication for pharmacologic treatment with osteoporosis medication to reduce subsequent fracture risk[18,21].Most vertebral fractures are asymptomatic when they first occur and often are undiagnosed for many years.Proactive vertebral imaging is the only way to diagnose these fractures.The finding of a previously unrecognized vertebral fracture may change the diagnostic classification,alter future fracture risk calculations,and affect treatment decisions[22].
Independent of BMD,age,and other clinical risk factors, radiographically confirmed vertebral fractures(even if completely asymptomatic)are a sign of impaired bone quality and strength and a strong predictor of new vertebral and other fractures.The presence of a single vertebral fracture increases the risk of subsequent fractures5-fold and the risk of hip and other fractures2-to3-fold[23].Vertebral imaging can be performed using a lateral thoracic and lumbar spine X-ray or lateral vertebral fracture assessment(VFA),available on most modern DXA machines.VFA can be conveniently performed at the time of BMD assessment,while conventional X-ray may require referral to a standard X-ray facility.
Table2Risk factors for falls From:Health Professional’s Guide to the Rehabilitation of the Patient with Osteoporosis[14]Environmental risk factors
Lack of assistive devices in bathrooms Obstacles in the walking path
Loose throw rugs Slippery conditions
Low level lighting
Medical risk factors
Age Medications causing sedation(narcotic
analgesics,anticonvulsants,psychotropics) Anxiety and agitation Orthostatic hypotension
Arrhythmias Poor vision
Dehydration Previous falls or fear of falling Depression Reduced problem solving or mental acuity
and diminished cognitive skills
Vitamin D insufficiency[serum25-hydroxyvitamin D
(25(OH)D)<30ng/ml(75nmol/L)]
Urgent urinary incontinence
Malnutrition
Neurological and musculoskeletal risk factors
Kyphosis Reduced proprioception
Poor balance Weak muscles/sarcopenia
Impaired transfer and mobility Deconditioning
Diseases listed in Table1
Table3Risk factors included in the WHO Fracture Risk Assess-ment Model
From:WHO Technical Report [11]Clinical risk factors included in the FRAX Tool
Current age Rheumatoid arthritis
Gender Secondary causes of osteoporosis:type1
(insulin dependent)diabetes,osteogenesis
imperfecta in adults,untreated long-standing
hyperthyroidism,hypogonadism or premature
menopause(<40years),chronic malnutrition
or malabsorption,and chronic liver disease
A prior osteoporotic fracture(including clinical
and asymptomatic vertebral fractures)
Parental history of hip fracture
Femoral neck BMD Current smoking
Low body mass index(BMI,kg/m2)Alcohol intake(3or more drinks/day)
Oral glucocorticoids≥5mg/d of prednisone
for>3months(ever)
Indications for vertebral imaging
Because vertebral fractures are so prevalent in older individ-uals and most produce no acute symptoms,vertebral imaging tests are recommended for the individuals defined in Table 7.
Once a first vertebral imaging test is done,it only needs to be repeated if prospective height loss is documented or new back pain or postural change occurs [3,24].A follow-up vertebral imaging test is also recommended in patients who are being considered for a medication holiday,since stopping medica-tion would not be recommended in patients who have recent vertebral fractures.
Biochemical markers of bone turnover
Bone remodeling (or turnover)occurs throughout life to repair fatigue damage and microfractures in bone and to maintain mineral homeostasis.Biochemical markers of bone remodel-ing [e.g.,resorption markers —serum C-telopeptide (CTX)and urinary N-telopeptide (NTX)—and formation markers —serum bone-specific alkaline phosphatase (BSAP),osteocalcin (OC),and aminoterminal propeptide of type I procollagen (PINP)]are best collected in the morning while patients are fasting.
Biochemical markers of bone turnover may [25]:&Predict risk of fracture independently of bone density in untreated patients
&Predict rapidity of bone loss in untreated patients
&Predict extent of fracture risk reduction when repeated after 3–6months of treatment with FDA-approved therapies &Predict magnitude of BMD increases with FDA-approved therapies
&
Help determine adequacy of patient compliance and per-sistence with osteoporosis therapy
&
Help determine duration of “drug holiday ”and when and if medication should be restarted.(Data are quite limited to support this use,but studies are underway.)
Use of WHO FRAX?in the USA
FRAX?was developed to calculate the 10-year probability of a hip fracture and the 10-year probability of a major osteopo-rotic fracture (defined as clinical vertebral,hip,forearm,or proximal humerus fracture),taking into account femoral neck BMD and the clinical risk factors shown in Table 3[11].The FRAX?algorithm is available at https://www.doczj.com/doc/ce17552289.html, as well as at https://www.doczj.com/doc/ce17552289.html,/FRAX .It is also available on newer DXA machines or with software upgrades that provide the FRAX?scores on the bone density report.
The WHO algorithm used in this Guide was calibrated to US fracture and mortality rates;therefore,the fracture risk figures herein are specific for the US population.Economic modeling was performed to identify the 10-year hip fracture risk above which it is cost-effective,from the societal perspec-tive,to treat with pharmacologic agents.The US-based eco-nomic modeling is described in one report [12],and the US-
Table 4Exclusion of secondary causes of osteoporosis Consider the following diagnostic studies for secondary causes of osteoporosis
Blood or serum
Complete blood count (CBC)
Chemistry levels (calcium,renal function,phosphorus,and magnesium)Liver function tests
Thyroid-stimulating hormone (TSH)+/?free T 425(OH)D
Parathyroid hormone (PTH)
Total testosterone and gonadotropin in younger men Bone turnover markers Consider in selected patients
Serum protein electrophoresis (SPEP),serum immunofixation,serum-free light chains
Tissue transglutaminase antibodies (IgA and IgG)Iron and ferritin levels Homocysteine Prolactin Tryptase Urine
24-h urinary calcium Consider in selected patients
Protein electrophoresis (UPEP)Urinary free cortisol level Urinary
histamine
Fig.3Z-and T-scores in women,from ISCD Bone Densitometry Clinician Course,Lecture 5(2008),with permission of the International Society for Clinical Densitometry
adapted WHO algorithm and its clinical application are illus-trated in a companion report[13].
The latter analyses generally confirm the previous NOF conclusion that it is cost-effective to treat individuals with a prior hip or vertebral fracture and those with a DXA femoral neck T-score≤?2.5.Previous analyses have established that a lumbar spine T-score≤?2.5also warrants treatment[26].
FRAX underestimates fracture risk in patients with recent fractures,multiple osteoporosis-related fractures,and those at increased risk for falling.FRAX?is most useful in patients with low femoral neck BMD.Utilizing FRAX?in patients with low BMD at the lumbar spine but a relatively normal BMD at the femoral neck underestimates fracture risk in these individuals.Specifically,the WHO algorithm has not been validated for the use of lumbar spine BMD.NOF recommends treatment of individuals with osteoporosis of the lumbar spine as well as the hip.
Application of US-adapted FRAX?in the USA
&FRAX?is intended for postmenopausal women and men age50and older;it is not intended for use in younger adults or children.
&The FRAX?tool has not been validated in patients cur-rently or previously treated with pharmacotherapy for osteoporosis.In such patients,clinical judgment must be exercised in interpreting FRAX?scores.Patients who
have been off osteoporosis medications for1to2years or more might be considered untreated[27].
&FRAX?can be calculated with either femoral neck BMD or total hip BMD,but,when available,femoral neck BMD is preferred.The use of BMD from nonhip sites is not recommended.
&The WHO determined that for many secondary causes of osteoporosis,fracture risk was mediated primarily through impact on BMD[28].For this reason,when femoral neck BMD is inserted into FRAX?,the secondary causes of osteoporosis button are automatically inactivated.
The therapeutic thresholds proposed in this Guide are for clinical guidance only and are not rules.All treatment decisions require clinical judgment and consideration of individual patient factors,including patient preferences,comorbidities,risk factors not captured in the FRAX?model(e.g.,frailty,falls),recent decline in bone density,and other sources of possible under-or overestimation of fracture risk by FRAX?.
The therapeutic thresholds do not preclude clinicians or patients from considering intervention strategies for those who
Table5Defining osteoporosis by BMD
WHO definition of osteoporosis based on BMD
Classification BMD T-score
Normal Within1SD of the mean level for a young-adult
reference population
T-score at?1.0and above
Low bone mass(osteopenia)Between1.0and2.5SD below that of the mean l
evel for a young-adult reference population
T-score between?1.0and?2.5
Osteoporosis 2.5SD or more below that of the mean level for
a young-adult reference population
T-score at or below?2.5
Severe or established osteoporosis 2.5SD or more below that of the mean level for
a young-adult reference population with fractures
T-score at or below?2.5with one or more fractures Although these definitions are necessary to establish the presence of osteoporosis,they should not be used as the sole determinant of treatment decisions
Table6Indications for BMD testing
Consider BMD testing in the following individuals:
?Women age65and older and men age70and older,regardless of clinical risk factors
?Younger postmenopausal women,women in the menopausal transition, and men age50to69with clinical risk factors for fracture ?Adults who have a fracture at or after age50
?Adults with a condition(e.g.,rheumatoid arthritis)or taking a medication(e.g.,glucocorticoids in a daily dose≥5mg prednisone or equivalent for≥3months)associated with low bone mass or bone loss Table7Indications for vertebral imaging
Consider vertebral imaging tests for the following individuals a:
?All women age70and older and all men age80and older if BMD T-score at the spine,total hip,or femoral neck is≤?1.0
?Women age65to69and men age70to79if BMD T-score at the spine, total hip,or femoral neck is≤?1.5
?Postmenopausal women and men age50and older with specific risk factors:
?Low-trauma fracture during adulthood(age50and older)
?Historical height loss of1.5in.or more(4cm)b
?Prospective height loss of0.8in.or more(2cm)c
?Recent or ongoing long-term glucocorticoid treatment
a If bone density testing is not available,vertebral imaging may be considered based on age alone
b Current height compared to peak height during young adulthood
c Cumulative height loss measure
d during interval medical assessment
do not have osteoporosis by BMD(WHO diagnostic criterion of T-score≤?2.5),do not meet the cut points after FRAX?,or are not at high enough risk of fracture despite low BMD. Conversely,these recommendations should not mandate treat-ment,particularly in patients with low bone mass above the osteoporosis range.Decisions to treat must still be made on a case-by-case basis.
Additional bone densitometry technologies
The following bone mass measurement technologies included in Table8are capable of predicting both site-specific and overall fracture risk.When performed according to accepted standards,these densitometric techniques are accurate and highly reproducible[19].However,T-scores from these tech-nologies cannot be used according to the WHO diagnostic classification because they are not equivalent to T-scores derived from DXA.
Universal recommendations for all patients
Several interventions to preserve bone strength can be recom-mended to the general population.These include an adequate intake of calcium and vitamin D,lifelong participation in regular weight-bearing and muscle-strengthening exercise, cessation of tobacco use,identification and treatment of alco-holism,and treatment of risk factors for falling.
Adequate intake of calcium and vitamin D
Advise all individuals to obtain an adequate intake of dietary calcium.Providing adequate daily calcium and vitamin D is a
safe and inexpensive way to help reduce fracture risk.Con-trolled clinical trials have demonstrated that the combination of supplemental calcium and vitamin D can reduce the risk of fracture[29].A balanced diet rich in low-fat dairy products, fruits,and vegetables provides calcium as well as numerous nutrients needed for good health.If adequate dietary calcium cannot be obtained,dietary supplementation is indicated up to the recommended daily intake.
Lifelong adequate calcium intake is necessary for the ac-quisition of peak bone mass and subsequent maintenance of bone health.The skeleton contains99%of the body’s calcium stores;when the exogenous supply is inadequate,bone tissue is resorbed from the skeleton to maintain serum calcium at a constant level.
NOF supports Institute of Medicine(IOM)recommenda-tions that men age50–70consume1000mg/day of calcium and that women age51and older and men age71and older consume1200mg/day of calcium[30].There is no evidence that calcium intake in excess of these amounts confers additional bone strength.Intakes in excess of1200to 1500mg/day may increase the risk of developing kidney stones,cardiovascular disease,and stroke.The scientific liter-ature is highly controversial in this area[31–34].
Table9illustrates a simple method for estimating the calcium content of a patient’s diet.The average daily dietary calcium intake in adults age50and older is600to700mg/ day.Increasing dietary calcium is the first-line approach,but calcium supplements should be used when an adequate die-tary intake cannot be achieved.
Vitamin D plays a major role in calcium absorption,bone health,muscle performance,balance,and risk of falling.NOF recommends an intake of800to1000international units(IU) of vitamin D per day for adults age50and older.Institute of Medicine Dietary Reference Intakes for vitamin D are600IU/ day until age70and800IU/day for adults age71years and older[30].
Chief dietary sources of vitamin D include vitamin D-fortified milk(400IU/quart,although certain products such Table8Additional bone densitometry technologies
CT-based absorptiometry:Quantitative computed tomography(QCT) measures volumetric integral,trabecular,and cortical bone density at the spine and hip and can be used to determine bone strength,whereas pQCT measures the same at the forearm or tibia.High-resolution pQCT(HR-pQCT)at the radius and tibia provides measures of volu-metric density,bone structure,and microarchitecture.In postmeno-pausal women,QCT measurement of spine trabecular BMD can predict vertebral fractures,whereas pQCT of the forearm at the ultradistal radius predicts hip but not vertebral fractures.There is insufficient evidence for fracture prediction in men.QCT and pQCT are associated with greater amounts of radiation exposure than central DXA or pDXA.
Trabecular Bone Score(TBS)is an FDA-approved technique which is available on some densitometers.It may measure the microarchitectural structure of bone tissue and may improve the ability to predict the risk of fracture.
The following technologies are often used for community-based screen-ing programs because of the portability of the equipment.Results are not equivalent to DXA and abnormal results should be confirmed by physical examination,risk assessment,and central DXA. Peripheral dual-energy x-ray absorptiometry(pDXA)measures areal bone density of the forearm,finger,or heel.Measurement by validated pDXA devices can be used to assess vertebral and overall fracture risk in postmenopausal women.There is insufficient evidence for fracture prediction in men.pDXA is associated with exposure to trivial amounts of radiation.pDXA is not appropriate for monitoring BMD after treatment.
Quantitative ultrasound densitometry(QUS)does not measure BMD directly but rather speed of sound(SOS)and/or broadband ultrasound attenuation(BUA)at the heel,tibia,patella,and other peripheral skeletal sites.A composite parameter using SOS and BUA may be used clinically.Validated heel QUS devices predict fractures in post-menopausal women(vertebral,hip,and overall fracture risk)and in men65and older(hip and nonvertebral fractures).QUS is not asso-ciated with any radiation exposure.
as soy milk are not always supplemented with vitamin D),some fortified juices and cereals(40to50IU/serving or more),salt water fish,and liver.Some calcium supplements and most multivitamin tablets also contain vitamin D.Supplementation with vitamin D2(ergocalciferol)or vitamin D3(cholecalciferol) may be used.Vitamin D2is derived from plant sources and may be used by individuals on a strict vegetarian diet.
Many older patients are at high risk for vitamin D deficien-cy,including patients with malabsorption(e.g.,celiac disease) or other intestinal diseases(e.g.,inflammatory bowel disease, gastric bypass surgery),chronic renal insufficiency,patients on medications that increase the breakdown of vitamin D (e.g.,some antiseizure drugs),housebound patients,chroni-cally ill patients and others with limited sun exposure,indi-viduals with very dark skin,and obese individuals.There is also a high prevalence of vitamin D deficiency in patients with osteoporosis,especially those with hip fractures,even in pa-tients taking osteoporosis medications[35,36].
Since vitamin D intakes required to correct vitamin D deficiency are so variable among individuals,serum 25(OH)D levels should be measured in patients at risk of deficiency.Vitamin D supplements should be recommended in amounts sufficient to bring the serum25(OH)D level to approximately30ng/ml(75nmol/L)and a maintenance dose recommended to maintain this level,particularly for individ-uals with osteoporosis.Many patients with osteoporosis will need more than the general recommendation of800–1000IU/ day.The safe upper limit for vitamin D intake for the general adult population was increased to4000IU/day in2010[30].
Treatment of vitamin D deficiency
Adults who are vitamin D deficient may be treated with 50,000IU of vitamin D2or vitamin D3once a week or the equivalent daily dose(7000IU vitamin D2or vitamin D3)for 8–12weeks to achieve a25(OH)D blood level of approximately30ng/ml.This regimen should be followed by maintenance therapy of1500–2000IU/day or whatever dose is needed to maintain the target blood level[37,38].Regular weight-bearing and muscle-strengthening exercise Recommend regular weight-bearing and muscle-strengthening exercise to reduce the risk of falls and fractures [39–42].Among the many health benefits,weight-bearing and muscle-strengthening exercise can improve agility,strength, posture,and balance,which may reduce the risk of falls.In addition,exercise may modestly increase bone density.NOF strongly endorses lifelong physical activity at all ages,both for osteoporosis prevention and overall health,as the benefits of exercise are lost when people stop exercising.
Weight-bearing exercise(in which bones and muscles work against gravity as the feet and legs bear the body’s weight) includes walking,jogging,Tai Chi,stair climbing,dancing, and tennis.Muscle-strengthening exercise includes weight training and other resistive exercises,such as yoga,Pilates, and boot camp programs.Before an individual with osteopo-rosis initiates a new vigorous exercise program,such as run-ning or heavy weight-lifting,a clinician’s evaluation is appropriate.
Fall prevention
Major risk factors for falling are shown in Table2.In addition to maintaining adequate vitamin D levels and physical activity,as described above,several strategies have been demonstrated to reduce falls.These include, but are not limited to,multifactorial interventions such as individual risk assessment,Tai Chi and other exercise programs,home safety assessment,and modification especially when done by an occupational therapist,and gradual withdrawal of psychotropic medication if possi-ble.Appropriate correction of visual impairment may improve mobility and reduce risk of falls.
There is a lack of evidence that the use of hip protectors by community-dwelling adults provides statistically significant reduction in the risk of hip or pelvis fractures.Also,there is no evidence that the use of hip protectors reduces the rate of falls. In long-term care or residential care settings,some studies
Table9Estimating daily dietary calcium intake
Step1:Estimate calcium intake from calcium-rich foods a
Product#of servings/day Estimated calcium/serving,in mg Calcium in mg
Milk(8oz.)__________×300=__________
Yogurt(6oz.)__________×300=__________
Cheese(1oz.or1cubic in.)__________×200=__________
Fortified foods or juices__________×80to1,000b=__________
Subtotal=__________
Step2:Add250mg for nondairy sources to subtotal above+250
Total calcium,in mg=__________
a About75to80%of the calcium consumed in American diets is from dairy products
b Calcium content of fortified foods varies
have shown a marginally significant reduction in hip fracture risk.There are no serious adverse effects of hip protectors; however,adherence to long-term use is poor[43].There is additional uncertainty as to which hip protector to use,as most of the marketed products have not been tested in randomized clinical trials.
Cessation of tobacco use and avoidance of excessive alcohol intake
Advise patients to stop tobacco smoking.The use of tobacco products is detrimental to the skeleton as well as to overall health[44–47].NOF strongly encourages a smoking cessation program as an osteoporosis intervention.
Recognize and treat patients with excessive alcohol intake. Moderate alcohol intake has no known negative effect on bone and may even be associated with slightly higher bone density and lower risk of fracture in postmenopausal women. However,alcohol intake of more than two drinks per day for women or three drinks a day for men may be detrimental to bone health,increases the risk of falling,and requires further evaluation for possible alcoholism[48].
Pharmacologic therapy
All patients being considered for treatment of osteoporosis should also be counseled on risk factor reduction including the importance of calcium,vitamin D,and exercise as part of any treatment program for osteoporosis.Prior to initiating treat-ment,patients should be evaluated for secondary causes of osteoporosis and have BMD measurements by central DXA, when available,and vertebral imaging studies when appropri-ate.Biochemical marker levels should be obtained if monitor-ing of treatment effects is planned.An approach to the clinical assessment of individuals with osteoporosis is outlined in Table10.
The percentage of risk reductions for vertebral and nonvertebral fractures cited below are those cited in the FDA-approved prescribing information.In the absence of
head-to-head trials,direct comparisons of risk reduction among drugs should be avoided.
Who should be considered for treatment? Postmenopausal women and men age50and older presenting with the following should be considered for treatment:
&A hip or vertebral fracture(clinically apparent or found on vertebral imaging).There are abundant data that patients with spine and hip fractures will have reduced fracture risk if treated with pharmacologic therapy.This is true for
fracture patients with BMD in both the low bone mass and osteoporosis range[49–58].In patients with a hip or spine fracture,the T-score is not as important as the fracture itself in predicting future risk of fracture and antifracture efficacy from treatment.
&T-score≤?2.5at the femoral neck,total hip,or lumbar spine.There is abundant evidence that the elevated risk of fracture in patients with osteoporosis by BMD is reduced with pharmacotherapy[52,57,59–70].
&Low bone mass(T-score between?1.0and?2.5at the femoral neck or lumbar spine)and a10-year probability of
a hip fracture≥3%or a10-year probability of a major Table10Clinical approach to managing osteoporosis in postmenopaus-al women and men age50and older
General principles:
?Obtain a detailed patient history pertaining to clinical risk factors for osteoporosis-related fractures and falls
?Perform physical examination and obtain diagnostic studies to
evaluate for signs of osteoporosis and its secondary causes ?Modify diet/supplements,lifestyle,and other modifiable clinical risk factors for fracture
?Estimate patient’s10-year probability of hip and any major
osteoporosis-related fracture using the US-adapted FRAX and per-form vertebral imaging when appropriate to complete risk assessment ?Decisions on whom to treat and how to treat should be based on
clinical judgment using this Guide and all available clinical
information
Consider FDA-approved medical therapies based on the following:?Vertebral fracture(clinical or asymptomatic)or hip fracture ?Hip DXA(femoral neck or total hip)or lumbar spine T-score≤?2.5?Low bone mass(osteopenia)and a US-adapted WHO10-year
probability of a hip fracture≥3%or10-year probability of any major osteoporosis-related fracture≥20%
?Patient preferences may indicate treatment for people with10-year fracture probabilities above or below these levels
Consider nonmedical therapeutic interventions:
?Modify risk factors related to falling
?Referrals for physical and/or occupational therapy evaluation(e.g., walking aids and other assistive devices)
?Weight-bearing,muscle-strengthening exercise,and balance training Follow-up:
?Patients not requiring medical therapies at the time of initial
evaluation should be clinically re-evaluated when medically appro-priate
?Patients taking FDA-approved medications should have laboratory and bone density re-evaluation after2years or more frequently when medically appropriate
?Vertebral imaging should be repeated if there is documented height loss,new back pain,postural change,or suspicious finding on chest X-ray,following the last(or first)vertebral imaging test or in patients being considered for a temporary cessation of drug therapy to make sure no new vertebral fractures have occurred in the interval ?Regularly,and at least annually,assess compliance and persistence with the therapeutic regimen
osteoporosis-related fracture≥20%based on the US-adapted WHO algorithm[13,15,71,72].
Although FRAX calculated fracture risk prediction has been confirmed in multiple studies,there are relatively few data confirming fracture risk reductions with pharmacothera-py in this group of patients.
US FDA-approved drugs for osteoporosis
Current FDA-approved pharmacologic options for the preven-tion and/or treatment of postmenopausal osteoporosis include, in alphabetical order:bisphosphonates(alendronate, alendronate plus D,ibandronate,risedronate and zoledronic acid),calcitonin,estrogens(estrogen and/or hormone thera-py),estrogen agonist/antagonist(raloxifene),tissue-selective estrogen complex(conjugated estrogens/bazedoxifene),para-thyroid hormone(PTH[1–34],teriparatide),and the receptor activator of nuclear factor kappa-B(RANK)ligand(RANKL) inhibitor denosumab.Please see prescribing information for specific details of their use.
The antifracture benefits of FDA-approved drugs have mostly been studied in women with postmenopausal osteopo-rosis.There are limited fracture data in glucocorticoid-induced osteoporosis and in men.FDA-approved osteoporosis treat-ments have been shown to decrease fracture risk in patients who have had fragility fractures and/or osteoporosis by DXA. Pharmacotherapy may also reduce vertebral fractures in pa-tients with low bone mass(osteopenia)without fractures,but the evidence supporting overall antifracture benefit is not as strong.Thus,the clinician should assess the potential benefits and risks of therapy in each patient and the effectiveness of a given osteoporosis treatment on reduction of vertebral and nonvertebral fractures.
Note that the intervention thresholds do not take into ac-count the nonskeletal benefits or risks associated with specific drug use.NOF does not advocate the use of drugs not ap-
proved by the FDA for prevention and treatment of osteopo-rosis.Examples of these drugs are listed in Table11for information only.
Bisphosphonates
Drug efficacy
Alendronate,brand name:Fosamax?,Fosamax Plus D, Binosto?,and generic alendronate Alendronate sodium is approved by the FDA for the prevention(5mg daily and 35mg weekly tablets)and treatment(10mg daily tablet, 70mg weekly tablet,70mg weekly tablet with2,800or 5,600IU of vitamin D3,and70mg effervescent tablet)of postmenopausal osteoporosis.Alendronate is also approved for treatment to increase bone mass in men with osteoporosis and for the treatment of osteoporosis in men and women taking glucocorticoids[73].
Alendronate reduces the incidence of spine and hip frac-tures by about50%over3years in patients with a prior vertebral fracture or in patients who have osteoporosis at the hip site[49,59].It reduces the incidence of vertebral fractures by48%over3years in patients without a prior vertebral fracture[74].
Ibandronate,brand name:Boniva?and generic ibandronate Ibandronate sodium is approved by the FDA for the treatment(150mg monthly tablet and3mg every 3months by intravenous injection)of postmenopausal osteo-porosis.Ibandronate is available as a generic preparation in the USA.The oral preparations are also approved for the prevention of postmenopausal osteoporosis.
Table11Non-FDA-approved drugs for osteoporosis
These drugs are listed for information only.Nonapproved agents include: Calcitriol:This synthetic vitamin D analogue,which promotes calcium absorption,has been approved by the FDA for managing hypocalcemia and metabolic bone disease in renal dialysis patients.It is also approved for use in hypoparathyroidism,both surgical and idiopathic,and pseudohypoparathyroidism.No reliable data demonstrate a reduction of risk for osteoporotic fracture. Genistein:An isoflavone phytoestrogen which is the main ingredient in the prescription“medical food”product Fosteum?and generally regarded as safe by the FDA.Genistein may benefit bone health in postmenopausal women but more data are needed to fully understand its effects on bone health and fracture risk.
Other bisphosphonates(etidronate,pamidronate,tiludronate):These medications vary chemically from alendronate,ibandronate, risedronate,and zoledronic acid but are in the same drug class.At this time,none is approved for prevention or treatment of osteoporosis. Most of these medications are currently approved for other conditions (e.g.,Paget’s disease,hypercalcemia of malignancy,myositis ossificans).
PTH(1-84):This medication is approved in some countries in Europe for treatment of osteoporosis in women.In one clinical study,PTH(1-84) effectively reduced the risk of vertebral fractures at a dose of100mcg/ day.
Sodium fluoride:Through a process that is still unclear,sodium fluoride stimulates the formation of new bone.The quality of bone mass thus developed is uncertain,and the evidence that fluoride reduces fracture risk is conflicting and controversial.
Strontium ranelate:This medication is approved for the treatment of osteoporosis in some countries in Europe.Strontium ranelate reduces the risk of both spine and nonvertebral fractures,but the mechanism is unclear.Incorporation of strontium into the crystal structure replacing calcium may be part of its mechanism of effect.These effects have only been documented with the pharmaceutical grade agent produced by Servier.This effect has not been studied in nutritional supplements containing strontium salts.
Tibolone:Tibolone is a tissue-specific,estrogen-like agent that may prevent bone loss and reduce menopausal symptoms.It is indicated in Europe for the treatment of vasomotor symptoms of menopause and for prevention of osteoporosis,but it is not approved for use in the USA.
Ibandronate reduces the incidence of vertebral fractures by about50%over3years,but reduction in risk of nonvertebral fracture with ibandronate has not been documented[50]. Risedronate,brand name:Actonel?,Atelvia?,and generic risedronate Risedronate sodium is approved by the FDA for the prevention and treatment(5mg daily tablet;35mg weekly tablet;35mg weekly delayed release tablet;35mg weekly tablet packaged with six tablets of500mg calcium carbonate; 75mg tablets on two consecutive days every month;and 150mg monthly tablet)of postmenopausal osteoporosis. Risedronate is also approved for treatment to increase bone mass in men with osteoporosis and for the prevention and treatment of osteoporosis in men and women who are either initiating or taking glucocorticoids[75].
Risedronate reduces the incidence of vertebral fractures by 41to49%and nonvertebral fractures by36%over3years, with significant risk reduction occurring within1year of treatment in patients with a prior vertebral fracture[51,52]. Zoledronic acid,brand name:Reclast?Zoledronic acid is approved by the FDA for the prevention and treatment(5mg by intravenous infusion over at least15min once yearly for treatment and once every2years for prevention)of osteoporosis in postmenopausal women.It is also approved to improve bone mass in men with osteoporosis and for the prevention and treatment of osteoporosis in men and women expected to be on glucocorticoid therapy for at least12months.Zoledronic acid is also indicated for the prevention of new clinical fractures in patients(both women and men)who have recently had a low-trauma(osteoporosis-related)hip fracture[58].
Zoledronic acid reduces the incidence of vertebral fractures by70%(with significant reduction at1year),hip fractures by 41%,and nonvertebral fractures by25%over3years in patients with osteoporosis defined by prevalent vertebral frac-tures and osteoporosis by BMD of the hip[66].
Drug administration
Alendronate(generic and Fosamax)and risedronate(Actonel) tablets must be taken on an empty stomach,first thing in the morning,with8oz of plain water(no other liquid).Binosto must be dissolved in4oz of room temperature water taken on an empty stomach,first thing in the morning.Delayed release risedronate(Atelvia)tablets must be taken immediately after breakfast with at least4oz of plain water(no other liquid).After taking these medications,patients must wait at least30min before eating,drinking,or taking any other medication.Patients should remain upright(sitting or standing)during this interval.
Ibandronate must be taken on an empty stomach,first thing in the morning,with8oz of plain water(no other liquid).After taking this medication,patients must remain upright and wait at least60min before eating,drinking,or taking any other medication.Ibandronate,3mg/3ml prefilled syringe,is given by intravenous injection over15to30s,once every3months. Serum creatinine should be checked before each injection.
Zoledronic acid,5mg in100ml,is given once yearly or once every2years by intravenous infusion over at least 15min.Patients should be well hydrated and may be pre-treated with acetaminophen to reduce the risk of an acute phase reaction(arthralgia,headache,myalgia,fever).These symptoms occurred in32%of patients after the first dose,7% after the second dose,and3%after the third dose.
Drug safety
Side effects are similar for all oral bisphosphonate medica-tions and include gastrointestinal problems such as difficulty swallowing and inflammation of the esophagus and stomach.
All bisphosphonates can affect renal function and are contraindicated in patients with estimated GFR below 30–35ml/min.Zoledronic acid is contraindicated in patients with creatinine clearance less than35mL/min or in patients with evidence of acute renal impairment. Healthcare professionals should screen patients prior to administering zoledronic acid in order to identify at-risk patients and should assess renal function by monitoring creatinine clearance prior to each dose of zoledronic acid[76].Eye inflammation can also occur.Any such complication should be reported to the healthcare pro-vider as soon as possible.
There have been rare reports of osteonecrosis of the jaw(ONJ)with long-term use of bisphosphonates for osteoporosis,though ONJ is much more common fol-lowing high-dose intravenous bisphosphonate treatment for patients with cancer.The risk of ONJ appears to increase with duration of treatment beyond5years [77].
Although rare,low-trauma atypical femur fractures may be associated with the long-term use of bisphosphonates(e.g.,>5years of use).Pain in the thigh or groin area,which can be bilateral,often pre-cedes these unusual fractures.Patients should be evalu-ated closely for these unusual fractures,including pro-active questioning regarding thigh and groin pain.For patients with thigh and groin pain,a stress fracture in the subtrochanteric region or femoral shaft of the femur may be present.Bilateral X-ray of the femurs should be ordered when an atypical femur fracture is suspected, followed by an MRI or a radionuclide bone scan when clinical suspicion is high enough[78].Surgical fixation is required in some cases,whereas medical conservative treatment is appropriate in other cases.Bisphosphonates should be stopped if atypical femur fractures have occurred.
Calcitonin
Drug efficacy
Brand name:Miacalcin?or Fortical?and generic calcitonin Salmon calcitonin is FDA-approved for the treat-ment of osteoporosis in women who are at least5years postmenopausal when alternative treatments are not suitable.
Miacalcin nasal spray has not been shown to increase bone mineral density in early postmenopausal women.
Calcitonin reduces vertebral fracture occurrence by about 30%in those with prior vertebral fractures but has not been shown to reduce the risk of nonvertebral fractures[54,79]. Due to the possible association between malignancy and calcitonin-salmon use,the need for continued therapy should be re-evaluated on a periodic basis.
Drug administration
Two hundred international units delivered as a single daily intranasal spray.Subcutaneous administration by injection also is available.
Drug safety
Intranasal calcitonin can cause rhinitis,epistaxis,and allergic reactions,particularly in those with a history of allergy to salmon.The FDA has reviewed long-term post-marketing data concerning calcitonin and the very small increase in the risk of certain cancers.A meta-analysis of21randomized, controlled clinical trials with calcitonin-salmon(nasal spray and investigational oral forms)suggests an increased risk of malignancies in calcitonin-salmon-treated patients compared to placebo-treated patients.The overall incidence of malig-nancies reported in the21trials was higher among calcitonin-salmon-treated patients(4.1%)compared with placebo-treated patients(2.9%).The data were not sufficient for further analyses by specific type of malignancy.Although a definitive causal relationship between the calcitonin-salmon use and malignancies cannot be established from this meta-analysis,the benefits for the individual patient should be carefully evaluated against all possible risks[80,81]. Estrogen/hormone therapy(ET/HT)
Drug efficacy
ET brand names:e.g.,Climara?,Estrace?,Estraderm?, Estratab?,Ogen?,Premarin?,Vivelle?;HT brand names: e.g.,A c t i v e l l a?,F e m h r t?,P r e m p h a s e?, Prempro?Estrogen/hormone therapy is approved by the FDA for the prevention of osteoporosis,relief of vasomotor symptoms,and vulvovaginal atrophy associated with menopause.Women who have not had a hysterectomy require HT,which also contains progestin to protect the uterine lining.
The Woman’s Health Initiative(WHI)found that5years of HT(Prempro?)reduced the risk of clinical vertebral fractures and hip fractures by34%and other osteoporotic fractures by 23%[69].
Drug administration
ET/HT is available in a wide variety of oral as well as trans-dermal preparations including estrogen only,progestin only, and combination estrogen–progestin.ET/HT dosages include cyclic,sequential,and continuous regimens.If and when treatment is stopped,bone loss can be rapid and alternative agents should be considered to maintain BMD.
Drug safety
The WHI reported increased risks of myocardial infarction, stroke,invasive breast cancer,pulmonary emboli,and deep vein thrombosis during5years of treatment with conjugated equine estrogen and medroxyprogesterone acetate (Prempro?)[69].Subsequent analyses of these data showed no increase in cardiovascular disease in women starting treat-ment within10years of menopause[82].In the estrogen only arm of WHI,no increase in breast cancer incidence was noted over7.1years of treatment.Other doses and combinations of estrogen and progestins were not studied and,in the absence of comparable data,their risks should be assumed to be comparable.Because of the risks,ET/HT should be used in the lowest effective doses for the shortest duration to treat moderately severe menopausal symptoms and should be con-sidered primarily for women within the first few years of menopause.When ET/HT use is considered solely for pre-vention of osteoporosis,the FDA recommends that approved nonestrogen treatments should first be carefully considered. When ET/HT treatments are stopped,bone loss can be rapid and alternative agents should be considered to maintain BMD. Estrogen agonist/antagonist(formerly known as SERMs): Raloxifene
Drug efficacy
Raloxifene,brand name:Evista?and generic raloxifene Raloxifene is approved by the FDA for both pre-vention and treatment of osteoporosis in postmenopausal women.
Raloxifene reduces the risk of vertebral fractures by about 30%in patients with a prior vertebral fracture and by about 55%in patients without a prior vertebral fracture over 3years[55].Reduction in risk of nonvertebral fracture with raloxifene has not been documented.Raloxifene is also
indicated for the reduction in risk of invasive breast cancer in postmenopausal women with osteoporosis[83–86].Raloxi-fene does not reduce the risk of coronary heart disease.
Drug administration
Available in a60-mg tablet form to be taken with or without food.
Drug safety
Raloxifene increases the risk of deep vein thrombosis to a degree similar to that observed with estrogen.It can also increase hot flashes and cause leg cramps.
Tissue-selective estrogen complex:conjugated
estrogens/bazedoxifene(conjugated estrogens paired
with estrogen agonist/antagonist)
Drug efficacy
Conjugated estrogens/bazedoxifene,brand name: Duavee?Conjugated estrogens/bazedoxifene is approved by the FDA for women who suffer from moderate-to-severe hot flashes(vasomotor symptoms)associated with menopause and to prevent osteoporosis after menopause.
The medication combines conjugated estrogen with an estrogen agonist/antagonist(bazedoxifene).The bazedoxifene component reduces the risk of endometrial hyperplasia(ex-cessive growth of the lining of the uterus)that can occur with the estrogen component of the drug.Therefore,progestins do not need to be taken with conjugated estrogens/bazedoxifene.
Use of this combination drug significantly increased mean lumbar spine BMD(treatment difference,1.51%),at 12months compared to placebo in women who had been postmenopausal between1and5years.Treatment with con-jugated estrogens/bazedoxifene also increased total hip BMD. The treatment difference in total hip BMD at12months was 1.21%[87–90].
Drug administration
Available as a tablet containing conjugated estrogens and bazedoxifene0.45mg/20mg,to be taken once daily without regard to meals.
Drug safety
Conjugated estrogens/bazedoxifene is intended only for post-menopausal women who still have a uterus.Like other products containing estrogen,it should be used for the shortest duration consistent with treatment goals and risks for the individual woman.When using this drug only for the prevention of osteoporosis,such use should be limited to women who are at significant risk of osteoporosis and only after carefully consider-ing alternatives that do not contain estrogen.
Side effects of conjugated estrogens/bazedoxifene include muscle spasms,nausea,diarrhea,dyspepsia,upper abdominal pain,oropharyngeal pain,dizziness,and neck pain.Because this product contains estrogen,it is approved with the same Boxed Warning and other Warnings and Precautions that have been approved with estrogen products.
Parathyroid hormone:teriparatide
Drug efficacy
PTH(1-34),teriparatide,brand name:Forteo?Teriparatide is approved by the FDA for the treatment of osteoporosis in postmenopausal women and men at high risk for fracture.It is also approved for treatment in men and women at high risk of fracture with osteoporosis associated with sustained systemic glucocorticoid therapy[91].Teriparatide reduces the risk of vertebral fractures by about65%and nonvertebral fragility fractures by about53%in patients with osteoporosis,after an average of18months of therapy[57].
Drug administration
Teriparatide is an anabolic(bone-building)agent administered by20μg daily subcutaneous injection.If and when treatment is stopped,bone loss can be rapid and alternative agents should be considered to maintain BMD.Treatment duration is recommended not to exceed18to24months.
Drug safety
Side effects of teriparatide include leg cramps,nausea,and dizziness.Because it caused an increase in the incidence of osteosarcoma in rats(high doses,long duration treatment in the rodent),patients with an increased risk of osteosarcoma(e.g., patients with Paget’s disease of bone and those having prior radiation therapy of the skeleton),bone metastases,hypercal-cemia,or a history of skeletal malignancy should not receive teriparatide therapy.It is common practice to follow teriparatide treatment with an antiresorptive agent,usually a bisphospho-nate,to maintain or further increase BMD.
RANKL/RANKL inhibitor:denosumab
Drug efficacy
Denosumab,brand name Prolia?Denosumab is approved by the FDA for the treatment of osteoporosis in postmeno-pausal women at high risk of fracture.Denosumab reduces the incidence of vertebral fractures by about68%,hip fractures
by about40%,and nonvertebral fractures by about20%over 3years[56].Denosumab is also indicated to increase bone mass in men at high risk of fracture,treat bone loss in women with breast cancer on aromatase inhibitor therapies,and to treat bone loss in men receiving gonadotropin-reducing hor-mone treatment for prostate cancer who are at high risk for fracture.
Drug administration
Administered by a health professional,60mg every6months as a subcutaneous injection.
Drug safety
Denosumab may cause hypocalcemia.Hypocalcemia must be corrected before starting denosumab.Denosumab increased the risk of serious skin infections(cellulitis)and skin rash. Denosumab has been rarely associated with the development of ONJ,both when used to treat osteoporosis and to treat patients with cancer(at much higher doses),although it is much more common in the latter setting.Denosumab has also been associated rarely with the development of atypical femur fractures.If and when denosumab treatment is stopped,bone loss can be rapid and alternative agents should be considered to maintain BMD.
Sequential and combination therapy
When osteoporosis is diagnosed in young individuals,choices of osteoporosis medication may change over time to take advantage of the best benefit to risk ratio at each stage of life (sequential monotherapy).For more severe osteoporosis,se-quential treatment with anabolic therapy followed by an antiresorptive agent is generally preferred to concomitant combination therapy.However,combination therapy with teriparatide and an antiresorptive can be considered in a few clinical settings in patients with very severe osteoporosis such as spine and hip fractures.There are few indications for combining two antiresorptive treatments,but such options could be considered in the short term in women who are experiencing active bone loss while on low dose HT for menopausal symptoms or raloxifene for breast cancer prevention.
Duration of treatment
No pharmacologic therapy should be considered indefinite in duration.All nonbisphosphonate medications produce tempo-rary effects that wane upon discontinuation.If these treat-ments are stopped,benefits rapidly disappear.In contrast, bisphosphonates may allow residual effects even after treat-ment discontinuation.Therefore,it may be possible to discontinue bisphosphonates and retain residual benefits against fracture at least for several years.
Evidence of efficacy beyond5years is limited,whereas rare safety concerns such as ONJ and atypical femur fractures be-come more common beyond5years[67,92].Since there is no extensive evidence base to guide treatment duration decisions, duration decisions need to be individualized[93].After the initial 3-to5-year treatment period,a comprehensive risk assessment should be performed.This should include interval clinical histo-ry,particularly with respect to intercurrent fracture history and new chronic diseases or medications,as well as height measure-ment,BMD testing,and vertebral imaging if there has been any documented height loss during the treatment period.It is reason-able to discontinue bisphosphonates after3to5years in people who appear to be at modest risk of fracture after the initial treatment period.In contrast,for those who appear to be at high risk for fracture,continued treatment with a bisphosphonate or an alternative therapy should be considered[94].
Monitoring patients
It is important to ask patients whether they are taking their medications and to encourage continued and appropriate com-pliance with their osteoporosis therapies to reduce fracture risk. It is also important to review their risk factors and encourage appropriate calcium and vitamin D intakes,exercise,fall pre-vention,and other lifestyle measures.Furthermore,the need for continued medication to treat osteoporosis should be reviewed annually.Duration of treatment must be individualized.Some patients may be able to discontinue treatment temporarily after several years of therapy,particularly after bisphosphonate ad-ministration[95,96].Other patients will need to continue treatment.If treatment is discontinued,serial monitoring should include clinical assessment for fractures,falling,any interval chronic disease occurrence and consideration of serial BMD testing,use of biochemical markers,and vertebral imaging in some patients.
Accurate yearly height measurement is a critical determi-nation of osteoporosis treatment efficacy.Patients who lose 2cm(or0.8in.)or more in height either acutely or cumula-tively should have a repeat vertebral imaging test to determine if new or additional vertebral fractures have occurred since the prior vertebral imaging test.
Serial central DXA testing is an important component of osteoporosis management.Measurements for monitoring pa-tients should be performed in accordance with medical neces-sity,expected response,and in consideration of local regula-tory requirements.NOF recommends that repeat BMD assess-ments generally agree with Medicare guidelines of every 2years but recognizes that testing more frequently may be warranted in certain clinical situations.
The following techniques may be used to monitor the effectiveness of treatment:
Central DXA Central DXA assessment of the hip or lumbar spine is the“gold standard”for serial assessment of BMD. Biological changes in bone density are small compared to the inherent error in the test itself,and interpretation of serial bone density studies depends on appreciation of the smallest change in BMD that is beyond the range of error of the test.This least significant change(LSC)varies with the specific instrument used,patient population being assessed,measurement site, technologist’s skill with patient positioning and test analysis, and the confidence intervals used[97].Changes in the BMD of less than3–6%at the hip and2–4%at the spine from test to test may be due to the precision error of the testing itself. Information on how to assess precision and calculate the LSC is available at https://www.doczj.com/doc/ce17552289.html,.
QCT V olumetric BMD of the lumbar spine can be used to monitor age-,disease,and treatment-related BMD changes in men and women.Precision of acquisition should be established by phantom data and analysis precision by re-analysis of patient data.
pDXA,pQCT,and QUS Peripheral skeletal sites do not re-spond with the same magnitude as the spine and hip to medications and thus are not appropriate for monitoring re-sponse to therapy at this time.
Biochemical markers of bone turnover Suppression of bio-chemical markers of bone turnover after3–6months of treat-ment and biochemical marker increases after1–3months of anabolic therapy have been predictive of greater BMD re-sponses and in some cases fracture risk reduction in large clinical trials.Biochemical marker changes in individuals must exceed the LSC in order to be clinically meaningful.The LSC is specific to the biomarker being utilized,which is calculated by multiplying the“precision error”of the specific biochemical marker(laboratory provided)by2.77(95%confidence level). Biological variability can be reduced by obtaining samples in the early morning after an overnight fast.Serial measurements should be made at the same time of day at the same laboratory. Vertebral imaging Once the first vertebral imaging test has been performed to determine prevalent vertebral fractures (indications above),repeat testing should be performed to identify incident vertebral fractures if there is a change in the patient’s status suggestive of new vertebral fracture,including documented prospective height loss,undiagnosed back pain, postural change,or a possible finding of new vertebral defor-mity on chest X-ray.If patients are being considered for a temporary cessation of drug therapy,vertebral imaging should be repeated to determine that no vertebral fractures have occurred in the interval off treatment.A new vertebral fracture on therapy indicates a need for more intensive or continued treatment rather than treatment cessation[95].Implementation of FLS secondary fracture prevention programs
FLS programs have been implemented successfully in a num-ber of closed and open settings over the last15years,both in the USA(including the American Orthopedic Association Own the Bone program)as well as abroad.These programs have accom-plished a reduction in secondary fracture rates as well as health care cost savings[98,99].In the USA,Kaiser Permanente’s Healthy Bones program has reduced the expected hip fracture rate by38%since1998[100];Geisinger Health System achieved$7.8million in cost savings over5years[101].
A Fracture Liaison Service is a coordinated care system headed by an FLS coordinator(a nurse practitioner,physician’s assistant,nurse,or other health professional)who ensures that individuals who suffer a fracture receive appropriate diagnosis, treatment,and support[102].The FLS uses established proto-cols to find and assess fracture patients.The program creates a population database of fracture patients and establishes a pro-cess and timeline for patient assessment and follow-up care.An FLS coordinator is frequently based in a hospital and requires support from a qualified physician or physician team. Physical medicine and rehabilitation
Physical medicine and rehabilitation can reduce disability, improve physical function,and lower the risk of subsequent falls in patients with osteoporosis.Rehabilitation and exercise are recognized means to improve function,such as activities of daily living.Psychosocial factors also strongly affect func-tional ability of the patient with osteoporosis who has already suffered fractures.
Recommendations from the Health Professional’s Guide to Rehabilitation of the Patient with Osteoporosis[14]:
&Evaluate and consider the patient’s physical and functional safety as well as psychological and social status,medical status,nutritional status,and medication use before pre-scribing a rehabilitation program.
&Evaluate the patient and her/his current medication use and consider possible interactions and risk for altered mental status.Intervene as appropriate.
&Provide training for the performance of safe movement and safe activities of daily living,including posture,trans-fers,lifting,and ambulation in populations with or at high risk for osteoporosis.Intervene as appropriate,e.g.,with prescription for assistive device for improved balance with mobility.
&Implement steps to correct underlying deficits whenever possible,i.e.,improve posture and balance and strengthen quadriceps muscles to allow a person to rise unassisted
from a chair;promote use of assistive devices to help with ambulation,balance,lifting,and reaching.
&Evaluate home environment for risk factors for falls and intervene as appropriate.
&Based on the initial condition of the patient,provide a complete exercise recommendation that includes weight-bearing aerobic activities for the skeleton,postural train-ing,progressive resistance training for muscle and bone strengthening,stretching for tight soft tissues and joints, and balance training.
&Advise patients to avoid forward bending and exercising with trunk in flexion,especially in combination with twisting.
&As long as principles of safe movement are followed, walking and daily activities,such as housework and gar-dening,are practical ways to contribute to maintenance of fitness and bone mass.Additionally,progressive resis-tance training and increased loading exercises,within the parameter of the person’s current health status,are bene-ficial for muscle and bone strength.Proper exercise may improve physical performance/function,bone mass,mus-cle strength,and balance,as well as reduce the risk of falling.
&Avoid long-term immobilization and recommend partial bed rest(with periodic sitting and ambulating)only when required and for the shortest periods possible.
&In patients with acute vertebral fractures or chronic pain after multiple vertebral fractures,the use of trunk orthoses
(e.g.,back brace,corset,posture training support devices)
may provide pain relief by reducing the loads on the fracture sites and aligning the vertebra.However,long-term bracing may lead to muscle weakness and further de-conditioning. &Effective pain management is a cornerstone in rehabilitation from vertebral fractures.Pain relief may be obtained by the use of a variety of physical,pharmacological,and behav-ioral techniques with the caveat that the benefit of pain relief should not be outweighed by the risk of side effects such as disorientation or sedation which may result in falls.
&Individuals with recent,painful vertebral fractures that fail conservative management may be candidates for interven-tions,such as kyphoplasty or vertebroplasty,when per-formed by experienced practitioners.
Conclusions and remaining questions
The Guide has focused on the prevention,diagnosis,and treatment of osteoporosis in postmenopausal women and men age50and older using the most common existing diag-nostic and treatment methods available.Many additional is-sues urgently need epidemiologic,clinical,and economic research.For example:&How can we better assess bone strength using noninvasive technologies and thus further refine or identify patients at high risk for fracture?
&Can we expand the WHO FRAX?algorithm to incorpo-rate information on lumbar spine BMD and to consider multiple fractures and recency of fractures in quantitative risk assessment.
&Can we develop a fracture risk calculator for patients who have already initiated pharmacologic therapy.
&How can children,adolescents,and young adults maxi-mize peak bone mass?
&What are the precise components(type,intensity,dura-tion,frequency)of an effective exercise program for oste-oporosis prevention and treatment?
&What should be done to identify and modify risk factors for falling,and what would be the magnitude of effect on fracture risk in a population?
&How effective are different FDA-approved treatments in preventing fractures in patients with moderately low bone mass?Do benefits exceed risks?
&What approaches are most effective in treating osteoporo-sis in disabled populations?
&How can we make the diagnosis of vertebral fractures more accurate and consistent,particularly mild fractures? &How long should antiresorptive therapies be continued, and are there long-term side effects as yet unknown?
&Are combination therapies useful and,if so,which drug combinations are best and when should they be used? &Can we identify agents or medications that will return bone mass and bone structure to normal even in those starting with severe osteoporosis?
&Should we treat patients to a certain goal and then recon-sider type and/or dose of therapy?If so,what should that goal be?
&How should therapeutic agents be sequentially prescribed in order to maximize benefits and minimize risks over the lifespan of the patient?
NOF is committed to continuing the effort to answer these and other questions related to this debilitating disease,with the goal of eliminating osteoporosis as a threat to the health of present and future generations.For additional resources on osteoporosis and bone health,visit https://www.doczj.com/doc/ce17552289.html,.
Acknowledgments The NOF acknowledges the members of the2008 Clinican’s Guide Develoment Committee,Bess Dawson-Hughes, Sundeep Khosla,L.Joseph Melton III,Anna N.A.Tosteson,Murray Favus,and Sanford Baim,and the consultants to the2014Update Committee,Karl Insogna,Douglas Kiel,Harold Rosen,and John Schousboe.
Disclosure policy It is the policy of NOF to ensure balance,indepen-dence,objectivity,and scientific rigor in all sponsored publications and programs.NOF requires disclosure of any financial interest or any other relationship that the committee members have with the manufacturer(s)of
any commercial product(s).All contributors to this publication have disclosed any real or apparent interest that may have direct bearing on the subject matter of this program.All potential conflicts have been resolved to the satisfaction of the NOF.Medication information included in this guidance follows the US FDA-approved label.
Conflicts of interest None.
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any non-commercial use,distribution,and reproduction in any medium,provided the original author(s)and the source are credited.
References
1.Office of the Surgeon General(US)(2004)Bone health and osteo-
porosis:a report of the Surgeon General.Office of the Surgeon General(US),Rockville(MD).Available from:http://www.ncbi.
https://www.doczj.com/doc/ce17552289.html,/books/NBK45513/.Accessed March2014
2.Wright NC,Looker A,Saag K,Curtis JR,Dalzell ES,Randall S,
Dawson-Hughes B(2014)The recent prevalence of osteoporosis and low bone mass based on bone mineral density at the femoral neck or lumbar spine in the United States.J Bone Miner Res.doi:
10.1002/jbmr.2269
3.Lewiecki EM,Laster AJ(2006)Clinical review:clinical applica-
tions of vertebral fracture assessment by dual-energy x-ray absorp-tiometry.J Clin Endocrinol Metab91(11):4215–4222
4.Abrahamsen B,van Staa T,Ariely R,Olson M,Cooper C(2009)
Excess mortality following hip fracture:a systematic epidemiolog-ical review.Osteoporos Int20(10):1633–1650
5.Colón-Emeric C,Kuchibhatla M,Pieper C et al(2003)The contri-
bution of hip fracture to risk of subsequent fractures:data from two longitudinal studies.Osteoporos Int11:879–883
6.Burge R,Dawson-Hughes B,Solomon DH,Wong JB,King AB,
Tosteson A(2007)Incidence and economic burden of osteoporosis-related fractures in the United States,2005–2025.J Bone Miner Res 22(3):465–475
7.National Committee for Quality Assurance.HEDIS&performance
measurement.Proposed changes to existing measure for HEDIS?1 2015:osteoporosis management in women who had a fracture (OMW).Washington,DC.Available at https://www.doczj.com/doc/ce17552289.html,/ HEDISQualityMeasurement.aspx.Accessed2March2014
8.Khosla S,Riggs BL(2005)Pathophysiology of age-related bone
loss and osteoporosis.Endocrinol Metab Clin N Am34:1015–1030 9.Dempster DW,Shane E,Horbert W,Lindsay R(1986)A simple
method for correlative light and scanning electron microscopy of human iliac crest bone biopsies:qualitative observations in normal and osteoporotic subjects.J Bone Miner Res1(1):15–21
10.Cooper C,Melton LJ3rd(1992)Epidemiology of osteoporosis.
Trends Endocrinol Metab3(6):224–229
11.Kanis JA,on behalf of the World Health Organization Scientific
Group(2007)Assessment of osteoporosis at the primary health care level.Technical Report.World Health Organization Collaborating Center for Metabolic Bone Diseases.University of Sheffield,UK 12.Tosteson ANA,Melton LJ3rd,Dawson-Hughes B,National
Osteoporosis Foundation Guide Committee et al(2008)Cost-effective osteoporosis treatment thresholds:the United States per-spective.Osteoporos Int19(4):437–447
13.Dawson-Hughes B,Tosteson ANA,Melton LJ3rd,National
Osteoporosis Foundation Guide Committee et al(2008) Implications of absolute fracture risk assessment for osteoporosis practice guidelines in the U.S.A.Osteoporos Int19(4):449–45814.National Osteoporosis Foundation(2003)Health professional’s
guide to rehabilitation of the patient with osteoporosis.National Osteoporosis Foundation,Washington,DC
15.American Geriatrics Society,British Geriatrics Society and
American Academy of Orthopaedic Surgeons Panel on Falls Prevention(2001)Guideline for the prevention of falls in older persons.J Am Geriatr Soc49:664–672
16.van den Bergh JP,van Geel TA,Geusens PP(2012)Osteoporosis,
frailty and fracture:implications for case finding and therapy.Nat Rev Rheumatol8(3):163–172
17.Watts NB,Adler RA,Bilezikian JP,Endocrine Society et al(2012)
Osteoporosis in men:an Endocrine Society clinical practice guide-line.J Clin Endocrinol Metab97(6):1802–1822.(Also available on the Endocrine Society’s website https://www.doczj.com/doc/ce17552289.html,/ guidelines/Current-Clinical-Practice-Guidelines.cfm)
18.Kanis JA,Melton LJ3rd,Christiansen C,Johnston CC,Khaltaev N
(1994)The diagnosis of osteoporosis.J Bone Miner Res9(8):1137–1141
19.International Society for Clinical Densitometry.2013Official
Positions—Adult.https://www.doczj.com/doc/ce17552289.html,/official-positions/2013-iscd-official-positions-adult/.Accessed Feb2014.
20.Nelson HD,Haney EM,Chou R,Dana T,Fu R,Bougatsos C(2010)
Screening for osteoporosis:systematic review to update the2002 US Preventive Services Task Force Recommendation.Evidence Syntheses No.77.AHRQ Publication No.10-05145-EF-1.
Agency for Healthcare Research and Quality,(US),Rockville 21.Melton LJ,Chrischilles EA,Cooper C,Lane AW,Riggs BL(2005)
How many women have osteoporosis?J Bone Miner Res20(5): 886–892
22.Lenchik L,Rogers LF,Delmas PD,Genant HK(2004)Diagnosis of
osteoporotic vertebral fractures:importance of recognition and de-scription by radiologists.Am J Roentgenol183(4):949–958
23.Ross PD,Davis JW,Epstein RS,Wasnich RD(1991)Pre-existing
fractures and bone mass predict vertebral fracture incidence in women.Ann Intern Med114(11):919–923
24.Schousboe JT,Ensrud KE,Nyman JA,Kane RL,Melton LJ3rd
(2005)Potential cost-effective use of spine radiographs to detect vertebral deformity and select osteopenic post-menopausal women for amino-bisphosphonate therapy.Osteoporos Int16(12):1883–1893
25.Burch J,Rice S,Yang H,Neilson A,Stirk L,Francis R,Holloway P,
Selby P,Craig D(2014)Systematic review of the use of bone turnover markers for monitoring the response to osteoporosis treat-ment:the secondary prevention of fractures,and primary prevention of fractures in high-risk groups.Health Technol Assess(Winchester, England)18(11):1–206
26.National Osteoporosis Foundation(2005)Physician’s guide to pre-
vention and treatment of osteoporosis.National Osteoporosis Foundation,Washington,DC
27.National Osteoporosis Foundation(NOF)and International Society
for Clinical Densitometry(ISCD).Recommendations to DXA Manufacturers for FRAX?Implementation.Available at http:// https://www.doczj.com/doc/ce17552289.html,/files/nof/public/content/resource/862/files/392.pdf.
Accessed28Jan2013
28.Kanis JA,Johnell O,Oden A,Johansson H,McCloskey E(2008)
FRAX and the assessment of fracture probability in men and wom-en from the UK.Osteoporos Int19(4):385–397
https://www.doczj.com/doc/ce17552289.html,rsen ER,Mosekilde L,Foldspang A(2004)Vitamin D and
calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents:a pragmatic population-based3-year intervention study.J Bone Miner Res19(3):370–378
30.Institute of Medicine(US)Committee to review dietary reference
intakes for vitamin D and calcium(2011).In:Ross AC,Taylor CL, Yaktine AL et al(eds)Dietary reference intakes for calcium and vitamin D.National Academies Press(US),Washington(DC).
关于文言文教学的浅略思考 语文组钱东梅文言文作为经典文学作品具有永恒的价值,尤其是我们选编入教材当中的一些名著名篇。它们跨越了古今,穿越了时空,对我们有着很重要的文学价值和意思,能够引起不同时代的读者的共鸣。而这种共鸣并非是无缘由的产生的。只有在理解文本的基础上才会产生。绝大多数的文言文本因时空的限制,古今语言的发展变化,学生在理解它们的意义和语境上产生了一定的难度,中国古代的经典文言作品,一是很多词语古今异义,一词多义,词义色彩的变化等等,导致学生很难读懂;二是因为时空的间隔,对于文本的理解需要一些知识背景,年代背景作为铺垫。而正是这些基础知识的缺乏,导致学生在学习文言文是遇到很多困难。有些学生甚至对文言文产生了厌恶心理,觉得一学习文言文就昏昏欲睡。因此,要让学生对学习文言文感兴趣,并有信心去学好文言文,就需要老师在教学过程中很好的处理好“言”的问题,只有弄懂了文章讲的是什么意思才会有学习的动力。而要让学生觉得学习文言文有意义,必然要让他从中学到一些知识,这就需要对文言文“文”的掌握。因此,教好文言文,让学生学好文言文就需要处理好“文”与“言”的关系。 在语文文言文教学中,一直存在着如何正确处理好“文”与“言”的关系这一难题。在教学过程当中,我们也想将文言文讲的生动形象,讲出风采。但是,无形当中,学生学习知识还要为了应付考试,尤其是对高中生来说极为重要的高考。所以在高考这一指挥棒下,我们老师在文言文教学的过程中有意无意的将重点偏向了“言”。而且偏向较为严重。对于一些课文,学生学完之后,老师抽出的重点也仅仅是一些文言重点实词和虚词的掌握。而对于文言文的“文”方面却很少涉及。所谓“文言文”,显而易见,既有“文”又有“言”,所谓“文”是指字词句中所蕴含的思想感情、文化底蕴等人文因素;所谓“言”是指字词句本身的意义或作用。二者都很重要,不可偏其一。离开“言”,古今汉语意义的差异导致文章无法理解;离开“文”,只剩下字词的意义,又会扼杀学生学习文言文的兴趣,将课堂变得枯燥无味。所以“文言兼顾”是非常必要的。 我觉得在文言文教学当中,既要重视“文”,又要重视“言”,在教学过程中可以通过精心的设计教案和上课思路将两者很好的融合在一起,做到“文言融合”。那么如何将文言融合了?我觉得应该在“言”的基础上深入对“文”的理解;在对“文”的掌握中巩固“言”的意义或作用。就拿《陈情表》这篇文章来举例,这篇文言文情感充沛,感情真挚,情感丰富。我们不仅要让学生掌握“闵”、“茕茕”、“吊”、“除”、“薄”、“矜”、“以”、“于”等实词虚词的意思,还应该引导学生深切的感受作者至真至诚的忠孝之情,血浓于水的亲情。从文章情感切入,提出疑问,李密是如何打动晋武帝让他暂且辞官侍奉祖母的?一下子抓住学生,从情感上激发学生学习文章的兴趣。那么接下来学生学习文言知识的积极性和主动性就会大大提高了。在弄懂“言”的基础上,通过提问如“李密非得辞官侍奉祖母的原因有哪些?”来深入理解李密至真至诚的忠孝之情。找出相关重要语句,重点解释说明,这又巩固了“言”的知识。这样“文言融合”既掌握了“言”的知识,又把握了“文”的内容,有助于提高文言文的教学效果。 学生学习文言文,除了掌握“文”和“言”之外,最好是将所学的知识运用到平时的语言运用或者写作当中。但如何运用这就需要我们对文本有着更深入的了解,因此学习文言文时,对于文言作品的时代背景和写作背景也是有必要了解,甚至是把握的。如学习《师说》,教师不仅要引导学生理解文章的大意,还要让学生了解到作者当时的写作背景。唐代仍在沿袭魏晋以来的门阀制度,贵族子弟都入弘文馆、崇文馆和国子学。他们无论学业如何,都有官可做。韩愈写《师说》的社会背景,可以从柳宗元《答韦中立论师道书》中的一段话里看出。柳宗元说:“由魏晋氏以下,人益不事师。今之世不闻有师,有,辄哗笑之,以为狂人。独韩愈奋不顾流俗,犯笑侮,收召后学,作《师说》,因抗颜而为师。世果群怪聚骂,指目
2019 年全国一级建造师执业资格考试试卷 《建设工程法规及相关知识》 一、单项选择题(共70 题,每题 1 分。每题的选项中。只有 1 个最符合题意) 1.在工程建设活动中,施工企业与建设单位形成的是() A.刑事法律关系 B.民事商事法律关系 C.社会法律关系 D.行政法律关系 【参考答案】B 在建设活动中,建设单位与施工企业之间的合同关系属于民事商事法律关系 2.不同行政法规对同一事项的新的一般规定与旧的特别规定不一致,不能确定如何适用时,由()裁决。 A.国务院 B.最高人民法院 C.国务院司法行政部门 D.全国人大常委会 【参考答案】A 【新思维解析】根据《立法法》第 85 条第2 款的规定,行政法规之间对同一事项的新的一般规定与旧的特别规定不一致,不能确定如何适用时,由国务院裁决 3.法人进行民事活动的物质基础是() A.有自己的名称 B.有自己的组织机构 C. 有必要的财产或经费D. 有自己的住所 【参考答案】C 有必要的财产和经费是法人进行民事活动的物质基础。 4.关于表见代理的说法,正确的是() A.表见代理属于无权代理,对本人不发生法律效力
B.表见代理中,由行为人和本人承担连带责任 C.表见代理对本人产生有权代理的效力 D.第三人明知行为人无代理权仍与之实施民事法律行为的,属于表见代理 【参考答案】B 表见代理是指行为人虽无权代理,但由于行为人的某些行为,造成了足以使善意相对人相信其有代理 权的表象,而与善意相对人进行的、由本人承担法律后果的代理行为。《合 同法》规定,行为人没有代理权、超越代理权或者代理权终止后以被代理人名义订立合同 相对人有理由相信行为人有代理权的,该代理行为有效。 5.关于建设工程中代理的说法,正确的是()A. 建设工程合同诉讼只能委托律师代理 B.建设工程中的代理主要是法定代理 C.建设工程中应当由本人实施的民事法律行为,不得代理 D.建设工程中为了被代理人的利益,代理人可以直接转托他人代理 【参考答案】C 《民法总则》规定,民事主体可以通过代理人实施民事法律行为。依照法律规定,当事人约定或者民事法律行为的性质,应当由本人亲自实施的民事法律行为,不得代理。代理人在代理权限内、以被代理人名义实施的民事法律行为,对被代理人发生效力。代理人不履行或者不完全履行职责,造成被代理人损害的,应当承担民事责任。代理人和相对人恶意串通,损害被代理人合法权益的,代理人和相对人应当承担连带责任。 6.建设用地使用权自()时设立 A.土地交付 B.支付出让金 C.转让 D.登记 【参考答案】D 不动产物权的设立、变更、转让消灭,应当依照法律规定登记,自记载于不动产登记薄时发生效力。经依法登记,发生效力:未经登记,不发生效力,但法律另有规定的除外。依法属于国家所有的自然资源,所有权可以不登记。当事人之间订立有关设立、变更、转让和消灭不动产物权的合同,除法律另有规定或者合同另有约定外,自合同成立时生效;未办理物权登记的,不影响合同效力。
浅谈言外之意 语言,在我们的生活中,像饮食起居一样不可或缺,是人类是最复杂最重要的交际工具。语言现象丰富复杂。语言的意义在理论上可以分为两个层次,一个是属于语义学研究的范围,研究的是语言符号以经济符号的组合与现实世界,人类经验的关系;有了这一层次的知识技能,但是在言语交际中我们往往会发现很多时候仅靠字面意思我们往往不能充分理解对方传达的意思。所以另一层次是语用义的层次,涉及语言形式与语境。语境包含物理语境,话语语境以及说话者和受话者的背景知识。进入语言交际的句子不再是孤立的语言单位,它是话语中的一个片段,反映与语境,特别是说话者相关的人类特定经验的信息。 言外之意,顾名思义就是说话或写文章没有明说而使人能体会出来的意思。在上面的三个语境中,说话者和受话者之间的背景知识是言外之意的基础言外之意是语言发展而来一种特殊的积极运用语言进行表达的一种交际方式,主要是根据日常生活常识推理,而根据推理可以得出的信息就不必在会话中出现,内容丰富,生动有趣。 言外之意这一个成语出自欧阳修《六一诗话》:“必能状难写之景,如在目前,含不尽之意,见于言外,然后为至矣。”宋·叶梦得《石林诗话》:“七言难于气象雄浑,句中有力而纡余,不失言外之意。”可见古人很早就懂得说含有言外之意的句子。中国不论绘画诗歌,都讲究一个“意境”,追求言有尽而意无穷的境界,这是文人气质水平的体现。在古诗里不胜枚举,如在《古诗十九首》里一首思妇诗“冉冉孤生竹,结根泰山阿。与君为新婚,菟丝附女萝。”菟丝是女萝都是柔弱的蔓生植物,以上四句是主人公说自己本无兄弟姐妹,犹如孤生之竹,未出嫁时依靠父母,犹如孤竹托根于泰山。出嫁之后,也不得依靠,好像以柔弱的菟丝依附着柔弱的女萝,暗指关系不牢靠。另一方面,古诗中的用典也是一种言外之意。如杜牧的《泊秦准》中“商女不知亡国恨,隔江犹唱《后庭花》”诗中的《后庭花》歌曲名,是引用的一个典故,南朝陈后主所作的《玉树后庭花》,被后人称为为“亡国之音”。诗人所处的晚唐时期正值国运衰微之际,而这些统治者不以国事为重,反而聚集于酒楼之中欣赏靡靡之音,怎能不使诗人产生历史可能重演的隐忧?所以,诗人这里是借陈后主因荒淫享乐终致亡国的历史讽刺晚唐那些醉生梦死的统治者不从中汲取教训。用典严谨,以典入诗别有意趣表达了诗人的愿望或情感,而增加词句之形象、含蓄与典雅,增加意境的内涵与深度力透纸背,掷地有声! 语言和文化密切相关。由于语言的产生可发展,人类文化才得以传承和发展,语言既是文化的载体,又是文化的真实写照。不同的语言反映了不同民族特定的文化风貌,思维方式.价值观念。语言又是一种社会现象,是社会交际需要和实践的产物。中国的和文化由来已久,我们讲求言语交际艺术,不直接表达。社会文化所决定的得体原则在日常会话中起作用。如在小辈和长辈,陌生人之间,在我们的社会中不宜直接提要求,发命令,所以常用言外之意的委婉方式表达自己的要求。我们总认为把话说得太直接不好,要委婉含蓄。但这种方式有的时候又把话说得不痛不痒,达不到说话者希望达到的效果。这已经成为一种集体无意识,有时你也说不上为什么要这样说。 在人们说话的时候的分别实施了三种行为,分别是言内行为,言外行为和言后行为。言内行为便是说出话语的行为,言外行为是说话人的话语要达到的目的
2016年一级建造师《工程法规》真题答案 一.单项选择题(共70题,每题1分。每题的备选项中,只有1个最符合题意) 1关于地方性法规批准和备案的说法,正确的是() A 设区的市的地方性法规应当报省级人大常委会备案 B 自治州的单行条例报送备案时,应当说明作出变通的情况 C 省级人大常委会的地方性法规应报全国人大常委会批准 D 自治县的单行条例由自治州人大常委会报送全国人大常委会和国务院备案 2.2015年9月15日,甲公司与丙公司订礼书面协议转让其对乙公司的30万元债权,同年9月25日甲公司将该债权转让通知了乙公司。关于该案的说法,正确的是() A 甲公司与丙公司之间的债权转让协议于2015年9月25日生效 B 丙公司自2015年9月15日起可以向乙公司主张30万元的债权 C 甲公司和乙公司就30万债务的清偿对丙公司承担连带责任 D 甲公司和丙公司之间的债权转让行为于2015年9月25日对乙公司发生效力 3.根据《立法法》,下列事项中必须由法律规定的是() A 税率的确定 B 环境保护 C 历史文化保护 D 增加施工许可证的申请条件 4.根据《环境保护法》,企业事业单位和其他生产经营者违法排放污染物受到罚款处罚,可以按日连续处罚。关于“按日连续处罚”的说法,正确的是() A 责令改正,拒不改正的,可以按原处罚数额按日连续处罚 B 是否可以按日连续处罚,与是否责令改正无关 C 责令改正,拒不改正的,可以重新确定处罚数额按日连续处罚 D 地方性法规不得增加按日处罚的违法行为的种类 5.在施工过程中,某施工企业的安全生产条件不符合国家规定,致使多人重伤,死亡。该施工企业的行为构成() A.重大责任事故罪 B.强令违章冒险作业罪 C.重大劳动安全事故罪 D.工程重大安全事故罪 6.根据《民事诉讼法》及司法解释,因建设工程施工合同纠纷提起诉讼的管辖法院为() A 工程所在地法院 B 被告所在地法院 C 原告所在地法院 D 合同签订地法院 7.根据《建筑起重机械安全监督管理规定》,关于建筑起重机械安装单位安全责任的说法,正确的是()
M1U1 托尼:呣…..好香啊。你做的比萨看上去不错。 贝蒂:谢谢!来一点尝尝? 托尼:好的。看上去不错,闻起来香喷喷的,呣,好吃。 大明:这上面是什么? 贝蒂:噢,是奶酪,想尝一块吗? 大明:啊!不用了,谢谢,我不喜欢奶酪。奶酪闻起来不新鲜,气味太大,吃起来有点酸。 贝蒂:嗯,我的巧克力饼干做好了,尝尝吧! 大明:谢谢!很甜,里面很酥软。 托尼:你是不是在做很多不同的食物啊?你看上去挺忙的! 贝蒂:是的。我做了比萨和饼干,现在我在做苹果派和蛋糕。 大明:苹果派听起来不错呢。我喜欢甜食,你知道的。我给你拿糖吧? 贝蒂:好。噢,你确定你拿的是糖吗?先尝一下,可能是盐。 大明:没拿错,是甜的,是糖。 托尼:这是什么?也是甜的。 贝蒂:是草莓酱,做蛋糕用的。 大明:太好了。每种东西都是甜丝丝的。我今天可真幸运啊! M1U2 玲玲: 你好! 谢谢你上次的来信,收到你的信真是太好了。真想马上见到你。 希望你能凭着照片在机场认出我来。我的个子比较高,留着一头金色短发,戴眼镜。为了旅行方便,我将穿牛仔裤和T恤,但我也会拿一件厚点的外套。我这里有你的照片,你非常漂亮,我想我们肯定能认出对方来! 谢谢你告诉我你的爱好,我俩的爱好非常相似!我花很多时间在学校和朋友弹奏古典音乐,我也喜欢舞曲——我喜欢跳舞。我也喜欢运动,尤其是网球。我哥哥在我们学校网球队,我为他感到非常自豪。他各方面都很优秀,而我不行。有时候考得不好,我会难过。我要更加努力。 你问我:“要来中国了,你有什么感受?”嗯,每当我要离开父母几天时,起初都会有点感伤。和陌生人一起的时候,我会很害羞,讲汉语时我会感到紧张,但是过几天就好了。当我不知道该如何正确处理事情时,心里总是难过,所以到中国和你在一起的时候,你要帮助我哟!对了,我还害怕做飞机。不过要去中国了,你不知道我有多兴奋!
理解言外之意 1、有记者问现代新加坡之父李光耀:“1997年之后香港将遭遇什么?”李光耀答道:“1998。”李光耀话语的言外之意是什么? 2、罗贯中的《三国演义》,写到晋国司马炎灭了吴国,俘虏了吴王孙皓,在接见孙皓时,司马炎说:“朕设此座久矣。” 3、自习课时,同学们都在安静地看书,李明和王玲因某一问题高声谈论起来。坐在一旁的张华笑着说:“你们俩谈论得真热烈呀!”张华的言外之意是: 4、50年代初,周总理接受美国的记者采访,随手将一支美国派克钢笔放在桌上。 记者:总理阁下,你们堂堂的中国人,为什么还要用我们美国生产的钢笔呢? 总理:提起这支笔啊,那可就话长了。这不是一支普通的笔,而是一个朝鲜朋友在朝鲜战场上得到的战利品,是作为礼物送给我的。我觉得有意义,就收下了贵国的这支笔。 (1)美国记者: (2)周总理: 5、阅读下面的材料,然后回答问题。 某单位正在召开总结大会,牛厂长表彰了厂里的科技人员。他说:“我厂的科技人员研制的新的照明系统,能节约电费将近65%以上。这项成果将为我厂带来很大的经济效益。”牛厂长讲完后,大会主持接着说:“下面欢送领导下台,请受表彰的科技人员上台。”牛厂长听了,很不自在。(1)牛厂长的话里有一个病句,请用横线在原文中标出。 (2)牛厂长听了会议主持人的话,为什么“很不自在。” 6、请根据下面情境,按要求回答 班里的“小书法家”小丽正在书写一幅参赛的书法作品。大功即将告成。毛手毛脚的小映突然凑上来碰到了她的手,一幅艺术作品立刻惨不忍睹。小丽气恼地瞪了小映一眼。小映赶忙道歉,见小丽还在气头上,又莞尔一笑,说:“微笑是人类最好看的表情。” (1)小映这句话的意思是:
2018年一建真题及答案-法规 2018法规真题及答案 、单项选择题 1关于建设活动中的民事商事法律关系的说法,正确的是()。 A.建设活动中的民事商事法律关系不是平等主体之间的关系 B.建设活动中的民事商事关系主要是非财产关系 C.惩罚性责任是建设活动中的民事商事关系的主要责任形式 D.在建设活动中,建设单位与施工企业之间的合同关系属于民事商事法律关 【答案】DP7 2.关于发的效力层级的说法,正确的是()。 A.当一般规定与特别规定不一致时,优先适用一般规定 B.地方性法规的效力高于本级地方政府规章 C.特殊情况下,法律、法规可以违背宪法 D.行政法规的法律地位仅次于宪法 【答案】BP4 3.下列法人中,属于特别法人的是()。 A.基金会法人
B.事业单位法人 C.社会团体法人 D.机关法人 【答案】DP10 4.关于表见代理的说法,正确的是()。 A.表见代理属于无权代理,对本人不发生法律效力 B本人承担表见代理产生的责任后,可以向无权代理人追偿因代理行为而遭受的损失 C.表见代理中,由行为人和本人承担连带责任 D.第三人明知行为人无代理权仍与之实施民事行为,构成表见代理
5.关于委托代理的说法,正确的是()。 A.委托代理授权必须采用书面形式 B.数人为同一事项的代理人,若无特别约定,应当分别行使代理权 C.代理人明知代理事项违法仍然实施代理行为,应与被代理人承担连带责任 D.被代理人明知代理人的代理行为违法末作反对表示,应由被代理人单独承 担责任 【答案】CP13 6.甲、乙两单位相邻,甲需经过乙的厂区道路出入,甲乙之间约定甲向乙支付定的费用。该约定中甲享有的权力是()。 A.土地承包经营权 B.地役权 C.土地使用权 D. 土地所有权 【答案】BP19 7.根据《建设工程质量管理条例》,县级以上人民政府建设行政主管部门和其他有关部门履行监督检查职责时,其有权采取的措施是()。 A.要求被检查单位提供工程质量保证金 B.进入被检查单位的施工现场进行检查 C.发现有严重影响工程质呈问时,责令停业整顿 D.调查建设单位和施工企业之间的银行往来账单 【答案】BP311 8.根据《建设工程质量管理条例》,建设工程竣工后,组织建设工程竣工验收的主体是() A.建设单位 B.建设行政主管部门
文言虚词意义和用法讲后练参考答案 文言虚词意义和用法讲后练1(“其”) 一、1第三人称的领属关系“他的”“他们的”“它的”;2—3第三人称代词“他们”“它”;4第一人称代词“我”;5指示代词“那”“那些”;6指示代词“其中的”;7表选择“是……还是”8表示推测、估计语气“恐怕、大概”;9—10表示祈使语气“应当”;11-12表示反问语气“难道、哪里”;13表示商量语气;14表示假设“假如”;19句中无实意,凑足音节;20多么 二、B(①他的②其中的③那④那⑤其中的⑥他,他们⑦我,自己⑧他,他们) ⑨大概 三、 断句:人言,蔺相如徒以其口舌之功垂于竹帛,以吾观之,则非徒口舌耳。相如观秦王无意偿赵城,则却立睨柱,秦王恐其破璧,遂许之斋戒,因得以完璧归赵,其仅口舌哉?若与庸人议之,其必曰:“吾其与之。”焉敢如此? (1)代词,可译为他的;(2)代词,作主谓短语中的小主语,可译为他;(3)副词,表示反问语气,可译为难道;(4)副词,表示商量语气,可译为还是;(5)指示代词,可译为那;(6)副词,表示推测语气,可译为大概;(7)副词,表示祈使语气,可译为一定;(8)代词,可译为其中;(9)连词,表示选择关系,可译为是……还是;(10)连词,表示假设关系,可译为如果;(11)助词,补足音节,可译为不译;(12)代词,可译为我,自己。 文言虚词意义和用法讲后练2(“之”) 一、1—2动词“到……去”;3—7第三人称代词“他”“它”“他们”“它们”;8—9指示代词“这”;10—12用在定语和中心语中间“的”;13用在中心语和补语中间;14—15用在主谓之间,取消句子独立性;16用在时间副词后,补足音节;17—19定语后置的标志;20—21宾语提前的标志。 二、BF(A这B助词,提前宾语C往,到……去D助词,得E取独F助词,提前宾语) 三、 断句:一僧欲之南海,询于唐僧,唐僧不之应。久之,此僧以箪食瓢饮之助至南海,夸之于唐僧:“此何难之有?”唐僧曰:“汝之百折不挠,实可钦佩。然汝之言亦过矣,君将骄而笑之乎?” 1、动词,可译为到、往
2011-2013年全国一级建造师历年真题 法规及相关知识
C?施工企业质量管理人员 D.质量监督部门 2011年全国一级建造师执业资格考试《建设工程法规与相关知识》试卷 一、单项选择题(共70题,每题1分,每题的备选项中,只有1个最符合题意) 1.不同行政法规对同一事项的规定,新的一般规定与旧的特别规定不一致,不能确定如何适用时,由( )裁决。 A.国务院主管部门 B.最高人民法院 C.国务院 D.全国人大常委会 2.某施工设备经销商规定其业务员按合同价5%提取奖金。业务员王某在与施工企业洽谈时提出,合同定价遵守公司规定, 但王某本人按每台50元补贴施工企业。施工企业表示同意,遂与王某签订了订货合同,并将获得的补贴款入账。王某 行为的法律定性是()。 A.合法行为 B.无权代理 C.不正当竞争 D.滥用代理权 3.被代理人因为向代理人授权不明确而给第三人造成的损失,应()。 A.由被代理人向第三人承担责任,代理人承担连带责任 B.由被代理人独自向第三人承担责任 C.由第三人自己承担损失 D.由代理人独自向第三人承担责任 4.施工企业以自有的房产作抵押,向银行借款100万元,后来施工企业无力还贷,经诉讼后其抵押房产被拍卖,拍得的 价款为150万元,贷款的利息及违约金为20万元,实现抵押权的费用为10万元,则拍卖后应返还施工企业的款项为 ()万元。 A.10 B.20 C.30 D.50 5.建设单位需要使用相邻企业的场地开辟道路就近运输建筑材料。经双方订立合同,约定建设单位向该企业支付用地费 用,该企业向建设单位提供场地。在此合同中,建设单位拥有的权利是()。 A.相邻权 B.地役权 C.土地出租权 D.建设用地使用权 6.施工企业购买材料设备后交付承运人运输,未按约定给付承运费用时,承运人有权扣留足以清偿其所欠运费的货 物,承运人行使的是()。 A.抵押权 B.质权 C.留置权 D.所有权 7.在建工程的建筑物、构筑物或者其他设施倒塌造成他人损害的,由建设单位与施工企业承担连带责任。该责任在债 的产生根据中属于()之债。 A.侵权 B.合同 C.无因管理 D.不当得利 8.施工人员对涉及结构安全的试块、试件以及有关材料,应当在()的监督下现场取样,并送具有相应资质等级的质量 检测单位进行检测。 A.建设单位或工程监理单位 B.施工项目技术负责人 9.因企业分立而新设立的建筑业企业,其资质等级应按()。 A.原企业的资质等级确定 B.降低一级原企业的资质等级确定 C.最低资质等级核定 D.实际达到的资质条件核定 10.2011年2月,下列人员向所在单位提出订立无固定期限劳动合同,所在单位不同意,其中不满足订立无固定期限 劳动合同法定条件的是()。 A.赵先生2010年1月入职丁企业后,该企业在2010年11月才与之签订书面劳动合同 B.张女士于1991年1月份到甲企业后一直在该企业工作 C.王先生于1989年进入乙国有企业工作,2008年3月,该企业改制,王先生已年满50岁 D.李女士已经连续与丙企业签订两次固定期限劳动合同,再次续订劳动合同时,该企业将李女士提升为市场部部长 11.根据相关法律规定,建设工程总承包单位完工后向建设单位出具质量保修书的时间为() A.竣工验收合格后 B.提交竣工验收报告时 C.竣工验收时 D.交付使用时 12.某建设工程施工项目招标文件要求中标人提交履约担保,中标人拒绝提交,则应()。 A.按中标无效处理 B.视为放弃投标 C.按废标处理 D.视为放弃中标项目 13.王某的日工资为80元。政府规定2010年10月1日至7日放假7天,其中3天属于法定休假日,4天属于前后两周的 周末休息日。公司安排王某在这7天加班不能安排补休。公司应当向王某支付加班费合计()元。 A.560 B.1360 C.800 D.1120 14.对于土方开挖工程,施工企业编制专项施工方案后,经()签字后实施。 A.施工企业项目经理、现场监理工程师 B.施工企业技术负责人、建设单位负责人 C.施工企业技术负责人、总监理工程师 D.建设单位负责人、总监理工程师 15.当分包工程发生安全事故给建设单位造成损失时,关于责任承担的说法,正确的是()。 A.建设单位可以要求分包单位和总承包单位承担无限连带责任
2004年一级建造师建设工程法规及相关知识真题及答案 一、单项选择题(共70题,每题1分。每题的备选项中,只有一个最符合题意) 1-级建造师执业资格的注册管理机构是( )。 A .省级建设行政主管部门 B .人事部或其授权机构 C .建设行业协会 D .建设部或其授权机构 2 )。 A .担任建设工程项目施工的项目经理 B .担任建设工程项目评估人员 C .从事建设工程项目咨询工作 D .从事建设工程项目预算工作 3事人意思表示真实是指行为人( )。 A .言行要有法律根据 B .作出承诺 C .语言规范 D .表现于外部的表示与其内在的真实意志相一致 4 )。 A .因法定事由的出现,权利人不能行使请求权的,诉讼时效中止 B .因原告起诉,诉讼时效中止 C .因被告应诉,诉讼时效中止 D .因证人要求,诉讼时效中止 5 应按( )顺序办理相应手续。 A .工程发包--报建登记--签订施工承包合同--申领施工许可证 B .报建登记--申领施工许可证--工程发包--签订施工承包合同 C .申领施工许可证--工程发包--签订施工承包合同--报建登记 D .报建登记--工程发包--签订施工承包合同--申领施工许可证 6.从事建筑活动的经济组织应当具备的条件是符合国家规定的( )。 A .注册资本.专业技术人员和技术装备 B .流动资金.专业技术人员和突出业绩 C .注册资本.专业管理人员并依法设立 D .流动资金.专业管理人员和资格证书 7.施工总承包单位与分包单位依法签订了"幕墙工程分包协议",在建设单位组织竣工验收时发现幕墙工程质量不合格。下列表述正确的是( )。 A .分包单位就全部工程对建设单位承担法律责任 B .分包单位可以不承担法律责任 C .总包单应就分包工程对建设单位承担全部法律责任 D .总包单位和分包单位就分包工程对建设单位承担连带责任。 8.下列各项,符合《建筑法》建设工程监理规定的是( )。 A .工程监理单位代理建设单位利益执行监理任务 B .工程监理人员发现工程施工不符合工程建设强制性标准的,有权要求施工单位整改 C .工程监理人员发现工程设计不符合工程建设强制性标准的,有权要求设计单位整改 D .工程监理单位可以转让工程监理业务 9.建设工程实施监理前,( )应当将委托的工程监理单位.监理权限等事项,书面通知被监理的建筑施工企业。 A .建设行政主管部门 B .行业协会 C .监理单位 D .建设单位 10.依据《工程建设项目招标范围和规模标准规定》,施工单项合同估算价( )万元人民币以上的工程建设项目,必须进行招标。 A .50 B .100 C .200 D .500 11.招标投标活动应当遵循的原则是( )。 A .公开、公平、公正和最低价中标 B .自愿、公平、公正和等价有偿 C .公开、公平、公正和诚实信用 D .自愿、公平、等价有偿和诚实信用 12.招标代理机构应当在招标人委托的范围内办理招标事宜,并遵守《招标投标法》关于( )的规定。 A .招标人 B .投标人 C .评标人 D .招标人和投标人 13.《招标投标法》规定的招标方式是( )。 A .公开招标.邀请招标和议标 B .公开招标和议标 C .邀请招标和议标 D .公开招标和邀请招标 14.投标人应当具备( )的能力。 A . 编制标底 B .组织评标 C .承担招标项目
2017年法规真题与答案 一、单项选择题 1.某施工企业与一仓储中心签订了仓储合同,合同约定:签约后一周内交付货物,届时合同生效。施工企业有权?……提取或…?提取货物,关于该仓储合同的说法,正确的是()。 A.该仓储合同签订即生效,不以交付为要件 B.如施工企业逾期提货,其有权拒绝仓储中心加收仓储费 C.该施工企业向仓储中心交付货物时合同生效 D.如施工企业提前提货,则有权要求仓储中心减收仓储费 答案:C 解析:超纲:附生效条件合同 2.根据《招标投标法实施条例》,下列情形中,属于不同投标人之间相互串通投标情形的是()。 A.约定部分投标人放弃投标或者中标 B.投标文件相互混装 C.投标文件载明的项目经理为同一人 D.委托同一单位或个人办理投标事宜 答案:A 解析:P94~95 3、关于建筑施工企业安全生产许可证的说法,正确的是()。 A.未取得安全生产许可证从事施工活动不会产生行政责任
B.申请补办安全生产许可证应当在公众媒体上声明原许可证作废 C.只有经过再次审查,安全生产许可证有效期才可能延期 D.施工企业是否具有安全生产许可证不影响施工许可证的核发 答案:B 解析:P221 4、甲建设单位拖欠乙施工企业工程款,乙发函催告甲还款。乙的催告行为在提起诉讼时产生的效果是()。 A.诉讼时效的中止 B.诉讼时效的中断 C.诉讼时效的延长 D.改变法定时效期间 答案:B 解析:P345 5、关于建设工程质量保修的说法,正确的是()。 A.不同类型的建设工程,质量保修范围不同 B.合同约定的保修期不能高于法定保修期限 C.工程的合理使用年限与施工企业的质量责任年限无关 D.建设工程保修期的起始日是工程实际竣工之日 答案:A 解析:P325 12.关于保险索赔的说法,正确的是()
跨文化交际行为的言后意义 摘要: 二十世纪七八十年代后,翻译研究开始突破传统美学和语言学的框架,从社会学、文化学的视角上讨论问题,一方面给翻译现象逐渐地钉上了“交际”理论的印记,另一方面对翻译“活动”引入了一个“跨文化”的“语境”;翻译研究者的注意力也逐渐地从语言形式的转换转向了文化内涵的转换,从而使传统的翻译“活动”变成可一种“跨文化”的交际“行为”(inter-cultural action of communication)。之后,人们的共识便是:离开了语言,文化便无以存附;离开了文化,语言就没有“意义”。本文要讨论的问题是:如果离开了对两种语言和文化“差异”的反映,翻译还有没有太多的实际意义? 关键词:言内意义言外意义言后意义跨文化 Perlocutionary Meaning With the Background of Intercultural Communication Abstract: Through the processing of language using, there exists two meanings commonly, locutionary meaning and illocutionary meaning. With the study of translation criteria, perlocutionary meaning is a more important element from the perspective of message receiver. In this paper, two aspects are stated. Firstly, how to deal with the message-expressing through i ntercultural communication. Secondly, perlocutionary meaning makes translator’s work is effectual or not. Only if perlocutionary meaning exists, the translator’s work is meaningful, and message is expressed successfully. Keywords: locutionary meaning, illocutionary meaning, perlocutionary meaning, intercultural communication 一言后意义的提出 1.1 言后意义 二十世纪七八十年代起,翻译研究便被引入了一个“跨文化和跨科学”的立体语境中,翻译的
2014一级建造师考试真题及参考答案 《建设工程法规及相关知识》 一、单选题(共70题,每题1分,每题的备选项中,只有一个最符合题意)。 1.下列仲裁协议约定的内容中,属于有效条款的是()。 A.仲裁协议约定两个仲裁机构,且当事人不能就仲裁机构选择达成一致 B.双方因履行合同发生纠纷向北京仲裁委员会申请仲裁 C.当事人约定争议可以向仲裁机构中申请仲裁也可以向人民法院起诉 D.劳动合同约定发生劳动争议向北京仲裁委员会申请仲裁 2.关于法人的说法,正确的是()。 A.法人以其登记注册地为住所 B.企业法人自取的营业执照时起取得法人资格 C.非企业法人是指行政法人和事业法人 D.建设单位可以是没有法人资格的其他组织 3.根据《著作权法》,著作权是()。 A.随作品的发表而自动产生 B.随作品的创作完成而自动产生 C.在作品上加注版权标记后自动产生 D.在作品以一定的物质形态固定后产生 4.关于环境保护设施竣工验收的说法,正确的是()。 A.环境保护设施未经竣工验收,主体工程投入使用的,由环境保护行政主管部门责令停止使用 B.需要进行试生产的建设项目,环境保护设施应当在投入试生产前申请竣工验收 C.分期建设、分期投入生产或者使用的建设项目,其相应的环境保护设施应当同时验收 D.建设项目投入试生产超过3个月,建设单位未申请环境保护设施竣工验收的,应当处10万元以下的罚款 5.关于民事诉讼证据的说法,正确的是()。 A.凡是知道案件情况的单位和个人,都有义务出庭作证 B.在民事诉讼中,书证可以只提交复印件 C.未经对方当事人同意私自录制的谈话资料不能作为证据使用 D.当事人对鉴定结论有异议,鉴定人可以书面答复而不必出庭作证 6.关于建设工程分包的说法,正确的有()。 A.总承包单位可以按照合同约定将全部建设工程拆分成若干部分非主体、非关键性工作分包给其他其他企业 B.总承包单位可以将全部建设工程拆分成若干部分包给其他施工企业 C.总承包单位可以将建设工程主题结构中技术较为复杂的部分分给其他企业 D.总承包单位经建设单位同意后,可以将建设工程的关键性工作分给其他企业 7.除双方当事人意思表示一致外,尚须交付标的物才能成立的合同,成为()。 A.要式合同B.实践合同 C.有偿合同D.双务合同 8.根据《民事诉讼法》,当事人申请司法确认调解协议,由双方当事人依法共同向()基层人民法院提出。
言外之意专项练习 1、李大华正在阳台上浇花,楼下的刘阿姨说:“小李,你真爱美啊,我刚晾的被单也锦上添花了。” A、你听出刘阿姨的言外之意是: B、如果你是李大华,应该这样回答刘阿姨: 答案:刘阿姨考虑邻里感情,用婉言暗示李大华浇花把自己晾晒的被子弄脏弄湿了。 2、著名电影演员李雪健因扮演焦裕禄而荣获“百花奖”最佳男主角奖。在颁奖仪式上,他说了这么一句话:“所有的苦和累都让焦裕禄受了,所有的荣誉都让—个傻小子得了。” 李雪健这句话的意思是: 答案:焦裕禄的事迹太感人,我获奖只是沾了扮演角色的光。 3、张明匆匆走进教室,习惯地用卫生纸把自己的座位擦干净,随手将纸扔在地上,同学王晓敏看见后说:“你很讲究个人卫生哩!”张明不好意思地笑了笑,说:“__________ 。”随手将纸团拾起来,扔进了教室外面的垃圾箱。 A、王晓敏的话言外之意是: B、张明该怎样说才得体? 答案:A、张明不讲究公共卫生,只顾自己。B、示例:幸亏你提醒,谢谢;我会注意的。 4、邻居说:“你家的小强真刻苦,每天夜里都十二点多了,我们还听见他在弹琴哩!”其言外之意是: 答案:小强半夜弹琴影响我们休息了。 5、一位作曲家带着自己创作的曲子向一位著名的音乐大师讨教。在听演奏的过程中,这位大师不断地脱帽。演奏完毕,作曲家连忙问道:“大师,是不是屋里太热?”大师说:“不热。我有碰到熟人就脱帽的习惯。在阁下的曲子中我碰到那么多的熟人,不得不连连脱帽。”这位大师的答话的意思是: 答案:作品重在个人的创造,不能照抄照搬别人的。 6、有两个朋友碰到了一起。第一个人说:"如果你对体操感兴趣的话,学校里有个不错的体操队。"第二人的回答:"我爬楼梯还得停下来喘几口气呢!" 他们两人的言外之意是: 答案:第一个人的言外之意是:"你想参加体操队吗?" 第二个人的言外之意是:不想参加,我身体不好。 7、有一回,马克&S226;吐温向邻居借阅一本书,邻居说:“可以,可以。但我定了一条规则:从我的图书室借去的图书必须当场阅读。”一星期后,这位邻居向马克&S226;吐温借割草机,马克&S226;吐温笑着说:“当然可以,毫无问题。不过我定了一条规则:从我家借去的割草机只能在我的草地上使用。” 马克&S226;吐温的言外之意: 答案:马克&S226;吐温的言外之意:讽刺邻居太小气,应大方地借给别人书读。
2018年一级建造师法律法规真题及答案 1.根据《民法总则》,法人分为()。 A.企业法人和非企业法人B.机关法人,企业法人和社团法人 C.一般法人和特别法人D.营利法人,非营利法人和特别法人 参考答案:D,第8页。 2.关于代理的说法,正确的是( )。 A.经被代理人同意的转代理,代理人不再承担责任 B.同一代理事项有数位代理人的,应当推选牵头人 C.作为委托人的法人、非法人组织终止的,委托代理终止 D.表见代理是有权代理 参考答案:C,第12页。 3.关于物权的说法,正确的是()。 A.同一物的担保物权人与所有权人应当为同一人B.用益物权人可以是该物的所有权人C.未经农村土地承包经营者同意,土地所有人不得在该地块设立地役 D.物权的变动只能基于合同关系 参考答案:C,第18页。 4.关于建设工程专利权保护范围的说法,正确的是( )。 A.实用新型以申请时所附的说明书为准B.建设工程发明以其附图为准 C.外观设计以在图片或照片中该产品的外观设计为准D.三类专利均以权利要求的内容为准参考答案:C,第27页。 5.关于留置的说法,正确的是( )。 A.留置权属于债权B.债权人不负责保管留置物C.建设工程合同可以适用留置权 D.留置权基于法定而产生 参考答案:D,第34页。 6.关于财产保险合同的说法,正确的是( )。 A.保险合同不可以转让B.保险人不得以诉讼方式要求投保人支付保费 C.保险合同中的危险具有损失发生的不确定性D.被保险人应当与投保人一致 参考答案:C,第35页。 7.下列法律后果中,属于民事责任承担方式的是( )。 A.解除合同B.继续履行C.罚款D.合同无效 参考答案:B,第41页。 8.根据《行政诉讼法》,下列情形中属于行政诉讼受案范围的是( )。 A.对于限制人身自由的行政强制措施不服的B.国防、外交等国家行为
2020年一建《建设工程法规》真题及答案解析 (多选题) 2014年一建《建设工程法规及相关知识》真题及答案解析 多项选择题 71.某工程已具备竣工条件,承包人在提交竣工验收报告的同时,向发包人递交竣工结算报告及完整的结算资料。关于该工程竣工验 收的质量责任等的说法,正确的有()。 A.工程质量保证金应在保修期满后返还 B.发包人要求承包人完成合同以外零星项目,承包人未在规定时间内向发包人提出施工签证的,施工后可向发包人申请费用赔偿 C.建设工程竣工时发现的质量问题或者质量缺陷,无论是建设单位的责任还是施工单位的责任,施工单位都有义务进行修复或返修 D.当事人对工程造价发生合同纠纷时,应当向仲裁机构申请仲裁或向人民法院起诉 E.承包人应当在建设工程的合理使用寿命内对地基基础工程和主体机构质量承担民事责任 【答案】CE 72.下列法律责任中,属于行政处罚的有()。 A.降低资质等级 B.罚金 C.记过 D.没收财产 E.罚款
【答案】AE 【解析】行政处罚的种类:(1)警告;(2)罚款;(3)没收违法所得,没收非法财物;(4)责令停产停业;(5)暂扣或者吊销许可证,暂扣或 者吊销执照;(6)行政拘留;(7)法律、行政法规规定的其他行政处罚。 73.下列情形中,属于我国法律规定的行政诉讼受案范围的是()。 A.对拘役不服的 B.行政机关工作人员对奖惩决定不服的 C.认为行政机关侵犯其财产权的 D.认为行政机关侵犯法律规定的经营自主权的 E.认为行政机关制定发布的具有普遍约束力的决定违法的 【答案】CD 【解析】法院不受理公民、法人或者其他组织对下列事项提起的诉讼:(1)国防、外交等国家行为;(2)行政法规、规章或者行政机关 制定、发布的具有普遍约束力的决定、命令;(3)行政机关对行政机 关工作人员的奖惩、任免等决定;(4)法律规定由行政机关最终裁决 的具体行政行为。 74.关于申请领取施工许可证的说法,正确的有()。 A.应当委托监理的工程已委托监理后才能申请领取施工许可证 B.领取施工许可证是确定建筑施工企业的前提条件 C.法律、行政法规和省、自治区、直辖市人民政府规章可以规定申请施工许可证的其他条件 D.在申请领取施工许可证之前需要楼市建设资金 E.在城市、镇规划区的建筑工程,需要同时取得建设用地规划许可证和建设工程规划许可证后,才能申请办理施工许可
言外教案 学习目标: 通过老师和同学们在堂上的共同活动,互动交流,希望能找到分析“言外之意”考题的思路,掌握此类题型的解题方法,提高答题效果。 重点以及难点:重点培养学生分析问题的能力,掌握分析题目的方法,让学生在快乐中得到快乐。 课时安排:1课时 教学过程: 一、导入:请同学们欣赏一下下面这个故事:一位著名的政治活动家进行竞选活动,他在参观精神病院时,有事儿想从医院打个电话出去,但没有打成。他暴跳如雷,冲着女接线员叫嚷起来:“姑娘,你知道我是谁?”“不知道。”接线员答道,“但我知道,你是从哪儿打来的?”接线员的言外之意:你是一位精神病人。这种话中有话的语言就是我们常说的言外之意,言外之意是口语交际的一个重点,也是我们在日常生活领域和在特定场合下经常用到的一种说话方式,更是衡量一个人在说话时的应变能力、个人的修养(或涵养)以及人格魅力的一个重要方面。近几年来,各地中考特别青睐这种题型。下面我们这一节课就来一起探讨一下,我们在考试中如何做好这些题目。 二、方法探究: 例 1 某上级主管对下属职员说:“看看你干的好事!”这位上级主管的言外之意是:“”你把事情搞得糟透了! 请你说说言外之意,你是如何看出来的? 从说话人语气语调分析,用祈使句,有斥责语气。所以我们可以根据语气不同,来判断。方法一:把握语气,领会感情 例2 某国王请阿凡提评论自己的诗,阿凡提规劝他不要再写诗了,因而被关进驴圈。后来国王又召见阿凡提看其新作,阿凡提转身就走,国王问他到哪里去,阿凡提答道:“到驴圈去,陛下!”阿凡提的言外之意是“好诗”仍不好! 请你说说言外之意,你是如何看出来的? 国王为什么要把阿凡提被关进驴圈,那是因为阿凡提说国王诗不好所以被关进驴圈由因及果。阿凡提进驴圈:结果是进了驴圈,为什么呢,还是因为国王的诗不好。由果析因方法二:查因推果,巧会意图 例3 《陈涉世家》中陈涉说:“苟富贵,无相忘。”后遭到庸者讥笑,陈涉叹息说:“燕雀安知鸿鹄之志哉!”这句话的言外之意是 请你说说言外之意,你是如何看出来的?你们怎能明白我的远大志向呢? 燕雀(喻体)------------ 你们,指庸者(本体) 鸿鹄(喻体)------------ 我,指陈涉自己(本体) 方法三:就是借用比喻 例4 李小华正在阳台上浇花,楼下的刘阿姨说:“小李,你真爱美啊,我晒的被子也锦上添花了。”你听出刘阿姨的言外之意是:你把我的被子弄脏弄湿了。 考虑到场合、对象,说话人(刘阿姨)采用了婉言来传达信息,暗示对方 方法四:联系语境,巧识婉言暗示 小结方法:(板书) 方法一:把握语气,领会感情 方法二:查因推果,巧会意图 方法三:思考喻体,巧悟本体